The growth of industry, agriculture, mining and manufacturing has been paralleled by the development of occupational diseases of the skin. The earliest reported harmful effects were ulcerations of the skin from metal salts in mining. As populations and cultures have expanded the uses of new materials, new skills and new processes have emerged. Such technological advances brought changes to the work environment and during each period some aspect of the technical change has impaired workers’ health. Occupational diseases, in general and skin diseases, in particular, have long been an unplanned by-product of industrial achievement.
Fifty years ago in the United States, for example, occupational diseases of the skin accounted for no less than 65-70% of all reported occupational diseases. Recently, statistics collected by the United States Department of Labor indicate a drop in frequency to approximately 34%. This decreased number of cases is said to have resulted from increased automation, from enclosure of industrial processes and from better education of management, supervisors and workers in the prevention of occupational diseases in general. Without doubt such preventive measures have benefited the workforce in many larger plants where good preventive services may be available, but many people are still employed in conditions which are conducive to occupational diseases. Unfortunately, there is no accurate assessment of the number of cases, causal factors, time lost or actual cost of occupational skin disease in most countries.
General terms, such as industrial or occupational dermatitis or professional eczema, are used for occupational skin diseases but names related both to cause and effect are also commonly used. Cement dermatitis, chrome holes, chloracne, fibreglass itch, oil bumps and rubber rash are some examples. Because of the variety of skin changes induced by agents or conditions at work, these diseases are appropriately called occupational dermatoses—a term which includes any abnormality resulting directly from, or aggravated by, the work environment. The skin can also serve as an avenue of entry for certain toxicants which cause chemical poisoning via percutaneous absorption.
Cutaneous Defence
From experience we know that the skin can react to a large number of mechanical, physical, biological and chemical agents, acting alone or in combination. Despite this vulnerability, occupational dermatitis is not an inevitable accompaniment of work. The majority of the workforce manages to remain free of disabling occupational skin problems, due in part to the inherent protection provided by the skin’s design and function, and in part due to the daily use of personal protective measures directed towards minimizing skin contact with known skin hazards at the worksite. Hopefully, the absence of disease in the majority of workers may also be due to jobs which have been designed to minimize exposure to conditions hazardous to the skin.
The skin
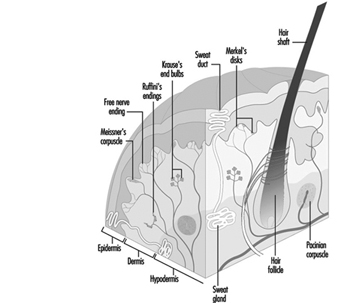
Human skin, except for palms and soles, is quite thin and of variable thickness. It has two layers: the epidermis (outer) and dermis (inner). Collagen and elastic components in the dermis allow it to function as a flexible barrier. The skin provides a unique shield which protects within limits against mechanical forces, or penetration by various chemical agents. The skin limits water loss from the body and guards against the effects of natural and artificial light, heat and cold. Intact skin and its secretions provide a fairly effective defence zone against micro-organisms, providing mechanical or chemical injury does not impair this defence. Figure 1 provides an illustration of the skin and description of its physiological functions.
Figure 1. Schematic representation of the skin.
The outer epidermal layer of dead cells (keratin) provides a shield against elements in the outside world. These cells, if exposed to frictional pressures, can form a protective callus and can thicken after ultraviolet exposure. Keratin cells are normally arranged in 15 or 16 shingle-like layers and provide a barrier, though limited, against water, water-soluble materials and mild acids. They are less able to act as a defence against repeated or prolonged contact with even low concentrations of organic or inorganic alkaline compounds. Alkaline materials soften but do not totally dissolve the keratin cells. The softening disturbs their inner structure enough to weaken cellular cohesiveness. The integrity of the keratin layer is allied to its water content which, in turn, influences its pliability. Lowered temperatures and humidity, dehydrating chemicals such as acids, alkali, strong cleaners and solvents, cause water loss from the keratin layer, which, in turn, causes the cells to curl and crack. This weakens its ability to serve as a barrier and compromises its defence against water loss from the body and entry of various agents from outside.
Cutaneous defence systems are effective only within limits. Anything which breaches one or more of the links endangers the entire defence chain. For example, percutaneous absorption is enhanced when the continuity of the skin has been altered by physical or chemical injury or by mechanical abrasion of the keratin layer. Toxic materials can be absorbed not only through the skin, but also through the hair follicules, sweat orifices and ducts. These latter routes are not as important as transepidermal absorption. A number of chemicals used in industry and in farming have caused systemic toxicity by absorption through the skin. Some well established examples are mercury, tetraethyllead, aromatic and amino nitro compounds and certain organophosphates and chlorinated hydrocarbon pesticides. It should be noted that for many substances, systemic toxicity generally arises through inhalation but percutaneous absorption is possible and should not be overlooked.
A remarkable feature of cutaneous defence is the ability of the skin to continually replace the basal cells which provide the epidermis with its own built-in replication and repair system.
The skin’s ability to act as a heat exchanger is essential to life. Sweat gland function, vascular dilation and constriction under nervous control are vital to regulating body heat, as is evaporation of surface water on skin. Constriction of the blood vessels protects against cold exposures by preserving central body heat. Multiple nerve endings within the skin act as sensors for heat, cold and other excitants by relaying the presence of the stimulant to the nervous system which responds to the provoking agent.
A major deterrent against injury from ultraviolet radiation, a potentially harmful component of sunlight and some forms of artificial light is the pigment (melanin) manufactured by the melanocytes located in the basal cell layer of the epidermis. Melanin granules are picked up by the epidermal cells and serve to add protection against the rays of natural or artificial light which penetrate the skin. Additional protection, though less in degree, is furnished by the keratin cell layer which thickens following ultraviolet exposure. (As discussed below, for those whose worksites are outdoors it is essential to protect exposed skin with a sun-screen coating agent having a protective against UV-A and against UV-B (rating of 15 or greater) together with appropriate clothing to provide a high level of shielding against sun light injury.)
Types of Occupational Skin Diseases
Occupational dermatoses vary both in their appearance (morphology) and severity. The effect of an occupational exposure may range from the slightest erythema (reddening) or discoloration of the skin to a far more complex change, as a malignancy. Despite the wide range of substances that are known to cause skin effects, in practice it is difficult to associate a specific lesion with exposure to a specific material. However, certain chemical groups are associated with characteristic reaction patterns. The nature of the lesions and their location may provide a strong clue as to causality.
A number of chemicals with or without direct toxic effect on the skin can also cause systemic intoxication following absorption through the skin. In order to act as a systemic toxin, the agent must pass through the keratin and the epidermal cell layers, then through the epidermal-dermal junction. At this point it has ready access to the bloodstream and the lymphatic system and can now be carried to vulnerable target organs.
Acute contact dermatitis (irritant or allergic).
Acute contact eczematous dermatitis can be caused by hundreds of irritant and sensitizing chemicals, plants and photoreactive agents. Most occupational allergic dermatoses can be classified as acute eczematous contact dermatitis. Clinical signs are heat, redness, swelling, vesiculation and oozing. Symptoms include itch, burning and general discomfort. The back of the hands, the inner wrists and the forearms are the usual sites of attack, but acute contact dermatitis can occur anywhere on the skin. If the dermatosis occurs on the forehead, the eyelids, the ears, the face or the neck, it is logical to suspect that a dust or a vapour may be involved in the reaction. When there is a generalized contact dermatitis, not restricted to one or a few specific sites, it is usually caused by a more extensive exposure, such as the wearing of contaminated clothing, or by autosensitization from a pre-existing dermatitis. Severe blistering or destruction of tissue generally indicates the action of an absolute or strong irritant. The exposure history, which is taken as part of the medical control of occupational dermatitis, may reveal the suspected causative agent. An accompanying article in this chapter provides more details on contact dermatitis.
Sub-acute contact dermatitis
Through a cumulative effect repeated contact with both weak and moderate irritants can cause a sub-active form of contact dermatitis characterized by dry, red plaques. If the exposure continues, the dermatitis will become chronic.
Chronic eczematous contact dermatitis
When a dermatitis recurs over an extended period of time it is called chronic eczematous contact dermatitis. The hands, fingers, wrists and forearms are the sites most often affected by chronic eczematous lesions, characterized by dry, thickened and scaly skin. Cracking and fissuring of the fingers and the palms may be present. Chronic nail dystrophy is also commonly found. Frequently, the lesions will begin to ooze (sometimes called “weeping”) because of re-exposure to the responsible agent or by imprudent treatment and care. Many materials not responsible for the original dermatosis will sustain this chronic recurrent skin problem.
Photosensitivity dermatitis (phototoxic or photoallergic)
Most photoreactions on the skin are phototoxic. Either natural and artificial light sources alone or in combination with various chemicals, plants or drugs can induce a phototoxic or photosensitive response. Phototoxic reaction is generally limited to light-exposed areas while photosensitive reaction can develop frequently on non-exposed body surfaces. Some examples of photoreactive chemicals are coal tar distillation products, such as creosote, pitch and anthracene. Members of the plant family Umbelliferae are well known photoreactors. Family members include cow parsnip, celery, wild carrot, fennel and dill. The reactive agent in these plants are psoralens.
Folliculitis and acneform dermatoses, including chloracne
Workers with dirty jobs often develop lesions involving the follicular openings. Comedones (blackheads) may be the only obvious effect of the exposure, but often a secondary infection of the follicle may ensure. Poor personal hygiene and ineffective cleansing habits can add to the problem. Follicular lesions generally occur on the forearms and less often on the thighs and buttocks, but they can occur anywhere except on the palms and soles.
Follicular and acneform lesions are caused by overexposure to insoluble cutting fluids, to various tar products, paraffin, and certain aromatic chlorinated hydrocarbons. The acne caused by any of the above agents can be extensive. Chloracne is the most serious form, not only because it can lead to disfigurement (hyperpigmentation and scarring) but also because of the potential liver damage, including porphyria cutanea tarda and other systemic effects that the chemicals can cause. Chloronaphthalenes, chlorodi-phenyls, chlorotriphenyls, hexachlorodibenzo-p-dioxin, tetrachloroazoxybenzene and tetrachlorodibenzodioxin (TCDD), are among the chloracne-causing chemicals. The blackheads and cystic lesions of chloracne often appear first on the sides of the forehead and the eyelids. If exposure continues, lesions may occur over widespread areas of the body, except for the palms and soles.
Sweat-induced reactions
Many types of work involve exposure to heat and where there is too much heat and sweating, followed by too little evaporation of the sweat from the skin, prickly heat can develop. When there is chafing of the affected area by skin rubbing against skin, a secondary bacterial or fungal infection may frequently occur. This happens particularly in the underarm area, under the breast, in the groin and between the buttocks.
Pigment change
Occupationally induced changes in skin colour can be caused by dyes, heavy metals, explosives, certain chlorinated hydrocarbons, tars and sunlight. The change in skin colour may be the result of a chemical reaction within the keratin, as for example, when the keratin is stained by metaphenylene-diamine or methylene blue or trinitrotoluene. Sometimes permanent discoloration may occur more deeply in the skin as with argyria or traumatic tattoo. Increased pigmentation induced by chlorinated hydrocarbons, tar compounds, heavy metals and petroleum oils generally results from melanin stimulation and overproduction. Hypopigmentation or depigmentation at selected sites can be caused by a previous burn, contact dermatitis, contact with certain hydroquinone compounds or other antioxidant agents used in selected adhesives and sanitizing products. Among the latter are tertiary amyl phenol, tertiary butyl catechol and tertiary butyl phenol.
New growths
Neoplastic lesions of occupational origin may be malignant or benign (cancerous or non-cancerous). Melanoma and non-melanocytic skin cancer are discussed in two other articles in this chapter. Traumatic cysts, fibromata, asbestos, petroleum and tar warts and keratoacanthoma, are typical benign new growths. Keratoacanthomas can be associated with excessive exposure to sunlight and also have been ascribed to contact with petroleum, pitch and tar.
Ulcerative changes
Chromic acid, concentrated potassium dichromate, arsenic trioxide, calcium oxide, calcium nitrate and calcium carbide are documented ulcerogenic chemicals. Favourite attack sites are the fingers, hands, folds and palmar creases. Several of these agents also cause perforation of the nasal septum.
Chemical or thermal burns, blunt injury or infections resulting from bacteria and fungi may result in ulcerous excavations on the affected part.
Granulomas
Granulomas can arise from many occupational sources if the appropriate circumstances are present. Granulomas can be caused by occupational exposures to bacteria, fungi, viruses or parasites. Inanimate substances, such as bone fragments, wood splinters, cinders, coral and gravel, and minerals such as beryllium, silica and zirconium, can also cause granulomas after skin embedment.
Other conditions
Occupational contact dermatitis accounts for at least 80% of all cases of occupational skin diseases. However, a number of other changes that affect the skin, hair and nails are not included in the foregoing classification. Hair loss caused by burns, or mechanical trauma or certain chemical exposures, is one example. A facial flush that follows the combination of drinking alcohol and inhaling certain chemicals, such as trichlorethylene and disulfuram, is another. Acroosteolysis, a type of bony disturbance of the digits, plus vascular changes of the hands and forearm (with or without Raynaud’s syndrome) has been reported among polyvinyl chloride polymerization tank cleaners. Nail changes are covered in a separate article in this chapter.
Physiopathology or Mechanismsof Occupational Skin Diseases
The mechanisms by which primary irritants act are understood only in part—for instance, vesicant or blister gases (nitrogen mustard or bromomethane and Lewisite, etc.)—interfere with certain enzymes and thereby block selective phases in the metabolism of carbohydrates, fats and proteins. Why and how the blister results is not clearly understood but observations of how chemicals react outside the body yield some ideas about possible biological mechanisms.
In brief, because alkali reacts with acid or lipid or protein, it has been presumed that it also reacts with skin lipid and protein. In so doing, surface lipids are changed and keratin structure becomes disturbed. Organic and inorganic solvents dissolve fats and oils and have the same effect on cutaneous lipids. Additionally, however, it appears that solvents abstract some substance or change the skin in such a way that the keratin layer dehydrates and the skin’s defence is no longer intact. Continued insult results in an inflammatory reaction eventuating in contact dermatitis.
Certain chemicals readily combine with the water within skin or on the surface of the skin, and cause a vigorous chemical reaction. Calcium compounds, such as calcium oxide and calcium chloride, produce their irritant effect in this way.
Substances such as coal tar pitch, creosote, crude petroleum, certain aromatic chlorinated hydrocarbons, in combination with sunlight exposure, stimulate the pigment-producing cells to over function, leading to hyperpigmentation. Acute dermatitis also may give rise to hyperpigmentation after healing. Conversely, burns, mechanical trauma, chronic contact dermatitis, contact with monobenzyl ether of hydroquinone or certain phenolics can induce hypo- or de-pigmented skin.
Arsenic trioxide, coal tar pitch, sunlight and ionizing radiation, among other agents, can damage the skin cells so that abnormal cell growth results in cancerous change of the exposed skin.
Unlike primary irritation, allergic sensitization is the result of a specifically acquired alteration in the capacity to react, brought about by T-cell activation. For several years it has been agreed that contact allergic eczematous dermatitis accounts for about 20% of all the occupational dermatoses. This figure is probably too conservative in view of the continued introduction of new chemicals, many of which have been shown to cause allergic contact dermatitis.
Causes of Occupational Skin Diseases
Materials or conditions known to cause occupational skin disease are unlimited. They are currently divided into mechanical, physical, biological and chemical categories, which continue to grow in number each year.
Mechanical
Friction, pressure or other forms of more forceful trauma may induce changes ranging from callus and blisters to myositis, tenosynovitis, osseous injury, nerve damage, laceration, shearing of tissue or abrasion. Lacerations, abrasions, tissue disruption and blisters additionally pave the way for secondary infection by bacteria or, less often, fungi to set in. Almost everyone is exposed each day to one or more forms of mechanical trauma which may be mild or moderate in degree. However, those who use pneumatic riveters, chippers, drills and hammers are at greater risk of suffering neurovascular, soft tissue, fibrous or bone injury to the hands and forearms. because of the repetitive trauma from the tool. The use of vibration-producing tools which operate in a certain frequency range can induce painful spasms in the fingers of the tool-holding hand. Transfer to other work, where possible, generally provides relief. Modern equipment is designed to reduce vibration and thus obviate the problems.
Physical agents
Heat, cold, electricity, sunlight, artificial ultraviolet, laser radiation and high energy sources such as x rays, radium and other radioactive substances are potentially injurious to skin and to the entire body. High temperature and humidity at work or in a tropical work environment can impair the sweat mechanism and cause systemic effects known as sweat retention syndrome. Milder exposure to heat may induce prickly heat, intertrigo (chafing), skin maceration and supervening bacterial or fungal infection, particularly in overweight and diabetic individuals.
Thermal burns are frequently experienced by electric furnace operators, lead burners, welders, laboratory chemists, pipe-line workers, road repairmen, roofers and tar plant workers contacting liquid tar. Prolonged exposure to cold water or lowered temperatures causes mild to severe injury ranging from erythema to blistering, ulceration and gangrene. Frostbite affecting the nose, ears, fingers and toes of construction workers, firemen, postal workers, military personnel and other outdoor workers is a common form of cold injury.
Electricity exposure resulting from contact with short circuits, bare wires or defective electrical apparatus cause burns of the skin and destruction of deeper tissue.
Few workers are without exposure to sunlight and some individuals with repeated exposure incur severe actinic damage to skin. Modern industry also has many sources of potentially injurious artificial ultraviolet wavelengths, such as in welding, metal burning, molten-metal pouring, glass blowing, electric furnace tending, plasma torch burning and laser beam operations. Apart from the natural capacity of ultraviolet rays in natural or artificial light to injure skin, coal tar and several of its by-products, including certain dyes, selected light-receptive components of plants and fruits and a number of topical and parenteral medications contain harmful chemicals which are activated by certain wavelengths of ultraviolet rays. Such photoreaction effects may operate by either phototoxic or photoallergic mechanisms.
High-intensity electromagnetic energy associated with laser beams is well able to injure human tissue, notably the eye. Skin damage is less of a risk but can occur.
Biological
Occupational exposures to bacteria, fungi, viruses or parasites may cause primary or secondary infections of the skin. Prior to the advent of modern antibiotic therapy, bacterial and fungal infections were more commonly encountered and associated with disabling illness and even death. While bacterial infections can occur in any kind of work setting, certain jobs, such as animal breeders and handlers, farmers, fishermen, food processors and hide handlers have greater exposure potential. Similarly, fungal (yeast) infections are common among bakers, bartenders, cannery workers, cooks, dishwashers, child-care workers and food processors. Dermatoses due to parasitic infections are not common, but when they do occur they are seen most often among agricultural and livestock workers, grain handlers and harvesters, longshoremen and silo workers.
Cutaneous viral infections caused by work are few in number, yet some, such as milker’s nodules among dairyworkers, herpes simplex among medical and dental personnel and sheep pox among livestock handlers continue to be reported.
Chemicals
Organic and inorganic chemicals are the major source of hazards to the skin. Hundreds of new agents enter the work environment each year and many of these will cause cutaneous injury by acting as primary skin irritants or allergic sensitizers. It has been estimated that 75% of the occupational dermatitis cases are caused by primary irritant chemicals. However, in clinics where the diagnostic patch test is commonly used, the frequency of occupational allergic contact dermatitis is increased. By definition, a primary irritant is a chemical substance which will injure every person’s skin if sufficient exposure takes place. Irritants can be rapidly destructive (strong or absolute) as would occur with concentrated acids, alkalis, metallic salts, certain solvents and some gases. Such toxic effects can be observed within a few minutes, depending upon the concentration of the contactant and the length of contact which occurs. Conversely, dilute acids and alkalis, including alkaline dusts, various solvents and soluble cutting fluids, among other agents, may require several days of repeated contact to produce observable effects. These materials are termed “marginal or weak irritants”.
Plants and woods
Plants and woods are often classified as a separate cause of skin disease, but they can also be correctly included in the chemical grouping. Many plants cause mechanical and chemical irritation and allergic sensitization, while others have gained attention because of their photoreactive capacity. The family Anacardiaceae, which includes poison ivy, poison oak, poison sumac, cashew-nut shell oil and the Indian marking nut, is a well-known cause of occupational dermatitis due to its active ingredients (polyhydric phenols). Poison ivy, oak and sumac are common causes of allergic contact dermatitis. Other plants associated with occupational and non-occupational contact dermatitis include castor bean, chrysanthemum, hops, jute, oleander, pineapple, primrose, ragweed, hyacinth and tulip bulbs. Fruits and vegetables, including asparagus, carrots, celery, chicory, citrus fruits, garlic and onions, have been reported as causing contact dermatitis in harvesters, food packing and food preparation workers.
Several varieties of wood have been named as causes of occupational dermatoses among lumberers, sawyers, carpenters and other wood craftspeople. However, the frequency of skin disease is much less than is experienced from contact with poisonous plants. It is likely that some of the chemicals used for preserving the wood cause more dermatitic reactions than the oleoresins contained in wood. Among the preservative chemicals used to protect against insects, fungi and deterioration from soil and moisture are chlorinated diphenyls, chlorinated naphthalenes, copper naphthenate, creosote, fluorides, organic mercurials, tar and certain arsenical compounds, all known causes of occupational skin diseases.
Non-Occupational Factors in OccupationalSkin Disease
Considering the numerous direct causes of occupational skin disease cited above, it can be readily understood that practically any job has obvious and often hidden hazards. Indirect or predisposing factors may also merit attention. A predisposition can be inherited and related to skin colour and type or it may represent a skin defect acquired from other exposures. Whatever the reason, some workers have lower tolerance to materials or conditions in the work environment. In large industrial plants, medical and hygiene programmes can provide the opportunity for placement of such employees in work situations that will not further impair their health. In small plants, however, predisposing or indirect causal factors may not be given proper medical attention.
Pre-existing skin conditions
Several non-occupational diseases affecting the skin can be worsened by various occupational influences.
Acne. Adolescent acne in employees is generally made worse by machine tool, garage and tar exposures. Insoluble oils, various tar fractions, greases and chloracnegenic chemicals are definite hazards to these people.
Chronic eczemas. Detecting the cause of chronic eczema affecting the hands and sometimes distant sites can be elusive. Allergic dermatitis, pompholyx, atopic eczema, pustular psoriasis and fungal infections are some examples. Whatever the condition, any number of irritant chemicals, including plastics, solvents, cutting fluids, industrial cleansers and prolonged moisture, can worsen the eruption. Employees who must continue to work will do so with much discomfort and probably lowered efficiency.
Dermatomycosis. Fungal infections can be worsened at work. When fingernails become involved it may be difficult to assess the role of chemicals or trauma in the nail involvement. Chronic tinea of the feet is subject to periodic worsening, particularly when heavy footgear is required.
Hyperhidrosis. Excessive sweating of the palms and soles can soften the skin (maceration), particularly when impervious gloves or protective footgear are required. This will increase a person’s vulnerability to the effects of other exposures.
Miscellaneous conditions. Employees with polymorphous light eruption, chronic discoid lupus erythematous, porphyria or vitiligo are definitely at greater risk, particularly if there is simultaneous exposure to natural or artificial ultraviolet radiation.
Skin type and pigmentation
Redheads and blue-eyed blondes, particularly those of Celtic origin, have less tolerance to sunlight than people of darker skin type. Such skin is also less able to tolerate exposures to photoreactive chemicals and plants and is suspected of being more susceptible to the action of primary irritant chemicals, including solvents. In general, black skin has a superior tolerance to sunlight and photoreactive chemicals and is less prone to the induction of cutaneous cancer. However, darker skin tends to respond to mechanical, physical or chemical trauma by displaying post-inflammatory pigmentation. It is also more prone to develop keloids following trauma.
Certain skin types, such as hairy, oily, swarthy skins, are more likely to incur folliculitis and acne. Employees with dry skin and those with ichthyoses are at a disadvantage if they must work in low humidity environments or with chemical agents which dehydrate skin. For those workers who sweat profusely, a need to wear impervious protective gear will add to their discomfort. Similarly, overweight individuals usually experience prickly heat during the warm months in hot working environments or in tropical climates. While sweat can be helpful in cooling the skin, it can also hydrolyze certain chemicals that will act as skin irritants.
Diagnosing Occupational Skin Diseases
Cause and effect of occupational skin disease can be best ascertained through a detailed history, which should cover the past and present health and work status of the employee. Family history, particularly of allergies, personal illness in childhood and the past, is important. The title of the job, the nature of the work, the materials handled, how long the job has been done, should be noted. It is important to know when and where on the skin the rash appeared, the behaviour of the rash away from work, whether other employees were affected, what was used to cleanse and protect the skin, and what has been used for treatment (both self-medication and prescribed medication); as well as whether the employee has had dry skin or chronic hand eczema or psoriasis or other skin problems; what drugs, if any, have been used for any particular disease; and finally, which materials have been used in home hobbies such as the garden or woodworking or painting.
The following elements are important parts of the clinical diagnosis:
- Appearance of the lesions. Acute or chronic eczematous contact dermatosis are most common. Follicular, acneform, pigmentary, neoplastic, ulcerative granulomatous lesions and conditions such as Raynaud’s syndrome and contact urticaria can occur.
- Sites involved. The hands, the digits, the wrists and the forearms are the most common sites affected. Exposure to dusts and fumes usually cause the dermatosis to appear on the forehead, face, and V of the neck. Widespread dermatitis can result from autosensitization (spread) of an occupational or nonoccupational dermatosis.
- Diagnostic tests. Laboratory tests should be employed when necessary for the detection of bacteria, fungi and parasites. When allergic reactions are suspect, diagnostic patch tests can be used to detect occupational as well as non-occupational allergies, including photosensitization. Patch tests are a highly useful procedure and are discussed in an accompanying article in this chapter. At times, useful information can be obtained through the use of analytical chemical examination of blood, urine, or tissue (skin, hair, nails).
- Course. Of all the cutaneous changes induced by agents or certain conditions at work, acute and chronic eczematous contact dermatoses are foremost in number. Next in frequency are follicular and acneform eruptions. The other categories, including chloracne, constitute a smaller but still important group because of their chronic nature and the scarring and disfigurement which may be present.
An occupationally induced acute contact eczematous dermatitis tends to improve upon cessation of contact. Additionally, modern therapeutic agents can facilitate the period of recovery. However, if a worker returns to work and to the same conditions, without proper preventive measures undertaken by the employer and necessary precautions explained and understood by the worker, it is probable that the dermatosis will recur soon after re-exposure.
Chronic eczematous dermatoses, acneform lesions and pigmentary changes are less responsive to treatment even when contact is eliminated. Ulcerations usually improve with elimination of the source. With granulomatous and tumour lesions, eliminating contact with the offending agent may prevent future lesions but will not dramatically change already existing disease.
When a patient with a suspected occupational dermatosis has not improved within two months after no longer having contact with the suspected agent, other reasons for the persistence of the disease should be explored. However, dermatoses caused by metals such as nickel or chrome have a notoriously prolonged course partly because of their ubiquitous nature. Even removal from work cannot eliminate the workplace as the source of the disease. If these and other potential allergens have been eliminated as causal, it is reasonable to conclude that the dermatitis is either non-occupational or is being perpetuated by non-occupational contacts, such as maintenance and repair of automobiles and boats, tile setting glues, garden plants or including even medical therapy, prescribed or otherwise.