Recognition of Hazards
A workplace hazard can be defined as any condition that may adversely affect the well-being or health of exposed persons. Recognition of hazards in any occupational activity involves characterization of the workplace by identifying hazardous agents and groups of workers potentially exposed to these hazards. The hazards might be of chemical, biological or physical origin (see table 1). Some hazards in the work environment are easy to recognize—for example, irritants, which have an immediate irritating effect after skin exposure or inhalation. Others are not so easy to recognize—for example, chemicals which are accidentally formed and have no warning properties. Some agents like metals (e.g., lead, mercury, cadmium, manganese), which may cause injury after several years of exposure, might be easy to identify if you are aware of the risk. A toxic agent may not constitute a hazard at low concentrations or if no one is exposed. Basic to the recognition of hazards are identification of possible agents at the workplace, knowledge about health risks of these agents and awareness of possible exposure situations.
Table 1. Hazards of chemical, biological and physical agents.
|
Type of hazard |
Description |
Examples |
|
CHEMICAL HAZARDS
|
Chemicals enter the body principally through inhalation, skin absorption or ingestion. The toxic effect might be acute, chronic or both., |
|
|
Corrosion |
Corrosive chemicals actually cause tissue destruction at the site of contact. Skin, eyes and digestive system are the most commonly affected parts of the body. |
Concentrated acids and alkalis, phosphorus |
|
Irritation |
Irritants cause inflammation of tissues where they are deposited. Skin irritants may cause reactions like eczema or dermatitis. Severe respiratory irritants might cause shortness of breath, inflammatory responses and oedema. |
Skin: acids, alkalis, solvents, oils Respiratory: aldehydes, alkaline dusts, ammonia, nitrogendioxide, phosgene, chlorine, bromine, ozone |
|
Allergic reactions |
Chemical allergens or sensitizers can cause skin or respiratory allergic reactions. |
Skin: colophony (rosin), formaldehyde, metals like chromium or nickel, some organic dyes, epoxy hardeners, turpentine Respiratory: isocyanates, fibre-reactive dyes, formaldehyde, many tropical wood dusts, nickel
|
|
Asphyxiation |
Asphyxiants exert their effects by interfering with the oxygenation of the tissues. Simple asphyxiants are inert gases that dilute the available atmospheric oxygen below the level required to support life. Oxygen-deficient atmospheres may occur in tanks, holds of ships, silos or mines. Oxygen concentration in air should never be below 19.5% by volume. Chemical asphyxiants prevent oxygen transport and the normal oxygenation of blood or prevent normal oxygenation of tissues. |
Simple asphyxiants: methane, ethane, hydrogen, helium Chemical asphyxiants: carbon monoxide, nitrobenzene, hydrogencyanide, hydrogen sulphide
|
|
Cancer |
Known human carcinogens are chemicals that have been clearly demonstrated to cause cancer in humans. Probable human carcinogens are chemicals that have been clearly demonstrated to cause cancer in animals or the evidence is not definite in humans. Soot and coal tars were the first chemicals suspected to cause cancer. |
Known: benzene (leukaemia); vinyl chloride (liver angio-sarcoma); 2-naphthylamine, benzidine (bladder cancer); asbestos (lung cancer, mesothelioma); hardwood dust (nasalor nasal sinus adenocarcinoma) Probable: formaldehyde, carbon tetrachloride, dichromates, beryllium |
|
Reproductive effects
|
Reproductive toxicants interfere with reproductive or sexual functioning of an individual. |
Manganese, carbon disulphide, monomethyl and ethyl ethers of ethylene glycol, mercury |
|
|
Developmental toxicants are agents that may cause an adverse effect in offspring of exposed persons; for example, birth defects. Embryotoxic or foetotoxic chemicals can cause spontaneous abortions or miscarriages. |
Organic mercury compounds, carbon monoxide, lead, thalidomide, solvents |
|
Systemic poisons
|
Systemic poisons are agents that cause injury to particular organs or body systems. |
Brain: solvents, lead, mercury, manganese Peripheral nervous system: n-hexane, lead, arsenic, carbon disulphide Blood-forming system: benzene, ethylene glycol ethers Kidneys: cadmium, lead, mercury, chlorinated hydrocarbons Lungs: silica, asbestos, coal dust (pneumoconiosis)
|
|
BIOLOGICAL HAZARDS
|
Biological hazards can be defined as organic dusts originating from different sources of biological origin such as virus, bacteria, fungi, proteins from animals or substances from plants such as degradation products of natural fibres. The aetiological agent might be derived from a viable organism or from contaminants or constitute a specific component in the dust. Biological hazards are grouped into infectious and non-infectious agents. Non-infectious hazards can be further divided into viable organisms, biogenic toxins and biogenic allergens. |
|
|
Infectious hazards |
Occupational diseases from infectious agents are relatively uncommon. Workers at risk include employees at hospitals, laboratory workers, farmers, slaughterhouse workers, veterinarians, zoo keepers and cooks. Susceptibility is very variable (e.g., persons treated with immunodepressing drugs will have a high sensitivity). |
Hepatitis B, tuberculosis, anthrax, brucella, tetanus, chlamydia psittaci, salmonella |
|
Viable organisms and biogenic toxins |
Viable organisms include fungi, spores and mycotoxins; biogenic toxins include endotoxins, aflatoxin and bacteria. The products of bacterial and fungal metabolism are complex and numerous and affected by temperature, humidity and kind of substrate on which they grow. Chemically they might consist of proteins, lipoproteins or mucopolysaccharides. Examples are Gram positive and Gram negative bacteria and moulds. Workers at risk include cotton mill workers, hemp and flax workers, sewage and sludge treatment workers, grain silo workers. |
Byssinosis, “grain fever”, Legionnaire’s disease |
|
Biogenic allergens |
Biogenic allergens include fungi, animal-derived proteins, terpenes, storage mites and enzymes. A considerable part of the biogenic allergens in agriculture comes from proteins from animal skin, hair from furs and protein from the faecal material and urine. Allergens might be found in many industrial environments, such as fermentation processes, drug production, bakeries, paper production, wood processing (saw mills, production, manufacturing) as well as in bio-technology (enzyme and vaccine production, tissue culture) and spice production. In sensitized persons, exposure to the allergic agents may induce allergic symptoms such as allergic rhinitis, conjunctivitis or asthma. Allergic alveolitis is characterized by acute respiratory symptoms like cough, chills, fever, headache and pain in the muscles, which might lead to chronic lung fibrosis. |
Occupational asthma: wool, furs, wheat grain, flour, red cedar, garlic powder Allergic alveolitis: farmer’s disease, bagassosis, “bird fancier’s disease”, humidifier fever, sequoiosis
|
|
PHYSICAL HAZARDS |
|
|
|
Noise |
Noise is considered as any unwanted sound that may adversely affect the health and well-being of individuals or populations. Aspects of noise hazards include total energy of the sound, frequency distribution, duration of exposure and impulsive noise. Hearing acuity is generally affected first with a loss or dip at 4000 Hz followed by losses in the frequency range from 2000 to 6000 Hz. Noise might result in acute effects like communication problems, decreased concentration, sleepiness and as a consequence interference with job performance. Exposure to high levels of noise (usually above 85 dBA) or impulsive noise (about 140 dBC) over a significant period of time may cause both temporary and chronic hearing loss. Permanent hearing loss is the most common occupational disease in compensation claims. |
Foundries, woodworking, textile mills, metalworking |
|
Vibration |
Vibration has several parameters in common with noise-frequency, amplitude, duration of exposure and whether it is continuous or intermittent. Method of operation and skilfulness of the operator seem to play an important role in the development of harmful effects of vibration. Manual work using powered tools is associated with symptoms of peripheral circulatory disturbance known as “Raynaud’s phenomenon” or “vibration-induced white fingers” (VWF). Vibrating tools may also affect the peripheral nervous system and the musculo-skeletal system with reduced grip strength, low back pain and degenerative back disorders. |
Contract machines, mining loaders, fork-lift trucks, pneumatic tools, chain saws |
|
Ionizing radiation
|
The most important chronic effect of ionizing radiation is cancer, including leukaemia. Overexposure from comparatively low levels of radiation have been associated with dermatitis of the hand and effects on the haematological system. Processes or activities which might give excessive exposure to ionizing radiation are very restricted and regulated. |
Nuclear reactors, medical and dental x-ray tubes, particle accelerators, radioisotopes |
|
Non-ionizing radiation
|
Non-ionizing radiation consists of ultraviolet radiation, visible radiation, infrared, lasers, electromagnetic fields (microwaves and radio frequency) and extreme low frequency radiation. IR radiation might cause cataracts. High-powered lasers may cause eye and skin damage. There is an increasing concern about exposure to low levels of electromagnetic fields as a cause of cancer and as a potential cause of adverse reproductive outcomes among women, especially from exposure to video display units. The question about a causal link to cancer is not yet answered. Recent reviews of available scientific knowledge generally conclude that there is no association between use of VDUs and adverse reproductive outcome. |
Ultraviolet radiation: arc welding and cutting; UV curing of inks, glues, paints, etc.; disinfection; product control Infrared radiation: furnaces, glassblowing Lasers: communications, surgery, construction
|
Identification and Classification of Hazards
Before any occupational hygiene investigation is performed the purpose must be clearly defined. The purpose of an occupational hygiene investigation might be to identify possible hazards, to evaluate existing risks at the workplace, to prove compliance with regulatory requirements, to evaluate control measures or to assess exposure with regard to an epidemiological survey. This article is restricted to programmes aimed at identification and classification of hazards at the workplace. Many models or techniques have been developed to identify and evaluate hazards in the working environment. They differ in complexity, from simple checklists, preliminary industrial hygiene surveys, job-exposure matrices and hazard and operability studies to job exposure profiles and work surveillance programmes (Renes 1978; Gressel and Gideon 1991; Holzner, Hirsh and Perper 1993; Goldberg et al. 1993; Bouyer and Hémon 1993; Panett, Coggon and Acheson 1985; Tait 1992). No single technique is a clear choice for everyone, but all techniques have parts which are useful in any investigation. The usefulness of the models also depends on the purpose of the investigation, size of workplace, type of production and activity as well as complexity of operations.
Identification and classification of hazards can be divided into three basic elements: workplace characterization, exposure pattern and hazard evaluation.
Workplace characterization
A workplace might have from a few employees up to several thousands and have different activities (e.g., production plants, construction sites, office buildings, hospitals or farms). At a workplace different activities can be localized to special areas such as departments or sections. In an industrial process, different stages and operations can be identified as production is followed from raw materials to finished products.
Detailed information should be obtained about processes, operations or other activities of interest, to identify agents utilized, including raw materials, materials handled or added in the process, primary products, intermediates, final products, reaction products and by-products. Additives and catalysts in a process might also be of interest to identify. Raw material or added material which has been identified only by trade name must be evaluated by chemical composition. Information or safety data sheets should be available from manufacturer or supplier.
Some stages in a process might take place in a closed system without anyone exposed, except during maintenance work or process failure. These events should be recognized and precautions taken to prevent exposure to hazardous agents. Other processes take place in open systems, which are provided with or without local exhaust ventilation. A general description of the ventilation system should be provided, including local exhaust system.
When possible, hazards should be identified in the planning or design of new plants or processes, when changes can be made at an early stage and hazards might be anticipated and avoided. Conditions and procedures that may deviate from the intended design must be identified and evaluated in the process state. Recognition of hazards should also include emissions to the external environment and waste materials. Facility locations, operations, emission sources and agents should be grouped together in a systematic way to form recognizable units in the further analysis of potential exposure. In each unit, operations and agents should be grouped according to health effects of the agents and estimation of emitted amounts to the work environment.
Exposure patterns
The main exposure routes for chemical and biological agents are inhalation and dermal uptake or incidentally by ingestion. The exposure pattern depends on frequency of contact with the hazards, intensity of exposure and time of exposure. Working tasks have to be systematically examined. It is important not only to study work manuals but to look at what actually happens at the workplace. Workers might be directly exposed as a result of actually performing tasks, or be indirectly exposed because they are located in the same general area or location as the source of exposure. It might be necessary to start by focusing on working tasks with high potential to cause harm even if the exposure is of short duration. Non-routine and intermittent operations (e.g., maintenance, cleaning and changes in production cycles) have to be considered. Working tasks and situations might also vary throughout the year.
Within the same job title exposure or uptake might differ because some workers wear protective equipment and others do not. In large plants, recognition of hazards or a qualitative hazard evaluation very seldom can be performed for every single worker. Therefore workers with similar working tasks have to be classified in the same exposure group. Differences in working tasks, work techniques and work time will result in considerably different exposure and have to be considered. Persons working outdoors and those working without local exhaust ventilation have been shown to have a larger day-to-day variability than groups working indoors with local exhaust ventilation (Kromhout, Symanski and Rappaport 1993). Work processes, agents applied for that process/job or different tasks within a job title might be used, instead of the job title, to characterize groups with similar exposure. Within the groups, workers potentially exposed must be identified and classified according to hazardous agents, routes of exposure, health effects of the agents, frequency of contact with the hazards, intensity and time of exposure. Different exposure groups should be ranked according to hazardous agents and estimated exposure in order to determine workers at greatest risk.
Qualitative hazard evaluation
Possible health effects of chemical, biological and physical agents present at the workplace should be based on an evaluation of available epidemiological, toxicological, clinical and environmental research. Up-to-date information about health hazards for products or agents used at the workplace should be obtained from health and safety journals, databases on toxicity and health effects, and relevant scientific and technical literature.
Material Safety Data Sheets (MSDSs) should if necessary be updated. Data Sheets document percentages of hazardous ingredients together with the Chemical Abstracts Service chemical identifier, the CAS-number, and threshold limit value (TLV), if any. They also contain information about health hazards, protective equipment, preventive actions, manufacturer or supplier, and so on. Sometimes the ingredients reported are rather rudimentary and have to be supplemented with more detailed information.
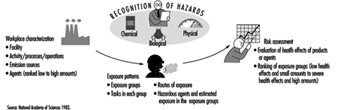
Monitored data and records of measurements should be studied. Agents with TLVs provide general guidance in deciding whether the situation is acceptable or not, although there must be allowance for possible interactions when workers are exposed to several chemicals. Within and between different exposure groups, workers should be ranked according to health effects of agents present and estimated exposure (e.g., from slight health effects and low exposure to severe health effects and estimated high exposure). Those with the highest ranks deserve highest priority. Before any prevention activities start it might be necessary to perform an exposure monitoring programme. All results should be documented and easily attainable. A working scheme is illustrated in figure 1.
Figure 1. Elements of risk assessment
In occupational hygiene investigations the hazards to the outdoor environment (e.g., pollution and greenhouse effects as well as effects on the ozone layer) might also be considered.
Chemical, Biological and Physical Agents
Hazards might be of chemical, biological or physical origin. In this section and in table 1 a brief description of the various hazards will be given together with examples of environments or activities where they will be found (Casarett 1980; International Congress on Occupational Health 1985; Jacobs 1992; Leidel, Busch and Lynch 1977; Olishifski 1988; Rylander 1994). More detailed information will be found elsewhere in this Encyclopaedia.
Chemical agents
Chemicals can be grouped into gases, vapours, liquids and aerosols (dusts, fumes, mists).
Gases
Gases are substances that can be changed to liquid or solid state only by the combined effects of increased pressure and decreased temperature. Handling gases always implies risk of exposure unless they are processed in closed systems. Gases in containers or distribution pipes might accidentally leak. In processes with high temperatures (e.g., welding operations and exhaust from engines) gases will be formed.
Vapours
Vapours are the gaseous form of substances that normally are in the liquid or solid state at room temperature and normal pressure. When a liquid evaporates it changes to a gas and mixes with the surrounding air. A vapour can be regarded as a gas, where the maximal concentration of a vapour depends on the temperature and the saturation pressure of the substance. Any process involving combustion will generate vapours or gases. Degreasing operations might be performed by vapour phase degreasing or soak cleaning with solvents. Work activities like charging and mixing liquids, painting, spraying, cleaning and dry cleaning might generate harmful vapours.
Liquids
Liquids may consist of a pure substance or a solution of two or more substances (e.g., solvents, acids, alkalis). A liquid stored in an open container will partially evaporate into the gas phase. The concentration in the vapour phase at equilibrium depends on the vapour pressure of the substance, its concentration in the liquid phase, and the temperature. Operations or activities with liquids might give rise to splashes or other skin contact, besides harmful vapours.
Dusts
Dusts consist of inorganic and organic particles, which can be classified as inhalable, thoracic or respirable, depending on particle size. Most organic dusts have a biological origin. Inorganic dusts will be generated in mechanical processes like grinding, sawing, cutting, crushing, screening or sieving. Dusts may be dispersed when dusty material is handled or whirled up by air movements from traffic. Handling dry materials or powder by weighing, filling, charging, transporting and packing will generate dust, as will activities like insulation and cleaning work.
Fumes
Fumes are solid particles vaporized at high temperature and condensed to small particles. The vaporization is often accompanied by a chemical reaction such as oxidation. The single particles that make up a fume are extremely fine, usually less than 0.1 μm, and often aggregate in larger units. Examples are fumes from welding, plasma cutting and similar operations.
Mists
Mists are suspended liquid droplets generated by condensation from the gaseous state to the liquid state or by breaking up a liquid into a dispersed state by splashing, foaming or atomizing. Examples are oil mists from cutting and grinding operations, acid mists from electroplating, acid or alkali mists from pickling operations or paint spray mists from spraying operations.
Goals, Definitions and General Information
Work is essential for life, development and personal fulfilment. Unfortunately, indispensable activities such as food production, extraction of raw materials, manufacturing of goods, energy production and services involve processes, operations and materials which can, to a greater or lesser extent, create hazards to the health of workers and those in nearby communities, as well as to the general environment.
However, the generation and release of harmful agents in the work environment can be prevented, through adequate hazard control interventions, which not only protect workers’ health but also limit the damage to the environment often associated with industrialization. If a harmful chemical is eliminated from a work process, it will neither affect the workers nor go beyond, to pollute the environment.
The profession that aims specifically at the prevention and control of hazards arising from work processes is occupational hygiene. The goals of occupational hygiene include the protection and promotion of workers’ health, the protection of the environment and contribution to a safe and sustainable development.
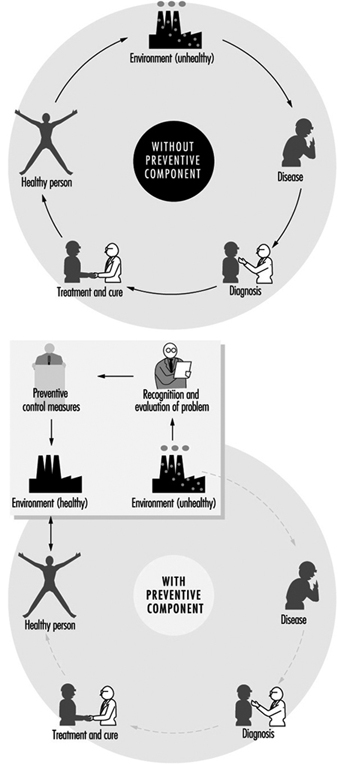
The need for occupational hygiene in the protection of workers’ health cannot be overemphasized. Even when feasible, the diagnosis and the cure of an occupational disease will not prevent further occurrences, if exposure to the aetiological agent does not cease. So long as the unhealthy work environment remains unchanged, its potential to impair health remains. Only the control of health hazards can break the vicious circle illustrated in figure 1.
Figure 1. Interactions between people and the environment
However, preventive action should start much earlier, not only before the manifestation of any health impairment but even before exposure actually occurs. The work environment should be under continuous surveillance so that hazardous agents and factors can be detected and removed, or controlled, before they cause any ill effects; this is the role of occupational hygiene.
Furthermore, occupational hygiene may also contribute to a safe and sustainable development, that is “to ensure that (development) meets the needs of the present without compromising the ability of the future generations to meet their own needs” (World Commission on Environment and Development 1987). Meeting the needs of the present world population without depleting or damaging the global resource base, and without causing adverse health and environmental consequences, requires knowledge and means to influence action (WHO 1992a); when related to work processes this is closely related to occupational hygiene practice.
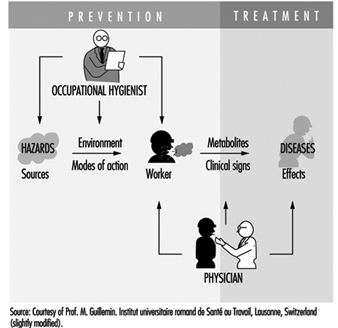
Occupational health requires a multidisciplinary approach and involves fundamental disciplines, one of which is occupational hygiene, along with others which include occupational medicine and nursing, ergonomics and work psychology. A schematic representation of the scopes of action for occupational physicians and occupational hygienists is presented in figure 2.
Figure 2. Scopes of action for occupational physicians and occupational hygienists.
It is important that decision makers, managers and workers themselves, as well as all occupational health professionals, understand the essential role that occupational hygiene plays in the protection of workers’ health and of the environment, as well as the need for specialized professionals in this field. The close link between occupational and environmental health should also be kept in mind, since the prevention of pollution from industrial sources, through the adequate handling and disposal of hazardous effluents and waste, should be started at the workplace level. (See “Evaluation of the work environment”).
Concepts and Definitions
Occupational hygiene
Occupational hygiene is the science of the anticipation, recognition, evaluation and control of hazards arising in or from the workplace, and which could impair the health and well-being of workers, also taking into account the possible impact on the surrounding communities and the general environment.
Definitions of occupational hygiene may be presented in different ways; however, they all have essentially the same meaning and aim at the same fundamental goal of protecting and promoting the health and well-being of workers, as well as protecting the general environment, through preventive actions in the workplace.
Occupational hygiene is not yet universally recognized as a profession; however, in many countries, framework legislation is emerging that will lead to its establishment.
Occupational hygienist
An occupational hygienist is a professional able to:
- anticipate the health hazards that may result from work processes, operations and equipment, and accordingly advise on their planning and design
- recognize and understand, in the work environment, the occurrence (real or potential) of chemical, physical and biological agents and other stresses, and their interactions with other factors, which may affect the health and well-being of workers
- understand the possible routes of agent entry into the human body, and the effects that such agents and other factors may have on health
- assess workers’ exposure to potentially harmful agents and factors and to evaluate the results
- evaluate work processes and methods, from the point of view of the possible generation and release/propagation of potentially harmful agents and other factors, with a view to eliminating exposures, or reducing them to acceptable levels
- design, recommend for adoption, and evaluate the effectiveness of control strategies, alone or in collaboration with other professionals to ensure effective and economical control
- participate in overall risk analysis and management of an agent, process or workplace, and contribute to the establishment of priorities for risk management
- understand the legal framework for occupational hygiene practice in their own country
- educate, train, inform and advise persons at all levels, in all aspects of hazard communication
- work effectively in a multidisciplinary team involving other professionals
- recognize agents and factors that may have environmental impact, and understand the need to integrate occupational hygiene practice with environmental protection.
It should be kept in mind that a profession consists not only of a body of knowledge, but also of a Code of Ethics; national occupational hygiene associations, as well as the International Occupational Hygiene Association (IOHA), have their own Codes of Ethics (WHO 1992b).
Occupational hygiene technician
An occupational hygiene technician is “a person competent to carry out measurements of the work environment” but not “to make the interpretations, judgements, and recommendations required from an occupational hygienist”. The necessary level of competence may be obtained in a comprehensive or limited field (WHO 1992b).
International Occupational Hygiene Association (IOHA)
IOHA was formally established, during a meeting in Montreal, on June 2, 1987. At present IOHA has the participation of 19 national occupational hygiene associations, with over nineteen thousand members from seventeen countries.
The primary objective of IOHA is to promote and develop occupational hygiene throughout the world, at a high level of professional competence, through means that include the exchange of information among organizations and individuals, the further development of human resources and the promotion of a high standard of ethical practice. IOHA activities include scientific meetings and publication of a newsletter. Members of affiliated associations are automatically members of IOHA; it is also possible to join as an individual member, for those in countries where there is not yet a national association.
Certification
In addition to an accepted definition of occupational hygiene and of the role of the occupational hygienist, there is need for the establishment of certification schemes to ensure acceptable standards of occupational hygiene competence and practice. Certification refers to a formal scheme based on procedures for establishing and maintaining knowledge, skills and competence of professionals (Burdorf 1995).
IOHA has promoted a survey of existing national certification schemes (Burdorf 1995), together with recommendations for the promotion of international cooperation in assuring the quality of professional occupational hygienists, which include the following:
- “the harmonization of standards on the competence and practice of professional occupational hygienists”
- “the establishment of an international body of peers to review the quality of existing certification schemes”.
Other suggestions in this report include items such as: “reciprocity” and “cross-acceptance of national designations, ultimately aiming at an umbrella scheme with one internationally accepted designation”.
The Practice of Occupational Hygiene
The classical steps in occupational hygiene practice are:
- the recognition of the possible health hazards in the work environment
- the evaluation of hazards, which is the process of assessing exposure and reaching conclusions as to the level of risk to human health
- prevention and control of hazards, which is the process of developing and implementing strategies to eliminate, or reduce to acceptable levels, the occurrence of harmful agents and factors in the workplace, while also accounting for environmental protection.
The ideal approach to hazard prevention is “anticipated and integrated preventive action”, which should include:
- occupational health and environmental impact assessments, prior to the design and installation of any new workplace
- selection of the safest, least hazardous and least polluting technology (“cleaner production”)
- environmentally appropriate location
- proper design, with adequate layout and appropriate control technology, including for the safe handling and disposal of the resulting effluents and waste
- elaboration of guidelines and regulations for training on the correct operation of processes, including on safe work practices, maintenance and emergency procedures.
The importance of anticipating and preventing all types of environmental pollution cannot be overemphasized. There is, fortunately, an increasing tendency to consider new technologies from the point of view of the possible negative impacts and their prevention, from the design and installation of the process to the handling of the resulting effluents and waste, in the so-called cradle-to-grave approach. Environmental disasters, which have occurred in both developed and developing countries, could have been avoided by the application of appropriate control strategies and emergency procedures in the workplace.
Economic aspects should be viewed in broader terms than the usual initial cost consideration; more expensive options that offer good health and environmental protection may prove to be more economical in the long run. The protection of workers’ health and of the environment must start much earlier than it usually does. Technical information and advice on occupational and environmental hygiene should always be available to those designing new processes, machinery, equipment and workplaces. Unfortunately such information is often made available much too late, when the only solution is costly and difficult retrofitting, or worse, when consequences have already been disastrous.
Recognition of hazards
Recognition of hazards is a fundamental step in the practice of occupational hygiene, indispensable for the adequate planning of hazard evaluation and control strategies, as well as for the establishment of priorities for action. For the adequate design of control measures, it is also necessary to physically characterize contaminant sources and contaminant propagation paths.
The recognition of hazards leads to the determination of:
- which agents may be present and under which circumstances
- the nature and possible extent of associated adverse effects on health and well-being.
The identification of hazardous agents, their sources and the conditions of exposure requires extensive knowledge and careful study of work processes and operations, raw materials and chemicals used or generated, final products and eventual by-products, as well as of possibilities for the accidental formation of chemicals, decomposition of materials, combustion of fuels or the presence of impurities. The recognition of the nature and potential magnitude of the biological effects that such agents may cause if overexposure occurs, requires knowledge on and access to toxicological information. International sources of information in this respect include International Programme on Chemical Safety (IPCS), International Agency for Research on Cancer (IARC) and International Register of Potentially Toxic Chemicals, United Nations Environment Programme (UNEP-IRPTC).
Agents which pose health hazards in the work environment include airborne contaminants; non-airborne chemicals; physical agents, such as heat and noise; biological agents; ergonomic factors, such as inadequate lifting procedures and working postures; and psychosocial stresses.
Occupational hygiene evaluations
Occupational hygiene evaluations are carried out to assess workers’ exposure, as well as to provide information for the design, or to test the efficiency, of control measures.
Evaluation of workers’ exposure to occupational hazards, such as airborne contaminants, physical and biological agents, is covered elsewhere in this chapter. Nevertheless, some general considerations are provided here for a better understanding of the field of occupational hygiene.
It is important to keep in mind that hazard evaluation is not an end in itself, but must be considered as part of a much broader procedure that starts with the realization that a certain agent, capable of causing health impairment, may be present in the work environment, and concludes with the control of this agent so that it will be prevented from causing harm. Hazard evaluation paves the way to, but does not replace, hazard prevention.
Exposure assessment
Exposure assessment aims at determining how much of an agent workers have been exposed to, how often and for how long. Guidelines in this respect have been established both at the national and international level—for example, EN 689, prepared by the Comité Européen de Normalisation (European Committee for Standardization) (CEN 1994).
In the evaluation of exposure to airborne contaminants, the most usual procedure is the assessment of inhalation exposure, which requires the determination of the air concentration of the agent to which workers are exposed (or, in the case of airborne particles, the air concentration of the relevant fraction, e.g., the “respirable fraction”) and the duration of the exposure. However, if routes other than inhalation contribute appreciably to the uptake of a chemical, an erroneous judgement may be made by looking only at the inhalation exposure. In such cases, total exposure has to be assessed, and a very useful tool for this is biological monitoring.
The practice of occupational hygiene is concerned with three kinds of situations:
- initial studies to assess workers’ exposure
- follow-up monitoring/surveillance
- exposure assessment for epidemiological studies.
A primary reason for determining whether there is overexposure to a hazardous agent in the work environment, is to decide whether interventions are required. This often, but not necessarily, means establishing whether there is compliance with an adopted standard, which is usually expressed in terms of an occupational exposure limit. The determination of the “worst exposure” situation may be enough to fulfil this purpose. Indeed, if exposures are expected to be either very high or very low in relation to accepted limit values, the accuracy and precision of quantitative evaluations can be lower than when the exposures are expected to be closer to the limit values. In fact, when hazards are obvious, it may be wiser to invest resources initially on controls and to carry out more precise environmental evaluations after controls have been implemented.
Follow-up evaluations are often necessary, particularly if the need existed to install or improve control measures or if changes in the processes or materials utilized were foreseen. In these cases, quantitative evaluations have an important surveillance role in:
- evaluating the adequacy, testing the efficiency or disclosing possible failures in the control systems
- detecting whether alterations in the processes, such as operating temperature, or in the raw materials, have altered the exposure situation.
Whenever an occupational hygiene survey is carried out in connection with an epidemiological study in order to obtain quantitative data on relationships between exposure and health effects, the exposure must be characterized with a high level of accuracy and precision. In this case, all exposure levels must be adequately characterized, since it would not be enough, for example, to characterize only the worst case exposure situation. It would be ideal, although difficult in practice, to always keep precise and accurate exposure assessment records since there may be a future need to have historical exposure data.
In order to ensure that evaluation data is representative of workers’ exposure, and that resources are not wasted, an adequate sampling strategy, accounting for all possible sources of variability, must be designed and followed. Sampling strategies, as well as measurement techniques, are covered in “Evaluation of the work environment”.
Interpretation of results
The degree of uncertainty in the estimation of an exposure parameter, for example, the true average concentration of an airborne contaminant, is determined through statistical treatment of the results from measurements (e.g., sampling and analysis). The level of confidence on the results will depend on the coefficient of variation of the “measuring system” and on the number of measurements. Once there is an acceptable confidence, the next step is to consider the health implications of the exposure: what does it mean for the health of the exposed workers: now? in the near future? in their working life? will there be an impact on future generations?
The evaluation process is only completed when results from measurements are interpreted in view of data (sometimes referred to as “risk assessment data”) derived from experimental toxicology, epidemiological and clinical studies and, in certain cases, clinical trials. It should be clarified that the term risk assessment has been used in connection with two types of assessments—the assessment of the nature and extent of risk resulting from exposure to chemicals or other agents, in general, and the assessment of risk for a particular worker or group of workers, in a specific workplace situation.
In the practice of occupational hygiene, exposure assessment results are often compared with adopted occupational exposure limits which are intended to provide guidance for hazard evaluation and for setting target levels for control. Exposure in excess of these limits requires immediate remedial action by the improvement of existing control measures or implementation of new ones. In fact, preventive interventions should be made at the “action level”, which varies with the country (e.g., one-half or one-fifth of the occupational exposure limit). A low action level is the best assurance of avoiding future problems.
Comparison of exposure assessment results with occupational exposure limits is a simplification, since, among other limitations, many factors which influence the uptake of chemicals (e.g., individual susceptibilities, physical activity and body build) are not accounted for by this procedure. Furthermore, in most workplaces there is simultaneous exposure to many agents; hence a very important issue is that of combined exposures and agent interactions, because the health consequences of exposure to a certain agent alone may differ considerably from the consequences of exposure to this same agent in combination with others, particularly if there is synergism or potentiation of effects.
Measurements for control
Measurements with the purpose of investigating the presence of agents and the patterns of exposure parameters in the work environment can be extremely useful for the planning and design of control measures and work practices. The objectives of such measurements include:
- source identification and characterization
- spotting of critical points in closed systems or enclosures (e.g., leaks)
- determination of propagation paths in the work environment
- comparison of different control interventions
- verification that respirable dust has settled together with the coarse visible dust, when using water sprays
- checking that contaminated air is not coming from an adjacent area.
Direct-reading instruments are extremely useful for control purposes, particularly those which can be used for continuous sampling and reflect what is happening in real time, thus disclosing exposure situations which might not otherwise be detected and which need to be controlled. Examples of such instruments include: photo-ionization detectors, infrared analysers, aerosol meters and detector tubes. When sampling to obtain a picture of the behaviour of contaminants, from the source throughout the work environment, accuracy and precision are not as critical as they would be for exposure assessment.
Recent developments in this type of measurement for control purposes include visualization techniques, one of which is the Picture Mix Exposure—PIMEX (Rosen 1993). This method combines a video image of the worker with a scale showing airborne contaminant concentrations, which are continuously measured, at the breathing zone, with a real-time monitoring instrument, thus making it possible to visualize how the concentration varies while the task is performed. This provides an excellent tool for comparing the relative efficacy of different control measures, such as ventilation and work practices, thus contributing to better design.
Measurements are also needed to assess the efficiency of control measures. In this case, source sampling or area sampling are convenient, alone or in addition to personal sampling, for the assessment of workers’ exposure. In order to assure validity, the locations for “before” and “after” sampling (or measurements) and the techniques used should be the same, or equivalent, in sensitivity, accuracy and precision.
Hazard prevention and control
The primary goal of occupational hygiene is the implementation of appropriate hazard prevention and control measures in the work environment. Standards and regulations, if not enforced, are meaningless for the protection of workers’ health, and enforcement usually requires both monitoring and control strategies. The absence of legally established standards should not be an obstacle to the implementation of the necessary measures to prevent harmful exposures or control them to the lowest level feasible. When serious hazards are obvious, control should be recommended, even before quantitative evaluations are carried out. It may sometimes be necessary to change the classical concept of “recognition-evaluation-control” to “recognition-control-evaluation”, or even to “recognition-control”, if capabilities for evaluation of hazards do not exist. Some examples of hazards in obvious need of action without the necessity of prior environmental sampling are electroplating carried out in an unventilated, small room, or using a jackhammer or sand-blasting equipment with no environmental controls or protective equipment. For such recognized health hazards, the immediate need is control, not quantitative evaluation.
Preventive action should in some way interrupt the chain by which the hazardous agent—a chemical, dust, a source of energy—is transmitted from the source to the worker. There are three major groups of control measures: engineering controls, work practices and personal measures.
The most efficient hazard prevention approach is the application of engineering control measures which prevent occupational exposures by managing the work environment, thus decreasing the need for initiatives on the part of workers or potentially exposed persons. Engineering measures usually require some process modifications or mechanical structures, and involve technical measures that eliminate or reduce the use, generation or release of hazardous agents at their source, or, when source elimination is not possible, engineering measures should be designed to prevent or reduce the spread of hazardous agents into the work environment by:
- containing them
- removing them immediately beyond the source
- interfering with their propagation
- reducing their concentration or intensity.
Control interventions which involve some modification of the source are the best approach because the harmful agent can be eliminated or reduced in concentration or intensity. Source reduction measures include substitution of materials, substitution/modification of processes or equipment and better maintenance of equipment.
When source modifications are not feasible, or are not sufficient to attain the desired level of control, then the release and dissemination of hazardous agents in the work environment should be prevented by interrupting their transmission path through measures such as isolation (e.g., closed systems, enclosures), local exhaust ventilation, barriers and shields, isolation of workers.
Other measures aiming at reducing exposures in the work environment include adequate workplace design, dilution or displacement ventilation, good housekeeping and adequate storage. Labelling and warning signs can assist workers in safe work practices. Monitoring and alarm systems may be required in a control programme. Monitors for carbon monoxide around furnaces, for hydrogen sulphide in sewage work, and for oxygen deficiency in closed spaces are some examples.
Work practices are an important part of control—for example, jobs in which a worker’s work posture can affect exposure, such as whether a worker bends over his or her work. The position of the worker may affect the conditions of exposure (e.g., breathing zone in relation to contaminant source, possibility of skin absorption).
Lastly, occupational exposure can be avoided or reduced by placing a protective barrier on the worker, at the critical entry point for the harmful agent in question (mouth, nose, skin, ear)—that is, the use of personal protective devices. It should be pointed out that all other possibilities of control should be explored before considering the use of personal protective equipment, as this is the least satisfactory means for routine control of exposures, particularly to airborne contaminants.
Other personal preventive measures include education and training, personal hygiene and limitation of exposure time.
Continuous evaluations, through environmental monitoring and health surveillance, should be part of any hazard prevention and control strategy.
Appropriate control technology for the work environment must also encompass measures for the prevention of environmental pollution (air, water, soil), including adequate management of hazardous waste.
Although most of the control principles hereby mentioned apply to airborne contaminants, many are also applicable to other types of hazards. For example, a process can be modified to produce less air contaminants or to produce less noise or less heat. An isolating barrier can isolate workers from a source of noise, heat or radiation.
Far too often prevention dwells on the most widely known measures, such as local exhaust ventilation and personal protective equipment, without proper consideration of other valuable control options, such as alternative cleaner technologies, substitution of materials, modification of processes, and good work practices. It often happens that work processes are regarded as unchangeable when, in reality, changes can be made which effectively prevent or at least reduce the associated hazards.
Hazard prevention and control in the work environment requires knowledge and ingenuity. Effective control does not necessarily require very costly and complicated measures. In many cases, hazard control can be achieved through appropriate technology, which can be as simple as a piece of impervious material between the naked shoulder of a dock worker and a bag of toxic material that can be absorbed through the skin. It can also consist of simple improvements such as placing a movable barrier between an ultraviolet source and a worker, or training workers in safe work practices.
Aspects to be considered when selecting appropriate control strategies and technology, include the type of hazardous agent (nature, physical state, health effects, routes of entry into the body), type of source(s), magnitude and conditions of exposure, characteristics of the workplace and relative location of workstations.
The required skills and resources for the correct design, implementation, operation, evaluation and maintenance of control systems must be ensured. Systems such as local exhaust ventilation must be evaluated after installation and routinely checked thereafter. Only regular monitoring and maintenance can ensure continued efficiency, since even well-designed systems may lose their initial performance if neglected.
Control measures should be integrated into hazard prevention and control programmes, with clear objectives and efficient management, involving multidisciplinary teams made up of occupational hygienists and other occupational health and safety staff, production engineers, management and workers. Programmes must also include aspects such as hazard communication, education and training covering safe work practices and emergency procedures.
Health promotion aspects should also be included, since the workplace is an ideal setting for promoting healthy life-styles in general and for alerting as to the dangers of hazardous non-occupational exposures caused, for example, by shooting without adequate protection, or smoking.
The Links among Occupational Hygiene, Risk Assessment and Risk Management
Risk assessment
Risk assessment is a methodology that aims at characterizing the types of health effects expected as a result of a certain exposure to a given agent, as well as providing estimates on the probability of occurrence of these health effects, at different levels of exposure. It is also used to characterize specific risk situations. It involves hazard identification, the establishment of exposure-effect relationships, and exposure assessment, leading to risk characterization.
The first step refers to the identification of an agent—for example, a chemical—as causing a harmful health effect (e.g., cancer or systemic poisoning). The second step establishes how much exposure causes how much of a given effect in how many of the exposed persons. This knowledge is essential for the interpretation of exposure assessment data.
Exposure assessment is part of risk assessment, both when obtaining data to characterize a risk situation and when obtaining data for the establishment of exposure-effect relationships from epidemiological studies. In the latter case, the exposure that led to a certain occupational or environmentally caused effect has to be accurately characterized to ensure the validity of the correlation.
Although risk assessment is fundamental to many decisions which are taken in the practice of occupational hygiene, it has limited effect in protecting workers’ health, unless translated into actual preventive action in the workplace.
Risk assessment is a dynamic process, as new knowledge often discloses harmful effects of substances until then considered relatively harmless; therefore the occupational hygienist must have, at all times, access to up-to-date toxicological information. Another implication is that exposures should always be controlled to the lowest feasible level.
Figure 3 is presented as an illustration of different elements of risk assessment.
Figure 3. Elements of risk assessment.
Risk management in the work environment
It is not always feasible to eliminate all agents that pose occupational health risks because some are inherent to work processes that are indispensable or desirable; however, risks can and must be managed.
Risk assessment provides a basis for risk management. However, while risk assessment is a scientific procedure, risk management is more pragmatic, involving decisions and actions that aim at preventing, or reducing to acceptable levels, the occurrence of agents which may pose hazards to the health of workers, surrounding communities and the environment, also accounting for the socio-economic and public health context.
Risk management takes place at different levels; decisions and actions taken at the national level pave the way for the practice of risk management at the workplace level.
Risk management at the workplace level requires information and knowledge on:
- health hazards and their magnitude, identified and rated according to risk assessment findings
- legal requirements and standards
- technological feasibility, in terms of the available and applicable control technology
- economic aspects, such as the costs to design, implement, operate and maintain control systems, and cost-benefit analysis (control costs versus financial benefits incurred by controlling occupational and environment hazards)
- human resources (available and required)
- socio-economic and public health context
to serve as a basis for decisions which include:
- establishment of a target for control
- selection of adequate control strategies and technologies
- establishment of priorities for action in view of the risk situation, as well as of the existing socio-economic and public health context (particularly important in developing countries)
and which should lead to actions such as:
- identification/search of financial and human resources (if not yet available)
- design of specific control measures, which should be appropriate for the protection of workers’ health and of the environment, as well as safeguarding as much as possible the natural resource base
- implementation of control measures, including provisions for adequate operation, maintenance and emergency procedures
- establishment of a hazard prevention and control programme with adequate management and including routine surveillance.
Traditionally, the profession responsible for most of these decisions and actions in the workplace is occupational hygiene.
One key decision in risk management, that of acceptable risk (what effect can be accepted, in what percentage of the working population, if any at all?), is usually, but not always, taken at the national policy-making level and followed by the adoption of occupational exposure limits and the promulgation of occupational health regulations and standards. This leads to the establishment of targets for control, usually at the workplace level by the occupational hygienist, who should have knowledge of the legal requirements. However, it may happen that decisions on acceptable risk have to be taken by the occupational hygienist at the workplace level—for example, in situations when standards are not available or do not cover all potential exposures.
All these decisions and actions must be integrated into a realistic plan, which requires multidisciplinary and multisectorial coordination and collaboration. Although risk management involves pragmatic approaches, its efficiency should be scientifically evaluated. Unfortunately risk management actions are, in most cases, a compromise between what should be done to avoid any risk and the best which can be done in practice, in view of financial and other limitations.
Risk management concerning the work environment and the general environment should be well coordinated; not only are there overlapping areas, but, in most situations, the success of one is interlinked with the success of the other.
Occupational Hygiene Programmes and Services
Political will and decision making at the national level will, directly or indirectly, influence the establishment of occupational hygiene programmes or services, either at the governmental or private level. It is beyond the scope of this article to provide detailed models for all types of occupational hygiene programmes and services; however, there are general principles that are applicable to many situations and may contribute to their efficient implementation and operation.
A comprehensive occupational hygiene service should have the capability to carry out adequate preliminary surveys, sampling, measurements and analysis for hazard evaluation and for control purposes, and to recommend control measures, if not to design them.
Key elements of a comprehensive occupational hygiene programme or service are human and financial resources, facilities, equipment and information systems, well organized and coordinated through careful planning, under efficient management, and also involving quality assurance and continuous programme evaluation. Successful occupational hygiene programmes require a policy basis and commitment from top management. The procurement of financial resources is beyond the scope of this article.
Human resources
Adequate human resources constitute the main asset of any programme and should be ensured as a priority. All staff should have clear job descriptions and responsibilities. If needed, provisions for training and education should be made. The basic requirements for occupational hygiene programmes include:
- occupational hygienists—in addition to general knowledge on the recognition, evaluation and control of occupational hazards, occupational hygienists may be specialized in specific areas, such as analytical chemistry or industrial ventilation; the ideal situation is to have a team of well-trained professionals in the comprehensive practice of occupational hygiene and in all required areas of expertise
- laboratory personnel, chemists (depending on the extent of analytical work)
- technicians and assistants, for field surveys and for laboratories, as well as for instrument maintenance and repairs
- information specialists and administrative support.
One important aspect is professional competence, which must not only be achieved but also maintained. Continuous education, in or outside the programme or service, should cover, for example, legislation updates, new advances and techniques, and gaps in knowledge. Participation in conferences, symposia and workshops also contribute to the maintenance of competence.
Health and safety for staff
Health and safety should be ensured for all staff in field surveys, laboratories and offices. Occupational hygienists may be exposed to serious hazards and should wear the required personal protective equipment. Depending on the type of work, immunization may be required. If rural work is involved, depending on the region, provisions such as antidote for snake bites should be made. Laboratory safety is a specialized field discussed elsewhere in this Encyclopaedia.
Occupational hazards in offices should not be overlooked—for example, work with visual display units and sources of indoor pollution such as laser printers, photocopying machines and air-conditioning systems. Ergonomic and psychosocial factors should also be considered.
Facilities
These include offices and meeting room(s), laboratories and equipment, information systems and library. Facilities should be well designed, accounting for future needs, as later moves and adaptations are usually more costly and time consuming.
Occupational hygiene laboratories and equipment
Occupational hygiene laboratories should have in principle the capability to carry out qualitative and quantitative assessment of exposure to airborne contaminants (chemicals and dusts), physical agents (noise, heat stress, radiation, illumination) and biological agents. In the case of most biological agents, qualitative assessments are enough to recommend controls, thus eliminating the need for the usually difficult quantitative evaluations.
Although some direct-reading instruments for airborne contaminants may have limitations for exposure assessment purposes, these are extremely useful for the recognition of hazards and identification of their sources, the determination of peaks in concentration, the gathering of data for control measures, and for checking on controls such as ventilation systems. In connection with the latter, instruments to check air velocity and static pressure are also needed.
One of the possible structures would comprise the following units:
- field equipment (sampling, direct-reading)
- analytical laboratory
- particles laboratory
- physical agents (noise, thermal environment, illumination and radiation)
- workshop for maintenance and repairs of instrumentation.
Whenever selecting occupational hygiene equipment, in addition to performance characteristics, practical aspects have to be considered in view of the expected conditions of use—for example, available infrastructure, climate, location. These aspects include portability, required source of energy, calibration and maintenance requirements, and availability of the required expendable supplies.
Equipment should be purchased only if and when:
- there is a real need
- skills for the adequate operation, maintenance and repairs are available
- the complete procedure has been developed, since it is of no use, for example, to purchase sampling pumps without a laboratory to analyse the samples (or an agreement with an outside laboratory).
Calibration of all types of occupational hygiene measuring and sampling as well as analytical equipment should be an integral part of any procedure, and the required equipment should be available.
Maintenance and repairs are essential to prevent equipment from staying idle for long periods of time, and should be ensured by manufacturers, either by direct assistance or by providing training of staff.
If a completely new programme is being developed, only basic equipment should be initially purchased, more items being added as the needs are established and operational capabilities ensured. However, even before equipment and laboratories are available and operational, much can be achieved by inspecting workplaces to qualitatively assess health hazards, and by recommending control measures for recognized hazards. Lack of capability to carry out quantitative exposure assessments should never justify inaction concerning obviously hazardous exposures. This is particularly true for situations where workplace hazards are uncontrolled and heavy exposures are common.
Information
This includes library (books, periodicals and other publications), databases (e.g. on CD-ROM) and communications.
Whenever possible, personal computers and CD-ROM readers should be provided, as well as connections to the INTERNET. There are ever-increasing possibilities for on-line networked public information servers (World Wide Web and GOPHER sites), which provide access to a wealth of information sources relevant to workers’ health, therefore fully justifying investment in computers and communications. Such systems should include e-mail, which opens new horizons for communications and discussions, either individually or as groups, thus facilitating and promoting exchange of information throughout the world.
Planning
Timely and careful planning for the implementation, management and periodic evaluation of a programme is essential to ensure that the objectives and goals are achieved, while making the best use of the available resources.
Initially, the following information should be obtained and analysed:
- nature and magnitude of prevailing hazards, in order to establish priorities
- legal requirements (legislation, standards)
- available resources
- infrastructure and support services.
The planning and organization processes include:
- establishment of the purpose of the programme or service, definition of objectives and the scope of the activities, in view of the expected demand and the available resources
- allocation of resources
- definition of the organizational structure
- profile of the required human resources and plans for their development (if needed)
- clear assignment of responsibilities to units, teams and individuals
- design/adaptation of the facilities
- selection of equipment
- operational requirements
- establishment of mechanisms for communication within and outside the service
- timetable.
Operational costs should not be underestimated, since lack of resources may seriously hinder the continuity of a programme. Requirements which cannot be overlooked include:
- purchase of expendable supplies (including items such as filters, detector tubes, charcoal tubes, reagents), spare parts for equipment, etc.
- maintenance and repairs of equipment
- transportation (vehicles, fuel, maintenance) and travel
- information update.
Resources must be optimized through careful study of all elements which should be considered as integral parts of a comprehensive service. A well-balanced allocation of resources to the different units (field measurements, sampling, analytical laboratories, etc.) and all the components (facilities and equipment, personnel, operational aspects) is essential for a successful programme. Moreover, allocation of resources should allow for flexibility, because occupational hygiene services may have to undergo adaptations in order to respond to the real needs, which should be periodically assessed.
Communication, sharing and collaboration are key words for successful teamwork and enhanced individual capabilities. Effective mechanisms for communication, within and outside the programme, are needed to ensure the required multidisciplinary approach for the protection and promotion of workers’ health. There should be close interaction with other occupational health professionals, particularly occupational physicians and nurses, ergonomists and work psychologists, as well as safety professionals. At the workplace level, this should include workers, production personnel and managers.
The implementation of successful programmes is a gradual process. Therefore, at the planning stage, a realistic timetable should be prepared, according to well-established priorities and in view of the available resources.
Management
Management involves decision-making as to the goals to be achieved and actions required to efficiently achieve these goals, with participation of all concerned, as well as foreseeing and avoiding, or recognizing and solving, the problems which may create obstacles to the completion of the required tasks. It should be kept in mind that scientific knowledge is no assurance of the managerial competence required to run an efficient programme.
The importance of implementing and enforcing correct procedures and quality assurance cannot be overemphasized, since there is much difference between work done and work well done. Moreover, the real objectives, not the intermediate steps, should serve as a yardstick; the efficiency of an occupational hygiene programme should be measured not by the number of surveys carried out, but rather by the number of surveys that led to actual action to protect workers’ health.
Good management should be able to distinguish between what is impressive and what is important; very detailed surveys involving sampling and analysis, yielding very accurate and precise results, may be very impressive, but what is really important are the decisions and actions that will be taken afterwards.
Quality assurance
The concept of quality assurance, involving quality control and proficiency testing, refers primarily to activities which involve measurements. Although these concepts have been more often considered in connection with analytical laboratories, their scope has to be extended to also encompass sampling and measurements.
Whenever sampling and analysis are required, the complete procedure should be considered as one, from the point of view of quality. Since no chain is stronger than the weakest link, it is a waste of resources to use, for the different steps of a same evaluation procedure, instruments and techniques of unequal levels of quality. The accuracy and precision of a very good analytical balance cannot compensate for a pump sampling at a wrong flowrate.
The performance of laboratories has to be checked so that the sources of errors can be identified and corrected. There is need for a systematic approach in order to keep the numerous details involved under control. It is important to establish quality assurance programmes for occupational hygiene laboratories, and this refers both to internal quality control and to external quality assessments (often called “proficiency testing”).
Concerning sampling, or measurements with direct-reading instruments (including for measurement of physical agents), quality involves adequate and correct:
- preliminary studies including the identification of possible hazards and the factors required for the design of the strategy
- design of the sampling (or measurement) strategy
- selection and utilization of methodologies and equipment for sampling or measurements, accounting both for the purpose of the investigation and for quality requirements
- performance of the procedures, including time monitoring
- handling, transport and storage of samples (if the case).
Concerning the analytical laboratory, quality involves adequate and correct:
- design and installation of the facilities
- selection and utilization of validated analytical methods (or, if necessary, validation of analytical methods)
- selection and installation of instrumentation
- adequate supplies (reagents, reference samples, etc.).
For both, it is indispensable to have:
- clear protocols, procedures and written instructions
- routine calibration and maintenance of the equipment
- training and motivation of the staff to adequately perform the required procedures
- adequate management
- internal quality control
- external quality assessment or proficiency testing (if applicable).
Furthermore, it is essential to have a correct treatment of the obtained data and interpretation of results, as well as accurate reporting and record keeping.
Laboratory accreditation, defined by CEN (EN 45001) as “formal recognition that a testing laboratory is competent to carry out specific tests or specific types of tests” is a very important control tool and should be promoted. It should cover both the sampling and the analytical procedures.
Programme evaluation
The concept of quality must be applied to all steps of occupational hygiene practice, from the recognition of hazards to the implementation of hazard prevention and control programmes. With this in mind, occupational hygiene programmes and services must be periodically and critically evaluated, aiming at continuous improvement.
Concluding Remarks
Occupational hygiene is essential for the protection of workers’ health and the environment. Its practice involves many steps, which are interlinked and which have no meaning by themselves but must be integrated into a comprehensive approach.
Commercial Fisheries: Environmental and Public Health Issues
Fisheries Bycatch and Discards
The capture of non-target species—termed bycatch (or in some cases by-kill)—ranks as one of the major environmental impacts of the global marine fisheries industry. Bycatch, the vast majority of which is “discarded” overboard, includes:
- marketable species that are too small or that are prohibited from landings
- species that are not marketable
- commercial species that are not the target of a species-specific fishery
- species that are not fishery related, such as sea birds, sea turtles and marine mammals.
In a major study done for the FAO (Alverson et al. 1994) it was provisionally and conservatively estimated that 27.0 million tonnes of fish and invertebrate life (thus not including marine mammals, seabirds or turtles) are caught and then discarded—much of it dead or dying—by commercial fishery operations each year. This is equivalent to more than one-third the weight of all reported marine landings in commercial fisheries worldwide, estimated at some 77 million tonnes.
In addition to the ethical issues associated with wastage, there is great public concern about the environmental impacts of discard mortalities, such as potential biodiversity loss and reduced fish stocks. Perhaps as many as 200,000 marine mammals are killed annually in fishing gear (Alverson et al. 1994). Gill net fishing is likely the most serious threat to many porpoise populations; at least one species (the yaquita in the Gulf of California) and several populations of harbour porpoise are nearing extinction due to this fishery type. The inadvertent capture and mortality of sea turtles, notably those associated with shrimp trawls and some long-line fisheries, is an important factor in the continued endangerment of various populations throughout the world’s oceans (Dayton et al. 1995). High numbers of seabirds are also killed in some fisheries; long-line operations kill many tens of thousands of albatross annually and are considered the major threat to the survival of many albatross species and populations (Gales 1993).
The issue of bycatch has been a major factor in the now negative public perception of the commercial marine fisheries. As a consequence, there has been much research in recent years to improve the selectivity of fishing gear and fishing methods. Indeed, the FAO (1995) estimates that a 60% reduction in discards could be achieved by the year 2000 if a major concerted effort is undertaken by governments and industry.
Fish/Seafood Waste and Bycatch Disposal
Fish and seafood wastes can include the internal organs (viscera), heads, tails, blood, scales and wastewater or sludge (e.g., cooker juices, chemical coagulants used in primary treatment systems, oil, grease, suspended solids and so on). In many regions, most seafood-processing material from land-based industry is converted to fishmeal or fertilizer, with any remaining waste either dumped at sea, discharged into coastal waters, applied directly on land or landfilled. Waste from ship-based processing (i.e., fish cleaning) is comprised of fish parts (offal) and is invariably dumped at sea.
The impact of processed fish material on aquatic systems can vary widely according to the type of waste, the rate and amount of discharge, the ecological sensitivity of the receiving environment and physical factors influencing waste mixing and dispersion. The greatest concern involves the discharge of waste by processing companies into coastal environments; here the influx of excessive nutrients can lead to eutrophication and, subsequently, loss of local aquatic plant and animal populations.
The discharge of offal and bycatch from fishing boats can result in oxygen depletion of benthic (i.e., bottom) habitats if sufficient quantities accumulate on the seabed. However, discards and offal are considered factors contributing to the rapid growth of some seabird populations, though this may be to the detriment of less competitive species (Alverson et al. 1994).
Commercial Whaling
Commercial whaling continues to provoke intense public and political focus due (1) to the perceived uniqueness of whales, (2) to concerns about the humaneness of hunting techniques and (3) to the fact that most populations of whales—such as of blues, fins and rights—have been dramatically reduced. The current focus of hunts is the minke whale, which had been spared by the historical whaling fleets because of its small size (7 to 10 m) relative to the much larger “great” whales.
In 1982, the International Whaling Commission (IWC) voted for a global moratorium on commercial whaling. This moratorium came into effect with the 1985/86 whaling season and is scheduled to last for an indefinite period. However, two countries—Norway and Russia—maintain official objections to the moratorium, and Norway uses that objection to continue commercial whaling in the Northeast Atlantic. Although Japan does not maintain an objection to the moratorium, it continues whaling in the North Pacific and the Southern Oceans, taking advantage of an article in the International Convention for the Regulation of Whaling which allows member States to kill whales for purposes of scientific research. Less than 1,000 whales are killed annually by the Japanese and Norwegian fleets; virtually all of the whale meat ends up in the Japanese market for human consumption (Stroud 1996).
Seafood Safety: Pathogens, Chemical Pollutants and Natural Toxins
Human illness can occur from ingestion of contaminated seafood through three main routes:
- Raw, undercooked or poorly processed fish and shellfish that are contaminated by pathogens that can cause such diseases as hepatitis A, cholera or typhoid. Untreated or inadequately treated domestic sewage is the primary source of microbial pathogens, such as viruses and bacteria, in seafood; some disease-causing organisms can persist for months in or on fish or within the digestive tracts or gills of fish and shellfish. The health risks posed by these pathogens can be virtually eliminated with proper sewage treatment and disposal, monitoring programmes, proper food processing and preparation techniques and, most importantly, through thorough cooking of seafood products (Food and Nutrition Board 1991).
- Consumption of seafood that has been contaminated by industrial chemicals such as mercury, lead and pesticides. The global nature and pervasiveness of environmental pollution means that a wide variety of industrial chemicals—such as pesticides and heavy metals (e.g., lead and mercury)—are typically found in seafood. However, the extent of contamination varies widely from region to region and between species. Of particular concern are those chemicals that can bioaccumulate in humans, such as PCBs, dioxins and mercury. In these cases, contaminant burdens (from a wide variety of sources, including seafood) increase over time to levels where toxic effects may be exerted. Though much remains to be understood concerning the effects on human health of chronic contaminant exposure, an impressive body of information suggests a clear potential for increased cancer risks, immunosuppression, reproductive impacts and subtle impairment of neurological development in foetuses and children. In a major report on seafood safety, the Institute of Medicine of the US Academy of Sciences (Food and Nutrition Board 1991) recommended—as have numerous environmental and human health organizations—that an active environmental stance aimed at pollution prevention would ultimately be the best means to avoid continuing human health problems and pollution disasters as a result of industrial chemicals.
- Consumption of seafood contaminated by natural algae-related toxins, such as domoic acid, ciguatoxin and saxitoxin. A wide range of toxins are produced by various algae species, and these can accumulate in a range of seafood products, notably shellfish (the exception being ciguatoxin, which is found only in reef fish). Resulting illnesses include “shellfish poisoning”—either paralytic (PSP), amnesic (ASP), diarrhetic (DSP) or neurotoxic (NSP)—and ciguatera. Mortalities continue to result from PSP and ciguatera; no fatalities have been reported from ASP since its discovery in 1987, when three people died. There has been what appears to be an increase in toxic algal blooms since the 1970s, as well as changes in the distribution and intensity of fish and shellfish toxicity. Though algal blooms are natural events, it is strongly suspected that coastal nutrient pollution—mainly from fertilizers and sewage—is enhancing bloom formation or duration and thereby increasing the likelihood of seafood toxicity episodes (Anderson 1994). It is important to note that, unlike for pathogens, thorough cooking does not reduce the toxicity of seafood contaminated by these natural poisons.
Musculoskeletal Disorders Among Fishermen and Workers in the Fish Processing Industry
The term musculoskeletal disorders is used collectively for symptoms and diseases of the muscles, tendons and/or joints. Such disorders are often unspecified and can vary in duration. The main risk factors for work-related musculoskeletal disorders are heavy lifting, awkward work postures, repetitive work tasks, psychological stress and improper job organization (see figure 1).
Figure 1. Manual handling of fish in a fish-packing plant in Thailand
In 1985, the World Health Organization (WHO) issued the following statement: “Work-related diseases are defined as multifactorial, where the work environment and the performance of work contribute significantly; but as one of a number of factors to the causation of disease” (WHO 1985). There are, however, no internationally accepted criteria for the causes of work-related musculoskeletal disorders. Work-related musculoskeletal disorders appear in both developing and developed countries. They have not disappeared despite the development of new technologies permitting machines and computers to take over what was previously manual work (Kolare 1993).
Work aboard vessels is physically and mentally demanding. Most of the well-known risk factors for musculoskeletal disorders mentioned above are often present in the fishermen’s work situation and organization.
Traditionally most fishery workers have been males. Swedish studies on fishermen have shown that symptoms from the musculoskeletal system are common, and that they follow a logical pattern according to the fishing and type of working tasks on board. Seventy-four per cent of the fishermen had experienced symptoms of the musculoskeletal system during the previous 12 months. The largest number of fishermen considered the motion of the vessel to be a major strain, not only on the musculoskeletal system, but on the individual as a whole (Törner et al. 1988).
There are not many published studies on musculoskeletal disorders among workers in fish processing. There is a long tradition of female domination in the job of cutting and trimming the fillets in the fish-processing industry. Results from Icelandic, Swedish and Taiwanese studies show that female workers in the fish-processing industry had a higher prevalence of symptoms of musculoskeletal disorders of the neck or shoulders than women who had more varied jobs (Ólafsdóttir and Rafnsson1997; Ohlsson et al. 1994; Chiang et al. 1993). These symptoms were thought to be causally related to the highly repetitive tasks with a short cycle time of less than 30 seconds. Work with highly repetitive tasks without the possibility of rotation between different jobs is a high risk factor. Chiang and co-workers (1993) studied workers in the fish-processing industry (men and women) and found a higher prevalence of symptoms of the upper limbs among those with jobs involving high repetitiveness or forceful movements, as compared to those in the same factories who had jobs with low repetitiveness and low-force movements.
As mentioned above, musculoskeletal disorders have not disappeared despite the development of new technologies. The flow line is an example of one new technique which has been introduced in the fish-processing industry ashore and on board larger processing vessels. The flow line consists of a system of conveyor belts which transport the fish through decapitating and filleting machines to the workers who seize each fillet and cut and trim it with a knife. Other conveyor belts transport the fish to the packing station, after which the fish is quick-frozen. The flow line has changed the prevalence of musculoskeletal symptoms among women working in fish-filleting plants. After the introduction of the flow line, the prevalence of symptoms of the upper limbs increased while the prevalence of symptoms of the lower limbs decreased (Ólafsdóttir and Rafnsson 1997).
In order to develop a strategy for their prevention it is important to understand the causes, mechanisms, prognosis and prevention of musculoskeletal disorders (Kolare et al. 1993). The disorders cannot be prevented by new technologies exclusively. The whole working environment, including the work organization, has to be taken into consideration.
Health Problems and Disease Patterns
Work in the fishing and fish-processing industry shows a clear differentiation according to gender, with the men traditionally doing the actual fishing while the women work at fish processing on shore. Many of the persons working on fishing vessels may be looked upon as unskilled; the deckhands, for instance, receive their training in the work on board. The navigators (captain, skipper and mate), the machine room personnel (engineer, machinist and stoker), the radio operators and the cooks all have different educational backgrounds. The main assignment is to fish; other tasks include loading of the vessel, which is done on the open sea, followed by the fish processing, which takes place to various stages of completion. The only common exposure of these groups occurs during their stay on board the vessel, which is in constant motion both while they are working and resting. Fish processing on shore will be dealt with later.
Accidents
The most dangerous work tasks for the individual fishers are related to the setting out and hauling in of the fishing gear. In trawler fishing, for example, the trawl is laid out in a sequence of tasks involving the complicated coordination of different types of winches (see “Major sectors and processes” in this chapter). All operations take place at great speed, and teamwork is absolutely essential. While setting the trawl, the connecting of the trawl doors to the warp (wire ropes) is one of the most dangerous moments, as these doors weigh several hundred kilograms. Other parts of the fishing gear are also too heavy to be handled without the use of derricks and winches while shooting the trawl (i.e., heavy gear and bobbings move freely around before being hoisted overboard).
The whole procedure of setting and hauling aboard the trawl, purse seine and nets is carried out using wire cables which pass across the working area often. The cables are at high tension, as there is often an extremely heavy pull from the fishing gear in a direction opposite of the forward motion of the fishing vessel itself. There is a great risk of getting entangled by or falling onto the fishing gear and thus being drawn overboard, or of falling overboard when laying out the fishing gear. There is a risk of crushing and trapping injuries to fingers, hands and arms, and the heavy gear may fall or roll and thus injure legs and feet.
Bleeding and gutting the fish are often done manually and take place on the deck or on a shelterdeck. The pitching and rolling of the vessels make injuries to the hands and fingers common from knife cuts or from pricks of fish bones and spines. Infections in wounds are frequent. Long-line and hand-line fishing involve the risk of wounds to fingers and hands from the hooks. As this type of fishing is becoming more and more automated it is becoming associated with dangers from line haulers and winches.
The method of managing fishing by limiting the amount caught from a restricted natural resource area also influences the injury rate. In some places pursuit quotas allocate to the vessels certain days when they are allowed to fish, and the fishers feel they have to go fishing at these times whatever the weather.
Fatal accidents
Fatal accidents at sea are easily studied through mortality registers, as accidents at sea are coded on the death certificates as water transport accidents according to the International Classification of Diseases, with an indication as to whether the injury was sustained while employed on board. Death rates from work-related fatal accidents among workers in the fishing industry are high, and higher than for many other occupational groups on shore. Table 1 shows the mortality rate per 100,000 for fatal accidents in different countries. The fatal injuries are traditionally classified as (1) individual accidents (i.e., individuals falling overboard, being swept overboard by heavy seas or being fatally injured by machinery) or (2) individuals lost as a result of vessel casualties (e.g., because of foundering, capsizing, missing vessels, explosions and fires). Both categories are related to the weather conditions. Accidents to individual crew members outnumber the others.
Table 1. Mortality figures on fatal injuries among fishermen as reported in studies from various countries
|
Country |
Study period |
Rates per 100,000 |
|
United Kingdom |
1958–67 |
140–230 |
|
United Kingdom |
1969 |
180 |
|
United Kingdom |
1971–80 |
93 |
|
Canada |
1975–83 |
45.8 |
|
New Zealand |
1975–84 |
260 |
|
Australia |
1982–84 |
143 |
|
Alaska |
1980–88 |
414.6 |
|
Alaska |
1991–92 |
200 |
|
California |
1983 |
84.4 |
|
Denmark |
1982–85 |
156 |
|
Iceland |
1966–86 |
89.4 |
The safety of a vessel depends on its design, size and type, and on factors such as stability, freeboard, weather-tight integrity and structural protection against fire. Negligent navigation or errors of judgement may result in casualties to vessels, and the fatigue which follows long spells of duty may also play a role, as well as being an important cause of personal accidents.
Better safety records of more modern vessels may be due to the combined effects of improved human and technical efficiency. Training of personnel, proper use of flotation support apparatus, suitable clothing and the use of buoyant overalls may all increase the probability of rescue of persons in the event of an accident. More widespread use of other safety measures, including safety lines, helmets and safety shoes, may be needed in the fishing industry in general, as discussed elsewhere in this Encyclopaedia.
Non-fatal injuries
Non-fatal injuries are also quite common in the fishing industry (see table 2). The body regions of injured workers most frequently mentioned are the hands, lower limbs, head and neck and upper limbs, followed by the chest, spine and abdomen, in decreasing order of frequency. The most common types of traumas are open wounds, fractures, strains, sprains and contusions. Many non-fatal injuries may be serious, involving, for instance, amputation of fingers, hands, arms and legs as well as injuries to the head and neck. Infections, lacerations and minor traumas of the hands and fingers are quite frequent, and treatment with antibiotics is often recommended by the ship’s doctors in all cases.
Table 2. The most important jobs or places related to risk of injuries
|
Job or tasks |
On board vessels injury |
On shore injury |
|
Setting and hauling trawl, purse seine and other fishing gear |
Entangled in the fishing gear or wire cables, crushing injuries, fall overboard |
|
|
Connecting trawl doors |
Crushing injuries, fall overboard |
|
|
Bleeding and gutting |
Cuts from knives or machines, |
Cuts from knives or machines, |
|
Long-line and hand-line |
Wounds from hooks, entangled in the line |
|
|
Heavy lifts |
Musculoskeletal disorders |
Musculoskeletal disorders |
|
Filleting |
Cuts, amputations using knives or machines, musculoskeletal disorders |
Cuts, amputations using knives or machines, musculoskeletal disorders |
|
Trimming fillets |
Cuts from knives, musculoskeletal disorders |
Cuts from knives, musculoskeletal disorders |
|
Work in confined spaces, loading and landing |
Intoxication, asphyxia |
Intoxication, asphyxia |
Morbidity
Information on the general health of fishers and overviews of their illnesses are mainly obtained from two types of reports. One source is the case series compiled by ships’ doctors, and the other is the medical advice reports, which report on evacuations, hospitalizations and repatriations. Unfortunately, most if not all of these reports give only the numbers of patients and percentages.
The most frequently reported non-traumatic conditions leading to consultations and hospitalization arise as a result of dental conditions, gastro-intestinal illness, musculoskeletal conditions, psychiatric/neurological conditions, respiratory conditions, cardiological conditions and dermatological complaints. In one series reported by a ship’s doctor, psychiatric conditions were the most common reason for evacuating workers from trawlers on long-term fishing voyages, with injuries only coming in second place as a reason for rescuing fishers. In another series the most common illnesses which necessitated repatriation were cardiological and psychiatric conditions.
Occupational asthma
Occupational asthma is frequently found among workers in the fish industry. It is associated with several types of fish, but most commonly it is related to exposure to crustaceans and molluscs—for example, shrimp, crabs, shellfish and so on. The processing of fishmeal is also often related to asthma, as are similar processes, such as grinding shells (shrimp shells in particular).
Hearing loss
Excessive noise as a cause of decreased hearing acuity is well recognized among workers in the fish-processing industry. The machine room personnel on the vessels are at extreme risk, but so are those working with the older equipment in fish processing. Organized hearing conservation programmes are widely needed.
Suicide
In some studies on fishers and sailors from the merchant fleet, high death rates because of suicide have been reported. There is also an excess of deaths in the category where the doctors were not able to decide whether the injury was accidental or self- inflicted. There is a widespread belief that suicides in general are underreported, and this is rumoured to be even greater in the fishing industry. Psychiatric literature gives descriptions of calenture, a behavioural phenomenon where the predominant symptom is an irresistible impulse for sailors to jump into the sea from their vessels. The underlying causes for the risk for suicide have not been studied among fishermen particularly; however, consideration of the psychosocial situation of the workforce at sea, as discussed in another article in this chapter, seems a not unlikely place to start. There are indications that the suicide risk increases when the workers stop fishing and go ashore both for a short while or definitely.
Fatal poisoning and asphyxia
Fatal poisoning occurs in incidents of fire on board fishing vessels, and is related to inhalation of toxic smoke. There are also reports of fatal and non-fatal intoxication resulting from the leak of refrigerants or the use of chemicals for preserving shrimp or fish, and from toxic gases from the anaerobic decay of organic material in unventilated holds. The refrigerants concerned range from the highly toxic methyl chloride to ammonia. Some deaths have been attributed to exposure to sulphur dioxide in confined spaces, which is reminiscent of the incidents of silo-filler’s disease, where there is exposure to nitrogen oxides. Research has similarly shown that there are mixtures of toxic gases (i.e., carbon dioxide, ammonia, hydrogen sulphide and carbon monoxide), along with low partial pressure of oxygen in holds on board ship and on shore, which have resulted in casualties, both fatal and non-fatal, often related to industrial fish such as herring and capelin. In commercial fishing, there are some reports of intoxication when landing fish that have been related to trimethylamine and endotoxins causing symptoms resembling influenza, which may, however, lead to death. Attempts could be made to reduce these risks through improved education and alterations to equipment.
Skin diseases
Skin diseases affecting hands are common. These may be related to contact with fish proteins or to the use of rubber gloves. If gloves are not used, the hands are constantly wet and some workers may become sensitized. Thus most of the skin diseases are contact eczema, either allergic or non-allergic, and the conditions are often constantly present. Boils and abscesses are recurrent problems also affecting hands and fingers.
Mortality
Some studies, although not all, show low mortality from all causes among fishermen as compared to the general male population. This phenomenon of low mortality in a group of workers is called the “healthy worker effect”, referring to the consistent tendency for actively employed people to have more favourable mortality experience than the population at large. However, due to high mortality from accidents at sea, the results from many mortality studies on fishermen show high death rates for all causes.
The mortality from ischemic heart diseases is either elevated or decreased in studies on fishermen. Mortality from cerebrovascular diseases and respiratory diseases is average among fishermen.
Unknown causes
Mortality from unknown causes is higher among fishermen than other men in several studies. Unknown causes are special numbers in the International Classification of Diseases used when the doctor who issues the death certificate is not able to state any specific disease or injury as the cause of death. Sometimes deaths registered under the category of unknown causes are due to accidents in which the body was never found, and are most likely water transport accidents or suicides when the death occurs at sea. In any case an excess of deaths from unknown causes can be an indication, not only of a dangerous job, but also of a dangerous lifestyle.
Accidents occurring other than at sea
An excess of fatal traffic accidents, various poisonings and other accidents, suicide and homicide have been found among fishermen (Rafnsson and Gunnarsdóttir 1993). In this connection the hypothesis has been suggested that seamen are influenced by their dangerous occupation towards hazardous behaviour or a hazardous lifestyle. The fishermen themselves have suggested that they become unaccustomed to traffic, which could provide an explanation for the traffic accidents. Other suggestions have focused on the attempts of fishermen, returning from long voyages during which they have been away from family and friends, to catch up on their social life. Sometimes fishermen spend only a short time ashore (a day or two) between long voyages. The excess of deaths from accidents other than those at sea points to an unusual lifestyle.
Cancer
The International Agency for Research on Cancer (IARC), which among other things has a role in evaluating industries in respect to the potential cancer risks for their workers, has not included fishing or the fish-processing industry among those industrial branches showing clear signs of cancer risk. Several mortality and cancer morbidity studies discuss the cancer risk among fishermen (Hagmar et al. 1992; Rafnsson and Gunnarsdóttir 1994, 1995). Some of them have found an increased risk for different cancers among fishermen, and suggestions are often given as to possible causes for the cancer risks which involve both occupational and lifestyle factors. The cancers which will be discussed here are cancer of the lip, lung and stomach.
Cancer of the lip
Fishing has traditionally been related to lip cancer. Previously this was thought to be related to exposure to tars used to preserve the nets, since the workers had used their mouths as “third hands” when handling the nets. Currently the aetiology of lip cancer among fishermen is considered to be the joint effect of exposure to ultraviolet radiation during outdoor work and smoking.
Cancer of the lung
The studies on lung cancer are not in accord. Some studies have not found increased risk of lung cancer among fishermen. Studies of fishermen from Sweden showed less lung cancer than the reference population (Hagmar et al. 1992). In an Italian study the lung cancer risk was thought to be related to smoking and not to the occupation. Other studies on fishermen have found increased risk of lung cancer, and still others have not confirmed this. Without information on smoking habits it has been difficult to evaluate the role of smoking versus the occupational factors in the possible cases. There are indications of the need to study separately the different occupational groups on the fishing vessels, as engine room personnel have elevated risk for lung cancer, thought to be due to exposure to asbestos or polycyclic aromatic hydrocarbons. Further studies are thus needed to clarify the relation of lung cancer and fishing.
Cancer of the stomach
Many studies have found elevated risk of stomach cancer in fishermen. In the Swedish studies the risk of stomach cancer was thought to be related to high consumption of fatty fish contaminated with organochlorine compounds (Svenson et al. 1995). At present it is uncertain what role dietary, lifestyle and occupational factors play in the association of stomach cancer with fishing.
Social Effects of One-Industry Fishery Villages
With the development of industrialized fish processing in the 19th and 20th centuries, wives and families were displaced from household-based processing and vending, and ended up unemployed or working for fish companies. The introduction of corporate-owned trawlers and, more recently, corporate-owned fish quotas (in the form of enterprise allocations and individual transferable quotas) has displaced male fishers. Changes of this kind have transformed many fishery communities into one-industry villages.
There are different kinds of one-industry fishery villages, but all are characterized by high dependence on a single employer for employment, and significant corporate influence within the community and sometimes the home lives of workers. In the most extreme case, one-industry fishery villages are actually company towns, in which a single corporation owns not only the plant and some of the vessels, but also local housing, stores, medical services and so on, and exercises significant control over local government representatives, the media and other social institutions.
Somewhat more common are villages in which local employment is dominated by a single, often vertically integrated corporate employer that uses its control over employment and markets to indirectly influence local politics and other social institutions associated with the family and community lives of workers. The definition of one-industry fishery villages can also be extended to include fish-processing firms that, despite their location within larger communities that are not fishery dependent, operate with significant autonomy from those communities. This structure is common in the shrimp-processing industry of India, which makes extensive use of young female migrant labourers, often recruited by contractors from nearby states. These workers generally live in compounds on company property. They are cut off from the local community by long working hours, a lack of kinship connections and by linguistic barriers. Such workplaces are like company towns in that companies exert significant influence over the non-working lives of their workers, and workers cannot easily turn to local authorities and other members of the community for support.
Economic uncertainty, unemployment, marginalization within decision-making processes, low income and limited access to and control over services are important determinants of health. These are all, to varying degrees, features of one-industry fishery villages. Fluctuations in fisheries markets and both natural and fishery-related fluctuations in the availability of fishery resources are a fundamental feature of fishery communities. Such fluctuations generate social and economic uncertainty. Fishery communities and households have often developed institutions that help them survive these periods of uncertainty. However, these fluctuations appear to be occurring more frequently in recent years. In the current context of global overfishing of commercial fish stocks, shifting effort to new species and regions, the globalization of markets and the development of aquacultured products which compete with wild fishery products in the marketplace, increased employment uncertainty, plant closures and low incomes are becoming common. In addition, when closures occur, they are more likely to be permanent because the resource is gone and work has moved elsewhere.
Employment uncertainty and unemployment are important sources of psychosocial stress that may affect men and women differently. The displaced worker/fisher must grapple with loss of self-esteem, loss of income, stress and, in extreme cases, loss of family wealth. Other family members must cope with the effects of workers’ displacement on their home and working lives. For example, household strategies for coping with prolonged male absence can become a problem when trawler workers find themselves unemployed and their wives find the autonomy and routines that helped them survive male absence threatened by the prolonged presence of displaced husbands. In small-scale fishing households, wives may have to adjust to longer absences and social isolation as their family members go further afield to find fish and employment. Where wives were also dependent on the fishery for wage employment, they may also have to struggle with the effects of their own unemployment on their health.
The stress of unemployment can be greater in one-industry communities where plant closures threaten the future of entire communities and the economic costs of job loss are enhanced by a collapse in the value of such personal assets as homes and cottages. Where, as is often the case, finding alternative employment requires moving away, there will be additional stresses on workers, their spouses and their children associated with displacement. When plant closures are accompanied by the transfer of fish quotas to other communities and the erosion of local educational, medical and other services in response to out migration and the collapse of local economies, the threats to health will be greater.
Dependence on a single employer can make it difficult for workers to participate in decision-making processes. In fisheries, as in other industries, some corporations have used the one-industry structure to control workers, oppose unionization and manipulate public understandings of issues and developments within the workplace and beyond. In the case of the Indian shrimp processing industry, migrant female processing workers suffer from terrible living conditions, extremely long hours, compulsory overtime and routine violation of their work contracts. In western countries, corporations may use their role as gate-keepers controlling seasonal workers’ eligibility for such programmes as unemployment insurance in negotiations with workers concerning unionization and working conditions. Workers in some one-industry towns are unionized, but their role in decision-making processes can still be mitigated by limited employment alternatives, by a desire to find local employment for their wives and children and by ecological and economic uncertainty. Workers can experience a sense of helplessness and may feel obliged to keep working despite illness when their ability to access work, housing and social programmes is controlled by a single employer.
Limited access to adequate medical services is also a psychosocial stressor. In company towns, medical professionals may be company employees and, as in mining and other industries, this can limit workers’ access to independent medical advice. In all types of one-industry villages, cultural, class and other differences between medical personnel and fishworkers, and high rates of turnover among medical professionals, can limit the quality of local medical services. Medical personnel rarely come from fishery communities and hence are often unfamiliar with the occupational health risks fishworkers encounter and the stresses associated with life in one-industry towns. Turnover rates among such personnel may be high due to relatively low professional incomes and discomfort with rural lifestyles and unfamiliar fishery cultures. In addition, medical personnel may tend to associate more with local elites, such as the plant management, than with workers and their families. These patterns can interfere with doctor-patient relations, continuity of care and medical expertise relevant to fisheries work. Access to appropriate diagnostic services for such fishery-related illnesses as repetitive strain injuries and occupational asthma may be very limited in these communities. Loss of work can also interfere with access to medical services by eliminating access to drug programmes and other insured medical services.
Strong social supports can help mitigate the health effects of unemployment, displacement and economic uncertainty. One-industry villages can encourage the development of dense social and kinship-based ties between workers and, particularly if plants are locally owned, between workers and employers. These social supports can mitigate the effects of economic vulnerability, difficult working conditions and ecological uncertainty. Family members can watch out for each other in the workplace and sometimes help out when workers get into financial trouble. Where fishery workers are able to maintain some economic independence through subsistence activities, they can retain more control over their lives and work than where access to these is lost. Increasing employment uncertainty, plant closures and local competition for jobs and government-adjustment programmes can erode the strength of these local networks, contributing to conflict and isolation within these communities.
When plant closures mean moving away, displaced workers risk loss of access to these social networks of support and subsistence-related sources of independence.
Psychosocial Characteristics of the Workforce in On-Shore Fish Processing
On-shore fish processing includes a variety of activities. The range is from small, low-technology fish processing, like drying or smoking of local catch for the local market, to the large, high-technology modern factory, producing highly specialized products that are consumer packed for an international market. In this article the discussion is limited to industrial fish processing. The level of technology is an important factor for the psychosocial environment in industrialized fish-processing plants. This influences the organization of work tasks, the wage systems, the control and monitoring mechanisms and the opportunities for the employees to have influence on their work and the corporate policy. Another important aspect when discussing psychosocial characteristics of the workforce in the on-shore fish-processing industry is the division of labour by sex, which is widespread in the industry. This means that men and women are assigned to different work tasks according to their sex and not to their skills.
In fish-processing plants, some departments are characterized by high technology and high degree of specialization, while others might use less advanced technology and be more flexible in their organization. The departments characterized by a high degree of specialization are, as a rule, those with a predominantly female workforce, while the departments where the work tasks are less specialized are those with a predominantly male workforce. This is based on an idea that certain work tasks are either fit for males only or females only. Tasks seen as fit only for males will have higher status than the tasks done by female workers only. Consequently, men will be unwilling to do “women’s work”, while most women are eager to do “men’s work” if allowed to. Higher status will also as a rule mean higher salary and better opportunities for advancement (Husmo and Munk-Madsen 1994; Skaptadóttir 1995).
A typical high-technology department is the production department, where the workers are lined up around the conveyor belt, cutting or packing fish fillets. The psychosocial environment is characterized by monotonous and repetitive tasks and a low degree of social interaction among the workers. The wage system is based on individual performance (bonus system), and individual workers are monitored by computer systems in addition to the supervisor. This causes high stress levels, and this type of work also increases the risk of developing strain-related syndromes among the workers. The workers’ restriction to the conveyor belt also reduces the possibilities for informal communication with the management in order to influence corporate policy and/or promote one’s self for a raise or a promotion (Husmo and Munk-Madsen 1994). Since the workers of highly specialized departments learn only a limited number of tasks, these are the most likely to be sent home when the production is reduced due to temporary lack of raw material or due to market problems. These are also the ones that are most likely to be replaced by machines or industrial robots as new technology is introduced (Husmo and Søvik 1995).
An example of a department of lower technology levels is the raw material department, where workers drive trucks and fork-lifts at the pier, unload, sort and wash the fish. Here we often find high flexibility in the work tasks, and the workers do different jobs throughout the day. The wage system is based on an hourly rate, and individual performance is not measured by computers, reducing stress and contributing to a more relaxed atmosphere. Variation in work tasks stimulates teamwork and improves the psycho- social environment in many ways. The social interactions increase, and the risk of strain-related syndromes is reduced. Possibilities for promotion increase, since learning a wider range of work tasks makes the workers more qualified for higher positions. Flexibility allows informal communication with the management/supervisor in order to influence corporate policy and individual promotion (Husmo 1993; Husmo and Munk-Madsen 1994).
The general trend is that the level of processing technology increases, leading to more specialization and automation in the fish-processing industry. This has consequences for the psychosocial environment of the workers as outlined above. The division of labour by sex means that the psychosocial environment for most women is worse than it is for men. The fact that women have the work tasks that are the most likely to be replaced by robots adds an additional dimension to this discussion, as it limits the work opportunities for women in general. In some cases these implications might apply not only to female workers, but also to lower social classes in the workforce or even to different races (Husmo 1995).
Psychosocial Characteristics of the Workforce at Sea
Two dimensions are of special importance in the psychosocial characteristic of fishwork at sea. One dimension is the issue of scale and technology. Fisheries may be divided into: small-scale, artisanal, coastal or in-shore fisheries; and large-scale, industrial, deep sea, distant water or off-shore fishing. The psychosocial working and living conditions of crew members in small-scale fishing differ tremendously from the conditions faced by crews on large-scale vessels.
The second dimension is gender. Fishing vessels are generally all-male environments. Although exceptions occur in both small-scale and large-scale fishing, one-gender crews are most common worldwide. However, gender plays a role in the character of all crews. The sea/land split which fishers face and have to cope with is to a large extent a gendered division.
Small Fishing Vessels
On board small fishing vessels the crew members are usually related in several ways. A crew may consist of father and son, of brothers or of a mixture of close or more distant kin. Other community members may be in the crew. Depending on availability of male relatives or local customs, women are crewing. Wives may be operating a vessel together with their husbands, or a daughter may be crewing for her father.
A crew is more than a company of workmates. As kinship ties, neighbourhood ties and local community life most often bind them together, the vessel and workforce at sea is socially integrated with family and community life on shore. The ties have a two-way effect. Cooperation in fishing and belonging to a vessel confirms and tightens other social relations as well. When relatives are fishing together, a crew member cannot be replaced by a stranger, even if someone more experienced comes looking for a berth. Fishers have security in their job in such a tight network. On the other hand this also puts restrictions on switching to another vessel out of loyalty to one’s family.
The many-sided social relations mitigate conflicts on board. Small-scale fishers share a narrow physical space and are subjected to unpredictable and sometimes dangerous conditions of nature. Under these demanding circumstances it may be necessary to avoid open conflicts. The authority of the skipper is also constrained by the knitted network of relations.
Generally small-scale vessels will come on shore every day, which gives crew members the opportunity to interact with others on a regular basis, although their working hours may be long. Isolation is rare but may be felt by fishers who operate a vessel alone. Nevertheless radio communication at sea and traditions of comrade vessels operating in the vicinity of each other diminish the isolative effects of working alone in modern small-scale fishing.
Learning processes and safety on board are marked by the ties of kinship and locality. The crew are responsible for and dependent on each other. To work skilfully and responsibly may be of utmost importance in unforeseen situations of bad weather or accidents. The spectrum of skills required in small-scale fishing is very wide. The smaller the crew, the lower the level of specialization—workers must have comprehensive knowledge and be able to do a variety of tasks.
Unawareness or unwillingness in work is severely sanctioned by stigmatization. Every crew member has to do necessary tasks willingly, preferably without being told. Orders are supposed to be unnecessary except for the timing of a series of tasks. Cooperation in mutual respect is thus an important skill. The display of serious interest and responsibility is helped by the socialization in a fishing family or village. The diversity of work furthers the respect for experience in any position on board, and egalitarian values are usual.
Successful coping with the demanding cooperation, timing and skills needed in small-scale fishing under changing conditions of weather and seasons creates a high level of job satisfaction and a locally rewarded and strong work identity. Women who go fishing appreciate the status rise connected to their successful participation in men’s work. However, they also have to cope with the risk of losing ascriptions of femininity. Men who fish with women, on the other hand, are challenged by the risk of losing ascriptions of masculine superiority when women show their ability in fishing.
Large Fishing Vessels
In large-scale fishing, crew members are isolated from family and community while at sea, and many have only short periods on shore between trips. The duration of a fishing trip generally varies between 10 days and 3 months. Social interaction is limited to the mates on board the vessel. This isolation is demanding. Integration into family and community life when on shore may also be difficult and awaken a sense of homelessness. Fishermen highly depend on wives to keep alive their social network.
In an all-male crew the absence of women and lack of intimacy may contribute to rough sexualized conversations, sexualized bragging and a focus on porno movies. Such a ship culture may develop as an unhealthy way of exposing and confirming masculinity. Partly to prevent the development of a harsh, sexist and deprived atmosphere, Norwegian companies have since the 1980s employed up to 20% women in the crew on factory ships. A gender-mixed work environment is said to reduce the psychological stress; women are reported to bring a softer tone and more intimacy into the social relations on board (Munk-Madsen 1990).
The mechanization and specialization of work on board industrialized vessels creates a repetitive working routine. Shift work in two watches is usual as fishing goes on round the clock. Life on board consists of a cycle of working, eating and sleeping. In cases of huge catches, sleeping hours may be cut down. The physical space is restricted, the work monotonous and tiring and social interaction with others than the workmates impossible. As long as the vessel is at sea there is no escape from tensions among crew members. This poses a psychological stress on the crew.
The crews of deep-sea vessels with 20 to 80 workers on board cannot be recruited in a tight network of kinship and neighbourhood ties. Yet some Japanese companies have changed recruitment policies and prefer to staff their vessels with personnel who know each other through community or kin relations and who come from communities with traditions of fishing. This is done to solve problems of violent conflicts and excess drinking (Dyer 1988). Also, in the North Atlantic, companies to some extent prefer to hire fishers from the same community to support the social control and create a friendly environment on board.
The major reward in deep sea fishing is the chance of earning good salaries. For women it is furthermore the chance of a rise in status as they cope with work that is traditionally male and culturally ranked as superior to female work (Husmo and Munk-Madsen 1994).
The international deep-sea fishing fleet exploiting global waters may operate their vessels with crews of mixed nationalities. For instance, this is the case with the Taiwanese fleet, the world’s largest deep-sea fishing fleet. This may also be the case in joint venture fisheries where industrialized nations’ vessels are operating in developing countries’ waters. In cross-national crews, communication on board may suffer from language difficulties. Also the maritime hierarchy on board such vessels may be further stratified by an ethnic dimension. Fish workers of different ethnicity and nationality than the mother country of the vessel, particularly if the vessel is operating in home waters, may be treated far below the level that is otherwise required by officers. This concerns wage conditions and basic provisioning on board as well. Such practices may create racist work environments, increase tensions in crew on board and skew power relations between officers and crew.
Poverty, the hope of good earnings and the globalization of deep-sea fishing has fostered illegal recruitment practices. Crews from the Philippines are reported to be indebted to recruitment agencies and working in foreign waters without contracts and without security in pay or safety measures. Working in a highly mobile deep-sea fleet far from home and without support of any authorities leads to high insecurity, which may exceed the risks faced in stormy weather on the open ocean (Cura 1995; Vacher 1994).
Case Study: Indigenous Divers
Indigenous peoples living in coastal areas have for centuries depended on the sea for their survival. In the more tropical waters they have not only fished from traditional boats but also engaged in spear fishing and shell gathering activities, diving either from shore or from boats. The waters in the past were plentiful and there was no need to dive deeply for long periods of time. More recently the situation has changed. Overfishing and the destruction of breeding grounds has made it impossible for indigenous peoples to sustain themselves. Many have turned to diving deeper for longer periods of time in order to bring home a sufficient catch. As the capacity of humans to stay underwater without some form of support is quite limited, indigenous divers in several parts of the world have begun using compressors to supply air from the surface or to use self-contained underwater breathing apparatus (SCUBA) to extend the amount of time that they are able to stay underwater (bottom time).
In the developing world, indigenous divers are found in Central and South America, Southeast Asia and the Pacific. It has been estimated by the University of California at Berkeley, Department of Geography’s Ocean Conservation and Environmental Action Network (OCEAN) Initiative, that there may be as many as 30,000 working indigenous divers in Central America, South America and the Caribbean. (It is estimated that the Moskito Indians in Central America may have a diving population as high as 450 divers.) Researchers at the Divers Diseases Research Centre of the United Kingdom estimate that in the Philippines there may be between 15,000 to 20,000 indigenous divers; in Indonesia the number has yet to be determined but it may be as many as 10,000.
In Southeast Asia some indigenous divers use compressors on boats with air lines or hoses attached to the divers. The compressors are normally commercial type compressors used in filling stations or are compressors salvaged from large trucks and driven by gasoline or diesel engines. Depths may range to more than 90 m and dives may exceed durations of 2 hours. Indigenous divers work to gather fish and shellfish for human consumption, aquaria fish, seashells for the tourist industry, pearl oysters and, at certain times of the year, sea cucumbers. Their fishing techniques include using underwater fish traps, spear fishing and pounding two stones together to drive fish into a net down current. Lobsters, crabs and shellfish are gathered by hand (see figure 1).
Figure 1. An indigenous diver gathering fish.
David Gold
The indigenous Sea Gypsy Divers of Thailand
In Thailand there are approximately 400 divers using compressors and living on the west coast. They are known as Sea Gypsies and were once a nomadic people that have settled in 12 rather permanent villages in three provinces. They are literate and almost all have completed compulsory education. Virtually all of the divers speak Thai and most speak their own language, Pasa Chaaw Lee, which is an unwritten Malay language.
Only males dive, starting as young as 12 years of age and stopping, if they survive, around the age of 50. They dive from open boats, ranging from 3 to 11 m in length. The compressors used are powered by either a gasoline or a diesel powered motor and are primitive, cycling unfiltered air into a pressure tank and down 100 m of hose to a diver. This practice of using ordinary air compressors without filtration can lead to contamination of breathing air with carbon monoxide, nitrogen dioxide from diesel motors, lead from leaded gasoline and combustion particulates. The hose is attached to a normal diving mask which covers the eyes and nose. Inspiration and expiration is done through the nose, with the expired air escaping from the skirt of the mask. The only protection from marine life and the temperature of the water is a roll collar, a long sleeve shirt, a pair of plastic shoes and a pair of athletic style trousers. A pair of cotton mesh gloves offers the hands a certain degree of protection (see figure 2).
Figure 2. A diver off of Phuket, Thailand, preparing to dive from an open boat.
David Gold
A research project was developed in concert with Thailand’s Ministry of Public Health to study the diving practices of the Sea Gypsies and to develop educational and informational interventions to raise the divers’ awareness of the risks they face and measures that can be taken to reduce those risks. As part of this project 334 divers were interviewed by trained public health care workers in 1996 and 1997. The response rate to the questionnaires was over 90%. Although the survey data are still under analysis, several points have been extracted for this case study.
Regarding diving practices, 54% of the divers were asked how many dives they made on their last day of diving. Of the 310 divers that responded to the question, 54% indicated that they made less than 4 dives; 35% indicated 4 to 6 dives and 11% indicated 7 or more dives.
When asked about the depth of their first dive of their last day of diving, of the 307 divers who responded to this question, 51% indicated 18 m or less; 38% indicated between 18 and 30 m; 8% indicated between 30 and 40 m; 2% indicated more than 40 m, with one diver reporting a dive at a depth of 80 m. A 16 year-old diver in one village reported that he had performed 20 dives on his last day of diving to depths of less than 10 m. Since he has been diving he has been struck 3 times by decompression sickness.
A high frequency of dives, deep depths, long bottom times and short surface intervals are factors which can increase the risk of decompression sickness.
Risks
An early random sampling of the survey revealed that the 3 most significant risks included an interruption of the air supply leading to an emergency ascent, injury from marine life and decompression sickness.
Unlike sport or professional divers, the indigenous diver has no alternative air supply. A cut, crimped or separated air hose leaves only two options. The first is to find a fellow diver and share air from one mask, a skill which is virtually unknown to the Sea Gypsies; the second is an emergency swim to the surface, which can and frequently does lead to barotrauma (injury related to rapidly reducing pressure) and decompression sickness (caused by expanding nitrogen gas bubbles in the blood and tissue as the diver surfaces). When asked about separation from diving partners during working dives, of the 331 divers who responded to the question, 113 (34%) indicated that they worked 10 m or more away from their partners and an additional 24 indicated that they were not concerned about the whereabouts of partners during dives. The research project is currently instructing the divers how to share air from one mask while encouraging them to dive closer together.
Since indigenous divers are frequently working with dead or injured marine life, there is always the potential that a hungry predator may also attack the indigenous diver. The diver may also be handling poisonous marine animals, thus increasing the risk of illness or injury.
Regarding decompression sickness, 83% of divers said they considered pain as part of the job; 34% indicated they had recovered from decompression sickness, and 44% of those had had decompression sickness 3 or more times.
An occupational health intervention
On the implementation side of this project, 16 health care workers at the village level along with 3 Sea Gypsies have been taught to be trainers. Their task is to work with the divers on a boat-by-boat basis using short (15 minute) interventions to raise the awareness of the divers about the risks they face; give the divers the knowledge and skills to reduce those risks; and develop emergency procedures to assist sick or injured divers. The train-the-trainer workshop developed 9 rules, a short lesson plan for each rule and an information sheet to use as a handout.
The rules are as follows:
- The deepest dive should be first, with each subsequent dive shallower.
- The deepest part of any dive should come first, followed by work in shallower water.
- A safety stop on ascent at 5 m after every deep dive is mandatory.
- Come up slowly from every dive.
- Allow a minimum of one hour on the surface between deep dives.
- Drink large amounts of water before and after each dive.
- Stay within sight of another diver.
- Never hold your breath.
- Always display the international dive flag whenever there are divers underwater.
The Sea Gypsies were born and raised next to or on the sea. They depend on the sea for their existence. Although they are sickened or injured as a result of their diving practices they continue to dive. The interventions listed above will probably not stop the Sea Gypsies from diving, but they will make them aware of the risk they face and provide them the means to reduce this risk.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."