100. Personal and Community Services
Chapter Editor: Angela Babin
Table of Contents
Tables and Figures
Indoor Cleaning Services
Karen Messing
Barbering and Cosmetology
Laura Stock and James Cone
Laundries, Garment and Dry Cleaning
Gary S. Earnest, Lynda M. Ewers and Avima M. Ruder
Funeral Services
Mary O. Brophy and Jonathan T. Haney
Domestic Workers
Angela Babin
Case Study: Environmental Issues
Michael McCann
Click a link below to view table in article context.
1. Postures observed during dusting in a hospital
2. Dangerous chemicals used in cleaning
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Indoor Cleaning Services
General Profile
Cleaning consists of dusting, washing and polishing surfaces; washing walls; mopping, sweeping and polishing floors; as well as disposing of waste and waste water. It is done in offices, public and commercial buildings, homes and factories. It may be done in confined spaces with little ventilation and in spaces not designed with cleaning in mind. Cleaners may be independent or be employed by the enterprise which owns the facilities being cleaned, or they may work for private contractors. Those who clean may be called cleaners, housekeepers, chars, custodians or janitors, depending on the spaces cleaned and the details of the assigned tasks. For example, janitors and custodians may combine cleaning with maintenance and repair work.
Cleaners have usually worked relatively autonomously, compared to other employment categories of similar prestige. Inspection is done by supervisors, although the users of the cleaned spaces also comment on the cleaners’ work. Workers tend to order the tasks themselves and develop their own procedures (Messing, Haëntjens and Doniol-Shaw 1993). However, in commercial spaces in North America, cleaners’ routes have increasingly been determined using software programmed to take account of furniture, floor surfaces and crowding. The desired frequency of operations, area to be cleaned and time estimated for the type of area are used to calculate the total time required. Inspection may be done using a computer-programmed spot check procedure. Some of these procedures may severely underestimate the task as performed in shared space, especially if the inventory is not brought regularly up to date (Messing, Chatigny and Courville 1996).
In Canada, cleaning is the eighth most common profession of men and the tenth most common profession of women; women make up 46% of the profession (Armstrong and Armstrong 1994). In France in 1991, 229,000 cleaners worked for 9,000 cleaning companies; about a third were immigrants and 64% were women (Bretin 1994). In Denmark 85% of the 130,000 cleaners are women (Nielsen 1995). In some countries, tasks in factories and services have often been divided into “light” and “heavy”, assigned formally or informally to female and male workers respectively, who may be paid at different rates (Government of Quebec 1994). Women may dust and polish surfaces, clean bathrooms and empty wastebaskets while men sweep, mop and polish floors and carry waste to incinerators (Messing, Haëntjens and Doniol-Shaw 1993; Messing, Doniol-Shaw and Haëntjens 1993; Messing, Chatigny and Courville 1996). In other countries, men and women can be assigned to all cleaning tasks (Nielsen 1995; Hagner and Hagberg 1989). Cleaners are often relatively old compared to other workers (Bretin et al. 1992; Messing 1991; Nielsen 1995).
Risk Factors and Prevention Strategies
Cleaning may be done with hand-held tools such as brushes, brooms, rags and mops, or may be aided by machines. A variety of chemicals are used to dissolve dirt and to make surfaces appear clean and shiny. The difficulty of the task varies according to the type of surface (rough, smooth, pitted), the height and geometry of the objects cleaned, the degree of crowding of spaces and the vocations exercised in the spaces cleaned. In some places, the need for cleaning may be reduced or eliminated by design changes in the object cleaned (such as self-flushing toilets).
Musculoskeletal load
Cleaning, particularly cleaning furniture and bathrooms and emptying wastebaskets, involves rapid postural changes and many awkward and constrained postures (see table 1). Many objects must be cleaned, at a variety of heights; a typical sequence observed for dusting in a hospital room was: table (81 cm), television (196 cm), table (81 cm), telephone (81 cm), lamp (extends to 188 cm), table foot (11 cm), chair (46 cm), screen (81 cm), armchair (46 cm), window ledge (89 cm), wall sphygmomanometer (154 cm), chair legs (floor to 46 cm), oxygen fixture (137 cm) (Messing, Chatigny and Courville 1995).
Table 1. Postures observed during dusting in a hospital.
|
Activity |
Duration |
Extension (%) |
Neutral (%) |
Bending <45º (%) |
Bending ≥45º (%) |
Not observable |
|
Clean nurse station |
3 m, 26 s |
— |
13.6 |
86.4 |
— |
— |
|
Waste-basket (3) |
1 m, 26 s |
— |
19.8 |
71.1 |
9.2 |
— |
|
Bath (2) |
5 m, 17 s |
2.8 |
26.6 |
63.1 |
7.5 |
— |
|
Bathroom corridor (2) |
3 m, 53 s |
6.6 |
18.6 |
71.0 |
3.8 |
0.3 |
|
Clean rooms |
8 m, 45 s |
3.7 |
29.8 |
60.1 |
2.9 |
3.5 |
|
Reception area |
3 m, 13 s |
— |
24.7 |
74.4 |
— |
0.9 |
|
Secretaries’ office |
10 m, 20 s |
3.6 |
32.0 |
59.7 |
0.3 |
4.4 |
|
Overall |
36 m, 20 s |
3.0 |
26.4 |
65.8 |
2.7 |
2.2 |
Source: Messing, Chatigny and Courville 1995.
Floor cleaning requires repeated movements (fundamental cycle time of 1 to 2 seconds in the Sogaard, Fallentin and Nielsen (1996) study) and a sustained moderate bending of the back. Constant pressure is exerted by the hands to push vacuum cleaners or buffers, tasks requiring forces near 10 kg (Messing, Chatigny and Courville 1996). Sogaard, Fallentin and Nielsen (1996) found mean back bending during floor mopping to be 28º and mean neck bending to be 51º. Hagner and Hagberg (1989) also noted static muscular loads especially at the shoulder joint. Nordin et al. (1986) found extensive forward trunk bending in a simulated janitorial task involving floor mopping. Cleaning floors and objects is usually done with repeated movements. Sogaard (1994) suggests that the sustained repetitive motions with infrequent pauses in activity may exhaust the relatively small numbers of muscle fibres involved and result in muscular disorders.
In order to clean, many objects must be moved. During 66 minutes cleaning and polishing floors, 0.7 objects had to be moved per minute, with weights up to 10 kg; during 23 minutes of dusting, 3.7 objects were moved per minute, with weights up to 2 kg (Messing, Chatigny and Courville 1995).
Winkel et al. (1983) and Hagner and Hagberg (1989) note that increasing specialization and standardization have reduced the number of opportunities to vary body movements and postures during cleaning work. It is therefore important to provide adequate break time. Formal or informal division of tasks according to sex may increase the likelihood of musculoskeletal problems by decreasing the variation in movements (Messing, Haëntjens and Doniol-Shaw 1993).
Cardiovascular load
The cardiovascular load can be quite heavy. Johansson and Ljunggren (1989) recorded the heart rate of female cleaners during office or toilet cleaning at 123 beats/minute, 65% of the maximum for their average age of 29.8 years (corresponding to about 35% of their estimated maximal oxygen uptake or VO2 max, close to that of construction workers). Swabbing or mopping resulted in similar heart rates of 122 to 127 beats/minute. Hagner and Hagberg (1989) found a high level of oxygen consumption (up to 40% of the VO2 max) among cleaners doing floor mopping under experimental conditions. Sogaard (1994) found that relative cardiovascular strain of female school cleaners measured in the workplace was 53% of the VO2 max.
To prevent musculoskeletal problems and decrease the cardiovascular load, workload should be appropriate and sufficient rest time should be allowed. Attention should be paid to ease of cleaning when spaces and procedures are being designed and when furnishings are purchased. Vacuuming requires less force if carpets are carefully laid so as not to wrinkle when the vacuum cleaner is passed. The use of adequate tools is important. For example, extendable brushes for dusting can reduce the necessity to reach or climb. Prolonged bending can be minimized if efficient chemicals and tools make it possible to clean quickly, and if cleaning is frequent enough so that dirt does not become hardened.
The common practice of reducing the rate of ventilation in buildings during the evening or night hours, when cleaning is done, reduces air quality for cleaning workers who work during these times and should be avoided. To prevent overwork in the case where cleaning is planned using purchased software, careful observation and verification should be done in order to make sure that times allotted are realistic and take into account multiple use of spaces cleaned. Inventories of rooms and objects cleaned should be updated frequently.
Procedures and apparatus for emptying wastebaskets into bins, and bins into incinerators, have been developed so that manual lifting can be avoided.
Chemicals
Chemicals can be classed as soaps, detergents, disinfectants, porcelain cleaners, scouring powders, wax removers and strippers, solvents, pesticides and drain cleaners. They may contain other ingredients such as fragrances and colouring agents. There may be surface skin contact or they may be inhaled or absorbed through the skin into the system. Damage to the skin, eyes, throat or lungs can result. The risk of exposure depends on the concentration of the chemical and how it is used. Sprays volatilize chemicals and increase exposure. Some chemicals are irritants at low concentration and corrosive at high concentration (acids, oxidizing agents or bases). Others are effective solvents or detergents which may damage the skin barrier and make it more vulnerable to other chemical agents. Still others contain metals (nickel, cobalt, chrome) or other substances which can act as allergens.
Cleaning agents are often sold at high concentrations and diluted on site for use. The common practice of using chemicals at a higher concentration than recommended, in the hope of cleaning more quickly or more efficiently, is a source of overexposure and should be remedied by proper education and by adjusting the workload. Mixing different chemicals can cause accidental intoxication or burns. Work with strong chemicals in poorly ventilated spaces can be a hazard for cleaners and should be avoided.
The Danish Product Register Data Base PROBAS contains information on 2,567 washing and cleaning agents. Of these, 70 are considered to be potentially harmful agents causing chronic or acute health damage, such as corrosives, carcinogens, reproductive toxicants, allergens and neurotoxic agents (Borglum and Hansen 1994). These agents are presented in table 2. A study of the PROBAS register found 33 contact allergens in cleaning agents (Flyvholm 1993).
Table 2. Dangerous chemicals used in cleaning.†
|
Chemical |
Health damage codes |
Other hazards |
|
Solvents |
||
|
Butylglycol |
N* |
|
|
Isopropyl benzene |
N |
|
|
Naphtha, white spirit, Stoddard solvent |
N,R |
|
|
Toluene |
N,R |
Flammable |
|
Ethanol |
R |
Flammable |
|
2-Ethoxyethanol |
N,R |
|
|
2-Methoxyethanol |
R |
|
|
1-Methyl-2-pyrrolido |
R |
|
|
Base oil, crude oil |
N |
|
|
Tetrachloroethylene |
N,R |
|
|
1,1,1-Trichloroethane |
N |
|
|
Xylene |
N,R* |
Flammable |
|
Butyldiglycol |
I |
|
|
Acids and bases |
||
|
Acetic acid |
C |
|
|
Ammonium hydroxide |
I |
Reacts with chlorine bleaches to liberate toxic gas |
|
Potassium hydroxide |
C |
|
|
Sodium carbonate |
I |
|
|
Sodium hydroxide |
C |
|
|
Phosphoric acid |
C |
|
|
Sulphuric acid |
C |
|
|
Residual monomers and impurities |
||
|
Formaldehyde |
A,K* |
|
|
Phenol |
N* |
|
|
Benzene |
K,R,N |
|
|
Acrylonitrile |
A,K |
|
|
Butylacrylate |
A |
|
|
Methylmethacrylate |
A,R |
|
|
Styrene |
R |
Flammable |
|
1-Propanol |
N |
Flammable |
|
Ethyl acrylate |
A,K* |
|
|
1,2-Ethylene diamine |
A |
|
|
Ethylene oxide |
A,K,R |
Flammable |
|
Propylene oxide |
K |
Flammable |
|
2-Methylaniline |
K |
|
|
2-Propyn-1-ol |
N |
|
|
Chelators |
||
|
Sodium EDTA (ethylene diamine tetraacetic acid) |
R |
|
|
Sodium NTA (nitrilotriacetic acid) |
K |
|
|
Anti-rusts |
||
|
2-Aminoethanol |
N |
|
|
Triethanolamine |
A |
|
|
Hexamethylene tetramine |
A |
|
|
2-Butyn-1,4-diol |
C,T |
|
|
Disodium metasilicate |
C,I |
|
|
2-(3H)-Benzothiazolethione |
A |
|
|
Disinfectants |
||
|
Borax |
R |
|
|
Disodium tetraborate |
R |
|
|
Morpholine |
N |
|
|
Benzalkonium chloride |
C |
|
|
Sodium dichloroisocyanurate |
I |
Reacts with acid to liberate toxic gas |
|
Sodium hypochlorite |
C |
Reacts with acid or ammonia to release toxic gases |
|
Preserving agents |
||
|
1,2-Bensisothiazol-3(2H)-one |
A |
|
|
5-Chlor-2-methyl-3-isothiazolone |
A |
|
|
2-Methyl-3-isothiazolone |
A |
|
|
2-Chloracetamide |
A |
|
|
p-Chlor-m-cresol |
A |
|
|
Hexahydro-1,3,5-tris- (2-hydroxyethyl)1,3,5-triazine |
A |
|
|
1,5-Pentadiol |
A |
|
|
2-Bromo-2-nitro-1,3-propanediol |
T |
|
|
Fillers |
||
|
Quartz |
K |
|
|
Silicon dioxide |
K |
|
|
Sodium hydrogen sulphate |
C |
|
|
Others |
||
|
Subtilisin (Enzyme) |
A |
|
|
Sodium saccharine |
K |
|
|
Ammonium peroxodisulphate (bleaching agent) |
A |
|
A = allergen; C = corrosive; I = irritant; K = carcinogen; N = neurotoxic agent; R = reproductive toxic agent; T = toxic if swallowed; * = danger dependent on concentration.
Determination of toxicity was done by the Danish Institute of Occupational Health. †Note that not all cleaning agents have been tested for all toxic properties, so that this list is not necessarily complete or comprehensive. Source: Summarized from Borglum and Hansen 1994. Cleaners who work in factories or hospitals may be exposed to chemicals (or biohazards) associated with the ongoing activities in the spaces they clean. If cleaners are not integrated into the training programmes and social network of the regular workforce, they may be less aware of these hazards than other workers. For example, one study showed that cleaners were the group most often exposed to harmful chemicals of all categories of hospital workers (Weaver et al. 1993). There is some controversy about the use of gloves for cleaning work. Gloves play an important role in protecting the skin from hazardous agents if they fit correctly and are made of impermeable and resistant materials. But wearing gloves constantly can keep perspiration from evaporating. The resulting damp area is a favourable growth medium for infectious agents. Wearing gloves was associated with skin problems in a large sample of Danish cleaners (Nielsen 1996). It is therefore best to wear gloves the minimum time compatible with protection. The necessity for wearing gloves can often be obviated by using tools with long handles, or by other changes in methods. Wearing cotton gloves under rubber or plastic gloves may reduce humidity and protect against allergies to some glove materials (Foussereau et al. 1982). Some hand creams may contain irritants and should be avoided (Hansen 1983). Several other practices diminish exposure to chemicals. When cleaning solutions are stored or prepared, there should be good ventilation, and procedures should permit preparation without any danger of touching or breathing the chemicals. The temptation to work with undiluted chemicals will diminish if workers have adequate time and implements. Also, cleaners may use undiluted chemicals or chemicals that have allergenic fragrances in order to signal to others that they have done their job. This can be done by other means, such as clear inspection procedures and communication links with other workers and with clients of cleaning services. Useful information on prevention of exposure to chemicals can be found in a handbook published by the City of New York (Michaels, undated). Other health risks Cleaners often work evening or night shifts, so as not to interfere with the other activities being carried out in the same spaces. They may therefore suffer the usual effects of shift work on biorhythms. In addition, they may risk violence if they work alone in isolated areas. Cleaners, particularly those who work outside regular building hours and/or who are not part of the regular personnel, may be ignored and excluded from the social network in their workplaces (Messing in press). They may not be given access to the appropriate facilities for breaks and meals. Aside from the psychological effects of exclusion, cleaners may be deprived of information on hazards routinely given to other workers, despite legal requirements in many jurisdictions to provide this information. Also, despite the importance of surface textures and design for their work, they and their supervisors may not be consulted when relevant purchasing and planning decisions are made. This is especially true if cleaning is contracted out. It is therefore important that a special effort be made to include cleaners in occupational health and safety promotion activities in the workplace. Information on characteristics of chemicals, on work procedures and on safety should be discussed with cleaners and clearly posted in the workplace. Health Effects and Disease Patterns Cleaners as a profession have poorer health than others (Nielsen 1995; ASSTSAS 1993; Sogaard 1994). Comparing cleaners with other workers, an analysis of the Quebec Health Survey found, after controlling for age, that women cleaners had the highest prevalence of chronic back problems and cardiopathies of all categories of women workers and that male cleaners had the highest prevalence of musculoskeletal problems and cardiopathies (Gervais 1993). Pregnant cleaners have an increased likelihood of miscarriage (McDonald et al. 1986), giving birth prematurely (McDonald et al. 1988) or bearing children with low birth weight (McDonald et al. 1987). Some large population-based epidemiological studies have found high cancer rates among cleaners. Rates of some brain tumours among US White men have been found to be especially high for cleaning service workers (Demers, Vaughan and Schommer 1991). Among women, invasive cervical cancer is almost five times more common among cleaners than other women (Savitz, Andrews and Brinton 1995). These results are attributed to chemical exposures, particularly solvents. Musculoskeletal problems are often encountered. In Denmark, Nielsen (1995) found that those who left cleaning had a reduced frequency of musculoskeletal symptoms compared to those who stayed in the profession. Cleaning was one of the five trades reporting the most shoulder/neck pain, tendovaginitis and low back pain (Sogaard, Fallentin and Nielsen 1996). A population-based epidemiological study found female cleaners to be particularly likely to have osteoarthritis of the knee, compared to other Swedish workers (Vingard et al. 1991). Cleaners in Quebec hospitals suffer almost twice as many occupational accidents and illnesses as the average Quebec health care worker: 23.8 compared to 13.9 per 100 full-time equivalent workers per year (ASSTSAS 1993). Most lesions involved the trunk or upper limbs (ASSTSAS 1993). Comparing male with female cleaners, a survey of cleaners in the Paris region in France found that men had more back pain and women had more joint pain (Opatowski et al. 1995). These differences are probably attributable to specificities in the tasks assigned to women and men cleaners (Messing, Haëntjens and Doniol-Shaw 1993; Messing, Doniol-Shaw and Haëntjens 1993; Messing, Chatigny and Courville 1996). Cleaners have a high level of skin problems, including dermatitis and eczema (Gawkrodger, Lloyd and Hunter 1986; Singgih et al. 1986). Point prevalences of skin diseases of 15 to 18%and a duration of employment prevalence of 39%have been found among large samples of hospital cleaners (Hansen 1983; Delaporte et al. 1990). Cleaners who spend more time with wet hands have more skin problems (Nielsen 1996). Cleaners may also be injured or infected by broken glass, needles or other sharp objects while handling waste (ASSTSAS 1993). Recently, occupational health specialists have noted symptoms of stress related to work among hospital cleaners, for which they suggest re-examination of the work process (Toivanen, Helin and Hänninen 1993). Low prestige of the profession may be a cause of distress for cleaners (Messing, in press). Accidents, infection and environmental contamination may be prevented by clear and well-publicized guidelines for disposal of dangerous waste in factories, hospitals, offices and public buildings. Since constraints placed on other workers may prevent them from paying full attention to prevention of hazards for cleaners, consultations between cleaners and other workers should be arranged, in order to decide on the appropriate size and placement of wastebaskets, waste separation and labelling. Cleaners should be included whenever waste disposal practices are being planned or reviewed so that realistic methods can be proposed.
Barbering and Cosmetology
General Profile
It has been estimated that over a million people work in approximately 150,000 salons and barber shops in the United States. These men and women, barbers and cosmetologists (also referred to as “technicians”), perform a wide range of services, including shaving; cutting and styling hair; giving manicures and pedicures; applying artificial nails; and performing a variety of chemical hair processes including bleaching, colouring, hair relaxing and permanent waving. In addition, some technicians provide facial treatments and removal of body hair.
Technicians may be exposed to a variety of potential health and safety hazards on the job, including:
Chemicals. According to an analysis conducted by the US National Institute for Occupational Safety and Health (NIOSH), 30% of the nearly 3,000 chemicals used in cosmetology are classified by the US government as toxic substances. Ventilation in many shops is often inadequate to eliminate chemical exposure.
Diseases. Because of their close contact with clients, technicians may be exposed to a variety of infectious diseases, ranging from colds and flu to impetigo, chicken pox and hepatitis.
Ergonomic hazards. Barbers and cosmetologists also suffer from a range of musculoskeletal disorders associated with repetitive motion, prolonged standing, cramped work spaces and poorly designed tools and equipment.
Scheduling. Working hours may be irregular and extended. Many technicians work in “split shifts”, splitting their work day to cover 12 to 14 hours of client services.
Other problems. These include poor housekeeping and electrical and fire hazards.
As a result of exposure to these and other hazards, an increasing number of people are being forced to leave their chosen profession. A recent study by Nellie Brown, director of the Chemical Hazards Information Program at Cornell University, found that 20% of US hair stylists leave their jobs because of work-related illness (New York Times Magazine, 7 March 1993).
Despite increasing evidence of risk, there are few regulations protecting barbers and cosmetologists. In the United States, cosmetic products are regulated by the Food and Drug Administration (FDA), which is oriented towards consumer protection and has a limited ability to address worker health and safety issues. Like regulatory agencies in many countries, the FDA does not require product manufacturers to conduct safety tests before public marketing, to list ingredients on the labels of products sold for professional use only or to give the FDA information on consumer complaints. Nor does the FDA routinely test products on its own initiative; any testing done by the FDA focuses on risks to consumers, not workers, although workers may be at greater risk due to their daily and prolonged use of cosmetic chemicals.
Attempts to regulate this industry are further complicated by the differing local, national and international definitions of the tasks barbers and cosmetologists perform. In the United States, licensing requirements vary from state to state. Many countries have no licensing requirements at all.
Major Processes and Hazards
Chemical hazards
Barbers and cosmetologists are exposed to a wide variety of chemicals during the course of a working day. Technicians are at risk for absorbing chemicals through the skin or eyes, inhaling dangerous vapours or particulates and ingesting toxins that have contaminated food, drink or cigarettes. Some guidelines for reducing hazardous exposure are given in figure 1 .
Figure 1. Reducing exposure to chemical hazards.
Chemicals can affect the body in different ways depending on the concentration of the chemical in a product; how toxic the chemical is; the route by which it enters the body (inhalation, skin contact, ingestion); and the length of time of the exposure. Individual characteristics, such as general health status, pregnancy and smoking, can also affect a person’s risk.
There are thousands of different chemicals associated with cosmetology processes. In order to determine the specific chemicals contained in a product and their effects, it is important that technicians have access to, and understand, product labels and material safety data sheets (MSDSs).
Common chemical processes
Colouring hair. Hair colouring solutions are applied manually to the hair with an applicator bottle or brush. It also is becoming very common for clients to request an eyebrow or eyelash tints.
Chemicals used in hair colouring include synthetic organic colorants, complex metallic colorants and vegetable dyes. Synthetic hair colorants often include permanent oxidative dyes which use hydrogen peroxide to oxidize aromatic diamines. These chemicals are eye, nose and throat irritants. Synthetic organic hair dyes containing an amine group are also among the most frequent causes of allergic sensitization. Metallic dyes may include lead-containing compounds.
Coal tar-based hair dyes may contain mutagens. Hair dyes which have been found to be mutagenic in in vitro testing pose uncertain human health risks. However, the production of non-mutagenic hair dyes appears to be possible and should be encouraged. For example, henna, a vegetable dye, is one of the oldest hair dyes and is not known to be either a mutagen or a carcinogen.
Bleaching hair. Bleaching solutions are applied manually with an applicator bottle or brush. These solutions may contain hydrogen peroxide, sodium peroxide, ammonium hydroxide, ammonium persulphate or potassium persulphate. These chemicals can cause skin, eye, nose, throat or lung irritation. Persulphate bleach powders have also been associated with asthma among cosmetologists (Blainey et al. 1986).
Permanent waving. Permanent waves usually involve several steps: washing the hair; rolling the hair in curlers; applying a thioglycolate or similar solution; and rinsing and neutralizing with an oxidizing agent. Water sprays may also be used.
Permanent-wave solutions may contain alcohol, bromates, sodium hydroxide, boric acid (perborate or borate), ammonium thioglycolate or glycerol monothioglycolate. Some of these chemicals may cause central nervous system effects (headache, dizziness, nausea, drowsiness); eye, nose and throat irritation; lung problems (breathing difficulty or coughing); skin irritation; burns; or allergic reactions (stuffy or runny nose, sneezing, asthma or allergic dermatitis).
Manicures, pedicures and artificial nails. Nail care involves soaking the cuticles in softening agents, using nail clippers, using emery boards or nail files to file the nails, using hand lotions and applying and removing polish. Artificial nails (acrylics, gels, fibreglass, porcelains and fabric wraps and tips) may be brushed onto the nail or attached to it with glue. They are allowed to harden and then filed to the desired shape.
The many chemicals found in nail products include acetone, ethyl methacrylate and other acrylates, methyl ethyl ketone, ethyl acetate, lanolin and dimethyl-p-toluidine. These can cause skin, eye, nose, throat and lung irritation, as well as central nervous system effects. Some nail products also contain formaldehyde, associated with allergies as well as cancer with long term use. Some products contain glycol ethers, xylene and toluene, all linked to reproductive problems in laboratory animals.
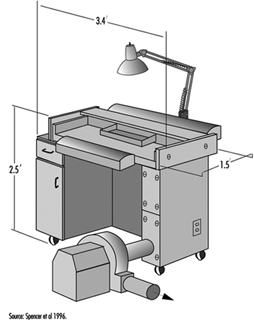
The use of methyl methacrylate (MMA) in artificial nail products was banned in the United States in 1974. Despite the ban, this chemical continues to be used. A 1982 study found that methyl methacrylate was present in 8 of 29 artificial nail products, and a 1986 study found measurable levels of MMA in the air of some nail salons. This chemical, if in contact with the skin, can cause tingling, numbness and whitening of the fingers. It also causes skin allergy in many people. An allergy to MMA can result in cross-sensitivity to other more commonly used methacrylates. In some products MMA has been replaced by other acrylates that may also be sensitizers. Figure 2 shows a downdraft table designed to minimize a manicurist’s exposure to the chemicals.
Figure 2. A modified commercial downdraft manicure table for application of artificial fingernails.
Washing and styling hair. Hair washing involves shampooing and rinsing with water. During this service, conditioners and other hair treatment products may also be applied. Hair drying is done in many ways: drying manually with towels, using a hand-held dryer or having the client sit under a fixed dryer. Styling generally involves the use of gels, creams or aerosol sprays. Washing the hair is often the first step for other services such as setting the hair, hair colouring and permanent waving. In large salons, one person may be assigned the job of washing clients’ hair, and do nothing other than that.
Shampoos and conditioners may contain alcohol, petroleum distillates and formaldehyde. All have been linked to dermatitis and allergies, including asthma. Long-term use of formaldehyde has also been linked to cancer.
Aerosol hair sprays may contain polyvinylpyrrolidone, which has been associated with lung and other respiratory diseases, including thesaurosis. They also contain a variety of solvents.
Straightening hair. Hair-straightening or hair-relaxing solutions are applied to the hair with a brush; then the hair is stretched to relax the natural curl. Hair straightener may contain sodium hydroxide, hydrogen peroxide, bromates, ammonium, thioglycolate and glycerol monothioglycolate. These chemicals may cause eye, nose and throat irritation, central nervous system effects and dermatitis.
Other chemical processes. A variety of cosmetics, including face creams and powders, mascara, eye liners, lipsticks and other products, may also be applied by cosmetologists. These can contain a wide variety of solvents, dyes, pigments, preservatives, oils, waxes and other chemicals that can cause skin allergies and/or irritation.
Cosmetologists may also remove body hair. Hair removal treatments can involve the application of hot wax and use of chemical depilatory products. These products often contain alkaline ingredients that can cause dermatitis.
Ergonomic hazards
Barbers and cosmetologists are at risk for musculoskeletal disorders due to the physical demands of their work and to poorly designed equipment, tools and work spaces. Such disorders can include:
- Wrist and hand problems, such as tendinitis and carpal tunnel syndrome. Risk factors include bending and twisting of the wrist while cutting and styling hair, holding hair dryers and using a round brush or curling iron. These disorders are also linked to forceful gripping or pinching caused by cutting with dull and/or poorly fitting shears.
- Shoulder problems, including tendinitis and bursitis. These are associated with constant reaching for supplies, or holding arms above shoulder height while cutting or styling hair. See figure 3.
- Neck and back problems, ranging from common aches and pains to serious conditions such as pinched nerves and ruptured discs. These are associated with frequent bending or twisting during activities such as shampooing, cutting hair below ear level, and performing manicures and pedicures.
- Foot and leg problems, including swelling, calluses and varicose veins. These may occur as a result of long periods of standing on hard floors in shoes with poor arch support.
Figure 3. Working with arms above shoulder level in a hairdressing salon in Zimbabwe.
Preventing musculoskeletal disorders
To prevent musculoskeletal disorders, it is important to apply ergonomic principles to the design of tasks, tools and workstations. Ergonomics is the science of adapting the workplace to the needs of the human body. It suggests ways to minimize awkward postures and repetitive motions, as well as the use of excessive force. It maximizes safety, health and comfort.
Ergonomic solutions may include:
- Adjustable furniture. For example, client chairs are available that can be raised, lowered and swiveled. Manicurist chairs are available with back support, armrests and seat pans that can be tilted to accommodate forward bending.
- Shears that are sharp, well-lubricated and designed to fit the individual’s hand.
- Curling irons and hair dryers with flexible handles. These can be used without excessive bending or twisting of the wrist.
- Free-standing sinks that allow technicians to wash hair without twisting and bending their backs.
- Rolling seats or stools that allow technicians to perform many procedures while seated, or to alternate between sitting and standing.
- Proper workstation designs such as storing commonly used supplies within easy reach; providing cushioned floor mats; and ensuring that cabinets are at the correct height to minimize reaching or bending.
- Client scheduling that varies the tasks and processes that a technician performs throughout the day.
- Training for technicians in good body mechanics and work practices such as proper lifting methods; bending at the hips instead of the waist; and using hair-cutting techniques that minimize reaching and bending of the wrist.
Infectious diseases
Work performed by barbers and cosmetologists involves close contact with clients. Understanding how infectious diseases are transmitted will help technicians prevent infection. Infectious diseases may be spread in the salon in the following ways:
- Through the air (e.g., upper respiratory illnesses such as colds and flu)
- Through contaminated water or food (e.g., hepatitis A, salmonella and giardia)
- Through insect or animal bites (e.g., lice)
- Through direct skin contact with infected persons (e.g., scabies, lice, ringworm, impetigo, herpes simplex, colds and chickenpox)
- Rarely, through exposure to the blood of an infected person (e.g., hepatitis B and HIV/AIDS)
While there is no recorded case of a barber or cosmetologist becoming infected with HIV/AIDS on the job, and work-related hepatitis B infection is extremely rare in these occupations, exposure to these bloodborne pathogens could possibly occur in rare instances of blood contact. Possible sources of exposure could include puncturing the skin with tools that carry infected blood (razors, tweezers, tattoo needles or clippers), or infected blood entering the body through an open wound, sore or skin rash.
This is one reason that shaving clients with razors has become uncommon in many countries. In addition to the risk to technicians, there is the possibility of skin and other infections being transferred from one client to another through unsterilized equipment.
Exposure to harmful organisms can be prevented by taking simple precautions:
- Hands should be washed frequently with soap and water.
- Latex gloves should be worn to protect technician and client if either has sores, lesions or skin rashes.
- Sharp instruments should be handled carefully and disposed of in approved puncture-proof containers.
- All tools, equipment and surfaces should be disinfected properly.
- Towels should be sanitized.
- Workers should be vaccinated against hepatitis B.
Other hazards
Fire hazards
Some products used in the salon may contain flammable or combustible chemicals. Sources of ignition can include flame from a cigarette, match or burner; a spark from a light switch, electric plug or frayed cord; or a hot object such as a curling iron, stove, light bulb or hotplate. To prevent accidents, it should be made sure that chemicals are used and stored properly. Flammables and combustibles should be kept away from flames, sparks or hot objects, and electrical equipment should be checked for broken or frayed cords that might spark or get hot. Each shop should also have a fire-prevention and evacuation plan, and appropriate and functioning fire extinguishers.
General housekeeping
Salons are often cramped and crowded work environments. Overstocked shelves may be unstable. Technicians may be at risk for slips and falls as a result of spilled liquids, poorly stored equipment or poorly positioned cords or wires. Narrow, crowded aisles limit workers’ ability to move freely without obstruction. All shops should practice good housekeeping, including: keeping aisles clear, cleaning up spills immediately, storing heavy objects on low shelves and making sure people can move freely through their workspace.
Electrical hazards
Electrical devices in the salon can include hair clippers, hair dryers, facial machines and electrolysis equipment and they should be checked for frayed wires and proper grounding. Since electrical equipment and outlets are often within splash range of water, red ground fault circuit interrupters to prevent shock should be used.
Health Problems and Disease Patterns
Skin diseases
Irritant and allergic dermatitis of the hands alone, or of hands and face together, is a common problem, experienced by 10 to 20% of cosmetologists (van der Walle and Brunsveld 1994). It often produces a characteristic rash in the spaces between the fingers. Signs of dermatitis generally include redness, drying and cracking on the skin of the hands. Eczema of the tips of the fingers may also occur, with ridging of the nail folds. Younger workers appear to be at highest risk, possibly because those with lower seniority tend to be assigned most often to shampooing and permanent-waving jobs. Most frequent causes of allergic skin rash in cosmetologists include glycerol thioglycolate, ammonium thioglycolate, nickel sulphate, ammonium persulphate preservatives and hair dyes (p-phenylenediamine or resorcinol) (Villaplana, Romaguera and Grimalt 1991).
In most cases, once an allergic dermatitis develops it does not improve, even with the wearing of gloves. Rubber latex glove use may itself be a significant risk factor for allergic responses, and vinyl gloves may need to be substituted if latex allergy develops. If one worker in a salon develops latex allergy, the entire salon may need to become latex-free to protect that worker from repeated allergic responses.
Other skin diseases of hairdressers include granuloma from hair implantation, and hot water burns. Also, varicose veins may result from the prolonged standing common to this occupation. Sharp tools such as scissors, shaving equipment and electric hair-cutting tools can cause skin lacerations. Such cuts may predispose the cosmetologist to dermatitis due to chemical exposures.
Lung problems
Allergic rhinitis (“hay fever”) and asthma have been associated with exposure to permanent-wave solution (Schwartz, Arnold and Strohl 1990), and in particular to ammonium persulphate (Gamboa et al. 1989). Hair bleach as well as henna (Starr, Yunginger and Brahser 1982) have been associated with occupational asthma in cosmetologists.
Reproductive health
A recent study found a moderately increased risk of spontaneous abortion among cosmetologists who worked full time and performed a large number of chemical services. The use of formaldehyde and exposure to manicuring and nail-sculpting chemicals were specifically associated with an increased risk of spontaneous abortion (John, Savitz and Shy 1994).
Cancer
Cosmetologists have been found to have a possible increased risk of developing certain types of cancer, including non-Hodgkin’s lymphoma (Zahm et al. 1992; Pearce 1992), bladder/urothelial cancer (Steineck et al. 1990) and breast cancer (Koenig 1994).
Laundries, Garment and Dry Cleaning
General Profile
Commercial laundries began as domestic enterprises, but have developed into businesses with many unique health and safety concerns. Laundries specializing in services for hospitals must deal with possible biological hazards, and those laundering work clothes for manufacturing or service workers may risk exposure to specific chemical hazards.
Dry cleaning reputedly originated in France in 1825 when a worker in a dye and cleaning factory spilled lamp oil on a soiled tablecloth (IARC 1995a). After the tablecloth dried, the spots had disappeared. Lamp oil is a hydrocarbon. Similar hydrocarbon solvents - turpentine, kerosene, benzene and gasoline - were used in the fledgling dry-cleaning industry. All these solvents had one major disadvantage: they were flammable, often resulting in fires and explosions (Wentz 1995). In 1928, W.J. Stoddard introduced a nearly odourless, petroleum-based solvent with a higher flashpoint, which reduced the risk of fire. Stoddard solvent gained widespread acceptance in the industry and is still used today.
At the turn of the century, advances in the synthesis of chlorinated hydrocarbons permitted development of nonflammable solvents for dry cleaning. Initially, carbon tetrachloride was preferred, but because of its toxicity and aggressiveness to metals, textiles and dyes, it was gradually replaced in the 1940s and 1950s by trichloroethylene and tetrachloroethylene (also commonly known as perchloroethylene, or PERC) (Wentz 1995). PERC (C2Cl4) is a colourless, clear, heavy liquid with an ethereal odour. Today, approximately 90% of US dry cleaners use PERC (EPA 1991a).
Although cleaning practices vary from country to country and from shop to shop, laundries and dry-cleaning shops are usually small businesses; about 70% of US dry-cleaning shops have fewer than four employees, who usually perform the cleaning at the same location as the shop. The employees of such a small business, many of whom typically labour more than eight hours per day, may be members of one family, sometimes including children. In many countries, the dry-cleaning family lives in the same building as the shop. An increasing trend among larger corporations is to operate multiple “drop” shops where customers leave soiled garments. The garments are transported to a central facility for cleaning, and later returned to the drop shops for customer pick-up. This arrangement confines hazardous waste to one site and reduces the solvent exposure of drop shop workers.
The Laundry and Dry-Cleaning Process
The dry-cleaning or laundry process usually begins when a customer brings soiled garments to a shop. Modern clothing is made from many different fibres and fabrics. Garments are inspected and sorted according to weight, colour, finish and fabric type prior to machine loading. Visible stains are treated at a spotting station with various chemicals, before or after cleaning, depending on the type of stain.
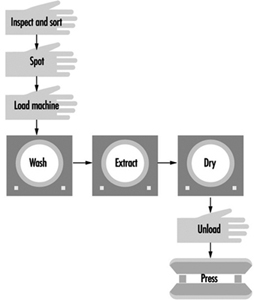
Cleaning is a three-step process: washing, extracting and drying (figure 1). Wet-process washing (laundering) uses detergent, water and possibly steam. In dry cleaning, detergent and water are added to the solvent to aid in soil removal. Clothes are manually loaded into the machine, and the cleaning solution is automatically injected. Machine contents are agitated for a period, then spun at high speed to extract the water or solvent and tumbled dry. Once garments have been removed from the dryer, they are pressed to remove wrinkles and restore their shape.
Figure 1. The dry cleaning process flow diagram.
Many countries have recently imposed stringent regulations for the control of PERC exposures and emissions because of associated health effects and environmental problems. In response to these regulations, dry-cleaning processes are changing. Improved solvent purification and vapour-recovery systems are available, alternative solvents are being developed, and wet methods using water immersion are being refined to clean garments traditionally cleaned in solvent. These processes are described below.
Transfer versus dry-to-dry equipment
Two basic types of machines used in dry cleaning are transfer and dry-to-dry. Transfer machines, older and less expensive, require manual transfer of solvent-laden clothing from the washer to the dryer. The transfer activity causes excessive worker exposure to PERC. Because of high solvent usage rates, emissions and exposures during transfer, PERC transfer machines are no longer manufactured in the United States; however, older used or reconditioned ones can still be purchased.
In 1994, at least 70% of PERC machines in the United States, for example, were dry-to-dry machines, using a one-step process that eliminates clothing transfer. Many shops are replacing or have replaced transfer machines with dry-to-dry machines because of the trend towards stricter environmental regulations; however, some shops still use transfer equipment for increased productivity and to avoid the capital expenditure required for new machines. In the United States, petroleum machines are primarily transfer units.
Dry-to-dry machines may be vented or ventless. Vented dry-to-dry machines vent residual solvent vapours directly to the atmosphere or through some form of vapour-recovery system during the aeration process. Ventless dry-to-dry machines are essentially closed systems, open to the atmosphere only when the machine door is opened. They recirculate the heated drying air through a vapour-recovery system and back to the drying drum. There is no aeration step.
Solvent purification: Filtration and distillation
Dry cleaners use filtration and/or distillation to recover and purify solvents. Filtration removes insoluble soils, non-volatile residues and loose dyes from the solvent. It is also sometimes used, primarily in the United States, to remove soluble soils. Filtration is a continuous process. The solvent passes through an adsorbent powder, cartridge or spin-disc filter, all requiring some level of periodic maintenance. Each filtration system produces contaminated cartridges or powders.
Distillation, used by 90% of US cleaners, removes soluble oils, fatty acids and greases not removed by filtration (International Fabricare Institute 1990). Distillation occurs when PERC is heated to its boiling point so that it vaporizes and later condenses back to liquid form. During this process, non-volatile impurities, which cannot be boiled off, remain in the still and are discarded as hazardous waste. Both filtration and distillation produce some solid wastes containing PERC; however, dry-cleaning machine manufacturers are striving to develop new filtration and distillation technologies that reduce the amount of hazardous waste produced. This ultimately results in important savings to the owner by reducing the cost of hazardous-waste disposal.
Recovery of PERC vapours
Two primary technologies are used to recover PERC vapours: the carbon adsorber and the refrigerated condenser. These two technologies, traditionally separate, are used together in more modern machines. Carbon adsorption is used in about 35% of the controlled machines in the United States, for example. Carbon adsorbers achieve a 95 to 99% vapour reduction by removing PERC from the air. Solvent-laden vapours pass over activated carbon having a high adsorption capacity. The carbon is later desorbed and the PERC recovered, or the carbon is discarded as hazardous waste when it becomes saturated with PERC. Carbon desorption typically occurs with steam or hot air. Desorption can be done automatically after each load, or it can be done at the end of the day. If not performed regularly, the carbon bed will become saturated and be ineffective for PERC recovery. The adsorption system can handle high volumes of air, having relatively low solvent concentrations while maintaining a high PERC removal efficiency, but frequent desorbing is needed and steam regeneration produces contaminated waste water.
Refrigerated condensers cool solvent-laden air below the dew point of the vapour to recover PERC, and operate on the principle that the ability of air to hold a solvent in the vapour state varies with temperature. Refrigerated condensers are used in approximately 65% of controlled machines. The process can achieve 95% vapour control in dry-to-dry machines and 85% control in transfer machines. Condensers require little maintenance and minimize the potential for waste water because steam regeneration is not required. They do require higher solvent concentrations than a carbon adsorber. Water vapour may pose a problem because it can condense and freeze, impeding gas flow and heat transfer (EPA 1991b).
Solvent alternatives to PERC
Alternative dry-cleaning solvents have been substituted for PERC. Flammable, petroleum-based solvents generally have higher exposure limits than PERC. These petroleum-based solvents are less aggressive at removing soils than PERC. Because their vapour pressures are lower than PERC, exposures from inhalation will generally be lower. However, adverse health effects are possible, including asphyxiation, central nervous system depression and skin and mucous membrane irritation. Contamination of aliphatic hydrocarbons with benzene will significantly increase the hazard.
Two different approaches have been taken in Germany to reduce the fire hazard posed by petroleum-based solvents: developing safer solvents and redesigning machines.
Recently developed petroleum-based solvents, widely used in Germany, are either straight-chain, branched or cyclic paraffins with a chain length of between 10 and 12 carbons. These petroleum-based solvents have an atmospheric lifetime of only a few days, are halogen-free, do not lead to ozone depletion and play only a minor role in the greenhouse effect. Some of the German requirements for petroleum-based, dry-cleaning solvents are outlined below (Hohenstein Institute 1995):
- Boiling range between 180° and 210ºC
- Aromatic, benzene, halogen and polycyclic aromatic content less than 0.01 wt%
- Flashpoint higher than 55ºC
- Thermally stable at operating conditions.
Dry-cleaning machines manufactured for petroleum-based solvents in Germany today are much safer than those of the past. Because petroleum-based solvents are combustible, additional safety measures are required on machines using them. Technical advances improve machine safety and greatly reduce the risk of fire/explosion. The following measures can be taken in combination or separately:
- Using an inert gas, such as nitrogen or argon, to displace oxygen in the drum and ensure that oxygen concentration is sufficiently low (approximately 4%) to prevent combustion
- Operating under a vacuum to remove oxygen and lower its concentration to below 4%
- Ensuring that the lower explosive limit (LEL) is not exceeded, or if the LEL is not known, ensuring that operating temperature remains 15ºC below the flashpoint
- Ensuring that vapour concentration remains below 50º of the LEL, by controlling operating temperatures or by providing sufficiently high airflow.
Wet cleaning
Wet cleaning is a developing technology, distinct from traditional laundering in that it is a more gentle process and can be used on many fabrics that were formerly dry cleaned. Four factors play an essential role in soil removal: temperature, time, mechanical action and chemical agents. Only the proper blend of these factors achieves the best cleaning results (Vasquez 1995). There are minor variations of machine wet cleaning, but all techniques use:
- Specially formulated wet-cleaning soaps and spotting agents
- Increased extraction of water prior to drying (extraction speeds as high as approximately 1,000 revolutions per minute)
- Close monitoring of heat and moisture content during the drying process
- Machines having less mechanical action during washing, accomplished by speed reduction and time limits.
Garments are washed with various levels of limited mechanical action, based on garment type and amount of soilage. The greatest risk occurs during drying. Many fibres can be fully dried with little or no difficulty. However, delicate garments or garments susceptible to shrinkage must be dried for only a few minutes before being hung to air dry. Because of these problems, most wet-cleaned garments require more finishing work than solvent-cleaned garments. Long drying times and more finishing work substantially increase processing time (Earnest and Spencer 1996).
Today, wet cleaning use is limited because the technology does not yet completely eliminate the need for solvents. It has been estimated that wet cleaning can safely clean approximately 30 to 70% of garments traditionally cleaned in solvent (Rice and Weinberg 1994). There are still problems with fibre damage, bleeding of dyes and, most importantly, cleaning ability. Inappropriate use of wet cleaning can expose shop owners to liability for damaged clothing. For this reason wet-cleaning advocates are working to persuade garment manufacturers to use fabrics that can be more easily wet cleaned.
Hazards in Laundries and Dry Cleaning Facilities
PERC hazards
In the workplace PERC can enter the human body through both respiratory and dermal exposure (ATSDR 1995). Symptoms associated with respiratory exposure include depression of the central nervous system; damage to the liver and kidneys (RSC 1986); impaired memory; confusion; dizziness; headache; drowsiness; and eye, nose and throat irritation. Repeated dermal exposure may result in dry, scaly and fissured dermatitis (NIOSH 1977).
US National Cancer Institute and National Toxicology Program studies have established a link between PERC exposure and cancer in animals. Human studies show an elevated risk of urinary tract (Duh and Asal 1984; Blair et al. 1990b; Katz and Jowett 1981), oesophageal (Duh and Asal 1984; Ruder, Ward and Brown 1994) and pancreatic cancer (Lin and Kessler 1981) among dry-cleaning workers. The International Agency for Research on Cancer (IARC) recently classified PERC in group 2A (probably carcinogenic to humans) and dry cleaning in group 2B (possibly carcinogenic to humans) (IARC 1995b). The Environmental Protection Agency (EPA) regulates PERC as a hazardous air pollutant.
US Occupational Safety and Health Administration (OSHA) data include numerous personal samples in dry-cleaning shops over the permissible exposure limit (PEL) of 100 ppm, 8-hour time-weighted average (TWA) (OSHA 1993). The machine operator is typically exposed to the greatest concentrations of PERC. US National Institute for Occupational Safety and Health (NIOSH) studies have shown that in many dry-cleaning shops having traditional machines, extremely high operator exposures occur during loading and unloading. Because loading/unloading occurs frequently throughout the day, in many instances exposure during this activity can account for 50 to 75% of the operator’s TWA exposure (Earnest 1996). Occupational exposures can be reduced by using modern dry-cleaning machines, solvent substitution, isolation of the process and effective local and general ventilation near the dry-cleaning machines.
Exposure to chemicals other than PERC
A wide variety of chemicals is present in laundries and dry-cleaning establishments. There is potential exposure through skin or eye contact or inhalation of vapours. Skin damage may occur from chronic or acute exposure. Chemicals that readily vaporize and have a high toxicity may pose a risk from inhalation, although this is generally considered to be of less concern than injury to the eyes or skin. The chemicals commonly used in the United States to treat stains through spotting are trichloroethylene; ketones, especially methyl isobutyl ketone (MIBK); petroleum naphtha; and hydrofluoric acid. Oxidizers, such as chlorine bleaches, may pose a hazard if used in the presence of many common compounds, such as turpentine, ammonia or fuel gases. Detergents containing enzymes may cause immune reactions in many workers. The combined exposures of the dry-cleaning solvent, PERC and various other chemicals is also a concern.
Ergonomic risk factors
Ergonomic hazards in the cleaning industry primarily occur among pressers. Pressing is a dynamic and repetitive task requiring reaching, precision gripping and awkward postures. Ergonomic risk factors are also present during material handling when heavy lifting may occur, especially in commercial laundries.
Fire hazards
The dry-cleaning industry has traditionally had a problem with fires. Part of the reason for this problem has been the widespread use of flammable and combustible liquids as a cleaning medium. The flammability of petroleum-based solvents continues to present an acute health and safety hazard. Approximately 10% of dry-cleaning shops in the United States use traditional, petroleum-based solvents, such as Stoddard solvent or mineral spirits. Even dry-cleaning shops that use non-flammable PERC face important fire hazards. If heated sufficiently, PERC will decompose into hydrogen chloride and phosgene gases. The production of hydrogen cyanide or carbon monoxide is another cause for concern during a fire. Hydrogen cyanide is produced when materials that contain nitrogen, such as many natural and synthetic fibres burn. Carbon monoxide is formed during incomplete combustion. All dry-cleaning shops have a large number of potential fuels and ignition sources.
Dry-cleaning machine designers must avoid conditions that can lead to a fire to occur and must ensure that their machines operate safely. Likewise, shop owners must take appropriate steps to prevent hazardous conditions from developing. Some common causes of fires in all businesses are electrical malfunctions, friction, open flames, sparks, static electricity, hot surfaces and smoking (NIOSH 1975).
Thermal burns
Cleaning facilities have several possible sources of severe burns. In the pressing station, burns may result from contact with the head of a press, lines transporting steam, or the steam itself. Insulation of pipes and surfaces, and use of various guarding techniques, can help prevent burns.
Although modern boilers are of safer design than earlier models, they are still used to produce large quantities of steam and must be operated safely. Many of the needed precautions can be found in the US National Fire Protection Association’s Code 32, Standard for Dry Cleaning Plants, and its Fire Protection Handbook (NFPA 1991). Recommendations in these documents include building code requirements, proper storage and isolation of flammables, fire extinguishers and sprinkler systems. Recommendations concerning the build-up of gases around the boiler address ways to eliminate gas leakage and ensure proper ventilation.
Mechanical hazards
Mechanical hazards are always a concern when powered equipment is used. Presses pose a significant mechanical hazard. Presses designed to be activated by only one hand leave a potential for the worker’s free hand to be caught between the presses. Belts, drive chains, shafts and couplings should be guarded to prevent accidental contact. All moving components of machines should be guarded to prevent body parts from becoming caught in a pinch, nip or shear point. The most common methods of guarding a hazard are enclosing the operation, interlocking devices, moving barriers, removal devices, remote controls, two-hand tripping devices and electronic safety devices.
Electrical hazards
Numerous measures can be taken to limit electrical hazards. Especially important is proper insulation and grounding. Identification and guarding of live parts also helps to prevent injury from electrical current. Electrical hazards can be compounded by the presence of moisture. Ground-fault circuit interrupters are designed to shut off power if high current passes through an unintended path. When selecting electrical equipment, the recommendations of established codes and standards, such as the US National Fire Protection Association 70, the National Electrical Code and the American National Standards Institute’s C2, should be followed. Guidelines for appropriate use of electrical equipment are given elsewhere in this Encyclopaedia.
Heat stress
Heat stress can afflict workers who must labour for extended periods of time in the hot environments that exist in many cleaning facilities. Heat stress may be compounded in the summer months, particularly if the shop is not air conditioned (air conditioning is not common in this industry). Both physical and environmental factors will modify the effects of heat. Acclimatization, body surface area to weight ratio, age and diseases, water and salt balance and physical fitness all play a role in the likelihood an individual will be affected by heat stress.
Slips, trips and falls
The hazard of slips, trips and falls are especially pertinent to cleaning facilities, which are often crowded with people and equipment. Without clearly established aisles and with a large number of containers holding solvents or water, spills can easily occur, resulting in a slippery floor. To control this hazard, regular housekeeping must be emphasized, facility layout must be carefully planned, and floor surfaces should be of non-slip materials. The workplace should be maintained in a clean, orderly, sanitary condition, and any spills should be cleaned up promptly.
Biological hazards
Laundering hospital linens puts sorters at risk from overlooked sharp objects in sheets or uniform pockets. Both dry cleaners and launderers may encounter freshly soiled garments that have been contaminated with human body fluids. Garments that have come from dental and medical offices or labs, blood banks, drug treatment centers, clinics, mortuaries, ambulances and other health-care facilities can be reasonably suspected to contain potentially infectious materials. In many countries, shops that handle garments from these sources must comply with the occupational standards governing exposures, such as the OSHA regulations governing bloodborne pathogens.
Environmental and Public Health Concerns
Environmental and public health concerns have resulted in dramatic changes in environmental regulations affecting the dry-cleaning industry in recent years. Adjacent apartments and businesses can be exposed to PERC vapours by diffusion through walls or ceilings; indoor airflow through holes in ceilings, pipe chases or vents; and through PERC emissions vented outside of the shop that are re-entrained through opened windows or ventilation units. Groundwater or soil contamination can occur through frequent or large solvent spills that might occur during transfer of solvent from a delivery truck to the dry-cleaning machine. Soil contamination might also occur through improper disposal of separator water into the sanitary sewer. Finally, consumers may be exposed from PERC residuals in poorly dried garments. This is of particular concern if the cleaning machine is not functioning properly or the dry cycle is shortened to improve productivity.
Acknowledgement: This article is largely based on materials assembled and published by the US National Institute for Occupational Safety and Health (NIOSH).
Funeral Services
General Profile
Assuming a world population of 5 billion, between one-quarter and one-half of a million people die each day. Many of the dead are infants or children, but eventually everyone who is born will also die. Despite the diversity in culture and religious beliefs surrounding death, the bodily remains of each person must be disposed of. In general, the two main methods of disposing of human remains consist of burial and cremation. Both of these disposal methods often have been applied to the untreated human remains. Many cultures, however, have developed funeral rites that prescribe some treatment of the dead body. Simpler rites may include the washing of the external surface with herbs and spices to slow or mask the onset of decay and the smell associated with dead tissue. More sophisticated rites include intrusive procedures such as embalming and removal of internal organs. Embalming usually involves replacement of blood with an embalming or preserving fluid. The Egyptians were among the first culture to develop and practice embalming of the dead. Embalming has been extensively practiced in the twentieth century throughout Western Europe and North America. Embalming may be followed either by burial or cremation. Outside of Western Europe and North America, burial or cremation is usually not preceded by embalming.
Funeral Processes
The preparation and burial of a deceased person can involve many processes, including:
- washing the surface of the body with various preparations
- dressing the body in burial clothes
- autopsies, in certain circumstances, which involve intrusive procedure, such as dissection and analysis of blood and body tissues
- embalming and removal of internal organs
- application of cosmetics to cover up visible damage if the body is to be viewed
- transporting the body to place of burial or cremation
- lifting of body and casket, and lowering it into the grave
- digging and filling of the grave
- possible exhumation of the body and subsequent autopsy.
Three types of hazard are always associated with the handling of deceased humans: microbial, psychological and ergonomic. A fourth type of hazard - chemical exposure - is introduced when embalming is performed. In the United States many states have enacted laws that require a body to be embalmed if the deceased person will be viewed in a open casket.
Microbial Hazards
Death is often caused by disease. After death the germs that caused the disease may continue to live in the deceased person and can infect the people handling the dead body.
Contagious diseases such as the plague and smallpox have been spread by improper handling of victims who died from the diseases. The route of exposure must be considered when evaluating the microbial hazard associated with the handling of dead bodies. Many diseases are spread by touching a source of contamination and then introducing that disease-causing organism, or pathogen, to one’s mucous membranes by rubbing the eyes or nose, or by ingesting the pathogen. Some diseases can be contracted simply by inhaling the pathogen. Inhalation can be a special hazard during exhumation, when the remains are dry, or during procedures that aerosolize parts of the human body, such as sawing through the bone of a deceased person. The contagion of diseases is further exacerbated when procedures with sharp instruments are used in funeral rites. Such practices introduce the possibility of parenteral exposure.
Microbial hazards can be classified in many different ways, including the type of disease-causing organism, the type of disease, the severity of the disease and the route of infection. Perhaps the most useful way of discussing microbial hazards encountered by funeral workers is by route of infection. The routes of infection are ingestion, inhalation, touch or surface contact and parenteral, or puncture of a body surface.
Ingestion as a route of exposure can be controlled by proper personal hygiene - that is, always washing hands before eating or smoking, and by keeping food, drink or any object that will be put in the mouth (such as cigarettes) out of areas of possible contamination. This is important for controlling chemical exposure as well. In addition to careful personal hygiene, wearing impermeable gloves when handling the dead can reduce the probability of infection.
Inhalation exposure occurs only when disease-causing organisms become airborne. For funeral workers the two primary ways that pathogens can become airborne are during an exhumation or during autopsy procedures in which a saw is used to cut through bone. A third possibility of aerosolizing a pathogen - tuberculosis, for example - is when air is forced out of the lungs of a corpse during handling. Although the epidemics of the past have included plague, cholera, typhoid, tuberculosis, anthrax and smallpox, only the organisms causing anthrax and smallpox appear capable of surviving any length of time after burial (Healing, Hoffman and Young 1995). These pathogens would be found in any of the soft tissues, not the bones, and particularly in soft tissues that have become mummified and/or dried out and friable. The anthrax bacterium can form spores that remain viable for long periods, especially under dry conditions. Intact smallpox viruses taken from the tissues of bodies buried in the 1850s were identified under the electron microscope. None of the viruses grew in tissue culture and they were deemed to be non-infective (Baxter, Brazier and Young 1988). Smallpox virus has remained infective, however, after 13 years in dry storage under laboratory conditions (Wolff and Croon 1968). An article appearing in the Journal of Public Health (UK) during the 1850s reports concern about smallpox infectivity from remains buried two hundred years earlier in Montreal, when smallpox was widespread in the New World (Sly 1994).
Perhaps a more probable source of inhalation exposure during exhumation are fungal spores. Whenever old material of any sort is disturbed, protection against the inhalation of fungal spores should be provided. Disposable high efficiency particulate (HEPA) respirators, developed primarily for protection against tuberculosis and lead dust, are quite effective against fungal spores as well. In addition to microbial concerns, the possibility of exposure to wood dust and/or lead needs to be evaluated before any exhumation proceeds.
The primary route of infection for tuberculosis is inhalation. The incidence of tuberculosis has increased during the last quarter of the twentieth century, primarily due to decreased public health vigilance and the emergence of bacterial strains that are resistant to several groups of antibiotics. A recent study conducted at Johns Hopkins School of Public Health (Baltimore, Maryland, US) indicates that 18.8% of embalmers demonstrated positive results to tuberculin skin tests. Only 6.8% of people employed in the funeral business who are not embalmers demonstrated positive results to the same test. The lower rate of reactivity is similar to the general public (Gershon and Karkashion 1996).
Hepatitis B virus (HBV) and the human immunodeficiency virus (HIV) are infective if they come in contact with mucous membranes or are introduced into the bloodstream through a cut or puncture. A study of funeral service practitioners in Maryland indicated that 10% had a mucous membrane exposure within the past 6 months and 15% reported a needle stick within the past 6 months (Gershon et al. 1995). Other US studies reported that between 39 and 53% of morticians had a needle stick within the past 12 months (Nwanyanwu, Tubasuri and Harris 1989). In the United States, the reported prevalence of HBV is between 7.5 and 12.0% in unvaccinated funeral directors, and 2.6% or less in vaccinated funeral workers. The reported vaccination rate varies between 19 and 60% of morticians in the United States. Although there is a vaccine for HBV, there is currently no vaccine for HIV.
HIV and HBV are infective only when the virus comes into contact with the mucous membranes or is introduced into the bloodstream of another human. The virus is not absorbed through intact skin. Mucous membranes include the mouth, nose and eyes. These viruses can be introduced into the bloodstream through a cut or abrasion in the skin, or by puncturing or cutting the skin with an instrument that is contaminated with the virus. Hands that are cracked due to dryness or a hangnail may provide routes of entry for these viruses. Therefore, to prevent transmission of these diseases it is important to provide a barrier impermeable to body fluids, to avoid splashing contaminated fluids on the eyes, nose or mouth, and to prevent puncturing or cutting the skin with an instrument contaminated with HIV or HBV. Use of latex gloves and a face shield can often provide this protection. Latex gloves, however, have a limited shelf life depending on the amount of sunlight and heat to which they have been exposed. In general, the latex should be stress tested if the gloves have been stored for more than a year. Stress testing involves filling the glove with water and observing if any leaks develop during a minimum of two minutes. Some countries in the West, such as the United States and Great Britain, have adopted the idea of universal precautions, which means that every corpse is treated as if it were infected with HIV and HBV.
Psychological Hazards
In many cultures the family of the deceased prepares the body of their dead relative for burial or cremation. In other cultures a specialized group of individuals prepares the bodies of the dead for burial or cremation. There is a psychological effect on the living when they are involved in handling dead bodies. The psychological effect is real regardless of the procedures used in the funeral rites. Recently there has been an interest in identifying and evaluating the effects of performing funeral rites on those who actually perform them.
Although the psychological hazards of being a professional funeral worker have not been extensively studied, the psychological effects of dealing with the human remains of traumatic death have been recently analyzed. The main psychological effects appear to be anxiety, depression and somatization (the tendency to report physical ailments), as well as irritability, appetite and sleep disturbances, and increased alcohol use (Ursano et al. 1995). Post-traumatic stress disorder (PTSD) occurred in a significant number of individuals who handled the victims of traumatic deaths. Immediately after a disaster in which human remains were handled by rescue workers, between 20 and 40% of the rescue workers were considered to be in a high risk category, as demonstrated by psychological testing, but only about 10% of the rescue workers were diagnosed with PTSD. The psychological effects were still present in rescue workers one year after the disaster, but the incidence was greatly reduced. Adverse psychological effects, however, have been detected in individuals several years after the traumatic event.
Many of these studies were performed on military personnel. They indicate that generalized stress rates are higher in inexperienced individuals who were not volunteers, and that there was an increased incidence of stress indicators up to one year after a traumatic incident. Empathy or self-identification of the mortuary worker with the deceased appeared to be associated with an increased level of psychological stress (McCarroll et al. 1993; McCarroll et al. 1995).
One study evaluated the causes of death in 4,046 embalmers and funeral directors in the United States between 1975 and 1985, and reported a proportionate mortality ratio (PMR) of 130 for suicide. The PMR is a ratio of the actual number of suicides in the embalmers and funeral directors divided by the number of suicides that would be expected in a group of individuals comparable in age, race and sex who are not embalmers or funeral directors. This ratio is then multiplied by 100. The purpose of this study was to assess the risk of cancer in morticians, and the suicide statistic was not elaborated any further.
Ergonomics
A deceased human adult is heavy and usually must be carried to a designated place of burial or cremation. Even when mechanical means of transportation are used, the dead body must be transferred from the place of death to the vehicle and from the vehicle to the burial or cremation site. Out of respect for the dead person, this transfer is usually performed by other humans.
Morticians are required to move corpses many times during the course of body preparation and funerals. Although there were no studies found that addressed this issue, low-back pain and injury is associated with prolonged repetitive lifting of heavy objects. There are lifting devices available which can assist with these types of lifts.
Chemical Hazards
Embalming procedures introduce a number of potent chemicals into the workspace of funeral workers. Perhaps the most widely used and toxic of these is formaldehyde. Formaldehyde is irritating to the mucous membranes, the eyes, the nasal lining and the respiratory system, and has been associated with mutagenic cell changes and the development of cancer, as well as occupational asthma. During the past several decades the occupational exposure level associated with no adverse effects has been consistently lowered. Current 8-hour time-weighted average permissible exposure limits range from 0.5 ppm in Germany, Japan, Norway, Sweden and Switzerland to 5 ppm in Egypt and Taiwan (IARC 1995c). Formaldehyde levels between 0.15 and 4.3 ppm, with instantaneous levels as high as 6.6 ppm, have been reported for individual embalmings. An embalming typically takes between 1 and 2 hours. Additional formaldehyde exposure is associated with the application of embalming creams and drying and hardening powders, and during spills.
Rats that have been chronically exposed to 6 to 15 ppm of formaldehyde (Albert et al. 1982; Kerns et al. 1982; Tobe et al. 1985), or repeatedly exposed to 20 ppm for 15-minute periods (Feron et al. 1988), have developed nasal carcinomas (Hayes et al. 1990). The IARC reports limited epidemiological evidence for an association between formaldehyde exposure in industry and the development of human nasal and pharyngeal cancers (Olsen and Asnaes 1986; Hayes et al. 1986; Roush et al. 1987; Vaughan et al. 1986; Blair et al. 1986; Stayner et al. 1988). Several studies of morticians, however, have reported an increased incidence of leukaemias and brain tumours (Levine, Andjelkovich and Shaw 1984; Walrath and Fraumeni 1983). In addition to the carcinogenic effects, formaldehyde is irritating to the mucous membranes and has been considered a strong sensitizer in the development of adult-onset asthma. The mechanism or mechanisms by which formaldehyde precipitates asthma are even less well characterized than its role in the development of cancer.
Other potentially toxic chemicals used in embalming fluids include phenol, methanol, isopropyl alcohol and glutaraldehyde (Hayes et al. 1990). Glutaraldehyde appears to be even more irritating than formaldehyde to the mucous membranes, and affects the central nervous system at levels well above 500 ppm. Methanol also affects the central nervous system and, in particular, the vision system. Phenol appears to affect the nervous system as well as the lungs, heart, liver and kidneys, and is absorbed quite rapidly through the skin. Our understanding of the toxicology of, and our ability to perform risk assessment for, exposure to multiple chemicals simultaneously are not sufficiently sophisticated to analyse the physiological effects of the mixtures to which embalmers and funeral directors are exposed. Blair et al. (1990a) thought that the increased incidence of leukaemias and brain tumours reported in professional, but not industrial, workers was a result of exposure to chemicals other than formaldehyde.
Recent advances in the design of dissecting tables indicate that local downdrafting of vapours significantly reduces the exposure of individuals working in the vicinity (Coleman 1995). Wearing gloves while performing procedures that require skin contact with embalming fluids and creams also reduces the hazard. There has been some concern, however, that some of the latex gloves on the market may be permeable to formaldehyde. Therefore, protective gloves should be selected carefully. In addition to the immediate concerns about the hazards of formaldehyde exposure, evidence has been accumulating that leachate from cemeteries may lead to formaldehyde contamination of groundwater.
Exhumation of bodies may also involve chemical exposures. Although used sporadically for centuries, lead was commonly used to line coffins beginning in the eighteenth and continuing into the nineteenth century. Inhalation of wood dust is associated with respiratory problems, and fungus-contaminated wood dust is a double-edged sword. Arsenic and mercury compounds were also used as preservatives in the past and could present a hazard during exhumation.
Domestic Workers
General Profile
Domestic work is characterized by labour for another family within their home. The term domestic workers should not be confused with homemakers and housewives, who work in their own home, or housekeepers, who work in institutions such as a hospital or school. The position of employment within a home is a unique and often isolated work environment. The position of domestic worker is almost always considered menial or inferior to the family for which they are employed. Indeed in the past, domestic work was sometimes done by slaves or indentured or bonded servants. Some of the job titles today for domestic workers include: servant, maid, housekeeper, au pair and nanny. While domestic workers can be either female or male, female workers are both much more commonly employed and most often paid less than males. Domestic workers are customarily immigrants or members of ethnic, national or religious minorities of the country of employment.
One should distinguish between domestic workers who are employed as live-in servants from those who live in their own home and commute to their place of work. Live-in domestic workers are isolated from their own family, as well as often from their own country of nationality. Because of the worker’s disenfranchisement, work contracts and health and other benefits are negligible. Sometimes, room and board are considered part or even complete payment for services rendered. This situation is particularly critical for the overseas domestic worker. Sometimes, infractions concerning agreed-upon salary, sick leave, working hours, vacation pay and regulation of working hours and duties cannot even be addressed because the worker is not fluent in the language, and lacks an advocate, union, work contract or money with which to exit a dangerous situation (Anderson 1993; ILO 1989). Domestic workers usually have no workers’ compensation, nowhere to report a violation, and are often unable to quit their employment.
Places where major employers of domestic workers are found include Britain, the Persian Gulf and Arab States, Greece, Hong Kong, Italy, Nigeria, Singapore and the United States. These domestic workers are from various countries, including Bangladesh, Brazil, Colombia, Ethiopia, Eritrea, India, Indonesia, Morocco, Nepal, Nigeria, the Philippines, Sierra Leone and Sri Lanka (Anderson 1993). In the United States, many domestic workers are immigrants from Central and Latin America and the Caribbean islands. Domestic workers are sometimes illegal immigrants, or have special limited visas. They are often not eligible for the basic social services available to others.
General Tasks
Tasks for domestic workers can include:
- Kitchen work: shopping for food, cooking and preparation of meals, waiting on the family and serving meals, cleaning up after mealtime and taking care of tableware
- Housecleaning and housekeeping: care of furniture and bric-a-brac, washing dishes, polishing silver and cleaning the house including bathrooms, floors, walls, windows and sometimes annexes, such as guest houses, garages and sheds
- Clothing care: washing, drying, ironing of clothing, sometimes mending of clothing or delivery/pick-up of clothing that is dry cleaned
- Child and elder care: babysitting or childcare, changing diapers and other clothes, washing children, supervision of meals and activities and delivery to and from school. Domestic workers will sometimes be given tasks that revolve around elder care such as supervision, bathing, companionship tasks, delivery to and from doctor visits and light medical chores.
Hazards and Precautions
In general, the intensity of hazards associated with live-in domestic workers is much greater than domestic workers who commute to work daily.
Physical hazards
Some physical hazards include: long working hours, insufficient rest time and sometimes insufficient food, exposures to hot and cold water, exposure to hot kitchen environments, musculoskeletal problems, especially back and spinal pain, from lifting children and furniture, and kneeling to clean floors. “Housemaid’s knee” has been likened to “carpet layer’s knee”, the injury sustained by carpet layers. While mechanization of certain floor-polishing and waxing processes has resulted in less work from the knees, many domestics still must work from their knees, and almost always without padding or protection (Tanaka et al. 1982; Turnbull et al. 1992).
Precautions include limitations of working hours, adequate rest and food breaks, gloves for dishwashing and other water immersion, training in proper lifting techniques, mechanized carpet cleaners and floor polishers to minimize the time spent on the knees and provision of knee pads for occasional tasks.
Chemical hazards
Domestic workers can be exposed to a wide variety of acids, alkalis, solvents and other chemicals in household cleaning products which can cause dermatitis. (See also “Indoor cleaning services” in this chapter). Dermatitis can often be exacerbated by the immersion of hands in hot or cold water (Scolari and Gardenghi 1966). Domestic workers may not know enough about the materials they use or how to use these products safely. There is inadequate training in chemical handling or hazard communication for materials that they use. For example, a severe poisoning case in a servant who was using cadmium carbonate silver-cleaning powder has been reported. The worker used the product for one-and-a-half days, and suffered abdominal cramps, tightness of the throat, vomiting and low pulse. Recovery took 24 days (Sovet 1958).
Many products used or handled by domestic workers are known allergens. These include natural rubber protective gloves, house plants, waxes and polishes, detergents, hand creams, antiseptics and impurities in detergents and whiteners. Irritant dermatitis may be a precursor to allergic contact dermatitis in housekeepers, and often starts with the development of erythema patches on the backs of hands (Foussereau et al. 1982). Inhalation of solvents, household pesticides, dusts, moulds and so on can cause respiratory problems.
Precautions include using the least toxic household cleaning products possible, training in materials handling and safety of the various detergents and cleaning fluids, as well as the use of protective hand creams and gloves. Unscented products may be better for those individuals prone to allergy (Foussereau et al. 1982).
Biological hazards
Domestic workers with responsibility for the care of young children in particular are at greater risk of becoming infected with a variety of illnesses, especially from changing diapers, and from contaminated food and water. Precautions include washing hands carefully after changing and handling soiled diapers, proper disposal of soiled items and proper food-handling procedures.
Psychological and stress hazards
Some psychological and stress hazards include isolation from one’s family and community; lack of paid vacation and sick or maternity leave; inadequate protection of wages; rape, physical and mental abuse; over-extended working hours; and general lack of benefits or contracts. Live-in domestic workers face greater danger from hazards including violence, harassment, physical and mental abuse and rape (Anderson 1993).
During a six-month period in 1990, there were eight deaths - six suicides and two murders - of Filipino domestic helpers recounted in a report filed by the Philippine Embassy in Singapore. Suicide is under-reported and not well documented; however, there were as many as 40 suicides reported to the Philippine Embassy in one time period (Gulati 1993).
To a lesser extent, these same hazards are relevant to non-residential domestic workers. In an Ohio (United States) study that looked at workers’ compensation claims filed for sexual assault from 1983 to 1985, 14% of the rapes occurred in motel maids and housekeepers (Seligman et al. 1987).
Prevention of abuses of domestic workers can be aided by establishment of laws that protect these comparatively defenceless workers. In the United States, the hiring of illegal immigrants as domestic workers was a common practice until the passage of the Immigration Reform and Control Act of 1986. This act increased the penalties that could be imposed on the employers of these workers. However, in developed countries the demand for domestic help is steadily increasing. In the United States, domestic workers must be paid at least the minimum wage and, if they earn $1,000 or more annually from any single employer, they are entitled to unemployment compensation and social security (Anderson 1993).
Other countries have taken steps to protect these vulnerable domestic workers. Canada started its Live-in Care-giver Program in 1981, which was amended in 1992. This programme involves recognition of immigrant domestic workers.
Acknowledgement of the immigrant domestic worker is the first step in being able to address heath and safety preventive issues for them. As initial recognition of these workers and their difficulties is achieved, dangerous working conditions can be addressed and improved with government regulations, unionization, private support groups and women’s health initiatives.
Health Effects and Disease Patterns
One study of mortality data of 1,382 female domestic workers in British Columbia (Canada) showed higher mortality than expected from cirrhosis of the liver, accidental death due to exposure, homicides and accidents of all types combined. Also, deaths due to pneumonia and rectal and eye cancer were higher than anticipated. The authors suggest that a major factor in the elevated deaths due to liver cirrhosis is because many domestic workers in British Columbia are from the Philippines, where hepatitis B is endemic (McDougal et al. 1992). Other studies point to alcoholism as a factor. In a review of a California (United States) mortality study, it was noted that the following occupations were associated with increased cirrhosis mortality rates in women: private housecleaner and servant; waitress; and nursing aide, orderly and attendant. The authors conclude that the study supports an association between occupation and cirrhosis mortality and, furthermore, that the greatest cirrhosis mortality is associated with low-status employment and jobs where alcohol is easily available (Harford and Brooks 1992).
In their 1989 study of occupational skin disease, the British Association of Dermatologists found that of 2,861 reported cases (of which 96%were contact dermatitis), the occupation of “cleaners and domestics” was the second-highest category of work listed for women (8.4%) (Cherry, Beck and Owen-Smith 1994). Similarly, in positive responses to dermatological patch tests performed on 6,818 patients, the most common professions of women studied were housekeeper, office worker, cleaner, needleworker and cosmetologist. Housework accounted for 943 of the positive responses to the patch tests (Dooms-Goossens 1986).
Other research has pointed to respiratory allergy and disease. Organic chemical-induced occupational allergic lung diseases were reviewed, and the category of domestic workers was noted as one occupation particularly affected by respiratory allergens (Pepys 1986). A Swedish study on mortality due to asthma looked at women who reported employment in the 1960 National Census. Smoking-adjusted standardized mortality ratios were calculated for each occupation. Increased mortality due to asthma was seen in caretakers, maids, waitresses and housekeepers (Horte and Toren 1993).
There is a lack of statistics and health information concerning domestic workers, especially for overseas immigrant workers, perhaps because of these workers’ temporary or even illegal status in their countries of employment. Governmental acknowledgement will only help enable more research and protection of these workers’ health.
Environmental Issues
Many of the processes described in the articles in this chapter can generate hazardous waste such as solvents, acids, alkalis, formaldehyde and so forth.
In dry cleaning, there has been concern about perchloroethylene vapours polluting the air of apartments above the dry-cleaning shops. The installation of machinery for purification and recovery of solvent vapours, the centralization of dry cleaning (using local shops just as drop-off and pickup places) and the development of wet cleaning methods that minimize solvent use are all methods that can minimize these problems.
Funeral parlours using embalming generate both chemical hazardous waste (e.g., formaldehyde) and biological hazardous waste (blood and blood-containing materials). Most countries where embalming is practised require these to be disposed of as hazardous waste. In crematoria, airborne mercury contamination can result from mercury amalgam fillings in teeth.
Most cosmetology shops that generate chemical waste pour it down the drain or place containers with residues in the trash. This is also true of cleaning personnel, both in homes and in institutions, who can generate waste in the form of solvents, acids and other cleaning products containing hazardous chemicals. The existence of many generators individually producing small amounts of waste creates a control problem; focused and standard control technologies are not easily implemented in these cases. For example, even in large institutions like hospitals, the cleaning chemicals are used in small amounts throughout the building, with cleaning chemicals often stored at many locations.
There are several solutions to this problem. One is the ongoing development of less hazardous substitutes, especially the replacement of solvents with water-based products. Another solution is the adoption of procedures to ensure that only the amounts of products needed for the near future are purchased, to avoid the accumulation of old products that must be disposed of. Using all the product in a container before discarding it in the trash can reduce the pollution from that source. In recent years, some countries, like the United States and Canada, have established local household hazardous waste programmes where waste such as solvents and cleaning products can be taken to central collection points that will accept the hazardous waste free of charge and dispose of it according to proper procedures.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."