Warshaw, Leon J.
Address: Institute of Environmental Medicine, 180 West End Avenue #6C, New York, New York 10023-4926
Country: United States
Phone: 1 (212) 877-1060
E-mail: 76451.333@compuserve.com
Past position(s): Executive Director, New York Business Group on Health; Deputy Director for Health Affairs, New York City Mayor's Office of Operations; Vice-President, Corporate Medical Director, Equitable Life Assurance Society of the US
Areas of interest: Organization of occupational health services; health promotion; stress; violence in the; workplace
Health Care: Its Nature and its Occupational Health Problems
Health care is a labour intensive industry and, in most countries, health care workers (HCWs) constitute a major sector of the workforce. They comprise a wide range of professional, technical and support personnel working in a large variety of settings. In addition to health professionals, laboratory technicians, pharmacists, social workers and others involved in clinical services, they include administrative and clerical personnel, housekeeping and dietary staff, laundry workers, engineers, electricians, painters and maintenance workers who repair and refurbish the building and the equipment it contains. In contrast with those providing direct care, these support workers usually have only casual, incidental contact with patients.
HCWs represent diverse educational, social and ethnic levels and are usually predominantly female. Many, particularly in home care, are employed in entry-level positions and require considerable basic training. Table 1 lists samples of health care functions and associated occupations.
Table 1. Examples of health care functions and associated occupations
|
Functions |
Occupational category * |
Specific occupations |
|
Direct patient care |
Health-diagnosing occupations |
Physicians |
|
Technical support |
Health technicians |
Clinical laboratory technicians |
|
Services |
Health services |
Dental assistants |
|
Administrative support |
Clerical services |
Billing clerks |
|
Research |
Scientific occupations |
Scientists and research |
* Occupational categories are, in part, adapted from those used by the US Department of Labor, Bureau of Labor Statistics.
A segment of the health sector (unfortunately, often too small and under-resourced in most communities) is devoted to direct and indirect preventive services. The major focus of the health care industry, however, is the diagnosis, treatment and care of the sick. This creates a special set of dynamics, for the sick exhibit varying levels of physical and emotional dependencies that set them apart from the customers in such personal services industries as, for example, retail trade, restaurants and hotels. They require, and traditionally receive, special services and considerations, often on an emergency basis, provided frequently at the expense of the HCWs’ personal comfort and safety.
Reflecting their size and numbers of employees, acute and long-term care facilities constitute perhaps the most prominent elements in the health care industry. They are supplemented by outpatient clinics, “surgicenters” (facilities for outpatient surgery), clinical and pathological laboratories, pharmacies, x-ray and imaging centres, ambulance and emergency care services, individual and group offices, and home care services. These may be located within a hospital or operated elsewhere under its aegis, or they may be free-standing and operated independently. It should be noted that there are profound differences in the way health services are delivered, ranging from the well-organized, “high tech” care available in urban centres in developed countries to the underserved areas in rural communities, in developing countries and in inner-city enclaves in many large cities.
Superimposed on the health care system is a massive educational and research establishment in which students, faculty, researchers and support staffs often come in direct contact with patients and participate in their care. This comprises schools of medicine, dentistry, nursing, public health, social work and the variety of technical disciplines involved in health care.
The health care industry has been undergoing profound changes during the past few decades. Ageing of the population, especially in developed countries, has amplified the use of nursing homes, domiciliary facilities and home care services. Scientific and technological developments have not only led to the creation of new types of facilities staffed by new classes of specially-trained personnel, but they have also de-emphasized the role of the acute care hospital. Now, many services requiring inpatient care are being provided on an ambulatory basis. Finally, fiscal constraints dictated by the continuing escalation of health care costs have been reconfiguring the health care industry, at least in developing countries, resulting in pressure for cost-containment to be achieved through changes in the organization of health care services.
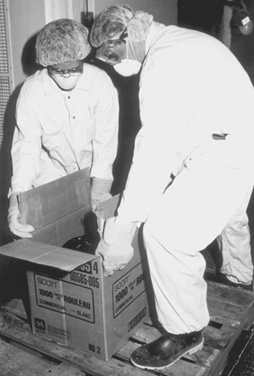
HCWs who are in direct contact with the sick, wherever they work, are exposed to a number of unique hazards. They face the risk of acquiring infections from the patients they serve, as well as the risk of musculoskeletal injuries when lifting, transferring or restraining them. Support staff not directly involved in patient care (e.g., laundry and housekeeping and materials handling workers) are not only routinely exposed to chemicals, such as cleaning agents and disinfectants of industrial strength, but are also exposed to biological hazards from contaminated linens and wastes (see figure 1). There is also the ethos of health care which, especially in emergency situations, requires HCWs to put the safety and comfort of their patients above their own. Coping with the stress of therapeutic failures, death and dying often takes its toll in worker burnout. All this is compounded by shift work, deliberate or inadvertent understaffing and the necessity of catering to the sometimes unreasonable demands from patients and their families. Finally, there is the threat of abuse and violence from patients, particularly when the job requires them to work alone or takes them into unsafe areas. All these are described in greater detail in other articles in this chapter and elsewhere in this Encyclopaedia.
Figure 1. Handling contaminated biological material
Health Sciences Centre, Winnipeg, Manitoba, Canada
The US National Institute for Occupational Safety and Health (NIOSH) reported that needle punctures, musculoskeletal sprains and back injuries probably were the most common injuries in the health care industry (Wugofski 1995). The World Health Organization (WHO) Conference on Occupational Hazards in 1981 identified as its five main areas of concern:
- cuts, lacerations and fractures
- back injuries
- lack of personal safety equipment
- poor maintenance of mechanical and electrical systems
- assault by patients.
Are they health care workers, too?
Often overlooked when considering the safety and well-being of health care workers are students attending medical, dental, nursing and other schools for health professionals and volunteers serving pro bono in healthcare facilities. Since they are not “employees” in the technical or legal sense of the term, they are ineligible for workers’ compensation and employment-based health insurance in many jurisdictions. Health care administrators have only a moral obligation to be concerned about their health and safety.
The clinical segments of their training bring medical, nursing and dental students into direct contact with patients who may have infectious diseases. They perform or assist in a variety of invasive procedures, including taking blood samples, and often do laboratory work involving body fluids and specimens of urine and faeces. They are usually free to wander about the facility, entering areas containing potential hazards often, since such hazards are rarely posted, without an awareness of their presence. They are usually supervised very loosely, if at all, while their instructors are often not very knowledgeable, or even interested, in matters of safety and health protection.
Volunteers are rarely permitted to participate in clinical care but they do have social contacts with patients and they usually have few restrictions with respect to areas of the facility they may visit.
Under normal circumstances, students and volunteers share with health care workers the risks of exposure to potentially harmful hazards. These risks are exacerbated at times of crisis and in emergencies when they step into or are ordered into the breech. Clearly, even though it may not be spelled out in laws and regulations or in organizational procedure manuals, they are more than entitled to the concern and protection extended to “regular” health care workers.
Leon Warshaw
Biological Hazards
Biological hazards, which pose a risk for infectious disease, are common throughout the world, but they are particularly problematic in developing countries. While the hepatitis B virus (HBV) is a nearly universal threat to HCWs, it is particularly important in African and Asian countries where this virus is endemic. As discussed later in this chapter, the risk of HBV transmission after percutaneous exposure to hepatitis B surface antigen (HBsAg) positive blood is approximately 100-fold higher than the risk of transmitting the human immunodeficiency virus (HIV) through percutaneous exposure to HIV-infected blood (i.e., 30% versus 0.3%). Nonetheless, there has indeed been an evolution of concern regarding parenteral exposure to blood and body fluids from the pre-HIV to the AIDS era. McCormick et al. (1991) found that the annual reported incidents of injuries from sharp instruments increased more than threefold during a 14-year period and among medical house officers the reported incidents increased ninefold. Overall, nurses incur approximately two-thirds of the needlestick injuries reported. Yassi and McGill (1991) also noted that nursing staff, particularly nursing students, are at highest risk for needlestick injuries, but they also found that approximately 7.5% of medical personnel reported exposures to blood and body fluids, a figure that is probably low because of underreporting. These data were consistent with other reports which indicated that, while there is increased reporting of needlesticks reflecting concerns about HIV and AIDS, certain groups continue to underreport. Sterling (1994) concludes that underreporting of needlestick injuries ranges from 40 to 60%.
Certain risk factors clearly enhance the likelihood of transmission of bloodborne diseases; these are discussed in the article “Prevention of occupational transmission of bloodborne pathogens”. Frequent exposure has indeed been associated with high seroprevalence rates of hepatitis B among laboratory workers, surgeons and pathologists. The risk of hepatitis C is also increased. The trend towards greater attention to prevention of needlestick injuries is, however, also noteworthy. The adoption of universal precautions is an important advance. Under universal precautions, it is assumed that all blood-containing fluid is potentially infectious and that appropriate safeguards should always be invoked. Safe disposal containers for needles and other sharp instruments are increasingly being placed in conveniently accessible locations in treatment areas, as illustrated in figure 2. The use of new devices, such as the needle-less access system for intravenous treatment and/or blood sampling has been shown to be a cost-effective method of reducing needlestick injuries (Yassi and McGill 1995).
Figure 2. Disposal container for sharp instruments and devices
Health Sciences Centre, Winnipeg, Manitoba, Canada
Blood and body fluids are not the only source of infection for HCWs. Tuberculosis (TB) is also on the rise again in parts of the world where previously its spread had been curtailed and, as discussed later in this chapter, is a growing occupational health concern. In this, as in other nosocomial infections, such concern is heightened by the fact that so many of the organisms involved have become drug-resistant. There is also the problem of new outbreaks of deadly infectious agents, such as the Ebola virus. The article “Overview of infectious diseases” summarizes the major infectious disease risks for HCWs.
Chemical Hazards
HCWs are exposed to a wide variety of chemicals, including disinfectants, sterilants, laboratory reagents, drugs and anaesthetic agents, to name just a few of the categories. Figure 3 shows a storage cabinet in an area of a large hospital where prosthetics are fabricated and clearly illustrates the vast array of chemicals that are present in health care facilities. Some of these substances are highly irritating and may also be sensitizing. Some disinfectants and antiseptics also tend to be quite toxic, also with irritating and sensitizing propensities that may induce skin or respiratory tract disease. Some, like formaldehyde and ethylene oxide, are classified as mutagens, teratogens and human carcinogens as well. Prevention depends on the nature of the chemical, the maintenance of the apparatus in which it is used or applied, environmental controls, worker training and, in some instances, the availability of correct personal protective equipment. Often such control is straightforward and not very expensive. For example, Elias et al. (1993) showed how ethylene oxide exposure was controlled in one health care facility. Other articles in this chapter address chemical hazards and their management.
Figure 3. Storage cabinet for hazardous chemicals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Physical Hazards and the Building Environment
In addition to the specific environmental contaminants faced by HCWs, many health care facilities also have documented indoor air quality problems. Tran et al. (1994), in studying symptoms experienced by operating room personnel, noted the presence of the “sick building syndrome” in one hospital. Building design and maintenance decisions are, therefore, extremely important in health care facilities. Particular attention must be paid to correct ventilation in specific areas such as laboratories, operating rooms and pharmacies, the availability of hoods and avoidance of the insertion of chemical-laden fumes into the general air-conditioning system. Controlling the recirculation of air and using special equipment (e.g., appropriate filters and ultraviolet lamps) is needed to prevent the transmission of air-borne infectious agents. Aspects of the construction and planning of health care facilities are discussed in the article “Buildings for health care facilities”.
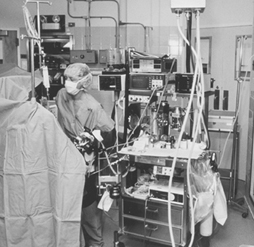
Physical hazards are also ubiquitous in hospitals (see “Exposure to physical agents” in this chapter). The wide variety of electrical equipment used in hospitals can present an electrocution hazard to patients and staff if not properly maintained and grounded (see figure 4). Especially in hot and humid environments, heat exposure may present a problem to workers in such areas as laundries, kitchens and boiler rooms. Ionizing radiation is a special concern for staff in diagnostic radiology (i.e., x ray, angiography, dental radiography and computerized axial tomography (CAT) scans) as well as for those in therapeutic radiology. Controlling such radiation exposures is a routine matter in designated departments where there is careful supervision, well-trained technicians and properly shielded and maintained equipment, but it can be a problem when portable equipment is used in emergency rooms, intensive care units and operating rooms. It can also be a problem to housekeeping and other support staff whose duties take them into areas of potential exposure. In many jurisdictions these workers have not been properly trained to avoid this hazard. Exposure to ionizing radiation may also present a problem in diagnostic and therapeutic nuclear medicine units and in preparing and distributing doses of radioactive pharmaceuticals. In some cases, however, radiation exposure remains a serious problem (see the article “Occupational health and safety practice: The Russian experience” in this chapter).
Figure 4. Electrical equipment in hospital
Health Sciences Centre, Winnipeg, Manitoba, Canada
Contradicting the prevailing impression of hospitals as quiet workplaces, Yassi et al. (1991) have documented the surprising extent of noise-induced hearing loss among hospital workers (see table 2). The article “Ergonomics of the physical work environment” in this chapter offers useful recommendations for controlling this hazard, as does table 3.
Table 2. 1995 integrated sound levels
|
Area monitored |
dBA (lex) Range |
|
Cast room |
76.32 to 81.9 |
|
Central energy |
82.4 to 110.4 |
|
Nutrition and food services (main kitchen) |
|
|
Housekeeping |
|
|
Laundry |
|
|
Linen service |
76.3 to 91.0 |
|
Mailroom |
|
|
Maintenance |
|
|
Materials handling |
|
|
Print shop |
|
|
Rehabilitation engineering |
|
Note: “Lex” means the equivalent sound level or the steady sound level in dBA which, if present in a workplace for 8 hours, would contain the same acoustic energy.
Table 3. Ergonomic noise reduction options
|
Work area |
Process |
Control options |
|
Central energy |
General area |
Enclose the source |
|
Dietetics |
Pot washer |
Automate process |
|
Housekeeping |
Burnishing |
Purchasing criteria |
|
Laundry |
Dryer/washer |
Isolate and reduce vibration |
|
Mailroom |
Tuberoom |
Purchasing criteria |
|
Maintenance |
Various equipment |
Purchasing criteria |
|
Materiel handling and |
Carts |
Maintenance |
|
Print shop |
Press operator |
Maintenance |
|
Rehabilitation |
Orthotics |
Purchasing criteria |
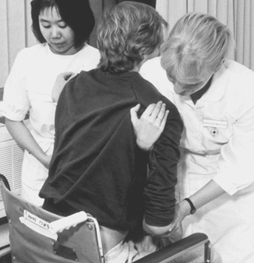
By far the most common and most costly type of injury faced by HCWs is back injury. Nurses and attendants are at greatest risk of musculoskeletal injuries due to the large amount of patient lifting and transferring that their jobs require. The epidemiology of back injury in nurses was summarized by Yassi et al. (1995a) with respect to one hospital. The pattern they observed mirrors those that have been universally reported. Hospitals are increasingly turning to preventive measures which may include staff training and the use of mechanical lifting devices. Many are also providing up-to-date diagnostic, therapeutic and rehabilitation health services that will minimize lost time and disability and are cost-effective (Yassi et al. 1995b). Hospital ergonomics has taken on increasing importance and, therefore, is the subject of a review article in this chapter. The specific problem of the prevention and management of back pain in nurses as one of the most important problems for this cohort of HCWs is also discussed in the article “Prevention and management of back pain in nurses” in this chapter. Table 4 lists the total number of injuries in a one-year period.
Table 4. Total number of injuries, mechanism of injury and nature of industry (one hospital, all departments), 1 April 1994 to 31 March 1995
|
Nature of injury sustained |
Total |
||||||||||||
|
Mechanism |
Blood/ |
Cut/ |
Bruise/ |
Sprain/ |
Fracture/ |
Burn/ |
Human |
Broken |
Head- |
Occupa- |
Other3 |
Un- |
|
|
Exertion |
|||||||||||||
|
Transferring |
105 |
105 |
|||||||||||
|
Lifting |
83 |
83 |
|||||||||||
|
Assisting |
4 |
4 |
|||||||||||
|
Turning |
27 |
27 |
|||||||||||
|
Breaking fall |
28 |
28 |
|||||||||||
|
Pushing |
1 |
25 |
26 |
||||||||||
|
Lifting |
1 |
52 |
1 |
54 |
|||||||||
|
Pulling |
14 |
14 |
|||||||||||
|
Combination- |
38 |
38 |
|||||||||||
|
Other |
74 |
74 |
|||||||||||
|
Fall |
3 |
45 |
67 |
3 |
1 |
119 |
|||||||
|
Struck/ |
66 |
76 |
5 |
2 |
2 |
1 |
152 |
||||||
|
Caught in/ |
13 |
68 |
8 |
1 |
1 |
91 |
|||||||
|
Exp. |
3 |
1 |
4 |
19 |
16 |
12 |
55 |
||||||
|
Staff abuse |
|||||||||||||
|
Patient |
16 |
11 |
51 |
28 |
8 |
3 |
1 |
2 |
120 |
||||
|
Spill/splashes |
80 |
1 |
81 |
||||||||||
|
Drug/ |
2 |
2 |
|||||||||||
|
Exp. |
5 |
5 |
10 |
||||||||||
|
Needlesticks |
159 |
22 |
181 |
||||||||||
|
Scalpel cuts |
34 |
14 |
48 |
||||||||||
|
Other5 |
3 |
1 |
29 |
1 |
6 |
40 |
|||||||
|
Unknown (no |
8 |
8 |
|||||||||||
|
Total |
289 |
136 |
243 |
558 |
5 |
33 |
8 |
7 |
19 |
25 |
29 |
8 |
1,360 |
1 No blood/body fluid. 2 This includes rashes/dermatitis/work-related illness/burning eyes, irritated eyes. 3 Exposure to chemical or physical agents but with no documented injuries affects. 4 Accident not reported. 5 Exposure to cold/heat, unknown.
In discussing musculoskeletal and ergonomic problems, it is important to note that while those engaged in direct patient care may be at greatest risk (see figure 5) many of the support personnel in hospital must contend with similar ergonomic burdens (see figure 6 and figure 7). The ergonomic problems facing hospital laundry workers have been well-documented (Wands and Yassi 1993) (see figure 8, figure 9 and figure 10) and they also are common among dentists, otologists, surgeons and especially microsurgeons, obstetricians, gynaecologists and other health personnel who often must work in awkward postures.
Figure 5. Patient lifting is an ergonomic hazard in most hospitals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 6. Overhead painting: A typical ergonomic hazard for a tradesworker
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 7. Cast-making involves many ergonomic stresses
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 8. Laundry work such as this can cause repetitive stress injury to the upper limbs
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 9. This laundry task requires working in an awkward position
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 10. A poorly designed laundry operation can cause back strain
Health Sciences Centre, Winnipeg, Manitoba, Canada
Organizational Problems
The article “Strain in health care work” contains a discussion of some of the organizational problems in hospitals and a summary of the principal findings of Leppanen and Olkinuora (1987), who reviewed Finnish and Swedish studies of stress among HCWs. With the rapid changes currently under way in this industry, the extent of alienation, frustration and burnout among HCWs is considerable. Added to that is the prevalence of staff abuse, an increasingly troublesome problem in many facilities (Yassi 1994). While it is often thought that the most difficult psychosocial problem faced by HCWs is dealing with death and dying, it is being recognized increasingly that the nature of the industry itself, with its hierarchical structure, its growing job insecurity and the high demands unsupported by adequate resources, is the cause of the variety of stress-related illness faced by HCWs.
The Nature of the Health Care Sector
In 1976, Stellman wrote, “If you ever wondered how people can manage to work with the sick and always stay healthy themselves, the answer is that they can’t” (Stellman 1976). The answer has not changed, but the potential hazards have clearly expanded from infectious diseases, back and other injuries, stress and burnout to include a large variety of potentially toxic environmental, physical and psychosocial exposures. The world of the HCW continues to be largely unmonitored and largely unregulated. None the less, progress is being made in addressing occupational health and safety hazards in hospitals. The International Commission on Occupational Health (ICOH) has a sub-committee addressing this problem, and several international conferences have been held with published proceedings that offer useful information (Hagberg et al. 1995). The US Centers for Disease Control and Prevention (CDC) and NIOSH have proposed guidelines to address many of the problems of the health care industry discussed in this article (e.g., see NIOSH 1988). The number of articles and books addressing health and safety issues for HCWs has been growing rapidly, and good overviews of health and safety in the US health care industry have been published (e.g., Charney 1994; Lewy 1990; Sterling 1994). The need for systematic data collection, study and analysis regarding hazards in the health care industry and the desirability of assembling interdisciplinary occupational health teams to address them have become increasingly evident.
When considering occupational health and safety in the health care industry, it is crucial to appreciate the enormous changes currently taking place in it. Health care “reform”, being instituted in most of the developed countries of the world, is creating extraordinary turbulence and uncertainty for HCWs, who are being asked to absorb rapid changes in their work tasks often with greater exposure to risks. The transformation of health care is spurred, in part, by advances in medical and scientific knowledge, the development of innovative technological procedures and the acquisition of new skills. It is also being driven, however, and perhaps to an even greater extent, by concepts of cost-effectiveness and organizational efficiency, in which “downsizing” and “cost control” have often seemed to become goals in themselves. New institutional incentives are being introduced at different organizational levels in different countries. The contracting out of jobs and services that had traditionally been carried out by a large stable workforce is now increasingly becoming the norm. Such contracting out of work is reported to have helped the health administrators and politicians achieve their long-term goal of making the process of health care more flexible and more accountable. These changes have also brought changes in roles that were previously rather well-defined, undermining the traditional hierarchical relationships among planners, administrators, physicians and other health professionals. The rise of investor-owned health care organizations in many countries has introduced a new dynamic in the financing and management of health services. In many situations, HCWs have been forced into new working relationships that involve such changes as downgrading services so that they can be performed by less-skilled workers at lower pay, reduced staffing levels, staff redeployments involving split shifts and part-time assignments. At the same time, there has been a slow but steady growth in the numbers of such physician surrogates as physician assistants, nurse practitioners, midwives and psychiatric social workers who command lower rates of pay than the physicians they are replacing. (The ultimate social and health costs both to HCWs and to the public, as patients and payers, is still to be determined.)
A growing trend in the US that is also emerging in the UK and northern European countries is “managed care”. This generally involves the creation of organizations paid on a per capita basis by insurance companies or government agencies to provide or contract for the provision of a comprehensive range of health services to a voluntarily-enrolled population of subscribers. Their aim is to reduce the costs of health care by “managing” the process: using administrative procedures and primary care physicians as “gatekeepers” to control the utilization of expensive in-patient hospital days, reducing referrals to high-priced specialists and use of costly diagnostic procedures, and denying coverage for expensive new forms of “experimental” treatment. The growing popularity of these managed care systems, fuelled by aggressive marketing to employer- and government-sponsored groups and individuals, has made it difficult for physicians and other health care providers to resist becoming involved. Once engaged, there is a variety of financial incentives and disincentives to influence their judgement and condition their behaviour. The loss of their traditional autonomy has been particularly painful for many medical practitioners and has had a profound influence on their patterns of practice and their relationships with other HCWs.
These rapid changes in the organization of the health care industry are having profound direct and indirect effects on the health and safety of HCWs. They affect the ways health services are organized, managed, delivered and paid for. They affect the ways HCWs are trained, assigned and supervised and the extent to which considerations of their health and safety are addressed. This should be kept in mind as the various occupational health hazards faced by HCWs are discussed in this chapter. Finally, although it may not appear to be directly relevant to the content of this chapter, thought should be given to the implications of the well-being and performance of HCWs to the quality and effectiveness of the services they provide to their patients.
Precarious Employment and Child Labour
The section of this article devoted to child labour is based largely on the report of the ILO Committee on Employment and Social Policy: Child Labour, GB.264/ESP/1, 264th Session, Geneva, November 1995
Throughout the world, not only in the developing but also in the industrialized countries, there are many millions of workers whose employment may be termed precarious from the standpoint of its potential effect on their health and well-being. They may be divided into a number of non-exclusive categories based on the kinds of work they perform and the types of relationship to their jobs and to their employers, such as the following:
- child labourers
- contract labourers
- enslaved and bonded workers
- informal sector workers
- migrant workers
- piece-workers
- unemployed and underemployed workers.
Their common denominators include: poverty; lack of education and training; exposure to exploitation and abuse; ill health and lack of adequate medical care; exposure to health and safety hazards; lack of protection by governmental agencies even where laws and regulations have been articulated; lack of social welfare benefits (e.g., minimum wages, unemployment insurance, health insurance and pensions); and lack of an effective voice in movements to improve their lot. In large part, their victimization stems from the poverty and the lack of education/training that force them to take whatever kind of work may be available. In some areas and in some industries, the existence of these classes of workers is fostered by explicit economic and social policies of the government or, even where they have been prohibited by local laws and/or endorsement of international Conventions, by the deliberate inattention of governmental regulatory agencies. The costs to these workers and their families in terms of ill-health, shortened life-expectancy and impact on well-being are imponderable; they often extend from one generation to the next. By any sort of measure, they may be considered disadvantaged.
The exploitation of labour is also one deleterious aspect of the global economy wherein the most dangerous and precarious work is transferred from the richer countries to the poorer ones. Thus, precarious employment can and should be viewed in macro-economic terms as well. This is discussed more fully elsewhere in this Encyclopaedia.
This article briefly summarizes the characteristics of the more important of these employment categories and their effects on workers’ health and well-being.
Migrant Workers
Migrant workers often represent a critically important segment of a country’s labour force. Some bring developed skills and professional competencies that are in short supply, particularly in areas of rapid industrial growth. Typically, however, they perform the unskilled and semi-skilled, low-paying jobs that are scorned by workers native to the area. These include “stooped labour” such as cultivating and harvesting crops, manual labour in the construction industry, menial services such as cleaning and refuse removal, and poorly remunerative repetitive jobs such as those in “sweatshops” in the apparel industry or on assembly-line work in light industries.
Some migrant workers find jobs in their own countries, but, more recently, they are for the most part “external” workers in that they come from another, usually less-developed country. Thus, they make unique contributions to the economy of two nations: by doing necessary work in the country in which they are working, and by their remittances of “hard” money to the families they leave behind in the country from which they came.
During the nineteenth century, large numbers of Chinese labourers were imported into the United States and Canada, for example, to work on the construction of the western portions of the transcontinental railroads. Later, during the Second World War, while American workers were serving in the armed forces or in the war industries, the United States reached a formal agreement with Mexico known as the Bracero Program (1942–1964) that provided millions of temporary Mexican workers for the vitally important agricultural industry. During the postwar period, “guest” workers from southern Europe, Turkey and North Africa helped to rebuild the war-ravaged countries of western Europe and, during the 1970s and 1980s, Saudi Arabia, Kuwait and the other newly rich oil-producing countries of the Near East imported Asians to build their new cities. During the early 1980s, external migrant workers accounted for approximately two-thirds of the workforces in the Arab Gulf states (citizen workers outnumbered the expatriates only in Bahrain).
Except for teachers and health workers, most of the migrants have been male. However, in most countries throughout these periods as families became wealthier, there has been an increasing demand for the importation of domestic workers, mostly women, to perform housework and provide care for infants and children (Anderson 1993). This has also been true in industrialized countries where increasing numbers of women were entering the workforce and needed household help to take up their traditional home-making activities.
Another example can be found in Africa. After the Republic of Transkei was created in 1976 as the first of the ten independent homelands called for in South Africa’s 1959 Promotion of Self-Government Act, migrant labour was its major export. Located on the Indian Ocean on the east coast of South Africa, it sent about 370,000 Xhosa males, its dominant ethnic group, as migrant workers to neighbouring South Africa, a number representing approximately 17% of its total population.
Some migrant workers have visas and temporary work permits, but these are often controlled by their employers. This means that they cannot change jobs or complain about mistreatment for fear that this will lead to revocation of their work permits and forced repatriation. Often, they evade the official immigration procedures of the host country and become “illegal” or “undocumented" workers. In some instances, migrant workers are recruited by labour “contractors” who charge exorbitant fees to smuggle them into the country to meet the needs of local employers. Fear of arrest and deportation, compounded by their unfamiliarity with the language, laws and customs of the host country, makes such workers particularly vulnerable to exploitation and abuse.
Migrant workers are frequently overworked, deprived of the benefit of proper tools and equipment, and often knowingly exposed to preventable health and safety hazards. Crowded, sub-standard housing (often lacking potable drinking water and basic sanitary facilities), malnutrition and the absence of access to medical care make them particularly subject to contagious diseases such as parasitic infections, hepatitis, tuberculosis and, more recently, AIDS. They are often underpaid or actually cheated of much of what they earn, especially when they are living illegally in a country and hence are denied basic legal rights. If apprehended by authorities, it is usually the “undocumented” migrant workers who are penalized rather than the employers and contractors who exploit them. Further, particularly during periods of economic downturn and rising unemployment, even documented migrant workers may be subject to deportation.
The International Labour Organization has for long been concerned with the problems of migrant workers. It first addressed them in its Migration for Employment Convention, 1949 (No. 97), and the related Recommendation No. 86, and revisited them in its Migrant Workers (Supplementary Provisions) Convention, 1975 (No. 143), and the related Recommendation No. 151. These Conventions, which have the force of treaties when ratified by countries, contain provisions aimed at eliminating abusive conditions and ensuring basic human rights and equal treatment for migrants. The recommendations provide non-binding guidelines to orient national policy and practice; Recommendation No. 86, for example, includes a model bilateral agreement that can be used by two countries as the basis for an operational agreement on the management of migrant labour.
In 1990, the United Nations adopted the International Convention on the Protection of the Rights of All Migrant Workers and Members of Their Families, which formulates basic human rights for migrant workers and their families, including: the right not to be subjected to torture or to cruel, inhuman or degrading treatment or punishment; the right to be treated no less favourably than national workers in respect to conditions of work and terms of employment; and the right to join unions and seek their assistance. This UN Convention will enter into force when it has been ratified by 20 nations; as of July 1995, it had been ratified by only five (Egypt, Colombia, Morocco, the Philippines and Seychelles) and it had been signed but not yet formally ratified by Chile and Mexico. It should be noted that neither the ILO nor the UN has any power to compel compliance with the Conventions other than collective political pressures, and must rely on the Member States to enforce them.
It has been observed that, at least in Asia, international dialogue on the matter of migrant workers has been hindered by its political sensitivity. Lim and Oishi (1996) note that countries exporting workers are fearful of losing their market share to others, especially since the recent global economic downturn has prompted more countries to enter the international market for migrant labour and to export their ‘‘cheap and docile’’ labour to a limited number of increasingly choosy host countries.
Piece-Workers
Piece-work is a compensation system that pays workers per unit of production accomplished. The unit of payment may be based on completion of the entire item or article or just one stage in its production. This system is generally applied in industries where the method of production consists of distinct, repetitive tasks whose performance can be credited to an individual worker. Thus, earnings are directly linked to the individual worker’s productivity (in some workplaces producing larger or more complicated items, such as automobiles, the workers are organized into teams which divide the per piece payment). Some employers share the rewards of greater productivity by supplementing the per piece payments with bonuses based on the profitability of the enterprise.
Piece-work is concentrated, by and large, in low-paying, light industries such as apparel and small assembly shops. It is also characteristic for sales people, independent contractors, repair personnel and others who are usually seen as different from shop workers.
The system can work well when employers are enlightened and concerned about workers’ health and welfare, and particularly where the workers are organized into a trade union in order to bargain collectively for rates of payment per unit, for appropriate and well-maintained tools and equipment, for a working environment where hazards are eliminated or controlled and personal protective equipment is provided when needed, and for pensions, health insurance and other such benefits. It is helped by the ready accessibility of managers or supervisors who are themselves skilled in the production process and can train or assist workers who may be having difficulty with it and who can help to maintain a high level of morale in the workplace by paying attention to workers’ concerns.
The piece-work system, however, readily lends itself to the exploitation of the workers, with adverse effects on their health and well-being, as in the following considerations:
- Piece-work is characteristic of the notorious sweatshops, unfortunately still common in the garment and electronic industries, where workers must toil at repetitive tasks, often for 12-hour days and 7-day weeks in sub-standard and hazardous workplaces.
- Even where the employer may manifest concern about potential occupational hazards—and this does not always occur—the pressure for productivity may leave little inclination for workers to devote what amounts to unpaid time to health and safety education. It may lead them to ignore or by-pass measures designed to control potential hazards, such as removing safety guards and shields. At the same time, employers have found that there may be a drop in the quality of the work, which dictates enhancement of product inspections to prevent defective merchandise from being passed along to the customers.
- The rate of pay may be so low that earning a living wage becomes difficult or nigh impossible.
- Piece-workers may be considered “temporary” workers and as such can be declared ineligible for benefits that may be mandatory for most workers.
- Less-skilled, slower workers may be denied training that would enable them to keep pace with those who can work faster, while employers may establish quotas based on what the best workers can produce and fire those unable to meet them. (In some workplaces, workers agree among themselves on production quotas that require the faster workers to slow down or stop working, thereby spreading the available work and the earnings more evenly among the work group.)
Contract Labour
Contract labour is a system in which a third party or organization contracts with employers to provide the services of workers when and where they are needed. They fall into three categories:
- Temporary workers are hired for a short period to fill in for employees who are absent because of illness or who are on leave, to augment the workforce when peaks in workload are not likely to be sustained, and when particular skills are needed only for a limited period.
- Leased workers are supplied on a more or less permanent basis to employers who, for a variety of reasons, do not wish to increase their workforces. These reasons include saving the effort and costs of personnel management and avoiding commitments such as rate of pay and the benefits won by the “regular” employees. In some instances, jobs have been eliminated in the course of a “downsizing” and the same people rehired as leased workers.
- Contract workers are groups of workers recruited by contractors and transported, sometimes for great distances and to other countries, to perform jobs that cannot be filled locally. These are usually low-paying, less desirable jobs involving hard physical labour or repetitive work. Some contractors recruit workers striving to improve their lots by emigrating to a new country and make them sign agreements committing them to work at the behest of the particular contractor until the often exorbitant transportation costs, fees and living expenses have been repaid.
One fundamental issue among the many possible problems with such arrangements, is whether the owner of the enterprise or the contractor supplying the workers is responsible for the safety, health and welfare of the workers. There is often “buck-passing”, in which each claims that the other is responsible for substandard working conditions (and, when the workers are migrants, living conditions) while the workers, who may be unfamiliar with the local language, laws and customs and too poor to obtain legal assistance, remain powerless to correct them. Contract workers are often exposed to physical and chemical hazards and are denied the education and training required to recognize and cope with them.
Informal Workers
The informal or “ undocumented” work sector includes workers who agree to work “off the books”—that is, without any formal registration or employer/employee arrangement. Payment may be in cash or in “in kind” goods or services and, since earnings are not reported to the authorities, they are not subject either to regulation or taxation for the worker and the employer. As a rule, there are no fringe benefits.
In many instances, informal work is done on an ad hoc, part-time basis, often while “moonlighting” during or after working hours on another job. It is also common among housekeepers and nannies who may be imported (sometimes illegally) from other countries where paid work is difficult to find. Many of these are required to “live in” and work long hours with very little time off. Since room and board may be considered part of their pay, their cash earnings may be very small. Finally, physical abuse and sexual harassment are not infrequent problems for these household workers (Anderson 1993).
The employer’s responsibility for the informal worker’s health and safety is only implicit, at best, and is often denied. Also, the worker is generally not eligible for workers’ compensation benefits in the event of a work-related accident or illness, and may be forced to take legal action when needed health services are not provided by the employer, a major undertaking for most of these individuals and not possible in all jurisdictions.
Slavery
Slavery is an arrangement in which one individual is regarded as an item of property, owned, exploited and dominated by another who can deny freedom of activity and movement, and who is obliged to provide only minimal food, shelter and clothing. Slaves may not marry and raise families without the owner’s permission, and may be sold or given away at will. Slaves may be required to perform any and all kinds of work without compensation and, short of the threat of impairing a valuable possession, with no concern for their health and safety.
Slavery has existed in every culture from the beginnings of human civilization as we know it down to the present. It was mentioned in the Sumerian legal codes recorded around 4,000 BC and in the Code of Hammurabi that was spelled out in ancient Babylon in the eighteenth century BC, and it exists today in parts of the world despite being prohibited by the UN’s 1945 Declaration of Human Rights and attacked and condemned by virtually every international organization including the UN Economic and Social Council, the Food and Agriculture Organization (FAO), the World Health Organization (WHO), and the ILO (Pinney 1993). Slaves have been employed in every kind of economy and, in some agricultural and manufacturing societies, have been the mainstay of production. In the slave-owning societies in the Middle East, Africa and China, slaves were employed primarily for personal and domestic services.
Slaves have traditionally been members of a different racial, ethnic, political or religious group from their owners. They were usually captured in wars or raids but, ever since the time of ancient Egypt, it has been possible for impoverished workers to sell themselves, or their wives and children, into bondage in order to pay off debts (ILO 1993b).
Unemployment and Employment Opportunity
In every country and in every type of economy there are workers who are unemployed (defined as those who are able and willing to work and who are seeking a job). Periods of unemployment are a regular feature of some industries in which the labour force expands and contracts in accord with the seasons (e.g., agriculture, construction and the apparel industry) and in cyclical industries in which workers are laid off when business declines and are rehired when it improves. Also, a certain level of turnover is characteristic of the labour market as employees leave one job to seek a better one and as young people enter the workforce replacing those who are retiring. This has been labelled frictional unemployment.
Structural unemployment occurs when whole industries decline as a result of technological advances (e.g., mining and the manufacture of steel) or in response to gross changes in the local economy. An example of the latter is the moving of manufacturing plants from an area where wages have become high to less developed areas where cheaper labour is available.
Structural unemployment, during recent decades, has also resulted from the spate of mergers, takeovers and restructurings of large enterprises that have been a common phenomenon, particularly in the United States which has far fewer mandated safeguards for worker and community well-being than do other industrialized countries. These have led to “downsizing” and shrinkage of their workforces as duplicative plants and offices have been eliminated and many jobs declared unnecessary. This has been damaging not only to those who lost their jobs but also to those who remained and were left with a loss of job security and a fear of being declared redundant.
Structural unemployment is often intractable as many workers lack the skill and flexibility to qualify for other jobs at a comparable level that may be available locally, and they often lack the resources to migrate to other areas where such jobs may be available.
When sizeable layoffs occur, there is often a “domino” effect on the community. The loss of earnings has a dampening effect on the local economy, causing the closing of shops and service enterprises frequented by the unemployed and, thereby, increasing their number.
The economic and mental stress resulting from unemployment often has significant adverse effects on the health of the workers and their families. Loss of job and, particularly, threats of job loss, have been found to be the most potent work-related stressors and have been shown to have precipitated emotional illnesses (this is discussed elsewhere in this Encyclopaedia). To prevent such adverse effects, some employers offer retraining and assistance in finding new jobs, and many countries have laws that place specific economic and social requirements on employers to provide financial and social benefits to the affected employees.
The underemployed comprise workers whose productive capacities are not fully utilized. They include part-time workers who are seeking full-time jobs, and those with higher levels of skill who can find only relatively unskilled work. In addition to lower earnings, they suffer the adverse effects of the stress of dissatisfaction with the job.
Child Labour
In most families, as soon as they are old enough to contribute, children are expected to work. This may involve helping with housekeeping chores, running errands or caring for younger siblings—in general, helping with the traditional homemaking responsibilities. In farming families or those engaged in some form of home industry, children are usually expected to help with tasks suited to their size and capabilities. These activities are almost invariably part-time, and often seasonal. Except in families where the children may be abused or exploited, this work is defined by the size and “values” of the particular family; it is unpaid and it usually does not interfere with nurturing, education and training. This article does not address such work. Rather, it focuses on children under the age of 14 who work outside the family framework in one industry or another, usually in defiance of laws and regulations governing the employment of children.
Although only sparse data are available, the ILO Bureau of Statistics has estimated that “in the developing countries alone, there are at least 120 million children between the ages of 5 and 14 who are fully at work, and more than twice as many (or about 250 million) if those for whom work is a secondary activity are included” (ILO 1996).
Earlier figures are thought to be grossly understated, as demonstrated by the much higher numbers yielded by independent surveys carried out in several countries in 1993–1994. For example, in Ghana, India, Indonesia and Senegal, approximately 25% of all children were engaged in some form of economic activity. For one-third of these children, work was their principal activity.
Child labour is found everywhere, although it is much more prevalent in poor and developing areas. It disproportionately involves girls who are not only likely to work for longer hours but, like older women, are also required to perform homemaking and housekeeping tasks to a much greater extent than their male counterparts. Children in rural areas are, on average, twice as likely to be economically active; among migrant farmworker families, it is almost the rule that all of the children work alongside their parents. However, the proportion of urban children who work is increasing steadily, mainly in the informal sector of the economy. Most urban children work in domestic services, although many are employed in manufacturing. While public attention has been focused on a few export industries such as textiles, clothing, footwear and carpets, the great majority work in jobs geared towards domestic consumption. On the whole, however, child labour remains more common on plantations than in manufacturing.
Child slavery
Many child workers are slaves. That is, the employer exercises the right of either temporary or permanent ownership in which the children have become “commodities” that can be rented out or exchanged. Traditional in South Asia, the sub-Saharan strip of East Africa and, more recently, in several South American countries, it appears to be evolving all over the world. Despite the facts that it is illegal in most countries where it exists and that the international Conventions banning it have been widely ratified, the ILO estimated (accurate data are not available) that there are tens of millions of child slaves around the world (ILO 1995). Large numbers of child slaves are to be found in agriculture, domestic service, the sex industry, the carpet and textile industries, quarrying and brick-making.
According to the report of an ILO Committee of Experts (ILO 1990), more than 30 million children are thought to be in slavery or bondage in several countries. The report cited, among others, India, Ghana, Gaza, Pakistan, Philippines, Dominican Republic, Haiti, Brazil, Peru, Mauritania, South Africa and Thailand. More than 10 million of them are concentrated in India and Pakistan. Common sites of employment for enslaved children are small workshops and as forced labour on plantations. In the informal sector they can be found in carpet weaving, match factories, glass factories, brick making, fish cleaning, mines and quarries. Children are also used as enslaved domestic labourers, as slave-prostitutes and drug carriers.
Child slavery predominates mainly where there are social systems that are based on the exploitation of poverty. Families sell the children outright or bond them into slavery in order to pay off debts or simply provide the wherewithal to survive, or to supply the means to meet social or religious obligations. In many instances, the payment is considered an advance against the wages the child slaves are expected to earn during their indenture. Wars and the forced migrations of large populations which disrupt the normal family structure force many children and adolescents into slavery.
Causes of child labour
Poverty is the greatest single factor responsible for the movement of children into the workplace. The survival of the family as well as the children themselves often dictates it; this is particularly the case when poor families have many children. The necessity of having them work full-time makes it impossible for families to invest in the children’s education.
Even where tuition is free, many poor families are unable to meet the ancillary costs of education (e.g., books and other school supplies, clothing and footwear, transportation and so on). In some places, these costs for one child attending a primary school may represent as much as one-third of the cash income of a typical poor family. This leaves going to work as the only alternative. In some large families, the older children will work to provide the means for educating their younger siblings.
In some areas, it is not so much the cost but the lack of schools providing an acceptable quality of education. In some communities, schools may just be unavailable. In others, children drop out because the schools serving the poor are of such abysmal quality that attendance does not seem to be worth the cost and effort involved. Thus, while many children drop out of school because they have to work, many become so discouraged that they prefer to work. As a result, they may remain totally or functionally illiterate and unable to develop the skills required for their advancement in the world of work and in society.
Finally, many large urban centres have developed an indigenous population of street children who have been orphaned or separated from their families. These scratch out a precarious existence by doing odd jobs, begging, stealing, and participating in the traffic of illegal drugs.
The demand for child labour
In most instances, children are employed because their labour is less expensive and they are less troublesome than adult workers. In Ghana, for example, an ILO-supported study showed that three-fourths of children engaged in paid work were paid less than one-sixth of the statutory minimum wage (ILO 1995). In other areas, although the differentials between the wages of children and adults were much less impressive, they were large enough to represent a very significant burden to the employers, who were usually poor, small contractors who enjoyed a very slim profit margin.
In some instances, as in the hand-woven carpet and glass bracelet (bangles) industries in India, child workers are preferred to adults because of their smaller size or the perception that their “nimble fingers” make for greater manual dexterity. An ILO study demonstrated that adults were no less competent in performing these tasks and that the child workers were not irreplaceable (Levison et al. 1995).
Parents are a major source of demand for the work of children in their own families. Huge numbers of children are unpaid workers in family farms, shops and stores that depend on family labour for their economic viability. It is conventionally assumed that these children are much less likely to be exploited than those working outside the family, but there is ample evidence that this is not always the case.
Finally, in urban areas in developed countries where the labour market is very tight, adolescents may be the only workers available and willing to take the minimum wage, mostly part-time jobs in retail establishments such as fast-food shops, retail trade and messenger services. Recently, where even these have not been available in sufficient numbers, employers have been recruiting elderly retirees for these positions.
Working conditions
In many establishments employing child labour, working conditions range from bad to abysmal. Since many of these enterprises are poor and marginal to start with, and are often operating illegally, little or no attention is paid to amenities that would be required to retain all but slave labourers. Lack of elementary sanitation, air quality, potable water and food are often compounded by crowding, harsh discipline, obsolete equipment, poor quality tools and the absence of protective measures to control exposure to occupational hazards. Even where some protective equipment may be available, it is rarely sized to fit the smaller frames of children and is often poorly maintained.
Too many children work too many hours. Dawn to dusk is not an unusual working day, and the need for rest periods and holidays is generally ignored. In addition to chronic fatigue, which is a major cause of accidents, the most damaging effect of the long hours is the inability to benefit from education. This may occur even where the children work only part-time; studies have shown that working more than 20 hours per week can negatively affect education (ILO 1995). Functional illiteracy and lack of training, in turn, lead to greatly diminished opportunities for advancing to improved employment.
Girls are particularly at risk. Because they are often also responsible for household tasks, they work longer hours than boys, who usually engage only in economic activities. As a result, they generally have lower rates of school attendance and completion.
Children are emotionally immature and need a nurturing psychological and social environment that will socialize them into their cultural environment and enable them to take their places as adults in their particular society. For many labouring children, the work environment is oppressive; in essence, they do not have a childhood.
Prevention of Injuries to Children
Child labour is not restricted to developing countries. The following set of precautions is adapted from advice put forth by the United States Centers for Disease Control and Prevention.
The risks for work-related injuries and illnesses in children, as in workers of all ages, can be reduced through adherence to routine precautions such as: prescribed housekeeping practices; training and safe work procedures; use of proper shoes, gloves and protective clothing; and maintenance and use of equipment with safety features. In addition, workers under the age of 18 should not be required to lift objects weighing more than 15 pounds (approximately 7kg) more than once per minute, or ever to lift objects weighing more than 30 pounds (14kg); tasks involving continuous lifting should never last more than 2 hours. Children under the age of 18 should not participate in work requiring the routine use of respirators as a means of preventing the inhalation of hazardous substances.
Employers should be knowledgeable about and comply with child labour laws. School counsellors and physicians who sign permits allowing children to work should be familiar with child labour laws and ensure that the work they approve does not involve prohibited activities.
Most children who begin working under the age of 18 enter the workplace with minimal prior experience for a job. Advanced industrial countries are not exempt from these hazards. For example, during the summer of 1992 in the United States, more than half (54%) of persons aged 14 to 16 years treated in emergency departments for work injuries reported that they had received no training in prevention of the injury they had sustained, and that a supervisor was present at the time of injury in only approximately 20% of the cases. Differences in maturity and developmental level regarding learning styles, judgement and behaviour should be considered when providing training for youth in occupational safety and health.
Centers for Disease Control and Prevention, 1996
Exposure to occupational hazards
In general, the risks that children face in the workplace are the same that adult workers encounter. However, their effects may be greater because of the kinds of tasks to which children are assigned and the biological differences between children and adults.
Children tend to be given more menial tasks, often without instruction and training in minimizing exposure to the hazards that may be encountered, and without proper supervision. They may be assigned to cleaning-up duties, often using solvents or strong alkalis, or they may be required to clean up hazardous wastes that have accumulated in the workplace without awareness of potential toxicity.
Because of their smaller size, children are more likely to be given tasks that require working in odd, confined places or long periods of stooping or kneeling. Often, they are required to handle objects that even adults would consider too bulky or too heavy.
Because of their continuing growth and development, children differ biologically from adults. These differences have not been quantified, but it is reasonable to assume that the more rapid cell division involved in the growth process may make them more vulnerable to many toxic agents. Exposure earlier in life to toxic agents with long latency periods may result in the onset of disabling chronic occupational diseases such as asbestosis and cancer in young adulthood rather than at older ages, and there is evidence that childhood exposure to toxic chemicals may alter the response to future toxic exposures (Weisburger et al. 1966).
Table 1 summarizes information on some of the hazardous agents to which working children may be exposed, according to the sources of exposure and the types of health consequences. It should be noted that these consequences may be aggravated when the exposed children are undernourished, anaemic or suffer from chronic diseases. Finally, the lack of primary medical care, much less the services of health professionals with some sophistication in occupational health, means that these health consequences are not likely to be recognized promptly or treated effectively.
Table 1. Some occupations and industries, and their associated hazards, where children are employed.
|
Occupation/industry |
Hazards |
|
Abattoirs and meat rendering |
Injuries from cuts, burns, falls, dangerous equipment; exposure to infectious disease; heat stress |
|
Agriculture |
Unsafe machinery; hazardous substances; accidents; chemical poisoning; arduous work; dangerous animals, insects and reptiles |
|
Alcohol production and/or sale |
Intoxication, addiction; environment may be prejudicial to morals; risk of violence |
|
Carpet-weaving |
Dust inhalation, poor lighting, poor posture (squatting); respiratory and musculoskeletal diseases; eye strain; chemical poisoning |
|
Cement |
Harmful chemicals, exposure to harmful dust; arduous work; respiratory and musculoskeletal disease |
|
Construction and/or demolition |
Exposure to heat, cold, dust; falling objects; sharp objects; accidents; musculoskeletal diseases |
|
Cranes/hoists/lifting machinery Tar, asphalt, bitumen |
Accidents; falling objects; musculoskeletal diseases; risk of injury to others Exposure to heat, burns; chemical poisoning; respiratory diseases |
|
Crystal and/or glass manufacture |
Molten glass; extreme heat; poor ventilation; cuts from broken glass; carrying hot glass; burns; respiratory disease; heat stress; toxic dust |
|
Domestic service |
Long hours; physical, emotional, sexual abuse; malnutrition; insufficient rest; isolation |
|
Electricity |
Dangerous work with high voltage; risk of falling; high level of responsibility for safety of others |
|
Entertainment (night clubs, bars, casinos, circuses, gambling halls) |
Long, late hours; sexual abuse; exploitation; prejudicial to morals |
|
Explosives (manufacture and handling) |
Risk of explosion, fire, burns, mortal danger |
|
Hospitals and work with risk of infection |
Infectious diseases; responsibility for well-being of others |
|
Lead/zinc metallurgy |
Cumulative poisoning; neurological damage |
|
Machinery in motion (operation, cleaning, repairs, etc.) |
Danger from moving engine parts; accidents; cuts, burns, exposure to heat and noise; noise stress; eye and ear injuries |
|
Maritime work (trimmers and stokers, stevedores) |
Accidents; heat, burns; falls from heights; heavy lifting, arduous work, musculoskeletal diseases; respiratory diseases |
|
Mining, quarries, underground work |
Exposure to dusts, gases, fumes, dirty conditions; respiratory and musculoskeletal diseases; accidents; falling objects; arduous work; heavy loads |
|
Rubber |
Heat, burns, chemical poisoning |
|
Street trades |
Exposure to drugs, violence, criminal activities; heavy loads; musculoskeletal diseases; venereal diseases; accidents |
|
Tanneries |
Chemical poisoning; sharp instruments; respiratory diseases |
|
Transportation, operating vehicles |
Accidents; danger to self and passengers |
|
Underwater (e.g., pearl diving) |
Decompression illness; dangerous fish; death or injury |
|
Welding and smelting of metals, metalworking |
Exposure to extreme heat; flying sparks and hot metal objects; accidents; eye injuries; heat stress |
Source: Sinclair and Trah 1991.
Social and economic consequences of child labour
Child labour is largely generated by poverty, as noted above, and child labour tends to perpetuate poverty. When child labour precludes or seriously handicaps education, lifetime earnings are reduced and upward social mobility is retarded. Work that hampers the physical, mental and social development ultimately taxes the health and welfare resources of the community and perpetuates poverty by degrading the stock of human capital needed for the economic and social development of the society. Since the societal costs of child labour are visited primarily on the population groups that already are poor and less privileged, access to democracy and social justice is eroded and social unrest is fomented.
Future trends
Although much is being done to eliminate child labour, it is clearly not enough nor is it effective enough. What is needed first is more and better information about the extent, dynamics and effects of child labour. The next step is to increase, amplify and improve educational and training opportunities for children from pre-school through universities and technical institutes, and then to provide the means for children of the poor to take advantage of them (e.g., adequate housing, nutrition and preventive health care).
Well-drafted legislation and regulations, reinforced by such international efforts as the ILO Conventions, need constantly to be revised and strengthened in the light of current developments in child labour, while the effectiveness of their enforcement should be enhanced.
The ultimate weapon may be the nurturing of greater awareness and abhorrence of child labour among the general public, which we are beginning to see in several industrialized countries (motivated in part by adult unemployment and the price competition that drives producers of consumer goods to migrate to areas where labour may be cheaper). The resultant publicity is leading to damage to the image of organizations marketing products produced by child labour, protests by their stockholders and, most important, refusal to purchase these products even though they may cost a bit less.
Conclusions
There are many forms of employment in which workers are vulnerable to impoverishment, exploitation and abuse, and where their safety, health and well-being are at great risk. Despite attempts at legislation and regulation, and notwithstanding their condemnation in international agreements, Conventions, and resolutions, such conditions are likely to persist as long as people are poor, ill-housed, malnourished and oppressed, and are denied the information, education and training and the curative and preventive health services required to enable them to extricate themselves from the social quicksand in which they exist. Wealthy people and nations often respond magnanimously to such natural disasters as storms, floods, fires, volcanic eruptions and earthquakes but, important as they are, the benefits of such help are short-lived. What is needed is a long-term application of human effort fortified by the needed resources that will overcome the political, racial and religious barriers that would thwart its thrust.
Finally, while it is entirely appropriate and healthy for children to work as part of normal development and family life, child labour as described in this article is a scourge that not only damages the health and well-being of the child workers but, in the long run, also impairs the social and economic security of communities and nations. It must be attacked with vigour and persistence until it is eradicated.
Pregnancy and US Work Recommendations
Changes in family life over recent decades have had dramatic effects on the relationship between work and pregnancy. These include the following:
- Women, particularly those of childbearing age, continue to enter the labour force in considerable numbers.
- A tendency has developed on the part of many of these women to defer starting their families until they are older, by which time they have often achieved positions of responsibility and become important members of the productive apparatus.
- At the same time, there is an increasing number of teenage pregnancies, many of which are high-risk pregnancies.
- Reflecting increasing rates of separation, of divorce and of choices of alternative lifestyles, as well as an increase in the number of families in which both parents must work, financial pressures are forcing many women to continue working for as long as possible during pregnancy.
The impact of pregnancy-related absences and lost or impaired productivity, as well as concern over the health and well-being of both the mothers and their infants, have led employers to become more proactive in dealing with the problem of pregnancy and work. Where employers pay all or part of health insurance premiums, the prospect of avoiding the sometimes staggering costs of complicated pregnancies and neonatal problems is a potent incentive. Certain responses are dictated by laws and government regulations, for example, guarding against potential occupational and environmental hazards and providing maternity leave and other benefits. Others are voluntary: prenatal education and care programmers, modified work arrangements such as flex-time and other work schedule arrangements, dependant care and other benefits.
Management of pregnancy
Of primary importance to the pregnant woman—and to her employer—whether or not she continues working during her pregnancy, is access to a professional health management programme designed to identify and avert or minimize risks to the mother and her foetus, thus enabling her to remain on the job without concern. At each of the scheduled prenatal visits, the physician or midwife should evaluate medical information (childbearing and other medical history, current complaints, physical examinations and laboratory tests) and information about her job and work environment, and develop appropriate recommendations.
It is important that health professionals not rely on the simple job descriptions pertaining to their patients’ work, as these are often inaccurate and misleading. The job information should include details concerning physical activity, chemical and other exposures and emotional stress, most of which can be provided by the woman herself. In some instances, however, input from a supervisor, often relayed by the safety department or the employee health service (where there is one), may be needed to provide a more complete picture of hazardous or trying work activities and the possibility of controlling their potential for harm. This can also serve as a check on patients who inadvertently or deliberately mislead their physicians; they may exaggerate the risks or, if they feel it is important to continue working, may understate them.
Recommendations for Work
Recommendations regarding work during pregnancy fall into three categories:
The woman may continue to work without changes in her activities or the environment. This is applicable in most instances. After extensive deliberation, the Task Force on the Disability of pregnancy comprising obstetrical health professionals, occupational physicians and nurses, and women’s representatives assembled by ACOG (the American College of Obstetricians and Gynecologists) and NIOSH (the National Institute for Occupational Safety and Health) concluded that “the normal woman with an uncomplicated pregnancy who is in a job that presents no greater hazards than those encountered in normal daily life in the community, may continue to work without interruption until the onset of labor and may resume working several weeks after an uncomplicated delivery” (Isenman and Warshaw, 1977).
The woman may continue to work, but only with certain modifications in the work environment or her work activities. These modifications would be either “desirable” or “essential” (in the latter case, she should stop work if they cannot be made).
The woman should not work. It is the physician’s or midwife’s judgement that any work would probably be detrimental to her health or to that of the developing foetus.
The recommendations should not only detail the needed job modifications but should also stipulate the length of time they should be in effect and indicate the date for the next professional examination.
Non-medical Considerations
The recommendations suggested above are based entirely on considerations of the health of the mother and her foetus in relation to job requirements. They do not take into account the burden of such off-the-job activities as commuting to and from the workplace, housework and care of other children and family members; these may sometimes be even more demanding than those of the job. When modification or restriction of activities is called for, one should consider the question whether it should be implemented on the job, in the home or both.
In addition, recommendations for or against continuing work may form the basis of a variety of non-medical considerations, for example, eligibility for benefits, paid versus unpaid leave or guaranteed job retention. A critical issue is whether the woman is considered disabled. Some employers categorically consider all pregnant workers to be disabled and strive to eliminate them from the workforce, even though many are able to continue to work. Other employers assume that all pregnant employees tend to magnify any disability in order to be eligible for all available benefits. And some even challenge the notion that a pregnancy, whether or not it is disabling, is a matter for them to be concerned about at all. Thus, disability is a complex concept which, although fundamentally based on medical findings, involves legal and social considerations.
Pregnancy and Disability
In many jurisdictions, it is important to distinguish between the disability of pregnancy and pregnancy as a period in life that calls for special benefits and dispensations. The disability of pregnancy falls into three categories:
- Disability following delivery. From a purely medical standpoint, recovery following the termination of pregnancy through an uncomplicated delivery lasts only a few weeks, but conventionally it extends to six or eight weeks because that is when most obstetricians customarily schedule their first postnatal check-up. However, from a practical and sociological point of view, a longer leave is considered by many to be desirable in order to enhance family bonding, to facilitate breast-feeding, and so on.
- Disability resulting from medical complications. Medical complications such as eclamsia, threatened abortion, cardiovascular or renal problems and so on, will dictate periods of reduced activity or even hospitalization that will last as long as the medical condition persists or until the woman has recovered from both the medical problem and the pregnancy.
- Disability reflecting the necessity of avoiding exposure to toxicity hazards or abnormal physical stress. Because of the greater sensitivity of the foetus to many environmental hazards, the pregnant woman may be considered disabled even though her own health might not be in danger of being compromised.
Conclusion
The challenge of balancing family responsibilities and work outside the home is not new to women. What may be new is a modern society that values the health and well-being of women and their offspring while confronting women with the dual challenges of achieving personal fulfillment through employment and coping with the economic pressures of maintaining an acceptable standard of living. The increasing number of single parents and of married couples both of whom must work suggest that work-family issues cannot be ignored. Many employed women who become pregnant simply must continue to work.
Whose responsibility is it to meet the needs of these individuals? Some would argue that it is purely a personal problem to be dealt with entirely by the individual or the family. Others consider it a societal responsibility and would enact laws and provide financial and other benefits on a community-wide basis.
How much should be loaded on the employer? This depends largely on the nature, the location and often the size of the organization. The employer is driven by two sets of considerations: those imposed by laws and regulations (and sometimes by the need to meet demands won by organized labour) and those dictated by social responsibility and the practical necessity of maintaining optimal productivity. In the last analysis, it hinges on lacing a high value on human resources and acknowledging the interdependence of work responsibilities and family commitments and their sometimes counterbalancing effects on health and productivity.
Occupational Health Services in Small-Scale Enterprises
The coverage of workers in small-scale enterprises (SSEs) is perhaps the most daunting challenge to systems for delivering occupational health services. In most countries, SSEs comprise the vast majority of the business and industrial undertakings—reaching as high as 90% in some of the developing and newly industrialized countries—and they are found in every sector of the economy. They employ on average nearly 40% of the workforce in the industrialized countries belonging to the Organization for Economic Cooperation and Development and up to 60% of the workforce in developing and newly industrialized countries. Although their workers are exposed to perhaps an even greater range of hazards than their counterparts in large enterprises (Reverente 1992; Hasle et al. 1986), they usually have little if any access to modern occupational health and safety services.
Defining Small-Scale Enterprises
Enterprises are categorized as small-scale on the basis of such characteristics as the size of their capital investment, the amount of their annual revenues or the number of their employees. Depending on the context, the number for the last category has ranged from one to 500 employees. In this article, the term SSE will be applied to enterprises having 50 or fewer employees, the most widely accepted definition (ILO 1986).
SSEs are gaining importance in national economies. They are employment-intensive, flexible in adapting to rapidly changing market situations, and provide job opportunities for many who would otherwise be unemployed. Their capital requirements are often low and they can produce goods and services near the consumer or client.
They also present disadvantages. Their lifetime is often brief, making their activities difficult to monitor and, frequently, their small margins of profits are achieved only at the expense of their workers (who are often also their owners) in terms of hours and intensity of workloads and exposure to occupational health risks.
The Workforce of SSEs
The workforce of SSEs is characterized by its diversity. In many instances, it comprises the manager as well as members of his or her family. SSEs provide entry to the world of work for young people and meaningful activities to elderly and redundant workers who have been separated from larger enterprises. As a result, they often expose such vulnerable groups as children, pregnant women and the elderly to occupational health risks. Further, since many SSEs are carried out in or near the home, they often expose family members and neighbours to the physical and chemical hazards of their workplaces and present public health problems through contamination of air or water or of food grown near the premises.
The educational level and socio-economic status of SSE workers vary widely but are often lower than the averages for the entire workforce. Of particular relevance is the fact that their owners/managers may have had little training in operation and management and even less in the recognition, prevention and control of occupational health risks. Even where appropriate educational resources are made available, they often lack the time, energy and financial resources to make use of them.
Occupational Hazards in SSEs and the Health Statusof their Workers
Like all other aspects of SSEs, their working conditions vary widely depending on the general nature of the enterprise, the type of production, the ownership and location. In general, the occupational health and safety hazards are much the same as those encountered in larger enterprises, but as noted above, the exposures to them are often substantially higher than in large enterprises. Occasionally, however, the working conditions in SSEs may be much better than those in larger enterprises with a similar type of production (Paoli 1992).
Although very few studies have been reported, it is not surprising that surveys of the health of workers in SSEs in such industrialized countries as Finland (Huuskonen and Rantala 1985) and Germany (Hauss 1992) have disclosed a relatively high incidence of health problems, many of which were associated with lowered capacity for work and/or were work-related in origin. In SSEs in developing countries an even higher prevalence of occupational diseases and work-related health problems has been reported (Reverente 1992).
Barriers to Occupational Health Services for SSEs
There are formidable structural, economic and psychological barriers to the provision of occupational health services to SSEs. They include the following:
- Traditionally, occupational safety and health legislation in most countries has exempted SSEs and is generally applicable only to manufacturing industries. The “informal sector” (this would include, say, the self-employed) and agriculture were not covered. Even where the legislation had wider coverage, it was not applicable to enterprises with small numbers of employees—500 employees was the usual lower limit. Re-cently, some countries (e.g., France, Belgium and the Nordic countries) have enacted legislation requiring the provision of occupational health service for all enterprises regardless of size or sector of the economy (Rantanen 1990).
- SSEs, as defined for this article, are too small to justify an in-plant occupational health service. Their wide diversity with respect to type of industry and methods of production as well as style of organization and operation, along with the fact that they are spread over wide geographic areas, makes it difficult to organize occupational health services that will meet all their needs.
- Economic barriers are substantial. Many SSEs hover on the edge of survival and just cannot afford any additions to their operating costs even though they may promise significant savings in the future. Further, they may not be able to afford education and training in hazard recognition, prevention and control for their owners/managers, much less their employees. Some countries have addressed the economic problem by providing subsidies either from governmental agencies or social security institutions (Rantanen 1994), or have included occupational health services in programmes promoting the general economic and social development of SSEs (Kogi, Phoon and Thurman 1988).
- Even when financial constraints are not inhibiting, there is often a disinclination among the owners/managers of SSEs to devote the time and energy needed to acquire the necessary basic understanding of the relationships between work and health. Once acquired, however, SSEs may be very successful in applying the information and abilities in their workplaces (Niemi and Notkola 1991; Niemi et al. 1991).
- Enterprises in the informal sector and small farming are seldom registered, and their formal links with official agencies may be weak or non-existent. Activities carried out as a business may be difficult to distinguish from those involving the private household and family. As a result, there may be concerns about privacy and resistance to interventions by “outsiders”. SSEs often resist becoming involved in trade associations and community organizations, and in perhaps the majority of instances their employees are not members of unions. To overcome such barriers, some countries have used extension organizations for the distribution of information, the creation of special training opportunities for the SSEs by official occupational safety and health agencies, and the adoption of the primary care model for the provision of occupational health services (Jeyaratnam 1992).
- Many SSEs are located in communities providing ready access to emergency and primary care services. However, the physicians’ and nurses’ lack of knowledge and experience with respect to occupational hazards and their effects often results in failure to recognize occupational diseases and, probably more important, loss of opportunities to install the necessary prevention and control measures.
International Instruments Covering OccupationalSafety and Health Services
In some countries, occupational safety and health activities are in the jurisdiction of labour ministries and are regulated by a special occupational safety and health authority; in others, this responsibility is shared by their ministries of labour, health and/or social affairs. In some countries, such as Italy, regulations covering occupational health services are embodied in health legislation or, as in Finland, in a special act. In the United States and in England, provision of occupational health services rests on a voluntary basis, while in Sweden, among others, it was once regulated by collective agreement.
The ILO Occupational Safety and Health Convention (No. 155) (ILO 1981a) requires governments to organize a policy for occupational safety and health to be applicable to all enterprises in all sectors of the economy that is to be implemented by a competent authority. This Convention stipulates the responsibilities of the authorities, employers and workers and, supplemented by the concomitant Recommendation No. 164, defines the key occupational safety and health activities of all relevant actors at both national and local levels.
The ILO supplemented these in 1985 by the International Convention No. 161 and Recommendation No. 171 on Occupational Health Services. These contain provisions on policy design, administration, inspection and collaboration of occupational health services, activities by occupational safety and health teams, conditions of operation, and responsibilities of employers and workers, and they furthermore offer guidelines for organizing occupational health services at the level of the enterprise. While they do not specify SSEs, they were developed with these in mind since no size limits were set for occupational health services and the necessary flexibility in their organization was emphasized.
Unfortunately, ratification of these ILO instruments has been limited, particularly in developing countries. On the basis of experience from the industrialized countries, it is likely that without special actions and support by government authorities, the implementation of the ILO principles will not take place in SSEs.
The WHO has been active in promoting the development of occupational health services. Examination of the legal requirements was carried out in a consultation in 1989 (WHO 1989a), and a series of about 20 technical documents on various aspects of occupational health services has been published by WHO headquarters. In 1985 and again in 1992, the WHO Regional Office in Europe carried out and reported surveys of occupational health services in Europe, while the Pan American Health Organization designated 1992 as a special year for occupational health by promoting occupational health activities in general and conducting a special programme in Central and South America.
The European Union has issued 16 directives concerning occupational safety and health, the most important of which is Directive 391/1989, which has been called the “Framework Directive” (CEC 1989). These contain provisions for specific measures such as requiring employers to organize health risk assessments of different technical facilities or to provide health examinations of workers exposed to special hazards. They also cover the protection of workers against physical, chemical and biological hazards including the handling of heavy loads and working at video display units.
While all of these international instruments and efforts were developed with SSEs in mind, the fact is that most of their provisions are practical only for larger enterprises. Effective models for organizing a similar level of occupational health services for SSEs remain to be developed.
Organizing Occupational Health Services for SSEs
As noted above, their small size, geographic dispersion and wide variation in types and conditions of work, coupled with great limitations in economic and human resources, make it difficult to efficiently organize occupational health services for SSEs. Only a few of the various models for delivering occupational health services described in detail in this chapter are adaptable to SSEs.
Perhaps the only exceptions are SSEs that are dispersed operating units of large enterprises. These usually are governed by policies established for the entire organization, participate in company-wide educational and training activities, and have access to a multidisciplinary team of specialists in occupational health located in a central occupational health service that is usually based at the headquarters of the enterprise. A major factor in the success of this model is having all of the costs of occupational safety and health activities covered by the central occupational health unit or the general corporate budget. When, as is increasingly common, the costs are allocated to the operating budget of the SSE, there may be difficulty in enlisting the full cooperation of its local manager, whose performance may be judged on the basis of the profitability of that particular enterprise.
Group services organized jointly by several small or medium-sized enterprises have been successfully implemented in several European countries—Finland, Sweden, Norway, Denmark, the Netherlands and France. In some other countries they have been experimented with, with the help of government subsidies or private foundations, but they have not survived after termination of subsidies.
An interesting modification of the group service model is the branch-oriented service, which provides services for a high number of enterprises operating all in the same type of industry, such as construction, forestry, agriculture, food industry and so on. The model enables the service units to specialize in the problems typical for the branch and thus accumulate high competence in the sector that they serve. A famous example of such a model is the Swedish Bygghälsan, which provides services for construction industries.
A notable exception is the arrangement organized by a trade union whose members are employed in widely scattered SSEs in a single industry (e.g., health care workers, meat cutters, office workers and garment workers). Usually organized under a collective agreement, they are financed by employers’ contributions but are usually governed by a board comprising representatives of both employers and workers. Some operate local health centres providing a broad range of primary and specialist clinical services not only for workers but often for their dependants as well.
In some instances, occupational health services are being provided by hospital outpatient clinics, private health centres and community primary care centres. They tend to focus on the treatment of acute work-related injuries and illnesses and, except perhaps for routine medical examinations, provide little in the way of preventive services. Their staffs often have a low level of sophistication in occupational safety and health, and the fact that they are usually paid on a fee-for-service basis provides no great incentive for their involvement in the surveillance, prevention and control of workplace hazards.
A particular disadvantage of these “external services” arrangements is that the customer or client relationship with those using them generally precludes the participation and collaboration of employers and workers in the planning and monitoring of these services that are stipulated in the ILO Conventions and the other international instruments created to guide occupational safety and health services.
Another variant is the “social security model”, in which occupational health services are provided by the same organization that is responsible for the cost of compensation for occupational diseases and injuries. This facilitates the availability of resources to finance the services in which, although curative and rehabilitative services are featured, preventive services are often prioritized.
An extensive study carried out in Finland (Kalimo et al. 1989), one of the very few attempts to evaluate occupational health services, showed that municipal health centres and private health centres were the dominant providers of occupational health services to SSEs, followed by the group or shared centres. The smaller the enterprise, the more likely it was to use the municipal health centre; up to 70% of SSEs with one to five workers were served by municipal health centres. Significant findings of the study included verification of the value of workplace visits by the personnel of the centres serving the SSEs to gain knowledge (1) of the working conditions and the particular occupational health problems of the client enterprises, and (2) of the need to provide them with special training in occupational safety and health before they undertake the provision of the services.
Types of Activities for Occupational Health Services for SSEs
The occupational health services designed for SSEs vary widely according to national laws and practices, the types of work and work environments involved, the characteristics and health status of the workers and the availability of resources (both in terms of the ability of the SSEs to afford the occupational health services and the availability of health care facilities and personnel in the locality). Based on the international instruments cited above and regional seminars and consultations, a list of activities for comprehensive occupational health services has been developed (Rantanen 1989; WHO 1989a, 1989b). A number of key activities that should always be found in an occupational health services programme, and that are relevant for SSEs, can be picked up from those reports. They include for example:
Assessment of occupational health needs of the enterprise
- preliminary analysis of the activities of the enterprise and identification of the health and safety hazards common to such workplaces
- inspection and surveillance of the workplace to identify and quantify the hazards actually present in the particular enterprise
- assessment of the extent of the risks they present and ranking them in order of their urgency and priority
- repeating the hazard assessment whenever there are changes in production methods, equipment and materials.
Prevention and control activities in the workplace
- communication of the results of the assessment to the owners/managers and the workers’ representatives
- identification of the prevention and control measures that are needed and available, assigning relative priority to them in terms of urgency and feasibility
- overseeing their installation and implementation
- monitoring their continuing effectiveness.
Preventive activities oriented to workers
- assessment and surveillance of workers’ health status by pre-placement, screening and periodic examinations which may be general as well as focused on the biological effects of particular hazards to which the workers may have been exposed
- adaptation of the job, the work station and the workplace environment to promote workers’ ongoing health and safety with special attention to such vulnerable groups as the very young, the elderly and those with acquired diseases and disabilities
- providing workers with health education and training in proper work practices
- providing education and training for owners/managers and supervisors that will inculcate awareness of the health needs of workers and motivation to initiate appropriate prevention and control measures.
Curative activities
- provide or arrange the delivery of the appropriate diagnostic, therapeutic and rehabilitative services for occupational injuries and diseases
- provide or arrange for early rehabilitation to obviate avoidable disability and encourage and oversee adjustments in the job that will permit early return to work
- provide education and training (and periodic retraining) in first aid and emergency procedures
- establish procedures and conduct training drills for coping with major emergencies such as spills, fires, explosions and so on
- provide or arrange for workers’ involvement in programmes that promote general health and well-being.
Record keeping and evaluation
- make and retain appropriate records on occupational accidents, injuries and diseases and if possible on exposure; evaluate the overall health and safety status of the enterprise on the basis of such data
- monitor the effectiveness of hazard prevention and control measures.
Implicit in the above list of core activities is the appropriate availability of advice and consultations in such occupational safety and health specialities as occupational hygiene, ergonomics, work physiology, safety engineering, occupational psychiatry and psychology and so on. Such specialists are not likely to be represented in the personnel of the facilities providing occupational health services to SSEs but, when needed, they can usually be provided by governmental agencies, universities and private consulting resources.
Because of their lack of sophistication and time, owners/managers of SSEs are forced to rely more heavily on the purveyors of safety equipment for the effectiveness and reliability of their products, and on the suppliers of chemicals and other production materials for complete and clear information (e.g., data sheets) about the hazards they may present and how these may be prevented or controlled. It is important, therefore, that there be national laws and regulations covering proper labelling, product quality and reliability, and the provision of easily understood information (in the local language) about equipment use and maintenance as well as product use and storage. As a backup, the trade and community organizations of which SSEs are often members should feature information about the prevention and control of potentially hazardous exposures in their newsletters and other communications.
Conclusions
In spite of their importance for the national economy and their role as employer of a majority of the nation’s workforce, SSEs, the self-employed and agriculture are sectors that are typically underserved by occupational health services. ILO Convention No. 161 and Recommendation No. 171 provide relevant guidelines for the development of such services for SSEs and should be ratified and implemented by all countries. National governments should develop the requisite legal, administrative and financial mechanisms to provide all workplaces with occupational safety and health services that will effectively identify, prevent and control exposures to potential hazards and promote the enhancement and maintenance of optimal levels of health status, well-being and productive capacity of all workers. Collaboration at international, regional and subregional levels, such as that provided by the ILO and the WHO, should be encouraged to foster the exchange of information and experience, the development of appropriate standards and guidelines and the undertaking of relevant training and research programmes.
SSEs may in many instances be reluctant to seek actively the services of occupational health units even though they might be the best beneficiaries of such services. Considering this, some governments and institutions, particularly in Nordic countries, have adopted a new strategy by starting wide-scale interventions for establishment or development of services. For instance the Finnish Institute of Occupational Health currently implements an Action Programme, for 600 SSEs employing 16,000 workers, aimed at the development of occupational health services, maintenance of work ability, prevention of environmental hazards in the neighbourhood and improving the competence of SSEs in occupational health and safety.
Outplacement
Outplacement is a professional consulting service that helps organizations plan and implement individual terminations or reductions in their workforces so as to minimize disruptions and avoid legal liability, and counsels terminated employees in order to minimize the trauma of separation while orienting them towards seeking alternative employment or new careers.
The economic downturn of the 1980s, which continues in the 1990s, has been characterized by a virtual pandemic of job terminations reflecting the closing down of obsolescent or unprofitable units, plants and businesses, the elimination of redundancies created by mergers, takeovers, consolidations and reorganizations, and the trimming of staff to reduce operating costs and produce a “lean and mean” workforce. Although less striking than in private industry thanks to the protection of civil service regulations and political pressures, the same phenomenon has also been seen in government organizations struggling to cope with budget deficits and a philosophy that less government is desirable.
For the terminated employees, job loss is a potent stressor and source of trauma, especially when the manner of dismissal is sudden and brutal. It generates anger, anxiety and depression and may cause decompensation in persons with marginal adjustment to chronic mental illness. Rarely, the anger may express itself in sabotage or violence aimed at the supervisors and managers responsible for the termination. Sometimes, the violence is directed at spouses and family members.
The trauma of job loss has also been associated with physical ailments ranging from headaches, gastrointestinal disturbances and other functional complaints to stress-related disorders such as heart attacks, bleeding peptic ulcers and colitis.
In addition to the financial impact of loss of earnings and, in the United States, loss of employer-sponsored health insurance, job loss also affects the health and well-being of the families of the terminated employees.
Employees who are not terminated are also affected. Despite employers’ reassurances, there often is concern over the possibility of additional layoffs (threatened job loss has been found to be an even more potent stressor than actual loss of the job). In addition, there is the stress of adjusting to changes in work load and job content as relationships with co-workers are reshuffled. “Downsizing”, or reduction in the size of a workforce, may also be traumatic to the employer. It may take significant time and effort to smooth out the resultant organizational disruptions and achieve the desired productive efficiency. Valuable employees not scheduled for termination may leave for other, ostensibly more secure jobs and better-organized firms. There is also the potential of legal liability stemming from discharged employees’ allegations of breach of contract or unlawful discrimination.
Outplacement—A Preventive Approach
Outplacement is a professional service offered to prevent, or at least minimize, the trauma of staff reduction for terminated employees, those who remain and the employer.
Not all discharged employees require assistance. For some, the termination precipitates an opportunity to seek new work that might provide welcome relief from a job that had become stultifying and offered little hope of advancement. For most, however, professional counselling in working through the almost inevitable disappointment and anger of dismissed employees and help in finding new jobs can facilitate the restoration of their sense of self-worth and their well-being. Even those who accept the lure of the “golden handshake” (a package of enhanced severance and retirement benefits) and leave voluntarily may benefit from help in making the necessary readjustments.
It is generally agreed that outplacement services are most inexpensively provided by in-house staff. However, even a large organization with a competent and well-functioning staff may not have had much experience with the sensitive work of downsizing and may be too busy planning the restructuring of the organization following the exodus to attend to the niceties that may be involved. Even hardened executives often find it difficult to deal with their erstwhile co-workers. Furthermore, the departing employees are more likely to give credibility to advice from a “neutral” resource.
Accordingly, the vast majority of organizations find it expedient to contract with an outplacement consultant or consulting firm. This neutrality is reinforced by having all possible outplacement contacts located offsite in separate quarters occupied even temporarily by the consultant(s).
Outplacement Process
The outplacement process for terminated employees needs to be individualized depending on their attitudes, capabilities and circumstances, and the nature of the job market locally or in other regions. For non-exempt production workers and first-line supervisors, it involves an inventory of the worker’s skills and, where there is a market for them, assistance in placement. Where no suitable jobs exist, it involves assessment of the potential for retraining, referral for retraining, and assistance in marketing the new skills. An unfortunate complication that is difficult to overcome arises when the pay scales for the available new jobs do not measure up to the earnings of the former employment.
For employees in managerial and “creative” positions, the process generally involves a number of phases that are frequently overlapping. These phases are considered under the following heads.
Leaving the past employer.
The object is to help the candidate through the stages of reaction, understanding and acceptance of his or her predicament. Occasionally, this may require the intervention of a mental health professional.
This usually involves a reevaluation of the termination event. To earn the candidate’s confidence and assist in establishing a desirable rapport, the consultant generally reviews the circumstances of the termination and makes certain that the candidate understands them and, furthermore, has received all of the monetary and other benefits to which he or she may be entitled.
This phase concludes when the candidate is able to deal constructively with the immediate problems and responsibilities and is ready to start preparing for the future with a positive attitude. Ideally, some measure of reconciliation has been established with the past employer and the candidate is willing to accept whatever support may be offered. Such support may include temporary use of an office with a business address and telephone, supplemented by the services of a secretary who can provide typing and photocopying services, take messages, confirm appointments, etc. Most candidates function more effectively from an business-like office environment than from their own homes. Also, the consultant helps formulate a mutually satisfactory reason for the termination and arrange a mutually acceptable response to requests for references from potential employers.
Preparation for new employment.
This phase is intended to provide the focus and structure for positive thinking and action. It involves a start of the recovery of self-confidence (which continues throughout the process) by building a personal data base of the candidate’s skills, abilities, knowledge and experience, and learning to communicate it in clear, functional terms. Simultaneously, the candidate begins to identify and confirm suitable job objectives and to consider the nature of the jobs for which his or her background might be particularly suitable. Through it all, the candidate acquires the knack of accumulating and organizing information that will highlight the range and depth of his or her experience and level of competence.
Résumé writing.
Here, the candidate learns to develop a flexible tool that will present his or her objectives, qualifications, and background, arouse the interest of potential employers, help obtain interviews, and serve as an aid during job interviews. Rather than being restricted to a fixed format, the résumé is varied to “package” skills and experiences to make them most attractive for particular job opportunities.
Assessing job opportunities.
The consultant guides the candidate to an assessment of the availability of potential jobs that might be suitable. This includes a survey of different industries, the job market in different localities, opportunities for growth and advancement, and likely earning potential. Experience indicates that about 80% of job opportunities are “hidden,” that is, they are not readily apparent on the basis of industry designation or job title. Where appropriate, the assessment also includes an appraisal of the potential of self-employment.
Job-hunting campaign.
This involves identifying and exploring existing and potential opportunities through direct approaches to potential employers and developing and making use of contacts and intermediaries. The campaign entails obtaining interviews with the “right” people on a right basis, and using letters both to obtain interviews and as a follow-up to interviews.
The consultant will, as part of enhancing the candidate’s job-hunting skills, improve his or her writing and interview techniques. Practice in letter writing is aimed at polishing a communication skill that is uniquely helpful in defining job opportunities, in identifying the “right” people and developing contacts with them, obtaining interviews with them and in following up on interviews. The candidate is further trained by interview coaching, which involves role playing and critiquing videotapes of practice interviews in order to maximize the effectiveness with which his or her personality, experience and desires are presented. The candidate’s chances of coming away from an interview, with, at least, an appointment for the next interview, if not an actual job offer, are by this means enhanced.
Negotiating compensation.
The consultant will help candidates overcome their dislike or even fear of discussing compensation in negotiating a potential position so that they can obtain the best compensation package possible under the existing circumstances, avoiding the possibility of over-selling or under-selling themselves or antagonizing the interviewer.
Control.
Within the limits of the consulting contract, regular contact with the candidate is maintained until a new position is maintained. This involves gathering and organizing information to track how the campaign is progressing and to ensure optimal use of time and effort. It will help the candidate to avoid errors of omission and provide a signal to correct errors of commission.
Following through.
When a new position is obtained, the candidate notifies the consultant and the old employer as well as other prospective employers with whom he or she may have been negotiating.
Follow-up.
Again, within the limits of the contract, the consultant maintains contact to assist the candidate’s adjustment to the new position to aid in overcoming any adverse factors and to encourage continuing career growth and development. Finally, at the close of the programme, the consultant provides the employer with an aggregate report of the results (personal and/or sensitive information is usually held confidential).
The organization
It is rare for the outplacement consultant to be involved in designating specifically which employees are to be separated and which will remain — that is a decision usually made by the organization’s top management, often in consultation with department heads and line supervisors and in the light of the structure envisioned for the revised organization. The consultant, however, does provide guidance on the planning, timing and staging of the downsizing process and on the communications with both those who will leave and those who will remain. Since the “grapevine” (i.e., rumors circulating in the workforce) is usually active, it is imperative that these communications be timely, complete and accurate. Proper communications will also help address potential allegations of discrimination. The consultant also often assists with public relations communications to the industry, customers and the community.
Caveats
The extent of downsizing during the last decade, at least in the United States, has given impetus to development of a veritable industry of outplacement consultants and firms. A number of search firms devoted to identifying candidates for job vacancies have taken up outplacement as a side-line. A variety of semiprofessionals, including former personnel directors, have become outplacement counsellors.
Until recently, there was no formally adopted code of practice and ethical standards. However, in 1992, the International Association of Outplacement Professionals (IAOP) sponsored the creation of the Outplacement Institute, membership in which requires meeting a set of criteria based on educational background and personal experience, evidence of continuing participation in programs of personal and professional development, and a commitment to uphold and observe the published IAOP Standards for Ethical Practice.
Conclusion
Reduction in the size of a workforce is, at best, a trying experience for the employees being terminated or forced into retirement, and for those remaining and for the organization as a whole. It is invariably traumatic. Outplacement is a professional consulting service designed to prevent or minimize the potential adverse effects and promote the health and well-being of those involved.
Stress Management Programmes
The essential mission of occupational health and safety is to protect and enhance the health, well-being and productivity of workers, individually and collectively. That mission cannot be accomplished without an understanding of stress and the mechanisms through which it affects individuals and organizations, and without a well-planned programme that will both alleviate its deleterious effects and, more important, prevent them.
Stress is an inescapable ingredient of the lives of all people everywhere. It stems from—and simultaneously affects—individuals’ inner sense of well-being; their relationships with family, friends, co-workers and strangers; and their capacity to function in the home, the workplace and the community. When excessive, it leads to physical or psychological symptoms and, when prolonged, it may lead to disability and disease. It modifies individuals’ perceptions, feelings, attitudes and behaviour and affects the organizations whose activities they direct or carry out. The subject of stress is covered extensively elsewhere in this Encyclopaedia.
Designing a Stress Management Programme
The effective workplace stress management programme will contain a number of overlapping elements operating concurrently. Some are formalized under the designation of a stress management programme while others are simply part of general organizational management even when they are explicitly aimed at controlling stress. Some of these are aimed at employees individually and in groups; others are aimed at stressors arising in the workplace; and still others address the stressors impinging on the organization as an entity in itself which inevitably filter down to affect some or all of the employees. The elements of a workplace stress management programme will be examined under the following headings.
1. Managing stress-related symptoms. This element deals with individuals already suffering from the effects of stress. Labelled the “medical model,” it attempts to identify individuals with signs and symptoms and to persuade them to come forward voluntarily or accept referral to professionals able to evaluate their problems, diagnose the causes and offer appropriate treatment. It may be based in the employee health service or in the employee assistance programme, or it may be associated with any other counselling services provided by the organization. The services may cover a broad range extending from one-on-one interviews and examinations to telephone “hot-lines” for emergency situations to comprehensive centres with multidisciplinary staffs of qualified professionals. It may be served by full- or part-time professionals or by contractual or casual referral arrangements with professionals who come to the worksite or are based in nearby facilities in the community. Some units deal with any and all problems, while others may more or less focus on such specific stress-related syndromes as hypertension, backache, alcoholism, drug abuse or family problems. The contributions of these service elements to the stress management programme are based on the following capabilities:
- An awareness that many recurrent or persistent somatic complaints such as muscular aches and pains, backache, headache, gastrointestinal upsets, and so on, are attributable to stress. Instead of simply providing palliative medications and advice, the alert health professional or counsellor will recognize the pattern and direct attention to the stressors that are actually responsible.
- Recognition that when a number of employees in a particular unit or area of the workplace present such functional complaints, a search should be initiated for a causative factor in the work environment which may prove to be a controllable stressor.
- Reaching out to individuals involved in or witnessing a cataclysmic occurrence such as a fatal accident, or an episode of violence.
- Seizing the opportunity to stay a disciplinary action faced by an employee because of inadequate performance or aberrant behaviour pending an opportunity to lower the stress level and restore his or her normal equanimity and work capacity.
2. Reducing individual vulnerability. The most common elements in stress management programmes are those that help individuals to cope with stress by reducing their vulnerability. These include series of seminars and workshops, supplemented by audiotapes or videotapes and pamphlets or other publications that educate employees to cope with stress more effectively. Their common denominators are these:
- Training in self-awareness and problem analysis to detect signs of increasing stress and identify the stressors that are responsible
- Assertiveness training enabling workers to become more dynamic in dealing with them
- Techniques that will reduce stress to more tolerable levels
Some of the tools they employ are listed in figure 1. For those not familiar with the term, “rap sessions” are meetings of groups of employees, with or without supervisors being present, in which experiences and problems are discussed and complaints freely ventilated. They are analogous to the shop meetings held under union auspices.
Figure 1. Some approaches to reducing vulnerability.
3. Interpersonal relations in the workplace. Organizations are being increasingly made aware of stressors emanating from the diversity of the workforce and the interpersonal problems they often present. Prejudice and bigotry do not stop at the gates of the worksite and are often compounded by insensitive or discriminatory behaviour on the part of managers and supervisors. Sexual and racial bias may take the form of harassment and may even be expressed in or evoke acts of violence. When rampant, such attitudes demand prompt correction through enunciation of an explicit policy that includes disciplinary actions against those who are guilty, coupled with protecting victims emboldened to complain against reprisals.
4. Managing job-related stressors. It is the organization’s responsibility to minimize job-related stressors that may have an adverse effect on employees’ capacity to function effectively. It is most important to ensure that supervisors and managers on all levels receive appropriate training to recognize and to deal promptly and effectively with the “people problems” that will inevitably arise in the workplace.
5. Managing the organization’s stress. The organization as an entity is exposed to stressors which, if not properly managed, filter down through the workforce, inevitably impinging on employees on all levels. This state of affairs requires the establishment of challenging but attainable goals and objectives, early identification and assessment of potential stressors that may thwart those plans, coordination of the organization’s capacities to deal with them and the communication of the results of those efforts to the workforce. The last-mentioned need is particularly critical at times of economic stringency, when employee collaboration and optimal productivity are especially important in dealing with such crises as changes in top management, threatened mergers and takeovers, plant closings or relocations. and downsizing.
6. Helping to manage personal stressors. While the management of stressors arising in the home and in the community is fundamentally a problem for the individual, employers are discovering that the stress they generate is inevitably brought into the workplace where, either on their own or in conjunction with job-related stressors, they often affect employees’ well-being and compromise their work performance. Accordingly, employers are finding it expedient (and in some instances, necessary) to establish programmes designed to assist employees to cope with stressors of this sort. A list of the most common personal stressors and workplace programmes aimed at them is presented in figure 2.
Figure 2. Stressors in the workplace and workplace programmes to help with them.
Basic Principles of the Programme
In establishing a worksite stress management programme, some basis principles must be emphasized.
First, it must be remembered that there are no boundaries between stress arising in the workplace, in the home and in the community. Each individual presents a unique composite of all of the factors which are carried wherever he or she may go. This means that while the programme must focus on those problems arising in the workplace, it must recognize that these continue to affect the worker’s outside life, nor can it ignore those originating off the job. Indeed, it has been shown that work itself and the support derived from co-workers and the organization may have a therapeutic value in dealing with personal and family problems. In fact, the loss of this support probably accounts for much of the disability associated with retirement, even when it is voluntary.
Second, stress is highly “contagious”. It not only affects particular individuals but also those about them with whom they must relate and collaborate. Thus, dealing with stress is simultaneously therapeutic and preventive.
Third, coping with stress is inherently an individual responsibility. Troubled employees can be identified and offered counselling and guidance. They can be given support and encouragement and taught to improve their coping skills. When necessary, they can be referred to qualified health professionals in the community for more intensive or prolonged therapy. But, in the last analysis, all this requires the consent and participation of the individual which, in turn, depends on the structure of the programme, its status in the organization, the competence of its staff and the reputations they earn, and its accessibility. Perhaps the most important determinant of programme success is the establishment of and strict adherence to a policy of observing the confidentiality of personal information.
Fourth, control of workplace stress is fundamentally a managerial responsibility. The programme must be based on an explicit organizational policy that places high value on employee’s health and well-being. And that policy must be reflected in the day-to-day operations by the attitudes and behaviour of managers on all levels,
Fifth, employee involvement in the programme’s design and operation and, particularly, in identifying stressors and devising ways to control them is an important ingredient of programme success. This is facilitated in many workplaces where safety and health joint labour-management committees function or where worker participation in managerial decision-making is encouraged.
Finally, a successful stress management programme requires an intimate understanding of the employees and the environment in which they work. It is most successful when stress-related problems are identified and resolved before any damage is done.
Conclusion
The essential mission of occupational health and safety is to protect and enhance the health, well-being and productivity of workers, individually and collectively. That mission cannot be accomplished without an understanding of stress and the mechanisms through which it affects individuals and organizations, and a well-planned programme that will both alleviate its deleterious effects and, more important, prevent them.
Cancer Prevention and Control
Within the next decade, it is predicted, cancer will become the leading cause of death in many developed countries. This reflects not so much an increase in the incidence of cancer but rather a decrease in mortality due to cardiovascular disease, currently topping the mortality tables. Equally with its high mortality rate, we are disturbed by the specter of cancer as a “dread” disease: one associated with a more or less rapid course of disability and a high degree of suffering. This somewhat fearsome picture is being made easier to contemplate by our growing knowledge of how to reduce risk, by techniques permitting early detection and by new and powerful achievements in the field of therapy. However, the latter may be associated with physical, emotional and economic costs for both the patients and those concerned about them. According to the US National Cancer Institute (NCI), a significant reduction in cancer morbidity and mortality rates is possible if current recommendations relating to use of tobacco, dietary changes, environmental controls, screening and state-of-the-art treatment are effectively applied.
To the employer, cancer presents significant problems entirely apart from the responsibility for possible occupational cancer. Workers with cancer may have impaired productivity and recurrent absenteeism due both to the cancer itself and the side effects of its treatment. Valuable employees will be lost through prolonged periods of disability and premature death, leading to the considerable cost of recruiting and training replacements.
There is a cost to the employer even when it is a spouse or other dependant rather than the healthy employee who develops the cancer. The caregiving burden may lead to distraction, fatigue and absenteeism which tax that employee’s productivity, and the often considerable medical expenses increase the cost of employer-sponsored health insurance. It is entirely appropriate, therefore, that cancer prevention should be a major focus of worksite wellness programs.
Primary Prevention
Primary prevention involves avoidance of smoking and modifying other host factors that may influence the development of cancer, and identifying potential carcinogens in the work environment and eliminating or at least limiting workers’ exposure to them.
Controlling exposures
Potential as well as proven carcinogens are identified through basic scientific research and by epidemiological studies of exposed populations. The latter involves industrial hygiene measurements of the frequency, magnitude and duration of the exposures, coupled with comprehensive medical surveillance of the exposed workers, including analysis of causes of disability and death. Controlling exposures involves the elimination of these potential carcinogens from the workplace or, when that is not possible, minimizing exposure to them. It also involves the proper labeling of such hazardous materials and continuing education of workers with respect to their handling, containment and disposal.
Smoking and cancer risk
Approximately one-third of all cancer deaths and 87% of all lung cancers in the US are attributable to smoking. Tobacco use is also the principal cause of cancers of the larynx, oral cavity and oesophagus and it contributes to the development of cancers of the bladder, pancreas, kidney, and uterine cervix. There is a clear dose-response relationship between lung cancer risk and daily cigarette consumption: those who smoke more than 25 cigarettes a day have a risk that is about 20 times greater than that of non-smokers.
Experts believe that the involuntary intake of the tobacco smoke emitted by smokers (“environmental tobacco smoke”) is a significant risk factor for lung cancer in non-smokers. In January 1993, the US Environmental Protection Agency (EPA) classified environmental tobacco smoke as a known human carcinogen which, it estimated, is responsible for approximately 3,000 lung cancer deaths annually among US non-smokers.
The 1990 US Surgeon General’s report on the health benefits of smoking cessation provides clear evidence that quitting smoking at any age is beneficial to one’s health. For example, five years after quitting, former smokers experience a diminished risk for lung cancer; their risk, however, remains higher than that of non-smokers for as long as 25 years.
The elimination of tobacco exposure by employer-sponsored/ labor union-sponsored smoking cessation programs and worksite policies enforcing a smoke-free working environment represent a major element in most worksite wellness programs.
Modifying host factors
Cancer is an aberration of normal cell division and growth in which certain cells divide at abnormal rates and grow abnormally, sometimes migrating to other parts of the body, affecting the form and function of involved organs, and ultimately causing death of the organism. Recent, continuing biomedical advances are providing increasing knowledge of the carcinogenesis process and are beginning to identify the genetic, humoral, hormonal, dietary and other factors that may accelerate or inhibit it—thus leading to research on interventions that have the potential to identify the early, precancerous process and so to help restore the normal cellular growth patterns.
Genetic factors
Epidemiologists continue to accumulate evidence of familial variations in the frequency of particular types of cancer. These data have been bolstered by molecular biologists who have already identified genes that appear to control steps in cellular division and growth. When these “tumor suppressor” genes are damaged by naturally-occurring mutations or the effects of an environmental carcinogen, the process may go out of control and a cancer is initiated.
Heritable genes have been found in patients with cancer and members of their immediate families. One gene has been associated with a high risk of colon cancer and endometrial or ovarian cancer in women; another with a high risk of breast and ovarian cancer; and a third with a form of malignant melanoma. These discoveries led to a debate about the ethical and sociological issues surrounding DNA testing to identify individuals carrying these genes with the implication that they then might be excluded from jobs involving possible exposure to potential or actual carcinogens. After studying this question, the National Advisory Council for Human Genome Research (1994), raising issues to do with the reliability of the testing, the present effectiveness of potential therapeutic interventions, and the likelihood of genetic discrimination against those found to be at high risk, concluded that “it is premature to offer DNA testing or screening for cancer predisposition outside a carefully monitored research environment”.
Humoral factors
The value of the prostate specific antigen (PSA) test as a routine screening test for prostatic cancer in older men has not been scientifically demonstrated in a clinical trial. However, in some instances, it is being offered to male workers, sometimes as a token of gender equity to balance the offering of mammography and cervical Pap smears to female workers. Clinics providing routine periodic examinations are offering the PSA test as a supplement to and, sometimes, even as a replacement for the traditional digital rectal examination as well as the recently introduced rectal ultrasound examination. Although its use appears to be valid in men with prostatic abnormalities or symptoms, a recent multinational review concludes that measurement of PSA should not be a routine procedure in screening healthy male populations (Adami, Baron and Rothman 1994).
Hormonal factors
Research has implicated hormones in the genesis of some cancers and they have been used in the treatment of others. Hormones, however, do not appear to be an appropriate item to emphasize in workplace health promotion programs. A possible exception would be warnings of their potential carcinogenic hazard in certain cases when recommending hormones for the treatment of menopausal symptoms and the prevention of osteoporosis.
Dietary factors
Researchers have estimated that approximately 35% of all cancer mortality in the US may be related to diet. In 1988, the US Surgeon General’s Report on Nutrition and Health indicated that cancers of the lung, colon-rectum, breast, prostate, stomach, ovary and bladder may be associated with diet. Research indicates that certain dietary factors—fat, fiber, and micronutrients such as beta-carotene, vitamin A, vitamin C, vitamin E and selenium—may influence cancer risk. Epidemiological and experimental evidence indicates that modulation of these factors in the diet can reduce the occurrence of some types of cancer.
Dietary fat
Associations between excess intake of dietary fat and the risk of various cancers, particularly cancers of the breast, colon and prostate, have been demonstrated in both epidemiological and laboratory studies. International correlational studies have shown a strong association between the incidence of cancers at these sites and total dietary fat intake, even after adjusting for total caloric intake.
In addition to the amount of fat, the type of fat consumed may be an important risk factor in cancer development. Different fatty acids may have various site-specific tumor-promoting or tumor-inhibiting properties. Intake of total fat and saturated fat has been strongly and positively associated with colon, prostate, and post-menopausal breast cancers; intake of polyunsaturated vegetable oil has been positively associated with post-menopausal breast and prostate cancers, but not with colon cancer. Conversely, consumption of highly polyunsaturated omega-3 fatty acids found in certain fish oils may not affect or may even decrease the risk of breast and colon cancers.
Dietary fiber
Epidemiological evidence suggests that the risk of certain cancers, particularly colon and breast cancers, may be lowered by increased intake of dietary fiber and other dietary constituents associated with high intakes of vegetables, fruits, and whole grains.
Micronutrients
Epidemiological studies generally show an inverse relationship between cancer incidence and intake of foods high in several nutrients having antioxidant properties, such as beta-carotene, vitamin C (ascorbic acid), and vitamin E (alpha-tocopherol). A number of studies have shown that low intakes of fruits and vegetables are associated with increased risk of lung cancer. Deficiencies of selenium and zinc have also been implicated in increased cancer risk.
In a number of studies in which the use of antioxidant supplements was shown to reduce the expected number of serious heart attacks and strokes, the data on cancer were less clear. However, results from the Alpha-Tocopherol, Beta-Carotene (ATBC) Lung Cancer Prevention clinical trial, conducted by the NCI in collaboration with the National Public Health Institute of Finland, indicated that vitamin E and beta-carotene supplements did not prevent lung cancer. Vitamin E supplementation also resulted in 34% fewer prostate cancers and 16% fewer colorectal cancers, but those subjects taking beta-carotene had 16% more lung cancers, which was statistically significant, and had slightly more cases of other cancers than those taking vitamin E or the placebo. There was no evidence that the combination of vitamin E and beta-carotene was better or worse than either supplement alone. The researchers have not yet determined why those taking beta-carotene in the study were observed to have more lung cancers. These results suggest the possibility that a different compound or compounds in foods which have high levels of beta-carotene or vitamin E may be responsible for the protective effect observed in epidemiological studies. The researchers also speculated that the length of time of supplementation may have been too short to inhibit the development of cancers in long-term smokers. Further analyses of the ATBC study, as well as results from other trials in progress, will help resolve some of the questions that have arisen in this trial, particularly the question of whether large doses of beta-carotene may be harmful to smokers.
Alcohol
Excessive use of alcoholic beverages has been associated with cancer of the rectum, pancreas, breast and liver. There is also strong evidence supporting a synergistic association of alcohol consumption and tobacco use with increased risk of cancer of the mouth, pharynx, oesophagus and larynx.
Dietary recommendations
Based on the compelling evidence that diet is related to cancer risk, the NCI has developed dietary guidelines that include the following recommendations:
- Reduce fat intake to 30% or less of calories.
- Increase fibre intake to 20 to 30 grams per day, with an upper limit of 35 grams.
- Include a variety of vegetables and fruits in the daily diet.
- Avoid obesity.
- Consume alcoholic beverages in moderation, if at all.
- Minimize consumption of salt-cured (packed in salt), salt-pickled (soaked in brine), or smoked foods (associated with increased incidence of stomach and oesophageal cancer).
These guidelines are intended to be incorporated into a general dietary regimen that can be recommended for the entire population.
Infectious diseases
There is increasing knowledge of the association of certain infectious agents with several types of cancer: for example, the hepatitis B virus with liver cancer, the human papillomavirus with cervical cancer, and the Epstein-Barr virus with Burkitt’s lymphoma. (The frequency of cancer among patients with AIDS is attributable to the patient’s immunodeficiency and is not a direct carcinogenic effect of the HIV agent.) A vaccine for hepatitis B is now available that, when given to children, ultimately will reduce their risk for liver cancer.
Worksite Cancer Prevention
To explore the potential of the workplace as an arena for the promotion of a broad set of cancer prevention and control behaviors, the NCI is sponsoring the Working Well Project. This project is designed to determine whether worksite-based interventions to reduce tobacco use, achieve cancer preventive dietary modifications, increase screening prevalence and reduce occupational exposure can be developed and implemented in a cost-effective way. It was initiated in September 1989 at the following four research centers in the United States.
- M.D. Anderson Cancer Center, Houston, Texas
- University of Florida, Gainesville, Florida
- Dana Farber Cancer Institute, Boston, Massachusetts
- Miriam Hospital/Brown University, Providence, Rhode Island
The project involves approximately 21,000 employees at 114 different worksites around the United States. Most of the selected worksites are involved predominantly in manufacturing; other types of worksites in the project included fire stations and newspaper printers. Tobacco reduction and dietary modification were areas of intervention included in all of the worksites; however, each site maximized or minimized particular intervention programs or included additional options to meet the climatic and socioeconomic conditions of the geographic area. The centers in Florida and Texas, for example, included and emphasized skin cancer screening and the use of sun screens because of increased exposure to the sun in those geographic regions. The centers in Boston and Texas offered programs that emphasized the relationship between cancer and tobacco use. The Florida centre enhanced the diet modification intervention with supplies of fresh citrus fruits, readily available from the state’s farming and fruit industry. Management-employee consumer boards also were established at the worksites of the Florida centre to work with the food service to ensure that the cafeterias offered fresh vegetable and fruit selections. Several of the worksites participating in the project offered small prizes—gift certificates or cafeteria lunches—for continued participation in the project or for achievement of a desired goal, such as smoking cessation. Reduction of exposure to occupational hazards was of special interest at those worksites where diesel exhaust, solvent use or radiation equipment were prevalent. The worksite-based programs included:
- group activities to generate interest, such as taste testing of various foods
- directed group activities, such as quit-smoking contests
- medical/scientific-based demonstrations, such as
 testing, to verify the effect of smoking on the respiratory system
testing, to verify the effect of smoking on the respiratory system - seminars on business practices and policy development aimed at significantly reducing or eliminating occupational exposure to potentially or actually dangerous or toxic materials
- computer-based self-help and self-assessment programmes on cancer risk and prevention
- manuals and self-help classes to help reduce or eliminate tobacco use, achieve dietary modifications, and increase cancer screening.
Cancer education
Worksite health education programs should include information about signs and symptoms that are suggestive of early cancer—for example, lumps, bleeding from the rectum and other orifices, skin lesions that do not appear to heal—coupled with advice to seek evaluation by a physician promptly. These programs might also offer instruction, preferably with supervised practice, in self-examination of the breast.
Cancer screening
Screening for precancerous lesions or early cancer is carried out with a view to their earliest possible detection and removal. Educating individuals about the early signs and symptoms of cancer so that they may seek the attention of a physician is an important part of screening.
A search for early cancer should be included in every routine or periodic medical examination. In addition, mass screenings for particular types of cancer may be carried out in the workplace or in a community facility near the worksite. Any acceptable and justifiable screening of an asymptomatic population for cancer should meet the following criteria:
- The disease in question should represent a substantial burden at the public health level and should have a prevalent, asymptomatic, nonmetastatic phase.
- The asymptomatic, nonmetastatic phase should be recognizable.
- The screening procedure should have reasonable specificity, sensitivity and predictive values; it should be of low risk and low cost, and be acceptable to both the screener and the person being screened.
- Early detection followed by appropriate treatment should offer a substantially greater potential for cure than exists in cases in which discovery was delayed.
- Treatment of lesions detected by screening should offer improved outcomes as measured in cause-specific morbidity and mortality.
The following additional criteria are particularly relevant in the workplace:
- Employees (and their dependants, when involved in the programme) should be informed of the purpose, nature and potential results of the screening, and a formal “informed consent” should be obtained.
- The screening programme should be conducted with due consideration for the comfort, dignity and privacy of the individuals consenting to be screened and should involve minimal interference with working arrangements and production schedules.
- Screening results should be conveyed promptly and privately, with copies forwarded to personal physicians designated by the workers. Counselling by trained health professionals should be available to those seeking clarification of the screening report.
- The individuals screened should be informed of the possibility of false negatives and warned to seek medical evaluation of any signs or symptoms developing soon after the screening exercise.
- A prearranged referral network should be in place to which those with positive results who are not able or do not wish to consult their personal physicians may be referred.
- The costs of the necessary confirmatory examinations and the costs of treatment should be covered by health insurance or otherwise be affordable.
- A prearranged follow-up system should be in place to be sure that positive reports have been promptly confirmed and proper interventions arranged.
A further final criterion is of fundamental importance: the screening exercise should be conducted by properly skilled and accredited health professionals using state-of-the-art equipment and interpretation and analysis of the results should be of the highest possible quality and accuracy.
In 1989 the US Preventive Services Task Force, a panel of 20 experts from medicine and other related fields drawing upon hundreds of “advisors” and others from the United States, Canada and the United Kingdom, assessed the effectiveness of some 169 preventive interventions. Its recommendations with respect to screening for cancer are summarized in table 1. Reflecting the Task Force’s somewhat conservative attitude and rigorously applied criteria, these recommendations may differ from those advanced by other groups.
Table 1. Screening for neoplastic diseases.
|
Types of cancer |
Recommendations of the US Preventive Services Task Force* |
|
Breast |
All women over age 40 should receive an annual clinical breast examination. Mammography every one to two years is recommended for all women beginning at age 50 and continuing until age 75 unless pathology has been detected. It may be prudent to begin mammography at an earlier age for women at high risk for breast cancer. Although the teaching of breast self-examination is not specifically recommended at this time, there is insufficient evidence to recommend any change in current breast self- examination practices (i.e., those who are now teaching it should continue the practice). |
|
Colorectal |
There is insufficient evidence to recommend for or against fecal occult blood testing or sigmoidoscopy as effective screening tests for colorectal cancer in asymptomatic individuals. There are also insufficient grounds for discontinuing this form of screening where it is currently practiced or for withholding it from persons who request it. It may be clinically prudent to offer screening to persons aged 50 or older with known risk factors for colorectal cancer. |
|
Cervical |
Regular Papanicolaou (Pap) testing is recommended for all women who are or have been sexually active. Pap smears should begin with the onset of sexual activity and should be repeated every one to three years at the physician’s discretion. They may be discontinued at age 65 if previous smears have been consistently normal. |
|
Prostate |
There is insufficient evidence to recommend for or against routine digital rectal examination as an effective screening test for prostate cancer in asymptomatic men. Transrectal ultrasound and serum tumor markers are not recommended for routine screening in asymptomatic men. |
|
Lung |
Screening asymptomatic persons for lung cancer by performing routine chest radiography or sputum cytology is not recommended. |
|
Skin |
Routine screening for skin cancer is recommended for persons at high risk. Clinicians should advise all patients with increased outdoor exposure to use sunscreen preparations and other measures to protect from ultraviolet rays. Currently there is no evidence for or against advising patients to perform skin self-examination. |
|
Testicular |
Periodic screening for testicular cancer by testicular examination is recommended for men with a history of cryptorchidism, orchiopexy, or testicular atrophy. There is no evidence of clinical benefit or harm to recommend for or against routine screening of other men for testicular cancer. Currently there is insufficient evidence for or against counseling patients to perform periodic self-examination of the testicles. |
|
Ovarian |
Screening of asymptomatic women for ovarian cancer is not recommended. It is prudent to examine the adnexa when performing gynecologic examinations for other reasons. |
|
Pancreatic |
Routine screening for pancreatic cancer in asymptomatic persons is not recommended. |
|
Oral |
Routine screening of asymptomatic persons for oral cancer by primary care clinicians is not recommended. All patients should be counseled to receive regular dental examinations, to discontinue the use of all forms of tobacco, and to limit consumption of alcohol. |
Source: Preventive Services Task Force 1989.
Screening for breast cancer
There is a general consensus among experts that screening with mammography combined with clinical breast examination every one to two years will save lives among women aged 50 to 69, reducing breast cancer deaths in this age group by up to 30%. Experts have not reached agreement, however, on the value of breast cancer screening with mammography for asymptomatic women aged 40 to 49. The NCI recommends that women in this age group should be screened every one to two years and that women at increased risk for breast cancer should seek medical advice about whether to begin screening before age 40.
The female population in most organizations may be too small to warrant the installation of mammography equipment onsite. Accordingly, most programs sponsored by employers or labor unions (or both) rely on contracts with providers who bring mobile units to the workplace or on providers in the community to whom participating female employees are referred either during working hours or on their own time. In making such arrangements, it is essential to be sure that the equipment meets standards for x-ray exposure and safety such as those promulgated by the American College of Radiology, and that the quality of the films and their interpretation is satisfactory. Further, it is imperative that a referral resource be prearranged for those women who will require a small needle aspiration or other confirmatory diagnostic procedures.
Screening for cervical cancer
Scientific evidence strongly suggests that regular screening with Pap tests will significantly decrease mortality from cervical cancer among women who are sexually active or who have reached the age of 18. Survival appears to be directly related to the stage of the disease at diagnosis. Early detection, using cervical cytology, is currently the only practical means of detecting cervical cancer in localized or premalignant stages. The risk of developing invasive cervical cancer is three to ten times greater in women who have never been screened than in those who have had Pap tests every two or three years.
Of particular relevance to the cost of workplace screening programs is the fact that cervical cytology smears can be obtained quite efficiently by properly trained nurses and do not require the involvement of a physician. Perhaps of even greater importance is the quality of the laboratory to which they are sent for interpretation.
Screening for colorectal cancer
It is generally agreed that early detection of precancerous colorectal polyps and cancers by periodic tests for fecal blood, as well as digital rectal and sigmoidoscopic examinations, and their timely removal, will reduce mortality from colorectal cancer among individuals aged 50 and over. The examination has been made less uncomfortable and more reliable with the replacement of the rigid sigmoidoscope by the longer, flexible fibreoptic instrument. There remains, however, some disagreement as to which tests should be relied upon and how often they should be applied.
Pros and cons of screening
There is general agreement about the value of cancer screening in individuals at risk because of family history, prior occurrence of cancer, or known exposure to potential carcinogens. But there appear to be justifiable concerns about the mass screening of healthy populations.
Advocates of mass screening for the detection of cancer are guided by the premise that early detection will be followed by improvements in morbidity and mortality. This has been demonstrated in some instances, but is not always the case. For example, although it is possible to detect lung cancer earlier by use of chest x rays and sputum cytology, this has not led to any improvement in treatment outcomes. Similarly, concern has been expressed that increasing the lead time for treatment of early prostatic cancers may not only be without benefit but may, in fact, be counterproductive in view of the longer period of well-being enjoyed by patients whose treatment is delayed.
In planning mass screening programs, consideration must also be given to the impact on the well-being and pocketbooks of patients with false positives. For example, in several series of cases, 3 to 8% of women with positive breast screenings had unnecessary biopsies for benign tumors; and in one experience with the fecal blood test for colorectal cancer, nearly one-third of those screened were referred for diagnostic colonoscopy, and most of them showed negative results.
It is clear that additional research is needed. To assess the efficacy of screening, the NCI has launched a major study, the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trials (PLCO) to evaluate early detection techniques for these four cancer sites. Enrolment for the PLCO began in November 1993, and will involve 148,000 men and women, aged 60 to 74 years, randomized to either the intervention or the control group. In the intervention group, men will be screened for lung, colorectal and prostatic cancer while women will be screened for lung, colorectal and ovarian cancer; those assigned to the control group will receive their usual medical care. For lung cancer, the value of an annual single-view chest x ray will be studied; for colorectal cancer, annual fibreoptic sigmoidoscopy will be performed; for prostate cancer, digital rectal examination and a blood test for PSA will be done; and for ovarian cancer, yearly physical and transvaginal ultrasound examinations will be supplemented by an annual blood test for the tumor marker known as CA-125. At the end of 16 years and the expenditure of US$ 87.8 million, it is hoped that solid data will be obtained about how screening may be used to obtain early diagnoses that may extend lives and reduce mortality.
Treatment and Continuing Care
Treatment and continuing care comprise efforts to enhance the quality of life for those in whom a cancer has taken hold and for those involved with them. Occupational health services and employee assistance programs sponsored by employers and unions can provide useful counsel and support to workers being treated for cancer or who have a dependant receiving treatment. This support can include explanations of what is going on and what to expect, information that is sometimes not provided by oncologists and surgeons; guidance in referrals for second opinions; and consultations and assistance with regard to access to centers of highly specialized care. Leaves of absence and modified work arrangements may make it possible for workers to remain productive while in treatment and to return to work earlier when a remission is achieved. In some workplaces, peer support groups have been formed to provide an exchange of experiences and mutual support for workers facing similar problems.
Conclusion
Programs for the prevention and detection of cancer can make a meaningful contribution to the well-being of the workers involved and their dependants and yield a significant return to the employers and labor unions that sponsor them. As with other preventive interventions, it is necessary that these programs be properly designed and carefully implemented and, since their benefits will accrue over many years, they should be continued on a steady basis.
Health Risk Appraisal
Introduction
Over the last few decades, the health risk appraisal (HRA), also known as a health hazard appraisal or a health risk assessment, has become increasingly popular, primarily in the United States, as an instrument for promoting health awareness and motivating behavioral change. It is also used as an introduction to periodic health screening or as a substitute for it and, when aggregated for a group of individuals, as the basis for identifying targets for a health education or health promotion program to be designed for them. It is based on the following concept:
- Ostensibly healthy, asymptomatic individuals may be at risk of developing a disease process that can cause morbidity in the future and may lead to premature death.
- Factors that lead to such risk can be identified.
- Some of those risk factors can be eliminated or controlled thereby preventing or attenuating the disease process and preventing or delaying the morbidity and mortality.
The development of the HRA in the 1940s and 1950s is credited to Dr. Lewis Robbins, working at the Framingham prospective study of heart disease and later at the National Cancer Institute (Beery et al. 1986). The 1960s saw additional models developed and, in 1970, Robbins and Hall produced the seminal work that defined the technique, described the survey instruments and the risk computations, and outlined the patient feedback strategy (Robbins and Hall 1970).
Interest in HRA and health promotion in general was stimulated by a growing awareness of the importance of risk factor control as a basis element in health promotion, the evolving use of computers for data compilation and analysis and, especially in the United States, increasing concern over the escalating cost of health care and the hope that preventing illness might slow its upward spiral of growth. By 1982, Edward Wagner and his colleagues at the University of North Carolina were able to identify 217 public and private HRA vendors in the United States (Wagner et al. 1982). A good many of these have since faded from the scene but they have been replaced, at least to a limited extent, by new entrants into the marketplace. According to a 1989 report of a survey of a random sample of US worksites, 29.5% have conducted HRA activities; for worksites with more than 750 employees, this figure rose to 66% (Fielding 1989). HRA use in other countries has lagged considerably.
What is the HRA?
For purposes of this article, an HRA is defined as a tool for assessing health risks that has three essential elements:
- A self-administered questionnaire inquiring about the individual’s demographic profile, medical background, family history, personal habits and lifestyle. This information is frequently supplemented by biomedical measurements such as height, weight, blood pressure, and skin-fold thickness, and data regarding the results of urinalysis, blood cholesterol level and other laboratory tests, either as reported by the individual or taken as part of the process.
- A quantitative estimation of the individual’s future risk of death or other adverse outcomes from specific causes based on a comparison of the individual’s responses to epidemiological data, national mortality statistics and actuarial calculations. Some questionnaires are self-scored: points are assigned to the response to each question and then added to derive a risk score. With the appropriate computer software, the responses may be entered into a microcomputer that will calculate the score. Most often the completed questionnaires are forwarded to a central point for batch processing and the individual results are mailed or delivered to the participants.
- Feedback to the individual with suggestions for changes in lifestyle and other actions that would improve well-being and reduce the risk of disease or premature death.
Originally, the total risk estimate was presented as a single number that could be targeted for reduction to a “normal” value or even to lower-than-normal values (vis-à-vis the general population) by implementing the suggested behavioral changes. To make the results more graphic and compelling, the risk is now sometimes expressed as a “health age” or “risk age” to be compared with the individual’s chronological age, and an “achievable age” as the target for the interventions. For example, a report might say, “Your present age is 35 but you have the life expectancy of a person aged 42. By following these recommendations, you could reduce your risk age to 32, thereby adding ten years to your projected life span.”
Instead of comparing the individual’s health status with the “norm” for the general population, some HRAs offer an “optimal health” score: the best attainable score that might be achieved by following all of the recommendations. This approach appears to be particularly useful in guiding young people, who may not yet have accumulated significant health risks, to an optimally desirable lifestyle.
The use of a “risk age” or a single number to represent the individual’s composite risk status may be misleading: a significant risk factor may be statistically offset by “good” scores on most other areas and lead to a false sense of security. For example, a person with normal blood pressure, a low blood cholesterol level, and a good family history who exercises and wears automobile seat belts may earn a good risk score despite the fact that he smokes cigarettes. This suggests the desirability of focusing on each “greater than average” risk item instead of relying on the composite score alone.
The HRA is not to be confused with health status questionnaires that are used to classify the eligibility of patients for particular treatments or to evaluate their outcomes, nor with the variety of instruments used to assess degree of disability, mental health, health distress or social functioning, although such scales are sometimes incorporated into some HRAs.
HRA Questionnaire
Although the HRA is sometimes used as a prelude to or part of a periodic, pre-employment or pre-placement medical examination, it is usually offered independently as a voluntary exercise. Many varieties of HRA questionnaires are in use. Some are limited to core questions that feed directly into the risk age calculations. In others, these core questions are interspersed with additional medical and behavioral topics: more extensive medical history; stress perceptions; scales to measure anxiety, depression and other psychological disorders; nutrition; use of preventive services; personal habits and even interpersonal relationships. Some vendors allow purchasers to add questions to the questionnaire, although responses to these are not usually incorporated into the health-risk computations.
Almost all HRAs now use forms with boxes to be checked or filled in by pencil for computer entry by hand or by an optical scanner device. As a rule, the completed questionnaires are collected and batch-processed, either in-house or by the HRA vendor. To encourage trust in the confidentiality of the program, completed questionnaires are sometimes mailed directly to the vendor for processing and the reports are mailed to the participants’ homes. In some programs, only “normal” results are mailed to participants, while those employees with results calling for intervention are invited for private interviews with trained staff persons who interpret them and outline the corrective actions that are indicated. Greater access to personal computers and more widespread familiarity with their use have led to the development of interactive software programs that allow direct entry of the responses into a microcomputer and immediate calculation and feedback of the results along with risk reduction recommendations. This approach leaves it up to the individual to take the initiative of seeking help from a staff person when clarification of the results and their implications is needed. Except when the software program allows storage of the data or their transfer to a centralized data bank, this approach does not provide information for systematic follow-up and it precludes the development of aggregate reports.
Managing the Program
Responsibility for managing the HRA program is usually assigned to the respective directors of the employee health service, the wellness program or, less frequently, the employee assistance program. Quite often, however, it is arranged and supervised by the personnel/human resources staff. In some instances, an advisory committee is created, often with employee or labor union participation. Programs incorporated into the organization’s operating routine appear to run more smoothly than those that exist as somewhat isolated projects (Beery et al. 1986). The organizational location of the program may be a factor in its acceptance by employees, particularly when confidentiality of personal health information is an issue. To preclude such a concern, the completed questionnaire is usually mailed in a sealed envelope to the vendor, who processes the data and mails the individual report (also in a sealed envelope) directly to the participant’s home.
To enhance participation in the program, most organizations publicize the program through preliminary hand-outs, posters and articles in the company newsletter. Occasionally, incentives (e.g., T-shirts, books and other prizes) are offered for completion of the exercise and there may even be monetary awards (e.g., reduction in the employee’s contribution to health insurance premiums) for successful reduction of excess risk. Some organizations schedule meetings where employees are told about the program’s purposes and procedures and are instructed in completing the questionnaire. Some, however, simply distribute a questionnaire with written instructions to each employee (and, if included in the program, to each dependant). In some instances, one or more reminders to complete and mail the questionnaire are distributed in order to increase participation. In any case, it is important to have a designated resource person, either in the organization or with the HRA program provider, to whom questions can be directed in person or by telephone. It may be important to note that, even when the questionnaire is not completed and returned, merely reading it can reinforce information from other sources and foster a health consciousness that may favorably influence future behavior.
Many of the forms call for clinical information that the respondent may or may not have. In some organizations, the program staff actually measures height, weight, blood pressure and skin-fold thickness and collects blood and urine samples for laboratory analysis. The results are then integrated with the questionnaire responses; where such data are not entered, the computer processing program may automatically insert figures representing the “norms” for persons of the same sex and age.
Turnaround time (the time between completing the questionnaire and receiving the results) may be a significant factor in the value of the program. Most vendors promise delivery of the results in ten days to two weeks, but batch processing and post office delays may extend this period. By the time the reports are received, some participants may have forgotten how they responded and may have disassociated themselves from the process; to obviate this possibility, some vendors either return the completed questionnaire or include key responses of the individual in the report.
Reports to the Individual
The reports may vary from a single-page statement of results and recommendations to a more than 20-page brochure replete with multicolor graphs and illustrations and extended explanations of the relevance of the results and the importance of the recommendations. Some rely almost entirely on preprinted general information while in others the computer generates an entirely individualized report. In some programs where the exercise has been repeated and the earlier data have been retained, comparisons of current results with those recorded earlier are provided; this may provide a sense of gratification that can serve as further motivation for behavior modification.
A key to the success of a program is the availability of a health professional or trained counselor who can explain the importance of the findings and offer an individualized program of interventions. Such personalized counseling can be extremely useful in allaying needless anxiety that may have been generated by misinterpretation of the results, in helping individuals establish behavioral change priorities, and in referring them to resources for implementation.
Reports to the Organization
In most programs, the individual results are summarized in an aggregate report sent to the employer or sponsoring organization. Such reports tabulate the demography of the participants, sometimes by geographic location and job classification, and analyze the range and levels of health risks discovered. A number of HRA vendors include projections of the increased health care costs likely to be incurred by high-risk employees. These data are extremely valuable in designing elements for the organization’s wellness and health promotion program and in stimulating consideration of changes in job structure, work environment and workplace culture that will promote the health and well-being of the workforce.
It should be noted that the validity of the aggregate report depends on the number of employees and the level of participation in the HRA program. Participants in the program tend to be more health conscious and, when their number is relatively small, their scores may not accurately reflect the characteristics of the entire workforce.
Follow-up and Evaluation
The effectiveness of the HRA program may be enhanced by a system of follow-up to remind participants of the recommendations and encourage compliance with them. This can involve individually addressed memoranda, one-on-one counseling by a physician, nurse or health educator, or group meetings. Such follow-up is particularly important for high-risk individuals.
HRA program evaluation should start with a tabulation of the level of participation, preferably analyzed by such characteristics as age, sex, geographic location or work unit, job and educational level. Such data may identify differences in acceptance of the program that might suggest changes in the way it is presented and publicized.
Increased participation in risk-reduction elements of the wellness program (e.g., a fitness program, smoking cessation courses, stress management seminars) may indicate that HRA recommendations are being heeded. Ultimately, however, evaluation will involve determination of changes in risk status. This may involve analyzing the results of the follow-up of high-risk individuals or repetition of the program after an appropriate interval. Such data may be fortified by correlation with data such as utilization of health benefits, absenteeism or productivity measures. Appropriate recognition, however, should be given to other factors that may have been involved (e.g., bias reflecting the sort of person who returns for retest, regression to the mean, and secular trends); truly scientific evaluation of the program impact requires a randomized prospective clinical trial (Schoenbach 1987; DeFriese and Fielding 1990).
Validity and Utility of the HRA
Factors that may affect the accuracy and validity of an HRA have been discussed elsewhere (Beery et al. 1986; Schoenbach 1987; DeFriese and Fielding 1990) and will only be listed here. They represent a checklist for workplace decision makers evaluating different instruments, and include the following:
- accuracy and consistency of self-reported information
- completeness and quality of the epidemiological and actuarial data on which the risk estimates are based
- limitations of the statistical methods for calculating risk, including combining risk factors for different problems into a single composite score and the distortions produced by substituting “average” values either for missing responses in the questionnaire or for measurements not taken
- reliability of the method for calculating the benefits of risk reduction
- applicability of the same mortality calculations to the young whose death rates are low and to older individuals for whom age alone may be the most significant factor in mortality. Furthermore, the validity of the HRA when applied to populations different from those on whom most of the research has been done (i.e., women, minorities, people of different educational and cultural backgrounds) must be regarded from a critical point of view.
Questions have also been raised about the utility of the HRA based on considerations such as the following:
- The primary focus of HRA is on life expectancy. Until recently, little or no attention has been paid to factors primarily influencing morbidity from conditions that are not usually fatal but which may have an even greater impact on well-being, productivity and health-related costs (e.g., arthritis, mental disorders, and long-term effects of treatments intended to reduce specific risks). The problem is the lack of good morbidity databases for the general population, to say nothing of subgroups defined by age, sex, race or ethnicity.
- Concern has been expressed about the ill effects of anxiety generated by reports of high-risk status reflecting factors which the individual is unable to modify (e.g., age, heredity, and past medical history), and about the possibility that reports of “normal” or low-risk status may lead individuals to ignore potentially significant signs and symptoms that were not reported or which developed after the HRA was completed.
- Participation in an HRA programme is usually voluntary, but allegations of coercion to participate or to follow the recommendations have been made.
- Charges of “blaming the victim” have rightfully been levelled at employers who offer HRA as part of a health promotion programme but do little or nothing to control health risks in the work environment.
- Confidentiality of personal information is an ever-present concern, especially when an HRA is conducted as an in-house programme and abnormal findings appear to be a trigger for discriminatory actions.PP9
Evidence of the value of health-risk reduction has been accumulating. For example, Fielding and his associates at Johnson and Johnson Health Management, Inc., found that the 18,000 employees who had completed the HRA provided through their employers used preventive services at a considerably higher rate than a comparable population responding to the National Health Interview Survey (Fielding et al. 1991). A five-year study of almost 46,000 DuPont employees demonstrated that those with any of the six behavioral cardiovascular risk factors identified by an HRA (e.g., cigarette smoking, high blood pressure, high cholesterol levels, lack of exercise) had significantly higher rates of absenteeism and use of health care benefits as compared to those without such risk factors (Bertera 1991). Furthermore, applying multivariate regression models to 12 health-related measures taken mainly from an HRA allowed Yen and his colleagues at the University of Michigan Fitness Research Center to predict which employees would generate higher costs for the employer for medical claims and absenteeism (Yen, Edington and Witting 1991).
Implementing an HRA Program
Implementing an HRA program is not a casual exercise and should not be undertaken without careful consideration and planning. The costs of an individual questionnaire and its processing may not be great but the aggregate costs to the organization may be considerable when such items as staff time for planning, implementation and follow-up, employee time for completing the questionnaires, and adjunct health-promotion programs are included. Some factors to be considered in implementation are presented in figure 1.
Figure 1. Checklist for health risk appraisal (HRA) implementation.
Should we have an HRA program?
An increasing number of companies, at least in the United States, are answering this question in the affirmative, abetted by the growing number of vendors energetically marketing HRA programs. The popular media and “trade” publications are replete with anecdotes describing “successful” programs, while in comparison there is a paucity of articles in professional journals offering scientific evidence of the accuracy of their results, their practical reliability and their scientific validity.
It seems clear that defining one’s health risk status is a necessary basis for risk reduction. But, some ask, does one need a formal exercise like the HRA to do this? By now, virtually everyone who persists in cigarette smoking has been exposed to evidence of the potential of adverse health effects, and the benefits of proper nutrition and physical fitness have been well publicized. Proponents of HRA counter by pointing out that receiving an HRA report personalizes and dramatizes the risk information, creating a “teachable moment” that can motivate individuals to take appropriate action. Further, they add, it can highlight risk factors of which the participants may have been unaware, allowing them to see just what their risk reduction opportunities are and to develop priorities for addressing them.
There is general agreement that HRA has limited value when used as a stand-alone exercise (i.e., in the absence of other modalities) and that its utility is fully realized only when it is part of an integrated health promotion program. That program should offer not only individualized explanations and counseling but also access to intervention programs that address the risk factors that were identified (these interventions may be provided in-house or in the community). Thus, the commitment to offer HRA must be broadened (and perhaps may become more costly) by offering or making available such activities as smoking cessation courses, fitness activities and nutrition counseling. Such a broad commitment should be made explicitly in the statement of objectives for the program and the budget allocation requested to support it.
In planning an HRA program, one must decide whether to offer it to the entire workforce or only to certain segments (e.g., to salaried or hourly workers, to both, or to workers of specified ages, lengths of service or in specified locations or job categories); and whether to extend the program to include spouses and other dependants (who, as a rule, account for more than half of the utilization of health benefits). A critical factor is the need to secure the availability of at least one person in the organization sufficiently knowledgeable and appropriately positioned to supervise the design and implementation of the program and the performance of both the vendor and the in-house staff involved.
In some organizations in which full-scale annual medical examinations are being eliminated or offered less frequently, HRA has been offered as a replacement either alone or in combination with selected health screening tests. This strategy has merit in terms of enhancing the cost/benefit ratio of a health promotion program, but sometimes it is based not so much on the intrinsic value of the HRA but on the desire to avoid the ill-will that might be generated by what could be perceived as elimination of an established employee benefit.
Conclusion
Despite its limitations and the paucity of scientific research that confirms the claims for its validity and utility, the use of HRA continues to grow in the United States and, much less rapidly, elsewhere. DeFriese and Fielding, whose studies have made them authorities on HRA, see a bright future for it based on their prediction of new sources of risk-relevant information and new technological developments such as improvements in computer hardware and software that will permit direct computer entry of questionnaire responses, allow modeling of the effects of changes in health behavior, and produce more effective full-color reports and graphics (DeFriese and Fielding 1990).
HRA should be used as an element in a well-conceived, continuing program of wellness or health promotion. It conveys an implicit commitment to provide activities and changes in the workplace culture that offer opportunities to help control the risk factors it will identify. Management should be aware of such a commitment and be willing to make the requisite budget allocations.
While much research remains to be done, many organizations will find HRA a useful adjunct to their efforts to improve the health of their employees. The implicit scientific authority of the information it provides, the use of computer technology, and the personalized impact of the results in terms of chronological versus risk age seem to enhance its power to motivate participants to adopt healthy, risk-reducing behaviors. Evidence is accumulating to show that employees and dependants who maintain healthy risk profiles have less absenteeism, demonstrate enhanced productivity, and use less medical care, all of which have a positive effect on the organization’s “bottom line”.
Health Protection and Promotion in the Workplace: An Overview
It has often been said that the workforce is the most critical element in the productive apparatus of the organization. Even in highly automated plants with their smaller number of workers, decrements in their health and well-being will sooner or later be reflected in impaired productivity or, sometimes, even in disasters.
Through governmental legislation and regulation, employers have been made responsible for maintaining the safety of the work environment and work practices, and for the treatment, rehabilitation and compensation of workers with occupational injuries and disease. In recent decades, however, employers have begun to recognize that disabilities and absences are costly even when they originate outside the workplace. Consequently, they have begun to provide more and more comprehensive health promotion and protection programs not only for employees but for their families as well. In opening a 1987 meeting of a World Health Organization (WHO) Expert Committee on Health Promotion in the Worksetting, Dr. Lu Rushan, Assistant Director-General of WHO, reiterated that WHO viewed workers’ health promotion as an essential component of occupational health services (WHO 1988).
Why the Workplace?
The rationale for employer sponsorship of health promotion programs includes preventing loss of worker productivity due to avoidable illnesses and disability and their associated absenteeism, improving employee well-being and morale, and controlling the costs of employer-paid health insurance by reducing the amount of health care services required. Similar considerations have stimulated union interest in sponsoring programs, particularly when their members are scattered among many organizations too small to mount effective programs on their own.
The workplace is uniquely advantageous as an arena for health protection and promotion. It is the place where workers congregate and spend a major portion of their waking hours, a fact that makes it convenient to reach them. In addition to this propinquity, their camaraderie and sharing of similar interests and concerns facilitate the development of peer pressures that can be a powerful motivator for participation and persistence in a health promotion activity. The relative stability of the workforce—most workers remain in the same organization for long periods of time—makes for the continuing participation in healthful behaviors necessary to achieve their benefit.
The workplace affords unique opportunities to promote the improved health and well-being of the workers by:
- integrating the health protection and promotion programme into the organization’s efforts to control occupational diseases and injuries
- modifying the structure of the job and its environment in ways that will make it less hazardous and less stressful
- providing employer- or union-sponsored programmes designed to enable employees to cope more effectively with personal or family burdens that may impinge on their well-being and work performance (i.e., modified work schedules and financial assistance benefits and programmes that address alcohol and drug abuse, pregnancy, child care, caring for elderly or disabled family members, marital difficulties or planning for retirement).
Does Health Promotion Work?
There is no doubt of the efficacy of immunizations in preventing infectious diseases or of the value of good occupational health and safety programs in reducing the frequency and severity of work-related diseases and injuries. There is general agreement that early detection and appropriate treatment of incipient diseases will reduce mortality and lower the frequency and extent of residual disability from many diseases. There is growing evidence that elimination or control of risk factors will prevent or, at least, substantially delay the onset of life-threatening diseases such as stroke, coronary artery disease and cancer. There is little doubt that maintaining a healthy lifestyle and coping successfully with psychosocial burdens will improve well-being and functional capacity so as to achieve the goal of wellness defined by the World Health Organization as a state beyond the mere absence of disease. Yet some remain skeptical; even some physicians, at least to judge by their actions.
There is perhaps a higher level of skepticism about the value of worksite health promotion programs. In large part, this reflects the lack of adequately designed and controlled studies, the confounding effect of secular events such as the declining incidence of mortality from heart disease and stroke and, most important, the length of time required for most preventive measures to have their effect. However, in the Health Project report, Freis et al. (1993) summarize the growing literature confirming the effectiveness of worksite health promotion programs in reducing health care costs. In its initial review of over 200 workplace programs, the Health Project, a voluntary consortium of business leaders, health insurers, policy scholars and members of government agencies which advocate health promotion to reduce the demand and the need for health services, found eight with convincing documentation of savings in health care costs.
Pelletier (1991) assembled 24 studies of comprehensive worksite programs published in peer-review journals between 1980 and 1990. (Reports of single-focus programs, such as those dealing with hypertension screening and smoking cessation, even though demonstrated to have been successful, were not included in this review.) He defined “comprehensive programs” as those which “provide an ongoing, integrated program of health promotion and disease prevention that knits the particular components (smoking cessation, stress management, coronary risk reduction, etc.) into a coherent, ongoing program that is consistent with corporate objectives and includes program evaluation.” All of the 24 programs summarized in this review achieved improvement in employees’ health practices, reductions in absenteeism and disability, and/or increases in productivity, while each of these studies that analyzed for impact on health care and disability costs, cost-effectiveness or cost/benefit changes demonstrated a positive effect.
Two years later, Pelletier reviewed an additional 24 studies published between 1991 and the early part of 1993 and found that 23 reported positive health gains and, again, all of those studies which analyzed cost-effectiveness or cost/benefit effects indicated a positive return (Pelletier 1993). Factors common to the successful programs, he noted, included specific program goals and objectives, easy access to the program and facilities, incentives for participation, respect and confidentiality, support of top management and a corporate culture that encourages health promotion efforts (Pelletier 1991).
While it is desirable to have evidence confirming the effectiveness and value of worksite health promotion programs, the fact is that such proof has rarely been required for the decision to initiate a program. Most programs have been based on the persuasive power of the conviction that prevention does work. In some instances, programs have been stimulated by interest articulated by employees and, occasionally, by the unexpected death of a top executive or a key employee from cancer or heart disease and the fond hope that a preventive program will keep “lightning from striking twice”.
Structure of a Comprehensive Program
In many organizations, particularly smaller ones, the health promotion and disease prevention program consists merely of one or more largely ad hoc activities that are informally related to each other, if at all, that have little or no continuity, and that often are triggered by a particular event and abandoned as it fades into memory. A truly comprehensive program should have a formal structure comprising a number of integrated elements, including the following:
- a clear statement of goals and objectives that are approved by management and acceptable to the employees
- explicit endorsement by top management and, where they exist, the labour organizations involved, with the continuing allocation of resources adequate to achieve desired goals and objectives
- appropriate placement in the organization, effective coordination with other health-related activities, and communication of programme plans across divisions and departments to mid-level managers and employees. Some organizations have found it expedient to create a labour-management committee comprising representatives from all levels and segments of the workforce for “political” reasons as well as to provide input on programme design
- designation of a “programme director,” a person with the requisite administrative skills who also has had training and experience in health promotion or has access to a consultant who might supply the necessary expertise
- a mechanism for feedback from participants and, if possible, non-participants as well, in order to confirm the validity of the programme design and to test the popularity and utility of particular programme activities
- procedures for maintaining the confidentiality of personal information
- systematic record-keeping to keep track of activities, participation and outcomes as a basis for monitoring and potential evaluation
- compilation and analysis of available relevant data, ideally for a scientific evaluation of the programme or, when that is not feasible, to generate a periodic report to management to justify continuation of the resource allocation and to form a basis for possible changes in the programme.
Program Objectives and Ideology
The basic objectives of the program are to enhance and maintain the health and well-being of employees on all levels, to prevent disease and disability, and to ease the burden on individuals and the organization when disease and disability cannot be prevented.
The occupational health and safety program is directed to those factors on the job and in the workplace that may affect employees’ health. The wellness program recognizes that their health concerns cannot be confined within the boundaries of the plant or office, that problems arising in the workplace inevitably affect the health and well-being of workers (and, by extension, also their families) in the home and in the community and that, just as inevitably, problems arising outside of work affect attendance and work performance. (The term wellness can be considered the equivalent of the expression health promotion and protection, and has been used increasingly in the field during the last two decades; it epitomizes the World Health Organization’s positive definition of health.) Accordingly, it is quite appropriate for the health promotion program to address problems that some argue are not proper concerns for the organization.
The need to achieve wellness assumes greater urgency when it is recognized that workers with diminished capacities, however acquired, may be potentially hazardous to their co-workers and, in certain jobs, to the public as well.
There are those who hold that, since health is fundamentally a personal responsibility of the individual, it is inappropriate, and even intrusive, for employers or labor unions (or both) to undertake involvement with it. They are correct insofar as overly paternalistic and coercive approaches are employed. However, health-promoting adjustments of the job and the workplace along with enhanced access to health-promoting activities provide the awareness, knowledge and tools that enable employees to address that personal responsibility more effectively.
Program Components
Needs assessment
While the alert program director will take advantage of a particular event that will create interest in a special activity (e.g., the unexpected illness of a popular person in the organization, reports of cases of an infectious disease that raise fears of contagion, warnings of a potential epidemic), the comprehensive program will be based on a more formal needs assessment. This may simply consist of a comparison of the demographic characteristics of the workforce with morbidity and mortality data reported by public health authorities for such population cohorts in the area, or it may comprise the aggregate analyses of company-specific health-related data, such as health care insurance claims and the recorded causes of absenteeism and of disability retirement. Determination of the health status of the workforce through compilation of the results of health screenings, periodic medical examinations and health risk appraisal programs can be supplemented by surveys of employees’ health-related interests and concerns to identify optimal targets for the program. (It should be borne in mind that health problems affecting particular cohorts of employees that warrant attention may be obscured by relying only on data aggregated for the entire workforce.) Such needs assessments are not only useful in selecting and prioritizing program activities but also in planning to “market” them to the employees most likely to find them beneficial. They also provide a benchmark for measuring the effectiveness of the program.
Program elements
A comprehensive health promotion and disease prevention program includes a number of elements, such as the following.
Promoting the program
A constant stream of promotional devices, such as handbills, memoranda, posters, brochures, articles in company periodicals, etc., will serve to call attention to the availability and desirability of participating in the program. With their permission, stories of the accomplishments of individual employees and any awards for achieving health promotion goals they may have earned may be highlighted.
Health assessment
Where possible, each employee’s health status should be assessed on entering the program to provide a basis for a “prescription” of personal objectives to be achieved and of the specific activities that are indicated, and periodically to assess progress and interim changes in health status. The health risk appraisal may be used with or without a medical examination as comprehensive as circumstances permit, and supplemented by laboratory and diagnostic studies. Health screening programs can serve to identify those for whom specific activities are indicated.
Activities
There is a long list of activities that may be pursued as part of the program. Some are continuing, others are addressed only periodically. Some are targeted to individuals or to particular cohorts of the workforce, others to the entire employee population. Prevention of illness and disability is a common thread that runs through each activity. These activities may be divided into the following overlapping categories:
- Clinical services. These require health professionals and include: medical examinations; screening programmes; diagnostic procedures such as mammography; Pap smears and tests for cholesterol level; immunizations and so forth. They also include counseling and behaviour modification in relation to weight control, fitness, smoking cessation and other lifestyle factors.
- Health education. Education to promote awareness of potential diseases, the importance of controlling risk factors, and the value of maintaining healthy lifestyles, for instance, through weight control, fitness training and smoking cessation. Such education should also point the way to appropriate interventions.
- Guidance in managing medical care. Advice should be given with regard to the following concerns: dealing with the health care system and procuring prompt and high-quality medical care; managing chronic or recurrent health problems; rehabilitation and return to work after disease or injury; treatment for alcohol and drug abuse; prenatal care and so on.
- Coping with personal problems. Coping skills to be developed include, for example, stress management, pre-retirement planning and outplacement. Help can also be provided for workers who need to deal with work and family problems such as family planning, prenatal care, dependant care, parenting, and so forth.
- Workplace amenities and policies. Workplace features and policies supplementary to those addressing occupational health and safety activities would include personal washing-up and locker facilities, laundry service where needed, catering facilities offering nutrition advice and helpful food choices, and the establishment of a smoke-free and drug-free workplace, among others.
In general, as programs have developed and expanded and awareness of their effectiveness has spread, the number and variety of activities have grown. Some, however, have been de-emphasized as resources have either been reduced because of financial pressures or shifted to new or more popular areas.
Tools
The tools employed in pursuing health promotion activities are determined by the size and location of the organization, the degree of centralization of the workforce with respect to geography and work schedules; the available resources in terms of money, technology and skills; the characteristics of the workforce (as regards educational and social levels); and the ingenuity of the program director. They include:
- Information gathering: employee surveys; focus groups
- Print materials: books; pamphlets (these may be distributed or displayed in take-away racks); pay envelope stuffers; articles in company publications; posters
- Audiovisual materials: audiotapes; recorded messages accessible by telephone; films; videos for both individual and group viewing. Some organizations maintain libraries of audiotapes and videos which employees may borrow for home use
- Professional health services: medical examinations; diagnostic and laboratory procedures; immunizations; individual counselling
- Training: first aid; cardiopulmonary resuscitation; healthy shopping and cooking
- Meetings: lectures; courses; workshops
- Special events: health fairs; contests
- Self-help and support groups: alcohol and drug abuse; breast cancer; parenting; eldercare
- Committees: an intramural task force or committee to coordinate health-related programmes among different departments and divisions and a labour-management committee for overall programme guidance are often useful. There may also be special committees centred on particular activities
- Sports programmes: intramural sports; the sponsoring of individual participation in community programmes; company teams
- Computer software: available for individual personal computers or accessed through the organization’s network; health-promotion-oriented computer or video games
- Screening programmes: general (e.g., health risk appraisal) or disease specific (e.g., hypertension; vision and hearing; cancer; diabetes; cholesterol)
- Information and referral: employee assistance programmes; telephone resource for personal questioning and advice
- Ongoing activities: physical fitness; healthful food selection in worksite catering facilities and vending machines
- Special benefits: released time for health promotion activities; tuition reimbursement; modified work schedules; leaves of absence for particular personal or family needs
- Incentives: awards for participation or goals achievement; recognition in company publications and on bulletin boards; contests and prizes.
Implementing the Program
In many organizations, particularly smaller ones, health promotion activities are pursued on an ad hoc, haphazard basis, often in response to actual or threatened health “crises” in the workforce or in the community. After a time, however, in larger organizations, they are often pulled together into a more or less coherent framework, labelled “a program,” and made the responsibility of an individual designated as program director, coordinator or given some other title.
Selection of activities for the program may be dictated by the responses to employee interest surveys, secular events, the calendar or the suitability of the available resources. Many programs schedule activities to take advantage of the publicity generated by the categorical voluntary health agencies in connection with their annual fund-raising campaigns, for example, Heart Month, or National Fitness and Sports Week. (Each September in the United States, the National Health Information Center in the Office of Disease Prevention and Health Protection publishes National Health Observances, a list of the designated months, weeks and days devoted to the promotion of particular health issues; it is now also available via electronic mail.)
It is generally agreed that it is prudent to install the program incrementally, adding activities and topics as it gains credibility and support among the employees and to vary the topics to which special emphasis is given so that the program does not become stale. J.P. Morgan & Co., Inc., the large financial organization based in New York City, has instituted an innovative “scheduled cyclical format” in its health promotion program that emphasizes selected topics sequentially over a four-year period (Schneider, Stewart and Haughey 1989). The first year (the Year of the Heart) focuses on cardiovascular disease prevention; the second (the Year of the Body) addresses AIDS and early cancer detection and prevention; the third (the Year of the Mind) deals with psychological and social issues; and the fourth (the Year of Good Health) covers such significant topics as adult immunization, arthritis and osteoporosis, accident prevention, diabetes and healthy pregnancy. At this point, the sequence is repeated. This approach, Schneider and his co-authors state, maximizes involvement of available corporate and community resources, encourages employee participation by sequential attention to different issues, and affords the opportunity for directing attention to program revisions and additions based on medical and scientific advances.
Evaluating the Program
It is always desirable to evaluate the program both to justify continuation of its resource allocations and to identify any need for improvement and to support recommendations for expansion. The evaluation may range from simple tabulations of participation (including drop-outs) coupled with expressions of employee satisfaction (solicited and unsolicited) to more formal surveys. The data obtained by all these means will demonstrate the degree of utilization and the popularity of the program as a whole entity and of its individual components, and are usually readily available soon after the end of the evaluation period.
Even more valuable, however, are data reflecting the outcomes of the program. In an article pointing the way to improving evaluations of health promotion programs, Anderson and O’Donnell (1994) offer a classification of areas in which health promotion programs may have significant results (see figure 1).
Figure 1. Categories of health promotion outcomes.
Outcome data, however, require an effort planned prior to the outset of the program, and they have to be collected over a time sufficient to allow the outcome to develop and be measured. For example, one can count the number of individuals who receive an influenza immunization and then follow the total population for a year to demonstrate that those inoculated had a lower incidence of influenza-like respiratory infections than those who refused the inoculation. The study can be enlarged to correlate rates of absenteeism of the two cohorts and compare the program costs with the direct and indirect savings accrued by the organization.
Furthermore, it is not too difficult to demonstrate individuals’ achievement of more desirable profiles of risk factors for cardiovascular disease. However, it will take at least one and probably several decades to demonstrate a reduction in morbidity and mortality from coronary heart disease in an employee population cohort. Even then, the size of that cohort may not be large enough to make such data significant.
The review articles cited above demonstrate that good evaluation research can be done and that it is increasingly being undertaken and reported. There is no question of its desirability. However, as Freis and his co-authors (1993) said, “There are already model programs that improve health and decrease costs. It is not knowledge that is lacking, but penetration of these programs into a greater number of settings.”
Comments and Caveats
Organizations contemplating the launching of a health promotion program should be cognizant of a number of potentially sensitive ethical issues to be considered and a number of pitfalls to avoid, some of which have already been alluded to. They are comprised under the following headings:
Elitism versus egalitarianism
A number of programs exhibit elitism in that some of the activities are limited to individuals above a certain rank. Thus, an in-plant physical fitness facility may be restricted to executives on the grounds that they are more important to the organization, they work longer hours, and they find it difficult to free up the time to go to an outside “health club”. To some, however, this seems to be a “perk” (i.e., a special privilege), like the key to the private washroom, admission to the free executive dining room, and use of a preferred parking space. It is sometimes resented by rank-and-file workers who find visiting a community facility too expensive and are not allowed the liberty of taking time during the working day for exercise.
A more subtle form of elitism is seen in some in-plant fitness facilities when the quota of available memberships is taken up by “jocks” (i.e., exercise enthusiasts) who would probably find ways to exercise anyway. Meanwhile, those who are sedentary and might derive much greater benefit from regular supervised exercise are denied entry. Even when they make it into the fitness program, their continued participation is often discouraged by embarrassment at being outperformed by lower-ranking workers. This is particularly true of the manager whose male self-image is tarnished when he finds that he cannot perform at the level of his female secretary.
Some organizations are more egalitarian. Their fitness facilities are open to all on a first-come, first-served basis, with continuing membership available only to those who use it frequently enough to be of value to them. Others go part of the way by reserving some of the memberships for employees who are being rehabilitated following an illness or injury, or for older workers who may require a greater inducement to participate than their younger colleagues.
Discrimination
In some areas, anti-discrimination laws and regulations may leave the organization open to complaints, or even litigation, if the health promotion program can be shown to have discriminated against certain individuals on the basis of age, sex or membership in minority or ethnic groups. This is not likely to happen unless there is a more pervasive pattern of bias in the workplace culture but discrimination in the health promotion program might trigger a complaint.
Even if formal charges are not made, however, resentment and dissatisfaction, which may be magnified as they are communicated informally among employees, are not conducive to good employee relations and morale.
Concern about allegations of sex discrimination may be exaggerated. For example, even though it is not recommended for routine use in asymptomatic men (Preventive Services Task Force 1989), some organizations offer screening for prostatic cancer to compensate for making Pap tests and mammography available to female employees.
Complaints of discrimination have come from individuals who are denied the opportunity of winning incentive awards because of congenital health problems or acquired diseases that preclude participation in health promotion activities or achieving the ideal personal health goals. At the same time, there is the equity issue of rewarding individuals for correcting a potential health problem (e.g., giving up smoking or losing excess weight) while denying such rewards to individuals who do not have such problems.
“Blaming the victim”
Growing out of the valid concept that health status is a matter of personal responsibility is the notion that individuals are culpable when health defects are found and are to be held guilty for failing to correct them on their own. This sort of thinking fails to take notice of the fact that genetic research is increasingly demonstrating that some defects are hereditary and, therefore, although they may sometimes be modified, are beyond the individual’s capacity to correct.
Examples of “blaming the victim” are (a) the too-prevalent attitude that HIV/AIDS is a fitting retribution for sexual “indiscretions” or intravenous drug use and, therefore, its victims do not deserve compassion and care, and (b) the imposition of financial and bureaucratic barriers that make it difficult for unmarried young women to get adequate prenatal care when they become pregnant.
Most important, focusing in the workplace on individuals’ responsibility for their own health problems tends to obscure the employer’s accountability for factors in job structure and work environment that may be hazardous to health and well-being. Perhaps the classic example is the organization that offers stress management courses to teach employees to cope more effectively but that does not examine and correct features of the workplace that are needlessly stressful.
It must be recognized that hazards present in the workplace may not only affect the workers, and by extension their families as well, but they may also precipitate and aggravate personal health problems generated away from the job. While retaining the concept of individual responsibility for health, it must be balanced by the understanding that factors in the workplace for which the employer is responsible may also have a health-related influence. This consideration highlights the importance of communication and coordination between the health promotion program and the employer’s occupational safety and health and other health-related programs, especially when they are not in the same box on the organization chart.
Persuasion, not coercion
A cardinal tenet of worksite health promotion programs is that participation should be voluntary. Employees should be educated about the desirability of suggested interventions, provided with access to them, and persuaded to participate in them. There often is, however, a narrow margin between enthusiastic persuasion and compulsion, between well-meaning paternalism and coercion. In many instances, the coercion may be more or less subtle: e.g., some health promotion professionals tend to be overly authoritarian; employees may be fearful of embarrassment, being ostracized or even penalized if they reject the advice given them; a worker’s choices as to recommended health promotion activities may be overly limited; and executives may make it unpleasant for their subordinates not to join them in a favorite activity, such as jogging in the very early morning.
While many organizations offer rewards for healthy behavior, for instance, certificates of achievement, prizes, and “risk-rated” health insurance (involving, in the United States, for example, a reduction in the employee’s share of the premiums), a few impose penalties on those who do not meet their arbitrary standards of health behavior. The penalties may range from refusing employment, withholding advancement, or even dismissal or denying benefits that might otherwise be forthcoming. An example of an American firm levying such penalties is E.A. Miller, a meat-packing plant located in Hyrum, Utah, a town of 4,000 inhabitants located some 40 miles north of Salt Lake City (Mandelker 1994). E.A. Miller is the largest employer in this small community and provides group health insurance for its 900 employees and their 2,300 dependants. Its health promotion activities are typical in many ways except that there are penalties for not participating:
- Employees and spouses who do not attend prenatal seminars are not reimbursed for the cost of obstetrical care or of the baby’s care in the hospital. Also, to qualify for the insurance benefits, the pregnant woman must visit a doctor during the first trimester.
- If employees or their dependants smoke, they must contribute over twice as much to their share of group health insurance premiums: $66 per month instead of $30. The plant has had a smoke-free policy since 1991 and the company offers smoking cessation courses onsite or pays employees’ tuition if they take the course in the community.
- The company will not cover any of the medical costs if a covered employee or dependant was injured in an automobile accident while driving under the influence of drugs or alcohol or was not wearing a seat belt, nor will it cover injuries sustained while riding a motorcycle without a helmet.
One form of coercion that has wide acceptance is “job jeopardy” for employees whose alcohol or drug abuse has had an impact on their attendance and work performance. Here, the employee is confronted with the problem and told that disciplinary actions will be stayed as long as he or she continues with the prescribed treatment and remains abstinent. With allowance for an occasional relapse (in some organizations, this is limited to a specific number), failure to comply results in dismissal. Experience has amply shown that the threat of job loss, regarded by some as the most potent stressor encountered in the workplace, is an effective motivator for many individuals with such problems to agree to take part in a program for their correction.
Confidentiality and privacy
Another hallmark of the successful health promotion program is that personal information about participating employees —and non-participants as well—must be kept confidential and, particularly, out of personnel files. To preserve the privacy of such information when it is needed for evaluative tabulations and research, some organizations have set up data bases in which individual employees are identified by code numbers or by some similar device. This is particularly relevant to mass screening and laboratory procedures where clerical errors are not unknown.
Who participates
Health promotion programs are criticized by some on the basis of evidence that participants tend to be younger, healthier and more health conscious than those who do not (the “coals to Newcastle” phenomenon). This presents to those designing and operating programs the challenge of involving those who have more to gain through their participation.
Who pays
Health promotion programs involve some costs to the organization. These may be expressed in terms of financial outlays for services and materials, time taken from work hours, distraction of participating employees, and the burden of management and administration. As noted above, there is increasing evidence that these are more than offset by reduced personnel costs and by improvements in productivity. There are also the less tangible benefits of embellishing the public relations image of the organization and of enhancing its reputation as a good place to work, thereby facilitating recruitment efforts.
Most of the time, the organization will cover the entire cost of the program. Sometimes, particularly when an activity is conducted off the premises in a community-based facility, the participants are required to share its cost. In some organizations, however, all or part of the employee’s portion is refunded on successful completion of the program or course.
Many group health insurance programs cover preventive services provided by health professionals including, for example, immunizations, medical examinations, tests, and screening procedures. Such health insurance coverage, however, presents problems: it may increase the cost of the insurance and the out-of-pocket costs of the deductible fees and co-payments usually required may constitute an effective obstacle to their use by low-salaried workers. In the last analysis, it may be less costly for employers to pay for preventive services directly, saving themselves the administrative costs of processing insurance claims and of reimbursement.
Conflicts of interest
While most health professionals exhibit exemplary integrity, vigilance must be exercised to identify and deal with those who do not. Examples include those who falsify records to make their efforts look good and those who have a relationship with an outside provider of services who provides kickbacks or other rewards for referrals. The performance of outside vendors should be monitored to identify those who underbid to win the contract and then, to save money, use poorly qualified personnel to deliver the services.
A more subtle conflict of interest exists when staff members and vendors subvert the needs and interests of employees in favor of the organization’s goals or the agenda of its managers. This sort of reprehensible action may not be explicit. An example is steering troubled employees into a stress management program without making a strenuous effort to persuade the organization to reduce inordinately high levels of stress in the workplace. Experienced professionals will have no difficulty in properly serving both the employees and the organization, but should be ready to move to a situation in which ethical values are more conscientiously observed whenever improper pressures on the part of management become too great.
Another subtle conflict that may affect employees adversely arises when a relationship of competition, rather than coordination and collaboration, develops between the health promotion program and other health-related activities in the organization. This state of affairs is found not infrequently when they are placed in different areas of the organization chart and report to different lines of management authority. As has been said before, it is critical that, even when part of the same entity, the health promotion program should not operate at the expense of the occupational safety and health program.
Stress
Stress is probably the most pervasive health hazard encountered both in the workplace and away from it. In a landmark survey sponsored by the St. Paul Fire and Marine Insurance Company and involving nearly 28,000 workers in 215 diverse American organizations, Kohler and Kamp (1992) found that work stress was strongly related to employee health and performance problems. They also found that among personal life problems, those created by the job are most potent, showing more impact than purely off-the-job issues such as family, legal or financial problems. This suggests, they said, that “some workers become caught in a downward spiral of work and home life problems—problems on the job create problems at home, which in turn are taken back to work, and so on.” Accordingly, while primary attention should be directed to the control of psychosocial risk factors intrinsic to the job, this should be complemented by health promotion activities aimed at personal stress factors most likely to affect work performance.
Access to health care
A subject worthy of attention in its own right, education in navigating the health care delivery system should be made part of the program with an eye to future needs for health services. This begins with self-care—knowing what to do when signs and symptoms appear and when professional services are needed—and goes on to selecting a qualified health professional or a hospital. It also includes inculcating both the ability to distinguish good from poor health care and an awareness of patients’ rights.
To save employees time and money, some in-plant medical units offer more or less extensive in-plant health services, (often including x rays, laboratory tests and other diagnostic procedures), reporting the results to the employees’ personal physicians. Others maintain a roster of qualified physicians, dentists and other health professionals to whom employees themselves and sometimes also their dependants may be referred. Time off from work to keep medical appointments is an important adjunct where health professional services are not available outside of working hours.
In the United States, even where there is a good group health insurance program, low-salaried workers and their families may find the deductible and coinsurance portions of covered charges to be barriers to procuring recommended health services in all but dire circumstances. Some employers are helping to overcome such obstacles by exempting these employees from such payments or by making special fee arrangements with their health care providers.
Worksite “climate”
Worksite health promotion programs are presented, often explicitly, as an expression of the employer’s concern for the health and well-being of the workforce. That message is contradicted when the employer is deaf to employees’ complaints about working conditions and does nothing to improve them. Employees are not likely to accept or participate in programs offered under such circumstances or at times of labor-management conflict.
Workforce diversity
The health promotion program should be designed to accommodate to the diversity increasingly characteristic of today’s workforce. Differences in ethnic and cultural background, educational levels, age and sex should be recognized in the content and presentation of health promotion activities.
Conclusion
It is clear from all of the above that the worksite health promotion program represents an extension of the occupational safety and health program which, when properly designed and implemented, can benefit individual employees, the workforce as a whole and the organization. In addition, it may also be a force for positive social change in the community.
Over the past few decades, worksite health promotion programs have increased in number and comprehensiveness, in small and medium-sized organizations as well as in larger ones, and in the private, voluntary and public sectors. As demonstrated by the array of articles contained in this chapter, they have also increased in scope, expanding from direct clinical services dealing, for example, with medical examinations and immunizations, to involvement with personal and family problems whose relationship to the workplace may seem more tenuous. One should allow one’s selection of program elements and activities to be guided by the particular characteristics of the workforce, the organization and the community, keeping in mind that some will be needed only by specific cohorts of employees rather than by the population as a whole.
In considering the creation of a worksite health promotion program, readers are advised to plan carefully, to implement incrementally, allowing room for growth and expansion, to monitor performance and program quality and, to the extent possible, evaluate outcomes. The articles in this chapter should prove to be uniquely helpful in such an endeavor.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."