Women's Health
There is a common misperception that, outside of reproductive differences, female and male workers will be similarly affected by workplace health hazards and attempts to control them. While women and men do suffer from many of the same disorders, they differ physically, metabolically, hormonally, physiologically and psychologically. For example, women’s smaller average size and muscle mass dictate special attention to the fitting of protective clothing and devices and the availability of properly designed hand tools, while the fact that their body mass is usually smaller than that of men makes them more susceptible, on average, to the effects of alcohol abuse on the liver and the central nervous system.
They also differ in the types of job they hold, in the social and economic circumstances that influence their lifestyles, and in their participation in and response to health promotion activities. Although there have been some recent changes, women are still more likely to be found in jobs that are stultifyingly routine and in which they are exposed to repetitive injury. They suffer from pay inequity and are much more likely than men to be burdened with homemaking responsibilities and the care of children and elderly dependants.
In industrialized countries women have a longer life expectancy than men; this applies to every age group. At age 45, a Japanese woman may expect to live on average another 37.5 years, and a 45-year-old Scottish woman another 32.8 years, with women from most of the other countries of the developed world falling between these limits. These facts lead to an assumption that women are, therefore, healthy. There is a lack of awareness that these “extra” years are frequently marred by chronic illness and disability much of which is preventable. Many women know far too little about the health risks they face and, therefore, about the measures they can take to control those risks and protect themselves against serious disease and injury. For example, many women are rightfully concerned about breast cancer but ignore the fact that heart disease is by far the major cause of death in women and that, owing primarily to the increase in their cigarette smoking—which is also a major risk factor for coronary artery disease—the incidence of lung cancer among women is increasing.
In the United States, a 1993 national survey (Harris et al. 1993), involving interviews of more than 2,500 adult women and 1,000 adult men, confirmed that women suffer from serious health problems and that many do not receive the care they need. Between three and four out of ten women, the survey found, are at risk for undetected treatable disease because they are not receiving appropriate clinical preventive services, largely because they lack health care insurance or because their doctors never suggested that appropriate tests were available and should be sought. Furthermore, a substantial number of the American women surveyed were not happy with their personal physicians: four out of ten (twice the proportion of men) said their physicians “spoke down” to them and 17% (compared to 10% of men) had been told that their symptoms were “all in the head”.
While overall rates of mental illness are roughly the same for men and women, the patterns are different: women suffer more from depression and anxiety disorders while drug and alcohol abuse and antisocial personality disorders are more common among men (Glied and Kofman 1995). Men are more likely to seek and receive care from mental health specialists while women are more often treated by primary care physicians, many of whom lack the interest if not the expertise to treat mental health problems. Women, especially older women, receive a disproportionate share of the prescriptions for psychotropic drugs, so that concern has arisen that these drugs are possibly being overutilized. All too often, difficulties stemming from inordinate levels of stress or from problems that are preventable and treatable are explained away by health professionals, family members, supervisors and co-workers, and even by women themselves, as being reflective of the “time of the month” or “change of life”, and, therefore, go untreated.
These circumstances are compounded by the assumption that women—young and old alike—know all there is to know about their bodies and how they function. This is far from the truth. There exists widespread ignorance and uncritically accepted misinformation. Many women feel ashamed to reveal their lack of knowledge and are being needlessly worried by symptoms that are in fact either “normal” or simply explained.
As women constitute some 50% of the workforce in a large section of the employment arena, and considerably more in some service industries, the consequences of their preventable and correctable health problems levy a significant and avoidable toll on their well-being and productivity and on the organization as well. That toll may be considerably reduced by a worksite health promotion program designed for women.
Worksite Health Promotion for Women
A good deal of health information is provided by newspapers and magazines and on television but much of that is incomplete, sensationalized or geared to the promotion of particular products or services. Too often, in reporting on current medical and scientific advances, the media raise more questions than they answer and even cause needless anxiety. Health care professionals in hospitals, clinics and private offices often fail to make sure that their patients are properly educated about the problems they present, to say nothing of taking the time to inform them about important health issues unrelated to their symptoms.
A properly designed and administered worksite health promotion program should provide accurate and complete information, opportunities to ask questions either in group or individual sessions, clinical preventive services, access to a variety of health promotion activities and counseling about adjustments that may prevent or minimize distress and disability. The worksite offers an ideal venue for the sharing of health experiences and information, particularly when they are relevant to circumstances encountered on the job. One can also take advantage of the peer pressure that is present in the workplace to provide workers with additional motivation for participating and persisting in health promoting activities and in maintaining a healthful lifestyle.
There is a variety of approaches to programming for women. Ernst and Young, the large accounting firm, offered its London employees a series of Health Seminars for Women conducted by an outside consultant. They were attended by all grades of staff and were well received. The women who attended were secure in the format of the presentations. As an outsider, the consultant posed no threat to their employment status, and together they cleared up many areas of confusion about women’s health.
Marks and Spencer, a major retailer in the United Kingdom, conducts a program through its in-house medical department using outside resources to provide services to employees in their many regional worksites. They offer screening examinations and individual advice to all their staff, together with an extensive range of health literature and videotapes, many of which are produced in-house.
Many companies use independent health advisers outside the company. An example in the United Kingdom is the service provided by the BUPA (British United Provident Association) Medical Centers, who see many thousands of women through their network of 35 integrated but geographically scattered units, supplemented by their mobile units. Most of these women are referred through their employers’ health promotion programs; the remainder come independently.
BUPA was probably the first, at least in the United Kingdom, to establish a women’s health centre dedicated to preventive services exclusively for women. Hospital-based and free-standing women’s health centers are becoming more common and are proving attractive to women who have not been well served by the prevailing health care system. In addition to providing prenatal and obstetrical care, they tend to offer broad-ranging primary care, with most placing particular emphasis on preventive services.
The National Survey of Women’s Health Centers, conducted in 1994 by researchers from the Johns Hopkins School of Hygiene and Public Health with support from the Commonwealth Foundation (Weisman 1995), estimated that there are 3,600 women’s health centers in the United States, of which 71% are reproductive health centers providing primarily routine outpatient gynaecological examinations, Pap tests and family planning services. They also provide pregnancy tests, abortion counseling (82%) and abortions (50%), screening and treatment for sexually transmitted diseases, breast examinations and blood pressure checks.
Twelve per cent are primary care centers (these include women’s college health services) which provide basic well-woman and preventive care including periodic physical examinations, routine gynaecological examinations and Pap tests, diagnosis and treatment of menstrual problems, menopausal counseling and hormone replacement therapy, and mental health services, including drug and alcohol abuse counseling and treatment.
Breast centers constitute 6% of the total (see below), while the remainder are centers providing various combinations of services. Many of these centers have demonstrated interest in contracting to provide services to female employees of nearby organizations as part of their worksite health promotion programs.
Regardless of the venue, the success of worksite health promotion programming for women hinges not only on the reliability of the information and services offered but, more important, on the manner in which they are presented. The programs must be sensitized to women’s attitudes and aspirations as well as to their concerns and, while being supportive, they should be free of the condescension with which these problems are so often addressed.
The remainder of this article will focus on three categories of problems regarded as particularly important health concerns for women—menstrual disorders, cervical and breast cancer and osteoporosis. However, in addressing other health categories, the worksite health promotion program should ensure that any other problems of particular relevance for women will not be overlooked.
Menstrual Disorders
For the great majority of women, menstruation is a “natural” process that presents few difficulties. The menstrual cycle may be disturbed by a variety of conditions which may cause discomfort or concern for the employee. These may lead her to take sick absence on a regular basis, often reporting a “cold” or “sore throat” rather than a menstrual problem, especially if the absence certificate is to be submitted to a male manager. However, the absence pattern is obvious and referral to a qualified health professional may resolve the problem rapidly. Menstrual problems that may affect the workplace include amenorrhoea, menorrhagia, dysmenorrhoea, the premenstrual syndrome (PMS) and menopause.
Amenorrhoea
While amenorrhoea may create concern, it does not ordinarily affect work performance. The most common cause of amenorrhoea in younger women is pregnancy and in older women it is menopause or a hysterectomy. However, it may also be attributable to the following circumstances:
- Poor nutrition or underweight. The reason for poor nutrition may be socioeconomic in that little food is available or affordable, but it may also be the result of self-starvation related to eating disorders such as anorexia nervosa or bulimia.
- Excessive exercise. In many developed countries. women train excessively in physical fitness or sports programmes. Even though their food intake may be adequate, they may have amenorrhoea.
- Medical conditions. Problems arising from hypothyroidism or other endocrine disorders, tuberculosis, anaemia from any cause and certain serious, life-threatening diseases can all cause amenorrhoea.
- Contraceptive measures. Medications containing progesterone only will commonly lead to amenorrhoea. It should be noted that sterilization without цphorectomy does not cause a woman’s periods to stop.
Menorrhagia
In the absence of any objective measure of menstrual flow, it is commonly accepted that any flow of menses which is heavy enough to interfere with a woman’s normal day-to-day activities, or which leads to anemia, is excessive. When the flow is heavy enough to overwhelm the normal circulating anti-clotting factor, the woman with “heavy periods” may complain of passing clots. Inability to control the blood flow by any normal sanitary protection can lead to considerable embarrassment in the workplace and may lead to a pattern of regular, monthly one- or two-day absences.
Menorrhagia may be caused by uterine fibroids or polyps. It can also be caused by an intrauterine contraceptive device (IUD) and, rarely, it may be the first indication of a severe anemia or other serious blood disorder such as leukaemia.
Dysmenorrhoea
Although the vast majority of menstruating women experience some discomfort at the time of menstruation, only a few have pain sufficient to interfere with normal activity and, thus, require referral for medical attention. Again, this problem may be suggested by a pattern of regular monthly absences. Such difficulties associated with menstruation may for certain practical purposes be classified thus:
- Primary dysmenorrhoea. Young women with no evidence of disease may suffer pain on the day before or on the first day of their period that is serious enough to induce them to take time off from work. Although no cause has been found, it is known to be associated with ovulation and, hence, can be prevented by the oral contraceptive pill or by other medication which prevents ovulation.
- Secondary dysmenorrhoea. The onset of painful periods in a woman in her middle thirties or later suggests pelvic pathology and should be fully investigated by a gynaecologist.
It should be noted that some over-the-counter or prescribed analgesics taken for dysmenorrhoea may cause drowsiness and can present a problem for women working in jobs that require alertness to occupational hazards.
Premenstrual syndrome
Premenstrual syndrome (PMS), a combination of physical and psychological symptoms experienced by a relatively small percentage of women during the seven or ten days prior to menstruation, has developed its own mythology. It has falsely been credited as the cause of women’s so-called emotionalism and “flightiness”. According to some men, all women suffer from it, while ardent feminists claim that no women have it. In the workplace, it has improperly been cited as a rationale for keeping women out of positions requiring decision making and the exercise of judgment, and it has served as a convenient excuse for denying women promotion to managerial and executive levels. It has been blamed for women’s problems with interpersonal relations and, indeed, in England it has provided the grounds for pleas of temporary insanity that enabled two separate female defendants to escape charges of murder.
The physical symptoms of PMS may include abdominal distention, breast tenderness, constipation, sleeplessness, weight gain due to increased appetite or to sodium and fluid retention, fine-movement clumsiness and inaccuracy in judgment. The emotional symptoms include excessive crying, temper tantrums, depression, difficulty in making decisions, an inability to cope in general and a lack of confidence. They always occur in the premenstrual days, and are always relieved by the onset of the period. Women taking the combined oral contraceptive pill and those who have had oophorectomies rarely get PMS.
The diagnosis of PMS is based on the history of its temporal relationship to menstrual periods; in the absence of definitive causes, there are no diagnostic tests. Its treatment, the intensity of which is determined by the intensity of the symptoms and their effect on normal activities, is empirical. Most cases respond to simple self-help measures which include abolishing caffeine from the diet (tea, coffee, chocolate and most cola soft drinks all contain significant amounts of caffeine), frequent small feedings to minimize any tendency to hypoglycemia, restricting sodium intake to minimize fluid retention and weight gain, and regular moderate exercise. When these fail to control the symptoms, physicians may prescribe mild diuretics (for two to three days only) that control sodium and fluid retention and/or oral hormones that modify ovulation and the menstrual cycle. In general, PMS is treatable and should not represent a significant problem to women in the workplace.
Menopause
Menopause reflecting ovarian failure may occur in women in their thirties or may be postponed to well beyond the age of 50; by the age of 48, about half of all women will have experienced it. The actual time of the menopause is influenced by general health, nutrition and familial factors.
The symptoms of the menopause are diminished frequency of periods usually coupled with scanty menstrual flow, hot flushes with or without night sweats, and a diminution in vaginal secretions, which may cause pain during sexual intercourse. Other symptoms frequently attributed to the menopause include depression, anxiety, tearfulness, lack of confidence, headaches, changes in skin texture, loss of sexual interest, urinary difficulties and sleeplessness. Interestingly, a controlled study involving a symptom questionnaire administered to both men and women showed that a significant portion of these complaints were shared by men of the same age (Bungay, Vessey and McPherson 1980).
The menopause, coming as it does at about the age of 50, may coincide with what has been called the “mid-life transition” or the “mid-life crisis”, terms coined to denote collectively the experiences which seem to be shared by both men and women in their middle years (if anything, they appear to be more common among men). These include loss of purpose, dissatisfaction with one’s job and with life in general, depression, waning interest in sexual activity and a tendency to diminished social contacts. It may be precipitated by the loss of spouse or partner through separation or death or, as regards one’s job, by failure to win an expected promotion or by separation, whether by termination or voluntary retirement. In contrast to menopause, there is no known hormonal basis for the mid-life transition.
Particularly in women, this period may be associated with the “empty nest syndrome,” the sense of purposelessness that may be felt when, their children having left the home, their whole perceived raison d’être seems to have been lost. In such cases, the job and the social contacts in the workplace often provide a stabilizing, therapeutic influence.
Like many of the other “female problems,” menopause has developed its own mythology. Preparatory education debunking these myths supplemented by sensitive supportive counseling will go far to preventing significant dislocations. Continuing to work and maintaining her satisfactory performance on the job may be of crucial value in sustaining a woman’s well-being at this time.
It is at this point that the advisability of hormone replacement therapy (HRT) needs to be considered. Currently the subject of some controversy, HRT was originally prescribed to control menopausal symptoms if they became excessively severe. While usually effective, the hormones commonly used often precipitated vaginal bleeding and, more important, they were suspected of being carcinogenic. As a result, they were prescribed only for limited periods of time, just long enough to control the troublesome menopausal symptoms.
HRT has no effect on the symptoms of the mid-life transition. However, if a woman’s flushes are controlled and she can get a good night’s sleep because her night sweats are prevented, or if she can respond to lovemaking more enthusiastically because it is no longer painful, then some of her other problems may be resolved.
Today, the value of long-term HRT is increasingly being recognized in maintaining the integrity of bone in women with osteoporosis (see below) and in reducing the risk of coronary heart disease, now the highest-ranking cause of death among women in industrialized countries. Newer hormones, combinations and sequences of administration may eliminate the occurrence of planned vaginal bleeding and there appears to be little or no risk of carcinogenesis, even among women with a history of cancer. However, because many physicians are strongly biased for or against HRT, women need to be educated about its benefits and disadvantages so that they can participate confidently in the decision about whether to use it or not.
Recently, calling to mind the millions of women “baby boomers” (children born after the Second World War) who will be reaching the age of menopause within the next decade, the American College of Obstetricians and Gynecologists (ACOG) warned that staggering increases in osteoporosis and heart disease could result unless women are better educated about menopause and the interventions designed to prevent disease and disability and to prolong and enhance their lives after menopause (Voelker 1995). ACOG president William C. Andrews, MD, has proposed a three-pronged program that includes a massive campaign to educate physicians about the menopause, a “perimenopausal visit” to a physician by all women over the age of 45 for a personal risk assessment and in-depth counseling, and involvement of the news media in educating women and their families about the symptoms of menopause and the benefits and risks of treatments like HRT before women reach menopause. The worksite health promotion program can make a major contribution to such an educational effort.
Screening for Cervical and Breast Disease
With regard to women’s needs, a health promotion program should either provide or, at least, recommend periodic screening for cervical and breast cancer.
Cervical disease
Regular screening for precancerous cervical changes by means of the Pap test is a well-established practice. In many organizations, it is made available in the workplace or in a mobile unit brought to it, eliminating the need for female employees to spend time traveling to a facility in the community or visiting their personal physicians. The services of a physician are not required in the administration of this procedure: satisfactory smears may be taken by a well-trained nurse or technician. More important is the quality of the reading of the smears and the integrity of the procedures for record-keeping and reporting of the results.
Breast cancer
Although breast screening by mammography is widely practiced in almost all developed countries, it has been established on a national basis only within the United Kingdom. Currently, over a million women in the United Kingdom are screened, with each woman aged 50 to 64 having a mammogram every three years. All the examinations, including any further diagnostic studies needed to clarify abnormalities in the initial films, are free of charge to the participants. The response to the offer of this three-year cycle of mammography has been over 70%. Reports for the 1993-1994 period (Patnick 1995) show a rate of 5.5% for referral to further assessment; 5.5 women per 1,000 women screened were discovered to have breast cancer. The positive predictive value for surgical biopsy was 70% in this program, compared to some 10% in programs reported elsewhere in the world.
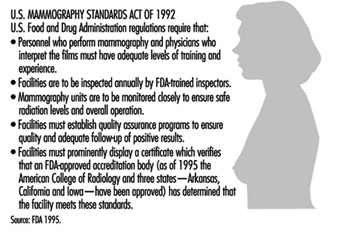
The critical issues in mammography are the quality of the procedure, with particular emphasis on minimizing radiation exposure, and the accuracy of the interpretation of the films. In the United States, the Food and Drug Administration (FDA) has promulgated a set of quality regulations proposed by the American College of Radiology that, commencing October 1, 1994, must be observed by the more than 10,000 medical units taking or interpreting mammograms around the country (Charafin 1994). In accordance with the national Mammography Standards Act (enacted in 1992), all mammography facilities in the United States (except those operated by the Department of Veterans Affairs, which is developing its own standards) had to be certified by the FDA as of this date. These regulations are summarized in figure 1.
Figure 1. Mammography quality standards in the United States.
A recent phenomenon in the United States is the increase in the number of breast or breast health centers, 76% of which have appeared since 1985 (Weisman 1995). They are predominantly hospital-affiliated (82%); the others are primarily profit-making enterprises owned by physician groups. About a fifth maintain mobile units. They provide outpatient screening and diagnostic services including physical breast examinations, screening and diagnostic mammography, breast ultrasound, fine-needle biopsy and instruction in breast self-examination. Slightly more than one-third also offer treatment for breast cancer. While primarily focused on attracting self-referrals and referrals by community physicians, many of these centers are making an effort to contract with employer- or labor union-sponsored health promotion programs to provide breast screening services to their female participants.
Introducing such screening programs into the workplace can generate considerable anxiety among some women, particularly those with personal or family histories of cancer and those found to have “abnormal” (or inconclusive) results. The possibility of such non-negative results should be carefully explained in presenting the program, along with the assurance that arrangements are in place for the additional examinations needed to explain and to act upon them. Supervisors should be educated to sanction absences by these women when the necessary follow-up procedures cannot be expeditiously arranged outside of working hours.
Osteoporosis
Osteoporosis is a metabolic bone disorder, much more prevalent in women than in men, that is characterized by a gradual decline in bone mass leading to susceptibility to fractures which may result from seemingly innocuous movements and accidents. It represents an important public health problem in most developed countries.
The most common sites for fractures are the vertebrae, the distal portion of the radius and the upper portion of the femur. All fractures at these sites in older individuals should cause one to suspect osteoporosis as a contributing cause.
While such fractures usually occur later in life, after the individual has left the workforce, osteoporosis is a desirable target for worksite health promotion programs for a number of reasons: (1) the fractures may involve retirees and add significantly to their medical care costs, for which the employer may be responsible; (2) the fractures may involve the elderly parents or in-laws of current employees, creating a dependant-care burden that can compromise their attendance and work performance; and (3) the workplace presents an opportunity to educate younger people about the eventual danger of osteoporosis and to urge them to initiate the lifestyle changes that can slow its progress.
There are two types of primary osteoporosis:
- Post-menopausal, which is related to loss of oestrogens and, hence, is more prevalent in women than in men (ratio = 6:1). It is commonly found in the 50-to-70 age group and is associated with vertebral fractures and Colles fractures (of the wrist).
- Involutional, which occurs mainly in those over the age of 70 and is only twice as common among women than in men. It is thought to be due to age-related changes in vitamin D synthesis and is associated chiefly with vertebral and femoral fractures.
Both types may be present simultaneously in women. In addition, in a small percentage of cases, osteoporosis has been attributed to a variety of secondary causes including: hyperparathyroidism; the use of corticosteroids, L-thyroxine, aluminum-containing antacids and other drugs; prolonged bed rest; diabetes mellitus; the use of alcohol and tobacco; and rheumatoid arthritis.
Osteoporosis may be present for years and even decades before fractures result. It can be detected by well-standardized x-ray measurements of bone density, calibrated for age and sex, and supplemented by laboratory evaluation of calcium and phosphorus metabolism. Unusual radiolucency of bone in conventional x rays may be suggestive, but such osteopenia usually cannot be reliably detected until more than 30% of the bone is lost.
It is generally agreed that screening asymptomatic individuals for osteoporosis should not be employed as a routine procedure, especially in worksite health promotion programs. It is costly, not very reliable except in the most well-staffed facilities, involves exposure to radiation and, most important, does not identify those women with osteoporosis who are most likely to have fractures.
Accordingly, although everyone is subject to some degree of bone loss, the prevention program for osteoporosis is focused on those individuals who are at higher risk for its more rapid progression and who are therefore more susceptible to fractures. A special problem is that although the earlier in life the preventive measures are started, the more effective they are, it is nonetheless difficult to motivate younger people to adopt lifestyle changes in the hope of avoiding a health problem that may develop at what many of them consider to be a very remote age of life. A saving grace is that many of the recommended changes are also useful in the prevention of other problems as well as in promoting general health and well-being.
Some risk factors for osteoporosis cannot be changed. They include:
- Race. On average, Whites and Orientals have lower bone density than Blacks matched age for age and are therefore at greater risk.
- Sex. Women have less dense bones than men when matched for age and race and therefore are at greater risk.
- Age. All people lose bone mass with age. The stronger the bones are in youth, the less likely is it that the loss will reach potentially dangerous levels in old age.
- Family history. There is some evidence of a genetic component in the attainment of peak bone mass and the rate of subsequent bone loss; thus, a family history of suggestive fractures in family members may represent an important risk factor.
The fact that these risk factors cannot be altered makes it important to give attention to those that can be modified. Among the measures that may be taken to delay the onset of osteoporosis or to diminish its severity, the following may be mentioned:
- Diet. If adequate amounts of calcium and vitamin D are not present in the diet, supplementation is recommended. This is particularly important for people with lactose intolerance who tend to avoid milk and milk products, the major sources of dietary calcium, and is most effective if maintained from childhood until the thirties as peak bone density is being achieved. Calcium carbonate, the most commonly used form of calcium supplementation, frequently causes side effects such as constipation, rebound hyperacidity, abdominal bloating and other gastrointestinal symptoms. Accordingly, many people substitute preparations of calcium citrate which, despite a significantly lower content of elemental calcium, is better absorbed and has fewer side-effects. The amounts of vitamin D present in the usual multivitamin preparation suffice for slowing the bone loss of osteoporosis. Women should be cautioned against excessive doses, which may lead to hypervitaminosis D, a syndrome that includes acute renal failure and increased resorption of bone.
- Exercise. Regular moderate weight-bearing exercise-for example, 45 to 60 minutes of walking at least three times a week-is advisable.
- Smoking. Women who smoke have their menopause on average two years earlier than non-smokers. Without hormone replacement, the earlier menopause will accelerate post-menopausal bone loss. This is another important reason to counter the current trend to increased cigarette smoking among women.
- Hormone replacement therapy. If oestrogen replacement is undertaken, it should be started early in the progress of the menopausal changes since the rate of bone loss is greatest during the first few years after menopause. Because bone loss is resumed after the discontinuation of oestrogen therapy, it should be maintained indefinitely.
Once osteoporosis is diagnosed, treatment is aimed at circumventing further bone loss by following all of the above recommendations. Some recommend using calcitonin, which has been shown to increase total body calcium. However, it must be given parenterally; it is expensive; and there is yet no evidence that it retards or reverses the loss of calcium in the bone or reduces the occurrence of fractures. Biphosphonates are gaining ground as anti-resorptive agents.
It must be remembered that osteoporosis sets the stage for fractures but it does not cause them. Fractures are caused by falls or sudden injudicious movements. While the prevention of falls should be an integral part of every worksite safety program, it is particularly important for individuals who may have osteoporosis. Thus, the health promotion program should include education about safeguarding the environment in both the workplace and in the home (e.g., eliminating or taping down trailing electrical wires, painting the edges of steps or irregularities in the floor, tacking down slippery rugs and promptly drying up any wet spots) as well as sensitizing individuals to such hazards as insecure footwear and seats that are difficult to get out of because they are too low or too soft.
Women’s Health and Their Work
Women are in the paid workforce to stay. In fact, they are the mainstay of many industries. They should be treated as equal to men in every respect; only some aspects of their health experience are different. The health promotion program should inform women about these differences and empower them to seek the kind and quality of health care they need and deserve. Organizations and those who manage them should be educated to understand that most women do not suffer from the problems described in this article, and that, for the small proportion of women who do, prevention or control is possible. Except in rare instances, no more frequent than among men with similar health problems, these problems do not constitute barriers to good attendance and effective work performance.
Many women managers get to their high positions not only because their work is excellent, but because they experience none of the problems of female health that have been outlined above. This can make some of them intolerant and unsupportive of other women who do have such difficulties. One major area of resistance to women’s status in the workplace, it appears, can be women themselves.
A worksite health promotion program that embodies a focus on women’s health issues and problems and addresses them with appropriate sensitivity and integrity can have an important positive impact for good, not only for the women in the workforce, but also for their families, the community and, most important, the organization.
Cancer Prevention and Control
Within the next decade, it is predicted, cancer will become the leading cause of death in many developed countries. This reflects not so much an increase in the incidence of cancer but rather a decrease in mortality due to cardiovascular disease, currently topping the mortality tables. Equally with its high mortality rate, we are disturbed by the specter of cancer as a “dread” disease: one associated with a more or less rapid course of disability and a high degree of suffering. This somewhat fearsome picture is being made easier to contemplate by our growing knowledge of how to reduce risk, by techniques permitting early detection and by new and powerful achievements in the field of therapy. However, the latter may be associated with physical, emotional and economic costs for both the patients and those concerned about them. According to the US National Cancer Institute (NCI), a significant reduction in cancer morbidity and mortality rates is possible if current recommendations relating to use of tobacco, dietary changes, environmental controls, screening and state-of-the-art treatment are effectively applied.
To the employer, cancer presents significant problems entirely apart from the responsibility for possible occupational cancer. Workers with cancer may have impaired productivity and recurrent absenteeism due both to the cancer itself and the side effects of its treatment. Valuable employees will be lost through prolonged periods of disability and premature death, leading to the considerable cost of recruiting and training replacements.
There is a cost to the employer even when it is a spouse or other dependant rather than the healthy employee who develops the cancer. The caregiving burden may lead to distraction, fatigue and absenteeism which tax that employee’s productivity, and the often considerable medical expenses increase the cost of employer-sponsored health insurance. It is entirely appropriate, therefore, that cancer prevention should be a major focus of worksite wellness programs.
Primary Prevention
Primary prevention involves avoidance of smoking and modifying other host factors that may influence the development of cancer, and identifying potential carcinogens in the work environment and eliminating or at least limiting workers’ exposure to them.
Controlling exposures
Potential as well as proven carcinogens are identified through basic scientific research and by epidemiological studies of exposed populations. The latter involves industrial hygiene measurements of the frequency, magnitude and duration of the exposures, coupled with comprehensive medical surveillance of the exposed workers, including analysis of causes of disability and death. Controlling exposures involves the elimination of these potential carcinogens from the workplace or, when that is not possible, minimizing exposure to them. It also involves the proper labeling of such hazardous materials and continuing education of workers with respect to their handling, containment and disposal.
Smoking and cancer risk
Approximately one-third of all cancer deaths and 87% of all lung cancers in the US are attributable to smoking. Tobacco use is also the principal cause of cancers of the larynx, oral cavity and oesophagus and it contributes to the development of cancers of the bladder, pancreas, kidney, and uterine cervix. There is a clear dose-response relationship between lung cancer risk and daily cigarette consumption: those who smoke more than 25 cigarettes a day have a risk that is about 20 times greater than that of non-smokers.
Experts believe that the involuntary intake of the tobacco smoke emitted by smokers (“environmental tobacco smoke”) is a significant risk factor for lung cancer in non-smokers. In January 1993, the US Environmental Protection Agency (EPA) classified environmental tobacco smoke as a known human carcinogen which, it estimated, is responsible for approximately 3,000 lung cancer deaths annually among US non-smokers.
The 1990 US Surgeon General’s report on the health benefits of smoking cessation provides clear evidence that quitting smoking at any age is beneficial to one’s health. For example, five years after quitting, former smokers experience a diminished risk for lung cancer; their risk, however, remains higher than that of non-smokers for as long as 25 years.
The elimination of tobacco exposure by employer-sponsored/ labor union-sponsored smoking cessation programs and worksite policies enforcing a smoke-free working environment represent a major element in most worksite wellness programs.
Modifying host factors
Cancer is an aberration of normal cell division and growth in which certain cells divide at abnormal rates and grow abnormally, sometimes migrating to other parts of the body, affecting the form and function of involved organs, and ultimately causing death of the organism. Recent, continuing biomedical advances are providing increasing knowledge of the carcinogenesis process and are beginning to identify the genetic, humoral, hormonal, dietary and other factors that may accelerate or inhibit it—thus leading to research on interventions that have the potential to identify the early, precancerous process and so to help restore the normal cellular growth patterns.
Genetic factors
Epidemiologists continue to accumulate evidence of familial variations in the frequency of particular types of cancer. These data have been bolstered by molecular biologists who have already identified genes that appear to control steps in cellular division and growth. When these “tumor suppressor” genes are damaged by naturally-occurring mutations or the effects of an environmental carcinogen, the process may go out of control and a cancer is initiated.
Heritable genes have been found in patients with cancer and members of their immediate families. One gene has been associated with a high risk of colon cancer and endometrial or ovarian cancer in women; another with a high risk of breast and ovarian cancer; and a third with a form of malignant melanoma. These discoveries led to a debate about the ethical and sociological issues surrounding DNA testing to identify individuals carrying these genes with the implication that they then might be excluded from jobs involving possible exposure to potential or actual carcinogens. After studying this question, the National Advisory Council for Human Genome Research (1994), raising issues to do with the reliability of the testing, the present effectiveness of potential therapeutic interventions, and the likelihood of genetic discrimination against those found to be at high risk, concluded that “it is premature to offer DNA testing or screening for cancer predisposition outside a carefully monitored research environment”.
Humoral factors
The value of the prostate specific antigen (PSA) test as a routine screening test for prostatic cancer in older men has not been scientifically demonstrated in a clinical trial. However, in some instances, it is being offered to male workers, sometimes as a token of gender equity to balance the offering of mammography and cervical Pap smears to female workers. Clinics providing routine periodic examinations are offering the PSA test as a supplement to and, sometimes, even as a replacement for the traditional digital rectal examination as well as the recently introduced rectal ultrasound examination. Although its use appears to be valid in men with prostatic abnormalities or symptoms, a recent multinational review concludes that measurement of PSA should not be a routine procedure in screening healthy male populations (Adami, Baron and Rothman 1994).
Hormonal factors
Research has implicated hormones in the genesis of some cancers and they have been used in the treatment of others. Hormones, however, do not appear to be an appropriate item to emphasize in workplace health promotion programs. A possible exception would be warnings of their potential carcinogenic hazard in certain cases when recommending hormones for the treatment of menopausal symptoms and the prevention of osteoporosis.
Dietary factors
Researchers have estimated that approximately 35% of all cancer mortality in the US may be related to diet. In 1988, the US Surgeon General’s Report on Nutrition and Health indicated that cancers of the lung, colon-rectum, breast, prostate, stomach, ovary and bladder may be associated with diet. Research indicates that certain dietary factors—fat, fiber, and micronutrients such as beta-carotene, vitamin A, vitamin C, vitamin E and selenium—may influence cancer risk. Epidemiological and experimental evidence indicates that modulation of these factors in the diet can reduce the occurrence of some types of cancer.
Dietary fat
Associations between excess intake of dietary fat and the risk of various cancers, particularly cancers of the breast, colon and prostate, have been demonstrated in both epidemiological and laboratory studies. International correlational studies have shown a strong association between the incidence of cancers at these sites and total dietary fat intake, even after adjusting for total caloric intake.
In addition to the amount of fat, the type of fat consumed may be an important risk factor in cancer development. Different fatty acids may have various site-specific tumor-promoting or tumor-inhibiting properties. Intake of total fat and saturated fat has been strongly and positively associated with colon, prostate, and post-menopausal breast cancers; intake of polyunsaturated vegetable oil has been positively associated with post-menopausal breast and prostate cancers, but not with colon cancer. Conversely, consumption of highly polyunsaturated omega-3 fatty acids found in certain fish oils may not affect or may even decrease the risk of breast and colon cancers.
Dietary fiber
Epidemiological evidence suggests that the risk of certain cancers, particularly colon and breast cancers, may be lowered by increased intake of dietary fiber and other dietary constituents associated with high intakes of vegetables, fruits, and whole grains.
Micronutrients
Epidemiological studies generally show an inverse relationship between cancer incidence and intake of foods high in several nutrients having antioxidant properties, such as beta-carotene, vitamin C (ascorbic acid), and vitamin E (alpha-tocopherol). A number of studies have shown that low intakes of fruits and vegetables are associated with increased risk of lung cancer. Deficiencies of selenium and zinc have also been implicated in increased cancer risk.
In a number of studies in which the use of antioxidant supplements was shown to reduce the expected number of serious heart attacks and strokes, the data on cancer were less clear. However, results from the Alpha-Tocopherol, Beta-Carotene (ATBC) Lung Cancer Prevention clinical trial, conducted by the NCI in collaboration with the National Public Health Institute of Finland, indicated that vitamin E and beta-carotene supplements did not prevent lung cancer. Vitamin E supplementation also resulted in 34% fewer prostate cancers and 16% fewer colorectal cancers, but those subjects taking beta-carotene had 16% more lung cancers, which was statistically significant, and had slightly more cases of other cancers than those taking vitamin E or the placebo. There was no evidence that the combination of vitamin E and beta-carotene was better or worse than either supplement alone. The researchers have not yet determined why those taking beta-carotene in the study were observed to have more lung cancers. These results suggest the possibility that a different compound or compounds in foods which have high levels of beta-carotene or vitamin E may be responsible for the protective effect observed in epidemiological studies. The researchers also speculated that the length of time of supplementation may have been too short to inhibit the development of cancers in long-term smokers. Further analyses of the ATBC study, as well as results from other trials in progress, will help resolve some of the questions that have arisen in this trial, particularly the question of whether large doses of beta-carotene may be harmful to smokers.
Alcohol
Excessive use of alcoholic beverages has been associated with cancer of the rectum, pancreas, breast and liver. There is also strong evidence supporting a synergistic association of alcohol consumption and tobacco use with increased risk of cancer of the mouth, pharynx, oesophagus and larynx.
Dietary recommendations
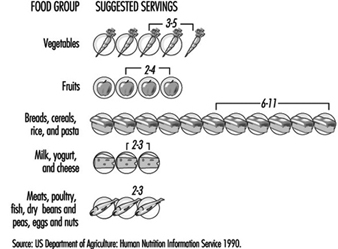
Based on the compelling evidence that diet is related to cancer risk, the NCI has developed dietary guidelines that include the following recommendations:
- Reduce fat intake to 30% or less of calories.
- Increase fibre intake to 20 to 30 grams per day, with an upper limit of 35 grams.
- Include a variety of vegetables and fruits in the daily diet.
- Avoid obesity.
- Consume alcoholic beverages in moderation, if at all.
- Minimize consumption of salt-cured (packed in salt), salt-pickled (soaked in brine), or smoked foods (associated with increased incidence of stomach and oesophageal cancer).
These guidelines are intended to be incorporated into a general dietary regimen that can be recommended for the entire population.
Infectious diseases
There is increasing knowledge of the association of certain infectious agents with several types of cancer: for example, the hepatitis B virus with liver cancer, the human papillomavirus with cervical cancer, and the Epstein-Barr virus with Burkitt’s lymphoma. (The frequency of cancer among patients with AIDS is attributable to the patient’s immunodeficiency and is not a direct carcinogenic effect of the HIV agent.) A vaccine for hepatitis B is now available that, when given to children, ultimately will reduce their risk for liver cancer.
Worksite Cancer Prevention
To explore the potential of the workplace as an arena for the promotion of a broad set of cancer prevention and control behaviors, the NCI is sponsoring the Working Well Project. This project is designed to determine whether worksite-based interventions to reduce tobacco use, achieve cancer preventive dietary modifications, increase screening prevalence and reduce occupational exposure can be developed and implemented in a cost-effective way. It was initiated in September 1989 at the following four research centers in the United States.
- M.D. Anderson Cancer Center, Houston, Texas
- University of Florida, Gainesville, Florida
- Dana Farber Cancer Institute, Boston, Massachusetts
- Miriam Hospital/Brown University, Providence, Rhode Island
The project involves approximately 21,000 employees at 114 different worksites around the United States. Most of the selected worksites are involved predominantly in manufacturing; other types of worksites in the project included fire stations and newspaper printers. Tobacco reduction and dietary modification were areas of intervention included in all of the worksites; however, each site maximized or minimized particular intervention programs or included additional options to meet the climatic and socioeconomic conditions of the geographic area. The centers in Florida and Texas, for example, included and emphasized skin cancer screening and the use of sun screens because of increased exposure to the sun in those geographic regions. The centers in Boston and Texas offered programs that emphasized the relationship between cancer and tobacco use. The Florida centre enhanced the diet modification intervention with supplies of fresh citrus fruits, readily available from the state’s farming and fruit industry. Management-employee consumer boards also were established at the worksites of the Florida centre to work with the food service to ensure that the cafeterias offered fresh vegetable and fruit selections. Several of the worksites participating in the project offered small prizes—gift certificates or cafeteria lunches—for continued participation in the project or for achievement of a desired goal, such as smoking cessation. Reduction of exposure to occupational hazards was of special interest at those worksites where diesel exhaust, solvent use or radiation equipment were prevalent. The worksite-based programs included:
- group activities to generate interest, such as taste testing of various foods
- directed group activities, such as quit-smoking contests
- medical/scientific-based demonstrations, such as
 testing, to verify the effect of smoking on the respiratory system
testing, to verify the effect of smoking on the respiratory system - seminars on business practices and policy development aimed at significantly reducing or eliminating occupational exposure to potentially or actually dangerous or toxic materials
- computer-based self-help and self-assessment programmes on cancer risk and prevention
- manuals and self-help classes to help reduce or eliminate tobacco use, achieve dietary modifications, and increase cancer screening.
Cancer education
Worksite health education programs should include information about signs and symptoms that are suggestive of early cancer—for example, lumps, bleeding from the rectum and other orifices, skin lesions that do not appear to heal—coupled with advice to seek evaluation by a physician promptly. These programs might also offer instruction, preferably with supervised practice, in self-examination of the breast.
Cancer screening
Screening for precancerous lesions or early cancer is carried out with a view to their earliest possible detection and removal. Educating individuals about the early signs and symptoms of cancer so that they may seek the attention of a physician is an important part of screening.
A search for early cancer should be included in every routine or periodic medical examination. In addition, mass screenings for particular types of cancer may be carried out in the workplace or in a community facility near the worksite. Any acceptable and justifiable screening of an asymptomatic population for cancer should meet the following criteria:
- The disease in question should represent a substantial burden at the public health level and should have a prevalent, asymptomatic, nonmetastatic phase.
- The asymptomatic, nonmetastatic phase should be recognizable.
- The screening procedure should have reasonable specificity, sensitivity and predictive values; it should be of low risk and low cost, and be acceptable to both the screener and the person being screened.
- Early detection followed by appropriate treatment should offer a substantially greater potential for cure than exists in cases in which discovery was delayed.
- Treatment of lesions detected by screening should offer improved outcomes as measured in cause-specific morbidity and mortality.
The following additional criteria are particularly relevant in the workplace:
- Employees (and their dependants, when involved in the programme) should be informed of the purpose, nature and potential results of the screening, and a formal “informed consent” should be obtained.
- The screening programme should be conducted with due consideration for the comfort, dignity and privacy of the individuals consenting to be screened and should involve minimal interference with working arrangements and production schedules.
- Screening results should be conveyed promptly and privately, with copies forwarded to personal physicians designated by the workers. Counselling by trained health professionals should be available to those seeking clarification of the screening report.
- The individuals screened should be informed of the possibility of false negatives and warned to seek medical evaluation of any signs or symptoms developing soon after the screening exercise.
- A prearranged referral network should be in place to which those with positive results who are not able or do not wish to consult their personal physicians may be referred.
- The costs of the necessary confirmatory examinations and the costs of treatment should be covered by health insurance or otherwise be affordable.
- A prearranged follow-up system should be in place to be sure that positive reports have been promptly confirmed and proper interventions arranged.
A further final criterion is of fundamental importance: the screening exercise should be conducted by properly skilled and accredited health professionals using state-of-the-art equipment and interpretation and analysis of the results should be of the highest possible quality and accuracy.
In 1989 the US Preventive Services Task Force, a panel of 20 experts from medicine and other related fields drawing upon hundreds of “advisors” and others from the United States, Canada and the United Kingdom, assessed the effectiveness of some 169 preventive interventions. Its recommendations with respect to screening for cancer are summarized in table 1. Reflecting the Task Force’s somewhat conservative attitude and rigorously applied criteria, these recommendations may differ from those advanced by other groups.
Table 1. Screening for neoplastic diseases.
|
Types of cancer |
Recommendations of the US Preventive Services Task Force* |
|
Breast |
All women over age 40 should receive an annual clinical breast examination. Mammography every one to two years is recommended for all women beginning at age 50 and continuing until age 75 unless pathology has been detected. It may be prudent to begin mammography at an earlier age for women at high risk for breast cancer. Although the teaching of breast self-examination is not specifically recommended at this time, there is insufficient evidence to recommend any change in current breast self- examination practices (i.e., those who are now teaching it should continue the practice). |
|
Colorectal |
There is insufficient evidence to recommend for or against fecal occult blood testing or sigmoidoscopy as effective screening tests for colorectal cancer in asymptomatic individuals. There are also insufficient grounds for discontinuing this form of screening where it is currently practiced or for withholding it from persons who request it. It may be clinically prudent to offer screening to persons aged 50 or older with known risk factors for colorectal cancer. |
|
Cervical |
Regular Papanicolaou (Pap) testing is recommended for all women who are or have been sexually active. Pap smears should begin with the onset of sexual activity and should be repeated every one to three years at the physician’s discretion. They may be discontinued at age 65 if previous smears have been consistently normal. |
|
Prostate |
There is insufficient evidence to recommend for or against routine digital rectal examination as an effective screening test for prostate cancer in asymptomatic men. Transrectal ultrasound and serum tumor markers are not recommended for routine screening in asymptomatic men. |
|
Lung |
Screening asymptomatic persons for lung cancer by performing routine chest radiography or sputum cytology is not recommended. |
|
Skin |
Routine screening for skin cancer is recommended for persons at high risk. Clinicians should advise all patients with increased outdoor exposure to use sunscreen preparations and other measures to protect from ultraviolet rays. Currently there is no evidence for or against advising patients to perform skin self-examination. |
|
Testicular |
Periodic screening for testicular cancer by testicular examination is recommended for men with a history of cryptorchidism, orchiopexy, or testicular atrophy. There is no evidence of clinical benefit or harm to recommend for or against routine screening of other men for testicular cancer. Currently there is insufficient evidence for or against counseling patients to perform periodic self-examination of the testicles. |
|
Ovarian |
Screening of asymptomatic women for ovarian cancer is not recommended. It is prudent to examine the adnexa when performing gynecologic examinations for other reasons. |
|
Pancreatic |
Routine screening for pancreatic cancer in asymptomatic persons is not recommended. |
|
Oral |
Routine screening of asymptomatic persons for oral cancer by primary care clinicians is not recommended. All patients should be counseled to receive regular dental examinations, to discontinue the use of all forms of tobacco, and to limit consumption of alcohol. |
Source: Preventive Services Task Force 1989.
Screening for breast cancer
There is a general consensus among experts that screening with mammography combined with clinical breast examination every one to two years will save lives among women aged 50 to 69, reducing breast cancer deaths in this age group by up to 30%. Experts have not reached agreement, however, on the value of breast cancer screening with mammography for asymptomatic women aged 40 to 49. The NCI recommends that women in this age group should be screened every one to two years and that women at increased risk for breast cancer should seek medical advice about whether to begin screening before age 40.
The female population in most organizations may be too small to warrant the installation of mammography equipment onsite. Accordingly, most programs sponsored by employers or labor unions (or both) rely on contracts with providers who bring mobile units to the workplace or on providers in the community to whom participating female employees are referred either during working hours or on their own time. In making such arrangements, it is essential to be sure that the equipment meets standards for x-ray exposure and safety such as those promulgated by the American College of Radiology, and that the quality of the films and their interpretation is satisfactory. Further, it is imperative that a referral resource be prearranged for those women who will require a small needle aspiration or other confirmatory diagnostic procedures.
Screening for cervical cancer
Scientific evidence strongly suggests that regular screening with Pap tests will significantly decrease mortality from cervical cancer among women who are sexually active or who have reached the age of 18. Survival appears to be directly related to the stage of the disease at diagnosis. Early detection, using cervical cytology, is currently the only practical means of detecting cervical cancer in localized or premalignant stages. The risk of developing invasive cervical cancer is three to ten times greater in women who have never been screened than in those who have had Pap tests every two or three years.
Of particular relevance to the cost of workplace screening programs is the fact that cervical cytology smears can be obtained quite efficiently by properly trained nurses and do not require the involvement of a physician. Perhaps of even greater importance is the quality of the laboratory to which they are sent for interpretation.
Screening for colorectal cancer
It is generally agreed that early detection of precancerous colorectal polyps and cancers by periodic tests for fecal blood, as well as digital rectal and sigmoidoscopic examinations, and their timely removal, will reduce mortality from colorectal cancer among individuals aged 50 and over. The examination has been made less uncomfortable and more reliable with the replacement of the rigid sigmoidoscope by the longer, flexible fibreoptic instrument. There remains, however, some disagreement as to which tests should be relied upon and how often they should be applied.
Pros and cons of screening
There is general agreement about the value of cancer screening in individuals at risk because of family history, prior occurrence of cancer, or known exposure to potential carcinogens. But there appear to be justifiable concerns about the mass screening of healthy populations.
Advocates of mass screening for the detection of cancer are guided by the premise that early detection will be followed by improvements in morbidity and mortality. This has been demonstrated in some instances, but is not always the case. For example, although it is possible to detect lung cancer earlier by use of chest x rays and sputum cytology, this has not led to any improvement in treatment outcomes. Similarly, concern has been expressed that increasing the lead time for treatment of early prostatic cancers may not only be without benefit but may, in fact, be counterproductive in view of the longer period of well-being enjoyed by patients whose treatment is delayed.
In planning mass screening programs, consideration must also be given to the impact on the well-being and pocketbooks of patients with false positives. For example, in several series of cases, 3 to 8% of women with positive breast screenings had unnecessary biopsies for benign tumors; and in one experience with the fecal blood test for colorectal cancer, nearly one-third of those screened were referred for diagnostic colonoscopy, and most of them showed negative results.
It is clear that additional research is needed. To assess the efficacy of screening, the NCI has launched a major study, the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trials (PLCO) to evaluate early detection techniques for these four cancer sites. Enrolment for the PLCO began in November 1993, and will involve 148,000 men and women, aged 60 to 74 years, randomized to either the intervention or the control group. In the intervention group, men will be screened for lung, colorectal and prostatic cancer while women will be screened for lung, colorectal and ovarian cancer; those assigned to the control group will receive their usual medical care. For lung cancer, the value of an annual single-view chest x ray will be studied; for colorectal cancer, annual fibreoptic sigmoidoscopy will be performed; for prostate cancer, digital rectal examination and a blood test for PSA will be done; and for ovarian cancer, yearly physical and transvaginal ultrasound examinations will be supplemented by an annual blood test for the tumor marker known as CA-125. At the end of 16 years and the expenditure of US$ 87.8 million, it is hoped that solid data will be obtained about how screening may be used to obtain early diagnoses that may extend lives and reduce mortality.
Treatment and Continuing Care
Treatment and continuing care comprise efforts to enhance the quality of life for those in whom a cancer has taken hold and for those involved with them. Occupational health services and employee assistance programs sponsored by employers and unions can provide useful counsel and support to workers being treated for cancer or who have a dependant receiving treatment. This support can include explanations of what is going on and what to expect, information that is sometimes not provided by oncologists and surgeons; guidance in referrals for second opinions; and consultations and assistance with regard to access to centers of highly specialized care. Leaves of absence and modified work arrangements may make it possible for workers to remain productive while in treatment and to return to work earlier when a remission is achieved. In some workplaces, peer support groups have been formed to provide an exchange of experiences and mutual support for workers facing similar problems.
Conclusion
Programs for the prevention and detection of cancer can make a meaningful contribution to the well-being of the workers involved and their dependants and yield a significant return to the employers and labor unions that sponsor them. As with other preventive interventions, it is necessary that these programs be properly designed and carefully implemented and, since their benefits will accrue over many years, they should be continued on a steady basis.
Smoking Control Programmes at Merrill Lynch and Company, Inc.: A Case Study
In 1990, the US Government demonstrated strong support for workplace health promotion programs with the publication of Healthy People 2000, setting forth the National Health Promotion and Disease Prevention Objectives for the Year 2000 (US Public Health Service 1991). One of these objectives calls for an increase in the percentage of worksites offering health promotion activities for their employees by the year 2000, “preferably as part of a comprehensive employee health promotion program” (Objective 8.6). Two objectives specifically include efforts to prohibit or severely restrict smoking at work by increasing the percentage of worksites with a formal smoking policy (Objective 3.11) and by enacting comprehensive state laws on clean indoor air (Objective 3.12).
In response to these objectives and employee interest, Merrill Lynch and Company, Inc. (hereafter called Merrill Lynch) launched the Wellness and You program for employees at headquarters locations in New York City and in the state of New Jersey. Merrill Lynch is a US-based, global financial management and advisory company, with a leadership position in businesses serving individuals as well as corporate and institutional clients. Merrill Lynch’s 42,000 employees in more than 30 countries provide services including securities underwriting, trading and brokering; investment banking; trading of foreign exchange, commodities and derivatives; banking and lending; and insurance sales and underwriting services. The employee population is diverse in terms of ethnicity, nationality, educational achievement and salary level. Nearly half of the employee population is headquartered in the New York City metropolitan area (includes part of New Jersey) and in two service centers in Florida and Colorado.
Merrill Lynch’s Wellness and You Program
The Wellness and You program is based in the Health Care Services Department and is managed by a doctorate-level health educator who reports to the medical director. The core wellness staff consists of the manager and a full-time assistant, and is supplemented by staff physicians, nurses and employee assistance counselors as well as outside consultants as needed.
In 1993, its initial year, over 9,000 employees representing approximately 25% of the workforce participated in a variety of Wellness and You activities, including the following:
- self-help and written information programmes, including the distribution of pamphlets on a diversity of health topics and a Merrill Lynch personal health guide designed to encourage employees to get the tests, immunizations, and guidance they need to stay healthy
- educational seminars and workshops on topics of broad interest such as smoking cessation, stress management, AIDS, and Lyme disease
- comprehensive screening programmes to identify employees at risk for cardiovascular disease, skin cancer, and breast cancer. These programmes were provided by outside contractors on company premises either in health services clinics or mobile van units
- ongoing programmes, including aerobic exercise in the company cafeteria and personal weight management classes in company conference rooms
- clinical care, including influenza immunizations, dermatology services, periodic health examinations and nutritional counselling in the employee health services clinics.
In 1994, the program expanded to include an onsite gynecology screening program comprising of Pap smears and pelvic and breast examinations; and a worldwide emergency medical assistance program to help American employees locate an English-speaking doctor anywhere in the world. In 1995, wellness programs will be extended to service offices in Florida and Colorado and will reach approximately half of the entire workforce. Most services are offered to employees free of charge or at nominal cost.
Smoking Control Programs at Merrill Lynch
Anti-smoking programs have gained a prominent place in the workplace wellness arena in recent years. In 1964, the US Surgeon General identified smoking as the single cause of the greater part of preventable disease and premature death (US Department of Health, Education, and Welfare 1964). Since then, research has demonstrated that the health risk from inhaling tobacco smoke is not limited to the smoker, but includes those who inhale second-hand smoke (US Department of Health and Human Services 1991). Consequently, many employers are taking steps to limit or curtail smoking by employees out of concern for employee health as well as their own “bottom lines”. At Merrill Lynch, Wellness and You includes three types of smoking cessation effort: (1) the distribution of written material, (2) smoking cessation programs, and (3) restrictive smoking policies.
Written materials
The wellness program maintains a wide selection of quality educational materials to provide information, assistance and encouragement to employees to improve their health. Self-help materials such as pamphlets and audiotapes designed to educate employees about the harmful effects of smoking and about the benefits of quitting are available in the health care clinic waiting rooms and through interoffice mail by request.
Written materials also are distributed at health fairs. Often these health fairs are sponsored in conjunction with national health initiatives so as to capitalize on existing media attention. For example, on the third Thursday of each November, the American Cancer Society sponsors the Great American Smokeout. This national campaign, designed to encourage smokers to give up cigarettes for 24 hours, is well publicized throughout the United States by television, radio and newspapers. The idea is that if smokers can prove to themselves that they can quit for the day, they might quit for good. In 1993’s Smokeout, 20.5% of smokers in the United States (9.4 million) stopped smoking or reduced the number of cigarettes they smoked for the day; 8 million of them reported continuing not to smoke or reducing their smoking one to ten days later.
Each year, members of Merrill Lynch’s medical department set up quit-smoking booths on the day of the Great American Smokeout at home office locations. Booths are stationed in high-traffic locations (lobbies and cafeterias) and provide literature, “survival kits” (containing chewing gum, cinnamon sticks, and self-help materials), and quit-smoking pledge cards to encourage smokers to quit smoking at least for the day.
Smoking cessation programs
Since no single smoking cessation program works for everyone, employees at Merrill Lynch are offered a variety of options. These include self-help written materials (“quit kits”), group programs, audiotapes, individual counseling and physician intervention. Interventions range from education and classic behavior modification to hypnosis, nicotine replacement therapy (e.g., “the patch” and nicotine chewing gum), or a combination. Most of these services are available to employees free of charge and some programs, such as group interventions, have been subsidized by the firm’s benefits department.
Non-smoking policies
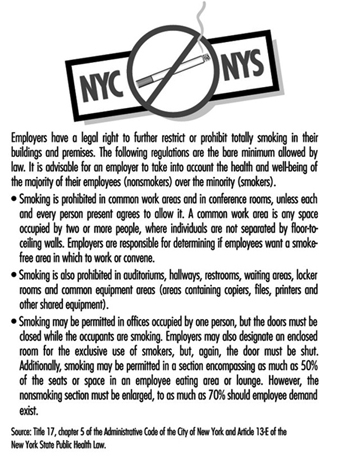
In addition to smoking cessation efforts aimed at individuals, smoking restrictions are becoming increasingly common in the workplace. Many jurisdictions in the United States, including the states of New York and New Jersey, have enacted strict workplace smoking laws that, for the most part, limit smoking to private offices. Smoking in common work areas and conference rooms is permitted, but only if each and every person present agrees to allow it. The statutes typically mandate that non-smokers’ preferences receive priority even to the point of banning smoking entirely. Figure 1 summarizes the city and state regulations applicable in New York City.
Figure 1. Summary of city and state restrictions on smoking in New York.
In many offices, Merrill Lynch has implemented smoking policies which extend beyond the legal requirements. Most headquarters cafeterias in New York City and in New Jersey have gone smoke-free. In addition, total smoking bans have been implemented in some office buildings in New Jersey and Florida, and in certain work areas in New York City.
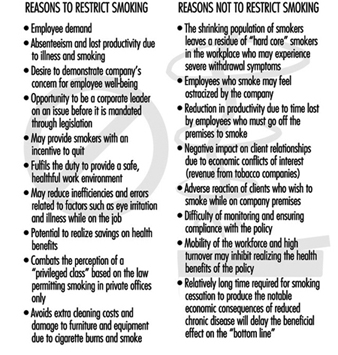
There seems to be little debate about the adverse health effects of tobacco exposure. However, other issues should be considered in developing a corporate smoking policy. Figure 2 outlines many of the reasons why a company may or may not elect to restrict smoking beyond the legal requirements.
Figure 2. Reasons for and against restricting smoking in the workplace.
Evaluation of Smoking Cessation Programs and Policies
Given the relative youth of the Wellness and You program, no formal evaluation has yet been conducted to determine the effect of these efforts on employee morale or smoking habits. However, some studies suggest that worksite smoking restrictions are favored by a majority of employees (Stave and Jackson 1991), result in decreased cigarette consumption (Brigham et al. 1994; Baile et al. 1991; Woodruff et al. 1993), and effectively increase smoking cessation rates (Sorensen et al. 1991).
Smoking Control in the Workplace
Introduction
Awareness of the adverse effects associated with cigarette smoking has increased since the 1960s when the first US Surgeon General’s report on this topic was released. Since that time, attitudes towards cigarette smoking have steadily grown towards the negative, with warning labels being required on cigarette packages and advertisements, bans on television advertising of cigarettes in some countries, the institution of non-smoking areas in some public places and the complete prohibition of smoking in others. Well-founded public health messages describing the dangers of tobacco products are increasingly widespread despite the tobacco industry’s attempts to deny that a problem exists. Many millions of dollars are spent each year by people trying to “kick the habit”. Books, tapes, group therapy, nicotine gum and skin patches, and even pocket computers have all been used with varying degrees of success in aiding those with nicotine addiction. Validation of the carcinogenic effects of passive, “second-hand” smoking has added impetus to the growing efforts to control the use of tobacco.
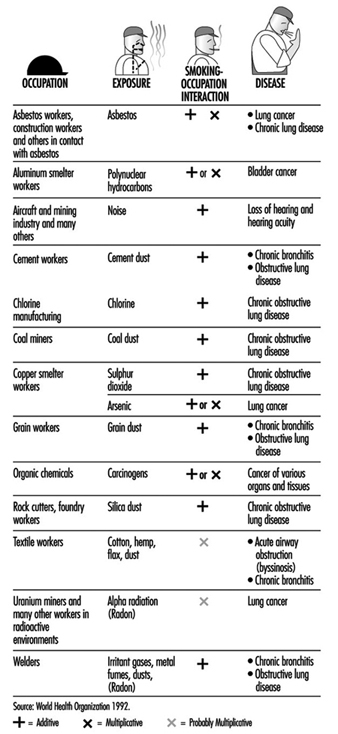
With this background, it is natural that smoking in the workplace should become a growing concern for employers and employees. On the most basic level, smoking represents a fire hazard. From a productivity standpoint, smoking represents either a distraction or an annoyance, depending on whether the employee is a smoker or a non-smoker. Smoking is a significant cause of morbidity in the workforce. It represents a drain in productivity in the form of the loss of work days due to illness, as well as a financial drain on an organization’s resources in terms of health-related costs. Furthermore, smoking has either an additive or multiplicative interaction with environmental hazards found in certain workplaces increasing significantly the risk of many occupational diseases (figure 1).
Figure 1. Examples of interactions between occupation and cigarette smoking causing disease.
This article will concern itself with the rationale for smoking control in the workplace and suggest a practical attitude and approach to managing it, recognizing that mere exhortation is not enough. At the same time, the terrible, addictive nature of nicotine and the human difficulties associated with quitting will not be underestimated. One hopes that it represents a more realistic approach to this complicated problem than some of those taken in the past.
Smoking in the Workplace
Organizations are increasingly associating unhealthy habits such as smoking with higher operating costs, and employers are taking measures to reduce the excess costs associated with employees who smoke. People who smoke one or more packs of cigarettes a day account for 18% higher medical claim costs than non-smokers, according to a study of the impact of various lifestyle risks compiled by the Ceridian Corporation, a technology services company based in Minneapolis, Minnesota. Heavy smokers spend 25% more days as inpatients in hospitals and are 29% more likely than non-smokers to have annual health care claims costs that exceed US$5,000, the study shows (Lesmes 1993).
The impact of smoking on the health of the population and the health care system is unparalleled (US Department of Health and Human Services 1989). According to the World Health Association (1992), tobacco kills at least 3 million people each year worldwide: in countries where smoking has been a long-established behavior, it is responsible for about 90% of all lung cancer deaths; 30% of all cancers; over 80% of cases of chronic bronchitis and emphysema; and some 20 to 25% of coronary heart disease and stroke deaths. Numerous other adverse health conditions, including respiratory diseases, peptic ulcers and pregnancy complications, are also attributable to smoking. Smoking remains the leading cause of avoidable death in many countries, so pervasive that it is responsible for about one sixth of deaths from all causes in the United States, for example (Davis 1987).
The combined effect of smoking and occupational hazards has been demonstrated by the significant differences in morbidity of smokers and non-smokers in many occupations. The interaction of the two types of hazards increases the risk of many diseases, particularly the chronic obstructive pulmonary diseases, lung cancer, cardiovascular diseases, as well as disabilities (figure 1).
Well-recognized complications resulting from exposure to tobacco-related hazards are outlined in great detail throughout the technical literature. Recent attention has focused on the following:
- Female risks. Changes in oestrogen metabolism, menstrual disorders, early menopause, delayed conception or infertility, cancer of the cervix.
- Maternal and pregnancy risks. Spontaneous abortion, ectopic pregnancy, placental irregularities, placenta praevia, abruptio placentae, vaginal bleeding, foetal mortality, preterm birth, retardation of foetal development, low birth weight, congenital anomalies and chronic hypoxia.
- Childhood complications. Increased neonatal mortality, sudden infant death syndrome (SIDS), impaired physical and intellectual development.
Environmental Tobacco Smoke (ETS)
Tobacco smoking is not only dangerous to the smoker but to non-smokers as well. ETS (“passive smoking” and “second-hand smoke”) is a unique risk for people, such as office workers, working in a closed environment. In developed countries, the World Health Organization (1992) points out, tobacco smoke is the most common pollutant of indoor air and is usually present at higher concentrations than other air pollutants. Besides the acute effects of eye and throat irritation, ETS increases the risk of lung cancer and possibly of cardiovascular disease. It is particularly troublesome to individuals with pre-existing health conditions, such as asthma, bronchitis, cardiovascular disease, allergies and upper respiratory infections, and also is a vexatious challenge to those who have recently given up smoking and are struggling to maintain their abstinence.
The US National Institute for Occupational Safety and Health, NIOSH, concluded that (1991):
- ETS is a potential carcinogen.
- Exposure to ETS should be reduced to the lowest possible concentration.
- Employers should minimize occupational exposure to ETS by using all available control measures.
- Worker exposure to ETS is most efficiently and completely controlled by simply eliminating tobacco smoke from the workplace.
- Employers should prohibit smoking at the workplace and provide sufficient disincentives for those who do not comply.
Except where legislation has mandated the smoke-free workplace, the protection of non-smoking employees from the health risks associated with exposure to ETS remains a formidable challenge for many public and private sector employees. Smokers, with encouragement from the tobacco industry, have maintained that continuation of smoking is inherently an individual right, despite the fact that eliminating tobacco smoke from the workplace has required innovations in ventilation engineering and expense by the employer. Legal precedents have established a clear duty for employers to provide workplaces free from hazards such as ETS and courts of law in some countries have found employers liable for the adverse health effects of ETS exposure on the job.
Surveys of public knowledge and attitudes about the risks of ETS and the desirability of workplace smoking restrictions show widespread concern about this sort of exposure and increasingly strong support for significant restrictions among both non-smokers and smokers (American Lung Association 1992). Governments have adopted an increasing number of ordinances and regulations limiting smoking in public and private workplaces (Corporate Health Policies Group 1993).
Impact of Smoking on Employers’ Costs
Historically, employers’ efforts to reduce smoking in the workplace have been driven by issues of cost and productivity losses related to smoking behavior. A number of studies have compared employers’ costs associated with smoking and non-smoking employees. For example, in one study of employees in a large-scale group health insurance plan, tobacco users had higher average outpatient medical care costs ($122 versus $75), higher average insured medical costs ($1,145 versus $762), more hospital admissions per 1,000 employees (174 versus 76), more hospital days per 1,000 employees (800 versus 381), and longer average lengths of hospital stay (6.47 versus 5.03 days) (Penner and Penner 1990).
Another study, undertaken over a period of three and one-half years by the Dow Chemical Company and covering 1,400 employees (Fishbeck 1979), showed that smokers were absent 5.5 days more per year than non-smokers, costing Dow over $650,000 annually in excess wages alone. This figure did not include extra health care costs. In addition, smokers had 17.4 disability days per year compared with 9.7 days for non-smokers. Smokers also had twice the frequency of circulatory disease problems, three times more pneumonia, 41% more bronchitis and emphysema, and 76% more respiratory diseases of all types. For every two non-smokers who died during the study period, seven smokers died.
A study by the United States Steel Corporation found that employees who smoke have more work-loss days than those who have never smoked. It also showed that in every age group, as the number of cigarettes smoked per day by confirmed smokers increased, so did the number of absences due to illness. Additionally, male smokers of more than two packs per day had nearly twice as much absence as their non-smoking counterparts. In a study on how much individual behavioral risk factors contribute to the total disability and health care costs of a large, multi-location industrial company, smokers had 32% greater absenteeism and $960 excess average annual illness costs per employee (Bertera 1991).
The annual report of the Kansas State Employees Health Care Commission found that smokers incurred 33% more hospital admissions than non-smokers (106.5 versus 71.06 hospital admissions per 1,000 persons). The total average claim payment per employee was $282.62 more for smokers than for non-smokers.
Results like these have prompted some US employers to add a “surcharge” to their smoking employees’ share of group health insurance premiums to cover the higher claims payments associated with this population. The Resinoid Engineering Corporation stopped hiring smokers in its Ohio plant because their health care claims were $6,000 higher per employee per year for smokers than for non-smokers; a similar move by a Chicago, Illinois company was barred because the state law prohibits discriminatory hiring on the basis of lifestyle.
Other employers, using the “carrot” rather than the “stick” approach, have offered inducements such as monetary or other types of awards to employees who successfully quit smoking. A popular approach is to refund the tuition required for participating in a smoking cessation program to those who complete the course or, more strictly, to those who remain abstinent for a defined period following the completion of the course.
In addition to increased health care costs and costs associated with lost productivity due to sickness among smokers, there are other increased costs associated with smoking, namely those arising from lost productivity during smoking breaks, higher fire and life insurance costs, and higher general cleaning costs related to smoking. For example, Air Canada identified savings of about US$700,000 per year by not having to clean ashtrays and being able to extend the frequency of deep cleaning of its planes from six to nine months after implementing its tobacco-free policy (WHO 1992). A study by Kristein (1983) designed to take into account all of the increased costs due to smoking estimated the total to be $1,300 per smoker per year (adjusted to 1993 dollars). He also discussed other areas of excess cost, including, in particular, the costs of higher levels of maintenance for computers and other sensitive equipment, and for installing and maintaining ventilation systems. Furthermore, he added that other costs result from the “inefficiency and errors based on the established literature as to the effects of higher carbon monoxide levels in smokers, eye irritation, measured lower attentiveness, cognitive and exercise capacity function”.
Smoking Policies and Regulations
In the 1980s, laws and voluntary policies to restrict smoking at the workplace increased in number and strength. Some pertain only to government worksites which, together with places of work where children are present, have often taken the lead. Others affect both government and private worksites. They are characterized by banning smoking altogether (“smoke-free” worksites); restricting smoking in common areas such as cafeterias and meeting rooms; allowing smoking only in special smoking areas; and requiring accommodation of the interests of smokers and non-smokers, with primacy given to the wishes of the latter.
Some programs regulate smoking in worksites where certain hazardous materials are present. For example, in 1976 Norway issued rules prohibiting the assignment of persons who smoke to areas where they may be exposed to asbestos. In 1988, Spain prohibited smoking in any place where the combination of smoking and occupational hazards results in greater risk to the health of workers. Spain also prohibits smoking in any worksite where pregnant women work. Other countries that have taken legislative measures to restrict smoking in the workplace include Costa Rica, Cuba, Denmark, Iceland and Israel (WHO 1992).
Increasingly, legislation restricting smoking at the worksite is part of a broader regulation covering public places. New Zealand, Norway and Sweden have enacted such legislation while Belgium, the Netherlands and Ireland have passed laws prohibiting smoking in most public places. The 1991 French law prohibits smoking in all places designed for collective use, notably schools and public transportation (WHO 1992).
In the United States and Canada, although federal agencies have adopted smoking control policies, legislation has been limited to states and provinces and to municipalities. By 1989, 45 US states had enacted laws restricting smoking in public places, while 19 states and the District of Columbia had adopted ordinances restricting smoking in private workplaces (Bureau of National Affairs 1989). The state of California has a bill pending that would totally ban smoking in all indoor employment areas and would also obligate an employer to take reasonable steps to prevent visitors from smoking (Maskin, Connelly and Noonan 1993). For some time, the Occupational Safety and Health Administration (OSHA) in the US Department of Labor has been considering the regulation of ETS in the workplace both as an independent toxicant and as a component of indoor air (Corporate Health Policies Group 1993).
Another incentive for employers to reduce smoking in the workplace comes from cases of disability stemming from exposure to ETS that have won worker’s compensation awards. In 1982, a federal appellate court found an employee eligible for disability retirement because she had been forced to work in a smoke-filled environment (Parodi vs. Veterans Administration 1982). Similarly, employees have been awarded worker’s compensation payments because of adverse reactions to tobacco smoke on the job. Indeed, William Reilly, the former administrator of the US Environmental Protection Agency (EPA) has expressed the hope that the threat of employer liability raised by the recent release of the EPA’s designation of EST as a significant health hazard would obviate the necessity of additional federal government regulations (Noah 1993).
Another factor favoring the establishment of policies curbing workplace smoking is the change in public attitudes reflecting (1) recognition of the mounting scientific evidence of the risks of cigarette smoke to smokers and non-smokers alike, (2) a decline in the prevalence of smoking, (3) a decline in the social acceptability of smoking and (4) a heightened awareness of the rights of non-smokers. The American Lung Association (1992) reported consistent increases in the overall percentage of adults who favor workplace smoking restrictions, from 81% in 1983 to 94% in 1992, while in the same period, those favoring a total ban increased from 17% to 30% and those favoring no restrictions fell from 15% to 5%.
Labor unions are also increasingly supportive of non-smoking policies (Corporate Health Policies Group 1993).
Recent US surveys have shown a marked trend towards not only increased adoption of smoking restrictions but also their increasing stringency (Bureau of National Affairs 1986, 1991). The percentage of companies with such policies rose from 36% in 1986 to 85% in 1991 while, in the same period, there was a sixteen-fold increase in the percentage with total bans or “smoke-free” policies (Bureau of National Affairs 1991; Coalition on Smoking and Health 1992).
Smoking Cessation Programs
Worksites are becoming increasingly common settings for health education and promotion efforts. Of several cited studies (Coalition on Smoking and Health 1992), one survey indicates that 35.6% of companies offer some kind of smoking cessation assistance. Another study shows that non-smoking policies may also provide environmental support to individuals attempting to quit smoking. Thus, a non-smoking policy may also be considered an important element in a smoking cessation program.
Smoking cessation methods are divided into two categories:
- Unassisted methods, which include going “cold turkey” (i.e., just stopping without recourse to any special techniques); gradually reducing the number of cigarettes smoked per day; using low-tar or low-nicotine cigarettes; quitting with friends, relatives or acquaintances; using special cigarette filters or holders; using other nonprescription products; or substituting another tobacco product for cigarettes (snuff, chewing tobacco, pipes or cigars).
- Assisted methods, which include attending a programme or a course with or without a fee; consulting a mental health professional; hypnosis; acupuncture; and using nicotine gum or nicotine skin patches.
The efficacy of these various methods is the subject of much controversy largely due to the difficulties and costs associated with long-term follow-up and the obvious self-interest of the vendors of programs and products. Another serious limitation relates to the ability to verify the smoking status of program participants (Elixhauser 1990). Saliva tests measuring cotinine, a metabolite of nicotine, are an effective objective indicator of whether an individual has recently been smoking, but they are moderately complicated and expensive and, thus. not widely used. Accordingly, one is forced to depend on the questionable reliability of the individual’s self-reports of success in either quitting or cutting down on the amount smoked. These problems make it extremely difficult to compare various methods to one another or even to make proper use of a control group.
Despite these encumbrances, two general conclusions can be drawn. First, those individuals most successful in permanently quitting do so largely on their own, often after numerous attempts to do so. Secondly, barring the individual “cold turkey” approach, multiple interventions in combination appear to enhance the effectiveness of efforts to quit, especially when accompanied by support in maintaining abstinence and reinforcement of the quit-smoking message (Bureau of National Affairs 1991). The importance of the latter is confirmed by a study (Sorenson, Lando and Pechacek 1993) which found that the highest overall cessation rate was achieved by smokers who worked among a high proportion of non-smokers and who were frequently asked not to smoke. Still, the six-month quitting rate was only 12%, compared to a rate of 9% among the control group. Obviously, cessation programs in general must not be expected to produce dramatic positive results but, instead, must be viewed as requiring a persistent, patient effort towards the goal of quitting smoking.
Some workplace smoking cessation programs have been overly simple or naive in their approach, while others have lacked long-term determination and commitment. Companies have tried everything from simply restricting smoking to specified areas of the worksite or autocratically making a sudden announcement banning all smoking, to providing expensive and intensive (but often short-lived) programs offered by outside consultants. The problem and the challenge is to successfully accomplish the transition to a smoke-free workplace without sacrificing worker morale or productivity.
The following section will present an approach that incorporates our present knowledge of the difficulties individuals face in quitting and the employer attitude necessary to best achieve the goal of non-smoking in the workplace.
An Alternative Approach to Achievinga Smoke-free Workplace
Past experience has shown that simply offering smoking cessation programs to volunteers does not advance the goal of a smoke-free workplace because the majority of smokers will not participate in them. At any given time, only about 20% of smokers are ready to quit and only a minority of this group will sign up for a cessation program. For the other 80% of smokers who don’t want to quit or who don’t believe they can quit when the enterprise goes smoke-free, instituting a ban on smoking in the workplace will just tend to cause them to move their smoking during working hours “out the door” to a designated smoking area or somewhere outside the building. This “80% problem”—the problem that 80% of the smokers are not going to be helped or even consider participating in the program if only smoking cessation programs are offered—has numerous consequent negative effects on employee relations, productivity, operating costs and health-related costs.
An alternative, and successful, approach has been developed by Addiction Management Systems, an organization based in Toronto, Canada. This approach is based on the knowledge that change and the modification of behavior is a process which can be planned and managed using organizational and behavioral techniques. It involves dealing with control of smoking in the workplace in the same way as any other major policy or procedural change for the company, with informed decisions made by management after input from representative employee groups. A controlled change is made by supporting those managers responsible for overseeing the change and making all smokers positive participants in the change by providing them with the “tools” to accommodate to the new non-smoking environment without requiring them to quit smoking. The focus is on communications and team-building by involving and educating all of those affected by the policy change.
The actual process of the transition to a smoke-free workplace begins with the announcement of the policy change and the start of a transition period of several months’ duration before the policy goes into effect. In behavioral terms, the upcoming policy change to becoming smoke-free acts as a “stimulus to change” and creates a new environment in which it is in the interest of all smokers to seek a means of successfully adapting to the new environment.
The announcement of this policy change is followed by a communication program aimed at all employees, but focused on two important groups: the supervisors who must implement and oversee the new non-smoking policy, and the smokers who need to learn to adapt to the new environment. An important part of the communication program is making smokers aware that, while they will not be required to quit smoking unless they so choose, they must nonetheless adhere to the new policy forbidding smoking in the workplace during the workday. All employees receive the communications about the policy and upcoming changes.
During the transition period, supervisors are provided with communications materials and a training program to enable them to understand the policy change and to anticipate questions, problems or other concerns which may come up during or after the change. As the group most directly affected when the policy goes into effect, smokers are consulted about their specific needs and also receive their own training program. The special focus of the latter is to acquaint them with a voluntary self-help “smoking control” program that contains a number of options and choices which allow the smokers to understand the program and to learn to modify their smoking behavior in order to refrain from smoking during the workday as required once the new policy goes into effect. This allows each smoker to personalize his or her own program, with “success” defined by the individual, whether it be quitting altogether or just learning how not to smoke during the workday. Accordingly, resentment is neutralized and the change to the smoke-free workplace becomes a positive motivating factor for the smoker.
The end result of this approach is that when the effective date of the policy arrives, the transition to a smoke-free workplace becomes a “non-event”—it simply happens, and it is successful. The reason this occurs is that the groundwork has been laid, the communications have been carried out, and all of those persons involved understand what needs to happen and have the means to make a successful transition.
What is important from an organizational standpoint is that the change is one which tends to be self-maintaining, with only minimal ongoing input from management. Also important is the effect that once successful in learning to “manage” their smoking problem, the smokers in the “80% group” tend to build on their success and to progress towards quitting completely. Finally, in addition to the beneficial effect on the well-being and morale of employees who are positively involved in the transition to a smoke-free environment, the organization accrues over time benefits in terms of higher productivity and reduced costs related to health care.
Evaluation of Effectiveness
In evaluating the effectiveness of the program, there are two separate criteria that must be considered. The first is whether the workplace truly becomes a smoke-free environment. Success with respect to this goal is relatively easy to measure: it is based on regular supervisors’ reports on violations of the policy within their work areas; monitoring complaints from other employees; and the results of unannounced spot checks of the workplace to reveal the presence or absence of cigarette butts, ashes and smoke-laden air.
The second measure of success, and more difficult to determine, is the number of employees who actually quit smoking and maintain their smoke-free status. While perhaps the most practical position to take is to be concerned only with worksite smoking, such a limited success will bring about fewer long-term benefits, especially with respect to decreasing illness and health care costs. While periodic mandatory saliva tests for cotinine to identify those who continue to smoke would be the best and most objective method for evaluating long-term program success, this is not only complicated and expensive but also is fraught with numerous legal and ethical questions regarding employee privacy. A compromise is the use of annual or semi-annual anonymous questionnaires that ask how individuals’ smoking habits have changed and how long abstinence from smoking has been maintained and that, at the same time, probe changes in employees’ attitudes toward the policy and the program. Such questionnaires have the added advantage of being a means of reinforcing the non-smoking message and of keeping the door open for those still smoking to reconsider dropping the habit.
A final long-term outcome evaluation involves monitoring employee absenteeism, illnesses and health care costs. Any changes would at first be subtle, but over a number of years they should be cumulatively significant. Death benefits paid prior to normal retirement age could be another long-term reflection of the success of the program. Of course, it is important to adjust such data for such factors as changes in the work force, employee characteristics such as age and sex, and other factors affecting the organization. Analysis of these data is manifestly subject to the rules of statistics and would probably be valid only in organizations with a large and stable workforce and adequate data collection, storage and analysis capabilities.
Smoking Control Worldwide
There is a growing worldwide unwillingness to continue to bear the burdens of cigarette smoking and nicotine addiction in terms of their effects on human well-being and productivity, on health and health care costs, and on the economic health of work organizations and nations. This is exemplified by the expanding participation in World No-Tobacco Day that has been spearheaded by the World Health Organization in May of each year since 1987 (WHO 1992).
The aim of this event is not only to ask people to stop smoking for one day but also to trigger interest in controlling smoking among public and private organizations and to promote pressure for the passage of laws, by-laws or regulations advancing the cause of tobacco-free societies. It is also hoped that the relevant agencies will be stimulated to initiate research on specific themes, publish information or initiate action. To this end, each World No-Tobacco Day is assigned a specific theme (table 1); of particular interest to readers of this article is the 1992 Day which addressed “Tobacco-free workplaces: safer and healthier”.
Table 1. Themes of "World No-Tobacco Days"
1992 Tobacco Free Workplaces: safer and healthier
1993 Health Services: our window to a tobacco-free world
1994 The Media and Tobacco: getting the health message across
1995 The Economics of Tobacco: tobacco costs more than you think
1996 Sports and the Arts
1997 United Nations and Specialized Agencies against Tobacco
A problem beginning to be recognized is the increase in cigarette smoking in developing countries where, prompted by the marketing blandishments of the tobacco industry, populations are being encouraged to view smoking as a hallmark of social advancement and sophistication.
Conclusion
The adverse effects of cigarette smoking on individuals and societies are increasingly being recognized and understood (except by the tobacco industry). Nevertheless, smoking continues to enjoy social acceptability and widespread use. A special problem is that many young people become addicted to nicotine years before they are old enough to work.
The workplace is an exceptionally useful arena for combating this health hazard. Workplace policies and programs can have a strong positive influence over the behavior of employees who smoke, abetted by peer pressure from non-smoking coworkers. The wise organization will not only appreciate that control of workplace smoking is something that serves its own self-interest in terms of legal liabilities, absenteeism, production and health-related costs, but will also recognize that it can be a matter of life and death for its employees.
Worksite Nutrition Programmes
Diet, physical activity and other lifestyle practices such as not smoking cigarettes and reduction of stress are important in the prevention of chronic diseases. Proper nutrition and other healthy lifestyle practices also aid in maintaining individual well-being and productivity. The worksite is an ideal place to teach people about good health habits, including sound nutrition, weight control and exercise practices. It is an excellent forum for efficiently disseminating information and monitoring and reinforcing changes that have been made (Kaplan and Brinkman-Kaplan 1994). Nutrition programs rank among the most commonly included activities in wellness programs sponsored by employers, labor unions and, sometimes, jointly. In addition to formal classes and programs, other supportive educational efforts such as newsletters, memos, payroll inserts, posters, bulletin boards, and electronic mail (e-mail) can be offered. Nutrition education materials can also reach employees’ dependants through mailings to the home and making classes and seminars available to homemakers who are the gatekeepers of their families’ food intake practices and habits. These approaches provide useful information that can be applied easily both at the worksite and elsewhere and can help reinforce formal instruction and encourage workers to enroll in programs or make informed and profitable use of worksite facilities (such as the cafeteria). Moreover, carefully targeted materials and classes can have a very significant impact on many people, including the families of workers, especially their children, who can learn and adopt good nutrition practices that will last a lifetime and be passed on to future generations.
Successful worksite intervention programs require a supportive environment that enables workers to act on nutrition messages. In this context, it is essential that employees have access to appropriate foods in cafeterias and vending machines that facilitate adherence to a recommended diet. For those whose lunches depend on “brown bags” or lunch boxes, worksite arrangements for storing the lunch bags or boxes are part of a supportive environment. In addition, employer-provided or entrepreneurial lunch wagons can offer nourishing food on the spot at field worksites remote from feeding facilities. Facilities for light personal washing before eating are also important. These employer-sponsored activities express a strong commitment to the health and well-being of their employees.
In-plant Catering Programs, Vending Machines, and Coffee and Tea Breaks
Many employers subsidize in-plant food services partially or totally, making them attractive as well as convenient. Even where there is only one shift, many cafeterias serve breakfasts and dinners as well as lunches and refreshments at breaks; this is of particular value to those who live alone or whose food preparation in the home may be less than adequate. Some worksite cafeterias are open to employees’ friends and families to encourage “lunching-in” rather than using more expensive and often less nutritionally desirable facilities in the community.
Modifying foods that are offered at the worksite provides support and encouragement of healthy eating patterns (Glanz and Mullis 1988). In fact, cafeteria interventions are one of the most popular worksite nutrition programs as they allow point-of-choice nutrition information to be readily made available (Glanz and Rogers 1994). Other interventions include modifying menu choices to provide low-fat, low-calorie and high-fiber foods or to highlight “heart healthy” foods (Richmond 1986). Worksites also can implement healthy catering policies and offer nutrient-dense foods that are low in fat, cholesterol and sodium (American Dietetic Association 1994). Negotiations can be conducted with food service vendors to also provide low-fat food items, including fruit, in vending machines. One such program resulted in a greater selection by employees of low-calorie foods (Wilber 1983). Food service management, caterers and vendors may realize greater sales and increased participation in the food service activities at the worksite especially when tasty, attractive, healthy foods are served (American Dietetic Association 1994).
Coffee and tea breaks with nutrient-dense snack foods available can help employees meet nutritional needs. Many “lunch hours” are only 30 or 40 minutes long and because some employees use that time for shopping, socializing or personal business, they skip eating. A supportive environment may require lengthening the lunch period. Moreover, maintaining proper hygiene in the in-plant catering facility and ensuring the health and proper training of all food service personnel (even when the facility is operated under contract with an outside vendor) demonstrates the worksite’s commitment to employee health, thereby increasing workers’ interest in supporting the onsite food service establishments as well as other programs.
General Nutrition Guidance
The basic dietary recommendations that have been issued by government agencies of different countries encourage health promotion and the prevention of diet-related, noncommunicable diseases (FAO and WHO 1992). The dietary guidelines adopted include the following principles:
- Adjust energy intake to meet energy expenditure in order to achieve and maintain desirable body weight.
- Avoid excessive fat intake and, especially, intake of saturated fat and cholesterol.
- Increase intake of complex carbohydrates and dietary fibre and limit sugar intake to moderate levels.
- Limit salt intake to a moderate level.
- Limit alcohol intake.
- Offer a variety of foods from all food groups.
There is compelling scientific evidence to support these dietary recommendations. Not only is abnormal body weight a risk factor for many chronic diseases, but fat distribution is also important to health (Bray 1989). Android obesity, or excess fat in the abdomen, is a greater health risk than gynoid obesity, the presence of excess weight below the waist (i.e., in the hips and thighs). A waist-to-hip ratio close to or above one is associated with a greater risk of hypertension, hyperlipidaemia, diabetes and insulin resistance (Seidell 1992). Thus, both body mass index (BMI)—that is, body weight (kilograms) divided by height (meters) squared—and the waist-to-hip ratio are useful in assessing weight status and the need to lose weight. Figure 1 presents BMI classifications of underweight, desirable weight, overweight and obesity.
Figure 1. Body mass index (BMI) classifications.
Essentially everyone, even individuals who are at an ideal body weight, would benefit from nutrition guidance aimed at preventing the weight gain that typically occurs with ageing. An effective weight control program integrates nutrition, exercise, and behavior modification principles and techniques.
A diet that provides less than 30% of calories from fat, less than 10% of calories from saturated fat, and less than 300 milligrams of cholesterol daily is typically recommended to help maintain a desirable blood cholesterol level (i.e., <200 mg/dl) (National Institutes of Health 1993b). Saturated fat and cholesterol raise blood cholesterol levels. A diet relatively low in total fat facilitates achieving the saturated fat recommendation. A 2,000-calorie diet can include 67 grams of total fat and less than 22 grams of saturated fat per day. A diet low in total fat also facilitates reducing calories for weight management and may be implemented by including a variety of foods in the diet so that nutrient needs are met without exceeding calorie needs.
Diets high in complex carbohydrates (the sort of carbohydrate found in grains, legumes, vegetables, and, to some extent, fruits) are also high in many other nutrients (including B vitamins, vitamins A and C, zinc and iron) and low in fat. The recommendation to use sugar in moderation has been made because sugar, despite being a source of energy, has limited nutrient value. Thus, for persons with low calorie needs, sugar should be used sparingly. In contrast, sugar can be used as a source of calories, in moderation, in higher calorie (nutritionally adequate) diets. Although sugar promotes dental caries, it is less cariogenic when consumed with meals than when consumed in frequent between-meal snacks.
Because of the association between sodium intake and systolic hypertension, dietary salt and sodium are recommended only in moderation. A diet that provides not more than 2,400 milligrams of sodium daily is recommended for the prevention of hypertension (National Institutes of Health 1993a). A high-sodium diet also has been shown to promote calcium excretion and, thus, may contribute to the development of osteoporosis, a female-predominant risk (Anderson 1992). The major sources of sodium in the diet include processed foods and salt (or high-sodium condiments such as soy sauce) added to food during cooking or at the table.
If alcohol is consumed, it should be used in moderation. This is because excessive alcohol consumption may cause liver and pancreatic disease, hypertension and damage to the brain and heart. Further adverse consequences associated with heavy alcohol consumption include addiction, increased risk of accidents and impaired job performance.
Another common recommendation is to consume a variety of foods from all food groups. More than 40 different nutrients are required for good health. Since no single food provides all nutrients, including a variety of foods facilitates achieving a nutritionally adequate diet. A typical food guide provides recommendations for the number of “servings” of foods from the different food groups (figure 2). The range of servings listed represents the minimum that should be consumed daily. As energy needs increase, the range should increase correspondingly.
Figure 2. Example of a good daily nutrition guide.
Other specific dietary recommendations have been made by different countries. Some countries recommend water fluoridation, breastfeeding, and iodine supplementation. Many also recommend that protein intake be adequate but that excess protein be avoided. Some have guidelines for the relative proportion of animal to vegetable protein in the diet. Others have emphasized vitamin C and calcium intake. Implicit to these country-specific recommendations is that they are targeted to the special needs identified for a particular area. Other nutritional issues that are important and relevant to individuals worldwide include those relating to calcium, hydration, and antioxidant vitamins and minerals.
An adequate calcium intake is important throughout life to build a strong skeleton and achieve a maximum peak bone mass (bone mass peaks between the ages of 18 and 30) and help retard age-associated bone mass loss that often leads to osteoporosis. At least 800 milligrams of calcium daily is recommended from age one year through old age. For adolescents, when bones are growing rapidly, 1,200 milligrams of calcium per day are recommended. Some authorities believe that young adults, postmenopausal women and men over 65 years of age need 1,500 milligrams of calcium per day and that the diet of all other adults should provide 1,000 milligrams. Pregnant and lactating women need 1,200 milligrams of calcium per day. Dairy products are rich sources of calcium. Low fat dairy products are recommended to control blood cholesterol levels.
Maintaining adequate hydration is essential for achieving maximal work performance. One serious consequence of dehydration is an inability to dissipate heat effectively, with a consequent increase in body temperature. Thirst usually is a good indicator of hydration status, except during heavy physical exertion. Workers always should respond to thirst and drink fluids liberally. Cool, dilute fluids replace water losses fastest. Laborers also should drink fluids liberally; for every 0.5 kilogram of weight lost per day due to exertion, one-half liter of water is recommended to replace the water lost via sweat.
Antioxidants have received a great deal of attention lately because of the growing evidence that suggests they may protect against the development of cancer, heart disease, cataracts and even slow the ageing process. The antioxidant vitamins are beta-carotene and vitamins A, E, and C. The mineral selenium also is an antioxidant. Antioxidants are thought to prevent the formation of harmful free radicals which destroy cell structures over time in a process that leads to the development of various diseases. The evidence to date suggests that antioxidants may protect against the development of cancer, heart disease and cataracts, although a causal relationship has not been established. Food sources of beta-carotene and vitamin A include green leafy vegetables, and red, orange and yellow fruits and vegetables. Grains and fish are significant sources of selenium. Citrus fruits are important sources of vitamin C, and vitamin E is found in sources of polyunsaturated fat, including nuts, seeds, vegetable oil and wheat germ.
The remarkable similarity in the dietary recommendations made by different countries underscores the consensus among nutritionists about the ideal diet for promoting health and well being. The challenge that lies before the nutrition community now is to implement these population-based dietary recommendations and assure proper nutrition globally. This will require not only providing a safe and adequate food supply to all persons everywhere, but also necessitates developing and implementing nutrition education programs worldwide that will teach virtually everyone the principles of a healthy diet.
Cultural and Ethnic Approaches to Foods and Diet
Effective nutrition education approaches must address cultural issues and ethnic food habits. Cultural sensitivity is important in planning nutrition intervention programs and in eliminating barriers to effective communication in individual counseling, as well. Given the current emphasis on cultural diversity, exposure to different cultures in the worksite, and a keen interest among individuals to learn about other cultures, pace-setting nutrition programs that embrace cultural differences should be well received.
Societies have vastly different beliefs about the prevention, cause, and treatment of disease. The value placed on good health and nutrition is highly variable. Helping people adopt healthy nutrition and lifestyle practices requires an understanding of their beliefs, culture and values (US Department of Health and Human Services 1990). Nutrition messages must be targeted to the specific practices of an ethnic population or group. Moreover, the intervention approach must be planned to address widely held beliefs about health and nutrition practices. For example, some cultures disapprove of alcohol whereas others consider it to be an essential part of the diet even when taken with meals eaten at the worksite. Thus, nutrition interventions must be specialized not only to meet the particular needs of a target group, but to embrace the values and beliefs that are unique to their culture.
Overweight
The key environmental factors that contribute to the development of overweight and obesity are principally caloric excess and lack of physical activity.
Overweight and obesity are most often classified on the basis of BMI, which is correlated with body composition (r = 0.7–0.8). Weight status classifications according to BMI for men and women less than 35 and greater than 35 years of age are presented in Figure 10. The health risks associated with overweight and obesity are clear. Data from a number of studies have shown a J-shape relationship between body weight and all-cause mortality. Although the mortality rate increases when BMI exceeds 25, there is a pronounced increase when BMI is greater than 30. Interestingly, underweight also increases risk of mortality, albeit not to the extent as does overweight. Whereas overweight and obese individuals are at higher risk of death due to cardiovascular disease, gallbladder disease and diabetes mellitus, underweight persons are at higher risk for the development of digestive and pulmonary diseases (Lew and Garfinkel 1979). The incidence of overweight and obesity in some developed countries may be as high as 25 to 30% of the population; it is even higher in certain ethnic groups and in groups of low socioeconomic status.
A low caloric diet that leads to a weight loss of 0.2 to 0.9 kilograms (0.5 to 2 pounds) per week is recommended for weight reduction. A low-fat diet (about 30% of calories from fat or lower) that is also high in fiber (15 grams per 1000 calories) is recommended to facilitate decreasing calories and providing bulk for satiety. A weight loss program should include both exercise and behavior modification. A slow, steady weight loss is recommended to successfully modify eating behaviors in order to maintain weight loss. Guidelines for a sound weight-reduction program appear in figure 3.
Figure 3. Guidelines for a sound weight-reduction programme.
A random-digit telephone survey of 60,589 adults across the United States revealed that approximately 38% of women and 24% of men were actively trying to lose weight. Reflecting the marketing efforts of what has become a veritable weight-reduction industry, the methods employed ranged from periodic fasting, participating in organized weight-reduction programs, often with commercially prepared foods and special supplements, and taking diet pills. Only half of those trying to lose weight reported using the recommended method of calorie restriction combined with exercise demonstrating the importance of worksite nutrition education programs (Serdula, Williamson et al. 1994).
Weight loss in overweight or obese persons beneficially affects various chronic disease risk factors (NIH 1993a). Weight loss leads to reductions in blood pressure, plasma lipids and lipoproteins (i.e., total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides) and increases high density lipoprotein (HDL) cholesterol, all of which are major risk factors for coronary heart disease (figure 4). Furthermore, blood glucose, insulin and glycosylated haemoglobin levels are favorably affected. With weight losses as modest as about four kilograms, even when some excess weight is regained, improvements in these parameters have been observed.
Figure 4. Major coronary heart-disease risk factors.
Weight control is essential for reducing chronic disease morbidity and mortality. This has formed the basis of the dietary recommendations of many groups worldwide to achieve and maintain a healthy body weight. These recommendations have been made mainly for developed countries where overweight and obesity are major public health concerns. While diet, exercise, and behavior modification are recommended for weight loss, the key to reducing the incidence of overweight and obesity is to implement effective prevention programs.
Underweight
Underweight (defined as a body weight of 15 to 20% or more below accepted weight standards) is a serious condition that results in a loss of energy and an increased susceptibility to injury and infection. It is caused by an insufficient food intake, excessive activity, malabsorption and poor utilization of food, wasting diseases or psychological stress. High-energy diets are recommended for a gradual, steady weight gain. A diet that provides 30 to 35% of calories from fat and an additional 500 to 1,000 calories per day is recommended. Underweight persons can be encouraged to eat calorie-dense meals and snacks at the worksite by offering them access to a wide variety of palatable, popular foods.
Special Diets
Special diets are prescribed for the treatment of certain diseases and conditions. In addition, dietary modifications should accompany preventive lifestyle and nutrition programs and should be implemented during various stages of the life cycle, such as during pregnancy and lactation. An important aspect of successfully implementing special diets is recognizing that a number of different strategies can be utilized to achieve the nutrient specifications of the special diet. Thus, individualizing diet plans to meet the unique needs of persons is essential for attaining long-term dietary adherence and, thereby, realizing the health benefits of the diet.
Low-fat, low-saturated fat, low-cholesterol diet
The recommended diets for the treatment of an elevated blood cholesterol level are the Step-One diet (<30% of calories from fat, 8 to 10% of calories from saturated fat and <300 milligrams of cholesterol) and the Step-Two diet (<30% of calories from fat, <7% of calories from saturated fat, and <200 milligrams of cholesterol) (NIH 1993b). These diets are designed to progressively reduce intake of saturated fat and cholesterol and to decrease total fat intake. The major sources of fat in the diet are meat, poultry; full-fat dairy products and fats and oils. In general, for most persons in developed countries, adherence to a Step-One diet requires reducing total fat and saturated fat by about 20 to 25%, whereas following a Step-Two diet requires decreasing total fat similarly but decreasing saturated fat by approximately 50%. A Step-One diet can be achieved rather easily by applying one or more fat reduction strategies to the diet, such as substituting lean meat, poultry and fish for higher-fat varieties, substituting low-fat and skim milk products for full-fat dairy products, using less fat in food preparation and adding less fat to food prior to consumption (e.g., butter, margarine or salad dressing) (Smith-Schneider, Sigman-Grant and Kris-Etherton 1992). A Step-Two diet requires more careful diet planning and the intensive nutrition education efforts of a qualified nutritionist.
Very low-fat diet
A diet that provides 20% or less of calories from fat is recommended by some nutritionists for the prevention of certain cancers that have been associated with diets high in fat (Henderson, Ross and Pike 1991). This diet is rich in fruits and vegetables, grains, cereals, legumes and skim milk dairy products. Red meat can be used sparingly, as can fats and oils. Foods are prepared with little or no added fat and are cooked by baking, steaming, boiling or poaching.
A diet that provides minimal amounts of saturated fat (3% of calories) and total fat (10% of calories), together with major lifestyle changes (smoking cessation, exercise and meditation) has been shown to result in the regression of atherosclerosis (Ornish et al. 1990). This particular diet requires major lifestyle changes (i.e., a change in habitual cuisine), including adopting a largely vegetarian diet and using meat, fish and poultry as a condiment, if at all, and emphasizing grains, legumes, fruits, vegetables, and skim milk dairy products. Adherence to this diet can require the purchase of special foods (fat-free products) while avoiding most commercially prepared foods. While this regimen is an option for some persons at high risk for cardiovascular disease, especially as an alternative to drug therapy, it requires a very high level of motivation and commitment.
Diet for workers with diabetes
An individually developed dietary prescription based on metabolic, nutrition, and lifestyle requirements is recommended (American Dietetic Association 1994). In general, dietary protein provides 10 to 20% of calories. Saturated fat should account for less than 10% of total caloric intake. The distribution of remaining energy from carbohydrate and fat varies according to the patient’s condition and reflects the specific glucose, lipid and weight outcomes chosen for him or her. For those who are at or close to ideal weight, 30% of calories from fat is recommended. For overweight persons, a reduction in total fat facilitates reducing calories, resulting in a corresponding weight loss. For persons who have an elevated triglyceride level, a diet higher in total fat, and, in particular, monounsaturated fat is recommended, together with close supervision; the higher-fat diet may perpetuate or aggravate obesity. The new model for the medical nutrition therapy for diabetes includes assessment of the individual’s metabolic and lifestyle parameters, an intervention plan and monitoring therapeutic outcomes.
Diet for pregnancy and lactation
Pregnancy and lactation represent periods when both energy and nutrient demands are high. For pregnancy, a diet should provide sufficient calories for adequate weight gain (National Research Council 1989). The calories and nutrients needed to maximally support pregnancy and lactation for as long as several years during multiple pregnancies and lengthy lactation periods can be obtained from a diet that includes the basic food groups. Other recommendations for both pregnant and lactating women include selecting a variety of foods from each food group, consuming regular meals and snacks, and including ample dietary fiber and fluid. Alcoholic beverages should be avoided or at least markedly restricted by pregnant and lactating women. Salt to taste is also recommended for pregnant women. An adequate diet during pregnancy and lactation is essential to assure normal fetal and infant growth and development and maternal health and well-being, and should be emphasized in worksite nutrition education programs and catering facilities.
Lactose Intolerance and Gluten Sensitivity
Many adults, especially those of certain ethnic groups, must restrict lactose in their diet due to a lactase deficiency. The major source of lactose in the diet is dairy products and foods prepared with them. It is important to note that the excipient in many medications is lactose, a circumstance that could pose problems to those who take a number of medications. For the small number of people who have a gluten sensitivity (coeliac disease), foods containing gluten must be eliminated from the diet. Sources of gluten in the diet include wheat, rye, barley and oats. Whereas many individuals with a lactose intolerance can tolerate small amounts of lactose, especially when eaten with foods that do not contain lactose, persons with a gluten sensitivity must avoid any food that contains gluten. Worksite catering facilities should have appropriate foods available if there are employees with these special conditions.
Summary
The worksite is an ideal setting for implementing nutrition programs aimed at teaching the principles of good nutrition and their application. There is a variety of programs that can be developed for the worksite. In addition to providing classes and nutrition education materials for all employees, special programs can be targeted to workers at high risk for different chronic diseases or for selected groups based on ethnic or demographic characteristics. Chronic disease risk reduction requires a long-term commitment by both workers and their employers. Effective worksite nutrition programs are beneficial in reducing the risk of chronic diseases in countries worldwide.
Physical Training and Fitness Programmes: An Organizational Asset
Physical training and fitness programs are generally the most frequently encountered element in worksite health promotion and protection programs. They are successful when they contribute to the goals of the organization, promote the health of employees, and remain pleasing and useful to those participating (Dishman 1988). Because organizations around the world have widely diverse goals, workforces and resources, physical training and fitness programs vary greatly in how they are organized and in what services they provide.
This article is concerned with the reasons for which organizations offer physical training and fitness programs, how such programs fit within an administrative structure, the typical services offered to participants, the specialized personnel who offer these services, and the issues most often involved in worksite fitness programming, including the needs of special populations within the workforce. It will focus primarily on programs conducted onsite in the workplace.
Quality and Fitness Programming
Today’s global economy shapes the goals and business strategies of tens of thousands of employers and affects millions of workers around the world. Intense international competition requires organizations to offer products and services of higher value at ever lower costs, that is, to pursue so-called “quality” as a goal. Quality-driven organizations expect workers to be “customer oriented,” to work energetically, enthusiastically and accurately throughout the entire day, to continually train and improve themselves professionally and personally, and to take responsibility for both their workplace behavior and their personal well-being.
Physical training and fitness programs can play a role in quality-driven organizations by helping workers to achieve a high level of “wellness”. This is particularly important in “white-collar” industries, where employees are sedentary. In manufacturing and heavier industries, strength and flexibility training can enhance work capacity and endurance and protect workers from occupational injuries. In addition to physical improvement, fitness activities offer relief from stress and carry a personal sense of responsibility for health into other aspects of lifestyle such as nutrition and weight control, avoidance of alcohol and drug abuse, and smoking cessation.
Aerobic conditioning, relaxation and stretching exercises, strength training, adventure and challenge opportunities and sports competitions are typically offered in quality-driven organizations. These offerings are often structured within the organization’s wellness initiatives—“wellness” involves helping people to actualize their full potential while leading a lifestyle that promotes health—and they are based on the awareness that, since sedentary living is a well-demonstrated risk factor, regular exercise is an important habit to foster.
Basic Fitness Services
Participants in fitness programs should be instructed in the rudiments of fitness training. The instruction includes the following components:
- a minimum number of exercise sessions per week to achieve fitness and good health (three or four times a week for 30 to 60 minutes per session)
- learning how to warm up, exercise and cool down
- learning how to monitor heart rate and how to safely raise one’s heart rate to a training level appropriate for one’s age and fitness level
- graduating training from light to heavy to ultimately achieve a high level of fitness
- techniques for cross training
- The principles of strength training, including resistance and overload, and combining repetitions and sets to achieve strengthening goals
- strategic rest and safe lifting techniques
- relaxation and stretching as an integral part of a total fitness programme
- learning how to customize workouts to suit one’s personal interests and lifestyle
- achieving an awareness of the role that nutrition plays in fitness and overall good health.
Besides instruction, fitness services include fitness assessment and exercise prescription, orientation to the facility and training in the use of the equipment, structured aerobic classes and activities, relaxation and stretching classes, and back-pain prevention classes. Some organizations offer one-on-one training, but this can be quite expensive since it is so staff-intensive.
Some programs offer special “work hardening” or “conditioning,” that is, training to enhance workers’ capacities to perform repetitive or rigorous tasks and to rehabilitate those recovering from injuries and illnesses. They often feature work breaks for special exercises to relax and stretch overused muscles and strengthen antagonistic sets of muscles to prevent overuse and repetitive injury syndromes. When advisable, they include suggestions for modifying the job content and/or the equipment used.
Physical Training and Fitness Personnel
Exercise physiologists, physical educators, and recreational specialists make up the majority of the professionals working in worksite physical fitness programs. Health educators and rehabilitation specialists also participate in these programs.
The exercise physiologist designs personalized exercise regimens for individuals based on a fitness assessment which generally includes a health history, a health risk screening, assessment of fitness levels and exercise capacity (essential for those with handicaps or recovering from injury), and confirmation of their fitness goals. The fitness assessment includes the determination of resting heart rate and blood pressure, body composition. muscle strength and flexibility, cardiovascular efficiency and, often, blood lipid profiles. Typically, the findings are compared with norms for people of the same sex and age.
None of the services offered by the physiologist are meant to diagnose disease; employees are referred to the employee health service or their personal physicians when abnormalities are found. In fact, many organizations require that a prospective applicant obtain clearance from a physician before joining the program. In the case of employees recovering from injuries or illness, the physiologist will work closely with their personal physicians and rehabilitation counselors.
Physical educators have been trained to lead exercise sessions, to teach the principles of healthy and safe exercise, to demonstrate and coach various athletic skills, and to organize and administer a multifaceted fitness program. Many have been trained to perform fitness assessments although, in this age of specialization, that task is performed more often by the exercise physiologist.
Recreational specialists carry out surveys of participants’ needs and interests to determine their lifestyles and their recreational requirements and preferences. They may conduct exercise classes but generally focus on arranging trips, contests and activities that instruct, physically challenge and motivate participants to engage in wholesome physical activity.
Verifying the training and competence of physical training and fitness personnel often presents problems to organizations seeking to staff a program. In the United States, Japan and many other countries, government agencies require academic credentials and supervised experience of physical educators who teach in school systems. Most governments do not require certification of exercise professionals; for example, in the United States, Wisconsin is the only state that has enacted legislation dealing with fitness instructors. In considering an involvement with health clubs in the community, whether voluntary like the YMCAs or commercial, special caution should be taken to verify the competence of the trainers they provide since many are staffed by volunteers or poorly trained individuals.
A number of professional associations offer certification for those working in the adult fitness field. For example, the American College of Sports Medicine offers a certificate for exercise instructors and the International Dance Education Association offers a certificate for aerobics instructors. These certificates, however, represent indicators of experience and advanced training rather than licenses to practice.
Fitness Programs and the Organization’s Structure
As a rule, only medium-sized to large-sized organizations (500 to 700 employees is generally considered the minimum) can undertake the task of providing physical training facilities for their employees at the worksite. Major considerations other than size include the ability and willingness to make the necessary budgetary allocations and availability of space to house the facility and whatever equipment it may require, including dressing and shower rooms.
Administrative placement of the program within the organization usually reflects the goals set for it. For example, if the goals are primarily health-related (e.g., cardiovascular risk reduction, reducing illness absences, prevention and rehabilitation of injuries, or contributing to stress management) the program will usually be found in the medical department or as a supplement to the employee health service. When the primary goals relate to employee morale and recreation, it will usually be found in the human resources or employee relations department. Since human resources departments are usually charged with implementing quality improvement programs, fitness programs with a wellness and quality focus will often be located there.
Training departments rarely are assigned responsibility for physical training and fitness programs since their mission is usually limited to specific skill development and job training. However, some training departments offer outdoor adventure and challenge opportunities to employees as ways to create a sense of teamwork, build self-confidence and explore ways to overcome adversity. When jobs involve physical activity, the training program may be responsible for teaching proper work techniques. Such training units will often be found in police, fire and rescue organizations, trucking and delivery firms, mining operations, oil exploration and drilling companies, diving and salvage organizations, construction firms, and the like.
Onsite or Community-based Fitness Programs
When space and economic considerations do not allow comprehensive exercise facilities, limited programs may still be conducted in the workplace. When not in use for their designed purposes, lunch and meeting rooms, lobbies and parking areas may be used for exercise classes. One New York City-based insurance company created an indoor jogging track in a large storage area by arranging a path between banks of filing cabinets containing important but infrequently consulted documents. In many organizations around the world, work breaks are regularly scheduled during which employees stand at their work stations and do calisthenics and other simple exercises.
When onsite fitness facilities are not feasible (or when they are too small to accommodate all the employees who would use them), organizations turn to community-based settings such as commercial health clubs, schools and colleges, churches, community centers, clubs and YMCAs, town- or union-sponsored recreation centers, and so on. Some industrial parks house an exercise facility shared by the corporate tenants.
On another level, fitness programs may consist of uncomplicated physical activities practiced in or about the home. Recent research has established that even low to moderate levels of daily activity may have protective health effects. Activities like recreational walking, biking or stair-climbing which require the person to dynamically exercise large muscle groups for 30 minutes five times a week, may prevent or delay the advance of cardiovascular disease while providing a pleasant respite from daily stress. Programs that encourage walking and bicycling to work can be developed for even very small companies and they cost very little to implement.
In some countries, workers are entitled to leaves that may be spent at spas or health resorts which offer a comprehensive program of rest, relaxation, exercise, healthful diet, massage and other forms of restorative therapy. The aim, of course, is to have them maintain such a healthful lifestyle after they return to their homes and jobs.
Exercise for Special Populations
Older workers, the obese and especially those who have been sedentary for long can be offered low-impact and low-intensity exercise programs in order to avert orthopedic injuries and cardiovascular emergencies. In onsite facilities, special times or separate workout spaces may be arranged to protect the privacy and dignity of these populations.
Pregnant women who have been physically active may continue to work or exercise with the advice and consent of their personal physicians, keeping in mind the medical guidelines concerning exercise during pregnancy (American College of Obstetricians and Gynecologists 1994). Some organizations offer special reconditioning exercise programs for women returning to work after delivery.
Physically challenged or handicapped workers should be invited to participate in the fitness program both as a matter of equity and because they may accrue even greater benefits from the exercise. Program staff, however, should be alert to conditions that may entail greater risk of injury or even death, such as Marfan’s syndrome (a congenital disorder) or certain forms of heart disease. For such individuals, preliminary medical evaluation and fitness assessment is particularly important, as is careful monitoring while exercising.
Setting Goals for the Exercise Program
The goals selected for an exercise program should complement and support those of the organization. Figure 1 presents a checklist of potential program goals which, when ranked in order of importance to a particular organization and aggregated, will help in shaping the program.
Figure 1. Suggested organizational goals for a fitness and exercise programme.
Eligibility for the Exercise Program
Since the demand may exceed both the program’s budget allocation and the available space and time, organizations have to carefully consider who should be eligible to participate. It is prudent to know in advance why this benefit is being offered and how many employees are likely to take advantage of it. Lack of preparation in this regard may lead to embarrassment and ill will when those who desire to exercise cannot be accommodated.
Particularly when providing an onsite facility, some organizations limit eligibility to managers above a certain level in the organization chart. They rationalize this by arguing that, since such individuals are paid more, their time is more valuable and it is proper to give them priority of access. The program then becomes a special privilege, like the executive dining room or a conveniently located parking space. Other organizations are more even-handed and offer the program to all on a first-come, first-served basis. Where demand exceeds the facility’s capacity, some use length of service as a criterion of priority. Rules setting minimum monthly use are sometimes used to help manage the space problem by discouraging the casual or episodic participant from continuing as a member.
Recruiting and Retaining Program Participants
One problem is that the convenience and low cost of the facility may make it particularly attractive to those already committed to exercise, who may leave little room for those who may need it much more. Most of the former will probably continue to exercise anyway while many of the latter will be discouraged by difficulties or delays in entering the program. Accordingly, an important adjunct to recruiting participants is simplifying and facilitating the enrolment process.
Active efforts to attract participants are usually necessary, at least when the program is initiated. They include in-house publicity via posters, flyers and announcements in available intramural communications media, as well as open visits to the exercise facility and the offer of experimental or trial memberships.
The problem of dropout is an important challenge to program administrators. Employees cite boredom with exercise, muscular aches and pains induced by exercise, and time pressure as the major reasons for dropping out. To counter this, facilities entertain members with music, videotapes and television programs, motivational games, special events, awards such as T-shirts and other gifts and certificates for attendance or reaching individual fitness goals. Properly designed and supervised exercise regimens will minimize injuries and aches and pains and, at the same time, make the sessions efficient and less time-consuming. Some facilities offer newspapers and business publications as well as business and training programs on television and videotape to be accessed while exercising to help justify the time spent in the facility.
Safety and Supervision
Organizations offering worksite fitness programs must do so in a safe manner. Potential members must be screened for medical conditions that might be affected adversely by exercise. Only well-designed and well-maintained equipment should be available and participants must be properly instructed in its use. Safety signs and rules on the appropriate use of the facility should be posted and enforced, and all staff should be trained in emergency procedures, including cardiopulmonary resuscitation. A trained exercise professional should oversee the operation of the facility.
Record Keeping and Confidentiality
Individual records containing information about health and physical status, fitness assessment and exercise prescription, fitness goals and progress toward their accomplishment and any relevant notes should be maintained. In many programs, the participant is allowed to chart for himself or herself what was done on each visit. At a minimum, the content of records should be kept secure from all but the individual participant and members of the program staff. Except for the staff of the employee health service, who are bound to the same rules of confidentiality and, in an emergency, the participant’s personal physician, details of the individual’s participation and progress should not be revealed to anyone without the individual’s express consent.
Program staff may be required to make periodic reports to management presenting aggregate data regarding participation in the program and the results.
Whose Time, Who Pays?
Since most worksite exercise programs are voluntary and established to benefit the worker, they are considered an extra benefit or privilege. Accordingly, the organization traditionally offers the program on the worker’s own time (during lunch time or after hours) and he or she is expected to pay all or part of the cost. This is generally applicable also to programs provided offsite in community facilities. In some organizations, the employees’ contributions are indexed to salary level and some offer “scholarships” to those who are low paid or those with financial problems.
Many employers allow participation during working hours, usually for higher-level employees, and pick up most if not all of the cost. Some refund employees’ contributions if certain attendance or fitness goals are attained.
When program participation is mandatory, as in training to prevent potential work injuries or to condition workers to perform certain tasks, government regulations and/or labor union agreements require it to be provided during work hours with all costs borne by the employer.
Managing Participants’ Aches and Pains
Many people believe that exercise must be painful in order to be beneficial. This is frequently expressed by the motto “No pain, no gain”. It is incumbent on the program staff to counter this erroneous belief by changing the perception of exercise through awareness campaigns and educational sessions and by ensuring that the intensity of the exercises is graduated so that they remain pain-free and enjoyable while still improving the participant’s level of fitness.
If participants complain of aches and pains, they should be encouraged to continue to exercise at a lower level of intensity or simply to rest until healed. They should be taught “RICE,” the acronym for the principles of treating sports injuries: Rest; Ice down the injury; Compress any swelling; and Elevate the injured body part.
Sports Programs
Many organizations encourage employees to participate in company-sponsored athletic events. These may range from softball or football games at the yearly company picnic, to intramural league play in a variety of sports, to inter-company competitions such as the Chemical Bank’s Corporate Challenge, a competitive distance run for teams of employees from participating organizations that originated in New York City and now has spread to other areas, with many more corporations joining as sponsors.
The key concept for sports programs is risk management. While the gains from competitive sports can be considerable, including better morale and stronger “team” feelings, they inevitably entail some risks. When workers engage in competition, they may bring to the game work-related psychological “baggage” that can cause problems, particularly if they are not in good physical condition. Examples include the middle-aged, out-of-shape manager who, seeking to impress younger subordinates, may be injured by exceeding his or her physical capabilities, and the worker who, feeling challenged by another in competing for status in the organization, may convert what is meant to be a friendly game into a dangerous, bruising mêlée.
The organization wishing to offer involvement in competitive sports should seriously consider the following advice:
- Be sure that participants understand the purpose of the event and remind them that they are employees of the organization and not professional athletes.
- Establish firm rules and guidelines governing safe and fair play.
- Although signed informed consent and waiver forms do not always protect the organization from liability in the event of injury, they help participants to comprehend the extent of the risk associated with the sport.
- Offer conditioning clinics and practice sessions prior to the opening of the competition so that participants can be in good physical shape when they begin to play.
- Require, or at least encourage, a complete physical examination by the employee’s personal physician if not available in the employee health service. (Note: the organization may have to accept financial responsibility for this.)
- Perform a safety inspection of the athletic field and all of the sports equipment. Provide or require personal protective equipment such as helmets, clothing, safety pads and goggles.
- Make sure that referees and security personnel as needed are on hand for the event.
- Have first aid supplies on hand and a pre-arranged plan for emergency medical care and evacuation if needed.
- Be sure that the organization’s liability and disability insurance coverage covers such events and that it is adequate and in force. (Note: it should cover employees and others who attend as spectators as well as those on the team.)
For some companies, sports competition is a major source of employee disability. The above recommendations indicate that the risk may be “managed,” but serious thought should be given to the net contribution that sports activities can reasonably be expected to provide to the physical fitness and training program.
Conclusion
Well-designed, professionally managed workplace exercise programs benefit employees by enhancing their health, well-being, morale and work performance. They benefit organizations by improving productivity qualitatively and quantitatively, preventing work-related injuries, accelerating employees’ recovery from illness and injury, and reducing absenteeism. The design and implementation of each program should be individualized in accord with the characteristics of the organization and its workforce, with the community in which it operates, and with the resources that can be made available for it. It should be managed or at least supervised by a qualified fitness professional who will consistently be mindful of what the program contributes to its participants and to the organization and who will be ready to modify it as new needs and challenges arise.
Health Risk Appraisal
Introduction
Over the last few decades, the health risk appraisal (HRA), also known as a health hazard appraisal or a health risk assessment, has become increasingly popular, primarily in the United States, as an instrument for promoting health awareness and motivating behavioral change. It is also used as an introduction to periodic health screening or as a substitute for it and, when aggregated for a group of individuals, as the basis for identifying targets for a health education or health promotion program to be designed for them. It is based on the following concept:
- Ostensibly healthy, asymptomatic individuals may be at risk of developing a disease process that can cause morbidity in the future and may lead to premature death.
- Factors that lead to such risk can be identified.
- Some of those risk factors can be eliminated or controlled thereby preventing or attenuating the disease process and preventing or delaying the morbidity and mortality.
The development of the HRA in the 1940s and 1950s is credited to Dr. Lewis Robbins, working at the Framingham prospective study of heart disease and later at the National Cancer Institute (Beery et al. 1986). The 1960s saw additional models developed and, in 1970, Robbins and Hall produced the seminal work that defined the technique, described the survey instruments and the risk computations, and outlined the patient feedback strategy (Robbins and Hall 1970).
Interest in HRA and health promotion in general was stimulated by a growing awareness of the importance of risk factor control as a basis element in health promotion, the evolving use of computers for data compilation and analysis and, especially in the United States, increasing concern over the escalating cost of health care and the hope that preventing illness might slow its upward spiral of growth. By 1982, Edward Wagner and his colleagues at the University of North Carolina were able to identify 217 public and private HRA vendors in the United States (Wagner et al. 1982). A good many of these have since faded from the scene but they have been replaced, at least to a limited extent, by new entrants into the marketplace. According to a 1989 report of a survey of a random sample of US worksites, 29.5% have conducted HRA activities; for worksites with more than 750 employees, this figure rose to 66% (Fielding 1989). HRA use in other countries has lagged considerably.
What is the HRA?
For purposes of this article, an HRA is defined as a tool for assessing health risks that has three essential elements:
- A self-administered questionnaire inquiring about the individual’s demographic profile, medical background, family history, personal habits and lifestyle. This information is frequently supplemented by biomedical measurements such as height, weight, blood pressure, and skin-fold thickness, and data regarding the results of urinalysis, blood cholesterol level and other laboratory tests, either as reported by the individual or taken as part of the process.
- A quantitative estimation of the individual’s future risk of death or other adverse outcomes from specific causes based on a comparison of the individual’s responses to epidemiological data, national mortality statistics and actuarial calculations. Some questionnaires are self-scored: points are assigned to the response to each question and then added to derive a risk score. With the appropriate computer software, the responses may be entered into a microcomputer that will calculate the score. Most often the completed questionnaires are forwarded to a central point for batch processing and the individual results are mailed or delivered to the participants.
- Feedback to the individual with suggestions for changes in lifestyle and other actions that would improve well-being and reduce the risk of disease or premature death.
Originally, the total risk estimate was presented as a single number that could be targeted for reduction to a “normal” value or even to lower-than-normal values (vis-à-vis the general population) by implementing the suggested behavioral changes. To make the results more graphic and compelling, the risk is now sometimes expressed as a “health age” or “risk age” to be compared with the individual’s chronological age, and an “achievable age” as the target for the interventions. For example, a report might say, “Your present age is 35 but you have the life expectancy of a person aged 42. By following these recommendations, you could reduce your risk age to 32, thereby adding ten years to your projected life span.”
Instead of comparing the individual’s health status with the “norm” for the general population, some HRAs offer an “optimal health” score: the best attainable score that might be achieved by following all of the recommendations. This approach appears to be particularly useful in guiding young people, who may not yet have accumulated significant health risks, to an optimally desirable lifestyle.
The use of a “risk age” or a single number to represent the individual’s composite risk status may be misleading: a significant risk factor may be statistically offset by “good” scores on most other areas and lead to a false sense of security. For example, a person with normal blood pressure, a low blood cholesterol level, and a good family history who exercises and wears automobile seat belts may earn a good risk score despite the fact that he smokes cigarettes. This suggests the desirability of focusing on each “greater than average” risk item instead of relying on the composite score alone.
The HRA is not to be confused with health status questionnaires that are used to classify the eligibility of patients for particular treatments or to evaluate their outcomes, nor with the variety of instruments used to assess degree of disability, mental health, health distress or social functioning, although such scales are sometimes incorporated into some HRAs.
HRA Questionnaire
Although the HRA is sometimes used as a prelude to or part of a periodic, pre-employment or pre-placement medical examination, it is usually offered independently as a voluntary exercise. Many varieties of HRA questionnaires are in use. Some are limited to core questions that feed directly into the risk age calculations. In others, these core questions are interspersed with additional medical and behavioral topics: more extensive medical history; stress perceptions; scales to measure anxiety, depression and other psychological disorders; nutrition; use of preventive services; personal habits and even interpersonal relationships. Some vendors allow purchasers to add questions to the questionnaire, although responses to these are not usually incorporated into the health-risk computations.
Almost all HRAs now use forms with boxes to be checked or filled in by pencil for computer entry by hand or by an optical scanner device. As a rule, the completed questionnaires are collected and batch-processed, either in-house or by the HRA vendor. To encourage trust in the confidentiality of the program, completed questionnaires are sometimes mailed directly to the vendor for processing and the reports are mailed to the participants’ homes. In some programs, only “normal” results are mailed to participants, while those employees with results calling for intervention are invited for private interviews with trained staff persons who interpret them and outline the corrective actions that are indicated. Greater access to personal computers and more widespread familiarity with their use have led to the development of interactive software programs that allow direct entry of the responses into a microcomputer and immediate calculation and feedback of the results along with risk reduction recommendations. This approach leaves it up to the individual to take the initiative of seeking help from a staff person when clarification of the results and their implications is needed. Except when the software program allows storage of the data or their transfer to a centralized data bank, this approach does not provide information for systematic follow-up and it precludes the development of aggregate reports.
Managing the Program
Responsibility for managing the HRA program is usually assigned to the respective directors of the employee health service, the wellness program or, less frequently, the employee assistance program. Quite often, however, it is arranged and supervised by the personnel/human resources staff. In some instances, an advisory committee is created, often with employee or labor union participation. Programs incorporated into the organization’s operating routine appear to run more smoothly than those that exist as somewhat isolated projects (Beery et al. 1986). The organizational location of the program may be a factor in its acceptance by employees, particularly when confidentiality of personal health information is an issue. To preclude such a concern, the completed questionnaire is usually mailed in a sealed envelope to the vendor, who processes the data and mails the individual report (also in a sealed envelope) directly to the participant’s home.
To enhance participation in the program, most organizations publicize the program through preliminary hand-outs, posters and articles in the company newsletter. Occasionally, incentives (e.g., T-shirts, books and other prizes) are offered for completion of the exercise and there may even be monetary awards (e.g., reduction in the employee’s contribution to health insurance premiums) for successful reduction of excess risk. Some organizations schedule meetings where employees are told about the program’s purposes and procedures and are instructed in completing the questionnaire. Some, however, simply distribute a questionnaire with written instructions to each employee (and, if included in the program, to each dependant). In some instances, one or more reminders to complete and mail the questionnaire are distributed in order to increase participation. In any case, it is important to have a designated resource person, either in the organization or with the HRA program provider, to whom questions can be directed in person or by telephone. It may be important to note that, even when the questionnaire is not completed and returned, merely reading it can reinforce information from other sources and foster a health consciousness that may favorably influence future behavior.
Many of the forms call for clinical information that the respondent may or may not have. In some organizations, the program staff actually measures height, weight, blood pressure and skin-fold thickness and collects blood and urine samples for laboratory analysis. The results are then integrated with the questionnaire responses; where such data are not entered, the computer processing program may automatically insert figures representing the “norms” for persons of the same sex and age.
Turnaround time (the time between completing the questionnaire and receiving the results) may be a significant factor in the value of the program. Most vendors promise delivery of the results in ten days to two weeks, but batch processing and post office delays may extend this period. By the time the reports are received, some participants may have forgotten how they responded and may have disassociated themselves from the process; to obviate this possibility, some vendors either return the completed questionnaire or include key responses of the individual in the report.
Reports to the Individual
The reports may vary from a single-page statement of results and recommendations to a more than 20-page brochure replete with multicolor graphs and illustrations and extended explanations of the relevance of the results and the importance of the recommendations. Some rely almost entirely on preprinted general information while in others the computer generates an entirely individualized report. In some programs where the exercise has been repeated and the earlier data have been retained, comparisons of current results with those recorded earlier are provided; this may provide a sense of gratification that can serve as further motivation for behavior modification.
A key to the success of a program is the availability of a health professional or trained counselor who can explain the importance of the findings and offer an individualized program of interventions. Such personalized counseling can be extremely useful in allaying needless anxiety that may have been generated by misinterpretation of the results, in helping individuals establish behavioral change priorities, and in referring them to resources for implementation.
Reports to the Organization
In most programs, the individual results are summarized in an aggregate report sent to the employer or sponsoring organization. Such reports tabulate the demography of the participants, sometimes by geographic location and job classification, and analyze the range and levels of health risks discovered. A number of HRA vendors include projections of the increased health care costs likely to be incurred by high-risk employees. These data are extremely valuable in designing elements for the organization’s wellness and health promotion program and in stimulating consideration of changes in job structure, work environment and workplace culture that will promote the health and well-being of the workforce.
It should be noted that the validity of the aggregate report depends on the number of employees and the level of participation in the HRA program. Participants in the program tend to be more health conscious and, when their number is relatively small, their scores may not accurately reflect the characteristics of the entire workforce.
Follow-up and Evaluation
The effectiveness of the HRA program may be enhanced by a system of follow-up to remind participants of the recommendations and encourage compliance with them. This can involve individually addressed memoranda, one-on-one counseling by a physician, nurse or health educator, or group meetings. Such follow-up is particularly important for high-risk individuals.
HRA program evaluation should start with a tabulation of the level of participation, preferably analyzed by such characteristics as age, sex, geographic location or work unit, job and educational level. Such data may identify differences in acceptance of the program that might suggest changes in the way it is presented and publicized.
Increased participation in risk-reduction elements of the wellness program (e.g., a fitness program, smoking cessation courses, stress management seminars) may indicate that HRA recommendations are being heeded. Ultimately, however, evaluation will involve determination of changes in risk status. This may involve analyzing the results of the follow-up of high-risk individuals or repetition of the program after an appropriate interval. Such data may be fortified by correlation with data such as utilization of health benefits, absenteeism or productivity measures. Appropriate recognition, however, should be given to other factors that may have been involved (e.g., bias reflecting the sort of person who returns for retest, regression to the mean, and secular trends); truly scientific evaluation of the program impact requires a randomized prospective clinical trial (Schoenbach 1987; DeFriese and Fielding 1990).
Validity and Utility of the HRA
Factors that may affect the accuracy and validity of an HRA have been discussed elsewhere (Beery et al. 1986; Schoenbach 1987; DeFriese and Fielding 1990) and will only be listed here. They represent a checklist for workplace decision makers evaluating different instruments, and include the following:
- accuracy and consistency of self-reported information
- completeness and quality of the epidemiological and actuarial data on which the risk estimates are based
- limitations of the statistical methods for calculating risk, including combining risk factors for different problems into a single composite score and the distortions produced by substituting “average” values either for missing responses in the questionnaire or for measurements not taken
- reliability of the method for calculating the benefits of risk reduction
- applicability of the same mortality calculations to the young whose death rates are low and to older individuals for whom age alone may be the most significant factor in mortality. Furthermore, the validity of the HRA when applied to populations different from those on whom most of the research has been done (i.e., women, minorities, people of different educational and cultural backgrounds) must be regarded from a critical point of view.
Questions have also been raised about the utility of the HRA based on considerations such as the following:
- The primary focus of HRA is on life expectancy. Until recently, little or no attention has been paid to factors primarily influencing morbidity from conditions that are not usually fatal but which may have an even greater impact on well-being, productivity and health-related costs (e.g., arthritis, mental disorders, and long-term effects of treatments intended to reduce specific risks). The problem is the lack of good morbidity databases for the general population, to say nothing of subgroups defined by age, sex, race or ethnicity.
- Concern has been expressed about the ill effects of anxiety generated by reports of high-risk status reflecting factors which the individual is unable to modify (e.g., age, heredity, and past medical history), and about the possibility that reports of “normal” or low-risk status may lead individuals to ignore potentially significant signs and symptoms that were not reported or which developed after the HRA was completed.
- Participation in an HRA programme is usually voluntary, but allegations of coercion to participate or to follow the recommendations have been made.
- Charges of “blaming the victim” have rightfully been levelled at employers who offer HRA as part of a health promotion programme but do little or nothing to control health risks in the work environment.
- Confidentiality of personal information is an ever-present concern, especially when an HRA is conducted as an in-house programme and abnormal findings appear to be a trigger for discriminatory actions.PP9
Evidence of the value of health-risk reduction has been accumulating. For example, Fielding and his associates at Johnson and Johnson Health Management, Inc., found that the 18,000 employees who had completed the HRA provided through their employers used preventive services at a considerably higher rate than a comparable population responding to the National Health Interview Survey (Fielding et al. 1991). A five-year study of almost 46,000 DuPont employees demonstrated that those with any of the six behavioral cardiovascular risk factors identified by an HRA (e.g., cigarette smoking, high blood pressure, high cholesterol levels, lack of exercise) had significantly higher rates of absenteeism and use of health care benefits as compared to those without such risk factors (Bertera 1991). Furthermore, applying multivariate regression models to 12 health-related measures taken mainly from an HRA allowed Yen and his colleagues at the University of Michigan Fitness Research Center to predict which employees would generate higher costs for the employer for medical claims and absenteeism (Yen, Edington and Witting 1991).
Implementing an HRA Program
Implementing an HRA program is not a casual exercise and should not be undertaken without careful consideration and planning. The costs of an individual questionnaire and its processing may not be great but the aggregate costs to the organization may be considerable when such items as staff time for planning, implementation and follow-up, employee time for completing the questionnaires, and adjunct health-promotion programs are included. Some factors to be considered in implementation are presented in figure 1.
Figure 1. Checklist for health risk appraisal (HRA) implementation.
Should we have an HRA program?
An increasing number of companies, at least in the United States, are answering this question in the affirmative, abetted by the growing number of vendors energetically marketing HRA programs. The popular media and “trade” publications are replete with anecdotes describing “successful” programs, while in comparison there is a paucity of articles in professional journals offering scientific evidence of the accuracy of their results, their practical reliability and their scientific validity.
It seems clear that defining one’s health risk status is a necessary basis for risk reduction. But, some ask, does one need a formal exercise like the HRA to do this? By now, virtually everyone who persists in cigarette smoking has been exposed to evidence of the potential of adverse health effects, and the benefits of proper nutrition and physical fitness have been well publicized. Proponents of HRA counter by pointing out that receiving an HRA report personalizes and dramatizes the risk information, creating a “teachable moment” that can motivate individuals to take appropriate action. Further, they add, it can highlight risk factors of which the participants may have been unaware, allowing them to see just what their risk reduction opportunities are and to develop priorities for addressing them.
There is general agreement that HRA has limited value when used as a stand-alone exercise (i.e., in the absence of other modalities) and that its utility is fully realized only when it is part of an integrated health promotion program. That program should offer not only individualized explanations and counseling but also access to intervention programs that address the risk factors that were identified (these interventions may be provided in-house or in the community). Thus, the commitment to offer HRA must be broadened (and perhaps may become more costly) by offering or making available such activities as smoking cessation courses, fitness activities and nutrition counseling. Such a broad commitment should be made explicitly in the statement of objectives for the program and the budget allocation requested to support it.
In planning an HRA program, one must decide whether to offer it to the entire workforce or only to certain segments (e.g., to salaried or hourly workers, to both, or to workers of specified ages, lengths of service or in specified locations or job categories); and whether to extend the program to include spouses and other dependants (who, as a rule, account for more than half of the utilization of health benefits). A critical factor is the need to secure the availability of at least one person in the organization sufficiently knowledgeable and appropriately positioned to supervise the design and implementation of the program and the performance of both the vendor and the in-house staff involved.
In some organizations in which full-scale annual medical examinations are being eliminated or offered less frequently, HRA has been offered as a replacement either alone or in combination with selected health screening tests. This strategy has merit in terms of enhancing the cost/benefit ratio of a health promotion program, but sometimes it is based not so much on the intrinsic value of the HRA but on the desire to avoid the ill-will that might be generated by what could be perceived as elimination of an established employee benefit.
Conclusion
Despite its limitations and the paucity of scientific research that confirms the claims for its validity and utility, the use of HRA continues to grow in the United States and, much less rapidly, elsewhere. DeFriese and Fielding, whose studies have made them authorities on HRA, see a bright future for it based on their prediction of new sources of risk-relevant information and new technological developments such as improvements in computer hardware and software that will permit direct computer entry of questionnaire responses, allow modeling of the effects of changes in health behavior, and produce more effective full-color reports and graphics (DeFriese and Fielding 1990).
HRA should be used as an element in a well-conceived, continuing program of wellness or health promotion. It conveys an implicit commitment to provide activities and changes in the workplace culture that offer opportunities to help control the risk factors it will identify. Management should be aware of such a commitment and be willing to make the requisite budget allocations.
While much research remains to be done, many organizations will find HRA a useful adjunct to their efforts to improve the health of their employees. The implicit scientific authority of the information it provides, the use of computer technology, and the personalized impact of the results in terms of chronological versus risk age seem to enhance its power to motivate participants to adopt healthy, risk-reducing behaviors. Evidence is accumulating to show that employees and dependants who maintain healthy risk profiles have less absenteeism, demonstrate enhanced productivity, and use less medical care, all of which have a positive effect on the organization’s “bottom line”.
Worksite Health Promotion in Japan
Health promotion in the workplace in Japan was substantially improved when the Occupational Health and Safety Law was amended in 1988 and employers were mandated to introduce health promotion programs (HPPs) in the workplace. Although the law as amended makes no provision for penalties, the Ministry of Labor at this time began actively encouraging employers to establish health promotion programs. For instance, the Ministry has provided support for training and education to increase the numbers of specialists qualified to work in such programs; among the specialists are occupational health promotion physicians (OHPPs), health care trainers (HCTs), health care leaders (HCLs), mental health counselors (MHCs), nutrition counselors (NCs) and occupational health counselors (OHCs). While employers are encouraged to establish health promotion organizations within their own enterprises, they can also elect to procure service from outside, especially if the business is small and it cannot afford to provide a program in-house. The Ministry of Labor furnishes guidelines for the operation of such service institutions. The newly conceived and mandated occupational health promotion program authorized by the Japanese government is called the “total health promotion” (THP) plan.
Recommended Standard Health Promotion Program
If an enterprise is sufficiently large to provide all the specialists listed above, it is strongly recommended that the company organize a committee comprising those specialists and make it responsible for the planning and execution of a health promotion program. Such a committee must first analyze the health status of the workers and determine the highest priorities that are to guide the actual planning of an appropriate health promotion program. The program should be a comprehensive one, based on both group and individual approaches.
On a group basis various health education classes would be offered, for example, on nutrition, life style, stress management and recreation. Cooperative group activities are recommended in addition to lectures in order to encourage workers to become involved in actual procedures so that information provided in class can result in behavioral changes.
As the first step to the individual approach, a health survey should be conducted by the OHPP. The OHPP then issues a plan to the individual based on the results of the survey after taking into account information obtained through counseling by the OHC or MHC (or both). Following this plan, relevant specialists will supply the necessary instructions or counseling. The HCT will design a personal physical training program based on the plan. The HCL will provide practical instruction to the individual in the gym. When necessary, an NC will teach personal nutrition and the MHC or OHC will meet the individual for specific counseling. The results of such individual programs should be evaluated periodically by the OHPP so the program can be improved over time.
Training of Specialists
The Ministry has appointed the Japan Industrial Safety and Health Association (JISHA), a semi-official organization for the promotion of voluntary safety and health activities in the private sector, to be the official body for conducting the training courses for health promotion specialists. To become one of the above six specialists a certain background is required and a course for each specialty must be completed. The OHPP, for instance, must have the national license for physicians and have completed a 22-hour course on conducting the health survey that will direct the planning of the HPP. The course for the HCT is 139 hours, the longest of the six courses; a prerequisite for taking the course is a bachelor’s degree in health sciences or athletics. Those who have three or more years’ practical experience as an HCL are also eligible to take the course. The HCL is the leader responsible for actually teaching workers according to the prescriptions drawn up by the HCT. The requirement for becoming an HCL is that he or she be 18 years of age or older and have completed the course, which covers 28.5 hours. To take the course for the MHC, one of the following degrees or experience is required: a bachelor’s degree in psychology; social welfare or health science; certification as a public health or registered nurse; HCT; completion of JISHA’s Health Listener’s Course; qualification as a health supervisor; or five or more years’ experience as a counselor. The length of the MHC course is 16.5 hours. Only qualified nutritionists can take the NC course, which is 16.0 hours long. Qualified public health nurses and nurses with three or more years of practical experience in counseling can take the OHC course, which is 20.5 hours long. The OHC is expected to be a comprehensive promoter of the health promotion program in the workplace. As of the end of December 1996, the following numbers of the specialists were registered with the JISHA as having completed the assigned courses: OHPP—2,895; HCT—2,800; HCL— 11,364; MHC—8,307; NC—3,888; OHC—5,233.
Service Institutions
Two kinds of health promotion service institutions are approved by JISHA and a list of the registered institutions is available to the public. One kind is authorized to conduct health surveys so that the OHPP can issue a plan to the individual. This type of institution can provide comprehensive health promotion service. The other kind of service institution is only permitted to provide physical training service in accordance with a program developed by an HCT. As of the end of March 1997 the number qualifying as the former type was 72 and that as the latter was 295.
Financial Support from the Ministry
The Ministry of Labor has a budget to support the training courses offered by JISHA, the establishment of new programs by enterprises and the acquisition by service institutions of equipment for physical exercise. When an enterprise establishes a new program, the expenditure will be supported by the Ministry through JISHA for a maximum of three years. The amount depends on size; if the number of employees of an enterprise is less than 300, two-thirds of the total expenditure will be met by the Ministry; for businesses of over 300 employees, financial support covers one-third of the total.
Conclusion
It is too early in the history of the THP project to make a reliable evaluation of its effectiveness, but a consensus prevails that THP should be part of any comprehensive occupational health program. The general status of Japanese occupational health service is still undergoing improvement. In advanced workplaces, that is, chiefly those of the large companies, THP has already developed to a level that an evaluation of the degree of health promotion among the workers and of the extent of improvement in productivity can be done. However, in smaller enterprises, even though the major part of the necessary expenditures for THP can be paid for by the government, the health care systems that are already in place very frequently are not able to undertake the introduction of additional health maintenance activities.
Role of the Employee Health Service in Prevention Programmes: A Case Study
First Chicago Corporation is the holding company for the First National Bank of Chicago, the eleventh largest bank in the United States. The corporation has 18,000 employees, 62% of whom are women. The average age is 36.6 years. Most of its employees are based in the states of Illinois, New York, New Jersey and Delaware. There are approximately 100 individual worksites ranging in size from 10 to over 4,000 employees. The six largest, each with over 500 employees (comprising in aggregate 80% of the workforce), have employee health units managed by the head office Medical Department in collaboration with the local manager for human resources. The small worksites are served by visiting occupational health nurses and participate in programs via printed materials, videotapes, and telephone communication and, for special programs, by contract with providers based in the local community.
In 1982, the company’s Medical and Benefits Administration Departments established a comprehensive Wellness Program that is managed by the Medical Department. Its goals included improving the overall health of employees and their families in order to reduce unnecessary health and disability costs as much as possible.
Need for Health Care Data
For First Chicago to gain any degree of control over the escalation of its health care costs, the company’s Medical and Benefits Departments agreed that a detailed understanding of the sources of expense was required. By 1987, its frustration with the inadequate quality and quantity of the health care data that were available led it to strategically design, implement and evaluate its health promotion programs. Two information system consultants were hired to help construct an in-house database which eventually became known as the Occupational Medicine and Nursing Information (OMNI) System (Burton and Hoy 1991). To maintain its confidentiality, the system resides in the Medical Department.
OMNI databases include claims for inpatient and outpatient health services and for disability and worker’s compensation benefits, services provided by the Bank’s employee assistance program (EAP), absenteeism records, wellness program participation, health risk appraisals (HRAs), prescription medications, and findings of laboratory tests and physical examinations. The data are analyzed periodically to evaluate the impact of the Wellness Program and to indicate any changes that may be advisable.
First Chicago’s Wellness Program
The Wellness Program comprises a broad range of activities that include the following:
- Health education. Pamphlets and brochures on a wide range of topics are made available to employees. A Wellness Newsletter sent to all employees is supplemented by articles which appear in the Bank’s publications and on cafeteria table cards. Videotapes on health topics may be viewed at the workplace and many are available for home viewing. Lunchtime workshops, seminars, and lectures on topics such as mental wellness, nutrition, violence, women’s health and cardiovascular disease are offered weekly at all major worksites.
- Individual counselling. Registered nurses are available in person to answer questions and provide individual counselling at the employee health units and by telephone to employees at the smaller worksites.
- Health risk assessment. A computerized health risk appraisal (HRA), including blood pressure and cholesterol testing, is offered to most new employees and periodically to current employees where there is an employee health unit. It is also offered periodically to employees of some satellite bank facilities.
- Periodic physical examinations. These are offered on a voluntary basis to management employees. Annual health examinations, including Pap smears and breast examinations, are available to female employees in Illinois. Mass screenings for hypertension, diabetes, breast cancer and cholesterol levels are conducted at worksites that have employee health units.
- Pre-retirement. Pre-retirement physical examinations are offered to all employees, starting at age 55 and continuing every three years thereafter until retirement. A comprehensive pre-retirement workshop is offered that includes sessions on healthy ageing.
- Health promotion programmes. Discounted fees are negotiated with community providers for employees participating in physical fitness programmes. Worksite programmes on prenatal education, smoking cessation, stress management, weight reduction, childhood wellness, cardiovascular risk factor reduction, and training for skin cancer and breast self-examination are provided at no cost.
- Cardiopulmonary resuscitation (CPR) and first aid training. CPR training is provided to all security personnel and designated employees. Infant CPR and first aid classes are also offered.
- Immunization programmes. Hepatitis B vaccination is offered to all health service workers who may become exposed to blood or body fluids. Foreign travellers are provided with immunizations, including routine tetanus-diphtheria boosters, as dictated by the risk of infection in the areas they will visit. Education is provided to employees on the value of flu shots. Employees are referred to their primary care physician or the local health department for this immunization.
Women’s Health Program
In 1982, The First National Bank of Chicago found that over 25% of health care costs for employees and their families were related to women’s health. In addition, over 40% of all employee short-term disability absences (i.e., lasting up to six months) were due to pregnancy. To control these costs by helping to ensure low-cost, high-quality health care, a comprehensive program was developed to focus on prevention and early detection and control of women’s health problems (Burton, Erikson, and Briones 1991). The program now includes these services:
- Worksite obstetrical and gynaecologic programme. Since 1985, the Bank has employed a part-time consulting gynaecologist from a major university teaching hospital at its home office in Chicago. Periodically, this service has been offered at two other locations and plans are in progress to establish the programme at another health service location. Voluntary annual health examinations are offered at the home office Medical Department to all female employees enrolled in the Bank’s self-insured benefit plan (employees electing enrolment in a health maintenance organization (HMO) may have these examinations carried out by their HMO doctors). The examination includes a medical history, gynaecological and general physical examinations, laboratory tests such as a Pap smear for cervical cancer, and other testing as may be indicated. In addition to providing examinations and consultations, the gynaecologist also conducts seminars on women’s health concerns. The worksite gynaecological programme has proven to be a convenient and cost-effective way to encourage preventive health care for women.
- Preconception and prenatal education. The United States ranks twenty-fourth among developed nations in infant mortality. At First Chicago, pregnancy-related claims accounted for about 19% of all health care costs in 1992 paid by the medical plan for employees and dependants. In 1987, to address this challenge, the Bank, in cooperation with the March of Dimes, began to offer a series of worksite classes led by a specially trained occupational health nurse. These are held during working hours and emphasize prenatal care, healthy lifestyles, proper nutrition, and indications for Caesarean section. On entering the programme, employees complete a pregnancy-related health risk appraisal questionnaire which is analysed by computer; both the women and their obstetricians receive a report highlighting potential risk factors for complications of pregnancy, such as adverse lifestyles, genetic diseases and medical problems. To encourage participation, female employees or spouses who complete the classes by the sixteenth week of pregnancy are eligible to have the 400 US$ deductible fee for the newborn’s health costs waived. Preliminary results of the prenatal education programme for employees in the Chicago, Illinois, area include the following:
- The Caesarean section rate is 19% for employees who participated in the worksite prenatal education programme compared to 28% for nonparticipants. The regional average Caesarean section rate is about 24%.
- The average cost of delivery in the Chicago, Illinois, area for employees who participated in the prenatal education classes was $7,793 compared to $9,986 for employees who did not participate.
- Absences from work for pregnancy (short-term disability) tend to be slightly reduced for employees who participate in the prenatal education classes.
- Breast feeding (lactation) programme. The Medical Department offers a private room and refrigerator to store breast milk to employees who wish to breast feed. Most employee health units have electric breast pumps and provide lactation supplies to employees in the Bank’s medical plan at no cost (and at cost to employees who are enrolled in HMOs).
- Mammography. Since 1991, mammography screening for breast cancer has been offered at no cost at employee health units in the United States. Mobile mammography units from fully accredited local providers are brought to all the six sites with employee health units from one to several times per year depending on need. Approximately 90% of eligible employees are within a 30 minute automobile drive of a screening mammography location. Female employees and wives of employees and of retirees are eligible to participate in the programme.
Employee Assistance Program and Mental Health Care
In 1979, the Bank implemented an employee assistance program (EAP) that provides consultation, counseling, referral, and follow-up for a wide range of personal problems such as emotional disorders, interpersonal conflict, alcohol and other drug dependencies and addictive disorders in general. Employees may refer themselves for these services or they may be referred by a supervisor who discerns any difficulties that they may be experiencing in performance or interpersonal relationships in the workplace. The EAP also provides workshops on a variety of topics such as stress management, violence and effective parenting. The EAP, which is a unit of the Medical Department, is now staffed by six full and part-time clinical psychologists. The psychologists are located at each of the six medical departments and in addition travel to satellite bank facilities where there is a need.
In addition, the EAP manages psychiatric short-term disability cases (up to six months of continuous absence). The goal of EAP management is to ensure that employees receiving disability payments for psychiatric reasons are receiving appropriate care.
In 1984, a comprehensive program was initiated to provide quality and cost-effective mental health care services for employees and dependants (Burton et al. 1989; Burton and Conti 1991). This program includes four components:
- the EAP for prevention and early intervention
- a review of the patient’s possible need for inpatient psychiatric hospitalization
- case management of mental health-related short-term disability by the EAP staff
- a network of selected mental health professionals who provide outpatient (i.e., ambulatory) services.
Despite enhancement of mental health insurance benefits to include 85% (instead of 50%) reimbursement for alternatives to inpatient hospitalization (e.g., partial hospitalization programs and intensive outpatient programs), First Chicago’s mental health care costs have dropped from nearly 15% of total medical costs in 1983 to under 9% in 1992.
Conclusion
More than a decade ago, First Chicago initiated a comprehensive wellness program with a motto—“First Chicago is Banking on Your Health”. The Wellness Program is a joint effort of the Bank’s Medical and Benefits Departments. It is regarded as having improved the health and productivity of employees and reduced avoidable health care costs for both the employees and the Bank. In 1993, First Chicago’s Wellness Program was awarded the C. Everett Koop National Health Award named in honor of the former Surgeon General of the United States.
Health Improvement Programmes at Maclaren Industries, Inc.: A Case Study
Introduction
The organization
James Maclaren Industries Inc., the industrial setting used for this case study, is a pulp and paper company located in the western part of the Province of Quebec, Canada. A subsidiary of Noranda Forest, Inc., it has three major divisions: a hardwood pulp mill, a groundwood newsprint mill and hydroelectric energy facilities. The pulp and paper industry is the predominant local industry and the company under study is over 100 years old. The work population, approximately 1,000 employees, is locally based and, frequently, several generations of the same family have worked for this employer. The working language is French but most employees are functionally bilingual, speaking French and English. There is a long history (over 40 years) of company-based occupational health services. While the services were initially of an older “traditional” nature, there has been an increasing trend towards the preventive approach during recent years. This is consistent with a “continual improvement” philosophy being adopted throughout the Maclaren organization.
Provision of occupational health services
The occupational health physician has corporate and site responsibilities and reports directly to the directors of health, safety and continuous improvement. The last position reports directly to the company president. Full-time occupational health nurses are employed at the two major sites (the pulp mill has 390 employees and the newsprint mill has 520 employees) and report directly to the physician on all health-related issues. The nurse working at the newsprint division is also responsible for the energy/forest division (60 employees) and the head office (50 employees). A full-time corporate hygienist and safety personnel at all three facilities round out the health, and health-related, professional team.
The Preventive Approach
Prevention of disease and injury is driven by the occupational health and industrial hygiene and safety team with input from all interested parties. Methods used frequently do not differentiate between work-related and non-work-related prevention. Prevention is considered to reflect an attitude or quality of an employee—an attitude that does not cease or start at the plant fence line. A further attribute of this philosophy is the belief that prevention is amenable to continual improvement, a belief furthered by the company’s approach to auditing its various programs.
Continual improvement of prevention programs
Health, industrial hygiene, environment, emergency preparedness, and safety audit programs are an integral part of the continuous improvement approach. The audit findings, although addressing legal and policy compliance concerns, also stress “best management practice” in those areas which are felt to be amenable to improvement. In this way, prevention programs are being repeatedly assessed and ideas presented which are used to further the preventive aims of occupational health and related programs.
Health assessments
Pre-placement health assessments are carried out for all new employees. These are designed to reflect the exposure hazards (chemical, physical, or biological) present in the workplace. Recommendations indicating fitness to work and specific job restrictions are made based on the pre-placement health assessment findings. These recommendations are designed to decrease the risk of employee injury and illness. Health teaching is part of the health assessment and is intended to better acquaint the employees with the potential human impact of workplace hazards. Measures to decrease risk, particularly those related to personal health, are also stressed.
Ongoing health assessment programs are based on hazard exposure and workplace risks. The hearing conservation program is a prime example of a program designed to prevent a health impact. Emphasis is on noise reduction at the source and employees participate in the evaluation of noise reduction priorities. An audiometric assessment is done every five years. This assessment provides an excellent opportunity to counsel employees on the signs and symptoms of noise-induced hearing loss and preventive measures while assisting in the evaluation of the efficacy of the control program. Employees are advised to follow the same advice off the job—that is, to use hearing protection and to diminish their exposure.
Risk-specific health assessments are also carried out for workers involved in special job assignments such as fire fighting, rescue work, water treatment plant operations, tasks requiring excessive heat exposure, crane operation and driving. Similarly, employees who use respirators are required to undergo an assessment to determine their medical fitness to use the respirator. Exposure risks incurred by contractors’ employees are also assessed.
Health hazard communication
There is a statutory requirement to communicate health hazard and health risk information to all employees. This is an extensive task and includes teaching employees about the health effects of designated substances to which they may be exposed. Examples of such substances include a variety of respiratory hazards which may be either byproducts of other materials’ reactions or may represent a direct exposure hazard: one might name in this connection such materials as sulphur dioxide; hydrogen sulphide; chlorine; chlorine dioxide; carbon monoxide; nitrogen oxides and welding fumes. Material Safety Data Sheets (MSDSs) are the prime source of information on this subject. Unfortunately, the suppliers’ MSDSs often lack the necessary quality of health and toxicity information and may not be available in both official languages. This deficiency is being addressed at one of the company’s sites (and will be extended to the other sites) through the development of one-page health information sheets based on an extensive and well-respected database (using a commercially available MSDS generation software system). This project was undertaken with company support by members of the joint labor-management health and safety committee, a process which not only solved a communication problem, but encouraged participation by all workplace parties.
Cholesterol screening programs
The company has made a voluntary cholesterol screening program available to employees at all sites. It offers advice on the health ramifications of high cholesterol levels, medical follow-up when indicated (done by family physicians), and nutrition. Where onsite cafeteria services exist, nutritious food alternatives are offered to the employees. The health staff also makes pamphlets on nutrition available for employees and their families to assist them to understand and diminish personal health risk factors.
Blood pressure screening programs
Both in conjunction with annual community programs (“Heart Month”) on heart health, and on a regular basis, the company encourages employees to have their blood pressure checked and, when necessary, monitored. Counseling is provided to employees to assist them, and indirectly their families, to understand the health concerns surrounding hypertension and to seek help through their community medical resources if further follow-up or treatment is needed.
Employee and family assistance programs
Problems that have an impact on employee performance are frequently the result of difficulties outside the workplace. In many cases, these reflect difficulties related to the employee’s social sphere, either home or community. Internal and external referral systems exist. The company has had a confidential employee (and, more recently, family) assistance program in place for over five years. The program assists about 5% of the employee population annually. It is well publicized and early use of the program is encouraged. Feedback received from the employees indicates that the program has been a significant factor in minimizing or preventing deterioration of work performance. The primary reasons for using the assistance program reflect family and social issues (90%); alcohol and drug problems account for only a small percentage of the total cases assisted (10%).
As part of the employee assistance program, the facility has instituted a serious-incident debriefing process. Serious incidents, such as fatalities or major accidents, can have an extremely unsettling effect on employees. There is also the potential for significant long-term consequences, not only to the efficient functioning of the company but, more particularly, to the individuals involved in the incident.
Wellness programs
A recent development has been the decision to take the first steps towards the development of a “wellness” program that targets disease prevention in an integrated approach. This program has several components: cardiorespiratory fitness; physical conditioning; nutrition; smoking cessation; stress management; back care; cancer prevention and substance abuse. Several of these topics have been mentioned previously in this case study. Others (not discussed in this article) will, however, be implemented in a stepwise fashion.
Special communication programs
- HIV/AIDS. The advent of HIV/AIDS in the general population signalled a need to communicate information to the workplace community for two reasons: to allay fear of contagion should a case become known from among the employee population and to ensure that employees are cognizant of preventive measures and the “real” facts about communicability. A communication programme was organized to meet these two objectives and made available to the employees on a voluntary basis. Pamphlets and literature could also be obtained from the health centers.
- Communication of research study results. The following are examples of two recent communications about health research studies in areas that were considered to be of special concern to employees.
- Electromagnetic field studies. The results of the electromagnetic field study undertaken by Electricitй (E.D.F.), Hydro Quebec, and Ontario Hydro (Thйriault 1994), were communicated to all exposed and potentially exposed employees. The objectives behind the communication were to prevent unwarranted fear and to ensure that employees had firsthand knowledge of issues affecting their workplace and, potentially, their health.
- Health outcome studies. Several studies in the pulp and paper industry relate to health outcomes from working in this industry. The outcomes being investigated include cancer incidence and cancer mortality. Communications to employees are planned to ensure their awareness of the existence of the studies, and, when available, to share the results. The objectives are to alleviate fear and ensure that employees have the opportunity to know the results of studies pertinent to their occupations.
- Community interest topics. As part of its preventive approach, the company has reached out to community physicians and invited them to tour the workplace and meet with the occupational health and hygiene staff. Presentations related to issues relevant to health and the pulp and paper industry have been made at the same time. This has assisted the local physicians to understand the working conditions, including potential hazardous exposures, as well as the job requirements of the employees. As a result, the company and the physicians have worked in concert to diminish the potential ill effects of injury and illness. Community meetings have also been held to provide the communities with information on environmental issues related to the company’s operations and to give the local citizens an opportunity to ask questions on matters of concern (including health issues). Prevention is thus carried to the community level.
- Future trends in prevention. Behaviour modification techniques are being considered to further improve the overall level of worker health and to diminish injuries and illness. Not only will these modifications have a positive effect on the health of the worker in the workplace, they will also carry over to the home environment.
Employee involvement in safety and health decision making already exists through the Joint Health and Safety Committees. Opportunities to extend the partnership to employees in other areas are being actively pursued.
Conclusions
The essential elements of the program at Maclaren are:
- a firm management commitment to health promotion and health protection
- integration of occupational health programs with those aimed at non-occupational health problems
- involvement of all workplace parties in program planning, implementation and evaluation
- coordination with community-based health care facilities and providers and agencies
- an incremental approach to program expansion
- audits of program effectiveness to identify problems that need addressing and areas where programs may be strengthened, combined with action plans to ensure appropriate follow-up activities
- effective integration of all environmental, health, hygiene and safety activities.
This case study has focused on existing programs designed to improve employee health and prevent unnecessary and unwanted health effects. The opportunities to further enhance this approach are boundless and particularly amenable to the company’s continual improvement philosophy.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."