Current knowledge of the short- and long-term manifestations of exposure to neurotoxic substances comes from experimental animal studies and human chamber studies, epidemiological studies of active and retired and/or diseased workers, clinical studies and reports, as well as large-scale disasters, such as those that occurred in Bhopal, following a leak of methyl isocyanate, and in Minamata, from methyl mercury poisoning.
Exposure to neurotoxic substances can produce immediate effects (acute) and/or long-term effects (chronic). In both cases, the effects can be reversible and disappear over time following reduction or cessation of exposure, or result in permanent, irreversible damage. The severity of acute and chronic nervous system impairment depends on exposure dose, which includes both the quantity and duration of exposure. Like alcohol and recreational drugs, many neurotoxic substances may initially be excitatory, producing a sensation of well-being or euphoria and/or speeding up motor functions; as the dose increases in quantity or in time, these same neurotoxins will depress the nervous system. Indeed, narcosis (a state of stupor or insensibility) is induced by a large number of neurotoxic substances, which are mind-altering and depress the central nervous system.
Acute Poisoning
Acute effects reflect the immediate response to the chemical substance. The severity of the symptoms and resulting disorders depends on the quantity that reaches the nervous system. With mild exposures, acute effects are mild and transient, disappearing when exposure ceases. Headache, tiredness, light-headedness, difficulty concentrating, feelings of drunkenness, euphoria, irritability, dizziness and slowed reflexes are the types of symptoms experienced during exposure to neurotoxic chemicals. Although these symptoms are reversible, when exposure is repeated day after day, the symptoms recur as well. Moreover, since the neurotoxic substance is not immediately eliminated from the body, symptoms can persist following work. Reported symptoms at a particular workstation are a good reflection of chemical interference with the nervous system and should be considered a warning signal for potential over-exposure; preventive measures to reduce exposure levels should be initiated.
If exposure is very high, as can occur with spills, leaks, explosions and other accidents, symptoms and signs of intoxication are debilitating (severe headaches, mental confusion, nausea, dizziness, incoordination, blurred vision, loss of consciousness); if exposure is high enough, effects can be long-lasting, possibly resulting in coma and death.
Acute pesticide-related disorders are a common occurrence among agricultural workers in food-producing countries, where large amounts of toxic substances are used as insecticides, fungicides, nematicides, and herbicides. Organophosphates, carbamates, organochlorines, pyrethrum, pyrethrin, paraquat and diquat are among the major categories of pesticides; however, there are thousands of pesticide formulations, containing hundreds of different active ingredients. Some pesticides, such as maneb, contain manganese, while others are dissolved in organic solvents. In addition to the symptoms mentioned above, acute organophosphate and carbamate poisoning may be accompanied by salivation, incontinence, convulsions, muscle twitching, diarrhoea, visual disturbances, as well as respiratory difficulties and a rapid heart rate; these result from an excess of the neurotransmitter acetylcholine, which occurs when these substances attack a chemical called cholinesterase. Blood cholinesterase decreases proportionally to the degree of acute organophosphate or carbamate intoxication.
With some substances, such as organophosphorus pesticides and carbon monoxide, high-level acute exposures can produce delayed deterioration of certain parts of the nervous system. For the former, numbness and tingling, weakness and disequilibrium can occur a few weeks after exposure, while for the latter, delayed neurologic deterioration can take place, with symptoms of mental confusion, ataxia, motor incoordination and paresis. Repeated acute episodes of high levels of carbon monoxide have been associated with later-life Parkinsonism. It is possible that high exposures to certain neurotoxic chemicals may be associated with an increased risk for neurodegenerative disorders later on in life.
Chronic Poisoning
Recognition of the hazards of neurotoxic chemicals has led many countries to reduce the permissible exposure levels. However, for most chemicals, the level at which no adverse effect will occur over long-term exposure is still unknown. Repeated exposure to low to medium levels of neurotoxic substances throughout many months or years can alter nervous system functions in an insidious and progressive manner. Continued interference with molecular and cellular processes causes neurophysiological and psychological functions to undergo slow alterations, which in the early stages may go unseen since there are large reserves in the nervous system circuitry and damage can, in the first stages, be compensated through new learning.
Thus, initial nervous system injury is not necessarily accompanied by functional disorders and may be reversible. However, as the damage progresses, symptoms and signs, often non-specific in nature, become apparent, and individuals may seek medical attention. Finally, impairment may become so severe that a clear clinical syndrome, generally irreversible, is manifest.
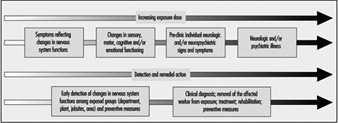
Figure 1 schematizes the health deterioration continuum associated with exposure to neurotoxic substances. Progression of neurotoxic dysfunction is dependent on both the duration and concentration of exposure (dose), and may be influenced by other workplace factors, individual health status and susceptibility as well as lifestyle, particularly drinking and exposure to neurotoxic substances used in hobbies, such as glues applied in furniture assembly or plastic model building, paints and paint removers.
Figure 1. Health deterioration on a continuum with increasing dosage
Different strategies are adopted for identification of neurotoxin-related illness among individual workers and for the surveillance of early nervous system deterioration among active workers. Clinical diagnosis relies on a constellation of signs and symptoms, coupled to the medical and exposure history for an individual; aetiologies other than exposure must be systematically ruled out. For the surveillance of early dysfunction among active workers, the group portrait of dysfunction is important. Most often, the pattern of dysfunction observed for the group will be similar to the pattern of impairment clinically observed in the disease. It is somewhat like summing early, mild alterations to produce a picture of what is happening to the nervous system. The pattern or profile of the overall early response provides an indication of the specificity and the type of action of the particular neurotoxic substance or mixture. In workplaces with potential exposure to neurotoxic substances, health surveillance of groups of workers may prove particularly useful for prevention and workplace action in order to avoid the development of more severe illness (see Figure 2). Workplace studies carried out throughout the world, with active workers exposed to specific neurotoxic substances or to mixtures of various chemicals, have provided valuable information on early manifestations of nervous system dysfunction in groups of exposed workers.
Figure 2. Preventing neurotoxicity at work.
Early symptoms of chronic poisoning
Altered mood states are most often the first symptoms of the initial changes in nervous system functioning. Irritability, euphoria, sudden mood changes, excessive tiredness, feelings of hostility, anxiousness, depression and tension are among the mood states most often associated with neurotoxic exposures. Other symptoms include memory problems, concentration difficulties, headaches, blurred vision, feelings of drunkenness, dizziness, slowness, tingling sensation in hands or feet, loss of libido and so on. Although in the early stages these symptoms are usually not sufficiently severe to interfere with work, they do reflect diminished well-being and affect one’s capacity to fully enjoy family and social relations. Often, because of the non-specific nature of these symptoms, workers, employers and occupational health professionals tend to ignore them and look for causes other than workplace exposure. Indeed, such symptoms may contribute to or aggravate an already difficult personal situation.
In workplaces where neurotoxic substances are used, workers, employers and occupational health and safety personnel should be particularly aware of the symptomatology of early intoxication, indicative of nervous system vulnerability to exposure. Symptom questionnaires have been developed for worksite studies and surveillance of workplaces where neurotoxic substances are used. Table 1 contains an example of such a questionnaire.
Table 1. Chronic symptoms checklist
Symptoms experienced in the past month
1. Have you tired more easily than expected for the type of activity you do?
2. Have you felt light-headed or dizzy?
3. Have you had difficulty concentrating?
4. Have you been confused or disoriented?
5. Have you had trouble remembering things?
6. Have your relatives noticed that you have trouble remembering things?
7. Have you had to make notes to remember things?
8. Have you found it hard to understand the meaning of newspapers?
9. Have you felt irritable?
10. Have you felt depressed?
11. Have you had heart palpitations even when you are not exerting yourself?
12. Have you had a seizure?
13. Have you been sleeping more often than is usual for you?
14. Have you had difficulty falling asleep?
15. Have you been bothered by incoordination or loss of balance?
16. Have you had any loss of muscle strength in your legs or feet?
17. Have you had any loss of muscle strength in your arms or hands?
18. Have you had difficulty moving your fingers or grasping things?
19. Have you had hand numbness and tingling in your fingers lasting for more than a day?
20. Have you had hand numbness and tinging in your toes lasting more than a day?
21. Have you had headaches at least once a week?
22. Have you had difficulty driving home from work because you felt dizzy or tired?
23. Have you felt “high” from the chemicals used at work?
24. Have you had a lower tolerance for alcohol (takes less to get drunk)?
Source: Taken from Johnson 1987.
Early motor, sensory and cognitive changes in chronicpoisoning
With increasing exposure, changes can be observed in motor, sensory and cognitive functions in workers exposed to neurotoxic substances, who do not present clinical evidence of abnormality. Since the nervous system is complex, and certain areas are vulnerable to specific chemicals, while others are sensitive to the action of a large number of toxic agents, a wide range of nervous system functions may be affected by a single toxic agent or a mixture of neurotoxins. Reaction time, hand-eye coordination, short-term memory, visual and auditory memory, attention and vigilance, manual dexterity, vocabulary, switching attention, grip strength, motor speed, hand steadiness, mood, colour vision, vibrotactile perception, hearing and smell are among the many functions that have been shown to be altered by different neurotoxic substances.
Important information on the type of early deficits that result from exposure has been provided by comparing performance between exposed and non-exposed workers and with respect to the degree of exposure. Anger (1990) provides an excellent review of worksite neurobehavioural research up to 1989. Table 2 adapted from this article, provides an example of the type of neuro-functional deficits that have been consistently observed in groups of active workers exposed to some of the most common neurotoxic substances.
Table 2. Consistent neuro-functional effects of worksite exposures to some leading neurotoxic substances
|
Mixed organic solvents |
Carbon disulphide |
Styrene |
Organophos- |
Lead |
Mercury |
|
|
Acquisition |
+ |
|
|
|
+ |
|
|
Affect |
+ |
|
+ |
|
+ |
|
|
Categorization |
+ |
|
|
|
|
|
|
Coding |
+ |
+ |
|
|
+ |
+ |
|
Colour vision |
+ |
|
+ |
|
|
|
|
Concept shifting |
+ |
|
|
|
|
|
|
Distractibility |
|
|
|
|
+ |
|
|
Intelligence |
+ |
+ |
|
+ |
+ |
+ |
|
Memory |
+ |
+ |
+ |
+ |
+ |
+ |
|
Motor coordination |
+ |
+ |
+ |
|
+ |
+ |
|
Motor speed |
+ |
+ |
+ |
|
+ |
+ |
|
Near visual contrast sensitivity |
+ |
|
|
|
|
|
|
Odour perception threshold |
+ |
|
|
|
|
|
|
Odour identification |
+ |
|
|
|
+ |
|
|
Personality |
+ |
+ |
|
|
|
+ |
|
Spatial relations |
+ |
+ |
|
|
+ |
|
|
Vibrotactile threshold |
+ |
|
|
+ |
|
+ |
|
Vigilance |
+ |
+ |
|
|
+ |
|
|
Visual field |
|
|
|
|
+ |
+ |
|
Vocabulary |
|
|
|
|
+ |
|
Source: Adapted from Anger 1990.
Although at this stage in the continuum from well-being to disease, loss is not in the clinically abnormal range, there can be health-related consequences associated with such changes. For example, decreased vigilance and reduced reflexes may put workers in greater danger of accidents. Smell is used to identify leaks and mask saturation (cartridge breakthrough), and acute or chronic loss of smell renders one less apt to identify a potentially hazardous situation. Mood changes may interfere with inter-personal relations at work, socially and in the home. These initial stages of nervous system deterioration, which can be observed by examining groups of exposed workers and comparing them to non-exposed workers or with respect to their degree of exposure, reflect diminished well-being and may be predictive of risk of more serious neurological problems in the future.
Mental health in chronic poisoning
Neuropsychiatric disorders have long been attributed to exposure to neurotoxic substances. Clinical descriptions range from affective disorders, including anxiety and depression, to manifestations of psychotic behaviour and hallucinations. Acute high-level exposure to many heavy metals, organic solvents and pesticides can produce delirium. “Manganese madness” has been described in persons with long-term exposure to manganese, and the well-known “mad hatter” syndrome results from mercury intoxication. Type 2a Toxic Encephalopathy, characterized by sustained change in personality involving fatigue, emotional lability, impulse control and general mood and motivation, has been associated with organic solvent exposure. There is growing evidence from clinical and population studies that personality disorders persist over time, long after exposure ceases, although other types of impairment may improve.
On the continuum from well-being to disease, mood changes, irritability and excessive fatigue are often the very first indications of over-exposure to neurotoxic substances. Although neuropsychiatric symptoms are routinely surveyed in worksite studies, these are rarely presented as a mental health problem with potential consequences on mental and social well-being. For example, changes in mental health status affect one’s behaviour, contributing to difficult inter-personal relationships and disagreements in the home; these in turn can aggravate one’s mental state. In workplaces with employee aid programmes, designed to help employees with personal problems, ignorance of the potential mental health effects of exposure to neurotoxic substances can lead to treatment dealing with the effects rather than the cause. It is interesting to note that among the many reported outbreaks of “mass hysteria” or psychogenic illness, industries with exposure to neurotoxic substances are over-represented. It is possible that these substances, which, for the large part, went unmeasured, contributed to the reported symptoms.
Mental health manifestations of neurotoxin exposure can be similar to those that are caused by psychosocial stressors associated with poor work organization, as well as psychological reactions to accidents, very stressful occurrences and severe intoxications, called post-traumatic stress disorder (as discussed elsewhere in this Encyclopaedia). A good understanding of the relation between mental health problems and working conditions is important to initiating adequate preventive and curative actions.
General considerations in assessing early neurotoxicdysfunction
When evaluating early nervous system dysfunction among active workers, a number of factors must be taken into account. Firstly, many of the neuropsychological and neurophysiological functions that are examined diminish with age; some are influenced by culture or educational level. These factors must be taken into account when considering the relation between exposure and nervous system alterations. This can be done by comparing groups with similar socio-demographic status or by using statistical methods of adjustment. There are, however, certain pitfalls that should be avoided. For example, older workers may have longer work histories, and it has been suggested that some neurotoxic substances may accelerate ageing. Job segregation may confine poorly educated workers, women and minorities in jobs with higher exposures. Secondly, alcohol consumption, smoking and drugs, which all contain neurotoxic substances, may also affect symptoms and performance. A good understanding of the workplace is important in unravelling the different factors that contribute to nervous system dysfunction and the implementation of preventive measures.