Introduction
Throughout history human beings have sought to alter their thoughts, feelings and perceptions of reality. Mind-altering techniques, including reduction of sensory input, repetitive dancing, sleep deprivation, fasting and prolonged meditation have been employed in many cultures. However, the most popular method for producing mood and perception changes has been the use of mind-altering drugs. Of the 800,000 species of plants on earth, about 4,000 are known to produce psychoactive substances. Approximately 60 of these have been used consistently as stimulants or intoxicants (Malcolm 1971). Examples are coffee, tea, the opium poppy, coca leaf, tobacco and Indian hemp, as well as those plants from which beverage alcohol is fermented. In addition to naturally occurring substances, modern pharmaceutical research has produced a range of synthetic sedatives, opiates and tranquillizers. Both plant-derived and synthetic psychoactive drugs are commonly used for medical purposes. Several traditional substances are also employed in religious rites and as part of socialization and recreation. In addition, some cultures have incorporated drug use into customary workplace practices. Examples include the chewing of coca leaves by Peruvian Indians in the Andes and the smoking of cannabis by Jamaican sugar cane workers. The use of moderate amounts of alcohol during farm labour was an accepted practice in the past in some Western societies, for example in the United States in the eighteenth century and the early nineteenth century. More recently, it was customary (and even required by some unions) for employers of battery burners (workers who incinerate discarded storage batteries to salvage their lead content) and house painters using lead-based paints to provide each worker with a daily bottle of whisky to be sipped during the work day in the belief—an erroneous one—that it would prevent lead poisoning. In addition, drinking has been a traditional part of certain occupations, as, for example, among brewery and distillery salespeople. These sales representatives are expected to accept the hospitality of the tavern owner on completing their order-taking.
Customs that dictate alcohol use persist in other work too, such as the “three martini” business lunch, and the expectation that groups of workers will stop at the neighbourhood pub or tavern for a few convivial rounds of drinks at the end of the work day. This latter practice poses a particular hazard for those who then drive home.
Mild stimulants also remain in use in contemporary industrial settings, institutionalized as coffee and tea breaks. However, several historical factors have combined to make the use of psychoactive substances at the workplace a major social and economic problem in contemporary life. The first of these is the trend towards employing increasingly sophisticated technology in today’s workplace. Modern industry requires alertness, unimpaired reflexes and accurate perception on the part of workers. Impairments in these areas can cause serious accidents on one hand and can interfere with the accuracy and efficiency of work on the other. A second important trend is the development of more powerful psychoactive drugs and more rapid means of drug administration. Examples are the intranasal or intravenous administration of cocaine and the smoking of purified cocaine (“freebase” or “crack” cocaine). These methods, delivering much more powerful cocaine effects than the traditional chewing of coca leaves, have greatly increased the dangers of cocaine use on the job.
Effects of Alcohol and Other Drug Usein the Workplace
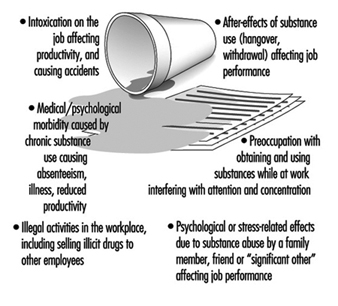
Figure 1 summarizes the various ways in which the use of psychoactive substances can influence the functioning of employees in the workplace. Intoxication (the acute effects of drug ingestion) is the most obvious hazard, accounting for a wide variety of industrial accidents, for example vehicle crashes due to alcohol-impaired driving. In addition, the impaired judgement, inattention and dulled reflexes produced by alcohol and other drugs also interferes with productivity at every level, from the board room to the production line. Furthermore, workplace impairment due to drug and alcohol use often lasts beyond the period of intoxication. The alcohol-related hangover may produce headache, nausea and photophobia (light sensitivity) for 24 to 48 hours after the last drink. Workers suffering from alcohol dependence may also undergo alcohol withdrawal symptoms on the job, with shaking, sweating and gastrointestinal disturbances. Heavy cocaine use is characteristically followed by a withdrawal period of depressed mood, low energy and apathy, all of which interfere with work. Both intoxication and the after-effects of drug and alcohol use also characteristically lead to lateness and absenteeism. In addition, the chronic use of psychoactive substances is implicated in a wide range of health problems that increase society’s medical costs and time lost from work. Cirrhosis of the liver, hepatitis, AIDS and clinical depression are examples of such problems.
Figure 1. Ways in which alcohol/drug use can cause problems in the workplace.
Workers who become heavy, frequent users of alcohol or other drugs (or both) may develop a dependency syndrome, which characteristically includes a preoccupation with obtaining the drug or the money needed to buy it. Even before other drug or alcohol-induced symptoms begin to interfere with work, this preoccupation may already have started to impair productivity. Furthermore, as a result of the need for money, the employee may resort to stealing items from the workplace or selling drugs on the job, creating another set of serious problems. Finally, the close friends and family members of drug and alcohol abusers (often referred to as “significant others”) are also affected in their ability to work by anxiety, depression and a variety of stress-related symptoms. These effects may even carry over into later generations in the form of residual work problems in adults whose parents suffered from alcoholism (Woodside 1992). Health expenditures for employees with serious alcohol problems are about twice as high as health costs for other employees (Institute for Health Policy 1993). Health costs for members of their families are also increased (Children of Alcoholics Foundation 1990).
Costs to Society
For the above reasons and others, drug and alcohol use and abuse have created a major economic burden on many societies. For the United States, the societal cost estimated for the year 1985 was US$70.3 billion (thousand millions) of for alcohol and $44 billion for other drugs. Of the total alcohol-related costs, $27.4 billion (about 39% of the total) was attributed to lost productivity. The corresponding figure for other drugs was $6 billion (about 14% of the total) (US Department of Health and Human Services 1990). The remainder of the cost accruing to society as a result of drug and alcohol abuse includes the costs for the treatment of medical problems (including AIDS and alcohol-related birth defects), vehicle crashes and other accidents, crime, property destruction, incarceration and the social welfare costs of family support. Although some of these costs may be attributed to the socially acceptable use of psychoactive substances, the vast majority are associated with drug and alcohol abuse and dependence.
Drug and Alcohol Use, Abuse and Dependence
A simple way to categorize the patterns of use of psychoactive substances is to distinguish among non-hazardous use (use in socially accepted patterns that neither create harm nor involve a high risk of harm), drug and alcohol abuse (use in high risk or harm-producing ways) and drug and alcohol dependence (use in a pattern characterized by signs and symptoms of the dependence syndrome).
Both the International Classification of Diseases, 10th edition (ICD-10) and the Diagnostic and Statistical Manual of the American Psychiatric Association, 4th edition (DSM-IV) specify diagnostic criteria for drug and alcohol-related disorders. The DSM-IV uses the term abuse to describe patterns of drug and alcohol use that cause impairment or distress, including interference with work, school, home or recreational activities. This definition of the term is also meant to imply recurrent use in physically hazardous situations, such as repeatedly driving while impaired by drugs or alcohol, even if no accident has yet occurred. The ICD-10 uses the term harmful use instead of abuse and defines it as any pattern of drug or alcohol use that has caused actual physical or psychological harm in an individual who does not meet the diagnostic criteria for drug or alcohol dependence. In some cases drug and alcohol abuse is an early or prodromal stage of dependence. In others, it constitutes an independent pattern of pathological behaviour.
Both the ICD-10 and the DSM-IV use the term psychoactive substance dependence to describe a group of disorders in which there is both interference with functioning (in job, family and social arenas) and an impairment in the individual’s ability to control the use of the drug. With some substances, a physiological dependence develops, with increased tolerance to the drug (higher and higher doses required to obtain the same effects) and a characteristic withdrawal syndrome when use of the drug is abruptly discontinued.
A definition recently prepared by the American Society of Addiction Medicine and the National Council on Alcoholism and Drug Dependence of the United States describes the features of alcoholism (a term usually employed as a synonym for alcohol dependence) as follows:
Alcoholism is a primary, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking, most notably denial. Each of these symptoms may be continuous or periodic. (Morse and Flavin 1992)
The definition then goes on to explain the terms used, for example, that the qualification “primary” implies that alcoholism is a discrete disease rather than a symptom of some other disorder, and that “impaired control” means that the affected person cannot consistently limit the duration of a drinking episode, the amount consumed or the resulting behaviour. “Denial” is described as referring to a complex of physiological, psychological and culturally-influenced manoeuvres that decrease the recognition of alcohol-related problems by the affected individual. Thus, it is common for persons suffering from alcoholism to regard alcohol as a solution to their problems rather than as a cause.
Drugs capable of producing dependence are commonly divided into several categories, as listed in table 1. Each category has both a specific syndrome of acute intoxication and a characteristic combination of destructive effects related to long-term heavy use. Although individuals often suffer from dependency syndromes relating to a single substance (e.g., heroin), patterns of multiple drug abuse and dependence are also common.
Table 1. Substances capable of producing dependence.
|
Category of drug |
Examples of general effects |
Comments |
|
Alcohol (e.g., beer, wine, spirits) |
Impaired judgement, slowed reflexes, impaired motor function, somnolence, coma-overdose may be fatal |
Withdrawal may be severe; danger to foetus if used excessively in pregnancy |
|
Depressants (e.g., sleeping medicines, sedatives, some tranquillizers) |
Inattention, slowed reflexes, depression, impaired balance, drowsiness, coma-overdose may be fatal |
Withdrawal may be severe |
|
Opiates (e.g., morphine, heroin, codeine, some prescription pain medications) |
Loss of interest, “nodding”-overdose may be fatal. Subcutaneous or intravenous abuse may spread Hepatitis B, C and HIV/AIDS via needle-sharing |
|
|
Stimulants (e.g., cocaine, amphetamines) |
Elevated mood, overactivity, tension/anxiety, rapid heartbeat, constriction of blood vessels |
Chronic heavy use may lead to paranoid psychosis. Use by injection may spread Hepatitis B, C and HIV/AIDS via needle-sharing |
|
Cannabis (e.g., marijuana, hashish) |
Distorted time sense, impaired memory, impaired coordination |
|
|
Hallucinogens (e.g., LSD (lysergic acid diethylamide), PCP (phencyclidine), mescaline) |
Inattention, sensory illusions, hallucinations, disorientation, psychosis |
Does not produce withdrawal symptoms but users may experience “flashbacks” |
|
Inhalants (e.g., hydrocarbons, solvents, gasoline) |
Intoxication similar to alcohol, dizziness, headache |
May cause long- term organ damage (brain, liver, kidney) |
|
Nicotine (e.g., cigarettes, chewing tobacco, snuff) |
Initial stimulant, later depressant effects |
May produce withdrawal symptoms. Implicated in causing a variety of cancers, cardiac and pulmonary diseases |
Drug and alcohol-related disorders often affect the employee’s family relationships, interpersonal functioning and health before obvious work impairments are noticed. Therefore, effective workplace programmes cannot be limited to efforts at achieving drug and alcohol abuse prevention on the job. These programmes must combine employee health education and prevention with adequate provisions for intervention, diagnosis and rehabilitation as well as long-term follow-up of affected employees after their reintegration into the workforce.
Approaches to Drug and Alcohol-relatedProblems in the Workplace
Concern over the serious productivity losses caused by drug and alcohol abuse and dependence have led to several related approaches on the part of governments, labour and industries. These approaches include so-called “drug-free workplace policies” (including chemical testing for drugs) and employee assistance programmes.
One example is the approach taken by the United States Military Services. In the early 1980s successful anti-drug policies and drug testing programmes were established in each branch of the US military. As a result of its programme, the US Navy reported a dramatic fall in the proportion of random urine tests of its personnel that were positive for illicit drugs. The positive test rates for those under age 25 fell from 47% in 1982, to 22% in 1984, to 4% in 1986 (DeCresce et al. 1989). In 1986 the President of the United States issued an executive order requiring that all federal government employees refrain from illegal drug use, whether on or off the job. As the largest single employer in the United States, with over two million civilian employees, the federal government thereby assumed the lead in developing a national drug-free workplace movement.
In 1987, following a fatal railway accident linked to marijuana abuse, the US Department of Transportation ordered a drug and alcohol testing programme for all transportation workers, including those in private industry. Managements in other work settings have followed suit, establishing a combination of supervision, testing, rehabilitation and follow-up in the workplace that has shown consistently successful results.
The case-finding, referral and follow-up component of this combination, the employee assistance programme (EAP), has become an increasingly common feature of employee health programmes. Historically, EAPs evolved from more narrowly-focused employee alcoholism programmes that had been pioneered in the United States during the 1920s and expanded more rapidly in the 1940s during and after the Second World War. Current EAPs are customarily established on the basis of a clearly enunciated company policy, often developed by joint agreement between management and labour. This policy includes rules of acceptable workplace behaviour (e.g., no alcohol or illicit drugs) and a statement that alcoholism and other drug and alcohol dependence are considered treatable diseases. It also includes a statement of confidentiality, guaranteeing the privacy of sensitive personal employee information. The programme itself conducts preventive education for all employees and special training for supervisory personnel in identifying job performance problems. Supervisors are not expected to learn to diagnose drug and alcohol-related problems. Rather, they are trained to refer employees who show problematic job performance to the EAP, where an assessment is made and a plan of treatment and follow-up is formulated, as appropriate. Treatment is usually provided by community resources outside the workplace. EAP records are kept confidentially as a matter of company policy, with reports relating only to the subject’s degree of cooperation and general progress released to management except in cases of imminent danger.
Disciplinary action is usually suspended as long as the employee cooperates with treatment. Self-referrals to the EAP are also encouraged. EAPs that help employees with a wide range of social, mental health and drug and alcohol-related problems are known as “broad-brush” programmes to distinguish them from programmes that focus only on drug and alcohol abuse.
There is no question of the appropriateness of employers’ prohibiting the use of alcohol and other drugs during working hours or in the workplace. However, the right of the employer to prohibit the use of such substances away from the workplace during off hours has been disputed. Some employers have said, “I don’t care what employees do off the job as long as they report on time and are able to perform adequately,” and some labour representatives have opposed such a prohibition as an intrusion on the worker’s privacy. Yet, as noted above, excess use of drugs or alcohol during off-hours can affect work performance. This is recognized by airlines when they prohibit all use of alcohol by air crews during a specified number of hours prior to flight time. Although the prohibitions of alcohol use by an employee before flying or driving a vehicle are generally accepted, blanket prohibitions of tobacco, alcohol or other drug use outside of the workplace have been more controversial.
Workplace drug testing programmes
Along with EAPs, increasing numbers of employers have also instituted workplace drug testing programmes. Some of these programmes test only for illicit drugs, while others include breath or urine testing for alcohol. Testing programmes may involve any of the following components:
- pre-employment testing
- random testing of employees in sensitive positions (e.g., nuclear reactor operators, pilots, drivers, operators of heavy machinery)
- testing “for cause” (e.g., after an accident or if a supervisor has good reason to suspect that the employee is intoxicated)
- testing as part of the follow-up plan for an employee returning to work after treatment for drug or alcohol abuse or dependence.
Drug testing programmes create special responsibilities for those employers who undertake them (New York Academy of Medicine 1989). This is discussed more fully under “Ethical Issues” in the Encyclopaedia. If employers rely on urine tests in making employment and disciplinary decisions in drug-related cases, the legal rights of both employers and employees must be protected by meticulous attention to collection and analysis procedures and to the interpretation of laboratory results. Specimens must be collected carefully and labelled immediately. Because drug users may attempt to evade detection by substituting a sample of drug-free urine for their own or by diluting their urine with water, the employer may require that the specimen be collected under direct observation. Because this procedure adds time and expense to the procedure it may be required only in special circumstances rather than for all tests. Once the specimen is collected, a chain-of-custody procedure is followed, documenting each movement of the specimen to protect it from loss or misidentification. Laboratory standards must ensure specimen integrity, with an effective programme of quality control in place, and staff qualifications and training must be adequate. The test used must employ a cut-off level for the determination of a positive result that minimizes the possibility of a false positive. Finally, positive results found by screening methods (e.g., thin-layer chromatography or immunological techniques) should be confirmed to eliminate false results, preferably by the techniques of gas chromatography or mass spectrometry, or both (DeCresce et al. 1989). Once a positive test is reported, a trained occupational physician (known in the United States as a medical review officer) is responsible for its interpretation, for example, ruling out prescribed medication as a possible reason for the test results. Performed and interpreted properly, urine testing is accurate and may be useful. However, industries must calculate the benefit of such testing in relationship to its cost. Considerations include the prevalence of drug and alcohol abuse and dependence in the prospective workforce, which will influence the value of pre-employment testing, and the proportion of the industry’s accidents, productivity losses and medical benefit costs related to the abuse of psychoactive substances.
Other methods of detecting drug and alcohol-related problems
Although urine testing is an established screening method for detecting drugs of abuse, there are other methods available to EAPs, occupational physicians and other health professionals. Blood alcohol levels may be estimated by means of breath testing. However, a negative chemical test of any kind does not rule out a drug or alcohol problem. Alcohol and some other drugs are metabolized rapidly and their aftereffects may continue to impair work performance even when the drugs are no longer detectable on a test. On the other hand, the metabolites produced by the human body after the ingestion of certain drugs may remain in the blood and urine for many hours after the drug’s effects and aftereffects have subsided. A positive urine test for drug metabolites therefore does not necessarily prove that the employee’s work is drug-impaired.
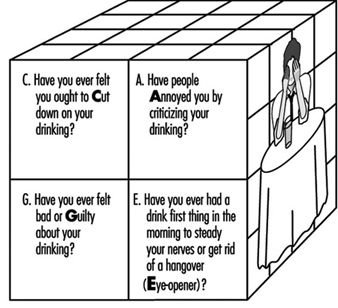
In making an assessment of employee drug and alcohol-related problems a variety of clinical screening instruments are used (Tramm and Warshaw 1989). These include pencil-and-paper tests, such as the Michigan Alcohol Screening Test (MAST) (Selzer 1971), the Alcohol Use Disorders Identification Test (AUDIT) developed for international use by the World Health Organization (Saunders et al. 1993), and the Drug Abuse Screening Test (DAST) (Skinner 1982). In addition, there are simple sets of questions that can be incorporated into history-taking, for example the four CAGE questions (Ewing 1984) illustrated in figure 2. All of these methods are used by EAPs to evaluate employees referred to them. Employees referred for job performance problems such as absences, lateness and decreased productivity on the job should additionally be evaluated for other mental health problems such as depression or compulsive gambling, which may also produce impairments in job performance and are often associated with drug and alcohol-related disorders (Lesieur, Blume and Zoppa 1986). With respect to pathological gambling, a paper-and-pencil screening test, the South Oaks Gambling Screen (SOGS) is available (Lesieur and Blume 1987).
Figure 2. The CAGE questions.
Treatment of Disorders Related to theUse of Drugs and Alcohol
Although each employee presents a unique combination of problems to the addiction treatment professional, the treatment of disorders related to drug and alcohol use usually consists of four overlapping phases: (1) identification of the problem and (as necessary) intervention, (2) detoxification and general health assessment, (3) rehabilitation, and (4) long-term follow-up.
Identification and intervention
The first phase of treatment involves confirming the presence of a problem caused by the use of drugs or alcohol (or both) and motivating the affected individual to enter treatment. The employee health programme or company EAP has the advantage of using the employee’s concern both for health and job security as motivational factors. Workplace programmes are also likely to understand the employee’s environment and his or her strengths and weaknesses, and can thus choose the most appropriate treatment facility for referral. An important consideration in making a referral for treatment is the nature and extent of workplace-based health insurance coverage for the treatment of drug and alcohol-induced disorders. Policies with coverage of the full range of inpatient and outpatient treatments offer the most flexible and effective options. In addition, the involvement of the employee’s family at the intervention stage is often helpful.
Detoxification and general health assessment
The second stage combines the appropriate treatment needed to help the employee attain a drug and alcohol-free state with a thorough evaluation of the patient’s physical, psychological, family, interpersonal and work-related problems. Detoxification involves a short period—several days to several weeks—of observation and treatment for the elimination of the drug of abuse, recovery from its acute effects, and control of any symptoms of withdrawal. While detoxification and the assessment activities are progressing, the patient and “significant others” are educated about the nature of drug and alcohol dependence and recovery. They and the patient are also introduced to the principles of self-help groups, where this modality is available, and the patient is motivated to continue in treatment. Detoxification may be carried out in an inpatient or outpatient setting, depending on the needs of the individual. Treatment techniques found useful include a variety of medications, augmented by counselling, relaxation training and other behavioural techniques. Pharmacological agents used in detoxification include drugs which can substitute for the drug of abuse to relieve withdrawal symptoms and then be gradually reduced in dosage until the patient is drug-free. Phenobarbital and the longer-acting benzodiazepines are often used this way to achieve detoxification in the case of alcohol and sedative drugs. Other medicines are used to relieve withdrawal symptoms without substituting a similarly-acting drug of abuse. For example, clonidine is sometimes used in the treatment of opiate withdrawal symptoms. Acupuncture has also been used as an aid in detoxification, with some positive results (Margolin et al. 1993).
Rehabilitation
The third phase of treatment combines helping the patient establish a stable state of ongoing abstinence from all substances of abuse (including those prescription drugs which may cause dependence) and treating whatever associated physical and psychological conditions accompany the drug-related disorder. Treatment may begin on an inpatient or intensive outpatient basis, but characteristically continues in an outpatient setting for a number of months. Group, individual and family counselling and behavioural techniques may be combined with psychiatric management, which may include medication. The goals include helping patients understand their patterns of drug or alcohol use, identifying triggers for relapse after past efforts at recovery, helping them to develop drug-free coping patterns in dealing with life problems, and helping them integrate into a clean and sober social support network in the community. In some cases of opiate dependence, long-term maintenance on a long-acting synthetic opiate (methadone) or an opiate receptor blocking drug (naltrexone) is the treatment of choice. Maintenance on a daily dose of methadone, a long-acting opiate, is recommended by some practitioners for individuals with long-term opiate addiction who are unwilling or unable to achieve drug-free status. Patients stably maintained on methadone over long periods are able to function successfully in the workforce. In many cases, such patients are eventually able to detoxify and become drug free. In these cases, maintenance is combined with counselling, social services and other rehabilitative treatment. Recovery is defined in terms of stable abstinence from all drugs other than the drug of maintenance.
Long-term follow-up
The final phase of treatment continues on an outpatient basis for a year or more after a stable remission is attained. The goal of long-term follow-up is preventing relapse and helping the patient internalize new patterns of coping with life problems. The EAP or employee health service can be a great help during the rehabilitation and follow-up phases by monitoring cooperation in treatment, encouraging the recovering employee to maintain abstinence and assisting him/her in readjusting to the workplace. Where self-help or peer assistance groups are available (for example, Alcoholics Anonymous or Narcotics Anonymous), these groups provide a life-long supportive programme for sustained recovery. Since drug or alcohol dependence is a chronic disorder in which there may be relapses, company policies often require follow-up and monitoring by the EAP for a year or more after abstinence is established. If an employee relapses the EAP usually re-evaluates the situation and a change in treatment plan may be instituted. Such relapses, if brief and followed by a return to abstinence, usually do not signal overall treatment failure. Employees who do not cooperate with treatment, deny their relapses in face of clear evidence or cannot maintain stable abstinence will continue to show poor work performance and may be terminated from employment on that basis.
Women and Substance Abuse
While social changes in some areas have narrowed the differences between men and women, substance abuse has traditionally been seen as a man’s problem. Substance abuse was felt to be incompatible with women’s role in society. Consequently, while men’s abuse ot substances could be excused, or even condoned, as an acceptable part of manhood, women’s abuse of substances attracted a negative stigma. While this latter fact may be claimed to have prevented many women from abusing drugs, it has also made it extremely difficult for substance-dependent women to seek assistance for their dependence in many societies.
Negative attitudes to women’s substance abuse, coupled with the reluctance of women to admit their abuse and dependence have resulted in scanty data being available specifically on women. Even in countries with considerable information about drug abuse and dependence, it is often hard to find data relating directly to women. In cases where studies have examined women’s role in substance abuse the approach has by no means been gender-specific, so that conclusions may have been clouded by viewing women’s involvement from a male perspective.
Another factor related to the concept of substance abuse as a male problem is the lack of services for women substance abusers. ... Where services, such as treatment and rehabilitation services, do exist, they frequently have an approach based on male role models of drug dependence. Where services are provided for women, it is clear that they must be accessible. This is not always easy when women’s drug dependence is stigmatized and when cost of treatment is beyond the means of the majority of women.
Quoted from: World Health Organization 1993.
Effectiveness of Workplace-based Programmes
An investment in workplace programmes to deal with drug and alcohol problems has been profitable in many industries. An example is a study of 227 employees of a large US manufacturing company who were referred for the treatment of alcoholism by the company’s EAP. Employees were randomly assigned to three treatment approaches: (1) mandatory inpatient care, (2) mandatory attendance at Alcoholics Anonymous (AA) or, (3) a choice of inpatient care, outpatient care or AA. At follow-up, two years later, only 13% of the employees had been discharged. Of the remainder, less than 15% had job problems and 76% were rated “good” or “excellent” by their supervisors. Time absent from work fell by more than a third. Although some differences were found between initial treatment approaches the two-year job outcomes were similar for all three (Walsh et al. 1991).
The US Navy has calculated that its inpatient drug and alcohol rehabilitation programmes have produced an overall ratio of financial benefit to cost of 12.9 to 1. This figure was calculated by comparing the cost of the programme with the costs that would have been incurred in replacing the successfully rehabilitated programme participants with new personnel (Caliber Associates 1989). The Navy found that the benefit to cost ratio was highest for those over 26 years of age (17.8 to 1) as compared to younger personnel (8.2 to 1) and found the greatest benefit for alcoholism treatment (13.8 to 1), versus other drug (10.3 to 1) or polydrug dependence treatment (6.8 to 1). Nevertheless, the programme produced financial savings in all categories.
In general, workplace-based programmes for the identification and rehabilitation of employees who suffer from alcohol and other drug problems have been found to benefit both employers and workers. Modified versions of EAP programmes have also been adopted by professional organizations, such as the medical societies, nursing associations and bar associations (associations of lawyers). These programmes receive confidential reports about possible signs of impairment in a professional from colleagues, families, clients or employers. Face-to-face intervention is performed by peers, and if treatment is required the programme makes the appropriate referral. It then monitors the recovery of the individual and helps the recovering professional deal with practice and licensing problems (Meek 1992).
Conclusion
Alcohol and other psychoactive drugs are significant causes of problems in the workplace in many parts of the world. Although the type of drug used and the route of administration may vary from place to place and with the type of industry, the abuse of drugs and alcohol creates health and safety hazards for users, for their families, for other workers and, in many cases, for the public. An understanding of the types of drug and alcohol problems that exist within a given industry and the intervention and treatment resources available in the community will allow rehabilitative programmes to be developed. Such programmes bring benefits to employers, employees, their families and the larger society in which these problems arise.