9. Reproductive System
Chapter Editor: Grace Kawas Lemasters
Table of Contents
Tables and Figures
Reproductive System: Introduction
Lowell E. Sever
Introduction to Male and Female Reproductive Function
Donald R. Mattison
Male Reproductive System and Toxicology
Steven Schrader and Grace Kawas Lemasters
Structure of the Female Reproductive System and Target Organ Vulnerability
Donald R. Mattison
Maternal Occupational Exposures and Adverse Pregnancy Outcomes
Grace Kawas Lemasters
Preterm Delivery and Work
Nicole Mamelle
Occupational and Environmental Exposures to the Newborn
Mary S. Wolff and Patrisha M. Woolard
Maternity Protection in Legislation
Marie-Claire Séguret
Pregnancy and US Work Recommendations
Leon J. Warshaw
Tables
Click a link below to view table in article context.
1. Exposures with multiple adverse endpoints
2. Epidemiological studies of paternal effects on pregnancy outcome
3. Potential female reproductive toxicants
4. Definition of foetal loss & infant death
5. Factors for small for gestational age and foetal loss
6. Identified sources of occupational fatigue
7. Relative risks & fatigue indices for preterm delivery
8. Prematurity risk by number of occupational fatigue indices
9. Relative risks and changes in working conditions
10. Newborn exposure sources and levels
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Reproductive System: Introduction
Male and female reproductive toxicity are topics of increasing interest in consideration of occupational health hazards. Reproductive toxicity has been defined as the occurrence of adverse effects on the reproductive system that may result from exposure to environmental agents. The toxicity may be expressed as alterations to the reproductive organs and/or the related endocrine system. The manifestations of such toxicity may include:
- alterations in sexual behaviour
- reduced fertility
- adverse pregnancy outcomes
- modifications of other functions that are dependent on the integrity of the reproductive system.
Mechanisms underlying reproductive toxicity are complex. More xenobiotic substances have been tested and demonstrated to be toxic to the male reproductive process than to the female. However, it is not known whether this is due to underlying differences in toxicity or to the greater ease of studying sperm than oocytes.
Developmental Toxicity
Developmental toxicity has been defined as the occurrence of adverse effects on the developing organism that may result from exposure prior to conception (either parent), during pprenatal development or postnatally to the time of sexual maturation. Adverse developmental effects may be detected at any point in the life span of the organism. The major manifestations of developmental toxicity include:
- death of the developing organism
- structural abnormality
- altered growth
- functional deficiency.
In the following discussion, developmental toxicity will be used as an all-inclusive term to refer to exposures to the mother, father or conceptus that lead to abnormal development. The term teratogenesis will be used to refer more specifically to exposures to the conceptus which produce a structural malformation. Our discussion will not include the effects of postnatal exposures on development.
Mutagenesis
In addition to reproductive toxicity, exposure to either parent prior to conception has the potential of resulting in developmental defects through mutagenesis, changes in the genetic material that is passed from parent to offspring. Such changes can occur either at the level of individual genes or at the chromosomal level. Changes in individual genes can result in the transmission of altered genetic messages while changes at the chromosomal level can result in the transmission of abnormalities in chromosomal number or structure.
It is interesting that some of the strongest evidence for a role for preconception exposures in developmental abnormalities comes from studies of paternal exposures. For example, Prader-Willi syndrome, a birth defect characterized by hypotonicity in the newborn period and, later, marked obesity and behaviour problems, has been associated with paternal occupational exposures to hydrocarbons. Other studies have shown associations between paternal preconception exposures to physical agents and congenital malformations and childhood cancers. For example, paternal occupational exposure to ionizing radiation has been associated with an increased risk of neural tube defects and increased risk of childhood leukaemia, and several studies have suggested associations between paternal preconception occupational exposure to electromagnetic fields and childhood brain tumours (Gold and Sever 1994). In assessing both reproductive and developmental hazards of workplace exposures increased attention must be paid to the ppossibleeffects among males.
It is quite likely that some defects of unknown aetiology involve a genetic component which may be related to parental exposures. Because of associations demonstrated between father’s age and mutation rates it is logical to believe that other paternal factors and exposures may be associated with gene mutations. The well-established association between maternal age and chromosomal non-disjunction, resulting in abnormalities in chromosomal number, suggests a significant role for maternal exposures in chromosomal abnormalities.
As our understanding of the human genome increases it is likely that we will be able to trace more developmental defects to mutagenic changes in the DNA of single genes or structural changes in portions of chromosomes.
Teratogenesis
The adverse effects on human development of exposure of the conceptus to exogenous chemical agents have been recognized since the discovery of the teratogenicity of thalidomide in 1961. Wilson (1973) has developed six “general principles of teratology” that are relevant to this discussion. These principles are:
- The final manifestations of abnormal development are death, malformation, growth retardation and functional disorder.
- Susceptibility of the conceptus to teratogenic agents varies with the developmental stage at the time of exposure.
- Teratogenic agents act in specific ways (mechanisms) on developing cells and tissues in initiating abnormal embryogenesis (pathogenesis).
- Manifestations of abnormal development increase in degree from the no-effect to the totally lethal level as dosage increases.
- The access of adverse environmental influences to developing tissues depends on the nature of the agent.
- Susceptibility to a teratogen depends on the genotype of the conceptus and on the manner in which the genotype interacts with environmental factors.
The first four of these principles will be discussed in further detail, as will the combination of principles 1, 2 and 4 (outcome, exposure timing and dose).
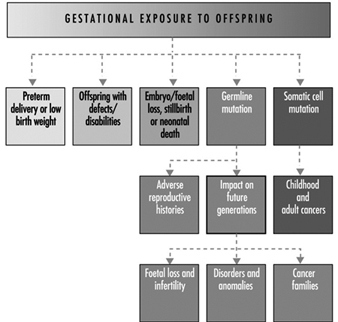
Spectrum of Adverse Outcomes Associatedwith Exposure
There is a spectrum of adverse outcomes potentially associated with exposure. Occupational studies that focus on a single outcome risk overlooking other important reproductive effects.
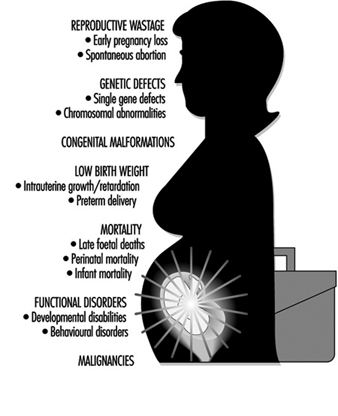
Figure 1 lists some examples of developmental outcomes potentially associated with exposure to occupational teratogens. Results of some occupational studies have suggested that congenital malformations and spontaneous abortions are associated with the same exposures—for example, anaesthetic gases and organic solvents.
Spontaneous abortion is an important outcome to consider because it can result from different mechanisms through several pathogenic processes. A spontaneous abortion can be the result of toxicity to the embryo or foetus, chromosomal alterations, single gene effects or morphological abnormalities. It is important to try to differentiate between karyotypically normal and abnormal conceptuses in studies of spontaneous abortions.
Figure 1. Developmental abnormalities and reproductive outcomes potentially associated with occupational exposures.
Timing of Exposure
Wilson’s second principle relates susceptibility to abnormal development to the time of exposure, that is, the gestational age of the conceptus. This principle has been well established for the induction of structural malformations, and the sensitive periods for organogenesis are known for many structures. Considering an expanded array of outcomes, the sensitive period during which any effect can be induced must be extended throughout gestation.
In assessing occupational developmental toxicity, exposure should be determined and classified for the appropriate critical period—that is, gestational age(s)—for each outcome. For example, spontaneous abortions and congenital malformations are likely to be related to first and second trimester exposure, whereas low birth weight and functional disorders such as seizure disorders and mental retardation are more likely to be related to second and third trimester exposure.
Teratogenic Mechanisms
The third principle is the importance of considering the potential mechanisms that might initiate abnormal embryogenesis. A number of different mechanisms have been suggested which could lead to teratogenesis (Wilson 1977). These include:
- mutational changes in DNA sequences
- chromosomal abnormalities leading to structural or quantitative changes in DNA
- alteration or inhibition of intracellular metabolism, e.g., metabolic blocks and lack of co-enzymes, precursors or substrates for biosynthesis
- interruption of DNA or RNA synthesis
- interference with mitosis
- interference with cell differentiation
- failure of cell-to-cell interactions
- failure of cell migrations
- cell death through direct cytotoxic effects
- effects on cell membrane permeability and osmolar changes
- physical disruption of cells or tissues.
By considering mechanisms, investigators can develop biologically meaningful groupings of outcomes. This can also provide insight into potential teratogens; for example, relationships between carcinogenesis, mutagenesis and teratogenesis have been discussed for some time. From the perspective of assessing occupational reproductive hazards, this is of particular importance for two distinct reasons: (1) substances that are carcinogenic or mutagenic have an increased probability of being teratogenic, suggesting that particular attention should be paid to the reproductive effects of such substances, and (2) effects on deoxyribonucleic acid (DNA), producing somatic mutations, are thought to be mechanisms for both carcinogenesis and teratogenesis.
Dose and Outcome
The fourth principle concerning teratogenesis is the relationship of outcome to dose. This principle is clearly established in many animal studies, and Selevan (1985) has discussed its potential relevance to the human situation, noting the importance of multiple reproductive outcomes within specific dose ranges and suggesting that a dose-response relationship could be reflected in an increasing rate of a particular outcome with increasing dose and/or a shift in the spectrum of the outcomes observed.
In regard to teratogenesis and dose, there is considerable concern about functional disturbances resulting from the ppossiblebehavioural effects of pprenatal exposure to environmental agents. Animal behavioural teratology is expanding rapidly, but human behavioural environmental teratology is in a relatively early stage of development. At present, there are critical limitations in the definition and ascertainment of appropriate behavioural outcomes for epidemiological studies. In addition it is ppossiblethat low-level exposures to developmental toxicants are important for some functional effects.
Multiple Outcomes and Exposure Timing and Dose
Of particular importance with respect to the identification of workplace developmental hazards are the concepts of multiple outcomes and exposure timing and dose. On the basis of what we know about the biology of development, it is clear that there are relationships between reproductive outcomes such as spontaneous abortion and intrauterine growth retardation and congenital malformations. In addition, multiple effects have been shown for many developmental toxicants (table 1).
Table 1. Examples of exposures associated with multiple adverse reproductive end-points
| Exposure | Outcome | |||
| Spontaneous abortion | Congenital malformation | Low birth weight | Developmental disabilities | |
| Alcohol | X | X | X | X |
| Anaesthetic gases |
X | X | ||
| Lead | X | X | X | |
| Organic solvents | X | X | X | |
| Smoking | X | X | X | |
Relevant to this are issues of exposure timing and dose-response relationships. It has long been recognized that the embryonic period during which organogenesis occurs (two to eight weeks post-conception) is the time of greatest sensitivity to the induction of structural malformations. The foetal period from eight weeks to term is the time of histogenesis, with rapid increase in cell number and cellular differentiation occurring during this time. It is then that functional abnormalities and growth retardation are most likely to be induced. It is ppossiblethat there may be relationships between dose and response during this period where a high dose might lead to growth retardation and a lower dose might result in functional or behavioural disturbance.
Male-Mediated Developmental Toxicity
While developmental toxicity is usually considered to result from exposure of the female and the conceptus—that is, teratogenic effects—there is increasing evidence from both animal and human studies for male-mediated developmental effects. Proposed mechanisms for such effects include transmission of chemicals from the father to the conceptus via seminal fluid, indirect contamination of the mother and the conceptus by substances carried from the workplace into the home environment through personal contamination, and—as noted earlier—paternal preconception exposures that result in transmissible genetic changes (mutations).
Introduction to the Male and Female Reproductive Function
Reproductive toxicity has many unique and challenging differences from toxicity to other systems. Whereas other forms of environmental toxicity typically involve development of disease in an exposed individual, because reproduction requires interaction between two individuals, reproductive toxicity will be expressed within a reproductive unit, or couple. This unique, couple- dependent aspect, although obvious, makes reproductive toxicology distinct. For example, it is ppossiblethat exposure to a toxicant by one member of a reproductive couple (e.g., the male) will be manifest by an adverse reproductive outcome in the other member of the couple (e.g., increased frequency of spontaneous abortion). Any attempt to deal with environmental causes of reproductive toxicity must address the couple-specific aspect.
There are other unique aspects that reflect the challenges of reproductive toxicology. Unlike renal, cardiac or pulmonary function, reproductive function occurs intermittently. This means that occupational exposures can interfere with reproduction but go unnoticed during periods when fertility is not desired. This intermittent characteristic can make the identification of a reproductive toxicant in humans more difficult. Another unique characteristic of reproduction, which follows directly from the consideration above, is that complete assessment of the functional integrity of the reproductive system requires that the couple attempt pregnancy.
Male Reproductive System and Toxicology
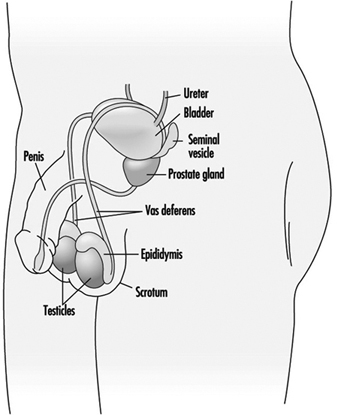
Spermatogenesis and spermiogenesis are the cellular processes that produce mature male sex cells. These processes take place within the seminiferous tubules of the testes of the sexually mature male, as shown in Figure 1. The human seminiferous tubules are 30 to 70 cm long and 150 to 300 mm in diameter (Zaneveld 1978). The spermatogonia (stem cells) are ppositioned along the basement membrane of the seminiferous tubules and are the basic cells for the production of sperm.
Figure 1. The male reproductive system
Sperm mature through a series of cellular divisions in which the spermatogonia proliferate and become primary spermatocytes. The resting primary spermatocytes migrate through tight junctions formed by the Sertoli cells to the luminal side of this testis barrier. By the time the spermatocytes reach the membrane barrier in the testis, the synthesis of DNA, the genetic material in the nucleus of the cell, is essentially complete. When the primary spermatocytes actually encounter the lumen of the seminiferous tubule, these undergo a special type of cell division which occurs only in germ cells and is known as meiosis. Meiotic cellular divison results in the splitting up of the chromosomes pairs in the nucleus, so that each resulting germ cell contains only a single copy of each chromosome strand rather than a matched pair.
During meiosis the chromosomes change shape by condensing and becoming filamentous. At a certain point, the nuclear membrane which surrounds them breaks down and microtubular spindles attach to the chromosomal pairs, causing them to separate. This completes the first meiotic division and two haploid secondary spermatocytes are formed. The secondary spermatocytes then undergo a second meiotic division to form equal numbers of X- and Y-chromosome bearing spermatids.
The morphological transformation of spermatids to spermatozoa is called spermiogenesis. When spermiogenesis is complete, each sperm cell is released by the Sertoli cell into the seminiferous tubule lumen by a process referred to as spermiation. The sperm migrate along the tubule to the rete testis and into the head of the epididymis. Sperm leaving the seminiferous tubules are immature: unable to fertilize an ovum and unable to swim. Spermatozoa released into the lumen of the seminiferous tubule are suspended in fluid pproduced primarily by the Sertoli cells. Concentrated sperm suspended within this fluid flow continuously from the seminiferous tubules, through slight changes in the ionic milieu within the rete testis, through the vasa efferentia, and into the epididymis. The epididymis is a single highly coiled tube (five to six metres long) in which sperm spend 12 to 21 days.
Within the epididymis, sperm progressively acquire motility and fertilizing capacity. This may be due to the changing nature of the suspension fluid in the epididymis. That is, as the cells mature the epididymis absorbs components from the fluid including secretions from the Sertoli cells (e.g., androgen binding protein), thereby increasing the concentration of spermatozoa. The epididymis also contributes its own secretions to the suspension fluid, including the chemicals glycerylphosphorylcholine (GPC) and carnitine.
Sperm morphology continues to transform in the epididymis. The cytoplasmic droplet is shed and the sperm nucleus condenses further. While the epididymis is the principal storage reservoir for sperm until ejaculation, about 30% of the sperm in an ejaculate have been stored in the vas deferens. Frequent ejaculation accelerates passage of sperm through the epididymis and may increase the number of immature (infertile) sperm in the ejaculate (Zaneveld 1978).
Ejaculation
Once within the vas deferens, the sperm are transported by the muscular contractions of ejaculation rather than by the flow of fluid. During ejaculation, fluids are forcibly expelled from the accessory sex glands giving rise to the seminal plasma. These glands do not expel their secretions at the same time. Rather, the bulbourethral (Cowper’s) gland first extrudes a clear fluid, followed by the prostatic secretions, the sperm-concentrated fluids from the epididymides and ampulla of the vas deferens, and finally the largest fraction primarily from the seminal vesicles. Thus, seminal plasma is not a homogeneous fluid.
Toxic Actions on Spermatogenesisand Spermiogenesis
Toxicants may disrupt spermatogenesis at several points. The most damaging, because of irreversibility, are toxicants that kill or genetically alter (beyond repair mechanisms) spermatogonia or Sertoli cells. Animal studies have been useful to determine the stage at which a toxicant attacks the spermatogenic process. These studies employ short term exposure to a toxicant before sampling to determine the effect. By knowing the duration for each spermatogenic stage, one can extrapolate to estimate the affected stage.
Biochemical analysis of seminal plasma pprovides insights into the function of the accessory sex glands. Chemicals that are secreted primarily by each of the accessory sex glands are typically selected to serve as a marker for each respective gland. For example, the epididymis is represented by GPC, the seminal vesicles by fructose, and the prostate gland by zinc. Note that this type of analysis pprovides only gross information on glandular function and little or no information on the other secretory constituents. Measuring semen pH and osmolality provide additional general information on the nature of seminal plasma.
Seminal plasma may be analysed for the presence of a toxicant or its metabolite. Heavy metals have been detected in seminal plasma using atomic absorption spectrophotometry, while halogenated hydrocarbons have been measured in seminal fluid by gas chromatography after extraction or protein-limiting filtration (Stachel et al. 1989; Zikarge 1986).
The viability and motility of spermatozoa in seminal plasma is typically a reflection of seminal plasma quality. Alterations in sperm viability, as measured by stain exclusion or by hypoosmotic swelling, or alterations in sperm motility parameters would suggest post-testicular toxicant effects.
Semen analyses also can indicate whether production of sperm cells has been affected by a toxicant. Sperm count and sperm morphology provide indices of the integrity of spermatogenesis and spermiogenesis. Thus, the number of sperm in the ejaculate is directly correlated with the number of germ cells per gram of testis (Zukerman et al. 1978), while abnormal morphology is probably a result of abnormal spermiogenesis. Dead sperm or immotile sperm often reflect the effects of post-testicular events. Thus, the type or timing of a toxic effect may indicate the target of the toxicant. For example, exposure of male rats to 2-methoxyethanol resulted in reduced fertility after four weeks (Chapin et al. 1985). This evidence, corroborated by histological examination, indicates that the target of toxicity is the spermatocyte (Chapin et al. 1984). While it is not ethical to intentionally expose humans to suspected reproductive toxicants, semen analyses of serial ejaculates of men inadvertently exposed for a short time to potential toxicants may provide similar useful information.
Occupational exposure to 1,2-dibromochloropropane (DBCP) reduced sperm concentration in ejaculates from a median of 79 million cells/ml in unexposed men to 46 million cells/ml in exposed workers (Whorton et al. 1979). Upon removing the workers from the exposure, those with reduced sperm counts experienced a partial recovery, while men who had been azoospermic remained sterile. Testicular biopsy revealed that the target of DBCP was the spermatogonia. This substantiates the severity of the effect when stem cells are the target of toxicants. There were no indications that DBCP exposure of men was associated with adverse pregnancy outcome (Potashnik and Abeliovich 1985). Another example of a toxicant targeting spermatogenesis/spermiogenesis was the study of workers exposed to ethylene dibromide (EDB). They had more sperm with tapered heads and fewer sperm per ejaculate than did controls (Ratcliffe et al. 1987).
Genetic damage is difficult to detect in human sperm. Several animal studies using the dominant lethal assay (Ehling et al. 1978) indicate that paternal exposure can produce an adverse pregnancy outcome. Epidemiological studies of large populations have demonstrated increased frequency of spontaneous abortions in women whose husbands were working as motor vehicle mechanics (McDonald et al. 1989). Such studies indicate a need for methods to detect genetic damage in human sperm. Such methods are being developed by several laboratories. These methods include DNA probes to discern genetic mutations (Hecht 1987), sperm chromosome karyotyping (Martin 1983), and DNA stability assessment by flow cytometry (Evenson 1986).
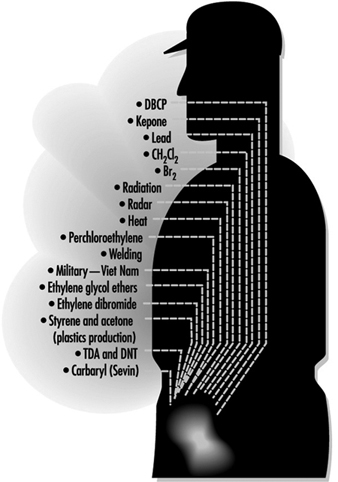
Figure 2. Exposures positively associated with adversely affecting semen quality
Figure 2 lists exposures known to affect sperm quality and table 1 provides a summary of the results of epidemiological studies of paternal effects on reproductive outcomes.
Table 1. Epidemiological studies of paternal effects on pregnancy outcome
| Reference | Type of exposure or occupation | Association with exposure1 | Effect |
| Record-based population studies | |||
| Lindbohm et al. 1984 | Solvents | – | Spontaneous abortion |
| Lindbohm et al. 1984 | Service station | + | Spontaneous abortion |
| Daniell and Vaughan 1988 | Organic solvents | – | Spontaneous abortion |
| McDonald et al. 1989 | Mechanics | + | Spontaneous abortion |
| McDonald et al. 1989 | Food processing | + | Developmental defects |
| Lindbohm et al. 1991a | Ethylene oxide | + | Spontaneous abortion |
| Lindbohm et al. 1991a | Petroleum refinery | + | Spontaneous abortion |
| Lindbohm et al. 1991a | Impregnates of wood | + | Spontaneous abortion |
| Lindbohm et al. 1991a | Rubber chemicals | + | Spontaneous abortion |
| Olsen et al. 1991 | Metals | + | Child cancer risk |
| Olsen et al. 1991 | Machinists | + | Child cancer risk |
| Olsen et al. 1991 | Smiths | + | Child cancer risk |
| Kristensen et al. 1993 | Solvents | + | Preterm birth |
| Kristensen et al. 1993 | Lead and solvents | + | Preterm birth |
| Kristensen et al. 1993 | Lead | + | Perinatal death |
| Kristensen et al. 1993 | Lead | + | Male child morbidity |
| Case-control studies | |||
| Kucera 1968 | Printing industry | (+) | Cleft lip |
| Kucera 1968 | Paint | (+) | Cleft palate |
| Olsen 1983 | Paint | + | Damage to central nervous system |
| Olsen 1983 | Solvents | (+) | Damage to central nervous system |
| Sever et al. 1988 | Low-level radiation | + | Neural tube defects |
| Taskinen et al. 1989 | Organic solvents | + | Spontaneous abortion |
| Taskinen et al. 1989 | Aromatic hydrocarbons | + | Spontaneous abortion |
| Taskinen et al. 1989 | Dust | + | Spontaneous abortion |
| Gardner et al. 1990 | Radiation | + | Childhood leukaemia |
| Bonde 1992 | Welding | + | Time to conception |
| Wilkins and Sinks 1990 | Agriculture | (+) | Child brain tumour |
| Wilkins and Sinks 1990 | Construction | (+) | Child brain tumour |
| Wilkins and Sinks 1990 | Food/tobacco processing | (+) | Child brain tumour |
| Wilkins and Sinks 1990 | Metal | + | Child brain tumour |
| Lindbohmn et al. 1991b | Lead | (+) | Spontaneous abortion |
| Sallmen et al. 1992 | Lead | (+) | Congenital defects |
| Veulemans et al. 1993 | Ethylene glycol ether | + | Abnormal spermiogram |
| Chia et al. 1992 | Metals | + | Cadmium in semen |
1 – no significant association; (+) marginally significant association; + significant association.
Source: Adapted from Taskinen 1993.
Neuroendocrine System
The overall functioning of the reproductive system is controlled by the nervous system and the hormones pproduced by the glands (the endocrine system). The reproductive neuroendocrine axis of the male involves principally the central nervous systems (CNS), the anterior pituitary gland and the testes. Inputs from the CNS and from the periphery are integrated by the hypothalamus, which directly regulates gonadotrophin secretion by the anterior pituitary gland. The gonadotrophins, in turn, act principally upon the Leydig cells within the interstitium and Sertoli and germ cells within the seminiferous tubules to regulate spermatogenesis and hormone production by the testes.
Hypothalamic–Pituitary Axis
The hypothalamus secretes the neurohormone gonadotrophin releasing hormone (GnRH) into the hypophysial portal vasculature for transport to the anterior pituitary gland. The pulsatile secretion of this decapeptide causes the concomitant release of luteinizing hormone (LH), and with lesser synchrony and one-fifth the potency, the release of follicle stimulating hormone (FSH) (Bardin 1986). Substantial evidence exists to support the presence of a separate FSH releasing hormone, although none has yet been isolated (Savy-Moore and Schwartz 1980; Culler and Negro-Vilar 1986). These hormones are secreted by the anterior pituitary gland. LH acts directly upon the Leydig cells to stimulate synthesis and release of testosterone, whereas FSH stimulates aromatization of testosterone to estradiol by the Sertoli cell. Gonadotropic stimulation causes the release of these steroid hormones into the spermatic vein.
Gonadotrophin secretion is, in turn, checked by testosterone and estradiol through negative feedback mechanisms. Testosterone acts principally upon the hypothalamus to regulate GnRH secretion and thereby reduces the pulse frequency, primarily, of LH release. Estradiol, on the other hand, acts upon the pituitary gland to reduce the magnitude of gonadotrophin release. Through these endocrine feedback loops, testicular function in general and testosterone secretion specifically are maintained at a relatively steady state.
Pituitary–Testicular Axis
LH and FSH are generally viewed as necessary for normal spermatogenesis. Presumably the effect of LH is secondary to inducing high intratesticular concentrations of testosterone. Therefore, FSH from the pituitary gland and testosterone from the Leydig cells act upon the Sertoli cells within the seminiferous tubule epithelium to initiate spermatogenesis. Sperm production persists, although quantitatively reduced, after removing either LH (and presumably the high intratesticular testosterone concentrations) or FSH. FSH is required for initiating spermatogenesis at puberty and, to a lesser extent, to reinitiate spermatogenesis that has been arrested (Matsumoto 1989; Sharpe 1989).
The hormonal synergism that serves to maintain spermatogenesis may entail recruitment by FSH of differentiated spermatogonia to enter meiosis, while testosterone may control specific, subsequent stages of spermatogenesis. FSH and testosterone may also act upon the Sertoli cell to stimulate production of one or more paracrine factors which may affect the number of Leydig cells and testosterone production by these cells (Sharpe 1989). FSH and testosterone stimulate protein synthesis by Sertoli cells including synthesis of androgen binding protein (ABP), while FSH alone stimulates synthesis of aromatase and inhibin. ABP is secreted primarily into the seminiferous tubular fluid and is transported to the proximal portion of the caput epididymis, possibly serving as a local carrier of androgens (Bardin 1986). Aromatase catalyses the conversion of testosterone to estradiol in the Sertoli cells and in other peripheral tissues.
Inhibin is a glycoprotein consisting of two dissimilar, disulphide-linked subunits, a and b. Although inhibin preferentially inhibits FSH release, it may also attenuate LH release in the presence of GnRH stimulation (Kotsugi et al. 1988). FSH and LH stimulate inhibin release with approximately equal potency (McLachlan et al. 1988). Interestingly, inhibin is secreted into the spermatic vein blood as pulses which are synchronous to those of testosterone (Winters 1990). This probably does not reflect direct actions of LH or testosterone on Sertoli cell activity, but rather the effects of other Leydig cell products secreted either into the interstitial spaces or the circulation.
Prolactin, which is also secreted by the anterior pituitary gland, acts synergistically with LH and testosterone to promote male reproductive function. Prolactin binds to specific receptors on the Leydig cell and increases the amount of androgen receptor complex within the nucleus of androgen responsive tissues (Baker et al. 1977). Hyperprolactinaemia is associated with reductions of testicular and prostate size, semen volume and circulating concentrations of LH and testosterone (Segal et al. 1979). Hyperprolactinaemia has also been associated with impotency, apparently independent of altering testosterone secretion (Thorner et al. 1977).
If measuring steroid hormone metabolites in urine, consideration must be given to the potential that the exposure being studied may alter the metabolism of excreted metabolites. This is especially pertinent since most metabolites are formed by the liver, a target of many toxicants. Lead, for example, reduced the amount of sulphated steroids that were excreted into the urine (Apostoli et al. 1989). Blood levels for both gonadotrophins become elevated during sleep as the male enters puberty, while testosterone levels maintain this diurnal pattern through adulthood in men (Plant 1988). Thus blood, urine or saliva samples should be collected at approximately the same time of day to avoid variations due to diurnal secretory patterns.
The overt effects of toxic exposure targeting the reproductive neuroendocrine system are most likely to be revealed through altered biological manifestations of the androgens. Manifestations significantly regulated by androgens in the adult man that may be detected during a basic physical examination include: (1) nitrogen retention and muscular development; (2) maintenance of the external genitalia and accessory sexual organs; (3) maintenance of the enlarged larynx and thickened vocal cords causing the male voice; (4) beard, axillary and pubic hair growth and temporal hair recession and balding; (5) libido and sexual performance; (6) organ specific proteins in tissues (e.g., liver, kidneys, salivary glands); and (7) aggressive behaviour (Bardin 1986). Modifications in any of these traits may indicate that androgen production has been affected.
Examples of Toxicant Effects
Lead is a classic example of a toxicant that directly affects the neuroendocrine system. Serum LH concentrations were elevated in men exposed to lead for less than one year. This effect did not progress in men exposed for more than five years. Serum FSH levels were not affected. On the other hand, serum levels of ABP were elevated and those of total testosterone were reduced in men exposed to lead for more than five years. Serum levels of free testosterone were significantly reduced after exposure to lead for three to five years (Rodamilans et al. 1988). In contrast, serum concentrations of LH, FSH, total testosterone, prolactin, and total neutral 17-ketosteroids were not altered in workers with lower circulating levels of lead, even though the distribution frequency of sperm count was altered (Assennato et al. 1986).
Exposure of shipyard painters to 2-ethoxyethanol also reduced sperm count without a concurrent change in serum LH, FSH, or testosterone concentrations (Welch et al. 1988). Thus toxicants may affect hormone production and sperm measures independently.
Male workers involved in the manufacture of the nematocide DBCP experienced elevated serum levels of LH and FSH and reduced sperm count and fertility. These effects are apparently sequelae to DBCP actions upon the Leydig cells to alter androgen production or action (Mattison et al. 1990).
Several compounds may exert toxicity by virtue of structural similarity to reproductive steroid hormones. Thus, by binding to the respective endocrine receptor, toxicants may act as agonists or antagonists to disrupt biological responses. Chlordecone (Kepone), an insecticide that binds to oestrogen receptors, reduced sperm count and motility, arrested sperm maturation and reduced libido. While it is tempting to suggest that these effects result from chlordecone interfering with oestrogen actions at the neuroendocrine or testicular level, serum levels of testosterone, LH and FSH were not shown to be altered in these studies in a manner similar to the effects of oestradiol therapy. DDT and its metabolites also exhibit steroidal properties and might be expected to alter male reproductive function by interfering with steroidal hormone functions. Xenobiotics such as polychlorinated biphenyls, polybrominated biphenyls, and organochlorine pesticides may also interfere with male reproductive functions by exerting oestrogenic agonist/antagonist activity (Mattison et al. 1990).
Sexual Function
Human sexual function refers to the integrated activities of the testes and secondary sex glands, the endocrine control systems, and the central nervous system-based behavioural and psychological components of reproduction (libido). Erection, ejaculation and orgasm are three distinct, independent, physiological and psychodynamic events which normally occur concurrently in men.
Little reliable data are available on occupational exposure effects on sexual function due to the problems described above. Drugs have been shown to affect each of the three stages xof male sexual function (Fabro 1985), indicating the potential for occupational exposures to exert similar effects. Antidepressants, testosterone antagonists and stimulants of prolactin release effectively reduce libido in men. Antihypertensive drugs which act on the sympathetic nervous system induce impotence in some men, but surprisingly, priapism in others. Phenoxybenzamine, an adrenoceptive antagonist, has been used clinically to block seminal emission but not orgasm (Shilon, Paz and Homonnai 1984). Anticholinergic antidepressant drugs permit seminal emission while blocking seminal ejection and orgasm which results in seminal plasma seeping from the urethra rather than being ejected.
Recreational drugs also affect sexual function (Fabro 1985). Ethanol may reduce impotence while enhancing libido. Cocaine, heroin and high doses of cannabinoids reduce libido. Opiates also delay or impair ejaculation.
The vast and varied array of pharmaceuticals that has been shown to affect the male reproductive system pprovides support for the notion that chemicals found in the workplace may also be reproductive toxicants. Research methods that are reliable and practical for field study conditions are needed to assess this important area of reproductive toxicology.
Structure of the Female Reproductive System and Target Organ Vulnerability
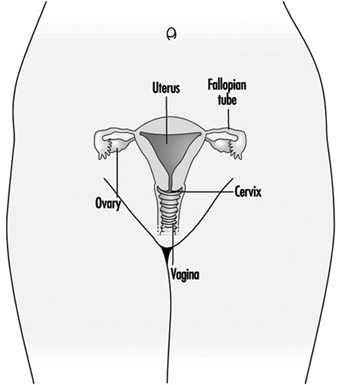
Figure 1. The female reproductive system.
The female reproductive system is controlled by components of the central nervous system, including the hypothalamus and pituitary. It consists of the ovaries, the fallopian tubes, the uterus and the vagina (Figure 1). The ovaries, the female gonads, are the source of oocytes and also synthesize and secrete oestrogens and progestogens, the major female sex hormones. The fallopian tubes transport oocytes to and sperm from the uterus. The uterus is a pear-shaped muscular organ, the upper part of which communicates through the fallopian tubes to the abdominal cavity, while the lower part is contiguous through the narrow canal of the cervix with the vagina, which passes to the exterior. Table 1 summarizes compounds, clinical manifestations, site and mechanisms of action of potential reproductive toxicants.
Table 1. Potential female reproductive toxicants
| Compound | Clinical manifestation | Site | Mechanism/target |
| Chemical reactivity | |||
| Alkylating agents |
Altered menses Amenorrhoea Ovarian atrophy Decreased fertility Premature menopause |
Ovary Uterus |
Granulosa cell cytotoxicity Oocyte cytotoxicity Endometrial cell cytotoxicity |
| Lead | Abnormal menses Ovarian atrophy Decreased fertility |
Hypothalamus Pituitary Ovary |
Decreased FSH Decreased progesterone |
| Mercury | Abnormal menses | Hypothalamus Ovary |
Altered gonadotrophin production and secretion Follicle toxicity Granulosa cell proliferation |
| Cadmium | Follicular atresia Persistent diestrus |
Ovary Pituitary Hypothalamus |
Vascular toxicity Granulosa cell cytotoxicity Cytotoxicity |
| Structural similarity | |||
| Azathioprine | Reduced follicle numbers | Ovary Oogenesis |
Purine analog Disruption of DNA/RNA synthesis |
| Chlordecone | Impaired fertility | Hypothalamus | Oestrogen agonist |
| DDT | Altered menses | Pituitary | FSH, LH disruption |
| 2,4-D | Infertility | ||
| Lindane | Amenorrhoea | ||
| Toxaphene | Hypermenorrhoea | ||
| PCBs, PBBs | Abnormal menses | FSH, LH disruption | |
Source: From Plowchalk, Meadows and Mattison 1992. These compounds are suggested to be direct-acting reproductive toxicants based primarily on toxicity testing in experimental animals.
The Hypothalamus and Pituitary
The hypothalamus is located in the diencephalon, which sits on top of the brainstem and is surrounded by the cerebral hemispheres. The hypothalamus is the principal intermediary between the nervous and the endocrine systems, the two major control systems of the body. The hypothalamus regulates the pituitary gland and hormone production.
The mechanisms by which a chemical might disrupt the reproductive function of the hypothalamus generally include any event that could modify the pulsatile release of gonadotrophin releasing hormone (GnRH). This may involve an alteration in either the frequency or the amplitude of GnRH pulses. The processes susceptible to chemical injury are those involved in the synthesis and secretion of GnRH—more specifically, transcription or translation, packaging or axonal transport, and secretory mechanisms. These processes represent sites where direct-acting chemically reactive compounds might interfere with hypothalmic synthesis or release of GnRH. An altered frequency or amplitude of GnRH pulses could result from disruptions in stimulatory or inhibitory pathways that regulate the release of GnRH. Investigations of the regulation of the GnRH pulse generator have shown that catecholamines, dopamine, serotonin, γ-aminobutyric acid, and endorphins all have some potential for altering the release of GnRH. Therefore, xenobiotics that are agonists or antagonists of these compounds could modify GnRH release, thus interfering with communication with the pituitary.
Prolactin, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are three protein hormones secreted by the anterior pituitary that are essential for reproduction. These play a critical role in maintaining the ovarian cycle, governing follicle recruitment and maturation, steroidogenesis, completion of ova maturation, ovulation and luteinization.
The precise, finely tuned control of the reproductive system is accomplished by the anterior pituitary in response to positive and negative feedback signals from the gonads. The appropriate release of FSH and LH during the ovarian cycle controls normal follicular development, and the absence of these hormones is followed by amenorrhoea and gonadal atrophy. The gonadotrophins play a critical role in initiating changes in the morphology of ovarian follicles and in their steroidal microenvironments through the stimulation of steroid production and the induction of receptor populations. Timely and adequate release of these gonadotrophins is also essential for ovulatory events and a functional luteal phase. Because gonadotrophins are essential for ovarian function, altered synthesis, storage or secretion may seriously disrupt reproductive capacity. Interference with gene expression—whether in transcription or translation, post-translational events or packaging, or secretory mechanisms—may modify the level of gonadotrophins reaching the gonads. Chemicals that act by means of structural similarity or altered endocrine homeostasis might produce effects by interference with normal feedback mechanisms. Steroid-receptor agonists and antagonists might initiate an inappropriate release of gonadotrophins from the pituitary, thereby inducing steroid-metabolizing enzymes, reducing steroid half-life and subsequently the circulating level of steroids reaching the pituitary.
The Ovary
The ovary in primates is responsible for the control of reproduction through its principal products, oocytes and steroid and protein hormones. Folliculogenesis, which involves both intraovarian and extraovarian regulatory mechanisms, is the process by which oocytes and hormones are produced. The ovary itself has three functional subunits: the follicle, the oocyte and the corpus luteum. During the normal menstrual cycle, these components, under the influence of FSH and LH, function in concert to produce a viable ovum for fertilization and a suitable environment for implantation and subsequent gestation.
During the preovulatory period of the menstrual cycle, follicle recruitment and development occur under the influence of FSH and LH. The latter stimulates the production of androgens by thecal cells, whereas the former stimulates the aromatization of androgens into oestrogens by the granulosa cells and the production of inhibin, a protein hormone. Inhibin acts at the anterior pituitary to decrease the release of FSH. This prevents excess stimulation of follicular development and allows continuing development of the dominant follicle—the follicle destined to ovulate. Oestrogen production increases, stimulating both the LH surge (resulting in ovulation) and the cellular and secretory changes in the vagina, cervix, uterus and oviduct that enhance spermatozoa viability and transport.
In the postovulatory phase, thecal and granulosa cells remaining in the follicular cavity of the ovulated ovum, form the corpus luteum and secrete progesterone. This hormone stimulates the uterus to provide a proper environment for implantation of the embryo if fertilization occurs. Unlike the male gonad, the female gonad has a finite number of germ cells at birth and is therefore uniquely sensitive to reproductive toxicants. Such exposure of the female can lead to decreased fecundity, increased pregnancy wastage, early menopause or infertility.
As the basic reproductive unit of the ovary, the follicle maintains the delicate hormonal environment necessary to support the growth and maturation of an oocyte. As previously noted, this complex process is known as folliculogenesis and involves both intraovarian and extraovarian regulation. Numerous morphological and biochemical changes occur as a primordial follicle progresses to a pre-ovulatory follicle (which contains a developing oocyte), and each stage of follicular growth exhibits unique patterns of gonadotrophin sensitivity, steroid production and feedback pathways. These characteristics suggest that a number of sites are available for xenobiotic interaction. Also, there are different follicle populations within the ovary, which further complicates the situation by allowing for differential follicle toxicity. This creates a situation in which the patterns of infertility induced by a chemical agent would depend on the follicle type affected. For example, toxicity to primordial follicles would not produce immediate signs of infertility but would ultimately shorten the reproductive lifespan. On the other hand, toxicity to antral or preovulatory follicles would result in an immediate loss of reproductive function. The follicle complex is composed of three basic components: granulosa cells, thecal cells and the oocyte. Each of these components has characteristics that may make it uniquely susceptible to chemical injury.
Several investigators have explored methodology for screening xenobiotics for granulosa cell toxicity by measuring the effects on progesterone production by granulosa cells in culture. Oestradiol suppression of progesterone production by granulosa cells has been utilized to verify granulosa cell responsiveness. The pesticide p,p’-DDT and its o,p’-DDT isomer produce supression of progesterone production apparently with potencies equal to that of oestradiol. By contrast, the pesticides malathion, arathion and dieldrin and the fungicide hexachlorobenzene are without effect. Further detailed analysis of isolated granulosa cell responses to xenobiotics is needed to define the utility of this assay system. The attractiveness of isolated systems such as this is economy and ease of use; however, it is important to remember that granulosa cells represent only one component of the reproductive system.
Thecal cells provide precursors for steroids synthesized by granulosa cells. Thecal cells are believed to be recruited from ovarian stroma cells during follicle formation and growth. Recruitment may involve stromal cellular proliferation as well as migration to regions around the follicle. Xenobiotics that impair cell proliferation, migration and communication will impact on thecal cell function. Xenobiotics that alter thecal androgen production may also impair follicle function. For example, the androgens metabolized to oestrogens by granulosa cells are provided by thecal cells. Alterations in thecal cell androgen production, either increases or decreases, are expected to have a significant effect on follicle function. For example, it is believed that excess production of androgens by thecal cells will lead to follicle atresia. In addition, impaired production of androgens by thecal cells may lead to decreased poestrogen production by granulosa cells. Either circumstance will clearly impact on reproductive performance. At resent, little is known about thecal cell vulnerability to xenobiotics.
Although there is a acuity of information defining the vulnerability of ovarian cells to xenobiotics, there are data clearly demonstrating that oocytes can be damaged or destroyed by such agents. Alkylating agents destroy oocytes in humans and experimental animals. Lead produces ovarian toxicity. Mercury and cadmium also produce ovarian damage that may be mediated through oocyte toxicity.
Fertilization to Implantation
Gametogenesis, release and union of male and female germ cells are all preliminary events leading to a zygote. Sperm cells deposited in the vagina must enter the cervix and move through the uterus and into the fallopian tube to meet the ovum. penetration of ovum by sperm and the merging of their respective DNA comprise the process of fertilization. After fertilization cell division is initiated and continues during the next three or four days, forming a solid mass of cells called a morula. The cells of the morula continue to divide, and by the time the developing embryo reaches the uterus it is a hollow ball called a blastocyst.
Following fertilization, the developing embryo migrates through the fallopian tube into the uterus. The blastocyst enters the uterus and implants in the endometrium approximately seven days after ovulation. At this time the endometrium is in the postovulatory phase. Implantation enables the blastocyst to absorb nutrients or toxicants from the glands and blood vessels of the endometrium.
Maternal Occupational Exposures and Adverse Pregnancy Outcomes
Paid employment among women is growing worldwide. For example, almost 70% of women in the United States are employed outside the home during their predominant childbearing years (ages 20 to 34). Furthermore, since the 1940s there has been an almost linear trend in synthetic organic chemical production, creating a more hazardous environment for the pregnant worker and her offspring.
Ultimately, a couple’s reproductive success depends on a delicate physiochemical balance within and between the father, the mother and the foetus. Metabolic changes occurring during a pregnancy can increase exposure to hazardous toxicants for both worker and concetus. These metabolic changes include increased pulmonary absorption, increased cardiac output, delayed gastric emptying, increased intestinal motility and increased body fat. As shown in figure 1, exposure of the concetus can produce varying effects depending on the phase of development—early or late embryogenesis or the foetal period.
Figure 1. Consequences of maternal exposure to toxicants on the offspring.
Transport time of a fertilized ovum before implantation is between two and six days. During this early stage the embryo may be exposed to chemical compounds that penetrate into the uterine fluids. Absorption of xenophobic compounds may be accompanied by degenerative changes, alteration in the blastocystic protein profile or failure to implant. Insult during this period is likely to lead to a spontaneous abortion. Based on experimental data, it is thought that the embryo is fairly resistant to teratogenic insult at this early stage because the cells have not initiated the complex sequence of chemical differentiation.
The period of later embryogenesis is characterized by differentiation, mobilization and organization of cells and tissue into organ rudiments. Early pathogenesis may induce cell death, failed cellular interaction, reduced biosynthesis, impaired morphogenic movement, mechanical disruption, adhesions or oedema (Paul 1993). The mediating factors that determine susceptibility include route and level of exposure, pattern of exposure and foetal and maternal genotype. Extrinsic factors such as nutritional deficiencies, or the additive, synergistic or antagonistic effects associated with multiple exposures may further impact the response. Untoward responses during late embryogenesis may culminate in spontaneous abortion, gross structural defects, foetal loss, growth retardation or developmental abnormalities.
The foetal period extends from embryogenesis to birth and is defined as beginning at 54 to 60 gestational days, with the concetus having a crown-rum length of 33 mm. The distinction between the embryonic and foetal period is somewhat arbitrary. The foetal period is characterized developmentally by growth, histogenesis and functional maturation. Toxicity may be manifested by a reduction in cell size and number. The brain is still sensitive to injury; myelination is incomplete until after birth. Growth retardation, functional defects, disruption in the pregnancy, behavioural effects, translacental carcinogenesis or death may result from toxicity during the foetal period. This article discusses the biological, sociological and epidemiological effects of maternal environmental/occupational exposures.
Embryonic/Foetal Loss
The developmental stages of the zygote, defined in days from ovulation (DOV), proceed from the blastocyst stage at days 15 to 20 (one to six DOV), with implantation occurring on day 20 or 21 (six or seven DOV), to the embryonic period from days 21 to 62 (seven to 48 DOV), and the foetal period from day 63 (49+ DOV) until the designated period of viability, ranging from 140 to 195 days. Estimates of the probability of pregnancy termination at one of these stages depend on both the definition of foetal loss and the method used to measure the event. Considerable variability in the definition of early versus late foetal loss exists, ranging from the end of week 20 to week 28. The definitions of foetal and infant death recommended by the World Health Organization (1977) are listed in table 1. In the United States the gestational age setting the lower limit for stillbirths is now widely accepted to be 20 weeks.
Table 1. Definition of foetal loss and infant death
| Spontaneous abortion | ≤500 g or 20-22 weeks or 25 cm length |
| Stillbirth | 500 g (1000 g International) nonviable |
| Early neonatal death | Death of a live-born infant ≤7 days (168 hours) |
| Late neonatal death | 7 days to ≤28 days |
Source: World Health Organization 1977.
Because the majority of early aborted foetuses have chromosomal anomalies, it has been suggested that for research purposes a finer distinction should be made—between early foetal loss, before 12 weeks’ gestation, and later foetal loss (Källén 1988). In examining late foetal losses it also may be appropriate to include early neonatal deaths, as the cause may be similar. WHO defines early neonatal death as the death of an infant aged seven days or younger and late neonatal death as occurring between seven and 29 days. In studies conducted in developing countries, it is important to distinguish between prepartum and intrapartum deaths. Because of problematic deliveries, intrapartum deaths account for a large portion of stillbirths in less developed countries.
In a review by Kline, Stein and Susser (1989) of nine retrospective or cross-sectional studies, the foetal loss rates before 20 weeks’ gestation ranged from 5.5 to 12.6%. When the definition was expanded to include losses u to 28 weeks’ gestation, the foetal loss rate varied between 6.2 and 19.6%. The rates of foetal loss among clinically recognized pregnancies in four prospective studies, however, had a relatively narrow range of 11.7 to 14.6% for the gestational period u to 28 weeks. This lower rate, seen in prospective versus retrospective or cross-sectional designs, may be attributable to differences in underlying definitions, misreporting of induced abortions as spontaneous or misclassification of delayed or heavy menses as foetal loss.
When occult abortions or early “chemical” losses identified by an elevated level of human chorionic gonadotrohins (hCG) are included, the total spontaneous abortion rate jumps dramatically. In a study using hCG methods, the incidence of post-implantation subclinical loss of fertilized ova was 22% (Wilcox et al. 1988). In these studies urinary hCG was measured with immunoradiometric assay using a detection antibody. The assay originally used by Wilcox employed a now extinct high affinity, polyclonal rabbit antibody. More recent studies have used an inexhaustible monoclonal antibody that requires less than 5 ml of urine for replicate samples. The limiting factor for use of these assays in occupational field studies is not only the cost and resources needed to coordinate collection, storage and analysis of urine samples but the large population needed. In a study of early pregnancy loss in women workers exposed to video display terminals (VDTs), approximately 7,000 women were screened in order to acquire a usable population of 700 women. This need for ten times the population size in order to achieve an adequate sample stems from reduction in the available number of women because of ineligibility due to age, sterility and the enrollment exclusively of women who are using either no contraceptives or relatively ineffective forms of contraception.
More conventional occupational studies have used recorded or questionnaire data to identify spontaneous abortions. Recorded data sources include vital statistics and hospital, private practitioner and outpatient clinic records. Use of record systems identifies only a subset of all foetal losses, principally those that occur after the start of prenatal care, typically after two to three missed periods. Questionnaire data are collected by mail or in personal or telephone interviews. By interviewing women to obtain reproductive histories, more complete documentation of all recognized losses is possible. Questions that are usually included in reproductive histories include all pregnancy outcomes; prenatal care; family history of adverse pregnancy outcomes; marital history; nutritional status; re-pregnancy weight; height; weight gain; use of cigarettes, alcohol and prescription and nonprescription drugs; health status of the mother during and prior to a pregnancy; and exposures at home and in the workplace to physical and chemical agents such as vibration, radiation, metals, solvents and pesticides. Interview data on spontaneous abortions can be a valid source of information, particularly if the analysis includes those of eight weeks’ gestation or later and those that occurred within the last 10 years.
The principal physical, genetic, social and environmental factors associated with spontaneous abortion are summarized in table 2. To ensure that the observed exposure-effect relationship is not due to a confounding relationship with another risk factor, it is important to identify the risk factors that may be associated with the outcome of interest. Conditions associated with foetal loss include syphilis, rubella, genital Mycolasma infections, herpes simplex, uterine infections and general hyperpyrexia. One of the most important risk factors for clinically recognized spontaneous abortion is a history of pregnancy ending in foetal loss. Higher gravidity is associated with increased risk, but this may not be independent of a history of spontaneous abortion. There are conflicting interpretations of gravidity as a risk factor because of its association with maternal age, reproductive history and heterogeneity of women at different gravidity ranks. Rates of spontaneous abortion are higher for women younger than 16 and older than 36 years. After adjusting for gravidity and a history of pregnancy loss, women older than 40 were shown to have twice the risk of foetal loss of younger women. The increased risk for older women has been associated with an increase in chromosomal anomalies, particularly trisomy. possiblemale-mediated effects associated with foetal loss have been recently reviewed (Savitz, Sonnerfeld and Olshaw 1994). A stronger relationship was shown with paternal exposure to mercury and anaesthetic gases, as well as a suggestive but inconsistent relationship with exposure to lead, rubber manufacturing, selected solvents and some pesticides.
Table 2. Factors associated with small for gestational age and foetal loss
| Small for gestational age | |
| Physical-genetic | Environmental-social |
| Preterm delivery Multiple births Malformed foetus Hypertension Placental or cord anomaly Maternal medical history History of adverse pregnancy outcomes Race Chromosome anomalies Sex Maternal height, weight, weight gain Paternal height Parity Length of gestation Short interval between pregnancies |
Malnutrition Low income/poor education Maternal smoking Maternal alcohol consumption Occupational exposure Psychosocial stress Altitude History of infections Marijuana use |
| Foetal loss | |
| Physical-genetic | Environmental-social |
| Higher gravidity Maternal age Birth order Race Repeat spontaneous abortion Insulin dependent diabetes Uterine disorders Twinning Immunological factor Hormonal factors |
Socio-economic status Smoking history Prescribed and recreational drugs Alcohol use Poor nutrition Infections/maternal fever Spermicides Employment factors Chemical exposure Irradiation |
Employment status may be a risk factor regardless of a specific physical or chemical hazard and may act as a confounder in assessment of occupational exposure and spontaneous abortion. Some investigators suggest that women who stay in the workforce are more likely to have an adverse pregnancy history and as a result are able to continue working; others believe this group is an inherently more fit subpopulation due to higher incomes and better prenatal care.
Congenital Anomalies
During the first 60 days after conception, the developing infant may be more sensitive to xenobiotic toxicants than at any other stage in the life cycle. Historically, terata and congenital malformations referred to structural defects resent at birth that may be gross or microscopic, internal or external, hereditary or nonhereditary, single or multiple. Congenital anomaly, however, is more broadly defined as including abnormal behaviour, function and biochemistry. Malformations may be single or multiple; chromosomal defects generally produce multiple defects, whereas single-gene changes or exposure to environmental agents may cause either single defects or a syndrome.
The incidence of malformations depends on the status of the concetus—live birth, spontaneous abortus, stillbirth. Overall, the abnormality rate in spontaneous abortuses is approximately 19%, a tenfold increase in what is seen in the live born (Sheard, Fantel and Fitsimmons 1989). A 32% rate of anomalies was found among stillborn foetuses weighing more than 500 g. The incidence of major defects in live births is about 2.24% (Nelson and Holmes 1989). The prevalence of minor defects ranges between 3 and 15% (averaging about 10%). Birth anomalies are associated with genetic factors (10.1%), multifactorial inheritance (23%), uterine factors (2.5%), twinning (0.4%) or teratogens (3.2%). The causes of the remaining defects are unknown. Malformation rates are approximately 41% higher for boys than for girls and this is explained by the significantly higher rate of anomalies for male genital organs.
One challenge in studying malformations is deciding how to group defects for analysis. Anomalies can be classified by several parameters, including seriousness (major, minor), pathogenesis (deformation, disruption), associated versus isolated, anatomic by organ system, and aetiological (e.g., chromosomal, single gene defects or teratogen induced). Often, all malformations are combined or the combination is based either on major or minor categorization. A major malformation can be defined as one that results in death, requires surgery or medical treatment or constitutes a substantial physical or psychological handicap. The rationale for combining anomalies into large groups is that the majority arise, at approximately the same time period, during organogenesis. Thus, by maintaining larger sample sizes, the total number of cases is increased with a concomitant increase in the statistical power. If, however, the exposure effect is specific to a particular type of malformation (e.g., central nervous system), such grouping may mask the effect. Alternatively, malformations may be grouped by organ system. Though this method may be an improvement, certain defects may dominate the class, such as varus deformities of the feet in the musculoskeletal system. Given a sufficiently large sample, the optimal approach is to divide the defects into embryologically or pathogenetically homogenous groups (Källén 1988). Considerations should be given to the exclusion or inclusion of certain malformations, such as those that are likely caused by chromosomal defects, autosomal dominant conditions or malposition in utero. Ultimately, in analysing congenital anomalies, a balance has to be maintained between maintaining precision and compromising statistical power.
A number of environmental and occupational toxicants have been associated with congenital anomalies in offspring. One of the strongest associations is maternal consumption of food contaminated with methylmercury causing morphological, central nervous system and neurobehavioural abnormalities. In Japan, the cluster of cases was linked to consumption of fish and shellfish contaminated with mercury derived from the effluent of a chemical factory. The most severely affected offspring developed cerebral palsy. Maternal ingestion of polychlorinated biphenyl’s (CBs) from contaminated rice oil gave rise to babies with several disorders, including growth retardation, dark brown skin pigmentation, early eruption of teeth, gingival hyperplasia, wide sagittal suture, facial oedema and exophthalmoses. Occupations involving exposures to mixtures have been linked with a variety of adverse outcomes. The offspring of women working in the ul and aer industry, in either laboratory work or jobs involving “conversions” or aer refinement, also had increased risk of central nervous system, heart and oral cleft defects. Women working in industrial or construction work with unspecified exposures had a 50% increase in central nervous system defects, and women working in transportation and communication had two times the risk of having a child with an oral cleft. Veterinarians represent a unique group of health care personnel exposed to anaesthetic gases, radiation, trauma from animal kicks, insecticides and zoonotic diseases. Though no difference was found in the rate of spontaneous abortions or in birth weight of the offspring between female veterinarians and female lawyers, there was a significant excess of birth defects among veterinarians (Schenker et al. 1990). Lists of known, possible and unlikely teratogens are available as well as computer databases and risk lines for obtaining current information on potential teratogens (Paul 1993). Evaluating congenital anomalies in an occupational cohort is particularly difficult, however, because of the large sample size needed for statistical power and our limited ability to identify specific exposures occurring during a narrow window of time, primarily the first 55 days of gestation.
Small for Gestational Age
Among the many factors linked with infant survival, physical underdevelopment associated with low birth weight (LBW) resents one of the greatest risks. Significant weight gain of the foetus does not begin until the second trimester. The concetus weighs 1 g at eight weeks, 14 g at 12 weeks, and reaches 1.1 kg at 28 weeks. An additional 1.1 kg is gained every six weeks thereafter until term. The normal newborn weighs approximately 3,200 g at term. The newborn’s weight is dependent on its rate of growth and its gestational age at delivery. An infant that is growth retarded is said to be small for gestational age (SGA). If an infant is delivered prior to term it will have a reduced weight but will not necessarily be growth retarded. Factors associated with a preterm delivery are discussed elsewhere, and the focus of this discussion is on the growth-retarded newborn. The terms SGA and LBW will be used interchangeably. A low birth-weight infant is defined as an infant weighing less than 2,500 g, a very low birth weight is defined as less than 1,500 g, and extremely low birth weight is one that is less than 1,000 g (WHO 1969).
When examining causes of reduced growth, it is important to distinguish between asymmetrical and symmetrical growth retardation. Asymmetrical growth retardation, i.e., where the weight is affected more than the skeletal structure, is primarily associated with a risk factor operating during late pregnancy. On the other hand, symmetrical growth retardation may more likely be associated with an aetiology that operates over the entire period of gestation (Kline, Stein and Susser 1989). The difference in rates between asymmetrical and symmetrical growth retardation is especially apparent when comparing developing and developed countries. The rate of growth retardation in developing countries is 10 to 43%, and is primarily symmetrical, with the most important risk factor being poor nourishment. In developed countries foetal growth retardation is usually much lower, 3 to 8%, and is generally asymmetrical with a multifactorial aetiology. Hence, worldwide, the proportion of low birth-weight infants defined as intrauterine growth retarded rather than preterm varies dramatically. In Sweden and the United States, the proportion is approximately 45%, while in developing countries, such as India, the proportion varies between approximately 79 and 96% (Villar and Belizan 1982).
Studies of the Dutch famine showed that starvation confined to the third trimester depressed foetal growth in an asymmetric pattern, with birth weight being primarily affected and head circumference least affected (Stein, Susser and Saenger 1975). Asymmetry of growth also has been observed in studies of environmental exposures. In a study of 202 expectant mothers residing in neighbourhoods at high risk for lead exposures, prenatal maternal blood samples were collected between the sixth and the 28th week of gestation (Bornschein, Grote and Mitchell 1989). Blood lead levels were associated with both a decreased birth weight and length, but not head circumference, after adjustment for other relevant risk factors including length of gestation, socioeconomic status and use of alcohol or cigarettes. The finding of maternal blood lead as a factor in birth length was seen entirely in Caucasian infants. The birth length of Caucasian infants decreased approximately 2.5 cm per log unit increment in maternal blood lead. Care should be given to selection of the outcome variable. If only birth weight had been selected for study, the finding of the effects of lead on other growth parameters might have been missed. Also, if Caucasians and African Americans had been pooled in the above analysis, the differential effects on Caucasians, perhaps due to genetic differences in the storage and binding capacity of lead, may have been missed. A significant confounding effect also was observed between prenatal blood lead and maternal age and the birth weight of the offspring after adjustment for other covariables. The findings indicate that for a 30-year-old woman with an estimated blood lead level of about 20 mg/dl, the offspring weighed proximately 2,500 g compared with proximately 3,000 g for a 20-year-old with similar lead levels. The investigators speculated that this observed difference may indicate that older women are more sensitive to the additional insult of lead exposure or that older women may have had higher total lead burden from greater numbers of years of exposure or higher ambient lead levels when they were children. Another factor may be increased blood pressure. Nonetheless, the important lesson is that careful examination of high-risk subpopulations by age, race, economic status, daily living habits, sex of the offspring and other genetic differences may be necessary in order to discover the more subtle effects of exposures on foetal growth and development.
Risk factors associated with low birth weight are summarized in Table 5. Social class as measured by income or education persists as a risk factor in situations in which there are no ethnic differences. Other factors that may be operating under social class or race may include cigarette smoking, physical work, prenatal care and nutrition. Women between the ages of 25 and 29 are least likely to deliver a growth-retarded offspring. Maternal smoking increases the risk of low birth-weight offspring by about 200% for heavy smokers. Maternal medical conditions associated with LBW include placental abnormalities, heart disease, viral pneumonia, liver disease, re-eclamsia, eclamsia, chronic hypertension, weight gain and hyeremesis. An adverse pregnancy history of foetal loss, preterm delivery or prior LBW infant increases the risk of a current preterm low birth-weight infant two- to fourfold. An interval between births of less than a year triples the risk of having a low birth-weight offspring. Chromosomal anomalies associated with abnormal growth include Down’s syndrome, trisomy 18 and most malformation syndromes.
Smoking cigarettes is one of the primary behaviours most directly linked with lower weight offspring. Maternal smoking during pregnancy has been shown to increase the risk of a low birth-weight offspring two to three times and to cause an overall weight deficit of between 150 and 400 g. Nicotine and carbon monoxide are considered the most likely causative agents since both are rapidly and referentially transferred across the placenta. Nicotine is a powerful vasoconstrictor, and significant differences in the size of umbilical vessels of smoking mothers have been demonstrated. Carbon monoxide levels in cigarette smoke range from 20,000 to 60,000 m. Carbon monoxide has an affinity for haemoglobin 210 times that of oxygen, and because of lower arterial oxygen tension the foetus is especially compromised. Others have suggested that these effects are not due to smoking but are attributable to characteristics of smokers. Certainly occupations with potential carbon monoxide exposure, such as those associated with ul and aer, blast furnaces, acetylene, breweries, carbon black, coke ovens, garages, organic chemical synthesizers and petroleum refineries should be considered possible high risk occupations for pregnant employees.
Ethanol is also a widely used and researched agent associated with foetal growth retardation (as well as congenital anomalies). In a prospective study of 9,236 births, it was found that maternal alcohol consumption of more than 1.6 oz per day was associated with an increase in stillbirths and growth-retarded infants (Kaminski, Rumeau and Schwartz 1978). Smaller infant length and head circumference also are related to maternal alcohol ingestion.
In evaluating the possible effects of exposures on birth weight, some problematic issues must be considered. preterm delivery should be considered as a possible mediating outcome and the potential effects on gestational age considered. In addition, pregnancies having longer gestational length also have a longer opportunity for exposure. If enough women work late in pregnancy, the longest cumulative exposure may be associated with the oldest gestational ages and heaviest babies purely as an artifact. There are a number of procedures that can be used to overcome this problem including a variant of the Cox life-table regression model, which has the ability to handle time-dependent covariables.
Another problem centres on how to define lowered birth weight. Often studies define lower birth weight as a dichotomous variable, less than 2,500 g. The exposure, however, must have a very powerful effect in order to produce a drastic drop in the infant’s weight. Birth weight defined as a continuous variable and analysed in a multiple regression model is more sensitive for detecting subtle effects. The relative paucity of significant findings in the literature in relationship to occupational exposures and SGA infants may, in art, be caused by ignoring these design and analysis issues.
Conclusions
Studies of adverse pregnancy outcomes must characterize exposures during a fairly narrow window of time. If the woman has been transferred to another job or laid off work during a critical period of time such as organogenesis, the exposure-effect relationship can be severely altered. Therefore, the investigator is held to a high standard of identifying the woman’s exposure during a critical small time period as compared with other studies of chronic diseases, where errors of a few months or even years may have minimal impact.
Uterine growth retardation, congenital anomaly and spontaneous abortions are frequently evaluated in occupational exposure studies. There is more than one approach available to assess each outcome. These end-points are of public health importance due to both the psychological and the financial costs. Generally, nonsecificity in the exposure-outcome relationships has been observed, e.g., with exposure to lead, anaesthetic gases and solvents. Because of the potential for nonsecificity in the exposure-effect relationship, studies should be designed to assess several end-points associated with a range of possible mechanisms.
Preterm Delivery and Work
The reconciliation of work and maternity is an important public health issue in industrialized countries, where more than 50% of women of child-bearing age work outside the home. Working women, unions, employers, politicians and clinicians are all searching for ways of preventing work-induced unfavourable reproductive outcomes. Women want to continue working while pregnant, and may even consider their physician’s advice about lifestyle modifications during pregnancy to be overprotective and unnecessarily restrictive.
physiological Consequences of pregnancy
At this point, it would be useful to review a few of the physiological consequences of pregnancy that may interfere with work.
A pregnant woman undergoes profound changes which allow her to adapt to the needs of the foetus. Most of these changes involve the modification of physiological functions that are sensitive to changes of posture or physical activity—the circulatory system, the respiratory system and water balance. As a result, physically active pregnant women may experience unique physiological and physiopathological reactions.
The main physiological, anatomical, and functional modifications undergone by pregnant women are (Mamelle et al. 1982):
- An increase in peripheral oxygen demand, leading to modification of the respiratory and circulatory systems. Tidal volume begins to increase in the third month and may amount to 40% of re-pregnancy values by the end of the pregnancy. The resultant increase in gas exchange may increase the hazard of the inhalation of toxic volatiles, while hyperventilation related to increased tidal volume may cause shortness of breath on exertion.
- Cardiac output increases from the very beginning of pregnancy, as a result of an increase in blood volume. This reduces the heart’s ability to adapt to exertion and also increases venous pressure in the lower limbs, rendering standing for long periods difficult.
- Anatomical modifications during pregnancy, including exaggeration of dorsolumbar lordosis, enlargement of the polygon of support and increases in abdominal volume, affect static activities.
- A variety of other functional modifications occur during pregnancy. Nausea and vomiting result in fatigue; daytime sleepiness results in inattention; mood changes and feelings of anxiety may lead to interpersonal conflicts.
- Finally, it is interesting to note that the daily energy requirements during pregnancy are equivalent to the requirements of two to four hours of work.
Because of these profound changes, occupational exposures may have special consequences in pregnant women and may result in unfavourable pregnancy outcomes.
Epidemiological Studies of Working Conditions and preterm Delivery
Although there are many possible unfavourable pregnancy outcomes, we review here the data on preterm delivery, defined as the birth of a child before the 37th week of gestation. preterm birth is associated with low birth weight and with significant complications for the newborn. It remains a major public health concern and is an ongoing reoccupation among obstetricians.
When we began research in this field in the mid-1980s, there was relatively strong legislative protection of pregnant women’s health in France, with prenatal maternity leave mandated to start six weeks prior to the due date. Although the preterm delivery rate has fallen from 10 to 7% since then, it appeared to have levelled off. Because medical prevention had apparently reached the limit of its powers, we investigated risk factors likely to be amenable to social intervention. Our hypotheses were as follows:
- Is working per se a risk factor for preterm birth?
- Are certain occupations associated with an increased risk of preterm delivery?
- Do certain working conditions constitute a hazard to the pregnant woman and foetus?
- Are there social preventive measures which could help reduce the risk of preterm birth?
Our first study, conducted in 1977–78 in two hospital maternity wards, examined 3,400 women, of whom 1,900 worked during pregnancy and 1,500 remained at home (Mamelle, Laumon and Lazar 1984). The women were interviewed immediately after delivery and asked to describe their home and work lifestyle during pregnancy as accurately as possible.
We obtained the following results:
Work per se
The mere fact of working outside the home cannot be considered to be a risk factor for preterm delivery, since women remaining at home exhibited a higher prematurely rate than did women who worked outside the home (7.2 versus 5.8%).
Working conditions
An excessively long work week appears to be a risk factor, since there was a regular increase in preterm delivery rate with the number of work hours. Retail-sector workers, medical social workers, specialized workers and service personnel were at higher risk of preterm delivery than were office workers, teachers, management, skilled workers or supervisors. The prematurely rates in the two groups were 8.3 and 3.8% respectively.
Table 1. Identified sources of occupational fatigue
| Occupational fatigue index | “HIGH” index if: |
| Posture | Standing for more than 3 hours per day |
| Work on machines | Work on industrial conveyor belts; independent work on industrial machines with strenuous effort |
| Physical load | Continuous or periodical physical effort; carrying loads of more than 10kg |
| Mental load | Routine work; varied tasks requiring little attention without stimulation |
| Environment | Significant noise level; cold temperature; very wet atmosphere; handling of chemical substances |
Source: Mamelle, Laumon and Lazar 1984.
Task analysis allowed identification of five sources of occupation fatigue: posture, work with industrial machines, physical workload, mental workload and the work environment. Each of these sources of occupational fatigue constitutes a risk factor for preterm delivery (see tables 1 and 2).
Table 2. Relative risks (RR) and fatigue indices for preterm delivery
| Index | Low index % | High index % | RR | Statistical significance |
| Posture | 4.5 | 7.2 | 1.6 | Significant |
| Work on machines | 5.6 | 8.8 | 1.6 | Significant |
| Physical load | 4.1 | 7.5 | 1.8 | Highly significant |
| Mental load | 4.0 | 7.8 | 2.0 | Highly significant |
| Environment | 4.9 | 9.4 | 1.9 | Highly significant |
Source: Mamelle, Laumon and Lazar 1984.
Exposure to multiple sources of fatigue may result in unfavourable pregnancy outcomes, as evidenced by the significant increase of the rate of preterm delivery with an increased number of sources of fatigue (table 3). Thus, 20% of women had concomitant exposure to at least three sources of fatigue, and experienced a preterm delivery rate twice as high as other women. Occupational fatigue and excessively long work weeks exert cumulative effects, such that women who experience intense fatigue during long work weeks exhibit an even higher prematurely rate. preterm delivery rates increase further if the woman also has a medical risk factor. The detection of occupational fatigue is therefore even more important than the detection of medical risk factors.
Table 3. Relative risk of prematurity according to number of occupational fatigue indices
| Number of high fatigue indices |
Proportion of exposed women % |
Estimated relative risk |
| 0 | 24 | 1.0 |
| 1 | 28 | 2.2 |
| 2 | 25 | 2.4 |
| 3 | 15 | 4.1 |
| 4-5 | 8 | 4.8 |
Source: Mamelle, Laumon and Lazar 1984
European and North American studies have confirmed our results, and our fatigue scale has been shown to be reproducible in other surveys and countries.
In a case-control follow-u study conducted in France a few years later in the same maternity wards (Mamelle and Munoz 1987) , only two of the five previously defined indices of fatigue were significantly related to preterm delivery. It should however be noted that women had a greater opportunity to sit down and were withdrawn from physically demanding tasks as a result of preventive measures implemented in the workplaces during this period. The fatigue scale nevertheless remained a predictor of preterm delivery in this second study.
In a study in Montreal, Quebec (McDonald et al. 1988), 22,000 pregnant women were interviewed retrospectively about their working conditions. Long work weeks, alternating shift work and carrying heavy loads were all shown to exert significant effects. The other factors studied did not appear to be related to preterm delivery, although there appears to be a significant association between preterm delivery and a fatigue scale based on the total number of sources of fatigue.
With the exception of work with industrial machines, no significant association between working conditions and preterm delivery was found in a French retrospective study of a representative sample of 5,000 pregnant women (Saurel-Cubizolles and Kaminski 1987). However, a fatigue scale inspired by our own was found to be significantly associated with preterm delivery.
In the United States, Homer, Beredford and James (1990), in a historical cohort study, confirmed the association between physical workload and an increased risk of preterm delivery. Teitelman and co-workers (1990), in a prospective study of 1,200 pregnant women, whose work was classified as sedentary, active or standing, on the basis of job description, demonstrated an association between work in a standing position and preterm delivery.
Barbara Luke and co-workers (in press) conducted a retrospective study of US nurses who worked during pregnancy. Using our occupational risk scale, she obtained similar results to ours, that is, an association between preterm delivery and long work weeks, standing work, heavy workload and unfavourable work environment. In addition, the risk of preterm delivery was significantly higher among women with concomitant exposure to three or four sources of fatigue. It should be noted that this study included over half of all nurses in the United States.
Contradictory results have however been reported. These may be due to small sample sizes (Berkowitz 1981), different definitions of prematurely (Launer et al. 1990) and classification of working conditions on the basis of job description rather than actual workstation analysis (Klebanoff, Shiono and Carey 1990). In some cases, workstations have been characterized on a theoretical basis only—by the occupational physician, for example, rather than by the women themselves (peoples-Shes et al. 1991). We feel that it is important to take subjective fatigue—that is, fatigue as it is described and experienced by women—into account in the studies.
Finally, it is possible that the negative results are related to the implementation of preventive measures. This was the case in the prospective study of Ahlborg, Bodin and Hogstedt (1990), in which 3,900 active Swedish women completed a self-administered questionnaire at their first prenatal visit. The only reported risk factor for preterm delivery was carrying loads weighing more than 12 kg more often than 50 times per week, and even then the relative risk of 1.7 was not significant. Ahlborg himself points out that preventive measures in the form of aid maternity leave and the right to perform less tiring work during the two months receding their due date had been implemented for pregnant women engaged in tiring work. Maternity leaves were five times as frequent among women who described their work as tiring and involving the carrying of heavy loads. Ahlborg concludes that the risk of preterm delivery may have been minimized by these preventive measures.
preventive Interventions: French Examples
Are the results of aetiological studies convincing enough for preventive interventions to be applied and evaluated? The first question which must be answered is whether there is a public health justification for the application of social preventive measures designed to reduce the rate of preterm delivery.
Using data from our previous studies, we have estimated the proportion of preterm births caused by occupational factors. Assuming a rate of preterm delivery of 10% in populations exposed to intense fatigue and a rate of 4.5% in non-exposed populations, we estimate that 21% of premature births are caused by occupational factors. Reducing occupational fatigue could therefore result in the elimination of one-fifth of all preterm births in French working women. This is ample justification for the implementation of social preventive measures.
What preventive measures can be applied? The results of all the studies lead to the conclusion that working hours can be reduced, fatigue can be lessened through workstation modification, work breaks can be allowed and prenatal leave can be lengthened. Three cost-equivalent alternatives are available:
- reducing the work week to 30 hours starting from the 20th week of gestation
- prescribing a work break of one week each month starting in the 20th week of gestation
- beginning prenatal leave at the 28th week of gestation.
It is relevant to recall here that French legislation provides the following preventive measures for pregnant women:
- guaranteed employment after childbirth
- reduction of the workday by 30 to 60 minutes, applied through collective agreements
- workstation modification in cases of incompatibility with pregnancy
- work breaks during pregnancy, prescribed by attending physicians
- prenatal maternity leave six weeks prior to the due date, with a further two weeks available in case of complications
- postnatal maternity leave of ten weeks.
A one-year prospective observational study of 23,000 women employed in 50 companies in the Rhône-Ales region of France (Bertucat, Mamelle and Munoz 1987) examined the effect of tiring work conditions on preterm delivery. Over the period of the study, 1,150 babies were born to the study population. We analysed the modifications of working conditions to accommodate pregnancy and the relation of these modifications to preterm delivery (Mamelle, Bertucat and Munoz 1989), and observed that:
- Workstation modification was reformed for only 8% of women.
- 33% of women worked their normal shifts, with the others having their workday reduced by 30 to 60 minutes.
- 50% of women took at least one work break, apart from their prenatal maternity leave; fatigue was the cause in one-third of cases.
- 90% of women stopped working before their legal maternity leave began and obtained at least the two weeks leave allowed for in the case of complications of pregnancy; fatigue was the cause in half the cases.
- In all, given the legal prenatal leave period of six weeks prior to the due date (with an additional two weeks available in some cases), the real duration of prenatal maternity leave was 12 weeks in this population of women subjected to tiring work conditions.
Do these modifications of work have any effect on the outcome of pregnancy? Workstation modification and the slight reduction of the workday (30 to 60 min) were both associated with non-significant reductions of the risk of preterm delivery. We believe that further reductions of the work week would have a greater effect (table 4).
Table 4. Relative risks of prematurity associated with modifications in working conditions
| Modifications in working conditions |
Number of women | Preterm birth rates (%) |
Relative risk (95% confidence intervals) |
| Change in work situation | |||
| No Yes |
1,062 87 |
6.2 3.4 |
0.5 (0.2-1.6) |
| Reduction of weekly working hours | |||
| No Yes |
388 761 |
7.7 5.1 |
0.7 (0.4-1.1) |
| Episodes of sick leave1 | |||
| No Yes |
357 421 |
8.0 3.1 |
0.4 (0.2-0.7) |
| Increase of antenatal maternity leave1 | |||
| None or only additional 2 weeks Yes |
487 291 |
4.3 7.2 |
1.7 (0.9-3.0) |
1 In a reduced sample of 778 women with no previous or present obstetric pathology.
Source: Mamelle, Bertucat and Munoz 1989.
To analyse the relation between prenatal leave, work breaks and preterm delivery, it is necessary to discriminate between preventive and curative work breaks. This requires restriction of the analysis to women with uncomplicated pregnancies. Our analysis of this subgroup revealed a reduction of the preterm delivery rate among women who took work breaks during their pregnancy, but not in those who took prolonged prenatal leave (Table 9).
This observational study demonstrated that women who work in tiring conditions take more work breaks during their pregnancies than do other women, and that these breaks, particularly when motivated by intense fatigue, are associated with reductions of the risk of preterm delivery (Mamelle, Bertucat and Munoz 1989).
Choice of preventive Strategies in France
As epidemiologists, we would like to see these observations verified by experimental preventive studies. We must however ask ourselves which is more reasonable: to wait for such studies or to recommend social measures aimed at preventing preterm delivery now?
The French Government recently decided to include a “work and pregnancy guide”, identical to our fatigue scale, in each pregnant woman’s medical record. Women can thus calculate their fatigue score for themselves. If work conditions are arduous, they may ask the occupational physician or the person responsible for occupational safety in their company to implement modifications aimed at alleviating their workload. Should this be refused, they can ask their attending physician to prescribe rest weeks during their pregnancy, and even to prolong their prenatal maternity leave.
The challenge is now to identify preventive strategies that are well adapted to legislation and social conditions in every country. This requires a health economics approach to the evaluation and comparison of preventive strategies. Before any preventive measure can be considered generally applicable, many factors have to be taken into consideration. These include effectiveness, of course, but also low cost to the social security system, resultant job creation, women’s references and the acceptability to employers and unions.
This type of problem can be resolved using multicriteria methods such as the Electra method. These methods allow both the classification of preventive strategies on the basis of each of a series of criteria, and the weighting of the criteria on the basis of political considerations. Special importance can thus be given to low cost to the social security system or to the ability of women to choose, for example (Mamelle et al. 1986). While the strategies recommended by these methods vary depending on the decision makers and political options, effectiveness is always maintained from the public health standpoint.
Occupational and Environmental Exposures to the Newborn
Environmental hazards pose a special risk for infants and young children. Children are not “little adults”, either in the way they absorb and eliminate chemicals or in their response to toxic exposures. Neonatal exposures may have a greater impact because the body surface area is disproportionately large and metabolic capacity (or the ability to eliminate chemicals) is relatively underdeveloped. At the same time, the potential toxic effects are greater, because the brain, the lungs and the immune system are still developing during the early years of life.
Opportunities for exposure exist at home, in day care facilities and on playgrounds:
- Young children can absorb environmental agents from the air (by inhalation) or through the skin.
- Ingestion is a major route of exposure, especially when children begin to exhibit hand-to-mouth activity.
- Substances on the hair, clothes or hands of the parents can be transferred to the young child.
- Breast milk is another potential source of exposure for infants, although the potential benefits of nursing far outweigh the potential toxic effects of chemicals in breast milk.
For a number of the health effects discussed in connection with neonatal exposures, it is difficult to distinguish prenatal from postnatal events. Exposures taking lace before birth (through the placenta) can continue to be manifest in early childhood. Both lead and environmental tobacco smoke have been associated with deficits in cognitive development and lung function both before and after birth. In this review, we have attempted to focus on postnatal exposures and their effects on the health of very young children.
Lead and Other Heavy Metals
Among the heavy metals, lead (b) is the most important elemental exposure for humans in both environmental and occupational circumstances. Significant occupational exposures occur in battery manufacture, smelters, soldering, welding, construction and paint removal. parents employed in these industries have long been known to bring dust home on their clothes that can be absorbed by their children. The primary route of absorption by children is through ingestion of lead-contaminated paint chips, dust and water. Respiratory absorption is efficient, and inhalation becomes a significant exposure pathway if an aerosol of lead or alkyl lead is resent (Clement International Corporation 1991).
Lead poisoning can damage virtually every organ system, but current levels of exposure have been associated chiefly with neurological and developmental changes in children. In addition, renal and haematological disease have been observed among both adults and children intensely exposed to lead. Cardiovascular disease as well as reproductive dysfunction are known sequelae of lead exposure among adults. Subclinical renal, cardiovascular and reproductive effects are suspected to arise from lower, chronic lead exposure, and limited data support this idea. Animal data support human findings (Sager and Girard 1994).
In terms of measurable dose, neurological effects range from IQ deficits at low exposures (blood lead = 10 μg/dl) to enceha-loathy (80 μg/dl). Levels of concern in children in 1985 were 25 μg/dl, which was lowered to 10 μg/dl in 1993.
Neonatal exposure, as it resulted from dust brought home by working parents, was described as “fouling the nest” by Chisholm in 1978. Since that time, preventive measures, such as showering and changing clothing before leaving the workplace, have reduced the take-home dust burden. However, occupationally derived lead is still an important potential source of neonatal exposure today. A survey of children in Denmark found that blood lead was approximately twice as high among children of exposed workers than in homes with only non-occupational exposures (Grandjean and Bach 1986). Exposure of children to occupationally derived lead has been documented among electric cable splicers (Rinehart and Yanagisawa 1993) and capacitor manufacturing workers (Kaye, Novotny and Tucker 1987).
Non-occupational sources of environmental lead exposure continue to be a serious hazard to young children. Since the gradual ban of tetraethyl lead as a fuel additive in the United States (in 1978), average blood lead levels in children have declined from 13 to 3 μg/dl (Pirkle et al. 1994). paint chips and paint dust are now the principal cause of childhood lead poisoning in the United States (Roer 1991). For example in one report, younger children (neonates aged less than 11 months) with excessive lead in their blood were at greatest risk of exposure through dust and water while older children (aged 24 months) were at risk more from ingestion of paint chips (ica) (Shannon and Graef 1992). Lead abatement through paint removal has been successful in protecting children from exposure to dust and paint chips (Farfel, Chisholm and Rohde 1994). Ironically, workers engaged in this enterprise have been shown to carry lead dust home on their clothes. In addition, it has been noted that the continuing exposure of young children to lead disproportionately affects economically disadvantaged children (Brody et al. 1994; Goldman and Carra 1994). art of this inequity arises from the poor condition of housing; as early as 1982, it was shown that the extent of deterioration of housing was directly related to blood lead levels in children (Clement International Corporation 1991).
Another potential source of occupationally derived exposure for the neonate is lead in breast milk. Higher levels of lead in breast milk have been linked to both occupational and environmental sources (Ryu, Ziegler and Fomon 1978; Dabeka et al. 1986). The concentrations of lead in milk are small relative to blood (approximately 1/5 to 1/2) (Wolff 1993), but the large volume of breast milk ingested by an infant can add milligram quantities to the body burden. In comparison, there is normally less than 0.03 mg b in the circulating blood of an infant and the usual intake is less than 20 mg per day (Clement International Corporation 1991). Indeed, absorption from breast milk is reflected in the blood lead level of infants (Rabinowitz, Leviton and Needleman 1985; Ryu et al. 1983; Ziegler et al. 1978). It should be noted that normal lead levels in breast milk are not excessive, and lactation contributes an amount similar to that from other sources of infant nutrition. By comparison, a small paint chi could contain more than 10 mg (10,000 mg) of lead.
Developmental decrements in children have been linked with both prenatal and postnatal exposures to lead. prenatal exposure is thought to be responsible for lead-related deficits in mental and behavioural development that have been found in children until the age of two to four years (Landrigan and Cambell 1991; Bellinger et al. 1987). The effects of postnatal lead exposure, such as that experienced by the neonate from occupational sources, may be detected in children from ages two to six and even later. Among these are problem behaviour and lower intelligence (Bellinger et al. 1994). These effects are not confined only to high exposures; they have been observed at relatively low levels, e.g., where blood lead levels are in the range of 10 mg/dl (Needleman and Bellinger 1984).
Mercury (Hg) exposure from the environment may occur as inorganic and organic (mainly methyl) forms. Recent occupational exposures to mercury have been found among workers in thermometer manufacture and in repair of high-voltage equipment containing mercury. Other occupations with potential exposures include painting, dentistry, plumbing and chlorine manufacture (Agency for Toxic Substance and Disease Registry 1992).
prenatal and postnatal mercury poisoning has been well documented among children. Children are more susceptible to effects of methylmercury than adults. This is largely because the developing human central nervous system is so “remarkably sensitive” to methylmercury, an effect also seen at low levels in animals (Clarkson, Nordberg and Sager 1985). Methylmercury exposures in children arise chiefly from ingestion of contaminated fish or from breast milk, while elemental mercury is derived from occupational exposures. Household exposure incidental to occupational exposure has been noted (Zirschky and Wetherell 1987). Accidental exposures in the home have been reported in recent years in domestic industries (Meeks, Keith and Tanner 1990; Rowens et al. 1991) and in an accidental sill of metallic mercury (Florentine and Sanfilio 1991). Elemental mercury exposure occurs mainly by inhalation, while alkyl mercury can be absorbed by ingestion, inhalation or dermal contact.
In the best-studied episode of poisoning, sensory and motor dysfunction and mental retardation were found following very high exposures to methylmercury either in utero or from breast milk (Bakir et al. 1973). Maternal exposures resulted from ingestion of methylmercury that had been used as a fungicide on grain.
pesticides and Related Chemicals
Several hundred million tons of pesticides are produced worldwide each year. Herbicides, fungicides and insecticides are employed mainly in agriculture by developed countries to improve crop yield and quality. Wood preservatives are a much smaller, but still a major, art of the market. Home and garden use represents a relatively minor proportion of total consumption, but from the point of view of neonatal toxicity, domestic poisonings are perhaps the most numerous. Occupational exposure is also a potential source of indirect exposure to infants if a parent is involved in work that uses pesticides. Exposure to pesticides is possible through dermal absorption, inhalation and ingestion. More than 50 pesticides have been declared carcinogenic in animals (McConnell 1986).
Organochlorine pesticides include aromatic compounds, such as DDT (bis(4-chlorohenyl)-1,1,1-trichloroethane), and cyclodienes, such as dieldrin. DDT came into use in the early 1940s as an effective means to eliminate mosquitoes carrying malaria, an application that is still widely employed today in developing countries. Lindane is an organochlorine used widely to control body lice and in agriculture, especially in developing countries. olychlorinated bihenyls (CBs), another fat-soluble organochlorine mixture used since the 1940s, pose a potential health risk to young children exposed through breast milk and other contaminated foods. Both lindane and CBs are discussed separately in this chapter. olybrominated bihenyls (BBs) also have been detected in breast milk, almost exclusively in Michigan. Here, a fire-retardant inadvertently mixed into livestock feed in 1973-74 became widely dispersed across the state through dairy and meat products.
Chlordane has been used as a pesticide and as a termiticide in houses, where it is effective for decades, no doubt because of its persistence. Exposure to this chemical can be from dietary and direct respiratory or dermal absorption. Levels in human milk in Japan could be related both to diet and to how recently homes had been treated. Women living in homes treated more than two years earlier had chlordane levels in milk three times those of women living in untreated homes (Taguchi and Yakushiji 1988).
Diet is the main source of persistent organochlorines, but smoking, air and water may also contribute to exposure. This class of pesticides, also termed halogenated hydrocarbons, is quite persistent in the environment, since these are lipophilic, resistant to metabolism or biodegradation and exhibit low volatility. Several hundreds of m have been found in human and animal fat among those with highest exposures. Because of their reproductive toxicity in wildlife and their tendency to bioaccumulate, organochlorines have been largely banned or restricted in developed countries.
At very high doses, neurotoxicity has been observed with organochlorines, but potential long-term health effects are of more concern among humans. Although chronic health effects have not been widely documented, heatotoxicity, cancer and reproductive dysfunction have been found in experimental animals and in wildlife. Health concerns arise mainly from observations in animal studies of carcinogenesis and of profound changes in the liver and the immune system.
Organohoshates and carbamates are less persistent than the organochlorines and are the most widely used class of insecticides internationally. pesticides of this class are degraded relatively quickly in the environment and in the body. A number of the organohoshates and carbamates exhibit high acute neurotoxicity and in certain cases chronic neurotoxicity as well. Dermatitis is also a widely reported symptom of pesticide exposure.
The petroleum-based products used to apply some pesticides are also of potential concern. Chronic effects including haematooietic and other childhood cancers have been associated with parental or residential exposures to pesticides, but the epidemiological data are quite limited. Nevertheless, based on the data from animal studies, exposures to pesticides should be avoided.
For the newborn, a wide spectrum of exposure possibilities and toxic effects have been reported. Among children who required hospitalization for acute poisoning, most had inadvertently ingested pesticide products, while a significant number had been exposed while laying on sprayed carets (Casey, Thomson and Vale 1994; Zwiener and Ginsburg 1988). Contamination of workers’ clothing by pesticide dust or liquid has long been recognized. Therefore, this route provides ample opportunity for home exposures unless workers take proper hygienic precautions after work. For example, an entire family had elevated levels of chlordecone (Keone) in their blood, attributed to home laundering of a worker’s clothes (Grandjean and Bach 1986). Household exposure to TCDD (dioxin) has been documented by the occurrence of chloracne in the son and wife of two workers exposed in the aftermath of an explosion (Jensen, Sneddon and Walker 1972).
Most of the possible exposures to infants arise from pesticide applications within and around the home (Lewis, Fortmann and Camann 1994). Dust in home carets has been found to be extensively contaminated with numerous pesticides (Fenske et al. 1994). Much of reported home contamination has been attributed to flea extermination or to lawn and garden application of pesticides (Davis, Bronson and Garcia 1992). Infant absorption of chloryrifos after treatment of homes for fleas has been predicted to exceed safe levels. Indeed, indoor air levels following such fumigation procedures do not always rapidly diminish to safe levels.
Breast milk is a potential source of pesticide exposure for the neonate. Human milk contamination with pesticides, especially the organochlorines, has been known for decades. Occupational and environmental exposures can lead to significant pesticide contamination of breast milk (D’Ercole et al. 1976; McConnell 1986). Organochlorines, which in the past have been resent in breast milk at excessive levels, are declining in developed countries, paralleling the decline in adipose concentrations that has occurred after restriction of these compounds. Therefore, DDT contamination of human milk is now highest in developing countries. There is little evidence of organohoshates in breast milk. This may be attributable to properties of water solubility and raid metabolism of these compounds in the body.
Ingestion of water contaminated with pesticides is also a potential health risk for the neonate. This problem is most renounced where infant formula must be reared using water. Otherwise, commercial infant formulae are relatively free of contaminants (National Research Council 1993). Food contamination with pesticides may also lead to infant exposure. Contamination of commercial milk, fruits and vegetables with pesticides exists at very low levels even in developed countries where regulation and monitoring are most vigorous (The Referee 1994). Although milk comprises most of the infant diet, fruits (especially ales) and vegetables (especially carrots) are also consumed in a significant amount by young children and therefore represent a possible source of pesticide exposure.
In the industrialized countries, including the United States and western Europe, most of the organochlorine pesticides, including DDT, chlordane, dieldrin and lindane, have been either banned, suspended or restricted since the 1970s (Maxcy Rosenau-Last 1994). pesticides still used for agricultural and non-agricultural purposes are regulated in terms of their levels in foods, water and pharmaceutical products. As a result of this regulation, the levels of pesticides in adipose tissue and human milk have significantly declined over the past four decades. However, the organochlorines are still widely used in developing countries, where, for example, lindane and DDT are among the most frequently employed pesticides for agricultural use and for malaria control (Awumbila and Bokuma 1994).
Lindane
Lindane is the γ-isomer and active ingredient of the technical grade of benzene hexachloride (BHC). BHC, also known as hexachlorocyclohexane (HCH), contains 40 to 90% of other isomers— α, β and δ. This organochlorine has been used as an agricultural and non-agricultural pesticide throughout the world since 1949. Occupational exposures may occur during the manufacture, formulation and application of BHC. Lindane as a pharmaceutical reparation in creams, lotions and shampoos is also widely used to treat scabies and body lice. Because these skin conditions commonly occur among infants and children, medical treatment can lead to absorption of BHC by infants through the skin. Neonatal exposure can also occur by inhalation of vapour or dust that may be brought home by a parent or that may linger after home use. Dietary intake is also a possible means of exposure to infants since BHC has been detected in human milk, dairy products and other foods, as have many organochlorine insecticides. Exposure through breast milk was more prevalent in the United States prior to the ban on the commercial production of lindane. According to the IARC (International Agency for Research on Cancer 1987), it is possible that hexachlorocyclohexane is carcinogenic to humans. However, evidence for adverse health outcomes among infants has been reported chiefly as effects on the neurological and haematooietic systems.
Household exposure to lindane has been described in the wife of a pesticide formulator, demonstrating the potential for similar neonatal exposures. The wife had 5 ng/ml of γ-BHC in her blood, a concentration lower than that of her husband (table 1) (Starr et al. 1974). presumably, γ-BHC was brought into the home on the body and/or clothes of the worker. Levels of γ-BHC in the woman and her husband were higher than those reported in children treated with lotion containing 0.3 to 1.0% BHC.
BHC in breast milk exists mainly as the β-isomer (Smith 1991). The half-life of the γ-isomer in the human body is approximately one day, while the β-isomer accumulates.
Table 1. Potential sources and levels of exposure to newborns
| Source of exposure | g-BHC in blood (ng/ml; ppb) |
|
| Occupational exposures | Low exposures High exposures |
5 36 |
| Adult male | Attempted suicide | 1300 |
| Child | Acute poisoning | 100-800 |
| Children | 1% BHC lotion (average) | 13 |
| Case report of home exposure1 | Husband Wife |
17 5 |
| Unexposed populations since1980 | Yugoslavia Africa Brazil India |
52 72 92 752 |
1Starr et al. (1974); other data from Smith (1991).
2Largely b-isomer.
Dermal absorption of lindane from pharmaceutical products is a function of the amount applied to the skin and duration of exposure. Compared with adults, infants and young children appear to be more susceptible to the toxic effects of lindane (Clement International Corporation 1992). One reason may be that dermal absorption is enhanced by increased permeability of the infant’s skin and a large surface-to-volume ratio. Levels in the neonate may persist longer because the metabolism of BHC is less efficient in infants and young children. In addition, exposure in neonates may be increased by licking or mouthing treated areas (Kramer et al. 1990). A hot shower or bath before dermal application of medical products may facilitate dermal absorption, thereby exacerbating toxicity.
In a number of reported cases of accidental lindane poisoning, overt toxic effects have been described, some in young children. In one case, a two-month-old infant died after multiple exposures to 1% lindane lotion, including a full-body application following a hot bath (Davies et al. 1983).
Lindane production and use is restricted in most developed countries. Lindane is still used extensively in other countries for agricultural purposes, as noted in a study of pesticide use on farms in Ghana, where lindane accounted for 35 and 85% of pesticide use for farmers and herdsmen, respectively (Awumbila and Bokuma 1994).
olychlorinated bihenyls
olychlorinated bihenyls were used from the mid-1940s until the late 1970s as insulating fluids in electrical capacitors and transformers. Residues are still resent in the environment because of pollution, which is due largely to improper disposal or accidental sills. Some equipment still in use or stored remains a potential source of contamination. An incident has been reported in which children had detectable levels of CBs in their blood following exposure while laying with capacitors (Wolff and Schecter 1991). Exposure in the wife of an exposed worker has also been reported (Fishbein and Wolff 1987).
In two studies of environmental exposures, re- and postnatal exposure to CBs has been associated with small but significant effects in children. In one study, slightly impaired motor development was detected among children whose mothers had immediate postnatal breast milk CB levels in the upper 95th percentile of the study group (Rogan et al. 1986). In the other, sensory deficits (as well as smaller gestational size) were seen among children with blood levels in approximately the to 25% (Jacobson et al. 1985; Fein et al. 1984). These exposure levels were in the upper range for the studies (above 3 m in mother’s milk (fat basis) and above 3 ng/ml in children’s blood), yet these are not excessively high. Common occupational exposures result in levels ten to 100 times higher (Wolff 1985). In both studies, effects were attributed to prenatal exposure. Such results however sound a cautionary note for unduly exposing neonates to such chemicals both pre- and postnatally.
Solvents
Solvents are a group of volatile or semi-volatile liquids that are used mainly to dissolve other substances. Exposure to solvents can occur in manufacturing processes, for example hexane exposure during distillation of petroleum products. For most persons, exposures to solvents will arise while these are being used on the job or in the home. Common industrial applications include dry cleaning, degreasing, painting and paint removal, and printing. Within the home, direct contact with solvents is possible during use of products such as metal cleaners, dry cleaning products, paint thinners or sprays.
The major routes of exposure for solvents in both adults and infants are through respiratory and dermal absorption. Ingestion of breast milk is one means of neonatal exposure to solvents derived from the parent’s work. Because of the brief half-life of most solvents, their duration in breast milk will be similarly short. However, following maternal exposure, some solvents will be resent in breast milk at least for a short time (at least one half-life). Solvents that have been detected in breast milk include tetrachloroethylene, carbon disulhide and halothane (an anaesthetic). A detailed review of potential infant exposure to tetrachloroethylene (TCE) has concluded that levels in breast milk can easily exceed recommended health risk guidelines (Schreiber 1993). Excess risk was highest for infants whose mothers might be exposed in the workplace (58 to 600 per million persons). For the highest non-occupational exposures, excess risks of 36 to 220 per 10 million persons were estimated; such exposures can exist in homes directly above dry-cleaners. It was further estimated that milk concentrations of TCE would return to “normal” (re-exposure) levels four to eight weeks after cessation of exposure.
Non-occupational exposures are possible for the infant in the home where solvents or solvent-based products are used. Indoor air has very low, but consistently detectable, levels of solvents like tetrachloroethylene. Water may also contain volatile organic compounds of the same type.
Mineral Dusts and Fibres: Asbestos, Fibreglass, Rock Wool, Zeolites, Talc
Mineral dust and fibre exposure in the workplace causes respiratory disease, including lung cancer, among workers. Dust exposure is a potential problem for the newborn if a parent carries articles into the home on the clothes or body. With asbestos, fibres from the workplace have been found in the home environment, and resulting exposures of family members have been termed bystander or family exposures. Documentation of familial asbestos disease has been possible because of the occurrence of a signal tumour, mesothelioma, that is primarily associated with asbestos exposure. Mesothelioma is a cancer of the leura or eritoneum (linings of lung and abdomen, respectively) that occurs following a long latency period, typically 30 to 40 years after the first asbestos exposure. The aetiology of this disease appears to be related only to the length of time after initial exposure, not to intensity or duration, nor to age at first exposure (Nicholson 1986; Otte, Sigsgaard and Kjaerulff 1990). Respiratory abnormalities have also been attributed to bystander asbestos exposure (Grandjean and Bach 1986). Extensive animal experiments support the human observations.
Most cases of familial mesothelioma have been reported among wives of exposed miners, millers, manufacturers and insulators. However, a number of childhood exposures have also been associated with disease. Quite a few of these children had initial contact that occurred at an early age (Dawson et al. 1992; Anderson et al. 1976; Roggli and Longo 1991). For example, in one investigation of 24 familial contacts with mesothelioma who lived in a crocidolite asbestos mining town, seven cases were identified whose ages were 29 to 39 years at diagnosis or death and whose initial exposure had occurred at less than one year of age (n=5) or at three years (n=2) (Hansen et al. 1993).
Exposure to asbestos is clearly causative for mesothelioma, but an epigenetic mechanism has been further pro[osed to account for unusual clustering of cases within certain families. Thus, the occurrence of mesothelioma among 64 persons in 27 families suggests a genetic trait that may render certain individuals more sensitive to the asbestos insult leading to this disease (Dawson et al. 1992; Bianchi, Brollo and Zuch 1993). However, it also has been suggested that exposure alone may provide an adequate explanation for the reported familial aggregation (Alderson 1986).
Other inorganic dusts associated with occupational disease include fibreglass, zeolites and talc. Both asbestos and fibreglass have been widely used as insulating materials. pulmonary fibrosis and cancer are associated with asbestos and much less clearly with fibreglass. Mesothelioma has been reported in areas of Turkey with indigenous exposures to natural zeolites. Exposures to asbestos may also arise from non-occupational sources. Diaers (“naies”) constructed from asbestos fibre were implicated as a source of childhood asbestos exposure (Li, Dreyfus and Antman 1989); however, parental clothing was not excluded as a source of asbestos contact in this report. Asbestos also has been found in cigarettes, hairdryers, floor tiles and some types of talcum powder. Its use has been eliminated in many countries. However, an important consideration for children is residual asbestos insulation in schools, which has been widely investigated as a potential public health problem.
Environmental Tobacco Smoke
Environmental tobacco smoke (ETS) is a combination of exhaled smoke and smoke emitted from the smoldering cigarette. Although ETS is not itself a source of occupational exposure that may affect the neonate, it is reviewed here because of its potential to cause adverse health effects and because it provides a good example of other aerosol exposures. Exposure of a non-smoker to ETS is often described as passive or involuntary smoking. prenatal exposure to ETS is clearly associated with deficits or impairments in foetal growth. It is difficult to distinguish postnatal outcomes from effects of ETS in the prenatal period, since parental smoking is rarely confined to one time or the other. However, there is evidence to support a relationship of postnatal exposure to ETS with respiratory illness and impaired lung function. The similarity of these findings to experiences among adults strengthens the association.
ETS has been well characterized and extensively studied in terms of human exposure and health effects. ETS is a human carcinogen (US Environmental protection Agency 1992). ETS exposure can be assessed by measuring levels of nicotine, a component of tobacco, and cotinine, its major metabolite, in biological fluids including saliva, blood and urine. Nicotine and cotinine have also been detected in breast milk. Cotinine has also been found in the blood and urine of infants who were exposed to ETS only by breast-feeding (Charlton 1994; National Research Council 1986).
Exposure of the neonate to ETS has been clearly established to result from paternal and maternal smoking in the home environment. Maternal smoking provides the most significant source. For example, in several studies urinary cotinine in children has been shown to correlate with the number of cigarettes smoked by the mother per day (Marbury, Hammon and Haley 1993). The major routes of ETS exposure for the neonate are respiratory and dietary (through breast milk). Day care centers represent another potential exposure situation; many child care facilities do not have a no-smoking policy (Sockrider and Coultras 1994).
Hospitalization for respiratory illness occurs more often among newborns whose parents smoke. In addition, the duration of hospital visits is longer among infants exposed to ETS. In terms of causation, ETS exposure has not been associated with specific respiratory diseases. There is evidence, however, that passive smoking increases the severity of re-existing illnesses such as bronchitis and asthma (Charlton 1994; Chilmonczyk et al. 1993; Rylander et al. 1993). Children and infants exposed to ETS also have higher frequencies of respiratory infections. In addition, smoking parents with respiratory illnesses can transmit airborne infections to infants by coughing.
Children exposed to ETS postnatally show small deficits in lung function which appear to be independent of prenatal exposures (Frischer et al. 1992). Although the ETS-related changes are small (0.5% decrement per year of forced expiratory volume), and while these effects are not clinically significant, they suggest changes in the cells of the developing lung that may portend later risk. parental smoking has also been associated with increased risk of otitis media, or middle ear effusion, in children from infancy to age nine. This condition is a common cause of deafness among children which can cause delays in educational progress. Associated risk is supported by studies attributing one-third of all cases of otitis media to parental smoking (Charlton 1994).
Radiation Exposures
Ionizing radiation exposure is an established health hazard which is generally the result of intense exposure, either accidental or for medical purposes. It can be damaging to highly proliferative cells, and can therefore be very harmful to the developing foetus or neonate. Radiation exposures that result from diagnostic x rays are generally very low level, and considered to be safe. A potential household source of exposure to ionizing radiation is radon, which exists in certain geographic areas in rock formations.
prenatal and postnatal effects of radiation include mental retardation, lower intelligence, growth retardation, congenital malformations and cancer. Exposure to high doses of ionizing radiation is also associated with increased prevalence of cancer. Incidence for this exposure is dependent upon dose and age. In fact, the highest relative risk observed for breast cancer (~9) is among women who were exposed to ionizing radiation at a young age.
Recently, attention has focused on the possible effects of non-ionizing radiation, or electromagnetic fields (EMF). The basis of a relationship between EMF exposure and cancer is not yet known, and the epidemiological evidence is still unclear. However, in several international studies an association has been reported between EMF and leukaemia and male breast cancer.
Childhood exposure to excessive sunlight has been associated with skin cancer and melanoma (Marks 1988).
Childhood Cancer
Although specific substances have not been identified, parental occupational exposures have been linked to childhood cancer. The latency period for developing childhood leukaemia can be two to 10 years following the onset of exposure, indicating that exposures in utero or in the early postnatal period may be implicated in the cause of this disease. Exposure to a number of organochlorine pesticides (BHC, DDT, chlordane) has been tentatively associated with leukaemia, although these data have not been confirmed in more detailed studies. Moreover, elevated risk of cancer and leukaemia has been reported for children whose parents engage in work that involves pesticides, chemicals and fumes (O’Leary et al. 1991). Similarly, risk of Ewing’s bone sarcoma in children was associated with parental occupations in agriculture or exposure to herbicides and pesticides (Holly et al. 1992).
Summary
Many nations attempt to regulate safe levels of toxic chemicals in ambient air and food products and in the workplace. Nevertheless, opportunities for exposure abound, and children are particularly susceptible to both absorption and to effects of toxic chemicals. It has been noted that “many of the 40,000 child lives lost in the developing world every day are a consequence of environmental abuses reflected in unsafe water supplies, disease, and malnutrition” (Schaefer 1994). Many environmental exposures are avoidable. Therefore, prevention of environmental diseases takes high priority as a defence against adverse health effects among children.
Maternity Protection in Legislation
During pregnancy, exposure to certain health and safety hazards of the job or the working environment may have adverse effects on the health of a woman worker and her unborn child. Before and after giving birth, she also needs a reasonable amount of time off from her job to recuperate, breast-feed and bond with her child. Many women want and need to be able to return to work after childbirth; this is increasingly recognized as a basic right in a world where the participation of women in the labour force is continuously increasing and approaching that of men in many countries. As most women need to support themselves and their families, continuity of income during maternity leave is vital.
Over time, governments have enacted a range of legislative measures to protect women workers during pregnancy and at childbirth. A feature of more recent measures is the prohibition of discrimination in employment on the grounds of pregnancy. Another trend is to provide the right for mothers and fathers to share leave entitlements after the birth so that either may care for the child. Collective bargaining in many countries contributes to the more effective application of such measures and often improves upon them. Employers also lay an important role in furthering maternity protection through the terms of individual contracts of employment and enterprise policies.
The Limits of Protection
Laws providing maternity protection for working women are usually restricted to the formal sector, which may represent a small proportion of economic activity. These do not apply to women working in unregistered economic activities in the informal sector, who in many countries represent the majority of working women. While there is a trend worldwide to improve and extend maternity protection, how to protect the large segment of the population living and working outside the formal economy remains a major challenge.
In most countries, labour legislation provides maternity protection for women employed in industrial and non-industrial enterprises in the private and often also the public sector. Homeworkers, domestic employees, own-account workers and workers in enterprises employing only family members are frequently excluded. Since many women work in small firms, the relatively frequent exclusion of undertakings which employ less than a certain number of workers (e.g., five permanent workers in the Republic of Korea) is of concern.
Many women workers in precarious employment, such as temporary workers, or casual workers in Ireland, are excluded from the scope of labour legislation in a number of countries. Depending on the number of hours they work, part-time workers may also be excluded. Other groups of women may be excluded, such as women managers (e.g., Singapore, Switzerland), women whose earnings exceed a certain maximum (e.g., Mauritius) or women who are paid by results (e.g., the Philippines). In rare cases, unmarried women (e.g., teachers in Trinidad and Tobago) do not qualify for maternity leave. However, in Australia (federal), where parental leave is available to employees and their spouses, the term “spouse” is defined to include a de facto spouse. Where age limits are set (e.g., in Israel, women below the age of 18) they usually do not exclude very many women as they are normally fixed below or above the prime child-bearing ages.
Public servants are often covered by special rules, which may provide for more favourable conditions than those applicable to the private sector. For example, maternity leave may be longer, cash benefits may correspond to the full salary instead of a percentage of it, parental leave is more likely to be available, or the right to reinstatement may be more clearly established. In a significant number of countries, conditions in the public service can act as an agent of progress since collective bargaining agreements in the private sector are often negotiated along the lines of public service maternity protection rules.
Similar to labour legislation, social security laws may limit their application to certain sectors or categories of workers. While this legislation is often more restrictive than the corresponding labour laws in a country, it may provide access to maternity cash benefits to groups not covered by labour laws, such as self-employed women or women who work with their self-employed husbands. In many developing countries, owing to a lack of resources, social security legislation may only apply to a limited number of sectors.
Over the decades, however, the coverage of legislation has been extended to more economic sectors and categories of workers. Yet, while an employee may be covered by a law, the enjoyment of certain benefits, in particular maternity leave and cash benefits, may depend on certain eligibility requirements. Thus, while most countries protect maternity, working women do not enjoy a universal right to such protection.
Maternity Leave
Time off work for childbirth can vary from a few weeks to several months, often divided into two parts, before and after the birth. A period of employment prohibition may be stipulated for a part or the whole of the entitlement to ensure that women have sufficient rest. Maternity leave is commonly extended in case of illness, preterm or late birth, and multiple births, or shortened in case of miscarriage, stillbirth or infant death.
Normal duration
Under the ILO’s Maternity protection Convention, 1919 (No. 3), “a woman shall not be permitted to work during the six weeks following her confinement; [and] shall have the right to leave her work if she produces a medical certificate stating that her confinement will probably take lace within six weeks”. The Maternity protection Convention (Revised), 1952 (No. 103), confirms the 12-week leave, including an employment prohibition for six weeks after the birth, but does not prescribe the use of the remaining six weeks. The Maternity protection Recommendation, 1952 (No. 95), suggests a 14-week leave. The Maternity protection Recommendation, 2000 (No. 191) suggests a 18-week leave [Edited, 2011]. Most of the countries surveyed meet the 12-week standard, and at least one-third grant longer periods.
A number of countries afford a possibility of choice in the distribution of maternity leave. In some, the law does not prescribe the distribution of maternity leave (e.g., Thailand), and women are entitled to start the leave as early or as late as they wish. In another group of countries, the law indicates the number of days to be taken after confinement; the balance can be taken either before or after the birth.
Other countries do not allow flexibility: the law provides for two periods of leave, before and after confinement. These periods may be equal, especially where the total leave is relatively short. Where the total leave entitlement exceeds 12 weeks, the prenatal period is often shorter than the postnatal period (e.g., in Germany six weeks before and eight weeks after the birth).
In a relatively small number of countries (e.g., Benin, Chile, Italy), the employment of women is prohibited during the whole period of maternity leave. In others, a period of compulsory leave is prescribed, often after confinement (e.g., Barbados, Ireland, India, Morocco). The most common requirement is a six-week compulsory period after birth. Over the past decade, the number of countries providing for some compulsory leave before the birth has increased. On the other hand, in some countries (e.g., Canada) there is no period of compulsory leave, as it is felt that the leave is a right that should be freely exercised, and that time off should be organized to suit the individual woman’s needs and preferences.
Eligibility for maternity leave
The legislation of most countries recognizes the right of women to maternity leave by stating the amount of leave to which women are entitled; a woman needs only to be employed at the time of going on leave to be eligible for the leave. In a number of countries, however, the law requires women to have been employed for a minimum period prior to the date on which they absent themselves. This period ranges from 13 weeks in Ontario or Ireland to two years in Zambia.
In several countries, women must have worked a certain number of hours in the week or month to be entitled to maternity leave or benefits. When such thresholds are high (as in Malta, 35 hours per week), they can result in excluding a large number of women, who form the majority of part-time workers. In a number of countries, however, thresholds have been lowered recently (e.g., in Ireland, from 16 to eight hours per week).
A small number of countries limit the number of times a woman may request maternity leave over a given period (for example two years), or restrict eligibility to a certain number of pregnancies, either with the same employer or throughout the woman’s life (e.g., Egypt, Malaysia). In Zimbabwe, for example, women are eligible for maternity leave once in every 24 months and for a maximum of three times during the period that they work for the same employer. In other countries, the women who have more than the prescribed number of children are eligible for maternity leave, but not for cash benefits (e.g., Thailand), or are eligible for a shorter period of leave with benefits (e.g., Sri Lanka: 12 weeks for the first two children, six weeks for the third and subsequent children). The number of countries that limit eligibility for maternity leave or benefits to a certain number of pregnancies, children or surviving children (between two and four) appears to be growing, although it is by no means certain that the duration of maternity leave is a decisive factor in motivating decisions about family size.
Advance notice to the employer
In most countries, the only requirement for women to be entitled to maternity leave is the presentation of a medical certificate. Elsewhere, women are also required to give their employer notice of their intention to take maternity leave. The period of notice ranges from as soon as the pregnancy is known (e.g., Germany) to one week before going on leave (e.g., Belgium). Failure to meet the notice requirement may lose women their right to maternity leave. Thus, in Ireland, information regarding the timing of maternity leave is to be supplied as soon as reasonably practicable, but not later than four weeks before the commencement of the leave. An employee loses her entitlement to maternity leave if she fails to satisfy this requirement. In Canada (federal), the notice requirement is waived where there is a valid reason why the notice cannot be given; at provincial level, the notice period ranges from four months to two weeks. If the notice period is not complied with, a woman worker is still entitled to the normal maternity leave in Manitoba; she is entitled to shorter periods (usually six weeks as opposed to 17 or 18) in most other provinces. In other countries, the law does not clarify the consequences of failing to give notice.
Cash Benefits
Most women cannot afford to forfeit their income during maternity leave; if they had to, many would not use all their leave. Since the birth of healthy children benefits the whole nation, as a matter of equity, employers should not bear the full cost of their workers’ absences. Since 1919, ILO standards have held that during maternity leave, women should receive cash benefits, and that these should be paid out of public funds or through a system of insurance. Convention No. 103 requires that contributions due under a compulsory social insurance scheme be paid based on the total number of men and women employed by the undertakings concerned, without distinction based on sex. Although in a few countries, maternity benefits represent only a relatively small percentage of wages, the level of two-thirds called for in Convention No. 103 is reached in several and exceeded in many others. In more than half of the countries surveyed, maternity benefits constitute 100% of insured wages or of full wages.
Many social security laws may provide a specific maternity benefit, thus recognizing maternity as a contingency in its own right. Others provide that during maternity leave, a worker will be entitled to sickness or unemployment benefits. Treating maternity as a disability or the leave as a period of unemployment could be considered unequal treatment since, in general, such benefits are only available during a certain period, and women who use them in connection with maternity may find they do not have enough left to cover actual sickness or unemployment periods later. Indeed, when the 1992 European Council Directive was drafted, a proposal that during maternity leave women would receive sickness benefits was strongly challenged; it was argued that in terms of equal treatment between men and women, maternity needed to be recognized as independent grounds for obtaining benefits. As a compromise, the maternity allowance was defined as guaranteeing an income at least equivalent to what the worker concerned would receive in the event of sickness.
In nearly 80 of the countries surveyed, benefits are paid by national social security schemes, and in over 40, these are at the expense of the employer. In about 15 countries, the responsibility for financing maternity benefits is shared between social security and the employer. Where benefits are financed jointly by social security and the employer, each may be required to pay half (e.g., Costa Rica), although other percentages may be found (e.g., Honduras: two-thirds by social security and one-third by the employer). Another type of contribution may be required of employers: when the amount of maternity benefit paid by social security is based on a statutory insurable income and represents a low percentage of a woman’s full wage, the law sometimes provides that the employer will pay the balance between the woman’s salary and the maternity benefit paid by the social security fund (e.g., in Burkina Faso). Voluntary additional payment by the employer is a feature of many collective agreements, and also of individual employment contracts. The involvement of employers in the payment of cash maternity benefits may be a realistic solution to the problem posed by the lack of other funds.
Protection of the Health of Pregnant and Nursing Women
In line with the requirements of the Maternity protection Recommendation, 1952 (No. 95), many countries provide for various measures to protect the health of pregnant women and their children, seeking to minimize fatigue by the reorganization of working time or to protect women against dangerous or unhealthy work.
In a few countries (e.g., the Netherlands, Panama), the law specifies an obligation of the employer to organize work so that it does not affect the outcome of the pregnancy. This approach, which is in line with modern occupational health and safety practice, permits matching the needs of individual women with the corresponding preventive measures, and is therefore most satisfactory. Much more generally, protection is sought through prohibiting or limiting work which may be harmful to the health of the mother or child. Such a prohibition may be worded in general terms or may apply to certain types of hazardous work. However, in Mexico, the prohibition of employing women in unhealthy or dangerous work does not apply if the necessary health protection measures have, in the opinion of the competent authority, been taken; nor does it apply to women in managerial positions or those who possess a university degree or technical diploma, or the necessary knowledge and experience to carry on the work.
In many countries, the law provides that pregnant women and nursing mothers may not be allowed to do work that is “beyond their strength”, which “involves hazards”, “is dangerous to their health or that of their child”, or “requires a physical effort unsuited to their condition”. The application of such a general prohibition, however, can present problems: how, and by whom, shall it be determined that a job is beyond a person’s strength? By the worker concerned, the employer, the labour inspector, the occupational health physician, the woman’s own doctor? Differences in appreciation might lead to a woman being kept away from work which she could in fact do, while another might not be removed from work which is too taxing.
Other countries list, sometimes in great detail, the type of work that is prohibited to pregnant women and nursing mothers (e.g., Austria, Germany). The handling of loads is frequently regulated. Legislation in some countries specifically prohibits exposure to certain chemicals (e.g., benzene), biological agents, lead and radiation. Underground work is prohibited in Japan during pregnancy and one year after confinement. In Germany, piece-rate work and work on an assembly line with a fixed pace are prohibited. In a few countries, pregnant workers may not be assigned to work outside their permanent place of residence (e.g., Ghana, after the fourth month). In Austria, smoking is not permitted in places where pregnant women are working.
In a number of countries (e.g., Angola, Bulgaria, Haiti, Germany), the employer is required to transfer the worker to suitable work. Often, the worker must retain her former salary even if the salary of the post to which she is transferred is lower. In the Lao people’s Democratic Republic, the woman keeps her former salary during a three-month period, and is then paid at the rate corresponding to the job she is actually performing. In the Russian Federation, where a suitable post is to be given to a woman who can no longer perform her work, she retains her salary during the period in which a new post is found. In certain cases (e.g., Romania), the difference between the two salaries is paid by social security, an arrangement which is to be referred, since the cost of maternity protection should not, as far as feasible, be borne by individual employers.
Transfer may also be available from work that is not dangerous in itself but which a medical practitioner has certified to be harmful to a particular woman’s state of health (e.g., France). In other countries, a transfer is possible at the request of the worker concerned (e.g., Canada, Switzerland). Where the law enables the employer to suggest a transfer, if there is a disagreement between the employer and the worker, an occupational physician will determine whether there is any medical need for changing jobs and whether the worker is fit to take up the job that has been suggested to her.
A few countries clarify the fact that the transfer is temporary and that the worker must be reassigned to her former job when she returns from maternity leave or at a specified time thereafter (e.g., France). Where a transfer is not possible, some countries provide that the worker will be granted sick leave (e.g., Seychelles) or, as was discussed above, that maternity leave will start early (e.g., Iceland).
Non-discrimination
Measures are taken in a growing number of countries to ensure that women do not suffer discrimination on account of pregnancy. Their aim is to ensure that pregnant women are considered for employment and treated during employment on an equal basis with men and with other women, and in particular are not demoted, do not lose seniority or are not denied promotion solely on the grounds of pregnancy. It is now more and more common for national legislation to prohibit discrimination on account of sex. Such a prohibition could be and indeed has been in many cases interpreted by the courts as a prohibition to discriminate on account of pregnancy. The European Court of Justice has followed this approach. In a 1989 judgement, the Court ruled that an employer who dismisses or refuses to recruit a woman because she is pregnant is in breach of Directive 76/207/EEC of the European Council on equal treatment. This judgement was important in clarifying the fact that sex discrimination exists when employment decisions are made on the basis of pregnancy even though the law does not specifically cite pregnancy as prohibited grounds for discrimination. It is customary in sex equality cases to compare the treatment given to a woman with the treatment given to a hypothetical man. The Court ruled that such comparison was not called for in the case of a pregnant woman, since pregnancy was unique to women. Where unfavourable treatment is made on grounds of pregnancy, there is by definition discrimination on grounds of sex. This is consistent with the position of the ILO Committee of Exerts on the Application of Conventions and Recommendations concerning the scope of the Discrimination (Employment and Occupation) Convention, 1958 (No. 111), which notes the discriminatory nature of distinctions on the basis of pregnancy, confinement and related medical conditions (ILO 1988).
A number of countries provide for an explicit prohibition of discrimination on the grounds of pregnancy (e.g., Australia, Italy, US, Venezuela). Other countries define discrimination on grounds of sex to include discrimination on grounds of pregnancy or absence on maternity leave (e.g., Finland). In the US, protection is further ensured through treating pregnancy as a disability: in undertakings with more than 15 workers, discrimination is prohibited against pregnant women, women at childbirth and women who are affected by related medical conditions; and policies and practices in connection with pregnancy and related matters must be applied on the same terms and conditions as applied to other disabilities.
In several countries, the law contains precise requirements which illustrate instances of discrimination on the grounds of pregnancy. For example, in the Russian Federation, an employer may not refuse to hire a woman because she is pregnant; if a pregnant woman is not hired, the employer must state in writing the reasons for not recruiting her. In France, it is unlawful for an employer to take pregnancy into account in refusing to employ a woman, in terminating her contract during a period of probation or in ordering her transfer. It is also unlawful for the employer to seek to determine whether an applicant is pregnant, or to cause such information to be sought. Similarly, women cannot be required to reveal the fact that they are pregnant, whether they apply for a job or are employed in one, except when they request to benefit from any law or regulation governing the protection of pregnant women.
Transfers unilaterally and arbitrarily imposed on a pregnant woman can constitute discrimination. In Bolivia, as in other countries in the region, a woman is protected against involuntary transfer during pregnancy and up to a year after the birth of her child.
The issue of combining the right of working women to health protection during pregnancy and their right not to suffer discrimination poses a special difficulty at the time of recruitment. Should a pregnant applicant reveal her condition, especially one who applies for a position involving work which is prohibited to pregnant women? In a 1988 judgement, the Federal Labour Court of Germany held that a pregnant woman applying for a job involving exclusively night work, which is prohibited to pregnant women under German legislation, should inform a potential employer of her condition. The judgement was overruled by the European Court of Justice as being contrary to the 1976 EC Directive on equal treatment. The Court found that the Directive precluded an employment contract from being held to be void on account of the statutory prohibition of night work, or from being avoided by the employer on account of a mistake on his or her part as to an essential personal characteristic of the woman at the time of the conclusion of the contract. The employee’s inability, due to pregnancy, to perform the work for which she was being recruited was temporary since the contract was not concluded with a fixed term. It would therefore be contrary to the objective of the Directive to hold it invalid or void because of such an inability.
Employment Security
Many women have lost their jobs because of a pregnancy. Nowadays, although the extent of protection varies, employment security is a significant component of maternity protection policies.
International labour standards address the issue in two different ways. The maternity protection Conventions prohibit dismissal during maternity leave and any extension thereof, or at such time as a notice of dismissal would expire during the leave under the terms of Convention No. 3, Article 4 and Convention No. 103, Article 6. Dismissal on grounds that might be regarded as legitimate is not considered to be permitted during this period (ILO 1965). In the event that a woman has been dismissed before going on maternity leave, the notice should be suspended for the time she is absent and continue after her return. The Maternity protection Recommendation, 1952 (No. 95), calls for the protection of a pregnant woman’s employment from the date the employer is informed of the pregnancy until one month after her return from maternity leave. It identifies cases of serious fault by the employed woman, the shutting down of the undertaking and the expiry of a fixed-term contract as legitimate grounds for dismissal during the protected period. The Termination of Employment Convention, 1982 (No. 158; Article 5(d)–(e)), does not prohibit dismissal, but provides that pregnancy or absence from work on maternity leave shall not constitute valid reasons for termination of employment.
At the level of the European Union, the 1992 Directive prohibits dismissal from the beginning of pregnancy until the end of the maternity leave, save in exceptional cases not connected with the worker’s condition.
Usually, countries provide for two sets of rules regarding dismissal. Dismissal with notice applies in such cases as the closure of the enterprise, redundancy and where, for a variety of reasons, the worker is unable to perform the work for which he or she has been recruited or fails to perform such work to the employer’s satisfaction. Dismissal without notice is used to terminate the services of a worker who is guilty of gross negligence, serious misconduct or other grave instances of behaviour, usually comprehensively listed in the legislation.
Where dismissal with notice is concerned, it is clear that employers could arbitrarily decide that pregnancy is incompatible with a worker’s tasks and dismiss her on grounds of pregnancy. Those who wish to avoid their obligations to pregnant women, or even simply do not like to have pregnant women around the workplace, could find a pretext to dismiss workers during pregnancy even if, in view of the existence of non-discrimination rules, they would refrain from using pregnancy as grounds for dismissal. Many people agree that it is legitimate to protect workers against such discriminatory decisions: the prohibition of dismissal with notice on grounds of pregnancy or during pregnancy and maternity leave is often viewed as a measure of equity and is in force in many countries.
The ILO Committee of Exerts on the Application of Conventions and Recommendations considers that protection against dismissal does not preclude an employer from terminating an employment relationship because he or she has detected a serious fault on the part of a woman employee: rather, when there are reasons such as this to justify dismissal, the employer is obliged to extend the legal period of notice by any period required to complete the period of protection under the Conventions. This is the situation, for example, in Belgium, where an employer who has legal grounds for dismissing a woman cannot do so while she is on maternity leave, but can serve notice so that it expires after the woman returns from leave.
The protection of pregnant women against dismissal in case of closure of the undertaking or economic retrenchment poses a similar problem. It is indeed a burden for a firm which ceases operation to continue to pay the salary of a person who is not working for them any more, even for a short period. However, recruitment prospects are often bleaker for women who are pregnant than for women who are not, or for men, and pregnant women particularly need the emotional and financial security of continuing to be employed. Where women may not be dismissed during pregnancy, they can put off looking for a job until after the birth. In fact, where legislation provides for the order in which various categories of workers to be retrenched are to be dismissed, pregnant women are among those to be dismissed last or next to last (e.g., Ethiopia).
Leave and Benefits for Fathers and Parents
Going beyond the protection of the health and employment status of pregnant and nursing women, many countries provide for paternity leave (a short period of leave at or about the time of birth). Other forms of leave are linked to the needs of children. One type is adoption leave, and another is leave to facilitate child-rearing. Many countries foresee the latter type of leave, but use different approaches. One group provides for time off for the mother of very young children (optional maternity leave), while another provides additional leave for both parents (parental education leave). The view that both the father and mother need to be available to care for young children is also reflected in integrated parental leave systems, which provide a long period of leave available to both parents.
Pregnancy and US Work Recommendations
Changes in family life over recent decades have had dramatic effects on the relationship between work and pregnancy. These include the following:
- Women, particularly those of childbearing age, continue to enter the labour force in considerable numbers.
- A tendency has developed on the part of many of these women to defer starting their families until they are older, by which time they have often achieved positions of responsibility and become important members of the productive apparatus.
- At the same time, there is an increasing number of teenage pregnancies, many of which are high-risk pregnancies.
- Reflecting increasing rates of separation, of divorce and of choices of alternative lifestyles, as well as an increase in the number of families in which both parents must work, financial pressures are forcing many women to continue working for as long as possible during pregnancy.
The impact of pregnancy-related absences and lost or impaired productivity, as well as concern over the health and well-being of both the mothers and their infants, have led employers to become more proactive in dealing with the problem of pregnancy and work. Where employers pay all or part of health insurance premiums, the prospect of avoiding the sometimes staggering costs of complicated pregnancies and neonatal problems is a potent incentive. Certain responses are dictated by laws and government regulations, for example, guarding against potential occupational and environmental hazards and providing maternity leave and other benefits. Others are voluntary: prenatal education and care programmers, modified work arrangements such as flex-time and other work schedule arrangements, dependant care and other benefits.
Management of pregnancy
Of primary importance to the pregnant woman—and to her employer—whether or not she continues working during her pregnancy, is access to a professional health management programme designed to identify and avert or minimize risks to the mother and her foetus, thus enabling her to remain on the job without concern. At each of the scheduled prenatal visits, the physician or midwife should evaluate medical information (childbearing and other medical history, current complaints, physical examinations and laboratory tests) and information about her job and work environment, and develop appropriate recommendations.
It is important that health professionals not rely on the simple job descriptions pertaining to their patients’ work, as these are often inaccurate and misleading. The job information should include details concerning physical activity, chemical and other exposures and emotional stress, most of which can be provided by the woman herself. In some instances, however, input from a supervisor, often relayed by the safety department or the employee health service (where there is one), may be needed to provide a more complete picture of hazardous or trying work activities and the possibility of controlling their potential for harm. This can also serve as a check on patients who inadvertently or deliberately mislead their physicians; they may exaggerate the risks or, if they feel it is important to continue working, may understate them.
Recommendations for Work
Recommendations regarding work during pregnancy fall into three categories:
The woman may continue to work without changes in her activities or the environment. This is applicable in most instances. After extensive deliberation, the Task Force on the Disability of pregnancy comprising obstetrical health professionals, occupational physicians and nurses, and women’s representatives assembled by ACOG (the American College of Obstetricians and Gynecologists) and NIOSH (the National Institute for Occupational Safety and Health) concluded that “the normal woman with an uncomplicated pregnancy who is in a job that presents no greater hazards than those encountered in normal daily life in the community, may continue to work without interruption until the onset of labor and may resume working several weeks after an uncomplicated delivery” (Isenman and Warshaw, 1977).
The woman may continue to work, but only with certain modifications in the work environment or her work activities. These modifications would be either “desirable” or “essential” (in the latter case, she should stop work if they cannot be made).
The woman should not work. It is the physician’s or midwife’s judgement that any work would probably be detrimental to her health or to that of the developing foetus.
The recommendations should not only detail the needed job modifications but should also stipulate the length of time they should be in effect and indicate the date for the next professional examination.
Non-medical Considerations
The recommendations suggested above are based entirely on considerations of the health of the mother and her foetus in relation to job requirements. They do not take into account the burden of such off-the-job activities as commuting to and from the workplace, housework and care of other children and family members; these may sometimes be even more demanding than those of the job. When modification or restriction of activities is called for, one should consider the question whether it should be implemented on the job, in the home or both.
In addition, recommendations for or against continuing work may form the basis of a variety of non-medical considerations, for example, eligibility for benefits, paid versus unpaid leave or guaranteed job retention. A critical issue is whether the woman is considered disabled. Some employers categorically consider all pregnant workers to be disabled and strive to eliminate them from the workforce, even though many are able to continue to work. Other employers assume that all pregnant employees tend to magnify any disability in order to be eligible for all available benefits. And some even challenge the notion that a pregnancy, whether or not it is disabling, is a matter for them to be concerned about at all. Thus, disability is a complex concept which, although fundamentally based on medical findings, involves legal and social considerations.
Pregnancy and Disability
In many jurisdictions, it is important to distinguish between the disability of pregnancy and pregnancy as a period in life that calls for special benefits and dispensations. The disability of pregnancy falls into three categories:
- Disability following delivery. From a purely medical standpoint, recovery following the termination of pregnancy through an uncomplicated delivery lasts only a few weeks, but conventionally it extends to six or eight weeks because that is when most obstetricians customarily schedule their first postnatal check-up. However, from a practical and sociological point of view, a longer leave is considered by many to be desirable in order to enhance family bonding, to facilitate breast-feeding, and so on.
- Disability resulting from medical complications. Medical complications such as eclamsia, threatened abortion, cardiovascular or renal problems and so on, will dictate periods of reduced activity or even hospitalization that will last as long as the medical condition persists or until the woman has recovered from both the medical problem and the pregnancy.
- Disability reflecting the necessity of avoiding exposure to toxicity hazards or abnormal physical stress. Because of the greater sensitivity of the foetus to many environmental hazards, the pregnant woman may be considered disabled even though her own health might not be in danger of being compromised.
Conclusion
The challenge of balancing family responsibilities and work outside the home is not new to women. What may be new is a modern society that values the health and well-being of women and their offspring while confronting women with the dual challenges of achieving personal fulfillment through employment and coping with the economic pressures of maintaining an acceptable standard of living. The increasing number of single parents and of married couples both of whom must work suggest that work-family issues cannot be ignored. Many employed women who become pregnant simply must continue to work.
Whose responsibility is it to meet the needs of these individuals? Some would argue that it is purely a personal problem to be dealt with entirely by the individual or the family. Others consider it a societal responsibility and would enact laws and provide financial and other benefits on a community-wide basis.
How much should be loaded on the employer? This depends largely on the nature, the location and often the size of the organization. The employer is driven by two sets of considerations: those imposed by laws and regulations (and sometimes by the need to meet demands won by organized labour) and those dictated by social responsibility and the practical necessity of maintaining optimal productivity. In the last analysis, it hinges on lacing a high value on human resources and acknowledging the interdependence of work responsibilities and family commitments and their sometimes counterbalancing effects on health and productivity.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."