China, the world’s largest developing country, is striving to accomplish unprecedented modernization. The “opening-up” policy to outside interests and the economic reform in effect since 1979 have brought profound changes to China’s economy and to every aspect of its society. The GNP increased from 358.8 billion yuan RMB in 1978 to 2,403.6 billion in 1992, an increase of more than three times in terms of constant money value. The average annual growth rate of GNP was 9.0%. The gross industrial output value was 3,706.6 billion in 1992, an average annual growth of 13.2% from 1979 to 1992 (National Statistics Bureau 1993). China is being increasingly regarded as a “potential centre of economic activity” and has attracted 40% of all of the direct foreign investment in the developing world. By the end of 1993, 174,000 foreign-funded projects had been approved, bringing US$63.9 billion into the country, and the total cumulatively pledged foreign input was $224 billion (China Daily 1994a, 1994b).
In order to advance current reforms in a comprehensive manner ensuring harmonious progress in all economic sectors, an in-depth reform decision has been made. The objective of this reform of the economic structure is to establish a socialist market economy that will further liberate and expand China’s productive forces. The centrally planned economy which has been favoured for 40 years is being transformed into a market system. Whatever the market can manage itself should be left to be controlled by the market. The government should guide the growth of the market by economic policies, regulations, planning and necessary administrative means.
During the period of rapid social change and industrialization, especially the transition from a centrally planned economic system to a market-oriented economy, great challenges had to be faced by China’s traditional occupational health service. At the same time, many new occupational health problems are continually emerging while older ones have not yet been solved.
Reviewing the history of over 40 years of development of occupational health in China, one can observe that great achievements have been made and many efforts have proved to be successful. However, there is still a big gap between the growing need for occupational health capabilities and the currently limited service capacity. Like many other aspects of Chinese life, occupational health service is undergoing a tremendous reform.
Historical Review
Occupational health service, as a subsystem of China’s public health services, was established in the early 1950s. In 1949, when the People’s Republic of China was founded, the health status of the Chinese people was poor. Life expectancy at birth was 35 years. The occupational safety and health status of workers presented an even worse picture. The prevalence of occupational diseases, communicable diseases and injuries among workers was high. Workers were generally prematurely withdrawn from their jobs. To counter the hazardous working conditions and poor sanitation left over in the factories of the “old China”, the new government took three measures (Zhu 1990): (1) the establishment of health service institutions in large-scale industrial enterprises; (2) an extensive investigation of sanitation and safety in the factories; and (3) the improvement of sanitary conditions at the workplace and of worker’s living facilities.
The statistical data relating to China’s oldest industrial bases showed that, by 1952, 28 factory hospitals, 795 clinics and 30 sanatoria had been established in eastern China; in the northeastern region, the level of medical and health services in industrial enterprises had increased 27.6%, the number of health workers increased 53.2% and the number of hospital beds increased 12%—all these improvements took place in the three-year period from 1950 through 1952. Most of the seriously unsafe working conditions found in state-run enterprises by governmental checkups were improved through the joint endeavours of government and workers’ participation. The government also gave financial support to the construction of housing and sanitary facilities. By 1952, workers’ housing had increased ten times compared to 1950, the number of bathroom facilities increased 216%, restrooms increased 844% and workers’ clubs increased 207% (from the northeastern region statistics). Nutrition subsidies have been given to workers exposed to occupational hazards since 1950. These developments greatly promoted the resumption of industrial production at the time.
Since 1954, following Chairman Mao Ze-dong’s call for “approaching a socialist industrialized nation step by step”, China speeded up its industrial development. The government’s priorities for workers’ health started to be transferred from sanitation to occupational and environmental health and concentrated on the prevention and control of serious occupational diseases and injuries. The first Constitution of the People’s Republic of China stipulated that labourers should enjoy the right of protection by government and that the health and welfare of all labourers must be improved.
The central government—State Council—has paid great attention to the serious situation of occupational health problems. The First National Conference on Silica Dust Control in Working Environments was jointly convened by the Ministries of Public Health (MOPH) and Labour (MOL), and the All-China Federation of Trade Unions (ACFTU) in Beijing in 1954, just four years after the founding of the People’s Republic of China. The Second Conference on Silica Dust Control was convened five years later by the above-mentioned three agencies in conjunction with such industrial administration sectors as the Ministry of the Coal Industry and the Ministry of Constructive Material Manufacture, among others.
At the same time, heat stress, occupational poisoning, industrial noise injuries and other illnesses induced by physical factors as well as pesticide poisoning in agriculture were put on the agenda of occupational health. Through the active recommendations to the State Council expressed through the joint efforts of MOPH, MOL, ACFTU and the Ministry of Industrial Administration (MOIA), a series of decisions, policies and strategies to strengthen the occupational health programme have been made by the State Council, including those relating to labour insurance, health and safety requirements for working environments, medical care for occupational illnesses, health examinations for workers engaged in hazardous work, establishing “health inspection” systems, and also the large amount of financial support needed to improve working conditions.
Organizational Structure of Occupational Health Delivery
The occupational health service network in China was initially established in the 1950s and has gradually taken shape over forty years. It can be seen at different levels:
In-plant service
As early as 1957, MOPH (1957) published a Recommendation on Establishing and Staffing Medical and Health Institutions in Industrial Enterprises. The principles of the document were adopted as national standards in the Hygienic Standards for Design of Industrial Premises (MOPH 1979) (see table 1). There should be a health department or a health and safety department at the management level of the enterprise, which should also be under the supervision of the local public health authority of the government. A workers’ hospital affiliated with the department functions as a medical/health centre, which provides preventive and curative services, including health surveillance of workers for occupational safety and health purposes, evaluation of working capacity from the medical point of view and approval of sick leaves of workers. There are health care stations near the workshops, which, under the management of and with the technical support of the workers’ hospital, play an important role in first aid, occupational health education for workers, collection of health information of workers at the workplaces and supervision of occupational safety and health jointly with trade unions and safety engineering departments.
Table 1. Minimum requirements of an in-plant health facility
|
Size of enterprise (employees) |
In-plant health facility |
Floor space ( m2 ) |
Minimum requirement |
|
>5,000 |
Hospital* |
To meet the construction standard for Comprehensive Hospitals |
|
|
3,501–5,000 |
Clinic |
140–190 |
Waiting room, consulting room, therapy room, clinic and IH laboratory x-ray room and pharmacy |
|
2,001–3,500 |
Clinic |
110–150 |
(same as above) |
|
1,001–2,000 |
Clinic |
70–110 |
X-ray is not required |
|
300–1,000 |
Clinic |
30–0 |
X-ray and laboratory are not required |
* Industrial enterprises with more than 3,000 employees can establish an in-plant hospital if they have high-risk productive processes, are located at far distances from a city or are situated in mountain areas with poor transportation.
Administrative division-based occupational health delivery
Providing health service is one of the responsibilities of governments. In the early 1950s, to prevent and control serious communicable diseases and to improve environment health, Health and Epidemic Prevention Stations (HEPSs) were established in every administrative division from provinces down to counties. The functions of the HEPSs were expanded with the growing needs of society and economic development to include preventive medical services, which covered occupational health, environmental health, food hygiene, school health, radiation protection as well as control of communicable and some non-communicable diseases. With health legislation being emphasized, the HEPSs are authorized to enforce the public health regulations and standards promulgated by the state or local governments and to implement inspection. The HEPSs, especially those at the provincial level, also provide public health technical assistance and services to the community and are involved in in-service training and scientific research.
The industrialization drive in China in the 1950s and early 1960s greatly accelerated the development of the occupational health service programme, which became one of the biggest departments in the HEPS system. Most medium and small industrial enterprises which were not able to maintain in-plant occupational health and industrial hygiene services could be covered by the HEPSs occupational health services, most of which were free of charge.
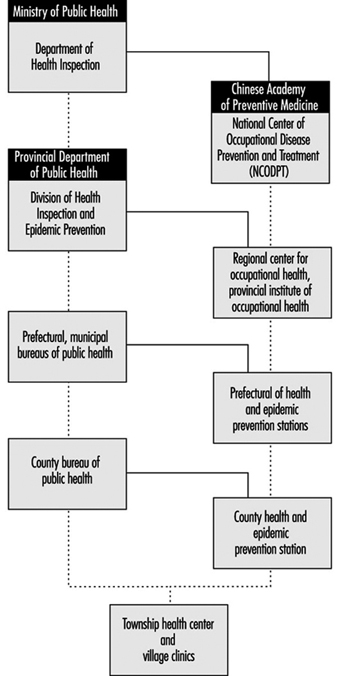
During the “Cultural Revolution” from 1966 to 1976, the occupational health service network and its activities were seriously damaged. This is one of the important reasons why some occupational diseases are still seriously prevalent in China. The reconstruction of the occupational health programme started in the late 1970s, when China began to realize once again the importance of economic development. Since the beginning of the 1980s, hospitals for occupational disease prevention and treatment and institutes of occupational health, called occupational health institutions (OHIs) have rapidly been established in most provinces and some industrial administrative sectors under the favourable policy of the government. OHIs were formed mainly on the basis of utilizing occupational health personnel in HEPS integrated with occupational physicians from hospitals. During the period 1983 to 1991, the central and local governments invested 33.8 million yuan RMB in total to support building OHIs. At provincial and prefecture levels, 138 OHIs were set up, with appropriate laboratory or clinical equipment. At present, the number of OHIs has reached 204, of which there are 60 established by the industrial sector. Another 110 million yuan RMB have been invested to equip 1,789 health and epidemic prevention stations at the county level (He 1993). The occupational health programmes in county HEPSs were one of the important parts of the project to be first equipped. To strengthen the national capacity of research, training and coordination of occupational health service, a National Centre for Occupational Disease Prevention and Treatment (NCODPT) was set up in the Institute of Occupational Medicine, Chinese Academy of Preventive Medicine (IOM/CAPM), and seven regional centres of occupational health, located in Beijing, Shanghai, Shenyang, Lanzhou, Chengdu, Changsa and Guangzhou, were also established. The current national network of occupational health services is illustrated in figure 1.
Figure 1. National network of occupational health services
So far, 34 schools or departments of public health have been established in the medical colleges or medical universities. These are the main resources of occupational health personnel. Six national occupational health in-service training centres were established in 1983. The total professional occupational health personnel, including physicians, industrial hygienists, technicians in laboratories and other health workers involved in occupational health programmes, reached about 30,000 in 1992.
Occupational Health Standards and Legislation.
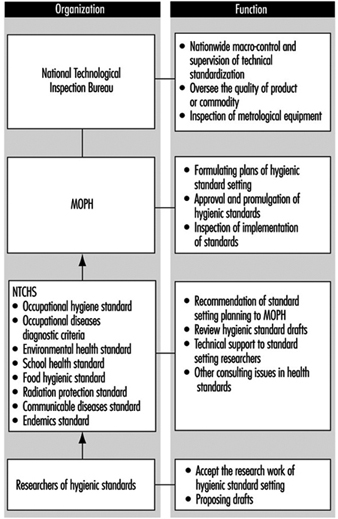
To encourage research in hygienic standards and in their establishment, a National Technical Committee of Hygienic Standards (NTCHS) was set up in 1981 as a consultative and technical reviewing agency of MOPH in hygienic standard setting. At present, NTCHS has eight subcommittees, which are responsible for occupational health, environmental health, school hygiene, food hygiene, radiation protection, occupational disease diagnosis, communicable disease and endemic disease prevention (figure 2). The members of NTCHS are experts from universities, research institutes, governmental agencies and the trade unions. The Hygienic Standards for Design of Industrial Premises (HSDIP) was first formulated in the 1950s and revised and promulgated again in 1979, so that it now contains a list of occupational exposure limits in terms of maximum allowable concentrations (MACs) for 120 toxic agents and dusts, and other requirements for hazards control measures in workplaces, sanitary and health facilities in plants and so forth. Also, there were 50 occupational hygienic standards for hazardous chemical and physical agents in the workplace promulgated by the Ministry of Public Health. Another 127 occupational hygienic standards are being reviewed. Diagnostic criteria for 50 compensable occupational diseases were issued by the Ministry of Public Health.
Figure 2. The management of health standard setting
As is known to all, China has had a centrally planned economic system and has been a country controlled by a unified central government for more than 40 years. So, most regulatory requirements in occupational safety and health at the national level were stipulated in the form of “Red Title” documents of the central government. These documents had, indeed, the highest legal effect and have constituted the basic regulatory framework of China’s occupational health. There are more than 20 documents of this kind promulgated by the State Council or its ministries. The major differences between these documents and legislation are that there are no stipulations for penalties in the documents, the compulsory effect is not as high as it is with laws and enforcement is weak.
Since economic reform has favoured the market-oriented system following the opening-up policy, national legislation has been greatly emphasized. Occupational health management is also being transformed from traditional administration to regulation-based approaches. One of the most important legal documents is the Regulation on Pneumoconioses Prevention and Control, issued by the State Council in 1987. Another milestone in protecting workers’ rights is the promulgation of the Labour Law by the National People’s Congress, with an anticipated effect date of 1 January 1995. The occupational safety and health of workers, as one of the major aims of this measure, is stipulated in the Law. To implement the Labour Law for occupational disease control, a draft law for occupational disease prevention and control was submitted to the Bureau of Legislation of the State Council by the Ministry of Public Health, in which most of the successful occupational health policies basic to occupational institutions, and experiences both in China and abroad. The draft must undergo further review and be submitted to the Standing Committee of the National People’s Congress.
Health Inspection System
“Putting prevention first” has been emphasized by the government and has become an important national basic public health principle. As early as 1954, when industrialization had just begun, the central government made the decision to establish a health inspection system to enforce the national health regulations and policies of industrial hygiene. HEPSs were authorized to implement health inspection on behalf of the public health authorities of the government. The main tasks of health inspection of enterprises include the following:
- to inspect the enterprise for hazard control in workplaces so that the concentrations/intensities of occupational hazards meet national industrial hygienic standards
- to check whether or not the pre-placement and periodic health examinations of exposed workers have been conducted in compliance with related national regulations or local governmental requirements
- to ensure that workers who are suffering from occupational diseases be properly treated, allowed to recuperate, transferred to other jobs or offered some other suitable option in line with related regulations
- to conduct hygienic evaluation and to supervise hazard control measures in workplaces
- to supervise occupational health record keeping, occupational disease reporting and working environmental monitoring in enterprises.
- The above activities are part of “regular health inspection” and are considered routine inspecting tasks that should be carried out periodically. To continue, the remaining chief tasks of health inspection are:
- preventive health inspection on industrial construction projects (prior to a new industrial construction or reconstruc-ting/expanding of old industrial enterprises, all engineering designs, hazard control facilities, medical/health and workers’ living facilities must pass an initial inspection for occupational health purposes)
- toxicological assessment of new industrial chemical substances.
Health inspection, especially preventive health inspection as a fundamental principle of public health intervention measures, has been stipulated in a number of laws and public health regulations. Since the 1970s, as great attention has been paid to the control of environmental pollution, preventive occupational health inspection has further been expanded to whole process inspection. The principle that “hazard control installations must be simultaneously designed, constructed and put into use/operation with the principal part of the project” was one of the important requirements in the Regulation on Pneumoconiosis Prevention and Control and the Environmental Protection Law.
Comprehensive Prevention Strategy for Occupational Diseases
Along the way to controlling pneumoconioses and serious dust contamination in the working environment, comprehensive prevention was emphasized, which was summed up in eight Chinese characters, and so called the “Eight Characters” strategy. The meanings are translated in English as follows:
- innovation: technological improvement, such as using safe or low-risk materials and more productive processes, and replacing outmoded productive methods by appropriate advanced techniques
- keep it wet: keeping a dusty worksite wet to decrease the concentration of dust, especially for drilling and grinding in mining industries
- enclosure: segregating workers, equipment and environmental areas to prevent the escape of dust and operators’ subsequent contamination
- ventilation: improving natural and mechanical ventilation
- protection: providing personal protection for exposed workers
- supervision: setting up regulations and safe operating rules, and supervising workers to ensure that they follow them strictly
- education: implementing health and safety education programmes to promote workers’ participation and enhance their awareness and skills with regard to personal protection
- checking up: inspecting the working environments to meet national standards and regularly examining the workers’ health in line with national requirements.
It has been proved by the practices of many enterprises that the “Eight Characters” strategy is important and effective in improving working conditions.
Environmental Monitoring in Workplaces
Enterprises with hazardous working environments should periodically monitor the concentrations or intensities of the hazards at worksites and take measures to control risks to meet national industrial hygienic standards (for example, with reference to values of MACs). If the enterprises are not able to conduct environmental monitoring by themselves, local OHIs or HEPSs can provide services.
To control the quality of workplace monitoring conducted by enterprises, OHIs or HEPSs must conduct inspection regularly or whenever necessary. NCODPT is responsible for the nationwide quality control of workplace hazard monitoring. A number of technical regulations for air monitoring in the workplace have been promulgated by MOPH or been published as national recommendations by NCODPT—for example, Methods for Airborne Dust Measurement in the Workplace (GB 5748–85) (MOPH 1985) and Methods for Monitoring and Analysis of Chemical Hazards in Air of Workplace (Institute of Occupational Medicine 1987).
To control further the quality of environmental monitoring in workplaces a set of quality assurance norms for measurement of hazardous substances in the working environment has been submitted to MOPH for further review and approval. The qualifications of institutions which undertake workplace monitoring would be reviewed and licensed, requiring:
- professional ability on the part of the person who takes the samples or engages in analytical work
- necessary equipment for sampling and analysis and their proper calibration
- reagents and standard solutions
- quality assurances for air and biological material sampling
- inter-laboratory quality assurances and similar checks.
At present, a pilot study on assessment of the laboratories is being conducting in 200 laboratories or institutions. This is the first step to implement the Quality Assurance Norm.
Health Examinations of Workers
Workers exposed to occupational hazards in workplaces should have occupational health examinations. This was first required for workers exposed to dust in the 1950s. It quickly expanded to cover workers exposed to toxic chemicals and physical hazards.
The health examinations include a pre-employment or fitness-to-work examination and periodic examinations. These medical examinations must be carried out by OHIs or competent medical/health institutions licensed by government public health administrations.
Pre-employment examination
A pre-employment examination is required for new workers or workers newly transferred to hazardous workplaces. The medical examinations focus on assessment of the health of workers in relation to the workplace conditions to ensure that the specific job they intend to hold will be of no damage to their health, and those who are not fit for a given job are excluded. Health criteria to determine job contraindications for different hazardous work conditions have been stipulated in detail in the National Diagnostic Criteria and Principles of Management of Occupational Diseases (Health Standards Office 1993) and Guideline of Occupational Health Service and Inspection promulgated by MOPH (1991b).
Periodic examination
Workers exposed to different hazards have different intervals of medical examinations. The period of examination for workers exposed to dust, for example, is illustrated in table 2. Workers suffering from pneumoconioses should have annual physical examinations.
Table 2. Periodic examination requirement for workers exposed to dust
|
Nature of dust |
Examination intervals (years) |
|
|
Workers in service |
Workers withdrawn |
|
|
Free silica content (%) |
||
|
80 |
0.5–1 |
1 |
|
40 |
1–2 |
2 |
|
10 |
2–3 |
3 |
|
10 |
3–5 |
5 |
|
Asbestos |
0.5–1 |
1 |
|
Other dust |
3–5 |
5 |
All medical records should be well secured both in enterprises and in local OHIs, and should be reported annually to the local government public health authority, and then to the NCODPT and the MOPH.
When anyone transfers to an enterprise from a plant involving risks of hazardous exposure, a health examination must be given by a local OHI to clarify whether his or her health has been damaged by exposure, and the health records must be sent to the new enterprise with the worker (MOPH 1987).
Table 3 shows the statistics of workers’ health examinations in the period 1988-1993. A total of 64 million workers were covered by the network of the occupational health service, which included state-owned and city collective-owned enterprises, and a part of rural industries at the township level. The workers exposed to occupational hazards account for 30% of the total workers. Nearly 4 million exposed workers, about 20% of the total, had medical examinations every year. In 1993, for example, the total number of the industrial population was 64,345,193, according to the report from the National Centre of Occupational Health Reporting (NCOHR 1994) (there was, however, a lack of data from Neimeng, Tibet and Taiwan). The proportion of workers exposed to occupational hazards accounted for 31.28% (20,126,929), of which 3,982,940 were examined, accounting for 19.79%. The total rate of detected compensable occupational diseases was 0.46% in 1993 (MOPH 1994).
Table 3. Physical examinations for workers exposed to occupational hazards
|
Year |
Number of |
Proportion of |
Examination rate |
Detected rate of |
|
1988 |
62,680 |
29.36 |
18.60 |
0.90 |
|
1989 |
62,791 |
29.92 |
20.67 |
0.57 |
|
1990 |
65,414 |
29.55 |
20.47 |
0.50 |
|
1991 |
66,039 |
30.30 |
21.03 |
0.57 |
|
1992 |
64,222 |
30.63 |
20.96 |
0.40 |
|
1993 |
64,345 |
31.28 |
17.97 |
0.46 |
The Management of Occupational Diseases
Compensable occupational diseases
Generally speaking, any illnesses caused by exposure to hazardous factors present in the workplace or resulting from processes of production is considered an occupational disease. However, for compensation purposes, a list of occupational diseases has been issued by the MOPH, the MOL, the Ministry of Finance and the ACFTU (MOPH 1987). The list covers nine categories, including pneumoconioses; acute and chronic occupational poisonings; diseases induced by physical factors; occupational communicable diseases; occupational dermatoses; occupational eye impairments; occupational ear, nose and throat diseases; and occupational tumours. The total is 99 diseases. If any other disease is proposed by local governments or governmental sectors to supplement the list, it should be submitted to the MOPH for approval.
Diagnosis of compensable occupational diseases
According to stipulations of the Administrative Rule of Occupational Disease Diagnosis issued by the MOPH, at the provincial and prefecture levels, compensable occupational diseases must be diagnosed by OHIs or by medical/health institutions licensed by the public health departments of local governments. In order to control the quality of diagnosis and to provide technical assistance for confirmation of complicated cases and adjudications of diagnostic disputes, expert committees on occupational disease diagnosis have been established at the national, provincial and prefecture/municipal levels (figure 3) (MOPH 1984).
Figure 3. The management of occupational disease diagnosis in China
The National Committee on Occupational Disease Diagnosis (NCODD) consists of five subcommittees concerned with occupational poisoning, pneumoconiosis, physical factor-induced occupational disease, radiation sickness and pneumoconiosis pathology, respectively. The headquarters of the Committee is in the Department of Inspection of the MOPH. The executive office of the NCODD is in the IOM/CAPM. All members of the Committee were appointed by the MOPH.
Diagnostic Criteria of occupational illnesses are promulgated by the MOPH. There are such criteria for 66 occupational diseases in effect right now. For other compensable occupational diseases without national diagnostic criteria, the provincial public health departments could formulate temporary diagnostic criteria to be put into effect in their own provinces after being submitted to the MOPH for the records.
According to the Diagnostic Criteria, the diagnosis of occupational disease must be based on the following sorts of evidence: a history of exposure, clinical symptoms and signs, laboratory findings and results of working environmental monitoring, and reasonable exclusion of other diseases. Once the diagnosis is made, an Occupational Disease Certification (ODC) must be issued by the OHI. Three copies of the ODC should be sent: one to the worker, one to the enterprise for proper compensation arrangements and one should be kept in the OHI for further medical treatment and working capacity evaluation.
Management of occupational disease patients
Compensation and other welfare for patients suffering from occupational diseases must be provided by the enterprises according to the Labour Insurance Regulations (LIR). The management, labour union and committee of working capacity evaluation in the enterprise must jointly take part in the discussion and decision on proper treatment and compensation for the patients based on the ODC and the degree of working capacity loss. For those who are proved to be not suitable for doing their original jobs after the completion of proper medical treatment, the enterprise should transfer them to other worksites or make proper employment arrangements according to their health conditions within two months, and for special cases, at the latest in six months. When a worker suffering from occupational disease moves to another enterprise, his or her occupational disease benefits should be borne by the original enterprise where the occupational disease was caused, or shared by both enterprises after they have come to an agreement. All the health records, the ODC and other information relating to the health care of the worker must be transferred to the new enterprise from the original one, and the transfer should be reported by both enterprises to their local OHIs for record-keeping and further follow-up purposes.
If the diagnosis of an occupational disease is made after the worker has moved to a new enterprise, all the compensation or benefits should be paid by the new enterprise where the worker is currently working, regardless of whether or not the affliction is connected with the present working conditions. For a contracted worker or temporarily employed worker, if the occupational disease is diagnosed during unemployed periods and there is evidence proving exposure to related hazardous working environments when he or she was hired by any enterprise, the compensation and medical care should be paid by the enterprise (MOPH 1987).
Achievements in Occupational Disease Prevention and Control
Improvement of working environments
The concentration or intensity of occupational hazards in the workplace has declined significantly. The statistics of working environmental monitoring as supplied from the NCOHR showed that the proportion of worksites in compliance with national standards has increased 15% from 1986 to 1993 (NCOHR 1994). This is particularly true for state-owned and urban collective-owned industrial enterprises, of whose working environments nearly 70% had met the national standards. The situation in rural industrial enterprises is also improving. The compliance rate for occupational hazards increased from 42.5% in 1986 to 54.8% in 1993 (table 4). It is important to note that the estimation of the compliance rates of township industries might be higher than the actual situation, because this routine report can cover only about 15% of the rural industries every year, and most of them are located near cities which have well-developed health service facilities.
Table 4. Results of environmental monitoring for hazards in the workplace
|
Year* |
State-owned industry |
Rural industry |
||
|
No. of environmental locales monitored |
Proportion of locales up to standards (%) |
No. of environmental locales monitored |
Proportion of locales up to standards (%) |
|
|
1986 |
417,395 |
51.40 |
53,798 |
42.50 |
|
1987 |
458,898 |
57.20 |
50,348 |
42.60 |
|
1988 |
566,465 |
55.40 |
68,739 |
38.50 |
|
1989 |
614,428 |
63.10 |
74,989 |
53.50 |
|
1990 |
606,519 |
66.40 |
75,398 |
50.30 |
|
1991 |
668,373 |
68.45 |
68,344 |
54.00 |
|
1992 |
646,452 |
69.50 |
89,462 |
54.90 |
|
1993 |
611,049 |
67.50 |
104,035 |
54.80 |
* Exclusive of data from 1988: Yunnan, Xinjiang; 1989: Tibet, Taiwan; 1990: Tibet, Taiwan; 1991: Tibet, Taiwan; 1992: Tibet, Taiwan; 1993: Neimeng, Tibet, Taiwan.
The prevalence of some serious occupational diseases andthe implementation of comprehensive preventive measures
The national occupational health report data indicated that the prevalence of compensable occupational diseases maintained itself at a rate of 0.4 to 0.6%, although industries developed very quickly in recent years. Silicosis, for example, has been controlled for years in some large state-owned industrial or mining enterprises. Tables 5 and 6illustrate the success of Yiao Gang Xian Tungsten Mine and Anshan Steel Company in controlling silicosis (Zhu 1990).
Table 5. Dust exposure and prevalences of silicosis in Yiao Gang Xian Tungsten Mine
|
Year |
Dust concentrations ( mg/m3 ) |
Detected rates of silicosis (%) |
|
1956 |
66 |
25.8 |
|
1960 |
3.5 |
18.6 |
|
1965 |
2.7 |
2.6 |
|
1970 |
5.1 |
0.3 |
|
1975 |
1.6 |
1.2 |
|
1980 |
0.7 |
2.1 |
|
1983 |
1.1 |
1.6 |
Table 6. Detection rate of silicosis in Anshan Steel Company
|
Year |
No. of examinations |
Cases |
Rate (%) |
Compliance rate of dust (%) |
|
1950s |
6,980 |
1,269 |
18.21 |
23.60 |
|
1960s |
48,929 |
1,454 |
2.97 |
29.70 |
|
1970s |
79,422 |
863 |
1.08 |
28.70 |
|
1980s |
33,786 |
420 |
1.24 |
64.10 |
The nationwide epidemiological survey of pneumoconiosis in 1987-90 has also shown that the average working time of patients from their first exposure to silica dust to the appearance of signs of pneumoconiosis had been significantly prolonged, from 9.54 years in the 1950s to 26.25 years in the 1980s for those with silicosis, and 16.24 years to 24.72 years for those with coal worker’s pneumoconiosis in the same period of time. The average age of patients suffering from silicosis at death had also been increased from 36.64 years to 60.64, and for patients with coal pneumoconiosis from 44.80 years to 61.43 years (MOPH 1992). These improvements could be partly attributed to the successful occupational health policies and interventions of governmental policies as well as to the great efforts of occupational health professionals.
Promoting occupational health programmes in small-scale industries
Facing the continuing rapid development of small-scale industries, especially of township industries, and the growing gap between occupational health services and practical needs, the Ministry of Public Health decided to conduct a further comprehensive intervention field study. This study is important not only for helping to solve occupational health problems in rural industries, but also for exploring approaches to reform the occupational health service system in state-owned enterprises in order to match the changing requirements of the market economic system that is being established. Therefore, in December 1992, the Expert Group for the Field Study of Occupational Health Service Policies for Small-scale Industries was set up in the Department of Health Inspection, Ministry of Public Health. The Group was formed to support provinces in developing occupational health service programmes and approaches to effective intervention in hazardous situations. As the first step, the Group has drafted a “Recommended National Field Study Program” for provincial governments, which was approved and issued by the MOPH in 1992. The primary strategy of the programme is described as follows:
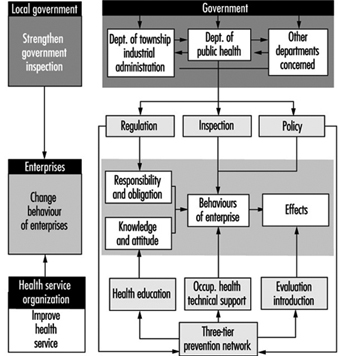
The enterprise, the provider of occupational health and the local government are the three key parts of the programme. The programme focuses on readjusting the relationship among the three parts to establish a new model of development. The basic objectives of the programme are to strengthen the regulatory control of government, to change the attitudes to health and the behaviours of the productive and operation functions of enterprises and to enlarge the coverage of minimum occupational health service while improving working conditions with appropriate technological measures (figure 4). Four counties (or districts) have been selected by the MOPH as national trial areas prior to the nationwide implementation of the programme, which include the Zhangdian district in Zibo municipality, Shandong province; the Baoshan District in Shanghai municipality; Jinhua County in Zhejiang province; and the Yuhong District in Shenyang municipality, Liaoning province.
Figure 4. The strategy of the pilot study on OHS in township enterprises
Seven spheres of policy interventions have been emphasized in the programme:
- strengthening the supervision and inspection provided by local governments of the occupational health of small-scale industries
- exploring how to integrate occupational health services for rural industries, with the goal “Health for All by the Year 2000” in China
- improving grass roots health organization networks to deliver occupational health services, management and supervision to the enterprises
- exploring practical approaches to enforce and implement occupational health inspection and service for township enterprises
- searching for and recommending appropriate technology for hazard control and personal protection for township enterprises
- implementing occupational health education programmes in township industries
- developing occupational health manpower and improving occupational health service working conditions to strengthen the occupational health service network, especially at the township and county levels.
Some preliminary results have been obtained in these four trial areas, and the basic ideas of the programme are being introduced to other areas in China and was scheduled for final evaluation in 1996.
The author thanks Prof. F. S. He for her assistance in reviewing this article.