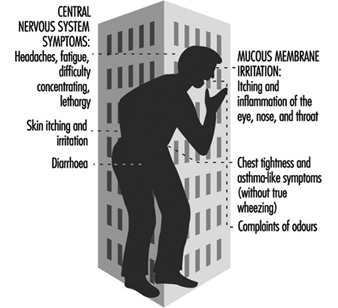
Sick building syndrome (SBS) is a term used to describe office worker discomfort and medical symptoms that are related to building characteristics, to pollutant exposures and to work organization, and that are mediated through personal risk factors. A wide range of definitions exists, but disagreement remains (a) as to whether a single individual in a building can develop this syndrome or whether a set numeric criterion (the proportion affected) should be used; and (b) as to the necessary symptom components. Figure 1 lists symptoms commonly included in SBS; in recent years, with increased understanding, complaints related to odours have generally been dropped from the list and chest symptoms included under mucous membrane irritation. A critical distinction needs to be made between SBS and building-related illness (BRI), where verifiable irritation, allergy or illness such as hypersensitivity pneumonitis, asthma or carbon monoxide-induced headaches may be present as an outbreak associated with a building. SBS should also be distinguished from multiple chemical sensitivities (MCS; see below) which is more sporadic in occurrence, often occurs within an SBS population, and is much less responsive to modifications of the office environment.
Figure 1. Sick building syndrome.
SBS should be simultaneously viewed from and informed by three disparate perspectives. For health professionals, the view is from the perspective of medicine and the health sciences as they define symptoms related to indoor work and their associated pathophysiological mechanisms. The second perspective is that of engineering, including design, commissioning, operations, maintenance and exposure assessment for specific pollutants. The third perspective includes the organizational, social and psychological aspects of work.
Epidemiology
Since the mid-1970s, increasingly voiced office worker discomfort has been studied in formal ways. These have included field epidemiological studies using a building or a workstation as the sampling unit to identify risk factors and causes, population-based surveys to define prevalence, chamber studies of humans to define effects and mechanisms, and field intervention studies.
Cross-sectional and case-control studies
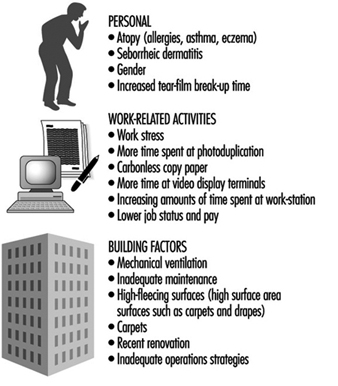
Approximately 30 cross-sectional surveys have been published (Mendell 1993; Sundell et al. 1994). Many of these have included primarily “non-problem” buildings, selected at random. These studies consistently demonstrate an association between mechanical ventilation and increased symptom reporting. Additional risk factors have been defined in several case-control studies. Figure 2 presents a grouping of widely recognized risk factors associated with increased rates of complaints.
Many of these factors overlap; they are not mutually exclusive. For example, the presence of inadequate housekeeping and maintenance, the presence of strong indoor pollution sources and increased individual susceptibility may lead to much greater problems than the presence of any one factor alone.
Figure 2. Risk factors for and causes of the sick building syndrome.
Factor and principal components analyses of questionnaire responses in cross-sectional surveys have explored the interrelationship of various symptoms. Consistently, symptoms related to single organ systems have clustered together more strongly than symptoms relating to different organ systems. That is, eye irritation, eye tearing, eye dryness, and eye itching all appear to correlate very strongly, and little benefit is obtained from looking at multiple symptoms within an organ system.
Controlled exposure studies
Animal testing to determine irritant properties and thresholds has become standard. A consensus method of the American Society for Testing and Materials (1984) is widely regarded as the basic instrument. This method has been used to develop structure-activity relationships, to demonstrate that more than one irritant receptor may exist in the trigeminal nerve and to explore interactions between multiple exposures. Most recently, it has been used to demonstrate the irritating properties of office equipment offgassing.
Analogous to this method, several approaches have been defined to document methods and dose-response relationships for irritation in humans. This work meanwhile suggests that, at least for “non-reactive” compounds such as saturated aliphatic hydrocarbons, the percentage of vapour pressure saturation of a compound is a reasonable predictor of its irritant potency. Some evidence also supports the view that increasing the number of compounds in complex mixtures decreases the irritant thresholds. That is, the more agents that are present, even at a constant mass, the greater the irritation.
Controlled exposure studies have been performed of volunteers in stainless steel chambers. Most have been performed with one constant mixture of volatile organic compounds (VOC) (Mølhave and Nielsen 1992). These consistently document relationships between symptoms and increasing exposure levels. Office workers who perceived themselves as “susceptible” to the effects of usual levels of VOCs indoors demonstrated some impairment on standard tests of neuropsychological performance (Mølhave, Bach and Pederson 1986). Healthy volunteers, on the other hand, demonstrated mucous membrane irritation and headaches at exposures in the range of 10 to 25 mg/m3, but no changes on neuropsychological performance. More recently, office workers demonstrated similar symptoms after simulated work in environments where pollutants from commonly used office equipment were generated. Animals reacted similarly when a standardized test of irritant potency was used.
Population-based studies
To date, three population-based studies have been published in Sweden, Germany and the United States. The questionnaires differed considerably, and thus prevalence estimates cannot be directly compared. Nevertheless, between 20 and 35% of respondents from various buildings not known to be sick were found to have complaints.
Mechanisms
A number of potential mechanisms and objective measures to explain and examine symptoms within specific organ systems have been identified. None of these has a high predictive value for the presence of disease, and they are therefore not suitable for clinical diagnostic use. They are useful in field research and epidemiological investigations. For many of these it is unclear whether they should be regarded as mechanisms, as markers of effect, or as measures of susceptibility.
Eyes
Both allergic and irritant mechanisms have been proposed as explanations for eye symptoms. Shorter tear-film break-up time, a measure of tear film instability, is associated with increased levels of symptoms. “Fat-foam thickness” measurement and photography for documentation of ocular erythema have also been used. Some authors attribute eye symptoms at least in part to increased individual susceptibility as measured by those factors. In addition, office workers with ocular symptoms have been demonstrated to blink less frequently when working at video display terminals.
Nose
Both allergic and irritant mechanisms have been proposed as explanations for nasal symptoms. Measures that have successfully been used include nasal swabs (eosinophils), nasal lavage or biopsy, acoustic rhinometry (nasal volume), anterior and posterior rhinomanometry (plethysmography) and measures of nasal hyperreactivity.
Central nervous system
Neuropsychological tests have been used to document decreased performance on standardized tests, both as a function of controlled exposure (Mølhave, Bach and Pederson 1986) and as a function of the presence of symptoms (Middaugh, Pinney and Linz 1982).
Individual risk factors
Two sets of individual risk factors have been discussed. First, two commonly recognized diatheses, atopy and seborrhea, are considered predisposing factors for medically defined symptoms. Second, psychological variables may be important. For example, personal traits such as anxiety, depression or hostility are associated with sick-role susceptibility. Similarly, work stress is so consistently associated with building-related symptoms that some causal association is likely to be present. Which of the three components of work stress—individual traits, coping skills, and organization function such as poor management styles—is the dominant cause remains undetermined. It is recognized that failing to intervene in a well-defined problem leads workers to experience their discomfort with increasing distress.
Engineering and Sources
Beginning in the late 1970s, the US National Institute for Occupational Safety and Health (NIOSH) responded to requests for help in identifying causes of occupant discomfort in buildings, attributing problems to ventilation systems (50%), microbiological contamination (3 to 5%), strong indoor pollution sources (tobacco 3%, others 14%), pollutants entrained from the outside (15%) and others. On the other hand, Woods (1989) and Robertson (et al. 1988) published two well-known series of engineering analyses of problem buildings, documenting on average the presence of three potential causal factors in each building.
One current professional ventilation standard (American Society of Heating, Refrigerating, and Airconditioning Engineers (1989) suggests two approaches to ventilation: a ventilation rate procedure and an air quality procedure. The former provides a tabular approach to ventilation requirements: office buildings require 20 cubic feet of outside air per occupant per minute to maintain occupant complaint rates of environmental discomfort at below 20%. This assumes relatively weak pollution sources. When stronger sources are present, that same rate will provide less satisfaction. For example, when smoking is permitted at usual rates (according to data from the early 1980s), approximately 30% of occupants will complain of environmental discomfort. The second approach requires the selection of a target concentration in air (particulates, VOCs, formaldehyde, etc.), information on emission rates (pollutant per time per mass or surface), and derives the ventilation requirements. Although this is an intellectually much more satisfying procedure, it remains elusive because of inadequate emissions data and disagreement on target concentrations.
Pollutants
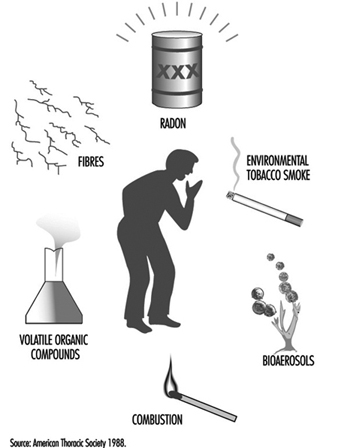
Environmental scientists have generally defined exposure and health effects on a pollutant-by-pollutant basis. The American Thoracic Society (1988) defined six important categories, listed in figure 3.
Figure 3. Principal pollutant categories.
Environmental criteria have been established for many of the individual substances in these six groups. The utility and applicability of such criteria for indoor environments is controversial for many reasons. For example, the goals of threshold limit values often do not include prevention of eye irritation, a common complaint in indoor environments with requirements for close eye work at video display units. For most of the pollutant categories, the problem of interactions, commonly termed the “multiple contaminants problem,” remains inadequately defined. Even for agents that are thought to affect the same receptor, such as aldehydes, alcohols and ketones, no prediction models are well established. Finally, the definition of “representative compounds” for measurement is unclear. That is, pollutants must be measurable, but complex mixtures vary in their composition. It is unclear, for instance, whether the chronic residual odor annoyance due to environmental tobacco smoke correlates better with nicotine, particulates, carbon monoxide or other pollutants. The measure “total volatile organic compounds” is meanwhile considered an interesting concept, but is not useful for practical purposes as the various components have such radically different effects (Mølhave and Nielsen 1992; Brown et al. 1994). Particulates indoors may differ in composition from their outdoor counterparts, as filter sizes affect entrained concentrations, and indoor sources may differ from outdoor sources. There are measurement problems as well, since the sizes of filters used will affect which particles are collected. Different filters may be needed for indoor measurements.
Finally, emerging data suggest that reactive indoor pollutants may interact with other pollutants and lead to new compounds. For example, the presence of ozone, either from office machines or entrained from outdoors, may interact with 4-phenylcyclohexene and generate aldehydes (Wechsler 1992).
Primary Aetiological Theories
Organic solvents
Buildings have always relied on general dilution strategies for pollutant removal, but designers have assumed that humans were the primary source of pollutants. More recently, emissions from “solid materials” (such as particle board desks, carpeting and other furniture), from wet products (such as glues, wall paints, office machine toners) and personal products (perfumes) have been recognized as contributors to a complex mixture of very low levels of individual pollutants (summarized in Hodgson, Levin and Wolkoff 1994).
Several studies suggest that the presence of reactive volatile organic compounds, such as aldehydes and halogenated hydrocarbons, are associated with increasing levels of symptoms. Offices with higher complaint rates have had greater “loss” of VOCs between incoming and outgoing air than did offices with lower complaints. In a prospective study of schools, short chain VOCs were associated with symptom development. In another survey, higher personal samples for VOCs using a screening sampler that “over-reacts” to reactive VOCs, such as aldehydes and halogenated hydrocarbons, were associated with higher symptom levels. In that study, women had higher levels of VOCs in their breathing zone, suggesting another potential explanation for the increased rate of complaints among women. VOCs might adsorb onto sinks, such as fleecy surfaces, and be re-emitted from such secondary sources. The interaction of ozone and relatively non-irritant VOCs to form aldehydes is also consistent with this hypothesis.
The presence of multiple potential sources, the consistency of VOC health effects and SBS symptoms, and the widely recognized problems associated with ventilation systems make VOCs an attractive aetiological agent. Solutions other than better design and operation of ventilation systems include the selection of low-emitting pollutants, better housekeeping and prevention of “indoor chemistry.”
Bioaerosols
Several studies have suggested that bioaerosols have the potential to contribute to occupant discomfort. They may do this through several different mechanisms: irritant emissions; release of fragments, spores or viable organisms leading to allergy; and secretion of complex toxins. Fewer data exist to support this theory than the others. Nevertheless, it is clear that heating, ventilating and air-conditioning systems may be sources of micro-organisms.
They have also been described in building construction materials (as a result of improper curing), as a result of unwanted water incursion and in office dust. The presence of sensitizers in the office environment, such as dust mites or cat dander brought in from home on clothing, presents another possibility of exposure. To the extent that biological agents contribute to the problem, dirt and water management become primary control strategies.
In addition, toxigenic fungi may be found on other porous products in buildings, including ceiling tile, spray-on insulation and wooden joists. Especially in residential environments, fungal proliferation associated with inadequate moisture control has been associated with symptoms.
Psychosocial aspects of work
In all studies where it has been examined, “work stress” was clearly associated with SBS symptoms. Workers’ perceptions of job pressures, task conflicts, and non-work stressors such as spousal or parental demands may clearly lead to the subjective experience of “stronger” irritation as a function of illness behaviour. At times, such perceptions may in fact result from poor supervisory practices. In addition, the presence of irritants leading to subjective irritation is thought to lead to “work stress”.
Evaluation of the Patient
The examination should be directed at identification or exclusion of a significant component of building related illness (BRI). Allergic disease should be identified and optimally managed. However, this must be done with awareness that non-allergic mechanisms may contribute to a substantial residual symptom burden. Sometimes individuals can be reassured of the absence of clear disease by studies such as portable peak flow monitoring or pre- and post-work pulmonary function tests. Once such observable or pathologically verifiable disease has been ruled out, evaluation of the building itself becomes paramount and should be done with industrial hygiene or engineering input. Documentation, management and remediation of identified problems is discussed in Controlling the Indoor Environment.
Conclusion
SBS is a phenomenon that can be experienced by an individual, but is usually seen in groups; it is associated with engineering deficiencies and is likely caused by a series of pollutants and pollutant categories. As with all “dis-ease,” a component of personal psychology serves as an effect modifier that can lead to varying degrees of symptom intensity at any given level of distress.