People are increasingly working at high altitudes. Mining operations, recreational facilities, modes of transportation, agricultural pursuits and military campaigns are often at high altitude, and all of these require human physical and mental activity. All such activity involves increased requirements for oxygen. A problem is that as one ascends higher and higher above sea level, both the total air pressure (the barometric pressure, PB) and the amount of oxygen in the ambient air (that portion of total pressure due to oxygen, PO2) progressively fall. As a result, the amount of work we can accomplish progressively decreases. These principles affect the workplace. For example, a tunnel in Colorado was found to require 25% more time to complete at an altitude of 11,000 ft than comparable work at sea level, and altitude effects were implicated in the delay. Not only is there increased muscular fatigue, but also, deterioration of mental function. Memory, computation, decision making and judgement all become impaired. Scientists doing calculations at the Mona Loa Observatory at an altitude above 4,000 m on the island of Hawaii have found they require more time to perform their calculations and they make more mistakes than at sea level. Because of the increasing scope, magnitude, variety and distribution of human activities on this planet, more people are working at high altitude, and effects of altitude become an occupational issue.
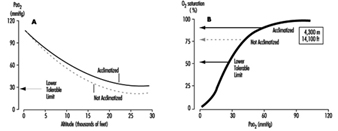
Fundamentally important to occupational performance at altitude is maintaining the oxygen supply to the tissues. We (and other animals) have defences against low oxygen states (hypoxia). Chief among these is an increase in breathing (ventilation), which begins when the oxygen pressure in the arterial blood (PaO2) decreases (hypoxemia), is present for all altitudes above sea level, is progressive with altitude and is our most effective defence against low oxygen in the environment. The process whereby breathing increases at high altitude is called ventilatory acclimatization. The importance of the process can be seen in figure 1, which shows that the oxygen pressure in the arterial blood is higher in acclimatized subjects than in unacclimatized subjects. Further, the importance of acclimatization in maintaining the arterial oxygen pressure increases progressively with increasing altitude. Indeed, the unacclimatized person is unlikely to survive above an altitude of 20,000 ft, whereas acclimatized persons have been able to climb to the summit of Mount Everest (29,029 ft, 8,848 m) without artificial sources of oxygen.
Figure 1. Ventilatory acclimatization
Mechanism
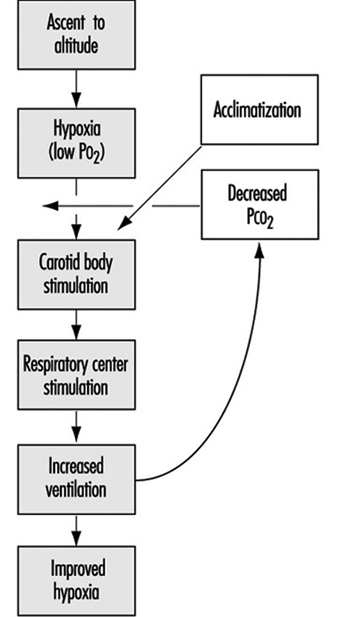
The stimulus for the increase in ventilation at high altitude largely and almost exclusively arises in a tissue which monitors the oxygen pressure in the arterial blood and is contained within an organ called the carotid body, about the size of a pinhead, located at a branch point in each of the two carotid arteries, at the level of the angle of the jaw. When the arterial oxygen pressure falls, nerve-like cells (chemoreceptor cells) in the carotid body sense this decrease and increase their firing rate along the 9th cranial nerve, which carries the impulses directly to the respiratory control centre in the brain stem. When the respiratory centre receives increased numbers of impulses, it stimulates an increase in the frequency and depth of breathing via complex nerve pathways, which activate the diaphragm and the muscles of the chest wall. The result is an increased amount of air ventilated by the lungs, figure 2, which in turn acts to restore the arterial oxygen pressure. If a subject breathes oxygen or air enriched with oxygen, the reverse happens. That is, the chemoreceptor cells decrease their firing rate, which decreases the nerve traffic to the respiratory centre, and breathing decreases. These small organs on each side of the neck are very sensitive to small changes in oxygen pressure in the blood. Also, they are almost entirely responsible for maintaining the body’s oxygen level, for when both of them are damaged or removed, ventilation no longer increases when blood oxygen levels fall. Thus an important factor controlling breathing is the arterial oxygen pressure; a decrease in oxygen level leads to an increase in breathing, and an increase in oxygen level leads to a decrease in breathing. In each case the result is, in effect, the body’s effort to maintain blood oxygen levels constant.
Figure 2. Sequence of events in acclimatization
Time course (factors opposing the increase in ventilation at altitude)
Oxygen is required for the sustained production of energy, and when oxygen supply to tissues is reduced (hypoxia), tissue function may become depressed. Of all organs, the brain is most sensitive to lack of oxygen, and, as noted above, centres within the central nervous system are important in the control of breathing. When we breathe a low-oxygen mixture, the initial response is an increase in ventilation, but after 10 minutes or so the increase is blunted to some extent. While the cause for this blunting is not known, its suggested cause is depression of some central neural function related to the ventilation pathway, and has been called hypoxic ventilatory depression. Such depression has been observed shortly after ascent to high altitude. The depression is transient, lasting only a few hours, possibly because there is some tissue adaptation within the central nervous system.
Nevertheless, some increase in ventilation usually begins immediately on going to high altitude, although time is required before maximum ventilation is achieved. On arrival at altitude, increased carotid body activity attempts to increase ventilation, and thereby to raise the arterial oxygen pressure back to the sea level value. However, this presents the body with a dilemma. An increase in breathing causes an increased excretion of carbon dioxide (CO2) in the exhaled air. When CO2 is in body tissues, it creates an acid aqueous solution, and when it is lost in exhaled air, the body fluids, including blood, become more alkaline, thus altering the acid-base balance in the body. The dilemma is that ventilation is regulated not only to keep oxygen pressure constant, but also for acid-base balance. CO2 regulates breathing in the opposite direction from oxygen. Thus when the CO2 pressure (i.e., the degree of acidity somewhere within the respiratory centre) rises, ventilation rises, and when it falls, ventilation falls. On arrival at high altitude, any increase in ventilation caused by the low oxygen environment will lead to a fall in CO2 pressure, which causes alkalosis and acts to oppose the increased ventilation (figure 2). Therefore, the dilemma on arrival is that the body cannot maintain constancy in both oxygen pressure and acid-base balance. Human beings require many hours and even days to regain proper balance.
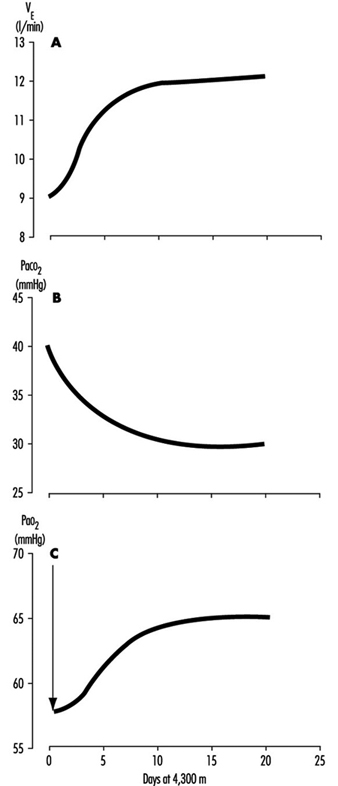
One method for rebalancing is for the kidneys to increase alkaline bicarbonate excretion in the urine, which compensates for the respiratory loss of acidity, thus helping to restore the body’s acid-base balance toward the sea-level values. The renal excretion of bicarbonate is a relatively slow process. For example, on going from sea level to 4,300 m (14,110 ft), acclimatization requires from seven to ten days (figure 3). This action of the kidneys, which reduces the alkaline inhibition of ventilation, was once thought to be the major reason for the slow increase in ventilation following ascent, but more recent research assigns a dominant role to a progressive increase in the sensitivity of the hypoxic sensing ability of the carotid bodies during the early hours to days following ascent to altitude. This is the interval of ventilatory acclimatization. The acclimatization process allows, in effect, ventilation to rise in response to low arterial oxygen pressure even though the CO2 pressure is falling. As the ventilation rises and CO2 pressure falls with acclimatization at altitude, there is a resultant and concomitant rise in oxygen pressure within the lung alveoli and the arterial blood.
Figure 3. Time course of ventilatory acclimatization for sea level subjects taken to 4,300 m altitude
Because of the possibility of transient hypoxic ventilatory depression at altitude, and because acclimatization is a process which begins only upon entering a low oxygen environment, the minimal arterial oxygen pressure occurs upon arrival at altitude. Thereafter, the arterial oxygen pressure rises relatively rapidly for the initial days and thereafter increases more slowly, as in figure 3. Because the hypoxia is worse soon after arrival, the lethargy and symptoms which accompany altitude exposure are also worse during the first hours and days. With acclimatization, a restored sense of well-being usually develops.
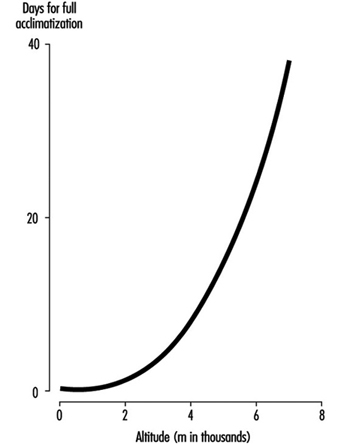
The time required for acclimatization increases with increasing altitude, consistent with the concept that greater increase in ventilation and acid-base adjustments require longer intervals for renal compensation to occur. Thus while acclimatization may require three to five days for a sea-level native to acclimatize at 3,000 m, for altitudes above 6,000 to 8,000 m, complete acclimatization, even if it is possible, may require six weeks or more (figure 4). When the altitude-acclimatized person returns to sea level, the process reverses. That is, the arterial oxygen pressure now rises to the sea-level value and ventilation falls. Now there is less CO2 exhaled, and CO2 pressure rises in the blood and in the respiratory centre. The acid-base balance is altered toward the acid side, and the kidneys must retain bicarbonate to restore balance. Although the time required for the loss of acclimatization is not as well understood, it seems to require approximately as long an interval as the acclimatization process itself. If so, then return from altitude, hypothetically, gives a mirror image of altitude ascent, with one important exception: arterial oxygen pressures immediately become normal on descent.
Figure 4. Effects of altitude on barometric pressure and inspired PO2
Variability among individuals
As might be expected, individuals vary with regard to time required for, and magnitude of, ventilatory acclimatization to a given altitude. One very important reason is the large variation between individuals in the ventilatory response to hypoxia. For example, at sea level, if one holds the CO2 pressure constant, so that it does not confound the ventilatory response to low oxygen, some normal persons show little or no increase in ventilation, while others show a very large (up to fivefold) increase. The ventilatory response to breathing low-oxygen mixtures seems to be an inherent characteristic of an individual, because family members behave more alike than do persons who are not related. Those persons who have poor ventilatory responses to low oxygen at sea level, as expected, also seem to have smaller ventilatory responses over time at high altitude. There may be other factors causing inter-individual variability in acclimatization, such as variability in the magnitude of ventilatory depression, in the function of the respiratory centre, in sensitivity to acid-base changes, and in renal handling of bicarbonate, but these have not been evaluated.
Sleep
Poor sleep quality, particularly before there is ventilatory acclimatization, is not only a common complaint, but also a factor that will impair occupational efficiency. Many things interfere with the act of breathing., including emotions, physical activity, eating and the degree of wakefulness. Ventilation decreases during sleep, and the capacity for breathing to be stimulated by low oxygen or high CO2 also decreases. Respiratory rate and depth of breathing both decrease. Further, at high altitude, where there are fewer oxygen molecules in the air, the amount of oxygen stored in the lung alveoli between breaths is less. Thus if breathing ceases for a few seconds (called apnoea, which is a common event at high altitude), the arterial oxygen pressure falls more rapidly than at sea level, where, in essence, the reservoir for oxygen is greater.
Periodic cessation of breathing is almost universal during the first few nights following ascent to high altitude. This is a reflection of the respiratory dilemma of altitude, described earlier, working in cyclic fashion: hypoxic stimulation increases ventilation, which in turn lowers carbon dioxide levels, inhibits breathing, and increases hypoxic stimulation, which again stimulates ventilation. Usually there is an apnoeic period of 15 to 30 seconds, followed by several very large breaths, which often briefly awakens the subject, after which there is another apnoea. The arterial oxygen pressure sometimes falls to alarming levels as a result of the apnoeic periods. There may be frequent awakenings, and even when total sleep time is normal its fragmentation impairs sleep quality such that there is the impression of having had a restless or sleepless night. Giving oxygen eliminates the cycling of hypoxic stimulation, and alkalotic inhibition abolishes the periodic breathing and restores normal sleep.
Middle-aged males in particular also are at risk for another cause of apnoea, namely intermittent obstruction of the upper airway, the common cause of snoring. While intermittent obstruction at the back of the nasal passages usually causes only annoying noise at sea level, at high altitude, where there is a smaller reservoir of oxygen in the lungs, such obstruction may lead to severely low levels of arterial oxygen pressure and poor sleep quality.
Intermittent Exposure
There are work situations, particularly in the Andes of South America, that require a worker to spend several days at altitudes above 3,000 to 4,000 m, and then to spend several days at home, at sea level. The particular work schedules (how many days are to be spent at altitude, say four to 14, and how many days, say three to seven, at sea level) are usually determined by the economics of the workplace more than by health considerations. However, a factor to be considered in the economics is the interval required both for acclimatization and loss of acclimatization to the altitude in question. Particular attention should be placed on the worker’s sense of well-being and performance on the job on arrival and the first day or two thereafter, regarding fatigue, time required to perform routine and non-routine functions, and errors made. Also strategies should be considered to minimize the time required for acclimatization at altitude, and to improve function during the waking hours.