This chapter provides an overview of major types of mental health disorder that can be associated with work—mood and affective disorders (e.g., dissatisfaction), burnout, post-traumatic stress disorder (PTSD), psychoses, cognitive disorders and substance abuse. The clinical picture, available assessment techniques, aetiological agents and factors, and specific prevention and management measures will be provided. The relationship with work, occupation or branch of industry will be illustrated and discussed where possible.
This introductory article first will provide a general perspective on occupational mental health itself. The concept of mental health will be elaborated upon, and a model will be presented. Next, we will discuss why attention should be paid to mental (ill) health and which occupational groups are at greatest risk. Finally, we will present a general intervention framework for successfully managing work-related mental health problems.
What Is Mental Health: A Conceptual Model
There are many different views about the components and processes of mental health. The concept is heavily value laden, and one definition is unlikely to be agreed upon. Like the strongly associated concept of “stress”, mental health is conceptualized as:
- a state—for example, a state of total psychological and social well-being of an individual in a given sociocultural environment, indicative of positive moods and affects (e.g., pleasure, satisfaction and comfort) or negative ones (e.g., anxiety, depressive mood and dissatisfaction).
- a process indicative of coping behaviour—for example, striving for independence, being autonomous (which are key aspects of mental health).
- the outcome of a process—a chronic condition resulting either from an acute, intense confrontation with a stressor, such as is the case in a post-traumatic stress disorder, or from the continuing presence of a stressor which may not necessarily be intense. This is the case in burnout, as well as in psychoses, major depressive disorders, cognitive disorders and substance abuse. Cognitive disorders and substance abuse are, however, often considered as neurological problems, since pathophysiological processes (e.g., degeneration of the myelin sheath) resulting from ineffective coping or from the stressor itself (alcohol use or occupational exposition to solvents, respectively) can underlie these chronic conditions.
Mental health may also be associated with:
- Person characteristics like “coping styles”—competence (including effective coping, environmental mastery and self-efficacy) and aspiration are characteristic of a mentally healthy person, who shows interest in the environment, engages in motivational activity and seeks to extend him- or herself in ways that are personally significant.
Thus, mental health is conceptualized not only as a process or outcome variable, but also as an independent variable—that is, as a personal characteristic that influences our behaviour.
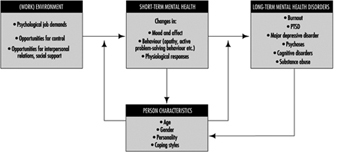
In figure 1 a mental health model is presented. Mental health is determined by environmental characteristics, both in and outside the work situation, and by characteristics of the individual. Major environmental job characteristics are elaborated upon in the chapter “Psychosocial and organizational factors”, but some points on these environmental precursors of mental (ill) health have to be made here as well.
Figure 1. A model for mental health.
There are many models, most of them stemming from the field of work and organizational psychology, that identify precursors of mental ill health. These precursors are often labelled “stressors”. Those models differ in their scope and, related to this, in the number of stressor dimensions identified. An example of a relatively simple model is that of Karasek (Karasek and Theorell 1990), describing only three dimensions: psychological demands, decision latitude (incorporating skill discretion and decision authority) and social support. A more elaborate model is that of Warr (1994), with nine dimensions: opportunity for control (decision authority), opportunity for skill use (skill discretion), externally generated goals (quantitative and qualitative demands), variety, environmental clarity (information about consequences of behaviour, availability of feedback, information about the future, information about required behaviour), availability of money, physical security (low physical risk, absence of danger), opportunity for interpersonal contact (prerequisite for social support), and valued social position (cultural and company evaluations of status, personal evaluations of significance). From the above it is clear that the precursors of mental (ill) health are generally psychosocial in nature, and are related to work content, as well as working conditions, conditions of employment and (formal and informal) relationships at work.
Environmental risk factors for mental (ill) health generally result in short-term effects such as changes in mood and affect, like feelings of pleasure, enthusiasm or a depressed mood. These changes are often accompanied by changes in behaviour. We may think of restless behaviour, palliative coping (e.g., drinking) or avoiding, as well as active problem-solving behaviour. These affects and behaviours are generally accompanied by physiological changes as well, indicative of arousal and sometimes also of a disturbed homeostasis. When one or more of these stressors remains active, the short-term, reversible responses may result in more stable, less reversible mental health outcomes like burnout, psychoses or major depressive disorder. Situations that are extremely threatening may even immediately result in chronic mental health disorders (e.g., PTSD) which are difficult to reverse.
Person characteristics may interact with psychosocial risk factors at work and exacerbate or buffer their effects. The (perceived) coping ability may not only moderate or mediate the effects of environmental risk factors, but may also determine the appraisal of the risk factors in the environment. Part of the effect of the environmental risk factors on mental health results from this appraisal process.
Person characteristics (e.g., physical fitness) may not only act as precursors in the development of mental health, but may also change as a result of the effects. Coping ability may, for example, increase as the coping process progresses successfully (“learning”). Long-term mental health problems will, on the other hand, often reduce coping ability and capacity in the long run.
In occupational mental health research, attention has been particularly directed to affective well-being—factors such as job satisfaction, depressive moods and anxiety. The more chronic mental health disorders, resulting from long-term exposure to stressors and to a greater or lesser extent also related to personality disorders, have a much lower prevalence in the working population. These chronic mental health problems have a multitude of causal factors. Occupational stressors will consequently be only partly responsible for the chronic condition. Also, people suffering from these kinds of chronic problem will have great difficulty in maintaining their position at work, and many are on sick leave or have dropped out of work for quite a long period of time (1 year), or even permanently. These chronic problems, therefore, are often studied from a clinical perspective.
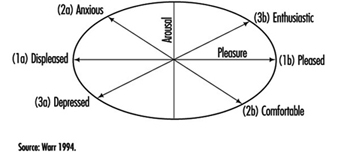
Since, in particular, affective moods and affects are so frequently studied in the occupational field, we will elaborate on them a little bit more. Affective well-being has been treated both in a rather undifferentiated way (ranging from feeling good to feeling bad), as well as by considering two dimensions: “pleasure” and “arousal” (figure 2). When variations in arousal are uncorrelated with pleasure, these variations alone are generally not considered to be an indicator of well-being.
Figure 2. Three principal axes for the measurement of affective well-being.
When, however, arousal and pleasure are correlated, four quadrants can be distinguished:
- Highly aroused and pleased indicates enthusiasm.
- Low aroused and pleased indicates comfort.
- Highly aroused and displeased indicates anxiety.
- Low aroused and displeased indicates depressed mood (Warr 1994).
Well-being can be studied at two levels: a general, context-free level and a context-specific level. The work environment is such a specific context. Data analyses support the general notion that the relation between job characteristics and context-free, non-work mental health is mediated by an effect on work-related mental health. Work-related affective well-being has commonly been studied along the horizontal axis (Figure 2) in terms of job satisfaction. Affects related to comfort in particular have, however, largely been ignored. This is regrettable, since this affect might indicate resigned job satisfaction: people may not complain about their jobs, but may still be apathetic and uninvolved (Warr 1994).
Why Pay Attention to Mental Health Issues?
There are several reasons that illustrate the need for attention to mental health issues. First of all, national statistics of several countries indicate that a lot of people drop out of work because of mental health problems. In the Netherlands, for example, for one-third of those employees who are diagnosed as disabled for work each year, the problem is related to mental health. The majority of this category, 58%, is reported to be work related (Gründemann, Nijboer and Schellart 1991). Together with musculoskeletal problems, mental health problems account for about two-thirds of those who drop out for medical reasons each year.
Mental ill health is an extensive problem in other countries as well. According to the Health and Safety Executive Booklet, it has been estimated that 30 to 40% of all sickness absence from work in the UK is attributable to some form of mental illness (Ross 1989; O’Leary 1993). In the UK, it has been estimated that one in five of the working population suffers each year from some form of mental illness. It is difficult to be precise about the number of working days lost each year because of mental ill health. For the UK, a figure of 90 million certified days—or 30 times that lost as a result of industrial disputes—is widely quoted (O’Leary 1993). This compares with 8 million days lost as a result of alcoholism and drink-related diseases and 35 million days as a result of coronary heart disease and strokes.
Apart from the fact that mental ill health is costly, both in human and financial terms, there is a legal framework provided by the European Union (EU) in its framework directive on health and safety at work (89/391/EEC), enacted in 1993. Although mental health is not as such an element which is central to this directive, a certain amount of attention is given to this aspect of health in Article 6. The framework directive states, among other things, that the employer has:
“a duty to ensure the safety and health of workers in every aspect related to work, following general principles of prevention: avoiding risks, evaluating the risks which cannot be avoided, combating the risks at source, adapting the work to the individual, especially as regards the design of workplaces, the choice of work equipment and the choice of work and production methods, with a view, in particular, to alleviating monotonous work and work at a predetermined work rate and to reduce their effects on health.”
Despite this directive, not all European countries have adopted framework legislation on health and safety. In a study comparing regulations, policies and practices concerning mental health and stress at work in five European countries, those countries with such framework legislation (Sweden, the Netherlands and the UK) recognize mental health issues at work as important health and safety topics, whereas those countries which do not have such a framework (France, Germany) do not recognize mental health issues as important (Kompier et al. 1994).
Last but not least, prevention of mental ill health (at its source) pays. There are strong indications that important benefits result from preventive programmes. For example, of the employers in a national representative sample of companies from three major branches of industry, 69% state that motivation increased; 60%, that absence due to sickness decreased ; 49%, that the atmosphere improved; and 40%, that productivity increased as a result of a prevention programme (Houtman et al. 1995).
Occupational Risk Groups of Mental Health
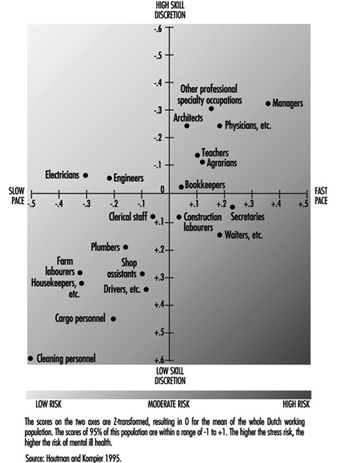
Are specific groups of the working population at risk of mental health problems? This question cannot be answered in a straightforward manner, since hardly any national or international monitoring systems exist which identify risk factors, mental health consequences or risk groups. Only a “scattergram” can be given. In some countries national data exist for the distribution of occupational groups with respect to major risk factors (e.g., for the Netherlands, Houtman and Kompier 1995; for the United States, Karasek and Theorell 1990). The distribution of the occupational groups in the Netherlands on the dimensions of job demands and skill discretion (figure 3) agree fairly well with the US distribution shown by Karasek and Theorell, for those groups that are in both samples. In those occupations with high work pace and/or low skill discretion, the risk of mental health disorders is highest.
Figure 3. Risk for stress and mental ill health for different occupational groups, as determined by the combined effects of work pace and skill discretion.
Also, in some countries there are data for mental health outcomes as related to occupational groups. Occupational groups that are especially prone to drop out for reasons of mental ill health in the Netherlands are those in the service sector, such as health care personnel and teachers, as well as cleaning personnel, housekeepers and occupations in the transport branch (Gründemann, Nijboer and Schellart1991).
In the United States, occupations which were highly prone to major depressive disorder, as diagnosed with standardized coding systems (i.e., the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM III)) (American Psychiatric Association 1980), are juridicial employees, secretaries and teachers (Eaton et al. 1990).
Management of Mental Health Problems
The conceptual model (figure 1) suggests at least two targets of intervention in mental health issues:
- The (work) environment.
- The person—either his or her characteristics or the mental health consequences.
Primary prevention, the type of prevention that should prevent mental ill health from occurring, should be directed at the precursors by alleviating or managing the risks in the environment and increasing the coping ability and capacity of the individual. Secondary prevention is directed at the maintenance of people at work who already have some form of (mental) health problem. This type of prevention should embrace the primary prevention strategy, accompanied by strategies to make both employees and their supervisors sensitive to signals of early mental ill health in order to reduce the consequences or prevent them from getting worse. Tertiary prevention is directed at the rehabilitation of people who have dropped out of work due to mental health problems. This type of prevention should be directed at adapting the workplace to the possibilities of the individual (which is often found to be quite effective), along with individual counselling and treatment. Table 1 provides a schematic framework for the management of mental health disorders at the workplace. Effective preventive policy plans of organizations should, in principle, take into account all three types of strategy (primary, secondary and tertiary prevention), as well as be directed at risks, consequences and person characteristics.
Table 1. A schematic overview of management strategies on mental health problems, and some examples.
|
Type of |
Intervention level |
|
|
Work environment |
Person characteristics and/or health outcomes |
|
|
Primary |
Redesign of task content Redesign of communication structure |
Training groups of employees on signalling and handling specific work- related problems (e.g., how to manage time pressure, robberies etc.) |
|
Secondary |
Introduction of a policy on how to act in case of absenteeism (e.g., training supervisors to discuss absence and return with employees concerned) Provide facilities within the organization, especially for risk groups (e.g., counsellor for sexual harassment) |
Training in relaxation techniques |
|
Tertiary |
Adaptation of an individual workplace |
Individual counselling Individual treatment or therapy (may also be with medication) |
The schedule as presented provides a method for systematic analysis of all possible types of measure. One can discuss whether a certain measure belongs somewhere else in the schedule; such a discussion is, however, not very fruitful, since it is often the case that primary preventive measures can work out positively for secondary prevention as well. The proposed systematic analysis may well result in a large number of potential measures, several of which may be adopted, either as a general aspect of the (health and safety) policy or in a specific case.
In conclusion: Although mental health is not a clearly defined state, process or outcome, it covers a generally agreed upon area of (ill) health. Part of this area can be covered by generally accepted diagnostic criteria (e.g., psychosis, major depressive disorder); the diagnostic nature of other parts is neither as clear nor as generally accepted. Examples of the latter are moods and affects, and also burnout. Despite this, there are many indications that mental (ill) health, including the more vague diagnostic criteria, is a major problem. Its costs are high, both in human and financial terms. In the following articles of this chapter, several mental health disorders—moods and affects (e.g., dissatisfaction), burnout, post-traumatic stress disorder, psychoses, cognitive disorders and substance abuse—will be discussed in much more depth with respect to the clinical picture, available assessment techniques, aetiological agents and factors, and specific prevention and management measures.