Employees in occupations that respond to hazardous-substance emergencies or incidents can be broadly classified as hazardous-response personnel. A hazardous-substance emergency or incident can be defined as an uncontrolled or illegal release or threatened release of a hazardous material or its hazardous by-products. A hazardous-substance emergency can arise from a transportation-related incident or at a fixed-site facility. Transportation-related incidents can occur as a result of accidents on land, water or in the air. Fixed-site facilities include industrial facilities, commercial office buildings, schools, farms or any other fixed site that contains hazardous materials.
Employees whose primary responsibility is response to hazardous-materials incidents are generally considered members of hazardous materials (HAZMAT) response teams. HAZMAT team professionals include public-sector employees such as fire-fighters, police and transportation officials who have received specialized training in managing hazardous-substance emergencies. Fixed-site facilities such as manufacturing plants, oil refineries or research laboratories often have internal HAZMAT teams who are trained to manage hazardous-materials incidents inside their facilities. Environmental regulations may necessitate that such facilities report incidents to public agencies when the surrounding community is at risk, or if a threshold quantity of a regulated hazardous material has been released. Public health professionals with training in exposure assessment and hazardous materials management, such as industrial (occupational) hygienists, are often members of public- or private-sector HAZMAT teams.
Police and fire personnel are frequently the first professionals to respond to hazardous-substance emergencies, since they may encounter a leak or release of a hazardous substance associated with a transportation accident or structural fire. These employees are typically considered to be first responders, and their primary responsibility is to isolate the public from the release by denying public access to the site of the incident. This is generally achieved through physical control measures such as physical barriers and crowd- and traffic-control measures. First responders typically do not take actions to contain or control the release. First responders may be at greater risk of exposure to hazardous materials than other HAZMAT teams since they may encounter a hazardous-material release without the benefit of full personal protective equipment, or encounter an unexpected exposure. First responders typically notify HAZMAT team members to manage the incident. The specific health concerns of police and fire personnel are described elsewhere in this chapter.
The primary responsibility of the HAZMAT team is to contain and control the release. This activity can be very hazardous when the incident involves explosive or highly toxic materials such as chlorine gas. The incident commander is responsible for deciding what actions should be taken to resolve the emergency. It may take a considerable amount of time to develop a plan of control for complex accidents such as a multiple railroad car derailment or a chemical plant explosion and fire. In some circumstances where mitigation measures involve a significant risk of major injury to HAZMAT personnel, a decision may be reached not to take specific containment measures, and the hazardous material may be released into the environment.
The final phase of a hazardous-substance emergency often involves the clean-up of residual hazardous substances. This is frequently done by labourers. In some jurisdictions, health and safety regulations mandate that such workers receive specialized training in hazardous-material response and participate in a programme of medical surveillance. These employees may be at a greater risk of exposure since clean-up operations can involve close contact with the hazardous materials. Other occupations at risk of chemical exposure from hazardous-substance emergencies are emergency heath-care providers including emergency medical technicians, paramedics, emergency room medical staff and other hospital personnel.
Potential Hazards
The potential hazards associated with a hazardous-substance emergency are incident specific and can include chemical, radiological and biological hazards. These agents can be gases or vapours, aerosols including mists, fumes, dusts or particulates, solids and/or liquids. The potential hazards faced by hazardous-substance response personnel depend on the exposure potential of the agent, reactivity (flammability, explosivity and so on) and toxicity potential.
Information regarding the type of agents involved in hazardous-substance emergencies is available in the United States from the Agency for Toxic Substances and Disease Registry (ATSDR) Hazardous Substances Emergency Events Surveillance (HSEES) system. The HSEES system is an active surveillance system which tracks incidents that have a public-health impact (Hall et al. 1994). The HSEES system was developed because of reported deficiencies in other national US systems that track releases of hazardous substances (Binder 1989). HSEES does not identify all releases since limited spills at fixed-site facilities are not recorded. The registry was established in 1990 and initially involved five states, but has grown to include eleven states. In 1993 HSEES recorded 3,945 hazardous-substances emergencies. Other countries and states also have systems that record hazardous-material events (Winder et al. 1992).
HSEES data summarizing the types of chemical substances released during hazardous substance emergencies including those associated with personnel injuries, during the two-year period 1990–1992 showed that the most common chemical classes of substances released were volatile organic compounds, herbicides, acids and ammonia. The greatest risk of developing an injury occurred during incidents involving cyanides, insecticides, chlorine, acids and bases. During 1990–1992, 93% of the incidents involved the release of only one chemical, and 84% of the releases occurred at fixed-site facilities.
Health Outcomes
Hazardous-substance personnel face several distinct types of acute health threats. The first category of health threat relates to the toxicity potential of the agent as well as potential contact with blood and other body fluids of incident victims. The second threat is the risk of sustaining major physical trauma including burns associated with an explosion and/or fire from an unexpected chemical reaction, or with structural collapse of a building or container. The third type of acute health effect is risk of heat stress or exhaustion associated with performing heavy work, often in chemical protective clothing, which impairs the body’s efficiency of evaporative cooling. Employees with pre-existing health problems such as cardiovascular disease, respiratory disease, diabetes, disorders of consciousness, or those who take medications that may impair heat exchange or cardiorespiratory response to exercise, are at additional risk when performing such arduous work.
There is limited information concerning the health outcomes of hazardous-substance personnel responding to hazardous-substance emergencies. The HSEES registry indicated that for 1990 to 1992, 467, or 15%, of 4,034 emergency response events resulted in 446 injuries. Two hundred of the injured persons were classified as first responders, including fire-fighters, law-enforcement personnel, emergency medical response personnel and HAZMAT team members. Nearly one-quarter of first responders (22%) did not utilize any type of personal protective equipment.
The principle reported health effects among all persons sustaining injuries included respiratory irritation (37.3%), eye irritation (22.8%) and nausea (8.9%). Chemical burns were reported in 6.1% of those injured. Heat stress was reported in 2%. Eleven deaths were recorded, including one in a first responder. The causes of death among the entire group were reported as trauma, chemical burns, asphyxiation, thermal burns, heat stress and cardiac arrest. Other reports have suggested that first responders are at risk of being injured in acute responses.
The health risks associated with chronic exposures to a wide array of hazardous-materials incidents have not been characterized. Epidemiological studies have not been completed of HAZMAT team members. Epidemiological studies of fire-fighters who perform first response activities at fire scenes have revealed that they may be at greater risk of developing several types of malignancies (see the article “Firefighting hazards” in this chapter).
Preventive Measures
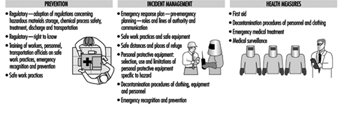
Several measures can reduce the incident of hazardous-substance emergencies. These are described in figure 1. First, prevention through the adoption and enforcement of regulations involving production, storage, transportation and use of hazardous substances can lessen the potential for unsafe work practices. Training of employees in proper workplace practices and hazard management is critical in preventing accidents.
Figure 1. Preventive guidelines.
Second, proper management and supervision of the incident can lessen the impact of an incident. The management of the activities of the first responders and clean-up workers by the incident commander is critical. There must be supervision and evaluation of the progress of the emergency response to ensure that the response objectives are being met safely, effectively and efficiently.
The third measure includes health-related actions that are taken during and after an incident. These actions include the provision of appropriate first aid at the scene and proper decontamination procedures. Failure to properly decontaminate a victim may result in ongoing absorption of the hazardous agent and place the HAZMAT or medical staff at risk of exposure from direct patient contact (Cox 1994). Medical personnel should also be trained regarding specific treatment and personal protective measures for unusual chemical events.
Participation in a medical surveillance programme by workers is a measure that can be utilized to prevent health problems among hazardous-response personnel. Medical surveillance can potentially detect conditions at an early stage before significant adverse health effects have occurred in workers. In addition, medical conditions which may place employees at significantly greater risk from performing the work, such as cardiovascular disease, can be identified and monitored. Sensory impairments that can interfere with field communications, including hearing and vision defects, can also be identified to determine whether they would pose a significant threat during hazardous emergency response.
Most of the identified preventive measures are based upon community awareness of local hazards. Implementation of hazardous-substance emergency plans by adequately trained staff and the wise allocation of resources are imperative. Community awareness of hazards includes informing communities of hazardous materials which are at fixed facilities or materials that are being transported through a community (e.g., by road, rail, airport or water). This information should enable fire departments and other agencies to plan for emergency incidents. Fixed facilities and transporters of hazardous materials should also have individual response plans developed that include specific provisions for notification of public agencies in a timely manner. Emergency medical personnel should have the necessary knowledge of the potential hazards in their local community. Trained medical staff should be available to provide appropriate treatment and diagnosis for the symptoms, signs and specific treatment recommendations for hazardous substances in their communities. Fixed site facilities should establish liaisons with local emergency departments and inform them of potential hazards in the workplace and the need for special supplies or mediations needed to manage potential incidents at these facilities. Planning and training should help enhance the provision of appropriate medical care and decrease the number of injuries and deaths from incidents.
The potential also exists for hazardous-substance emergencies to occur as a result of a natural disaster such as floods, earthquakes, lightning, hurricanes, winds or severe storms. Although the number of such events appears to be increasing, planning and preparation for these potential emergencies is very limited (Showalter and Myers 1994). Planning efforts need to include natural causes of emergency incidents.