Introduction
Over the last few decades, the health risk appraisal (HRA), also known as a health hazard appraisal or a health risk assessment, has become increasingly popular, primarily in the United States, as an instrument for promoting health awareness and motivating behavioral change. It is also used as an introduction to periodic health screening or as a substitute for it and, when aggregated for a group of individuals, as the basis for identifying targets for a health education or health promotion program to be designed for them. It is based on the following concept:
- Ostensibly healthy, asymptomatic individuals may be at risk of developing a disease process that can cause morbidity in the future and may lead to premature death.
- Factors that lead to such risk can be identified.
- Some of those risk factors can be eliminated or controlled thereby preventing or attenuating the disease process and preventing or delaying the morbidity and mortality.
The development of the HRA in the 1940s and 1950s is credited to Dr. Lewis Robbins, working at the Framingham prospective study of heart disease and later at the National Cancer Institute (Beery et al. 1986). The 1960s saw additional models developed and, in 1970, Robbins and Hall produced the seminal work that defined the technique, described the survey instruments and the risk computations, and outlined the patient feedback strategy (Robbins and Hall 1970).
Interest in HRA and health promotion in general was stimulated by a growing awareness of the importance of risk factor control as a basis element in health promotion, the evolving use of computers for data compilation and analysis and, especially in the United States, increasing concern over the escalating cost of health care and the hope that preventing illness might slow its upward spiral of growth. By 1982, Edward Wagner and his colleagues at the University of North Carolina were able to identify 217 public and private HRA vendors in the United States (Wagner et al. 1982). A good many of these have since faded from the scene but they have been replaced, at least to a limited extent, by new entrants into the marketplace. According to a 1989 report of a survey of a random sample of US worksites, 29.5% have conducted HRA activities; for worksites with more than 750 employees, this figure rose to 66% (Fielding 1989). HRA use in other countries has lagged considerably.
What is the HRA?
For purposes of this article, an HRA is defined as a tool for assessing health risks that has three essential elements:
- A self-administered questionnaire inquiring about the individual’s demographic profile, medical background, family history, personal habits and lifestyle. This information is frequently supplemented by biomedical measurements such as height, weight, blood pressure, and skin-fold thickness, and data regarding the results of urinalysis, blood cholesterol level and other laboratory tests, either as reported by the individual or taken as part of the process.
- A quantitative estimation of the individual’s future risk of death or other adverse outcomes from specific causes based on a comparison of the individual’s responses to epidemiological data, national mortality statistics and actuarial calculations. Some questionnaires are self-scored: points are assigned to the response to each question and then added to derive a risk score. With the appropriate computer software, the responses may be entered into a microcomputer that will calculate the score. Most often the completed questionnaires are forwarded to a central point for batch processing and the individual results are mailed or delivered to the participants.
- Feedback to the individual with suggestions for changes in lifestyle and other actions that would improve well-being and reduce the risk of disease or premature death.
Originally, the total risk estimate was presented as a single number that could be targeted for reduction to a “normal” value or even to lower-than-normal values (vis-à-vis the general population) by implementing the suggested behavioral changes. To make the results more graphic and compelling, the risk is now sometimes expressed as a “health age” or “risk age” to be compared with the individual’s chronological age, and an “achievable age” as the target for the interventions. For example, a report might say, “Your present age is 35 but you have the life expectancy of a person aged 42. By following these recommendations, you could reduce your risk age to 32, thereby adding ten years to your projected life span.”
Instead of comparing the individual’s health status with the “norm” for the general population, some HRAs offer an “optimal health” score: the best attainable score that might be achieved by following all of the recommendations. This approach appears to be particularly useful in guiding young people, who may not yet have accumulated significant health risks, to an optimally desirable lifestyle.
The use of a “risk age” or a single number to represent the individual’s composite risk status may be misleading: a significant risk factor may be statistically offset by “good” scores on most other areas and lead to a false sense of security. For example, a person with normal blood pressure, a low blood cholesterol level, and a good family history who exercises and wears automobile seat belts may earn a good risk score despite the fact that he smokes cigarettes. This suggests the desirability of focusing on each “greater than average” risk item instead of relying on the composite score alone.
The HRA is not to be confused with health status questionnaires that are used to classify the eligibility of patients for particular treatments or to evaluate their outcomes, nor with the variety of instruments used to assess degree of disability, mental health, health distress or social functioning, although such scales are sometimes incorporated into some HRAs.
HRA Questionnaire
Although the HRA is sometimes used as a prelude to or part of a periodic, pre-employment or pre-placement medical examination, it is usually offered independently as a voluntary exercise. Many varieties of HRA questionnaires are in use. Some are limited to core questions that feed directly into the risk age calculations. In others, these core questions are interspersed with additional medical and behavioral topics: more extensive medical history; stress perceptions; scales to measure anxiety, depression and other psychological disorders; nutrition; use of preventive services; personal habits and even interpersonal relationships. Some vendors allow purchasers to add questions to the questionnaire, although responses to these are not usually incorporated into the health-risk computations.
Almost all HRAs now use forms with boxes to be checked or filled in by pencil for computer entry by hand or by an optical scanner device. As a rule, the completed questionnaires are collected and batch-processed, either in-house or by the HRA vendor. To encourage trust in the confidentiality of the program, completed questionnaires are sometimes mailed directly to the vendor for processing and the reports are mailed to the participants’ homes. In some programs, only “normal” results are mailed to participants, while those employees with results calling for intervention are invited for private interviews with trained staff persons who interpret them and outline the corrective actions that are indicated. Greater access to personal computers and more widespread familiarity with their use have led to the development of interactive software programs that allow direct entry of the responses into a microcomputer and immediate calculation and feedback of the results along with risk reduction recommendations. This approach leaves it up to the individual to take the initiative of seeking help from a staff person when clarification of the results and their implications is needed. Except when the software program allows storage of the data or their transfer to a centralized data bank, this approach does not provide information for systematic follow-up and it precludes the development of aggregate reports.
Managing the Program
Responsibility for managing the HRA program is usually assigned to the respective directors of the employee health service, the wellness program or, less frequently, the employee assistance program. Quite often, however, it is arranged and supervised by the personnel/human resources staff. In some instances, an advisory committee is created, often with employee or labor union participation. Programs incorporated into the organization’s operating routine appear to run more smoothly than those that exist as somewhat isolated projects (Beery et al. 1986). The organizational location of the program may be a factor in its acceptance by employees, particularly when confidentiality of personal health information is an issue. To preclude such a concern, the completed questionnaire is usually mailed in a sealed envelope to the vendor, who processes the data and mails the individual report (also in a sealed envelope) directly to the participant’s home.
To enhance participation in the program, most organizations publicize the program through preliminary hand-outs, posters and articles in the company newsletter. Occasionally, incentives (e.g., T-shirts, books and other prizes) are offered for completion of the exercise and there may even be monetary awards (e.g., reduction in the employee’s contribution to health insurance premiums) for successful reduction of excess risk. Some organizations schedule meetings where employees are told about the program’s purposes and procedures and are instructed in completing the questionnaire. Some, however, simply distribute a questionnaire with written instructions to each employee (and, if included in the program, to each dependant). In some instances, one or more reminders to complete and mail the questionnaire are distributed in order to increase participation. In any case, it is important to have a designated resource person, either in the organization or with the HRA program provider, to whom questions can be directed in person or by telephone. It may be important to note that, even when the questionnaire is not completed and returned, merely reading it can reinforce information from other sources and foster a health consciousness that may favorably influence future behavior.
Many of the forms call for clinical information that the respondent may or may not have. In some organizations, the program staff actually measures height, weight, blood pressure and skin-fold thickness and collects blood and urine samples for laboratory analysis. The results are then integrated with the questionnaire responses; where such data are not entered, the computer processing program may automatically insert figures representing the “norms” for persons of the same sex and age.
Turnaround time (the time between completing the questionnaire and receiving the results) may be a significant factor in the value of the program. Most vendors promise delivery of the results in ten days to two weeks, but batch processing and post office delays may extend this period. By the time the reports are received, some participants may have forgotten how they responded and may have disassociated themselves from the process; to obviate this possibility, some vendors either return the completed questionnaire or include key responses of the individual in the report.
Reports to the Individual
The reports may vary from a single-page statement of results and recommendations to a more than 20-page brochure replete with multicolor graphs and illustrations and extended explanations of the relevance of the results and the importance of the recommendations. Some rely almost entirely on preprinted general information while in others the computer generates an entirely individualized report. In some programs where the exercise has been repeated and the earlier data have been retained, comparisons of current results with those recorded earlier are provided; this may provide a sense of gratification that can serve as further motivation for behavior modification.
A key to the success of a program is the availability of a health professional or trained counselor who can explain the importance of the findings and offer an individualized program of interventions. Such personalized counseling can be extremely useful in allaying needless anxiety that may have been generated by misinterpretation of the results, in helping individuals establish behavioral change priorities, and in referring them to resources for implementation.
Reports to the Organization
In most programs, the individual results are summarized in an aggregate report sent to the employer or sponsoring organization. Such reports tabulate the demography of the participants, sometimes by geographic location and job classification, and analyze the range and levels of health risks discovered. A number of HRA vendors include projections of the increased health care costs likely to be incurred by high-risk employees. These data are extremely valuable in designing elements for the organization’s wellness and health promotion program and in stimulating consideration of changes in job structure, work environment and workplace culture that will promote the health and well-being of the workforce.
It should be noted that the validity of the aggregate report depends on the number of employees and the level of participation in the HRA program. Participants in the program tend to be more health conscious and, when their number is relatively small, their scores may not accurately reflect the characteristics of the entire workforce.
Follow-up and Evaluation
The effectiveness of the HRA program may be enhanced by a system of follow-up to remind participants of the recommendations and encourage compliance with them. This can involve individually addressed memoranda, one-on-one counseling by a physician, nurse or health educator, or group meetings. Such follow-up is particularly important for high-risk individuals.
HRA program evaluation should start with a tabulation of the level of participation, preferably analyzed by such characteristics as age, sex, geographic location or work unit, job and educational level. Such data may identify differences in acceptance of the program that might suggest changes in the way it is presented and publicized.
Increased participation in risk-reduction elements of the wellness program (e.g., a fitness program, smoking cessation courses, stress management seminars) may indicate that HRA recommendations are being heeded. Ultimately, however, evaluation will involve determination of changes in risk status. This may involve analyzing the results of the follow-up of high-risk individuals or repetition of the program after an appropriate interval. Such data may be fortified by correlation with data such as utilization of health benefits, absenteeism or productivity measures. Appropriate recognition, however, should be given to other factors that may have been involved (e.g., bias reflecting the sort of person who returns for retest, regression to the mean, and secular trends); truly scientific evaluation of the program impact requires a randomized prospective clinical trial (Schoenbach 1987; DeFriese and Fielding 1990).
Validity and Utility of the HRA
Factors that may affect the accuracy and validity of an HRA have been discussed elsewhere (Beery et al. 1986; Schoenbach 1987; DeFriese and Fielding 1990) and will only be listed here. They represent a checklist for workplace decision makers evaluating different instruments, and include the following:
- accuracy and consistency of self-reported information
- completeness and quality of the epidemiological and actuarial data on which the risk estimates are based
- limitations of the statistical methods for calculating risk, including combining risk factors for different problems into a single composite score and the distortions produced by substituting “average” values either for missing responses in the questionnaire or for measurements not taken
- reliability of the method for calculating the benefits of risk reduction
- applicability of the same mortality calculations to the young whose death rates are low and to older individuals for whom age alone may be the most significant factor in mortality. Furthermore, the validity of the HRA when applied to populations different from those on whom most of the research has been done (i.e., women, minorities, people of different educational and cultural backgrounds) must be regarded from a critical point of view.
Questions have also been raised about the utility of the HRA based on considerations such as the following:
- The primary focus of HRA is on life expectancy. Until recently, little or no attention has been paid to factors primarily influencing morbidity from conditions that are not usually fatal but which may have an even greater impact on well-being, productivity and health-related costs (e.g., arthritis, mental disorders, and long-term effects of treatments intended to reduce specific risks). The problem is the lack of good morbidity databases for the general population, to say nothing of subgroups defined by age, sex, race or ethnicity.
- Concern has been expressed about the ill effects of anxiety generated by reports of high-risk status reflecting factors which the individual is unable to modify (e.g., age, heredity, and past medical history), and about the possibility that reports of “normal” or low-risk status may lead individuals to ignore potentially significant signs and symptoms that were not reported or which developed after the HRA was completed.
- Participation in an HRA programme is usually voluntary, but allegations of coercion to participate or to follow the recommendations have been made.
- Charges of “blaming the victim” have rightfully been levelled at employers who offer HRA as part of a health promotion programme but do little or nothing to control health risks in the work environment.
- Confidentiality of personal information is an ever-present concern, especially when an HRA is conducted as an in-house programme and abnormal findings appear to be a trigger for discriminatory actions.PP9
Evidence of the value of health-risk reduction has been accumulating. For example, Fielding and his associates at Johnson and Johnson Health Management, Inc., found that the 18,000 employees who had completed the HRA provided through their employers used preventive services at a considerably higher rate than a comparable population responding to the National Health Interview Survey (Fielding et al. 1991). A five-year study of almost 46,000 DuPont employees demonstrated that those with any of the six behavioral cardiovascular risk factors identified by an HRA (e.g., cigarette smoking, high blood pressure, high cholesterol levels, lack of exercise) had significantly higher rates of absenteeism and use of health care benefits as compared to those without such risk factors (Bertera 1991). Furthermore, applying multivariate regression models to 12 health-related measures taken mainly from an HRA allowed Yen and his colleagues at the University of Michigan Fitness Research Center to predict which employees would generate higher costs for the employer for medical claims and absenteeism (Yen, Edington and Witting 1991).
Implementing an HRA Program
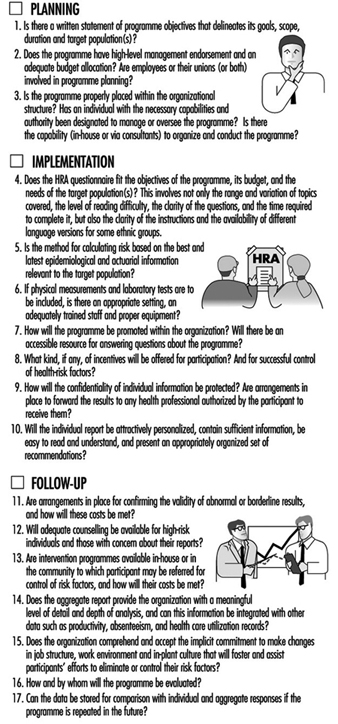
Implementing an HRA program is not a casual exercise and should not be undertaken without careful consideration and planning. The costs of an individual questionnaire and its processing may not be great but the aggregate costs to the organization may be considerable when such items as staff time for planning, implementation and follow-up, employee time for completing the questionnaires, and adjunct health-promotion programs are included. Some factors to be considered in implementation are presented in figure 1.
Figure 1. Checklist for health risk appraisal (HRA) implementation.
Should we have an HRA program?
An increasing number of companies, at least in the United States, are answering this question in the affirmative, abetted by the growing number of vendors energetically marketing HRA programs. The popular media and “trade” publications are replete with anecdotes describing “successful” programs, while in comparison there is a paucity of articles in professional journals offering scientific evidence of the accuracy of their results, their practical reliability and their scientific validity.
It seems clear that defining one’s health risk status is a necessary basis for risk reduction. But, some ask, does one need a formal exercise like the HRA to do this? By now, virtually everyone who persists in cigarette smoking has been exposed to evidence of the potential of adverse health effects, and the benefits of proper nutrition and physical fitness have been well publicized. Proponents of HRA counter by pointing out that receiving an HRA report personalizes and dramatizes the risk information, creating a “teachable moment” that can motivate individuals to take appropriate action. Further, they add, it can highlight risk factors of which the participants may have been unaware, allowing them to see just what their risk reduction opportunities are and to develop priorities for addressing them.
There is general agreement that HRA has limited value when used as a stand-alone exercise (i.e., in the absence of other modalities) and that its utility is fully realized only when it is part of an integrated health promotion program. That program should offer not only individualized explanations and counseling but also access to intervention programs that address the risk factors that were identified (these interventions may be provided in-house or in the community). Thus, the commitment to offer HRA must be broadened (and perhaps may become more costly) by offering or making available such activities as smoking cessation courses, fitness activities and nutrition counseling. Such a broad commitment should be made explicitly in the statement of objectives for the program and the budget allocation requested to support it.
In planning an HRA program, one must decide whether to offer it to the entire workforce or only to certain segments (e.g., to salaried or hourly workers, to both, or to workers of specified ages, lengths of service or in specified locations or job categories); and whether to extend the program to include spouses and other dependants (who, as a rule, account for more than half of the utilization of health benefits). A critical factor is the need to secure the availability of at least one person in the organization sufficiently knowledgeable and appropriately positioned to supervise the design and implementation of the program and the performance of both the vendor and the in-house staff involved.
In some organizations in which full-scale annual medical examinations are being eliminated or offered less frequently, HRA has been offered as a replacement either alone or in combination with selected health screening tests. This strategy has merit in terms of enhancing the cost/benefit ratio of a health promotion program, but sometimes it is based not so much on the intrinsic value of the HRA but on the desire to avoid the ill-will that might be generated by what could be perceived as elimination of an established employee benefit.
Conclusion
Despite its limitations and the paucity of scientific research that confirms the claims for its validity and utility, the use of HRA continues to grow in the United States and, much less rapidly, elsewhere. DeFriese and Fielding, whose studies have made them authorities on HRA, see a bright future for it based on their prediction of new sources of risk-relevant information and new technological developments such as improvements in computer hardware and software that will permit direct computer entry of questionnaire responses, allow modeling of the effects of changes in health behavior, and produce more effective full-color reports and graphics (DeFriese and Fielding 1990).
HRA should be used as an element in a well-conceived, continuing program of wellness or health promotion. It conveys an implicit commitment to provide activities and changes in the workplace culture that offer opportunities to help control the risk factors it will identify. Management should be aware of such a commitment and be willing to make the requisite budget allocations.
While much research remains to be done, many organizations will find HRA a useful adjunct to their efforts to improve the health of their employees. The implicit scientific authority of the information it provides, the use of computer technology, and the personalized impact of the results in terms of chronological versus risk age seem to enhance its power to motivate participants to adopt healthy, risk-reducing behaviors. Evidence is accumulating to show that employees and dependants who maintain healthy risk profiles have less absenteeism, demonstrate enhanced productivity, and use less medical care, all of which have a positive effect on the organization’s “bottom line”.