Tenosynovitis and Peritendinitis
Wrist and finger extensors and flexors
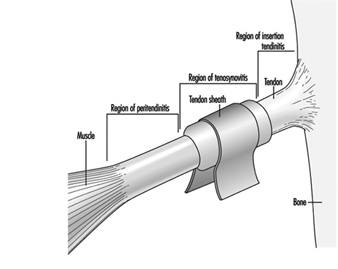
In the wrist and hand the tendons are surrounded by tendon sheaths, which are tubular structures containing fluid to provide lubrication and protection for the tendon. An inflammation of the tendon sheath is called tenosynovitis. Inflammation of the site where the muscle meets the tendon is called peritendinitis The location of wrist tenosynovitis is at the tendon sheath area in the wrist, and the location of peritendinitis is above the tendon sheath area in the forearm. Insertion tendinitis denotes an inflammation of the tendon at the site where it meets the bone (figure 1).
Figure 1. The muscle-tendon unit.
The terminology for the diseases of the tendon and its adjacent structures is often used loosely, and sometimes “tendinitis” has been used for all painful conditions in the forearm-wrist-hand region, regardless of the type of clinical appearance. In North America an umbrella diagnosis “cumulative trauma disorder” (CTD) has been used for all upper extremity soft tissue disorders believed to be caused, precipitated or aggravated by repetitive exertions of the hand. In Australia and some other countries, the diagnosis of “repetitive strain injury” (RSI) or “overuse injury” has been used, while in Japan the concept of “occupational cervicobrachial disorder” (OCD) has covered soft-tissue disorders of the upper limb. The two latter diagnoses include also shoulder and neck disorders.
The occurrence of tenosynovitis or peritendinitis varies widely according to the type of work. High incidences have been reported typically among manufacturing workers, such as food-processing workers, butchers, packers and assemblers. Some recent studies show that high incidence rates exist even in modern industries, as shown in table 1. Tendon disorders are more common on the back side than on the flexor side of the wrist. Upper extremity pain and other symptoms are prevalent also in other types of tasks, such as modern keyboard work. The clinical signs that keyboard workers present are, however, rarely compatible with tenosynovitis or peritendinitis.
Table 1. Incidence of tenosynovitis/peritendinitis in various populations.
|
Study population |
Rate per 100 person-years |
Reference |
|
700 Muscovite tea packers |
40.5 |
Obolenskaja and Goljanitzki 1927 |
|
12,000 car factory workers |
0.3 |
Thompson et al. 1951 |
|
7,600 workers of diverse trades |
0.4 |
Kivi 1982 |
|
102 male meatcutters |
12.5 |
Kurppa et al. 1991 |
|
107 female sausage makers |
16.8 |
Kurppa et al. 1991 |
|
118 female packers |
25.3 |
Kurppa et al. 1991 |
|
141 men in non-strenuous jobs |
0.9 |
Kurppa et al. 1991 |
|
197 women in non-strenuous jobs |
0.7 |
Kurppa et al. 1991 |
Frequent repetition of work movements and high force demands on the hand are powerful risk factors, especially when they occur together (Silverstein, Fine and Armstrong 1986). Generally accepted values for acceptable repetitiveness and use of force do not, however, yet exist (Hagberg et al. 1995). Being unaccustomed to hand-intensive work, either as a new worker or after an absence from work, increases the risk. Deviated or bent postures of the wrist at work and low environmental temperature have also been considered as risk factors, although the epidemiological evidence to support this is weak. Tenosynovitis and peritendinitis occur at all ages. Some evidence exists that women might be more susceptible than men (Silverstein, Fine and Armstrong 1986). This has, however, been difficult to investigate, because in many industries the tasks differ so widely between women and men. Tenosynovitis may be due to bacterial infection, and some systemic diseases such as rheumatoid arthritis and gout are often associated with tenosynovitis. Little is known about other individual risk factors.
In tenosynovitis the tendon sheath area is painful, especially at the ends of the tendon sheath. The movements of the tendon are restricted or locked, and there is weakness in gripping. The symptoms are often worst in the morning, and functional ability improves after some activity. The tendon sheath area is tender on palpation, and tender nodes may be found. Bending of the wrist increases pain. The tendon sheath area may also be swollen, and bending the wrist back and forth may produce crepitation or crackling. In peritendinitis, a typical fusiform swelling is often visible on the backside of the forearm.
Tenosynovitis of the flexor tendons at the palmar aspect of the wrist may cause entrapment of the median nerve as it runs through the wrist, resulting in carpal tunnel syndrome.
The pathology at an acute stage of the disease is characterized by the accumulation of fluid and a substance called fibrin in the tendon sheath in tenosynovitis, and in the paratenon and between the muscle cells in peritendinitis. Later, cell growth is noticed (Moore 1992).
It should be emphasized that tenosynovitis or peritendinitis that is clinically identifiable as occupational is found in only a minor proportion of cases of wrist and forearm pain among working populations. The majority of workers first seek medical attention with the symptom of tenderness to palpation as the sole clinical finding. It is not fully known whether the pathology in such conditions is similar to that in tenosynovitis or peritendinitis.
In the prevention of tenosynovitis and peritendinitis, highly repetitive and forceful work movements should be avoided. In addition to attention to work methods, work organizational factors (the quantity and pace of work, pauses and work rotation) also determine the local load imposed on the upper limb, and the possibility of introducing variability to work by affecting these factors should be considered as well. New workers and workers returning from a leave or changing tasks should be gradually accustomed to repetitive work.
For industrial workers with hand-intensive tasks, the typical length of sick leave due to tenosynovitis or peritendinitis has been about ten days. The prognosis of tenosynovitis and peritendinitis is usually good, and most workers are able to resume their previous work tasks.
De Quervain’s tenosynovitis
De Quervain’s tenosynovitis is a stenosing (or constricting) tenosynovitis of the tendon sheaths of the muscles that extend and abduct the thumb at the outer aspect of the wrist. The condition occurs in early childhood and at any age later. It may be more common among women than among men. Prolonged repetitive movements of the wrist and blunt trauma have been suggested as causative factors, but this has not been epidemiologically investigated.
The symptoms include local pain at the wrist and weakness of grip. The pain may sometimes extend into the thumb or up into the forearm. There is tenderness and eventual thickening on palpation at the constriction site. Sometimes nodular thickening may be visible. Bending the wrist towards the little finger with the thumb flexed in the palm (Finkelstein’s test) typically exacerbates the symptoms. Some cases show triggering or snapping upon moving the thumb.
The pathological changes include thickened outer layers of the tendon sheaths. The tendon may be constricted and show enlargement beyond the site of constriction.
Stenosing tenosynovitis of the fingers
The tendon sheaths of the flexor tendons of the fingers are held close to the joint axes by tight bands, called pulleys . The pulleys may thicken and the tendon may show nodular swelling beyond the pulley, resulting in stenosing tenosynovitis often accompanied by painful locking or triggering of the finger. Trigger finger or trigger thumb have been used to denote such conditions.
The causes of trigger finger are largely unknown. Some cases that occur in early childhood are likely to be congenital, and some seem to appear after trauma. Trigger finger has been postulated to be caused by repetitive movements, but no epidemiological studies to test this have been carried out.
The diagnosis is based on local swelling, eventual nodular thickening, and snapping or locking. The condition is often encountered in the palm at the level of the metacarpal heads (the knuckles), but may occur also elsewhere and in multiple sites.
Osteoarthrosis
The prevalence of radiographically detectable osteoarthrosis in the wrist and hand is rare in the normal population under the age of 40, and is more common among men than women (Kärkkäinen 1985). After the age of 50, hand arthrosis is more prevalent among women than among men. Heavy manual labour with and without exposure to low-frequency (below 40 Hz) vibration have been associated, although not consistently, with excess prevalence of osteoarthrosis in the wrist and hand. For higher frequencies of vibration, no excess joint pathology has been reported (Gemne and Saraste 1987).
Osteoarthrosis of the first joint between the base of the thumb and the wrist (carpometacarpal joint) occurs fairly commonly among the general population and is more common among women than men. Osteoarthrosis is less common in the knuckles (metacarpo-phalangeal joints), with the exception of the meta- carpophalangeal joint of the thumb. Aetiology of these disorders is not well known.
Osteoarthrotic changes are common in the joints closest to the fingertip (distal interphalangeal joints of fingers), in which the age-adjusted prevalence of radiographically detectable changes (mild to severe) in different fingers varies between 9 and 16% among the men and 13 and 22% among the women of a normal population. Distal interphalangeal osteoarthrosis can be detected by clinical examination as nodular outgrowths on the joints, called Heberden’s nodes. In a Swedish population study among 55-year-old women and men, Heberden’s nodes were detected in 5% of men and 28% of women. Most subjects showed changes in both hands. The presence of Heberden’s nodes showed a correlation with heavy manual labour (Bergenudd, Lindgärde and Nilsson 1989).
Joint load associated with the manipulation of tools, repetitive movements of the hand and arm possibly together with minor traumatization, loading of the joint surfaces in extreme postures, and static work have been considered as possible causative factors for wrist and hand osteoarthrosis. Although osteoarthrosis has not been considered specific to low-frequency vibration, the following factors might play a role as well: damage of the joint cartilage from shocks from the tool, additional joint load associated with a vibration- induced increase in the need for joint stabilization, the tonic vibration reflex and a stronger grip on the tool handle induced when sensitivity to touch is diminished by vibration (Gemne and Saraste 1987).
The symptoms of osteoarthrosis include pain during movement in the initial stages, later also during rest. Limitation of motion in the wrist does not markedly interfere with work activities or other activities of daily living, whereas osteoarthrosis of the finger joints may interfere with gripping.
To avoid osteoarthrosis, tools should be developed that help to minimize heavy manual labour. Vibration from tools should be minimized as well.
Compartment Syndrome
The muscles, nerves and blood vessels in the forearm and hand are located in specific compartments limited by bones, membranes and other connective tissues. Compartment syndrome denotes a condition in which the intracompartmental pressure is constantly or repeatedly increased to a level at which the compartmental structures may be injured (Mubarak 1981). This may occur after trauma, such as fracture or crush injury to the arm. Compartment syndrome after strenuous exertion of the muscles is a well-known disease in the lower extremity. Some cases of exertional compartment syndrome in the forearm and hand have also been described, although the cause of these conditions is not known. Neither have generally accepted diagnostic criteria nor indications for treatment been defined. The afflicted workers have usually had hand-intensive work, although no epidemiological studies on the association between work and these diseases have been published.
The symptoms of compartment syndrome include tenseness of the fascial boundaries of the compartment, pain during muscle contraction and later also during rest, and muscle weakness. In clinical examination, the compartment area is tender, painful on passive stretching, and there may be diminished sensitivity in the distribution of the nerves running through the compartment. Intracompartmental pressure measurements during rest and activity, and after activity, have been used to confirm the diagnosis, but full agreement on normal values does not exist.
Intracompartmental pressure increases when the volume of the contents increases in the rigid compartment. This is followed by an increase in venous blood pressure, a decrease in the arterial and venous blood pressure difference which in turn affects blood supply of the muscle. This is followed by anaerobic energy production and muscle injury.
The prevention of exertional compartment syndrome includes avoiding or restricting the activity causing the symptoms to a level that can be tolerated.
Ulnar Artery Thrombosis(Hypothenar Hammer Syndrome)
The ulnar artery may undergo damage and subsequent thrombosis and occlusion of the vessel in the Guyon’s canal on the inner (ulnar) aspect of the palm. A history of repeated trauma to the ulnar side of the palm (hypothenar eminence), such as intensive hammering or using the hypothenar eminence as a hammer, has often preceded the disease (Jupiter and Kleinert 1988).
The symptoms include pain and cramping and cold intolerance of the fourth and fifth fingers. Neurological complaints may also be present, such as aching, numbness and tingling, but the performance of the muscles is usually normal. On clinical examination, coolness and blanching of the fourth and fifth fingers may be observed, as well as nutritional changes of the skin. The Allen’s test is usually positive, indicating that after compressing the radial artery, no blood flows to the palm via the ulnar artery. A palpable tender mass may be found in the hypothenar region.
Dupuytren’s Contracture
Dupuytren’s contracture is a progressive shortening (fibrosis) of the palmar fascia (connective tissue joining the flexor tendons of the fingers) of the hand, leading to permanent contracture of the fingers in a flexion posture. It is a common condition in people of North-European origin, affecting about 3% of the general population. The prevalence of the disease among the men is twice that among the women, and may be as high as 20% among males aged over 60. Dupuytren’s contracture is associated with epilepsy, type 1 diabetes, alcohol consumption and smoking. There is evidence for an association between vibration exposure from hand-held tools and Dupuytren’s contracture. The presence of the disease has been associated also with single injury and heavy manual labour. Some evidence exists to support an association between heavy manual work and Dupuytren’s contracture, whereas the role of single injury has not been adequately addressed (Liss and Stock 1996).
The fibrotic change appears first as a node. Later the fascia thickens and shortens, forming a chordlike attachment to the digit. As the process progresses, the fingers turn to permanent flexion. The fifth and fourth fingers are usually affected first, but other fingers also may be involved. Knuckle pads may be seen on the back side of the digits.
Wrist and Hand Ganglia
A ganglion is a soft, liquid-filled small sac; ganglia represent the majority of all soft tissue tumours of the hand. Ganglia are common, although the prevalence in populations is not known. In clinical populations, women have shown a higher prevalence than men, and both children and adults have been represented. Controversy exists on the causes of ganglia. Some consider them inborn while others believe that acute or repeated trauma play a role in their development. Different opinions exist also on the development process (Angelides 1982).
The most typical location of the ganglion is at the outer aspect of the back of the wrist (dorsoradial ganglion), where it can present as a soft, clearly visible formation. A smaller dorsal ganglion may not be noticeable without flexing the wrist markedly. The volar wrist ganglion (at the palmar aspect of the wrist) is typically located on the outer side of the tendon of the radial flexor of the wrist. The third commonly occurring ganglion is located at the pulley of the finger flexor tendon sheath at the level of the knuckles. A volar wrist ganglion may cause entrapment of the median nerve in the wrist, resulting in carpal tunnel syndrome. In rare cases a ganglion may be located in the ulnar canal (Guyon’s canal) in the inner palm and cause entrapment of the ulnar nerve.
The symptoms of wrist ganglia include local pain typically during exertion and deviated postures of the wrist. The ganglia in the palm and fingers are usually painful during gripping.
Disorders of Motor Control of the Hand(Writer’s Cramp)
Tremor and other uncontrolled movements may disturb hand functions which demand high precision and control, such as writing, assembly of small parts and playing musical instruments. The classical form of the disorder is writer’s cramp . The occurrence rate of writer’s cramp is not known. It affects both sexes and seems to be common in the third, fourth and fifth decades.
The causes of writer’s cramp and the related disorders are not fully understood. A hereditary predisposition has been suggested. The conditions are nowadays considered as a form of task-specific dystonia. (Dystonias are a group of disorders characterized by involuntary sustained muscle contractions, causing twisting and repetitive movements, or abnormal postures.) Pathological evidence of brain disease has not been reported for patients with writer’s cramp. Electrophysiological investigations have revealed abnormally prolonged activation of muscles involved in writing, and excess activation of those muscles that are not directly involved with the task (Marsden and Sheehy 1990).
In writer’s cramp, usually painless muscle spasm appears immediately or shortly after starting to write. The fingers, wrist and hand may assume abnormal postures, and the pen is often gripped with excessive force. The neurological status may be normal. In some cases an increased tension or tremor of the affected arm is observed.
Some of the subjects with writer’s cramp learn to write with the non-dominant hand, and a small proportion of these do develop cramp in the non-dominant hand as well. Spontaneous healing of writer’s cramp is rare.