Definition of Neurotoxicity
Neurotoxicity refers to the capability of inducing adverse effects in the central nervous system, peripheral nerves or sensory organs. A chemical is considered to be neurotoxic if it is capable of inducing a consistent pattern of neural dysfunction or change in the chemistry or structure of the nervous system.
Neurotoxicity is generally manifested as a continuum of symptoms and effects, which depend on the nature of the chemical, the dose, the duration of exposure and the traits of the exposed individual. The severity of the observed effects, as well as the evidence for neurotoxicity, increases through levels 1 to 6, shown in Table 1. Short-term or low-dose exposure to a neurotoxic chemical may result in subjective symptoms such as headache and dizziness, but the effect usually is reversible. With increasing dose, neurological changes may show up, and eventually irreversible morphological changes are generated. The degree of abnormality needed for implying neurotoxicity of a chemical agent is a controversial issue. According to the definition, a consistent pattern of neural dysfunction or change in the chemistry or structure of the nervous system is considered if there is well-documented evidence for persistent effects on level 3, 4, 5 or 6 in Table 1. These levels reflect the weight of evidence provided by different signs of neurotoxicity. Neurotoxic substances include naturally occurring elements such as lead, mercury and manganese; biological compounds such as tetrodotoxin (from the puffer fish, a Japanese delicacy) and domoic acid (from contaminated mussels); and synthetic compounds including many pesticides, industrial solvents and monomers.
Table 1. Grouping neurotoxic effects to reflect their relative strength for establishing neurotoxicity
|
Level |
Grouping |
Explanation/Examples |
|
6 |
Morphological changes |
Morphological changes include cell death and axonopathy as well as subcellular morphological changes. |
|
5 |
Neurological changes |
Neurological change embraces abnormal findings in neurological examinations on single individuals. |
|
4 |
Physiological/behavioural changes |
Physiological/behavioural changes comprise experimental findings on groups of animals or humans such as changes in evoked potentials and EEG, or changes in psychological and behavioural tests. |
|
3 |
Biochemical changes |
Biochemical changes cover changes in relevant biochemical parameters (e.g., transmitter level, GFA-protein content (glial fibrillary acidic protein) or enzyme activities). |
|
21 |
Irreversible, subjective symptoms |
Subjective symptoms. No evidence of abnormality on neurological, psychological or other medical examination. |
|
11 |
Reversible, subjective symptoms |
Subjective symptoms. No evidence of abnormality on neurological, psychological, or other medical examination. |
1 Humans only
Source: Modified from Simonsen et al. 1994.
In the United States between 50,000 and 100,000 chemicals are in commerce, and 1,000 to 1,600 new chemicals are submitted for evaluation each year. More than 750 chemicals and several classes or groups of chemical compounds are suspected to be neurotoxic (O’Donoghue 1985), but the majority of chemicals have never been tested for neurotoxic properties. Most of the known neurotoxic chemicals available today have been identified by case-reports or through accidents.
Although neurotoxic chemicals often are produced to fulfil specific uses, exposure may arise from several sources—use in private homes, in agriculture and in industries, or from polluted drinking water and so on. Fixed a priori preconceptions about which neurotoxic compounds are expected to be found in which occupations should therefore be viewed with caution, and the following citations should be looked upon as possible examples including a few of the most common neurotoxic chemicals (Arlien-Søborg 1992; O’Donoghue 1985; Spencer and Schaumburg 1980; WHO 1978).
Symptoms of Neurotoxicity
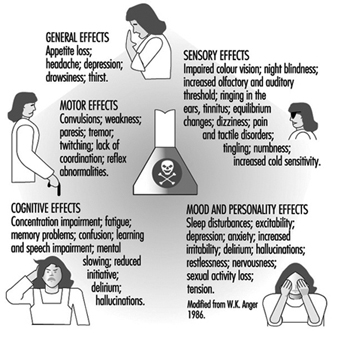
The nervous system generally reacts rather stereotypically to exposure to neurotoxic substances Figure 1. Some typical syndromes are indicated below.
Figure 1. Neurological and behavioural effects of exposure to neurotoxic chemicals.
Polyneuropathy
This is caused by impairment of motor and sensory nerve function leading to weakness of the muscles, with paresis usually most pronounced peripherally in the upper and lower extremities (hands and feet). Prior or simultaneous paraesthesia (tingling or numbness in the fingers and toes) may occur. This may lead to difficulties in walking or in the fine coordination of hands and fingers. Heavy metals, solvents and pesticides, among other chemicals, may result in such disability, even if the toxic mechanism of these compounds may be totally different.
Encephalopathy
This is caused by a diffuse impairment of the brain, and may result in fatigue; impairment of learning, memory and ability to concentrate; anxiety, depression, increased irritability and emotional instability. Such symptoms may indicate early diffuse degenerative brain disorder as well as occupational chronic toxic encephalopathy. Often increased frequency of headaches, dizziness, changes in sleep pattern and reduced sexual activity may also be present from the early stages of the disease. Such symptoms may develop following long-term, low-level exposure to several different chemicals such as solvents, heavy metals or hydrogen sulphide, and are also seen in several dementing disorders not related to work. In some cases more specific neurological symptoms can be seen (e.g., Parkinsonism with tremor, rigidity of the muscles and slowing of movements, or cerebellar symptoms such as tremor and reduced coordination of hand movements and gait). Such clinical pictures can be seen following exposure to some specific chemicals such as manganese, or MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) in the former condition, and toluene or mercury in the latter.
Gases
A wide variety of chemicals with totally different chemical structures are gases at normal temperature and have been proven neurotoxic Table 3. Some of them are extremely toxic even in very small doses, and have even been used as war gases (phosgene and cyanide); others require high doses over longer periods to give symptoms (e.g., carbon dioxide). Some are used for general anaesthesia (e.g., nitrous oxide); others are widely used in industry and in agents used for disinfection (e.g., formaldehyde). The former may induce irreversible changes in the nervous system after repeated low-level exposure, the latter apparently produce only acute symptoms. Exposure in small rooms with poor ventilation is particularly hazardous. Some of the gases are odourless, which makes them particularly dangerous (e.g., carbon monoxide). As shown in Table 2, some gases are important constituents in industrial production, while others are the result of incomplete or complete combustion (e.g., CO and CO2 respectively). This is seen in mining, steel works, power stations and so on, but may also be seen in private homes with insufficient ventilation. Essential for treatment is to stop further exposure and provide fresh air or oxygen, and in severe cases artificial ventilation.
Table 2. Gases associated with neurotoxic effects
|
Chemical |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Carbon dioxide (CO2 ) |
Welding; fermentation; manufacture, storage and use of dry ice |
Metal industry; mining; breweries |
M: Dilate vessels A: Headache; dyspnoea; tremor; loss of consciousness C: Hardly any |
|
Carbon monoxide (CO) |
Car repair; welding; metal melting; drivers; firemen |
Metal industry; mining; transportation; power station |
M: Deprivation of oxygen A: Headache; drowsiness; loss of consciousness |
|
Hydrogen sulphide (H2S) |
Fumigating of green house; manure; fishermen; fish unloading; sewerage handling |
Agriculture; fishing; sewer work |
M: Blocking oxidative metabolism A: Loss of consciousness C: Encephalopathy |
|
Cyanide (HCN) |
Electro-welding; galvanic surface treatment with nickel; copper and silver; fumigation of ships, houses foods and soil in green houses |
Metal industry; chemical industry; nursery; mining; gasworks |
M: Blocking of respiratory enzymes A: Dyspnoea; falling blood pressure; convulsions; loss of consciousness; death C: Encephalopathy; ataxia; neuropathy (e.g., aftereating cavasava) Occupational impairment uncertain |
|
Nitrous oxide (N2O) |
General anaesthesia during operation; light narcosis at dental care and delivery |
Hospitals (anaesthesia); dentists; midwife |
M: Acute change in nerve cell membrane; degeneration of nerve cells after long-term exposure A: Light-headedness; drowsiness; loss of consciousness C: Numbness of fingers and toes; reduced coordination; encephalopathy |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor- and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain.
Ataxia: impaired motor coordination.
Metals
As a rule the toxicity of metals increases with increasing atomic weight, lead and mercury being particularly toxic. Metals are usually found in nature at low concentrations, but in certain industries they are used in great amounts (see Table 3) and may give rise to occupational risk for the workers. Moreover, considerable amounts of metals are found in waste water and may give rise to environmental risk for the residents close to the plants but also at greater distances. Often the metals (or, for example, organic mercury compounds) are taken up into the food chain and will accumulate in fish, birds and animals, representing a risk for consumers. The toxicity and the way in which the metals are handled by the organism may depend on the chemical structure. Pure metals may be taken up by inhalation or skin contact of vapour (mercury) and/or small particles (lead), or orally (lead). Inorganic mercury compounds (e.g., HgCl2) are mainly taken up by mouth, while organic metal compounds (e.g., tetraethyl lead) mainly are taken up by inhalation or by skin contact. The body burden may to a certain degree be reflected in the concentration of metal in the blood or urine. This is the basis for biological monitoring. In treatment it must be recalled that especially lead is released very slowly from deposits in the body. The amount of lead in bones will normally be reduced by only 50% over 10 years. This release may be speeded up by the use of chelating agents: BAL (dimercapto-1-propanol), Ca-EDTA or penicillamine.
Table 3. Metals and their inorganic compounds associated with neurotoxicity
|
Chemical |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Lead |
Melting; soldering; grinding; repair; glazing; plasticizer |
Metal work; mining; accumulator plants; car repair; shipyards; glass workers; ceramics; pottery; plastic |
M: Impairment of oxidative metabolism of nerve cells and glia A: Abdominal pain; headache; encephalopathy; seizures C: Encephalopathy; polyneuropathy, including drop hand |
|
Mercury Elemental |
Electrolysis; electrical instruments (gyroscope; manometer; thermometer; battery; electric bulb; tubes, etc.); amalgam filling |
Chloralkali plants; mining; electronics; dentistry; polymer production; paper and pulp industry |
M: Impairment at multiple sites in nerve cells A: Lung inflammation; headache; impaired speech C: Inflammation of gums; appetite loss; encephalopathy; including tremor; irritability |
|
Calomel Hg2Cl2 |
Laboratories |
A: Low acute toxicity chronic toxic effects, see above |
|
|
Sublimate HgCl2 |
Disinfection |
Hospitals; clinics; laboratories |
M: Acute tubular and glomerular renal degeneration. Verytoxic even in small oral doses, lethal down to 30 mg/kgweight C: See above. |
|
Manganese |
Melting (steel alloy); cutting; welding in steel; dry batteries |
Manganese mining; steel and aluminium production; metal industry; battery production; chemical industry; brickyard |
M: Not known, possible changes in dopamine and catecholamine in basal ganglia in the centre of the brain A: Dysphoria C: Encephalopathy including Parkinsonism; psychosis; appetite loss; irritability; headache; weakness |
|
Aluminium |
Metallurgy; grinding; polishing |
Metal industry |
M: Unknown C: Possibly encephalopathy |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor- and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain.
Monomers
Monomers constitute a large, heterogeneous group of reactive chemicals used for chemical synthesis and production of polymers, resins and plastics. Monomers comprise polyhalogenated aromatic compounds such as p-chlorobenzene and 1,2,4-trichlorbenzene; unsaturated organic solvents such as styrene and vinyltoluene, acrylamide and related compounds, phenols, ɛ-caprolactam and ζ-aminobutyrolactam. Some of the widely used neurotoxic monomers and their effect on the nervous system are listed in Table 3. Occupational exposure to neurotoxic monomers may take place at industries manufacturing, transporting and using chemical products and plastic products. During handling of polymers containing rest monomers, and during moulding in boat yards and in dental clinics, a substantial exposure to neurotoxic monomers takes place. Upon exposure to these monomers uptake may take place during inhalation (e.g., carbon disulphide and styrene) or by skin contact (e.g., acrylamide). As monomers are a heterogeneous group of chemicals, several different mechanisms of toxicity are likely. This is reflected by differences in symptoms (Table 4).
Table 4. Neurotoxic monomers
|
Compound |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Acrylamide |
Employees exposed to the monomer |
Polymer production; tunnelling and drilling operations |
M: Impaired axonal transport C: Polyneuropathy; dizziness; tremor and ataxia |
|
Acrylonitrile |
Accidents in labs and industries; house fumigation |
Polymer and rubber production; chemical synthesis |
A: Hyperexcitability; salivation; vomiting; cyanosis; ataxia; difficulty breathing |
|
Carbon disulphide |
Production of rubber and viscose rayon |
Rubber and viscose rayon industries |
M: Impaired axonal transport and enzyme activity is likely C: Peripheral neuropathy; encephalopathy; headache; vertigo; gastrointestinal disturbances |
|
Styrene |
Production of glass-reinforced plastics; monomer manufacture and transportation; use of styrene-containing resins and coatings |
Chemical industry; fibreglass production; polymer industry |
M: Unknown A: Central nervous system depression; headache C: Polyneuropathy; encephalopathy; hearing loss |
|
Vinyltoluene |
Resin production; insecticide compounds |
Chemical and polymer industry |
C: Polyneuropathy; reduced motor nerve conductionvelocity |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain.
Ataxia: impaired motor coordination.
Organic solvents
Organic solvents is a common designation for a large group of more than 200 lipophilic chemical compounds capable of dissolving fats, oils, waxes, resins, rubber, asphalt, cellulose filaments and plastic materials. They are usually fluids at room temperature with boiling points below 200 to 250°C, and are easily evaporated. They are mainly taken up via the lungs but some may penetrate the skin as well. Due to their lipophilicity they are distributed to organs rich in fat. Thus high concentrations are found in body fat, bone marrow, liver and brain, which also may act as reservoirs of solvents. The partition coefficient octanol/water can indicate whether high brain concentrations are to be expected. The mechanism of toxicity is not yet known, but several possibilities have been envisioned: blocking important enzymes in the metabolic breakdown of glucose and thus reducing energy available for neuronal processing; reducing energy formation in the mitochondria; changing neuronal membranes, leading to impairment of ion channel function; slowing of axonal flow. Methylene chloride is metabolized to CO, which blocks the transport of oxygen in the blood. Large groups of workers in a great variety of professions are exposed daily or at least frequently (see Table 5). In some countries the consumption of organic solvents has declined in some occupations due to hygienic improvements and substitution (e.g., house painters, graphic industry workers, metal workers), while in other occupations the pattern of exposure has changed but the total amount of organic solvents has remained unchanged. For example, trichloroethylene has been replaced by 1,1,1-trichloroethane and freon. So solvents are still a major hygienic problem at many workplaces. People are at particular risk when exposed in small rooms with poor ventilation and with high temperature, increasing the evaporation. Physical work increases the pulmonary uptake of solvents. In several countries (in particular the Nordic countries), compensation has been given to workers who have developed chronic toxic encephalopathy following long-term, low-level exposure to solvents.
Table 5. Organic solvents associated with neurotoxicity
|
Chemical |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Chlorinated hydrocarbons: trichloroethylene; 1,1,1-trichloroethane; tetrachloroethylene |
Degreasing; electroplating; painting; printing; cleaning; general and light anaesthesia |
Metal industry; graphic industry; electronic industry; dry cleaners; anaesthetists |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy; polyneuropathy; trigeminal affection (TRI); hearing loss |
|
Methylene chloride |
Extraction, including extraction of caffeine; paint remover |
Food industry; painters; graphic industry |
M: Metabolism ® CO A: Prenarcotic symptoms; coma C: Encephalopathy |
|
Methyl chloride |
Refrigerator production and repair |
Refrigerator production; rubber industry; plastic industry |
M: Unknown A: Prenarcotic symptoms; loss of consciousness; death C: Encephalopathy |
|
Toluene |
Printing; cleaning; degreasing; electroplating; painting; spray painting |
Graphic industry; electronic industry |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy; cerebellar dysfunction; polyneuropathy; hearing loss; visual disturbance |
|
Xylene |
Printing; synthesis of phthalic anhydride; painting; histology laboratory procedures |
Graphic industry; plastic industry; histology laboratories |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy; visual disturbance; hearing loss |
|
Styrene |
Polymerization; moulding |
Plastic industry; fibreglass production |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy; polyneuropathy; hearing loss |
|
Hexacarbons: n-hexane; methyl butyl ketone (MBK); methyl ethyl ketone (MEK) |
Gluing; printing; plastic coating; painting; extraction |
Leather and shoe industry; graphic industry; painter; laboratories |
M: Impairment of axonal transport A: Prenarcotic C: Polyneuropathy; encephalopathy |
|
Various solvents: Freon 113 |
Refrigerator production and repair; dry cleaning; degreasing |
Refrigerator production; metal industry; electronic industry; dry cleaning |
M: Unknown A: Mild prenarcotic symptoms C: Encephalopathy |
|
Diethylether; halothane |
General anaesthetics (nurses; doctors) |
Hospitals; clinics |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy |
|
Carbon disulphide |
See monomers |
See monomers |
See monomers |
|
Mixtures: white spirit and thinner |
Painting; degreasing; cleaning; printing; impregnation; surface treatment |
Metal industry; graphic industry; wood industry; painters |
M: Unknown A: Prenarcotic symptoms C: Encephalopathy |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor- and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain
Pesticides
Pesticides is used as a generic term for any chemical designed to kill groups of plants or animals that are a human health hazard or may cause economic loss. It includes insecticides, fungicides, rodenticides, fumigants and herbicides. Approximately 5 billion pounds of pesticide products made up of more than 600 active pesticide ingredients are annually used in agriculture worldwide. Organophosphorus, carbamate and organochlorine pesticides together with pyrethroids, chlorophenoxy herbicides and organic metal compounds used as fungicides have neurotoxic properties (Table 6). Among the many different chemicals used as rodenticides, some (e.g., strychnine, zinc phosphide and thallium) are neurotoxic too. Occupational exposure to neurotoxic pesticides is mainly associated with agricultural work such as pesticide handling and working with treated crops, but exterminators, pesticide manufacturing and formulating employees, highway and railway workers, as well as greenhouse, forestry and nursery workers may have a substantial risk of being exposed to neurotoxic pesticides as well. Children, who constitute a significant proportion of the agricultural workforce, are especially vulnerable because their nervous systems are not fully developed. The acute effects of pesticides are generally well described, and long-lasting effects upon repeated exposure or single high dose exposure are often seen (Table 6), but the effect of repeated subclinical exposure is uncertain.
Table 6. Classes of common neurotoxic pesticides, exposure, effects and associated symptoms
|
Compound |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Organo-phosphorus compounds: Beomyl; Demethon; Dichlorvos; Ethyl parathion; Mevinphos; Phosfolan; Terbufos; Malathion |
Handling; treatment of crops; working with treated crops; dock labourer |
Agriculture; forestry; chemical; gardening |
M: Acetyl cholinesterase inhibition A: Hyperactivity; neuromuscular paralysis; visual impairment; breathing difficulty; restlessness; weakness; vomiting; convulsions |
|
Carbamates: Aldicarb; Carbaryl; Carbofuran; Propoxur |
M: Delayed neurotoxicity axonopathy2 C: Polyneuropathy; numbness and tingling in feet; muscle weakness; sensory disturbance; paralysis |
||
|
Organochlorine: Aldrin; Dieldrin; DDT; Endrin; Heptachlor; Lindane; Methoxychlor; Mirex; Toxaphene |
See above |
See above |
A: Excitability; apprehension; dizziness; headache; confusion; loss of balance; weakness; ataxia; tremors; convulsions; coma C: Encephalopathy |
|
Pyrethroids |
See above |
See above |
M: Altering flow of sodium ions through nerve cellmembrane A: Repeated firing of the nerve cell; tremor; convulsion |
|
2,4-D |
Herbicide |
Agriculture |
C: Polyneuropathy |
|
Triethyltin hydroxide |
Surface treatment; handling treated wood |
Wood and wood products |
A: Headache; weakness; paralysis; visual disturbances C: Polyneuropathy; CNS effects |
|
Methyl bromide |
Fumigating |
Greenhouses; insecticide; manufacture of refrigerators |
M: Unknown A: Visual and speech disturbances; delirium; convulsion C: Encephalopathy |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain.
Ataxia: impaired motor coordination.
2 Mainly phosphates or phosphonates.
Other chemicals
Several different chemicals which do not fit into the above-mentioned groups also possess neurotoxicity. Some of these are used as pesticides but also in different industrial processes. Some have well-documented acute and chronic neurotoxic effects; others have obvious acute effects, but the chronic effects are only poorly examined. Examples of these chemicals, their uses and effects are listed in Table 7.
Table 7. Other chemicals associated with neurotoxicity
|
Chemical |
Examples of source of exposure |
Selected industries at risk |
Effects1 |
|
Boric acid |
Welding; fluxes; preservation |
Metal; glass |
A: Delirium; convulsion C: CNS depression. |
|
Disulfiram |
Pharmaceutical |
Rubber |
C: Fatigue; peripheral neuropathy; sleepiness |
|
Hexachlorophene |
Antibacterial soaps |
Chemical |
C: CNS oedema; peripheral nerve damage |
|
Hydrazine |
Reducing agents |
Chemical; army |
A: Excitement; appetite loss; tremor; convulsion |
|
Phenol/Cresol |
Antiseptics |
Plastics; resins; chemical; hospitals; laboratories |
M: Denatures proteins and enzymes A: Reflex loss; weakness; tremor; sweating; coma C: Appetite loss; mental disturbance; ringing in the ears |
|
Pyridine |
Ethanol denaturation |
Chemical; textile |
A: CNS depression; mental depression; fatigue; appetite loss C: Irritability; sleep disorders; polyneuropathy; double vision |
|
Tetraethyl lead |
Gasoline additive |
Chemical; transport |
C: Irritability; weakness; tremor; vision difficulties |
|
Arsine |
Batteries; insecticide; melting |
Smelting; glasswork; ceramics; manufacture of paper |
M: Impairing enzyme function A: Reduced sensation; paresis; convulsion; coma C: Motor impairment; ataxia; vibration sense loss; polyneuropathy |
|
Lithium |
Oil additive; pharmaceutical |
Petrochemical |
A/C: Appetite loss; ringing in the ears; vision blurring; tremor; ataxia |
|
Selenium |
Melting; production of rectifiers; vulcanization; cutting oils; antioxidant |
Electronic; glass works; metal industry; rubber industry |
A: Delirium; anosmia C: Odour of garlic; polyneuropathy; nervousness |
|
Thallium |
Rodenticide |
Glass; glass products |
A: Appetite loss; tiredness; drowsiness; metallic taste; numbness; ataxia |
|
Tellurium |
Melting; rubber production; catalyst |
Metal; chemical; rubber; electronic |
A: Headache; drowsiness; neuropathy C: Odour of garlic; metallic taste; Parkinsonism; depression |
|
Vanadium |
Melting |
Mining; steel production; chemical industry |
A: Appetite loss; ringing in the ears; somnolence, tremor C: Depression; tremor; blindness |
1 M: mechanism; A: acute effects; C: chronic effects.
Neuropathy: dysfunction of motor and sensory peripheral nerve fibres.
Encephalopathy: brain dysfunction due to generalized impairment of the brain.
Ataxia: impaired motor coordination