Infrastructures, Practice and Approaches in Occupational Health
While much progress has been made since the 1980s towards a comprehensive approach in occupational health where the protection and promotion of workers’ health are pursued together with the maintenance and promotion of their working capacity, with a special emphasis on the establishment and maintenance of a safe and healthy working environment for all, there is much room for discussion as to the manner in which occupational health is actually implemented. The expression occupational health practice is currently used to cover the whole spectrum of activities undertaken by employers, workers and their organizations, designers and architects, manufacturers and suppliers, legislators and parliamentarians, labour and health inspectors, work analysts and work organization specialists, standardization organizations, universities and research institutions to protect health and to promote occupational safety and health.
The expression occupational health practice includes the contribution of occupational health professionals, but it is not limited to their practice of occupational health.
Confusion often occurs because the term occupational health services may be used to denote:
- the provision of occupational health services (i.e., the contribution of occupational health professionals to occupational safety and health)
- the institutionalized organizational arrangements to provide such services (i.e., the occupational health services which are part of the infrastructure to protect and promote workers’ health).
In order to overcome this difficulty and several other common causes of misunderstanding, the following wording was used for the second point on the agenda of the Twelfth Session of the Joint ILO/WHO Committee on Occupational Health: “Infrastructures for occupational health practice: options and models for national policies, primary health care approaches, strategies and programmes, and functions of occupational health services” (1995b) with the following understanding of the terms:
- Occupational health practice encompasses the activities of all those who contribute to the protection and promotion of workers’ health and to the improvement of working conditions and environment; these terms should not be understood as merely the practice of occupational health professionals.
- Occupational health approaches embodies a number of principles and approaches to guide action, such as the general principle of primary health care advocated by the WHO and the improvement of the working conditions and environment advocated by the ILO.
- Infrastructures for occupational health practice means the organizational arrangements to implement a national policy and to conduct action at the enterprise level; infrastructures may take the form of “institutionalized” occupational health services and include many other bodies such as national institutes for occupational safety and health.
The use of the key words infrastructures, practice and approaches permits the various actors and partners in prevention to play their individual roles in their respective fields of competence and to act jointly, as well.
Occupational health services contribute to the occupational health practice, which is intrinsically multidisciplinary and intersectoral and involves other specialists both in the enterprise and outside in addition to occupational health and safety professionals, as well as the appropriate governmental authorities, employers, workers and their representatives. Functionally, occupational health services must be considered both a part of country-level health infrastructures as well as of the infrastructures that exist for the implementation of relevant legislation on occupational safety and health. It is a national decision to determine whether such services should be under the supervision of the ministry of labour, the ministry of health, the social security institutions, a tripartite national committee or other bodies.
There are a large number of models for occupational health services. One of them enjoys the support of a large consensus at the international level: the model proposed by the ILO Occupational Health Services Convention (No. 161) and Recommendation (No. 171) adopted by the International Labour Conference in 1985. Countries should consider this model as an objective towards which progress should be made, taking into account, of course, local differences and the availability of specialized personnel and financial resources. A national policy should be adopted to develop progressively occupational health services for all workers, taking into account the specific risks of the undertakings. Such policy should be formulated, implemented and periodically reviewed in the light of national conditions and practice in consultation with the most representative organizations of employers and workers. Plans should be established indicating the steps which will be taken when occupational health services cannot be immediately established for all undertakings.
Multidisciplinary Cooperation and Intersectoral Collaboration: An Overall Perspective
The ILO and the WHO have a common definition of occupational health (see box), which was adopted by the Joint ILO/WHO Committee on Occupational Health at its first session (1950) and revised at its twelfth session (1995).
Governments, in collaboration with employers’ and workers’ organizations and professional organizations concerned, should design adequate and appropriate policies, programmes and plans of action for the development of occupational health with multidisciplinary content and comprehensive coverage. In each country, the scope and content of programmes should be adapted to national needs, should take into account local conditions and should be incorporated into national development plans. The Joint ILO/WHO Committee emphasized that the principles embodied in the ILO Conventions No. 155 and No. 161 and their accompanying Recommendations, as well as WHO resolutions, guidelines and approaches related to occupational health, provide a universally accepted guide for design of such policies and programmes (Joint ILO/WHO Committee on Occupational Health 1992).
Definition of occupational health adopted by the Joint
ILO/WHO Committee on Occupational Health (1950)
Occupational health should aim at the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations; the prevention amongst workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological capabilities and; to summarize: the adaptation of work to man and of each man to his job.
The main focus in occupational health is on three different objectives: (i) the maintenance and promotion of workers’ health and working capacity; (ii) the improvement of working environment and work to become conducive to safety and health and (iii) development of work organizations and working cultures in a direction which supports health and safety at work and in doing so also promotes a positive social climate and smooth operation and may enhance productivity of the undertakings. The concept of working culture is intended in this context to mean a reflection of the essential value systems adopted by the undertaking concerned. Such a culture is reflected in practice in the managerial systems, personnel policy, principles for participation, training policies and quality management of the undertaking.
There are similar features between the ILO strategy for the improvement of the working conditions and environment and the WHO general principle of primary health care. Both rest on similar technical, ethical and social considerations and they both:
- aim at all concerned, workers or the public
- define policies, strategies and means of action
- insist on the responsibility of each employer for the health and safety of the workers in his or her employment
- emphasize primary prevention and the control of risk at the source
- give special importance to information, health education and training
- indicate the need to develop an occupational health practice that is easily accessible to all and available at the workplace
- recognize the central place of participation, community participation in health programmes, inter-sectoral participation and workers’ participation in the improvement of the working conditions and the working environment
- highlight the interactions between health, environment and development, as well as between occupational safety and health and productive employment.
The main focus of ILO activity has been on the provision of international guidelines and a legal framework for the development of occupational health policies and infrastructures on a tripartite basis (including governments, employers and workers) and the practical support for improvement actions at the workplace, while the WHO has concentrated on the provision of scientific backgrounds, methodologies, technical support and on the training of health and related manpower for occupational health (Joint ILO/WHO Committee on Occupational Health 1992).
Multidisciplinary cooperation
For the WHO, occupational health includes safety at work. Hygiene is conceptualized as directed towards disease prevention while safety is thought of as the discipline that prevents bodily injuries due to accidents. For the ILO, occupational safety and health is considered as a discipline aiming at the prevention of work injuries (both occupational diseases and accidents) and at the improvement of working conditions and the environment. The terms occupational safety, occupational health, occupational medicine, occupational hygiene and occupational health nursing are used to acknowledge the contribution of different professions (e.g., engineers, physicians, nurses, hygienists) and in recognition of the fact that the organization of occupational safety and health at the enterprise level very often comprises separate occupational safety services and occupational health services, as well as safety and health committees.
To some extent, occupational safety and primary prevention are more directly linked to the technology which is used, to the process of production and to daily management than is occupational health, which focuses more on the relationships between work and health, in particular on the surveillance of the working environment and of workers’ health (secondary prevention), as well as on human factors and ergonomic aspects. Further, at the enterprise level, engineers are a necessary presence and are inte-gral to the management line (production engineers, maintenance, technicians and so on), while occupational health and hygiene requires the intervention of specialists in the health field who need not be present for the enterprise to function, but can be consultants or belong to an external occupational health service.
Whatever organizational arrangements and terminology are used, the most important thing is that occupational safety and health professionals work as a team. They need not necessarily be in the same unit or service, although this may be desirable where appropriate. The emphasis should not be on the structure of services but on the execution of their functions at the enterprise level in a sound manner (from a scientific, technical and ethical point of view). The emphasis should be on cooperation and coordination in the elaboration and implementation of a programme of action, as well as on the development of unifying concepts, such as “working cultures” (safety culture, labour protection culture, corporate culture) that are conducive to safety and health at work and “continuing quality improvement” of the working conditions and environment.
In 1992, the Joint ILO/WHO Committee emphasized that the scope of occupational health is very broad (as shown in table 1), encompassing disciplines such as occupational medicine, occupational nursing, occupational hygiene, occupational safety, ergonomics, engineering, toxicology, environmental hygiene, occupational psychology and personnel management. Collaboration and participation of employers and workers in occupational health programmes is an essential prerequisite for successful occupational health practice.
Table 1. Six principles and three levels for a sound occupational health practice
|
Principles |
|||||
|
Levels |
Prevention |
Protection |
Adaptation |
Promotion |
Mitigation |
|
Individuals (diversity) |
Accident prevention Industrial hygiene 1920s |
Industrial medicine Personal protective equipment 1930s |
Scientific organization of work Job analysis 1950s |
Employee assistance programmes 1950s |
Treatment compensation 1910s |
|
Groups (exposed groups, special needs) |
Safe and healthy working environment Built-in safety 1970s |
Occupational medicine Machine guarding 1940s |
Ergonomics including design 1950s |
Workers’ health promotion programmes 1980s |
Emergency planning and preparedness 1970s |
|
Society and all workers |
Control technologies Environmental health management 1970s |
Environmental health Epidemiology Preventive health care 1960s |
Appropriate technologies Consumers’ protection 1970s |
Health education and promotion programmes 1970s |
Curative health care 1920s |
Note: The times (1910, 1920, etc.) are arbitrary. Dates are merely given to provide an idea of the time scale for the progressive development of a comprehensive approach in occupational health. Dates will vary from country to country and may indicate the beginning or the full development of a discipline or the appearance of new terms or approaches for a practice which has been carried out for many years. This table does not intend to delineate exact disciplines involved in the process but to present in a concise manner their relationships within the framework of a mutlidisciplinary approach and intersectoral cooperation, towards a safe and healthy working environment and health for all, with a participatory approach and the objective of new forms of development which should be equitable if they are to be sustainable.
The definition of a common goal is one of the solutions to avoid the trap of an excessive compartmentalization of disciplines. Such compartmentalization of disciplines may sometimes be an asset since it allows for a specialized in-depth analysis of the problems. It may often be a negative factor, because it prevents the development of a multidisciplinary approach. There is a need to develop unifying concepts which open fields of cooperation. The new definition of occupational health adopted by the Joint Committee in 1995 serves this purpose.
Sometimes there can be heated arguments as to whether occupational health is a discipline in itself, or is part of labour protection, of environmental health or of public health. When the issue is more than academic and involves such decisions as which organization or ministry is competent for specific subject areas, the outcome can have significant consequences with regard to the allocation of funds and distribution of resources available in the form of expertise and equipment.
One of the solutions to such a problem is to advocate convergent approaches based on the same values with a common objective. The WHO approach of primary health care and the ILO approach of improving the working conditions and environment can serve this purpose. With common values of equity, solidarity, health and social justice in mind, these approaches can be translated into strategies (the WHO’s strategy of occupational health for all) and programmes (the ILO International Programme for the Improvement of Working Conditions and Environment) as well as into plans of action and activities implemented or carried out at the enterprise, national and international levels by all partners in prevention, protection and promotion of workers’ health, independently or jointly.
There are other possibilities. The International Social Security Association (ISSA) proposes the “concept of prevention” as a golden path to social security to address “safety worldwide” at work and at home, on the road and during leisure time. The International Commission on Occupational Health (ICOH) is developing an approach of ethics in occupational health and catalyses a rapprochement and cross-fertilization between occupational health and environment health. A similar trend can be seen in many countries where, for example, professional associations now get together occupational health and environmental health specialists.
Intersectoral collaboration
In 1984, the ILO’s annual International Labour Conference adopted a resolution concerning the improvement of working conditions and environment incorporating the concept that the improvement of the working conditions and environment is an element essential to the promotion of social justice. It stressed that improved working conditions and environment are a positive contribution to national development and represent a measure of success of any economic and social policy. It spelled out three fundamental principles:
- Work should take place in a safe and healthy environment.
- Conditions of work should be consistent with workers’ well-being and human dignity.
- Work should offer real possibilities for personal achievement, self-fulfilment and service to society.
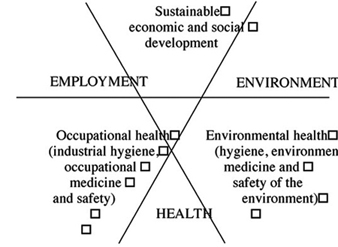
During the 1980s a shift occurred from the concept of development towards the concept of “sustainable development”, which includes “the right to a healthy and productive life in harmony with nature” as indicated in the first principle of the Rio Declaration (United Nations Conference on Environment and Development—UNCED 1992). The objective of a safe and healthy environment has thus become an integral part of the concept of sustainable development, which also implies balancing environment protection with generation of opportunity for employment, improved livelihoods and health for all. Both environmental health and occupational health contribute to make development sustainable, equitable and sound not only from an economic but also from a human, social and ethical point of view. This paradigm shift is illustrated in figure 1.
Figure 1. A multidisciplinary approach towards a sustainable and equitable development
The purpose of this figure is to illustrate the interaction between occupational health and environmental health and their mutually supportive contribution to a sustainable development. It identifies an area which represents the integration of the economic and social objectives which can be met while at the same time taking account of the environment, employment and health.
The WHO Commission on Health and Environment has further recognized that “the kind of development needed to safeguard health and welfare will depend on many conditions, including respect for the environment, while development without regard for the environment would inevitably result in impairment of human health” (WHO 1992). In the same vein, occupational health should be recognized as an “added value”, that is, a positive contribution to national development and a condition of its sustainability.
Of particular significance to the work of the ILO and the WHO are the Declaration and Programme of Action adopted by the World Summit for Social Development held in Copenhagen in 1995. The Declaration commits the nations of the world to pursuing the goal of full, productive and freely chosen employment as a basic priority of their economic and social policies. The Summit clearly indicated that the goal must not be to create just any sort of jobs, but quality jobs that safeguard the basic rights and interests of workers. It made clear that the creation of good quality jobs must include measures to achieve a healthy and safe working environment, to eliminate environmental health hazards and provide for occupational health and safety. This is an indication that the future of occupational health may well be active partnership in reconciling employment, health and environment towards an equitable and sustainable development.
The primary health care approach emphasizes social equity, affordability and accessibility, participation and community involvement, as noted by the Joint ILO/WHO Committee on Occupational Health in 1995. These basic moral and ethical values are common to the ILO and the WHO. The primary health care approach is innovative because it applies social values to preventive and curative health care. This complementarity has not always been clearly understood; sometimes confusion is due to the interpretation of common words, which has led to a degree of misunderstanding in discussing actual roles and activities to be undertaken by the ILO and the WHO, which are complementary and mutually supportive.
Primary health care can be considered to be based on principles of social equity, self-reliance and community development. It may also be considered to be a strategy for reorienting health systems, in order to promote individual and community involvement and collaboration between all sectors concerned with health. A general principle should be that primary health care should incorporate an occupational health component and specialized occupational health services should apply the general principle of primary health care, regardless of the structural model in place.
There are many partners in prevention, sharing the philosophy of both the ILO and the WHO, who should provide the necessary inputs to implement a good occupational practice. The Joint ILO/WHO Committee has indicated that the ILO and the WHO should promote an inclusive approach to occupational health in their member countries. If such an approach is used, occupational health can be seen as a multidisciplinary and integrated subject. Taken in this light, activities of different organizations and ministries will not be competitive or contradictory but will be complementary and mutually supportive, working towards an equitable and sustainable development. The emphasis should be on common goals, unified concepts and basic values.
As pointed out by the Joint ILO/WHO Committee in 1995, there is a need to develop occupational health indicators for the promotion and monitoring of the progression towards health and sustainable development. Forms of development which jeopardize health cannot claim the quality of being equitable or sustainable. Indicators towards “sustainability” necessarily include health indicators, since UNCED emphasized that the commitment of “protecting and promoting human health” is a fundamental principle for sustainable development (Agenda 21, Chapter 6). The WHO has taken a leading role in developing both the concept and use of environmental health indicators, some of which concern health and the working environment.
The WHO and the ILO are expected to develop occupational health indicators which could help countries in the evaluation, both retrospective and prospective, of their occupational health practice, and assist them in monitoring the progress made towards the objectives set by national policies on occupational safety, occupational health and the working environment. The development of such indicators focusing on the interactions between work and health could also assist occupational health services in evaluating and guiding their programmes and their activities to improve the working conditions and environment (i.e., in monitoring the efficiency and the manner in which they carry out their functions).
Standards and Guidance
The ILO Conventions and Recommendations on occupational safety and health define the rights of the workers and allocate duties and responsibilities to appropriate authorities, to the employers, and to the workers in the field of occupational safety and health. The ILO Conventions and Recommendations adopted by the International Labour Conference, taken as a whole, constitute the International Labour Code which defines minimum standards in the labour field.
The ILO policy on occupational health and safety is essentially contained in two international Conventions and their accompanying Recommendations. The ILO Occupational Safety and Health Convention (No. 155) and its Recommendation (No. 164), 1981, provide for the adoption of a national occupational safety and health policy at the national level and describe the actions needed at the national and at the enterprise levels to promote occupational safety and health and to improve the working environment. The ILO Occupational Health Services Convention (No. 161) and its Recommendation (No. 171), 1985, provide for the establishment of occupational health services which will contribute to the implementation of the occupational safety and health policy and will perform their functions at the enterprise level.
These instruments provide for a comprehensive approach to occupational health that includes primary, secondary and tertiary prevention and is consistent with general principles of primary health care. They indicate the manner in which occupational health care should ideally be delivered to the working populations, and propose a model that channels towards the workplace organized activities which require expert staff in order to catalyse an interaction between various disciplines to promote cooperation between all partners in prevention. These instruments also provide an organizational framework wherein occupational health professionals can deliver efficiently quality services to ensure workers’ health protection and promotion and contribute to the health of enterprises.
Functions
Convention No. 161 defines occupational health services as services dedicated to essentially preventive functions and responsible for advising employers, workers and their representatives at the enterprise on the requirements for establishing and maintaining a safe and healthy working environment that will optimize physical and mental health in relation to work and on the adaptation of work to the capabilities of workers, taking into consideration their state of physical and mental health.
The Convention specifies that occupational health services should include those of the following functions that are adequate and appropriate to the occupational risks at the worksite:
- identification and assessment of the risks from health hazards in the workplace
- surveillance of the factors in the working environment and working practices which may affect workers’ health, including sanitary installations, canteens and housing where these facilities are provided by the employer
- advice on planning and organization of work, including the design of workplaces, on the choice, maintenance and condition of machinery and other equipment and on substances used in work
- participation in the development of programmes for the improvement of working practices, as well as testing and evaluation of health aspects of new equipment
- advice on occupational health, safety and hygiene and on ergonomics and individual and collective protective equipment
- surveillance of workers’ health in relation to work
- promoting the adaptation of work to the worker
- contributing to measures of vocational rehabilitation
- collaborating in providing information, training and education in the fields of occupational health and hygiene and ergonomics
- organizing first aid and emergency treatment
- participating in analysis of occupational accidents and occupational diseases.
The ILO Convention and Recommendation are very flexible with regard to the forms of organization of occupational health services. The establishment of occupational health services may be done by laws or regulations, by collective agreements, or in any other manner approved by the appropriate authority, after consultation with the representative organizations of concerned employers and workers. Occupational health services may be organized as a service for a single enterprise or as a service common to a number of enterprises. As far as possible, the occupational health services should be located near the place of employment or should be organized to ensure their proper functioning at the place of employment. They may be organized by the concerned enterprises, by the public authorities or official services, by social security institutions, by any other bodies authorized by the authorities or, indeed, by combination of any of these. This offers a large degree of flexibility and, even in the same country, several or all of these methods may be used, according to local conditions and practice.
The flexibility of the Convention demonstrates that the spirit of the ILO instruments on occupational health services is to place more emphasis on its objectives rather than on the administrative rules for achieving them. It is important to ensure occupational health to all workers, or at least to make progress towards this objective. Such progress is usually achievable by degrees but it is necessary to make some progress towards achieving these aims and to mobilize resources in the most efficient manner for this purpose.
Various methods of financing occupational health exist. In many countries the obligation of establishing and maintaining occupational health services rests with employers. In other countries they are part of national health schemes or public health services. Staffing, financing and training of personnel are not detailed in the Convention but are individual national approaches.
Many examples exist of occupational health services set up by social security institutions or financed by special workers’ insurance schemes. Sometimes their financing is governed by an arrangement agreed upon by the ministry of labour and the ministry of health or by the social security institutions. In some countries trade unions run occupational health services. There are also special arrangements wherein funds are collected from employers by a central institution or tripartite body and then disbursed to provide occupational health care or distributed to finance the functioning of occupational health services.
The sources of financing occupational health services may also vary according to their activities. For example, when they have curative activities, social security may contribute to their financing. If occupational health services take part in public health programmes and in health promotion or in research activities, other funding sources may be found or become available. Financing will depend not only on the structural model chosen to organize the occupational health services, but also on the value that society concedes to health protection and promotion and its willingness to invest in occupational health and in the prevention of occupational hazards.
Conditions of Operation
A special emphasis is placed on the conditions of operation of occupational health services. It is not only necessary for the occupational health services to execute a number of tasks but it is equally important that these tasks should be performed in an appropriate manner, taking into consideration technical and ethical aspects.
There are some basic requirements as regards the operation of occupational health services which are spelled out in the ILO Convention, and especially in the Recommendation on Occupational Health Services. These may be summarized as follows:
- The personnel in occupational health services should be qualified and benefit from a full professional independence.
- Confidentiality should be ensured.
- Workers should be informed of the activities of the services and of the results of their health assessments.
- Employers, workers and their representatives should participate in the operation of the services and in the design of their programmes.
Ethical dimensions of occupational health are increasingly taken into account, and emphasis is placed on the need for both quality and on-going evaluation of occupational health services. It is not only necessary to determine what should be done but also for which purpose and under which conditions. The ILO Recommendation on Occupational Health Services (No. 171) introduced a first set of principles in this respect. Further guidance is given by the International Code of Ethics for Occupational Health Professionals adopted by the International Commission on Occupational Health (ICOH 1992).
In 1995, the Joint ILO/WHO Committee on Occupational Health emphasized that “quality assurance of services must be an integral part of the occupational health services development. It is unethical to give poor quality of service”. The ICOH Code of Ethics prescribes that “occupational health professionals should institute a programme of professional audit of their own activities in order to ensure that appropriate standards have been set, that they are being met and that deficiencies, if any, are detected and corrected”.
Common Goals and Values
The role of institutionalized occupational health services should be seen within the broader framework of health and social policies and infrastructures. The functions of occupational health services contribute to the implementation of the national policies on occupational safety, occupational health and the working environment advocated by the ILO Occupational Safety and Health Convention (No. 155) and Recommendation (No. 164), 1981. Occupational health services contribute also to the attainment of the objectives embodied in the “Health For All” strategy advocated by the WHO as a policy for equity, solidarity and health.
There are signs of an increasing trend to mobilize expertise and resources within the framework of networking arrangements and joint ventures. At the international level, such is already the case for chemical safety, where there is an interorganization me-chanism for chemical safety: the Inter-Organization Programme for the Sound Management of Chemicals (IOMC). There are many other fields where new flexible forms of international cooperation among countries and international organizations are emerging or could be developed, such as radiation protection and biological safety.
Networking arrangements open new fields of cooperation which may be adapted in a flexible manner to the theme which is to be addressed, such as occupational stress, coordinating research or updating this Encyclopaedia. The emphasis is placed on interactions and not any more on vertical compartmentalization of disciplines. The concept of leadership gives way to active partnership. International networking for occupational safety and health is developing rapidly and could be further developed on the basis of existing structures which could be interconnected. The roles of the ILO and the WHO may well be to initiate international networks designed to fulfil the needs and demands of their constituents and to meet the common goal of protecting the people at work.
The social and ethical values agreed upon by the international community are incorporated into the ILO Conventions and Recommendations, as well as in the WHO policy on “Health For All”. Since the 1980s the concept of sustainable development has progressively emerged and, after the Rio Conference and the Social Summit in Copenhagen, now takes into account the interrelationships between employment, health and the environment. The common goal of a safe and healthy working environment for all will reinforce the determination of all those involved in occupational safety and health to better serve the health of workers and to contribute to a sustainable and equitable development for all. One of the main challenges in occupational health may well be to resolve the conflict between values such as the right to health and the right to work at the level both of the individual and all workers, with the aim of protecting health and allowing employment.