Disorders of the shoulder region are common problems in both the general and working population. As many as one-third of all women and one-quarter of all men report feeling pain in the neck and shoulder every day or every other day. It is estimated that the prevalence of shoulder tendinitis in the general population is about 2%. Among male and female workers in the United States, the prevalence of shoulder tendinitis has been estimated to be as high as 8% among those exposed to highly repetitive or high-force hand motions, compared to about 1% for those without this type of musculoskeletal stress.
Anatomy
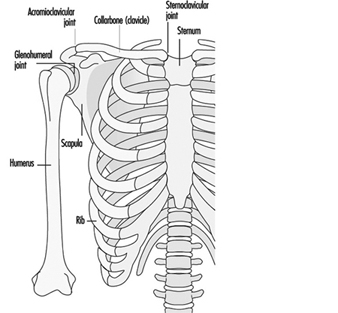
The bones in the shoulder include the collarbone (clavicle), the shoulder blade (scapula) and the (shoulder) glenohumeral joint, as shown in figure 1. The collarbone is connected to the body by the sternoclavicular joint, and to the shoulder-blades by the acromioclavicular joint. The sternoclavicular joint is the sole connection between the upper extremity and the rest of the body. The shoulder blade has no direct connection of its own and thus the shoulder is dependent on muscles for being fixed to the trunk. The upper arm is connected to the shoulder blade by the glenohumeral joint.
Figure 1. Schematic view of the skeletal parts of the shoulder-girdle.
The function of the shoulder is to provide a platform for the upper extremity, and for some of its muscles. Although the glenohumeral joint has a greater range of movement than, for example, the lower extremity in the hip, this flexibility has developed at the price of stability. While the hip joint has very strong ligaments, the ligaments in the glenohumeral joint are few and weak. In order to compensate for this comparative weakness, the glenohumeral joint is surrounded by shoulder muscles in the form of a cuff and is called the rotator cuff.
Biomechanics
The arm represents about 5% of the total body weight, and its centre of gravity is about midway down between the glenohumeral joint and the wrist. When the arm is raised and bent either away from or towards the body (abduction or flexion), a lever is created in which the distance from the centre of gravity increases, and hence the twisting force, and the loading torque, on the glenohumeral joint increases. The rate at which the torque increases, however, is not simply directly proportional to the angle at which the arm is bent, because the mathematical function which describes the biomechanical forces is not linear but is rather a sine function of the abduction angle. The torque will decrease only by about 10% if the flexion or abduction angle is decreased from 90 to 60 degrees. However, if the angle is decreased from 60 to 30 degrees, torque is reduced by as much as 50%.
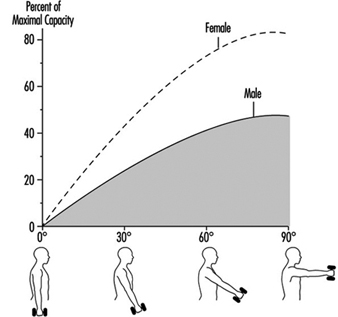
The flexion strength in the glenohumeral joint is about 40 to 50 Nm for women and about 80 to 100 Nm for men. When the arm is held straight out (90-degree forward flexion) and no external load is placed on the arm—that is, the person is not holding anything or using the arm to exert a force—the static load is still about 15 to 20% of the maximal voluntary capacity (MVC) for women and about 10 to 15% MVC for men. If a tool weighing 1 kg is held in the hand with an arm extended, the corresponding load in the shoulder would be about 80% of the MVC for women, as illustrated in figure 2.
Figure 2. Female and male strength showing the results of holding a 1 kilogramme tool in the hand with the arm held straight at different angles of shoulder flexion.
The most important muscles for abduction—or raising the arm away from the body to the side—are the deltoid muscle, the rotator cuff muscles and the long head of the biceps. The most important muscles for forward flexion—raising the arm away from the body to the front—are the anterior part of the deltoid muscle, the rotator cuff muscles, the coracobrachialis muscle and the short head of the biceps brachii muscle. Inward rotation is performed by the pectoralis major muscle, the subscapularis muscle, the anterior part of the deltoid muscle and by the latissimus dorsi muscle. Outward rotation is performed by the posterior part of the deltoid muscle, the infraspinatus muscle and the minor and major teres muscles.
Rotator cuff muscles are engaged in any movement of the glenohumeral joint, which is to say any movement of the arm. The rotator cuff muscles originate from the shoulder blade, and their tendons are arranged around the humerus in the form of a cuff, from which their name is derived. The four rotator cuff muscles are the supraspinate, the infraspinate, the teres minor and the subscapularis muscle. These muscles function as ligaments in the glenohumeral joint and also keep the humeral head against the shoulder-blade. A rupture of the rotator cuff (e.g., of the supraspinous tendon) will cause a reduction in abduction strength, particularly involving those positions where the arm is bent away from the body. When the function of the deltoid muscles is lost, the abduction strength can be reduced by as much as 50%, regardless of the angle at which the arm is being bent.
Any time there is forward flexion or abduction of the arm, a load will be placed on the system. Many motions will cause a twisting force, or torque, as well. Since the arm is connected to the shoulder blade by the glenohumeral joint, any load that is placed on this joint will be transferred to the shoulder-blade. The load in the glenohumeral joint, measured in % MVC, is almost directly proportional to the load placed on the muscle which fixes the shoulder blade into place, the upper trapezius.
Major Specific Work-Related Diseases
Rotator cuff disorders and biceps tendinitis
Tendinitis and tenosynovitis are inflammations of a tendon and the synovial membrane of a tendon sheath. The tendons to the rotator cuff muscles (supraspinatus, infraspinatus, subscapularis, and teres minor muscles) and the long head of the biceps brachii are common sites for inflammation in the shoulder. Large movements of the tendons are involved at these locations. During elevation, as the tendons pass to the shoulder joint and under the bony structure there (the coraco-acromial arch), they may be impinged upon, and inflammation may result. These disorders are sometimes termed impingement syndromes. Inflammation of a tendon may be part of a general inflammatory disease, such as in rheumatoid arthritis, but also may be caused by local inflammation which results from mechanical irritation and friction.
Shoulder joint and acromioclavicular joint osteoarthritis
Shoulder joint and acromioclavicular joint osteoarthritis, OA, are degenerative changes of cartilage and bone in the joints and intervertebral discs.
Epidemiology
There is a high prevalence of shoulder tendinitis among welders and steel-platers, with rates of 18% and 16%, respectively. In one study which compared welders and steel-platers to male office workers, the welders and steel-platers were 11 to 13 times more likely to suffer from the disorder, as measured by the odds ratio. A similar odds ratio of 11 was found in a case-control study of male industrial workers who worked with their hands held at or about shoulder level. Automobile assemblers who suffered from acute shoulder pain and tendinitis were required to elevate their arms more frequently and for longer durations than were workers who did not have such job requirements.
Studies of industrial workers in the United States have shown there to be a prevalence of 7.8% of shoulder tendinitis and degenerative joint disease (shoulder) of cumulative trauma disorders (CTDs) among workers whose tasks involved exerting force or repetitive motions, or both, on the wrist and hands. In one study, female students performing repetitive shoulder flexion developed reversible shoulder tendinitis. They developed the condition when the flexion rate, over the course of one hour, was 15 forward flexions per minute and the angle of flexion was between 0 and 90 degrees. Boarding, folding and sewing workers suffered about twice as much shoulder tendinitis as did knitting workers. Among professional baseball pitchers, approximately 10% have experienced shoulder tendinitis. A survey of swimmers in Canadian swimming clubs found that 15% of the swimmers reported having significant shoulder disability, primarily due to impingement. The problem was particularly related to the butterfly and freestyle strokes. Tendinitis of the biceps brachii was found in 11% of the 84 best tennis players in the world.
Another study showed that shoulder joint osteoarthritis was more common in dentists than among farmers, but the ergonomic exposure related to shoulder joint OA has not been identified. An increased risk for acromioclavicular OA has been reported among construction workers. Heavy lifting and handling of heavy tools with hand-arm vibration have been suggested as the exposure related to acromioclavicular joint OA.
Mechanisms and Risk Factors of Disease
Pathophysiology of shoulder tendinitis
Tendon degeneration is often the predisposing factor for development of shoulder tendinitis. Such degeneration of the tendon can be caused by impairment of circulation to the tendon so that metabolism is disrupted. Mechanical stress may also be a cause. Cell death within the tendon, which forms debris and in which calcium may deposit, may be the initial form of degeneration. The tendons to the supraspinatus, the biceps brachii (long head) and the upper parts of the infraspinatus muscles have a zone in which there are no blood vessels (avascularity), and it is in this area that signs of degeneration, including cell death, calcium deposits and microscopic ruptures, are predominantly located. When blood circulation is impaired, such as through compression and static load on the shoulder tendons, then degeneration can be accelerated because normal body maintenance will not be functioning optimally.
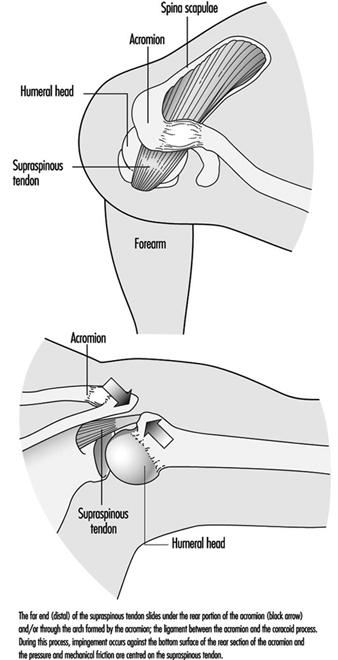
Compression of the tendons occurs when the arm is elevated. A process that is often referred to as impingement involves forcing the tendons through the bony passageways of the shoulder, as illustrated in figure 3. Compression of the rotator cuff tendons (especially the supraspinatus tendon) results because the space between the humeral head and the tight coracoacromial arch is narrow. People who are suffering with long-term disability due to chronic bursitis or complete or partial tears of the rotator cuff tendons or biceps brachii usually also have impingement syndrome.
Figure 3. Impingement
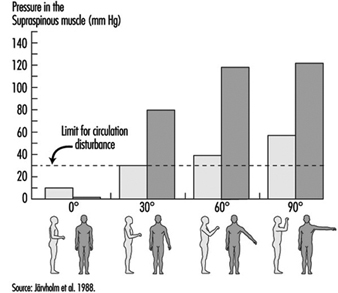
The circulation of blood to the tendon also depends on muscle tension. In the tendon, circulation will be inversely proportional to the tension. At very high tension levels, circulation may cease completely. Recent studies have shown that the intramuscular pressure in the supraspinous muscle can exceed 30 mm Hg at 30 degrees of forward flexion or abduction in the shoulder joint, as shown in figure 4. Impairment of blood circulation occurs at this pressure level. Since the major blood vessel supplying the supraspinous tendon runs through the supraspinous muscle, it is likely that the circulation of the tendon may even be disturbed at 30 degrees of forward flexion or abduction in the shoulder joint.
Figure 4. Raising the arm to different elevations and at different angles exerts different intramuscular pressures on the supraspinous muscle.
Because of these biomechanical effects, it is not surprising to find a high risk of shoulder tendon injuries among those who are involved in activities that require static contractions of the supraspinatus muscle or repetitive shoulder forward flexions or abductions. Welders, steel-platers and sewers are among the occupational groups whose work involves static tension of these muscles. Assembly line workers in the automotive industry, painters, carpenters and athletes such as swimmers are other occupational groups in which repetitive shoulder joint movements are performed.
In the degenerated tendon, exertion may trigger an inflammatory response to the debris of dead cells, resulting in an active tendinitis. Also, infection (e.g., viral, urogenital) or systemic inflammation may predispose an individual to reactive tendinitis in the shoulder. One hypothesis is that an infection, which makes the immune system active, increases the possibility of a foreign body response to the degenerative structures in the tendon.
Pathogenesis of osteoarthrosis
The pathogenesis of osteoarthrosis, OA, is not known. Primary (idiopathic) OA is the most common diagnosis in absence of predisposing factors such as previous fractures. If predisposing factors exist, the OA is termed secondary. There are disputes between those who claim (primary) OA to be a metabolic or genetic disorder and those who claim that cumulative mechanical trauma also may play a part in the pathogenesis of primary OA. Microfractures due to sudden impact or repetitive impact loading may be one pathogenic mechanism for load-related OA.
Management and Prevention
In this section, non-medical management of shoulder disorders is considered. A change of workplace design or change of work task is necessary if the tendinitis is considered to be due to high local shoulder load. A history of shoulder tendinitis makes a worker doing repetitive or overhead work susceptible to a relapse of tendinitis. Loading of the osteoarthritic joint should be minimized by ergonomic optimization of work.
Primary prevention
Prevention of work-related musculoskeletal disorders in the shoulder can be achieved by improving work postures, motions, material handling and work organization, and eliminating external hazardous factors such as hand-arm vibration or whole body vibration. A methodology that may be advantageous in improving ergonomic working conditions is participatory ergonomics, taking a macro-ergonomic approach.
- Work postures: Since compression of the shoulder tendons occurs at 30 degrees of arm elevation (abduction), work should be designed that allows the upper arm to be kept close to the trunk.
- Motions: Repetitive arm elevations may trigger shoulder tendinitis, and work should be designed to avoid highly repetitive arm motions.
- Material handling: Handling of tools or objects may cause severe loading on shoulder tendons and muscles. Hand-held tools and objects should be kept at the lowest weight feasible and should be used with supports to assist in lifting.
- Work organization: Work organization should be designed to allow pauses and rests. Vacations, rotations and job enlargement are all techniques which may avoid repetitive loading of single muscles or structures.
- External factors: Impact vibration and other impacts from power tools may cause strain on both tendons and joint structures, increasing risk of osteoarthrosis. Vibration levels of power tools should be minimized and impact vibration and other types of impact exposure avoided by using different types of support or levers. Whole-body vibrations may cause reflectory contractions of shoulder muscles and increase the load on the shoulder.
- Participatory ergonomics: This method involves workers themselves in defining the problems, and solutions, and in the evaluation of the solutions. Participatory ergonomics starts from a macro-ergonomic view, involving analysis of the whole production system. Results of this analysis might lead to large-scale changes in production methods that could increase health and safety as well as profit and productivity. The analysis could lead to smaller-scale changes as well, such as in workstation design.
- Preplacement examinations: Current available information does not support the idea that preplacement screening is effective in reducing the occurrence of work-related shoulder disorders.
- Medical control and surveillance: Surveillance of shoulder symptoms is readily carried out using standardized questionnaires and inspection walk-throughs of workplaces.