Geopolitical Background
The predominant development of heavy industry (the iron and steel industry, smelting and refinery plants), metalworking and machinery industries, and the emphasis on the production of energy in Central and Eastern Europe, have significantly predetermined the structure of the economies in the region for the last four decades. This state of affairs has resulted in the relatively high exposures to certain types of occupational hazards in the workplace. Current efforts to transform the existing economies along the lines of the market economy model and to improve occupational safety and health have been considerably successful so far, given the short period of time for such an endeavour.
Until recently, ensuring the prevention of adverse health effects of chemicals present in occupational settings and in the environment, the drinking water and the food basket of the population was provided for by the compulsory observance of hygienic and sanitary standards and occupational exposure limits such as Maximum Allowable Concentrations (MACs), Threshold Limit Values (TLVs) and Acceptable Daily Intake (ADI). The principles of toxicity testing and exposure evaluation recommended by various international organizations, including standards applied in the countries of the European Union, will become more and more compatible with those used in the Central and Eastern European countries as the latter gradually integrate with other European economies.
During the 1980s the need was increasingly recognized to harmonize the methodologies and scientific approaches in the field of toxicology and hygienic standardization applied in the OECD countries with those used in the member countries of the Council of Mutual Economic Assistance (CMEA). This was mainly due to growing levels of production and trade, including industrial and agricultural chemicals. A contributing factor favouring the urgency with which these considerations were viewed was a growing problem of air and river pollution across national boundaries in Europe (Bencko and Ungváry 1994).
The Eastern and Central European economic model was based on a centrally planned economic policy oriented to the development of basic metal industries and the energy sector. As of 1994, except for minor changes, the economies of the Russian Federation, Ukraine, Belarus, Poland, and the Czech and the Slovak Republics had preserved their old structures (Pokrovsky 1993).
Coal mining is a widely developed industry in the Czech Republic. At the same time, black coal mining (e.g., in the northern Moravian region of the Czech Republic) is a cause of 67% of all new cases of pneumoconioses in the country. Brown coal is extracted in opencast mines in northern Bohemia, southern Silesia and neighbouring parts of Germany. Thermal power stations, chemical plants and brown coal mining heavily contributed to the environmental pollution of this region, forming the so-called “black” or “dirty triangle” of Europe. Uncontrolled use of pesticides and fertilizers in agriculture was not exceptional (Czech and Slovak Federal Republic 1991b).
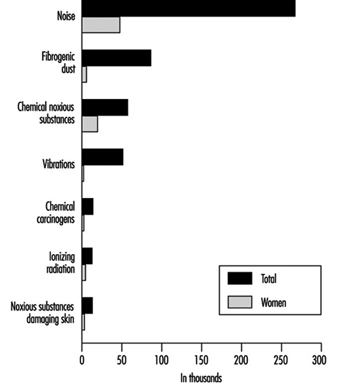
The labour force of the Czech Republic numbers some 5 million employees. About 405,500 workers (that is, 8.1% of the working population) are involved in hazardous operations (Ministry of Health of the Czech Republic 1992). Figure 1 presents data on the number of workers exposed to different occupational hazards and the proportion of women among them.
Figure 1. Number of workers in the Czech Republic exposed to the most serious occupational risks
Changing Needs
The occupational health system of the Czech Republic underwent three consecutive stages in its development and was influenced by the political and economic changes in the country (Pelclová, Weinstein and Vejlupková 1994).
Stage 1: 1932-48. This period was marked by the foundation of the first Department of Occupational Medicine by Professor J. Teisinger at the oldest university in Central Europe—Charles University (founded in 1348). Later, in 1953, this department became the Clinic of Occupational Medicine, with 27 beds. Professor Teisinger also founded the Research Institute of Occupational Health and in 1962 the Poison Information Centre at the Clinic. He was granted several international awards, including an award from the American Association of Industrial Hygienists in 1972 for his personal contribution to occupational health development.
Stage 2: 1949-88. This period exhibited numerous inconsistencies, in some respects being marked by notable deficiencies and in others showing distinct advantages. It was recognized that the existing system of occupational health, in many ways reliable and well developed, nevertheless had to be reorganized. Health care was considered as a basic civil right guaranteed by the Constitution. The six basic principles of the health system (Czech and Slovak Federal Republic 1991a) were:
- planned integration of health care into the society
- promotion of a healthy lifestyle
- scientific and technical development
- prevention of physical and mental illnesses
- free and universal access to health care services
- concern on the part of the state for a healthy environment.
Despite certain progress none of these goals had been fully achieved. Life expectancy (67 years for men and 76 years for women) is the shortest among the industrialized countries. There is a high mortality rate from cardiovascular diseases and cancer. About 26% of adult Czechs are obese and 44% of them have cholesterol levels above 250 mg/dl. The diet contains much animal fat and is low in fresh vegetables and fruits. Alcohol consumption is relatively high, and around 45% of adults smoke; smoking kills about 23,000 persons a year.
Medical care, dental care and medicines were provided free of charge. The numbers of physicians (36.6 per 10,000 inhabitants) and nurses (68.2 per 10,000) were among the highest in the world. But in the course of time the government became unable to cover the continually increasing and abundant expenses needed for public health. There had been temporary shortages of some drugs and equipment as well as difficulties in providing health care services and rehabilitation. The existing structure, which did not allow a patient to choose his primary health care physician, created many problems. Medical staff working in the state-run hospitals received low fixed salaries and had no incentives to provide more health care services. A private health care system did not exist. In hospitals, the main criterion of acceptable functioning was the “percentage of occupied beds” and not the quality of the health care provided.
However, there were positive features of the state-run centralized system of occupational health. One of them was an almost complete registration of hazardous workplaces and a well-organized system of hygienic control provided by the Hygienic Service. In-plant occupational health services established in large industrial enterprises facilitated the provision of comprehensive health care services, including periodic medical examinations and treatment of workers. Small private enterprises, which usually pose many problems to occupational health programmes, did not exist.
The situation was similar in agriculture, where there were no small private farms, but large-scale cooperative ones: an occupational physician working in a health centre of a factory or a cooperative farm provided occupational health services for the workers.
Enforcement of occupational safety and health legislation was sometimes contradictory. After an inspection of a hazardous workplace was carried out by an industrial hygienist or factory inspector, who had required the reduction of the level of occupational exposure and the enforcement of prescribed health and safety standards, rather than correct the hazards the workers would receive monetary compensation instead. Besides the fact that enterprises often took no action at all to improve working conditions, the workers themselves were not interested in improving their working conditions but opted to continue receiving bonuses in lieu of changes in the working environment. Furthermore, a worker who contracted an occupational disease received a substantial monetary recompense according to the severity of the disease and to the level of his or her previous salary. Such a situation produced conflicts of interests among industrial hygienists, occupational physicians, trade unions and enterprises. As many of the benefits were paid by the state and not by the enterprise, the latter often found it cheaper not to improve safety and health in the workplace.
Strange as it may seem, some hygienic standards, including permissible levels and occupational exposure limits, were more rigorous than those in the United States and in the western European countries. Thus, it was sometimes impossible not to exceed them with outdated machinery and equipment. Workplaces exceeding the limits were classified under “category 4”, or most hazardous, but for economic reasons manufacturing was not stopped and workers were offered compensatory benefits instead.
Stage 3: 1989–the present. The “velvet revolution” of 1989 enabled an inevitable change of the public health care system. The reorganization has been rather complex and sometimes difficult to accomplish: consider, for example, that the health care system has more beds in hospitals and doctors per 10,000 inhabitants than any industrialized country while it uses disproportionately less financial resources.
The Current Status of Occupational Safety and Health
The most frequent occupational hazard at the workplace in the Czech Republic is noise—about 65.8% of all workers at risk are exposed to this occupational hazard (Figure 8). The second major work-related hazard is fibrogenic dust, which represents an occupational hazard to about 21.3% of all workers at risk. Approximately 14.3% of workers are exposed to toxic chemicals. More than one thousand of these are exposed to toluene, carbon monoxide, lead, gasoline, benzene, xylene, organophosphorus compounds, cadmium, mercury, manganese, trichlorethylene, styrene, tetrachloroethylene, aniline and nitrobenzene. Another physical hazard—local hand-arm vibration—is a danger for 10.5% of all workers at risk. Other workers are exposed to chemical carcinogens, ionizing radiation and dangerous substances causing skin lesions.
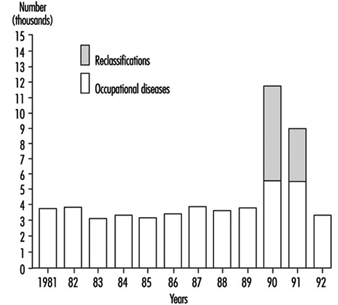
The number of acknowledged cases of occupational disease in the Czech Republic in 1981-92 is presented in figure 2.
Figure 2. Occupational diseases in the Czech Republic in the period 1981-1992
The increase of morbidity from occupational diseases in 1990–91 had been due to the process of reclassification of occupational illnesses requested by miners and workers in other occupations and by their trade unions. They asked to change the status of “being endangered with an occupational disease”, used for less obvious forms of occupational impairment with low compensation, to fully compensated disease. The status of “endangerment” was reconsidered by the Ministry of Health in 1990 for the following kinds of occupational pathology:
- mild forms of pneumoconioses
- mild forms of chronic musculoskeletal disorders due to overload and vibration
- mild forms of occupational hearing loss.
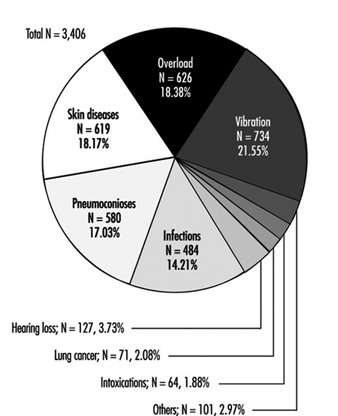
Reclassification was done for all cases before 1990 and concerned 6,272 cases in 1990 and 3,222 cases in 1991 (figure 2). After that the status of “endangerment” was abolished. Figure 3 presents data on 3,406 new cases of occupational diseases by category diagnosed in the Czech Republic in 1992; 1,022 cases of these occupational diseases were diagnosed in women (Urban, Hamsova and Neecek 1993).
Figure 3. Occupational diseases in the Czech Republic in 1992
Some shortages in the supply of measuring equipment for sampling and analysis of toxic substances make it difficult to conduct occupational hygiene evaluations in the workplace. On the other hand, the use of biomarkers in exposure tests for the monitoring of workers in hazardous occupations is practised for a variety of dangerous substances according to the regulations of the Czech Republic. Similar tests have already been legally codified in Hungary, Slovakia, Slovenia, Croatia, Poland, and in some other countries of Central and Eastern Europe. The use of exposure tests for periodic medical examinations has proved to be a very efficient tool for personnel exposure monitoring. This practice has enabled early detection of some occupational diseases and permitted their prevention, thus decreasing compensation costs.
The transition to the market economy and the rising costs of health care services in the Czech Republic have had their influence on occupational health services. In the past, the in-plant based occupational health service or centre provided both health surveillance and treatment for workers. Nowadays, these activities are subjected to some restrictions. This has resulted in reduced activities in health surveillance and hazard control and in an increased number of occupational accidents and diseases. Workers in rapidly emerging small-scale enterprises, which often operate with unreliable machinery and equipment, are practically out of the reach of occupational health professionals.
Projects for the Future
A new system of public health in the Czech Republic is expected to incorporate the following principles:
- prevention and health promotion
- overall access to “standard” health care
- decentralized policy determining delivery of services
- integration of health services in a territorial network
- increased autonomy of health care professionals
- emphasis on outpatient care
- compulsory health insurance
- community participation
- more options for patients
- new public/private sector partnership to provide an “above standard” health care no longer offered by the public sector.
The introduction of the compulsory health insurance system and the creation of the General Health Insurance Office, which began operating in January 1993, as well as minor health insurance companies in the Czech Republic have marked the beginning of reform in the public health sector. These changes have brought some problems to the occupational health services, given their preventive character and the high cost of treatment in hospitals. Thus, the role of outpatient medical settings in treating patients with conventional as well as work-related diseases is steadily increasing.
The Potential Impact of Continuing Changes on Occupational Safety and Health
The growth of reform in the public health sector has created a need for change for occupational physicians, industrial hygienists and in-patient medical settings, and has also led to a focus on prevention. The ability to focus on prevention and milder forms of disease is partly explained by earlier positive results and by the relatively good functioning of the previous occupational health system, which had worked effectively towards eliminating major serious occupational diseases. The changes have involved a shift of attention from severe forms of occupational pathology that needed urgent treatment (such as industrial poisoning and pneumoconioses with respiratory and right-heart failure) to mild forms of disease. The change in the activities of the occupational health services from a curative orientation to early diagnosis now concerns such conditions as mild forms of pneumoconioses, farmer’s lung, chronic liver illnesses and chronic musculoskeletal disorders due to overload or vibration. Preventive measures at the earlier stages of occupational diseases also should be undertaken.
Industrial hygiene activities are not covered by the health insurance system, and the industrial hygienists in the hygienic stations are still paid by the government. Lowering their number and the reorganization of hygienic stations are also expected.
Another change in the health care system is the privatization of some health services. The privatization of small out-patient medical centres has already started. Hospitals—including university hospitals—are not involved in this process at present and details of their privatization still need to be clarified. New legislation concerning the duties of the enterprises, workers and occupational health services is being gradually created.
Occupational Health at the Crossroads
Thanks to the advanced system of occupational health founded by Professor Teisinger in 1932, the Czech Republic does not face a serious problem of education in occupational health for university students, even though in some countries of Central and Eastern Europe the rate of recognized occupational diseases is about five times less than that of the Czech Republic. The Czech List of Occupational Diseases does not differ notably from that appended to the ILO Employment Injury Benefits Convention, (No. 121), (ILO 1964). The proportion of unrecognized principal occupational diseases is low.
The occupational health system in the Czech Republic is now at the crossroads and there is an obvious need for its reorganization. But it is necessary at the same time to preserve whatever positive features have been acquired from experience with the previous occupational health system, namely:
- registration of working conditions at the workplaces
- maintaining in operation a broad system of periodic medical examinations of employees
- provision of curative health care services at large-scale enterprises
- offering a system of vaccination and communicable disease control
- preserving the system whereby occupational health services admit patients with various occupational illnesses, a system that would involve the university hospitals in providing treatment to patients as well as education and training to medical students and graduates.