Tendons
The deformation that occurs as force is applied and removed is called “elastic” deformation. The deformation that occurs after force application or removal is called “viscous” deformation. Because tissues of the body exhibit both elastic and viscous properties, they are called “viscoelastic”. If the recovery time between successive exertions is not long enough for a given force and duration, the recovery will not be complete and the tendon will be stretched further with each successive exertion. Goldstein et al. (1987) found that when finger flexor tendons were subjected to 8 seconds (s) physiological loads and 2 s rest, the accumulated viscous strain after 500 cycles was equal to the elastic strain. When the tendons were subjected to 2 s work and 8 s rest, the accumulated viscous strain after 500 cycles was negligible. Critical recovery times for given work-rest profiles have not yet been determined.
Tendons can be characterized as composite structures with parallel bundles of collagen fibres arranged in a gelatinous matrix of mucopolysaccharide. Tensile forces on the ends of the tendon cause unfolding of corrugations and straightening of the collagen strands. Additional loads cause stretching of the straightened strands. Consequently, the tendon gets stiffer as it gets longer. Compressive forces perpendicular to the long axis of the tendon cause the collagen strands to be forced closer together, and result in a flattening of the tendon. Shear forces on the side of the tendon cause displacement of the collagen strands closest to the surface with respect to those farthest away, and gives the side view of the tendon a skewed look.
Tendons as Structures
Forces are transmitted through tendons to maintain static and dynamic balance for specified work requirements. Contracting muscles tend to rotate the joints in one direction while the weight of the body and of work objects tends to rotate them in the other. Exact determination of these tendon forces is not possible because there are multiple muscles and tendons acting about each joint structure; however, it can be shown that the muscle forces acting on the tendons are much greater than the weight or reaction forces of work objects.
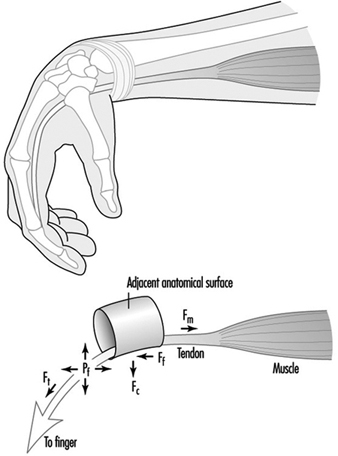
The forces exerted by contracting muscles are called tensile forces because they stretch the tendon. Tensile forces can be demonstrated by pulling on the ends of a rubber band. Tendons also are subjected to compressive and shear forces and to fluid pressures, which are illustrated in Figure 4 for the finger flexor tendons in the wrist.
Figure 1. Schematic diagram of tendon stretched around an anatomical surface or pulley and the corresponding tensile forces (Ft), compressive forces (Fc), friction forces (Ff) and hydrostatic or fluid pressure (Pf).
Exertion of the fingers to grasp or manipulate work objects requires the contraction of muscles in the forearm and hand. As the muscles contract, they pull on the ends of their respective tendons, which pass through the centre and circumference of the wrist. If the wrist is not held in a position so that the tendons are perfectly straight, they will press against adjacent structures. The finger flexor tendons press against the bones and ligaments inside the carpal tunnel. These tendons can be seen to protrude under the skin toward the palm during forceful pinching with a flexed wrist. Similarly, the extensor and abductor tendons can be seen to protrude on the back and side of the wrist when it is extended with outstretched fingers.
Friction or shear forces are caused by dynamic exertions in which the tendons rub against adjacent anatomical surfaces. These forces act on and parallel to the surface of the tendon. Friction forces can be felt by simultaneously pressing and sliding the hand against a flat surface. The sliding of tendons over an adjacent anatomical surface is analogous to a belt sliding around a pulley.
Fluid pressure is caused by exertions or postures that displace fluid out of the spaces around the tendons. Studies of carpal canal pressure show that wrist contact with external surfaces and certain postures produce pressures high enough to impair circulation and threaten tissue viability (Lundborg 1988).
Contraction of a muscle produces an immediate stretching of its tendon. Tendons join muscles together. If the exertion is sustained, the tendon will continue to stretch. Relaxation of the muscle will result in a rapid recovery of the tendon followed by a slowed recovery. If the initial stretching was within certain limits, the tendon will recover to its initial unloaded length (Fung 1972).
Tendons as Living Tissues
The strength of tendons belies the delicacy of the underlying physiological mechanisms by which they are nourished and heal. Interspersed within the tendon matrix are living cells, nerve endings and blood vessels. Nerve endings provide information to the central nervous system for motor control and warning of acute overload. Blood vessels play an important role in the nourishment of some areas of the tendon. Some areas of tendons are avascular and rely on diffusion from fluid secreted by synovial linings of outer tendon sheaths (Gelberman et al. 1987). Synovial fluid also lubricates movements of the tendons. Synovial sheaths are found at locations where tendons come into contact with adjacent anatomical surfaces.
Excessive elastic or viscous deformation of the tendon can damage these tissues and impair their ability to heal. It is hypothesized that deformation may impede or arrest circulation and nourishment of tendons (Hagberg 1982; Viikari-Juntura 1984; Armstrong et al. 1993). Without adequate circulation, cell viability will be impaired and the tendon’s capacity to heal will be reduced. Tendon deformation can lead to small tears that further contribute to cell damage and inflammation. If circulation is restored and the tendon is given adequate recovery time, the damaged tissues will heal (Gelberman et al. 1987; Daniel and Breidenbach 1982; Leadbetter 1989).
Tendon Disorders
It has been shown that tendon disorders occur in predictable patterns (Armstrong et al. 1993). Their locations occur in those parts of the body associated with high stress concentrations (e.g., in the tendons of the supraspinatus, the biceps, the extrinsic finger flexor and extensor muscles). Also, there is an association between the intensity of work and the prevalence of tendon disorders. This pattern also has been shown for amateur and professional athletes (Leadbetter 1989). The common factors in both workers and athletes are repetitive exertions and overloading of the muscle-tendon units.
Within certain limits, the injuries produced by mechanical loading will heal. The healing process is divided into three stages: inflammatory, proliferatory and remodelling (Gelberman et al. 1987; Daniel and Breidenbach 1982). The inflammatory stage is characterized by the presence of polymorphonuclear cell infilt- ration, capillary budding and exudation, and lasts for several days. The proliferatory stage is characterized by the proliferation of fibroblasts and randomly oriented collagen fibres between areas of the wound and adjacent tissues, and lasts for several weeks. The remodelling phase is characterized by the alignment of the collagen fibres along the direction of loading, and lasts for several months. If the tissues are re-injured before healing is complete, recovery may be delayed and the condition may worsen (Leadbetter 1989). Normally healing leads to a strengthening or adaptation of the tissue to mechanical stress.
The effects of repetitive loading are apparent in the forearm finger flexor tendons where they contact the inside walls of the carpal tunnel (Louis 1992; Armstrong et al. 1984). It has been shown that there is progressive thickening of the synovial tissue between the edges of the carpal tunnel and the centre where the contact stresses on the tendons are the greatest. Thickening of the tendons is accompanied by synovial hyperplasia and proliferation of connective tissue. Thickening of the tendon sheaths is a widely cited factor in compression of the median nerve inside the carpal tunnel. It can be argued that thickening of the synovial tissues is an adaptation of the tendons to mechanical trauma. Were it not for the secondary effect on the median nerve compression resulting in carpal tunnel syndrome, it might be considered a desirable outcome.
Until optimal tendon loading regimes are determined, employers should monitor workers for signs or symptoms of tendon disorders so that they can intervene with work modifications to prevent further injuries. Jobs should be inspected for conspicuous risk factors any time an upper limb problem is identified or suspected. Jobs also should be inspected any time there is a change in the work standard, procedure or tooling, to insure that risk factors are minimized.
Muscles
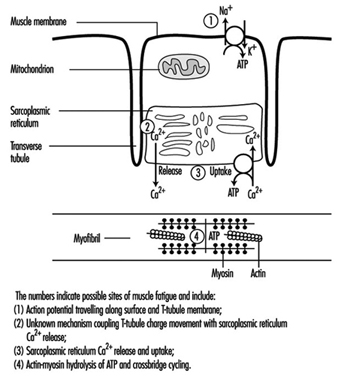
Physical activity may increase muscle strength and working capa-city through changes such as growth in muscle volume and increased metabolic capacity. Different activity patterns cause a variety of biochemical and morphological adaptations in the muscles. In general, a tissue must be active to remain capable of living. Inactivity causes atrophy, especially in muscle tissue. Sports medicine and scientific investigations have shown that various training regimes can produce very specific muscular changes. Strength training, which places strong forces on the muscles, increases the number of contractile filaments (myofibrils) and the volume of the sarcoplasmic reticulum (see figure 1). High-intensity exercise increases muscular enzyme activity. The fractions of glycolytic and oxidative enzymes are closely related to the work intensity. In addition, prolonged intense exercise increases the capillary density.
Figure 1. A diagrammatic representation of the major components of a muscle cell involved in excitation-contraction coupling as well as the site for ATP production, the mitochondrion.
Sometimes, too much exercise can induce muscle soreness, a phenomenon well known to everyone who has demanded muscular performance beyond his or her capacity. When a muscle is overused, first deteriorating processes set in, which are followed by reparative processes. If sufficient time for repair is allowed, the muscle tissue may end up with increased capacities. Prolonged overuse with insufficient time for repair, on the other hand, causes fatigue and impairs muscle performance. Such prolonged overuse may induce chronic degenerative changes in the muscles.
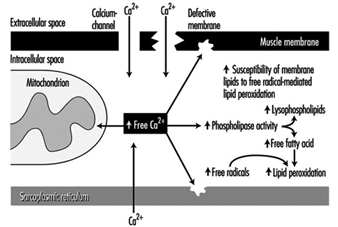
Other aspects of muscle use and misuse include the motor control patterns for various work tasks, which depend on force level, rate of force development, type of contraction, duration and the precision of the muscle task (Sjøgaard et al. 1995). Individual muscle fibres are “recruited” for these tasks, and some recruitment patterns may induce a high load on individual motor units even when the load on the muscle as a whole is small. Extensive recruitment of a particular motor unit will inevitably induce fatigue; and occupational muscle pain and injury may follow and could easily be related to the fatigue caused by insufficient muscle blood flow and intramuscular biochemical changes due to this high demand (Edwards 1988). High muscle tissue pressures may also impede muscle blood flow, which can reduce the ability of essential chemicals to reach the muscles, as well as the ability of the blood to remove waste products; this can cause energy crises in the muscles. Exercise can induce calcium to accumulate, and free radical formation may also promote degenerative processes such as the breakdown of muscle membrane and the impairment of normal metabolism (mitochondrial energy turnover) (figure 2). These processes may ultimately lead to degenerative changes in the muscle tissue itself. Fibres with marked degenerative characteristics have been found more frequently in muscle biopsies from patients with work-related chronic muscle pain (myalgia) than in normal subjects. Interestingly, the degenerated muscle fibres thus identified are “slow twitch fibres”, which connect with low-threshold motor nerves. These are the nerves normally recruited at low sustained forces, not high force related tasks. The perception of fatigue and pain may play an important role in preventing muscle injury. Protective mechanisms induce the muscles to relax and recover in order to regain strength (Sjøgaard 1990). If such biofeedback from the peripheral tissues is ignored, the fatigue and pain may eventually result in chronic pain.
Figure 2. A blow-up of the muscle membrane and structures inside the muscle in figure 2. The chain of events in the pathogenesis of calcium () induced damage in muscle cells is illustrated
Sometimes, after frequent overuse, various normal cellular chemical substances may not only cause pain themselves but may increase the response of muscular receptors to other stimuli, thereby lowering the threshold of activation (Mense 1993). The nerves which carry the signals from the muscles to the brain (sensory afferents) may thus be sensitized over time, which means that a given dose of substances which cause pain elicit a stronger excitation response. That is, the threshold of activation is reduced and smaller exposures may cause larger responses. Interestingly, the cells which normally serve as pain receptors (nociceptors) in uninjured tissue are silent, but these nerves may also develop ongoing pain activity which can persist even after the cause of the pain has terminated. This effect may explain chronic states of pain which are present after the initial injury has healed. When pain persists after healing, the original morphological changes in the soft tissues may be difficult to identify, even if the primary or initial cause of the pain is located in these peripheral tissues. Thus, the real “cause” of the pain may be impossible to trace.
Risk Factors and Preventive Strategies
Work-related risk factors of muscle disorders include repetition, force, static load, posture, precision, visual demand and vibration. Inappropriate work/rest cycles may be a potential risk factor for musculoskeletal disorders if sufficient recovery periods are not allowed before the next working period, thus never affording enough time for physiological rest. Environmental, sociocultural or personal factors may also play a role. Musculoskeletal disorders are multifactorial, and, in general, simple cause-effect relationships are difficult to detect. It is, however, important to document the extent to which occupational factors can be causally related to the disorders, since, only in the case of causality, the elimination or minimization of the exposure will help prevent the disorders. Of course, different preventive strategies must be implemented depending on the type of work task. In the case of high-intensity work the aim is to reduce force and work intensity, while for monotonous repetitive work it is more important to induce variation in the work. In short, the aim is optimization of the exposure.
Occupational Diseases
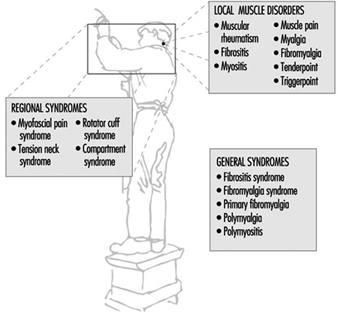
Work-related muscle pain is reported most frequently in the neck and shoulder area, the forearm and the low back. Although it is a major cause of sick-leave there is much confusion with regard to classifying the pain and specifying diagnostic criteria. Common terms which are used are given in three categories (see figure 3).
Figure 3. Classification of muscle diseases.
When muscular pain is assumed to be work-related, it can be classified into one of the following disorders:
- Occupational cervicobrachial disorders (OCD)
- Repetition strain injury (RSI)
- Cumulative trauma disorders (CTD)
- Overuse (injury) syndrome
- Work-related neck and upper-limb disorders.
The taxonomy of the work-related neck and upper-limb disorders clearly demonstrates that the aetiology includes external mechanical loads, which may well occur in the work place. Besides disorders in the muscle tissue itself, this category includes also disorders in other soft tissues of the musculoskeletal system. Of note is, that the diagnostic criteria may not allow to identify the location of the disorder specifically to one of these soft tissues. In fact it is likely that morphological changes at the musculo-tendinous junctions are related to the perception of muscle pain. This advocates the term fibromyalgia to be used among local muscle disorders. (See figure 3)
Unfortunately, different terms are used for essentially the same medical condition. In recent years, the international scientific community has focused increasingly on classification and diagnostic criteria for musculoskeletal disorders. A distinction is made between generalized and local or regional pain (Yunus 1993). Fibromyalgia syndrome is a generalized pain condition but is not considered to be work related. On the other hand, localized pain disorders are likely to be associated with specific work tasks. Myofascial pain syndrome, tension neck and rotator cuff syndrome are localized pain disorders that can be considered as work-related diseases.
Overview
Musculoskeletal disorders are among the most important occupational health problems in both developed and developing countries. These disorders affect the quality of life of most people during their lifetime. The annual cost of musculoskeletal disorders is great. In the Nordic countries, for example, it is estimated to vary from 2.7 to 5.2 % of the gross national product (Hansen 1993; Hansen and Jensen 1993). The proportion of all musculo-skeletal diseases that are attributable to work is thought to be approximately 30%. Thus, much is to be gained by prevention of work-related musculoskeletal disorders. To accomplish this goal, a good understanding is needed of the healthy musculoskeletal system, musculoskeletal diseases and the risk factors for musculo-skeletal disorders.
Most musculoskeletal diseases cause local ache or pain and restriction of motion that may hinder normal performance at work or in other everyday tasks. Nearly all musculoskeletal diseases are work-related in the sense that physical activity can aggravate or provoke symptoms even if the diseases were not directly caused by work. In most cases, it is not possible to point to one causal factor for musculoskeletal diseases. Conditions caused solely by accidental injuries are an exception; in most cases several factors play a role. For many of the musculoskeletal diseases, mechanical load at work and leisure is an important causal factor. Sudden overload, or repetitive or sustained loading can injure various tissues of the musculoskeletal system. On the other hand, too low a level of activity can lead to deterioration of the condition of muscles, tendons, ligaments, cartilage and even bones. Keeping these tissues in good condition requires appropriate use of the musculoskeletal system.
The musculoskeletal system essentially consists of similar tissues in different parts of the body, which provide a panorama of diseases. The muscles are the most common site of pain. In the lower back the intervertebral discs are common problem tissues. In the neck and the upper limbs, tendon and nerve disorders are common, while in the lower limbs, osteoarthritis is the most important pathological condition.
In order to understand these bodily differences, it is necessary to comprehend basic anatomical and physiological features of the musculoskeletal system and to learn the molecular biology of various tissues, the source of nutrition and the factors affecting normal function. The biomechanical properties of various tissues are also fundamental. It is necessary to understand both the physiology of normal function of the tissues, and pathophysi- ology—that is, what goes wrong. These aspects are described in the first articles for intervertebral discs, bones and joints, tendons, muscles and nerves. In the articles which follow, musculoskeletal disorders are described for the different anatomical regions. Symptoms and signs of the most important diseases are outlined and the occurrence of the disorders in populations is described. Current understanding, based on epidemiological research, of both work-and person- related risk factors is presented. For many disorders there are quite convincing data on work-related risk factors, but, for the time being, only limited data are available on exposure effect relationships between the risk factors and the disorders. Such data are needed in order to set guidelines to design safer work.
Despite the lack of quantitative knowledge, directions for prevention can be proposed. The primary approach to prevention of work-related musculoskeletal disorders is redesign of work in order to optimize the workload and make it compatible with the physical and mental performance capacity of the workers. It is also important to encourage workers to keep fit through regular physical exercise.
Not all musculoskeletal diseases described in this chapter have a causal relationship to work. It is, however, important for occupational health and safety personnel to be aware of such diseases and consider workload also in relation to them. Fitting the work to the performance capacity of the worker will help him or her to work successfully and healthfully.
Karoshi: Death from Overwork
What Is Karoshi?
Karoshi is a Japanese word which means death from overwork. The phenomenon was first identified in Japan, and the word is being adopted internationally (Drinkwater 1992). Uehata (1978) reported 17 karoshi cases at the 51st annual meeting of the Japan Association of Industrial Health. Among them seven cases were compensated as occupational diseases, but ten cases were not. In 1988 a group of lawyers established the National Defense Counsel for Victims of Karoshi (1990) and started telephone consultation to handle inquiries about karoshi-related workers’ compensation insurance. Uehata (1989) described karoshi as a sociomedical term that refers to fatalities or associated work disability due to cardiovascular attacks (such as strokes, myocardial infarction or acute cardiac failure) which could occur when hypertensive arteriosclerotic diseases are aggravated by a heavy workload. Karoshi is not a pure medical term. The media have frequently used the word because it emphasizes that sudden deaths (or disabilities) were caused by overwork and should be compensated. Karoshi has become an important social problem in Japan.
Research on Karoshi
Uehata (1991a) conducted a study of 203 Japanese workers (196 males and seven females) who had cardiovascular attacks. They or their next of kin consulted with him regarding workers’ compensation claims between 1974 and 1990. A total of 174 workers had died; 55 cases had already been compensated as occupational disease. A total of 123 workers had suffered strokes (57 arachnoidal bleedings, 46 cerebral bleedings, 13 cerebral infarctions, seven unknown types); 50, acute heart failure; 27, myocardial infarctions; and four, aortic ruptures. Autopsies were performed in only 16 cases. More than half of the workers had histories of hypertension, diabetes or other atherosclerotic problems. A total of 131 cases had worked for long hours—more than 60 hours per week, more than 50 hours overtime per month or more than half of their fixed holidays. Eighty-eight workers had identifiable trigger events within 24 hours before their attack. Uehata concluded that these were mostly male workers, working for long hours, with other stressful overload, and that these working styles exacerbated their other lifestyle habits and resulted in the attacks, which were finally triggered by minor work-related troubles or events.
Karasek Model and Karoshi
According to the demand-control model by Karasek (1979), a high-strain job—one with a combination of high demand and low control (decision latitude)—increases the risk of psychological strain and physical illness; an active job—one with a combination of high demand and high control—requires learning motivation to develop new behaviour patterns. Uehata (1991b) reported that the jobs in karoshi cases were characterized by a higher degree of work demands and lower social support, whereas the degree of work control varied greatly. He described the karoshi cases as very delighted and enthusiastic about their work, and consequently likely to ignore their needs for regular rest and so on—even the need for health care. It is suggested that workers in not only high-strain jobs but also active jobs could be at high risk. Managers and engineers have high decision latitude. If they have extremely high demands and are enthusiastic in their work, they may not control their working hours. Such workers may be a risk group for karoshi.
Type A Behaviour Pattern in Japan
Friedman and Rosenman (1959) proposed the concept of Type A behaviour pattern (TABP). Many studies have showed that TABP is related to the prevalence or incidence of coronary heart disease (CHD).
Hayano et al. (1989) investigated the characteristics of TABP in Japanese employees using the Jenkins Activity Survey (JAS). Responses of 1,682 male employees of a telephone company were analysed. The factor structure of the JAS among the Japanese was in most respects equal to that found in the Western Collaborative Group Study (WCGS). However, the average score of factor H (hard-driving and competitiveness) among the Japanese was considerably lower than that in the WCGS.
Monou (1992) reviewed TABP research in Japan and summarized as follows: TABP is less prevalent in Japan than in the United States; the relationship between TABP and coronary heart disease in Japan seems to be significant but weaker than that in the US; TABP among Japanese places more emphasis on “workaholism” and “directivity into the group” than in the US; the percentage of highly hostile individuals in Japan is lower than in the US; there is no relationship between hostility and CHD.
Japanese culture is quite different from those of Western countries. It is strongly influenced by Buddhism and Confucianism. Generally speaking, Japanese workers are organization centred. Cooperation with colleagues is emphasized rather than competition. In Japan, competitiveness is a less important factor for coronary-prone behaviour than job involvement or a tendency to overwork. Direct expression of hostility is suppressed in Japanese society. Hostility may be expressed differently than in Western countries.
Working Hours of Japanese Workers
It is well known that Japanese workers work long hours compared with workers in other developed industrial countries. Normal annual working hours of manufacturing workers in 1993 were 2,017 hours in Japan; 1,904 in the United States; 1,763 in France; and 1,769 in the UK (ILO 1995). However, Japanese working hours are gradually decreasing. Average annual working hours of manufacturing employees in enterprises with 30 employees or more was 2,484 hours in 1960, but 1,957 hours in 1994. Article 32 of the Labor Standards Law, which was revised in 1987, provides for a 40-hour week. The general introduction of the 40-hour week is expected to take place gradually in the 1990s. In 1985, the 5-day work week was granted to 27% of all employees in enterprises with 30 employees or more; in 1993, it was granted to 53% of such employees. The average worker was allowed 16 paid holidays in 1993; however, workers actually used an average of 9 days. In Japan, paid holidays are few, and workers tend to save them to cover absence due to sickness.
Why do Japanese workers work such long hours? Deutschmann (1991) pointed out three structural conditions underlying the present pattern of long working hours in Japan: first, the continuing need of Japanese employees to increase their income; second, the enterprise-centred structure of industrial relations; and third, the holistic style of Japanese personnel management. These conditions were based on historical and cultural factors. Japan was defeated in war in 1945 for the first time in history. After the war Japan was a cheap wage country. The Japanese were used to working long and hard to earn their subsistence. As labour unions were cooperative with employers, there have been relatively few labour disputes in Japan. Japanese companies adopted the seniority-oriented wage system and lifetime employment. The number of hours is a measure of the loyalty and cooperativeness of an employee, and becomes a criterion for promotion. Workers are not forced to work long hours; they are willing to work for their companies, as if the company is their family. Working life has priority over family life. Such long working hours have contributed to the remarkable economic achievements of Japan.
National Survey of Workers’ Health
The Japanese Ministry of Labour conducted surveys on the state of employees’ health in 1982, 1987 and 1992. In the survey in 1992, 12,000 private worksites employing 10 or more workers were identified, and 16,000 individual workers from them were randomly selected nationwide based on industry and job classification to fill out questionnaires. The questionnaires were mailed to a representative at the workplace who then selected workers to complete the survey.
Sixty-five per cent of these workers complained of physical fatigue due to their usual work, and 48% complained of mental fatigue. Fifty-seven per cent of workers stated that they had strong anxieties, worries or stress concerning their job or working life. The prevalence of stressed workers was increasing, as the prevalence had been 55% in 1987 and 51% in 1982. The main causes of stress were: unsatisfactory relations in the workplace, 48%; quality of work, 41%; quantity of work, 34%.
Eighty-six per cent of these worksites conducted periodic health examinations. Worksite health promotion activities were conducted at 44% of the worksites. Of these worksites, 48% had sports events, 46% had exercise programmes and 35% had health counselling.
National Policy to Protect and PromoteWorkers’ Health
The purpose of the Industrial Safety and Health Law in Japan is to secure the safety and health of workers in workplaces as well as to facilitate the establishment of a comfortable working environment. The law states that the employer shall not only comply with the minimum standards for preventing occupational accidents and diseases, but also endeavour to ensure the safety and health of workers in workplaces through the realization of a comfortable working environment and the improvement of working conditions.
Article 69 of the law, amended in 1988, states that the employer shall make continuous and systematic efforts for the maintenance and promotion of workers’ health by taking appropriate measures, such as providing health education and health counselling services to the workers. The Japanese Ministry of Labour publicly announced guidelines for measures to be taken by employers for the maintenance and promotion of workers’ health in 1988. It recommends worksite health promotion programmes called the Total Health Promotion Plan (THP): exercise (training and counselling), health education, psychological counselling and nutritional counselling, based on the health status of employees.
In 1992, the guidelines for the realization of a comfortable working environment were announced by the Ministry of Labour in Japan. The guidelines recommend the following: the working environment should be properly maintained under comfortable conditions; work conditions should be improved to reduce the workload; and facilities should be provided for the welfare of employees who need to recover from fatigue. Low-interest loans and grants for small and medium-sized enterprises for workplace improvement measures have been introduced to facilitate the realization of a comfortable working environment.
Conclusion
The evidence that overwork causes sudden death is still incomplete. More studies are needed to clarify the causal relationship. To prevent karoshi, working hours should be reduced. Japanese national occupational health policy has focused on work hazards and health care of workers with problems. The psychological work environment should be improved as a step towards the goal of a comfortable working environment. Health examinations and health promotion programmes for all workers should be encouraged. These activities will prevent karoshi and reduce stress.
Cognitive Disorders
A cognitive disorder is defined as a significant decline in one’s ability to process and recall information. The DSM IV (American Psychiatric Association 1994) describes three major types of cognitive disorder: delirium, dementia and amnestic disorder. A delirium develops over a short period of time and is characterized by an impairment of short-term memory, disorientation and perceptual and language problems. Amnestic disorders are characterized by impairment of memory such that sufferers are unable to learn and recall new information. However, no other declines in cognitive functioning are associated with this type of disorder. Both delirium and amnestic disorders are usually due to the physiological effects of a general medical condition (e.g., head injuries, high fevers) or of substance use. There is little reason to suspect that occupational factors play a direct role in the development of these disorders.
However, research has suggested that occupational factors may influence the likelihood of developing the multiple cognitive deficits involved in dementia. Dementia is characterized by memory impairment and at least one of the following problems: (a) reduced language function; (b) a decline in one’s ability to think abstractly; or (c) an inability to recognize familiar objects even though one’s senses (e.g., vision, hearing, touch) are not impaired. Alzheimer’s disease is the most common type of dementia.
The prevalence of dementia increases with age. Approximately 3% of people over the age of 65 years will suffer from a severe cognitive impairment during any given year. Recent studies of elderly populations have found a link between a person’s occupational history and his or her likelihood of suffering from dementia. For example, a study of the rural elderly in France (Dartigues et al. 1991) found that people whose primary occupation had been farm worker, farm manager, provider of domestic service or blue-collar worker had a significantly elevated risk of having a severe cognitive impairment when compared to those whose primary occupation had been teacher, manager, executive or professional. Furthermore, this elevated risk was not due to differences between the groups of workers in terms of age, sex, education, drinking of alcoholic beverages, sensory impairments or the taking of psychotropic drugs.
Because dementia is so rare among people younger than 65 years, no study has examined occupation as a risk factor among this population. However, a large study in the United States (Farmer et al. 1995) has shown that people under the age of 65 who have high levels of education are less likely to experience declines in cognitive functioning than are similarly aged people with less education. The authors of this study commented that education level may be a “marker variable” that is actually reflecting the effects of occupational exposures. At this point, such a conclusion is highly speculative.
Although several studies have found an association between one’s principal occupation and dementia among the elderly, the explanation or mechanism underlying the association is not known. One possible explanation is that some occupations involve higher exposure to toxic materials and solvents than do other occupations. For example, there is growing evidence that toxic exposures to pesticides and herbicides can have adverse neurological effects. Indeed, it has been suggested that such exposures may explain the elevated risk of dementia found among farm workers and farm managers in the French study described above. In addition, some evidence suggests that the ingestion of certain minerals (e.g., aluminium and calcium as components of drinking water) may affect the risk of cognitive impairment. Occupations may involve differential exposure to these minerals. Further research is needed to explore possible pathophysiological mechanisms.
Psychosocial stress levels of employees in various occupations may also contribute to the link between occupation and dementia. Cognitive disorders are not among the mental health problems that are commonly thought to be stress related. A review of the role of stress in psychiatric disorders focused on anxiety disorders, schizophrenia and depression, but made no mention of cognitive disorders (Rabkin 1993). One type of disorder, called dissociative amnesia, is characterized by an inability to recall a previous traumatic or stressful event but carries with it no other type of memory impairment. This disorder is obviously stress-related, but is not categorized as a cognitive disorder according to the DSM IV.
Although psychosocial stress has not been explicitly linked to the onset of cognitive disorders, it has been demonstrated that the experience of psychosocial stress affects how people process information and their ability to recall information. The arousal of the autonomic nervous system that often accompanies exposure to stressors alerts a person to the fact that “all is not as expected or as it should be” (Mandler 1993). At first, this arousal may enhance a person’s ability to focus attention on the central issues and to solve problems. However, on the negative side, the arousal uses up some of the “available conscious capacity” or the resources that are available for processing incoming information. Thus, high levels of psychosocial stress ultimately (1) limit one’s ability to scan all of the relevant available information in an orderly fashion, (2) interfere with one’s ability to rapidly detect peripheral cues, (3) decrease one’s ability to sustain focused attention and (4) impair some aspects of memory performance. To date, even though these decrements in information-processing skills can result in some of the symptomatology associated with cognitive disorders, no relationship has been demonstrated between these minor impairments and the likelihood of exhibiting a clinically diagnosed cognitive disorder.
A third possible contributor to the relationship between occupation and cognitive impairment may be the level of mental stimulation demanded by the job. In the study of rural elderly residents in France described above, the occupations associated with the lowest risk of dementia were those that involved substantial intellectual activity (e.g., physician, teacher, lawyer). One hypothesis is that the intellectual activity or mental stimulation inherent in these jobs produces certain biological changes in the brain. These changes, in turn, protect the worker from decline in cognitive function. The well-documented protective effect of education on cognitive functioning is consistent with such a hypothesis.
It is premature to draw any implications for prevention or treatment from the research findings summarized here. Indeed, the association between one’s lifetime principal occupation and the onset of dementia among the elderly may not be due to occupational exposures or the nature of the job. Rather, the relationship between occupation and dementia may be due to differences in the characteristics of workers in various occupations. For example, differences in personal health behaviours or in access to quality medical care may account for at least part of the effect of occupation. None of the published descriptive studies can rule out this possibility. Further research is needed to explore whether specific psychosocial, chemical and physical occupational exposures are contributing to the aetiology of this cognitive disorder.
Stress and Burnout and their Implication in the Work Environment
“An emerging global economy mandates serious scientific attention to discoveries that foster enhanced human productivity in an ever-changing and technologically sophisticated work world” (Human Capital Initiative 1992). Economic, social, psychological, demographic, political and ecological changes around the world are forcing us to reassess the concept of work, stress and burnout on the workforce.
Productive work “calls for a primary focus on reality external to one self. Work therefore emphasizes the rational aspects of people and problem solving” (Lowman 1993). The affective and mood side of work is becoming an ever-increasing concern as the work environment becomes more complex.
A conflict that may arise between the individual and the world of work is that a transition is called for, for the beginning worker, from the self-centredness of adolescence to the disciplined subordination of personal needs to the demands of the workplace. Many workers need to learn and adapt to the reality that personal feelings and values are often of little importance or relevance to the workplace.
In order to continue a discussion of work-related stress, one needs to define the term, which has been used widely and with varying meanings in the behavioural science literature. Stress involves an interaction between a person and the work environment. Something happens in the work arena which presents the individual with a demand, constraint, request or opportunity for behaviour and consequent response. “There is a potential for stress when an environmental situation is perceived as presenting a demand which threatens to exceed the person’s capabilities and resources for meeting it, under conditions where he/she expects a substantial differential in the rewards and costs from meeting the demand versus not meeting it” (McGrath 1976).
It is appropriate to state that the degree to which the demand exceeds the perceived expectation and the degree of differential rewards expected from meeting or not meeting that demand reflect the amount of stress that the person experiences. McGrath further suggests that stress may present itself in the following ways: “Cognitive-appraisal wherein subjectively experienced stress is contingent upon the person’s perception of the situation. In this category the emotional, physiological and behavioural responses are significantly influenced by the person’s interpretation of the ‘objective’ or external stress situation.”
Another component of stress is the individual’s past experience with a similar situation and his or her empirical response. Along with this is the reinforcement factor, whether positive or negative, successes or failures which can operate to reduce or enhance, respectively, levels of subjectively experienced stress.
Burnout is a form of stress. It is a process defined as a feeling of progressive deterioration and exhaustion and an eventual depletion of energy. It is also often accompanied by a loss of motivation, a feeling that suggests “enough, no more”. It is an overload that tends during the course of time to affect attitudes, mood and general behaviour (Freudenberger 1975; Freudenberger and Richelson 1981). The process is subtle; it develops slowly and sometimes occurs in stages. It is often not perceived by the person most affected, since he or she is the last individual to believe that the process is taking place.
The symptoms of burnout manifest themselves on a physical level as ill-defined psychosomatic complaints, sleep disturbances, excessive fatigue, gastrointestinal symptoms, backaches, headaches, various skin conditions or vague cardiac pains of an unexplained origin (Freudenberger and North 1986).
Mental and behavioural changes are more subtle. “Burnout is often manifest by a quickness to be irritated, sexual problems (e.g. impotence or frigidity), fault finding, anger and low frustration threshold” (Freudenberger 1984a).
Further affective and mood signs may be progressive detachment, loss of self-confidence and lowered self-esteem, depression, mood swings, an inability to concentrate or pay attention, an increased cynicism and pessimism, as well as a general sense of futility. Over a period of time the contented person becomes angry, the responsive person becomes silent and withdrawn and the optimist becomes a pessimist.
The affect feelings that appear to be most common are anxiety and depression. The anxiety most typically associated with work is performance anxiety. The forms of work conditions that are relevant in promoting this form of anxiety are role ambiguity and role overload (Srivastava 1989).
Wilke (1977) has indicated that “one area that presents particular opportunity for conflict for the personality-disordered individual concerns the hierarchical nature of work organizations. The source of such difficulties can rest with the individual, the organization, or some interactive combination.”
Depressive features are frequently found as part of the presenting symptoms of work-related difficulties. Estimates from epidemiological data suggest that depression affects 8 to 12% of men and 20 to 25% of women. The life expectancy experience of serious depressive reactions virtually assures that workplace issues for many people will be affected at some time by depression (Charney and Weissman 1988).
The seriousness of these observations was validated by a study conducted by Northwestern National Life Insurance Company—“Employee Burnout: America’s Newest Epidemic” (1991). It was conducted among 600 workers nationwide and identified the extent, causes, costs and solutions related to workplace stress. The most striking research findings were that one in three Americans seriously thought about quitting work in 1990 because of job stress, and a similar portion expected to experience job burnout in the future. Nearly half of the 600 respondents experienced stress levels as “extremely or very high.” Workplace changes such as cutting employee benefits, change of ownership, required frequent overtime or reduced workforce tend to speed up job stress.
MacLean (1986) further elaborates on job stressors as uncomfortable or unsafe working conditions, quantitative and qualitative overload, lack of control over the work process and work rate, as well as monotony and boredom.
Additionally, employers are reporting an ever-increasing number of employees with alcohol and drug abuse problems (Freudenberger 1984b). Divorce or other marital problems are frequently reported as employee stressors, as are long-term or acute stressors such as caring for an elderly or disabled relative.
Assessment and classification to diminish the possibility of burnout may be approached from the points of view related to vocational interests, vocational choices or preferences and characteristics of people with different preferences (Holland 1973). One might utilize computer-based vocational guidance systems, or occupational simulation kits (Krumboltz 1971).
Biochemical factors influence personality, and the effects of their balance or imbalance on mood and behaviour are found in the personality changes attendant on menstruation. In the last 25 years a great deal of work has been done on the adrenal catecholamines, epinephrine and norepinephrine and other biogenic amines. These compounds have been related to the experiencing of fear, anger and depression (Barchas et al. 1971).
The most commonly used psychological assessment devices are:
- Eysenck Personality Inventory and Mardsley Personality Inventory
- Gordon Personal Profile
- IPAT Anxiety Scale Questionnaire
- Study of Values
- Holland Vocational Preference Inventory
- Minnesota Vocational Interest Test
- Rorschach Inkblot Test
- Thematic Apperception Test
A discussion of burnout would not be complete without a brief overview of the changing family-work system. Shellenberger, Hoffman and Gerson (1994) indicated that “Families are struggling to survive in an increasingly complex and bewildering world. With more choices than they can consider, people are struggling to find the right balance between work, play, love and family responsibility.”
Concomitantly, women’s work roles are expanding, and over 90% of women in the US cite work as a source of identity and self-worth. In addition to the shifting roles of men and women, the preservation of two incomes sometimes requires changes in living arrangements, including moving for a job, long-distance commuting or establishing separate residences. All of these factors can put a great strain on a relationship and on work.
Solutions to offer to diminish burnout and stress on an individual level are:
- Learn to balance your life.
- Share your thoughts and communicate your concerns.
- Limit alcohol intake.
- Re-evaluate personal attitudes.
- Learn to set priorities.
- Develop interests outside of work.
- Do volunteer work.
- Re-evaluate your need for perfectionism.
- Learn to delegate and ask for assistance.
- Take time off.
- Exercise, and eat nutritional meals.
- Learn to take yourself less seriously.
On a larger scale, it is imperative that government and corporations accommodate to family needs. To reduce or diminish stress in the family-work system will require a significant reconfiguration of the entire structure of work and family life. “A more equitable arrangement in gender relationships and the possible sequencing of work and non-work over the life span with parental leaves of absence and sabbaticals from work becoming common occurrences” (Shellenberger, Hoffman and Gerson 1994).
As indicated by Entin (1994), increased differentiation of self, whether in a family or corporation, has important ramifications in reducing stress, anxiety and burnout.
Individuals need to be more in control of their own lives and take responsibility for their actions; and both individuals and corporations need to re-examine their value systems. Dramatic shifts need to take place. If we do not heed the statistics, then most assuredly burnout and stress will continue to remain the significant problem it has become for all society.
Post-Traumatic Stress Disorder and its Relation to Occupational Health and Injury Prevention
Beyond the broad concept of stress and its relationship to general health issues, there has been little attention to the role of psychiatric diagnosis in the prevention and treatment of the mental health consequences of work-related injuries. Most of the work on job stress has been concerned with the effects of exposure to stressful conditions over time, rather than to problems associated with a specific event such as a traumatic or life-threatening injury or the witnessing of an industrial accident or act of violence. At the same time, Post-traumatic Stress Disorder (PTSD), a condition which has received considerable credibility and interest since the mid-1980s, is being more widely applied in contexts outside of cases involving war trauma and victims of crime. With respect to the workplace, PTSD has begun to appear as the medical diagnosis in cases of occupational injury and as the emotional outcome of exposure to traumatic situations occurring in the workplace. It is often the subject of controversy and some confusion with respect to its relationship to work conditions and the responsibility of the employer when claims of psychological injury are made. The occupational health practitioner is called upon increasingly to advise on company policy in the handling of these exposures and injury claims, and to render medical opinions with respect to the diagnosis, treatment and ultimate job status of these employees. Familiarity with PTSD and its related conditions is therefore increasingly important for the occupational health practitioner.
The following topics will be reviewed in this article:
- differential diagnosis of PTSD with other conditions such as primary depression and anxiety disorders
- relationship of PTSD to stress-related somatic complaints
- prevention of post-traumatic stress reactions in survivors and witnesses of psychologically traumatic events occurring in the workplace
- prevention and treatment of complications of work injury related to post-traumatic stress.
Post-traumatic Stress Disorder affects people who have been exposed to traumatizing events or conditions. It is characterized by symptoms of numbing, psychological and social withdrawal, difficulties controlling emotion, especially anger, and intrusive recollection and reliving of experiences of the traumatic event. By definition, a traumatizing event is one that is outside the normal range of everyday life events and is experienced as overwhelming by the individual. A traumatic event usually involves a threat to one’s own life or to someone close, or the witnessing of an actual death or serious injury, especially when this occurs suddenly or violently.
The psychiatric antecedents of our current concept of PTSD go back to the descriptions of “battle fatigue” and “shell shock” during and after the World Wars. However, the causes, symptoms, course and effective treatment of this often debilitating condition were still poorly understood when tens of thousands of Vietnam-era combat veterans began to appear in the US Veterans Administration Hospitals, offices of family doctors, jails and homeless shelters in the 1970s. Due in large part to the organized effort of veterans’ groups, in collaboration with the American Psychiatric Association, PTSD was first identified and described in 1980 in the 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM III) (American Psychiatric Association 1980). The condition is now known to affect a wide range of trauma victims, including survivors of civilian disasters, victims of crime, torture and terrorism, and survivors of childhood and domestic abuse. Although changes in the classification of the disorder are reflected in the current diagnostic manual (DSM IV), the diagnostic criteria and symptoms remain essentially unchanged (American Psychiatric Association 1994).
Diagnostic Criteria for Post-TraumaticStress Disorder
A. The person has been exposed to a traumatic event in which both of the following were present:
- The person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others.
- The person’s response involved intense fear, helplessness or horror.
B. The traumatic event is persistently re-experienced in one (or more) of the following ways:
- Recurrent and intrusive distressing recollections of the event, including images, thoughts or perceptions.
- Recurrent distressing dreams of the event.
- Acting or feeling as if the traumatic event were recurring.
- Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event.
- Physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event.
C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three (or more) of the following:
- Efforts to avoid thoughts, feelings or conversations associated with the trauma.
- Efforts to avoid activities, places or people that arouse recollections of the trauma.
- Inability to recall an important aspect of the trauma.
- Markedly diminished interest or participation in significant activities.
- Feeling of detachment or estrangement from others.
- Restricted range of affect (e.g., unable to have loving feelings).
- Sense of a foreshortened future (e.g., does not expect to have a career, marriage, children or a normal life span).
D. Persistent symptoms of increased arousal (not present before the trauma), as indicated by two (or more) of the following:
- Difficulty falling or staying asleep.
- Irritability or outbursts of anger.
- Difficulty concentrating.
- Hypervigilance.
- Exaggerated startle response.
E. Duration of the disturbance (symptoms in criteria B, C and D) is more than 1 month.
F. The disturbance causes clinically significant distress or impairment in social, occupational or other important areas of functioning.
Specify if:
Acute: if duration of symptoms is less than 3 months
Chronic: if duration of symptoms is 3 months or more.
Specify if:
With Delayed Onset: if onset of symptoms is at least 6 months after the stressor.
Psychological stress has achieved increasing recognition as an outcome of work-related hazards. The link between work hazards and post-traumatic stress was first established in the 1970s with the discovery of high incident rates of PTSD in workers in law enforcement, emergency medical, rescue and firefighting. Specific interventions have been developed to prevent PTSD in workers exposed to job-related traumatic stressors such as mutilating injury, death and use of deadly force. These interventions emphasize providing exposed workers with education about normal traumatic stress reactions, and the opportunity to actively surface their feelings and reactions with their peers. These techniques have become well established in these occupations in the United States, Australia and many European nations. Job-related traumatic stress, however, is not limited to workers in these high-risk industries. Many of the principles of preventive intervention developed for these occupations can be applied to programmes to reduce or prevent traumatic stress reactions in the general workforce.
Issues in Diagnosis and Treatment
Diagnosis
The key to the differential diagnosis of PTSD and traumatic-stress-related conditions is the presence of a traumatic stressor. Although the stressor event must conform to criterion A—that is, be an event or situation that is outside of the normal range of experience—individuals respond in various ways to similar events. An event that precipitates a clinical stress reaction in one person may not affect another significantly. Therefore, the absence of symptoms in other similarly exposed workers should not cause the practitioner to discount the possibility of a true post-trauma reaction in a particular worker. Individual vulnerability to PTSD has as much to do with the emotional and cognitive impact of an experience on the victim as it does to the intensity of the stressor itself. A prime vulnerability factor is a history of psychological trauma due to a previous traumatic exposure or significant personal loss of some kind. When a symptom picture suggestive of PTSD is presented, it is important to establish whether an event that may satisfy the criterion for a trauma has occurred. This is particularly important because the victim himself may not make the connection between his symptoms and the traumatic event. This failure to connect the symptom with the cause follows the common “numbing” reaction, which may cause forgetting or dissociation of the event, and because it is not unusual for symptom appearance to be delayed for weeks or months. Chronic and often severe depression, anxiety and somatic conditions are often the result of a failure to diagnose and treat. Thus, early diagnosis is particularly important because of the often hidden nature of the condition, even to the sufferer him- or herself, and because of the implications for treatment.
Treatment
Although the depression and anxiety symptoms of PTSD may respond to usual therapies such as pharmacology, effective treatment is different from those usually recommended for these conditions. PTSD may be the most preventable of all psychiatric conditions and, in the occupational health sphere, perhaps the most preventable of all work-related injuries. Because its occurrence is linked so directly to a specific stressor event, treatment can focus on prevention. If proper preventive education and counselling are provided soon after the traumatic exposure, subsequent stress reactions can be minimized or prevented altogether. Whether the intervention is preventive or therapeutic depends largely on timing, but the methodology is essentially similar. The first step in successful treatment or preventive intervention is allowing the victim to establish the connection between the stressor and his or her symptoms. This identification and “normalization” of what are typically frightening and confusing reactions is very important for reduction or prevention of symptoms. Once the normalization of the stress response has been accomplished, treatment addresses the controlled processing of the emotional and cognitive impact of the experience.
PTSD or conditions related to traumatic stress result from the sealing off of unacceptable or unacceptably intense emotional and cognitive reactions to traumatic stressors. It is generally considered that the stress syndrome can be prevented by providing the opportunity for controlled processing of the reactions to the trauma before the sealing off of the trauma occurs. Thus, prevention through timely and skilled intervention is the keystone for the treatment of PTSD. These treatment principles may depart from the traditional psychiatric approach to many conditions. Therefore, it is important that employees at risk of post-traumatic stress reactions be treated by mental health professionals with specialized training and experience in treating trauma-related conditions. The length of treatment is variable. It will depend on the timing of the intervention, the severity of the stressor, symptom severity and the possibility that a traumatic exposure may precipitate an emotional crisis linked to earlier or related experiences. A further issue in treatment concerns the importance of group treatment modalities. Victims of trauma can achieve enormous benefit from the support of others who have shared the same or similar traumatic stress experience. This is of particular importance in the workplace context, when groups of co-workers or entire work organizations are affected by a tragic accident, act of violence or traumatic loss.
Prevention of Post-Traumatic Stress Reactionsafter Incidents of Workplace Trauma
A range of events or situations occurring in the workplace may put workers at risk of post-traumatic stress reactions. These include violence or threat of violence, including suicide, inter-employee violence and crime, such as armed robbery; fatal or severe injury; and sudden death or medical crisis, such as heart attack. Unless properly managed, these situations can cause a range of negative outcomes, including post-traumatic stress reactions that may reach clinical levels, and other stress-related effects that will affect health and work performance, including avoidance of the workplace, concentration difficulties, mood disturbances, social withdrawal, substance abuse and family problems. These problems can affect not only line employees but management staff as well. Managers are at particular risk because of conflicts between their operational responsibilities, their feelings of personal responsibility for the employees in their charge and their own sense of shock and grief. In the absence of clear company policies and prompt assistance from health personnel to deal with the aftermath of the trauma, managers at all levels may suffer from feelings of helplessness that compound their own traumatic stress reactions.
Traumatic events in the workplace require a definite response from upper management in close collaboration with health, safety, security, communications and other functions. A crisis response plan fulfils three primary goals:
- prevention of post-traumatic stress reactions by reaching affected individuals and groups before they have a chance to seal over
- communication of crisis-related information in order to contain fears and control rumours
- fostering of confidence that management is in control of the crisis and demonstrating concern for employees’ welfare.
The methodology for the implementation of such a plan has been fully described elsewhere (Braverman 1992a,b; 1993b). It emphasizes adequate communication between management and employees, assembling of groups of affected employees and prompt preventive counselling of those at highest risk for post-traumatic stress because of their levels of exposure or individual vulnerability factors.
Managers and company health personnel must function as a team to be sensitive for signs of continued or delayed trauma-related stress in the weeks and months after the traumatic event. These can be difficult to identify for manager and health professional alike, because post-traumatic stress reactions are often delayed, and they can masquerade as other problems. For a supervisor or for the nurse or counsellor who becomes involved, any signs of emotional stress, such as irritability, withdrawal or a drop in productivity, may signal a reaction to a traumatic stressor. Any change in behaviour, including increased absenteeism, or even a marked increase in work hours (“workaholism”) can be a signal. Indications of drug or alcohol abuse or change in moods should be explored as possibly linked to post-traumatic stress. A crisis response plan should include training for managers and health professionals to be alert for these signs so that intervention can be rendered at the earliest possible point.
Stress-related Complications of Occupational Injury
It has been our experience reviewing workers’ compensation claims up to five years post-injury that post-traumatic stress syndromes are a common outcome of occupational injury involving life-threatening or disfiguring injury, or assault and other exposures to crime. The condition typically remains undiagnosed for years, its origins unsuspected by medical professionals, claims administrators and human resource managers, and even the employee him- or herself. When unrecognized, it can slow or even prevent recovery from physical injury.
Disabilities and injuries linked to psychological stress are among the most costly and difficult to manage of all work-related injuries. In the “stress claim”, an employee maintains he or she has been emotionally damaged by an event or conditions at work. Costly and hard to fight, stress claims usually result in litigation and in the separation of the employee. There exists, however, a vastly more frequent but seldom recognized source of stress-related claims. In these cases, serious injury or exposure to life-threatening situations results in undiagnosed and untreated psychological stress conditions that significantly affect the outcome of work-related injuries.
On the basis of our work with traumatic worksite injuries and violent episodes over a wide range of worksites, we estimate that at least half of disputed workers’ compensation claims involve unrecognized and untreated post-traumatic stress conditions or other psychosocial components. In the push to resolve medical problems and determine the employee’s employment status, and because of many systems’ fear and mistrust of mental health intervention, emotional stress and psychosocial issues take a back seat. When no one deals with it, stress can take the form of a number of medical conditions, unrecognized by the employer, the risk manager, the health care provider and the employee him- or herself. Trauma-related stress also typically leads to avoidance of the workplace, which increases the risk of conflicts and disputes regarding return to work and claims of disability.
Many employers and insurance carriers believe that contact with a mental health professional leads directly to an expensive and unmanageable claim. Unfortunately, this is often the case. Statistics bear out that claims for mental stress are more expensive than claims for other kinds of injuries. Furthermore, they are increasing faster than any other kind of injury claim. In the typical “physical-mental” claim scenario, the psychiatrist or psychologist appears only at the point—typically months or even years after the event—when there is a need for expert assessment in a dispute. By this time, the psychological damage has been done. The trauma-related stress reaction may have prevented the employee from returning to the workplace, even though he or she appeared visibly healed. Over time, the untreated stress reaction to the original injury has resulted in a chronic anxiety or depression, a somatic illness or a substance abuse disorder. Indeed, it is rare that mental health intervention is rendered at the point when it can prevent the trauma-related stress reaction and thus help the employee fully recover from the trauma of a serious injury or assault.
With a small measure of planning and proper timing, the costs and suffering associated with injury-related stress are among the most preventable of all injuries. The following are the components of an effective post-injury plan (Braverman 1993a):
Early intervention
Companies should require a brief mental health intervention whenever a severe accident, assault or other traumatic event impacts on an employee. This evaluation should be seen as preventive, rather than as tied to the standard claims procedure. It should be provided even if there is no lost time, injury or need for medical treatment. The intervention should emphasize education and prevention, rather than a strictly clinical approach that may cause the employee to feel stigmatized. The employer, perhaps in conjunction with the insurance provider, should take responsibility for the relatively small cost of providing this service. Care should be taken that only professionals with specialized expertise or training in post-traumatic stress conditions be involved.
Return to work
Any counselling or assessment activity should be coordinated with a return-to-work plan. Employees who have undergone a trauma often feel afraid or tentative about returning to the worksite. Combining brief education and counselling with visits to the workplace during the recovery period has been used to great advantage in accomplishing this transition and speeding return to work. Health professionals can work with the supervisor or manager in developing gradual re-entry into job functioning. Even when there is no remaining physical limitation, emotional factors may necessitate accommodations, such as allowing a bank teller who was robbed to work in another area of the bank for part of the day as she gradually becomes comfortable returning to work at the customer window.
Follow-up
Post-traumatic reactions are often delayed. Follow-up at 1- and 6-month intervals with employees who have returned to work is important. Supervisors are also provided with fact sheets on how to spot possible delayed or long-term problems associated with post-traumatic stress.
Summary: The Link between Post-Traumatic Stress Studies and Occupational Health
Perhaps more than any other health science, occupational medicine is concerned with the relationship between human stress and disease. Indeed, much of the research in human stress in this century has taken place within the occupational health field. As the health sciences in general became more involved in prevention, the workplace has become increasingly important as an arena for research into the contribution of the physical and psychosocial environment to disease and other health outcomes, and into methods for the prevention of stress-related conditions. At the same time, since 1980 a revolution in the study of post-traumatic stress has brought important progress to the understanding of the human stress response. The occupational health practitioner is at the intersection of these increasingly important fields of study.
As the landscape of work undergoes revolutionary transformation, and as we learn more about productivity, coping and the stressful impact of continued change, the line between chronic stress and acute or traumatic stress has begun to blur. The clinical theory of traumatic stress has much to tell us about how to prevent and treat work-related psychological stress. As in all health sciences, knowledge of the causes of a syndrome can help in prevention. In the area of traumatic stress, the workplace has shown itself to be an excellent place to promote health and healing. By being well acquainted with the symptoms and causes of post-traumatic stress reactions, occupational health practitioners can increase their effectiveness as agents of prevention.
Work-Related Anxiety
Anxiety disorders as well as subclinical fear, worry and apprehension, and associated stress-related disorders such as insomnia, appear to be pervasive and increasingly prevalent in workplaces in the 1990s—so much so, in fact, that the Wall Street Journal has referred to the 1990s as the work-related “Age of Angst” (Zachary and Ortega 1993). Corporate downsizing, threats to existing benefits, lay-offs, rumours of impending lay-offs, global competition, skill obsolescence and “de-skilling”, re-structuring, re-engineering, acquisitions, mergers and similar sources of organizational turmoil have all been recent trends that have eroded workers’ sense of job security and have contributed to palpable, but difficult to precisely measure, “work-related anxiety” (Buono and Bowditch 1989). Although there appear to be some individual differences and situational moderator variables, Kuhnert and Vance (1992) reported that both blue-collar and white-collar manufacturing employees who reported more “job insecurity” indicated significantly more anxiety and obsessive-compulsive symptoms on a psychiatric checklist. For much of the 1980s and accelerating into the 1990s, the transitional organizational landscape of the US marketplace (or “permanent whitewater”, as it has been described) has undoubtedly contributed to this epidemic of work-related stress disorders, including, for example, anxiety disorders (Jeffreys 1995; Northwestern National Life 1991).
The problems of occupational stress and work-related psychological disorders appear to be global in nature, but there is a dearth of statistics outside of the United States documenting their nature and extent (Cooper and Payne 1992). The international data that are available, mostly from European countries, seem to confirm similar adverse mental health effects of job insecurity and high-strain employment on workers as those seen in US workers (Karasek and Theorell 1990). However, because of the very real stigma associated with mental disorders in most other countries and cultures, many, if not most, psychological symptoms, such as anxiety, related to work (outside of the United States) go unreported, undetected and untreated (Cooper and Payne 1992). In some cultures, these psychological disorders are somatized and manifested as “more acceptable” physical symptoms (Katon, Kleinman and Rosen 1982). A study of Japanese government workers has identified occupational stressors such as workload and role conflict as significant correlates of mental health in these Japanese workers (Mishima et al. 1995). Further studies of this kind are needed to document the impact of psychosocial job stressors on workers’ mental health in Asia, as well as in the developing and post-Communist countries.
Definition and Diagnosis of Anxiety Disorders
Anxiety disorders are evidently among the most prevalent of mental health problems afflicting, at any one time, perhaps 7 to 15% of the US adult population (Robins et al. 1981). Anxiety disorders are a family of mental health conditions which include agoraphobia (or, loosely, “houseboundness”), phobias (irrational fears), obsessive-compulsive disorder, panic attacks and generalized anxiety. According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM IV), symptoms of a generalized anxiety disorder include feelings of “restlessness or feeling keyed up or on edge”, fatigue, difficulties with concentration, excess muscle tension and disturbed sleep (American Psychiatric Association 1994). An obsessive-compulsive disorder is defined as either persistent thoughts or repetitive behaviours that are excessive/unreasonable, cause marked distress, are time consuming and can interfere with a person’s functioning. Also, according to DSM IV, panic attacks, defined as brief periods of intense fear or discomfort, are not actually disorders per se but may occur in conjunction with other anxiety disorders. Technically, the diagnosis of an anxiety disorder can be made only by a trained mental health professional using accepted diagnostic criteria.
Occupational Risk Factors for Anxiety Disorders
There is a paucity of data pertaining to the incidence and prevalence of anxiety disorders in the workplace. Furthermore, since the aetiology of most anxiety disorders is multifactorial, we cannot rule out the contribution of individual genetic, developmental and non-work factors in the genesis of anxiety conditions. It seems likely that both work-related organizational and such individual risk factors interact, and that this interaction determines the onset, progression and course of anxiety disorders.
The term job-related anxiety implies that there are work conditions, tasks and demands, and/or related occupational stressors that are associated with the onset of acute and/or chronic states of anxiety or manifestations of anxiety. These factors may include an overwhelming workload, the pace of work, deadlines and a perceived lack of personal control. The demand-control model predicts that workers in occupations which offer little personal control and expose employees to high levels of psychological demand would be at risk of adverse health outcomes, including anxiety disorders (Karasek and Theorell 1990). A study of pill consumption (mostly tranquilizers) reported for Swedish male employees in high-strain occupations supported this prediction (Karasek 1979). Certainly, the evidence for an increased prevalence of depression in certain high-strain occupations in the United States is now compelling (Eaton et al. 1990). More recent epidemiological studies, in addition to theoretical and biochemical models of anxiety and depression, have linked these disorders not only by identifying their co-morbidity (40 to 60%), but also in terms of more fundamental commonalities (Ballenger 1993). Hence, the Encyclopaedia chapter on job factors associated with depression may provide pertinent clues to occupational and individual risk factors also associated with anxiety disorders. In addition to risk factors associated with high-strain work, a number of other workplace variables contributing to employee psychological distress, including an increased prevalence of anxiety disorders, have been identified and are briefly summarized below.
Individuals employed in dangerous lines of work, such as law enforcement and firefighting, characterized by the probability that a worker will be exposed to a hazardous agent or injurious activity, would also seem to be at risk of heightened and more prevalent states of psychological distress, including anxiety. However, there is some evidence that individual workers in such dangerous occupations who view their work as “exhilarating” (as opposed to dangerous) may cope better in terms of their emotional responses to work (McIntosh 1995). Nevertheless, an analysis of stress symptomatology in a large group of professional firefighters and paramedics identified a central feature of perceived apprehension or dread. This “anxiety stress pathway” included subjective reports of “being keyed up and jittery” and “being uneasy and apprehensive.” These and similar anxiety-related complaints were significantly more prevalent and frequent in the firefighter/paramedic group relative to a male community comparison sample (Beaton et al. 1995).
Another worker population evidently at risk of experiencing high, and at times debilitating, levels of anxiety are professional musicians. Professional musicians and their work are exposed to intense scrutiny by their supervisors; they must perform before the public and must cope with performance and pre-performance anxiety or “stage fright”; and they are expected (by others as well as by themselves) to produce “note-perfect performances” (Sternbach 1995). Other occupational groups, such as theatrical performers and even teachers who give public performances, may have acute and chronic anxiety symptoms related to their work, but very little data on the actual prevalence or significance of such occupational anxiety disorders have been collected.
Another class of work-related anxiety for which we have little data is “computer phobics”, people who have responded anxiously to the advent of computing technology (Stiles 1994). Even though each generation of computer software is arguably more “user-friendly”, many workers are uneasy, while other workers are literally panicked by challenges of “techno-stress”. Some fear personal and professional failure associated with their inability to acquire the necessary skills to cope with each successive generation of technology. Finally, there is evidence that employees subjected to electronic performance monitoring perceive their jobs as more stressing and report more psychological symptoms, including anxiety, than workers not so monitored (Smith et al. 1992).
Interaction of Individual and Occupational Risk Factors for Anxiety
It is likely that individual risk factors interact with and may potentiate the above-cited organizational risk factors at the onset, progression and course of anxiety disorders. For example, an individual employee with a “Type A personality” may be more prone to anxiety and other mental health problems in high-strain occupational settings (Shima et al. 1995). To offer a more specific example, an overly responsible paramedic with a “rescue personality” may be more on edge and hypervigilant while on duty then another paramedic with a more philosophical work attitude: “You can’t save them all” (Mitchell and Bray 1990). Individual worker personality variables may also serve to potentially buffer attendant occupational risk factors. For instance, Kobasa, Maddi and Kahn (1982) reported that corporate managers with “hardy personalities” seem better able to cope with work-related stressors in terms of health outcomes. Thus, individual worker variables need to be considered and evaluated within the context of the particular occupational demands to predict their likely interactive impact on a given employee’s mental health.
Prevention and Remediation ofWork-related Anxiety
Many of the US and global workplace trends cited at the beginning of this article seem likely to persist into the foreseeable future. These workplace trends will adversely impact workers’ psychological and physical health. Psychological job enhancement, in terms of interventions and workplace redesign, may deter and prevent some of these adverse effects. Consistent with the demand-control model, workers’ well-being can be improved by increasing their decision latitude by, for example, designing and implementing a more horizontal organizational structure (Karasek and Theorell 1990). Many of the recommendations made by NIOSH researchers, such as improving workers’ sense of job security and decreasing work role ambiguity, if implemented, would also likely reduce job strain and work-related psychological disorders considerably, including anxiety disorders (Sauter, Murphy and Hurrell 1992).
In addition to organizational policy changes, the individual employee in the modern workplace also has a personal responsibility to manage his or her own stress and anxiety. Some common and effective coping strategies employed by US workers include separating work and non-work activities, getting sufficient rest and exercise, and pacing oneself at work (unless, of course, the job is machine paced). Other helpful cognitive-behavioural alternatives in self-managing and preventing anxiety disorders include deep-breathing techniques, biofeedback-aided relaxation training, and meditation (Rosch and Pelletier 1987). In certain cases medications may be necessary to treat a severe anxiety disorder. These medications, including antidepressants and other anxiolytic agents, are generally available only by prescription.
Depression
Depression is an enormously important topic in the area of workplace mental health, not only in terms of the impact depression can have on the workplace, but also the role the workplace can play as an aetiological agent of the disorder.
In a 1990 study, Greenberg et al. (1993a) estimated that the economic burden of depression in the United States that year was approximately US$ 43.7 billion. Of that total, 28% was attributable to direct costs of medical care, but 55% was derived from a combination of absenteeism and decreased productivity while at work. In another paper, the same authors (1993b) note:
“two distinguishing features of depression are that it is highly treatable and not widely recognized. The NIMH has noted that between 80% and 90% of individuals suffering from a major depressive disorder can be treated successfully, but that only one in three with the illness ever seeks treatment.… Unlike some other diseases, a very large share of the total costs of depression falls on employers. This suggests that employers as a group may have a particular incentive to invest in programs that could reduce the costs associated with this illness.”
Manifestations
Everyone feels sad or “depressed” from time to time, but a major depressive episode, according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM IV) (American Psychiatric Association 1994), requires that several criteria be met. A full description of these criteria is beyond the scope of this article, but portions of criterion A, which describes the symptoms, can give one a sense of what a true major depression looks like:
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is number 1 or 2.
- depressed mood most of the day, nearly every day
- markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
- significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day
- insomnia or hypersomnia nearly every day
- psychomotor agitation or retardation nearly every day
- fatigue or loss of energy nearly every day
- feelings of worthlessness or excessive or inappropriate guilt nearly every day
- diminished ability to think or concentrate, or indecisiveness nearly every day
- recurrent thoughts of death, recurrent suicidal ideation, with or without a plan, or a suicide attempt.
Besides giving one an idea of the discomfort suffered by a person with depression, a review of these criteria also shows the many ways depression can impact negatively on the workplace. It is also important to note the wide variation of symptoms. One depressed person may present barely able to move to get out of bed, while others may be so anxious they can hardly sit still and describe themselves as crawling out of their skin or losing their mind. Sometimes multiple physical aches and pains without medical explanation may be a hint of depression.
Prevalence
The following passage from Mental Health in the Workplace (Kahn 1993) describes the pervasiveness (and increase) of depression in the workplace:
“Depression … is one of the most common mental health problems in the workplace. Recent research … suggests that in industrialized countries the incidence of depression has increased with each decade since 1910, and the age at which someone is likely to become depressed has dropped with every generation born after 1940. Depressive illnesses are common and serious, taking a tremendous toll on both workers and workplace. Two out of ten workers can expect a depression during their lifetime, and women are one and a half times more likely than men to become depressed. One out of ten workers will develop a clinical depression serious enough to require time off from work.”
Thus, in addition to the qualitative aspects of depression, the quantitative/epidemiological aspects of the disease make it a major concern in the workplace.
Related Illnesses
Major depressive disorder is only one of a number of closely related illnesses, all under the category of “mood disorders”. The most well known of these is bipolar (or “manic-depressive”) illness, in which the patient has alternating periods of depression and mania, which includes a feeling of euphoria, a decreased need for sleep, excessive energy and rapid speech, and can progress to irritability and paranoia.
There are several different versions of bipolar disorder, depending on the frequency and severity of the depressive and manic episodes, the presence or absence of psychotic features (delusions, hallucinations) and so on. Similarly, there are several different variations on the theme of depression, depending on severity, presence or absence of psychosis, and types of symptom most prominent. Again, it is beyond the scope of this article to delineate all of these, but the reader is again referred to DSM IV for a complete listing of all the different forms of mood disorder.
Differential Diagnosis
The differential diagnosis of major depression involves three major areas: other medical disorders, other psychiatric disorders and medication-induced symptoms.
Just as important as the fact that many patients with depression first present to their general practitioners with physical complaints is the fact that many patients who initially present to a mental health clinician with depressive complaints may have an undiagnosed medical illness causing the symptoms. Some of the most common illnesses causing depressive symptoms are endocrine (hormonal), such as hypothyroidism, adrenal problems or changes related to pregnancy or the menstrual cycle. Particularly in older patients, neurological diseases, such as dementia, strokes or Parkinson’s disease, become more prominent in the differential diagnosis. Other illnesses that can present with depressive symptoms are mononucleosis, AIDS, chronic fatigue syndrome and some cancers and joint diseases.
Psychiatrically, the disorders which share many common features with depression are the anxiety disorders (including generalized anxiety, panic disorder and post-traumatic stress disorder), schizophrenia and drug and alcohol abuse. The list of medications that can cause depressive symptoms is quite lengthy, and includes pain medications, some antibiotics, many anti-hypertensives and cardiac drugs, and steroids and hormonal agents.
For further detail on all three areas of the differential diagnosis of depression, the reader is referred to Kaplan and Sadock’s Synopsis of Psychiatry (1994), or the more detailed Comprehensive Textbook of Psychiatry (Kaplan and Sadock 1995).
Workplace Aetiologies
Much can be found elsewhere in this Encyclopaedia regarding workplace stress, but what is important in this article is the manner in which certain aspects of stress can lead to depression. There are many schools of thought regarding the aetiology of depression, including biological, genetic and psychosocial. It is in the psychosocial realm that many factors relating to the workplace can be found.
Issues of loss or threatened loss can lead to depression and, in today’s climate of downsizing, mergers and shifting job descriptions, are common problems in the work environment. Another result of frequently changing job duties and the constant introduction of new technologies is to leave workers feeling incompetent or inadequate. According to psychodynamic theory, as the gap between one’s current self image and “ideal self” widens, depression ensues.
An animal experimental model known as “learned helplessness” can also be used to explain the ideological link between stressful workplace environments and depression. In these experiments, animals were exposed to electric shocks from which they could not escape. As they learned that none of the actions they took had any effect on their eventual fate, they displayed increasingly passive and depressive behaviours. It is not difficult to extrapolate this model to today’s workplace, where so many feel a sharply decreasing amount of control over both their day-to-day activities and long-range plans.
Treatment
In light of the aetiological link of the workplace to depression described above, a useful way of looking at the treatment of depression in the workplace is the primary, secondary, tertiary model of prevention. Primary prevention, or trying to eliminate the root cause of the problem, entails making fundamental organizational changes to ameliorate some of the stressors described above. Secondary prevention, or trying to “immunize” the individual from contracting the illness, would include such interventions as stress management training and lifestyle changes. Tertiary prevention, or helping to return the individual to health, involves both psychotherapeutic and psychopharmacological treatment.
There is an increasing array of psychotherapeutic approaches available to the clinician today. The psychodynamic therapies look at the patient’s struggles and conflicts in a loosely structured format that allows explorations of whatever material may come up in a session, however tangential it may initially appear. Some modifications of this model, with boundaries set in terms of number of sessions or breadth of focus, have been made to create many of the newer forms of brief therapy. Interpersonal therapy focuses more exclusively on the patterns of the patient’s relationships with others. An increasingly popular form of therapy is cognitive therapy, which is driven by the precept, “What you think is how you feel”. Here, in a very structured format, the patient’s “automatic thoughts” in response to certain situations are examined, questioned and then modified to produce a less maladaptive emotional response.
As rapidly as the psychotherapies have developed, the psychopharmacological armamentarium has probably grown even faster. In the few decades before the 1990s, the most common medications used to treat depression were the tricyclics (imipramine, amitriptyline and nortriptyline are examples) and the monoamine oxidase inhibitors (Nardil, Marplan and Parnate). These medications act on neurotransmitter systems thought to be involved with depression, but also affect many other receptors, resulting in a number of side effects. In the early 1990s, several new medications (fluoxetine, sertraline, Paxil, Effexor, fluvoxamine and nefazodone) were introduced. These medications have enjoyed rapid growth because they are “cleaner” (bind more specifically to depression-related neurotransmitter sites) and can thus effectively treat depression while causing much fewer side effects.
Summary
Depression is extremely important in the world of workplace mental health, both because of depression’s impact on the workplace, and the workplace’s impact on depression. It is a highly prevalent disease, and very treatable; but unfortunately frequently goes undetected and untreated, with serious consequences for both the individual and the employer. Thus, increased detection and treatment of depression can help lessen individual suffering and organizational losses.
Work-Related Psychosis
Psychosis is a general term often used to describe a severe impairment in mental functioning. Usually, this impairment is so substantial that the individual is unable to carry on normal activities of daily living, including most work activities. More formally, Yodofsky, Hales and Fergusen (1991) define psychosis as:
“A major mental disorder of organic or emotional origin in which a person’s ability to think, respond emotionally, remember, communicate, interpret reality and behave appropriately is sufficiently impaired so as to interfere grossly with the capacity to meet the ordinary demands of life. [Symptoms are] often characterized by regressive behaviour, inappropriate mood, diminished impulse control and such abnormal mental context as delusions and hallucinations [p. 618].”
Psychotic disorders are comparatively rare in the general population. Their incidence in the workplace is even lower, probably due to the fact that many individuals who frequently become psychotic often have problems maintaining stable employment (Jorgensen 1987). Precisely how rare it is, is difficult to estimate. However, there are some suggestions that the prevalence within the general population of psychoses (e.g., schizophrenia) is less than 1% (Bentall 1990; Eysenck 1982). While psychosis is rare, individuals who are actively experiencing a psychotic state usually exhibit profound difficulties in functioning at work and in other aspects of their lives. Sometimes acutely psychotic individuals exhibit behaviours which are engaging, inspiring or even humorous. For example, some individuals who suffer from bipolar illness and are entering a manic phase exhibit high energy and grand ideas or plans. For the most part, however, psychosis is associated with behaviours which evoke reactions such as discomfort, anxiety, anger or fear in co-workers, supervisors and others.
This article will first provide an overview of the various neurological conditions and mental states in which psychosis can occur. Then, it will review workplace factors potentially associated with the occurrence of psychosis. Finally, it will summarize treatment approaches for managing both the psychotic worker and the work environment (i.e., medical management, return-to-work clearance procedures, workplace accommodations and workplace consultations with supervisors and co-workers).
Neurological Conditions and Mental Stateswithin which Psychosis Occurs
Psychosis can occur within a number of diagnostic categories identified in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM IV) (American Psychiatric Association 1994). At this point, there is no commonly agreed upon definitive diagnostic set. The following are widely accepted as medical conditions within which psychoses arise.
Neurological and general medical conditions
Delusional symtomatology can be caused by a range of neurological disorders affecting the limbic system or basal ganglia, where cerebral cortical functioning remains intact. Partial complex seizure episodes are often preceded by olfactory hallucinations of peculiar smells. To an external observer, this seizure activity may appear to be simple staring or day-dreaming. Cerebral neoplasms, especially in temporal and occipital areas, can cause hallucinations. Also, delirium-causing diseases, such as Parkinson’s, Huntington’s, Alzheimer’s, and Pick’s, can result in altered states of consciousness. Several sexually transmitted diseases such as tertiary syphilis and AIDS can also produce psychosis. Lastly, deficiencies of certain nutrients, such as B-12, niacin, folic acid and thiamine, have the potential of causing neurological problems which can result in psychosis.
Psychotic symptoms such as hallucinations and delusions also occur among patients with various general medical conditions. These include several systemic diseases, such as hepatic encephalopathy, hypercalcaemia, diabetic ketoacidosis, and malfunction of endocrine glands (i.e., adrenal, thyroid, parathyroid and pituitary). Sensory and sleep deprivation have also been shown to cause psychosis.
Mental states
Schizophrenia is probably the most widely known of the psychotic disorders. It is a progressively deteriorating condition which usually has an insidious onset. A number of specific subcategories have been identified including paranoid, disorganized, catatonic, undifferentiated and residual types. People who suffer from this disorder often have limited work histories and often do not remain in the workforce. Occupational impairment among schizophrenics is very common, and many schizophrenics lose their interest or will to work as the disease progresses. Unless a job is of very low complexity, it is usually very difficult for them to stay employed.
Schizophreniform disorder is similar to schizophrenia, but an episode of this disorder is of short duration, usually lasting less than six months. Generally, persons with this disorder have good premorbid social and occupational functioning. As the symptoms resolve, the person returns to baseline functioning. Consequently, the occupational impact of this disorder may be significantly less than in cases of schizophrenia.
Schizoaffective disorder also has a better prognosis than schizophrenia but a worse prognosis than affective disorders. Occupational impairment is quite common in this group. Psychosis is also sometimes observed in major affective disorders. With appropriate treatment, occupational functioning among workers suffering from major affective disorders is generally substantially better than for those with schizophrenia or schizoaffective disorders.
Severe stressors such as losing a loved one or losing one’s job can result in a brief reactive psychosis. This psychotic disorder is probably observed more frequently in the workplace than other types of psychotic disorder, especially with schizoid, schizotypal and borderline features.
Delusional disorders are probably relatively common in the workplace. There are several types. The erotomanic type typically believes that another person, usually of a higher social status, is in love with them. Sometimes, they harass the person who they believe is in love with them by attempting contact via telephone calls, letters or even stalking. Often, individuals with these disorders are employed in modest occupations, living isolated and withdrawn lives with limited social and sexual contact. The grandiose type usually exhibits delusions of inflated worth, power, knowledge or a special relationship with a deity or a famous person. The jealous type believes inaccurately that their sexual partner has been unfaithful. The persecutory type believes inaccurately that they (or someone to whom they are close) are being cheated, maligned, harassed or in other ways malevolently treated. These persons are often resentful and angry and may resort to violence against those they believe to be hurting them. They rarely want to seek help, as they do not think there is anything wrong with them. Somatic types develop delusions, contrary to all evidence, that they are afflicted with infections. They can also believe that a part of their body is disfigured, or worry about having a bad body odour. These workers with delusional beliefs can often create work-related difficulties.
Work-related chemical factors
Chemical factors such as mercury, carbon disulphide, toluene, arsenic and lead have been known to cause psychosis in blue-collar workers. For example, mercury has been found to be responsible for causing psychosis in workers in the hat industry, appropriately named the “Mad Hatter’s psychosis” (Kaplan and Sadock 1995). Stopford (personal communication, 6 November 1995) suggests that carbon disulphide was found to cause psychosis among workers in France in 1856. In the United States, in 1989, two brothers in Nevada purchased a carbon disulphide compound to kill gophers. Their physical contact with this chemical resulted in severe psychosis—one brother shooting a person and the other shooting himself due to severe confusion and psychotic depression. The incidence of suicide and homicide increases thirteenfold with exposure to carbon disulphide. Further, Stopford reports that exposure to toluene (used in making explosives and dyestuffs) is known to cause acute encephalopathy and psychosis. Symptoms can manifest also as memory loss, mood changes (e.g., dysphoria), deterioration in eye-hand coordination and speech impediments. Hence, some organic solvents, especially those found in the chemical industry, have a direct influence on the human central nervous system (CNS), causing biochemical changes and unpredictable behaviour (Levi, Frandenhaeuser and Gardell 1986). Special precautions, procedures and protocols have been established by the US Occupational Safety and Health Administration (OSHA), National Institute for Occupational Safety and Health (NIOSH) and the chemical industry to ensure minimum risk to employees working with toxic chemicals in their work environments.
Other factors
A number of medications can cause delirium which in turn can result in psychosis. These include antihypertensives, anticholinergics (including a number of medications used to treat the common cold), antidepressants, anti-tuberculosis medicines, anti-Parkinson’s disease medicines, and ulcer medicines (such as cimetidine). Further, substance-induced psychosis can be caused by a number of licit and illicit drugs which are sometimes abused, such as alcohol, amphetamines, cocaine, PCP, anabolic steroids and marijuana. The delusions and hallucinations which result are usually temporary. Although the content may vary, persecutory delusions are quite common. In alcohol-related hallucinations a person may believe that he or she is hearing voices which are threatening, insulting, critical or condemning. Sometimes, these insulting voices speak in the third person. As with individuals exhibiting paranoid or persecutory delusions, these individuals should be carefully evaluated for dangerousness to self or others.
Post-partum psychosis is comparatively uncommon in the workplace, but is worth noting as some women are returning to work more quickly. It tends to occur in new mothers (or more rarely fathers), usually within two to four weeks after delivery.
In a number of cultures, psychosis may result from various commonly held beliefs. A number of culturally based psychotic reactions have been described, including episodes such as “koro” in South and East Asia, “qi-gong psychotic reaction” within Chinese populations, “piblokto” in Eskimo communities and “whitigo” among several American Indian groups (Kaplan and Sadock 1995). The relationship of these psychotic phenomena to various occupational variables does not appear to have been studied.
Workplace Factors Associated with the Occurrence of Psychosis
Although information and empirical research on work-related psychosis are extremely scarce, due in part to the low prevalence in the work setting, researchers have noted a relationship between psychosocial factors in the work environment and psychological distress (Neff 1968; Lazarus 1991; Sauter, Murphy and Hurrell 1992; Quick et al. 1992). Significant psychosocial stressors on the job, such as role ambiguity, role conflicts, discrimination, supervisor-supervisee conflicts, work overload and work setting have been found to be associated with greater susceptibility to stress-related illness, tardiness, absenteeism, poor performance, depression, anxiety and other psychological distress (Levi, Frandenhaeuser and Gardell 1986; Sutherland and Cooper 1988).
Stress appears to have a prominent role in the complex manifestations of various types of physiological and psychological disorders. In the workplace, Margolis and Kroes (1974) believe that occupational stress occurs when some factor or combination of factors at work interact with the worker to disrupt his or her psychological or physiological homeostasis. These factors can be external or internal. External factors are the various pressures or demands from the external environment which stem from a person’s occupation, as well as from marriage, family or friends, whereas internal factors are the pressures and demands a worker places upon him- or herself—for example, by being “ambitious, materialistic, competitive and aggressive” (Yates 1989). It is these internal and external factors, separately or in combination, which can result in occupational distress whereby the worker experiences significant psychological and physical health problems.
Researchers have speculated on whether severe or cumulative stress, known as “stress-induced arousal”, originating from the work environment, could induce work-related psychotic disorders (Bentall, Dohrenwend and Skodol 1990; Link, Dohrenwend and Skodol 1986). For example, there is evidence linking hallucinatory and delusional experiences to specific stressful events. Hallucinations have been associated with stress-induced arousal occurring as a result of mining accidents, hostage situations, chemical-factory explosions, wartime exposure, sustained military operations and loss of a spouse (Comer, Madow and Dixon 1967; Hobfoll 1988; Wells 1983).
DeWolf (1986) believes that either the exposure to or interaction of multiple stressful conditions over an extended period of time is a complex process whereby some workers experience psychological health-related problems. Brodsky (1984) found in her examination of 2,000 workers who were her patients over 18 years that: (1) the timing, frequency, intensity and duration of unpleasant work conditions were potentially harmful, and she believed that 8 to 10% of the workforce experienced disabling psychological, emotional and physical health-related problems; and (2) workers react to work-related stress in part as “a function of perceptions, personality, age, status, life stage, unrealized expectations, prior experiences, social support systems and their capacity to respond adequately or adapt.” In addition, psychological distress can potentially be exacerbated by the worker feeling a sense of uncontrollability (e.g., inability to make decisions) and unpredictability in the work environment (e.g., corporate downsizing and reorganizing) (Labig 1995; Link and Stueve 1994).
Specific examination of the work-related “antecedents” of workers experiencing psychosis has received limited attention. The few researchers who have empirically examined the relationship between psychosocial factors in the work environment and severe psychopathology have found a relationship between “noisome” work conditions (i.e., noise, hazardous conditions, heat, humidity, fumes and cold) and psychosis (Link, Dohrenwend and Skodol 1986; Muntaner et al. 1991). Link, Dohrenwend and Skodol (1986) were interested in understanding the types of jobs schizophrenics had when they experienced their first schizophrenic episode. First full-time occupations were examined for workers who experienced: (a) schizophrenic or schizophrenic-like episodes; (b) depression; and (c) no psychopathology. These researchers found that noisome work conditions existed among more blue-collar than white-collar professions. These researchers concluded that noisome work conditions were potentially significant risk factors in the manifestation of psychotic episodes (i.e., schizophrenia).
Muntaner et al. (1991) replicated the findings of Link, Dohrenwend and Skodol (1986) and examined in greater detail whether various occupational stressors contributed to increased risk of developing or experiencing psychoses. Three types of psychotic condition were examined using the criteria of DSM III—schizophrenia; schizophrenia criterion A (hallucinations and delusions); and schizophrenia criterion A with affective episode (psychotic-affective disorder). Participants in their retrospective study were from a larger Epidemiologic Catchment Area (ECA) study examining the incidence of psychiatric disorders across five sites (Connecticut, Maryland, North Carolina, Missouri and California). These researchers found that psychosocial work characteristics (i.e., high physical demands, lack of control over work and working conditions—noisome factors) placed participants at increased risk of psychotic occurrences.
As illustrations, in the Muntaner et al. (1991) study, people in construction trade occupations (i.e., carpenters, painters, roofers, electricians, plumbers) were 2.58 times more likely to experience delusions or hallucinations than people in managerial occupations. Workers in housekeeping, laundry, cleaning and servant-type occupations were 4.13 times more likely to become schizophrenic than workers in managerial occupations. Workers who identified themselves as writers, artists, entertainers and athletes were 3.32 times more likely to experience delusions or hallucinations in comparison to workers in executive, administrative and managerial occupations. Lastly, workers in occupations such as sales, mail and message delivery, teaching, library science and counselling were more at risk of psychotic, affective disorders. It is important to note that the associations between psychotic conditions and occupational variables were examined after alcohol and drug use was controlled for in their study.
A significant difference between blue-collar and white-collar professions is the types of psychological demand and psychosocial stress placed on the worker. This is illustrated in the findings of Muntaner et al. (1993). They found an association between a work environment’s cognitive complexity and psychotic forms of mental illness. The most frequent occupations held by schizophrenic patients during their last full-time job were characterized by their low level of complexity in dealing with people, information and objects (e.g., janitors, cleaners, gardeners, guards). A few researchers have examined some of the consequences of first episodic psychosis relative to employment, job performance and capacity to work (Jorgensen 1987; Massel et al. 1990; Beiser et al. 1994). For example, Beiser and co-workers examined occupational functioning after the first episode of psychosis. These researchers found 18 months after the first episode that the “psychosis compromise[d] occupational functioning”. In other words, there was a higher post-morbid decline among schizophrenic workers than among those suffering from affective disorders. Similarly, Massel et al. (1990) found that the work capacity of psychotics (e.g., people with schizophrenia, affective disorders with psychotic features or atypical psychotic disorders) was impaired in comparison to non-psychotics (e.g., people with affective disorders without psychotic features, anxiety disorders, personality disorders and substance abuse disorders). Psychotics in their study showed marked thought disturbance, hostility and suspiciousness which correlated with poor work performance.
In summary, our knowledge about the relationship between work-related factors and psychosis is in the embryonic stage. As Brodsky (1984) states, “the physical and chemical hazards of the workplace have received considerable attention, but the psychological stresses associated with work have not been as widely discussed, other than in relation to managerial responsibilities or to the coronary-prone behaviour pattern”. This means that research on the topic of work-related psychosis is vitally needed, especially since workers spend an average of 42 to 44% of their lives working (Hines, Durham and Geoghegan 1991; Lemen 1995) and work has been associated with psychological well-being (Warr 1978). We need to have a better understanding of what types of occupational stressor under what types of condition influence which types of psychological disorder. For example, research is needed to determine whether there are stages which workers move through based upon intensity, duration and frequency of psychosocial stress in the work environment, in conjunction with personal, social, cultural and political factors occurring in their daily lives. We are dealing with complex issues which will require in-depth inquiries and ingenious solutions.
Acute Management of the Psychotic Worker
Typically, the primary role of persons in the workplace is to respond to an acutely psychotic worker in a manner which facilitates the person being transported safely to an emergency room or psychiatric treatment facility. The process may be greatly facilitated if the organization has an active employee assistance programme and a critical incident response plan. Ideally, the organization will train key employees in advance for emergency crisis responses and will have a plan in place for coordinating as needed with local emergency response resources.
Treatment approaches for the psychotic worker will vary depending upon the specific type of underlying problem. In general, all psychotic disorders should be evaluated by a professional. Often, immediate hospitalization is warranted for the safety of the worker and the workplace. Thereafter, a thorough evaluation can be completed to establish a diagnosis and develop a treatment plan. The primary goal is to treat the underlying cause(s). However, even prior to conducting a comprehensive evaluation or initiating a comprehensive treatment plan, the physician responding to the emergency may need to focus initially on providing symptomatic relief. Providing a structured, low-stress environment is desirable. Neuroloptics may be used to help the patient calm down. Benzodiazepines may help reduce acute anxiety.
After managing the acute crisis, a comprehensive evaluation may include collecting a detailed history, psychological testing, a risk assessment to establish dangerousness to self or others and careful monitoring of response to treatment (including not only response to medications, but also to psychotherapeutic interventions). One of the more difficult problems with many patients who exhibit psychotic symptomatology is treatment compliance. Often these individuals tend not to believe that they have serious difficulties, or, even if they recognize the problem, they are sometimes inclined to decide unilaterally to discontinue treatment prematurely. In these instances, family members, co-workers, treating clinicians, occupational health personnel and employers are sometimes placed in awkward or difficult situations. Sometimes, for the safety of the employee and the workplace, it becomes necessary to mandate compliance with treatment as a condition for returning to the job.
Managing the Psychotic Worker and the Work Environment
Case example
A skilled worker on the third shift at a chemical plant began to exhibit unusual behaviour as the company began to modify its production schedule. For several weeks, instead of leaving work after his shift ended, he began to stay for several hours discussing his concerns about increased job demands, quality control and changes in production procedures with his counterparts on the morning shift. He appeared quite distressed and behaved in a manner which was atypical for him. He had formerly been somewhat shy and distant, with an excellent job performance history. During this period of time, he became more verbal. He also approached individuals and stood close to them in a manner which several co-workers reported made them feel uncomfortable. While these co-workers later reported that they felt his behaviour was unusual, no one notified the employee assistance programme (EAP) or management of their concerns. Then, suddenly one evening, this employee was observed by his co-workers as he began to shout incoherently, walked over to a storage area for volatile chemicals, laid down on the ground and began to flick a cigarette lighter on and off. His co-workers and supervisor interfered and, after consultation with the EAP, he was taken by ambulance to a nearby hospital. The treating physician determined that he was acutely psychotic. After a brief treatment period he was successfully stabilized on medications.After several weeks, his treating physician felt he was able to return to his job. He underwent a formal return-to-work evaluation with an independent clinician and was judged ready to return to work. While his company doctor and the treating physician determined that it was safe for him to return, his co-workers and supervisors expressed substantial concerns. Some employees noted that they might be harmed if this episode were repeated and the chemical storage areas ignited. The company took steps to increase security in safety sensitive areas. Another concern also surfaced. A number of workers stated that they believed this individual might bring a weapon to work and start shooting. None of the professionals involved in treating this worker or in evaluating him for return to work believed that there was a risk of violent behaviour. The company then elected to bring in mental health professionals (with the worker’s consent) to assure co-workers that the risk of violent behaviour was exceedingly low, to provide education on mental illnesses, and to identify proactive steps that co-workers could take to facilitate the return to work of a colleague who had undergone treatment. However, in this situation, even after this educational intervention, co-workers were unwilling to interact with this worker, further compounding the return-to-work process. While the legal rights of individuals suffering from mental disorders, including those associated with psychotic states, have been addressed by the Americans with Disabilities Act, practically speaking the organizational challenges to effectively managing occurrences of psychosis at work are often as great or greater than the medical treatment of psychotic workers.
Return to Work
The primary question to be addressed after a psychotic episode is whether the employee can safely return to his or her current job. Sometimes organizations permit this decision to be made by the treating clinicians. However, ideally, the organization should require their occupational medical system to conduct an independent fitness-for-duty evaluation (Himmerstein and Pransky 1988). In the fitness-for-duty evaluation process a number of key pieces of information should be reviewed, including the treating clinician’s evaluation, treatment and recommendations, as well as the worker’s prior job performance and the specific features of the job, including the required job tasks and the organizational environment.
If the occupational medical physician is not trained in psychiatric or psychological fitness-for-duty evaluation, then the evaluation should be performed by an independent mental health professional who is not the treating clinician. If some aspects of the job pose safety risks, then specific work restrictions should be developed. These restrictions may range from minor alterations in work activities or work schedule to more significant modifications such as alternate job placement (e.g., a light-duty assignment or a job transfer to an alternate position). In principle, these work restrictions are not different in kind from other restrictions commonly provided by occupational health physicians, such as specifying the amount of weight which a worker may be cleared to lift following a musculoskeletal injury.
As is evident in the case example above, the return to work often raises challenges not only for the affected worker, but also for co-workers, supervisors and the broader organization. While professionals are obligated to protect the confidentiality of the affected worker to the fullest extent permitted by law, if the worker is willing and competent to sign an appropriate release of information, then the occupational medical system can provide or coordinate consultation and educational interventions to facilitate the return-to-work process. Often, coordination between the occupational medical system, the employee assistance programme, supervisors, union representatives and co-workers is critical to a successful outcome.
The occupational health system should also periodically monitor the worker’s readjustment to the workplace in collaboration with the supervisor. In some instances, it may be necessary to monitor the worker’s compliance with a medication regimen recommended by the treating physician—for example, as a precondition for being permitted to engage in certain safety-sensitive job tasks. More importantly, the occupational medical system must consider not only what is best for the worker, but also what is safe for the workplace. The occupational medical system may also play a critical role in assisting the organization in complying with legal requirements such as the Americans with Disabilities Act as well as in interfacing with treatments provided under the organization’s health care plan and/or the workers’ compensation system.
Prevention Programming
At present, there is no literature on specific prevention or early intervention programmes for reducing the incidence of psychosis in the workforce. Employee assistance programmes may play a crucial role in the early identification and treatment of psychotic workers. Since stress may contribute to the incidence of psychotic episodes within working populations, various organizational interventions which identify and modify organizationally created stress may also be helpful. These general programmatic efforts may include job redesign, flexible scheduling, self-paced work, self-directed work teams and microbreaks, as well as specific programming to reduce the stressful impact of reorganization or downsizing.
Conclusion
While psychosis is a comparatively rare and multiply determined phenomenon, its occurrence within working populations raises substantial practical challenges for co-workers, union representatives, supervisors and occupational health professionals. Psychosis may occur as a direct consequence of a work-related toxic exposure. Work-related stress may also increase the incidence of psychosis among workers who suffer from (or are at risk of developing) mental disorders which place them at risk of psychosis. Additional research is needed to: (1) better understand the relationship between workplace factors and psychosis; and (2) develop more effective approaches for managing psychosis in the workplace and reduce its incidence.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."