20. Development, Technology and Trade
Chapter Editor: Jerry Jeyaratnam
Table of Contents
Figures and Tables
Occupational Health Trends in Development
Jerry Jeyaratnam
Industrialized Countries and Occupational Health and Safety
Toshiteru Okubo
Case Studies in Technological Change
Michael J. Wright
Small Enterprises and Occupational Health and Safety
Bill Glass
Transfer of Technology and Technological Choice
Joseph LaDou
Free-Trade Agreements
Howard Frumkin
Case Study: World Trade Organization
Product Stewardship and the Migration of Industrial Hazards
Barry Castleman
Economic Aspects of Occupational Health and Safety
Alan Maynard
Case Study: Industrialization and Occupational Health Problems in China
Su Zhi
Tables
Click a link below to view table in the article context.
1. Small-scale enterprises
2. Information from foreign investors
3. Costs of work accidents & health (Britain)
4. Types of economic evaluation
5. Development of China’s township enterprises
6. Country HEPS & OHS coverages in China
7. Compliance rates of 6 hazards in worksites
8. Detectable rates of occupational diseases
9. Hazardous working & employers, China
10. OHS background in foreign-funded enterprises
11. Routine instruments for OHS, 1990, China
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Occupational Health Trends in Development
This article discusses some of the currently specific concerns and issues relating to occupational health in the developing world and elsewhere. The general technical subjects common to both the developed and the developing world (e.g., lead and pesticides) are not dealt with in this article as they have been addressed elsewhere in the Encyclopaedia. In addition to the developing countries, some of the emerging occupational health issues of the Eastern European nations too have been addressed separately in this chapter.
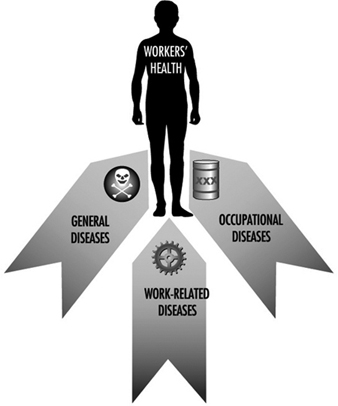
It is estimated that by the year 2000 eight out of ten workers in the global workforce will be from the developing world, demonstrating the need to focus on the occupational health priority needs of these nations. Furthermore, the priority issue in occupational health for these nations is a system for the provision of health care to their working population. This need fits in with the World Health Organization (WHO) definition of occupational health, which expresses the concern for the total health of the worker and is not confined merely to occupational diseases. As shown in figure 1 the worker may be affected by the general diseases of the community which may occur among workers, such as malaria, as well as multi-factorial work-related diseases, in which work may contribute to or aggravate the condition. Examples are cardiovascular diseases, psychosomatic illnesses and cancers. Finally, there are the occupational diseases, in which exposure at the workplace is essential to causation, such as with lead poisoning, silicosis or noise-induced deafness.
Figure 1. Categories of disease affecting workers
The WHO philosophy recognizes the two-way relationship between work and health, as represented in figure 2. Work may have an adverse or beneficial effect on health, while the health status of the worker has an impact on work and productivity.
Figure 2. Two-way relationship between work and health
A healthy worker contributes positively to productivity, quality of products, work motivation and job satisfaction, and thereby to the overall quality of life of individuals and society, making health at work an important policy goal in national development. To achieve this goal, the WHO has recently proposed the Global Strategy on Occupational Health for All (WHO 1995), in which the ten priority objectives are:
- strengthening of international and national policies for health at work and developing the necessary policy tools
- development of healthy work environment
- development of healthy work practices and promotion of health at work
- strengthening of occupational health services
- establishment of support services for occupational health
- development of occupational health standards based on scientific risk assessment
- development of human resources for occupational health
- establishment of registration and data systems, development of information services for experts, effective transmission of data and raising of public awareness through public information
- strengthening of research
- development of collaboration in occupational health and with other activities and services.
Occupational Health and National Development
It is useful to view occupational health in the context of national development as the two are intimately linked. Every nation wishes to be in a state of advanced development, but it is the countries of the developing world which are most anxious—almost demanding—for rapid development. More often than not, it is the economic advantages of such development which are most sought after. True development is, however, generally understood to have a wider meaning and to encompass the process of improving the quality of human life, which in turn includes aspects of economic development, of improving self-esteem and of increasing people’s freedom to choose. Let us examine the impact of this development on the health of the working population, i.e., development and occupational health.
While the global gross domestic product (GDP) has remained almost unchanged for the period 1965-89, there has been an almost tenfold increase in the GDP of the developing world. But this rapid economic growth of the developing world must be seen in the context of overall poverty. With the developing world constituting three quarters of the world’s population, it accounts for only 15% of the global domestic product. Taking Asia as a case in point, all of the countries of Asia except for Japan are categorized as part of the developing world. But it needs to be recognized that there is no uniformity of development even among the developing nations of Asia. For instance, today, countries and areas such as Singapore, Republic of Korea, Hong Kong and Taiwan (China) have been categorized as newly industrialized countries (NICs). Though arbitrary, this implies a transition stage from developing country status to industrialized nation status. However, it must be recognized that there are no clear criteria defining a NIC. Nevertheless, some of the salient economic features are high sustained growth rates, diminishing income inequality, an active government role, low taxes, underdeveloped welfare state, high savings rate and an economy geared to exports.
Health and Development
There exists an intimate relationship between health, development and the environment. Rampant and uncontrolled development measures purely in terms of economic expansion could, under certain circumstances, be considered to have an adverse impact on health. Usually, though, there exists a strong positive relationship between a nation’s economic status and health as indicated by life expectancy.
As much as development is positively linked to health, it is not adequately recognized that health is a positive force driving development. Health must be considered to be more than a consumer item. Investing in health increases the human capital of a society. Unlike roads and bridges, whose investment values dwindle as they deteriorate over time, the returns on health investments can generate high social returns for a lifetime and well into the next generation. It should be recognized that any health impairment that the worker may suffer is likely to have an adverse effect on work performance, a matter of considerable interest particularly to nations in the throes of rapid development. For instance, it is estimated that poor occupational health and reduced working capacity of workers may cause an economic loss of up to 10 to 20% of gross national product (GNP). Furthermore, the World Bank estimates that two-thirds of occupationally determined disability adjusted life years (DALYS) could be prevented by occupational health and safety programmes. As such, the provision of an occupational health service should not be viewed as a national expense to be avoided, but rather as one that is necessary for the national economy and development. It has been observed that a high standard of occupational health correlates positively with a high GNP per capita (WHO 1995). The countries investing most in occupational health and safety show the highest productivity and strongest economies, while countries with the lowest investment have the lowest productivity and the weakest economies. Globally, each worker is said to contribute US$9,160 to the annual domestic product. Evidently the worker is the engine of the national economy and the engine needs to be kept in good health.
Development results in many changes to the social fabric, including the pattern of employment and changes in the productivity sectors. In the early stages of development, agriculture contributes extensively to national wealth and the workforce. With development, the role of agriculture begins to decline and the contribution of the manufacturing sector to national wealth and the workforce becomes dominant. Finally, there comes a situation where the service sector becomes the largest income source, as in the advanced economies of industrialized countries. This is clearly evident when a comparison is made between the group of NICs and the group of Association of Southeast Asian (ASEAN) nations. The latter could be categorized as middle income nations of the developing world, while the NICs are countries straddling the developing and the industrialized worlds. Singapore, a member of ASEAN, is also a NIC. The ASEAN nations, though deriving approximately a quarter of their gross domestic product from agriculture, have almost half of their GDP drawn from industry and manufacturing. The NICs, on the other hand, particularly Hong Kong and Singapore, have approximately two-thirds of their GDP from the service sector, with very little or none from agriculture. The recognition of this changing pattern is important in that occupational health services must respond to the needs of each nation’s workforce depending on their stage of development (Jeyaratnam and Chia 1994).
In addition to this transition in the workplace, there also occurs a transition in disease patterns with development. A change in disease patterns is seen with increasing life expectancy, with the latter indicative of increasing GDP. It is seen that with development or an increase in life expectancy, there is a large decrease in death from infectious diseases while there are large increases in deaths from cardiovascular diseases and cancers.
Occupational Health Concerns and Development
The health of the workforce is an essential ingredient for national development. But, at the same time, adequate recognition of the potential pitfalls and dangers of development must be recognized and safeguarded against. The potential damage to human health and the environment consequent to development must not be ignored. Planning for development can avert and prevent harms associated therewith.
Lack of adequate legal and institutional structure
The developed nations evolved their legal and administrative structure to keep pace with their technological and economic advancements. In contrast, the countries of the developing world have access to the advanced technologies from the developed world without having developed either legal or administrative infrastructure to control their adverse consequences to the workforce and the environment, causing a mismatch between technological development and social and administrative development.
Further, there is also careless disregard of control mechanisms for economic and/or political reasons (e.g., the Bhopal chemical disaster, where an administrator’s advice was overruled for political and other reasons). Often, the developing countries will adopt standards and legislation from the developed countries. There is, however, a lack of trained personnel to administer and enforce them. Furthermore, such standards are often inappropriate and have not taken into account differences in nutritional status, genetic predisposition, exposure levels and work schedules.
In the area of waste management, most developing countries do not have an adequate system or a regulatory authority to ensure proper disposal. Although the absolute amount of waste produced may be small in comparison to developed countries, most of the wastes are disposed of as liquid wastes. Rivers, streams and water sources are severely contaminated. Solid wastes are deposited on land sites without proper safeguards. Furthermore, developing countries have often been the recipients of hazardous wastes from the developed world.
Without proper safeguards in hazardous waste disposal, the effects of environmental pollution will be seen for several generations. Lead, mercury and cadmium from industrial waste are known to contaminate water sources in India, Thailand and China.
Lack of proper planning in siting of industries and residential areas
In most countries, the planning of industrial areas is undertaken by the government. Without the presence of proper regulations, residential areas will tend to congregate around such industrial areas because the industries are a source of employment for the local population. Such was the case in Bhopal, India, as discussed above, and the Ulsan/Onsan industrial complex of the Republic of Korea. The concentration of industrial investment in the Ulsan/Onsan complex brought about a rapid influx of population to Ulsan City. In 1962, the population was 100,000; within 30 years, it increased to 600,000. In 1962, there were 500 households within the boundaries of the industrial complex; in 1992, there were 6,000. Local residents complained of a variety of health problems that are attributable to industrial pollution (WHO 1992).
As a result of such high population densities in or around the industrial complexes, the risk of pollution, hazardous wastes, fires and accidents is greatly multiplied. Furthermore, the health and future of the children living around these areas are in real jeopardy.
Lack of safety-conscious culture among workers and management
Workers in developing countries are often inadequately trained to handle the new technologies and industrial processes. Many workers have come from a rural agricultural background where the pace of work and type of work hazards are completely different. The educational standards of these workers are often much lower as compared to the developed countries. All these contribute to a general state of ignorance on health risks and safe workplace practices. The toy factory fire in Bangkok, Thailand, discussed in the chapter Fire, is an example. There were no proper fire safety precautions. Fire exits were locked. Flammable substances were poorly stored and these had blocked all the available exits. The end result was the worst factory fire in history with a death toll of 187 and another 80 missing (Jeyaratnam and Chia 1994).
Accidents are often a common feature because of a lack of commitment of management to the health and safety of the workers. Part of the reason is the lack of skilled personnel in maintaining and servicing industrial equipment. There is also a lack of foreign exchange, and government import controls make it difficult to obtain proper spare parts. High turnover of workers and the large readily available labour market also make it unprofitable for management to invest heavily in workers’ training and education.
Transfer of hazardous industries
Hazardous industries and unsuitable technologies in the developed countries are often transferred to the developing countries. It is cheaper to transfer the entire production to a country where the environmental and health regulations are more easily and cheaply met. For example, industries in the Ulsan/Onsan industrial complex, Republic of Korea, were applying emission control measures in keeping with local Korean legislation. These were less stringent than in the home country. The net effect is a transfer of potentially polluting industries to the Republic of Korea.
High proportion of small-scale industries
Compared to the developed countries, the proportion of small-scale industries and the proportion of workers in these industries are higher in the developing countries. It is more difficult in these countries to maintain and enforce compliance in occupational health and safety regulations.
Lower health status and quality of health care
With economic and industrial development, new health hazards are introduced against a backdrop of poor health status of the population and a less than adequate primary health care system. This will further tax the limited health care resources.
The health status of workers in the developing countries is often lower compared to that of workers in developed countries. Nutritional deficiencies and parasitic and other infectious diseases are common. These can increase the susceptibility of the worker to developing occupational diseases. Another important observation is the combined effect of workplace and non-workplace factors on the health of the worker. Workers with nutritional anaemias are often very sensitive to very low levels of inorganic lead exposure. Significant anaemias are often seen with blood lead levels of around 20 μg/dl. A further example is seen among workers with congenital anaemias like thalassaemias, the carrier rate for which in some countries is high. It has been reported that these carriers are very sensitive to inorganic lead, and the time taken for the haemoglobin to return to normal is longer than in non-carriers.
This situation reveals a narrow dividing line between traditional occupational diseases, work-related diseases and the general diseases prevalent in the community. The concern in the countries of the developing world should be for the overall health of all people at work. In order to achieve this objective, the nation’s health sector must accept responsibility for organizing a programme of work for the provision of health care services for the working population.
It must also be recognized that the labour sector has an important role in ensuring the safety of the work environment. In order to achieve this, there is a need to review legislation so that it covers all workplaces. It is inadequate to have legislation limited to factory premises. Legislation should not only provide a secure and safe workplace, but also ensure the provision of regular health services to the workers.
Thus it would be evident that two important sectors, namely the labour sector and the health sector, have important roles to play in occupational health. This recognition of the intersectoriality of occupational health is an extremely important ingredient for the success of any such programme. In order to achieve proper coordination and cooperation between these two sectors, it is necessary to develop an intersectorial coordinating body.
Finally, legislation for the provision of occupational health services and ensuring the safety of the workplace is fundamental. Again, many Asian countries have recognized this need and have such legislation today, although its implementation may be wanting to some extent.
Conclusions
In developing countries, industrialization is a necessary feature of economic growth and development. Although industrialization can bring about adverse health effects, the accompanying economic development can have many positive effects on human health. The aim is to minimize the adverse health and environmental problems and maximize the benefits of industrialization. In the developed countries, experience from the adverse effects of the Industrial Revolution has led to regulation of the pace of development. These countries have generally coped fairly well and had the time to develop all the necessary infrastructure to control both health and environmental problems.
The challenge today for the developing countries who, because of international competition, do not have the luxury of regulating their pace of industrialization, is to learn from the mistakes and lessons of the developed world. On the other hand, the challenge for the developed countries is to assist the developing countries. The developed countries should not take advantage of the workers in developing countries or their lack of financial capacity and regulatory mechanisms because, at the global level, environmental pollution and health problems do not respect political or geographical boundaries.
Industrialized Countries and Occupational Health and Safety
Overview
Economic activity, as expressed by per capita gross national product (GNP), differs substantially between developing countries and industrialized countries. According to a ranking by the World Bank, the GNP of the country heading the list is approximately fifty times that of the country at the bottom. The share of the world’s total GNP by the member countries of the Organization for Economic Co-operation and Development (OECD) is almost 20%.
OECD member countries account for almost one-half the world’s total energy consumption. Carbon dioxide emissions from the top three countries account for 50% of the earth’s total burden; these countries are responsible for major global pollution problems. However, since the two oil crises in 1973 and 1978, industrialized countries have been making efforts to save energy by replacing old processes with more efficient types. Simultaneously, heavy industries consuming much energy and involving much heavy labour and exposure to hazardous or dangerous work have been moving from these countries to less industrialized countries. Thus, the consumption of energy in developing countries will increase in the next decade and, as this occurs, problems related to environmental pollution and occupational health and safety are expected to become more serious.
In the course of industrialization, many countries experienced ageing of the population. In the major industrialized nations, those 65 years or older account for 10 to 15% of the total population. This is a significantly higher proportion than that of developing countries.
This disparity reflects the lower reproduction rate and lower mortality rates in the industrialized countries. For example, the reproduction rate in industrialized countries is less than 2%, whereas the highest rates, more than 5%, are seen in African and Middle Eastern countries and 3% or more is common in many developing countries. The increased proportion of female workers, ranging from 35 to 50% of the work force in industrialized countries (it is usually under 30% in less industrialized countries), may be related to the decreased number of children.
Greater access to higher education is associated with a higher proportion of professional workers. This is another significant disparity between industrialized and developing countries. In the latter, the proportion of professional workers has never exceeded 5%, a figure in sharp contrast to the Nordic countries, where it ranges from 20 to 30%. The other European and the North American countries fall in between, with professionals making up more than 10% of the workforce. Industrialization depends primarily on research and development, work that is associated more with excess stress or strain in contrast to the physical hazards characteristic of much of the work in developing countries.
Current Status of Occupational Health and Safety
The economic growth and the changes in the structure of major industries in many industrializing countries has been associated with reduced exposure to hazardous chemicals, both in terms of the levels of exposure and the numbers of workers exposed. Consequently, instances of acute intoxication as well as typical occupational diseases are diminishing. However, the delayed or chronic effects due to exposures many years previously (e.g., pneumoconiosis and occupational cancer) are still seen even in the most industrialized countries.
At the same time, technical innovations have introduced the use of many newly created chemicals into industrial processes. In December, 1982, to guard against the hazards presented by such new chemicals, OECD adopted an international recommendation on a Minimum Premarketing Set of Data for Safety.
Meanwhile, life in the workplace and in the community have continued to become more stressful than ever. The proportions of troubled workers with problems related to or resulting in alcohol and/or drug abuse and absenteeism have been on the rise in many industrialized countries.
Work injuries have been decreasing in many industrialized countries largely due to progress in safety measures at work and the extensive introduction of automated processes and equipment. The reduction of the absolute number of workers engaging in more dangerous work due to the change of industrial structure from heavy to light industry is also an important factor in this decrease. The number of workers killed in work accidents in Japan decreased from 3,725 in 1975 to 2,348 in 1995. However, analysis of the time trend indicates that the rate of decrease has been slowing over the past ten years. The incidence of work injuries in Japan (including fatal cases) fell from 4.77 per one million working hours in 1975 to 1.88 in 1995; a rather slower decrease was seen in the years 1989 to 1995. This bottoming out of the trend toward reductions in industrial accidents has also been seen in some other industrialized countries; for example, the frequency of work injuries in the United States has not improved for more than 40 years. In part, this reflects the replacement of classic work accidents which can be prevented by various safety measures, by the new types of accidents caused by the introduction of automated machines in these countries.
The ILO Convention No. 161 adopted in 1985 has provided an important standard for occupational health services. Even though its scope includes both developing and developed countries, its fundamental concepts are based on existing programmes and experience in industrialized countries.
The basic framework of an occupational health service system of a given country is generally described in legislation. There are two major types. One is represented by the United States and the United Kingdom, in which the legislation stipulates only the standards to be satisfied. Achievement of the goals is left to the employers, with the government providing information and technical assistance on request. Verifying compliance with the standards is a major administrative responsibility.
The second type is represented by the legislation of France, which not only prescribes the goals but also details the procedures for reaching them. It requires employers to provide specialized occupational health services to the employees, using physicians who have become certified specialists, and it requires service institutions to offer such services. It specifies the number of workers to be covered by the appointed occupational physician: in worksites without a hazardous environment more than 3,000 workers can be covered by a single physician, whereas the number is smaller for those exposed to defined hazards.
Specialists working in the occupational health setting are expanding their target fields in the industrialized countries. Physicians have become more specialized in preventive and health management than ever before. In addition, occupational health nurses, industrial hygienists, physiotherapists and psychologists are playing important roles in these countries. Industrial hygienists are popular in the United States, while environment measurement specialists are much more common in Japan. Occupational physiotherapists are rather specific to the Nordic countries. Thus, there are some differences in the kind and distribution of existing specialists by region.
Establishments with more than several thousand workers usually have their own independent occupational health service organization. Employment of specialists including those other than occupational physicians, and provision of the minimum facilities necessary to provide comprehensive occupational health services, are generally feasible only when the size of the workforce exceeds that level. Provision of occupational health services for small establishments, especially for those with only a few workers, is another matter. Even in many industrialized countries, occupational health service organizations for smaller-scale establishments have not yet been established in a systematic manner. France and some other European countries have legislation articulating minimum requirements for the facilities and services to be provided by occupational health service organizations, and each enterprise without its own service is required to contract with one such organization to provide the workers with the prescribed occupational health services.
In some industrialized countries, the content of the occupational health programme is focused mainly on preventive rather than on curative services, but this is often a matter of debate. In general, countries with a comprehensive community health service system tend to limit the area to be covered by the occupational health programme and regard treatment as a discipline of community medicine.
The question of whether periodic health check-ups should be provided for the ordinary worker is another matter of debate. Despite the view held by some that check-ups involving general health screening have not proven to be beneficial, Japan is one of a number of countries in which a requirement that such health examinations be offered to employees has been imposed on employers. Extensive follow-up, including continuing health education and promotion, is strongly recommended in such programmes, and longitudinal record keeping on an individual basis is considered indispensable for achieving its goals. Evaluation of such programmes requires long-term follow-up.
Insurance systems covering medical care and compensation for workers involved in work-related injuries or diseases are found in almost all industrialized countries. However, there is much variation among these systems with regard to management, coverage, premium payment, types of benefits, extent of the commitment to prevention, and the availability of technical support. In the United States, the system is independent in each state, and private insurance companies play a large role, whereas in France the system is managed completely by the government and incorporated extensively into the occupational health administration. Specialists working for the insurance system often play an important part in technical assistance for the prevention of occupational accidents and diseases.
Many countries provide a post-graduate educational system as well as residency training courses in occupational health. The doctorate is usually the highest academic degree in occupational health, but specialist qualification systems also exist.
The schools of public health play an important part in the education and training of occupational health experts in the United States. Twenty-two of the 24 accredited schools provided occupational health programmes in 1992: 13 provided programmes in occupational medicine and 19 had programmes in industrial hygiene. The occupational health courses offered by these schools do not necessarily lead to an academic degree, but they are closely related to the accreditation of specialists in that they are among the qualifications needed to qualify for the examinations that must be passed in order to become a diplomat of one of the boards of specialists in occupational health.
The Educational Resource Program (ERC), funded by the National Institute for Occupational Safety and Health (NIOSH), has been supporting residency programmes at these schools. The ERC has designated 15 schools as regional centres for the training of occupational health professionals.
It is often difficult to arrange education and training in occupational health for physicians and other health professionals who are already involved in primary health care services in the community. A variety of distance-learning methods have been developed in some countries—for example, a correspondence course in the United Kingdom and a telephone communication course in New Zealand, both of which have received good evaluations.
Factors Influencing Occupational Health and Safety
Prevention at the primary, secondary and tertiary levels should be a basic aim of the occupational safety and health programme. Primary prevention through industrial hygiene has been highly successful in decreasing the risk of occupational disease. However, once a level sufficiently below the permissible standard has been reached, this approach becomes less effective, especially when cost/benefit is taken into consideration.
The next step in primary prevention involves biological monitoring, focusing on differences in individual exposure. Individual susceptibility is also important at this stage. Determination of fitness to work and allocation of reasonable numbers of workers to particular operations are receiving increasing attention. Ergonomics and various mental health techniques to reduce stress at work represent other indispensable adjuncts in this stage.
The goal of preventing worksite exposures to hazards has been gradually overshadowed by that of health promotion. The final goal is to establish self-management of health. Health education to achieve this end is regarded as a major area to be covered by specialists. The Japanese government has launched a health promotion programme entitled “Total Health Promotion Plan”, in which the training of specialists and financial support for each worksite programme are major components.
In most industrialized countries, labour unions play an important part in occupational health and safety efforts from the central to peripheral levels. In many European countries union representatives are officially invited to be members of committees responsible for deciding the basic administrative directions of the programme. The mode of labour commitment in Japan and the United States is indirect, while the government ministry or department of labour wields administrative power.
Many industrialized countries have a workforce which comes from outside the country both officially and unofficially. There are various problems presented by these immigrant workers, including language, ethnic and cultural barriers, educational level, and poor health.
Professional societies in the field of occupational health play an important part in supporting training and education and providing information. Some academic societies issue specialist certification. International cooperation is also supported by these organizations.
Projections for the Future
Coverage of workers by specialized occupational health services is still not satisfactory except in some European countries. As long as provision of the service remains voluntary, there will be many uncovered workers, especially in small enterprises. In high-coverage countries like France and some Nordic countries, insurance systems play an important part in the availability of financial support and/or technical assistance. To provide services for small establishments, some level of commitment by social insurance may be necessary.
Occupational health service usually proceeds faster than community health. This is especially the case in large companies. The result is a gap in services between occupational and community settings. Workers receiving better health service throughout working life frequently experience health problems after retirement. Sometimes, the gap between large and small establishments cannot be ignored as, for example, in Japan, where many senior workers continue to work in smaller companies after mandatory retirement from large companies. The establishment of a continuity of services between these different settings is a problem that will inevitably have to be addressed in the near future.
As the industrial system becomes more complicated, control of environmental pollution becomes more difficult. An intensive anti-pollution activity in a factory may simply result in moving the pollution source to another industry or factory. It may also lead to the export of the factory with its pollution to a developing country. There is a growing need for integration between occupational health and environmental health.
Case Studies in Technological Change
Changes in plant technologies production pressures and the need for continually training workers are essential to the safe and healthful environment. The following three examples occurred in the United States. Technological change affects all workers around the world.
Production versus Safety
Production pressures can severely compromise safety and health unless management is careful to analyse the potential consequences of decisions designed to increase productivity. One example comes from a 1994 accident in a small steel plant in the United States.
At about 4:00 a.m. several workers were preparing to tap molten steel from an electric arc furnace. The steel market was good and the enterprise was selling all the steel it could produce. Workers were on heavy overtime schedules and the plant was working at full capacity. The furnace had been scheduled for a shutdown in order to replace its refractory lining, which had worn dangerously thin. Hot spots had already developed in the furnace shell, but the company wanted a couple of final batches of steel.
As the tap began, the lining of the vessel burned through. Steel and slag poured from the break and quickly melted through a water line supplying the cooling system for the furnace. The water exploded into steam with tremendous force. Two workers were in the path. Both were severely burned. One of them died three days later.
One obvious cause of the accident was operating the furnace beyond the safe life of its refractory lining. In addition, electric furnaces are generally designed to keep the main cooling water lines above the height of the molten steel and slag at all times, in order to prevent exactly this kind of accident. However, this furnace had been modified in the recent past to increase its capacity by raising the level of the molten material, and the engineers overlooked the water line. A simple breakout of molten metal and slag would have been serious, but without the water line it would not have caused a steam explosion, and the injuries would not have been as severe. Both factors resulted from the demand for productivity without sufficient concern for safety.
Training
Worker training should include more than a set of specific safety rules. The best safety training conveys a comprehensive understanding of the process, equipment and potential hazards. It is important that workers understand the reason for each safety rule and can respond to unforeseen situations not covered by the rules.
The importance of comprehensive training is illustrated by a 1986 accident in a North American steel plant. Two workers entered a furnace vessel in order to remove scaffolding that had been used to reline the vessel with new refractory brick. The workers followed a detailed “job safety analysis”, which outlined each step in the operation. However, the job safety analysis was defective. The vessel had been refitted two years previously with a system for blowing argon gas through the molten metal, in order to stir it more effectively, and the job safety analysis had never been updated to account for the new argon system.
Another work crew reconnected the argon system shortly before the two workers entered the vessel. The valves were leaking, and the lines had not been blanked out. The atmospheric test required for confined space entry was not properly done and the workers who entered the vessel were not present to observe the test.
Both workers died from oxygen deficiency. A third worker entered the vessel in a rescue effort, but was himself overcome. His life was saved by a fourth worker, who cut the end from a compressed air hose and threw the hose in the vessel, thus providing oxygen to the unconscious victim.
One obvious cause of the accident was the failure of the enterprise to update the job safety analysis. However, comprehensive training in the process, equipment and hazards might have enabled the workers to identify the deficiencies in the job analysis and take steps to ensure that they could enter the vessel safely.
Technological Change
The importance of analysing new or changed technology is illustrated by a 1978 accident in a North American chemical plant. The enterprise was reacting toluene and other organic chemicals in a closed vessel. The reaction was driven by heat, which was supplied to the vessel through a heating coil with circulating hot water. The plant engineering department decided to replace the water with molten sodium nitrate, in order to speed the reaction. However, the coil had been repaired with braising compounds which melted at a temperature lower than the temperature of the sodium nitrate. As a result, sodium nitrate began to leak into the vessel, where it reacted with the organic compounds to form unstable organic nitrates.
The subsequent explosion injured several workers, destroyed the reactor vessel, and damaged the building. However, the consequences could have been much worse. The accident happened late at night, when no workers were near the vessel. In addition, hot shrapnel entered a nearby process unit containing large amounts of diethyl ether. Fortunately, none of those vessels or lines were hit. An explosion on the day shift, or one which released a vapour cloud of diethyl ether, could have caused multiple deaths.
Small Enterprises and Occupational Health and Safety
Small workplaces have been a characteristic mode of production since earliest times. Cottage industries where members of a family work on the basis of a division of labour still exist in both urban and rural situations to this day. In fact, it is true of all countries that the majority of workers, paid or unpaid, work in enterprises which can be classified as small.
Before defining their health problems, it is necessary to define a small enterprise. It is generally recognized that a small enterprise is one employing 50 or fewer workers. It may be located in the home, a farm, a small office, a factory, mine or quarry, a forestry operation, a garden or a fishing boat. The definition is based on the number of workers, not what they do or whether they are paid or unpaid. The home is clearly a small enterprise.
Common Features of Small Enterprises
Common features of small enterprises include (see table 1):
- They are likely to be undercapitalized.
- They are usually non-unionized (the home and the farm in particular) or under-unionized (office, factory, food shop, etc.).
- They are less likely to be inspected by government agencies. In fact, a study carried out some years ago indicated that the existence of many small enterprises was not even known to the government department responsible for them (Department of Community Health 1980).
Table 1. Features of small-scale enterprises and their consequences
Lack of capital
- poor environmental conditions
- cheaper raw materials
- inferior equipment maintenance
- inadequate personal protection
Non- or under-unionization
- inferior pay rates
- longer working hours
- non-compliance with award conditions
- exploitation of child labour
Inferior inspection services
- poor environmental conditions
- greater hazard level
- higher injury/illness rates
As a result, workplace environmental conditions, which generally reflect available capital, are inevitably inferior to those in larger enterprises: cheaper raw materials will be purchased, maintenance of machinery will be reduced and personal protective equipment will be less available.
Under- or non-unionization will lead to inferior pay rates, longer working hours and non-compliance with award conditions. Work will often be more intensive and children and old people are more likely to be exploited.
Inferior inspection services will result in poorer working environments, more workplace hazards and higher injury and illness rates.
These characteristics of small enterprises place them at the edge of economic survival. They come into and go out of existence on a regular basis.
To balance these significant disadvantages, small enterprises are flexible in their productive systems. They can respond quickly to change and often develop imaginative and flexible solutions to the requirements of technical challenge. At a social level, the owner is usually a working manager and interacts with the workers on a more personal level.
There is evidence to support these beliefs. For example, one US study found that the workers in neighbourhood panel beating shops were regularly exposed to solvents, metal pigments, paints, polyester plastic fumes and dust, noise and vibration (Jaycock and Levin 1984). Another US survey showed that multiple short-term exposures to chemical substances were characteristic of small industries (Kendrick, Discher and Holaday 1968).
A Finnish study investigating this occurrence in 100 workplaces found that short-duration exposures to chemicals were typical in small industry and that the duration of exposure increased as the firm grew (Vihina and Nurminen 1983). Associated with this pattern were multiple exposures to different chemicals and frequent exposures to peak levels. This study concluded that chemical exposure in small enterprises is complex in character.
Perhaps the most dramatic illustration of the impact of size on occupational health risk was presented at the Second International Workshop on Benzene in Vienna, 1980. For most of the delegates from the petroleum industry, benzene posed little health risk in the workplace; their workplaces employed sophisticated medical, hygiene and engineering techniques to monitor and eliminate any potential exposure. In contrast, a delegate from Turkey when commenting on the boot-making industry, which to a large extent was a cottage industry carried out in the home, reported that men, women and children were exposed to high concentrations of “an unlabelled solvent”, benzene, which resulted in the occurrence of anaemias and leukaemias (Aksoy et al. 1974). The difference in exposure in the two situations was a direct consequence of workplace size and the more intimate contact of the workers in the cottage-style, boot-making industry, compared with the large-scale petroleum enterprises.
Two Canadian researchers have identified the main difficulties faced by small businesses as: a lack of awareness of health hazards by managers; the higher cost per worker to reduce these hazards; and an unstable competitive climate which makes it unlikely that such businesses can afford to implement the safety standards and regulations (Lees and Zajac 1981).
Thus, much of the experience and recorded evidence indicate that the workers in small enterprises constitute an under-served population from the standpoint of their health and safety. Rantanan (1993) attempted a critical review of available sources for the WHO Interregional Task Group on Health Protection and Health Promotion of Workers in Small Scale Industries, and found that reliable quantitative data on illnesses and injuries to workers in small-scale industries are unfortunately sparse.
In spite of the lack of reliable quantitative data, experience has demonstrated that the characteristics of small-scale industries result in a greater likelihood of musculoskeletal injuries, lacerations, burns, puncture wounds, amputations and fractures, poisonings from inhalation of solvents and other chemicals and, in the rural sector, pesticide poisonings.
Serving the Health Needs of Workers in Small-Scale Enterprises
The difficulty in serving the health and safety needs of workers in small enterprises stems from a number of features:
- Rural enterprises are often isolated as a result of being located at a distance from main centres with bad roads and poor communications.
- Workers on small fishing vessels or in forestry operations also have limited access to health and safety services.
- The home, where most cottage industry and unpaid “housework” is located, is frequently ignored in health and safety legislation.
- Educational levels of workers in small-scale industries are likely to be lower as a result of leaving school earlier or the lack of access to schools. This is accentuated by the employment of children and migrant workers (legal and illegal) who have cultural and language difficulties.
- Although it is clear that small-scale enterprises contribute significantly to the gross domestic product, the fragility of the economies in developing countries makes it difficult to provide funds to serve the health and safety needs of their workers.
- The great number and variability of small-scale enterprises make it difficult to effectively organize health and safety services for them.
In summary, workers in small-scale enterprises have certain characteristics which make them vulnerable to health problems and make it difficult to provide them with health care. These include:
- Inaccessibility to available health services for geographic or economic reasons and a willingness to tolerate unsafe and unhealthy conditions of work, primarily because of poverty or ignorance.
- Deprivation because of poor education, housing, transport and recreation.
- An inability to influence policy making.
What are the Solutions?
These exist at several levels: international, national, regional, local and workplace. They involve policy, education, practice and funding.
A conceptual approach was developed at the Colombo meeting (Colombo Statement 1986), although this looked particularly at developing countries. A restatement of these principles as applicable to small-scale industry, wherever it is located, follows:
- National policies need to be formulated to improve health and safety of all workers in small-scale industries with special emphasis on education and training of managers, supervisors and workers and the means of ensuring that they receive adequate information to protect the health and safety of all workers.
- Occupational health services for small-scale industries need to be integrated with the existing health systems providing primary health care.
- Adequate training for occupational health personnel is needed. This should be tailored to the type of work carried out, and would include training for primary health care workers and specialists as well as the public health inspectors and nurses mentioned above.
- Adequate communication systems are needed to ensure the free flow of occupational health and safety information among workers, management and occupational health personnel at all levels.
- Occupational health care for small isolated groups through primary health care workers (PHCWs) or their equivalent should be provided. In rural areas, such a person is likely to be providing general health care on a part-time basis and an occupational health content can be added. In small urban workplaces, such a situation is less likely. Persons from the workforce selected by their fellow workers will be needed.
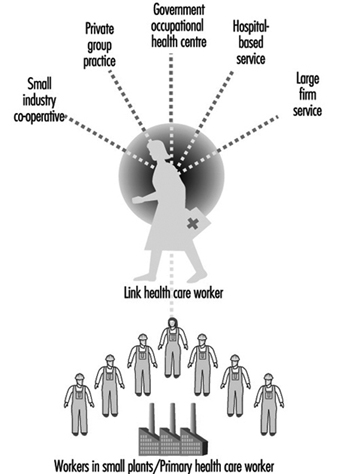
- These rural and urban PHCWs, who will require initial and ongoing training and supervision, need to be linked to the existing health services. The “link health worker” should be an appropriate full-time health professional with at least three years of training. This health professional is the crucial link in the effective functioning of the service. (See figure 1.)
- Occupational hygiene which measures, evaluates and controls environmental hazards, is an essential part of occupational health care. Appropriate occupational hygiene services and skills should be introduced into the service both centrally and peripherally.
Figure 1. Patterns of health care for workers in small plants
Despite the establishment of these principles, very little progress has been made, almost certainly because small workplaces and the workers who work in them are given a low priority in the health service planning of most countries. Reasons for this include:
- lack of political pressure by such workers
- difficulty in servicing the health needs because of such features as isolation, educational levels and innate traditionalism, already mentioned
- the lack of an effective primary health care system.
Approaches to the solution of this problem are international, national and local.
International
A troublesome feature of the global economy is the negative aspects associated with the transfer of technology and the hazardous processes associated with it from developed to developing countries. A second concern is “social dumping”, in which, in order to compete in the global marketplace, wages are lowered, safety standards ignored, hours of work extended, age of employment is lowered and a form of modern-day slavery is instituted. It is urgent that new ILO and WHO instruments (Conventions and Recommendations) banning these practices be developed.
National
All-embracing occupational safety and health legislation is needed, backed up by a will to implement and enforce it. This legislation needs to be supported by positive and widespread health promotion.
Local
There are a number of organizational models for occupational health and safety services which have been successful and which, with appropriate modifications, can accommodate most local situations. They include:
- An occupational health centre can be established in localities where there is a dense population of small workplaces, to provide both accident and emergency treatment as well as education and intervention functions. Such centres are usually supported by government funding, but they may also be funded through a sharing of costs by a number of local small industries, usually on a per-employee basis.
- A big company’s occupational health service may be extended to surrounding small industries.
- A hospital-based occupational health service which already covers accident and emergency services can supplement this with a visiting primary health care service concentrating on education and intervention.
- A service can be provided where a general practitioner provides treatment services in a clinic but uses a visiting occupational health nurse to offer education and intervention in the workplace.
- A specialist occupational health service staffed by a multidisciplinary team comprising occupational physicians, general practitioners, occupational health nurses, physiotherapists and specialists in radiography, pathology and so on, may be established.
- Whatever the model employed, the service must be linked to the workplace by a “link health care worker”, a trained health professional multiskilled in both the clinical and hygiene aspects of the workplace. (See figure 1)
Regardless of the organizational form utilized, the essential functions should include (Glass 1982):
- a centre for training first-aiders among the workers in surrounding small industries
- a centre for the treatment of minor injuries and other work-related health problems
- a centre for the provision of basic biological monitoring including screening examinations of hearing, lung function, vision, blood pressure and so on, as well as the earliest signs of the toxic effects of exposure to occupational hazards
- a centre for the provision of basic environmental investigations to be integrated with the biological monitoring
- a centre for the provision of health and safety education that is directed by or at least coordinated by safety consultants familiar with the kinds of workplaces being served
- a centre from which rehabilitation programmes could be planned, provided and coordinated with return to work.
Conclusion
Small enterprises are a widespread, fundamental and essential form of production. Yet, the workers who work in them frequently lack coverage by health and safety legislation and regulation, and lack adequate occupational health and safety services. Consequently, reflecting the unique characteristics of small enterprises, workers in them have greater exposures to work hazards.
Current trends in the global economy are increasing the extent and the degree of exploitation of workers in small workplaces and, thereby, increasing the risk of exposure to hazardous chemicals. Appropriate international, national and local measures have been designed to diminish such risks and enhance the health and well-being of those working in small-scale enterprises.
Transfer of Technology and Technological Choice
The Recent Period of Rapid Transition
The migration of industry from developed to developing countries is usually explained by the lower cost of labour. Companies also establish operations abroad to reduce transportation costs by producing within foreign markets, to overcome trade barriers and to avoid fluctuations in currency markets. But some companies migrate to developing nations to escape occupational and environmental regulations and enforcement at home. For many nations such investment is the primary source of new jobs.
Foreign companies and investors have been responsible for more than 60% of all industrial investment in developing countries over the past decade. During the 1980s, a global financial market began to emerge. In a span of ten years, international bank lending by the major developed countries rose from 4% of GDP to 44%. Between 1986 and 1990, foreign investment by the United States, Japan, West Germany, France and Britain grew at an annual rate of 27%. Global cross-border investment is now estimated to be $1,700 billion (LaDou and Levy 1995). There are about 35,000 transnational corporations, with 147,000 foreign affiliates. Much of the investment in the developing world comes from these corporations. The total annual sales of the 350 biggest transnational corporations are equal to one-third of the combined gross domestic products of the industrial world and exceed by far that of the developing world.
Most investment in developing countries goes to Asia. Between 1986 and 1990, East and Southeast Asia received $14 billion, Latin America $9 billion and Africa $3 billion. Central Europe is now openly competing for a share of global investment. India, Vietnam, Egypt, Nicaragua and Uzbekistan have recently liberalized their ownership rules to increase their attractiveness to investors.
Japanese companies and investments are found in almost every country in the world. With limited land and great population density, Japan has a pressing need to export its waste-producing industries. European nations have exported hazardous and environmentally outmoded industries to Africa and the Middle East and are now beginning to export them to Central Europe. Western European corporations are the largest investors in Bangladesh, India, Pakistan, Singapore and Sri Lanka.
China and India, with the world’s largest populations, have had dramatic policy reversals in recent years and as a result have welcomed industries from many countries. United States corporations are dominant in China, Indonesia, the Philippines, Thailand and Hong Kong and Taiwan (China). US companies were expected to commit $l billion of investment to Singapore in 1995, up 31% from 1994.
The Industrialized Countries’ Motivation
In the developed countries, industry provides jobs, pays taxes that support community services and is subject to environmental and occupational health laws. As industrialized nations enact laws to limit the environmental hazards associated with many industrial operations, production costs rise and undermine competitive advantages. To offset this problem, manufacturers move many of their hazardous operations to the newly industrialized countries. They are welcomed because the creation of an infrastructure in many developing nations relies on industrial expansion by foreigners.
When industry migrates to developing nations, companies not only take advantage of lower wages, but also benefit from the low tax rates in communities that are not spending much on such things as sewage systems, water treatment plants, schools and public transportation. When companies establish plants in developing countries, their tax burden is a small fraction of what it would be in most developed countries.
Anecdotal evidence in support of the transition
The University of California, the Johns Hopkins University and the University of Massachusetts have all recently studied the health of American semiconductor workers. The studies demonstrate that women have a major increase in the risk of miscarriage when they work in semiconductor plants. Researchers participating in these studies remark that the companies are laying off the workers and shutting down the plants so rapidly that these studies will probably be the last of sufficient size to give reliability to the findings to be conducted with US workers.
Predictions for a reduction in studies on occupational health
The migration of American and Japanese semiconductor companies to Southeast Asia is dramatically demonstrated in the newly industrialized country of Malaysia. Since the mid-1970s, Malaysia has become the world’s third largest semiconductor manufacturer and the world’s largest exporter of semiconductors. It is very unlikely that foreign companies will continue to fund research on occupational and environmental health in a distant country with foreign workers. The savings realized by the foreign manufacture of semiconductors will be enhanced by the ability of these companies to neglect health and safety as do their international rivals. The miscarriage rate of semiconductor workers will be ignored by governments and by industry in newly industrialized countries. Workers, for the most part, will not recognize the association between work and miscarriage.
The Developing Countries’ Environmental and Occupational Health Decline
Developing countries seldom have enforceable occupational and environmental regulations. They are concerned with overwhelming problems of unemployment, malnutrition and infectious diseases, often to the exclusion of environmental hazards. Newly industrialized countries are eager for the financial benefits that foreign companies and foreign investors bring them. But with those benefits come social and ecological problems.
The positive economic and social results of industrial activity in developing nations are accompanied by serious environmental degradation. The major cities of developing nations are now reeling with the impact of air pollution, the absence of sewage treatment and water purification, the growing quantities of hazardous waste buried in or left on the soil or dumped into rivers or the oceans. In many of the world’s countries, there are no environmental regulations or, if they exist at all, there is little or no enforcement.
The workforce of developing nations is accustomed to working in small industry settings. Generally, the smaller the industry, the higher the rate of workplace injury and illness. These workplaces are characterized by unsafe buildings and other structures, old machinery, poor ventilation, and noise, as well as with workers of limited education, skill and training and employers with limited financial resources. Protective clothing, respirators, gloves, hearing protectors and safety glasses are seldom available. The companies are often inaccessible to inspections by government health and safety enforcement agencies. In many instances, they operate as an “underground industry” of companies not even registered with the government for tax purposes.
The common public perception of off-shore industries is that of the major multinationals. Far more common than these industrial giants are the many thousands of small companies owned by foreign interests and operated or supervised by local managers. The ability of most foreign governments to regulate industry or even to monitor the passage of goods and materials is extremely limited. Migrating industries generally conform to the environmental and occupational health and safety standards of the host country. Consequently, worker fatality rates are much higher in newly industrialized countries than in the developed nations, and workplace injuries occur with rates common to the developed nations during the early years of the Industrial Revolution. In this regard, the Industrial Revolution is taking place all over again, but with much larger populations of workers and in many more countries.
Virtually all of the world’s population growth is occurring in the developing world. At present, the labour force in developing countries totals around 1.76 billion, but it will rise to more than 3.1 billion in 2025— implying a need for 38 to 40 million new jobs every year (Kennedy 1993). This being the case, worker demands for better working conditions are not likely to occur.
Migration of Occupational Illness and Injury to the Developing World
The incidence of occupational diseases has never been greater than it is today. The United Nations estimates that 6 million occupational disease cases occur each year worldwide. Occupational diseases occur with greater frequency per exposed worker in the developing countries, and, of even greater significance, they occur with greater severity. Among miners, construction and asbestos workers in some developing countries, asbestos is the major cause of disability and ill health and, by some counts, the major cause of deaths. The occupational and environmental hazards posed by asbestos products do not discourage the asbestos industry from promoting asbestos in the developing world, where demand for low-cost building materials outweighs health concerns.
Lead smelting and refining is migrating from developed countries to developing countries. Recycling of lead products also passes from developed countries to poorer nations that are often ill-prepared to deal with the occupational and environmental hazards created by lead. Developed nations have few lead smelters today, this industrial activity having been passed to the newly industrialized countries. Many lead-smelting activities in the developing world operate with technologies that are unchanged from a century ago. When developed countries boast of accomplishments in the area of lead recycling, almost invariably the lead is recycled in developing countries and returned to the developed countries as finished products.
In developing countries, governments and industries accept the hazardous materials knowing that reasonable exposure levels are not likely to be legislated or enforced. Leaded gasoline, paints, inks and dyes, batteries and many other lead-containing products are produced in developing countries by companies that are usually foreign-owned and the products are then sold internationally by the controlling interests.
In developing countries, where the majority of workers are in agriculture, pesticides are often applied by hand. Three million pesticide poisonings occur each year in Southeast Asia (Jeyaratnam 1992). Most pesticide manufacture in developing countries is done by foreign-owned companies or local companies with capital invested by foreigners. The use of pesticides in the developing countries is growing rapidly as they learn the advantages that such chemicals offer to the agricultural industry and as they gain the capability to produce the pesticides in their own countries. Pesticides such as DDT and dibromochloropropane (DBCP), which are banned in most developed nations, are widely sold and used without restrictions in the developing world. When health hazards cause removal of a pesticide from a developed country’s market, it often finds its way to the unregulated markets in developing countries.
The chemical industry is one of the most rapidly growing industrial sectors in the emerging global economy. The chemical companies of the developed countries are found throughout the world. Many smaller chemical companies migrate to the developing countries, making the chemical industry a major contributor to environmental contamination. As population growth and industrialization continue throughout the poorer regions of the world, demand for pesticides, chemical fertilizers and industrial chemicals grows as well. To compound this problem, chemicals that are banned in developed countries are often manufactured in increased quantities in the newly industrialized countries. DDT is a compelling example. Its worldwide production is at record levels, yet it has been illegal to produce or use DDT in most developed countries since the 1970s.
Costs Shifting to Developing World
The experience of industrialized countries with the costs of occupational safety and environmental programmes is that a very substantial financial burden is being shifted to newly-industrialized nations. The cost of future accidents such as Bhopal, mitigation of environmental damage and effects on the public health are not often discussed with candour in the developing world. The consequences of global industry may become the roots of widespread international conflicts when the long-term economic realities of industrial migration become more apparent.
The Developing Nation Conundrum
Developing nations seldom support the adoption of the environmental standards of the developed world. In some instances, opponents argue that it is a matter of national sovereignty that allows each nation to develop its own standards. In other cases, there is long-standing resentment of any foreign influence, especially from the nations that have already increased their standard of living from the industrial activities that are now being regulated. Developing nations take the position that after they have the standard of living of the developed nations, they will then adopt stricter regulatory policies. When developed nations are asked to provide developing nations with industries whose technology is environmentally benign, interest in industrial migration lessens dramatically.
The Need for International Intervention
International organizations must take a stronger lead in approving and coordinating technology transfer. The shameful practice of exporting obsolete and hazardous technologies to developing countries when these processes can no longer satisfy the environmental standards of the developed countries must be stopped. International agreements must replace the perverse incentives that threaten the world’s environment.
There have been many efforts to control the behaviour of industry. The Organization for Economic Cooperation and Development (OECD) Guidelines for Multinational Enterprises, the United Nations (UN) Code of Conduct on Transnational Corporations and the International Labour Organization (ILO) Tripartite Declaration of Principles Concerning Multinational Enterprises and Social Policy attempt to provide a framework of ethical behaviour. The Basel Convention on the Control of Transboundary Movements of Hazardous Wastes and Their Disposal was adopted in March 1994. Although it halts most hazardous wastes from crossing borders, it also serves to institutionalize a trade in recyclable wastes that reflected the need for political compromise.
Some international lending institutions are now producing environmental impact assessments (EIAs) when the host country is unable to perform this task. Assessment of the local impact potential of at least certain hazardous industry sitings ought to be mandatory and occupational health and safety standards could be added to plant siting assessments.
The International Organization for Standardization (ISO) has undertaken the development of voluntary standards, the ISO 14000 series that are likely to become the international standard for environmental management. These encompass environmental management systems, environmental audits, eco-labelling, environmental performance evaluations, life-cycle assessment and environmental aspects in product standards (Casto and Ellison, 1996).
Many developed nations have established recommended exposure levels for workers that cannot be exceeded without regulatory or legal action. But in developing countries, exposure standards are often non-existent, not enforced, or too lax to be of use. International standards can and should be developed. Developing countries, and particularly the foreign companies that manufacture there, can be given a reasonable period of time to comply with the standards that are enforced throughout most of the developed world. If this is not done, some workers in these countries will pay an inordinate part of the cost of industrialization.
Conclusions
The most logical international standard of occupational health and safety is the development of an international workers’ compensation insurance system. Workers in all countries are entitled to the basic benefits of workers’ compensation law. The incentive for employers to provide a healthy and safe work setting that workers’ compensation insurance provides for should be such as to benefit workers in all countries, regardless of the ownership of the company.
There must be an international legal system to deal with the environment and there must be an enforcement capability strong enough to discourage even the most criminal of polluters. In 1972, the member countries of OECD agreed to base their environmental policies on a “polluter pays” principle (OECD 1987). The intent was to encourage industries to internalize environmental costs and reflect them in the prices of products. Expanding on the principle, strict liability provision in the laws of all countries could be developed for both property and third-party damage. Thus, the waste generator would be responsible through an international system of strict liability for management of waste from its production to its disposal.
Developing countries do not have large, well-funded environmental groups such as those that exist in developed countries. Enforcement will require the training of personnel and the support of governments which, until recently, placed so much emphasis on industrial expansion that the issue of environmental protection was not even a consideration.
Free-Trade Agreements
Economists have long viewed free trade as an ideal. In 1821 economist David Ricardo argued that each country should export those commodities it could produce with comparative advantage. Although Ricardo considered only a single factor of production, labour, later theorists of relative factor proportions extended this framework to capital, natural resources and other factors. Most modern economists believe that restrictions on trade—protective tariffs, export subsidies and import quotas—create economic inefficiencies, distorting the incentives of both producers and consumers and costing nations money. They argue that in restricted national markets small firms proliferate to serve small markets, violating economies of scale, and that incentives for producers to innovate and compete are blunted. Free-trade advocates believe that arguments for trade restrictions, while often based on “the national interest”, are usually disguised claims on behalf of special interests.
However, there are several economic arguments against free trade. One is based on domestic market failures. If a domestic market such as the labour market does not function properly, then deviation from free trade may help to restore that market or may yield compensatory gains in other parts of the domestic economy. A second argument is that a fundamental assumption of free-trade theory, immobility of capital, is no longer correct, so free trade may disadvantage some countries. Daly and Cobb (1994) write:
The free flow of capital and goods (instead of goods only) means that investment is governed by absolute profitability and not by comparative advantage. The absence of a free flow of labour means that opportunities for employment decline for workers in the country in which investments are not being made. This represents a more nearly accurate account of the world in which we live than does the principle of comparative advantage, however applicable that may have been in Ricardo’s day.
Within a free-trade area, the prices of goods that are traded tend to equalize. According to the factor price equalization theorem, this is also true of factors of production, including wages, costs of regulatory compliance, and perhaps externalized factors such as air pollution. That leads to a third argument against free trade: it may exert downward pressure on wages, on health, safety, and environmental practices, and on other factors of production, towards the lowest levels of any of the trading countries. This raises serious occupational health and safety concerns.
Since the Second World War, industry has become increasingly international. Communications and transportation have advanced rapidly. Information and capital are increasingly mobile. Multinational firms have become an ever more prominent part of the world economy. In the process, production patterns change, plants relocate, and employment is destabilized. Unlike capital, labour is relatively immobile, both geographically and in terms of skills. Industrial relocation has therefore placed considerable strains on workers.
Against this background free trade has steadily increased. Eight rounds of multilateral trade negotiations have taken place since 1947 under the General Agreement on Tariffs and Trade (GATT). The most recent, the Uruguay Round, concluded in 1994 with the formation of the World Trade Organization (WTO). GATT (and now WTO) member nations agree to three general principles: they refrain from export subsidies (except in agriculture); they refrain from unilateral import quotas (except when imports threaten “market disruption”); and any new or increased tariffs must be offset by reductions in other tariffs to compensate trading partners. The WTO does not eliminate tariffs but it limits and regulates them. Over 130 nations, many of them developing or “transition” nations, are WTO members. Total membership is expected to exceed 150.
Since the 1980s further moves towards free trade have occurred on a regional level, through preferential trading agreements. Under these agreements, countries agree to eliminate tariffs on trade with each other while continuing to maintain tariff barriers against the rest of the world. These agreements are known as customs unions, common markets or free-trade areas; examples include the European Union and the three nations of North America. More loosely knit economic alliances, such as the Asian Pacific Economic Cooperation (APEC), the Association of South-East Asian Nations (ASEAN) and the Mercado Común del Sur (MERCOSUR), also promote trade among their members.
Job Health and Safety in Free-Trade Agreements
Free-trade agreements are designed to promote trade and economic development and most address social issues such as worker health and safety only indirectly, if at all. However, a wide range of issues affecting job health and safety may arise in the context of free-trade agreements.
Worker dislocation, unemployment and migration
Free-trade agreements occur in the context of larger economic and social trends, and may in turn influence these trends. Consider free trade between two countries with different levels of development, different wage scales and different employment opportunities. In this situation industries may relocate, displacing workers from their jobs and creating unemployment in the country of origin. The newly unemployed workers may then migrate to areas of greater employment opportunity, especially if, as in Europe, barriers to emigration have also been lifted.
Unemployment, fear of unemployment, migration and the accompanying stress and social disruption have a profound impact on the health of workers and their families. Some governments have attempted to mitigate these effects with social programmes, including job retraining, relocation assistance and similar supports, with mixed success.
Job health and safety standards
The member countries of a free-trade agreement may differ in their job health and safety standards. This implies lower production costs for the countries with less stringent standards, an important trade advantage. One likely result is political pressure within more protective countries to lower their standards, and within less protective countries not to advance their standards, in order to preserve trade advantages. Advocates of occupational health and safety cite this scenario as one of the major adverse consequences of free trade.
Another likely result is also worrisome. A country may decide to block the importation of certain hazardous materials or equipment to advance its occupational health agenda. Its trading partners may charge it with unfair trade practices, viewing this policy as a disguised trade barrier. In 1989, under the US-Canada Free Trade Agreement, Canada accused the United States of unfair trading when the United States moved to phase out asbestos imports. Such disputes can undermine the health and safety standards of a country with more stringent standards.
On the other hand, free trade may also provide an opportunity to improve standards through collaborative standard-setting, sharing of the technical information on which standards are based and harmonization of disparate standards up to high levels. This is true of both occupational health and safety standards and related labour standards such as child labour laws, minimum-wage requirements and collective-bargaining regulations. A major obstacle to harmonization has been the issue of national sovereignty; some countries have been reluctant to negotiate away any control over their labour standards.
Enforcement practices
Identical concerns arise with regard to enforcement of regulations that are on the books. Even if two trading partners have comparable occupational health and safety standards, one may enforce them less scrupulously than the other, lowering production costs and gaining a competitive advantage. Remedies include a dispute resolution process to allow countries to appeal an alleged unfair trade practice, and collaborative efforts to harmonize enforcement practices.
Hazard communication
Hazard communication refers to a wide range of practices: worker training, provision of written materials on hazards and protective measures, container labelling and worker access to medical and exposure records. These practices are widely recognized as key components of successful occupational health and safety programmes. Free trade and international commerce more generally have an impact on hazard communication in at least two ways.
First, if hazardous chemicals or processes are transported across national borders, workers in the receiving country may be placed at risk. The receiving country may lack the capacity for appropriate hazard communication. Information sheets, training materials and warning labels need to be provided in the language of the receiving country, at a reading level appropriate for the exposed workers, as part of the import-export process.
Second, inconsistent requirements for hazard communication place a burden on companies that operate in more than one country. Uniform requirements, such as a single format for chemical information sheets, help address this problem, and may be encouraged in the context of free trade.
Training and human resource development
When trading partners differ in their levels of economic development, they are likely also to differ in their human resources. Less affluent nations face shortages of industrial hygienists, safety engineers, occupational physicians and nurses, trained labour educators and other key professionals. Even when two nations have comparable levels of development, they may differ in their technical approaches to occupational health and safety. Free-trade agreements provide an opportunity to reconcile these disparities. Through parallel structures the occupational health and safety professionals from trading nations can meet, compare their practices, and agree on common procedures when appropriate. Similarly, when a country has a shortage of certain professionals relative to one or more of its trading partners, they can cooperate in offering formal training, short courses and other means of human resource development. Such efforts are a necessary part of harmonizing occupational health practice effectively.
Data collection
An important aspect of coordinated efforts to protect worker health and safety is data collection. Under a free-trade agreement several kinds of data collection may bear on worker health and safety. First, information on each country’s occupational health practices, particularly its means of implementing workplace standards, is necessary. Such information helps monitor progress towards harmonization and can disclose violations that may constitute unfair trade practices. Data on workplace exposures must be collected, not only for these reasons but also as part of routine occupational health practice. Exposure data must be collected according to good industrial hygiene practice; if member countries use consistent measurement procedures then comparisons among them are possible. Similarly, morbidity and mortality data are essential as part of good occupational health and safety programmes. If the countries of a free-trade agreement use consistent methods of collecting this information, then they can compare their health effects, identify problem areas and target interventions. This may be difficult to achieve since many countries collect their health and safety data from workers’ compensation statistics, and compensation schemes vary widely.
Prevention
Finally, free trade provides an opportunity for harmonization of preventive approaches, technical assistance among member nations and sharing of solutions. This may occur in the private sector when a company operates in several countries and can implement a preventive practice or technology across borders. Companies that specialize in occupational health services may themselves function internationally, spurred by a free-trade agreement, and function to diffuse preventive practices among member countries. National labour unions in a free-trade agreement may also collaborate. For example, the European Trade Union Technical Bureau for Health and Safety in Brussels was created by the European Parliament with the support of key unions. Such efforts can push member countries towards upward harmonization of preventive activities. Harmonization of preventive approaches may also occur at the governmental level, through collaboration in technology development, training and other activities. Ultimately, the most positive effect of free trade on occupational health and safety is improved prevention in each of the member countries.
Conclusion
Free-trade agreements are primarily designed to lower trade barriers and most do not directly address social issues such as worker health and safety (see also "Case Study: World Trade Organization"). In Europe, free trade developed over several decades in a process that embraced social concerns to an unusual extent. The organizations in Europe responsible for occupational health and safety are well funded, include representation from all sectors, and can pass directives that are binding on member countries; this is clearly the most advanced of the world’s free-trade agreements with respect to worker health. In North America, NAFTA includes a detailed dispute resolution process that extends to occupational health and safety, but few other initiatives to improve working conditions in the three member countries. Other regional trade pacts have not incorporated occupational health and safety initiatives.
Economic integration of the world’s nations is moving forward, due to rapid advances in communications, transportation and capital investment strategies. Free-trade agreements govern some but not all of this increased trade among nations. The changes in commercial patterns and the expansion of international trade have major implications for worker health and safety. It is essential to link trade issues with occupational health and safety issues, using free-trade agreements and other means, to ensure that advances in commerce are accompanied by advances in worker protection.
Product Stewardship and the MIgration of Industrial Hazards
Multinational corporations are dominant in the manufacturing and marketing of chemicals and other products where occupational health and safety hazards are known to exist. These corporations have long but variable experience in managing to control such hazards and some have developed large staffs and procedures for this purpose. With the trend towards ever more free-trade agreements, the dominance of multinational corporations (MNCs) is expected to expand, with a corresponding decline in the scale of state-owned industries and privately owned industries within nations. It is thus appropriate to consider the proper role of MNCs as industries are expanded all over the world, particularly in countries that have to date had minimal resources made available for worker and environmental protection.
The European Chemical Industry Council (CEFIC), in its CEFIC Guidelines on Transfer of Technology (Safety, Health and Environment Aspects), says that transferred technology should achieve a degree of safety, health protection and protection of the environment equal to that of the technology supplier from which it is derived and “equivalent to that achieved in the home facilities of the technology supplier” (CEFIC 1991). This would seem especially applicable to the worldwide subsidiary operations of MNCs.
Double Standards
There have been many examples where MNCs have not been as thorough in controlling industrial hazards in developing countries as they were in their home countries. The most numerous reports of this double standard have arisen in connection with asbestos and other ultra-hazardous materials, where substantial control of the hazards would represent a major share of overall costs of production and reduce sales in other ways. The cases described in the 1970s and early 1980s involved firms based in West Germany, the United States, the United Kingdom, Switzerland, Italy, Austria and Japan (Castleman and Navarro 1987).
The best-examined case of this double standard involves the pesticide manufacturing plant which caused thousands of deaths and permanent health impairment to many thousands of people in Bhopal, India, in 1984. Comparison of the Bhopal plant with a similar plant operated in the United States showed numerous double standards in plant design and operation, safety auditing, worker training, staffing of hazardous jobs, plant maintenance and management accountability. Additional relevant factors were the relative lack of government regulation and civil liability in India, compared with the United States (Castleman and Purkayastha 1985).
The Bhopal disaster focused world attention on the policies and practices of MNCs for safeguarding worker health and safety and the environment. Many giant manufacturing companies suddenly realized that they were running excessive, reducible risks and moved to reduce the amounts of highly toxic compressed gases they were storing and transporting. Transport of large cylinders of phosgene gas, for example, went from being a common practice in the United States to being completely avoided. Such changes were in no small part due to the fact that insurance for the consequences of chemical releases into communities became virtually unavailable. But above and beyond purely economic considerations, the ethics and morality of the conduct of the multinational companies were subjected to unprecedented scrutiny.
Obviously, lower standards of worker and environmental protection can confer at least short-term savings on factory owners. The temptation to increase profits by cutting costs is especially great where there is virtually no governmental regulation, public awareness, trade union pressure or liability for damages when something does go wrong. The Bhopal case showed that when profit levels are low, there is an added pressure on management to reduce operating costs by methods whose immediate costs are slight but whose long-term risks may be catastrophic. The structure of MNCs seemed ideal, moreover, for insulating top management from bearing any personal responsibility for the consequences of complying with local standards around the world.
The ILO investigation, Safety and Health Practices of Multinational Enterprises, found that “in comparing the health and safety performance of home-based (MNCs) with that of the subsidiaries, it could generally be said that the home country operations were better than those of the subsidiaries in the developing countries” (ILO 1984). A United Nations Centre on Transnational Corporations (UNCTC) report urged examination of MNC policies with regard to “occupational health and safety in their global operations.” The report concluded that there were “numerous examples of a ‘double standard’ in which worker and community health protection measures by transnational corporations are far weaker in the developing countries than in the transnational corporations’ home nations”. Examples of this were in vinyl chloride, pesticides, chromates, steel, chlorine and asbestos industries (UNCTC 1985).
The response of the very largest chemical MNCs based in the United States and the United Kingdom was to deny that it was company policy to have different standards in different countries for protecting people from the same industrial hazards. However, these sentiments have been expressed in different ways, some of which entail greater commitment than others. Moreover, many remain sceptical that a wide gulf remains between corporate policy statements and the reality of double standards in corporate conduct.
Product Stewardship
Product stewardship refers to a seller’s responsibility for preventing harm arising from products marketed, throughout the life cycle of product use and disposal. It includes the responsibility of assuring that a company buying the seller’s chemical product does not use it in a hazardous manner; at least one US firm, Dow Chemical, has long expressed a policy of refusing to sell chemicals to such customers. In 1992, the Chemical Manufacturers Association member companies in the United States adopted a code that contemplates termination of sales to customers who do not correct “improper practices” in the use of the chemicals they sell.
Examples of the need for product stewardship by pesticide producers abound. Repackaging of pesticides in food containers and the use of pesticide drums to store drinking water are causes of widespread death and disease. Small farmers’ use and storage of pesticides and pesticide containers reflect a general lack of training that manufacturers could provide.
In the Dominican Republic’s Costanza Valley, defoliation from overuse of pesticides has caused the area to be called the “Valley of Death”. As the area gained media attention in 1991, Ciba-Geigy, a major chemical MNC, introduced a programme to teach small farmers something about agronomy, integrated pest management and safety. It was recognized that pesticide use in the valley had to be reduced. Community response to Ciba’s effort to “prove the economic and social benefits of a sustainable market” was reported to be encouraging in the trade press. Ciba operates similar small farmer programmes in Colombia, the Philippines, Indonesia, Pakistan, Mali, Mozambique and Nigeria. The Pesticide Action Network is sceptical of corporate versions of “integrated pest management” that stress the “best mix” of pesticides instead of training people in techniques whereby pesticide use is seen as a last resort.
An important aspect of product stewardship is educational outreach to workers and the public using the product, through warning labels, brochures and customer training programmes. For certain hazardous products and containers in which they are sold, product stewardship entails retrieving materials that customers would otherwise use improperly or dispose of as hazardous wastes.
In US courts, product stewardship is strongly encouraged by the existence of liability for damages caused by hazardous products and pollution. Individuals harmed by products whose dangers were not always expressed in warnings by manufacturers have been awarded substantial compensation for economic loss, pain and suffering and in some cases punitive damages in addition. Manufacturers have withdrawn from the US market products shown in animal experiments to cause reproductive abnormalities—rather than risk multimillion dollar lawsuits from children of workers using the agent who have been born with birth defects. These same products have sometimes continued to be marketed by the same companies in other countries, where product liability is not a factor.
Liability and regulation have thus imposed a duty on manufacturers in some countries to develop less toxic processes and products. But in the absence of public awareness, liability and regulation, there is the possibility that the discredited, more hazardous technologies will remain economically competitive, and there may even be a market for the older technology that can be exploited in many countries. Thus, despite the advances being made by MNCs in the development of “clean technology”, there is no reason to expect that these improvements will be promptly transmitted to Africa, Asia, Latin America and Central and Eastern Europe. It is very possible that some of the newly built industry in these regions will be made with used, imported equipment. This poses an ethical challenge to the MNCs who own equipment that is being replaced in Europe and North America.
Public Health Advances
A number of advances have occurred in recent years, which would unquestionably contribute to the protection of public health and the environment wherever they take root. Industrial research chemists, whose goal has traditionally been the maximization of product yield with little concern about toxicity of products and by-products, now discuss developments in less toxic technology at symposia on “green chemistry”, or “industrial ecology” (Illman 1994). Examples include:
- the replacement of glycol ethers, chlorinated solvents and chlorofluorocarbon solvents as cleaning agents in microelectronics processing
- replacement of organic solvents by water-based solvents in adhesives and sealants
- reduction of volatile, organic solvents in many paints, in favour of water-based paints, spray-painting technology using supercritical carbon dioxide, and powder coatings
- replacement of cadmium and lead in pigments
- elimination of nitrous oxide air pollution in making adipic acid (used to make nylon, polyester and polyurethane)
- replacement of acrylamide in grouting compounds
- replacement of chlorine bleaching in making paper
- conversion of phosgene, arsine and other toxic gases to less toxic intermediates which can be handled instead in industrial processes, thus avoiding the need to store and transport large quantities of highly toxic, compressed gases
- replacement of the phosgene process for making polycarbonates with a dimethyl carbonate process
- synthesis of aliphatic isocyanates from amines and carbon dioxide instead of processes using phosgene
- replacement of hydrofluoric acid with sulphuric acid or, better still, with solid catalysts, in oil refinery gasoline alkylation units
- use of zeolite catalysts in cumene production, replacing phosphoric acid or aluminium chloride catalysts and eliminating problems of acid waste disposal and the handling of corrosive materials.
The worldwide promotion of less toxic technologies can be carried on both by individual MNCs and through collective bodies. The Industry Cooperative for Ozone Layer Protection is one vehicle major firms have used to promote environmentally superior technology. Through this organization, with additional support by the World Bank, IBM has tried to help companies in Asia and Latin America to switch to water-based cleaning and drying of circuit boards and disk components.
Roles of Government
Industrial expansion is taking place in many countries, and in considering applications for new industrial projects, governments have the opportunity and responsibility to evaluate health and safety hazards of the imported technology. The host country should seek to ensure that new operations will achieve high standards of performance. The project applicant should make the commitment to achieve specific levels of pollutant release that will not be exceeded during plant operations, and limits of worker exposure to toxic substances that will be attained. The applicant should be willing to pay for the government to obtain the necessary monitoring equipment to assure that these limits are observed in practice and to allow immediate access to government inspectors at any time.
Special attention should be directed towards having project applicants describe their past experience with the technology involved and its hazards. The host government has every reason and right to know what workplace hazards and pollution levels exist at similar factories operated by the project applicants. Similarly, it is important to know what laws, regulations and standards for public health protection are honoured by the applicants at similar facilities in other countries.
The host government application process should include critical evaluation from the standpoint, “Do we really need this?” And if the answer is yes, follow-up analysis should proceed along the lines of trying to ensure that the technology is designed to produce the least hazardous processes and products to provide whatever needs are served. This procedure comports with the stated policies of leading MNCs. The fulfilment of ethical duties by governments and corporations can best assure that public health related advances in technology are transmitted rapidly around the world.
Major new projects in developing countries usually involve participation of foreign investor MNCs. The accompanying guidelines (table 1) have been published by Greenpeace and Third World Network (Malaysia), detailing information that governments can request from foreign investors (Bruno 1994). To the extent that information on the technology and its hazards is not submitted by the prospective foreign investors, governments can and should take steps to obtain information on it independently.
Table 1. Information from foreign investors for environmental review
A. The foreign investor shall provide an Environmental Impact Analysis of the proposed project, including:
1. list of all raw materials, intermediates, products and wastes (with flow diagram)
2. list of all occupational health and safety standards and environment standards (wastewater effluent releases, atmospheric emission rates for all air pollutants, detailed description and rate of generation of solid wastes or other wastes to be disposed of on land or by incineration)
3. plan for control of all occupational health and safety hazards in plant operation, storage, and transport of potentially hazardous raw materials, products and wastes
4. copy of corporation guidelines of the foreign investor for conducting environmental and occupational health and safety impact analyses for new projects
5. manufacturer’s safety data sheets on all substances involved.
B. The foreign investor shall provide complete information on locations, ages and performance of existing plants and plants closed within the past five years in which the foreign investor has partial or full ownership, where similar processes and products are used, including:
1. list of all applicable occupational health and safety standards and environmental standards, including both legal requirements (standards, laws, regulations) and corporate voluntary standards and practices for the control of occupational and environmental hazards of all kinds
2. description of all cases of permanent and/or total disability sustained or allegedly sustained by workers, including workers’ compensation claims
3. explanation of all fines, penalties, citations, violations, regulatory agreements, and civil damage claims involving environmental and occupational health and safety matters as well as hazards from or harm attributed to the marketing and transport of the products of such enterprises
4. description of the foreign investor’s percentage of ownership and technology involvement in each plant location and similar information for other equity partners and providers of technology
5. names and addresses of governmental authorities who regulate or oversee environmental and occupational health and safety for each plant location
6. explanation of cases where any plant’s environmental impact has been the subject of controversy within the local community or with regulatory authorities, including description of the practices criticized and how criticism was resolved in each case
7. copies, with summary, of all corporate occupational health and safety and environmental audits and inspection reports for each location, including such audits and reports by consultants
8. copies of safety reports, reports of hazard assessment, and risk analysis reports carried out with similar technology by the foreign investor and its consultants
9. copies of toxic release forms that have been submitted to governmental bodies (e.g., the US Environmental Protection Agency or similar agencies in other countries) within the past five years, for all plant locations
10.any information considered relevant by the foreign investor.
C. The foreign investor shall submit a statement of corporate policy on health, safety, and environmental performance of worldwide operations. This must include the corporate policy on laws, regulations, standards, guidelines, and practices for new industrial projects and production facilities. The foreign investor shall explain how its global policy is implemented by: describing the staff responsible for carrying out this policy, its authority and responsibilities, and its position in the foreign investor corporate structure. Such descriptions will also include the name, address, and telephone number of senior corporate management officials in charge of this staff function. The foreign investor shall state whether it follows the same standards worldwide for worker and environmental protection in all new projects; and if not, explain why not.
D. The foreign investor shall agree to provide the developing country immediate access to the proposed industrial facility at any time during its operation to conduct inspections, monitor exposure of workers to hazards, and sample for pollution releases.
E. The foreign investor shall agree to fully train all employees exposed to potential occupational hazards, including training on potential health effects of all exposures and the most effective control measures.
F. The foreign investor shall agree to provide the developing country with equipment to analyze workplace exposures and pollutant generation, including but not limited to all limits specified in A(2) above, for the lifetime of the proposed project. The foreign investor shall agree that the proposed project will pay the cost to the developing country government for all medical and exposure monitoring during the lifetime of the proposed project.
G. The foreign investor shall agree that the proposed project will fully compensate any person whose health, earning capacity, or property is harmed as a result of the project’s occupational hazards and environmental impacts, as determined by the government of the developing country.
H. The foreign investor shall follow marketing safeguards as restrictive as those it applies anywhere in the world, to assure that workers and members of the public are not harmed as a result of the use of its products.
I. If the foreign investor becomes aware of a substantial risk of injury to health or the environment from a substance it manufactures or sells in the developing country, a risk not known and disclosed at the time of this application, the foreign investor agrees to notify the environmental protection agency of the government of the developing country immediately of such risk. (This is similar to requirements under section 8e of the Toxic Substances Control Act of the USA.)
J. The foreign investor shall provide the names, titles, addresses, phone, and fax numbers of its senior corporate officials charged with implementing environmental and occupational and safety and health policies including plant design and operations, corporate inspections and reviews of plant performance, and product stewardship.
Source: Bruno 1994.
Industrial hazards are not the only reason countries have for wanting to do environmental impact reviews, and industrial projects are not the only ones warranting such scrutiny. The importation and widespread use of energy-inefficient technology for manufacture of refrigerators, electric motors and lighting has caused significant problems. In many countries, electrical power generation could hardly keep up with demand even if energy efficiency were a criterion in the evaluation of new technology and the design of commercial buildings. Energy inefficiency poses major problems in development, including the cost of building and operating excessive power generation capacity, pollution and the disincentives to expansion caused by unreliable power supplies and breakdowns. Energy efficiency could free tremendous resources for meeting basic needs instead of building and operating unneeded power plants.
Conclusion
Multinational corporations are in the most powerful position to determine what types of technology will be transferred to countries in Asia, Africa, Latin America and Eastern and Central Europe. The big companies have an ethical and moral obligation to promptly implement global policies to eliminate double standards with respect to public health and the environment. The lives of present and future generations will be vitally affected by the rate of transfer of improved, less hazardous technologies throughout the world.
Governments, further, have the ethical duty to independently and critically screen industrial and commercial projects. This role is best fulfilled by conducting searching analyses of the technologies and companies involved. The credibility and effectiveness of the screening process will depend greatly upon the transparency of the process and public participation in it.
Quotations from corporate sources are based on reports published in chemical trade journals and communications to the author
Economic Aspects of Occupational Health and Safety
The losses to society from work-related accidents and illnesses are very large, but no society can afford to prevent all these losses. Because of the scarcity of resources, limited investments have to be targeted carefully to give the “biggest bang for the buck”. The mere costing of occupational ill-health does not facilitate the targeting of investment. Proper economic evaluation can be helpful if it is well designed and executed. The results of such evaluation can be used, with appropriate critical appraisal of the practice of evaluations, to inform investment choices. Economic evaluation will not and should not determine investment decisions. Such decisions will be the product of economic, political and social values. As Fuchs (1974) argued:
At the root of most of our major health problems are value choices. What kind of people are we? What kind of life do we want to lead? What kind of society do we want to build for our children and grandchildren? How much weight do we want to put on individual freedom? How much to equality? How much to material progress? How much to the realm of the spirit? How important is our own health to us? How important is our neighbour’s health to us? The answers we give to these questions, as well as the guidance we get from economics, will and should shape health care policy.
A decision to regulate the mining industry so that fewer workers are killed and maimed will, if successful, bring health benefits to the workforce. These benefits, however, have associated costs. In real-life situations, the increased costs of improving safety will drive up prices and reduce sales in competitive world markets and may induce in employers deviance from regulations. Such deviation may be condoned by labour unions and their members, who may prefer imperfect implementation of health and safety laws if it improves incomes and employment prospects.
The purpose of economic analysis in occupational health is to facilitate the identification of that level of safety investment which is efficient. Efficiency means that the costs of doing a little more (the marginal cost) to enhance safety equal the benefits (the marginal returns in terms of health and welfare enhancements result from risk reduction). The economic aspects of occupational health and safety are central to decision making at all levels: the shop floor, the firm, the industry and the society. To behave as if all workplace risks to workers’ health can be eradicated may be inefficient. Risks should be eradicated where it is cost effective. But some risks are rare and too costly to eradicate: they have to be tolerated and when these rare events damage workers’ welfare, they have to be accepted as unfortunate but efficient. There is an optimal level of occupational risk beyond which the costs of risk reduction exceed the benefits. Investment in safety beyond this point will generate safety benefits which should be bought only if society is prepared to act inefficiently. This is a social policy decision.
Types of Economic Analysis
Cost analysis
Cost analysis involves the identification, measurement and valuation of the resource consequences of occupational accidents and ill health. Such descriptions illuminate the size of the problem but do not inform decision makers about which of many competing interventions by all who govern and regulate the workplace environment is the most efficient.
A nice example of this is a British study of the costs to economy of work accidents and work related illness (Davies and Teasdale 1994). In the year 1990 there were 1.6 million accidents reported at work, and 2.2 million people suffered ill health which was caused or exacerbated by the working environment. As a result of the events, 20,000 people were obliged to give up work and 30 million working days were lost. The loss of income and welfare to the victims and their families was estimated to be £5.2 billion. The loss to employers was between £4.4 and £9.4 billion. The loss to society as a whole was £10.9 to £16.3 billion (see table 1). The authors of the British report noted that whilst the numbers of reported accidents and industrial diseases had fallen, the estimated costs were higher.
Table 1. The costs to the British economy of work accidents and work-related health (1990 £m)
|
Costs to individual victims and their families |
Costs to their employers |
Costs to society as a whole |
|||
|
Loss of income |
(£m) |
Extra production costs |
(£m) |
Lost output |
(£m) |
|
Injury Illness |
376 579 |
Injury Illness |
336 230 |
Injury Illness |
1,365 1,908 |
|
Damage and loss in accidents |
Resource costs: Damage in accidents |
||||
|
Injury Non-injury Insurance |
15-140 2,152-6,499 505 |
Injury Non-injury Insured |
15-140 2,152-6,499 430 |
||
|
Medical treatment |
|||||
|
Injury Illness |
58-244 58-219 |
||||
|
Administration/recruitment |
Administration, etc. |
||||
|
Injury Illness Non-injury |
58-69 79-212 307-712 |
Injury Illness Non-injury |
132-143 163-296 382-787 |
||
|
Loss of welfare |
Loss of welfare |
||||
|
Injury Illness |
1,907 2,398 |
Employer liability Insurance |
750 |
Injury Illness |
1,907 2,398 |
|
Total |
5,260 |
Total |
4,432-9,453 |
Total |
10,968-16,336 |
|
Less: compensation from employers’ liability insurance |
650 |
||||
|
Net total |
4,610 |
||||
Source: Davies and Teasdale 1994.
The costs were higher than those reported in previous studies because of revised techniques of welfare loss estimation and better sources of information. The central information ingredient in this sort of costing exercise is the epidemiology of work-related accidents and diseases. As in all other areas of social cost analysis (e.g., alcohol—see McDonnell and Maynard 1985) the measurement of the volume of events tends to be poor. Some (how many?) accidents are not reported. The link between disease and the workplace may be obvious in some cases (e.g., asbestos-related diseases) but uncertain in other cases (e.g., heart disease and occupational risk factors). Thus it is difficult to identify the volume of work-related events.
The costing of those events which are identified is also problematic. If work stress leads to alcoholism and dismissal from employment, how are the effects of these events on the family to be valued? If an accident at work causes pain for life, how is that to be valued? Many costs can be identified, some can be measured, but often a considerable proportion of costs which are measured and even quantified, cannot be valued.
Before too much effort is expended on the costing of work-related health events, it is essential to be certain about the purpose of such work and the value of great accuracy. The costing of accidents and work-related illness does not inform the decision-making about investments in prevention of such events because it tells managers nothing about the costs and benefits of doing a little bit more or a little bit less of that prevention activity. The cost of events related to occupational ill health can identify section losses (to the individual, the family and the employer) and the costs to society. Such work does not inform prevention activity. The relevant information for such choices can be derived only from economic evaluation.
The principles of economic evaluation
There are four types of economic evaluation: cost minimization analysis, cost benefit analysis, cost effectiveness analysis and cost utility analysis. The characteristics of these approaches are outlined in table 2.
Table 2. Types of economic evaluation
|
Cost measurement |
Outcome measurement: What? |
Outcome measurement: How valued? |
|
|
Cost minimization analysis |
£ |
Assumed identical |
None |
|
Cost benefit analysis |
£ |
All effects producedby the alternative |
Pounds |
|
Cost effectiveness analysis |
£ |
Single common specific variable achieved to varying extents |
Common units (e.g., life years) |
|
Cost utility analysis |
£ |
Effects of the competing therapies and achieved to differing levels |
QALYs or DALYs |
In cost minimization analysis (CMA) it is assumed that the outcome effect is identical in each of the alternatives being compared. Thus we may have two interventions to reduce the carcinogenic effects of a production process, and engineering and other data shows that the effects are identical in terms of exposure and cancer reductions. CMA can be used to cost the alternative strategies in order to identify the cheapest alternative.
Obviously the assumption of identical effects is strong and not likely to be met in most investment cases; for example, the effects of alternative safety strategies on the length and quality of workers’ lives will be unequal. In this case alternative evaluation methods have to be used.
The most ambitious of these methods is cost benefit analysis (CBA). This requires the analyst to identify, measure and value both the costs and the benefits of the alternative prevention strategies in terms of a common monetary measure. Valuing the costs of such investments can be difficult. However these problems tend to be slight compared to the monetary valuation of the benefits of such investments: how much is an injury avoided or life saved worth? As a consequence of such difficulties CBA has not been used extensively in the accident and health areas.
A more restricted form of economic evaluation, cost effectiveness analysis (CEA), has been used extensively in the health field. (CEA) was developed by the US military, whose analysts adopted the notorious measure of effect, “body count”, and sought then to identify which was the cheapest way of achieving a given enemy body count (i.e., what were the relative costs of artillery barrages, napalm bombing, infantry charges, tank advances and other “investments” in achieving a target mortality effect on the enemy).
Thus in CEA there is usually a simple, sector-specific effect measure, and the costs of achieving differing levels of reduction in, for instance, workplace events or workplace mortality can thus be computed.
The limitation of the CEA approach is that the effect measures may not be generalizable—that is, a measure used in one sector (e.g., reducing exposure to asbestos) may not be usable in another area (e.g., reducing electrical accident rates in the power distribution industry). Thus CEA may inform the decision making in a particular area but will not generate evaluative information to elucidate the costs and effects of investment choices across a wide range of prevention strategies.
Cost utility analysis (CUA) was devised to overcome this problem by using a generic effect measure, such as a quality adjusted life year (QALY) or disability adjusted life year (DALY) (see Williams 1974 and World Bank Report on Health 1993, for example). CUA techniques can be used to identify the cost/QALY effects of alternative strategies and such information can inform prevention investment strategies in a more comprehensive manner.
The use of techniques of economic evaluation in health care is well established, although their use in occupational medicine is more limited. Such techniques, given the difficulties of measuring and valuing both costs and benefits (e.g., QALYs), are useful, if not essential, in informing choices about prevention investment. It is extraordinary that they are used all too rarely and that, as a consequence, investment is determined “by guess and by God” rather than by careful measurement within an agreed analytical framework.
The Practice of Economic Evaluation
As in all other areas of scientific endeavour, there is variance between the principles of economic evaluation and its practice. Thus when using studies about the economic aspects of occupational accidents and diseases, it is essential to evaluate the evaluations with care! The criteria to judge the merit of economic evaluations have long been established (e.g., Drummond, Stoddart and Torrance 1987 and Maynard 1990). A pioneer in this work, Alan Williams, set out the following list of relevant issues over two decades ago (Williams 1974):
- What precisely is the question which the study was trying to answer?
- What is the question that it has actually answered?
- What are the assumed objectives of the activity studied?
- By what measures are these represented?
- How are they weighted?
- Do they enable us to tell whether the objectives are being attained?
- What range of options was considered?
- What other options might there have been?
- Were they rejected, or not considered, for good reasons?
- Would their inclusion have been likely to change the results?
- Is anyone who has not been considered in the analysis likely to be affected?
- If so why are they excluded?
- Does the notion of cost go wider or deeper than the expenditure of the agency concerned?
- If not, is it clear that these expenditures cover all the resources used and accurately represent their value if released for other uses?
- If so, is the line drawn so as to include all potential beneficiaries and losers, and are resources costed at their value in their best alternative use?
- Is the differential timing of the items in the streams of benefits and costs suitably taken care of (e.g., by discounting) and, if so, at what rate?
- Where there is uncertainty, or there are known margins of error, is it made clear how sensitive the outcome is to these elements?
- Are the results, on balance, good enough for the job at hand?
- Has anyone else done better?
There are several areas in economic evaluation where practice tends to be defective. For instance in the area of back pain, which causes major work-related illness losses to society, there is dispute about the competing treatments and their effects. The “old-fashioned” treatment for back pain was bed rest, but the preferred modern treatment is activity and exercise to dissipate the muscle strain which generates the pain (Klaber Moffett et al. 1995). Any economic evaluation has to build on clinical knowledge, and this is often uncertain. Thus without careful appraisal of the effectiveness knowledge base, modelling of the economic effects of alternative interventions may be biased and confusing for decision makers, as happens in the health care field (Freemantle and Maynard 1994).
High quality economic evaluations of prevention investments to reduce work-related illness and accidents are few in number. As in health care in general, the studies that are available are often of poor quality (Mason and Drummond 1995). Thus, buyer beware! Economic evaluations are essential but deficiencies in current practice are such that users of this science must be able to appraise critically the available knowledge base before committing society’s scarce resources.
Case Study: Industrialization and Occupational Health Problems in China
The Chinese farmer’s achievements in rural industrialization and in developing township enterprises (table 1) have been remarkable. This development has indeed been the most important opportunity for rural people to escape poverty quickly. Since about the seventies, more than 100 million farmers have moved to township enterprises, a number of workers exceeding the total number of employees then in state-owned and city/collectively owned enterprises. At present, one out of every five rural labourers works in various township enterprises. A total of 30% to 60% of the total average personal net income of rural people comes from the value created by township enterprises. The output value from township industries accounted for 30.8% of the total value of national industrial production in 1992. It is predicted that by the year 2000, more than 140 million surplus farm labourers, or some 30% of the estimated rural labour force, will be absorbed by township industries (Chen 1993; China Daily, 5 Jan. 1993).
Table 1. Development of China’s township enterprises
|
1978 |
1991 |
|
|
Number of enterprises (million) |
1.52 |
19 |
|
Number of employees (million) |
28 |
96 |
|
Fixed assets (billion yuan RMB) |
22.96 |
338.56 |
|
Total output value (billion yuan RMB) |
49.5 |
1,162.1 |
This quick transfer of the labour force from agriculture to non-agricultural work in rural areas has imposed heavy pressure on the resources of occupational health services. The Survey on Occupational Health Service Needs and Countermeasures in Township Industries (SOHSNCTI) in 30 sample counties of 13 provinces and 2 municipalities, organized by the Ministry of Public Health (MOPH) and the Ministry of Agriculture (MOA) jointly in 1990, showed that most township enterprises had not provided basic occupational health service (MOPH 1992). The coverage of five routine occupational health service activities provided for township enterprises by local occupational health institutions (OHIs) or health and epidemic prevention stations (HEPSs) was very low, only 1.37% to 35.64% (table 2). Those services which need complicated techniques or well-trained occupational health professionals are particularly limited. For example, preventive occupational health inspection, physical examination for workers exposed to hazards, and workplace monitoring were evidently insufficient.
Table 2. The coverages of OHS provided to township industries by county HEPS
|
Items |
Enterprises |
Enterprises covered by OHS |
% |
|
Preventive OH inspection |
7,716 |
106 |
1.37 |
|
General industrial hygiene walk-through |
55,461 |
19,767 |
35.64 |
|
Workplace hazard monitoring |
55,461 |
2,164 |
3.90 |
|
Worker’s physical examination |
55,461 |
1,494 |
2.69 |
|
Help to set up OH record keeping |
55,461 |
16,050 |
28.94 |
Meanwhile, there is a trend that occupational health problems in rural enterprises are worsening. First, the survey showed that 82.7% of rural industrial enterprises had at least one type of occupational hazard in the workplace. Workers exposed to at least one kind of hazard accounted for 33.91% of the blue-collar workers. The air samples of lead, benzene analogues, chromium, silica dust, coal dust and asbestos dust at 2,597 worksites in 1,438 enterprises indicated that the total compliance rate was 40.82% (table 3); the compliance rates with respect to dusts were very low: 7.31% for silica, 28.57% for coal dust, and 0.00% for asbestos. The total compliance rate for noise in 1,155 enterprises was 32.96%. Physical examinations for workers exposed to more than seven hazards were conducted (table 4). The total prevalence of occupational diseases caused only by exposures to these seven types of hazard was 4.36%, much higher than the prevalence of total compensable occupational diseases in state-owned enterprises. There were another 11.42% of exposed workers suspected of having occupational diseases. Next, hazardous industries continue transferring from urban to rural areas, and from state-owned enterprises to township enterprises. Most of the workers in these industries used to be farmers before employment and lacked education. Even the employers and the managers still have very little education. A survey covering 29,000 township enterprises indicated that 78% of the employers and managers had only junior middle school or primary school education and that some of them were simply illiterate (table 5). A total of 60% of employers and managers were not aware of governmental occupational health requirements. It predicted that the prevalence of occupational diseases in rural industries will increase and reach a peak by the year 2000.
Table 3. The compliance rates of six hazards in worksites
|
Hazards1 |
Enterprises |
Worksites monitored |
Worksites complying |
Compliance rate (%)2 |
|
Lead |
177 |
250 |
184 |
73.60 |
|
Benzene analogues |
542 |
793 |
677 |
85.37 |
|
Chromium |
56 |
64 |
61 |
95.31 |
|
Silica dust |
589 |
1,338 |
98 |
7.31 |
|
Coal dust |
68 |
140 |
40 |
28.57 |
|
Asbestos dust |
6 |
12 |
0 |
0.00 |
|
Total |
1,438 |
2,597 |
1,060 |
40.82 |
1 Mercury was not found in sample areas.
2 The compliance rate for noise was 32.96%; see text for details.
Table 4. The detectable rates of occupational diseases
|
Occupational diseases |
Persons checked |
No illness |
With illness |
Suspected illness |
|||
|
No. |
No. |
% |
No. |
% |
No. |
% |
|
|
Silicosis |
6,268 |
6,010 |
95.88 |
75 |
1.20 |
183 |
2.92 |
|
Coal workers pneumoconiosis |
1,653 |
1,582 |
95.70 |
18 |
1.09 |
53 |
3.21 |
|
Asbestosis |
87 |
66 |
75.86 |
3 |
3.45 |
18 |
20.69 |
|
Chronic lead poisoning |
1,085 |
800 |
73.73 |
45 |
4.15 |
240 |
22.12 |
|
Benzene analogues poisoning1 |
3,071 |
2,916 |
94.95 |
16 |
0.52 |
139 |
4.53 |
|
Chronic chromium poisoning |
330 |
293 |
88.79 |
37 |
11.21 |
- |
- |
|
Noise-induced hearing loss |
6,453 |
4,289 |
66.47 |
6332 |
9.81 |
1,5313 |
23.73 |
|
Total |
18,947 |
15,956 |
84.21 |
827 |
4.36 |
2,164 |
11.42 |
1 Benzene, toluene and xylene, measured separately.
2 Hearing impairment in sound frequency.
3 Hearing impairment in high frequency.
Table 5. Distribution of hazardous working and the education of employers
|
Education of employers |
Total no. of enterprises (1) |
Enterprises with hazardous working (2) |
Blue-collar workers (3) |
Workers exposed (4) |
Hazardous enterprises (%) (2)/(1) |
Exposed workers (%) (4)/(3) |
|
Illiteracy |
239 |
214 |
8,660 |
3,626 |
89.54 |
41.87 |
|
Primary school |
6,211 |
5,159 |
266,814 |
106,076 |
83.06 |
39.76 |
|
Junior middle school |
16,392 |
13,456 |
978,638 |
338,450 |
82.09 |
34.58 |
|
Middle technical school |
582 |
486 |
58,849 |
18,107 |
83.51 |
30.77 |
|
Senior middle school |
5,180 |
4,324 |
405,194 |
119,823 |
83.47 |
29.57 |
|
Universities |
642 |
544 |
74,750 |
21,840 |
84.74 |
29.22 |
|
Total |
29,246 |
24,183 |
1,792,905 |
607,922 |
82.69 |
33.91 |
The Challenge of the Mass Migration of the Labour Force
The social labour force in China in 1992 was 594.32 million, of which 73.7% were classified as rural (National Statistics Bureau 1993). It is reported that one-third of the country’s 440 million rural labourers are actually unemployed (China Daily, 7 Dec. 1993). The vast surplus of labourers who have far exceeded the pool of employability in rural industries are migrating towards urban areas. The mass movement of farmers to the urban areas over the last few years, especially heavy since the beginning of the 1990s, has been the big challenge to the central and local governments. For example, in the first half of 1991, only 200,000 farmers left their hometowns in Jiangxi province, but in 1993, more than three million followed the tide, which accounted for one-fifth of the province’s rural labourers (China Daily, 21 May 1994). On the basis of state statistics, it has been predicted that 250 million rural workers would hit the urban labour market by the end of the century (China Daily, 25 Nov. 1993). In addition, there are about 20 million young people every year entering legal employment age in the entire country (National Statistics Bureau 1993). Thanks to widespread urbanization and the extensive opening to the outside world, which is attracting foreign investment, more job opportunities for migrant rural labourers have been created. The migrants are engaged in a greater variety of business in the cities, including industry, civil engineering, transport, commerce and service trades and most high-risk or hazardous work which urban people do not like to do. These workers have the same personal background as those in the rural township enterprises and are facing similar occupational health problems. In addition, because of their mobility, it is difficult to trace them and employers could easily escape from their responsibilities for the workers’ health. Furthermore, these workers are often involved in various occupations in which the health risk from hazardous exposures might be complicated and it is hard to provide them access to occupational health services. These conditions make the situation more serious.
The Occupational Health Problems Faced in Foreign-Funded Industries
There are currently more than 10 million domestic labourers nationwide employed in over 70,000 foreign-funded enterprises. Preferential policies for encouraging investment of foreign capital, the existence of vast natural resources and a cheap labour force are attracting more and more investors. The State Planning Commission of the State Council has decided to impose fewer administrative examinations on applicants. Local governments were given more power to approve the investment projects. Those involving funding under US$30 million can be decided by local authorities, with registration at the State Planning Commission, and foreign enterprises are encouraged to bid for them (China Daily, 18 May 1994). Of course, foreign-funded enterprises are also very attractive to many Chinese labourers, mainly because of the higher wages to be earned.
During the course of encouraging foreign investment, hazardous industries have also been transferred to this country. The MOPH and other related agencies have long been concerned for the occupational health of the workers in these sectors. Some local surveys have indicated the magnitude of the problem, which involves high exposure to occupational hazards, long working hours, poor working arrangements, special problems for female workers, no proper personal protection, no health examination and education, no medical insurance and discharge of workers who are affected by occupational diseases, among other problems.
The incidence of chemical poisoning accidents has been increasing in recent years. Information from the Guangdong Provincial Institute of Occupational Disease Prevention and Treatment in 1992 reported that two accidents of solvent poisoning happened simultaneously in two overseas-funded toy factories in the Zhuhai special economic zone, resulting in a total of 23 cases of worker toxicity. Of these, 4 persons were afflicted by 1,2-dichloroethane poisoning and three of them died; another 19 cases had benzene analogues (benzene, xylene and toluene) poisoning. These workers had worked in the factories for just less than one year, a few of them for only 20 days (Guangdong Provincial Occupational Disease Prevention and Treatment Hospital 1992). In the same year, two poisoning accidents were reported from Dalian City, Liaoning Province; one had involved 42 workers and another involved 1,053 workers (Dalian City Occupational Disease Prevention and Treatment Institute 1992b). Table 6 shows some basic occupational health–related conditions in three special economic zones (SEZs) in Guangdong and the Dalian Economic and Technological Development Area, surveyed by local OHIs or HEPSs (Dalian City Occupational Disease Prevention and Treatment Institute 1992b).
Table 6. Occupational health-related background in foreign-funded enterprises
|
Area |
No. of enterprises |
No. of employees |
Enterprises with occupational hazards (%) |
Exposed workers (%) |
Enterprises having OHSO1 (%) |
Enterprises providing health examinations (%) |
||
|
Periodic |
Pre-employment |
|||||||
|
Guangdong2 |
657 |
69,996 |
86.9 |
17.9 |
29.3 |
19.6 |
31.2 |
|
|
Dalian3 |
72 |
16,895 |
84.7 |
26.9 |
19.4 |
0.0 |
0.0 |
|
1 Any form of occupational health and safety organization in plan, e.g. clinics, OHS committee, etc.
2 The survey in 1992, in three special economic zones (SEZs): Shenzhen, Zhuhai and Shantou.
3 The survey in 1991 in Dalian Economic and Technological Development Area.
The employers of foreign-funded enterprises, especially small manufacturing factories, ignore governmental regulations and rules in protecting workers’ rights and their health and safety. Only 19.6% or 31.2% of workers in three Guongdong SEZs could get any kind of health examination (see table 6). Those enterprises making no provision for personal protective equipment for exposed workers accounted for 49.2% and only 45.4% of the enterprises provided hazard exposure subsidies (China Daily, 26 Nov. 1993). In Dalian, the situation was even worse. Another survey conducted by the Guangdong Provincial Trade Union in 1993 indicated that more than 61% of employees worked over six days a week (China Daily, 26 Nov. 1993).
Female workers suffer even more from appalling work conditions, according to a report released in June by the All-China Confederation of Trade Unions (ACFTU). A poll conducted by the ACFTU in 1991 and 1992 among 914 foreign-funded enterprises showed that women accounted for 50.4% of the total 160 thousand employees. The proportion of women is higher in some areas in recent years. Many foreign firms did not sign labour contracts with their employees and some factories hired and fired woman workers at will. Some overseas investors employed only unmarried girls between the ages of 18 and 25 years, whom they dismissed once they got married or became pregnant. Meanwhile, many women were often forced to work overtime without extra pay. In a toy factory in Guangzhou, capital of Guangdong Province, workers, most of them women, had to work 15 hours a day. Even then, they were not allowed to take Sundays off or enjoy any annual holiday (China Daily, 6 July 1994). This is not a very rare phenomenon. Details of workers’ occupational health status in foreign-funded enterprises have not yet been made known. From the information above, however, one can imagine the gravity of the problem.
New Problems in State-Owned Enterprises
In order to meet the requirements of a market economy, the state-owned enterprises, especially the large and medium ones, have to transform the traditional operational mechanism and establish a modern enterprise system which would clearly outline property rights and enterprise rights and responsibilities and at the same time push the state-owned enterprises into the market to increase their vitality and efficiency. Some small state-owned enterprises may be leased or sold to collectives or individuals. The reforms have to affect every aspect of business, including occupational health programmes.
At present, losing money is a serious problem faced by many state-owned enterprises. It is reported that about one-third of the enterprises are in deficit. The reasons for this are diverse. First, there is a heavy tax and financial burden intended to take care of a large contingent of retired employees and to provide a host of social welfare benefits to current workers. Second, a huge surplus labour force, about 20 to 30% on average, in an enterprise cannot be released into the existing fragile social security system. Third, the outdated management system was adapted to the traditional planned economy. Fourth, the state-owned enterprises have no competitive policy advantages over foreign-funded firms (China Daily, 7 April 1994).
Under these circumstances, occupational health in the state-owned enterprises tends to become inevitably weakened. First, financial support for health programmes has been reduced in the case of some enterprises and the medical/health institutions in enterprises which used to offer health care only to their own employees before are opening them now to communities. Second, some in-plant health facilities are being divorced from affiliation with enterprises as part of an effort to shift the burden of costs from state-owned enterprises. Before the new social security system was set up, there was concern, too, that funding for occupational health in-plant programmes might also be affected. Third, much outdated technology and equipment has been operating for decades, usually with high levels of hazardous emissions, and cannot be improved or replaced in a short period of time. More than 30% of the worksites of state-owned and city-collective enterprises are not in compliance with national hygienic standards (MAC or MAI). Fourth, the implementation of occupational health regulations or rules has been weakened in recent years; of course, one of the reasons for this is the incompatibility between the old management system of occupational health in the days of central planning with the new situation of enterprise reform. Fifth, to decrease the cost of labour and to offer more widespread employment opportunities, the hiring of temporary or seasonal workers, most of whom are migrants from rural areas, to engage in hazardous work in state-owned enterprises has become a common phenomenon. Many of them cannot get even the simplest personal protective equipment or any safety training from their employers. This has continued to be a potential health threat affecting the working population of China.
Problems in the Occupational Health Service System
The coverage of occupational health services is not extensive enough. As mentioned above, only 20% of the workers exposed to hazards can be covered by periodic health examination, most of whom are working in state-owned enterprises. The reasons why the coverage is so low are as follows:
First, the shortage of occupational health service resources is one of the main factors. This is especially the case for rural industries, which have no capacity to provide such services themselves. The data from the SOHSNCTI has shown that there were 235 occupational health professionals in county HEPSs in 30 sampled counties. They have to deliver occupational health service to 170,613 enterprises with 3,204,576 employees in those areas (MOPH 1992). Thus, each full-time occupational health worker covered an average of 1,115 enterprises and 20,945 employees. Also emerging from the 1989 survey was the fact that the health expenditures of 30 county governments accounted for 3.06% of the total county government expenditures. The total expenditures for both disease prevention and health inspection accounted for only 8.36% of the total county governmental health expenditures. The fraction expended purely on occupational health services was even smaller. Lack of basic equipment for occupational health service is a big problem in the surveyed counties. The average availability of thirteen categories of equipment in 28 of the 30 counties was only 24% of the requirement defined in the national standard (table 7).
Table 7. Routine instruments for occupational health in HEPS of 28 countries in 1990, China
|
Items |
Number of instruments |
Number of instruments required by standard |
Per cent (%) |
|
Air sampler |
80 |
140 |
57.14 |
|
Personal sampler |
45 |
1,120 |
4.02 |
|
Dust sampler |
87 |
224 |
38.84 |
|
Detector for noise |
38 |
28 |
135.71 |
|
Detector for vibration |
2 |
56 |
3.57 |
|
Detector for heat radiation |
31 |
28 |
110.71 |
|
Spectrophotometer (Type 721) |
38 |
28 |
135.71 |
|
Spectrophotometer (Type 751) |
10 |
28 |
35.71 |
|
Mercury determination meter |
20 |
28 |
71.43 |
|
Gas chromatograph |
22 |
28 |
78.57 |
|
Weighing balance (1/10,000g) |
31 |
28 |
110.71 |
|
Electrocardiograph |
25 |
28 |
89.29 |
|
Lung function test |
7 |
28 |
25.00 |
|
Total |
436 |
1,820 |
23.96 |
Second, low utilization of existing occupational health facilities is another factor. The shortage of resources on the one hand and insufficient utilization on the other is the case with occupational health service in China right now. Even at higher levels, for example, with the provincial OHIs, the equipment is still not being fully put to use. The reasons for this are complicated. Traditionally, occupational health and various preventive medical services were all financed and maintained by government, including the wages of health workers, the equipment and buildings, routine outlays and so forth. All occupational health services provided by governmental OHIs were free of charge. With the rapid industrialization and economic reform since 1979, the needs of society for occupational health service have been increasing, and the cost for providing services at the same time increased rapidly, reflecting an increasing price index. The budgets of the OHIs from government, however, have not increased to keep pace with their needs. The more services an OHI provides, the more funding it needs. To promote the development of public health service and meet growing social needs, the central government has instituted the policy of allowing the public health sector to subsidize payments for services, and stipulations have been made to control the price of health services. Because of weak compulsory legislation in providing occupational health service for enterprises in the past, OHIs are finding it difficult to maintain themselves by collecting payment for services.
Further Policy Considerations and Trends in Occupational Health Services
Without doubt, occupational health service is one of the most important issues in a developing country like China, which is undergoing rapid modernization and possesses such huge numbers of workers. While facing the great challenges, the country is also, at the same time, welcoming the great opportunities arising from present social reforms. Many successful experiences exemplified across the international scene can be taken as references. In opening up so widely to the world today, China is willing actively to absorb the advanced occupational health managerial ideas and technologies of the broader world.
Case Study: World Trade Organization
The World Trade Organization (WTO), established in 1995 as the result of the Uruguay Round of multilateral trade negotiations, is the successor to the General Agreement on Tariffs and Trade (GATT), the international trade agreement dating from the late 1940s. The WTO is the legal and institutional foundation of the world’s multilateral trading system. It aims to promote open international trade, not only in goods (as in GATT), but also in services and intellectual property. The WTO also has an explicit goal of advancing development, especially of the least developed countries.
The WTO is designed to promote trade, and related issues such as occupational safety and health are addressed only insofar as they may interfere with free trade. Two Agreements are relevant. The Agreement on the Application of Sanitary and Phytosanitary Measures addresses food safety and animal and plant health regulations. It permits countries to promulgate such regulations, but requires that they be based on science, applied only to the extent necessary to protect human, animal, or plant life or health, and should not arbitrarily discriminate between member countries. While member countries are encouraged to base their regulations on international standards, they are permitted to set more stringent standards if there is scientific justification or if they have based their standards on an appropriate risk assessment. The Agreement on Technical Barriers to Trade reinforces these precepts. Its goal is to prevent technical regulations and standards from posing unnecessary obstacles to trade. To this end, there is a code of good practice for promulgating standards and a requirement that standards be applied equitably to domestic and imported products.
While the foregoing two Agreements pertain principally to environmental, food quality, and pharmaceutical regulations, they could conceivably be applied to occupational health and safety. The summary statement from the 1995 Marrakesh meeting of the WTO provided for the formation of a working party on International Labour Standards. However, the WTO has thus far avoided addressing occupational health and safety, and several member governments, especially those of developing countries, have held that worker health should remain a national prerogative, uncoupled from international trade considerations. Therefore, the WTO has to date played no role in advancing occupational health and safety.
Europe
Economic integration in Europe is distinguished by its early origins, dating to the Treaty of Rome in 1957, and by the prominence that social and political issues have assumed alongside economic considerations. In fact, integration in Europe extends well beyond lowering trade barriers; it also includes the free movement of workers (and soon of people in general), the promulgation of binding transnational laws and regulations, and the creation of a transnational bureaucracy with substantial financial backing. As a result, occupational health has received considerable attention.
The European Economic Community (EEC), or Common Market, was established by the Treaty of Rome in 1957. This Treaty began to lift trade barriers among member nations, and established the EEC’s organizational structure. The Commission of the European Communities became the EEC’s civil service and bureaucracy, with its work carried out by 23 Directorates General (including one, DG V, responsible for employment, industrial relations and social affairs). The Council of Ministers handles major policy-making, while the European Parliament has a co-decision-making role.
The Court of Justice adjudicates disputes that arise under treaties. The Advisory Committee on Safety, Hygiene and Health Protection at Work (ACSH), established by the Council in 1974 to advise the Commission, includes representatives of labour, management, and the governments from each member country, and is supported by staff from the Health and Safety Directorate of the DG V. The ACSH reviews legislative proposals relevant to occupational health, initiates activities on specific hazards, and coordinates joint efforts. The Economic and Social Committee has a consultative role.
In 1978 the Commission introduced the first Action Programme on Health and Safety, with considerable support from the ACSH. It focused on hazardous substances, prevention of machinery hazards, monitoring and inspections and the improvement of attitudes towards health and safety. Since then, successive action programmes have been directed at other occupational health concerns such as ergonomics, occupational health statistics, assistance for small enterprises and training. These have promoted occupational health solutions throughout the member nations, providing training, technical advice and written materials. For example, in 1982 the Commission convened an informal group of senior labour inspectors to encourage personnel and information exchanges among the 12 nations, comparison of member countries’ practices and improved practice. Such initiatives exemplify how the integration of national economies can have positive effects on the practice of occupational health and safety.
The Single European Act (SEA) of 1987 signalled a major step forward in European integration and in the development of the European Free Trade Area. A firm date was set for the establishment of a Single Market, 1992, and activity in a range of social issues, including occupational health, was stimulated. Unanimity among member nations was no longer needed to set policy; instead, a “qualified majority” could do so. Two of the Act’s articles are especially relevant to occupational health. Article 100(a) aims to harmonize product standards in the member countries, a process that has important safety implications. This Article specifies that standards should achieve a “high level of health protection”. Article 118(a) directly addresses occupational health and safety, holding that member countries “shall pay particular attention to encouraging improvements, especially in the working environments, as regards the health and safety of workers, and shall set as their objective the harmonization of conditions in this area while maintaining the improvements made”.
In 1989, two important events further solidified the role of occupational health in the process of European integration. The Social Charter was adopted by 11 of the then 12 Member States, including a clause that emphasized “the need for training, information, consultation and balanced participation of workers as regards the risks incurred and the steps taken to eliminate or reduce them”.
Also in 1989, the Framework Directive was adopted by the Council, the first major policy initiative under the SEA. It defined the EC (now the European Union (EU)) approach to worker health and safety, extending to public and private employees in all member countries. Employers were assigned a general “duty to ensure the safety and heath of workers in every aspect related to work”, and specific duties to:
- evaluate workplace risks
- integrate preventive measures into all aspects of production
- inform workers and their representatives of risks and preventive measures taken
- consult workers and their representatives in all health and safety matters
- provide worker health and safety training
- designate workers with specific health and safety responsibilities
- provide appropriate health surveillance
- protect sensitive risk groups
- maintain injury and illness records.
The Framework Directive adopted a broad view of what workplace factors were relevant to occupational health, including design issues, monotonous work and piece-work. It called for active worker participation in health and safety programmes, including rights to advance consultation with employers on health and safety initiatives, paid time off to perform health and safety functions, meetings with government inspectors and refusal to work in case of “serious, imminent and unavoidable danger” (subject to national laws). A series of so-called daughter directives issued in the wake of the Framework Directive address the use of personal protective equipment, manual handling of loads, work with video display terminals and other issues.
Will the Framework Directive translate into effective national policy? Underlying this issue is the EU’s explicit commitment to the principle of subsidiarity, which holds that all policy should be implemented by member countries rather than by the EU, unless “by reason of the scale of effects of the proposed action” it is better carried out centrally. This will result in tension between the mandates of the central directives and the sovereign actions of the member countries.
Each member country is required to transpose the Framework Directive (like all directives) into national law, to implement policies accordingly and to enforce them in practice. This process leaves countries room for discretion and may allow some non-compliance. By all accounts the EU is not well equipped to monitor member country compliance with its occupational health and safety directives. Closer monitoring of each country’s practices, and the political will to use available remedies in cases of non-compliance (including appeal to the Court of Justice) will be necessary if the EU’s full potential in promoting occupational health is to be realized.
A related question concerns the fate of national policies that are more protective than those of the EU. Since Article 118(a) requires only a minimum common level of workplace protection, there may be a tendency towards downward harmonization in response to economic pressures.
In 1994 the Council, acting on a three-year-old proposal from the Commission, established the European Agency for Safety and Health at Work, sited in Bilbao, Spain. The Agency’s aim is to “provide the Community bodies, the Member States and those involved in the field with the technical, scientific and economic information of use in the field of safety and health at work”. It will focus on technical and scientific consultation to the Commission, information exchange, training, consistent data collection and promoting research.
In 1995 the Commission published its action programme for the period 1996-2000. One important component was continued attention to legislative initiatives—ensuring that Community directives be accurately transported into national law, and promulgating new directives on physical agents, chemical agents, transport, and work equipment. A longstanding Committee of Senior Labour Inspectors was formalized to harmonize methods of workplace inspection and to monitor the implementation of national labour laws. However, there was also considerable emphasis on non-legislative measures, principally information and persuasion. A new initiative, SAFE (Safety Actions for Europe) was announced, to address health and safety problems in small and medium-sized firms. The approach planned was to identify successful initiatives in model firms and to use these as examples for other firms.
In summary, European economic integration and free trade have evolved as part of a broader programme of social and political integration. This process has included serious discussions of social issues, including occupational health and safety. A complicated bureaucracy has several components that bear on workplace health and safety. The reference point for the EU is community law rather than national law, in contrast to every other free-trade agreement. This arrangement is the world’s most advanced example of promoting occupational health and safety as a component of free trade. It will affect more than the EU countries; occupational health and safety considerations will be part of every association, partnership and cooperation agreement between the EU and the countries of Central and Eastern Europe, extending this progressive tradition. The problems that persist—reconciling national sovereignty with coordinated progress, monitoring compliance with Community directives, reconciling differences between more and less progressive countries and sharing scarce technical expertise and resources—will continue to pose challenges to European integration in coming years.
North America
The three nations of North America have been major trading partners for many decades. The first step towards a regional trading agreement was the US-Canada Free Trade Agreement of 1987, which lowered tariffs and other trading restrictions between those two countries. In the early 1990s, in preparation for a continent-wide trade agreement, US and Mexican labour authorities began several cooperative efforts, such as the training of labour inspectors. In 1993 Mexico, Canada and the US ratified the North American Free Trade Agreement (NAFTA), which took effect in 1994 for full implementation over about a decade. NAFTA was designed to abolish most trade restrictions among the three countries.
The process that led to NAFTA differed from the European experience in several ways. NAFTA had a shorter history and was negotiated rapidly. There was no tradition of incorporating social issues into the process. Environmental and labour concerns were ultimately codified in a pair of side agreements that were adopted alongside the NAFTA proper. Environmental groups had been active in the debate leading to NAFTA and won a number of environmental safeguards in the environmental side agreement, but labour groups took a different approach. Unions and their allies, especially in the US and Canada, vigorously opposed NAFTA and campaigned more to block the treaty altogether than for specific labour-friendly provisions. Moreover, there was reluctance among the three governments to relinquish any sovereignty regarding their respective labour laws. As a result NAFTA’s labour side agreement is relatively narrow compared to the environmental side agreement or to the European experience.
The labour side agreement, in an Annex, defines “guiding principles that the Parties are committed to promote, subject to each Party’s domestic law, but do not establish common minimum standards”. These principles include prevention of occupational injuries and illnesses, compensation in cases of occupational injuries and illnesses, protection of migrant workers and children, more traditional labour rights such as freedom of association, the rights to organize, bargain collectively and strike, and prohibition of forced labour. The stated objectives of the side agreement are to improve working conditions, encourage information exchange, data collection and collaborative studies and promote compliance with each country’s labour laws.
The early Articles of the labour side agreement urge each country to publicize its own labour laws internally and to enforce them fairly, equitably and transparently. Next, a Commission for Labour Cooperation is formed. It consists of a Council of the three labour ministers or their designees, which is responsible for policy-making and promoting cooperative activities, and a Secretariat headed by an Executive Director that will prepare background reports and studies and otherwise support the Council. Moreover, each nation is directed to establish a National Administrative Office which will serve as its liaison to the Commission and assist the Commission in its work. Several general procedures are set forth, such as a direction to seek expertise through cooperation with the ILO. However, the agreement defines few specific procedures in support of its objectives.
Much of the concern that drove the side agreement was that a member nation, usually presumed to be Mexico, might, through lax labour practices, gain an unfair trade advantage; this would expose Mexican workers to low wages and unwholesome working conditions and would transfer jobs away from US and Canadian workers. Hence, a large part of the side agreement is dedicated to procedures for handling complaints and grievances. If such a concern arises, the first step is supposed to be consultation between the governments involved at the ministerial level. Next, the Commission may form an Expert Committee of Evaluation (ECE), usually three qualified people “chosen strictly on the basis of objectivity, reliability and sound judgement”, to consider the matter, provided that the matter is trade related and is “covered by mutually recognized labour laws”. The ECE may rely on information provided by the Commission, each member nation, organizations or individuals with relevant expertise, or the public. The ECE report is provided to each member nation.
If the ECE concludes that one country may have failed to enforce its labour standards then a formal dispute resolution process may be triggered. Significantly, this process is available only if the dispute pertains to occupational health and safety, child labour or minimum wages. First, the involved nations attempt to negotiate a settlement. If they cannot agree, an arbitral panel is convened from a roster of experts established and maintained by the Council. The panel presents its findings of fact, its conclusion regarding whether a nation has failed to enforce its standards, and its recommendations for corrective action. If the involved nation does not comply with its recommendations, the panel may be reconvened and may impose fines. If a nation refuses to pay its fine, the ultimate penalty is a suspension of NAFTA benefits, usually through tariff imposition in the sector where the violation occurred, in order to recover the amount of the fine.
Overall, the labour side agreement, as a framework for occupational health and safety under NAFTA, is less extensive than corresponding European arrangements. The focus in NAFTA is on dispute resolution rather than on joint research, information sharing, training, technology development and related initiatives. The dispute resolution process, in the view of labour advocates, is cumbersome, time-consuming and relatively toothless. More importantly, the side agreement expresses no shared commitment to fundamental labour rights. It is assiduous in respecting each nation’s labour laws, and has no provisions for upgrading or harmonizing those that are deficient. Its scope is narrow, and although there has been little experience to date, it is likely that the broad European approach to occupational health, extending to such concerns as shiftwork and stress, will not be replicated.
Asia and Latin America
Although Asia is the world’s fastest growing economic region, free-trade negotiations in the region have not advanced significantly. Neither the ASEAN nor the APEC has addressed occupational health and safety in its trade negotiations. Similarly, the growing trading pacts of Latin America, such as MERCOSUR and the Andean Pact, have included no occupational health and safety initiatives.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."