This article describes aspects of radiation safety programmes. The objective of radiation safety is to eliminate or minimize harmful effects of ionizing radiation and radioactive material on workers, the public and the environment while allowing their beneficial uses.
Most radiation safety programmes will not have to implement every one of the elements described below. The design of a radiation safety programme depends on the types of ionizing radiation sources involved and how they are used.
Radiation Safety Principles
The International Commission on Radiological Protection (ICRP) has proposed that the following principles should guide the use of ionizing radiation and the application of radiation safety standards:
- No practice involving exposures to radiation should be adopted unless it produces sufficient benefit to the exposed individuals or to society to offset the radiation detriment it causes (the justification of a practice).
- In relation to any particular source within a practice, the magnitude of individual doses, the number of people exposed, and the likelihood of incurring exposures where these are not certain to be received should all be kept as low as reasonably achievable (ALARA), economic and social factors being taken into account. This procedure should be constrained by restrictions on the doses to individuals (dose constraints), so as to limit the inequity likely to result from the inherent economic and social judgements (the optimization of protection).
- The exposure of individuals resulting from the combination of all the relevant practices should be subject to dose limits, or to some control of risk in the case of potential exposures. These are aimed at ensuring that no individual is exposed to radiation risks that are judged to be unacceptable from these practices in any normal circumstances. Not all sources are susceptible of control by action at the source and it is necessary to specify the sources to be included as relevant before selecting a dose limit (individual dose and risk limits).
Radiation Safety Standards
Standards exist for radiation exposure of workers and the general public and for annual limits on intake (ALI) of radionuclides. Standards for concentrations of radionuclides in air and in water can be derived from the ALIs.
The ICRP has published extensive tabulations of ALIs and derived air and water concentrations. A summary of its recommended dose limits is in table 1.
Table 1. Recommended dose limits of the International Commission on Radiological Protection1
|
Application |
Dose limit |
|
|
Occupational |
Public |
|
|
Effective dose |
20 mSv per year averaged over |
1 mSv in a year3 |
|
Annual equivalent dose in: |
||
|
Lens of the eye |
150 mSv |
15 mSv |
|
Skin4 |
500 mSv |
50 mSv |
|
Hands and feet |
500 mSv |
- |
1 The limits apply to the sum of the relevant doses from external exposure in the specified period and the 50-year committed dose (to age 70 years for children) from intakes in the same period.
2 With the further provision that the effective dose should not exceed 50 mSv in any single year. Additional restrictions apply to the occupational exposure of pregnant women.
3 In special circumstances, a higher value of effective dose could be allowed in a single year, provided that the average over 5 years does not exceed 1 mSv per year.
4 The limitation on the effective dose provides sufficient protection for the skin against stochastic effects. An additional limit is needed for localized exposures in order to prevent deterministic effects.
Dosimetry
Dosimetry is used to indicate dose equivalents that workers receive from external radiation fields to which they may be exposed. Dosimeters are characterized by the type of device, the type of radiation they measure and the portion of the body for which the absorbed dose is to be indicated.
Three main types of dosimeters are most commonly employed. They are thermoluminescent dosimeters, film dosimeters and ionization chambers. Other types of dosimeters (not discussed here) include fission foils, track-etch devices and plastic “bubble” dosimeters.
Thermoluminescent dosimeters are the most commonly used type of personnel dosimeter. They take advantage of the principle that when some materials absorb energy from ionizing radiation, they store it such that later it can be recovered in the form of light when the materials are heated. To a high degree, the amount of light released is directly proportional to the energy absorbed from the ionizing radiation and hence to the absorbed dose the material received. This proportionality is valid over a very wide range of ionizing radiation energy and absorbed dose rates.
Special equipment is necessary to process thermoluminescent dosimeters accurately. Reading the thermoluminescent dosimeter destroys the dose information contained in it. However, after appropriate processing, thermoluminescent dosimeters are reusable.
The material used for thermoluminescent dosimeters must be transparent to the light it emits. The most common materials used for thermoluminescent dosimeters are lithium fluoride (LiF) and calcium fluoride (CaF2). The materials may be doped with other materials or made with a specific isotopic composition for specialized purposes such as neutron dosimetry.
Many dosimeters contain several thermoluminescent chips with different filters in front of them to allow discrimination between energies and types of radiation.
Film was the most popular material for personnel dosimetry before thermoluminescent dosimetry became common. The degree of film darkening depends on the energy absorbed from the ionizing radiation, but the relationship is not linear. Dependence of film response on total absorbed dose, absorbed dose rate and radiation energy is greater than that for thermoluminescent dosimeters and can limit film’s range of applicability. However, film has the advantage of providing a permanent record of the absorbed dose to which it was exposed.
Various film formulations and filter arrangements may be used for special purposes, such as neutron dosimetry. As with thermoluminescent dosimeters, special equipment is needed for proper analysis.
Film is generally much more sensitive to ambient humidity and temperature than thermoluminescent materials, and can give falsely high readings under adverse conditions. On the other hand, dose equivalents indicated by thermoluminescent dosimeters may be affected by the shock of dropping them on a hard surface.
Only the largest of organizations operate their own dosimetry services. Most obtain such services from companies specializing in providing them. It is important that such companies be licensed or accredited by appropriate independent authorities so that accurate dosimetry results are assured.
Self-reading, small ionization chambers, also called pocket chambers, are used to obtain immediate dosimetry information. Their use is often required when personnel must enter high or very high radiation areas, where personnel could receive a large absorbed dose in a short period of time. Pocket chambers often are calibrated locally, and they are very sensitive to shock. Consequently, they should always be supplemented by thermoluminescent or film dosimeters, which are more accurate and dependable but do not provide immediate results.
Dosimetry is required for a worker when he or she has a reasonable probability of accumulating a certain percentage, usually 5 or 10%, of the maximum permissible dose equivalent for the whole-body or certain parts of the body.
A whole-body dosimeter should be worn somewhere between the shoulders and the waist, at a point where the highest exposure is anticipated. When conditions of exposure warrant, other dosimeters may be worn on fingers or wrists, at the abdomen, on a band or hat at the forehead, or on a collar, to assess localized exposure to extremities, a foetus or embryo, the thyroid or the lenses of the eyes. Refer to appropriate regulatory guidelines about whether dosimeters should be worn inside or outside protective garments such as lead aprons, gloves and collars.
Personnel dosimeters indicate only the radiation to which the dosimeter was exposed. Assigning the dosimeter dose equivalent to the person or organs of the person is acceptable for small, trivial doses, but large dosimeter doses, especially those greatly exceeding regulatory standards, should be analysed carefully with respect to dosimeter placement and the actual radiation fields to which the worker was exposed when estimating the dose that the worker actually received. A statement should be obtained from the worker as part of the investigation and included in the record. However, much more often than not, very large dosimeter doses are the result of deliberate radiation exposure of the dosimeter while it was not being worn.
Bioassay
Bioassay (also called radiobioassay) means the determination of kinds, quantities or concentrations, and, in some cases, the locations of radioactive material in the human body, whether by direct measurement (in vivo counting) or by analysis and evaluation of materials excreted or removed from the human body.
Bioassay is usually used to assess worker dose equivalent due to radioactive material taken into the body. It also can provide an indication of the effectiveness of active measures taken to prevent such intake. More rarely it may be used to estimate the dose a worker received from a massive external radiation exposure (for example, by counting white blood cells or chromosomal defects).
Bioassay must be performed when a reasonable possibility exists that a worker may take or has taken into his or her body more than a certain percentage (usually 5 or 10%) of the ALI for a radionuclide. The chemical and physical form of the radionuclide sought in the body determines the type of bioassay necessary to detect it.
Bioassay can consist of analysing samples taken from the body (for example, urine, faeces, blood or hair) for radioactive isotopes. In this case, the amount of radioactivity in the sample can be related to the radioactivity in the person’s body and subsequently to the radiation dose that the person’s body or certain organs have received or are committed to receive. Urine bioassay for tritium is an example of this type of bioassay.
Whole or partial body scanning can be used to detect radionuclides that emit x or gamma rays of energy reasonably detectable outside the body. Thyroid bioassay for iodine-131 (131I) is an example of this type of bioassay.
Bioassay can be performed in-house or samples or personnel can be sent to a facility or organization that specializes in the bioassay to be performed. In either case, proper calibration of equipment and accreditation of laboratory procedures is essential to ensure accurate, precise, and defensible bioassay results.
Protective Clothing
Protective clothing is supplied by the employer to the worker to reduce the possibility of radioactive contamination of the worker or his or her clothing or to partially shield the worker from beta, x, or gamma radiation. Examples of the former are anti-contamination clothing, gloves, hoods and boots. Examples of the latter are leaded aprons, gloves and eyeglasses.
Respiratory Protection
A respiratory protection device is an apparatus, such as a respirator, used to reduce a worker’s intake of airborne radioactive materials.
Employers must use, to the extent practical, process or other engineering controls (for example, containment or ventilation) to limit the concentrations of the radioactive materials in air. When this is not possible for controlling the concentrations of radioactive material in air to values below those that define an airborne radioactivity area, the employer, consistent with maintaining the total effective dose equivalent ALARA, must increase monitoring and limit intakes by one or more of the following means:
- control of access
- limitation of exposure times
- use of respiratory protection equipment
- other controls.
Respiratory protection equipment issued to workers must comply with applicable national standards for such equipment.
The employer must implement and maintain a respiratory protection programme that includes:
- air sampling sufficient to identify the potential hazard, permit proper equipment selection and estimate exposures
- surveys and bioassays, as appropriate, to evaluate actual intakes
- testing of respirators for operability immediately prior to each use
- written procedures regarding selection, fitting, issuance, maintenance and testing of respirators, including testing for operability immediately prior to each use; supervision and training of personnel; monitoring, including air sampling and bioassays; and record-keeping
- determination by a physician prior to the initial fitting of respirators, and periodically at a frequency determined by a physician, that the individual user is medically fit to use the respiratory protection equipment.
The employer must advise each respirator user that the user may leave the work area at any time for relief from respirator use in the event of equipment malfunction, physical or psychological distress, procedural or communication failure, significant deterioration of operating conditions, or any other conditions that might require such relief.
Even though circumstances may not require routine use of respirators, credible emergency conditions may mandate their availability. In such cases, the respirators also must be certified for such use by an appropriate accrediting organization and maintained in a condition ready for use.
Occupational Health Surveillance
Workers exposed to ionizing radiation should receive occupational health services to the same extent as workers exposed to other occupational hazards.
General preplacement examinations assess the overall health of the prospective employee and establish baseline data. Previous medical and exposure history should always be obtained. Specialized examinations, such as of lens of the eye and blood cell counts, may be necessary depending on the nature of the expected radiation exposure. This should be left to the discretion of the attending physician.
Contamination Surveys
A contamination survey is an evaluation of the radiological conditions incident to the production, use, release, disposal or presence of radioactive materials or other sources of radiation. When appropriate, such an evaluation includes a physical survey of the location of radioactive material and measurements or calculations of levels of radiation, or concentrations or quantities of radioactive material present.
Contamination surveys are performed to demonstrate compliance with national regulations and to evaluate the extent of radiation levels, concentrations or quantities of radioactive material, and the potential radiological hazards that could be present.
The frequency of contamination surveys is determined by the degree of potential hazard present. Weekly surveys should be performed in radioactive waste storage areas and in laboratories and clinics where relatively large amounts of unsealed radioactive sources are used. Monthly surveys suffice for laboratories that work with small amounts of radioactive sources, such as laboratories that perform in vitro testing using isotopes such as tritium, carbon-14 (14C), and iodine-125 (125I) with activities less than a few kBq.
Radiation safety equipment and survey meters must be appropriate for the types of radioactive material and radiations involved, and must be properly calibrated.
Contamination surveys consist of measurements of ambient radiation levels with a Geiger-Mueller (G-M) counter, ionization chamber or scintillation counter; measurements of possible α or βγ surface contamination with appropriate thin-window G-M or zinc sulphide (ZnS) scintillation counters; and wipe tests of surfaces to be later counted in a scintillation (sodium iodide (NaI)) well counter, a germanium (Ge) counter or a liquid scintillation counter, as appropriate.
Appropriate action levels must be established for ambient radiation and contamination measurement results. When an action level is exceeded, steps must be taken immediately to mitigate the detected levels, restore them to acceptable conditions and prevent unnecessary personnel exposure to radiation and the uptake and spread of radioactive material.
Environmental Monitoring
Environmental monitoring refers to collecting and measuring environmental samples for radioactive materials and monitoring areas outside the environs of the workplace for radiation levels. Purposes of environmental monitoring include estimating consequences to humans resulting from the release of radionuclides to the biosphere, detecting releases of radioactive material to the environment before they become serious and demonstrating compliance with regulations.
A complete description of environmental monitoring techniques is beyond the scope of this article. However, general principles will be discussed.
Environmental samples must be taken that monitor the most likely pathway for radionuclides from the environment to man. For example, soil, water, grass and milk samples in agricultural regions around a nuclear power plant should be taken routinely and analysed for iodine-131 (131I) and strontium-90 (90Sr) content.
Environmental monitoring can include taking samples of air, ground water, surface water, soil, foliage, fish, milk, game animals and so on. The choices of which samples to take and how often to take them should be based on the purposes of the monitoring, although a small number of random samples may sometimes identify a previously unknown problem.
The first step in designing an environmental monitoring programme is to characterize the radionuclides being released or having the potential for being accidentally released, with respect to type and quantity and physical and chemical form.
The possibility of transport of these radionuclides through the air, ground water and surface water is the next consideration. The objective is to predict the concentrations of radionuclides reaching humans directly through air and water or indirectly through food.
The bioaccumulation of radionuclides resulting from deposition in aquatic and terrestrial environments is the next item of concern. The goal is to predict the concentration of radionuclides once they enter the food chain.
Finally, the rate of human consumption of these potentially contaminated foodstuffs and how this consumption contributes to human radiation dose and resultant health risk are examined. The results of this analysis are used to determine the best approach to environmental sampling and to ensure that the goals of the environmental monitoring programme are met.
Leak Tests of Sealed Sources
A sealed source means radioactive material that is encased in a capsule designed to prevent leakage or escape of the material. Such sources must be tested periodically to verify that the source is not leaking radioactive material.
Each sealed source must be tested for leakage before its first use unless the supplier has provided a certificate indicating that the source was tested within six months (three months for α emitters) before transfer to the present owner. Each sealed source must be tested for leakage at least once every six months (three months for α emitters) or at an interval specified by the regulatory authority.
Generally, leak tests on the following sources are not required:
- sources containing only radioactive material with a half-life of less than 30 days
- sources containing only radioactive material as a gas
- sources containing 4 MBq or less of βγ-emitting material or 0.4 MBq or less of α-emitting material
- sources stored and not being used; however, each such source must be tested for leakage before any use or transfer unless it has been leakage-tested within six months before the date of use or transfer
- seeds of iridium-192 (192Ir) encased in nylon ribbon.
A leak test is performed by taking a wipe sample from the sealed source or from the surfaces of the device in which the sealed source is mounted or stored on which radioactive contamination might be expected to accumulate or by washing the source in a small volume of detergent solution and treating the entire volume as the sample.
The sample should be measured so that the leakage test can detect the presence of at least 200 Bq of radioactive material on the sample.
Sealed radium sources require special leak test procedures to detect leaking radon (Rn) gas. For example, one procedure involves keeping the sealed source in a jar with cotton fibres for at least 24 hours. At the end of the period, the cotton fibres are analysed for the presence of Rn progeny.
A sealed source found to be leaking in excess of allowable limits must be removed from service. If the source is not repairable, it should be handled as radioactive waste. The regulatory authority may require that leaking sources be reported in case the leakage is a result of a manufacturing defect worthy of further investigation.
Inventory
Radiation safety personnel must maintain an up-to-date inventory of all radioactive material and other sources of ionizing radiation for which the employer is responsible. The organization’s procedures must ensure that radiation safety personnel are aware of the receipt, use, transfer and disposal of all such material and sources so that the inventory can be kept current. A physical inventory of all sealed sources should be done at least once every three months. The complete inventory of ionizing radiation sources should be verified during the annual audit of the radiation safety programme.
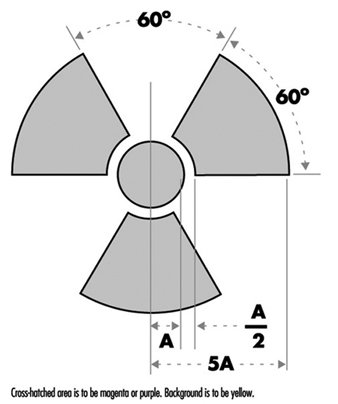
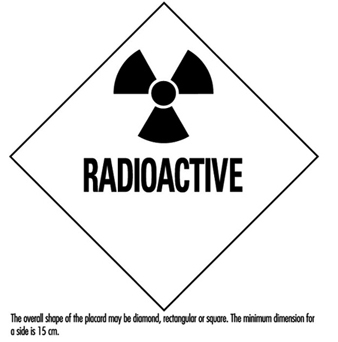
Posting of Areas
Figure 1 shows the international standard radiation symbol. This must appear prominently on all signs denoting areas controlled for the purposes of radiation safety and on container labels indicating the presence of radioactive materials.
Figure 1. Radiation symbol
Areas controlled for the purposes of radiation safety are often designated in terms of increasing dose rate levels. Such areas must be conspicuously posted with a sign or signs bearing the radiation symbol and the words “CAUTION, RADIATION AREA,” “CAUTION (or DANGER), HIGH RADIATION AREA,” or “GRAVE DANGER, VERY HIGH RADIATION AREA,” as appropriate.
- A radiation area is an area, accessible to personnel, in which radiation levels could result in an individual receiving a dose equivalent in excess of 0.05 mSv in 1 h at 30 cm from the radiation source or from any surface that the radiation penetrates.
- A high radiation area is an area, accessible to personnel, in which radiation levels could result in an individual receiving a dose equivalent in excess of 1 mSv in 1 h at 30 cm from the radiation source or from any surface that the radiation penetrates.
- A very high radiation area is an area, accessible to personnel, in which radiation levels could result in an individual receiving an absorbed dose in excess of 5 Gy in 1 h at 1 m from a radiation source or from any surface that the radiation penetrates.
If an area or room contains a significant amount of radioactive material (as defined by the regulatory authority), the entrance to such area or room must be conspicuously posted with a sign bearing the radiation symbol and the words “CAUTION (or DANGER), RADIOACTIVE MATERIALS”.
An airborne radioactivity area is a room or area in which airborne radioactivity exceeds certain levels defined by the regulatory authority. Each airborne radioactivity area must be posted with a conspicuous sign or signs bearing the radiation symbol and the words “CAUTION, AIRBORNE RADIOACTIVITY AREA” or “DANGER, AIRBORNE RADIOACTIVITY AREA”.
Exceptions for these posting requirements may be granted for patients’ rooms in hospitals where such rooms are otherwise under adequate control. Areas or rooms in which the sources of radiation are to be located for periods of eight hours or less and are otherwise constantly attended under adequate control by qualified personnel need not be posted.
Access Control
The degree to which access to an area must be controlled is determined by the degree of the potential radiation hazard in the area.
Control of access to high radiation areas
Each entrance or access point to a high radiation area must have one or more of the following features:
- a control device that, upon entry into the area, causes the level of radiation to be reduced below that level at which an individual might receive a dose of 1 mSv in 1 h at 30 cm from the radiation source or from any surface that the radiation penetrates
- a control device that energizes a conspicuous visible or audible alarm signal so that the individual entering the high radiation area and the supervisor of the activity are made aware of the entry
- entryways that are locked, except during periods when access to the area is required, with positive control over each individual entry.
In place of the controls required for a high radiation area, continuous direct or electronic surveillance that is capable of preventing unauthorized entry may be substituted.
The controls must be established in a way that does not prevent individuals from leaving the high radiation area.
Control of access to very high radiation areas
In addition to the requirements for a high radiation area, additional measures must be instituted to ensure that an individual is not able to gain unauthorized or inadvertent access to areas in which radiation levels could be encountered at 5 Gy or more in 1 h at 1 m from a radiation source or any surface through which the radiation penetrates.
Markings on Containers and Equipment
Each container of radioactive material above an amount determined by the regulatory authority must bear a durable, clearly visible label bearing the radiation symbol and the words “CAUTION, RADIOACTIVE MATERIAL” or “DANGER, RADIOACTIVE MATERIAL”. The label must also provide sufficient information - such as the radionuclide(s) present, an estimate of the quantity of radioactivity, the date for which the activity is estimated, radiation levels, kinds of materials and mass enrichment - to permit individuals handling or using the containers, or working in the vicinity of the containers, to take precautions to avoid or minimize exposures.
Prior to removal or disposal of empty uncontaminated containers to unrestricted areas, the radioactive material label must be removed or defaced, or it must be clearly indicated that the container no longer contains radioactive materials.
Containers need not be labelled if:
- the containers are attended by an individual who takes the precautions necessary to prevent the exposure of individuals in excess of the regulatory limits
- containers, when they are in transport, are packaged and labelled in accordance with appropriate transportation regulations
- containers are accessible only to individuals authorized to handle or use them, or to work in the vicinity of the containers, if the contents are identified to these individuals by a readily available written record (examples of containers of this type are containers in locations such as water-filled canals, storage vaults or hot cells); the record must be retained as long as the containers are in use for the purpose indicated on the record; or
- the containers are installed in manufacturing or process equipment, such as reactor components, piping and tanks.
Warning Devices and Alarms
High radiation areas and very high radiation areas must be equipped with warning devices and alarms as discussed above. These devices and alarms can be visible or audible or both. Devices and alarms for systems such as particle accelerators should be automatically energized as part of the start-up procedure so that personnel will have time to vacate the area or turn off the system with a “scram” button before radiation is produced. “Scram” buttons (buttons in the controlled area that, when pressed, cause radiation levels to drop immediately to safe levels) must be easily accessible and prominently marked and displayed.
Monitor devices, such as continuous air monitors (CAMs), can be preset to emit audible and visible alarms or to turn off a system when certain action levels are exceeded.
Instrumentation
The employer must make available instrumentation appropriate for the degree and kinds of radiation and radioactive material present in the workplace. This instrumentation may be used to detect, monitor or measure the levels of radiation or radioactivity.
The instrumentation must be calibrated at appropriate intervals using accredited methods and calibration sources. The calibration sources should be as much as possible like the sources to be detected or measured.
Types of instrumentation include hand-held survey instruments, continuous air monitors, hand-and-feet portal monitors, liquid scintillation counters, detectors containing Ge or NaI crystals and so on.
Radioactive Material Transportation
The International Atomic Energy Agency (IAEA) has established regulations for the transportation of radioactive material. Most countries have adopted regulations compatible with IAEA radioactive shipment regulations.
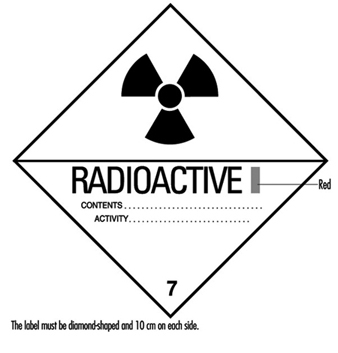
Figure 2. Category I - WHITE label
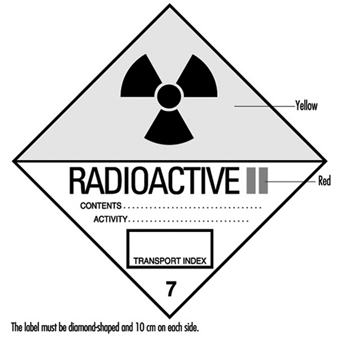
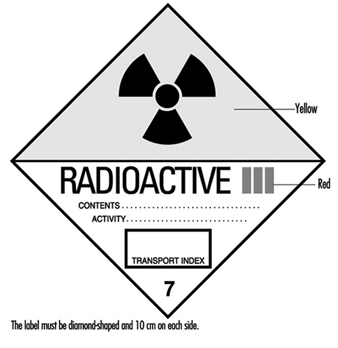
Figure 2, figure 3 and figure 4 are examples of shipping labels that IAEA regulations require on the exterior of packages presented for shipment that contain radioactive materials. The transport index on the labels shown in figure 3 and figure 4 refer to the highest effective dose rate at 1 m from any surface of the package in mSv/h multiplied by 100, then rounded up to the nearest tenth. (For example, if the highest effective dose rate at 1 m from any surface of a package is 0.0233 mSv/h, then the transport index is 2.4.)
Figure 3. Category II - YELLOW label
Figure 5 shows an example of a placard that ground vehicles must prominently display when carrying packages containing radioactive materials above certain amounts.
Figure 5. Vehicle placard
Packaging intended for use in shipping radioactive materials must comply with stringent testing and documentation requirements. The type and quantity of radioactive material being shipped determines what specifications the packaging must meet.
Radioactive material transportation regulations are complicated. Persons who do not routinely ship radioactive materials should always consult experts experienced with such shipments.
Radioactive Waste
Various radioactive waste disposal methods are available, but all are controlled by regulatory authorities. Therefore, an organization must always confer with its regulatory authority to ensure that a disposal method is permissible. Radioactive waste disposal methods include holding the material for radioactive decay and subsequent disposal without regard to radioactivity, incineration, disposal in the sanitary sewerage system, land burial and burial at sea. Burial at sea is often not permitted by national policy or international treaty and will not be discussed further.
Radioactive waste from reactor cores (high-level radioactive waste) presents special problems with regard to disposal. Handling and disposal of such wastes is controlled by national and international regulatory authorities.
Often radioactive waste may have a property other than radioactivity that by itself would make the waste hazardous. Such wastes are called mixed wastes. Examples include radioactive waste that is also a biohazard or is toxic. Mixed wastes require special handling. Refer to regulatory authorities for proper disposition of such wastes.
Holding for radioactive decay
If the half-life of the radioactive material is short (generally less than 65 days) and if the organization has enough storage space, the radioactive waste can be held for decay with subsequent disposal without regard to its radioactivity. A holding period of at least ten half-lives usually is sufficient to make radiation levels indistinguishable from background.
The waste must be surveyed before it may be disposed of. The survey should employ instrumentation appropriate for the radiation to be detected and demonstrate that radiation levels are indistinguishable from background.
Incineration
If the regulatory authority allows incineration, then usually it must be demonstrated that such incineration does not cause the concentration of radionuclides in air to exceed permissible levels. The ash must be surveyed periodically to verify that it is not radioactive. In some circumstances it may be necessary to monitor the stack to ensure that permissible air concentrations are not being exceeded.
Disposal in the sanitary sewerage system
If the regulatory authority allows such disposal, then usually it must be demonstrated that such disposal does not cause the concentration of radionuclides in water to exceed permissible levels. Material to be disposed of must be soluble or otherwise readily dispersible in water. The regulatory authority often sets specific annual limits to such disposal by radionuclide.
Land burial
Radioactive waste not disposable by any other means will be disposed of by land burial at sites licensed by national or local regulatory authorities. Regulatory authorities control such disposal tightly. Waste generators usually are not allowed to dispose of radioactive waste on their own land. Costs associated with land burial include packaging, shipping and storage expenses. These costs are in addition to the cost of the burial space itself and can often be reduced by compacting the waste. Land burial costs for radioactive waste disposal are rapidly escalating.
Programme Audits
Radiation safety programmes should be audited periodically for effectiveness, completeness and compliance with regulatory authority. The audit should be done at least once a year and be comprehensive. Self-audits are usually permissible but audits by independent outside agencies are desirable. Outside agency audits tend to be more objective and have a more global point of view than local audits. An auditing agency not associated with day-to-day operations of a radiation safety programme often can identify problems not seen by the local operators, who may have become accustomed to overlooking them.
Training
Employers must provide radiation safety training to all workers exposed or potentially exposed to ionizing radiation or radioactive materials. They must provide initial training before a worker begins work and annual refresher training. In addition, each female worker of child-bearing age must be provided special training and information about the effects of ionizing radiation on the unborn child and about appropriate precautions she should take. This special training must be given when she is first employed, at annual refresher training, and if she notifies her employer that she is pregnant.
All individuals working in or frequenting any portion of an area access to which is restricted for the purposes of radiation safety:
- must be kept informed of the storage, transfer or use of radioactive materials or of radiation in such portions of the restricted area
- must be instructed in the health protection problems associated with exposure to such radioactive materials or radiation, in precautions or procedures to minimize exposure, and in the purposes and functions of protective devices employed
- must be instructed in, and instructed to observe, to the extent within the worker’s control, the applicable provisions of national and employer regulations for the protection of personnel from exposures to radiation or radioactive materials occurring in such areas
- must be instructed of their responsibility to report promptly to the employer any condition which may lead to or cause a violation of national or employer regulations or unnecessary exposure to radiation or to radioactive material
- must be instructed in the appropriate response to warnings made in the event of any unusual occurrence or malfunction that may involve exposure to radiation or radioactive material
- must be advised as to the radiation exposure reports that workers may request.
The extent of radiation safety instructions must be commensurate with potential radiological health protection problems in the controlled area. Instructions must be extended as appropriate to ancillary personnel, such as nurses who attend radioactive patients in hospitals and fire-fighters and police officers who might respond to emergencies.
Worker Qualifications
Employers must ensure that workers using ionizing radiation are qualified to perform the work for which they are employed. The workers must have the background and experience to perform their jobs safely, particularly with reference to exposure to and use of ionizing radiation and radioactive materials.
Radiation safety personnel must have the appropriate knowledge and qualifications to implement and operate a good radiation safety programme. Their knowledge and qualifications must be at least commensurate with the potential radiological health protection problems that they and the workers are reasonably likely to encounter.
Emergency Planning
All but the smallest operations that use ionizing radiation or radioactive materials must have emergency plans in place. These plans must be kept current and exercised on a periodic basis.
Emergency plans should address all credible emergency situations. The plans for a large nuclear power plant will be much more extensive and involve a much larger area and number of people than the plans for a small radioisotope laboratory.
All hospitals, especially in large metropolitan areas, should have plans for receiving and caring for radioactively contaminated patients. Police and fire-fighting organizations should have plans for dealing with transportation accidents involving radioactive material.
Record Keeping
The radiation safety activities of an organization must be fully documented and appropriately retained. Such records are essential if the need arises for past radiation exposures or radioactivity releases and for demonstrating compliance with regulatory authority requirements. Consistent, accurate and comprehensive record keeping must receive high priority.
Organizational Considerations
The position of the person primarily responsible for radiation safety must be placed in the organization so that he or she has immediate access to all echelons of workers and management. He or she must have free access to areas to which access is restricted for purposes of radiation safety and the authority to halt unsafe or illegal practices immediately.