Health care is a labour intensive industry and, in most countries, health care workers (HCWs) constitute a major sector of the workforce. They comprise a wide range of professional, technical and support personnel working in a large variety of settings. In addition to health professionals, laboratory technicians, pharmacists, social workers and others involved in clinical services, they include administrative and clerical personnel, housekeeping and dietary staff, laundry workers, engineers, electricians, painters and maintenance workers who repair and refurbish the building and the equipment it contains. In contrast with those providing direct care, these support workers usually have only casual, incidental contact with patients.
HCWs represent diverse educational, social and ethnic levels and are usually predominantly female. Many, particularly in home care, are employed in entry-level positions and require considerable basic training. Table 1 lists samples of health care functions and associated occupations.
Table 1. Examples of health care functions and associated occupations
|
Functions |
Occupational category * |
Specific occupations |
|
Direct patient care |
Health-diagnosing occupations |
Physicians |
|
Technical support |
Health technicians |
Clinical laboratory technicians |
|
Services |
Health services |
Dental assistants |
|
Administrative support |
Clerical services |
Billing clerks |
|
Research |
Scientific occupations |
Scientists and research |
* Occupational categories are, in part, adapted from those used by the US Department of Labor, Bureau of Labor Statistics.
A segment of the health sector (unfortunately, often too small and under-resourced in most communities) is devoted to direct and indirect preventive services. The major focus of the health care industry, however, is the diagnosis, treatment and care of the sick. This creates a special set of dynamics, for the sick exhibit varying levels of physical and emotional dependencies that set them apart from the customers in such personal services industries as, for example, retail trade, restaurants and hotels. They require, and traditionally receive, special services and considerations, often on an emergency basis, provided frequently at the expense of the HCWs’ personal comfort and safety.
Reflecting their size and numbers of employees, acute and long-term care facilities constitute perhaps the most prominent elements in the health care industry. They are supplemented by outpatient clinics, “surgicenters” (facilities for outpatient surgery), clinical and pathological laboratories, pharmacies, x-ray and imaging centres, ambulance and emergency care services, individual and group offices, and home care services. These may be located within a hospital or operated elsewhere under its aegis, or they may be free-standing and operated independently. It should be noted that there are profound differences in the way health services are delivered, ranging from the well-organized, “high tech” care available in urban centres in developed countries to the underserved areas in rural communities, in developing countries and in inner-city enclaves in many large cities.
Superimposed on the health care system is a massive educational and research establishment in which students, faculty, researchers and support staffs often come in direct contact with patients and participate in their care. This comprises schools of medicine, dentistry, nursing, public health, social work and the variety of technical disciplines involved in health care.
The health care industry has been undergoing profound changes during the past few decades. Ageing of the population, especially in developed countries, has amplified the use of nursing homes, domiciliary facilities and home care services. Scientific and technological developments have not only led to the creation of new types of facilities staffed by new classes of specially-trained personnel, but they have also de-emphasized the role of the acute care hospital. Now, many services requiring inpatient care are being provided on an ambulatory basis. Finally, fiscal constraints dictated by the continuing escalation of health care costs have been reconfiguring the health care industry, at least in developing countries, resulting in pressure for cost-containment to be achieved through changes in the organization of health care services.
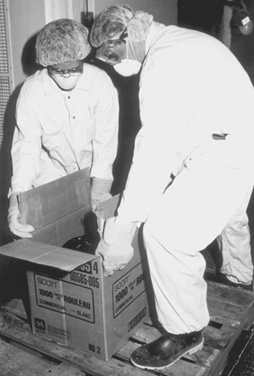
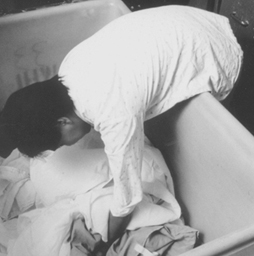
HCWs who are in direct contact with the sick, wherever they work, are exposed to a number of unique hazards. They face the risk of acquiring infections from the patients they serve, as well as the risk of musculoskeletal injuries when lifting, transferring or restraining them. Support staff not directly involved in patient care (e.g., laundry and housekeeping and materials handling workers) are not only routinely exposed to chemicals, such as cleaning agents and disinfectants of industrial strength, but are also exposed to biological hazards from contaminated linens and wastes (see figure 1). There is also the ethos of health care which, especially in emergency situations, requires HCWs to put the safety and comfort of their patients above their own. Coping with the stress of therapeutic failures, death and dying often takes its toll in worker burnout. All this is compounded by shift work, deliberate or inadvertent understaffing and the necessity of catering to the sometimes unreasonable demands from patients and their families. Finally, there is the threat of abuse and violence from patients, particularly when the job requires them to work alone or takes them into unsafe areas. All these are described in greater detail in other articles in this chapter and elsewhere in this Encyclopaedia.
Figure 1. Handling contaminated biological material
Health Sciences Centre, Winnipeg, Manitoba, Canada
The US National Institute for Occupational Safety and Health (NIOSH) reported that needle punctures, musculoskeletal sprains and back injuries probably were the most common injuries in the health care industry (Wugofski 1995). The World Health Organization (WHO) Conference on Occupational Hazards in 1981 identified as its five main areas of concern:
- cuts, lacerations and fractures
- back injuries
- lack of personal safety equipment
- poor maintenance of mechanical and electrical systems
- assault by patients.
Are they health care workers, too?
Often overlooked when considering the safety and well-being of health care workers are students attending medical, dental, nursing and other schools for health professionals and volunteers serving pro bono in healthcare facilities. Since they are not “employees” in the technical or legal sense of the term, they are ineligible for workers’ compensation and employment-based health insurance in many jurisdictions. Health care administrators have only a moral obligation to be concerned about their health and safety.
The clinical segments of their training bring medical, nursing and dental students into direct contact with patients who may have infectious diseases. They perform or assist in a variety of invasive procedures, including taking blood samples, and often do laboratory work involving body fluids and specimens of urine and faeces. They are usually free to wander about the facility, entering areas containing potential hazards often, since such hazards are rarely posted, without an awareness of their presence. They are usually supervised very loosely, if at all, while their instructors are often not very knowledgeable, or even interested, in matters of safety and health protection.
Volunteers are rarely permitted to participate in clinical care but they do have social contacts with patients and they usually have few restrictions with respect to areas of the facility they may visit.
Under normal circumstances, students and volunteers share with health care workers the risks of exposure to potentially harmful hazards. These risks are exacerbated at times of crisis and in emergencies when they step into or are ordered into the breech. Clearly, even though it may not be spelled out in laws and regulations or in organizational procedure manuals, they are more than entitled to the concern and protection extended to “regular” health care workers.
Leon Warshaw
Biological Hazards
Biological hazards, which pose a risk for infectious disease, are common throughout the world, but they are particularly problematic in developing countries. While the hepatitis B virus (HBV) is a nearly universal threat to HCWs, it is particularly important in African and Asian countries where this virus is endemic. As discussed later in this chapter, the risk of HBV transmission after percutaneous exposure to hepatitis B surface antigen (HBsAg) positive blood is approximately 100-fold higher than the risk of transmitting the human immunodeficiency virus (HIV) through percutaneous exposure to HIV-infected blood (i.e., 30% versus 0.3%). Nonetheless, there has indeed been an evolution of concern regarding parenteral exposure to blood and body fluids from the pre-HIV to the AIDS era. McCormick et al. (1991) found that the annual reported incidents of injuries from sharp instruments increased more than threefold during a 14-year period and among medical house officers the reported incidents increased ninefold. Overall, nurses incur approximately two-thirds of the needlestick injuries reported. Yassi and McGill (1991) also noted that nursing staff, particularly nursing students, are at highest risk for needlestick injuries, but they also found that approximately 7.5% of medical personnel reported exposures to blood and body fluids, a figure that is probably low because of underreporting. These data were consistent with other reports which indicated that, while there is increased reporting of needlesticks reflecting concerns about HIV and AIDS, certain groups continue to underreport. Sterling (1994) concludes that underreporting of needlestick injuries ranges from 40 to 60%.
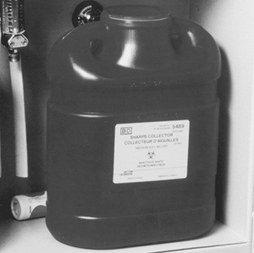
Certain risk factors clearly enhance the likelihood of transmission of bloodborne diseases; these are discussed in the article “Prevention of occupational transmission of bloodborne pathogens”. Frequent exposure has indeed been associated with high seroprevalence rates of hepatitis B among laboratory workers, surgeons and pathologists. The risk of hepatitis C is also increased. The trend towards greater attention to prevention of needlestick injuries is, however, also noteworthy. The adoption of universal precautions is an important advance. Under universal precautions, it is assumed that all blood-containing fluid is potentially infectious and that appropriate safeguards should always be invoked. Safe disposal containers for needles and other sharp instruments are increasingly being placed in conveniently accessible locations in treatment areas, as illustrated in figure 2. The use of new devices, such as the needle-less access system for intravenous treatment and/or blood sampling has been shown to be a cost-effective method of reducing needlestick injuries (Yassi and McGill 1995).
Figure 2. Disposal container for sharp instruments and devices
Health Sciences Centre, Winnipeg, Manitoba, Canada
Blood and body fluids are not the only source of infection for HCWs. Tuberculosis (TB) is also on the rise again in parts of the world where previously its spread had been curtailed and, as discussed later in this chapter, is a growing occupational health concern. In this, as in other nosocomial infections, such concern is heightened by the fact that so many of the organisms involved have become drug-resistant. There is also the problem of new outbreaks of deadly infectious agents, such as the Ebola virus. The article “Overview of infectious diseases” summarizes the major infectious disease risks for HCWs.
Chemical Hazards
HCWs are exposed to a wide variety of chemicals, including disinfectants, sterilants, laboratory reagents, drugs and anaesthetic agents, to name just a few of the categories. Figure 3 shows a storage cabinet in an area of a large hospital where prosthetics are fabricated and clearly illustrates the vast array of chemicals that are present in health care facilities. Some of these substances are highly irritating and may also be sensitizing. Some disinfectants and antiseptics also tend to be quite toxic, also with irritating and sensitizing propensities that may induce skin or respiratory tract disease. Some, like formaldehyde and ethylene oxide, are classified as mutagens, teratogens and human carcinogens as well. Prevention depends on the nature of the chemical, the maintenance of the apparatus in which it is used or applied, environmental controls, worker training and, in some instances, the availability of correct personal protective equipment. Often such control is straightforward and not very expensive. For example, Elias et al. (1993) showed how ethylene oxide exposure was controlled in one health care facility. Other articles in this chapter address chemical hazards and their management.
Figure 3. Storage cabinet for hazardous chemicals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Physical Hazards and the Building Environment
In addition to the specific environmental contaminants faced by HCWs, many health care facilities also have documented indoor air quality problems. Tran et al. (1994), in studying symptoms experienced by operating room personnel, noted the presence of the “sick building syndrome” in one hospital. Building design and maintenance decisions are, therefore, extremely important in health care facilities. Particular attention must be paid to correct ventilation in specific areas such as laboratories, operating rooms and pharmacies, the availability of hoods and avoidance of the insertion of chemical-laden fumes into the general air-conditioning system. Controlling the recirculation of air and using special equipment (e.g., appropriate filters and ultraviolet lamps) is needed to prevent the transmission of air-borne infectious agents. Aspects of the construction and planning of health care facilities are discussed in the article “Buildings for health care facilities”.
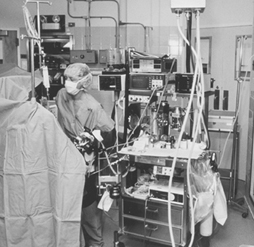
Physical hazards are also ubiquitous in hospitals (see “Exposure to physical agents” in this chapter). The wide variety of electrical equipment used in hospitals can present an electrocution hazard to patients and staff if not properly maintained and grounded (see figure 4). Especially in hot and humid environments, heat exposure may present a problem to workers in such areas as laundries, kitchens and boiler rooms. Ionizing radiation is a special concern for staff in diagnostic radiology (i.e., x ray, angiography, dental radiography and computerized axial tomography (CAT) scans) as well as for those in therapeutic radiology. Controlling such radiation exposures is a routine matter in designated departments where there is careful supervision, well-trained technicians and properly shielded and maintained equipment, but it can be a problem when portable equipment is used in emergency rooms, intensive care units and operating rooms. It can also be a problem to housekeeping and other support staff whose duties take them into areas of potential exposure. In many jurisdictions these workers have not been properly trained to avoid this hazard. Exposure to ionizing radiation may also present a problem in diagnostic and therapeutic nuclear medicine units and in preparing and distributing doses of radioactive pharmaceuticals. In some cases, however, radiation exposure remains a serious problem (see the article “Occupational health and safety practice: The Russian experience” in this chapter).
Figure 4. Electrical equipment in hospital
Health Sciences Centre, Winnipeg, Manitoba, Canada
Contradicting the prevailing impression of hospitals as quiet workplaces, Yassi et al. (1991) have documented the surprising extent of noise-induced hearing loss among hospital workers (see table 2). The article “Ergonomics of the physical work environment” in this chapter offers useful recommendations for controlling this hazard, as does table 3.
Table 2. 1995 integrated sound levels
|
Area monitored |
dBA (lex) Range |
|
Cast room |
76.32 to 81.9 |
|
Central energy |
82.4 to 110.4 |
|
Nutrition and food services (main kitchen) |
|
|
Housekeeping |
|
|
Laundry |
|
|
Linen service |
76.3 to 91.0 |
|
Mailroom |
|
|
Maintenance |
|
|
Materials handling |
|
|
Print shop |
|
|
Rehabilitation engineering |
|
Note: “Lex” means the equivalent sound level or the steady sound level in dBA which, if present in a workplace for 8 hours, would contain the same acoustic energy.
Table 3. Ergonomic noise reduction options
|
Work area |
Process |
Control options |
|
Central energy |
General area |
Enclose the source |
|
Dietetics |
Pot washer |
Automate process |
|
Housekeeping |
Burnishing |
Purchasing criteria |
|
Laundry |
Dryer/washer |
Isolate and reduce vibration |
|
Mailroom |
Tuberoom |
Purchasing criteria |
|
Maintenance |
Various equipment |
Purchasing criteria |
|
Materiel handling and |
Carts |
Maintenance |
|
Print shop |
Press operator |
Maintenance |
|
Rehabilitation |
Orthotics |
Purchasing criteria |
By far the most common and most costly type of injury faced by HCWs is back injury. Nurses and attendants are at greatest risk of musculoskeletal injuries due to the large amount of patient lifting and transferring that their jobs require. The epidemiology of back injury in nurses was summarized by Yassi et al. (1995a) with respect to one hospital. The pattern they observed mirrors those that have been universally reported. Hospitals are increasingly turning to preventive measures which may include staff training and the use of mechanical lifting devices. Many are also providing up-to-date diagnostic, therapeutic and rehabilitation health services that will minimize lost time and disability and are cost-effective (Yassi et al. 1995b). Hospital ergonomics has taken on increasing importance and, therefore, is the subject of a review article in this chapter. The specific problem of the prevention and management of back pain in nurses as one of the most important problems for this cohort of HCWs is also discussed in the article “Prevention and management of back pain in nurses” in this chapter. Table 4 lists the total number of injuries in a one-year period.
Table 4. Total number of injuries, mechanism of injury and nature of industry (one hospital, all departments), 1 April 1994 to 31 March 1995
|
Nature of injury sustained |
Total |
||||||||||||
|
Mechanism |
Blood/ |
Cut/ |
Bruise/ |
Sprain/ |
Fracture/ |
Burn/ |
Human |
Broken |
Head- |
Occupa- |
Other3 |
Un- |
|
|
Exertion |
|||||||||||||
|
Transferring |
105 |
105 |
|||||||||||
|
Lifting |
83 |
83 |
|||||||||||
|
Assisting |
4 |
4 |
|||||||||||
|
Turning |
27 |
27 |
|||||||||||
|
Breaking fall |
28 |
28 |
|||||||||||
|
Pushing |
1 |
25 |
26 |
||||||||||
|
Lifting |
1 |
52 |
1 |
54 |
|||||||||
|
Pulling |
14 |
14 |
|||||||||||
|
Combination- |
38 |
38 |
|||||||||||
|
Other |
74 |
74 |
|||||||||||
|
Fall |
3 |
45 |
67 |
3 |
1 |
119 |
|||||||
|
Struck/ |
66 |
76 |
5 |
2 |
2 |
1 |
152 |
||||||
|
Caught in/ |
13 |
68 |
8 |
1 |
1 |
91 |
|||||||
|
Exp. |
3 |
1 |
4 |
19 |
16 |
12 |
55 |
||||||
|
Staff abuse |
|||||||||||||
|
Patient |
16 |
11 |
51 |
28 |
8 |
3 |
1 |
2 |
120 |
||||
|
Spill/splashes |
80 |
1 |
81 |
||||||||||
|
Drug/ |
2 |
2 |
|||||||||||
|
Exp. |
5 |
5 |
10 |
||||||||||
|
Needlesticks |
159 |
22 |
181 |
||||||||||
|
Scalpel cuts |
34 |
14 |
48 |
||||||||||
|
Other5 |
3 |
1 |
29 |
1 |
6 |
40 |
|||||||
|
Unknown (no |
8 |
8 |
|||||||||||
|
Total |
289 |
136 |
243 |
558 |
5 |
33 |
8 |
7 |
19 |
25 |
29 |
8 |
1,360 |
1 No blood/body fluid. 2 This includes rashes/dermatitis/work-related illness/burning eyes, irritated eyes. 3 Exposure to chemical or physical agents but with no documented injuries affects. 4 Accident not reported. 5 Exposure to cold/heat, unknown.
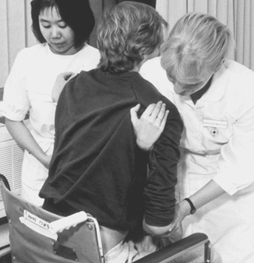
In discussing musculoskeletal and ergonomic problems, it is important to note that while those engaged in direct patient care may be at greatest risk (see figure 5) many of the support personnel in hospital must contend with similar ergonomic burdens (see figure 6 and figure 7). The ergonomic problems facing hospital laundry workers have been well-documented (Wands and Yassi 1993) (see figure 8, figure 9 and figure 10) and they also are common among dentists, otologists, surgeons and especially microsurgeons, obstetricians, gynaecologists and other health personnel who often must work in awkward postures.
Figure 5. Patient lifting is an ergonomic hazard in most hospitals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 6. Overhead painting: A typical ergonomic hazard for a tradesworker
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 7. Cast-making involves many ergonomic stresses
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 8. Laundry work such as this can cause repetitive stress injury to the upper limbs
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 9. This laundry task requires working in an awkward position
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 10. A poorly designed laundry operation can cause back strain
Health Sciences Centre, Winnipeg, Manitoba, Canada
Organizational Problems
The article “Strain in health care work” contains a discussion of some of the organizational problems in hospitals and a summary of the principal findings of Leppanen and Olkinuora (1987), who reviewed Finnish and Swedish studies of stress among HCWs. With the rapid changes currently under way in this industry, the extent of alienation, frustration and burnout among HCWs is considerable. Added to that is the prevalence of staff abuse, an increasingly troublesome problem in many facilities (Yassi 1994). While it is often thought that the most difficult psychosocial problem faced by HCWs is dealing with death and dying, it is being recognized increasingly that the nature of the industry itself, with its hierarchical structure, its growing job insecurity and the high demands unsupported by adequate resources, is the cause of the variety of stress-related illness faced by HCWs.
The Nature of the Health Care Sector
In 1976, Stellman wrote, “If you ever wondered how people can manage to work with the sick and always stay healthy themselves, the answer is that they can’t” (Stellman 1976). The answer has not changed, but the potential hazards have clearly expanded from infectious diseases, back and other injuries, stress and burnout to include a large variety of potentially toxic environmental, physical and psychosocial exposures. The world of the HCW continues to be largely unmonitored and largely unregulated. None the less, progress is being made in addressing occupational health and safety hazards in hospitals. The International Commission on Occupational Health (ICOH) has a sub-committee addressing this problem, and several international conferences have been held with published proceedings that offer useful information (Hagberg et al. 1995). The US Centers for Disease Control and Prevention (CDC) and NIOSH have proposed guidelines to address many of the problems of the health care industry discussed in this article (e.g., see NIOSH 1988). The number of articles and books addressing health and safety issues for HCWs has been growing rapidly, and good overviews of health and safety in the US health care industry have been published (e.g., Charney 1994; Lewy 1990; Sterling 1994). The need for systematic data collection, study and analysis regarding hazards in the health care industry and the desirability of assembling interdisciplinary occupational health teams to address them have become increasingly evident.
When considering occupational health and safety in the health care industry, it is crucial to appreciate the enormous changes currently taking place in it. Health care “reform”, being instituted in most of the developed countries of the world, is creating extraordinary turbulence and uncertainty for HCWs, who are being asked to absorb rapid changes in their work tasks often with greater exposure to risks. The transformation of health care is spurred, in part, by advances in medical and scientific knowledge, the development of innovative technological procedures and the acquisition of new skills. It is also being driven, however, and perhaps to an even greater extent, by concepts of cost-effectiveness and organizational efficiency, in which “downsizing” and “cost control” have often seemed to become goals in themselves. New institutional incentives are being introduced at different organizational levels in different countries. The contracting out of jobs and services that had traditionally been carried out by a large stable workforce is now increasingly becoming the norm. Such contracting out of work is reported to have helped the health administrators and politicians achieve their long-term goal of making the process of health care more flexible and more accountable. These changes have also brought changes in roles that were previously rather well-defined, undermining the traditional hierarchical relationships among planners, administrators, physicians and other health professionals. The rise of investor-owned health care organizations in many countries has introduced a new dynamic in the financing and management of health services. In many situations, HCWs have been forced into new working relationships that involve such changes as downgrading services so that they can be performed by less-skilled workers at lower pay, reduced staffing levels, staff redeployments involving split shifts and part-time assignments. At the same time, there has been a slow but steady growth in the numbers of such physician surrogates as physician assistants, nurse practitioners, midwives and psychiatric social workers who command lower rates of pay than the physicians they are replacing. (The ultimate social and health costs both to HCWs and to the public, as patients and payers, is still to be determined.)
A growing trend in the US that is also emerging in the UK and northern European countries is “managed care”. This generally involves the creation of organizations paid on a per capita basis by insurance companies or government agencies to provide or contract for the provision of a comprehensive range of health services to a voluntarily-enrolled population of subscribers. Their aim is to reduce the costs of health care by “managing” the process: using administrative procedures and primary care physicians as “gatekeepers” to control the utilization of expensive in-patient hospital days, reducing referrals to high-priced specialists and use of costly diagnostic procedures, and denying coverage for expensive new forms of “experimental” treatment. The growing popularity of these managed care systems, fuelled by aggressive marketing to employer- and government-sponsored groups and individuals, has made it difficult for physicians and other health care providers to resist becoming involved. Once engaged, there is a variety of financial incentives and disincentives to influence their judgement and condition their behaviour. The loss of their traditional autonomy has been particularly painful for many medical practitioners and has had a profound influence on their patterns of practice and their relationships with other HCWs.
These rapid changes in the organization of the health care industry are having profound direct and indirect effects on the health and safety of HCWs. They affect the ways health services are organized, managed, delivered and paid for. They affect the ways HCWs are trained, assigned and supervised and the extent to which considerations of their health and safety are addressed. This should be kept in mind as the various occupational health hazards faced by HCWs are discussed in this chapter. Finally, although it may not appear to be directly relevant to the content of this chapter, thought should be given to the implications of the well-being and performance of HCWs to the quality and effectiveness of the services they provide to their patients.