General Profile
Overview
Fishing is among the oldest production activities of humankind. Archaeological and historical research shows that fishing—both freshwater and ocean fishing—was widespread in ancient civilizations. In fact, it seems that human settlements were frequently established in areas of good fishing. These findings concerning the role of fishing for human sustenance are confirmed by modern day anthropological research of primitive societies.
During the past few centuries, the world’s fisheries have been radically transformed. Traditional fishing methods have to a large extent been superseded by a more modern technology stemming from the industrial revolution. This has been followed by a dramatic increase in effective fishing effort, a much smaller increase in global catch levels and a serious decline in many fish stocks. The industrialization of global fishing has also led to destabilization and decline of many traditional fisheries. Finally, increased worldwide fishing pressure has given rise to international disputes about fishing rights.
In 1993, the world harvest of fish was in the neighbourhood of 100 million metric tonnes per annum (FAO 1995). Of this quantity, fish-farming (aqua- and mariculture) accounted for about 16 million tonnes. So the world’s fisheries produced some 84 million tonnes per annum. About 77 million tonnes come from marine fisheries and the rest, some 7 million tonnes, from inland fisheries. To catch this quantity, there was a fishing fleet counting 3.5 million vessels and measuring about 30 million gross registered tonnes (FAO 1993, 1995). There are few hard data about the number of fishermen employed in the operation of this fleet. The Food and Agriculture Organization of the United Nations (FAO 1993) has estimated that they may be as many as 13 million. There is even less information about the number of workers employed in the processing and distribution of the catch. Conservatively estimated they may be 1 to 2 times the number of fishermen. This means that 25 to 40 million people may be directly employed in the fishing industry worldwide.
Asia is by far the largest fishing continent in the world, with close to half of the total annual fish harvest (FAO 1995). North and South America together (30%) come next, followed by Europe (15%). As fishing continents, Africa and Oceania are relatively insignificant, with combined harvest of about 5% of the annual global catch.
In 1993, the largest fishing nation in terms of harvesting volume was China, with about 10 million tonnes of marine catch, corresponding to about 12% of the global marine fish catch. Second and third place were taken by Peru and Japan, with about 10% of the global marine catch each. In 1993, 19 nations had a marine catch in excess of 1 million tonnes.
The world’s harvest of fish is distributed over a large number of species and fisheries. Very few fisheries have an annual yield in excess of 1 million tonnes. The largest ones in 1993 were the Peruvian anchovy fishery (8.3 million tonnes), the Alaska pollock fishery (4.6 million tonnes) and the Chilean horse mackerel fishery (3.3 million tonnes). Together these three fisheries account for about 1/5 of the world’s total marine harvest.
Evolution and Structure of the Fishing Industry
The combination of population growth and advances in fishing technology has led to a great expansion in fishing activity. Commencing centuries ago in Europe, this expansion has been particularly pronounced worldwide during the current century. According to FAO statistics (FAO 1992, 1995), total world catches have quadrupled since 1948, from under 20 million tonnes to the current level of about 80 million tonnes. This corresponds to almost 3% annual growth. However, during the last few years, the ocean harvest has stagnated at about 80 million tonnes annually. As the global fishing effort has continued to increase, this suggests that the exploitation of the world’s most important fish stocks is already at or in excess of the maximum sustainable yield. Hence, unless new fish stocks come under exploitation, the ocean fish catch cannot increase in the future.
The processing and marketing of the fish harvest have also expanded greatly. Assisted by improvements in transportation and conservation technology, and spurred by increased real personal incomes, ever increasing volumes of catch are processed, packaged and marketed as high-value food commodities. This trend is likely to continue at an even faster rate in the future. This means a substantially increased value added per unit of catch. However, it also represents a replacement of the traditional fish-processing and distribution activity by high-technology, industrial production methods. More seriously, this process (sometimes referred to as the globalization of fish markets) threatens to strip underdeveloped communities of their staple fish supply due to overbidding from the industrial world.
The world’s fisheries today are composed of two quite distinct sectors: artisanal fisheries and industrial fisheries. Most artisanal fisheries are a continuation of the traditional local fisheries that have changed very little over the centuries. Consequently, they are usually low technology, labour-intensive fisheries confined to near-shore or inshore fishing grounds (see the article “Case Study: Indigenous Divers”). The industrial fisheries, by contrast, are high technology and extremely capital intensive. The industrial fishing vessels are generally large and well equipped, and can range widely over the oceans.
With regard to vessel numbers and employment, the artisanal sector dominates the world’s fisheries. Almost 85% of the world’s fishing vessels and 75% of the fishermen are artisanal ones. In spite of this, due to its low technology and limited range, the artisanal fleet accounts for only a small fraction of the world’s catch of fish. Moreover, due to the low productivity of the artisanal fleet, the artisanal fishermen’s income is generally low and their working conditions poor. The industrial fishing sector is economically much more efficient. Although the industrial fleet only comprises 15% of the world’s fishing vessels and approximately 50% of the total tonnage of the world’s fishing fleet, it accounts for over 80% of the volume of marine catch in the world.
The increase in fishing during this century is mostly caused by an expansion of the industrial fisheries. The industrial fleet has increased the effectiveness of the harvesting activity in traditional fishing areas and expanded the geographical reach of the fisheries from relatively shallow inshore areas to almost all parts of the oceans where fish are to be found. By contrast, the artisanal fishery has remained relatively stagnant, although there has been technical progress in this part of the fishery as well.
Economic Importance
The current value of the global fish harvest at dockside is estimated to be about US$60 to 70 billion (FAO 1993, 1995). Although fish processing and distribution may be assumed to double or triple this amount, fishing is nevertheless a relatively minor industry from a global perspective, especially when compared to agriculture, the major food production industry of the world. For certain nations and regions, however, fishing is very important. This applies, for instance, to many communities bordering the North Atlantic and North Pacific. Moreover, in many communities of West Africa, South America and Southeast Asia, fishing is the population’s main source of animal protein and, consequently, is economically very important.
Fisheries Management
The global fishing effort has risen sharply during this century, especially after the end of the Second World War. As a result, many of the world’s most valuable fish stocks have been depleted to the point where increased fishing effort actually leads to a drop in the sustainable catch level. The FAO estimates that most of the world’s major fish stocks are either fully utilized or overfished in this sense (FAO 1995). As a result, the harvest from many of the world’s most important species has actually contracted, and, in spite of continuing advances in fishing technology and increases in the real price of fish, the economic returns from the fishing activity have declined.
Faced with diminishing fish stocks and declining profitability of the fishing industry, most of the world’s fishing nations have actively sought means to remedy the situation. These efforts have generally followed two routes: extensions of the national fisheries jurisdictions to 200 nautical miles and more, and an imposition of new fisheries management systems within the national fisheries jurisdictions.
Many different fisheries management methods have been employed for the purpose of improving the economics of fishing. Recognizing that the source of the fisheries problem is the common property nature of the fish stocks, the most advanced fisheries management systems seek to solve the problem by defining quasi-property rights in the fisheries. A common method is to set the total allowable catch for each species and then to allocate this total allowable catch to individual fishing companies in the form of individual catch quotas. These catch quotas constitute a property right in the fishery. Provided the quotas are tradable, the fishing industry finds it to its advantage to restrict fishing effort to the minimum needed to take the total allowable catch and, provided the quotas are also permanent, to adjust the size of the fishing fleet to the long-term sustainable yield of the fishery. This method of fisheries management (usually referred to as the individual transferable quota (ITQ) system) is rapidly expanding in the world today and seems likely to become the management norm for the future.
The expanding range of national fisheries jurisdictions and the property-rights-based management systems being implemented within them imply a substantial restructuring of fishing. The virtual enclosure of the world’s oceans by national fisheries jurisdictions, already well under way, will obviously all but eliminate distant water fishing. The property-rights-based fisheries management systems also represent increased incursion of market forces into fishing. Industrial fishing is economically more efficient than artisanal fishing. Moreover, the industrial fishing companies are in a better position to adjust to new fisheries management systems than artisanal fishermen. Hence, it seems that the current evolution of fisheries management poses yet another threat to the artisanal way of fishing. Given this and the need to curtail overall fishing effort, it seems inevitable that the level of employment in the world’s fisheries will fall drastically in the future.
Environmental and Public Health Issues in Agriculture
As the world’s population continues to increase, demand grows for more food, but the increasing population is claiming more arable land for non-agricultural uses. Agriculturists need options to feed the world’s growing population. These options include augmenting output per hectare, developing unused land into farmland and reducing or stopping the destruction of existing farmland. Over the past 25 years, the world has seen a “green revolution”, particularly in North America and Asia. This revolution resulted in a tremendous increase in food production, and it was stimulated by developing new, more productive genetic strains and increasing inputs of fertilizer, pesticides and automation. The equation for producing more food is confounded by the need to address several environmental and public health issues. These issues include the need to prevent pollution and soil depletion, new ways to control pests, making farming sustainable, abating child labour and eliminating illicit drug cultivation.
Water and Conservation
Water pollution may be the most widespread environmental problem caused by agriculture. Agriculture is a large contributor to nonpoint pollution of surface water, including sediments, salts, fertilizers and pesticides. Sediment runoff results in soil erosion, a loss to agricultural production. Replacing 2.5 cm of topsoil naturally from bedrock and surface material takes between 200 and 1,000 years, a long time in human terms.
Sediment loading of rivers, streams, lakes and estuaries increases water turbidity, which results in decreased light for submerged aquatic vegetation. Species that depend upon this vegetation can thus experience a decline. Sediment also causes deposition in waterways and reservoirs, which adds to dredging expense and reduces water storage capacity of water supplies, irrigation systems and hydroelectric plants. Fertilizer waste, both synthetic and natural, contributes phosphorus and nitrates to the water. Nutrient loading stimulates algal growth, which can lead to eutrophication of lakes and related reduction in fish populations. Pesticides, particularly herbicides, contaminate surface water, and conventional water treatment systems are ineffective at removing them from water downstream. Pesticides contaminate food, water and feed. Groundwater is a source of drinking water for many people, and it is also contaminated with pesticides and nitrate from fertilizers. Groundwater is also used for animals and irrigation.
Irrigation has made farming possible in places where intensive farming was previously impossible, but irrigation has its negative consequences. Aquifers are depleted in places where groundwater use exceeds recharging; aquifer depletion can also lead to land subsidence. In arid areas, irrigation has been associated with mineralization and salinization of soils and water, and it has also depleted rivers. More efficient use and conservation of water can help alleviate these problems (NRC 1989).
Pest Control
Following the Second World War, the use of synthetic organic pesticides—fumigants, insecticides, herbicides and fungicides—grew dramatically, but a plethora of problems has resulted from the use of these chemicals. Growers saw the success of broad-spectrum, synthetic pesticides as a solution to pest problems that had plagued agriculture from its beginning. Not only did problems with human health effects emerge, but environmental scientists recognized ecological damage as extensive. For example, chlorinated hydrocarbons are persistent in soil and bioaccumulate in fish, shellfish and birds. The body burden of these hydrocarbons has declined in these animals where communities have eliminated or reduced chlorinated hydrocarbon use.
Pesticide applications have adversely affected non-targeted species. In addition, pests can become resistant to the pesticides, and examples of resistant species that became more virulent crop predators are numerous. Thus, growers need other approaches for pest control. Integrated pest management is an approach aimed at putting pest control on a sound ecological basis. It integrates chemical control in a way that is least disruptive to biological control. It aims, not to eliminate a pest, but to control the pest to a level that avoids economic damage (NRC 1989).
Genetically engineered crops are increasing in use (see table 1), but in addition to a positive result, they have a negative consequence. An example of a positive result is a genetically engineered strain of insect-resistant cotton. This strain, now in use in the United States, requires only one application of insecticide as contrasted with the five or six applications that would have been typical. The plant generates its own pesticide, and this reduces cost and environmental contamination. The potential negative consequence of this technology is the pest’s developing resistance to the pesticide. When a small number of pests survive the engineered pesticide, they can grow resistant to it. The more virulent pest can then survive the engineered pesticide and similar synthetic pesticides. Thus, the pest problem can magnify beyond the one crop to other crops. The cotton boll weevil is now controlled in this way through an engineered cotton strain. With the emergence of a resistant boll weevil, another 200 crops can fall victim to the weevil, which would no longer be susceptible to the pesticide (Toner 1996).
Table 1. Genetically engineered crops
|
Crop |
Varieties |
|
Cotton |
Three varieties, incorporating insect and herbicide resistance |
|
Corn |
Two varieties, incorporating insect resistance |
|
Soybeans |
One variety, with herbicide resistance |
|
Potatoes |
One variety, incorporating insect resistance |
|
Tomatoes |
Five varieties, with delayed ripening traits, thicker skin |
|
Squash |
One variety, resistant to two viruses |
|
Canola |
One variety, engineered to produce oil rich in lauric acid |
Source: Toner 1996.
Sustainable Farming
Because of environmental and economic concerns, farmers have started using alternative approaches to farming to reduce input costs, preserve resources and protect human health. The alternative systems emphasize management, biological relationships and natural processes.
In 1987, the World Commission on Environment and Development defined sustainable development to meet “the needs and aspirations of the present without compromising the ability of future generations to meet their own needs” (Myers 1992). A sustainable farm, in the broadest sense, produces adequate amounts of high-quality food, protects its resources, and is both environmentally safe and profitable. It addresses risks to human health using a systems-level approach. The concept of sustainable agriculture incorporates the term farm safety across the entire workplace environment. It includes the availability and the appropriate use of all our resources including soil, water, fertilizers, pesticides, the buildings on our farms, the animals, capital and credit, and the people who are part of the agricultural community.
Child and Migrant Labour
Children labour in agriculture throughout the world. The industrialized world in no exception. Of the 2 million children under age 19 who reside on United States farms and ranches, an estimated 100,000 are injured each year in incidents related to production agriculture. They are typically children of either farmers or farm employees (National Committee for Childhood Agricultural Injury Prevention 1996). Agriculture is one of the few occupational settings in both developed and developing countries where children can engage in work typically done by adults. Children are also exposed to hazards when they accompany their parents during work and during leisure-time visits to the farm. The primary agents of farm injuries are tractors, farm machinery, livestock, building structures and falls. Children are also exposed to pesticides, fuels, noxious gases, airborne irritants, noise, vibration, zoonoses and stress. Child labour is employed on plantations around the world. Children work with their parents as part of a team for task-based compensation on plantations and as migrant farmworkers, or they are employed directly for special plantation jobs (ILO 1994).
Table 2. Illicit drug cultivation, 1987, 1991 and 1995
|
Crop |
Product |
Hectares cultivated |
||
|
1987 |
1991 |
1995 |
||
|
Opium poppy |
Opiates |
112,585 |
226,330 |
234,214 |
|
Coca (leaf) |
Cocaine |
175,210 |
206,240 |
214,800 |
|
Cannabis |
Marijuana |
24,423 |
20,919 |
12,205 |
Source: US Department of State 1996.
Some of the problems and conditions of the migrant labour and child workforce as discussed elsewhere in this chapter and in this Encyclopaedia.
Illicit Drug Crops
Some crops do not appear in official records because they are illicit. These crops are cultivated to produce narcotics for human consumption, which alter judgement, are addictive and can cause death. Moreover, they add to the loss of productive land for food production. These crops comprise the poppy (used to make opium and heroine), coca leaf (used to make cocaine and crack) and cannabis (used to produce marijuana). Since 1987, world production of the opium poppy and coca has increased, and cultivation of cannabis has decreased, as shown in table 2). Five links are involved in the farm-to-user chain in the illicit drug trade: cultivation, processing, transit, wholesale distribution and retail sale. To interdict the supply of illicit drugs, governments concentrate on eradicating the production of the drugs. For example, eliminating 200 hectares of coca can deprive the drug market of about one metric ton of finished cocaine for a period of 2 years, since that is how long it would take to grow back mature plants. The most efficient means for eliminating the crops is through aerial application of herbicides, although some governments resist this measure. Manual eradication is another option, but it exposes personnel to violent reaction from the growers (US Department of State 1996). Some of these crops have a legal use, such as the manufacture of morphine and codeine from opium, and exposure to their dusts can lead to narcotic hazards in the workplace (Klincewicz et al. 1990).
Case Study: Argomedicine
Since animal husbandry and crop production began, agriculture and medicine have been interrelated. A healthy farm or livestock operation requires healthy workers. Famine, drought, or pestilence can overwhelm the well-being of all of the interrelated species on the farm; especially in developing countries that depend on agriculture for survival. In colonial times plantation-owners had to be aware of hygienic measures to protect their plants, animals and human workers. At present, examples of agromedical teamwork include: integrated pest management (an ecological approach to pests); tuberculosis (TB) prevention and control (livestock, dairy products and workers); and agricultural engineering (to reduce trauma and farmer’s lung). Agriculture and medicine succeed when they work together as one.
Definitions
The following terms are used interchangeably, but there are noteworthy connotations:
- Agricultural medicine refers to the subdivision of public health and/or occupational medicine included in the training and practice of health professionals.
- Agromedicine is a term coined in the 1950s to emphasize interdisciplinary, programmatic approaches which give a greater role for the agricultural professional based upon the equal partnership of the two disciplines (medicine and agriculture).
In recent years, the definition of agricultural medicine as a subspeciality of occupational/environmental medicine located on the health sciences campus has been challenged to develop a broader definition of agromedicine as a process of linking agricultural and health resources of a state or a region in a partnership dedicated to public service, along the lines of the original land-grant university model.
The essential unity of biological science is well known to plant chemists (nutrition), animal chemists (nutrition) and human chemists (nutrition); the areas of overlap and integration go beyond the boundaries of narrowly defined specialization.
Content areas
Agromedicine has focused on three core areas:
- traumatic injury
- pulmonary exposures
- agrichemical injury.
Other content areas, including zoonoses, rural health services and other community services, food safety (e.g., the relationship between nutrition and cancer), health education and environmental protection, have received secondary emphasis. Other initiatives relate to biotechnology, the challenge of population growth and sustainable agriculture.
Each core area is emphasized in university training and research programmes depending on faculty expertise, grants and funding initiatives, extension needs, commodity producers’ or corporate requests for consultation and networks of inter-university cooperation. For example, traumatic injury skills may be supported by a faculty in agricultural engineering leading to a degree in that branch of agricultural science; farmer’s lung will be covered in a pulmonary medicine rotation in a residency in occupational medicine (post-graduate specialization residency) or in preventive medicine (leading to a master’s or doctorate in public health); an inter-university food safety programme may link the veterinary discipline, the food science discipline and the infectious disease medical speciality. Table 1 compares two types of programmes.
Table 1. Comparison of two types of agromedicine programmes
|
Parameter |
Model A |
Model B |
|
Site (campus) |
Medical |
Medical and agricultural |
|
Support |
Federal, foundation |
State, foundation |
|
Research |
Primary (basic) |
Secondary (applied) |
|
Patient education |
Yes |
Yes |
|
Producer/worker education |
Yes |
Yes |
|
Health provider education |
Yes |
Yes |
|
Extension education |
Elective |
Yes |
|
Cross-discipline education |
Elective |
Yes |
|
Statewide community outreach |
Intermittent |
Ongoing (40 hours/wk) |
|
Constituency:sustainability |
Academic peers |
Growers, consumers, |
|
Prestige (academic) |
Yes |
Little |
|
Growth (capital, grants) |
Yes |
Little |
|
Administration |
Single |
Dual (partners) |
|
Primary focus |
Research, publication, policy recommendations |
Education, public service, client-based research |
In the United States, a number of states have established agromedicine programmes. Alabama, California, Colorado, Georgia, Iowa, Kansas, Kentucky, Minnesota, Mississippi, Nebraska, New York, Oregon, Pennsylvania, South Carolina, Virginia and Wisconsin have active programmes. Other states have programmes which do not use the terms agromedicine or agricultural medicine or which are at early stages of development. These include Michigan, Florida and Texas. Saskatchewan, Canada, also has an active agromedicine programme.
Conclusion
In addition to collaboration across disciplines in so-called basic science, communities need greater coordination of agricultural expertise and medical expertise. Dedicated localized teamwork is required to implement a preventive, educational approach that delivers the best science and the best outreach that a state-funded university system can provide to its citizens.
Health Problems and Disease Patterns in Agriculture
At the end of the twentieth century, less than 5% of the workforce in industrialized nations is employed in agriculture, while nearly 50% of the worldwide workforce is engaged in agriculture (Sullivan et al. 1992). The work varies from highly mechanized to the manually arduous. Some agribusiness has been historically international, such as plantation farming and the growing of export crops. Today, agribusiness is international and is organized around commodities such as sugar, wheat and beef. Agriculture covers many settings: family farms, including subsistence agriculture; large corporate farms and plantations; urban farms, including specialty enterprises and subsistence agriculture; and migrant and seasonal work. Crops vary from widely used staples, such as wheat and rice, to specialty crops such as coffee, fruits and seaweed. Moreover, the young and the old engage in agricultural work to a greater extent than any other industry. This article addresses health problems and disease patterns among agricultural workers except for livestock rearing, which is covered in another chapter.
Overview
The image of agricultural work is that of a healthy pursuit, far from congested and polluted cities, that provides an opportunity for plenty of fresh air and exercise. In some ways, this is true. US farmers, for example, have a lower mortality rate for ischemic heart disease and cancer as compared with other occupations.
However, agricultural work is associated with a variety of health problems. Agricultural workers are at a high risk for particular cancers, respiratory diseases and injuries (Sullivan et al. 1992). Because of the remote location of much of this work, emergency health services are lacking, and agromedicine has been viewed as a vocation without high social status (see article “Agromedicine” and table 1). The work environment involves exposure to the physical hazards of weather, terrain, fires and machinery; toxicological hazards of pesticides, fertilizers and fuels; and health insults of dust. As shown in table 1, table 2, table 3, table 4, table 5, table 6 and table 7, agriculture is associated with a variety of health hazards. In these tables and the corresponding descriptions that follow, six categories of hazards are summarized: (1) respiratory, (2) dermatological, (3) toxic and neoplastic, (4) injury, (5) mechanical and thermal stress and (6) behavioural hazards. Each table also provides a summary of interventions to prevent or control the hazard.
Respiratory Hazards
Agricultural workers are subject to several pulmonary diseases related to exposures at work as shown in table 1. An excess of these diseases has been found in several countries..
Table 1. Respiratory hazards
|
Exposures |
Health effects |
|
Cereal grain pollen, livestock dander, fungal antigens in grain dust and on crops, dust mites, organophosphorus insecticides |
Asthma and rhinitis: Immunoglobin E-mediated asthma |
|
Organic dusts |
Nonimmunologic asthma (grain dust asthma) |
|
Specific plant parts, endotoxins, mycotoxins |
Mucous membrane inflammation |
|
Insecticides, arsenic, irritant dust, ammonia, fumes, grain dust (wheat, barley) |
Bronchospasm, acute and chronic bronchitis |
|
Fungal spores or thermophilic actinomycetes released from mouldy grain or hay, antigens of less than 5 mm in diameter |
Hypersensitivity pneumonitis |
|
Thermophilic actinomycetes: mouldy sugar cane |
Bagassosis |
|
Mushroom spores (during clean-out of beds) |
Mushroom worker’s lung |
|
Mouldy hay, compost |
Farmer’s lung |
|
Fungi: mouldy maple bark |
Maple bark stripper’s disease |
|
Anthropoids: infested wheat |
Wheat weevil disease |
|
Plant debris, starch granules, moulds, endotoxins, mycotoxins, spores, fungi, gram-negative bacteria, enzymes, allergens, insect parts, soil particles, chemical residues |
Organic dust toxic syndrome |
|
Dust from stored grain |
Grain fever |
|
Mouldy silage on top of silage in silo |
Silo unloader’s syndrome |
|
Decomposition gases: ammonia, hydrogen sulphide, carbon monoxide, methane, phosgene, chlorine, sulphur dioxide, ozone, paraquat (herbicide), anhydrous ammonia (fertilizer), oxides of nitrogen |
Acute pulmonary responses |
|
Nitrogen dioxide from fermenting silage |
Silo filler’s disease |
|
Welding fumes |
Metal fume fever |
|
Oxygen deficiency in confined spaces |
Asphyxiation |
|
Soil dust of arid regions |
Valley fever (coccidiomycosis) |
|
Mycobacterium tuberculosis |
Tuberculosis (migrant workers) |
Interventions: ventilation, dust suppression or containment, respirators, mould prevention, smoking cessation.
Sources: Merchant et al. 1986; Meridian Research, Inc. 1994; Sullivan et al. 1992;
Zejda, McDuffie et al. 1994.
Exacerbation of asthma by specific allergens and nonspecific causes has been associated with airborne dust. Several farm antigen exposures can trigger asthma, and they include pollen, storage mites and grain dust. Mucous membrane inflammation is a common reaction to airborne dust in individuals with allergic rhinitis or a history of atopy. Plant parts in grain dust appear to cause mechanical irritation to the eyes, but endotoxin and mycotoxin exposure may also be associated with the inflammation of the eyes, nasal passages and throat.
Chronic bronchitis is more common among farmers than among the general population. The majority of farmers with this illness have a history of exposure to grain dust or work in swine confinement buildings. It is believed that cigarette smoking is additive and a cause of this illness. In addition, acute bronchitis has been described in grain farmers, especially during grain harvest.
Hypersensitivity pneumonitis is caused by repeated antigen exposures from a variety of substances. Antigens include micro-organisms found in spoiled hay, grain and silage. This problem has also been seen among workers who clean out mushroom bed houses.
Organic dust toxic syndrome was originally associated with exposure to mouldy silage and was, thus, called silage unloader’s syndrome. A similar illness, called grain fever, is associated with exposure to stored grain dust. This syndrome occurs without prior sensitization, as is the case with hypersensitivity pneumonitis. The epidemiology of the syndrome is not well defined.
Farmers may be exposed to several different substances that can cause acute pulmonary responses. Nitrogen dioxide generated in silos can cause death among silo workers. Carbon monoxide generated by combustion sources, including space heaters and internal combustion engines, can cause death of agricultural workers exposed to high concentrations inside of buildings. In addition to toxic exposures, oxygen deficiency in confined spaces on farms is a continuing problem.
Many agricultural crops are causative agents for pulmonary diseases when they are processed. These include hypersensitivity pneumonitis caused by mouldy malt (from barley), paprika dust and coffee dust. Byssinosis is caused by cotton, flax and hemp dusts. Several natural products are also associated with occupational asthma when processed: vegetable gums, flax seed, castor bean, soybean, coffee bean, grain products, flour, orris root, papain and tobacco dust (Merchant et al. 1986; Meridian Research, Inc. 1994; Sullivan et al. 1992).
Dermatological Hazards
Farmers are exposed to several skin hazards, as shown table 2. The most common type of agriculture-related skin disease is irritant contact dermatitis. In addition, allergic contact dermatosis is a reaction to exposures to sensitizers including certain plants and pesticides. Other skin diseases include photo-contact, sun-induced, heat-induced, and arthropod-induced dermatoses.
Table 2. Dermatological hazards
|
Exposures |
Health effects |
|
Ammonia and dry fertilizers, vegetable crops, bulb plants, fumigants, oat and barley dust, several pesticides, soaps, petroleum products, solvents, hypochlorite, phenolic compounds, amniotic fluid, animal feeds, furazolidone, hydroquinone, halquinol |
Irritant contact dermatitis |
|
Mites |
Grain itch |
|
Sensitizing plants (poison ivy or oak), certain pesticides (dithiocarbamates, pyrethrins, thioates, thiurams, parathion, and malathion) |
Allergic contact dermatitis |
|
Handling tulips and tulip bulbs |
Tulip finger |
|
Creosote, plants containing furocoumarins |
Photo-contact dermatitis |
|
Sunlight, ultraviolet radiation |
Sun-induced dermatitis, melanoma, lip cancer |
|
Moist and hot environments |
Heat-induced dermatitis |
|
Wet tobacco leaf contact |
Nicotine poisoning (green tobacco sickness) |
|
Fire, electricity, acid or caustic chemicals, dry (hygroscopic) fertilizer, friction, liquified anhydrous ammonia |
Burns |
|
Bites and stings from wasps, chiggers, bees, grain mites, hornets, fire ants, spiders, scorpions, centipedes, other arthropods, snakes |
Arthropod-induced dermatitis, envenomation, Lyme disease, malaria |
|
Punctures and thorn pricks |
Tetanus |
Interventions: Integrated pest management, protective clothing, good sanitation, vaccination, insect control, barrier creams.
Sources: Estlander, Kanerva and Piirilä 1996; Meridian Research, Inc. 1994; Raffle et al. 1994; Sullivan et al. 1992.
The skin can be burned in several ways. Burns can result from dry fertilizer, which is hygroscopic and attracts moisture (Deere & Co. 1994). When on the skin, it can draw out moisture and cause skin burns. Liquid anhydrous ammonia is used for injecting nitrogen into the soil, where it expands into a gas and readily combines with moisture. If the liquid or gas contacts the body—especially the eyes, skin and respiratory tract—cell destruction and burns can occur, and permanent injury can result without immediate treatment.
Tobacco croppers and harvesters can experience green tobacco sickness when working with damp tobacco. Water from rain or dew on the tobacco leaves probably dissolves nicotine to facilitate its absorption through the skin. Green tobacco sickness is manifested with complaints of headache, pallor, nausea, vomiting and prostration following the worker’s contact with wet tobacco leaves. Other insults to the skin include arthropod and reptile stings and bites, and thorn punctures, which can carry diseases.
Toxic and Neoplastic Hazards
The potential for toxic substances exposure in agriculture is great, as can be seen table 3. Chemicals used in agriculture include fertilizers, pesticides (insecticides, fumigants and herbicides) and fuels. Human exposures to pesticides are widespread in developing countries as well as in the developed countries. The United States has registered more than 900 different pesticides with more than 25,000 brand names. About 65% of the registered uses of pesticides are for agriculture. They are primarily used to control insects and to reduce crop loss. Two-thirds (by weight) of the pesticides are herbicides. Pesticides may be applied to seed, soil, crops or the harvest, and they may be applied with spray equipment or crop dusters. After application, pesticide exposures can result from off-gassing, dispersion by the wind, or contact with the plants through skin or clothing. Dermal contact is the most common type of occupational exposure. A number of health effects have been associated with pesticide exposure. These include acute, chronic, carcinogenic, immunologic, neurotoxic and reproductive effects.
Table 3. Toxic and neoplastic hazards
|
Exposures |
Possible health effects |
|
Solvents, benzene, fumes, fumigants, insecticides (e.g., organophosphates, carbamates, organochlorines), herbicides (e.g., phenoxy-aliphatic acids, bipyridyls, triazines, arsenicals, acentanilides, dinitro-toluidine), fungicides (e.g., thiocarbamates, dicarboximides) |
Acute intoxication, Parkinson’s disease, peripheral neuritis, Alzheimer’s disease, acute and chronic encephalopathy, non-Hodgkin lymphoma, Hodgkin’s lymphoma, multiple myeloma, soft-tissue sarcoma, leukaemias, cancers of the brain, prostrate, stomach, pancreas and testicle, glioma |
|
Solar radiation |
Skin cancer |
|
Dibromochloropropane (DBCP), ethylene dibromide |
Sterility (male) |
Interventions: integrated pest management, respiratory and dermal protection, good pesticide application practices, safe re-entry time into fields after pesticide application, container labelling with safety procedures, carcinogen identification and elimination.
Sources: Connally et al. 1996; Hanrahan et al. 1996; Meridian Research, Inc. 1994; Pearce and Reif 1990; Popendorf and Donham 1991; Sullivan et al. 1992; Zejda, McDuffie and Dosman 1993.
Farmers experience a higher risk for some site-specific cancers. These include brain, stomach, lymphatic and haematopoietic, lip, prostrate and skin cancer. Solar and pesticide (especially herbicide) exposure have been related to higher cancer risks for farm populations (Meridian Research, Inc. 1994; Popendorf and Donham 1991; Sullivan et al. 1992).
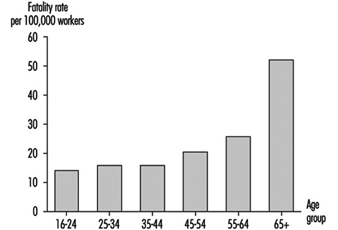
Injury Hazards
Studies have consistently shown that agricultural workers are at increased risk of death due to injury. In the United States, a study of work-related fatalities for 1980 to 1989 reported rates in agricultural production of 22.9 deaths per 100,000 workers, as compared to 7.0 deaths per 100,000 for all workers. The average fatality rate for males and females, respectively, was 25.5 and 1.5 deaths per 100,000 workers. The leading causes of death in agricultural production were machinery and motor vehicles. Many studies report the tractor as the leading machine involved in fatalities, frequently from tractor rollovers. Other leading causes of death include electrocutions, caught in, flying objects, environmental causes and drowning. Age is an important risk factor related to agricultural fatalities for males. For example, the fatality rate for agricultural workers in the US over the age of 65 was over 50 per 100,000 workers, more than double the overall average (Meyers and Hard 1995) (see figure 1). Table 4 shows several injury hazard exposures, their consequences and recognized interventions.
Figure 1. Agricultural workers fatality rates, US, 1980-89
|
Exposures |
Health effects |
|
Road vehicle crashes, machinery and vehicles, struck by objects, falls, oxygen depletion, fires |
Fatalities |
|
Tractors |
Crushing of the chest, extravasation (escape of fluids—e.g., blood—and surrounding tissue), strangulation/asphyxia, drowning |
|
Augers |
Hypovolemia (loss of blood), sepsis and asphyxia |
|
Electricity |
Electrocutions |
|
Machinery and vehicles, draught animal kicks and assaults, falls |
Nonfatal injuries: injury infection (e.g., tetanus) |
|
Hay balers |
Friction burns, crushing, neurovascular disruption, avulsion, fractures, amputation |
|
Power take-offs |
Skin or scalp avulsion or degloving, amputation, multiple blunt injury |
|
Corn pickers |
Hand injuries (friction burns, crushing, avulsion or degloving, finger amputation) |
|
Fires and explosions |
Serious or fatal burns, smoke inhalation, |
Interventions: rollover protective structures, guards, good practices, safe electrical wiring, fire prevention, protective equipment, good housekeeping practices.
Sources: Deere & Co. 1994; Meridian Research, Inc. 1994; Meyers and Hard 1995.
A 1993 survey of farm injuries in the United States found the major injury sources to be livestock (18%), machinery (17%) and hand tools (11%). The most frequent injuries reported in this study were sprain and strain (26%), cut (18%) and fracture (15%). Males represented 95% of the injuries, while the highest concentration of injuries occurred among workers 30 to 39 years of age. Table 5 shows the source and nature of injury and the activity during injury for four major crop production categories. The National Safety Council estimated a US rate of 13.2 occupational injuries and illnesses per 100 crop production workers in 1992. More than half of these injures and illnesses resulted in an average of 39 days away from work. In contrast, the manufacturing and construction sectors had an injury and illness incidence rate of, respectively, 10.8 and 5.4 per 100 workers. In another study in the United States, investigators determined that 65% of all farm injuries required medical attention and that machinery other than tractors caused nearly half of the injuries that resulted in permanent disability (Meridian Research, Inc. 1994; Boxer, Burnett and Swanson 1995).
Table 5. Percentages of lost time injuries by source of injury, nature of injury, and activity for four types of agricultural operations, United States, 1993.
|
Cash grain |
Field crops |
Vegetables, fruits, nuts |
Nursery crops |
|
|
Source of Injury |
||||
|
Tractors |
11.0 |
9.7 |
– |
1.0 |
|
Machinery |
18.2 |
18.6 |
25.1 |
12.5 |
|
Livestock |
11.0 |
12.1 |
1.7 |
– |
|
Hand tools |
13.4 |
13.0 |
19.3 |
3.8 |
|
Power tools |
4.3 |
4.6 |
0.4 |
17.9 |
|
Pesticides/chemicals |
1.3 |
2.8 |
0.4 |
0.5 |
|
Plants or trees |
2.2 |
3.1 |
7.4 |
4.6 |
|
Working surfaces |
11.5 |
11.6 |
6.8 |
5.1 |
|
Trucks or automobiles |
4.7 |
1.4 |
1.5 |
– |
|
Other vehicles |
3.6 |
– |
3.5 |
– |
|
Liquids |
3.1 |
1.0 |
– |
– |
|
Other |
15.6 |
22.2 |
34.0 |
54.5 |
|
Nature of Injury |
||||
|
Sprain/strain |
20.5 |
23.5 |
39.3 |
38.0 |
|
Cut |
16.4 |
32.3 |
18.9 |
21.7 |
|
Fracture |
20.3 |
6.5 |
4.3 |
5.6 |
|
Bruise |
9.3 |
9.5 |
12.6 |
14.8 |
|
Crush |
10.4 |
2.6 |
2.4 |
1.0 |
|
Other |
23.1 |
25.6 |
22.5 |
18.9 |
|
Activity |
||||
|
Farm maintenance |
23.8 |
19.1 |
10.8 |
33.3 |
|
Field work |
17.2 |
34.6 |
34.0 |
38.2 |
|
Crop handling |
14.1 |
13.8 |
9.4 |
7.7 |
|
Livestock handling |
17.1 |
14.7 |
5.5 |
3.2 |
|
Machine maintenance |
22.6 |
10.1 |
18.0 |
– |
|
Other |
5.1 |
7.5 |
22.3 |
17.6 |
Source: Meyers 1997.
Mechanical and Thermal Stress Hazards
As discussed above, sprains and strains are a significant problem among agricultural workers, and as shown in table 6, agricultural workers are exposed to several mechanical and thermal stresses that result in injury. Many of these problems result from handling heavy loads, repetitive motion, poor posture and dynamic motion. In addition, agricultural vehicle operators are exposed to whole-body vibration. One study reported the prevalence of low-back pain to be 10% greater among tractor drivers.
Table 6. Mechanical and thermal stress hazards
|
Exposures |
Health effects |
Interventions |
|
Tendon overuse, stretching; excessive force |
Tendon-related disorders (tendinitis, tenosynovitis) |
Ergonomic design, vibration dampening, warm clothing, rest periods |
|
Repetitive motion, awkward wrist posture |
Carpal tunnel syndrome |
|
|
Vibration of the hands |
Raynaud’s syndrome |
|
|
Repetition, high force, poor posture, whole-body vibration |
Degenerative changes, low-back pain, intervertebral disk herniation; peripheral nerve and vascular, |
|
|
Motor and machinery noise |
Hearing loss |
Noise control, hearing protection |
|
Increased metabolism, high temperatures and humidity, limited water and electrolytes |
Heat cramps, heat exhaustion, heat stroke |
Drinking water, rest breaks, protection from the sunshine |
|
Low temperatures, lack of dry clothing |
Frost nip, chilblains, frostbite, systemic hypothermia |
Dry, warm clothing, heat generation from activity |
Source: Meridian Research, Inc. 1994.
Noise-induced hearing loss is common among agricultural workers. One study reported that farmers more than 50 years of age have as much as 55% hearing loss. A study of rural students found that they have two times greater hearing loss than urban students.
Agricultural workers are exposed to temperature extremes. They may be exposed to hot, humid environments in work in the tropical and subtropical zones, and during the summer in the temperate zones. Heat stress and stroke are hazards under these conditions. Conversely, they may be exposed to extreme cold in the temperate zones in the winters and possible frostbite or death from hypothermia (Meridian Research, Inc. 1994).
Behavioural Hazards
Some aspects of farming can cause stress among farmers. As shown in table 7, these include isolation, risk taking, patriarchal attitudes, pesticide exposures, unstable economies and weather, and immobility. Problems associated with these circumstances include dysfunctional relationships, conflicts, substance abuse, home violence and suicide. Most suicides associated with depression on farms in North America involve victims who are married and are full-time farmers, and most use firearms to commit suicide. The suicides tend to happen during peak farming periods (Boxer, Burnett and Swanson 1995).
Table 7. Behavioural hazards
|
Exposures |
Health effects |
Interventions |
|
Isolation, economic threats, intergenerational problems, violence, substance abuse, incest, pesticides, risk taking, patriarchal attitudes, unstable weather, immobility |
Depression, anxiety, suicide, poor coping |
Early diagnosis, counselling, empowerment, pesticide control, community support |
|
Tuberculosis, sexually transmitted diseases (migrant workers) |
Interpersonal illness |
Early diagnosis, vaccination, condom use |
Sources: Boxer, Burnett and Swanson 1995; Davies 1995; Meridian Research, Inc. 1994; Parrón, Hernández and Villanueva 1996.
Migrant farm labourers are at high risk of tuberculosis, and where male workers predominate, sexually transmitted diseases are a problem. Female migrant workers experience problems of appropriate perinatal outcome, high infant mortality rates, and low occupational risk perceptions. A broad range of behavioural issues is currently being investigated among migrant workers, including child abuse and neglect, domestic violence, substance abuse, mental disorders and stress-related conditions (ILO 1994).
Hops
Hops are used in brewing and are commonly grown in the Pacific Northwest of the United States, Europe (especially Germany and the United Kingdom), Australia and New Zealand.
Hops grow from rhizome cuttings of female hop plants. Hop vines grow up to 4.5 to 7.5 m or more during the growing season. These vines are trained to climb up heavy trellis wire or heavy cords. Hops are traditionally spaced 2 m apart in each direction with two cords per plant going to the overhead trellis wire at about 45° angles. Trellises are about 5.5 m high and are made from 10 ´ 10 cm pressure-treated timbers or poles sunk 0.6 to 1 m into the ground.
Manual labour is used to train the vines after the vines reach about a third of a metre in length; additionally, the lowest metre is pruned to allow air circulation to reduce disease development.
Hops vines are harvested in the fall. In the United Kingdom, some hops are grown in trellises 3 m high and harvested with an over-the-row mechanical harvester. In the United States, hop combines are available to harvest 5.5-m-high trellises. The areas that the harvesters (field strippers) are unable to get are harvested by hand with a machete. Newly harvested hops are then kiln dried from 80% moisture to about 10%. Hops are cooled, then baled and taken to cold storage for end use.
Safety Concerns
Workers need to wear long sleeves and gloves when working near the vines, because hooked hairs of the plant may cause a rash on the skin. Some individuals become more sensitized to the vines than others.
A majority of the injuries involve strains and sprains due to lifting materials such as irrigation pipes and bales, and over-reaching when working on trellises. Workers should be trained in lifting or mechanical aids should be used.
Workers need to wear chaps at the knee and below to protect the leg from cuts while cutting the vines by hand. Eye protection is a must while working with the vines.
Many injuries occur while workers tie twine to the wire trellis wire. Most work is performed while standing on high trailers or platforms on tractors. Accidents have been reduced by providing safety belts or guard rails to prevent falls, and by wearing eye protection. Because there is much movement with the hands, carpal tunnel syndrome may be a problem.
Since hops are often treated with fungicides during the season, proper posting of re-entry intervals is needed.
Worker’s compensation claims in Washington State (US) tend to indicate that injury incidence ranges between 30 and 40 injuries per 100 person years worked. Growers through their association have safety committees that actively work to lower injury rates. Injury rates in Washington are similar to those found in the tree fruit industry and dairy. Highest injury incidence tends to occur in August and September.
The industry has unique practices in the production of the product, where much of the machinery and equipment is locally manufactured. By the vigilance of the safety committees to provide adequate machine guarding, they are able to reduce “caught in” type injuries within the harvesting and processing operations. Training should focus on proper use of knives, PPE and prevention of falls from vehicles and other machines.
Tea Cultivation
Adapted from 3rd edition, “Encyclopaedia of Occupational Health and Safety”.
Tea (Camellia sinensis) was originally cultivated in China, and most of the world’s tea still comes from Asia, with lesser quantities from Africa and South America. Ceylon and India are now the largest producers, but sizeable quantities also come from China, Japan, the former USSR, Indonesia and Pakistan. The Islamic Republic of Iran, Turkey, Viet Nam and Malaysia are small-scale growers. Since the Second World War, the area under tea cultivation in Africa has been expanding rapidly, particularly in Kenya, Mozambique, Congo, Malawi, Uganda and the United Republic of Tanzania. Mauritius, Rwanda, Cameroon, Zambia and Zimbabwe also have small acreages. The main South American producers are Argentina, Brazil and Peru.
Plantations
Tea is most efficiently and economically produced in large plantations, although it is also grown as a smallholder crop. In Southeast Asia, the tea plantation is a self-contained unit, providing accommodation and all facilities for its workers and their families, each unit forming a virtually closed community. Women form a large proportion of the workers in India and Ceylon, but the pattern is somewhat different in Africa, where mainly male migrant and seasonal labour is employed and families do not have to be housed. See also the article “Plantations” [AGR03AE] in this chapter.
Cultivation
Land is cleared and prepared for new planting, or areas of old, poor-quality tea are uprooted and replanted with high-yielding vegetatively propagated cuttings. New fields take a couple of years to come into full bearing. Regular programmes of manuring, weeding and pesticide application are carried on throughout the year.
The plucking of the young tea leaves—the famous “two leaves and a bud”—takes place the year round in most of Southeast Asia, but is restricted in areas with a marked cold season (see figure 1). After a cycle of plucking which lasts about 3 to 4 years, bushes are pruned back fairly drastically and the area weeded. Hand weeding is now widely giving way to the use of chemical herbicides. The plucked tea is collected in baskets carried on the backs of the pluckers and taken down to centrally located weighing sheds, and from these to the factories for processing. In some countries, notably Japan and the former USSR, mechanical plucking has been carried out with some success, but this requires a reasonably flat terrain and bushes grown in set rows.
Figure 1. Tea pluckers at work on a plantation in Uganda
Hazards and Their Prevention
Falls and injuries caused by agricultural implements of the cutting and digging type are the most common types of accidents. This is not unexpected, considering the steep slopes on which tea is generally grown and the type of work involved in the processes of clearing, uprooting and pruning. Apart from exposure to natural hazards like lightning, workers are liable to be bitten by snakes or stung by hornets, spiders, wasps or bees, although highly venomous snakes are seldom found at the high altitudes at which the best tea grows. An allergic condition caused by contact with a certain species of caterpillar has been recorded in Assam, India.
The exposure of workers to ever-increasing quantities of highly toxic pesticides requires careful control. Substitution with less-toxic pesticides and attention to personal hygiene are necessary measures here. Mechanization has been fairly slow, but an increasing number of tractors, powered vehicles and implements are coming into use, with a concomitant increase in accidents from these causes (see figure 2). Well-designed tractors with safety cabs, operated by trained, competent drivers will eliminate many accidents.
Figure 2. Mechanical harvesting on a tea plantation near the Black Sea
In Asia, where the non-working population resident on the tea estates is almost as great as the workforce itself, the total number of accidents in the home is equal to that of accidents in the field.
Housing is generally substandard. The most common diseases are those of the respiratory system, closely followed by enteric diseases, anaemia and substandard nutrition. The former are mainly the outcome of working and living conditions at high altitudes and exposure to low temperatures and inclement weather. The intestinal diseases are due to poor sanitation and low standards of hygiene among the labour force. These are mainly preventable conditions, which underlines the need for better sanitary facilities and improved health education. Anaemia, particularly among working mothers of child-bearing age, is all too common; it is partly the result of ankylostomiasis, but is due mainly to protein-deficient diets. However, the principal causes of lost work time are generally from the more minor ailments and not serious diseases. Medical supervision of both housing and working conditions is an essential preventive measure, and official inspection, either at local or national level, is also necessary to ensure that proper health facilities are maintained.
Coffee Cultivation
It is thought that the word coffee derives from Kaffa, a village in Ethiopia where the plant is thought to have its origin. Some, however, consider that the word stems from qahwa, meaning wine in Arabic. Coffee cultivation spread the world over, starting in Arabia (one species is called Coffea arabica, and a variety is Moka, named after an Arab village), passing through many countries, such as Ceylon, Java, India, the Philippines, Hawaii and Viet Nam, among others, some of which are important producers to this day. In America, coffee was introduced from plants previously adapted to the climate in Amsterdam and Paris, planted in Martinique, Surinam and French Guyana, from where it was brought to Brazil, the largest producing country in the world.
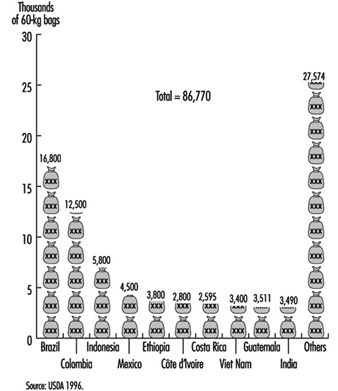
World production may be estimated from figure 1. The 1995–96 crop generated wealth estimated at approximately US$27 million, indicating the economic significance of this product worldwide.
Figure 1. World coffee production for 1995 - 96
The trend towards a global economy, growing competition and the search for technologies with higher productivity also have effects upon coffee cultivation. Mechanization is being disseminated and updated. Moreover, new methods of cultivation are introduced, among them high-density cultivation, in which the distance between plants is being reduced. This modern method increases the number of coffee trees from 3,000 or 4,000 to 100,000 plants per hectare, with an increase in productivity of around 50% over the traditional method. This procedure is important for workers’ health, since lower risks are involved and less herbicide is applied, especially after the third year. On the other hand, there is an increase in the frequency of tree cutting and higher demand for control of fungus disease in the plants.
Coffee is highly sensitive to fluctuations in international commerce; many countries tend to replace coffee with other crops in which financial return is more predictable. In Brazil, for instance, coffee represented 68% of the total volume of exports in 1920; in the 1990s it is only 4%. Coffee is being replaced by soy bean, citric fruits, corn, latex and especially sugar cane.
It is extremely difficult to obtain a reliable estimate of the total labour force involved in coffee cultivation because the number of employed workers is quite variable. During harvest, a large number of seasonal workers are hired, to be dismissed soon after the crop is over. Moreover, in small properties, very often workers are not legally registered, and therefore are not shown in official reports. In Brazil in 1993, for a production of 28.5 million coffee bags, the number of workers was estimated at 1.1 million in direct and 4 to 5 million in indirect jobs. If the same parameters are applied to world production for the same year, coffee workers around the world could be estimated at approximately 3.6 million.
It is equally difficult to know the average figure of workers per rural property. In general, small or medium-sized properties are predominant. The sex and age distribution of the working population is equally unknown, even though female population among workers is increasing and children are known to be employed in coffee plantations. Figures for unionized workers vary according to the labour policies in each country, but they are known to be generally scarce.
Operations
Coffee cultivation and treatment involve the following steps: tree abatement; soil preparation; planting (small plants are usually grown in nurseries in the same or in external properties); treatment (soil correction, fertilizing, pest control and terrain cleaning manually or with herbicides); fruit picking (ripe fruit is usually red and therefore called a berry—see figure 2; sieving to get rid of impurities; transportation; washing to remove pulp and membranes; sun drying, revolving grains with a rake, or mechanical drying through hot air blasting; hand separation of grains; storing in silos; and bagging.
Figure 2. High-density coffee cultivation showing berries
[Missing]
Potential Risks
Risk factors that may affect workers’ health in coffee cultivation are the same as for agricultural workers in general.
From tree abatement and terrain preparation to the final storage of coffee bags, each step may involve several risk factors for workers’ health and safety. Injury risks are present mainly in mechanized processes, tree abatement, terrain preparation, mechanical picking, transportation of coffee and workers as well, fruit treatment (including the risk of boiler explosion) and use of hand tools (very often improvised or without maintenance).
Potential risks of occupational diseases due to physical conditions are related to heat exposure in drying operations, solar radiation, machine noise, ergonomic problems from hand tools, vibration from machinery and tractors, and cold and humidity from outdoor exposure.
The main chemical agents present as potential risks for workers’ health are pesticides and herbicides. Those most often used are gliphosate as an herbicide, copper salts as fungicides and organophosphorus compounds for other pests commonly found on coffee trees. The number of pesticide applications varies according to tree age, soil composition, climatic conditions, vegetation species or variety, cultivation system (e.g., high or low density) and other factors. Spraying is usually done individually with backpack equipment, or from tractors. Large amounts are usually required, and it is said that “without spraying no crop is available”.
Chemical fertilizers may also present a health risk. Often used are compounds derived from boron, zinc, nitrogen, sodium, potassium, calcium, magnesium and sulphur. The release of particles from fertilizer handling should be kept under control.
Biological agents may represent important risks for workers’ health. They may include, for instance, bites or stings from snakes, spiders, bees, mosquitoes and acarids, some of them important as disease vectors. In certain areas, endemic diseases may be serious risks for coffee workers.
Ergonomic, psychosocial and organizational factors are discussed below.
Health Effects
Examples of injuries related to work are cuts from hand tools, sprains and fractures from machines and injuries from tractors. Fatal injuries, even if unusual, have occurred as a result of overturning of tractors or inadequate vehicles used in transportation of workers. When artificial drying is employed, heat sources may cause burns and explosions.
Occupational diseases may result from exposure to solar ultraviolet radiation; cutaneous conditions may range from a simple erythema to skin cancer. Hearing loss among machine operators, pulmonary allergic conditions, poisoning from herbicides and pesticides, callosities, lung diseases, bone and circulatory conditions due to vibration, and muscular and skeletal trouble due to poor ergonomic positions or excessive weight (one coffee bag can weigh 60 kg) are other occupational conditions that may occur among coffee cultivation workers. Although primarily a problem among workers processing coffee beans, green bean handlers have complained of respiratory and eye problems. Coffee bean dust has been associated with occupational dust diseases.
Tropical diseases such as malaria, yellow fever, filariasis, trypanossomiasis, leishmaniasis and onchocercosis are prevalent in certain cultivating areas. Tetanus is still prevalent in many rural areas.
More complex health problems related to psychosocial and organizational factors may also affect coffee workers. Since large numbers of workers are required during harvest, and very few during the rest of the year, seasonal contracts are usually practised, often resulting in difficult health problems.
In many cases, workers leave their families and remain during the harvest season in precarious lodgings under inadequate sanitary conditions. If the planting area is close to town, the farmer will contract only one man in the family. However, to increase the profit, the worker himself may bring his whole family to help, including women and children. In some areas, the number of children at work is so high that schools will be closed during the whole harvest season.
In this type of seasonal activity, workers will turn from one type of cultivation to another, according to each harvest period. Since men leave their families, women are called “widows with living husbands”. Very often, a man will raise another family, away from his original town.
Proper compliance with labour legislation and social security is usually restricted to large plantations, and labour inspection in rural areas is generally ineffective. Health care is usually very limited. Duration of work is extended to many hours daily; weekends and normal vacations are seldom respected.
These psychosocial and organizational factors result in marked deterioration in workers’ health, manifested through early ageing, low life expectancy, increase in prevalence and longer duration of diseases, malnutrition (eating the food taken to the field in cans without heating it has led to workers being given a nickname—boias frias in Portuguese), anaemia and hypovitaminoses leading to loss of disposition to work, mental trouble and other manifestations.
Prevention
Preventive measures concerning coffee are the same that apply to rural work in general. Collective protection includes machine guarding, care in application of pesticides and herbicides, mechanizing operations that require undue effort and energy consumption, and adequate transportation of workers. In high-density plantations, regular cutting will not allow the trees to grow, which will eliminate the use of dangerous and uncomfortable ladders for hand picking. When drying requires the use of boilers, careful periodic preventive maintenance is of utmost importance. Biological pest control and proper selection of species resistant to plagues are important preventive measures concerning pesticides, avoiding workers’ disease and environmental protection as well.
Implementation of the use of recommended PPE is difficult because such equipment is usually not adapted to climatic conditions or to the biotype of workers. Moreover, there is usually no educational orientation to facilitate the use, and the selection of equipment is not always correct. Equipment in general use is restricted to boots, hats and clothing to protect from the weather, even though hand, lung, eye and ear protection may be required.
Prevention to control psychosocial and organizational factors may bring up many difficulties. Workers’ awareness should be raised through educational activities, especially in unions and other workers’ organizations, increasing perceptions about workers’ rights to better living and working conditions; moreover, employers should develop their perceptions concerning their social responsibilities towards the labour force. The State should exercise an effective and constant orientation and enforcement wherever legal action is required. Some countries have developed rules and regulations specifically applicable to rural workers. In Brazil, for example, Rural Regulatory Standards establish general directives concerning safety in rural activities, the organization of occupational health services and safety committees in plantations, use of personal protective equipment and handling of chemicals (pesticides, fertilizers and soil-correcting products).
Health control through occupational medicine should cover the evaluation of health effects due to exposure to pesticides, ultraviolet radiation, excessive noise and many other hazards. It may, in many circumstances, be more necessary to control worm diseases, anaemia, hypertension, behavioural problems, eye defects and similar problems, due to their high prevalence in rural areas. Health education should be stressed, as well as tetanus immunization, including for pregnant workers to prevent neonatal tetanus. In some regions, immunization against yellow fever is necessary. Chemoprophylaxis is recommended in areas where malaria is endemic, together with the use of repellents and a preventive orientation against mosquitoes, until sanitation is adequate to control or suppress vectors of the aetiological agent. Serum against snake poison should be available.
Acknowledgement: The authors are obliged to the cooperation received from Professor Nelson Batista Martin, from the Institute of Rural Economy, State Secretary of Agriculture, Sao Paulo; Andre Nasser and Ricardo Luiz Zucas, from the Brazilian Rural Society; and Monica Levy Costa, from the School Health Center, School of Public Health, Sao Paulo University.
Aquatic Plants
Adapted from J.W.G. Lund’s article, “Algae”, “Encyclopaedia of Occupational Health and Safety,” 3rd edition.
Worldwide aquaculture production totalled 19.3 million tonnes in 1992, of which 5.4 million tonnes came from plants. In addition, much of the feed used on fish farms is water plants and algae, contributing to their growth as a part of aquaculture.
Water plants that are grown commercially include water spinach, watercress, water chestnuts, lotus stems and various seaweeds, which are grown as low-cost foods in Asia and Africa. Floating water plants that have commercial potential are duckweed and water hyacinth (FAO 1995).
Algae are a diverse group of organisms; if the cyanobacteria (blue-green algae) are included, they come in a range of sizes from bacteria (0.2 to 2 microns) to giant kelps (40 m). All algae are capable of photosynthesis and can liberate oxygen.
Algae are nearly all aquatic, but they may also live as a dual organism with fungi as lichens on drier rocks and on trees. Algae are found wherever there is moisture. Plant plankton consists almost exclusively of algae. Algae abound in lakes and rivers, and on the seashore. The slipperiness of stones and rocks, the slimes and discolourations of water usually are formed by aggregations of microscopic algae. They are found in hot springs, snowfields and Antarctic ice. On mountains they can form dark slippery streaks (Tintenstriche) that are dangerous to climbers.
There is no general agreement about algae classification, but they are commonly divided into 13 major groups whose members may differ markedly from one group to another in colour. The blue-green algae (Cyanophyta) are also considered by many microbiologists to be bacteria (Cyanobacteria) because they are procaryotes, which lack the membrane-bounded nuclei and other organelles of eukaryotic organisms. They are probably descendants of the earliest photosynthetic organisms, and their fossils have been found in rocks some 2 billion years old. Green algae (Chlorophyta), to which Chlorella belongs, has many of the characteristics of other green plants. Some are seaweeds, as are most of the red (Rhodophyta) and brown (Phaeophyta) algae. Chrysophyta, usually yellow or brownish in colour, include the diatoms, algae with walls made of polymerized silicon dioxide. Their fossil remains form industrially valuable deposits (Kieselguhr, diatomite, diatomaceous earth). Diatoms are the main basis of life in the oceans and contribute about 20 to 25% of the world’s plant production. Dinoflagellates (Dinophyta) are free-swimming algae especially common in the sea; some are toxic.
Uses
Water culture can vary greatly from the traditional 2-month to annual growing cycle of planting, then fertilizing and plant maintenance, followed by harvesting, processing, storage and sale. Sometimes the cycle is compressed to 1 day, such as in duckweed farming. Duckweed is the smallest flowering plant.
Some seaweeds are valuable commercially as sources of alginates, carrageenin and agar, which are used in industry and medicine (textiles, food additives, cosmetics, pharmaceuticals, emulsifiers and so on). Agar is the standard solid medium on which bacteria and other micro-organisms are cultivated. In the Far East, especially in Japan, a variety of seaweeds are used as human food. Seaweeds are good fertilizers, but their use is decreasing because of the labour costs and the availability of relatively cheap artificial fertilizers. Algae play an important part in tropical fish farms and in rice fields. The latter are commonly rich in Cyanophyta, some species of which can utilize nitrogen gas as their sole source of nitrogenous nutrient. As rice is the staple diet of the majority of the human race, the growth of algae in rice fields is under intensive study in countries such as India and Japan. Certain algae have been employed as a source of iodine and bromine.
The use of industrially cultivated microscopic algae has often been advocated for human food and has a potential for very high yields per unit area. However, the cost of dewatering has been a barrier.
Where there is a good climate and inexpensive land, algae can be used as part of the process of sewage purification and harvested as animal food. While a useful part of the living world of reservoirs, too much algae can seriously impede, or increase the cost of water supply. In swimming pools, algal poisons (algicides) can be used to control algal growth, but, apart from copper in low concentrations, such substances cannot be added to water or domestic supplies. Over-enrichment of water with nutrients, notably phosphorus, with consequent excessive growth of algae, is a major problem in some regions and has led to bans on the use of phosphorus-rich detergents. The best solution is to remove the excess phosphorus chemically in a sewage plant.
Duckweed and a water hyacinth are potential livestock feeds, compost input or fuel. Aquatic plants are also used as feed for noncarnivorous fish. Fish farms produce three primary commodities: finfish, shrimp and mollusc. Of the finfish portion, 85% are made up of noncarnivorous species, primarily the carp. Both the shrimp and mollusc depend upon algae (FAO 1995).
Hazards
Abundant growths of freshwater algae often contain potentially toxic blue-green algae. Such “water blooms” are unlikely to harm humans because the water is so unpleasant to drink that swallowing a large and hence dangerous amount of algae is unlikely. On the other hand, cattle may be killed, especially in hot, dry areas where no other source of water may be available to them. Paralytic shellfish poisoning is caused by algae (dinoflagellates) on which the shellfish feed and whose powerful toxin they concentrate in their bodies with no apparent harm to themselves. Humans, as well as marine animals, can be harmed or killed by the toxin.
Prymnesium (Chrysophyta) is very toxic to fish and flourishes in weakly or moderately saline water. It presented a major threat to fish farming in Israel until research provided a practical method of detecting the presence of the toxin before it reached lethal proportions. A colourless member of the green algae (Prototheca) infects humans and other mammals from time to time.
There have been a few reports of algae causing skin irritations. Oscillatoria nigroviridis are known to cause dermatitis. In freshwater, Anaebaena, Lyngbya majuscula and Schizothrix can cause contact dermatitis. Red algae are known to cause breathing distress. Diatoms contain silica, so they could pose a silicosis hazard as a dust. Drowning is a hazard when working in deeper water while cultivating and harvesting water plants and algae. The use of algicides also poses hazards, and precautions provided on the pesticide label should be followed.
Mushrooms
The world’s most widely cultivated edible fungi are: the common white button mushroom, Agaricus bisporus, with an annual production in 1991 of approximately 1.6 million tonnes; the oyster mushroom, Pleurotus spp. (about 1 million tonnes); and the shiitake, Lentinus edodes (about 0.6 million tonnes) (Chang 1993). Agaricus is mainly grown in the western hemisphere, whereas oyster mushrooms, shiitake and a number of other fungi of lesser production are mostly produced in East Asia.
The production of Agaricus and the preparation of its substrate, compost, are for a large part strongly mechanized. This is generally not the case for the other edible fungi, although exceptions exist.
The Common Mushroom
The common white button mushroom, Agaricus bisporus, is grown on compost consisting of a fermented mixture of horse manure, wheat straw, poultry manure and gypsum. The materials are wetted, mixed and set in large heaps when fermented outdoors, or brought into special fermentation rooms, called tunnels. Compost is usually made in quantities of up to several hundred tonnes per batch, and large, heavy equipment is used for mixing heaps and for filling and emptying the tunnels. Composting is a biological process that is guided by a temperature regime and that requires thorough mixing of the ingredients. Before being used as a substrate for growth, compost should be pasteurized by heat treatment and conditioned to get rid of the ammonia. During composting, a considerable amount of sulphur-containing organic volatiles evaporates, which can cause odour problems in the surroundings. When tunnels are used, the ammonia in the air can be cleaned by acid washing, and odour escape can be prevented by either biological or chemical oxidation of the air (Gerrits and Van Griensven 1990).
The ammonia-free compost is then spawned (i.e., inoculated with a pure culture of Agaricus growing on sterilized grain). Mycelial growth is carried out during a 2-week incubation at 25 °C in a special room or in a tunnel, after which the grown compost is placed in growing rooms in trays or in shelves (i.e., a scaffold system with 4 to 6 beds or tiers above each other with a distance of 25 to 40 cm in between), covered with a special casing consisting of peat and calcium carbonate. After a further incubation, mushroom production is induced by a temperature change combined with strong ventilation. Mushrooms appear in flushes with weekly intervals. They are either harvested mechanically or hand-picked. After 3 to 6 flushes, the growing room is cooked out (i.e., steam pasteurized), emptied, cleaned and disinfected, and the next growing cycle can be started.
Success in mushroom cultivation depends heavily on cleanliness and prevention of pests and diseases. Although management and farm hygiene are key factors in disease prevention, a number of disinfectants and a limited number of pesticides and fungicides are still used in the industry.
Health Risks
Electrical and mechanical equipment
A pre-eminent risk in mushroom farms is the accidental exposure to electricity. Often high voltage and amperage is used in humid environments. Ground fault circuit interrupters and other electrical precautions are necessary. National labour legislation usually sets rules for the protection of labourers; this should be strictly followed.
Also, mechanical equipment may pose dangerous threats by its damaging weight or function, or by the combination of both. Composting machines with their large moving parts require care and attention to prevent accidents. Equipment used in cultivation and harvesting often has rotating parts used as grabbers or harvesting knives; their use and transport require great care. Again, this holds for all machines that are moving, whether they be self-propelled or pulled over beds, shelves or rows of trays. All such equipment should be properly guarded. All personnel whose duties include handling electrical or mechanical equipment in mushroom farms should be carefully trained before work is started and safety rules should be adhered to. Maintenance ordinances of equipment and machines should be taken very seriously. A proper lockout/tagout programme is needed as well. Lack of maintenance causes mechanical equipment to become extremely dangerous. For example, breaking pull chains have caused several deaths in mushroom farms.
Physical factors
Physical factors such as climate, lighting, noise, muscle load and posture strongly influence the health of workers. The difference between ambient outside temperature and that of a growing room can be considerable, especially in the winter. One should allow the body to adapt to a new temperature with every change of location; not doing so may lead to diseases of the airways and eventually to a susceptibility to bacterial and viral infections. Further, exposure to excessive temperature changes may cause muscles and joints to become stiff and inflamed. This may lead to a stiff neck and back, a painful condition causing unfitness for work.
Insufficient lighting in mushroom-growing rooms not only causes dangerous working conditions but also slows down picking, and it prevents pickers from seeing the possible symptoms of disease in the crop. The lighting intensity should be at least 500 lux.
Muscle load and posture largely determine the weight of labour. Unnatural body positions are often required in manual cultivation and picking tasks due to the limited space in many growing rooms. Those positions may damage joints and cause static overload of the muscles; prolonged static loading of muscles, such as that which occurs during picking, can even cause inflammation of joints and muscles, eventually leading to partial or total loss of function. This can be prevented by regular breaks, physical exercises and ergonomic measures (i.e., adaptation of the actions to the dimensions and possibilities of the human body).
Chemical factors
Chemical factors such as exposure to hazardous substances create possible health risks. The large-scale preparation of compost has a number of processes that can pose lethal risks. Gully pits in which recirculation water and drainage from compost is collected are usually devoid of oxygen, and the water contains high concentrations of hydrogen sulphide and ammonia. A change in acidity (pH) of the water may cause a lethal concentration of hydrogen sulphide to occur in the areas surrounding the pit. Piling wet poultry or horse manure in a closed hall may cause the hall to become an essentially lethal environment, due to the high concentrations of carbon dioxide, hydrogen sulphide and ammonia which are generated. Hydrogen sulphide has a powerful odour at low concentrations and is especially threatening, since at lethal concentrations this compound appears to be odourless because it inactivates human olfactory nerves. Indoor compost tunnels do not have sufficient oxygen to support human life. They are confined spaces, and testing of air for oxygen content and toxic gases, wearing of appropriate PPE, having an outside guard and proper training of involved personnel are essential.
Acid washers used for removal of ammonia from the air of compost tunnels require special care because of the large quantities of strong sulphuric or phosphoric acid that are present. Local exhaust ventilation should be provided.
Exposure to disinfectants, fungicides and pesticides can take place through the skin by exposure, through the lungs by breathing, and through the mouth by swallowing. Usually fungicides are applied by a high-volume technique such as by spray lorries, spray guns and drenching. Pesticides are applied with low-volume techniques such as misters, dynafogs, turbofogs and by fumigation. The small particles that are created remain in the air for hours. The right protective clothing and a respirator that has been certified as appropriate for the chemicals involved should be worn. Although the effects of acute poisoning are very dramatic, it should not be forgotten that the effects of chronic poisoning, although less dramatic at first glance, also always require occupational health surveillance.
Biological factors
Biological agents can cause infectious diseases as well as severe allergic reactions (Pepys 1967). No human infectious disease cases caused by the presence of human pathogens in compost have been reported. However, mushroom worker’s lung (MWL) is a severe respiratory disease that is associated with handling the compost for Agaricus (Bringhurst, Byrne and Gershon-Cohen 1959). MWL, which belongs to the group of diseases designated extrinsic allergic alveolitis (EAA), arise from exposure to spores of the thermophilic actinomycetes Excellospora flexuosa, Thermomonospora alba, T. curvata and T. fusca that have grown during the conditioning phase in compost. They can be present in high concentrations in the air during spawning of phase 2 compost (i.e., over 109 colony-forming units (CFU) per cubic metre of air) (Van den Bogart et al. 1993); for causation of EAA symptoms, 108 spores per cubic metre of air are sufficient (Rylander 1986). The symptoms of EAA and thus MWL are fever, difficult respiration, cough, malaise, increase in number of leukocytes and restrictive changes of lung function, starting only 3 to 6 hours after exposure (Sakula 1967; Stolz, Arger and Benson 1976). After a prolonged period of exposure, irreparable damage is done to the lung due to inflammation and reactive fibrosis. In one study in the Netherlands, 19 MWL patients were identified among a group of 1,122 workers (Van den Bogart 1990). Each patient demonstrated a positive response to inhalation provocation and possessed circulating antibodies against spore antigens of one or more of the actinomycetes mentioned above. No allergic reaction had been found with Agaricus spores (Stewart 1974), which may indicate low antigenicity of the mushroom itself or low exposure. MWL can easily be prevented by providing workers with powered air-purifying respirators equipped with a fine dust filter as part of their normal work gear during spawning of compost.
Some pickers have been found to suffer from damaged skin of finger tips, caused by exogenous glucanases and proteases of Agaricus. Wearing gloves during picking prevents this.
Stress
Mushroom growing has a short and complicated growing cycle. Thus managing a mushroom farm brings worries and tensions which may extend to the workforce. Stress and its management are discussed elsewhere in this Encyclopaedia.
The Oyster Mushroom
Oyster mushrooms, Pleurotus spp., can be grown on a number of different lignocellulose-containing substrates, even on cellulose itself. The substrate is wetted and usually pasteurized and conditioned. After spawning, mycelial growth takes place in trays, shelves, special containers or in plastic bags. Fructification takes place when the ambient carbon dioxide concentration is decreased by ventilation or by opening the container or bag.
Health risks
Health risks associated with the cultivation of oyster mushrooms are comparable to those linked to Agaricus as described above, with one major exception. All Pleurotus species have naked lamellae (i.e., not covered by a veil), which results in the early shedding of a large number of spores. Sonnenberg, Van Loon and Van Griensven (1996) have counted spore production in Pleurotus spp. and found up to a billion spores produced per gram of tissue per day, depending on species and developmental stage. The so-called sporeless varieties of Pleurotus ostreatus produced about 100 million spores. Many reports have described the occurrence of EAA symptoms after exposure to Pleurotus spores (Hausen, Schulz and Noster 1974; Horner et al. 1988; Olson 1987). Cox, Folgering and Van Griensven (1988) have established the causal relation between exposure to Pleurotus spores and occurrence of EAA symptoms caused by inhalation. Because of the serious nature of the disease and the high sensitivity of humans, all workers should be protected with dust respirators. Spores in the growing room should at least partially be removed before workers enter the room. This can be done by directing the circulation air over a wet filter or by setting ventilation at full power 10 minutes before workers enter the room. Weighing and packing of mushrooms can be done under a hood, and during storage the trays should be covered by foil to prevent release of spores into the working environment.
Shiitake Mushrooms
In Asia this tasty mushroom, Lentinus edodes, has been grown on wood logs in the open air for centuries. The development of a low-cost cultivation technique on artificial substrate in growing rooms rendered its culture economically feasible in the western world. The artificial substrates usually consist of a wetted mixture of hardwood sawdust, wheat straw and high-concentration protein meal, which is pasteurized or sterilized before spawning. Mycelial growth takes place in bags, or in trays or shelves, depending on the system used. Fruiting is commonly induced by temperature shock or by immersion in ice-cold water, as is done to induce production on wood logs. Due to its high acidity (low pH), the substrate is susceptible to infection by green moulds such as Penicillium spp. and Trichoderma spp. Prevention of the growth of those heavy sporulators requires either sterilization of the substrate or use of fungicides.
Health risks
The health risks associated with the cultivation of shiitake are comparable with those of Agaricus and Pleurotus. Many strains of shiitake sporulate easily, leading to concentrations of up to 40 million spores per cubic metre of air (Sastre et al. 1990).
Indoor cultivation of shiitake has regularly led to EAA symptoms in workers (Cox, Folgering and Van Griensven 1988, 1989; Nakazawa, Kanatani and Umegae 1981; Sastre et al. 1990) and inhalation of spores of shiitake is the cause of the disease (Cox, Folgering and Van Griensven 1989). Van Loon et al. (1992) have shown that in a group of 5 patients tested, all had circulating IgG-type antibodies against shiitake spore antigens. Despite the use of protective mouth masks, a group of 14 workers experienced a rise in antibody titres with increased duration of employment, indicating the need for better prevention, such as powered air-purifying respirators and appropriate engineering controls.
Acknowledgement: The view and results presented here are strongly influenced by the late Jef Van Haaren, M.D., a fine person and gifted occupational health physician, whose humane approach to the effects of human labour was best reflected in Van Haaren (1988), his chapter in my textbook that formed the basis of the present article.
Ginseng, Mint and Other Herbs
There is no standard definition for the term herb, and the distinction between the herbs and spice plants is unclear. This article provides an overview of general aspects of some herbs. There are more than 200 herbs, which we are here considering to be those plants originally grown mainly in temperate or Mediterranean climates for their leaves, stems and flowering tops. The primary use for herbs is to flavour foods. Important culinary herbs include basil, bay or laurel leaf, celery seed, chervil, dill, marjoram, mint, oregano, parsley, rosemary, sage, savory, tarragon and thyme. The major demand for culinary herbs comes from the retail sector, followed by the food processing and food service sectors. The United States is by far the major consumer of culinary herbs, followed by the United Kingdom, Italy, Canada, France and Japan. Herbs are also used in cosmetics and pharmaceutical products to impart desirable flavours and odours. Herbs are used medicinally by the pharmaceutical industry and in the practice of herbal medicine.
Ginseng
Ginseng root is used in the practice of herbal medicine. China, the Republic of Korea and the United States are major producers. In China, most operations have historically been plantations owned and run by the government. In the Republic of Korea, the industry is made up of more than 20,000 family operations, most of which are smallholdings, family operations that plant less than an acre each year. In the United States, the largest proportion of producers work on smallholdings and plant less than two acres per year. However, the largest proportion of the US crop is produced by a minority of growers with a hired workforce and mechanization that allows them to plant as much as 60 acres per year. Ginseng is usually grown in open field plots covered by artificial shade structures that simulate the effects of the forest canopy.
Ginseng is also grown in intensively cultivated forest plots. A few per cent of the world’s production (and most organic ginseng) is gathered by wild collectors. The roots take 5 to 9 years to reach marketable size. In the United States, bed preparation for either forest plot or open field methods is typically accomplished by a tractor-towed plow. Some hand labour may be required to clear ditches and give the beds their final shape. Mechanized planters pulled behind a tractor are often used for seeding, although the more labour-intensive practice of transplanting nursery seedlings into beds is common in the Republic of Korea and China. Constructing the 7- to 8-foot-high pole and wood lath or cloth shade structures over open field plots is labour intensive and involves considerable lifting and overhead work. In Asia, locally available woods and thatch or woven reeds are used in the shade structures. In mechanized operations in the United States, mulching the plants is accomplished with straw shredders which are adapted from machines used in the strawberry industry and pulled behind a tractor.
Depending on the adequacy and condition of machine guarding, contact with the tractor PTO shaft, the straw shredder’s intake or other moving machinery parts can present a risk of entanglement injury. For each year until harvest, three hand weedings are required, which involve crawling, bending and stooping to work at crop level and which place high demands on the musculoskeletal system. Weeding, especially for the first- and second-year plants, is intensive work. One acre of field-grown ginseng may require more than 3,000 total hours of weeding over the 5 to 9 years preceding harvest. New chemical and non-chemical weed control methods, including better mulching, may be able to reduce the musculoskeletal demands posed by weeding. New tools and mechanization also hold promise for reducing the demands of weeding work. In Wisconsin, US, some herb growers are testing an adapted pedal cycle that allows weeding in a seated posture.
Artificial shade creates an especially humid environment susceptible to fungus and mould infestation. Fungicides are routinely applied at least monthly in the United States with tractor-towed application machinery or backpack garden sprayers. Insecticides are also spray applied as needed, and rodenticides put out. The use of lower-toxicity chemicals, improvements in application machinery and alternative pest management practices are strategies for reducing the repeated, low-dose pesticide exposures experienced by employees.
When the roots are ready for harvest, the shade structures are disassembled and stored. Mechanized operations utilize digging machinery adapted from the potato industry which is towed behind a tractor. Here again, inadequate machine guarding of the tractor PTO and moving machinery parts may present a risk of entanglement injuries. Picking, the last step in harvesting, involves hand labour and bending and stooping to gather roots from the soil surface.
On smaller holdings in the United States, China and the Republic of Korea, most or all of the steps in the production process are typically done by hand.
Mint and Other Herbs
There is considerable diversity in herb production methods, geographical locations, work methods and hazards. Herbs can be collected in the wild or grown under cultivation. Cultivated plant production has the advantages of greater efficiency, more consistent quality and timing of the harvest, and the potential for mechanization. Much of the mint and other herb production in the United States is highly mechanized. Soil preparation, planting, cultivation, pest control and harvesting are all done from the seat of a tractor with towed machinery.
Potential hazards resemble those in other mechanized crop production and include motor vehicle collisions on public roads, traumatic injuries involving tractors and machinery and agricultural chemical poisonings and burns.
More labour-intensive cultivation methods are typical in Asia, North Africa, the Mediterranean and other areas (e.g., mint production in China, India, the Philippines and Egypt). Plots are ploughed, often with animals, and then beds are prepared and fertilized by hand. Depending on the climate, a network of irrigation trenches is excavated. Depending on the type of herb produced, seeds, cuttings, seedlings or rhizome portions are planted. Periodic weeding is especially labour intensive and the day-long shifts of stooping, bending and pulling place high demands on the musculoskeletal system. Despite extensive use of manual labour, weed control in herb cultivation is sometimes inadequate. For a few crops, chemical weeding with herbicides, sometimes followed by manual weeding, is used, but herbicide use is not widespread since herb crops are often herbicide sensitive. Mulching crops can reduce weeding labour needs as well as conserve soil and soil moisture. Mulching also generally aids plant growth and yield, since mulch adds organic matter to soils as it decomposes.
Aside from weeding, labour-intensive soil preparation methods, planting, construction of shade or support structures, harvesting and other operations can also result in high musculoskeletal demands for prolonged periods. Modifications in production methods, specialized hand tools and techniques, and mechanization are possible directions to explore for reducing musculoskeletal and labour demands.
The potential for pesticide and other agricultural chemical burns and poisonings can be a concern on labour-intensive operations since backpack sprayers and other manual application methods may not prevent adverse exposures via the skin, mucous membranes or breathing air. Work in greenhouse production poses special hazards due to the confined breathing atmosphere. Substituting lower toxicity chemicals and alternative pest management strategies, improving application equipment and application practices, and making better PPE available may be ways to reduce risks.
The extraction of volatile oils from the harvested crop is common for certain herbs (e.g., mint stills). Cut and chopped plant material is loaded into an enclosed wagon or other structure. Boilers produce live steam which is forced into the sealed structure through low-pressure hoses, and the oil is floated and extracted from the resulting vapour.
Possible hazards associated with the process include burns from live steam and, less frequently, boiler explosions. Preventive measures include regular inspections of boilers and live steam lines to ensure structural integrity.
Herb production with low levels of mechanization may require prolonged close contact with plant surfaces and oils and, less often, associated dusts. Some reports are available in the medical literature of sensitization reactions, occupational dermatitis, occupational asthma and other respiratory and immunological problems associated with a number of herbs and spices. The available literature is small and may reflect underreporting rather than a low likelihood of health problems.
Occupational dermatitis has been associated with mint, laurel, parsley, rosemary and thyme, as well as cinnamon, chicory, cloves, garlic, nutmeg and vanilla. Occupational asthma or respiratory symptoms have been associated with dust from Brazilian ginseng and parsley as well as black pepper, cinnamon, cloves, coriander, garlic, ginger, paprika and red chillies (capsaicin), along with bacteria and endotoxins in dusts from grains and herbs. However, most cases have occurred in the processing industry, and only a few of these reports have described problems arising directly from exposures incurred in herb cultivation work (e.g., dermatitis after parsley picking, asthma after chicory root handling, immunologic reactivity after greenhouse work with paprika plants). In most reports, a proportion of the workforce develops problems while other employees are less affected or asymptomatic.
Processing Industry
The herb and spice crop processing industry represents a higher order of magnitude exposure to certain hazards than herb crop cultivation. For example, the grinding, crushing and mixing of leaves, seeds and other plant materials can involve work in noisy, extremely dusty conditions. Hazards in herb processing operations include hearing loss, traumatic injuries from inadequately guarded moving machinery parts, dust exposures in breathing air, and dust explosions. Closed processing systems or enclosures for machinery can reduce noise. Feed openings of grinding machines should not permit the entry of hands or fingers.
Health conditions including skin diseases, irritation of the eyes, mouth and gastrointestinal tract, and respiratory and immunological problems have been linked to dusts, fungi and other air contaminants. Self selection based on ability to tolerate health effects has been noted in spice grinders, usually within the first 2 weeks of work. Segregation of the process, effective local exhaust ventilation, improved dust collection, regular mopping and vacuuming of work areas, and personal protective equipment can help reduce risks from dust explosions and contaminants in breathing air.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."