12. Skin Diseases
Chapter Editor: Louis-Philippe Durocher
Table of Contents
Tables and Figures
Overview: Occupational Skin Diseases
Donald J. Birmingham
Non-Melanocytic Skin Cancer
Elisabete Weiderpass, Timo Partanen, Paolo Boffetta
Malignant Melanoma
Timo Partanen, Paolo Boffetta, Elisabete Weiderpass
Occupational Contact Dermatitis
Denis Sasseville
Prevention of Occupational Dermatoses
Louis-Phillipe Durocher
Occupational Nail Dystrophy
C.D. Calnan
Stigmata
H. Mierzecki
Tables
Click a link below to view table in article context.
1. Occupations at risk
2. Types of contact dermatitis
3. Common irritants
4. Common skin allergens
5. Predisposing factors for occupational dermatitis
6. Examples of skin irritants & sensitizers with occupations
7. Occupational dermatoses in Quebec in 1989
8. Risk factors & their effects on the skin
9. Collective measures (group approach) to prevention
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Overview: Occupational Skin Diseases
The growth of industry, agriculture, mining and manufacturing has been paralleled by the development of occupational diseases of the skin. The earliest reported harmful effects were ulcerations of the skin from metal salts in mining. As populations and cultures have expanded the uses of new materials, new skills and new processes have emerged. Such technological advances brought changes to the work environment and during each period some aspect of the technical change has impaired workers’ health. Occupational diseases, in general and skin diseases, in particular, have long been an unplanned by-product of industrial achievement.
Fifty years ago in the United States, for example, occupational diseases of the skin accounted for no less than 65-70% of all reported occupational diseases. Recently, statistics collected by the United States Department of Labor indicate a drop in frequency to approximately 34%. This decreased number of cases is said to have resulted from increased automation, from enclosure of industrial processes and from better education of management, supervisors and workers in the prevention of occupational diseases in general. Without doubt such preventive measures have benefited the workforce in many larger plants where good preventive services may be available, but many people are still employed in conditions which are conducive to occupational diseases. Unfortunately, there is no accurate assessment of the number of cases, causal factors, time lost or actual cost of occupational skin disease in most countries.
General terms, such as industrial or occupational dermatitis or professional eczema, are used for occupational skin diseases but names related both to cause and effect are also commonly used. Cement dermatitis, chrome holes, chloracne, fibreglass itch, oil bumps and rubber rash are some examples. Because of the variety of skin changes induced by agents or conditions at work, these diseases are appropriately called occupational dermatoses—a term which includes any abnormality resulting directly from, or aggravated by, the work environment. The skin can also serve as an avenue of entry for certain toxicants which cause chemical poisoning via percutaneous absorption.
Cutaneous Defence
From experience we know that the skin can react to a large number of mechanical, physical, biological and chemical agents, acting alone or in combination. Despite this vulnerability, occupational dermatitis is not an inevitable accompaniment of work. The majority of the workforce manages to remain free of disabling occupational skin problems, due in part to the inherent protection provided by the skin’s design and function, and in part due to the daily use of personal protective measures directed towards minimizing skin contact with known skin hazards at the worksite. Hopefully, the absence of disease in the majority of workers may also be due to jobs which have been designed to minimize exposure to conditions hazardous to the skin.
The skin
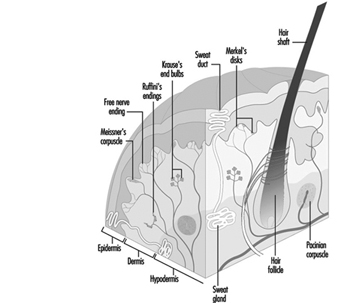
Human skin, except for palms and soles, is quite thin and of variable thickness. It has two layers: the epidermis (outer) and dermis (inner). Collagen and elastic components in the dermis allow it to function as a flexible barrier. The skin provides a unique shield which protects within limits against mechanical forces, or penetration by various chemical agents. The skin limits water loss from the body and guards against the effects of natural and artificial light, heat and cold. Intact skin and its secretions provide a fairly effective defence zone against micro-organisms, providing mechanical or chemical injury does not impair this defence. Figure 1 provides an illustration of the skin and description of its physiological functions.
Figure 1. Schematic representation of the skin.
The outer epidermal layer of dead cells (keratin) provides a shield against elements in the outside world. These cells, if exposed to frictional pressures, can form a protective callus and can thicken after ultraviolet exposure. Keratin cells are normally arranged in 15 or 16 shingle-like layers and provide a barrier, though limited, against water, water-soluble materials and mild acids. They are less able to act as a defence against repeated or prolonged contact with even low concentrations of organic or inorganic alkaline compounds. Alkaline materials soften but do not totally dissolve the keratin cells. The softening disturbs their inner structure enough to weaken cellular cohesiveness. The integrity of the keratin layer is allied to its water content which, in turn, influences its pliability. Lowered temperatures and humidity, dehydrating chemicals such as acids, alkali, strong cleaners and solvents, cause water loss from the keratin layer, which, in turn, causes the cells to curl and crack. This weakens its ability to serve as a barrier and compromises its defence against water loss from the body and entry of various agents from outside.
Cutaneous defence systems are effective only within limits. Anything which breaches one or more of the links endangers the entire defence chain. For example, percutaneous absorption is enhanced when the continuity of the skin has been altered by physical or chemical injury or by mechanical abrasion of the keratin layer. Toxic materials can be absorbed not only through the skin, but also through the hair follicules, sweat orifices and ducts. These latter routes are not as important as transepidermal absorption. A number of chemicals used in industry and in farming have caused systemic toxicity by absorption through the skin. Some well established examples are mercury, tetraethyllead, aromatic and amino nitro compounds and certain organophosphates and chlorinated hydrocarbon pesticides. It should be noted that for many substances, systemic toxicity generally arises through inhalation but percutaneous absorption is possible and should not be overlooked.
A remarkable feature of cutaneous defence is the ability of the skin to continually replace the basal cells which provide the epidermis with its own built-in replication and repair system.
The skin’s ability to act as a heat exchanger is essential to life. Sweat gland function, vascular dilation and constriction under nervous control are vital to regulating body heat, as is evaporation of surface water on skin. Constriction of the blood vessels protects against cold exposures by preserving central body heat. Multiple nerve endings within the skin act as sensors for heat, cold and other excitants by relaying the presence of the stimulant to the nervous system which responds to the provoking agent.
A major deterrent against injury from ultraviolet radiation, a potentially harmful component of sunlight and some forms of artificial light is the pigment (melanin) manufactured by the melanocytes located in the basal cell layer of the epidermis. Melanin granules are picked up by the epidermal cells and serve to add protection against the rays of natural or artificial light which penetrate the skin. Additional protection, though less in degree, is furnished by the keratin cell layer which thickens following ultraviolet exposure. (As discussed below, for those whose worksites are outdoors it is essential to protect exposed skin with a sun-screen coating agent having a protective against UV-A and against UV-B (rating of 15 or greater) together with appropriate clothing to provide a high level of shielding against sun light injury.)
Types of Occupational Skin Diseases
Occupational dermatoses vary both in their appearance (morphology) and severity. The effect of an occupational exposure may range from the slightest erythema (reddening) or discoloration of the skin to a far more complex change, as a malignancy. Despite the wide range of substances that are known to cause skin effects, in practice it is difficult to associate a specific lesion with exposure to a specific material. However, certain chemical groups are associated with characteristic reaction patterns. The nature of the lesions and their location may provide a strong clue as to causality.
A number of chemicals with or without direct toxic effect on the skin can also cause systemic intoxication following absorption through the skin. In order to act as a systemic toxin, the agent must pass through the keratin and the epidermal cell layers, then through the epidermal-dermal junction. At this point it has ready access to the bloodstream and the lymphatic system and can now be carried to vulnerable target organs.
Acute contact dermatitis (irritant or allergic).
Acute contact eczematous dermatitis can be caused by hundreds of irritant and sensitizing chemicals, plants and photoreactive agents. Most occupational allergic dermatoses can be classified as acute eczematous contact dermatitis. Clinical signs are heat, redness, swelling, vesiculation and oozing. Symptoms include itch, burning and general discomfort. The back of the hands, the inner wrists and the forearms are the usual sites of attack, but acute contact dermatitis can occur anywhere on the skin. If the dermatosis occurs on the forehead, the eyelids, the ears, the face or the neck, it is logical to suspect that a dust or a vapour may be involved in the reaction. When there is a generalized contact dermatitis, not restricted to one or a few specific sites, it is usually caused by a more extensive exposure, such as the wearing of contaminated clothing, or by autosensitization from a pre-existing dermatitis. Severe blistering or destruction of tissue generally indicates the action of an absolute or strong irritant. The exposure history, which is taken as part of the medical control of occupational dermatitis, may reveal the suspected causative agent. An accompanying article in this chapter provides more details on contact dermatitis.
Sub-acute contact dermatitis
Through a cumulative effect repeated contact with both weak and moderate irritants can cause a sub-active form of contact dermatitis characterized by dry, red plaques. If the exposure continues, the dermatitis will become chronic.
Chronic eczematous contact dermatitis
When a dermatitis recurs over an extended period of time it is called chronic eczematous contact dermatitis. The hands, fingers, wrists and forearms are the sites most often affected by chronic eczematous lesions, characterized by dry, thickened and scaly skin. Cracking and fissuring of the fingers and the palms may be present. Chronic nail dystrophy is also commonly found. Frequently, the lesions will begin to ooze (sometimes called “weeping”) because of re-exposure to the responsible agent or by imprudent treatment and care. Many materials not responsible for the original dermatosis will sustain this chronic recurrent skin problem.
Photosensitivity dermatitis (phototoxic or photoallergic)
Most photoreactions on the skin are phototoxic. Either natural and artificial light sources alone or in combination with various chemicals, plants or drugs can induce a phototoxic or photosensitive response. Phototoxic reaction is generally limited to light-exposed areas while photosensitive reaction can develop frequently on non-exposed body surfaces. Some examples of photoreactive chemicals are coal tar distillation products, such as creosote, pitch and anthracene. Members of the plant family Umbelliferae are well known photoreactors. Family members include cow parsnip, celery, wild carrot, fennel and dill. The reactive agent in these plants are psoralens.
Folliculitis and acneform dermatoses, including chloracne
Workers with dirty jobs often develop lesions involving the follicular openings. Comedones (blackheads) may be the only obvious effect of the exposure, but often a secondary infection of the follicle may ensure. Poor personal hygiene and ineffective cleansing habits can add to the problem. Follicular lesions generally occur on the forearms and less often on the thighs and buttocks, but they can occur anywhere except on the palms and soles.
Follicular and acneform lesions are caused by overexposure to insoluble cutting fluids, to various tar products, paraffin, and certain aromatic chlorinated hydrocarbons. The acne caused by any of the above agents can be extensive. Chloracne is the most serious form, not only because it can lead to disfigurement (hyperpigmentation and scarring) but also because of the potential liver damage, including porphyria cutanea tarda and other systemic effects that the chemicals can cause. Chloronaphthalenes, chlorodi-phenyls, chlorotriphenyls, hexachlorodibenzo-p-dioxin, tetrachloroazoxybenzene and tetrachlorodibenzodioxin (TCDD), are among the chloracne-causing chemicals. The blackheads and cystic lesions of chloracne often appear first on the sides of the forehead and the eyelids. If exposure continues, lesions may occur over widespread areas of the body, except for the palms and soles.
Sweat-induced reactions
Many types of work involve exposure to heat and where there is too much heat and sweating, followed by too little evaporation of the sweat from the skin, prickly heat can develop. When there is chafing of the affected area by skin rubbing against skin, a secondary bacterial or fungal infection may frequently occur. This happens particularly in the underarm area, under the breast, in the groin and between the buttocks.
Pigment change
Occupationally induced changes in skin colour can be caused by dyes, heavy metals, explosives, certain chlorinated hydrocarbons, tars and sunlight. The change in skin colour may be the result of a chemical reaction within the keratin, as for example, when the keratin is stained by metaphenylene-diamine or methylene blue or trinitrotoluene. Sometimes permanent discoloration may occur more deeply in the skin as with argyria or traumatic tattoo. Increased pigmentation induced by chlorinated hydrocarbons, tar compounds, heavy metals and petroleum oils generally results from melanin stimulation and overproduction. Hypopigmentation or depigmentation at selected sites can be caused by a previous burn, contact dermatitis, contact with certain hydroquinone compounds or other antioxidant agents used in selected adhesives and sanitizing products. Among the latter are tertiary amyl phenol, tertiary butyl catechol and tertiary butyl phenol.
New growths
Neoplastic lesions of occupational origin may be malignant or benign (cancerous or non-cancerous). Melanoma and non-melanocytic skin cancer are discussed in two other articles in this chapter. Traumatic cysts, fibromata, asbestos, petroleum and tar warts and keratoacanthoma, are typical benign new growths. Keratoacanthomas can be associated with excessive exposure to sunlight and also have been ascribed to contact with petroleum, pitch and tar.
Ulcerative changes
Chromic acid, concentrated potassium dichromate, arsenic trioxide, calcium oxide, calcium nitrate and calcium carbide are documented ulcerogenic chemicals. Favourite attack sites are the fingers, hands, folds and palmar creases. Several of these agents also cause perforation of the nasal septum.
Chemical or thermal burns, blunt injury or infections resulting from bacteria and fungi may result in ulcerous excavations on the affected part.
Granulomas
Granulomas can arise from many occupational sources if the appropriate circumstances are present. Granulomas can be caused by occupational exposures to bacteria, fungi, viruses or parasites. Inanimate substances, such as bone fragments, wood splinters, cinders, coral and gravel, and minerals such as beryllium, silica and zirconium, can also cause granulomas after skin embedment.
Other conditions
Occupational contact dermatitis accounts for at least 80% of all cases of occupational skin diseases. However, a number of other changes that affect the skin, hair and nails are not included in the foregoing classification. Hair loss caused by burns, or mechanical trauma or certain chemical exposures, is one example. A facial flush that follows the combination of drinking alcohol and inhaling certain chemicals, such as trichlorethylene and disulfuram, is another. Acroosteolysis, a type of bony disturbance of the digits, plus vascular changes of the hands and forearm (with or without Raynaud’s syndrome) has been reported among polyvinyl chloride polymerization tank cleaners. Nail changes are covered in a separate article in this chapter.
Physiopathology or Mechanismsof Occupational Skin Diseases
The mechanisms by which primary irritants act are understood only in part—for instance, vesicant or blister gases (nitrogen mustard or bromomethane and Lewisite, etc.)—interfere with certain enzymes and thereby block selective phases in the metabolism of carbohydrates, fats and proteins. Why and how the blister results is not clearly understood but observations of how chemicals react outside the body yield some ideas about possible biological mechanisms.
In brief, because alkali reacts with acid or lipid or protein, it has been presumed that it also reacts with skin lipid and protein. In so doing, surface lipids are changed and keratin structure becomes disturbed. Organic and inorganic solvents dissolve fats and oils and have the same effect on cutaneous lipids. Additionally, however, it appears that solvents abstract some substance or change the skin in such a way that the keratin layer dehydrates and the skin’s defence is no longer intact. Continued insult results in an inflammatory reaction eventuating in contact dermatitis.
Certain chemicals readily combine with the water within skin or on the surface of the skin, and cause a vigorous chemical reaction. Calcium compounds, such as calcium oxide and calcium chloride, produce their irritant effect in this way.
Substances such as coal tar pitch, creosote, crude petroleum, certain aromatic chlorinated hydrocarbons, in combination with sunlight exposure, stimulate the pigment-producing cells to over function, leading to hyperpigmentation. Acute dermatitis also may give rise to hyperpigmentation after healing. Conversely, burns, mechanical trauma, chronic contact dermatitis, contact with monobenzyl ether of hydroquinone or certain phenolics can induce hypo- or de-pigmented skin.
Arsenic trioxide, coal tar pitch, sunlight and ionizing radiation, among other agents, can damage the skin cells so that abnormal cell growth results in cancerous change of the exposed skin.
Unlike primary irritation, allergic sensitization is the result of a specifically acquired alteration in the capacity to react, brought about by T-cell activation. For several years it has been agreed that contact allergic eczematous dermatitis accounts for about 20% of all the occupational dermatoses. This figure is probably too conservative in view of the continued introduction of new chemicals, many of which have been shown to cause allergic contact dermatitis.
Causes of Occupational Skin Diseases
Materials or conditions known to cause occupational skin disease are unlimited. They are currently divided into mechanical, physical, biological and chemical categories, which continue to grow in number each year.
Mechanical
Friction, pressure or other forms of more forceful trauma may induce changes ranging from callus and blisters to myositis, tenosynovitis, osseous injury, nerve damage, laceration, shearing of tissue or abrasion. Lacerations, abrasions, tissue disruption and blisters additionally pave the way for secondary infection by bacteria or, less often, fungi to set in. Almost everyone is exposed each day to one or more forms of mechanical trauma which may be mild or moderate in degree. However, those who use pneumatic riveters, chippers, drills and hammers are at greater risk of suffering neurovascular, soft tissue, fibrous or bone injury to the hands and forearms. because of the repetitive trauma from the tool. The use of vibration-producing tools which operate in a certain frequency range can induce painful spasms in the fingers of the tool-holding hand. Transfer to other work, where possible, generally provides relief. Modern equipment is designed to reduce vibration and thus obviate the problems.
Physical agents
Heat, cold, electricity, sunlight, artificial ultraviolet, laser radiation and high energy sources such as x rays, radium and other radioactive substances are potentially injurious to skin and to the entire body. High temperature and humidity at work or in a tropical work environment can impair the sweat mechanism and cause systemic effects known as sweat retention syndrome. Milder exposure to heat may induce prickly heat, intertrigo (chafing), skin maceration and supervening bacterial or fungal infection, particularly in overweight and diabetic individuals.
Thermal burns are frequently experienced by electric furnace operators, lead burners, welders, laboratory chemists, pipe-line workers, road repairmen, roofers and tar plant workers contacting liquid tar. Prolonged exposure to cold water or lowered temperatures causes mild to severe injury ranging from erythema to blistering, ulceration and gangrene. Frostbite affecting the nose, ears, fingers and toes of construction workers, firemen, postal workers, military personnel and other outdoor workers is a common form of cold injury.
Electricity exposure resulting from contact with short circuits, bare wires or defective electrical apparatus cause burns of the skin and destruction of deeper tissue.
Few workers are without exposure to sunlight and some individuals with repeated exposure incur severe actinic damage to skin. Modern industry also has many sources of potentially injurious artificial ultraviolet wavelengths, such as in welding, metal burning, molten-metal pouring, glass blowing, electric furnace tending, plasma torch burning and laser beam operations. Apart from the natural capacity of ultraviolet rays in natural or artificial light to injure skin, coal tar and several of its by-products, including certain dyes, selected light-receptive components of plants and fruits and a number of topical and parenteral medications contain harmful chemicals which are activated by certain wavelengths of ultraviolet rays. Such photoreaction effects may operate by either phototoxic or photoallergic mechanisms.
High-intensity electromagnetic energy associated with laser beams is well able to injure human tissue, notably the eye. Skin damage is less of a risk but can occur.
Biological
Occupational exposures to bacteria, fungi, viruses or parasites may cause primary or secondary infections of the skin. Prior to the advent of modern antibiotic therapy, bacterial and fungal infections were more commonly encountered and associated with disabling illness and even death. While bacterial infections can occur in any kind of work setting, certain jobs, such as animal breeders and handlers, farmers, fishermen, food processors and hide handlers have greater exposure potential. Similarly, fungal (yeast) infections are common among bakers, bartenders, cannery workers, cooks, dishwashers, child-care workers and food processors. Dermatoses due to parasitic infections are not common, but when they do occur they are seen most often among agricultural and livestock workers, grain handlers and harvesters, longshoremen and silo workers.
Cutaneous viral infections caused by work are few in number, yet some, such as milker’s nodules among dairyworkers, herpes simplex among medical and dental personnel and sheep pox among livestock handlers continue to be reported.
Chemicals
Organic and inorganic chemicals are the major source of hazards to the skin. Hundreds of new agents enter the work environment each year and many of these will cause cutaneous injury by acting as primary skin irritants or allergic sensitizers. It has been estimated that 75% of the occupational dermatitis cases are caused by primary irritant chemicals. However, in clinics where the diagnostic patch test is commonly used, the frequency of occupational allergic contact dermatitis is increased. By definition, a primary irritant is a chemical substance which will injure every person’s skin if sufficient exposure takes place. Irritants can be rapidly destructive (strong or absolute) as would occur with concentrated acids, alkalis, metallic salts, certain solvents and some gases. Such toxic effects can be observed within a few minutes, depending upon the concentration of the contactant and the length of contact which occurs. Conversely, dilute acids and alkalis, including alkaline dusts, various solvents and soluble cutting fluids, among other agents, may require several days of repeated contact to produce observable effects. These materials are termed “marginal or weak irritants”.
Plants and woods
Plants and woods are often classified as a separate cause of skin disease, but they can also be correctly included in the chemical grouping. Many plants cause mechanical and chemical irritation and allergic sensitization, while others have gained attention because of their photoreactive capacity. The family Anacardiaceae, which includes poison ivy, poison oak, poison sumac, cashew-nut shell oil and the Indian marking nut, is a well-known cause of occupational dermatitis due to its active ingredients (polyhydric phenols). Poison ivy, oak and sumac are common causes of allergic contact dermatitis. Other plants associated with occupational and non-occupational contact dermatitis include castor bean, chrysanthemum, hops, jute, oleander, pineapple, primrose, ragweed, hyacinth and tulip bulbs. Fruits and vegetables, including asparagus, carrots, celery, chicory, citrus fruits, garlic and onions, have been reported as causing contact dermatitis in harvesters, food packing and food preparation workers.
Several varieties of wood have been named as causes of occupational dermatoses among lumberers, sawyers, carpenters and other wood craftspeople. However, the frequency of skin disease is much less than is experienced from contact with poisonous plants. It is likely that some of the chemicals used for preserving the wood cause more dermatitic reactions than the oleoresins contained in wood. Among the preservative chemicals used to protect against insects, fungi and deterioration from soil and moisture are chlorinated diphenyls, chlorinated naphthalenes, copper naphthenate, creosote, fluorides, organic mercurials, tar and certain arsenical compounds, all known causes of occupational skin diseases.
Non-Occupational Factors in OccupationalSkin Disease
Considering the numerous direct causes of occupational skin disease cited above, it can be readily understood that practically any job has obvious and often hidden hazards. Indirect or predisposing factors may also merit attention. A predisposition can be inherited and related to skin colour and type or it may represent a skin defect acquired from other exposures. Whatever the reason, some workers have lower tolerance to materials or conditions in the work environment. In large industrial plants, medical and hygiene programmes can provide the opportunity for placement of such employees in work situations that will not further impair their health. In small plants, however, predisposing or indirect causal factors may not be given proper medical attention.
Pre-existing skin conditions
Several non-occupational diseases affecting the skin can be worsened by various occupational influences.
Acne. Adolescent acne in employees is generally made worse by machine tool, garage and tar exposures. Insoluble oils, various tar fractions, greases and chloracnegenic chemicals are definite hazards to these people.
Chronic eczemas. Detecting the cause of chronic eczema affecting the hands and sometimes distant sites can be elusive. Allergic dermatitis, pompholyx, atopic eczema, pustular psoriasis and fungal infections are some examples. Whatever the condition, any number of irritant chemicals, including plastics, solvents, cutting fluids, industrial cleansers and prolonged moisture, can worsen the eruption. Employees who must continue to work will do so with much discomfort and probably lowered efficiency.
Dermatomycosis. Fungal infections can be worsened at work. When fingernails become involved it may be difficult to assess the role of chemicals or trauma in the nail involvement. Chronic tinea of the feet is subject to periodic worsening, particularly when heavy footgear is required.
Hyperhidrosis. Excessive sweating of the palms and soles can soften the skin (maceration), particularly when impervious gloves or protective footgear are required. This will increase a person’s vulnerability to the effects of other exposures.
Miscellaneous conditions. Employees with polymorphous light eruption, chronic discoid lupus erythematous, porphyria or vitiligo are definitely at greater risk, particularly if there is simultaneous exposure to natural or artificial ultraviolet radiation.
Skin type and pigmentation
Redheads and blue-eyed blondes, particularly those of Celtic origin, have less tolerance to sunlight than people of darker skin type. Such skin is also less able to tolerate exposures to photoreactive chemicals and plants and is suspected of being more susceptible to the action of primary irritant chemicals, including solvents. In general, black skin has a superior tolerance to sunlight and photoreactive chemicals and is less prone to the induction of cutaneous cancer. However, darker skin tends to respond to mechanical, physical or chemical trauma by displaying post-inflammatory pigmentation. It is also more prone to develop keloids following trauma.
Certain skin types, such as hairy, oily, swarthy skins, are more likely to incur folliculitis and acne. Employees with dry skin and those with ichthyoses are at a disadvantage if they must work in low humidity environments or with chemical agents which dehydrate skin. For those workers who sweat profusely, a need to wear impervious protective gear will add to their discomfort. Similarly, overweight individuals usually experience prickly heat during the warm months in hot working environments or in tropical climates. While sweat can be helpful in cooling the skin, it can also hydrolyze certain chemicals that will act as skin irritants.
Diagnosing Occupational Skin Diseases
Cause and effect of occupational skin disease can be best ascertained through a detailed history, which should cover the past and present health and work status of the employee. Family history, particularly of allergies, personal illness in childhood and the past, is important. The title of the job, the nature of the work, the materials handled, how long the job has been done, should be noted. It is important to know when and where on the skin the rash appeared, the behaviour of the rash away from work, whether other employees were affected, what was used to cleanse and protect the skin, and what has been used for treatment (both self-medication and prescribed medication); as well as whether the employee has had dry skin or chronic hand eczema or psoriasis or other skin problems; what drugs, if any, have been used for any particular disease; and finally, which materials have been used in home hobbies such as the garden or woodworking or painting.
The following elements are important parts of the clinical diagnosis:
- Appearance of the lesions. Acute or chronic eczematous contact dermatosis are most common. Follicular, acneform, pigmentary, neoplastic, ulcerative granulomatous lesions and conditions such as Raynaud’s syndrome and contact urticaria can occur.
- Sites involved. The hands, the digits, the wrists and the forearms are the most common sites affected. Exposure to dusts and fumes usually cause the dermatosis to appear on the forehead, face, and V of the neck. Widespread dermatitis can result from autosensitization (spread) of an occupational or nonoccupational dermatosis.
- Diagnostic tests. Laboratory tests should be employed when necessary for the detection of bacteria, fungi and parasites. When allergic reactions are suspect, diagnostic patch tests can be used to detect occupational as well as non-occupational allergies, including photosensitization. Patch tests are a highly useful procedure and are discussed in an accompanying article in this chapter. At times, useful information can be obtained through the use of analytical chemical examination of blood, urine, or tissue (skin, hair, nails).
- Course. Of all the cutaneous changes induced by agents or certain conditions at work, acute and chronic eczematous contact dermatoses are foremost in number. Next in frequency are follicular and acneform eruptions. The other categories, including chloracne, constitute a smaller but still important group because of their chronic nature and the scarring and disfigurement which may be present.
An occupationally induced acute contact eczematous dermatitis tends to improve upon cessation of contact. Additionally, modern therapeutic agents can facilitate the period of recovery. However, if a worker returns to work and to the same conditions, without proper preventive measures undertaken by the employer and necessary precautions explained and understood by the worker, it is probable that the dermatosis will recur soon after re-exposure.
Chronic eczematous dermatoses, acneform lesions and pigmentary changes are less responsive to treatment even when contact is eliminated. Ulcerations usually improve with elimination of the source. With granulomatous and tumour lesions, eliminating contact with the offending agent may prevent future lesions but will not dramatically change already existing disease.
When a patient with a suspected occupational dermatosis has not improved within two months after no longer having contact with the suspected agent, other reasons for the persistence of the disease should be explored. However, dermatoses caused by metals such as nickel or chrome have a notoriously prolonged course partly because of their ubiquitous nature. Even removal from work cannot eliminate the workplace as the source of the disease. If these and other potential allergens have been eliminated as causal, it is reasonable to conclude that the dermatitis is either non-occupational or is being perpetuated by non-occupational contacts, such as maintenance and repair of automobiles and boats, tile setting glues, garden plants or including even medical therapy, prescribed or otherwise.
Non-Melanocytic Skin Cancer
There are three histological types of non-melanocytic skin cancers (NMSC) (ICD-9: 173; ICD-10: C44): basal cell carcinoma, squamous cell carcinoma and rare soft tissue sarcomas involving the skin, subcutaneous tissue, sweat glands, sebaceous glands and hair follicles.
Basal cell carcinoma is the most common NMSC in white populations, representing 75 to 80% of them. It develops usually on the face, grows slowly and has little tendency to metastasize.
Squamous cell cancers account for 20 to 25% of reported NMSCs. They can occur on any part of the body, but especially on the hands and legs and can metastasize. In darkly pigmented populations squamous cell cancers are the most common NMSC.
Multiple primary NMSCs are common. The bulk of the NMSCs occur on the head and neck, in contrast with most of the melanomas which occur on the trunk and limbs. The localization of NMSCs reflects clothing patterns.
NMSCs are treated by various methods of excision, radiation and topical chemotherapy. They respond well to treatment and over 95% are cured by excision (IARC 1990).
The incidence of NMSCs is hard to estimate because of gross underreporting and since many cancer registries do not record these tumours. The number of new cases in the US was estimated at 900,000 to 1,200,000 in 1994, a frequency comparable to the total number of all non-cutaneous cancers (Miller & Weinstock 1994). The reported incidences vary widely and are increasing in a number of populations, e.g., in Switzerland and the US. The highest annual rates have been reported for Tasmania (167/100,000 in men and 89/100,000 in women) and the lowest for Asia and Africa (overall 1/100,000 in men and 5/100,000 in women). NMSC is the most common cancer in Caucasians. NMSC is about ten times as common in White as in non-White populations. The lethality is very low (Higginson et al. 1992).
Susceptibility to skin cancer is inversely related to the degree of melanin pigmentation, which is thought to protect by buffering against the carcinogenic action of solar ultraviolet (UV) radiation. Non-melanoma risk in white-skinned populations increases with the proximity to the equator.
In 1992, the International Agency for Research on Cancer (IARC 1992b) evaluated the carcinogenicity of solar radiation and concluded that there is sufficient evidence in humans for the carcinogenicity of solar radiation and that solar radiation causes cutaneous malignant melanoma and NMSC.
Reduction of exposure to sunlight would probably reduce the incidence of NMSCs. In Whites, 90 to 95% of NMSCs are attributable to solar radiation (IARC 1990).
NMSCs may develop in areas of chronic inflammation, irritation and scars from burns. Traumas and chronic ulcers of the skin are important risk factors for squamous cell skin cancers, particularly in Africa.
Radiation therapy, chemotherapy with nitrogen mustard, immunosuppressive therapy, psoralen treatment combined with UV-A radiation and coal tar preparations applied on skin lesions have been associated with an increased risk of NMSC. Environmental exposure to arsenic trivalent and arsenical compounds have been confirmed to be associated with skin cancer excess in humans (IARC 1987). Arsenicism can give rise to palmar or plantar arsenical keratoses, epidermoid carcinoma and superficial basal cell carcinoma.
Hereditary conditions such as lack of enzymes required to repair the DNA damaged by UV radiation may increase the risk of NMSC. Xeroderma pigmentosum represents such a hereditary condition.
A historical example of an occupational skin cancer is scrotal cancer that Sir Percival Pott described in chimney sweeps in 1775. The cause of these cancers was soot. In the early 1900s, scrotal cancers were observed in mulespinners in cotton textile factories where they were exposed to shale oil, which was used as a lubricant for cotton spindles. The scrotal cancers in both chimney sweeps and mulespinners were later associated with polycyclic aromatic hydrocarbons (PAHs), many of which are animal carcinogens, particularly some 3-, 4- and 5-ring PAHs such as benz(a)pyrene and dibenz(a,h)anthracene (IARC 1983, 1984a, 1984b, 1985a). In addition to mixtures that readily contain carcinogenic PAHs, carcinogenic compounds may be formed by cracking when organic compounds are heated.
Further occupations with which PAH-related excesses of NMSC have been associated include: aluminium reduction workers, coal gasification workers, coke oven workers, glass blowers, locomotive engineers, road pavers and highway maintenance workers, shale oil workers, tool fitters and tool setters (see table 1). Coal tars, coal-based pitches, other coal-derived products, anthracene oil, creosote oil, cutting oils and lubricating oils are some of the materials and mixtures that contain carcinogenic PAHs.
Table 1. Occupations at risk
|
Carcinogenic |
Industry or hazard |
Process or group at risk |
|
Pitch, tar or |
Aluminium reduction |
Pot room worker |
|
Soot |
Chimney sweeps |
|
|
Lubricating and |
Glass blowing |
|
|
Arsenic |
Oil refinery |
Still cleaners |
|
Ionizing radiation |
Radiologists |
|
|
Ultraviolet radiation |
Outdoor workers |
Farmers, fishermen, vineyard and |
Additional job titles that have been associated with increased NMSC risk include jute processors, outdoor workers, pharmacy technicians, sawmill workers, shale oil workers, sheep-dip workers, fishermen, tool setters, vineyard workers and watermen. The excess for watermen (who are primarily involved in traditional fishing tasks) was noticed in Maryland, USA and was confined to squamous cell cancers. Solar radiation probably explains fishermen’s, outdoor workers’, vineyard workers’ and watermen’s excess risks. Fishermen also may be exposed to oils and tar and inorganic arsenic from the consumed fish, which may contribute to the observed excess, which was threefold in a Swedish study, as compared with the county-specific rates (Hagmar et al. 1992). The excess in sheep dip workers may be explained by arsenical compounds, which induce skin cancers through ingestion rather than through skin contact. While farmers have slightly increased risk of melanoma, they do not appear to have increased risk of NMSC, based on epidemiological observations in Denmark, Sweden and the USA (Blair et al. 1992).
Ionizing radiation has caused skin cancer in early radiologists and workers who handled radium. In both situations, the exposures were long-lasting and massive. Occupational accidents involving skin lesions or long-term cutaneous irritation may increase the risk on NMSC.
Prevention (of Non-Melanocytic OccupationalSkin Cancer)
The use of appropriate clothing and a sunscreen having a protective UV-B factor of 15 or greater will help protect outdoor workers exposed to ultraviolet radiation. Further, the replacement of carcinogenic materials (such as feed stocks) by non-carcinogenic alternatives is another obvious protective measure which may, however, not always be possible. The degree of exposure to carcinogenic materials can be reduced by the use of protective shields on equipment, protective clothing and hygienic measures.
Of overriding importance is the education of the workforce about the nature of the hazard and the reasons for and value of the protective measures.
Finally, skin cancers usually take many years to develop and many of them pass through several premalignant stages before achieving their full malignant potential such as arsenic keratoses and actinic keratoses. These early stages are readily detectable by visual inspection. For this reason, skin cancers offer the real possibility that regular screening could reduce mortality among those known to have been exposed to any skin carcinogen.
Malignant Melanoma
Malignant melanoma is rarer than non-melanocytic skin cancer. Apart from exposure to solar radiation, no other environmental factors show a consistent association with malignant melanoma of the skin. Associations with occupation, diet and hormonal factors are not firmly established (Koh et al. 1993).
Malignant melanoma is an aggressive skin cancer (ICD-9 172.0 to 173.9; ICD-10: C43). It arises from pigment-producing cells of the skin, usually in an existing naevus. The tumour is usually a few millimetres to several centimetres thick, brown or black in colour, that has grown in size, changed colour and may bleed or ulcerate (Balch et al. 1993).
Indicators of poor prognosis of malignant melanoma of the skin include nodular subtype, tumour thickness, multiple primary tumours, metastases, ulceration, bleeding, long tumour duration, body site and, for some tumour sites, male sex. A history of malignant melanoma of the skin increases the risk for a secondary melanoma. Five-year post-diagnosis survival rates in high incidence areas are 80 to 85%, but in low incidence areas the survival is poorer (Ellwood and Koh 1994; Stidham et al. 1994).
There are four histologic types of malignant melanoma of the skin. Superficial spreading melanomas (SSM) represent 60 to 70% of all melanomas in Whites and less in non-Whites. SSMs tend to progress slowly and are more common in women than in men. Nodular melanomas (NM) account for 15 to 30% of malignant melanomas of the skin. They are invasive, grow rapidly and are more frequent in men. Four to 10% of malignant melanomas of the skin are lentigo malignant melanomas (LMM) or Hutchinson’s melanotic freckles. LMMs grow slowly, occur frequently in the face of old persons and rarely metastasize. Acral lentiginous melanomas (ALM) represent 35 to 60% of all malignant melanomas of the skin in non-Whites and 2 to 8% in Whites. They occur frequently on the sole of the foot (Bijan 1993).
For the treatment of malignant melanomas of the skin, surgery, radiation therapy, chemotherapy and biologic therapy (interferon alpha or interleukin-2) may be applied singly or in combination.
During the 1980s, the reported age-standardized annual incidence rates of malignant melanoma of the skin varied per 100,000 from 0.1 in males in Khon Kaen, Thailand to around 30.9 in males and 28.5 in females in Queensland, Australia (IARC 1992b). Malignant melanomas of the skin represent less than 1% of all cancers in most populations. An annual increase of about 5% in melanoma incidence has been observed in most white populations from the early 1960s to about 1972. Melanoma mortality has increased in the last decades in most populations, but less rapidly than incidence, probably due to early diagnoses and awareness of the disease (IARC 1985b, 1992b). More recent data show different rates of change, some of them suggesting even downward trends.
Malignant melanomas of the skin are among the ten most frequent cancers in incidence statistics in Australia, Europe and North America, representing a lifetime risk of 1 to 5%. White-skinned populations are more susceptible than non-White populations. Melanoma risk in white-skinned populations increases with proximity to the equator.
The gender distribution of melanomas of the skin varies widely between populations (IARC 1992a). Women have lower incidence rates than men in most populations. There are gender differences in patterns of body distribution of the lesions: trunk and face dominate in men, extremities in women.
Malignant melanomas of the skin are more common in higher than in lower socio-economic groups (IARC 1992b).
Familial melanomas are uncommon, but have been well documented. with between 4% and 10% of patients describing a history of melanoma among their first degree relatives.
Solar UV-B irradiation is probably the major cause for the widespread increase in the incidence of melanomas of the skin (IARC 1993). It is not clear whether depletion of the stratospheric ozone layer and the consequent increase in UV irradiance has caused the increase in the incidence of malignant melanoma (IARC 1993, Kricker et al. 1993). The effect of UV irradiation depends on some characteristics, such as I or II phenotype and blue eyes. A role for UV radiation emanating from fluorescent lamps is suspected, but not conclusively established (Beral et al. 1982).
It has been estimated that reduction in recreational sun exposure and use of sun-screens could reduce the incidence of malignant melanomas in high risk populations by 40% (IARC 1990). Among outdoor workers, the application of sunscreens having a protective UV-B factor rating of at least 15 and UV-A sunscreen and the use of appropriate clothing are practical protective measures. Although a risk from outdoor occupations is plausible, given the increased exposure to solar radiation, results of studies on regular outdoor occupational exposure are inconsistent. This is probably explained by the epidemiological findings suggesting that it is not regular exposures but rather intermittent high doses of solar radiation that are associated with excess melanoma risk (IARC 1992b).
Therapeutic immunosuppression may result in increased risk of malignant melanoma of the skin. An increased risk with the use of oral contraceptives has been reported, but it seems unlikely to increase the risk of malignant melanoma of the skin (Hannaford et al. 1991). Melanomas can be produced by oestrogen in hamsters. There is no evidence of such an effect in humans.
In White adults, the majority of primary intraocular malignant tumours are melanomas, usually arising from uveal melanocytes. The estimated rates for these cancers do not show the geographic variations and increasing time trends observed for melanomas of the skin. The incidence and mortality of ocular melanomas are very low in Black and Asiatic populations (IARC 1990, Sahel et al. 1993) The causes of ocular melanoma are unknown (Higginson et al. 1992).
In epidemiological studies, excess risk for malignant melanoma has been observed in administrators and managers, airline pilots, chemical processing workers, clerks, electrical power workers, miners, physical scientists, policemen and guards, refinery workers and gasoline exposed workers, salesmen and warehouse clerks. Excess melanoma risks have been reported in industries such as cellulose fibre production, chemical products, clothing industry, electrical and electronics products, metal industry, non-metallic mineral products, petrochemical industry, printing industry and telecommunications. Many of these findings are, however, solitary and have not been replicated in other studies. A series of meta-analyses of cancer risks in farmers (Blair et al. 1992; Nelemans et al. 1993) indicated a slight, but significant excess (aggregated risk ratio of 1.15) of malignant melanoma of the skin in 11 epidemi-ological studies.
In a multi-site case-control study of occupational cancer in Montreal, Canada (Siemiatycki et al. 1991), the following occupational exposures were associated with a significant excess of malignant melanoma of the skin: chlorine, propane engine emissions, plastics pyrolysis products, fabric dust, wool fibres, acrylic fibres, synthetic adhesives, “other” paints, varnishes, chlorinated alkenes, trichloroethylene and bleaches. It was estimated that the population attributable risk due to occupational exposures based on the significant associations in the data of the same study was 11.1%.
Occupational Contact Dermatitis
The terms dermatitis and eczema are interchangeable and refer to a particular type of inflammatory reaction of the skin which may be triggered by internal or external factors. Occupational contact dermatitis is an exogenous eczema caused by the interaction of the skin with chemical, biological or physical agents found in the work environment.
Contact dermatitis accounts for 90% of all occupational dermatoses and in 80% of the cases, it will impair a worker’s most important tool, the hands (Adams 1988). Direct contact with the offending agent is the usual mode of production of the dermatitis, but other mechanisms may be involved. Particulate matter such as dust or smoke, or vapours from volatile substances, may give rise to airborne contact dermatitis. Some substances will be transferred from the fingers to distant sites on the body to produce ectopic contact dermatitis. Finally, a photocontact dermatitis will be induced when a contactant has become activated by exposure to ultraviolet light.
Contact dermatitis is divided into two broad categories based on different mechanisms of production. Table 1 lists the salient features of irritant contact dermatitis and of allergic contact dermatitis.
Table 1. Types of contact dematitis
|
Features |
Irritant contact dermatitis |
Allergic contact dermatitis |
|
Mechanism of production |
Direct cytotoxic effect |
Delayed–type cellular immunity |
|
Potential victims |
Everyone |
A minority of individuals |
|
Onset |
Progressive, after repeated or prolonged exposure |
Rapid, within 12–48 hours in sensitized individuals |
|
Signs |
Subacute to chronic eczema with erythema, desquamation and fissures |
Acute to subacute eczema with erythema, oedema, bullae and vesicles |
|
Symptoms |
Pain and burning sensation |
Pruritus |
|
Concentration of contactant |
High |
Low |
|
Investigation |
History and examination |
History and examination |
Irritant Contact Dermatitis
Irritant contact dermatitis is caused by a direct cytotoxic action of the offending agent. Participation of the immune system is secondary to cutaneous damage and results in visible skin inflammation. It represents the most common type of contact dermatitis and accounts for 80% of all cases.
Irritants are mostly chemicals, which are classified as immediate or cumulative irritants. Corrosive substances, such as strong acids and alkalis are examples of the former in that they produce skin damage within minutes or hours of exposure. They are usually well identified, so that contact with them is most often accidental. By contrast, cumulative irritants are more insidious and often are not recognized by the worker as deleterious because damage occurs after days, weeks or months of repeated exposure. As shown in table 2 (overleaf) such irritants include solvents, petroleum distillates, dilute acids and alkalis, soaps and detergents, resins and plastics, disinfectants and even water (Gellin 1972).
Table 2. Common irritants
Acids and alkalis
Soaps and detergents
Solvents
Aliphatic: Petroleum distillates (kerosene, gasoline, naphta)
Aromatic: Benzene, toluene, xylene
Halogenated: Trichloroethylene, chloroform, methylene chloride
Miscellaneous: Turpentine, ketones, esters, alcohols, glycols, water
Plastics
Epoxy, phenolic, acrylic monomers
Amine catalysts
Styrene, benzoyl peroxide
Metals
Arsenic
Chrome
Irritant contact dermatitis, which appears after years of trouble-free handling of a substance, may be due to loss of tolerance, when the epidermal barrier ultimately fails after repeated subclinical insults. More rarely, thickening of the epidermis and other adaptive mechanisms can induce a greater tolerance to some irritants, a phenomenon called hardening.
In summary, irritant contact dermatitis will occur in a majority of individuals if they are exposed to adequate concentrations of the offending agent for a sufficient length of time.
Allergic Contact Dermatitis
A cell-mediated, delayed allergic reaction, similar to that seen in graft rejection, is responsible for 20% of all cases of contact dermatitis. This type of reaction, which occurs in a minority of subjects, requires active participation of the immune system and very low concentrations of the causative agent. Many allergens are also irritants, but the threshold for irritancy is usually much higher than that required for sensitization. The sequence of events which culminate in visible lesions is divided in two phases.
The sensitization (induction or afferent) phase
Allergens are heterogeneous, organic or non-organic chemicals, capable of penetrating the epidermal barrier because they are lipophilic (attracted to the fat in the skin) and of small molecular weight, usually less than 500 daltons (table 3). Allergens are incomplete antigens, or haptens; that is, they must bind to epidermal proteins to become complete antigens.
Langerhans cells are antigen-presenting dendritic cells which account for less than 5% of all epidermal cells. They trap cutaneous antigens, internalize and process them before re-expressing them on their outer surface, bound to proteins of the major histocompatibility complex. Within hours of contact, Langerhans cells leave the epidermis and migrate via the lymphatics towards draining lymph nodes. Lymphokines such as interleukin-1 (IL-1) and tumour necrosis factor alpha (TNF-α) secreted by keratinocytes are instrumental in the maturation and migration of Langerhans cells.
Table 3. Common skin allergens
Metals
Nickel
Chrome
Cobalt
Mercury
Rubber additives
Mercaptobenzothiazole
Thiurams
Carbamates
Thioureas
Dyes
Paraphenylene diamine
Photographic colour developers
Disperse textile dyes
Plants
Urushiol (Toxicodendron)
Sesquiterpene lactones (Compositae)
Primin (Primula obconica)
Tulipalin A (Tulipa, Alstroemeria)
Plastics
Epoxy monomer
Acrylic monomer
Phenolic resins
Amine catalysts
Biocides
Formaldehyde
Kathon CG
Thimerosal
In the paracortical area of regional lymph nodes, Langerhans cells make contact with naive CD4+ helper T cells and present them with their antigenic load. Interaction between Langerhans cells and helper T cells involve recognition of the antigen by T-cell receptors, as well as the interlocking of various adhesion molecules and other surface glycoproteins. Successful antigen recognition results in a clonal expansion of memory T cells, which spill into the bloodstream and the entire skin. This phase requires 5 to 21 days, during which no lesion occurs.
The elicitation (efferent) phase
Upon re-exposure to the allergen, sensitized T cells become activated and secrete potent lymphokines such as IL-1, IL-2 and interferon gamma (IFN-γ). These in turn induce blast transformation of T cells, generation of cytotoxic as well as suppressor T cells, recruitment and activation of macrophages and other effector cells and production of other mediators of inflammation such as TNF-α and adhesion molecules. Within 8 to 48 hours, this cascade of events results in vasodilatation and reddening (erythema), dermal and epidermal swelling (oedema), blister formation (vesiculation) and oozing. If left untreated, this reaction may last between two and six weeks.
Dampening of the immune response occurs with shedding or degradation of the antigen, destruction of Langerhans cells, increased production of CD8+ suppressor T cells and production by keratinocytes of IL-10 which inhibits the proliferation of helper/cytotoxic T cells.
Clinical Presentation
Morphology. Contact dermatitis may be acute, subacute or chronic. In the acute phase, lesions appear rapidly and present initially as erythematous, oedematous and pruritic urticarial plaques. The oedema may be considerable, especially where the skin is loose, such as the eyelids or the genital area. Within hours, these plaques become clustered with small vesicles which may enlarge or coalesce to form bullae. When they rupture, they ooze an amber- coloured, sticky fluid.
Oedema and blistering are less prominent in subacute dermatitis; which is characterized by erythema, vesiculation, peeling of skin (desquamation), moderate oozing and formation of yellowish crusts.
In the chronic stage, vesiculation and oozing are replaced by increased desquamation, thickening of the epidermis, which becomes greyish and furrowed (lichenification) and painful, deep fissures over areas of movement or trauma. Long-lasting lymphoedema may result after years of persistent dermatitis.
Distribution. The peculiar pattern and distribution of a dermatitis will often allow the clinician to suspect its exogenous origin and sometimes identify its causative agent. For example, linear or serpiginous streaks of erythema and vesicles on uncovered skin are virtually diagnostic of a plant contact dermatitis, while an allergic reaction due to rubber gloves will be worse on the back of the hands and around the wrists.
Repeated contact with water and cleansers is responsible for the classic “housewives’ dermatitis”, characterized by erythema, desquamation and fissures of the tips and backs of the fingers and involvement of the skin between the fingers (interdigital webs). By contrast, dermatitis caused by friction from tools, or by contact with solid objects tends to be localized on the palm and underside (volar) area of the fingers.
Irritant contact dermatitis due to fibreglass particles will involve the face, hands and forearms and will be accentuated in flexures, around the neck and waist, where movement and friction from clothes will force the spicules into the skin. Involvement of the face, upper eyelids, ears and submental area suggests an airborne dermatitis. A photocontact dermatitis will spare sun-protected areas such as the upper eyelids, the submental and retroauricular areas.
Extension to distant sites. Irritant dermatitis remains localized to the area of contact. Allergic contact dermatitis, especially if acute and severe, is notorious for its tendency to disseminate away from the site of initial exposure. Two mechanisms may explain this phenomenon. The first, autoeczematization, also known as id-reaction or the excited skin syndrome, refers to a state of hypersensitivity of the entire skin in response to a persistent or severe localized dermatitis. Systemic contact dermatitis occurs when a patient topically sensitized to an allergen is re-exposed to the same agent by oral or parenteral route. In both cases, a widespread dermatitis will ensue, which may easily be mistaken for an eczema of endogenous origin.
Predisposing factors
The occurrence of an occupational dermatitis is influenced by the nature of the contactant, its concentration and the duration of contact. The fact that under similar conditions of exposure only a minority of workers will develop a dermatitis is proof of the importance of other personal and environmental predisposing factors (table 4).
Table 4. Predisposing factors for occupational dermatitis
|
Age |
Younger workers are often inexperienced or careless and are more likely to develop occupational dermatitis than older workers |
|
Skin type |
Orientals and Blacks are generally more resistant to irritation than Whites |
|
Pre-existing disease |
Atopy predisposes to irritant contact dermatitis Psoriasis or lichen planus may worsen because of the Koebner phenomenon |
|
Temperature and humidity |
High humidity reduces the effectiveness of the epidermal barrier Low humidity and cold cause chapping and desiccation of the epidermis |
|
Working conditions |
A dirty worksite is more often contaminated with toxic or allergenic chemicals Obsolete equipment and lack of protective measures increase the risk of occupational dermatitis Repetitive movements and friction may cause irritation and calluses |
Age. Younger workers are more likely to develop occupational dermatitis. It may be that they are often less experienced than their older colleagues, or may have a more careless attitude about safety measures. Older workers may have become hardened to mild irritants, or they have learned how to avoid contact with hazardous substances, or older workers may be a self-selected group that did not experience problems while others who did may have left the job.
Skin type. Most Black or Oriental skin appears to be more resistant to the effects of contact irritants than the skin of most Caucasians.
Pre-existing disease. Allergy-prone workers (having a background of atopy manifested by eczema, asthma or allergic rhinitis) are more likely to develop irritant contact dermatitis. Psoriasis and lichen planus may be aggravated by friction or repetitive trauma, a phenomenon called koebnerization. When such lesions are limited to the palms, they may be difficult to distinguish from chronic irritant contact dermatitis.
Temperature and humidity. Under conditions of extreme heat, workers often neglect to wear gloves or other appropriate protective gear. High humidity reduces the effectiveness of the epidermal barrier, while dry and cold conditions promote chapping and fissures.
Working conditions. The incidence of contact dermatitis is higher in worksites which are dirty, contaminated with various chemicals, have obsolete equipment, or lack protective measures and hygiene facilities. Some workers are at higher risk because their tasks are manual and they are exposed to strong irritants or allergens (e.g., hairdressers, printers, dental technicians).
Diagnosis
A diagnosis of occupational contact dermatitis can usually be made after a careful history and a thorough physical examination.
History. A questionnaire that includes the name and address of the employer, the worker’s job title and a description of functions should be completed The worker should provide a list of all the chemicals handled and supply information about them, such as is found on the Material Safety Data Sheets. The date of onset and location of the dermatitis should be noted. It is important to document the effects of vacation, sick leave, sun exposure and treatment on the course of the disease. The examining physician should obtain information about the worker’s hobbies, personal habits, history of pre-existing skin disease, general medical background and current medication, as well.
Physical examination. The involved areas must be carefully examined. Note should be taken of the severity and stage of the dermatitis, of its precise distribution and of its degree of interference with function. A complete skin examination must be performed, looking for tell-tale stigmata of psoriasis, atopic dermatitis, lichen planus, tinea, etc., which may signify that the dermatitis is not of occupational origin.
Complementary investigation
The information obtained from history and physical examination is usually sufficient to suspect the occupational nature of a dermatitis. However, additional tests are required in most cases to confirm the diagnosis and to identify the offending agent.
Patch testing. Patch testing is the technique of choice for the identification of cutaneous allergens and it should be routinely performed in all cases of occupational dermatitis (Rietschel et al. 1995). More than 300 substances are now commercially available. The standard series, which regroup the most common allergens, can be supplemented with additional series aimed at specific categories of workers such as hairdressers, dental technicians, gardeners, printers, etc. Table 6 lists the various irritants and sensitizers encountered in some of these occupations.
Table 5. Examples of skin irritants and sensitizers with occupations where contact can occur
|
Occupation |
Irritants |
Sensitizers |
|
Construction |
Turpentine, thinner, |
Chromates, epoxy and phenolic |
|
Dental |
Detergents, disinfectants |
Rubber, epoxy and acrylic monomer, amine catalysts, local anaesthetics, mercury, gold, nickel, eugenol, formaldehyde, glutaraldehyde |
|
Farmers, florists, |
Fertilizers, disinfectants, |
Plants, woods, fungicides, insecticides |
|
Food handlers, |
Soaps and detergents, |
Vegetables, spices, garlic, rubber, benzoyl peroxide |
|
Hairdressers, |
Shampoos, bleach, peroxide, |
Paraphenylenediamine in hair dye, glycerylmonothioglycolate in permanents, ammonium persulphate in bleach, surfactants in shampoos, nickel, perfume, essential oils, preservatives in cosmetics |
|
Medical |
Disinfectants, alcohol, soaps |
Rubber, colophony, formaldehyde, glutaraldehyde, disinfectants, antibiotics, local anaesthetics, pheno-thiazines, benzodiazepines |
|
Metal workers, |
Soaps and detergents, cutting |
Nickel, cobalt, chrome, biocides in cutting oils, hydrazine and colophony in welding flux, epoxy resins and amine catalysts, rubber |
|
Printers and |
Solvents, acetic acid, ink, |
Nickel, cobalt, chrome, rubber,colophony, formaldehyde, paraphenylene diamine and azo dyes, hydroquinone, epoxy and acrylic monomer, amine catalysts, B&W and colour developers |
|
Textile workers |
Solvents, bleaches, natural |
Formaldehyde resins, azo- and anthraquinone dyes, rubber, biocides |
The allergens are mixed in a suitable vehicle, usually petroleum jelly, at a concentration which was found by trial and error over the years to be non-irritant but high enough to reveal allergic sensitization. More recently, prepackaged, ready-to-apply allergens embedded in adhesive strips have been introduced, but so far only the 24 allergens of the standard series are available. Other substances must be bought in individual syringes.
At the time of testing, the patient must be in a quiescent phase of dermatitis and not be taking systemic corticosteroids. A small amount of each allergen is applied to shallow aluminium or plastic chambers mounted on porous, hypoallergenic adhesive tape. These rows of chambers are affixed to an area free of dermatitis on the patient’s back and left in place for 24 or more commonly 48 hours. A first reading is done when the strips are removed, followed by a second and sometimes a third reading after four and seven days respectively. Reactions are graded as follows:
Nul no reaction
? doubtful reaction, mild macular erythema
+ weak reaction, mild papular erythema
++ strong reaction, erythema, oedema, vesicles
+++ extreme reaction, bullous or ulcerative;
IR irritant reaction, glazed erythema or erosion resemblinga burn.
When a photocontact dermatitis (one that requires exposure to ultraviolet light, UV-A) is suspected, a variant of patch testing, called photopatch testing, is performed. Allergens are applied in duplicate to the back. After 24 or 48 hours, one set of allergens is exposed to 5 joules of UV-A and the patches are put back in place for another 24 to 48 hours. Equal reactions on both sides signify allergic contact dermatitis, positive reactions on the UV-exposed side only is diagnostic of photocontact allergy, while reactions on both sides but stronger on the UV-exposed side mean contact and photocontact dermatitis combined.
The technique of patch testing is easy to perform. The tricky part is the interpretation of the results, which is best left to the experienced dermatologist. As a general rule, irritant reactions tend to be mild, they burn more than they itch, they are usually present when the patches are removed and they fade rapidly. By contrast, allergic reactions are pruritic, they reach a peak at four to seven days and may persist for weeks. Once a positive reaction has been identified, its relevance must be assessed: is it pertinent to the current dermatitis, or does it reveal past sensitization? Is the patient exposed to that particular substance, or is he allergic to a different but structurally-related compound with which it cross-reacts?
The number of potential allergens far exceeds the 300 or so commercially available substances for patch testing. It is therefore often necessary to test patients with the actual substances that they work with. While most plants can be tested “as is,” chemicals must be precisely identified and buffered if their acidity level (pH) falls outside the range of 4 to 8. They must be diluted to the appropriate concentration and mixed in a suitable vehicle according to current scientific practice (de Groot 1994). Testing a group of 10 to 20 control subjects will ensure that irritant concentrations are detected and rejected.
Patch testing is usually a safe procedure. Strong positive reactions may occasionally cause exacerbation of the dermatitis under investigation. On rare occasions, active sensitization may occur, especially when patients are tested with their own products. Severe reactions may leave hypo- or hyperpigmented marks, scars or keloids.
Skin biopsy. The histological hallmark of all types of eczema is epidermal intercellular oedema (spongiosis) which stretches the bridges between keratinocytes to the point of rupture, causing intraepidermal vesiculation. Spongiosis is present even in the most chronic dermatitis, when no macroscopic vesicle can be seen. An inflammatory infiltrate of lymphohistiocytic cells is present in the upper dermis and migrates into the epidermis (exocytosis). Because a skin biopsy cannot distinguish between the various types of dermatitis, this procedure is rarely performed, except in rare cases where the clinical diagnosis is unclear and in order to rule out other conditions such as psoriasis or lichen planus.
Other procedures. It may at times be necessary to perform bacterial, viral or fungal cultures, as well as potassium hydroxide microscopic preparations in search of fungi or ectoparasites. Where the equipment is available, irritant contact dermatitis can be assessed and quantified by various physical methods, such as colorimetry, evaporimetry, Laser-Doppler velocimetry, ultrason- ography and the measurement of electrical impedance, conductance and capacitance (Adams 1990).
Workplace. On occasion, the cause of an occupational dermatitis is uncovered only after a careful observation of a particular worksite. Such a visit allows the physician to see how a task is performed and how it might be modified to eliminate the risk of occupational dermatitis. Such visits should always be arranged with the health officer or supervisor of the plant. The information that it generates will be useful to both the worker and the employer. In many localities, workers have the right to request such visits and many work sites have active health and safety committees which do provide valuable information.
Treatment
Local treatment of an acute, vesicular dermatitis will consist of thin, wet dressings soaked in lukewarm saline, Burow’s solution or tap water, left in place for 15 to 30 minutes, three to four times a day. These compresses are followed by the application of a strong topical corticosteroid. As the dermatitis improves and dries up, the wet dressings are spaced and stopped and the strength of the corticosteroid is decreased according to the part of the body being treated.
If the dermatitis is severe or widespread, it is best treated with a course of oral prednisone, 0.5 to 1.0 mg/kg/day for two to three weeks. Systemic first-generation antihistamines are given as needed to provide sedation and relief from pruritus.
Subacute dermatitis usually responds to mid-strength corticosteroid creams applied two to three times a day, often combined with protective measures such as the use of cotton liners under vinyl or rubber gloves when contact with irritants or allergens cannot be avoided.
Chronic dermatitis will require the use of corticosteroid ointments, coupled with the frequent application of emollients, the greasier the better. Persistent dermatitis may need to be treated with psoralen and ultraviolet-A (PUVA) phototherapy, or with systemic immunosuppressors such as azathioprine (Guin 1995).
In all cases, strict avoidance of causative substances is a must. It is easier for the worker to stay away from offending agents if he or she is given written information which specifies their names, synonyms, sources of exposure and cross-reaction patterns. This printout should be clear, concise and written in terms that the patient can easily understand.
Worker’s compensation
It is often necessary to withdraw a patient from work. The physician should specify as precisely as possible the estimated length of the disability period, keeping in mind that full restoration of the epidermal barrier takes four to five weeks after the dermatitis is clinically cured. The legal forms that will allow the disabled worker to receive adequate compensation should be diligently filled out. Finally, the extent must be determined of permanent impairment or the presence of functional limitations, which may render a patient unfit to return to his former work and make him a candidate for rehabilitation.
Prevention of Occupational Dermatoses
The goal of occupational health programmes is to allow workers to maintain their job and their health over several years. The development of effective programmes requires the identification of sectoral, population-based, and workplace-specific risk factors. This information can then be used to develop prevention policies both for groups and individuals.
The Québec Occupational Health and Safety Commission (Commission de la santé et de la sécurité au travail du Québec) has characterized work activities in 30 industrial, commercial, and service sectors (Commission de la santé et de la sécurité au travail 1993). Its surveys reveal that occupational dermatoses are most prevalent in the food and beverage industries, medical and social services, miscellaneous commercial and personal services and construction (including public works). Affected workers are typically engaged in service, manufacturing, assembly, repair, materials handling, food-processing, or health-care activities.
Occupational dermatoses are particularly prevalent in two age groups: young and inexperienced workers who may be unaware of the sometimes insidious risks associated with their work, and those workers approaching retirement age who may not have noticed the progressive drying of their skin over the years, which increases over several consecutive workdays. Because of such dehydration, repeated exposure to previously well-tolerated irritant or astringent substances may cause irritative dermatitis in these workers.
As table 1 indicates, even though most cases of occupational dermatoses do not involve compensation exceeding two weeks, a significant number of cases may persist for over two months (Durocher and Paquette 1985). This table clearly illustrates the importance of preventing chronic dermatoses requiring prolonged work absences.
Table 1. Occupational dermatoses in Quebec in 1989: Distribution by length of compensation
|
Length of compensation (days) |
0 |
1–14 |
15–56 |
57–182 |
>183 |
|
Number of cases (total: 735) |
10 |
370 |
195 |
80 |
80 |
Source: Commission de la santé et de la sécurité au travail, 1993.
Risk Factors
Many substances used in industry are capable of causing dermatoses, the risk of which depends on the concentration of the substance and the frequency and duration of skin contact. The general classification scheme presented in table 2 (overleaf) based on the classification of risk factors as mechanical, physical, chemical or biological, is a useful tool for the identification of risk factors during site visits. During workplace evaluation, the presence of risk factors may be either directly observed or suspected on the basis of observed skin lesions. Particular attention is paid to this in the classification scheme presented in table 2. In some cases effects specific to a given risk factor may be present, while in others, the skin disorders may be associated with several factors in a given category. Disorders of this last type are known as group effects. The specific cutaneous effects of physical factors are listed in table 2 and described in other sections of this chapter.
Table 2. Risk factors and their effects on the skin
Mechanical factors
Trauma
Friction
Pressure
Dusts
Physical factors
Radiation
Humidity
Heat
Cold
Chemical factors
Acids, bases
Detergents, solvents
Metals, resins
Cutting oils
Dyes, tar
Rubber, etc.
Biological factors
Bacteria
Viruses
Dermatophytes
Parasites
Plants
Insects
Risk co-factors
Eczema (atopic, dyshidrotic, seborrhoeic, nummular)
Psoriasis
Xeroderma
Acne
Group effects
Cuts, punctures, blisters
Abrasions, isomorphism
Lichenification
Calluses
Specific effects
Photodermatitis, radiodermatitis, cancer
Maceration, irritation
Heat rash, burns, erythema
Frostbite, xeroderma, urticaria, panniculitis, Raynaud’s phenomenon
Group effects
Dehydration
Inflammation
Necrosis
Allergy
Photodermatitis
Dyschromia
Specific effects
Pyodermatitis
Multiple warts
Dermatomycosis
Parasitosis
Phytodermatitis
Urticaria
Mechanical factors include repeated friction, excessive and prolonged pressure, and the physical action of some industrial dusts, whose effects are a function of the shape and size of the dust particles and the extent of their friction with the skin. The injuries themselves may be mechanical (especially in workers exposed to repeated vibrations), chemical, or thermal, and include physical lesions (ulcers, blisters), secondary infection, and isomorphism (Koebner phenomenon). Chronic changes, such as scars, keloid, dyschromia, and Raynaud’s phenomenon, which is a peripheral neurovascular alteration caused by prolonged use of vibrating tools, may also develop.
Chemical factors are by far the most common cause of occupational dermatoses. To establish an exhaustive list of the many chemicals is not practical. They may cause allergic, irritant or photodermatotic reactions, and may leave dyschromic sequelae. The effects of chemical irritation vary from simple drying to inflammation to complete cell necrosis. More information on this subject is provided in the article on contact dermatitis. Material Safety Data Sheets, which provide toxicological and other information are indispensable tools for developing effective preventive measures against chemicals. Several countries, in fact, require chemical manufacturers to provide every workplace using their products with information on the occupational health hazards posed by their products.
Bacterial, viral and fungal infections contracted in the workplace arise from contact with contaminated materials, animals, or people. Infections include pyodermatitis, folliculitis, panaris, dermatomycosis, anthrax, and brucellosis. Workers in the food-processing sector may develop multiple warts on their hands, but only if they have already suffered microtraumas and are exposed to excessive levels of humidity for prolonged periods (Durocher and Paquette 1985). Both animals and humans such as day-care and health-care workers, may act as vectors for parasitic contamination like mites, scabies and head lice. Phytodermatitis may be caused by plants (Rhus sp.) or flowers (alstromeria, chrysanthemums, tulips). Finally, some wood extracts may cause contact dermatitis.
Risk Co-factors
Some non-occupational cutaneous pathologies may exacerbate the effects of environmental factors on workers’ skin. For example, it has long been recognized that the risk of irritant contact dermatitis is greatly increased in individuals with a medical history of atopy, even in the absence of an atopic dermatitis. In a study of 47 cases of irritant contact dermatitis of the hands of food-processing workers, 64% had a history of atopy (Cronin 1987). Individuals with atopic dermatitis have been shown to develop more severe irritation when exposed to sodium lauryl sulphate, commonly found in soaps (Agner 1991). Predisposition to allergies (Type I) (atopic diathesis) does not however increase the risk of delayed allergic (Type IV) contact dermatitis, even to nickel (Schubert et al. 1987), the allergen most commonly screened for. On the other hand, atopy has recently been shown to favour the development of contact urticaria (Type I allergy) to rubber latex among health-care workers (Turjanmaa 1987; Durocher 1995) and to fish among caterers (Cronin 1987).
In psoriasis, the outmost layer of the skin (stratum corneum) is thickened but not calloused (parakeratotic) and less resistant to skin irritants and mechanical traction. Frequent skin injury may worsen pre-existing psoriasis, and new isomorphic psoriatic lesions may develop on scar tissue.
Repeated contact with detergents, solvents, or astringent dusts may lead to secondary irritant contact dermatitis in individuals suffering from xeroderma. Similarly, exposure to frying oils may exacerbate acne.
Prevention
A thorough understanding of relevant risk factors is a prerequisite to establishing prevention programmes, which may be either institutional or personal ones such as relying on personal protective equipment. The efficacy of prevention programmes depends on the close collaboration of workers and employers during their development. Table 3 provides some information on prevention.
Table 3. Collective measures (group approach) to prevention
Collective measures
- Substitution
- Environmental control:
Use of tools for handling materials
Ventilation
Closed systems
Automation
- Information and training
- Careful work habits
- Follow-up
Personal protection
- Skin hygiene
- Protective agents
- Gloves
Workplace Prevention
The primary goal of workplace preventive measures is the elimination of hazards at their source. When feasible, substitution of a toxic substance by a non-toxic one is the ideal solution. For example, the toxic effects of a solvent being incorrectly used to clean the skin can be eliminated by substituting a synthetic detergent that presents no systemic hazard and that is less irritating. Several non-allergenic cement powders which substitute ferrous sulphate for hexavalent chromium, a well-known allergen, are now available. In water-based cooling systems, chromate-based anti-corrosion agents can be replaced by zinc borate, a weaker allergen (Mathias 1990). Allergenic biocides in cutting oils can be replaced by other preservatives. The use of gloves made of synthetic rubber or PVC can eliminate the development of latex allergies among health-care workers. Replacement of aminoethanolamine by triethanolamine in welding fluxes used to weld aluminium cables has led to a reduction in allergies (Lachapelle et al. 1992).
Modification of production processes to avoid skin contact with hazardous substances may be an acceptable alternative when substitution is impossible or the risk is low. Simple modifications include using screens or flexible tubes to eliminate splashing during the transfer of liquids, or filters that retain residues and reduce the need for manual cleaning. More natural grasp points on tools and equipment that avoid exerting excessive pressure and friction on the hands and that prevent skin contact with irritants may also work. Local capture ventilation with capture inlets that limit nebulisation or reduce the concentration of airborne dusts are useful. Where processes have been completely automated in order to avoid environmental hazards, particular attention should be paid to training workers responsible for repairing and cleaning the equipment and specific preventive measures may be required to limit their exposure (Lachapelle et al. 1992).
All personnel must be aware of the hazards present in their workplace, and collective measures can only be effective when implemented in conjunction with a comprehensive information programme. Material Safety Data Sheets can be used to identify hazardous and potentially hazardous substances. Hazard warning signs can be used to rapidly identify these substances. A simple colour code allows visual coding of the risk level. For example, a red sticker could signal the presence of a hazard and the necessity of avoiding direct skin contact. This code would be appropriate for a corrosive substance that rapidly attacks the skin. Similarly, a yellow sticker could indicate the need for prudence, for example when dealing with a substance capable of damaging the skin following repeated or prolonged contact (Durocher 1984). Periodic display of posters and the occasional use of audio-visual aids reinforce the information delivered and stimulate interest in occupational dermatosis prevention programmes.
Complete information on the hazards associated with work activities should be provided to workers prior to starting work. In several countries, workers are given special occupational training by professional instructors.
Workplace training must be repeated each time a process or task is changed with resulting change in risk factors. Neither an alarmist nor paternalistic attitude favours good working relationships. Employers and workers are partners who both desire work to be executed safely, and the information delivered will only be credible if it is realistic.
Given the absence of safety standards for dermatotoxic substances (Mathias 1990), preventive measures must be supported by vigilant observation of the state of workers’ skin. Fortunately this is easily implemented, since the skin, particularly that on the hands and face, can be directly observed by everyone. The goal of this type of observation is the identification of early signs of cutaneous modifications indicating an overwhelming of the body’s natural equilibrium. Workers and health and safety specialists should therefore be on the lookout for the following early warning signs:
- progressive drying
- maceration
- localized thickening
- frequent trauma
- redness, particularly around hairs.
Prompt identification and treatment of cutaneous pathologies is essential, and their underlying causal factors must be identified, to prevent them from becoming chronic.
When workplace controls are unable to protect the skin from contact with hazardous substances, the duration of skin contact should be minimized. For this purpose, workers should have ready access to appropriate hygienic equipment. Contamination of cleaning agents can be avoided by using closed containers equipped with a pump that dispenses an adequate amount of the cleanser with a single press. Selecting cleansers requires compromising between cleaning power and the potential for irritation. For example, so-called high-performance cleansers often contain solvents or abrasives which increase irritation. The cleanser selected should take into account the specific characteristics of the workplace, since workers will often simply use a solvent if available cleansers are ineffective. Cleansers may take the form of soaps, synthetic detergents, waterless pastes or creams, abrasive preparations and antimicrobial agents (Durocher 1984).
In several occupations, the application of a protective cream before work facilitates skin cleaning, regardless of the cleaner used. In all cases, the skin must be thoroughly rinsed and dried after each washing. Failure to do so may increase irritation, for example by re-emulsification of the soap residues caused by the humidity inside impermeable gloves.
Industrial soaps are usually provided as liquids dispensed by hand pressure. They are composed of fatty acids of animal (lard) or vegetable (oil) origin, buffered with a base (e.g., sodium hydroxide). Buffering may be incomplete and may leave residual free radicals that are capable of irritating the skin. To avoid this, a near-neutral pH (4 to 10) is desirable. These liquid soaps are adequate for many tasks.
Synthetic detergents, available in both liquid and powder form, emulsify greases. Thus they usually remove the human skin’s sebum, which is a substance that protects the skin against drying. Skin emulsification is generally less marked with soaps than with synthetic detergents and is proportional to detergent concentration. Emollients such as glycerine, lanolin, and lecithin are often added to detergents to counteract this effect.
Pastes and creams, also known as “waterless soaps” are emulsions of oil-based substances in water. Their primary cleaning agent is a solvent, generally a petroleum derivative. They are called “waterless” because they are effective in the absence of tap water, and are typically used to remove stubborn soils or to wash hands when water is unavailable. Because of their harshness, they are not considered cleansers of choice. Recently, “waterless soaps” containing synthetic detergents that are less irritating to the skin than solvents have become available. The American Association of Soap and Detergent Manufacturers recommends washing with a mild soap after using solvent-based “waterless soaps.” Workers who use “waterless soaps” three or four times per day should apply a moisturizing lotion or cream at the end of the work day, in order to prevent drying.
Abrasive particles, which are often added to one of the cleaners described above to increase their cleaning power are irritants. They may be soluble (e.g., borax) or insoluble. Insoluble abrasives may be mineral (e.g., pumice), vegetal (e.g., nut shells) or synthethic (e.g., polystyrene).
Antimicrobial cleaners should only be used in workplaces where there is a real risk of infection, since several of them are potential allergens and workers should not be exposed needlessly.
Under the influence of certain substances or repeated washings, workers’ hands may tend to dry out. Long-term maintenance of good skin hygiene under these conditions requires daily moisturizing, the frequency of which will depend on the individual and the type of work. In many cases, moisturizing lotions or creams, also known as hand creams, are adequate. In cases of severe drying or when the hands are immersed for prolonged periods, hydrophilic vaselines are more appropriate. So-called protective or barrier creams are usually moisturizing creams; they may contain silicones or zinc or titanium oxides. Exposure-specific protective creams are rare, with the exception of those which protect against ultraviolet radiation. These have been greatly improved over the last few years and now provide effective protection against both UV-A and UV-B. A minimum protection factor of 15 (North American scale) is recommended. StokogarÔ cream appears to be effective against contact dermatitis caused by poison ivy. Protective or barrier creams should never be seen as equivalent to some form of invisible impermeable glove (Sasseville 1995). Furthermore, protective creams are only effective on healthy skin.
While few people like wearing protective equipment, there may be no choice when the measures described above are inadequate. Protective equipment includes: boots, aprons, visors, sleeves, overalls, shoes, and gloves. These are discussed elsewhere in the Encyclopaedia.
Many workers complain that protective gloves reduce their dexterity, but their use is nevertheless inevitable in some situations. Special efforts are required to minimize their inconvenience. Many types are available, both permeable (cotton, leather, metal mesh, KevlaÔasbestos) and impermeable (rubber latex, neoprene, nitrile, polyvinyl chloride, VitoÔ, polyvinyl alcohol, polyethylene) to water. The type selected should take into account the specific needs of each situation. Cotton offers minimal protection but good ventilation. Leather is effective against friction, pressure, traction, and some types of injury. Metal mesh protects against cuts. KevlaÔis fire-resistant. Asbestos is fire- and heat-resistant. The solvent resistance of water-impermeable gloves is highly variable and depends on their composition and thickness. To increase solvent resistance, some researchers have developed gloves incorporating multiple polymer layers.
Several characteristics have to be taken into account when selecting gloves. These include thickness, flexibility, length, roughness, wrist and finger adjustment, and chemical, mechanical, and thermal resistance. Several laboratories have developed techniques, based on the measurement of break-through times and permeability constants, with which to estimate the resistance of gloves to specific chemicals. Lists to help guide glove selection are also available (Lachapelle et al. 1992; Berardinelli 1988).
In some cases, the prolonged wear of protective gloves may cause allergic contact dermatitis due to glove components or to allergens that penetrate the gloves. Wearing protective gloves is also associated with an increased risk of skin irritation, due to prolonged exposure to high levels of humidity within the glove or penetration of irritants through perforations. To avoid deterioration of their condition, all workers suffering from hand dermatitis, regardless of its origin, should avoid wearing gloves that increase the heat and humidity around their lesions.
Establishing a comprehensive occupational dermatosis prevention programme depends on careful adaptation of standards and principles to the unique characteristics of each workplace. To ensure their effectiveness, prevention programmes should be revised periodically to take into account changes in the workplace, experience with the programme and technological advances.
Occupational Nail Dystrophy
The function of the epithelium of the epidermis is to form the surface or horny layer of the skin, of which the major component is the fibrous protein, keratin. In certain areas the epithelium is specially developed to produce a particular type of keratin structure. One of these is hair, and another is nail. The nail plate is formed partly by the epithelium of the matrix and partly by that of the nail bed. The nail grows in the same way as the hair and the horny layer and is affected by similar pathogenic mechanisms to those responsible for diseases of the hair and epidermis. Some elements such as arsenic and mercury accumulate in the nail as in the hair.
Figure 1 shows that the nail matrix is an invagination of the epithelium and it is covered by the nail fold at its base. A thin film of horny layer called the cuticle serves to seal the paronychial space by stretching from the nail fold to the nail plate.
Figure 1. The structure of the nail.
The most vulnerable parts of the nail are the nail fold and the area beneath the tip of the nail plate, although the nail plate itself may suffer direct physical or chemical traumata. Chemical substances or infective agents may penetrate under the nail plate at its free margin. Moisture and alkali may destroy the cuticle and allow the entry of bacteria and fungi which will cause inflammation of the paronychial tissue and produce secondary growth disturbance of the nail plate.
The most frequent causes of nail disease are chronic paronychia, ringworm, trauma, psoriasis, impaired circulation and eczema or other dermatitis. Paronychia is an inflammation of the nail fold. Acute paronychia is a painful suppurative condition requiring antibiotic and sometimes surgical treatment. Chronic paronychia follows loss of the cuticle which allows water, bacteria and Candida albicans to penetrate into the paronychial space. It is common among persons with intense exposure to water, alkaline substances and detergents, such as kitchen staff, cleaners, fruit and vegetable preparers and canners and housewives. Full recovery cannot be achieved until the integrity of the cuticle and eponychium sealing the paronychial space has been restored.
Exposure to cement, lime and organic solvents, and work such as that of a butcher or poulterer may also cause trauma of the cuticle and nail folds.
Any inflammation or disease of the nail matrix may result in dystrophy (distortion) of the nail plate, which is usually the symptom which has brought the condition to medical attention. Exposure to chilling cold, or the arterial spasm of Raynaud’s phenomenon, can also damage the matrix and produce nail dystrophy. Sometimes the damage is temporary and the nail dystrophy will disappear after removal of the cause and treatment of the inflammatory condition. (An example is shown in figure 2.)
Figure 2. Onychodystrophy secondary to contact dermatitis resulting from chronic irritation.
One cause of nail damage is the direct application of certain cosmetic preparations, such as base coats under nail polish, nail hardeners and synthetic nail dressings to the nail.
Some special occupations may cause nail damage. There has been a report of dystrophy due to handling the concentrated dipyridylium pesticide compounds paraquat and diquat. During the manufacture of selenium dioxide, a fine powder of this substance may get under the fringe of the nail plate and cause intense irritation and necrosis of the finger tip and damage to the nail plate. Care should be taken to warn workers of this hazard and advise them always to clean the subungual areas of their fingers each day.
Certain types of allergic contact dermatitis of the finger tips frequently result in secondary nail dystrophy. Six common sensitizers which will do this are:
- amethocaine and chemically related local anaesthetics used by dental surgeons
- formalin used by mortuary attendants, anatomy, museum and laboratory assistants
- garlic and onion used by cooks
- tulip bulbs and flowers handled by horticulturists and florists
- p-tert-butylphenol formaldehyde resin used by shoe manufacturers and repairers
- aminoethylethanolamine used in some aluminium fluxes.
The diagnosis can be confirmed by a positive patch test. The condition of the skin and nails will recover when contact ceases.
Protective measures
In many cases nails can be safeguarded by the use of suitable hand protection. However, where hand exposure exists, nails should receive adequate care, consisting essentially of preserving the cuticle and protecting the subungual area. The skin under the free margin of the nails should be cleaned daily in order to remove foreign debris or chemical irritants. Where barrier creams or lotions are employed, care should be taken to ensure that the cuticle and the area under the free margin are coated.
To preserve the intact cuticle it is necessary to avoid excessive manicure or trauma, maceration by prolonged exposure to water, and dissolution by repeated exposure to alkali, solvent and detergent solutions.
Stigmata
Occupational stigma or occupational marks are work-induced anatomical lesions which do not impair working capacity. Stigmata are generally caused by mechanical, chemical or thermal skin irritation over a long period and are often characteristic of a particular occupation. Any kind of pressure or friction on the skin may produce an irritating effect, and a single violent pressure may break the epidermis, leading to the formation of excoriations, seropurulent blisters and infection of the skin and underlying tissues. On the other hand, however, frequent repetition of moderate irritant action does not disrupt the skin but stimulates defensive reactions (thickening and keratinization of the epidermis). The process may take three forms:
- a diffuse thickening of the epidermis which merges into the normal skin, with preservation and occasional accentuation of skin ridges and unimpaired sensitivity
- a circumscribed callosity made up of smooth, elevated, yellowish, horny lamellae, with partial or complete loss of skin ridges and impairment of sensitivity. The lamellae are not circumscribed; they are thicker in the centre and thinner towards the periphery and blend into the normal skin
- a circumscribed callosity, mostly raised above the normal skin, 15 mm in diameter, yellowish-brown to black in colour, painless and occasionally associated with hypersecretion of the sweat glands.
Callosities are usually produced by mechanical agents, sometimes with the aid of a thermal irritant (as in the case of glass- blowers, bakers, firefighters, meat curers, etc.), when they are dark-brown to black in colour with painful fissures. If, however, the mechanical or thermal agent is combined with a chemical irritant, callosities undergo discoloration, softening and ulceration.
Callosities which represent a characteristic occupational reaction (particularly on the skin of the hand as shown in figure 1 and 2) are seen in many occupations. Their form and localization are determined by the site, force, manner and frequency of the pressure exerted, as well as by the tools or materials used. The size of callosities may also reveal a congenital tendency to skin keratinization (ichthyosis, hereditary keratosis palmaris). These factors may also often be decisive as concerns deviations in the localization and size of callosities in manual workers.
Figure 1. Occupational stigmata on the hands.
(a) Tanner’s ulcers; (b) Blacksmith; (c) Sawmill worker; (d) Stonemason; (e) Mason; (f) Marble Mason; (g) Chemical factory worker; (h) Paraffin refinery worker; (I) Printer; (j) Violinist
(Photos: Janina Mierzecka.)
Figure 2. Calluses at pressure points on the palm of the hand.
Callosities normally act as protective mechanisms but may, under certain conditions, acquire pathological features; for this reason they should not be overlooked when pathogenesis and, particularly, prophylaxis of occupational dermatoses are envisaged.
When a worker gives up a callosity-inducing job, the superfluous horny layers undergo exfoliation, the skin becomes thin and soft, the discoloration disappears and the normal appearance is restored. The time required for skin regeneration varies: occupational callosities on the hands may occasionally be seen several months or years after the work has been given up (especially in blacksmiths, glass-blowers and sawmill workers). They persist longer in senile skin and when associated with connective tissue degeneration and bursitis.
Fissures and erosions of the skin are characteristic of certain occupations (railway workers, gunsmiths, bricklayers, goldsmiths, basket weavers, etc.). The painful “tanner’s ulcer” associated with chromium compound exposures (figure 1) round or oval in shape and from 2-10 mm in diameter. The localisation of occupational lesions (e.g. on confectioners’ fingers, tailors’ fingers and palms, etc.) is also characteristic.
Pigment spots are caused by the absorption of dyes through the skin, the penetration of particles of solid chemical compounds or industrial metals, or the excessive accumulation of the skin pigment, melanin, in workers in coking or generator plants, after three to five years of work. In some establishments, about 32% of workers were found to exhibit melanomata. Pigment spots are mostly found in chemical workers.
As a rule, dyes absorbed through the skin cannot be removed by routine washing, hence their permanence and significance as occupational stigmata. Pigment spots occasionally result from impregnation with chemical compounds, plants, soil or other substances to which the skin is exposed during the work process.
A number of occupational stigmata may be seen in the region of the mouth (e.g. Burton’s line within the gums of workers exposed to lead, teeth erosion in workers exposed to acid fumes, etc. blue colouring of the lips in workers engaged in aniline manufacture and in the form of acne. Characteristic odours connected with certain occupations may also be considered as occupational stigmata.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."