13. Systemic Conditions
Chapter Editor: Howard M. Kipen
Table of Contents
Figures
Systemic Conditions: An Introduction
Howard M. Kipen
Sick Building Syndrome
Michael J. Hodgson
Multiple Chemical Sensitivities
Mark R. Cullen
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Systemic Conditions: An Introduction
The last edition of this Encyclopaedia did not contain articles on either sick building syndrome (SBS) or multiple chemical sensitivities (MCS) (the latter term was coined by Cullen, 1987). Most practitioners of occupational medicine are not comfortable with such symptomatically driven and frequently psychologically related phenomena, at least partly for the reason that patients with these syndromes do not respond reliably to the standard means of occupational health intervention, namely, exposure reduction. Non-occupational physicians in general medical practice also react similarly: patients with little verifiable pathology, such as those complaining of chronic fatigue syndrome or fibromyalgia, are regarded as more difficult to treat (and generally regard themselves as more disabled) than patients with deforming conditions such as rheumatoid arthritis. There is clearly less regulatory imperative for sick building syndrome and multiple chemical sensitivities than for the classic occupational syndromes such as lead intoxication or silicosis. This discomfort on the part of treating physicians and the lack of appropriate regulatory guidance is unfortunate, however understandable it may be, because it leads to minimization of the importance of these increasingly common, albeit largely subjective and non-lethal complaints. Since many workers with these conditions claim total disability, and few examples of cures can be found, multiple chemical sensitivities and sick building syndrome present important challenges to compensation systems.
In the developed world, since many classic occupational toxins are better controlled, symptomatic syndromes, such as those under present scrutiny that are associated with lower-level exposures, are assuming increasing recognition as significant economic and health concerns. Managers are frustrated by these conditions for a number of reasons. As there are no clear-cut regulatory requirements in most jurisdictions which cover indoor air or hypersusceptible individuals (with the important exception being persons with recognized allergic disorders), it is impossible for management to be certain whether or not they are in compliance. Agent-specific contaminant levels developed for industrial settings, such as the US Occupational Safety and Health Administration’s (OSHA’s) permissible exposure levels (PELs) or the American Conference of Governmental Industrial Hygienists’ (ACGIH’s) threshold limit values (TLVs), are clearly not able to prevent or predict symptomatic complaints in office and school workers. Finally, because of the apparent importance of individual susceptibility and psychological factors as determinants of response to low levels of contaminants, the impact of environmental interventions is not as predictable as many would like before a decision is taken to commit scarce building or maintenance resources. Often after complaints arise, a potential culprit such as elevated volatile organic compound levels with respect to outdoor air is found, and yet following remediation, complaints persist or reoccur.
Employees who suffer from symptoms of either sick building syndrome or multiple chemical sensitivities are often less productive and frequently accusatory when management or government is reluctant to commit themselves to interventions which cannot be reliably predicted to ameliorate symptoms. Clearly, occupational health providers are among the few key individuals who may be able to facilitate reasonable middle ground outcomes to the advantage of all concerned. This is true whether or not an underlying cause is low levels of contaminants, or even in the rare case of true mass hysteria, which may often have low-level environmental triggers. Using skill and sensitivity to address, evaluate and incorporate a combination of factors into solutions is an important approach to management.
Sick building syndrome is the more contained and definable of the two conditions, and has even had definitions established by the World Health Organization (1987). Although there is debate, both in general and in specific instances, about whether a given lesion is more attributable to individual workers or to the building, it is widely acknowledged, based on controlled exposure studies with volatile organic compounds, as well as survey epidemiology, that modifiable environmental factors do drive the kinds of symptom which are subsumed under the following article entitled Sick Building Syndrome. In that article, Michael Hodgson (1992) details the triad of personal, work activity and building factors which may contribute in various proportions to symptoms among a population of workers. A major problem is in maintaining good employee-employer communication while investigation and attempts at remediation take place. Health professionals will usually require expert environmental consultation to assist in the evaluation and remediation of identified outbreaks.
Multiple chemical sensitivities is a more problematic condition to define than sick building syndrome. Some organized medical entities, including the American Medical Association, have published position papers which question the scientific basis of the diagnosis of this condition. Many physicians who practise without a rigorous scientific basis have nevertheless championed the validity of this diagnosis. They rely on unproven or over-interpreted diagnostic tests such as lymphocyte activation or brain imaging and may recommend treatments such as sauna therapies and megadoses of vitamins, practices which have in large part engendered the animosity of groups such as the American Medical Association. However, no one denies that there is a group of patients who present with complaints of becoming symptomatic in response to low levels of ambient chemicals. Their constitutional symptoms overlap those of other subjective syndromes such as chronic fatigue syndrome and fibromyalgia. These symptoms include pain, fatigue and confusion, they worsen with low-level chemical exposure and they are reported to be present in a substantial percentage of patients who have been diagnosed with these other syndromes. Of great import, but still unresolved, is the question whether chemical sensitivity symptoms are acquired (and to what extent) because of a preceding chemical overexposure, or whether—as in the commonly reported situation—they arise without a major identified precipitating event.
Multiple chemical sensitivities is sometimes invoked as an outcome in certain sick building syndrome outbreaks which are not resolved or ameliorated after routine investigation and remediation. Here it is clear that MCS afflicts an individual or small number of people, rarely a population; it is the effect on a population that may even be a criterion for the sick building syndrome by some definitions. MCS seems to be endemic in populations, whereas sick building syndrome is often epidemic; however, preliminary investigations suggest that some degree of chemical sensitivity (and chronic fatigue) may occur in outbreaks, as was found among American veterans of the Persian Gulf conflict. The controlled exposure studies which have done much to clarify the role of volatile organic compounds and irritants in sick building syndrome have yet to be performed in a controlled manner for multiple chemical sensitivities.
Many practitioners claim to recognize MCS when they see it, but there is no agreed-upon definition. It may well be included as a condition which “overlaps” other non-occupational syndromes such as chronic fatigue syndrome, fibromyalgia, somatization disorder and others. Sorting out its relationship to both psychiatric diagnoses and to early reports suggests that when the onset of the syndrome is fairly definable, there is a much lower rate of diagnosable psychiatric co-morbidity (Fiedler et al. 1996). The phenomenon of odor-triggered symptoms is distinctive, but clearly not unique, and the extent to which this is an occupational condition at all is debated. This is important because Dr. Cullen’s (1987) definition, like many others, describes multiple chemical sensitivities as a sequel to a better-characterized occupational or environmental disorder. However, as stated above, symptoms following exposure to ambient levels of odorants are common among individuals both with and without clinical diagnoses, and it may be just as important to explore the similarities between MCS and other conditions as to define the differences (Kipen et al. 1995; Buchwald and Garrity 1994).
Sick Building Syndrome
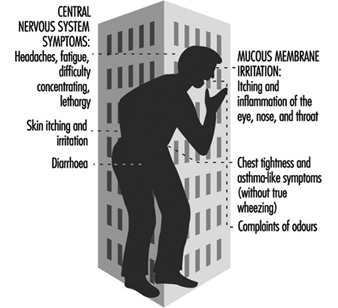
Sick building syndrome (SBS) is a term used to describe office worker discomfort and medical symptoms that are related to building characteristics, to pollutant exposures and to work organization, and that are mediated through personal risk factors. A wide range of definitions exists, but disagreement remains (a) as to whether a single individual in a building can develop this syndrome or whether a set numeric criterion (the proportion affected) should be used; and (b) as to the necessary symptom components. Figure 1 lists symptoms commonly included in SBS; in recent years, with increased understanding, complaints related to odours have generally been dropped from the list and chest symptoms included under mucous membrane irritation. A critical distinction needs to be made between SBS and building-related illness (BRI), where verifiable irritation, allergy or illness such as hypersensitivity pneumonitis, asthma or carbon monoxide-induced headaches may be present as an outbreak associated with a building. SBS should also be distinguished from multiple chemical sensitivities (MCS; see below) which is more sporadic in occurrence, often occurs within an SBS population, and is much less responsive to modifications of the office environment.
Figure 1. Sick building syndrome.
SBS should be simultaneously viewed from and informed by three disparate perspectives. For health professionals, the view is from the perspective of medicine and the health sciences as they define symptoms related to indoor work and their associated pathophysiological mechanisms. The second perspective is that of engineering, including design, commissioning, operations, maintenance and exposure assessment for specific pollutants. The third perspective includes the organizational, social and psychological aspects of work.
Epidemiology
Since the mid-1970s, increasingly voiced office worker discomfort has been studied in formal ways. These have included field epidemiological studies using a building or a workstation as the sampling unit to identify risk factors and causes, population-based surveys to define prevalence, chamber studies of humans to define effects and mechanisms, and field intervention studies.
Cross-sectional and case-control studies
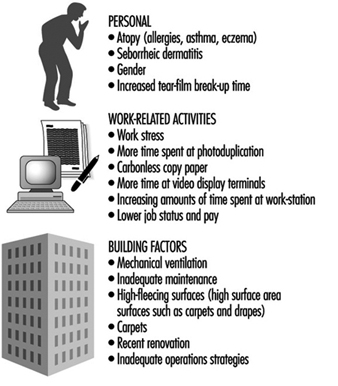
Approximately 30 cross-sectional surveys have been published (Mendell 1993; Sundell et al. 1994). Many of these have included primarily “non-problem” buildings, selected at random. These studies consistently demonstrate an association between mechanical ventilation and increased symptom reporting. Additional risk factors have been defined in several case-control studies. Figure 2 presents a grouping of widely recognized risk factors associated with increased rates of complaints.
Many of these factors overlap; they are not mutually exclusive. For example, the presence of inadequate housekeeping and maintenance, the presence of strong indoor pollution sources and increased individual susceptibility may lead to much greater problems than the presence of any one factor alone.
Figure 2. Risk factors for and causes of the sick building syndrome.
Factor and principal components analyses of questionnaire responses in cross-sectional surveys have explored the interrelationship of various symptoms. Consistently, symptoms related to single organ systems have clustered together more strongly than symptoms relating to different organ systems. That is, eye irritation, eye tearing, eye dryness, and eye itching all appear to correlate very strongly, and little benefit is obtained from looking at multiple symptoms within an organ system.
Controlled exposure studies
Animal testing to determine irritant properties and thresholds has become standard. A consensus method of the American Society for Testing and Materials (1984) is widely regarded as the basic instrument. This method has been used to develop structure-activity relationships, to demonstrate that more than one irritant receptor may exist in the trigeminal nerve and to explore interactions between multiple exposures. Most recently, it has been used to demonstrate the irritating properties of office equipment offgassing.
Analogous to this method, several approaches have been defined to document methods and dose-response relationships for irritation in humans. This work meanwhile suggests that, at least for “non-reactive” compounds such as saturated aliphatic hydrocarbons, the percentage of vapour pressure saturation of a compound is a reasonable predictor of its irritant potency. Some evidence also supports the view that increasing the number of compounds in complex mixtures decreases the irritant thresholds. That is, the more agents that are present, even at a constant mass, the greater the irritation.
Controlled exposure studies have been performed of volunteers in stainless steel chambers. Most have been performed with one constant mixture of volatile organic compounds (VOC) (Mølhave and Nielsen 1992). These consistently document relationships between symptoms and increasing exposure levels. Office workers who perceived themselves as “susceptible” to the effects of usual levels of VOCs indoors demonstrated some impairment on standard tests of neuropsychological performance (Mølhave, Bach and Pederson 1986). Healthy volunteers, on the other hand, demonstrated mucous membrane irritation and headaches at exposures in the range of 10 to 25 mg/m3, but no changes on neuropsychological performance. More recently, office workers demonstrated similar symptoms after simulated work in environments where pollutants from commonly used office equipment were generated. Animals reacted similarly when a standardized test of irritant potency was used.
Population-based studies
To date, three population-based studies have been published in Sweden, Germany and the United States. The questionnaires differed considerably, and thus prevalence estimates cannot be directly compared. Nevertheless, between 20 and 35% of respondents from various buildings not known to be sick were found to have complaints.
Mechanisms
A number of potential mechanisms and objective measures to explain and examine symptoms within specific organ systems have been identified. None of these has a high predictive value for the presence of disease, and they are therefore not suitable for clinical diagnostic use. They are useful in field research and epidemiological investigations. For many of these it is unclear whether they should be regarded as mechanisms, as markers of effect, or as measures of susceptibility.
Eyes
Both allergic and irritant mechanisms have been proposed as explanations for eye symptoms. Shorter tear-film break-up time, a measure of tear film instability, is associated with increased levels of symptoms. “Fat-foam thickness” measurement and photography for documentation of ocular erythema have also been used. Some authors attribute eye symptoms at least in part to increased individual susceptibility as measured by those factors. In addition, office workers with ocular symptoms have been demonstrated to blink less frequently when working at video display terminals.
Nose
Both allergic and irritant mechanisms have been proposed as explanations for nasal symptoms. Measures that have successfully been used include nasal swabs (eosinophils), nasal lavage or biopsy, acoustic rhinometry (nasal volume), anterior and posterior rhinomanometry (plethysmography) and measures of nasal hyperreactivity.
Central nervous system
Neuropsychological tests have been used to document decreased performance on standardized tests, both as a function of controlled exposure (Mølhave, Bach and Pederson 1986) and as a function of the presence of symptoms (Middaugh, Pinney and Linz 1982).
Individual risk factors
Two sets of individual risk factors have been discussed. First, two commonly recognized diatheses, atopy and seborrhea, are considered predisposing factors for medically defined symptoms. Second, psychological variables may be important. For example, personal traits such as anxiety, depression or hostility are associated with sick-role susceptibility. Similarly, work stress is so consistently associated with building-related symptoms that some causal association is likely to be present. Which of the three components of work stress—individual traits, coping skills, and organization function such as poor management styles—is the dominant cause remains undetermined. It is recognized that failing to intervene in a well-defined problem leads workers to experience their discomfort with increasing distress.
Engineering and Sources
Beginning in the late 1970s, the US National Institute for Occupational Safety and Health (NIOSH) responded to requests for help in identifying causes of occupant discomfort in buildings, attributing problems to ventilation systems (50%), microbiological contamination (3 to 5%), strong indoor pollution sources (tobacco 3%, others 14%), pollutants entrained from the outside (15%) and others. On the other hand, Woods (1989) and Robertson (et al. 1988) published two well-known series of engineering analyses of problem buildings, documenting on average the presence of three potential causal factors in each building.
One current professional ventilation standard (American Society of Heating, Refrigerating, and Airconditioning Engineers (1989) suggests two approaches to ventilation: a ventilation rate procedure and an air quality procedure. The former provides a tabular approach to ventilation requirements: office buildings require 20 cubic feet of outside air per occupant per minute to maintain occupant complaint rates of environmental discomfort at below 20%. This assumes relatively weak pollution sources. When stronger sources are present, that same rate will provide less satisfaction. For example, when smoking is permitted at usual rates (according to data from the early 1980s), approximately 30% of occupants will complain of environmental discomfort. The second approach requires the selection of a target concentration in air (particulates, VOCs, formaldehyde, etc.), information on emission rates (pollutant per time per mass or surface), and derives the ventilation requirements. Although this is an intellectually much more satisfying procedure, it remains elusive because of inadequate emissions data and disagreement on target concentrations.
Pollutants
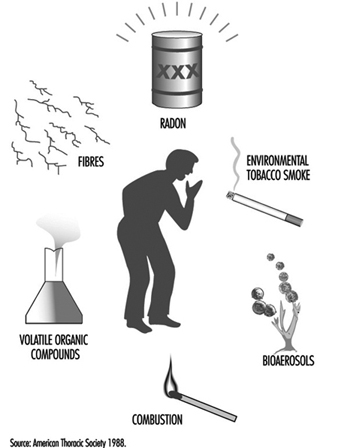
Environmental scientists have generally defined exposure and health effects on a pollutant-by-pollutant basis. The American Thoracic Society (1988) defined six important categories, listed in figure 3.
Figure 3. Principal pollutant categories.
Environmental criteria have been established for many of the individual substances in these six groups. The utility and applicability of such criteria for indoor environments is controversial for many reasons. For example, the goals of threshold limit values often do not include prevention of eye irritation, a common complaint in indoor environments with requirements for close eye work at video display units. For most of the pollutant categories, the problem of interactions, commonly termed the “multiple contaminants problem,” remains inadequately defined. Even for agents that are thought to affect the same receptor, such as aldehydes, alcohols and ketones, no prediction models are well established. Finally, the definition of “representative compounds” for measurement is unclear. That is, pollutants must be measurable, but complex mixtures vary in their composition. It is unclear, for instance, whether the chronic residual odor annoyance due to environmental tobacco smoke correlates better with nicotine, particulates, carbon monoxide or other pollutants. The measure “total volatile organic compounds” is meanwhile considered an interesting concept, but is not useful for practical purposes as the various components have such radically different effects (Mølhave and Nielsen 1992; Brown et al. 1994). Particulates indoors may differ in composition from their outdoor counterparts, as filter sizes affect entrained concentrations, and indoor sources may differ from outdoor sources. There are measurement problems as well, since the sizes of filters used will affect which particles are collected. Different filters may be needed for indoor measurements.
Finally, emerging data suggest that reactive indoor pollutants may interact with other pollutants and lead to new compounds. For example, the presence of ozone, either from office machines or entrained from outdoors, may interact with 4-phenylcyclohexene and generate aldehydes (Wechsler 1992).
Primary Aetiological Theories
Organic solvents
Buildings have always relied on general dilution strategies for pollutant removal, but designers have assumed that humans were the primary source of pollutants. More recently, emissions from “solid materials” (such as particle board desks, carpeting and other furniture), from wet products (such as glues, wall paints, office machine toners) and personal products (perfumes) have been recognized as contributors to a complex mixture of very low levels of individual pollutants (summarized in Hodgson, Levin and Wolkoff 1994).
Several studies suggest that the presence of reactive volatile organic compounds, such as aldehydes and halogenated hydrocarbons, are associated with increasing levels of symptoms. Offices with higher complaint rates have had greater “loss” of VOCs between incoming and outgoing air than did offices with lower complaints. In a prospective study of schools, short chain VOCs were associated with symptom development. In another survey, higher personal samples for VOCs using a screening sampler that “over-reacts” to reactive VOCs, such as aldehydes and halogenated hydrocarbons, were associated with higher symptom levels. In that study, women had higher levels of VOCs in their breathing zone, suggesting another potential explanation for the increased rate of complaints among women. VOCs might adsorb onto sinks, such as fleecy surfaces, and be re-emitted from such secondary sources. The interaction of ozone and relatively non-irritant VOCs to form aldehydes is also consistent with this hypothesis.
The presence of multiple potential sources, the consistency of VOC health effects and SBS symptoms, and the widely recognized problems associated with ventilation systems make VOCs an attractive aetiological agent. Solutions other than better design and operation of ventilation systems include the selection of low-emitting pollutants, better housekeeping and prevention of “indoor chemistry.”
Bioaerosols
Several studies have suggested that bioaerosols have the potential to contribute to occupant discomfort. They may do this through several different mechanisms: irritant emissions; release of fragments, spores or viable organisms leading to allergy; and secretion of complex toxins. Fewer data exist to support this theory than the others. Nevertheless, it is clear that heating, ventilating and air-conditioning systems may be sources of micro-organisms.
They have also been described in building construction materials (as a result of improper curing), as a result of unwanted water incursion and in office dust. The presence of sensitizers in the office environment, such as dust mites or cat dander brought in from home on clothing, presents another possibility of exposure. To the extent that biological agents contribute to the problem, dirt and water management become primary control strategies.
In addition, toxigenic fungi may be found on other porous products in buildings, including ceiling tile, spray-on insulation and wooden joists. Especially in residential environments, fungal proliferation associated with inadequate moisture control has been associated with symptoms.
Psychosocial aspects of work
In all studies where it has been examined, “work stress” was clearly associated with SBS symptoms. Workers’ perceptions of job pressures, task conflicts, and non-work stressors such as spousal or parental demands may clearly lead to the subjective experience of “stronger” irritation as a function of illness behaviour. At times, such perceptions may in fact result from poor supervisory practices. In addition, the presence of irritants leading to subjective irritation is thought to lead to “work stress”.
Evaluation of the Patient
The examination should be directed at identification or exclusion of a significant component of building related illness (BRI). Allergic disease should be identified and optimally managed. However, this must be done with awareness that non-allergic mechanisms may contribute to a substantial residual symptom burden. Sometimes individuals can be reassured of the absence of clear disease by studies such as portable peak flow monitoring or pre- and post-work pulmonary function tests. Once such observable or pathologically verifiable disease has been ruled out, evaluation of the building itself becomes paramount and should be done with industrial hygiene or engineering input. Documentation, management and remediation of identified problems is discussed in Controlling the Indoor Environment.
Conclusion
SBS is a phenomenon that can be experienced by an individual, but is usually seen in groups; it is associated with engineering deficiencies and is likely caused by a series of pollutants and pollutant categories. As with all “dis-ease,” a component of personal psychology serves as an effect modifier that can lead to varying degrees of symptom intensity at any given level of distress.
Multiple Chemical Sensitivities
Introduction
Since the 1980s, a new clinical syndrome has been described in occupational and environmental health practice characterized by the occurrence of diverse symptoms after exposure to low levels of artificial chemicals, although as yet it lacks a widely accepted definition. The disorder may develop in individuals who have experienced a single episode, or recurring episodes of a chemical injury such as solvent or pesticide poisoning. Subsequently, many types of environmental contaminant in air, food or water may elicit a wide range of symptoms at doses below those which produce toxic reactions in others.
Although there may not be measurable impairment of specific organs, the complaints are associated with dysfunction and disability. Although idiosyncratic reactions to chemicals are probably not a new phenomenon, it is believed that multiple chemical sensitivities (MCSs), as the syndrome is now most frequently called, is being brought by patients to the attention of medical practitioners far more commonly than in the past. This syndrome is prevalent enough to have generated substantial public controversy as to who should treat patients suffering with the disorder and who should pay for the treatment, but research has yet to elucidate many scientific issues relevant to the problem, such as its cause, pathogenesis, treatment and prevention. Despite this, MCS clearly does occur and causes significant morbidity in the workforce and general population. It is the purpose of this article to elucidate what is known about it at this time in the hope of enhancing its recognition and management in the face of uncertainty.
Definition and Diagnosis
Although there is no general consensus on a definition for MCS, certain features allow it to be differentiated from other well-characterized entities. These include the following:
- Symptoms typically occur after a definitely characterizable occupational or environmental incident, such as an inhalation of noxious gases or vapours or other toxic exposure. This “initiating” event may be a single episode, such as an exposure to a pesticide spray, or a recurrent one, such as frequent solvent overexposure. Often the effects of the apparently precipitating event, or events, are mild and may merge without clear demarcation into the syndrome which follows.
- Acute symptoms similar to those of the preceding exposure begin to occur after re-exposures to lower levels of various materials, such as petroleum derivatives, perfumes and other common work and household products.
- Symptoms are referrable to multiple organ systems. Central nervous system complaints, such as fatigue, confusion and headache, occur in almost every case. Upper and lower respiratory, cardiac, dermal, gastrointestinal and musculoskeletal symptoms are common.
- It is generally the case that very diverse agents may elicit the symptoms at levels of exposure orders of magnitude below accepted TLVs or guidelines.
- Complaints of chronic symptomatology, such as fatigue, cognitive difficulties, gastrointestinal and musculoskeletal disturbances are common. Such persistent symptoms may predominate over reactions to chemicals in some cases.
- Objective impairment of the organs which would explain the pattern or intensity of complaints is typically absent. Patients examined during acute reactions may hyperventilate or demonstrate other manifestations of excess sympathetic nervous system activity.
- No better established diagnosis easily explains the range of responses or symptoms.
While not every patient precisely meets the criteria, each point should be considered in the diagnosis of MCS. Each serves to rule out other clinical disorders which MCS may resemble, such as somatization disorder, sensitization to environmental antigens (as with occupational asthma), late sequelae of organ system damage (e.g., reactive airways dysfunction syndrome after a toxic inhalation) or a systemic disease (e.g., cancer). On the other hand, MCS is not a diagnosis of exclusion and exhaustive testing is not required in most cases. While many variations occur, MCS is said to have a recognizable character which facilitates diagnosis as much or more than the specific criteria themselves.
In practice, diagnostic problems with MCS occur in two situations. The first is with a patient early in the course of the condition in whom it is often difficult to distinguish MCS from the more proximate occupational or environmental health problem which precedes it. For example, patients who have experienced symptomatic reactions to pesticide spraying indoors may find that their reactions are persisting, even when they avoid direct contact with the materials or spraying activities. In this situation a clinician might assume that significant exposures are still occurring and direct unwarranted effort to altering the environment further, which generally does not relieve the recurrent symptoms. This is especially troublesome in an office setting where MCS may develop as a complication of sick building syndrome. Whereas most office workers will improve after steps are taken to improve air quality, the patient who has acquired MCS continues to experience symptoms, despite the lower exposures involved. Efforts to improve the air quality further typically frustrate patient and employer.
Later in the course of MCS, diagnostic difficulty occurs because of the chronic aspects of the illness. After many months, the MCS patient is often depressed and anxious, as are other medical patients with new chronic diseases. This may lead to an exaggeration of psychiatric manifestations, which may predominate over chemically stimulated symptoms. Without diminishing the importance of recognizing and treating these complications of MCS, nor even the possibility that MCS itself is psychological in origin (see below), the underlying MCS must be recognized in order to develop an effective mode of management which is acceptable to the patient.
Pathogenesis
The pathogenic sequence which leads in certain people from a self-limited episode or episodes of an environmental exposure to the development of MCS is not known. There are several current theories. Clinical ecologists and their adherents have published extensively to the effect that MCS represents immune dysfunction caused by accumulation in the body of exogenous chemicals (Bell 1982; Levin and Byers 1987). At least one controlled study did not confirm immune abnormalities (Simon, Daniel and Stockbridge 1993). Susceptibility factors under this hypothesis may include nutritional deficiencies (e.g., lack of vitamins or antioxidants) or the presence of subclinical infections such as candidiasis. In this theory, the “initiating” illness is important because of its contribution to lifelong chemical overload.
Less well developed, but still very biologically oriented, are the views that MCS represents unusual biological sequelae of chemical injury. As such, the disorder may represent a new form of neurotoxicity due to solvents or pesticides, injury to the respiratory mucosae after an acute inhalational episode or similar phenomena. In this view, MCS is seen as a final common pathway of different primary disease mechanisms (Cullen 1994; Bascom 1992).
A more recent biological perspective has focused on the relationship between the mucosae of the upper respiratory tract and the limbic system, especially with respect to the linkage in the nose (Miller 1992). Under this perspective, relatively small stimulants to the nasal epithelium could produce an amplified limbic response, explaining the dramatic, and often stereotypic, responses to low-dose exposures. This theory also may explain the prominent role of highly odoriferous materials, such as perfumes, in triggering responses in many patients.
Conversely, however, many experienced investigators and clinicians have invoked psychological mechanisms to explain MCS, linking it to other somatoform disorders (Brodsky 1983; Black, Ruth and Goldstein 1990). Variations include the theory that MCS is a variant of post-traumatic stress disorder (Schottenfeld and Cullen 1985) or a conditioned response to an initial toxic experience (Bolle-Wilson, Wilson and Blecker 1988). One group has hypothesized MCS as a late-life response to early childhood traumas such as sexual abuse (Selner and Strudenmayer 1992). In each of these theories, the precipitating illness plays a more symbolic than biological role in the pathogenesis of MCS. Host factors are seen as very important, especially the predisposition to somaticize psychological distress.
Although there is much published literature on the subject, few clinical or experimental studies have appeared to support strongly any of these views. Investigators have not generally defined their study populations nor compared them with appropriately matched groups of control subjects. Observers have not been blinded to subject status or research hypotheses. As a result, most available data are effectively descriptive. Furthermore, the legitimate debate over the aetiology of MCS has been distorted by dogma. Since major economic decisions (e.g., patient benefit entitlements and physician reimbursement acceptance) may hinge upon the way in which cases are viewed, many physicians have very strong opinions about the illness, which limit the scientific value of their observations. Caring for MCS patients requires a recognition of the fact that these theories are often well known to patients, who may also have very strong views on the matter.
Epidemiology
Detailed knowledge of the epidemiology of MCS is not available. Estimates of its prevalence in the US population (from where most reports continue to come) range as high as several percentage points, but the scientific basis for these is obscure, and other evidence exists to suggest that MCS in its clinically apparent form is rare (Cullen, Pace and Redlich 1992). Most available data derive from case series by practitioners who treat MCS patients. These shortcomings notwithstanding, some general observations can be made. Although patients of virtually all ages have been described, MCS occurs most commonly among mid-life subjects. Workers in jobs of higher socio-economic status seem disproportionately affected, while the economically disadvantaged and non-White population seems underrepresented; this may be an artefact of differential access or of clinician bias. Women are more frequently affected than men. Epidemiological evidence strongly implicates some host idiosyncrasy as a risk factor, since mass outbreaks have been uncommon and only a small fraction of victims of chemical accidents or overexposures appear to develop MCS as a sequela (Welch and Sokas 1992; Simon 1992). Perhaps surprising in this regard is the fact that common atopic allergic disorders do not appear to be a strong risk factor for MCS among most groups.
Several groups of chemicals have been implicated in the majority of initiating episodes, specifically organic solvents, pesticides and respiratory irritants. This may be a function of the widespread usage of these materials in the workplace. The other commonplace setting in which many cases occur is in the sick building syndrome, some patients evolving from typical SBS-type complaints into MCS. Although the two illnesses have much in common, their epidemiological features should distinguish them. Sick building syndrome typically affects most individuals sharing a common environment, who improve in response to environmental remediation; MCS occurs sporadically and does not respond predictably to modifications of the office environment.
Finally, there is great interest in whether MCS is a new disorder or a new presentation or perception of an old one. Views are divided according to the proposed pathogenesis of MCS. Those favouring a biological role for environmental agents, including the clinical ecologists, postulate that MCS is a twentieth century disease with rising incidence related to increased chemical usage (Ashford and Miller 1991). Those who support the role of psychological mechanisms see MCS as an old somatoform illness with a new societal metaphor (Brodsky 1983; Shorter 1992). According to this view, the social perception of chemicals as agents of harm has resulted in the evolution of new symbolic content to the historic problem of psychosomatic disease.
Natural History
MCS has not yet been studied sufficiently to define its course or outcome. Reports of large numbers of patients have provided some clues. First, the general pattern of illness appears to be one of early progression as the process of generalization develops, followed by less predictable periods of incremental improvements and exacerbations. While these cycles may be perceived by the patient to be due to environmental factors or treatment, no scientific evidence for such relationships has been established.
Two important inferences follow. First, there is little evidence to suggest that MCS is progressive. Patients do not deteriorate from year to year in any measurable physical way, nor have complications such as infections or organ system failure resulted in the absence of intercurrent illness. There is no evidence that MCS is potentially lethal, despite the perceptions of the patients. While this may be the basis of a hopeful prognosis and reassurance, it has been equally clear from clinical descriptions that complete remissions are rare. While significant improvement occurs, this is generally based on enhanced patient function and sense of well-being. The underlying tendency to react to chemical exposures tends to persist, although symptoms may become sufficiently bearable to allow the victim to return to a normal lifestyle.
Clinical Management
Very little is known about the treatment of MCS. Many traditional and non-traditional methods have been tried, though none has been subjected to the usual scientific standards to confirm their efficacy. As with other conditions, approaches to treatment have paralleled theories of pathogenesis. Clinical ecologists and others, who believe that MCS is caused by immune dysfunction due to high burdens of exogenous chemicals, have focused attention on avoidance of artificial chemicals. This view has been accompanied by use of diagnostic strategies to determine “specific” sensitivities by various invalidated tests to “desensitize” patients. Coupled with this have been strategies to enhance underlying immunity with dietary supplements, such as vitamins and antioxidants, and efforts to eradicate yeasts or other commensal organisms. A most radical approach involves efforts to eliminate toxins from the body by chelation or accelerated turnover of fat where lipid-soluble pesticides, solvents and other organic chemicals are stored.
Those inclined to a psychological view of MCS have tried appropriately alternative approaches. Supportive individual or group therapies and more classic behavioural modification techniques have been described, though the efficacy of these approaches remains conjectural. Most observers have been struck by the intolerance of the patients to pharmacological agents typically employed for affective and anxiety disorders, an impression supported by a small placebo-controlled double-blind trial with fluvoxamine that was conducted by the author and aborted due to side effects in five of the first eight enrolees.
The limitations of present knowledge notwithstanding, certain treatment principles can be enunciated.
First, to the extent possible, the search for a specific “cause” of MCS in the individual case should be minimized—it is fruitless and counterproductive. Many patients have had considerable medical evaluation by the time MCS is considered and equate testing with evidence of pathology and the potential for a specific cure. Whatever the theoretical beliefs of the clinician, it is vital that the existing knowledge and uncertainty about MCS be explained to the patient, including specifically that its cause is unknown. The patient should be reassured that consideration of psychological issues does not make the illness less real, less serious or less worthy of treatment. Patients can also be reassured that MCS is not likely to be progressive or fatal, and they should be made to understand that total cures are not likely with present modalities.
Uncertainty about pathogenesis aside, it is most often necessary to remove the patient from components of their work environment which trigger symptoms. Although radical avoidance is of course counterproductive to the goal of enhancing the worker’s functioning, regular and severe symptomatic reactions should be controlled as far as possible as the basis for a strong therapeutic relationship with the patient. Often this requires a job change. Workers’ compensation may be available; even in the absence of detailed understanding of disease pathogenesis, MCS may correctly be characterized as a complication of a work exposure which is more readily identified (Cullen 1994).
The goal of all subsequent therapy is improvement of function. Psychological problems, such as adjustment difficulties, anxiety and depression should be treated, as should coexistent problems like typical atopic allergies. Since MCS patients do not tolerate chemicals in general, non-pharmacological approaches may be necessary. Most patients need direction, counselling and reassurance to adjust to an illness without an established treatment (Lewis 1987). To the extent possible, patients should be encouraged to expand their activities and should be discouraged from passivity and dependence, which are common responses to the disorder.
Prevention and Control
Obviously, primary prevention strategies cannot be developed given present knowledge of the pathogenesis of the disorder or of its predisposing host risk factors. On the other hand, reduction of opportunities in the workplace for the uncontrolled acute exposures which precipitate MCS in some hosts, such as those involving respiratory irritants, solvents and pesticides, will likely reduce the occurrence of MCS. Proactive measures to improve the air quality of poorly ventilated offices would also probably help.
Secondary prevention would appear to offer a greater opportunity for control, although no specific interventions have been studied. Since psychological factors may play a role in victims of occupational overexposures, careful and early management of exposed persons is advisable even when the prognosis from the point of view of the exposure itself is good. Patients seen in clinics or emergency rooms immediately after acute exposures should be assessed for their reactions to the events and should probably receive very close follow-up where undue concerns of long-term effects or persistent symptoms are noted. Obviously, efforts should be made for such patients to ensure that preventable reoccurrences do not come about, since this kind of exposure may be an important risk factor for MCS regardless of the causal mechanism.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."