The German Berufsgenossenschaften (BG)
Under the social insurance system in Germany, statutory accident insurance covers the results of accidents at work and accidents on the way to and from work, as well as occupational diseases. This statutory accident insurance is organized into three areas:
- industrial accident insurance (represented by the BGs)
- agricultural accident insurance
- public sector’s own accident insurance scheme.
The 35 Berufsgenossenschaften (BG) cover the various branches of the industrial economy in Germany. They are responsible for 39 million employees insured in 2.6 million enterprises. Every person in a work, service or training position is insured, regardless of age, sex or income level. Their umbrella organization is the Central Federation of the Berufsgenossenschaften (HVBG).
By law, the BG is responsible for using all appropriate means to prevent workplace accidents and occupational diseases, to provide effective first aid and optimal medical, occupational and social rehabilitation, and to pay benefits to the injured and sick, and to survivors. Thus prevention, rehabilitation and compensation are all under one roof.
The premiums to finance these benefits are paid exclusively by the employers. In 1993 all industrial employers paid on average DM 1.44 to the BG for every DM 100 wages, or 1.44%. In all, the premiums came to DM 16 billion (US billion used—one thousand million), of which about 80% was spent for rehabilitation and pensions. The remainder was used primarily for prevention programmes.
Occupational Safety and Health Protection
The employer is responsible for the health and safety of the employee at work. The legal scope of this responsibility is set by government in laws and ordinances, and in the protective labour regulations of the industrial BGs, which complete and concretize governmental protective labour law for each branch of industry. The system of prevention of the BGs is notable for its orientation to actual practice, its constant adaptation to the needs of the industry and to the state of technology, as well as for its effective support of the employer and the employee.
The BGs’ tasks of prevention, which are primarily carried out by the Technical Inspection Service (TAD) of the BG and the Occupational Medical Service (AMD), include:
- advising and motivating the employer
- supervising industrial occupational protective measures
- occupational medical care
- informing and training company staff
- safety checking on appliances and equipment
- initiating, carrying out and financing research.
Responsibility for implementing industrial occupational protection lies with the employer, who is legally obliged to hire appropriately qualified personnel to assist in occupational protection. These are specialists in work safety (safety officers, safety technicians and safety engineers) and company doctors. In companies with more than 20 employees, one or more safety representatives must be hired. The scope of the responsibility of the company for occupational safety specialists and company doctors is set by trade association regulations that are specific to the branch of industry and degree of hazard. In companies where an occupational safety specialist or a company doctor is employed, the employer must organize an occupational safety committee, made up of one company representative, two workers’ representatives, the company doctor, and occupational safety specialists and safety representatives. First-aid personnel, whose training is directed by the BG, also belong to the company occupational safety organization.
Occupational medical care has a special significance. Every employee who is at risk for a specific type of health threat at the workplace is examined in a uniform manner, and the results of the examination are assessed according to stated guidelines. In 1993 approximately four million occupational preventive medical examinations were carried out by specially authorized doctors. Lasting health concerns were ascertained in less than 1% of the examinations.
Employees who work with hazardous/carcinogenic materials also have a right to be medically examined even after the hazardous activity has been completed. The BGs have established services to be able to examine these employees. There are now three such services:
- Organizational Service for On-going Examinations (ODIN)
- Central Registration Service for Asbestos Dust-Endangered Employees (ZAs)
- Wismut Central Care Office (ZeBWis).
The three services cared for approximately 600,000 people in 1993. Collecting examination data assists in individual care and also helps improve scientific research for early detection of cancer cases.
Statistics on Workplace Accidents
Goal. The primary goal of collecting statistics on workplace accidents is to improve workplace safety by assessing and interpreting data on accident occurrences. These data are compiled from reports on workplace accidents; 5% to 10% of the accidents (approximately 100,000 accidents) are investigated each year by the Technical Inspection Services of the BGs.
Employers’ reporting responsibility. Every employer is obliged to report a workplace accident to his responsible BG within three days if the accident results in an incapacity to work for three calendar days or causes the death of the insured (“legally reportable workplace accident”). This includes accidents going to or from work. Accidents that cause only property damage or prevent the injured person from working for less than three days do not have to be reported. For reportable workplace accidents, a form “Accident Notification” (figure 1) is submitted by the employer. The time away from work is the significant factor for reporting purposes, regardless of the seriousness of the injury. Accidents that appear harmless must be reported if the injured person cannot work for longer than three days. This three-day requirement facilitates pursuing later claims. Failure to file an accident report, or filing one late, constitutes a violation of regulations that can be punished by the BG with a monetary fine of up to DM 5,000.
Figure 1. An example of an accident notification form
Notification by the attending physician. To optimize medical rehabilitation and to determine how long the employee is unable to work, the injured person receives treatment from a medical specialist selected for this work. The doctor is paid by the responsible industrial BG. Thus, the BG also receives notification of reportable workplace injuries from the doctor if the employer has failed to (promptly) file an accident report. The BG can then request the employer to file a workplace accident notification. This dual reporting system (employer and doctor) assures the BG of receiving knowledge of practically all reportable workplace accidents.
Using the information on the accident notification report and the medical report, the BG checks whether the accident is, in the legal sense, a workplace accident within its jurisdictional competence. On the basis of the medical diagnosis, the BG can, if needed, proceed immediately to ensuring optimal treatment.
A correct and complete description of the circumstances of the accident is especially important for prevention. This enables the BG’s Technical Inspection Service to draw conclusions about defective machinery and equipment that require immediate action to avoid further similar accidents. In the case of serious or fatal workplace accidents, regulations require the employer to immediately notify the BG. These occurrences are immediately investigated by the BG’s occupational safety experts.
In calculating a company’s premium, the BG takes into account the number and cost of workplace accidents that have taken place at this company. A bonus/malus procedure set by law is used in the calculation, and a portion of the company’s premium is determined by the company’s accident trend. This can lead to a higher or lower premium, thus creating financial incentives for employers to maintain safe workplaces.
Collaboration of the employees’ representatives and the safety representatives. Any accident report must also be signed by the workers’ council (Betriebsrat) and by the safety representatives (if these exist). The purpose of this rule is to inform the workers’ council and the safety representatives of the company’s overall accident situation, so that they can effectively exercise their collaborative rights in questions of workplace safety.
Compiling workplace accident statistics. On the basis of the information that the BG receives on a workplace accident from the accident report and the doctor’s report, the accounts are translated into statistical code numbers. The coding covers three areas, among others:
- description of the injured (age, sex, job)
- description of the injury (location of injury, type of injury)
- description of the accident (location, object causing the accident and circumstances of the accident).
Coding is performed by highly trained data specialists who are familiar with the organization of BG industries, utilizing a list of accident and injury codes which contains over 10,000 entries. In order to achieve the highest quality statistics, the classifications are regularly reworked, in order, for example, to adapt them to new technological developments. Furthermore, coding personnel are periodically retrained, and the data are subject to formal-logical and content-sensitive tests.
Uses of workplace accident statistics
An important task of these statistics is to describe the circumstances of the accident at the workplace. Table 1 portrays trends in reportable workplace accidents, new accident pension cases and fatal workplace accidents between 1981 and 1993. Column 3 (“New pension cases”) shows cases for which, because of the seriousness of the accident, a pension payment was first made by the industrial BGs in the given year.
Table 1. Occurrences of workplace accidents, Germany, 1981-93
|
Year |
Workplace accidents |
||
|
Reportable accidents |
New pension cases |
Deaths |
|
|
1981 |
1,397,976 |
40,056 |
1,689 |
|
1982 |
1,228,317 |
39,478 |
1,492 |
|
1983 |
1,144,814 |
35,119 |
1,406 |
|
1984 |
1,153,321 |
34,749 |
1,319 |
|
1985 |
1,166,468 |
34,431 |
1,204 |
|
1986 |
1,212,064 |
33,737 |
1,069 |
|
1987 |
1,211,517 |
32,537 |
1,057 |
|
1988 |
1,234,634 |
32,256 |
1,130 |
|
1989 |
1,262,374 |
30,840 |
1,098 |
|
1990 |
1,331,395 |
30,142 |
1,086 |
|
1991 |
1,587,177 |
30,612 |
1,062 |
|
1992 |
1,622,732 |
32,932 |
1,310 |
|
1993 |
1,510,745 |
35,553 |
1,414 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
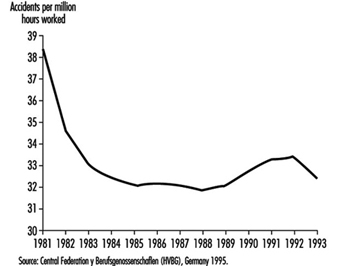
To judge the average accident risk of an insured, the number of workplace accidents is divided by the actual time worked, to produce an accident rate. The rate per one million hours worked is used for comparison internationally and across years. Figure 2 shows how this rate varied between 1981 and 1993.
Figure 2. Frequency of workplace accidents
Industry-specific accident statistics. In addition to describing general trends, workplace statistics can be broken down by industry. For example, one might ask, “How many workplace accidents with portable grinders in the metalworking trade were there in the last few years; how and where did they take place; and what injuries resulted?” Such analyses may be useful to many people and institutions, such as government ministries, supervisory officials, research institutes, universities, businesses and workplace safety experts (table 2).
Table 2. Workplace accidents with portable grinders in metalworking, Germany, 1984-93
|
Year |
Reportable accidents |
New accident pensions |
|
1984 |
9,709 |
79 |
|
1985 |
10,560 |
62 |
|
1986 |
11,505 |
76 |
|
1987 |
11,852 |
75 |
|
1988 |
12,436 |
79 |
|
1989 |
12,895 |
76 |
|
1990 |
12,971 |
78 |
|
1991 |
19,511 |
70 |
|
1992 |
17,180 |
54 |
|
1993 |
17,890 |
70 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
For example, table 2 shows that reportable workplace accidents with portable grinders in metalworking rose continuously from the middle of the 1980s to 1990. From 1990 to 1991 a considerable increase in the accident figures is to be noted. This is an artefact resulting from the inclusion, beginning in 1991, of figures encompassing the new borders of reunited Germany. (The earlier figures cover only the Federal Republic of Germany.)
Other data compiled from accident reports reveal that not all accidents with metalworking portable grinders take place primarily in companies in the metalworking industry. Portable grinders, which of course are often used as angle grinders to cut pipes, iron bars and other objects, are frequently employed on construction sites. Accordingly, nearly one-third of the accidents are concentrated in companies in the construction industry. Working with portable grinders in metalworking results mainly in head and hand injuries. The most common head injuries affect the eyes and the area surrounding the eyes, which are injured by broken pieces, splinters and flying sparks. The tool has a fast-spinning grinding wheel, and hand injuries result when the person using the portable machine loses control of it. The high number of eye injuries proves that the importance and obligation of wearing safety glasses while grinding metal with this portable machine must be emphasized within companies.
Comparison of accident rates within and between industries. Although in 1993 there were nearly 18,000 workplace accidents with portable grinders in metalworking, compared to only 2,800 workplace accidents with hand-held power saws in woodworking, one cannot automatically conclude that this machinery poses a greater risk to metalworkers. To assess accident risk for specific industries, the number of accidents must first be related to a measure of exposure to danger, such as hours worked (see “Risk analysis of nonfatal workplace injuries and illnesses” [REC05AE]). However, this information is not always available. Therefore, a surrogate rate is derived as the proportion which serious accidents make of all reportable accidents. Comparing the serious-injury proportions for portable grinders in metalworking and portable circular saws in woodworking demonstrates that portable circular saws have an accident seriousness rate ten times higher than portable grinders. For prioritizing workplace safety measures, this is an important finding. This type of comparative risk analysis is an important component of an overall industrial accident prevention strategy.
Occupational Disease Statistics
Definition and reporting
In Germany an occupational disease is legally defined as a disease whose cause can be traced to the occupational activity of the affected person. An official list of occupational diseases exists. Therefore, assessing whether a sickness constitutes an occupational disease is both a medical and legal question and is referred by public law to the BG. If an occupational disease is suspected, it is not sufficient to prove that the employee suffers from, for example, an eczema. Additional knowledge is required about substances used at work and their potential for harming the skin.
Compiling occupational disease statistics. Because the BGs are responsible for compensating workers with occupational diseases as well as for providing rehabilitation and prevention, they have a considerable interest in application of statistics derived from occupational disease reports. These applications include targeting preventive measures on the basis of identified high-risk industries and occupations, and also providing their findings to the public, the scientific community and political authorities.
To support these activities, the BGs introduced in 1975 a set of occupational disease statistics, which contain data on every occupational disease report and its final determination—whether recognized or denied—including the reasons for the decision at the level of the individual case. This data base contains anonymous data on:
- the person, such as sex, year of birth, nationality
- diagnosis
- hazardous exposures
- the legal decision, including outcome of claim, determination of disability and any further actions taken by the BGs.
Results of the occupational disease statistics. An important function of the occupational disease statistics is to track the occurrence of occupational diseases over time. Table 3 charts the notifications of suspected occupational disease, the number of recognized occupational disease cases overall and the payment of pensions, as well as the number of fatal cases between 1980 and 1993. It should be cautioned that these data are not easy to interpret, since definitions and criteria differ widely. Furthermore, during this time period the number of officially designated occupational diseases rose from 55 to 64. Also, the figures from 1991 encompass the new borders of reunited Germany, whereas the earlier ones cover the Federal Republic of Germany alone.
Table 3. Occurrences of occupational disease, Germany, 1980-93
|
Year |
Notifications |
Recognized occupational disease cases |
Of those with |
Occupational disease fatalities |
|
1980 |
40,866 |
12,046 |
5,613 |
1,932 |
|
1981 |
38,303 |
12,187 |
5,460 |
1,788 |
|
1982 |
33,137 |
11,522 |
4,951 |
1,783 |
|
1983 |
30,716 |
9,934 |
4,229 |
1,557 |
|
1984 |
31,235 |
8,195 |
3,805 |
1,558 |
|
1985 |
32,844 |
6,869 |
3,439 |
1,299 |
|
1986 |
39,706 |
7,317 |
3,317 |
1,548 |
|
1987 |
42,625 |
7,275 |
3,321 |
1,455 |
|
1988 |
46,280 |
7,367 |
3,660 |
1,363 |
|
1989 |
48,975 |
9,051 |
3,941 |
1,281 |
|
1990 |
51,105 |
9,363 |
4,008 |
1,391 |
|
1991 |
61,156 |
10,479 |
4,570 |
1,317 |
|
1992 |
73,568 |
12,227 |
5,201 |
1,570 |
|
1993 |
92,058 |
17,833 |
5,668 |
2,040 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
Example: infectious diseases. Table 4 shows the decline in the number of recognized cases of infectious diseases during the period 1980 to 1993. It specifically singles out viral hepatitis, for which one can clearly see that a strongly declining trend developed from approximately the mid-1980s in Germany, when employees at risk in the health service were given preventive inoculations. Thus occupational disease statistics can serve not only to find high rates of illnesses, but can also document the successes of protective measures. Declines in disease rates may of course have other explanations. In Germany, for example, the reduction in the number of cases of silicosis during the past two decades is chiefly a result of the decline in the number of jobs in mining.
Table 4. Infectious diseases recognized as occupational diseases, Germany, 1980-93
|
Year |
Total recognized cases |
Of those: hepatitis viral |
|
1980 |
1173 |
857 |
|
1981 |
883 |
736 |
|
1982 |
786 |
663 |
|
1983 |
891 |
717 |
|
1984 |
678 |
519 |
|
1985 |
417 |
320 |
|
1986 |
376 |
281 |
|
1987 |
224 |
152 |
|
1988 |
319 |
173 |
|
1989 |
303 |
185 |
|
1990 |
269 |
126 |
|
1991 |
224 |
121 |
|
1992 |
282 |
128 |
|
1993 |
319 |
149 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
Sources of Information
The HVBG, as umbrella organization for the BGs, centralizes the common statistics and produces analyses and brochures. Furthermore, the HVBG sees statistical information as an aspect of the overall information that must be available to carry out the broad range of mandated responsibilities of the accident insurance system. For this reason, the Central Information System of the BGs (ZIGUV) was formed in 1978. It prepares relevant literature and makes it available to the BGs.
Workplace safety as an interdisciplinary, comprehensive approach requires optimum access to information. The BGs in Germany have resolutely taken this path and thereby made a considerable contribution to the efficient workplace safety system in Germany.