It has often been said that the workforce is the most critical element in the productive apparatus of the organization. Even in highly automated plants with their smaller number of workers, decrements in their health and well-being will sooner or later be reflected in impaired productivity or, sometimes, even in disasters.
Through governmental legislation and regulation, employers have been made responsible for maintaining the safety of the work environment and work practices, and for the treatment, rehabilitation and compensation of workers with occupational injuries and disease. In recent decades, however, employers have begun to recognize that disabilities and absences are costly even when they originate outside the workplace. Consequently, they have begun to provide more and more comprehensive health promotion and protection programs not only for employees but for their families as well. In opening a 1987 meeting of a World Health Organization (WHO) Expert Committee on Health Promotion in the Worksetting, Dr. Lu Rushan, Assistant Director-General of WHO, reiterated that WHO viewed workers’ health promotion as an essential component of occupational health services (WHO 1988).
Why the Workplace?
The rationale for employer sponsorship of health promotion programs includes preventing loss of worker productivity due to avoidable illnesses and disability and their associated absenteeism, improving employee well-being and morale, and controlling the costs of employer-paid health insurance by reducing the amount of health care services required. Similar considerations have stimulated union interest in sponsoring programs, particularly when their members are scattered among many organizations too small to mount effective programs on their own.
The workplace is uniquely advantageous as an arena for health protection and promotion. It is the place where workers congregate and spend a major portion of their waking hours, a fact that makes it convenient to reach them. In addition to this propinquity, their camaraderie and sharing of similar interests and concerns facilitate the development of peer pressures that can be a powerful motivator for participation and persistence in a health promotion activity. The relative stability of the workforce—most workers remain in the same organization for long periods of time—makes for the continuing participation in healthful behaviors necessary to achieve their benefit.
The workplace affords unique opportunities to promote the improved health and well-being of the workers by:
- integrating the health protection and promotion programme into the organization’s efforts to control occupational diseases and injuries
- modifying the structure of the job and its environment in ways that will make it less hazardous and less stressful
- providing employer- or union-sponsored programmes designed to enable employees to cope more effectively with personal or family burdens that may impinge on their well-being and work performance (i.e., modified work schedules and financial assistance benefits and programmes that address alcohol and drug abuse, pregnancy, child care, caring for elderly or disabled family members, marital difficulties or planning for retirement).
Does Health Promotion Work?
There is no doubt of the efficacy of immunizations in preventing infectious diseases or of the value of good occupational health and safety programs in reducing the frequency and severity of work-related diseases and injuries. There is general agreement that early detection and appropriate treatment of incipient diseases will reduce mortality and lower the frequency and extent of residual disability from many diseases. There is growing evidence that elimination or control of risk factors will prevent or, at least, substantially delay the onset of life-threatening diseases such as stroke, coronary artery disease and cancer. There is little doubt that maintaining a healthy lifestyle and coping successfully with psychosocial burdens will improve well-being and functional capacity so as to achieve the goal of wellness defined by the World Health Organization as a state beyond the mere absence of disease. Yet some remain skeptical; even some physicians, at least to judge by their actions.
There is perhaps a higher level of skepticism about the value of worksite health promotion programs. In large part, this reflects the lack of adequately designed and controlled studies, the confounding effect of secular events such as the declining incidence of mortality from heart disease and stroke and, most important, the length of time required for most preventive measures to have their effect. However, in the Health Project report, Freis et al. (1993) summarize the growing literature confirming the effectiveness of worksite health promotion programs in reducing health care costs. In its initial review of over 200 workplace programs, the Health Project, a voluntary consortium of business leaders, health insurers, policy scholars and members of government agencies which advocate health promotion to reduce the demand and the need for health services, found eight with convincing documentation of savings in health care costs.
Pelletier (1991) assembled 24 studies of comprehensive worksite programs published in peer-review journals between 1980 and 1990. (Reports of single-focus programs, such as those dealing with hypertension screening and smoking cessation, even though demonstrated to have been successful, were not included in this review.) He defined “comprehensive programs” as those which “provide an ongoing, integrated program of health promotion and disease prevention that knits the particular components (smoking cessation, stress management, coronary risk reduction, etc.) into a coherent, ongoing program that is consistent with corporate objectives and includes program evaluation.” All of the 24 programs summarized in this review achieved improvement in employees’ health practices, reductions in absenteeism and disability, and/or increases in productivity, while each of these studies that analyzed for impact on health care and disability costs, cost-effectiveness or cost/benefit changes demonstrated a positive effect.
Two years later, Pelletier reviewed an additional 24 studies published between 1991 and the early part of 1993 and found that 23 reported positive health gains and, again, all of those studies which analyzed cost-effectiveness or cost/benefit effects indicated a positive return (Pelletier 1993). Factors common to the successful programs, he noted, included specific program goals and objectives, easy access to the program and facilities, incentives for participation, respect and confidentiality, support of top management and a corporate culture that encourages health promotion efforts (Pelletier 1991).
While it is desirable to have evidence confirming the effectiveness and value of worksite health promotion programs, the fact is that such proof has rarely been required for the decision to initiate a program. Most programs have been based on the persuasive power of the conviction that prevention does work. In some instances, programs have been stimulated by interest articulated by employees and, occasionally, by the unexpected death of a top executive or a key employee from cancer or heart disease and the fond hope that a preventive program will keep “lightning from striking twice”.
Structure of a Comprehensive Program
In many organizations, particularly smaller ones, the health promotion and disease prevention program consists merely of one or more largely ad hoc activities that are informally related to each other, if at all, that have little or no continuity, and that often are triggered by a particular event and abandoned as it fades into memory. A truly comprehensive program should have a formal structure comprising a number of integrated elements, including the following:
- a clear statement of goals and objectives that are approved by management and acceptable to the employees
- explicit endorsement by top management and, where they exist, the labour organizations involved, with the continuing allocation of resources adequate to achieve desired goals and objectives
- appropriate placement in the organization, effective coordination with other health-related activities, and communication of programme plans across divisions and departments to mid-level managers and employees. Some organizations have found it expedient to create a labour-management committee comprising representatives from all levels and segments of the workforce for “political” reasons as well as to provide input on programme design
- designation of a “programme director,” a person with the requisite administrative skills who also has had training and experience in health promotion or has access to a consultant who might supply the necessary expertise
- a mechanism for feedback from participants and, if possible, non-participants as well, in order to confirm the validity of the programme design and to test the popularity and utility of particular programme activities
- procedures for maintaining the confidentiality of personal information
- systematic record-keeping to keep track of activities, participation and outcomes as a basis for monitoring and potential evaluation
- compilation and analysis of available relevant data, ideally for a scientific evaluation of the programme or, when that is not feasible, to generate a periodic report to management to justify continuation of the resource allocation and to form a basis for possible changes in the programme.
Program Objectives and Ideology
The basic objectives of the program are to enhance and maintain the health and well-being of employees on all levels, to prevent disease and disability, and to ease the burden on individuals and the organization when disease and disability cannot be prevented.
The occupational health and safety program is directed to those factors on the job and in the workplace that may affect employees’ health. The wellness program recognizes that their health concerns cannot be confined within the boundaries of the plant or office, that problems arising in the workplace inevitably affect the health and well-being of workers (and, by extension, also their families) in the home and in the community and that, just as inevitably, problems arising outside of work affect attendance and work performance. (The term wellness can be considered the equivalent of the expression health promotion and protection, and has been used increasingly in the field during the last two decades; it epitomizes the World Health Organization’s positive definition of health.) Accordingly, it is quite appropriate for the health promotion program to address problems that some argue are not proper concerns for the organization.
The need to achieve wellness assumes greater urgency when it is recognized that workers with diminished capacities, however acquired, may be potentially hazardous to their co-workers and, in certain jobs, to the public as well.
There are those who hold that, since health is fundamentally a personal responsibility of the individual, it is inappropriate, and even intrusive, for employers or labor unions (or both) to undertake involvement with it. They are correct insofar as overly paternalistic and coercive approaches are employed. However, health-promoting adjustments of the job and the workplace along with enhanced access to health-promoting activities provide the awareness, knowledge and tools that enable employees to address that personal responsibility more effectively.
Program Components
Needs assessment
While the alert program director will take advantage of a particular event that will create interest in a special activity (e.g., the unexpected illness of a popular person in the organization, reports of cases of an infectious disease that raise fears of contagion, warnings of a potential epidemic), the comprehensive program will be based on a more formal needs assessment. This may simply consist of a comparison of the demographic characteristics of the workforce with morbidity and mortality data reported by public health authorities for such population cohorts in the area, or it may comprise the aggregate analyses of company-specific health-related data, such as health care insurance claims and the recorded causes of absenteeism and of disability retirement. Determination of the health status of the workforce through compilation of the results of health screenings, periodic medical examinations and health risk appraisal programs can be supplemented by surveys of employees’ health-related interests and concerns to identify optimal targets for the program. (It should be borne in mind that health problems affecting particular cohorts of employees that warrant attention may be obscured by relying only on data aggregated for the entire workforce.) Such needs assessments are not only useful in selecting and prioritizing program activities but also in planning to “market” them to the employees most likely to find them beneficial. They also provide a benchmark for measuring the effectiveness of the program.
Program elements
A comprehensive health promotion and disease prevention program includes a number of elements, such as the following.
Promoting the program
A constant stream of promotional devices, such as handbills, memoranda, posters, brochures, articles in company periodicals, etc., will serve to call attention to the availability and desirability of participating in the program. With their permission, stories of the accomplishments of individual employees and any awards for achieving health promotion goals they may have earned may be highlighted.
Health assessment
Where possible, each employee’s health status should be assessed on entering the program to provide a basis for a “prescription” of personal objectives to be achieved and of the specific activities that are indicated, and periodically to assess progress and interim changes in health status. The health risk appraisal may be used with or without a medical examination as comprehensive as circumstances permit, and supplemented by laboratory and diagnostic studies. Health screening programs can serve to identify those for whom specific activities are indicated.
Activities
There is a long list of activities that may be pursued as part of the program. Some are continuing, others are addressed only periodically. Some are targeted to individuals or to particular cohorts of the workforce, others to the entire employee population. Prevention of illness and disability is a common thread that runs through each activity. These activities may be divided into the following overlapping categories:
- Clinical services. These require health professionals and include: medical examinations; screening programmes; diagnostic procedures such as mammography; Pap smears and tests for cholesterol level; immunizations and so forth. They also include counseling and behaviour modification in relation to weight control, fitness, smoking cessation and other lifestyle factors.
- Health education. Education to promote awareness of potential diseases, the importance of controlling risk factors, and the value of maintaining healthy lifestyles, for instance, through weight control, fitness training and smoking cessation. Such education should also point the way to appropriate interventions.
- Guidance in managing medical care. Advice should be given with regard to the following concerns: dealing with the health care system and procuring prompt and high-quality medical care; managing chronic or recurrent health problems; rehabilitation and return to work after disease or injury; treatment for alcohol and drug abuse; prenatal care and so on.
- Coping with personal problems. Coping skills to be developed include, for example, stress management, pre-retirement planning and outplacement. Help can also be provided for workers who need to deal with work and family problems such as family planning, prenatal care, dependant care, parenting, and so forth.
- Workplace amenities and policies. Workplace features and policies supplementary to those addressing occupational health and safety activities would include personal washing-up and locker facilities, laundry service where needed, catering facilities offering nutrition advice and helpful food choices, and the establishment of a smoke-free and drug-free workplace, among others.
In general, as programs have developed and expanded and awareness of their effectiveness has spread, the number and variety of activities have grown. Some, however, have been de-emphasized as resources have either been reduced because of financial pressures or shifted to new or more popular areas.
Tools
The tools employed in pursuing health promotion activities are determined by the size and location of the organization, the degree of centralization of the workforce with respect to geography and work schedules; the available resources in terms of money, technology and skills; the characteristics of the workforce (as regards educational and social levels); and the ingenuity of the program director. They include:
- Information gathering: employee surveys; focus groups
- Print materials: books; pamphlets (these may be distributed or displayed in take-away racks); pay envelope stuffers; articles in company publications; posters
- Audiovisual materials: audiotapes; recorded messages accessible by telephone; films; videos for both individual and group viewing. Some organizations maintain libraries of audiotapes and videos which employees may borrow for home use
- Professional health services: medical examinations; diagnostic and laboratory procedures; immunizations; individual counselling
- Training: first aid; cardiopulmonary resuscitation; healthy shopping and cooking
- Meetings: lectures; courses; workshops
- Special events: health fairs; contests
- Self-help and support groups: alcohol and drug abuse; breast cancer; parenting; eldercare
- Committees: an intramural task force or committee to coordinate health-related programmes among different departments and divisions and a labour-management committee for overall programme guidance are often useful. There may also be special committees centred on particular activities
- Sports programmes: intramural sports; the sponsoring of individual participation in community programmes; company teams
- Computer software: available for individual personal computers or accessed through the organization’s network; health-promotion-oriented computer or video games
- Screening programmes: general (e.g., health risk appraisal) or disease specific (e.g., hypertension; vision and hearing; cancer; diabetes; cholesterol)
- Information and referral: employee assistance programmes; telephone resource for personal questioning and advice
- Ongoing activities: physical fitness; healthful food selection in worksite catering facilities and vending machines
- Special benefits: released time for health promotion activities; tuition reimbursement; modified work schedules; leaves of absence for particular personal or family needs
- Incentives: awards for participation or goals achievement; recognition in company publications and on bulletin boards; contests and prizes.
Implementing the Program
In many organizations, particularly smaller ones, health promotion activities are pursued on an ad hoc, haphazard basis, often in response to actual or threatened health “crises” in the workforce or in the community. After a time, however, in larger organizations, they are often pulled together into a more or less coherent framework, labelled “a program,” and made the responsibility of an individual designated as program director, coordinator or given some other title.
Selection of activities for the program may be dictated by the responses to employee interest surveys, secular events, the calendar or the suitability of the available resources. Many programs schedule activities to take advantage of the publicity generated by the categorical voluntary health agencies in connection with their annual fund-raising campaigns, for example, Heart Month, or National Fitness and Sports Week. (Each September in the United States, the National Health Information Center in the Office of Disease Prevention and Health Protection publishes National Health Observances, a list of the designated months, weeks and days devoted to the promotion of particular health issues; it is now also available via electronic mail.)
It is generally agreed that it is prudent to install the program incrementally, adding activities and topics as it gains credibility and support among the employees and to vary the topics to which special emphasis is given so that the program does not become stale. J.P. Morgan & Co., Inc., the large financial organization based in New York City, has instituted an innovative “scheduled cyclical format” in its health promotion program that emphasizes selected topics sequentially over a four-year period (Schneider, Stewart and Haughey 1989). The first year (the Year of the Heart) focuses on cardiovascular disease prevention; the second (the Year of the Body) addresses AIDS and early cancer detection and prevention; the third (the Year of the Mind) deals with psychological and social issues; and the fourth (the Year of Good Health) covers such significant topics as adult immunization, arthritis and osteoporosis, accident prevention, diabetes and healthy pregnancy. At this point, the sequence is repeated. This approach, Schneider and his co-authors state, maximizes involvement of available corporate and community resources, encourages employee participation by sequential attention to different issues, and affords the opportunity for directing attention to program revisions and additions based on medical and scientific advances.
Evaluating the Program
It is always desirable to evaluate the program both to justify continuation of its resource allocations and to identify any need for improvement and to support recommendations for expansion. The evaluation may range from simple tabulations of participation (including drop-outs) coupled with expressions of employee satisfaction (solicited and unsolicited) to more formal surveys. The data obtained by all these means will demonstrate the degree of utilization and the popularity of the program as a whole entity and of its individual components, and are usually readily available soon after the end of the evaluation period.
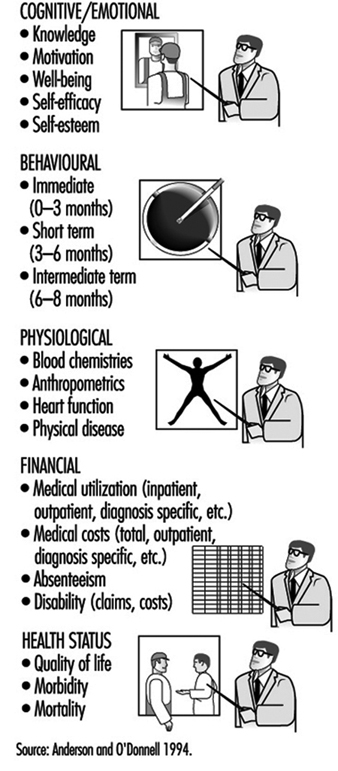
Even more valuable, however, are data reflecting the outcomes of the program. In an article pointing the way to improving evaluations of health promotion programs, Anderson and O’Donnell (1994) offer a classification of areas in which health promotion programs may have significant results (see figure 1).
Figure 1. Categories of health promotion outcomes.
Outcome data, however, require an effort planned prior to the outset of the program, and they have to be collected over a time sufficient to allow the outcome to develop and be measured. For example, one can count the number of individuals who receive an influenza immunization and then follow the total population for a year to demonstrate that those inoculated had a lower incidence of influenza-like respiratory infections than those who refused the inoculation. The study can be enlarged to correlate rates of absenteeism of the two cohorts and compare the program costs with the direct and indirect savings accrued by the organization.
Furthermore, it is not too difficult to demonstrate individuals’ achievement of more desirable profiles of risk factors for cardiovascular disease. However, it will take at least one and probably several decades to demonstrate a reduction in morbidity and mortality from coronary heart disease in an employee population cohort. Even then, the size of that cohort may not be large enough to make such data significant.
The review articles cited above demonstrate that good evaluation research can be done and that it is increasingly being undertaken and reported. There is no question of its desirability. However, as Freis and his co-authors (1993) said, “There are already model programs that improve health and decrease costs. It is not knowledge that is lacking, but penetration of these programs into a greater number of settings.”
Comments and Caveats
Organizations contemplating the launching of a health promotion program should be cognizant of a number of potentially sensitive ethical issues to be considered and a number of pitfalls to avoid, some of which have already been alluded to. They are comprised under the following headings:
Elitism versus egalitarianism
A number of programs exhibit elitism in that some of the activities are limited to individuals above a certain rank. Thus, an in-plant physical fitness facility may be restricted to executives on the grounds that they are more important to the organization, they work longer hours, and they find it difficult to free up the time to go to an outside “health club”. To some, however, this seems to be a “perk” (i.e., a special privilege), like the key to the private washroom, admission to the free executive dining room, and use of a preferred parking space. It is sometimes resented by rank-and-file workers who find visiting a community facility too expensive and are not allowed the liberty of taking time during the working day for exercise.
A more subtle form of elitism is seen in some in-plant fitness facilities when the quota of available memberships is taken up by “jocks” (i.e., exercise enthusiasts) who would probably find ways to exercise anyway. Meanwhile, those who are sedentary and might derive much greater benefit from regular supervised exercise are denied entry. Even when they make it into the fitness program, their continued participation is often discouraged by embarrassment at being outperformed by lower-ranking workers. This is particularly true of the manager whose male self-image is tarnished when he finds that he cannot perform at the level of his female secretary.
Some organizations are more egalitarian. Their fitness facilities are open to all on a first-come, first-served basis, with continuing membership available only to those who use it frequently enough to be of value to them. Others go part of the way by reserving some of the memberships for employees who are being rehabilitated following an illness or injury, or for older workers who may require a greater inducement to participate than their younger colleagues.
Discrimination
In some areas, anti-discrimination laws and regulations may leave the organization open to complaints, or even litigation, if the health promotion program can be shown to have discriminated against certain individuals on the basis of age, sex or membership in minority or ethnic groups. This is not likely to happen unless there is a more pervasive pattern of bias in the workplace culture but discrimination in the health promotion program might trigger a complaint.
Even if formal charges are not made, however, resentment and dissatisfaction, which may be magnified as they are communicated informally among employees, are not conducive to good employee relations and morale.
Concern about allegations of sex discrimination may be exaggerated. For example, even though it is not recommended for routine use in asymptomatic men (Preventive Services Task Force 1989), some organizations offer screening for prostatic cancer to compensate for making Pap tests and mammography available to female employees.
Complaints of discrimination have come from individuals who are denied the opportunity of winning incentive awards because of congenital health problems or acquired diseases that preclude participation in health promotion activities or achieving the ideal personal health goals. At the same time, there is the equity issue of rewarding individuals for correcting a potential health problem (e.g., giving up smoking or losing excess weight) while denying such rewards to individuals who do not have such problems.
“Blaming the victim”
Growing out of the valid concept that health status is a matter of personal responsibility is the notion that individuals are culpable when health defects are found and are to be held guilty for failing to correct them on their own. This sort of thinking fails to take notice of the fact that genetic research is increasingly demonstrating that some defects are hereditary and, therefore, although they may sometimes be modified, are beyond the individual’s capacity to correct.
Examples of “blaming the victim” are (a) the too-prevalent attitude that HIV/AIDS is a fitting retribution for sexual “indiscretions” or intravenous drug use and, therefore, its victims do not deserve compassion and care, and (b) the imposition of financial and bureaucratic barriers that make it difficult for unmarried young women to get adequate prenatal care when they become pregnant.
Most important, focusing in the workplace on individuals’ responsibility for their own health problems tends to obscure the employer’s accountability for factors in job structure and work environment that may be hazardous to health and well-being. Perhaps the classic example is the organization that offers stress management courses to teach employees to cope more effectively but that does not examine and correct features of the workplace that are needlessly stressful.
It must be recognized that hazards present in the workplace may not only affect the workers, and by extension their families as well, but they may also precipitate and aggravate personal health problems generated away from the job. While retaining the concept of individual responsibility for health, it must be balanced by the understanding that factors in the workplace for which the employer is responsible may also have a health-related influence. This consideration highlights the importance of communication and coordination between the health promotion program and the employer’s occupational safety and health and other health-related programs, especially when they are not in the same box on the organization chart.
Persuasion, not coercion
A cardinal tenet of worksite health promotion programs is that participation should be voluntary. Employees should be educated about the desirability of suggested interventions, provided with access to them, and persuaded to participate in them. There often is, however, a narrow margin between enthusiastic persuasion and compulsion, between well-meaning paternalism and coercion. In many instances, the coercion may be more or less subtle: e.g., some health promotion professionals tend to be overly authoritarian; employees may be fearful of embarrassment, being ostracized or even penalized if they reject the advice given them; a worker’s choices as to recommended health promotion activities may be overly limited; and executives may make it unpleasant for their subordinates not to join them in a favorite activity, such as jogging in the very early morning.
While many organizations offer rewards for healthy behavior, for instance, certificates of achievement, prizes, and “risk-rated” health insurance (involving, in the United States, for example, a reduction in the employee’s share of the premiums), a few impose penalties on those who do not meet their arbitrary standards of health behavior. The penalties may range from refusing employment, withholding advancement, or even dismissal or denying benefits that might otherwise be forthcoming. An example of an American firm levying such penalties is E.A. Miller, a meat-packing plant located in Hyrum, Utah, a town of 4,000 inhabitants located some 40 miles north of Salt Lake City (Mandelker 1994). E.A. Miller is the largest employer in this small community and provides group health insurance for its 900 employees and their 2,300 dependants. Its health promotion activities are typical in many ways except that there are penalties for not participating:
- Employees and spouses who do not attend prenatal seminars are not reimbursed for the cost of obstetrical care or of the baby’s care in the hospital. Also, to qualify for the insurance benefits, the pregnant woman must visit a doctor during the first trimester.
- If employees or their dependants smoke, they must contribute over twice as much to their share of group health insurance premiums: $66 per month instead of $30. The plant has had a smoke-free policy since 1991 and the company offers smoking cessation courses onsite or pays employees’ tuition if they take the course in the community.
- The company will not cover any of the medical costs if a covered employee or dependant was injured in an automobile accident while driving under the influence of drugs or alcohol or was not wearing a seat belt, nor will it cover injuries sustained while riding a motorcycle without a helmet.
One form of coercion that has wide acceptance is “job jeopardy” for employees whose alcohol or drug abuse has had an impact on their attendance and work performance. Here, the employee is confronted with the problem and told that disciplinary actions will be stayed as long as he or she continues with the prescribed treatment and remains abstinent. With allowance for an occasional relapse (in some organizations, this is limited to a specific number), failure to comply results in dismissal. Experience has amply shown that the threat of job loss, regarded by some as the most potent stressor encountered in the workplace, is an effective motivator for many individuals with such problems to agree to take part in a program for their correction.
Confidentiality and privacy
Another hallmark of the successful health promotion program is that personal information about participating employees —and non-participants as well—must be kept confidential and, particularly, out of personnel files. To preserve the privacy of such information when it is needed for evaluative tabulations and research, some organizations have set up data bases in which individual employees are identified by code numbers or by some similar device. This is particularly relevant to mass screening and laboratory procedures where clerical errors are not unknown.
Who participates
Health promotion programs are criticized by some on the basis of evidence that participants tend to be younger, healthier and more health conscious than those who do not (the “coals to Newcastle” phenomenon). This presents to those designing and operating programs the challenge of involving those who have more to gain through their participation.
Who pays
Health promotion programs involve some costs to the organization. These may be expressed in terms of financial outlays for services and materials, time taken from work hours, distraction of participating employees, and the burden of management and administration. As noted above, there is increasing evidence that these are more than offset by reduced personnel costs and by improvements in productivity. There are also the less tangible benefits of embellishing the public relations image of the organization and of enhancing its reputation as a good place to work, thereby facilitating recruitment efforts.
Most of the time, the organization will cover the entire cost of the program. Sometimes, particularly when an activity is conducted off the premises in a community-based facility, the participants are required to share its cost. In some organizations, however, all or part of the employee’s portion is refunded on successful completion of the program or course.
Many group health insurance programs cover preventive services provided by health professionals including, for example, immunizations, medical examinations, tests, and screening procedures. Such health insurance coverage, however, presents problems: it may increase the cost of the insurance and the out-of-pocket costs of the deductible fees and co-payments usually required may constitute an effective obstacle to their use by low-salaried workers. In the last analysis, it may be less costly for employers to pay for preventive services directly, saving themselves the administrative costs of processing insurance claims and of reimbursement.
Conflicts of interest
While most health professionals exhibit exemplary integrity, vigilance must be exercised to identify and deal with those who do not. Examples include those who falsify records to make their efforts look good and those who have a relationship with an outside provider of services who provides kickbacks or other rewards for referrals. The performance of outside vendors should be monitored to identify those who underbid to win the contract and then, to save money, use poorly qualified personnel to deliver the services.
A more subtle conflict of interest exists when staff members and vendors subvert the needs and interests of employees in favor of the organization’s goals or the agenda of its managers. This sort of reprehensible action may not be explicit. An example is steering troubled employees into a stress management program without making a strenuous effort to persuade the organization to reduce inordinately high levels of stress in the workplace. Experienced professionals will have no difficulty in properly serving both the employees and the organization, but should be ready to move to a situation in which ethical values are more conscientiously observed whenever improper pressures on the part of management become too great.
Another subtle conflict that may affect employees adversely arises when a relationship of competition, rather than coordination and collaboration, develops between the health promotion program and other health-related activities in the organization. This state of affairs is found not infrequently when they are placed in different areas of the organization chart and report to different lines of management authority. As has been said before, it is critical that, even when part of the same entity, the health promotion program should not operate at the expense of the occupational safety and health program.
Stress
Stress is probably the most pervasive health hazard encountered both in the workplace and away from it. In a landmark survey sponsored by the St. Paul Fire and Marine Insurance Company and involving nearly 28,000 workers in 215 diverse American organizations, Kohler and Kamp (1992) found that work stress was strongly related to employee health and performance problems. They also found that among personal life problems, those created by the job are most potent, showing more impact than purely off-the-job issues such as family, legal or financial problems. This suggests, they said, that “some workers become caught in a downward spiral of work and home life problems—problems on the job create problems at home, which in turn are taken back to work, and so on.” Accordingly, while primary attention should be directed to the control of psychosocial risk factors intrinsic to the job, this should be complemented by health promotion activities aimed at personal stress factors most likely to affect work performance.
Access to health care
A subject worthy of attention in its own right, education in navigating the health care delivery system should be made part of the program with an eye to future needs for health services. This begins with self-care—knowing what to do when signs and symptoms appear and when professional services are needed—and goes on to selecting a qualified health professional or a hospital. It also includes inculcating both the ability to distinguish good from poor health care and an awareness of patients’ rights.
To save employees time and money, some in-plant medical units offer more or less extensive in-plant health services, (often including x rays, laboratory tests and other diagnostic procedures), reporting the results to the employees’ personal physicians. Others maintain a roster of qualified physicians, dentists and other health professionals to whom employees themselves and sometimes also their dependants may be referred. Time off from work to keep medical appointments is an important adjunct where health professional services are not available outside of working hours.
In the United States, even where there is a good group health insurance program, low-salaried workers and their families may find the deductible and coinsurance portions of covered charges to be barriers to procuring recommended health services in all but dire circumstances. Some employers are helping to overcome such obstacles by exempting these employees from such payments or by making special fee arrangements with their health care providers.
Worksite “climate”
Worksite health promotion programs are presented, often explicitly, as an expression of the employer’s concern for the health and well-being of the workforce. That message is contradicted when the employer is deaf to employees’ complaints about working conditions and does nothing to improve them. Employees are not likely to accept or participate in programs offered under such circumstances or at times of labor-management conflict.
Workforce diversity
The health promotion program should be designed to accommodate to the diversity increasingly characteristic of today’s workforce. Differences in ethnic and cultural background, educational levels, age and sex should be recognized in the content and presentation of health promotion activities.
Conclusion
It is clear from all of the above that the worksite health promotion program represents an extension of the occupational safety and health program which, when properly designed and implemented, can benefit individual employees, the workforce as a whole and the organization. In addition, it may also be a force for positive social change in the community.
Over the past few decades, worksite health promotion programs have increased in number and comprehensiveness, in small and medium-sized organizations as well as in larger ones, and in the private, voluntary and public sectors. As demonstrated by the array of articles contained in this chapter, they have also increased in scope, expanding from direct clinical services dealing, for example, with medical examinations and immunizations, to involvement with personal and family problems whose relationship to the workplace may seem more tenuous. One should allow one’s selection of program elements and activities to be guided by the particular characteristics of the workforce, the organization and the community, keeping in mind that some will be needed only by specific cohorts of employees rather than by the population as a whole.
In considering the creation of a worksite health promotion program, readers are advised to plan carefully, to implement incrementally, allowing room for growth and expansion, to monitor performance and program quality and, to the extent possible, evaluate outcomes. The articles in this chapter should prove to be uniquely helpful in such an endeavor.