Introduction
Awareness of the adverse effects associated with cigarette smoking has increased since the 1960s when the first US Surgeon General’s report on this topic was released. Since that time, attitudes towards cigarette smoking have steadily grown towards the negative, with warning labels being required on cigarette packages and advertisements, bans on television advertising of cigarettes in some countries, the institution of non-smoking areas in some public places and the complete prohibition of smoking in others. Well-founded public health messages describing the dangers of tobacco products are increasingly widespread despite the tobacco industry’s attempts to deny that a problem exists. Many millions of dollars are spent each year by people trying to “kick the habit”. Books, tapes, group therapy, nicotine gum and skin patches, and even pocket computers have all been used with varying degrees of success in aiding those with nicotine addiction. Validation of the carcinogenic effects of passive, “second-hand” smoking has added impetus to the growing efforts to control the use of tobacco.
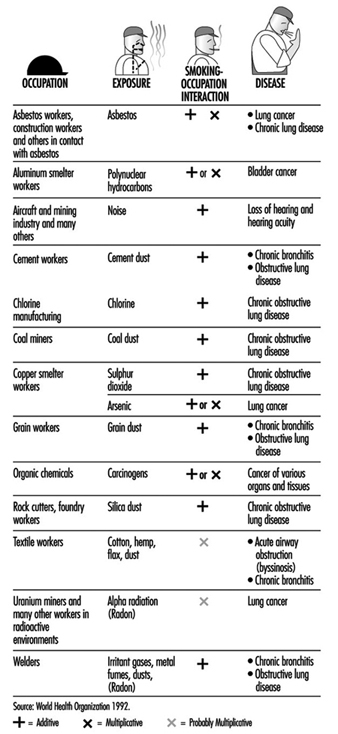
With this background, it is natural that smoking in the workplace should become a growing concern for employers and employees. On the most basic level, smoking represents a fire hazard. From a productivity standpoint, smoking represents either a distraction or an annoyance, depending on whether the employee is a smoker or a non-smoker. Smoking is a significant cause of morbidity in the workforce. It represents a drain in productivity in the form of the loss of work days due to illness, as well as a financial drain on an organization’s resources in terms of health-related costs. Furthermore, smoking has either an additive or multiplicative interaction with environmental hazards found in certain workplaces increasing significantly the risk of many occupational diseases (figure 1).
Figure 1. Examples of interactions between occupation and cigarette smoking causing disease.
This article will concern itself with the rationale for smoking control in the workplace and suggest a practical attitude and approach to managing it, recognizing that mere exhortation is not enough. At the same time, the terrible, addictive nature of nicotine and the human difficulties associated with quitting will not be underestimated. One hopes that it represents a more realistic approach to this complicated problem than some of those taken in the past.
Smoking in the Workplace
Organizations are increasingly associating unhealthy habits such as smoking with higher operating costs, and employers are taking measures to reduce the excess costs associated with employees who smoke. People who smoke one or more packs of cigarettes a day account for 18% higher medical claim costs than non-smokers, according to a study of the impact of various lifestyle risks compiled by the Ceridian Corporation, a technology services company based in Minneapolis, Minnesota. Heavy smokers spend 25% more days as inpatients in hospitals and are 29% more likely than non-smokers to have annual health care claims costs that exceed US$5,000, the study shows (Lesmes 1993).
The impact of smoking on the health of the population and the health care system is unparalleled (US Department of Health and Human Services 1989). According to the World Health Association (1992), tobacco kills at least 3 million people each year worldwide: in countries where smoking has been a long-established behavior, it is responsible for about 90% of all lung cancer deaths; 30% of all cancers; over 80% of cases of chronic bronchitis and emphysema; and some 20 to 25% of coronary heart disease and stroke deaths. Numerous other adverse health conditions, including respiratory diseases, peptic ulcers and pregnancy complications, are also attributable to smoking. Smoking remains the leading cause of avoidable death in many countries, so pervasive that it is responsible for about one sixth of deaths from all causes in the United States, for example (Davis 1987).
The combined effect of smoking and occupational hazards has been demonstrated by the significant differences in morbidity of smokers and non-smokers in many occupations. The interaction of the two types of hazards increases the risk of many diseases, particularly the chronic obstructive pulmonary diseases, lung cancer, cardiovascular diseases, as well as disabilities (figure 1).
Well-recognized complications resulting from exposure to tobacco-related hazards are outlined in great detail throughout the technical literature. Recent attention has focused on the following:
- Female risks. Changes in oestrogen metabolism, menstrual disorders, early menopause, delayed conception or infertility, cancer of the cervix.
- Maternal and pregnancy risks. Spontaneous abortion, ectopic pregnancy, placental irregularities, placenta praevia, abruptio placentae, vaginal bleeding, foetal mortality, preterm birth, retardation of foetal development, low birth weight, congenital anomalies and chronic hypoxia.
- Childhood complications. Increased neonatal mortality, sudden infant death syndrome (SIDS), impaired physical and intellectual development.
Environmental Tobacco Smoke (ETS)
Tobacco smoking is not only dangerous to the smoker but to non-smokers as well. ETS (“passive smoking” and “second-hand smoke”) is a unique risk for people, such as office workers, working in a closed environment. In developed countries, the World Health Organization (1992) points out, tobacco smoke is the most common pollutant of indoor air and is usually present at higher concentrations than other air pollutants. Besides the acute effects of eye and throat irritation, ETS increases the risk of lung cancer and possibly of cardiovascular disease. It is particularly troublesome to individuals with pre-existing health conditions, such as asthma, bronchitis, cardiovascular disease, allergies and upper respiratory infections, and also is a vexatious challenge to those who have recently given up smoking and are struggling to maintain their abstinence.
The US National Institute for Occupational Safety and Health, NIOSH, concluded that (1991):
- ETS is a potential carcinogen.
- Exposure to ETS should be reduced to the lowest possible concentration.
- Employers should minimize occupational exposure to ETS by using all available control measures.
- Worker exposure to ETS is most efficiently and completely controlled by simply eliminating tobacco smoke from the workplace.
- Employers should prohibit smoking at the workplace and provide sufficient disincentives for those who do not comply.
Except where legislation has mandated the smoke-free workplace, the protection of non-smoking employees from the health risks associated with exposure to ETS remains a formidable challenge for many public and private sector employees. Smokers, with encouragement from the tobacco industry, have maintained that continuation of smoking is inherently an individual right, despite the fact that eliminating tobacco smoke from the workplace has required innovations in ventilation engineering and expense by the employer. Legal precedents have established a clear duty for employers to provide workplaces free from hazards such as ETS and courts of law in some countries have found employers liable for the adverse health effects of ETS exposure on the job.
Surveys of public knowledge and attitudes about the risks of ETS and the desirability of workplace smoking restrictions show widespread concern about this sort of exposure and increasingly strong support for significant restrictions among both non-smokers and smokers (American Lung Association 1992). Governments have adopted an increasing number of ordinances and regulations limiting smoking in public and private workplaces (Corporate Health Policies Group 1993).
Impact of Smoking on Employers’ Costs
Historically, employers’ efforts to reduce smoking in the workplace have been driven by issues of cost and productivity losses related to smoking behavior. A number of studies have compared employers’ costs associated with smoking and non-smoking employees. For example, in one study of employees in a large-scale group health insurance plan, tobacco users had higher average outpatient medical care costs ($122 versus $75), higher average insured medical costs ($1,145 versus $762), more hospital admissions per 1,000 employees (174 versus 76), more hospital days per 1,000 employees (800 versus 381), and longer average lengths of hospital stay (6.47 versus 5.03 days) (Penner and Penner 1990).
Another study, undertaken over a period of three and one-half years by the Dow Chemical Company and covering 1,400 employees (Fishbeck 1979), showed that smokers were absent 5.5 days more per year than non-smokers, costing Dow over $650,000 annually in excess wages alone. This figure did not include extra health care costs. In addition, smokers had 17.4 disability days per year compared with 9.7 days for non-smokers. Smokers also had twice the frequency of circulatory disease problems, three times more pneumonia, 41% more bronchitis and emphysema, and 76% more respiratory diseases of all types. For every two non-smokers who died during the study period, seven smokers died.
A study by the United States Steel Corporation found that employees who smoke have more work-loss days than those who have never smoked. It also showed that in every age group, as the number of cigarettes smoked per day by confirmed smokers increased, so did the number of absences due to illness. Additionally, male smokers of more than two packs per day had nearly twice as much absence as their non-smoking counterparts. In a study on how much individual behavioral risk factors contribute to the total disability and health care costs of a large, multi-location industrial company, smokers had 32% greater absenteeism and $960 excess average annual illness costs per employee (Bertera 1991).
The annual report of the Kansas State Employees Health Care Commission found that smokers incurred 33% more hospital admissions than non-smokers (106.5 versus 71.06 hospital admissions per 1,000 persons). The total average claim payment per employee was $282.62 more for smokers than for non-smokers.
Results like these have prompted some US employers to add a “surcharge” to their smoking employees’ share of group health insurance premiums to cover the higher claims payments associated with this population. The Resinoid Engineering Corporation stopped hiring smokers in its Ohio plant because their health care claims were $6,000 higher per employee per year for smokers than for non-smokers; a similar move by a Chicago, Illinois company was barred because the state law prohibits discriminatory hiring on the basis of lifestyle.
Other employers, using the “carrot” rather than the “stick” approach, have offered inducements such as monetary or other types of awards to employees who successfully quit smoking. A popular approach is to refund the tuition required for participating in a smoking cessation program to those who complete the course or, more strictly, to those who remain abstinent for a defined period following the completion of the course.
In addition to increased health care costs and costs associated with lost productivity due to sickness among smokers, there are other increased costs associated with smoking, namely those arising from lost productivity during smoking breaks, higher fire and life insurance costs, and higher general cleaning costs related to smoking. For example, Air Canada identified savings of about US$700,000 per year by not having to clean ashtrays and being able to extend the frequency of deep cleaning of its planes from six to nine months after implementing its tobacco-free policy (WHO 1992). A study by Kristein (1983) designed to take into account all of the increased costs due to smoking estimated the total to be $1,300 per smoker per year (adjusted to 1993 dollars). He also discussed other areas of excess cost, including, in particular, the costs of higher levels of maintenance for computers and other sensitive equipment, and for installing and maintaining ventilation systems. Furthermore, he added that other costs result from the “inefficiency and errors based on the established literature as to the effects of higher carbon monoxide levels in smokers, eye irritation, measured lower attentiveness, cognitive and exercise capacity function”.
Smoking Policies and Regulations
In the 1980s, laws and voluntary policies to restrict smoking at the workplace increased in number and strength. Some pertain only to government worksites which, together with places of work where children are present, have often taken the lead. Others affect both government and private worksites. They are characterized by banning smoking altogether (“smoke-free” worksites); restricting smoking in common areas such as cafeterias and meeting rooms; allowing smoking only in special smoking areas; and requiring accommodation of the interests of smokers and non-smokers, with primacy given to the wishes of the latter.
Some programs regulate smoking in worksites where certain hazardous materials are present. For example, in 1976 Norway issued rules prohibiting the assignment of persons who smoke to areas where they may be exposed to asbestos. In 1988, Spain prohibited smoking in any place where the combination of smoking and occupational hazards results in greater risk to the health of workers. Spain also prohibits smoking in any worksite where pregnant women work. Other countries that have taken legislative measures to restrict smoking in the workplace include Costa Rica, Cuba, Denmark, Iceland and Israel (WHO 1992).
Increasingly, legislation restricting smoking at the worksite is part of a broader regulation covering public places. New Zealand, Norway and Sweden have enacted such legislation while Belgium, the Netherlands and Ireland have passed laws prohibiting smoking in most public places. The 1991 French law prohibits smoking in all places designed for collective use, notably schools and public transportation (WHO 1992).
In the United States and Canada, although federal agencies have adopted smoking control policies, legislation has been limited to states and provinces and to municipalities. By 1989, 45 US states had enacted laws restricting smoking in public places, while 19 states and the District of Columbia had adopted ordinances restricting smoking in private workplaces (Bureau of National Affairs 1989). The state of California has a bill pending that would totally ban smoking in all indoor employment areas and would also obligate an employer to take reasonable steps to prevent visitors from smoking (Maskin, Connelly and Noonan 1993). For some time, the Occupational Safety and Health Administration (OSHA) in the US Department of Labor has been considering the regulation of ETS in the workplace both as an independent toxicant and as a component of indoor air (Corporate Health Policies Group 1993).
Another incentive for employers to reduce smoking in the workplace comes from cases of disability stemming from exposure to ETS that have won worker’s compensation awards. In 1982, a federal appellate court found an employee eligible for disability retirement because she had been forced to work in a smoke-filled environment (Parodi vs. Veterans Administration 1982). Similarly, employees have been awarded worker’s compensation payments because of adverse reactions to tobacco smoke on the job. Indeed, William Reilly, the former administrator of the US Environmental Protection Agency (EPA) has expressed the hope that the threat of employer liability raised by the recent release of the EPA’s designation of EST as a significant health hazard would obviate the necessity of additional federal government regulations (Noah 1993).
Another factor favoring the establishment of policies curbing workplace smoking is the change in public attitudes reflecting (1) recognition of the mounting scientific evidence of the risks of cigarette smoke to smokers and non-smokers alike, (2) a decline in the prevalence of smoking, (3) a decline in the social acceptability of smoking and (4) a heightened awareness of the rights of non-smokers. The American Lung Association (1992) reported consistent increases in the overall percentage of adults who favor workplace smoking restrictions, from 81% in 1983 to 94% in 1992, while in the same period, those favoring a total ban increased from 17% to 30% and those favoring no restrictions fell from 15% to 5%.
Labor unions are also increasingly supportive of non-smoking policies (Corporate Health Policies Group 1993).
Recent US surveys have shown a marked trend towards not only increased adoption of smoking restrictions but also their increasing stringency (Bureau of National Affairs 1986, 1991). The percentage of companies with such policies rose from 36% in 1986 to 85% in 1991 while, in the same period, there was a sixteen-fold increase in the percentage with total bans or “smoke-free” policies (Bureau of National Affairs 1991; Coalition on Smoking and Health 1992).
Smoking Cessation Programs
Worksites are becoming increasingly common settings for health education and promotion efforts. Of several cited studies (Coalition on Smoking and Health 1992), one survey indicates that 35.6% of companies offer some kind of smoking cessation assistance. Another study shows that non-smoking policies may also provide environmental support to individuals attempting to quit smoking. Thus, a non-smoking policy may also be considered an important element in a smoking cessation program.
Smoking cessation methods are divided into two categories:
- Unassisted methods, which include going “cold turkey” (i.e., just stopping without recourse to any special techniques); gradually reducing the number of cigarettes smoked per day; using low-tar or low-nicotine cigarettes; quitting with friends, relatives or acquaintances; using special cigarette filters or holders; using other nonprescription products; or substituting another tobacco product for cigarettes (snuff, chewing tobacco, pipes or cigars).
- Assisted methods, which include attending a programme or a course with or without a fee; consulting a mental health professional; hypnosis; acupuncture; and using nicotine gum or nicotine skin patches.
The efficacy of these various methods is the subject of much controversy largely due to the difficulties and costs associated with long-term follow-up and the obvious self-interest of the vendors of programs and products. Another serious limitation relates to the ability to verify the smoking status of program participants (Elixhauser 1990). Saliva tests measuring cotinine, a metabolite of nicotine, are an effective objective indicator of whether an individual has recently been smoking, but they are moderately complicated and expensive and, thus. not widely used. Accordingly, one is forced to depend on the questionable reliability of the individual’s self-reports of success in either quitting or cutting down on the amount smoked. These problems make it extremely difficult to compare various methods to one another or even to make proper use of a control group.
Despite these encumbrances, two general conclusions can be drawn. First, those individuals most successful in permanently quitting do so largely on their own, often after numerous attempts to do so. Secondly, barring the individual “cold turkey” approach, multiple interventions in combination appear to enhance the effectiveness of efforts to quit, especially when accompanied by support in maintaining abstinence and reinforcement of the quit-smoking message (Bureau of National Affairs 1991). The importance of the latter is confirmed by a study (Sorenson, Lando and Pechacek 1993) which found that the highest overall cessation rate was achieved by smokers who worked among a high proportion of non-smokers and who were frequently asked not to smoke. Still, the six-month quitting rate was only 12%, compared to a rate of 9% among the control group. Obviously, cessation programs in general must not be expected to produce dramatic positive results but, instead, must be viewed as requiring a persistent, patient effort towards the goal of quitting smoking.
Some workplace smoking cessation programs have been overly simple or naive in their approach, while others have lacked long-term determination and commitment. Companies have tried everything from simply restricting smoking to specified areas of the worksite or autocratically making a sudden announcement banning all smoking, to providing expensive and intensive (but often short-lived) programs offered by outside consultants. The problem and the challenge is to successfully accomplish the transition to a smoke-free workplace without sacrificing worker morale or productivity.
The following section will present an approach that incorporates our present knowledge of the difficulties individuals face in quitting and the employer attitude necessary to best achieve the goal of non-smoking in the workplace.
An Alternative Approach to Achievinga Smoke-free Workplace
Past experience has shown that simply offering smoking cessation programs to volunteers does not advance the goal of a smoke-free workplace because the majority of smokers will not participate in them. At any given time, only about 20% of smokers are ready to quit and only a minority of this group will sign up for a cessation program. For the other 80% of smokers who don’t want to quit or who don’t believe they can quit when the enterprise goes smoke-free, instituting a ban on smoking in the workplace will just tend to cause them to move their smoking during working hours “out the door” to a designated smoking area or somewhere outside the building. This “80% problem”—the problem that 80% of the smokers are not going to be helped or even consider participating in the program if only smoking cessation programs are offered—has numerous consequent negative effects on employee relations, productivity, operating costs and health-related costs.
An alternative, and successful, approach has been developed by Addiction Management Systems, an organization based in Toronto, Canada. This approach is based on the knowledge that change and the modification of behavior is a process which can be planned and managed using organizational and behavioral techniques. It involves dealing with control of smoking in the workplace in the same way as any other major policy or procedural change for the company, with informed decisions made by management after input from representative employee groups. A controlled change is made by supporting those managers responsible for overseeing the change and making all smokers positive participants in the change by providing them with the “tools” to accommodate to the new non-smoking environment without requiring them to quit smoking. The focus is on communications and team-building by involving and educating all of those affected by the policy change.
The actual process of the transition to a smoke-free workplace begins with the announcement of the policy change and the start of a transition period of several months’ duration before the policy goes into effect. In behavioral terms, the upcoming policy change to becoming smoke-free acts as a “stimulus to change” and creates a new environment in which it is in the interest of all smokers to seek a means of successfully adapting to the new environment.
The announcement of this policy change is followed by a communication program aimed at all employees, but focused on two important groups: the supervisors who must implement and oversee the new non-smoking policy, and the smokers who need to learn to adapt to the new environment. An important part of the communication program is making smokers aware that, while they will not be required to quit smoking unless they so choose, they must nonetheless adhere to the new policy forbidding smoking in the workplace during the workday. All employees receive the communications about the policy and upcoming changes.
During the transition period, supervisors are provided with communications materials and a training program to enable them to understand the policy change and to anticipate questions, problems or other concerns which may come up during or after the change. As the group most directly affected when the policy goes into effect, smokers are consulted about their specific needs and also receive their own training program. The special focus of the latter is to acquaint them with a voluntary self-help “smoking control” program that contains a number of options and choices which allow the smokers to understand the program and to learn to modify their smoking behavior in order to refrain from smoking during the workday as required once the new policy goes into effect. This allows each smoker to personalize his or her own program, with “success” defined by the individual, whether it be quitting altogether or just learning how not to smoke during the workday. Accordingly, resentment is neutralized and the change to the smoke-free workplace becomes a positive motivating factor for the smoker.
The end result of this approach is that when the effective date of the policy arrives, the transition to a smoke-free workplace becomes a “non-event”—it simply happens, and it is successful. The reason this occurs is that the groundwork has been laid, the communications have been carried out, and all of those persons involved understand what needs to happen and have the means to make a successful transition.
What is important from an organizational standpoint is that the change is one which tends to be self-maintaining, with only minimal ongoing input from management. Also important is the effect that once successful in learning to “manage” their smoking problem, the smokers in the “80% group” tend to build on their success and to progress towards quitting completely. Finally, in addition to the beneficial effect on the well-being and morale of employees who are positively involved in the transition to a smoke-free environment, the organization accrues over time benefits in terms of higher productivity and reduced costs related to health care.
Evaluation of Effectiveness
In evaluating the effectiveness of the program, there are two separate criteria that must be considered. The first is whether the workplace truly becomes a smoke-free environment. Success with respect to this goal is relatively easy to measure: it is based on regular supervisors’ reports on violations of the policy within their work areas; monitoring complaints from other employees; and the results of unannounced spot checks of the workplace to reveal the presence or absence of cigarette butts, ashes and smoke-laden air.
The second measure of success, and more difficult to determine, is the number of employees who actually quit smoking and maintain their smoke-free status. While perhaps the most practical position to take is to be concerned only with worksite smoking, such a limited success will bring about fewer long-term benefits, especially with respect to decreasing illness and health care costs. While periodic mandatory saliva tests for cotinine to identify those who continue to smoke would be the best and most objective method for evaluating long-term program success, this is not only complicated and expensive but also is fraught with numerous legal and ethical questions regarding employee privacy. A compromise is the use of annual or semi-annual anonymous questionnaires that ask how individuals’ smoking habits have changed and how long abstinence from smoking has been maintained and that, at the same time, probe changes in employees’ attitudes toward the policy and the program. Such questionnaires have the added advantage of being a means of reinforcing the non-smoking message and of keeping the door open for those still smoking to reconsider dropping the habit.
A final long-term outcome evaluation involves monitoring employee absenteeism, illnesses and health care costs. Any changes would at first be subtle, but over a number of years they should be cumulatively significant. Death benefits paid prior to normal retirement age could be another long-term reflection of the success of the program. Of course, it is important to adjust such data for such factors as changes in the work force, employee characteristics such as age and sex, and other factors affecting the organization. Analysis of these data is manifestly subject to the rules of statistics and would probably be valid only in organizations with a large and stable workforce and adequate data collection, storage and analysis capabilities.
Smoking Control Worldwide
There is a growing worldwide unwillingness to continue to bear the burdens of cigarette smoking and nicotine addiction in terms of their effects on human well-being and productivity, on health and health care costs, and on the economic health of work organizations and nations. This is exemplified by the expanding participation in World No-Tobacco Day that has been spearheaded by the World Health Organization in May of each year since 1987 (WHO 1992).
The aim of this event is not only to ask people to stop smoking for one day but also to trigger interest in controlling smoking among public and private organizations and to promote pressure for the passage of laws, by-laws or regulations advancing the cause of tobacco-free societies. It is also hoped that the relevant agencies will be stimulated to initiate research on specific themes, publish information or initiate action. To this end, each World No-Tobacco Day is assigned a specific theme (table 1); of particular interest to readers of this article is the 1992 Day which addressed “Tobacco-free workplaces: safer and healthier”.
Table 1. Themes of "World No-Tobacco Days"
1992 Tobacco Free Workplaces: safer and healthier
1993 Health Services: our window to a tobacco-free world
1994 The Media and Tobacco: getting the health message across
1995 The Economics of Tobacco: tobacco costs more than you think
1996 Sports and the Arts
1997 United Nations and Specialized Agencies against Tobacco
A problem beginning to be recognized is the increase in cigarette smoking in developing countries where, prompted by the marketing blandishments of the tobacco industry, populations are being encouraged to view smoking as a hallmark of social advancement and sophistication.
Conclusion
The adverse effects of cigarette smoking on individuals and societies are increasingly being recognized and understood (except by the tobacco industry). Nevertheless, smoking continues to enjoy social acceptability and widespread use. A special problem is that many young people become addicted to nicotine years before they are old enough to work.
The workplace is an exceptionally useful arena for combating this health hazard. Workplace policies and programs can have a strong positive influence over the behavior of employees who smoke, abetted by peer pressure from non-smoking coworkers. The wise organization will not only appreciate that control of workplace smoking is something that serves its own self-interest in terms of legal liabilities, absenteeism, production and health-related costs, but will also recognize that it can be a matter of life and death for its employees.