Water Pollution
For at least two millennia natural water quality has deteriorated progressively and reached contamination levels where water uses are severely limited or the water can be harmful to humans. This deterioration is related to the socio-economic development within a river basin, but long-range atmospheric transport of contaminants has now changed this picture: even remote areas can be indirectly polluted (Meybeck and Helmer 1989).
Medieval reports and complaints about inadequate excreta disposal, foul and stinking water courses within overcrowded cities and other similar problems were an early manifestation of urban water pollution. The first time that a clear causal linkage between bad water quality and human health effects was established was in 1854, when John Snow traced back the outbreak of cholera epidemics in London to a particular drinking water source.
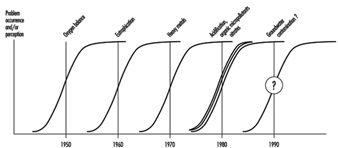
Since the middle of the twentieth century, and concurrent with the onset of accelerated industrial growth, various types of water pollution problems have occurred in rapid succession. Figure 1 illustrates the types of problems as they became apparent in European freshwaters.
Figure 1. Types of water pollution problems
In summarizing the European situation it can be stated that: (1) the challenges of the past (pathogens, oxygen balance, eutrophication, heavy metals) have been recognized, researched and the necessary controls identified and more or less implemented and (2) the challenges of today are of a different nature—on the one hand, “traditional” point and non-point pollution sources (nitrates) and ubiquitous environmental contamination problems (synthetic organics), and, on the other hand, “third generation” problems interfering with global cycles (acidification, climate change).
In the past, water pollution in the developing countries resulted mainly from the discharge of untreated wastewater. Today it is more complex as a result of the production of hazardous wastes from industries and the rapidly increasing use of pesticides in agriculture. In fact, water pollution today in some developing countries, at least in the newly industrializing ones, is worse than in industrialized countries (Arceivala 1989). Unfortunately, developing countries, on the whole, are badly lagging behind in getting control over their major pollution sources. As a consequence, their environmental quality is gradually deteriorating (WHO/UNEP 1991).
Types and Sources of Pollution
There are a large number of microbial agents, elements and compounds which may cause water pollution. They can be classified as: microbiological organisms, biodegradable organic compounds, suspended matter, nitrates, salts, heavy metals, nutrients and organic micropollutants.
Microbiological organisms
Microbiological organisms are common in freshwater bodies polluted particularly by discharges of untreated domestic wastewater. These microbial agents include pathogenic bacteria, viruses, helminths, protozoa and several more complex multicellular organisms that can cause gastro-intestinal illness. Other organisms are more opportunistic in nature, infecting susceptible individuals through body contact with contaminated water or by inhalation of poor quality water droplets in aerosols of various origins.
Biodegradable organic compounds
Organic substances of either natural origin (allochthonous terrestrial detritus or autochthonous debris of aquatic plants) or from anthropogenic sources (domestic, agricultural and some industrial wastes) are decomposed by aerobic microbes as the river continues its course. The consequence is a lowering of the oxygen level downstream of the wastewater discharge, impairing the quality of the water and the survival of the aquatic biota, particularly of high-quality fish.
Particulate matter
Particulate matter is a major carrier of organic and inorganic pollutants. Most toxic heavy metals, organic pollutants, pathogens and nutrients, such as phosphorus, are found in suspended matter. An appreciable amount of the biodegradable organic material responsible for consumption of dissolved oxygen from rivers is also found in suspended particles. Particulate matter comes from urbanization and road construction, deforestation, mining operations, dredging operations in rivers, natural sources which are linked to continental erosion, or natural catastrophic events. Coarser particles are deposited on river beds, in reservoirs, in the flood plain and in wetlands and lakes.
Nitrates
The concentration of nitrates in unpolluted surface waters ranges from less than 0.1 to one milligrams per litre (expressed as nitrogen), so nitrate levels in excess of 1 mg/l indicate anthropogenic influences such as discharge of municipal wastes and urban and agricultural run-off. Atmospheric precipitation is also an important source of nitrate and ammonia to river basins, particularly in areas not affected by direct pollution sources—for example, some tropical regions. High concentrations of nitrate in drinking water may lead to acute toxicity in bottle-fed infants during their first months of life, or in the elderly, a phenomenon called methaemoglobinaemia.
Salts
Water salinization may be caused by natural conditions, such as geochemical interaction of waters with salty soils or by anthropogenic activities, including irrigated agriculture, sea water intrusion due to excessive pumping of groundwaters in islands and coastal areas, disposal of industrial wastes and of oilfield brines, highway de-icing, landfill leachates and leaking sewers.
While hampering beneficial uses, particularly for irrigation of sensitive crops or for drinking, salinity in itself may not, at even quite high levels, be directly harmful to health, but the indirect effects can be dramatic. The loss of fertile agricultural land and reduced crop yields caused by waterlogging and soil salinization of irrigated areas destroy the livelihood of whole communities and cause hardships in the form of food shortages.
Heavy metals
Heavy metals such as lead, cadmium and mercury are micro-pollutants and of special interest as they have health and environmental significance due to their persistence, high toxicity and bio-accumulation characteristics.
There are basically five sources of heavy metals contributing to water pollution: geological weathering, which provides the background level; industrial processing of ores and metals; the use of metal and metal compounds, such as chromium salts in tanneries, copper compounds in agriculture, and tetraethyl lead as an anti-knock agent in gasoline; leaching of heavy metals from domestic wastes and solid waste dumps; and heavy metals in human and animal excretions, particularly zinc. Metals released to the air from automobiles, fuel burning and industrial process emissions may settle on land and ultimately run off to surface waters.
Nutrients
Eutrophication is defined as the enrichment of waters with plant nutrients, primarily phosphorus and nitrogen, leading to enhanced plant growth (both algae and macrophytes) which results in visible algae blooms, floating algal or macrophyte mats, benthic algae and submerged macrophyte agglomerations. When decaying, this plant material leads to the depletion of the oxygen reserves of water bodies, which, in turn, causes an array of secondary problems such as fish mortality and liberation of corrosive gases and other undesirable substances, such as carbonic gas, methane, hydrogen sulphide, organoleptic substances (causing taste and odour), toxins and so on.
The source of phosphorus and nitrogen compounds is primarily untreated domestic wastewater, but other sources such as drainage of artificially fertilized agricultural land, surface run-off from intensive livestock farming and some industrial wastewaters can also substantially increase the trophic level of lakes and reservoirs, particularly in tropical developing countries.
The main problems associated with eutrophication of lakes, reservoirs and impoundments are: oxygen depletion of the bottom layer of lakes and reservoirs; water quality impairment, leading to treatment difficulties, particularly for the removal of taste- and odour-causing substances; recreational impairment, increased health hazards to bathers and unsightliness; fisheries impairment due to fish mortality and the development of undesirable and low-quality fish stocks; ageing and reducing the holding capacity of lakes and reservoirs by silting; and increase of corrosion problems in pipes and other structures.
Organic micropollutants
Organic micropollutants can be classified in groups of chemical products on the basis of how they are used and consequently how they are dispersed in the environment:
- Pesticides are substances, generally synthetic, that are deliberately introduced into the environment to protect crops or control disease vectors. They are found in various distinct families, such as organochloride insecticides, organophosphate insecticides, herbicides of the plant hormone type, triazines, substituted ureas and others.
- Materials for widespread household and industrial use comprise volatile organic substances used as extraction solvents, solvents for degreasing metals and dry-cleaning clothes, and propellants for use in aerosol containers. This group also includes halogenated derivatives of methane, ethane and ethylene. As they are widely used their rates of dispersion in the environment, compared with the amounts produced, are generally high. The group also contains the polycyclic aromatic hydrocarbons, whose presence in the environment results from the extraction, transport and refining of petroleum products and the dispersion of combustion products resulting from their use (petrol and heating oil).
- Materials used essentially in industry include substances which are direct or intermediate agents of chemical synthesis, such as carbon tetrachloride for synthesizing freons; vinyl chloride for polymerizing PVC; and chlorinated derivates of benzene, naphthalene, phenol and aniline for manufacturing dyestuffs. The group also contains finished products used in closed systems, such as heat-exchange fluids and dielectrics.
Organic micropollutants are generated from point and diffuse sources, either urban or rural. The largest part originates in major industrial activities such as petrol refining, coal mining, organic synthesis and the manufacture of synthetic products, the iron and steel industries, the textile industry and the wood and pulp industry. Effluents from pesticides factories may contain considerable quantities of these manufactured products. A significant proportion of organic pollutants are discharged into the aquatic environment as run-off from urban surfaces; and in agricultural areas, pesticides applied to crops may reach surface waters through rainwater run-off and artificial or natural drainage. Also, accidental discharges have led to severe ecological damage and temporary closure of water supplies.
Urban Pollution
Owing to this continuously expanding, aggressive and multi-faceted pollution scenario, the problem of maintaining the quality of water resources has become acute, particularly in the more urbanized areas of the developing world. Maintaining water quality is hampered by two factors: failure to enforce pollution control at the main sources, especially industries, and inadequacy of sanitation systems and of garbage collection and disposal (WHO 1992b). See some examples of water pollution in different cities in developing countries.
Examples of water pollution in selected cities
Karachi (Pakistan)
The Lyari river, which runs through Karachi, Pakistan’s largest industrial city, is an open drain from both the chemical and the microbiological point of view, a mixture of raw sewage and untreated industrial effluents. Most industrial effluents come from an industrial estate with some 300 major industries and almost three times as many small units. Three-fifths of the units are textile mills. Most other industries in Karachi also discharge untreated effluents into the nearest water body.
Alexandria (Egypt)
Industries in Alexandria account for around 40% of all Egypt’s industrial output, and most discharge untreated liquid wastes into the sea or into Lake Maryut. In the past decade, fish production in Lake Maryut declined by some 80% because of the direct discharge of industrial and domestic effluents. The lake has also ceased to be a prime recreational site because of its poor condition. Similar environmental degradation is taking place along the seafront as a result of the discharge of untreated wastewater from poorly located outfalls.
Shanghai (China)
Some 3.4 million cubic metres of industrial and domestic waste pour mostly into the Suzhou Creek and the Huangpu River, which flows through the heart of the city. These have become the main (open) sewers for the city. Most of the waste is industrial, since few houses possess flush toilets. The Huangpu has essentially been dead since 1980. In all, less than 5% of the city’s wastewater is treated. The normally high water table also means that a variety of toxins from industrial plants and local rivers find their way into groundwater and contaminate wells, which also contribute to the city water supply.
São Paulo (Brazil)
The Tiete River, as it passes through Greater São Paulo, one of the world’s largest urban agglomerations, receives 300 tonnes of effluents each day from 1,200 industries located in the region. Lead, cadmium and other heavy metals are among the main pollutants. It also receives 900 tonnes of sewage each day, of which only 12.5% is treated by the five sewage treatment stations located in the area.
Source: Based on Hardoy and Satterthwaite 1989.
Health Impacts of Microbial Pollution
Diseases arising from the ingestion of pathogens in contaminated water have the greatest impact worldwide. “An estimated 80% of all diseases, and over one-third of deaths in developing countries are caused by the consumption of contaminated water, and on average as much as one-tenth of each person’s productive time is sacrificed to water-related diseases” (UNCED 1992). Water-borne diseases are the largest single category of communicable diseases contributing to infant mortality in developing countries and second only to tuberculosis in contributing to adult mortality, with one million deaths per year.
The total annual number of cholera cases reported to the WHO by its member states has reached levels unprecedented during the seventh pandemic, with a peak of 595,000 cases in 1991 (WHO 1993). Table 1 shows the global morbidity and mortality rates of the major water-related diseases. These figures are, in many cases, grossly underestimated, since reporting of disease cases is done quite erratically by many countries.
Table 1. Global morbidity and mortality rates of main diseases related to water
|
Number/Year or Reporting Period |
||
|
Disease |
Cases |
Deaths |
|
Cholera - 1993 |
297,000 |
4,971 |
|
Typhoid |
500,000 |
25,000 |
|
Giardiasis |
500,000 |
Low |
|
Amoebiasis |
48,000,000 |
110,000 |
|
Diarrhoeal disease (under 5 years) |
1,600,000,000 |
3,200,000 |
|
Dracunculiasis (Guinea Worm) |
2,600,000 |
- |
|
Schistosomiasis |
200,000,000 |
200,000 |
Source: Galal-Gorchev 1994.
Health Impacts of Chemical Pollution
The health problems associated with chemical substances dissolved in water arise primarily from their ability to cause adverse effects after prolonged periods of exposure; of particular concern are contaminants that have cumulative toxic properties such as heavy metals and some organic micropollutants, substances that are carcinogenic and substances that may cause reproductive and developmental effects. Other dissolved substances in water are essential ingredients of dietary intake and yet others are neutral with regards to human needs. Chemicals in water, particularly in drinking water, may be classified into three typical categories for the purpose of health impact (Galal-Gorchev 1986):
- Substances exerting an acute or chronic toxicity upon consumption. The severity of the health impairment increases with the increase of their concentration in drinking water. On the other hand, below a certain threshold concentration no health effects can be observed—that is, the human metabolism can handle this exposure without measurable long-term effects. Various metals, nitrates, cyanides and so on fall within this category.
- Genotoxic substances, which cause health effects such as carcinogenicity, mutagenicity and birth-defects. According to present scientific thinking there is no threshold level which could be considered safe, since any amount of the substance ingested contributes to an increase in cancer and similar risks. Complex mathematical extrapolation models are used to determine such risks, since very little epidemiological evidence exists. Synthetic organics, many chlorinated organic micropollutants, some pesticides and arsenic fall within this category.
- For some elements, such as fluoride, iodine and selenium, the contribution made by drinking water is crucial and, if deficient, causes more or less severe health effects. At high concentrations, however, these same substances cause equally severe health effects, but of a different nature.
Environmental Impacts
The impacts of environmental pollution on freshwater quality are numerous and have existed for a long time. Industrial development, the advent of intensive agriculture, the exponential development of human populations and the production and use of tens of thousands of synthetic chemicals are among the main causes of water quality deterioration at local, national and global scales. The major issue of water pollution is the interference with actual or planned water uses.
One of the most severe and ubiquitous causes of environmental degradation is the discharge of organic wastes into watercourses (see “Biodegradable organic compounds” above). This pollution is mainly of concern in the aquatic environment where many organisms, for example fish, require high oxygen levels. A serious side effect of water anoxia is the release of toxic substances from particulates and bottom sediments in rivers and lakes. Other pollution effects from domestic sewage discharges into watercourses and aquifers include the build-up of nitrate levels in rivers and groundwaters, and the eutrophication of lakes and reservoirs (see above, “Nitrates” and “Salts”). In both cases, the pollution is a synergistic effect of sewage effluents and agricultural run-off or infiltration.
Economic Impacts
The economic consequences of water pollution can be rather severe due to detrimental effects on human health or on the environment. Impaired health often lowers human productivity, and environmental degradation reduces the productivity of water resources used directly by people.
The economic disease burden can be expressed not only in costs of treatment, but also in quantifying the loss of productivity. This is particularly true for primarily disabling diseases, such as diarrhoea or Guinea Worm. In India, for example, there are about 73 million workdays per year estimated to be lost due to water-related diseases (Arceivala 1989).
Deficiencies in sanitation and the resulting epidemics can also lead to severe economic penalties. This became most apparent during the recent cholera epidemic in Latin America. During the cholera epidemic in Peru, losses from reduced agricultural exports and tourism were estimated at one billion US dollars. This is more than three times the amount that the country had invested in water supply and sanitation services during the 1980s (World Bank 1992).
Water resources affected by pollution become less suitable as sources of water for municipal supply. As a consequence, expensive treatment has to be installed or clean water from far away has to be piped to the city at much higher costs.
In the developing countries of Asia and the Pacific, environmental damage was estimated by Economic and Social Commission for Asia and the Pacific (ESCAP) in 1985 to cost about 3% of the GNP, amounting to US$250 billion, while the cost of repairing such damage would range around 1%.
Land Pollution
The amount of waste produced by human society is increasing. Commercial and domestic solid waste is a great practical problem for many local governments. Industrial wastes are usually much smaller in volume but are more likely to contain hazardous materials, such as toxic chemicals, flammable liquids and asbestos. Although the total amount is less, the disposal of hazardous industrial waste has been a greater concern than of domestic waste because of the perceived hazard to health and the risk of environmental contamination.
The generation of hazardous waste has become a major problem worldwide. The root cause of the problem is industrial production and distribution. Land pollution occurs when hazardous wastes contaminate soil and groundwater due to inadequate or irresponsible disposal measures. Abandoned or neglected waste disposal sites are a particularly difficult and expensive problem for society. Sometimes, hazardous waste is disposed of illegally and in an even more dangerous manner because the owner cannot find a cheap way to get rid of it. One of the major unresolved issues in managing hazardous waste is to find methods of disposal that are both safe and inexpensive. Public concern over hazardous waste focuses on the potential health effects of exposure to toxic chemicals, and particularly the risk of cancer.
The Basel Convention passed in 1989 is an international agreement to control the transboundary movement of hazardous waste and to prevent dangerous wastes from being shipped for disposal to countries that do not have the facilities to process them safely. The Basel Convention requires that the generation of hazardous wastes and transboundary movement of the wastes be kept to a minimum. Traffic in hazardous wastes is subject to the informed permission and laws of the receiving country. Transboundary movement of hazardous wastes is subject to good environmental practices and assurance that the receiving country is able to handle them safely. All other traffic in hazardous wastes is considered illegal and therefore criminal in intent, subject to national laws and penalties. This international convention provides an essential framework for controlling the problem at an international level.
Hazardous Properties of Chemicals
Hazardous substances are compounds and mixtures that pose a threat to health and property because of their toxicity, flammability, explosive potential, radiation or other dangerous properties. Public attention tends to focus on carcinogens, industrial wastes, pesticides and radiation hazards. However, innumerable compounds that do not fall into these categories can pose a threat to the public’s safety and health.
Hazardous chemicals may present physical hazards, although this is more common in transportation and industrial incidents. Hydrocarbons may catch fire and even explode. Fires and explosions may generate their own toxic hazards depending on the chemicals that were initially present. Fires involving pesticide storage areas are a particularly dangerous situation, as the pesticides may be converted into even more highly toxic combustion products (such as paraoxons in the case of organophosphates) and substantial amounts of environmentally damaging dioxins and furans may be generated from combustion in the presence of chlorine compounds.
Toxicity, however, is the principal concern of most people with respect to hazardous waste. Chemicals may be toxic to human beings and they may also be damaging to the environment through toxicity to animal and plant species. Those that do not readily degrade in the environment (a characteristic called biopersistence) or that accumulate in the environment (a characteristic called bioaccumulation) are of particular concern.
The number and hazardous nature of toxic substances in common use has changed dramatically. In the last generation, research and development in organic chemistry and chemical engineering have introduced thousands of new compounds into widespread commercial use, including persistent compounds such as the polychlorinated biphenyls (PCBs), more potent pesticides, accelerators and plasticizers with unusual and poorly understood effects. The production of chemicals has risen dramatically. In 1941 production of all synthetic organic compounds in the United States alone, for example, was less than one billion kilograms. Today it is much greater than 80 billion kilograms. Many compounds in common use today underwent little testing and are not well understood.
Toxic chemicals are also much more intrusive in daily life than in the past. Many chemical plants or disposal sites which were once isolated or on the edge of town have become incorporated into urban areas by suburban growth. Communities now lie in closer proximity to the problem than they have in the past. Some communities are built directly over old disposal sites. Although incidents involving hazardous substances take many forms and may be highly individual, the great majority seem to involve a relatively narrow range of hazardous substances, which include: solvents, paints and coatings, metal solutions, polychlorinated biphenyls (PCBs), pesticides, and acids and alkalis. In studies conducted in the United States, the ten most common hazardous substances found in disposal sites requiring government intervention were lead, arsenic, mercury, vinyl chloride, benzene, cadmium, PCBs, chloroform, benzo(a)pyrene and trichloroethylene. However, chromium, tetrachloroethylene, toluene and di-2-ethylhexylphthalate were also prominent among those substances that could be shown to migrate or for which there was an opportunity for human exposure. The origin of these chemical wastes varies greatly and depends on the local situation, but typically elecroplating solutions, discarded chemicals, manufacturing by-products and waste solvents contribute to the waste stream.
Groundwater Contamination
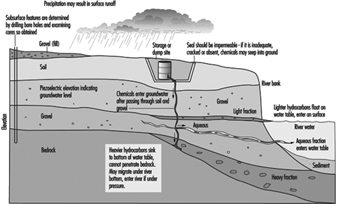
Figure 1 presents a cross-section of a hypothetical hazardous waste site to illustrate problems that may be encountered. (In practice, such a site should never be placed near a body of water or over a gravel bed.) In well-designed hazardous waste disposal (containment) facilities, there is an effectively impermeable seal to prevent hazardous chemicals from migrating out of the site and into the underlying soil. Such a site also has facilities to treat those chemicals that can be neutralized or transformed and to reduce the volume of waste that goes into the site; those chemicals that cannot be so treated are contained in impermeable containers. (Permeability, however, is relative, as described below.)
Figure 1. Cross-section of a hypothetical hazardous waste site
Chemicals may escape by leaking if the container is compromised, leaching if water gets in or spilling during handling or after the site is disturbed. Once they permeate the liner of a site, or if the liner is broken or if there is no liner, they enter the ground and migrate downward due to gravity. This migration is much more rapid through porous soil and is slow through clay and bedrock. Even underground, water flows downhill and will take the path of least resistance, and so the groundwater level will fall slightly in the direction of flow and the flow will be much faster through sand or gravel. If there is a water table under the ground, the chemicals will eventually reach it. Lighter chemicals tend to float on the groundwater and form an upper layer. Heavier chemicals and water-soluble compounds tend to dissolve or be carried along by the groundwater as it flows slowly underground through porous rock or gravel. The region of contamination, called the plume, can be mapped by drilling test wells, or bore holes. The plume slowly expands and moves in the direction of groundwater movement.
Surface water contamination may occur by runoff from the site, if the top layer of soil is contaminated, or by groundwater. When the groundwater feeds into a local body of water, such as a river or lake, the contamination is carried into this body of water. Some chemicals tend to deposit in the bottom sediment and others are carried along by the flow.
Groundwater contamination may take centuries to clear by itself. If shallow wells are used as a water source by local residents, there is a possibility of exposure by ingestion and by skin contact.
Human Health Concerns
People come into contact with toxic substances in many ways. Exposure to a toxic substance may occur at several points in the use cycle of the substance. People work in a plant where the substances arise as waste from an industrial process and do not change clothes or wash before coming home. They may reside near hazardous waste disposal sites which are illegal or poorly designed or managed, with opportunities for exposure as a result of accidents or careless handling or lack of containment of the substance, or lack of fencing to keep children off the site. Exposure may occur in the home as the result of consumer products that are mislabelled, poorly stored and not child-proof.
Three routes of exposure are by far the most important in considering the implications for toxicity of hazardous waste: inhalation, ingestion and absorption through the skin. Once absorbed, and depending on the route of exposure, there are many ways in which people can be affected by toxic chemicals. Obviously, the list of possible toxic effects associated with hazardous waste is very long. However, public concern and scientific studies have tended to concentrate on the risk of cancer and reproductive effects. In general, this has reflected the profile of chemical hazards at these sites.
There have been many studies of residents who live around or near such sites. With a few exceptions, these studies have shown remarkably little in the way of verifiable, clinically significant health problems. The exceptions have tended to be situations where the contamination is exceptionally severe and there has been a clear pathway of exposure of residents immediately adjacent to the site or who drink well water drawing on groundwater contaminated by the site. There are several likely reasons for this surprising absence of documentable health effects. One is that unlike air pollution and surface water pollution, the chemicals in land pollution are not easily available to people. People may live in areas highly contaminated by chemicals, but unless they actually come in contact with the chemicals by one of the routes of exposure mentioned above, no toxicity will result. Another reason may be that the chronic effects of exposure to these toxic chemicals take a long time to develop and are very difficult to study. Yet another reason may be that these chemicals are less potent in causing chronic health effects in humans than is usually supposed.
Notwithstanding the human health effects, the damage of land pollution to ecosystems may be very great. Plant and animal species, soil bacteria (which contribute to agricultural productivity) and other ecosystem constituents may be irreversibly damaged by degrees of pollution that are not associated with any visible human health effect.
Control of the Problem
Because of population distributions, land use restrictions, transportation costs and concern from society over environmental effects, there is intense pressure to find a solution to the problem of economical disposal of hazardous waste. This has led to increased interest in methods such as source reduction, recycling, chemical neutralization and secure hazardous waste disposal (containment) sites. The first two reduce the amount of waste that is produced. Chemical neutralization reduces the toxicity of the waste and may convert it into a more easily handled solid. Whenever possible, it is preferred that this be done at the site of production of the waste to reduce the amount of waste that must be moved. Well-designed hazardous waste disposal facilities, using the best available technologies of chemical processing and containment, are needed for the residual waste.
Secure hazardous waste containment sites are relatively expensive to build. The site needs to be selected carefully to ensure that pollution of surface water and major aquifers (groundwater) will not readily occur. The site must be designed and built with impermeable barriers to prevent contamination of soil and groundwater. These barriers are typically heavy plastic liners and layers of tamped clay fill under the holding areas. In reality, the barrier acts to delay breakthrough and to slow the permeation that eventually does occur to an acceptable rate, one that will not result in accumulation or significant pollution of groundwater. Permeability is a property of the material, described in terms of the resistance of the material to a liquid or gas penetrating it under given conditions of pressure and temperature. Even the least permeable barrier, such as plastic liners or packed clay, will eventually allow the passage of some liquid chemical through the barrier, although it may take years and even centuries, and once breakthrough occurs the flow becomes continuous, although it may occur at a very low rate. This means that groundwater immediately below a hazardous waste disposal site is always at some risk of contamination, even if it is very small. Once groundwater is contaminated, it is very difficult and often impossible to decontaminate.
Many hazardous waste disposal sites are regularly monitored with collection systems and by testing nearby wells to ensure that pollution is not spreading. The more advanced are built with recycling and processing facilities on-site or nearby to further reduce the waste that goes into the disposal site.
Hazardous waste containment sites are not a perfect solution to the problem of land pollution. They require expensive expertise to design, are expensive to build, and may require monitoring, which creates an ongoing cost. They do not guarantee that groundwater contamination will not occur in the future, although they are effective in minimizing this. A major disadvantage is that someone, inevitably, must live near one. Communities where hazardous waste sites are located or proposed to be located usually oppose them strongly and make it difficult for governments to grant approval. This is called the “not in my back yard” (NIMBY) syndrome and is a common response to the siting of facilities considered undesirable. In the case of hazardous waste sites, the NIMBY syndrome tends to be especially strong.
Unfortunately, without hazardous waste containment sites, society may lose control of the situation entirely. When no hazardous waste site is available, or when it is too expensive to use one, hazardous waste is often disposed of illegally. Such practices include pouring liquid waste on the ground in remote areas, dumping the waste into drains that go into local waterways and shipping the waste to jurisdictions that have more lax laws governing the handling of hazardous waste. This may create an even more dangerous situation than a poorly managed disposal site would create.
There are several technologies that can be used to dispose of the remaining waste. High-temperature incineration is one of the cleanest and most effective means of disposing of hazardous waste, but the cost of these facilities is very high. One of the more promising approaches has been to incinerate liquid toxic waste in cement kilns, which operate at the necessary high temperatures and are found throughout the developing as well as the developed world. Injection into deep wells, below the water table, is one option for chemicals that cannot be disposed of in any other way. However, groundwater migration can be tricky and sometimes unusual pressure situations underground or leaks in the well lead to groundwater contamination anyway. Dehalogenation is a chemical technology that strips the chlorine and bromine atoms from halogenated hydrocarbons, such as PCBs, so that they can be easily disposed of by incineration.
A major unresolved issue in municipal solid waste handling is contamination by hazardous waste discarded by accident or intent. This can be minimized by diverting disposal into a separate waste stream. Most municipal solid waste systems divert chemical and other hazardous wastes so that they do not contaminate the solid waste stream. The separate waste stream should, ideally, be diverted to a secure hazardous waste disposal site.
There is a pressing need for facilities to collect and properly dispose of small quantities of hazardous waste, at minimal cost. Individuals who find themselves in possession of a bottle or can of solvents, pesticides or some unknown powder or fluid usually cannot afford the high cost of proper disposal and do not understand the risk. Some system for collecting such hazardous waste from consumers is needed before it is poured on the ground, flushed down the toilet or burned and released into the air. A number of municipalities sponsor “toxic roundup” days, when residents bring small quantities of toxic materials to a central location for safe disposal. Decentralized systems have been introduced in some urban areas, involving home or local pick-up of small quantities of toxic substances to be discarded. In the United States, experience has shown that people are willing to drive up to five miles to dispose of household toxic wastes safely. Consumer education to promote awareness of the potential toxicity of common products is urgently needed. Pesticides in aerosol cans, bleaches, household cleaners and cleaning fluids are potentially dangerous, especially to children.
Abandoned Hazardous Waste Disposal Sites
Abandoned or insecure hazardous waste sites are a common problem worldwide. Hazardous waste sites that need to be cleaned up are great liabilities to society. The ability of countries and local jurisdictions to clean up major hazardous waste sites varies greatly. Ideally, the owner of the site or the person who created the site should pay for its clean-up. In practice, such sites have often changed hands and the past owners have often gone out of business, the current owners may not have the financial resources to clean up, and the clean-up effort tends to be delayed for very long periods by expensive technical studies followed by legal battles. Smaller and less affluent countries have little leverage in negotiating clean-ups with the current site owners or the responsible parties, and no substantial resources to clean up the site.
The traditional approaches to cleaning up hazardous waste sites are very slow and expensive. It requires highly specialized expertise that is often in short supply. A hazardous waste site is first evaluated to determine how serious the land pollution is and whether the groundwater is contaminated. The likelihood of residents coming into contact with hazardous substances is determined and, in some cases, an estimate of the risk to health that this poses is calculated. Acceptable clean-up levels must be decided upon, the extent to which exposure must ultimately be reduced to protect human health and the environment. Most governments make decisions about clean-up levels by applying various applicable environmental laws, air pollution standards, drinking water standards, and based on a hazards assessment of health risks posed by the particular site. Clean-up levels are therefore set to reflect both health and environmental concerns. A decision must be made on how the site is to be remediated, or how best to achieve this reduction in exposure. Remediation is a technical problem of achieving these clean-up levels by engineering and other methods. Some of the techniques that are used include incineration, solidification, chemical treatment, evaporation, repeated flushing of soil, biodegradation, containment, removal of soil off-site and pumping out groundwater. These engineering options are too complex and specific to the circumstances to describe in detail. Solutions must fit the particular situation and the funds available to achieve control. In some cases, remediation is not feasible. A decision then has to be made on what land use will be permitted on the site.
Air Pollution
The problem of air pollution has grown steadily since the Industrial Revolution began 300 years ago. Four major factors have exacerbated air pollution: growing industrialization; increasing traffic; rapid economic development; and higher levels of energy consumption. The available information shows that the WHO guidelines for the major air pollutants are regularly exceeded in many major urban centres. Although progress has been made in controlling air pollution problems in many industrialized countries over the last two decades, air quality—particularly in the larger cities in the developing world—is worsening. Of major concern are the adverse health effects of ambient air pollutants in many urban areas, where levels are sufficiently high to contribute to increased mortality and morbidity, deficits in pulmonary function and cardiovascular and neurobehavioural effects (Romieu, Weizenfeld and Finkelman 1990; WHO/UNEP 1992). Indoor air pollution due to domestic combustion products is also a major issue in developing countries (WHO 1992b), but it is not part of this review, which considers only the sources, dispersion and health effects of outdoor air pollution, and includes a case study of the situation in Mexico.
Source of Air Pollutants
The most common air pollutants in urban environments include sulphur dioxide (SO2), suspended particulate matter (SPM), the nitrogen oxides (NO and NO2, collectively termed NOX), ozone (O3), carbon monoxide (CO) and lead (Pb). Combustion of fossil fuels in stationary sources leads to the production of SO2, NOX and particulates, including sulphate and nitrate aerosols formed in the atmosphere following gas to particle conversion. Petrol-fuelled motor vehicles are the principal sources of NOX, CO and Pb, whereas diesel-fuelled engines emit significant quantities of particulates, SO2 and NOX. Ozone, a photochemical oxidant and the main constituent of photochemical smog, is not emitted directly from combustion sources but is formed in the lower atmosphere from NOX and volatile organic compounds (VOCs) in the presence of sunlight (UNEP 1991b). Table 1 presents the major sources of outdoor air pollutants.
Table 1. Major sources of outdoor air pollutants
Pollutants Sources
Sulphur oxides Coal and oil combustion, smelters
Suspended particulate matter Combustion products (fuel, biomass), tobacco smoke
Nitrogen oxides Fuel and gas combustion
Carbon monoxide Incomplete petrol and gas combustion
Ozone Photochemical reaction
Lead Petrol combustion, coal combustion, producing batteries, cables, solder, paint
Organic substances Petrochemical solvents, vaporization of unburnt fuels
Source: Adapted from UNEP 1991b.
Dispersion and Transport of Air Pollutants
The two major influences on the dispersion and transport of air pollutant emissions are the meteorology (including microclimate effects such as “heat islands”) and the topography in relation to the population distribution. Many cities are surrounded by hills which may act as a downwind barrier, trapping pollution. Thermal inversions contribute to a particulate problem in temperate and cold climates. Under normal dispersion conditions, hot pollutant gases rise as they come into contact with colder air masses with increasing altitude. However, under certain circumstances the temperature may increase with altitude, and an inversion layer forms, trapping pollutants close to the emission source and delaying their diffusion. Long-range transport of air pollution from large urban areas may have national and regional impacts. Oxides of nitrogen and sulphur may contribute to acid deposition at great distances from the emission source. Ozone concentrations are often elevated downwind of urban areas due to the time lag involved in photochemical processes (UNEP 1991b).
Health Effects of Air Pollutants
Pollutants and their derivatives can cause adverse effects by interacting with and impairing molecules crucial to the biochemical or physiological processes of the human body. Three factors influence the risk of toxic injury related to these substances: their chemical and physical properties, the dose of the material that reaches the critical tissue sites and the responsiveness of these sites to the substance. The adverse health effects of air pollutants may also vary across population groups; in particular, the young and the elderly may be especially susceptible to deleterious effects. Persons with asthma or other pre-existing respiratory or cardiac diseases may experience aggravated symptoms upon exposure (WHO 1987).
Sulphur Dioxide and Particulate Matter
During the first half of the twentieth century, episodes of marked air stagnation resulted in excess mortality in areas where fossil-fuel combustion produced very high levels of SO2 and SMP. Studies of long-term health effects have also related the annual mean concentrations of SO2 and SMP to mortality and morbidity. Recent epidemiological studies have suggested an adverse effect of inhalable particulate levels (PM10) at relatively low concentrations (not exceeding the standard guidelines) and have shown a dose-response relationship between exposure to PM10 and respiratory mortality and morbidity (Dockery and Pope 1994; Pope, Bates and Razienne 1995; Bascom et al. 1996) as shown in table 2.
Table 2. Summary of short-term exposure-response relationship of PM10 with different health effects indicators
|
Health effect |
% changes for each 10 μg/m3 |
|
|
Mean |
Range |
|
|
Mortality |
||
|
Total |
1.0 |
0.5-1.5 |
|
Cardiovascular |
1.4 |
0.8-1.8 |
|
Respiratory |
3.4 |
1.5-3.7 |
|
Morbidity |
||
|
Hospital admission for respiratory condition |
1.1 |
0.8-3.4 |
|
Emergency visits for respiratory conditions |
1.0 |
0.5-4 |
|
Symptom exacerbations among asthmatics |
3.0 |
1.1-11.5 |
|
Changes in peak expiratory flow |
0.08 |
0.04-0.25 |
Nitrogen Oxides
Some epidemiological studies have reported adverse health effects of NO2 including increased incidence and severity of respiratory infections and increase in respiratory symptoms, especially with long-term exposure. Worsening of the clinical status of persons with asthma, chronic obstructive pulmonary disease and other chronic respiratory conditions has also been described. However, in other studies, investigators have not observed adverse effects of NO2 on respiratory functions (WHO/ECOTOX 1992; Bascom et al. 1996).
Photochemical Oxidants and Ozone
The health effects of photochemical oxidants exposure cannot be attributed only to oxidants, because photochemical smog typically consists of O3, NO2, acid and sulphate and other reactive agents. These pollutants may have additive or synergistic effects on human health, but O3 appears to be the most biologically active. Health effects of ozone exposure include decreased pulmonary function (including increased airway resistance, reduced air flow, decreased lung volume) due to airway constriction, respiratory symptoms (cough, wheezing, shortness of breath, chest pains), eye, nose and throat irritation, and disruption of activities (such as athletic performance) due to less oxygen availability (WHO/ECOTOX 1992). Table 3 summarizes the major acute health effects of ozone (WHO 1990a, 1995). Epidemiological studies have suggested a dose-response relationship between exposure to increasing ozone levels and the severity of respiratory symptoms and the decrement in respiratory functions (Bascom et al. 1996).
Table 3. Health outcomes associated with changes in peak daily ambient ozone concentration in epidemiological studies
|
Health outcome |
Changes in |
Changes in |
|
Symptom exacerbations among healthy children |
||
|
25% increase |
200 |
100 |
|
50% increase |
400 |
200 |
|
100% increase |
800 |
300 |
|
Hospital admissions for respiratory |
||
|
5% |
30 |
25 |
|
10% |
60 |
50 |
|
20% |
120 |
100 |
a Given the high degree of correlation between the 1-h and 8-h O3 concentrations in field studies, an improvement in health risk associated with decreasing 1- or 8-h O3 levels should be almost identical.
Source: WHO 1995.
Carbon Monoxide
The main effect of CO is to decrease oxygen transport to the tissues through the formation of carboxyhaemoglobin (COHb). With increasing levels of COHb in blood, the following health effects can be observed: cardiovascular effects in subjects with previous angina pectoris (3 to 5%); impairment of vigilance tasks (>5%); headache and dizziness (≥10%); fibrinolysis and death (WHO 1987).
Lead
Lead exposure principally affects haem biosynthesis, but also may act on the nervous system and other systems such as the cardiovascular system (blood pressure). Infants and young children less than five years old are particularly sensitive to lead exposure because of its effect on neurological development at blood lead levels close to 10 μg/dl (CDC 1991).
Several epidemiological studies have investigated the effect of air pollution, especially ozone exposure, on the health of the population of Mexico City. Ecological studies have shown an increase in mortality with respect to exposure to fine particulates (Borja-Arburto et al. 1995) and an increase in emergency visits for asthma among children (Romieu et al. 1994). Studies of the adverse effect of ozone exposure conducted among healthy children have shown an increase in school absenteeism due to respiratory illnesses (Romieu et al. 1992), and a decrease in lung function after both acute and subacute exposure (Castillejos et al. 1992, 1995). Studies conducted among asthmatic children have shown an increase in respiratory symptoms and a decrease in peak expiratory flow rate after exposure to ozone (Romieu et al. 1994) and to fine particulate levels (Romieu et al. in press). Although, it seems clear that acute exposure to ozone and particulates is associated with adverse health effects in the population of Mexico City, there is a need to evaluate the chronic effect of such exposure, in particular given the high levels of photo-oxidants observed in Mexico City and the ineffectiveness of control measures.
Case study: Air pollution in Mexico City
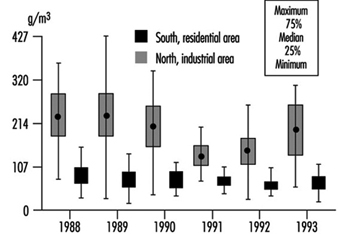
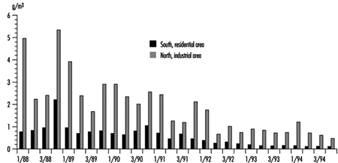
The metropolitan area of Mexico City (MAMC) is situated in the Mexican Basin at a mean altitude of 2,240 metres. The basin covers 2,500 square kilometres and is surrounded by mountains, two of which are over 5,000 metres high. The total population was estimated at 17 million in 1990. Due to the particular geographic characteristics and the light winds, ventilation is poor with a high frequency of thermic inversions, especially during the winter. More than 30,000 industries in the MAMC and the three million motor vehicles circulating daily are responsible for 44% of the total energy consumption. Since 1986, air pollution has been monitored, including SO2, NOx, CO, O3, particulate matter and non-methane hydrocarbon (HCNM). The main air pollutant problems are related to ozone, especially in the southwest part of the city (Romieu et al. 1991). In 1992 the Mexican norm for ozone (110 ppb one-hour maximum) was exceeded in the southwest part more than 1,000 hours and reached a maximum of 400 ppb. Particulate levels are high in the northeast section of the city, close to the industrial park. In 1992, the annual average of inhalable particulate (PM10) was 140 μg/m3. Since 1990, important control measures have been taken by the government to decrease air pollution, including a programme that prohibits use of cars one day a week depending on their terminating licence plate number, the closure of one of the most polluting refineries located in Mexico City, and the introduction of unleaded fuel. These measures have led to a decrease in various air pollutants, mainly SO2, particulate matter, NO2, CO and lead. However the ozone level remains a major problem (see figure 1, figure 2 and figure 3).
Figure 1. Ozone levels in two zones of Mexico City. One-hour daily maximum by month, 1994
Figure 2. Particulates (PM10) in two zones of Mexico City, 1988-1993
Figure 3. Air lead levels in two zones of Mexico City, 1988-1994
Developing Countries and Pollution
Industrial pollution is a more complicated problem in developing countries than in developed economies. There are greater structural obstacles to preventing and cleaning up pollution. These obstacles are largely economic, because developing countries do not have the resources to control pollution to the extent that developed countries can. On the other hand, the effects of pollution may be very costly to a developing society, in terms of health, waste, environmental degradation, reduced quality of life and clean-up costs in the future. An extreme example is concern for the future of children exposed to lead in some megacities in countries where leaded gasoline is still used, or in the vicinity of smelters. Some of these children have been found to have blood lead levels high enough to impair intelligence and cognition.
Industry in developing countries usually operates short of capital compared to industry in developed countries, and those investment funds that are available are first put into the equipment and resources necessary for production. Capital that is applied toward control of pollution is considered “unproductive” by economists because such investment does not lead to increased production and financial return. However, the reality is more complicated. Investment in control of pollution may not bring an obvious direct return on investment to the company or industry, but that does not mean that there is no return on investment. In many cases, as in an oil refinery, control of pollution also reduces the amount of wastage and increases the efficiency of the operation so that the company does benefit directly. Where public opinion carries weight and it is to the advantage of a company to maintain good public relations, industry may make an effort to control pollution in its own interest. Unfortunately, the social structure in many developing countries does not favour this because the people most negatively affected by pollution tend to be those who are impoverished and marginalized in society.
Pollution may damage the environment and society as a whole, but these are “externalized dis-economies” that do not substantially hurt the company itself, at least not economically. Instead, the costs of pollution tend to be carried by society as a whole, and the company is spared the costs. This is particularly true in situations where the industry is critical to the local economy or national priorities, and there is a high tolerance for the damage it causes. One solution would be to “internalize” the external dis-economies by incorporating the costs of clean-up or the estimated costs of environmental damage into the operating costs of the company as a tax. This would give the company a financial incentive to control its costs by reducing its pollution. Virtually no government in any developing country is in a position to do this and to enforce the tax, however.
In practice, capital is rarely available to invest in equipment to control pollution unless there is pressure from government regulation. However, governments are rarely motivated to regulate industry unless there are compelling reasons to do so, and pressure from their citizens. In most developed countries, people are reasonably secure in their health and their lives, and expect a higher quality of life, which they associate with a cleaner environment. Because there is more economic security, these citizens are more willing to accept an apparent economic sacrifice in order to achieve a cleaner environment. However, in order to be competitive in world markets, many developing countries are very reluctant to impose regulation on their industries. Instead, they hope that industrial growth today will lead to a society rich enough tomorrow to clean up the pollution. Unfortunately, the cost of clean-up increases as fast as, or faster than, the costs associated with industrial development. At an early stage of industrial development, a developing country would in theory have very low costs associated with the prevention of pollution, but hardly ever do such countries have the capital resources they need to do so. Later, when such a country does have the resources, the costs are often staggeringly high and the damage has already been done.
Industry in developing countries tends to be less efficient than in developed countries. This lack of efficiency is a chronic problem in developing economies, reflecting untrained human resources, the cost of importing equipment and technology, and the inevitable wastage that occurs when some parts of the economy are more developed than others.
This inefficiency is also based in part on the need to rely on outdated technologies which are freely available, do not require an expensive licence or that do not cost as much to use. These technologies are often more polluting than the state-of-the-art technologies available to industry in developed countries. An example is the refrigeration industry, where the use of chlorofluorocarbons (CFCs) as refrigerant chemicals is much cheaper than the alternatives, despite the serious effects of these chemicals in depleting ozone from the upper atmosphere and thereby reducing the earth’s shield from ultraviolet radiation; some countries had been very reluctant to agree to prohibit the use of CFCs because it would then be economically impossible for them to manufacture and purchase refrigerators. Technology transfer is the obvious solution, but companies in developed countries who developed or hold the licence for such technologies are understandably reluctant to share them. They are reluctant because they spent their own resources developing the technology, wish to retain the advantage they have in their own markets by controlling such technology, and may make their money from using or selling the technology only during the limited term of the patent.
Another problem faced by developing countries is lack of expertise in and awareness of the effects of pollution, monitoring methods and the technology of pollution control. There are relatively few experts in the field in developing countries, in part because there are fewer jobs and a smaller market for their services even though the need may actually be greater. Because the market for pollution control equipment and services may be small, this expertise and technology may have to be imported, adding to the costs. General recognition of the problem by managers and supervisors in industry may be lacking or very low. Even when an engineer, manager or supervisor in industry realizes that an operation is polluting, it may be difficult to persuade others in the company, their bosses or the owners that there is a problem that must be solved.
Industry in most developing countries competes at the low end of international markets, meaning that it produces products that are competitive on the basis of price and not quality or special features. Few developing countries specialize in making very fine grades of steel for surgical instruments and sophisticated machinery, for example. They manufacture lesser grades of steel for construction and manufacturing because the market is much larger, the technical expertise required to produce it is less, and they can compete on the basis of price as long as the quality is good enough to be acceptable. Pollution control reduces the price advantage by increasing the apparent costs of production without increasing output or sales. The central problem in developing countries is how to balance this economic reality against the need to protect their citizens, the integrity of their environment, and their future, realizing that after development the costs will be even higher and the damage may be permanent.
Industrial Pollution in Developing Countries
While industrialization is an essential feature of economic growth in developing countries, industrial practices may also produce adverse environmental health consequences through the release of air and water pollutants and the disposal of hazardous wastes. This is often the case in developing countries, where less attention is paid to environmental protection, environmental standards are often inappropriate or not effectively implemented, and pollution control techniques are not yet fully developed. With rapid economic development, many developing countries, like China and other Asian countries, face some additional environmental problems. One is the environmental pollution from hazardous industries or technologies transferred from developed countries, which are no longer acceptable for occupational and environmental health reasons in developed countries, but still allowable in developing countries due to looser environmental legislation. Another problem is the rapid proliferation of informal small-scale enterprises in townships as well as in rural areas, which often create serious air and water pollution because of lack of sufficient knowledge and funds.
Air Pollution
Air pollution in developing countries is derived not only from stack emission of pollutants from relatively large industries, like iron and steel, non-ferrous metals and petroleum products industries, but also from fugitive emission of pollutants from small-scale factories, such as cement mills, lead refineries, chemical fertilizer and pesticide factories and so on, where inadequate pollution control measures exist and pollutants are allowed to escape to the atmosphere.
Since industrial activities always involve energy generation, the combustion of fossil fuels is a main source of air pollution in the developing countries, where coal is widely used not only for industrial, but also for domestic consumption. For instance, in China, more than 70% of total energy consumption relies on direct coal combustion, from which large amounts of pollutants (suspended particulates, sulphur dioxide, etc.) are emitted under incomplete combustion and inadequate emission controls.
The kinds of air pollutants emitted vary from industry to industry. The concentrations of different pollutants in the atmosphere also vary widely from process to process, and from place to place with different geographic and climatic conditions. It is difficult to estimate specific exposure levels of various pollutants from different industries to the general population in developing countries, as elsewhere. In general, the workplace exposure levels are much higher than that of the general population, because the emissions are rapidly diluted and dispersed by the wind. But the exposure duration of the general population is much longer than that of workers.
The exposure levels of the general population in developing countries are usually higher than that in developed countries, where air pollution is more strictly controlled and resident areas are usually far from industries. As discussed further on in this chapter, a large number of epidemiological studies have already showed the close association of reduction in pulmonary function and increased incidence of chronic respiratory diseases among residents with long-term exposure to the common air pollutants.
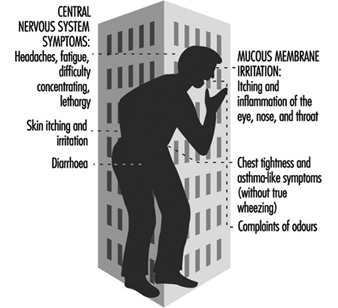
A case study of air pollution effects on the health of 480 primary school children in Cubatao, Brazil, where large quantities of mixed pollutants were emitted from 23 industries (steel mill, chemical industries, cement factory, fertilizer plants, etc.), showed that 55.3% of the children had decreases in pulmonary function. Another example of health effects of air pollution appeared in the Ulsan/Onsan special industrial zone, Republic of Korea, where many large-scale plants (mainly petrochemical plants and metal refineries) are concentrated. Local residents complained of a variety of health problems, particularly of the nervous system disorder called “Onsan Disease”.
Accidental releases of toxic substances into the atmosphere resulting in serious health risks are usually more common in developing countries. The reasons include inadequate safety planning, lack of skilled technical personnel to maintain proper facilities, and difficulties in obtaining spare parts and so on. One of the worst of such accidents occurred in Bhopal, India, in 1984, where leaking methyl isocyanide killed 2,000 people.
Water and Soil Pollution
Inappropriate and often careless disposal of industrial wastes—uncontrolled discharge into watercourses and uncontrolled disposal on the land, which often causes water and soil pollution—is another crucial environmental health problem, in addition to industrial air pollution, in developing countries, particularly with numerous small-scale township enterprises, like those in China. Some small-scale factories, such as textile dyeing, pulp and paper, leather tanning, electroplating, fluorescent lamp, lead battery and metal smelting, always produce a large amount of wastes, containing toxic or hazardous substances like chromium, mercury, lead, cyanide and so on, which may pollute the rivers, streams and lakes, and soil as well, when they are untreated. The soil pollution in turn may contaminate groundwater resources.
In Karachi, the Lyan river, which runs through the city, has become an open drain of sewage and untreated industrial effluent from some 300 large and small industries. There is a similar case in Shanghai. Some 3.4 million cubic metres of industrial and domestic waste pour into Suzhou creek and Huangpu river, which flow through the heart of the city. Because of serious pollution, the river and creek have essentially become devoid of life and often produce smells and sights that are unpleasant and offensive to the public living in the surrounding area.
A further problem of water and soil pollution in developing countries is the transfer of toxic or hazardous wastes from developed to developing countries. The cost of transporting these wastes to simple storage sites in developing countries is a mere fraction of the cost required for safely storing or incinerating them in their countries of origin in compliance with the applicable government regulations there. This has occurred in Thailand, Nigeria, Guinea-Bissau and so on. The toxic wastes inside the barrels can leak and pollute the air, water and soil, posing a potential health risk to the people living in the vicinity.
Thus the environmental health problems discussed in this chapter tend to apply to an even greater extent to developing countries.
Food and Agriculture
This article has been prepared by Dr F. Käferstein, Chief, Food Safety, World Health Organization. It is entirely based on the report of a WHO Panel on Food and Agriculture which had supported the WHO Commission on Health and Environment to prepare a report for the United Nations Conference on Environment and Development (UNCED), Rio de Janeiro, 1992. Both reports are available from the WHO.
Production Needs in the Face of Population Pressure and Other Forces
Rapid population growth continues in some regions of the world. As compared with the situation in 1990, by the year 2010 there will be an extra 1,900 million people to be fed, a rise of 36% from 5,300 to 7,200 million people.
Ninety per cent of the entire projected growth over the next 20 years is expected to take place in the countries which are currently classified as developing nations. Progressive urbanization of society is taking place. The urban population of the world will reach 3,600 million, a rise of 62% from the 2,200 million city dwellers in 1990. Moreover the urban population of developing countries will increase by 92% (from 1,400 million to 2,600 million) in the twenty years from 1990, a fourfold increase since 1970. Even if family planning receives the urgent attention that it desperately requires from all rapidly growing populations, population growth and urbanization will continue to dominate the scene for the next two decades.
A 36% increase in food, other agricultural products and potable water will be required over the next twenty years simply to match the rise in population; the need for half a billion people to be properly fed instead of remaining undernourished, and the greater demand from populations with a rising income, will all lead to a vast increase in total food production. An excessive demand for food of animal origin will continue to characterize people in the higher income groups, leading to increases in animal feed production.
The pressure on agriculture and food production, as both population and per capita demand increase, will lead to a greater burden on the environment. This burden will be unevenly generated and have uneven environmental effects. Globally, these will be adverse and will require concerted action.
This increased demand will fall on resources of land and water which are finite, where the most productive areas have already been used, and where the cost of bringing marginal land into production, and of using less readily available water, will be high. Much of this marginal land may have only temporary fertility unless specific measures are taken to maintain it, while the productivity of natural fisheries is also sharply limited. The area of arable land will decrease due to soil erosion from over-grazing; laterization of clearfelled areas; soil salinization and other types of land degradation; and the expansion of urban, industrial and other developments.
Water availability and quality, already totally inadequate in much of the world, will remain major problems for rural areas of developing countries and also for many urban populations, who may face the additional problem of high utilization charges. Needs for water will increase greatly, and for several large cities the meeting of water demands will become increasingly costly as supplies will have to be brought from far away. Re-use of water implies more stringent standards for treatment. The increasing production of wastewater and sewage will require more extensive treatment facilities, as well as large outlays of capital.
The continuing long-term need for industrial development to produce goods, services and employment will lead to more intensive food production, which will itself become more industrialized. Consequently, and especially because of urbanization, the demand for, and the resources employed in, packaging, processing, storage and distribution of food will increase in volume and importance.
The public is becoming much more aware of the need to produce, protect and market food in ways which minimize adverse change in our environment, and is more demanding in this respect. The emergence of revolutionary scientific tools (e.g., biotechnological advances) offers the possibility of significantly increasing food production, reducing waste and enhancing safety.
The principal challenge is to meet the increasing demands for food, other agricultural products and water in ways that foster long-term improvements in health, and which are also sustainable, economical and competitive.
Despite the fact that globally there is at present sufficient food for all, great difficulties have to be overcome to ensure the availability and equitable distribution of safe, nutritious and affordable food supplies to meet health needs in many parts of the world, and notably in areas of rapid population growth.
There is often a failure to take the possible health consequences fully into account in the design and implementation of agricultural and fisheries policies and programmes. An example is the production of tobacco, which has very serious and negative impacts on human health and on scarce land and fuelwood resources. Moreover, the lack of an integrated approach to development of the agriculture and forestry sectors results in failure to recognize the important relationship of both sectors to the protection of wildlife habitats, biological diversity and genetic resources.
If timely and appropriate action is not taken to mitigate the environmental impacts of agriculture, fisheries, food production and water use, then the following situations will prevail:
- As the urban population increases, the difficulty of maintaining and extending an efficient food distribution system will become greater. This may increase the prevalence of household food insecurity, associated malnutrition and health risks among the growing masses of urban poor.
- Microbial, viral and parasitic diseases from contaminated food and water will continue to be serious health problems. New agents of public health importance will continue to emerge. The diarrhoeal diseases related to food and water, causing high infant mortality and universal morbidity, will increase.
- Vector-borne diseases from irrigation, other water resource developments, and uncontrolled wastewater will increase substantially. Malaria, schistosomiasis, filariasis and arbovirus fevers will continue to be major problems.
- The problems outlined above will be reflected in static or rising levels of infant and young child malnutrition and mortality, as well as morbidity at all ages, but predominantly among the poor, the very young, the aged and the sick.
- diseases linked to inappropriate life-styles, smoking and diet (for example, obesity, diabetes or coronary heart disease), which are characteristic of the more affluent countries, are now emerging and becoming significant problems also in developing countries. The increasing urbanization will accelerate this trend.
- As the intensity of food production increases, the risk of occupational diseases and accidents among those working in this and related sectors will increase substantially unless sufficient efforts for safety and prevention are made.
Health Consequences of Biological Contamination and Chemicals in Food
Despite progress in science and technology, contaminated food and water remain to this day major public health problems. Foodborne diseases are perhaps the most widespread health problems in the contemporary world and important causes of reduced economic productivity (WHO/FAO 1984). They are caused by a wide range of agents, and cover all degrees of severity, from mild indispositions to life-threatening illnesses. However, only a small proportion of cases comes to the notice of health services and even fewer are investigated. As a result, it is believed that in industrialized countries only approximately 10% of the cases are reported, whilst in developing countries reported cases probably account for not more than 1% of the total.
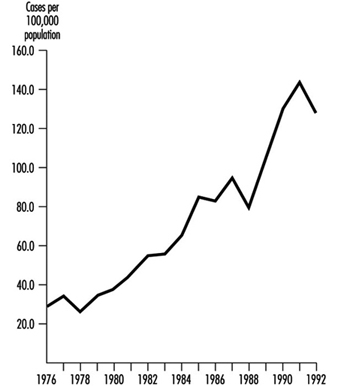
Despite these limitations, the data that are available indicate that foodborne diseases are increasing all over the world, both in developing and industrialized countries. Experience in Venezuela illustrates this trend (PAHO/WHO 1989) (figure 1).
Figure 1. Foodborne diseases in Venezuela
Developing countries
Available information clearly indicates that biological contaminants (bacteria, viruses and parasites) are the major causes of foodborne diseases (table 1).
Table 1. Some agents of important foodborne diseases and salient epidemiological features
|
Agents |
Important reservoir/carrier |
Transmissiona by |
Multiplication |
Examples of some incriminated foods |
||
|
Water |
Food |
Person to person |
||||
|
Bacteria |
||||||
|
Baccillus cereus |
Soil |
- |
+ |
- |
+ |
Cooked rice, cooked meats, vegetables, |
|
Brucella species |
Cattle, goats, sheep |
- |
+ |
- |
+ |
Raw milk, dairy products |
|
Campylobacter jejuni |
Chickens, dogs, cats, cattle, |
+ |
+ |
+ |
-b |
Raw milk, poultry |
|
Clostridium botulinum |
Soil, mammals, birds, fish |
- |
+ |
- |
+ |
Fish, meat, vegetables (home preserved), |
|
Clostridium perfringens |
Soil, animals, humans |
- |
+ |
- |
+ |
Cooked meat and poultry, gravy, beans |
|
Escherichia coli |
||||||
|
Enterotoxigenic |
Humans |
+ |
+ |
+ |
+ |
Salad, raw vegetables |
|
Enteropathogenic |
Humans |
+ |
+ |
+ |
+ |
Milk |
|
Enteroinvasive |
Humans |
+ |
+ |
0 |
+ |
Cheese |
|
Enterohaemorrhagic |
Cattle, poultry, sheep |
+ |
+ |
+ |
+ |
Undercooked meat, raw milk, cheese |
|
Listeria monocytogenes |
Environment |
+ |
+ |
-c |
+ |
Cheese, raw milk, coleslaw |
|
Mycobacterium bovis |
Cattle |
- |
+ |
- |
- |
Raw milk |
|
Salmonella typhi and |
Humans |
+ |
+ |
± |
+ |
Dairy products, meat products, shellfish, |
|
Salmonella (non-typhi) |
Humans and animals |
± |
+ |
± |
+ |
Meat, poultry, eggs, dairy products, |
|
Shigella spp. |
Humans |
+ |
+ |
+ |
+ |
Potato/egg salads |
|
Staphylococcus aureus |
- |
+ |
- |
+ |
Ham, poultry and egg salads, cream-filled |
|
|
Vibrio cholerae, 01 |
Humans, marine life |
+ |
+ |
± |
+ |
Salad, shellfish |
|
Vibrio cholerae, non-01 |
Humans, marine life |
+ |
+ |
± |
+ |
Shellfish |
|
Vibrio parahaemolyticus |
Sea water, marine life |
- |
+ |
- |
+ |
Raw fish, crabs, and other shellfish |
|
Vibrio vulnificus |
Sea water, marine life |
+ |
+ |
- |
+ |
Shellfish |
|
Yersinia enterocolitica |
Water, wild animals, pigs, |
+ |
+ |
- |
+ |
Milk, pork, and poultry |
|
Viruses |
||||||
|
Hepatitis A virus |
Humans |
+ |
+ |
+ |
- |
Shellfish, raw fruit and vegetables |
|
Norwalk agents |
Humans |
+ |
+ |
- |
- |
Shellfish, salad |
|
Rotavirus |
Humans |
+ |
+ |
+ |
- |
0 |
|
Protozoa |
+ |
+ |
+ |
+ |
||
|
Cryptosporidium parvum |
Humans, animals |
+ |
+ |
+ |
- |
Raw milk, raw sausage (non-fermented) |
|
Entamoeba histolytica |
Humans |
+ |
+ |
+ |
- |
Vegetables and fruits |
|
Giardia lamblia |
Humans, animals |
+ |
± |
+ |
- |
Vegetables and fruits |
|
Toxoplasma gondii |
Cats, pigs |
0 |
+ |
- |
- |
Undercooked meat, raw vegetables |
|
Helminths |
||||||
|
Ascaris lumbricoides |
Humans |
+ |
+ |
- |
- |
Soil-contaminated food |
|
Clonorchis sinensis |
Freshwater fish |
- |
+ |
- |
- |
Undercooked/raw fish |
|
Fasciola hepatica |
Cattle, goats |
+ |
+ |
- |
- |
Watercress |
|
Opisthorclis viverrini/felinus |
Freshwater fish |
- |
+ |
- |
- |
Undercooked/raw fish |
|
Paragonimus sp. |
Freshwater crabs |
- |
+ |
- |
- |
Undercooked/raw crabs |
|
Taenia saginata and T. solium |
Cattle, swine |
- |
+ |
- |
- |
Undercooked meat |
|
Trichinella spiralis |
Swine, carnivora |
- |
+ |
- |
- |
Undercooked meat |
|
Trichuris trichiura |
Humans |
0 |
+ |
- |
- |
Soil-contaminated food |
a Almost all acute enteric infections show increased transmission during the summer and/or wet months, except infections due to Rotavirus and Yersinia enterocolitica, which show increased transmission in cooler months.
b Under certain circumstances, some multiplication has been observed. The epidemiological significance of this observation is not clear.
c Vertical transmission from pregnant woman to foetus occurs frequently.
+ = Yes; ± = Rare; - = No; 0 = No information.
Adapted from WHO/FAO 1984.
In the developing countries, they are responsible for a wide range of foodborne diseases (e.g., cholera, salmonellosis, shigellosis, typhoid and paratyphoid fevers, brucellosis, poliomyelitis and amoebiasis). Diarrhoeal diseases, especially infant diarrhoea, are the dominant problem and indeed one of massive proportions. Annually, some 1,500 million children under the age of five suffer from diarrhoea and of these over three million die as a result. Formerly it was thought that contaminated water supplies were the main direct source of pathogens causing diarrhoea, but now it has been shown that up to 70% of diarrhoeal episodes may be due to foodborne pathogens (WHO 1990c). However, the contamination of the food may in many cases originate from contaminated water that is used for irrigation and similar purposes.
Industrialized countries
Although the situation regarding foodborne diseases is very serious in developing countries, the problem is not limited to these countries, and in recent years, industrialized countries have experienced a succession of major epidemics. In the United States it is estimated there are 6.5 million cases per year, with 9,000 fatalities, but according to the US Food and Drug Administration this figure is an underestimate and may be as high as 80 million cases (Cohen 1987; Archer and Kvenberg 1985; Young 1987). The estimate for former West Germany was one million cases in 1989 (Grossklaus 1990). A study in the Netherlands found that as many as 10% of the population may be affected by foodborne or waterborne diseases (Hoogenboom-Vergedaal et al. 1990).
With today’s improvements in standards of personal hygiene, development of basic sanitation, safe water supplies, effective infrastructure and the increasing application of technologies such as pasteurization, many foodborne diseases have been either eliminated or considerably reduced in certain industrialized countries (e.g., milkborne salmonellosis). Nevertheless, most countries are now experiencing an important increase in several other foodborne diseases. The situation in former West Germany (1946-1991) illustrates this phenomenon (figure 2) (Statistisches Bundesamt 1994).
Figure 2. Infectious enteritis, typhoid fever and para-typhoid fever (A, B and C), Germany
Salmonellosis, specifically, has increased tremendously on both sides of the Atlantic over the past few years (Rodrigue 1990). In many cases it is due to Salmonella enteritidis. Figure 3 shows the increase of this micro-organism in relation to other Salmonella strains in Switzerland. In many countries, poultry meat, eggs and foods containing eggs have been identified as the predominant sources of this pathogen. In certain countries, 60 to 100% of poultry meat is contaminated with Salmonella spp., and meat, frogs’ legs, chocolate and milk have also been implicated (Notermans 1984; Roberts 1990). In 1985, some 170,000 to 200,000 persons were involved in an outbreak of salmonellosis in Chicago which was caused by contaminated pasteurized milk (Ryzan 1987).
Figure 3. Serotypes of Salmonella in Switzerland
Chemicals and toxicants in food
Considerable efforts have been undertaken at the national and international levels to ensure the chemical safety of food supplies. Two joint FAO/WHO committees have, over a period of three decades, evaluated a large number of food chemicals. The Joint FAO/WHO Expert Committee on Food Additives (JECFA) evaluates food additives, contaminants and veterinary drug residues, and the Joint FAO/WHO Meeting on Pesticide Residues (JMPR) evaluates pesticide residues. Recommendations are made on the acceptable daily intake (ADI), on maximum residue levels (MRLs) and maximum levels (MLs). Based on these recommendations, the Codex Alimentarius Commission and governments establish food standards and safe levels for these substances in foodstuffs. Moreover, the Joint UNEP/FAO/WHO Food Contamination Monitoring Programme (GEMS/Food) provides information on the levels of contaminants in food and on time trends of contamination, enabling preventive and control measures.
While information from most of the developing countries is scarce, surveys made in the industrialized countries suggest that the food supply is largely safe from the chemical viewpoint owing to the extensive food safety infrastructure (i.e., legislation, enforcement mechanisms, surveillance and monitoring systems) and the general level of responsibility of the food industry. However, accidental contamination or adulteration does occur, in which case the health consequences may be grave. For example, in Spain in 1981-82, adulterated cooking oil killed some 600 people and disabled—temporarily or permanently—another 20,000 (WHO 1984). The agent responsible for this mass poisoning has not yet been identified in spite of intensive investigations.
Environmental chemicals
A number of chemical substances may occur in the food supply as a result of environmental contamination. Their effects on health may be extremely serious and have caused great concern in recent years.
Serious consequences have been reported when foods contaminated with heavy metals such as lead, cadmium or mercury have been ingested over extended periods of time.
The Chernobyl accident provoked great concern over the health risks to people exposed to accidental radionuclide emissions. People living in the vicinity of the accident were exposed, and this exposure included radioactive contaminants in food and water. In other parts of Europe and elsewhere, at some distance from the accident, this concern focused on contaminated foods as a source of exposure. In most countries, the estimated average dose acquired from eating contaminated foods amounted to only a very small fraction of the dose normally received from background radiation (IAEA 1991).
Other environmental chemicals of interest are polychlorinated biphenyls (PCBs). PCBs are used in various industrial applications. Information on the effects of PCBs on human health were originally noted following from two large-scale incidents which occurred in Japan (1968) and in Taiwan, China (1979). Experience from these outbreaks showed that as well as their acute effects, PCBs may also have carcinogenic effects.
DDT was widely used between 1940 and 1960 as an insecticide for agricultural purposes and for the control of vector-borne diseases. It is now banned or restricted in many countries because of its potential risk to the environment. In many tropical countries, DDT is still an important chemical, used for the control of malaria. No confirmed ill effects have been reported due to residues of DDT in food (UNEP 1988).
Mycotoxins
Mycotoxins, the toxic metabolites of certain microscopic fungi (moulds), may cause serious adverse effects in humans, as well as in animals. Animal studies have shown that besides acute intoxication, mycotoxins are capable of causing carcinogenic, mutagenic and teratogenic effects.
Biotoxins
Intoxication by marine biotoxin (also known as “fish poisoning”) is another problem of concern. Examples of such intoxications are ciguatera and various kinds of shellfish poisoning.
Plant toxicants
Toxicants in edible plants and poisonous plants which resemble them (mushrooms, certain wild green plants) are important causes of ill health in many areas of the world and present a troublesome problem for food safety (WHO 1990b).
Linkages Between Environmental and Occupational Health
Development, and industrialization in particular, have made immense positive contributions to health, including greater personal and social wealth, as well as vastly improved health and education services, transportation and communication. Unquestionably, on the global scale, people are living longer and are healthier than they were centuries and even decades ago. However, industrialization has also had adverse health consequences not only for workforces, but for the general population as well. These effects have been caused either directly by exposure to safety hazards and harmful agents, or indirectly through environmental degradation locally and globally (see “Industrial pollution in developing countries” in this chapter).
This article outlines the nature of environmental health hazards and the reasons for linking environmental health with occupational health.
Environmental health hazards, like occupational health hazards, may be biological, chemical, physical, biomechanical or psychosocial in nature. Environmental health hazards include traditional hazards of poor sanitation and shelter, as well as agricultural and industrial contamination of air, water, food and land. These hazards have resulted in a host of health impacts, ranging from catastrophic direct effects (e.g., the recent cholera epidemic in Latin America and the chemical poisoning outbreak in Bhopal, India), to chronic effects (e.g., in Minamata, Japan), to subtle, indirect, and even disputed effects (e.g., in Love Canal, USA). Table 1 summarizes some of the major notorious disasters in the last half century that have caused “environmental disease” outbreaks. There are undeniably countless other examples of environmental disease outbreaks, some of which are not easily detectable on the macrostatistical level. Meanwhile, over a billion people in the world lack access to safe drinking water (WHO 1992b) and over 600 million are exposed to ambient levels of sulphur dioxide that well exceed recommended levels. Moreover the pressure on agriculture and food production as both population and per capita demand increase, will likely lead to a greater burden on the environment (see “Food and agriculture” in this chapter). Environmental health impacts thus include the indirect effects of industrial disruption of adequate food and housing, as well as the degradation of the global systems on which the health of the planet depends.
Table 1. Selected major "environmental disease" outbreaks
|
Location and year |
Environmental hazard |
Type of disease |
Number affected |
|
London, UK 1952 |
Severe air-pollution with sulphur dioxide and suspended particulate matter (SPM) |
Increase in heart and lung disease manifestations |
3,000 deaths, many others ill |
|
Toyama, Japan 1950s |
Cadmium in rice |
Kidney and bone disease (“Itai-itai disease”) |
200 with severe disease, many more with slight effects |
|
South-east Turkey 1955-61 |
Hexachlorobenzene in seed grains |
Porphyria; neurological disease |
3,000 |
|
Minamata, Japan 1956 |
Methylmercury in fish |
Neurological disease (“Minimata disease”) |
200 with severe disease, 2,000 suspected |
|
USA cities 1960s-70s |
Lead in paint |
Anaemia, behavioural and mental effects |
Many thousands |
|
Fukuoka, Japan 1968 |
Polychlorinated biphenyls (PCBs) in food oil |
Skin disease, general weakness |
Several thousands |
|
Iraq 1972 |
Methylmercury in seed grains |
Neurological disease |
500 deaths, 6,500 hospitalized |
|
Madrid, Spain 1981 |
Aniline or other toxin in food oil |
Various symptoms |
340 deaths, 20,000 cases |
|
Bhopal, India 1985 |
Methylisocyanate |
Acute lung disease |
2,000 deaths, 200,000 poisoned |
|
California, USA 1985 |
Carbamate pesticide in watermelons |
Gastrointestinal, skeletal, muscle, autonomic and central nervous system effects (Carbamate illness) |
1,376 reported cases of illness resulting from consumption, 17 severely ill |
|
Chernobyl, USSR 1986 |
Iodine-134, Caesium-134 and -137 from a reactor explosion |
Radiation illness (including increases in cancer and thyroid diseases in children) |
300 injured, 28 died within 3 months, more than 600 cases of thyroid cancer |
|
Goiánia, Brazil 1987 |
Caesium-137 from an abandoned cancer therapy machine |
Radiation illness (follow-up of in utero exposures continuing) |
Some 240 people were contaminated and 2 died |
|
Peru 1991 |
Cholera epidemic |
Cholera |
139 deaths, many thousand ill |
In many countries large-scale agriculture and the concomitant active use of toxic pesticides is a major health hazard both for workers and for their households. Pollution by fertilizers or biological waste from the food industry, paper industry and so on can also have harmful effects on waterways, reducing fishing and food supplies. The fishermen and gatherers of other seafood may have to travel much further to get their daily catch, with increased risks of drowning accidents and other mishaps. The spread of tropical disease by the environmental changes associated with developments such as the building of dams, roads and so on constitutes another type of environmental health risk. The new dam may create breeding grounds for schistosomiasis, a debilitating disease affecting rice farmers who have to walk in water. The new road may create fast communication between an area with endemic malaria and another area hitherto spared from this disease.
It should be pointed out that the major basis for a harmful environment in the workplace or in the general environment is poverty. The traditional health threats in developing countries or in poor sections of any country include poor sanitation, water and food which spreads communicable diseases, poor housing with high exposures to cooking smoke and high fire risks, as well as high injury risks in small-scale agriculture or cottage industries. Reduction of poverty and improved living and working conditions is a fundamental priority for improved occupational and environmental health for billions of people. Despite efforts for energy conservation and sustainable development, failure to address the underlying inequities in wealth distribution threatens the global ecosystem.
Forests, for example, which represent the culmination of ecological successional processes, are being destroyed at an alarming rate, due to commercial logging and clearance by impoverished peoples for agriculture and firewood. The effects of forest depletion include soil erosion, which, if extreme, can lead to desertification. Loss of biodiversity is an important consequence (see “Species extinction, biodiversity loss and human health” in this chapter). It is estimated that one-third of all carbon dioxide emissions are from the burning of tropical forests (the importance of carbon dioxide in creating global warming is discussed in “Global climate change and ozone depletion” in this chapter). Thus, addressing poverty is imperative with respect to global environmental health as well as individual, community and regional well-being.
Reasons for Linking Environmental and Occupational Health
The main link between the workplace and the general environment is that the source of the hazard is usually the same, whether it is an agricultural activity or an industrial activity. In order to control the health hazard, a common approach may work effectively in both settings. This is particularly so when it comes to the choice of chemical technologies for production. If an acceptable result or product can be produced with a less toxic chemical, the choice of such a chemical can reduce or even eliminate the health risk. One example is the use of safer water-based paints instead of paints made with toxic organic solvents. Another example is the choice of non-chemical pest-control methods whenever this is possible. In fact, in many cases, particularly in the developing world, there is no separation between the home and the workplace; thus the setting is truly the same.
It is now well recognized that the scientific knowledge and training required to assess and control environmental health hazards are, for the most part, the same skills and knowledge required to address health hazards within the workplace. Toxicology, epidemiology, occupational hygiene, ergonomics, safety engineering - in fact, the very disciplines included in this Encyclopaedia - are the basic tools of environmental science. The process of risk assessment and risk management is also the same: identify the hazards, categorize the risks, assess the exposure and estimate risk. This is followed by evaluating control options, controlling the exposure, communicating the risk to the public and establishing an on-going exposure- and risk-monitoring programme. Thus occupational and environmental health are strongly linked by common methodologies, particularly in health assessment and exposure control.
The identification of environmental health hazards has often come from observations of adverse health outcomes among workers; and unquestionably it is in the workplace that the impact of industrial exposures is best understood. Documentation of health effects generally comes from one of three sources: animal or other laboratory experiments (both non-human and controlled human), accidental high-level exposures or the epidemiological studies that usually follow such exposures. To conduct an epidemiological study it is necessary to be able to define both the exposed population and the nature and level of the exposure, as well as to ascertain the negative health effect. It is generally easier to define the members of a workforce than to determine the membership of a community, particularly in a community that is transient; the nature and level of exposure to various members of the cohort are generally more clear-cut in a workplace population than in a community; and the outcomes of high levels of exposure are almost always easier to delineate than more subtle changes attributable to low-level exposure. While there are some examples of exposure outside factory gates approaching the worst occupational exposures (e.g., cadmium exposure from mining in China and Japan; lead and cadmium emissions from smelters in Upper Silesia, Poland), the levels of exposure are generally much higher to a workforce than to the surrounding community (WHO 1992b).
Since adverse health outcomes are more apparent in workers, information on occupational health effects of many toxic exposures (including heavy metals such as lead, mercury, arsenic and nickel, as well as such well-known carcinogens as asbestos) has been used to calculate the health risk to the wider community. With respect to cadmium, for example, as early as 1942 reports began to appear of cases of osteomalacia with multiple fractures among workers in a French factory producing alkaline batteries. During the 1950s and 1960s cadmium intoxication was considered to be strictly an occupational disease. However, the knowledge gained from the workplace helped achieve the recognition that osteomalacia and kidney disease that was occurring in Japan at this time, “Itai-itai” disease, was indeed due to contamination of rice from irrigation of soil with water contaminated with cadmium from industrial sources (Kjellström 1986). Thus occupational epidemiology has been able to make a substantive contribution to knowledge of the effects of environmental exposure, constituting another reason for linking the two fields.
On an individual level, occupational disease affects well-being in the home and the community; and, universally, an individual who is ill from inadequacies in the home and the community cannot be productive in the workplace.
Strictly from a scientific viewpoint, there is a need to consider total (environmental plus occupational) exposures in order to truly assess health impact and establish dose-response relationships. Pesticide exposure is a classic example wherein occupational exposure may be supplemented by considerable environmental exposure, through food and water-source contamination, and through non-occupational airborne exposure. From outbreaks in which over 100 poisonings occurred from contaminated food alone, over 15,000 cases and 1,500 deaths due to pesticide poisoning have been documented by the WHO (1990e). In one study of Central American cotton growers using pesticides, not only did very few of the workers have access to protective clothing, but virtually all of the workers lived within 100 metres of the cotton fields, many in temporary housing with no walls for protection from aerial pesticide spraying. The workers also often washed in irrigation channels containing pesticide residues, resulting in increased exposures (Michaels, Barrera and Gacharna 1985). To understand the relationship between pesticide exposure and any health effects reported, all sources of exposure should be taken into consideration. Thus ensuring that occupational and environmental exposures are evaluated together improves the accuracy of exposure assessment in both areas.
The health problems caused by occupational and environmental hazards are particularly acute in developing countries, where well established methods of hazard control are less likely to be applied because of limited awareness of the hazards, low political priority of health and environment matters, limited resources or lack of appropriate occupational and environmental health management systems. A major impediment to environmental health hazard control in many parts of the world is the lack of people with appropriate training. It has been documented that developing countries suffer from a severe shortage of expert staff in occupational health (Noweir 1986). In 1985 a WHO expert committee also concluded that there is an urgent need for staff trained in environmental health matters; indeed Agenda 21, the internationally agreed upon strategy taken by the United Nations Conference on Environment and Development (UN 1993), identifies training (national “capacity building”) as a key element of promoting human health through sustainable development. Where resources are limited, it is not feasible to train one group of people to look after health concerns within the workplace, and another group to attend to hazards outside the factory gate.
Even in developed countries, there is a strong trend to make most efficient use of resources by training and employing “occupational and environmental health” professionals. Today, businesses must find ways to manage their affairs logically and efficiently within the societal framework of duty, law and financial policy. Combining occupational and environment health under one roof is one way of achieving this goal.
Broad environmental concerns must be taken into consideration in designing workplaces and deciding on industrial hygiene control strategies. Substituting for one substance another one that is less acutely toxic may make good occupational health sense; however, if the new substance is not biodegradable, or damages the ozone layer, it would not be an appropriate exposure control solution—it would only move the problem elsewhere. The use of chlorofluorocarbons, now widely used as a refrigerant instead of the more acutely dangerous substance ammonia, is the classic example of what is now known to have been an environmentally inappropriate substitution. Thus linking occupational and environmental health minimizes unwise exposure control decisions.
While understanding of the health effects of various deleterious exposures has usually come from the workplace, the public health impact of environmental exposures to these same agents has often been a major force in stimulating clean-up efforts both inside the workplace and in the surrounding community. For example, discovery of high lead levels in workers’ blood by an industrial hygienist in a lead foundry in Bahia, Brazil, led to investigations of lead in the blood of children in nearby residential areas. The finding that the children had high lead levels was a major impetus in the company taking action to reduce occupational exposures as well as lead emissions from the factory (Nogueira 1987), although occupational exposures still remain substantially higher than would be tolerated by the general community.
In fact, environmental health standards are usually much stricter than occupational health standards. The WHO’s recommended guideline values for selected chemicals provide an example. The rationale for the difference is generally that the community consists of sensitive populations including the very old, the ill, young children and pregnant women, whereas the workforce is at least healthy enough to work. Also, it is often argued that risk is more “acceptable” to a workforce, as these people are benefiting by having a job, and are therefore more willing to accept the risk. Many political, ethical, as well as scientific, debates rage around the question of standards. Linking occupational and environmental health can be a positive contribution to sorting out these controversies. In this regard, tightening the connection between occupational and environmental health may facilitate greater consistency in approaches to standard setting.
Likely inspired at least in part by the active debate about the environment and sustainable development brought to the forefront by Agenda 21, many occupational health professional organizations have changed their names to “occupational and environmental” organizations in acknowledgement that their members are increasingly devoting their attention to environmental health hazards both inside and outside the workplace. Further, as noted in the chapter on ethics , the International Code of Ethics for Occupational Health Professionals states that the duty to protect the environment is part and parcel of the ethical obligations of occupational health professionals.
In summary, occupational and environmental health are strongly linked by:
- the very fact that the source of the health threat is usually the same
- common methodologies, particularly in health assessment and exposure control
- the contribution that occupational epidemiology makes to knowledge of the effects of environmental exposure
- the effects that occupational disease has on well-being in the home and the community, and conversely the effect of environmental pathology on worker productivity
- the scientific need to consider total exposures in order to determine dose-response relationships
- the efficiency in human resource development and utilization gained by such a linkage
- improvements in exposure control decisions stemming from the broader view
- greater consistency in standard setting facilitated by the link
- the fact that linking environmental and occupational health enhances the incentive for rectification of hazards to both the workforce and the community.
The desirability of bringing together occupational and environmental health notwithstanding, each has a unique and specific orientation that should not be lost. Occupational health must continue to focus on workers’ health, and environmental health must continue to concern itself with the health of the general public. None the less, even where it is desirable for professionals to operate strictly in only one of these fields, having a good appreciation of the other enhances the credibility, knowledge base and effectiveness of the overall endeavour. It is in this spirit that this chapter is presented.
Multiple Chemical Sensitivities
Introduction
Since the 1980s, a new clinical syndrome has been described in occupational and environmental health practice characterized by the occurrence of diverse symptoms after exposure to low levels of artificial chemicals, although as yet it lacks a widely accepted definition. The disorder may develop in individuals who have experienced a single episode, or recurring episodes of a chemical injury such as solvent or pesticide poisoning. Subsequently, many types of environmental contaminant in air, food or water may elicit a wide range of symptoms at doses below those which produce toxic reactions in others.
Although there may not be measurable impairment of specific organs, the complaints are associated with dysfunction and disability. Although idiosyncratic reactions to chemicals are probably not a new phenomenon, it is believed that multiple chemical sensitivities (MCSs), as the syndrome is now most frequently called, is being brought by patients to the attention of medical practitioners far more commonly than in the past. This syndrome is prevalent enough to have generated substantial public controversy as to who should treat patients suffering with the disorder and who should pay for the treatment, but research has yet to elucidate many scientific issues relevant to the problem, such as its cause, pathogenesis, treatment and prevention. Despite this, MCS clearly does occur and causes significant morbidity in the workforce and general population. It is the purpose of this article to elucidate what is known about it at this time in the hope of enhancing its recognition and management in the face of uncertainty.
Definition and Diagnosis
Although there is no general consensus on a definition for MCS, certain features allow it to be differentiated from other well-characterized entities. These include the following:
- Symptoms typically occur after a definitely characterizable occupational or environmental incident, such as an inhalation of noxious gases or vapours or other toxic exposure. This “initiating” event may be a single episode, such as an exposure to a pesticide spray, or a recurrent one, such as frequent solvent overexposure. Often the effects of the apparently precipitating event, or events, are mild and may merge without clear demarcation into the syndrome which follows.
- Acute symptoms similar to those of the preceding exposure begin to occur after re-exposures to lower levels of various materials, such as petroleum derivatives, perfumes and other common work and household products.
- Symptoms are referrable to multiple organ systems. Central nervous system complaints, such as fatigue, confusion and headache, occur in almost every case. Upper and lower respiratory, cardiac, dermal, gastrointestinal and musculoskeletal symptoms are common.
- It is generally the case that very diverse agents may elicit the symptoms at levels of exposure orders of magnitude below accepted TLVs or guidelines.
- Complaints of chronic symptomatology, such as fatigue, cognitive difficulties, gastrointestinal and musculoskeletal disturbances are common. Such persistent symptoms may predominate over reactions to chemicals in some cases.
- Objective impairment of the organs which would explain the pattern or intensity of complaints is typically absent. Patients examined during acute reactions may hyperventilate or demonstrate other manifestations of excess sympathetic nervous system activity.
- No better established diagnosis easily explains the range of responses or symptoms.
While not every patient precisely meets the criteria, each point should be considered in the diagnosis of MCS. Each serves to rule out other clinical disorders which MCS may resemble, such as somatization disorder, sensitization to environmental antigens (as with occupational asthma), late sequelae of organ system damage (e.g., reactive airways dysfunction syndrome after a toxic inhalation) or a systemic disease (e.g., cancer). On the other hand, MCS is not a diagnosis of exclusion and exhaustive testing is not required in most cases. While many variations occur, MCS is said to have a recognizable character which facilitates diagnosis as much or more than the specific criteria themselves.
In practice, diagnostic problems with MCS occur in two situations. The first is with a patient early in the course of the condition in whom it is often difficult to distinguish MCS from the more proximate occupational or environmental health problem which precedes it. For example, patients who have experienced symptomatic reactions to pesticide spraying indoors may find that their reactions are persisting, even when they avoid direct contact with the materials or spraying activities. In this situation a clinician might assume that significant exposures are still occurring and direct unwarranted effort to altering the environment further, which generally does not relieve the recurrent symptoms. This is especially troublesome in an office setting where MCS may develop as a complication of sick building syndrome. Whereas most office workers will improve after steps are taken to improve air quality, the patient who has acquired MCS continues to experience symptoms, despite the lower exposures involved. Efforts to improve the air quality further typically frustrate patient and employer.
Later in the course of MCS, diagnostic difficulty occurs because of the chronic aspects of the illness. After many months, the MCS patient is often depressed and anxious, as are other medical patients with new chronic diseases. This may lead to an exaggeration of psychiatric manifestations, which may predominate over chemically stimulated symptoms. Without diminishing the importance of recognizing and treating these complications of MCS, nor even the possibility that MCS itself is psychological in origin (see below), the underlying MCS must be recognized in order to develop an effective mode of management which is acceptable to the patient.
Pathogenesis
The pathogenic sequence which leads in certain people from a self-limited episode or episodes of an environmental exposure to the development of MCS is not known. There are several current theories. Clinical ecologists and their adherents have published extensively to the effect that MCS represents immune dysfunction caused by accumulation in the body of exogenous chemicals (Bell 1982; Levin and Byers 1987). At least one controlled study did not confirm immune abnormalities (Simon, Daniel and Stockbridge 1993). Susceptibility factors under this hypothesis may include nutritional deficiencies (e.g., lack of vitamins or antioxidants) or the presence of subclinical infections such as candidiasis. In this theory, the “initiating” illness is important because of its contribution to lifelong chemical overload.
Less well developed, but still very biologically oriented, are the views that MCS represents unusual biological sequelae of chemical injury. As such, the disorder may represent a new form of neurotoxicity due to solvents or pesticides, injury to the respiratory mucosae after an acute inhalational episode or similar phenomena. In this view, MCS is seen as a final common pathway of different primary disease mechanisms (Cullen 1994; Bascom 1992).
A more recent biological perspective has focused on the relationship between the mucosae of the upper respiratory tract and the limbic system, especially with respect to the linkage in the nose (Miller 1992). Under this perspective, relatively small stimulants to the nasal epithelium could produce an amplified limbic response, explaining the dramatic, and often stereotypic, responses to low-dose exposures. This theory also may explain the prominent role of highly odoriferous materials, such as perfumes, in triggering responses in many patients.
Conversely, however, many experienced investigators and clinicians have invoked psychological mechanisms to explain MCS, linking it to other somatoform disorders (Brodsky 1983; Black, Ruth and Goldstein 1990). Variations include the theory that MCS is a variant of post-traumatic stress disorder (Schottenfeld and Cullen 1985) or a conditioned response to an initial toxic experience (Bolle-Wilson, Wilson and Blecker 1988). One group has hypothesized MCS as a late-life response to early childhood traumas such as sexual abuse (Selner and Strudenmayer 1992). In each of these theories, the precipitating illness plays a more symbolic than biological role in the pathogenesis of MCS. Host factors are seen as very important, especially the predisposition to somaticize psychological distress.
Although there is much published literature on the subject, few clinical or experimental studies have appeared to support strongly any of these views. Investigators have not generally defined their study populations nor compared them with appropriately matched groups of control subjects. Observers have not been blinded to subject status or research hypotheses. As a result, most available data are effectively descriptive. Furthermore, the legitimate debate over the aetiology of MCS has been distorted by dogma. Since major economic decisions (e.g., patient benefit entitlements and physician reimbursement acceptance) may hinge upon the way in which cases are viewed, many physicians have very strong opinions about the illness, which limit the scientific value of their observations. Caring for MCS patients requires a recognition of the fact that these theories are often well known to patients, who may also have very strong views on the matter.
Epidemiology
Detailed knowledge of the epidemiology of MCS is not available. Estimates of its prevalence in the US population (from where most reports continue to come) range as high as several percentage points, but the scientific basis for these is obscure, and other evidence exists to suggest that MCS in its clinically apparent form is rare (Cullen, Pace and Redlich 1992). Most available data derive from case series by practitioners who treat MCS patients. These shortcomings notwithstanding, some general observations can be made. Although patients of virtually all ages have been described, MCS occurs most commonly among mid-life subjects. Workers in jobs of higher socio-economic status seem disproportionately affected, while the economically disadvantaged and non-White population seems underrepresented; this may be an artefact of differential access or of clinician bias. Women are more frequently affected than men. Epidemiological evidence strongly implicates some host idiosyncrasy as a risk factor, since mass outbreaks have been uncommon and only a small fraction of victims of chemical accidents or overexposures appear to develop MCS as a sequela (Welch and Sokas 1992; Simon 1992). Perhaps surprising in this regard is the fact that common atopic allergic disorders do not appear to be a strong risk factor for MCS among most groups.
Several groups of chemicals have been implicated in the majority of initiating episodes, specifically organic solvents, pesticides and respiratory irritants. This may be a function of the widespread usage of these materials in the workplace. The other commonplace setting in which many cases occur is in the sick building syndrome, some patients evolving from typical SBS-type complaints into MCS. Although the two illnesses have much in common, their epidemiological features should distinguish them. Sick building syndrome typically affects most individuals sharing a common environment, who improve in response to environmental remediation; MCS occurs sporadically and does not respond predictably to modifications of the office environment.
Finally, there is great interest in whether MCS is a new disorder or a new presentation or perception of an old one. Views are divided according to the proposed pathogenesis of MCS. Those favouring a biological role for environmental agents, including the clinical ecologists, postulate that MCS is a twentieth century disease with rising incidence related to increased chemical usage (Ashford and Miller 1991). Those who support the role of psychological mechanisms see MCS as an old somatoform illness with a new societal metaphor (Brodsky 1983; Shorter 1992). According to this view, the social perception of chemicals as agents of harm has resulted in the evolution of new symbolic content to the historic problem of psychosomatic disease.
Natural History
MCS has not yet been studied sufficiently to define its course or outcome. Reports of large numbers of patients have provided some clues. First, the general pattern of illness appears to be one of early progression as the process of generalization develops, followed by less predictable periods of incremental improvements and exacerbations. While these cycles may be perceived by the patient to be due to environmental factors or treatment, no scientific evidence for such relationships has been established.
Two important inferences follow. First, there is little evidence to suggest that MCS is progressive. Patients do not deteriorate from year to year in any measurable physical way, nor have complications such as infections or organ system failure resulted in the absence of intercurrent illness. There is no evidence that MCS is potentially lethal, despite the perceptions of the patients. While this may be the basis of a hopeful prognosis and reassurance, it has been equally clear from clinical descriptions that complete remissions are rare. While significant improvement occurs, this is generally based on enhanced patient function and sense of well-being. The underlying tendency to react to chemical exposures tends to persist, although symptoms may become sufficiently bearable to allow the victim to return to a normal lifestyle.
Clinical Management
Very little is known about the treatment of MCS. Many traditional and non-traditional methods have been tried, though none has been subjected to the usual scientific standards to confirm their efficacy. As with other conditions, approaches to treatment have paralleled theories of pathogenesis. Clinical ecologists and others, who believe that MCS is caused by immune dysfunction due to high burdens of exogenous chemicals, have focused attention on avoidance of artificial chemicals. This view has been accompanied by use of diagnostic strategies to determine “specific” sensitivities by various invalidated tests to “desensitize” patients. Coupled with this have been strategies to enhance underlying immunity with dietary supplements, such as vitamins and antioxidants, and efforts to eradicate yeasts or other commensal organisms. A most radical approach involves efforts to eliminate toxins from the body by chelation or accelerated turnover of fat where lipid-soluble pesticides, solvents and other organic chemicals are stored.
Those inclined to a psychological view of MCS have tried appropriately alternative approaches. Supportive individual or group therapies and more classic behavioural modification techniques have been described, though the efficacy of these approaches remains conjectural. Most observers have been struck by the intolerance of the patients to pharmacological agents typically employed for affective and anxiety disorders, an impression supported by a small placebo-controlled double-blind trial with fluvoxamine that was conducted by the author and aborted due to side effects in five of the first eight enrolees.
The limitations of present knowledge notwithstanding, certain treatment principles can be enunciated.
First, to the extent possible, the search for a specific “cause” of MCS in the individual case should be minimized—it is fruitless and counterproductive. Many patients have had considerable medical evaluation by the time MCS is considered and equate testing with evidence of pathology and the potential for a specific cure. Whatever the theoretical beliefs of the clinician, it is vital that the existing knowledge and uncertainty about MCS be explained to the patient, including specifically that its cause is unknown. The patient should be reassured that consideration of psychological issues does not make the illness less real, less serious or less worthy of treatment. Patients can also be reassured that MCS is not likely to be progressive or fatal, and they should be made to understand that total cures are not likely with present modalities.
Uncertainty about pathogenesis aside, it is most often necessary to remove the patient from components of their work environment which trigger symptoms. Although radical avoidance is of course counterproductive to the goal of enhancing the worker’s functioning, regular and severe symptomatic reactions should be controlled as far as possible as the basis for a strong therapeutic relationship with the patient. Often this requires a job change. Workers’ compensation may be available; even in the absence of detailed understanding of disease pathogenesis, MCS may correctly be characterized as a complication of a work exposure which is more readily identified (Cullen 1994).
The goal of all subsequent therapy is improvement of function. Psychological problems, such as adjustment difficulties, anxiety and depression should be treated, as should coexistent problems like typical atopic allergies. Since MCS patients do not tolerate chemicals in general, non-pharmacological approaches may be necessary. Most patients need direction, counselling and reassurance to adjust to an illness without an established treatment (Lewis 1987). To the extent possible, patients should be encouraged to expand their activities and should be discouraged from passivity and dependence, which are common responses to the disorder.
Prevention and Control
Obviously, primary prevention strategies cannot be developed given present knowledge of the pathogenesis of the disorder or of its predisposing host risk factors. On the other hand, reduction of opportunities in the workplace for the uncontrolled acute exposures which precipitate MCS in some hosts, such as those involving respiratory irritants, solvents and pesticides, will likely reduce the occurrence of MCS. Proactive measures to improve the air quality of poorly ventilated offices would also probably help.
Secondary prevention would appear to offer a greater opportunity for control, although no specific interventions have been studied. Since psychological factors may play a role in victims of occupational overexposures, careful and early management of exposed persons is advisable even when the prognosis from the point of view of the exposure itself is good. Patients seen in clinics or emergency rooms immediately after acute exposures should be assessed for their reactions to the events and should probably receive very close follow-up where undue concerns of long-term effects or persistent symptoms are noted. Obviously, efforts should be made for such patients to ensure that preventable reoccurrences do not come about, since this kind of exposure may be an important risk factor for MCS regardless of the causal mechanism.
Sick Building Syndrome
Sick building syndrome (SBS) is a term used to describe office worker discomfort and medical symptoms that are related to building characteristics, to pollutant exposures and to work organization, and that are mediated through personal risk factors. A wide range of definitions exists, but disagreement remains (a) as to whether a single individual in a building can develop this syndrome or whether a set numeric criterion (the proportion affected) should be used; and (b) as to the necessary symptom components. Figure 1 lists symptoms commonly included in SBS; in recent years, with increased understanding, complaints related to odours have generally been dropped from the list and chest symptoms included under mucous membrane irritation. A critical distinction needs to be made between SBS and building-related illness (BRI), where verifiable irritation, allergy or illness such as hypersensitivity pneumonitis, asthma or carbon monoxide-induced headaches may be present as an outbreak associated with a building. SBS should also be distinguished from multiple chemical sensitivities (MCS; see below) which is more sporadic in occurrence, often occurs within an SBS population, and is much less responsive to modifications of the office environment.
Figure 1. Sick building syndrome.
SBS should be simultaneously viewed from and informed by three disparate perspectives. For health professionals, the view is from the perspective of medicine and the health sciences as they define symptoms related to indoor work and their associated pathophysiological mechanisms. The second perspective is that of engineering, including design, commissioning, operations, maintenance and exposure assessment for specific pollutants. The third perspective includes the organizational, social and psychological aspects of work.
Epidemiology
Since the mid-1970s, increasingly voiced office worker discomfort has been studied in formal ways. These have included field epidemiological studies using a building or a workstation as the sampling unit to identify risk factors and causes, population-based surveys to define prevalence, chamber studies of humans to define effects and mechanisms, and field intervention studies.
Cross-sectional and case-control studies
Approximately 30 cross-sectional surveys have been published (Mendell 1993; Sundell et al. 1994). Many of these have included primarily “non-problem” buildings, selected at random. These studies consistently demonstrate an association between mechanical ventilation and increased symptom reporting. Additional risk factors have been defined in several case-control studies. Figure 2 presents a grouping of widely recognized risk factors associated with increased rates of complaints.
Many of these factors overlap; they are not mutually exclusive. For example, the presence of inadequate housekeeping and maintenance, the presence of strong indoor pollution sources and increased individual susceptibility may lead to much greater problems than the presence of any one factor alone.
Figure 2. Risk factors for and causes of the sick building syndrome.
Factor and principal components analyses of questionnaire responses in cross-sectional surveys have explored the interrelationship of various symptoms. Consistently, symptoms related to single organ systems have clustered together more strongly than symptoms relating to different organ systems. That is, eye irritation, eye tearing, eye dryness, and eye itching all appear to correlate very strongly, and little benefit is obtained from looking at multiple symptoms within an organ system.
Controlled exposure studies
Animal testing to determine irritant properties and thresholds has become standard. A consensus method of the American Society for Testing and Materials (1984) is widely regarded as the basic instrument. This method has been used to develop structure-activity relationships, to demonstrate that more than one irritant receptor may exist in the trigeminal nerve and to explore interactions between multiple exposures. Most recently, it has been used to demonstrate the irritating properties of office equipment offgassing.
Analogous to this method, several approaches have been defined to document methods and dose-response relationships for irritation in humans. This work meanwhile suggests that, at least for “non-reactive” compounds such as saturated aliphatic hydrocarbons, the percentage of vapour pressure saturation of a compound is a reasonable predictor of its irritant potency. Some evidence also supports the view that increasing the number of compounds in complex mixtures decreases the irritant thresholds. That is, the more agents that are present, even at a constant mass, the greater the irritation.
Controlled exposure studies have been performed of volunteers in stainless steel chambers. Most have been performed with one constant mixture of volatile organic compounds (VOC) (Mølhave and Nielsen 1992). These consistently document relationships between symptoms and increasing exposure levels. Office workers who perceived themselves as “susceptible” to the effects of usual levels of VOCs indoors demonstrated some impairment on standard tests of neuropsychological performance (Mølhave, Bach and Pederson 1986). Healthy volunteers, on the other hand, demonstrated mucous membrane irritation and headaches at exposures in the range of 10 to 25 mg/m3, but no changes on neuropsychological performance. More recently, office workers demonstrated similar symptoms after simulated work in environments where pollutants from commonly used office equipment were generated. Animals reacted similarly when a standardized test of irritant potency was used.
Population-based studies
To date, three population-based studies have been published in Sweden, Germany and the United States. The questionnaires differed considerably, and thus prevalence estimates cannot be directly compared. Nevertheless, between 20 and 35% of respondents from various buildings not known to be sick were found to have complaints.
Mechanisms
A number of potential mechanisms and objective measures to explain and examine symptoms within specific organ systems have been identified. None of these has a high predictive value for the presence of disease, and they are therefore not suitable for clinical diagnostic use. They are useful in field research and epidemiological investigations. For many of these it is unclear whether they should be regarded as mechanisms, as markers of effect, or as measures of susceptibility.
Eyes
Both allergic and irritant mechanisms have been proposed as explanations for eye symptoms. Shorter tear-film break-up time, a measure of tear film instability, is associated with increased levels of symptoms. “Fat-foam thickness” measurement and photography for documentation of ocular erythema have also been used. Some authors attribute eye symptoms at least in part to increased individual susceptibility as measured by those factors. In addition, office workers with ocular symptoms have been demonstrated to blink less frequently when working at video display terminals.
Nose
Both allergic and irritant mechanisms have been proposed as explanations for nasal symptoms. Measures that have successfully been used include nasal swabs (eosinophils), nasal lavage or biopsy, acoustic rhinometry (nasal volume), anterior and posterior rhinomanometry (plethysmography) and measures of nasal hyperreactivity.
Central nervous system
Neuropsychological tests have been used to document decreased performance on standardized tests, both as a function of controlled exposure (Mølhave, Bach and Pederson 1986) and as a function of the presence of symptoms (Middaugh, Pinney and Linz 1982).
Individual risk factors
Two sets of individual risk factors have been discussed. First, two commonly recognized diatheses, atopy and seborrhea, are considered predisposing factors for medically defined symptoms. Second, psychological variables may be important. For example, personal traits such as anxiety, depression or hostility are associated with sick-role susceptibility. Similarly, work stress is so consistently associated with building-related symptoms that some causal association is likely to be present. Which of the three components of work stress—individual traits, coping skills, and organization function such as poor management styles—is the dominant cause remains undetermined. It is recognized that failing to intervene in a well-defined problem leads workers to experience their discomfort with increasing distress.
Engineering and Sources
Beginning in the late 1970s, the US National Institute for Occupational Safety and Health (NIOSH) responded to requests for help in identifying causes of occupant discomfort in buildings, attributing problems to ventilation systems (50%), microbiological contamination (3 to 5%), strong indoor pollution sources (tobacco 3%, others 14%), pollutants entrained from the outside (15%) and others. On the other hand, Woods (1989) and Robertson (et al. 1988) published two well-known series of engineering analyses of problem buildings, documenting on average the presence of three potential causal factors in each building.
One current professional ventilation standard (American Society of Heating, Refrigerating, and Airconditioning Engineers (1989) suggests two approaches to ventilation: a ventilation rate procedure and an air quality procedure. The former provides a tabular approach to ventilation requirements: office buildings require 20 cubic feet of outside air per occupant per minute to maintain occupant complaint rates of environmental discomfort at below 20%. This assumes relatively weak pollution sources. When stronger sources are present, that same rate will provide less satisfaction. For example, when smoking is permitted at usual rates (according to data from the early 1980s), approximately 30% of occupants will complain of environmental discomfort. The second approach requires the selection of a target concentration in air (particulates, VOCs, formaldehyde, etc.), information on emission rates (pollutant per time per mass or surface), and derives the ventilation requirements. Although this is an intellectually much more satisfying procedure, it remains elusive because of inadequate emissions data and disagreement on target concentrations.
Pollutants
Environmental scientists have generally defined exposure and health effects on a pollutant-by-pollutant basis. The American Thoracic Society (1988) defined six important categories, listed in figure 3.
Figure 3. Principal pollutant categories.
Environmental criteria have been established for many of the individual substances in these six groups. The utility and applicability of such criteria for indoor environments is controversial for many reasons. For example, the goals of threshold limit values often do not include prevention of eye irritation, a common complaint in indoor environments with requirements for close eye work at video display units. For most of the pollutant categories, the problem of interactions, commonly termed the “multiple contaminants problem,” remains inadequately defined. Even for agents that are thought to affect the same receptor, such as aldehydes, alcohols and ketones, no prediction models are well established. Finally, the definition of “representative compounds” for measurement is unclear. That is, pollutants must be measurable, but complex mixtures vary in their composition. It is unclear, for instance, whether the chronic residual odor annoyance due to environmental tobacco smoke correlates better with nicotine, particulates, carbon monoxide or other pollutants. The measure “total volatile organic compounds” is meanwhile considered an interesting concept, but is not useful for practical purposes as the various components have such radically different effects (Mølhave and Nielsen 1992; Brown et al. 1994). Particulates indoors may differ in composition from their outdoor counterparts, as filter sizes affect entrained concentrations, and indoor sources may differ from outdoor sources. There are measurement problems as well, since the sizes of filters used will affect which particles are collected. Different filters may be needed for indoor measurements.
Finally, emerging data suggest that reactive indoor pollutants may interact with other pollutants and lead to new compounds. For example, the presence of ozone, either from office machines or entrained from outdoors, may interact with 4-phenylcyclohexene and generate aldehydes (Wechsler 1992).
Primary Aetiological Theories
Organic solvents
Buildings have always relied on general dilution strategies for pollutant removal, but designers have assumed that humans were the primary source of pollutants. More recently, emissions from “solid materials” (such as particle board desks, carpeting and other furniture), from wet products (such as glues, wall paints, office machine toners) and personal products (perfumes) have been recognized as contributors to a complex mixture of very low levels of individual pollutants (summarized in Hodgson, Levin and Wolkoff 1994).
Several studies suggest that the presence of reactive volatile organic compounds, such as aldehydes and halogenated hydrocarbons, are associated with increasing levels of symptoms. Offices with higher complaint rates have had greater “loss” of VOCs between incoming and outgoing air than did offices with lower complaints. In a prospective study of schools, short chain VOCs were associated with symptom development. In another survey, higher personal samples for VOCs using a screening sampler that “over-reacts” to reactive VOCs, such as aldehydes and halogenated hydrocarbons, were associated with higher symptom levels. In that study, women had higher levels of VOCs in their breathing zone, suggesting another potential explanation for the increased rate of complaints among women. VOCs might adsorb onto sinks, such as fleecy surfaces, and be re-emitted from such secondary sources. The interaction of ozone and relatively non-irritant VOCs to form aldehydes is also consistent with this hypothesis.
The presence of multiple potential sources, the consistency of VOC health effects and SBS symptoms, and the widely recognized problems associated with ventilation systems make VOCs an attractive aetiological agent. Solutions other than better design and operation of ventilation systems include the selection of low-emitting pollutants, better housekeeping and prevention of “indoor chemistry.”
Bioaerosols
Several studies have suggested that bioaerosols have the potential to contribute to occupant discomfort. They may do this through several different mechanisms: irritant emissions; release of fragments, spores or viable organisms leading to allergy; and secretion of complex toxins. Fewer data exist to support this theory than the others. Nevertheless, it is clear that heating, ventilating and air-conditioning systems may be sources of micro-organisms.
They have also been described in building construction materials (as a result of improper curing), as a result of unwanted water incursion and in office dust. The presence of sensitizers in the office environment, such as dust mites or cat dander brought in from home on clothing, presents another possibility of exposure. To the extent that biological agents contribute to the problem, dirt and water management become primary control strategies.
In addition, toxigenic fungi may be found on other porous products in buildings, including ceiling tile, spray-on insulation and wooden joists. Especially in residential environments, fungal proliferation associated with inadequate moisture control has been associated with symptoms.
Psychosocial aspects of work
In all studies where it has been examined, “work stress” was clearly associated with SBS symptoms. Workers’ perceptions of job pressures, task conflicts, and non-work stressors such as spousal or parental demands may clearly lead to the subjective experience of “stronger” irritation as a function of illness behaviour. At times, such perceptions may in fact result from poor supervisory practices. In addition, the presence of irritants leading to subjective irritation is thought to lead to “work stress”.
Evaluation of the Patient
The examination should be directed at identification or exclusion of a significant component of building related illness (BRI). Allergic disease should be identified and optimally managed. However, this must be done with awareness that non-allergic mechanisms may contribute to a substantial residual symptom burden. Sometimes individuals can be reassured of the absence of clear disease by studies such as portable peak flow monitoring or pre- and post-work pulmonary function tests. Once such observable or pathologically verifiable disease has been ruled out, evaluation of the building itself becomes paramount and should be done with industrial hygiene or engineering input. Documentation, management and remediation of identified problems is discussed in Controlling the Indoor Environment.
Conclusion
SBS is a phenomenon that can be experienced by an individual, but is usually seen in groups; it is associated with engineering deficiencies and is likely caused by a series of pollutants and pollutant categories. As with all “dis-ease,” a component of personal psychology serves as an effect modifier that can lead to varying degrees of symptom intensity at any given level of distress.
Systemic Conditions: An Introduction
The last edition of this Encyclopaedia did not contain articles on either sick building syndrome (SBS) or multiple chemical sensitivities (MCS) (the latter term was coined by Cullen, 1987). Most practitioners of occupational medicine are not comfortable with such symptomatically driven and frequently psychologically related phenomena, at least partly for the reason that patients with these syndromes do not respond reliably to the standard means of occupational health intervention, namely, exposure reduction. Non-occupational physicians in general medical practice also react similarly: patients with little verifiable pathology, such as those complaining of chronic fatigue syndrome or fibromyalgia, are regarded as more difficult to treat (and generally regard themselves as more disabled) than patients with deforming conditions such as rheumatoid arthritis. There is clearly less regulatory imperative for sick building syndrome and multiple chemical sensitivities than for the classic occupational syndromes such as lead intoxication or silicosis. This discomfort on the part of treating physicians and the lack of appropriate regulatory guidance is unfortunate, however understandable it may be, because it leads to minimization of the importance of these increasingly common, albeit largely subjective and non-lethal complaints. Since many workers with these conditions claim total disability, and few examples of cures can be found, multiple chemical sensitivities and sick building syndrome present important challenges to compensation systems.
In the developed world, since many classic occupational toxins are better controlled, symptomatic syndromes, such as those under present scrutiny that are associated with lower-level exposures, are assuming increasing recognition as significant economic and health concerns. Managers are frustrated by these conditions for a number of reasons. As there are no clear-cut regulatory requirements in most jurisdictions which cover indoor air or hypersusceptible individuals (with the important exception being persons with recognized allergic disorders), it is impossible for management to be certain whether or not they are in compliance. Agent-specific contaminant levels developed for industrial settings, such as the US Occupational Safety and Health Administration’s (OSHA’s) permissible exposure levels (PELs) or the American Conference of Governmental Industrial Hygienists’ (ACGIH’s) threshold limit values (TLVs), are clearly not able to prevent or predict symptomatic complaints in office and school workers. Finally, because of the apparent importance of individual susceptibility and psychological factors as determinants of response to low levels of contaminants, the impact of environmental interventions is not as predictable as many would like before a decision is taken to commit scarce building or maintenance resources. Often after complaints arise, a potential culprit such as elevated volatile organic compound levels with respect to outdoor air is found, and yet following remediation, complaints persist or reoccur.
Employees who suffer from symptoms of either sick building syndrome or multiple chemical sensitivities are often less productive and frequently accusatory when management or government is reluctant to commit themselves to interventions which cannot be reliably predicted to ameliorate symptoms. Clearly, occupational health providers are among the few key individuals who may be able to facilitate reasonable middle ground outcomes to the advantage of all concerned. This is true whether or not an underlying cause is low levels of contaminants, or even in the rare case of true mass hysteria, which may often have low-level environmental triggers. Using skill and sensitivity to address, evaluate and incorporate a combination of factors into solutions is an important approach to management.
Sick building syndrome is the more contained and definable of the two conditions, and has even had definitions established by the World Health Organization (1987). Although there is debate, both in general and in specific instances, about whether a given lesion is more attributable to individual workers or to the building, it is widely acknowledged, based on controlled exposure studies with volatile organic compounds, as well as survey epidemiology, that modifiable environmental factors do drive the kinds of symptom which are subsumed under the following article entitled Sick Building Syndrome. In that article, Michael Hodgson (1992) details the triad of personal, work activity and building factors which may contribute in various proportions to symptoms among a population of workers. A major problem is in maintaining good employee-employer communication while investigation and attempts at remediation take place. Health professionals will usually require expert environmental consultation to assist in the evaluation and remediation of identified outbreaks.
Multiple chemical sensitivities is a more problematic condition to define than sick building syndrome. Some organized medical entities, including the American Medical Association, have published position papers which question the scientific basis of the diagnosis of this condition. Many physicians who practise without a rigorous scientific basis have nevertheless championed the validity of this diagnosis. They rely on unproven or over-interpreted diagnostic tests such as lymphocyte activation or brain imaging and may recommend treatments such as sauna therapies and megadoses of vitamins, practices which have in large part engendered the animosity of groups such as the American Medical Association. However, no one denies that there is a group of patients who present with complaints of becoming symptomatic in response to low levels of ambient chemicals. Their constitutional symptoms overlap those of other subjective syndromes such as chronic fatigue syndrome and fibromyalgia. These symptoms include pain, fatigue and confusion, they worsen with low-level chemical exposure and they are reported to be present in a substantial percentage of patients who have been diagnosed with these other syndromes. Of great import, but still unresolved, is the question whether chemical sensitivity symptoms are acquired (and to what extent) because of a preceding chemical overexposure, or whether—as in the commonly reported situation—they arise without a major identified precipitating event.
Multiple chemical sensitivities is sometimes invoked as an outcome in certain sick building syndrome outbreaks which are not resolved or ameliorated after routine investigation and remediation. Here it is clear that MCS afflicts an individual or small number of people, rarely a population; it is the effect on a population that may even be a criterion for the sick building syndrome by some definitions. MCS seems to be endemic in populations, whereas sick building syndrome is often epidemic; however, preliminary investigations suggest that some degree of chemical sensitivity (and chronic fatigue) may occur in outbreaks, as was found among American veterans of the Persian Gulf conflict. The controlled exposure studies which have done much to clarify the role of volatile organic compounds and irritants in sick building syndrome have yet to be performed in a controlled manner for multiple chemical sensitivities.
Many practitioners claim to recognize MCS when they see it, but there is no agreed-upon definition. It may well be included as a condition which “overlaps” other non-occupational syndromes such as chronic fatigue syndrome, fibromyalgia, somatization disorder and others. Sorting out its relationship to both psychiatric diagnoses and to early reports suggests that when the onset of the syndrome is fairly definable, there is a much lower rate of diagnosable psychiatric co-morbidity (Fiedler et al. 1996). The phenomenon of odor-triggered symptoms is distinctive, but clearly not unique, and the extent to which this is an occupational condition at all is debated. This is important because Dr. Cullen’s (1987) definition, like many others, describes multiple chemical sensitivities as a sequel to a better-characterized occupational or environmental disorder. However, as stated above, symptoms following exposure to ambient levels of odorants are common among individuals both with and without clinical diagnoses, and it may be just as important to explore the similarities between MCS and other conditions as to define the differences (Kipen et al. 1995; Buchwald and Garrity 1994).
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."