Children categories

94. Education and Training Services (7)

94. Education and Training Services
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Diseases affecting day-care workers & teachers
2. Hazards & precautions for particular classes
3. Summary of hazards in colleges & universities
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

95. Emergency and Security Services (9)

95. Emergency and Security Services
Chapter Editor: Tee L. Guidotti
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Recommendations & criteria for compensation
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

96. Entertainment and the Arts (31)

96. Entertainment and the Arts
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Arts and Crafts
Performing and Media Arts
Entertainment
Tables
Click a link below to view table in article context.
1. Precautions associated with hazards
2. Hazards of art techniques
3. Hazards of common stones
4. Main risks associated with sculpture material
5. Description of fibre & textile crafts
6. Description of fibre & textile processes
7. Ingredients of ceramic bodies & glazes
8. Hazards & precautions of collection management
9. Hazards of collection objects
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

97. Health Care Facilities and Services (25)

97. Health Care Facilities and Services
Chapter Editor: Annelee Yassi
Table of Contents
Tables and Figures
Health Care: Its Nature and Its Occupational Health Problems
Annalee Yassi and Leon J. Warshaw
Social Services
Susan Nobel
Home Care Workers: The New York City Experience
Lenora Colbert
Occupational Health and Safety Practice: The Russian Experience
Valery P. Kaptsov and Lyudmila P. Korotich
Ergonomics and Health Care
Hospital Ergonomics: A Review
Madeleine R. Estryn-Béhar
Strain in Health Care Work
Madeleine R. Estryn-Béhar
Case Study: Human Error and Critical Tasks: Approaches for Improved System Performance
Work Schedules and Night Work in Health Care
Madeleine R. Estryn-Béhar
The Physical Environment and Health Care
Exposure to Physical Agents
Robert M. Lewy
Ergonomics of the Physical Work Environment
Madeleine R. Estryn-Béhar
Prevention and Management of Back Pain in Nurses
Ulrich Stössel
Case Study: Treatment of Back Pain
Leon J. Warshaw
Health Care Workers and Infectious Disease
Overview of Infectious Diseases
Friedrich Hofmann
Prevention of Occupational Transmission of Bloodborne Pathogens
Linda S. Martin, Robert J. Mullan and David M. Bell
Tuberculosis Prevention, Control and Surveillance
Robert J. Mullan
Chemicals in the Health Care Environment
Overview of Chemical Hazards in Health Care
Jeanne Mager Stellman
Managing Chemical Hazards in Hospitals
Annalee Yassi
Waste Anaesthetic Gases
Xavier Guardino Solá
Health Care Workers and Latex Allergy
Leon J. Warshaw
The Hospital Environment
Buildings for Health Care Facilities
Cesare Catananti, Gianfranco Damiani and Giovanni Capelli
Hospitals: Environmental and Public Health Issues
M.P. Arias
Hospital Waste Management
M.P. Arias
Managing Hazardous Waste Disposal Under ISO 14000
Jerry Spiegel and John Reimer
Tables
Click a link below to view table in article context.
1. Examples of health care functions
2. 1995 integrated sound levels
3. Ergonomic noise reduction options
4. Total number of injuries (one hospital)
5. Distribution of nurses’ time
6. Number of separate nursing tasks
7. Distribution of nurses' time
8. Cognitive & affective strain & burn-out
9. Prevalence of work complaints by shift
10. Congenital abnormalities following rubella
11. Indications for vaccinations
12. Post-exposure prophylaxis
13. US Public Health Service recommendations
14. Chemicals’ categories used in health care
15. Chemicals cited HSDB
16. Properties of inhaled anaesthetics
17. Choice of materials: criteria & variables
18. Ventilation requirements
19. Infectious diseases & Group III wastes
20. HSC EMS documentation hierarchy
21. Role & responsibilities
22. Process inputs
23. List of activities
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

98. Hotels and Restaurants (4)

98. Hotels and Restaurants
Chapter Editor: Pam Tau Lee
Table of Contents

99. Office and Retail Trades (7)
99. Office and Retail Trades
Chapter Editor: Jonathan Rosen
Table of Contents
Tables and Figures
The Nature of Office and Clerical Work
Charles Levenstein, Beth Rosenberg and Ninica Howard
Professionals and Managers
Nona McQuay
Offices: A Hazard Summary
Wendy Hord
Bank Teller Safety: The Situation in Germany
Manfred Fischer
Telework
Jamie Tessler
The Retail Industry
Adrienne Markowitz
Case Study: Outdoor Markets
John G. Rodwan, Jr.
Tables
Click a link below to view table in article context.
1. Standard professional jobs
2. Standard clerical jobs
3. Indoor air pollutants in office buildings
4. Labour statistics in the retail industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

100. Personal and Community Services (6)
100. Personal and Community Services
Chapter Editor: Angela Babin
Table of Contents
Tables and Figures
Indoor Cleaning Services
Karen Messing
Barbering and Cosmetology
Laura Stock and James Cone
Laundries, Garment and Dry Cleaning
Gary S. Earnest, Lynda M. Ewers and Avima M. Ruder
Funeral Services
Mary O. Brophy and Jonathan T. Haney
Domestic Workers
Angela Babin
Case Study: Environmental Issues
Michael McCann
Click a link below to view table in article context.
1. Postures observed during dusting in a hospital
2. Dangerous chemicals used in cleaning
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

101. Public and Government Services (12)

101. Public and Government Services
Chapter Editor: David LeGrande
Table of Contents
Tables and Figurs
Occupational Health and Safety Hazards in Public and Governmental Services
David LeGrande
Case Report: Violence and Urban Park Rangers in Ireland
Daniel Murphy
Inspection Services
Jonathan Rosen
Postal Services
Roxanne Cabral
Telecommunications
David LeGrande
Hazards in Sewage (Waste) Treatment Plants
Mary O. Brophy
Domestic Waste Collection
Madeleine Bourdouxhe
Street Cleaning
J.C. Gunther, Jr.
Sewage Treatment
M. Agamennone
Municipal Recycling Industry
David E. Malter
Waste Disposal Operations
James W. Platner
The Generation and Transport of Hazardous Wastes: Social and Ethical Issues
Colin L. Soskolne
Tables
Click a link below to view table in article context.
1. Hazards of inspection services
2. Hazardous objects found in domestic waste
3. Accidents in domestic waste collection (Canada)
4. Injuries in the recycling industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

102. Transport Industry and Warehousing (18)

102. Transport Industry and Warehousing
Chapter Editor: LaMont Byrd
Table of Contents
Tables and Figures
General Profile
LaMont Byrd
Case Study: Challenges to Workers’ Health and Safety in the Transportation and Warehousing Industry
Leon J. Warshaw
Air Transport
Airport and Flight Control Operations
Christine Proctor, Edward A. Olmsted and E. Evrard
Case Studies of Air Traffic Controllers in the United States and Italy
Paul A. Landsbergis
Aircraft Maintenance Operations
Buck Cameron
Aircraft Flight Operations
Nancy Garcia and H. Gartmann
Aerospace Medicine: Effects of Gravity, Acceleration and Microgravity in the Aerospace Environment
Relford Patterson and Russell B. Rayman
Helicopters
David L. Huntzinger
Road Transport
Truck and Bus Driving
Bruce A. Millies
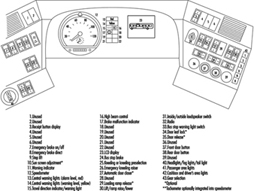
Ergonomics of Bus Driving
Alfons Grösbrink and Andreas Mahr
Motor Vehicle Fuelling and Servicing Operations
Richard S. Kraus
Case Study: Violence in Gasoline Stations
Leon J. Warshaw
Rail Transport
Rail Operations
Neil McManus
Case Study: Subways
George J. McDonald
Water Transport
Water Transportation and the Maritime Industries
Timothy J. Ungs and Michael Adess
Storage
Storage and Transportation of Crude Oil, Natural Gas, Liquid Petroleum Products and Other Chemicals
Richard S. Kraus
Warehousing
John Lund
Case Study: US NIOSH Studies of Injuries among Grocery Order Selectors
Tables
Click a link below to view table in article context.
1. Bus driver seat measurements
2. Illumination levels for service stations
3. Hazardous conditions & administration
4. Hazardous conditions & maintenance
5. Hazardous conditions & right of way
6. Hazard control in the Railway industry
7. Merchant vessel types
8. Health hazards common across vessel types
9. Notable hazards for specific vessel types
10. Vessel hazard control & risk-reduction
11. Typical approximate combustion properties
12. Comparison of compressed & liquified gas
13. Hazards involving order selectors
14. Job safety analysis: Fork-lift operator
15. Job safety analysis: Order selector
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Dancers
Dance involves patterned and rhythmic body movements, usually performed to music, that serve as a form of expression or communication. There are many different types of dances, including ceremonial, folk, ballroom, classical ballet, modern dance, jazz, flamenco, tap and so forth. Each of these has its unique movements and physical demands. Audiences associate dance with grace and enjoyment, yet very few people regard dance as one of the most demanding and strenuous athletic activities. Sixty-five to 80% of dance-related injuries are in the lower limbs, out of which about 50% are in the foot and ankle (Arheim 1986). Most of the injuries are due to over-use (about 70%) and the rest are of the acute type (ankle sprain, fractures and so on).
Dance medicine is a multidisciplinary profession because causes of injuries are multifactorial and hence treatment should be comprehensive and take into consideration the specific needs of dancers as artists. The goal of the treatment should be to prevent potentially dangerous specific stresses, allowing the dancer to keep active, acquiring and perfecting physical creativity and psychological well-being.
Training should preferably start at an early age in order to develop strength and flexibility. However, incorrect training results in injury to young dancers. Proper technique is the main concern, as incorrect posture and other bad dancing habits and methods will cause permanent deformities and over-use injuries (Hardaker 1987). One of the most basic movements is the turn-out—opening of the lower limbs outwards. This should take place in the hip joints; if it is forced more than the anatomic external rotation these joints will allow, compensations occur. The most common compensations are rolling-in of the feet, internal flexing of the knees and hyperlordosis of the lower back. These positions contribute to deformities such as hallux valgus (displacement of the great toe towards the other toes). Inflammations of tendons such as the flexor hallucis longus (the tendon for the great toe) and others may also result (Hamilton 1988; Sammarco 1982).
Being cognizant of individual anatomic differences in addition to the unusual biomechanical loads, such as in point position (standing on the tip of the toes), allows one to take actions to prevent some of these undesired outcomes (Teitz, Harrington and Wiley 1985).
The environment of dancers has great influence on their well-being. A proper floor should be resilient and absorb shock to prevent cumulative trauma to the feet, legs and spine (Seals 1987). Temperature and humidity also influence performance. Diet is a major issue as dancers are always under pressure to keep slim and look light and pleasing (Calabrese, Kirkendal and Floyd 1983). Psychological maladjustment may lead to anorexia or bulimia.
Psychological stress may contribute to some hormonal disturbances, which may present as amenorrhoea. The incidence of stress fractures and osteoporosis may increase in hormonally imbalanced dancers (Warren, Brooks-Gunn and Hamilton 1986). Emotional stress due to competition between peers, and direct pressure from choreographers, teachers and directors may enhance psychological problems (Schnitt and Schnitt 1987).
A good screening method for both students and professional dancers should detect psychological and physical risk factors and avoid problems.
Any change in activity levels (whether return from a holiday, sickness or pregnancy), intensity of work (rehearsals before a premiere tour), choreographer, style or technique, or environment (such as floors, stages or even type of dance shoes) makes the dancer more vulnerable.
Exposure to Physical Agents
Health care workers (HCWs) confront numerous physical hazards.
Electrical Hazards
Failure to meet standards for electrical equipment and its use is the most frequently cited violation in all industries. In hospitals, electrical malfunctions are the second leading cause of fires. Additionally, hospitals require that a wide variety of electrical equipment be used in hazardous environments (i.e., in wet or damp locations or adjacent to flammables or combustibles).
Recognition of these facts and the danger they may pose to patients has led most hospitals to put great effort into electrical safety promotion in patient-care areas. However, non-patient areas are sometimes neglected and employee- or hospital-owned appliances may be found with:
- three-wire (grounded) plugs attached to two-wire (ungrounded) cords
- ground prongs bent or cut off
- ungrounded appliances attached to ungrounded multiple-plug “spiders”
- extension cords with improper grounding
- cords moulded to plugs not properly wired (25% of the x-ray equipment in one hospital study was incorrectly wired).
Prevention and control
It is critical that all electrical installations be in accordance with prescribed safety standards and regulations. Measures that can be taken to prevent fires and avoid shocks to employees include the following:
- provision for regular inspection of all employee work areas by an electrical engineer to discover and correct hazardous conditions such as ungrounded or poorly maintained appliances or tools
- inclusion of electrical safety in both orientation and in-service training programmes.
Employees should be instructed:
- not to use electrical equipment with wet hands, on wet surfaces or when standing on wet floors
- not to use devices that blow a fuse or trip a circuit breaker until they have been inspected
- not to use any appliance, equipment or wall receptacle that appears to be damaged or in poor repair
- to use extension cords only temporarily and only in emergency situations
- to use extension cords designed to carry the voltage required
- to turn off equipment before unplugging it
- to report all shocks immediately (including small tingles) and not to use equipment again until it has been inspected.
Heat
Although heat-related health effects on hospital workers can include heat stroke, exhaustion, cramps and fainting, these are rare. More common are the milder effects of increased fatigue, discomfort and inability to concentrate. These are important because they may increase the risk of accidents.
Heat exposure can be measured with wet bulb and globe thermometers, expressed as the Wet Bulb Globe Temperature (WBGT) Index, which combines the effects of radiant heat and humidity with the dry bulb temperature. This testing should only be done by a skilled individual.
The boiler room, laundry and kitchen are the most common high-temperature environments in the hospital. However, in old buildings with inadequate ventilation and cooling systems heat may be a problem in many locations in summer months. Heat exposure may also be a problem where ambient temperatures are elevated and health care personnel are required to wear occlusive gowns, caps, masks and gloves.
Prevention and control
Although it may be impossible to keep some hospital settings at a comfortable temperature, there are measures to keep temperatures at acceptable levels and to ameliorate the effects of heat upon workers, including:
- provision of adequate ventilation. Central air-conditioning systems may need to be supplemented by floor fans, for example.
- making cool drinking water easily accessible
- rotating employees so that periodic relief is scheduled
- scheduling frequent breaks in cool areas.
Noise
Exposure to high levels of noise in the workplace is a common job hazard. The “quiet” image of hospitals notwithstanding, they can be noisy places to work.
Exposure to loud noises can cause a loss in hearing acuity. Short-term exposure to loud noises can cause a decrease in hearing called a “temporary threshold shift” (TTS). While these TTSs can be reversed with sufficient rest from high noise levels, the nerve damage resulting from long-term exposure to loud noises cannot.
The US Occupational Safety and Health Administration (OSHA) has set 90 dBA as the permissible limit per 8 hours of work. For 8-hour average exposures in excess of 85 dBA, a hearing conservation programme is mandated. (Sound level meters, the basic noise measuring instrument, are provided with three weighting networks. OSHA standards use the A scale, expressed as dBA.)
The effects of noise at the 70-dB level are reported by the National Institute of Environmental Health Sciences to be:
- blood vessel constriction that can lead to higher blood pressure and decreased circulation in the hands and feet (perceived as coldness)
- headaches
- increased irritability
- difficulty in communicating with co-workers
- reduced ability to work
- more difficulty with tasks that require alertness, concentration and attention to detail.
Food service areas, laboratories, engineering areas (which usually includes the boiler room), business office and medical records and nursing units can be so noisy that productivity is reduced. Other departments where noise levels are sometimes quite high are laundries, print shops and construction areas.
Prevention and control
If a noise survey of the facility shows that employees’ noise exposure is in excess of the OSHA standard, a noise abatement programme is required. Such a programme should include:
- periodic measurement
- engineering controls such as isolating noisy equipment, installing mufflers and acoustic ceilings and carpets
- administrative controls limiting workers’ exposure time to excessive noise.
In addition to abatement measures, a hearing conservation programme should be established that provides for:
- hearing tests for new employees to provide baselines for future testing
- annual audiometric testing
- hearing protection for use while controls are being implemented and for situations where levels cannot be brought within approved limits.
Inadequate Ventilation
The specific ventilation requirements for various types of equipment are engineering matters and will not be discussed here. However, both old and new facilities present general ventilation problems that warrant mentioning.
In older facilities built before central heating and cooling systems were common, ventilation problems must often be solved on a location-by-location basis. Frequently, the problem rests in achieving uniform temperatures and correct circulation.
In newer facilities that are hermetically sealed, a phenomenon called “tight-building syndrome” or “sick building syndrome” is sometimes experienced. When the circulation system does not exchange the air rapidly enough, concentrations of irritants may build up to the extent that employees may experience such reactions as sore throat, runny nose and watery eyes. This situation can provoke severe reaction in sensitized individuals. It can be exacerbated by various chemicals emitted from such sources as foam insulation, carpeting, adhesives and cleaning agents.
Prevention and control
While careful attention is paid to ventilation in sensitive areas such as surgical suites, less attention is given to general-purpose areas. It is important to alert employees to report irritant reactions that appear only in the workplace. If local air quality cannot be improved with venting, it may be necessary to transfer individuals who have become sensitized to some irritant in their workstation.
Laser Smoke
During surgical procedures using a laser or electrosurgical unit, the thermal destruction of tissue creates smoke as a by-product. NIOSH has confirmed studies showing that this smoke plume can contain toxic gases and vapours such as benzene, hydrogen cyanide and formaldehyde, bioaerosols, dead and live cellular material (including blood fragments) and viruses. At high concentrations, the smoke causes ocular and upper respiratory tract irritation in health care personnel and may create visual problems for the surgeon. The smoke has an unpleasant odour and has been shown to have mutagenic material.
Prevention and control
Exposure to airborne contaminants in such smoke can be effectively controlled by proper ventilation of the treatment room, supplemented by local exhaust ventilation (LEV) using a high-efficiency suction unit (i.e., a vacuum pump with an inlet nozzle held within 2 inches of the surgical site) that is activated throughout the procedure. Both the room ventilation system and the local exhaust ventilator should be equipped with filters and absorbers that capture particulates and absorb or inactivate airborne gases and vapours. These filters and absorbers require monitoring and replacement on a regular basis and are considered a possible biohazard requiring proper disposal.
Radiation
Ionizing radiation
When ionizing radiation strikes cells in living tissue, it may either kill the cell directly (i.e., cause burns or hair loss) or it may alter the genetic material of the cell (i.e., cause cancer or reproductive damage). Standards involving ionizing radiation may refer to exposure (the amount of radiation the body is exposed to) or dose (the amount of radiation the body absorbs) and may be expressed in terms of millirem (mrem), the usual measure of radiation, or rems (1,000 millirems).
Various jurisdictions have developed regulations governing the procurement, use, transportation and disposal of radioactive materials, as well as established limits for exposure (and in some places specific limits for dosage to various parts of the body), providing a strong measure of protection for radiation workers. In addition, institutions using radioactive materials in treatment and research generally develop their own internal controls in addition to those prescribed by law.
The greatest dangers to hospital workers are from scatter, the small amount of radiation that is deflected or reflected from the beam into the immediate vicinity, and from unexpected exposure, either because they are inadvertently exposed in an area not defined as a radiation area or because the equipment is not well maintained.
Radiation workers in diagnostic radiology (including x ray, fluoroscopy and angiography for diagnostic purposes, dental radiography and computerized axial tomography (CAT) scanners), in therapeutic radiology, in nuclear medicine for diagnostic and therapeutic procedures, and in radiopharmaceutical laboratories are carefully followed and checked for exposure, and radiation safety is usually well managed in their workstations, although there are many localities in which control is inadequate.
There are other areas not usually designated as “radiation areas”, where careful monitoring is needed to ensure that appropriate precautions are being taken by staff and that correct safeguards are provided for patients who might be exposed. These include angiography, emergency rooms, intensive care units, locations where portable x rays are being taken and operating rooms.
Prevention and control
The following protective measures are strongly recommended for ionizing radiation (x rays and radioisotopes):
- Rooms that house radiation sources should be properly marked and entered only by authorized personnel.
- All films should be held in place by patients or members of the patient’s family. If the patient must be held, a member of the family should do so. If staff must hold film or patients, the task should be rotated through the staff to minimize the overall dose per individual.
- Where portable x-ray units and radioisotopes are used, only the patient and trained personnel should be allowed in the room.
- Adequate warning should be given to nearby workers when x rays using portable units are about to be taken.
- X-ray controls should be located to prevent the unintentional energizing of the unit.
- X-ray room doors should be kept closed when equipment is in use.
- All x-ray machines should be checked before each use to ensure that the secondary radiation cones and filters are in place.
- Patients who have received radioactive implants or other therapeutic radiology procedures should be clearly identified. Bedding, dressings, wastes and so forth from such patients should be so labelled.
Lead aprons, gloves and goggles must be worn by employees working in the direct field or where scatter radiation levels are high. All such protective equipment should be checked annually for cracks in the lead.
Dosimeters must be worn by all personnel exposed to ionizing radiation sources. Dosimeter badges should be regularly analysed by a laboratory with good quality control, and the results should be recorded. Records must be kept not only of each employee’s personal radiation exposure but also of the receipt and disposition of all radioisotopes.
In therapeutic radiology settings, periodic dose checks should be done using lithium fluoride (LiF) solid-state dosimeters to check on system calibration. Treatment rooms should be equipped with radiation monitor-door interlock and visual-alarm systems.
During internal or intravenous treatment with radioactive sources, the patient should be housed in a room located to minimize exposure to other patients and staff and signs posted warning others not to enter. Staff contact time should be limited, and staff should be careful in handling bedding, dressings and wastes from these patients.
During fluoroscopy and angiography, the following measures can minimize unnecessary exposure:
- full protective equipment
- minimal number of personnel in the room
- “dead-man” switches (must have active operator control)
- minimal beam size and energy
- careful shielding to reduce scatter.
Full protective equipment should also be used by operating-room personnel during radiation procedures, and, when possible, personnel should stand 2 m or more from the patient.
Non-ionizing radiation
Ultraviolet radiation, lasers and microwaves are non-ionizing radiation sources. They are generally far less hazardous than ionizing radiation but nevertheless require special care to prevent injury.
Ultraviolet radiation is used in germicidal lamps, in certain dermatology treatments and in air filters in some hospitals. It is also produced in welding operations. Exposure of the skin to ultraviolet light causes sunburn, ages the skin and increases the risk of skin cancer. Eye exposure can result in temporary but extremely painful conjunctivitis. Long-term exposure can lead to partial loss of vision.
Standards regarding exposure to ultraviolet radiation are not widely applicable. The best approach to prevention is education and wearing shaded protective eyeglasses.
The Bureau of Radiological Health of the US Food and Drug Administration regulates lasers and classifies them into four classes, I to IV. The laser used to position patients in radiology is considered Class I and represents minimal risk. Surgical lasers, however, can pose a significant hazard to the retina of the eye where the intense beam can cause total loss of vision. Because of the high voltage supply required, all lasers present the risk of electrical shock. The accidental reflection of the laser beam during surgical procedures can result in injury to the staff. Guidelines for laser use have been developed by the American National Standards Institute and the US Army; for example, laser users should wear protective goggles specifically designed for each type of laser and take care not to focus the beam on reflecting surfaces.
The primary concern regarding exposure to microwaves, which are used in hospitals chiefly for cooking and heating food and for diathermy treatments, is the heating effect they have on the body. The eye lens and gonads, having fewer vessels with which to remove heat, are most vulnerable to damage. The long-term effects of low-level exposure have not been established, but there is some evidence that nervous system effects, decreased sperm count, sperm malformations (at least partially reversible after exposure ceases) and cataracts may result.
Prevention and control
The OSHA standard for exposure to microwaves is 10 milliwatts per square centimetre (10 mW/cm). This is the level established to protect against the thermal effects of microwaves. In other countries where levels have been established to protect against reproductive and nervous system damage, the standards are as much as two orders of magnitude lower, that is, 0.01 mW/cm2 at 1.2 m.
To ensure the safety of workers, microwave ovens should be kept clean to protect the integrity of the door seals and should be checked for leakage at least every three months. Leakage from diathermy equipment should be monitored in the vicinity of the therapist before each treatment.
Hospital workers should be aware of the radiation hazards of ultraviolet exposure and of infrared heat used for therapy. They should have appropriate eye protection when using or repairing ultraviolet equipment, such as germicidal lamps and air purifiers or infrared instruments and equipment.
Conclusion
Physical agents represent an important class of hazards to workers in hospitals, clinics and private offices where diagnostic and therapeutic procedures are performed. These agents are discussed in more detail elsewhere in this Encyclopaedia. Their control requires education and training of all health professionals and support staff who may be involved and constant vigilance and systemic monitoring of both the equipment and the way it is used.
Truck and Bus Driving
Transport by road includes the movement of people, livestock and freight of all kinds. Freight and livestock generally move in some form of truck, although buses often carry packages and passenger baggage and may transport fowl and small animals. People generally move by bus on the road, although in many areas trucks of various kinds serve this function.
Truck (lorry) drivers may operate several different types of vehicles, including, for example, semi-trailers, tanker trucks, dump trucks, double and triple trailer combinations, mobile cranes, delivery trucks and panel or pickup vehicles. Legal gross vehicle weights (which vary by jurisdiction) range from 2,000 kg to over 80,000 kg. Truck cargo may include any imaginable item—for example, small and large packages, machinery, rock and sand, steel, lumber, flammable liquids, compressed gases, explosives, radioactive materials, corrosive or reactive chemicals, cryogenic liquids, food products, frozen foods, bulk grain, sheep and cattle.
In addition to driving the vehicle, truck drivers are responsible for inspecting the vehicle prior to use, checking shipping papers, verifying that proper placards and markings are in place and maintaining a log book. Drivers may also be responsible for servicing and repairing the vehicle, loading and unloading cargo (either by hand or using a fork truck, crane or other equipment) and collecting money received for goods delivered. In the event of an accident, the driver is responsible for securing the cargo and summoning assistance. If the incident involves hazardous materials, the driver may attempt, even without proper training or necessary equipment, to control spills, stop leaks or put out a fire.
Bus drivers may carry a few people in a small van or operate medium and large buses carrying 100 or more passengers. They are responsible for boarding and discharging passengers safely, providing information and possibly collecting fares and maintaining order. Bus drivers may also be responsible for servicing and repairing the bus and loading and unloading cargo and baggage.
Motor vehicle accidents are one of the most serious hazards facing both truck and bus drivers. This hazard is aggravated if the vehicle is not properly maintained, especially if the tyres are worn or the brake system is faulty. Driver fatigue caused by a long or irregular schedules, or by other stress, increases the likelihood of accidents. Excessive speed and hauling excessive weight add to the risk, as do heavy traffic and adverse weather conditions which impair traction or visibility. An accident involving hazardous materials may cause additional injury (toxic exposure, burns and so on) to the driver or passengers and may affect a wide area surrounding the accident.
Drivers face a variety of ergonomic hazards. The most obvious are back and other injuries caused by lifting excessive weight or using improper lifting technique. The use of back belts is quite common, although their efficacy has been questioned, and their use may create a false sense of security. The necessity of loading and unloading cargo at locations where fork-lift trucks, cranes or even dollies are not available and the great variety of package weights and configurations add to the risk of lifting injuries.
Driver’s seats are often poorly designed and cannot be adjusted to provide proper support and long-term comfort, resulting in back problems or other musculoskeletal damage. Drivers may experience damage to the shoulder caused by vibration as the arm may rest for long periods in a somewhat raised position on the window opening. Whole-body vibration can cause damage to the kidneys and back. Ergonomic injury may also result from repetitive use of poorly placed vehicle controls or fare box keypads.
Drivers are at risk of industrial hearing loss caused by long-term exposure to loud engine noises. Poor maintenance, faulty mufflers and inadequate cab insulation aggravate this hazard. Hearing loss may be more pronounced in the ear adjacent to the driver’s window.
Drivers, especially long-haul truck drivers, often work excessive hours without adequate rest. The International Labour Organization (ILO) Hours of Work and Rest Periods (Road Transport) Convention, 1979 (No. 153), requires a break after 4 hours of driving, limits total driving time to 9 hours per day and 48 hours per week and requires at least 10 hours of rest in each 24-hour period. Most nations also have laws which govern driving times and rest periods and require drivers to maintain logbooks indicating hours worked and rest periods taken. However, management expectations and economic necessity, as well as certain terms of remuneration, such as pay per load or the lack of pay for an empty return trip, put strong pressure on the driver to operate for excessive hours and to make bogus log entries. Long hours cause psychological stress, aggravate ergonomic problems, contribute to accidents (including accidents caused by falling asleep at the wheel) and may cause the driver to use artificial, addictive stimulants.
In addition to ergonomic conditions, long work hours, noise and economic anxiety, drivers experience psychological and physiological stress and fatigue caused by adverse traffic conditions, poor road surfaces, bad weather, night driving, the fear of assault and robbery, concern about faulty equipment and continuous intense concentration.
Truck drivers are potentially exposed to any chemical, radioactive or biological hazard associated with their load. Leaking containers, faulty valves on tanks and emissions during loading or unloading may cause worker exposures to toxic chemicals. Improper packaging, inadequate shielding or improper placement of radioactive cargo may allow radiation exposure. Workers transporting livestock may be infected with animal-borne infections such as brucellosis. Bus drivers are exposed to infectious diseases of their passengers. Drivers are also exposed to fuel vapours and engine exhaust, especially if there are fuel-line or exhaust system leaks or if the driver makes repairs or handles freight while the engine is running.
In the event of an accident involving hazardous materials, the driver may experience acute chemical or radiation exposures or may be injured by a fire, explosion or chemical reaction. Drivers generally lack the training or equipment to deal with hazardous materials incidents. Their responsibility should be limited to protecting themselves and summoning emergency responders. The driver faces additional risks in attempting emergency response actions for which he or she is not properly trained and adequately equipped.
The driver may be injured in the course of making mechanical repairs to the vehicle. A driver could be struck by another vehicle while working on a truck or bus alongside the road. Wheels with split rims pose a special injury hazard. Improvised or inadequate jacks may cause a crushing injury.
Truck drivers face the risk of assault and robbery, especially if the vehicle carries a valuable cargo or if the driver is responsible for collecting money for goods delivered. Bus drivers are at risk of fare box robberies and abuse or assault by impatient or inebriated passengers.
Many aspects of a driver’s life may contribute to poor health. Because they work long hours and need to eat on the road, drivers often suffer from poor nutrition. Stress and peer pressure may lead to drug and alcohol use. Using the services of prostitutes increases the risk of AIDS and other sexually transmitted diseases. The drivers appear to be one of the main vectors for carrying AIDS in some countries.
The risks described above are all preventable, or at least controllable. As with most safety and health issues, what is needed is a combination of adequate remuneration, worker training, a strong union contract and strict adherence to applicable standards on the part of management. If drivers receive adequate pay for their work, based on proper work schedules, there is less incentive to speed, work excessive hours, drive unsafe vehicles, carry overweight loads, take drugs or make bogus log entries. Management must require drivers to comply with all safety laws, including keeping an honest logbook.
If management invests in well-made vehicles and assures their regular inspection, maintenance and servicing, breakdowns and accidents can be greatly reduced. Ergonomic injury can be reduced if management is willing to pay for the well-designed cabs, fully adjustable driver’s seats and good vehicle control arrangements that are now available. Proper maintenance, especially of exhaust systems, will reduce noise exposure.
Toxic exposures can be reduced if management assures compliance with packaging, labelling, loading and placarding standards for hazardous materials. Measures which reduce vehicular accidents also reduce the risk of a hazardous materials incident.
Drivers must be given time to thoroughly inspect the vehicle prior to use and must not face any penalty or disincentive for refusing to operate a vehicle that is not functioning properly. Drivers must also receive adequate driver training, vehicle inspection training, hazard recognition training and first-responder training.
If drivers are responsible for loading and unloading, they must receive training in proper lifting technique and be provided with hand-trucks, fork-lifts, cranes or other equipment necessary to handle goods without excessive strain. If drivers are expected to make repairs to vehicles, they must be provided with the correct tools and proper training. Adequate security measures must be taken to protect drivers who transport valuables or handle passenger fares or money received for goods delivered. Bus drivers should have proper supplies for dealing with body fluids from sick or injured passengers.
Drivers must receive medical services both to assure their fitness for work and to maintain their health. Medical surveillance must be provided for drivers who handle hazardous materials or are involved in an incident with exposure to blood-borne pathogens or hazardous materials . Both management and drivers must comply with standards governing the evaluation of medical fitness.
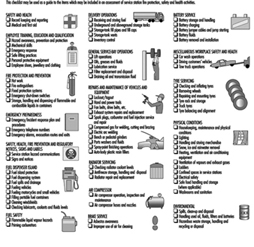
Firefighting Procedures
Firefighting is one of the world’s most honoured but hazardous operations. By becoming fire-fighters, people join an organization rich in heritage of dedication, unselfish sacrifice and inspired human action. The job of a fire-fighter is not comfortable or easy. It is one that requires a high sense of personal dedication, a genuine desire to help people and a devotion to a profession that requires a high level of skill. It is also a profession that exposes an individual to a high level of personal danger.
Whenever there is a disaster, the fire department is one of the first called to the scene. Because it is a disaster, the conditions will not always be favourable. There will be hard, fast work that will drain energy and test endurance. The situation will not always involve fire. There will be cave-ins, building collapses, auto accidents, aircraft crashes, tornadoes, dangerous-goods incidents, civil disturbances, rescue operations, explosions, water incidents and medical emergencies. The emergency list is unlimited.
All fire-fighters use the same tactics and strategies to combat a fire. The strategies are simple—fight this fire offensively or defensively. Regardless, the goal is the same—extinguishment of the fire. Urban firefighting deals with structural firefighting. (The management of forest fires is dealt with in the chapter Forestry). It includes dealing with hazardous goods, water and ice, as well as high-angle rescue and emergency medicine. Fire service personnel must respond day and night to emergencies.
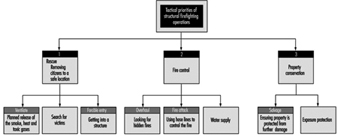
The tactical priorities that fire-fighters engage in during the course of the fire are shown in figure 1. It is during these operations that hose lays using attack lines, back up lines and supply lines can be employed. Other commonly used equipment are ladders and pushing/pulling and striking tools like axes and pike poles. Specialty equipment includes tarps that are used for salvage or hydraulic tools used for a rescue. The fire-fighter must use and be familiar with all of them. See figure 1.
Figure 1. The tactical priorities of structural firefighting operations.
Figure 2 shows a fire-fighter with appropriate personal protection laying water on a structural fire with a fire hose.
Figure 2. Firefighter laying water on a structural fire.
These operations expose the fire-fighter to the greatest risks and injuries regardless of the tool used or the operation engaged in. Back injuries, sprains, fall-related injuries and heat stress commonly occur. Heart and lung diseases are quite common among fire-fighters, which is thought to be due, in part, to the toxic gases and the level of physical activity required on the fire ground. Therefore, many departments are aggressively pursuing the addition of fitness programmes within their departments’ overall safety programme. Many jurisdictions have programmes in place to deal with critical incident stress, because the fire-fighter faces incidents that can create severe emotional reactions. Such reactions are normal reactions in the face of very abnormal situations.
The mission of every fire department is the preservation of life and property; therefore, safety on the fire ground is of paramount importance. Many of the operations discussed here have an underlying goal of providing greater safety on the fire ground. Many of the dangers that exist on the fire ground are due to the nature of fire. Backdraft and flashover kill fire-fighters. Backdraft is caused by the introduction of air into a superheated oxygen-starved area. Flashover is the build-up of heat within an area until it suddenly ignites everything within that area. These two conditions reduce the level of safety and increase property damage. Ventilation is one method of control that fire-fighters use. Increasing ventilation can lead to much damage to property. The fire-fighter is often observed breaking windows or cutting holes in the roof and intensity of the fire appears to grow. This is because smoke and toxic gases are released from the fire area. But this is a necessary part of firefighting. Special attention must be paid to roof collapse, to establishing a quick means of egress and to back-up hose lines for protection of the personnel and property.
The fire-fighter must put safety first and must work with a safety-conscious attitude and within organizational environments that promote safety. In addition, proper protective clothing must be provided and maintained. Clothing should be designed for freedom of movement and protection from heat. The structural fire-fighter must be outfitted with heavy fire-resistant fibre suits and a self-contained breathing apparatus.
The type of clothing worn is generally specific to the types of hazards faced by the fire-fighter outside the fire area on the fire line; the urban fire-fighter is generally inside a structure where intense heat and toxic gases are present. Helmets, boots and gloves designed specifically for the hazard that is faced by the fire-fighter provide head, foot and hand protection. Fire crews need training to ensure that fire-fighters have the knowledge and skills necessary to perform safely and efficiently. Training is usually provided through an in-house training programme, which can consist of a combination of on-the-job training and a formalized theory programme. Most provincial and state governments have agencies that promote various types of training programmes.
North America leads the world in property loss and many North American departments engage in preventive programmes to reduce the life and property losses within their jurisdictions. Public education and enforcement programmes are aggressively pursued by the most pro-active departments because, according to available statistics, the cost of prevention is cheaper than the cost of rebuilding. Furthermore, only 10% of businesses that suffer a total fire loss successfully rebuild. Thus the costs of a fire loss to a community can be staggering, since in addition to the cost to rebuild, sources of tax revenue, jobs and lives may also be lost forever. It is important, therefore, that both the community and the fire service work together to ensure that lives and property are preserved.
History of Performing Arts Medicine
While interest in the physiology of music making dates back to antiquity, the first real summary of the occupational diseases of performing artists is Bernardino Ramazzini’s 1713 treatise Diseases of Workers. Sporadic interest in arts medicine continued through the eighteenth and nineteenth centuries. In 1932 the English translation of Kurt Singer’s Diseases of the Music Profession: A Systematic Presentation of Their Causes, Symptoms and Methods of Treatment appeared. This was the first textbook to bring together all the current knowledge on performing arts medicine. After World War II, the medical literature began to feature case reports of injured artists. The musical literature also began to carry short items and letters. There was a parallel growth of awareness among dancers.
One of the catalysts for the development of performing arts medicine as a cross-disciplinary field was the Danube Symposium on Neurology, held in Vienna in 1972. The conference focused on music and led to the publication of Music and the Brain: Studies in the Neurology of Music, by MacDonald Critchley and R.A. Henson. Also in 1972 the first Care of the Professional Voice Symposium was organized by the Voice Foundation. This has become an annual conference, with proceedings appearing in the Journal of Voice.
While injured performers and the health professionals serving them began to cooperate more closely, the general public was unaware of these developments. In 1981 a New York Times article described the hand problems suffered by pianists Gary Graffman and Leon Fleisher, and their treatment at Massachusetts General Hospital. These were virtually the first well-known musicians to admit to physical problems, so the publicity generated by their cases brought forth a large, previously unknown group of injured artists.
Since then, the field of performing arts medicine has advanced rapidly, with conferences, publications, clinics and associations. In 1983 the first Medical Problems of Musicians and Dancers symposium was held, in conjunction with the Aspen Music Festival, in Aspen, Colorado. This has become an annual conference and is perhaps the most important in the field. Meetings such as these usually include lectures by health professionals as well as demonstrations and master classes by artists.
In 1986 the journal Medical Problems of Performing Artists was launched. This is the only journal completely dedicated to arts medicine, and it publishes many of the Aspen symposium presentations. Related journals include the Journal of Voice, Kinesiology and Medicine for Dance, and the International Journal of Arts-Medicine. In 1991 the Textbook of Performing Arts Medicine, edited by Robert Sataloff, Alice Brandfonbrener and Richard Lederman, became the first modern, comprehensive text on the subject.
As publishing grew and conferences continued, clinics serving the performing arts community were organized. Generally these clinics are in large cities that support an orchestra or dance company, such as New York, San Francisco and Chicago. There are now more than twenty such centres in the United States and several in various other countries.
Those active in the field of performing arts medicine have also founded associations to further research and education. The Performing Arts Medicine Association, set up in 1989, now co-sponsors the Aspen symposiums. Other organizations include the International Association for Dance Medicine and Science, the International Arts-Medicine Association and the Association of Medical Advisors to British Orchestras.
Research in performing arts medicine has grown from case reports and prevalence studies to sophisticated projects using advanced technology. New treatments, more responsive to the artists’ specific needs, are being developed and the emphasis is beginning to shift to prevention and education.
Ergonomics of the Physical Work Environment
Several countries have established recommended noise, temperature and lighting levels for hospitals. These recommendations are, however, rarely included in the specifications given to hospital designers. Further, the few studies examining these variables have reported disquieting levels.
Noise
In hospitals, it is important to distinguish between machine-generated noise capable of impairing hearing (above 85 dBA) and noise which is associated with a degradation of ambiance, administrative work and care (65 to 85 dBA).
Machine-generated noise capable of impairing hearing
Prior to the 1980s, a few publications had already drawn attention to this problem. Van Wagoner and Maguire (1977) evaluated the incidence of hearing loss among 100 employees in an urban hospital in Canada. They identified five zones in which noise levels were between 85 and 115 dBA: the electrical plant, laundry, dish-washing station and printing department and areas where maintenance workers used hand or power tools. Hearing loss was observed in 48% of the 50 workers active in these noisy areas, compared to 6% of workers active in quieter areas.
Yassi et al. (1992) conducted a preliminary survey to identify zones with dangerously high noise levels in a large Canadian hospital. Integrated dosimetry and mapping were subsequently used to study these high-risk areas in detail. Noise levels exceeding 80 dBA were common. The laundry, central processing, nutrition department, rehabilitation unit, stores and electrical plant were all studied in detail. Integrated dosimetry revealed levels of up to 110 dBA at some of these locations.
Noise levels in a Spanish hospital’s laundry exceeded 85 dBA at all workstations and reached 97 dBA in some zones (Montoliu et al. 1992). Noise levels of 85 to 94 dBA were measured at some workstations in a French hospital’s laundry (Cabal et al. 1986). Although machine re-engineering reduced the noise generated by pressing machines to 78 dBA, this process was not applicable to other machines, due to their inherent design.
A study in the United States reported that electrical surgical instruments generate noise levels of 90 to 100 dBA (Willet 1991). In the same study, 11 of 24 orthopaedic surgeons were reported to suffer from significant hearing loss. The need for better instrument design was emphasized. Vacuum and monitor alarms have been reported to generate noise levels of up to 108 dBA (Hodge and Thompson 1990).
Noise associated with a degradation of ambiance, administrative work and care
A systematic review of noise levels in six Egyptian hospitals revealed the presence of excessive levels in offices, waiting rooms and corridors (Noweir and al-Jiffry 1991). This was attributed to the characteristics of hospital construction and of some of the machines. The authors recommended the use of more appropriate building materials and equipment and the implementation of good maintenance practices.
Work in the first computerized facilities was hindered by the poor quality of printers and the inadequate acoustics of offices. In the Paris region, groups of cashiers talked to their clients and processed invoices and payments in a crowded room whose low plaster ceiling had no acoustic absorption capacity. Noise levels with only one printer active (in practice, all four usually were) were 78 dBA for payments and 82 dBA for invoices.
In a 1992 study of a rehabilitation gymnasium consisting of 8 cardiac rehabilitation bicycles surrounded by four private patient areas, noise levels of 75 to 80 dBA and 65 to 75 dBA were measured near cardiac rehabilitation bicycles and in the neighbouring kinesiology area, respectively. Levels such as these render personalized care difficult.
Shapiro and Berland (1972) viewed noise in operating theatres as the “third pollution”, since it increases the fatigue of the surgeons, exerts physiological and psychological effects and influences the accuracy of movements. Noise levels were measured during a cholecystectomy and during tubal ligation. Irritating noises were associated with the opening of a package of gloves (86 dBA), the installation of a platform on the floor (85 dBA), platform adjustment (75 to 80 dBA), placing surgical instruments upon each other (80 dBA), suctioning of trachea of patient (78 dBA), continuous suction bottle (75 to 85 dBA) and the heels of nurses’ shoes (68 dBA). The authors recommended the use of heat-resistant plastic, less noisy instruments and, to minimize reverberation, easily cleaned materials other than ceramic or glass for walls, tiles and ceilings.
Noise levels of 51 to 82 dBA and 54 to 73 dBA have been measured in the centrifuge room and automated analyser room of a medical analytical laboratory. The Leq (reflecting full-shift exposure) at the control station was 70.44 dBA, with 3 hours over 70 dBA. At the technical station, the Leq was 72.63 dBA, with 7 hours over 70 dBA. The following improvements were recommended: installing telephones with adjustable ring levels, grouping centrifuges in a closed room, moving photocopiers and printers and installing hutches around the printers.
Patient Care and Comfort
In several countries, recommended noise limits for care units are 35 dBA at night and 40 dBA during the day (Turner, King and Craddock 1975). Falk and Woods (1973) were the first to draw attention to this point, in their study of noise levels and sources in neonatology incubators, recovery rooms and two rooms in an intensive-care unit. The following mean levels were measured over a 24-hour period: 57.7 dBA (74.5 dB) in the incubators, 65.5 dBA (80 dB linear) at the head of patients in the recovery room, 60.1 dBA (73.3 dB) in the intensive care unit and 55.8 dBA (68.1 dB) in one patient room. Noise levels in the recovery room and intensive-care unit were correlated with the number of nurses. The authors emphasized the probable stimulation of patients’ hypophyseal-corticoadrenal system by these noise levels, and the resultant increase in peripheral vasoconstriction. There was also some concern about the hearing of patients receiving aminoglycoside antibiotics. These noise levels were considered incompatible with sleep.
Several studies, most of which have been conducted by nurses, have shown that noise control improves patient recovery and quality of life. Reports of research conducted in neonatology wards caring for low-birth-weight babies emphasized the need to reduce the noise caused by personnel, equipment and radiology activities (Green 1992; Wahlen 1992; Williams and Murphy 1991; Oëler 1993; Lotas 1992; Halm and Alpen 1993). Halm and Alpen (1993) have studied the relationship between noise levels in intensive-care units and the psychological well-being of patients and their families (and in extreme cases, even of post-resuscitation psychosis). The effect of ambient noise on the quality of sleep has been rigorously evaluated under experimental conditions (Topf 1992). In intensive care units, the playing of pre-recorded sounds was associated with a deterioration of several sleep parameters.
A multi-ward study reported peak noise levels at the head of patients in excess of 80 dBA, especially in intensive- and respiratory-care units (Meyer et al. 1994). Lighting and noise levels were recorded continuously over seven consecutive days in a medical intensive-care unit, one-bed and multi-bed rooms in a respiratory-care unit and a private room. Noise levels were very high in all cases. The number of peaks exceeding 80 dBA was particularly high in the intensive- and respiratory-care units, with a maximum observed between 12:00 and 18:00 and a minimum between 00:00 and 06:00. Sleep deprivation and fragmentation were considered to have a negative impact on the respiratory system of patients and impair the weaning of patients from mechanical ventilation.
Blanpain and Estryn-Béhar (1990) found few noisy machines such as waxers, ice machines and hotplates in their study of ten Paris-area wards. However, the size and surfaces of the rooms could either reduce or amplify the noise generated by these machines, as well as that (albeit lower) generated by passing cars, ventilation systems and alarms. Noise levels in excess of 45 dBA (observed in 7 of 10 wards) did not promote patient rest. Furthermore, noise disturbed hospital personnel performing very precise tasks requiring close attention. In five of 10 wards, noise levels at the nursing station reached 65 dBA; in two wards, levels of 73 dBA were measured. Levels in excess of 65 dBA were measured in three pantries.
In some cases, architectural decorative effects were instituted with no thought to their effect on acoustics. For example, glass walls and ceilings have been in fashion since the 1970s and have been used in patient admission open-space offices. The resultant noise levels do not contribute to the creation of a calm environment in which patients about to enter the hospital can fill out forms. Fountains in this type of hall generated a background noise level of 73 dBA at the reception desk, requiring receptionists to ask one-third of people requesting information to repeat themselves.
Heat stress
Costa, Trinco and Schallenberg (1992) studied the effect of installing a laminar flow system, which maintained air sterility, on heat stress in an orthopaedic operating theatre. Temperature in the operating theatre increased by approximately 3 °C on average and could reach 30.2 °C. This was associated with a deterioration of the thermal comfort of operating-room personnel, who must wear very bulky clothes that favour heat retention.
Cabal et al. (1986) analysed heat stress in a hospital laundry in central France prior to its renovation. They noted that the relative humidity at the hottest workstation, the “gown-dummy”, was 30%, and radiant temperature reached 41 °C. Following installation of double-pane glass and reflective outside walls, and implementation of 10 to 15 air changes per hour, thermal comfort parameters fell within standard levels at all workstations, regardless of the weather outside. A study of a Spanish hospital laundry has shown that high wet-bulb temperatures result in oppressive work environments, especially in ironing areas, where temperatures may exceed 30 °C (Montoliu et al. 1992).
Blanpain and Estryn-Béhar (1990) characterized the physical work environment in ten wards whose work content they had already studied. Temperature was measured twice in each of ten wards. The nocturnal temperature in patient rooms may be below 22 °C, as patients use covers. During the day, as long as patients are relatively inactive, a temperature of 24 °C is acceptable but should not be exceeded, since some nursing interventions require significant exertion.
The following temperatures were observed between 07:00 and 07:30: 21.5 °C in geriatric wards, 26 °C in a non-sterile room in the haematology ward. At 14:30 on a sunny day, the temperatures were as follows: 23.5 °C in the emergency room and 29 °C in the haematology ward. Afternoon temperatures exceeded 24 °C in 9 of 19 cases. The relative humidity in four out of five wards with general air-conditioning was below 45% and was below 35% in two wards.
Afternoon temperature also exceeded 22 °C at all nine care preparation stations and 26 °C at three care stations. The relative humidity was below 45% in all five stations of wards with air-conditioning. In the pantries, temperatures ranged between 18 °C and 28.5 °C.
Temperatures of 22 °C to 25 °C were measured at the urine drains, where there were also odour problems and where dirty laundry was sometimes stored. Temperatures of 23 °C to 25 °C were measured in the two dirty-laundry closets; a temperature of 18 °C would be more appropriate.
Complaints concerning thermal comfort were frequent in a survey of 2,892 women working in Paris-area wards (Estryn-Béhar et al. 1989a). Complaints of being often or always hot were reported by 47% of morning- and afternoon-shift nurses and 37% of night-shift nurses. Although nurses were sometimes obliged to perform physically strenuous work, such as making several beds, the temperature in the various rooms was too high to perform these activities comfortably while wearing polyester-cotton clothes, which hinder evaporation, or gowns and masks necessary for the prevention of nosocomial infections.
On the other hand, 46% of night-shift nurses and 26% of morning- and afternoon-shift nurses reported being often or always cold. The proportions reporting never suffering from the cold were 11% and 26%.
To conserve energy, the heating in hospitals was often lowered during the night, when patients are under covers. However nurses, who must remain alert despite chronobiologically mediated drops in core body temperatures, were required to put on jackets (not always very hygienic ones) around 04:00. At the end of the study, some wards installed adjustable space-heating at nursing stations.
Studies of 1,505 women in 26 units conducted by occupational physicians revealed that rhinitis and eye irritation were more frequent among nurses working in air-conditioned rooms (Estryn-Béhar and Poinsignon 1989) and that work in air-conditioned environments was related to an almost twofold increase in dermatoses likely to be occupational in origin (adjusted odds ratio of 2) (Delaporte et al. 1990).
Lighting
Several studies have shown that the importance of good lighting is still underestimated in administrative and general departments of hospitals.
Cabal et al. (1986) observed that lighting levels at half of the workstations in a hospital laundry were no higher than 100 lux. Lighting levels following renovations were 300 lux at all workstations, 800 lux at the darning station and 150 lux between the washing tunnels.
Blanpain and Estryn-Béhar (1990) observed maximum night lighting levels below 500 lux in 9 out of 10 wards. Lighting levels were below 250 lux in five pharmacies with no natural lighting and were below 90 lux in three pharmacies. It should be recalled that the difficulty in reading small lettering on labels experienced by older persons may be mitigated by increasing the level of illumination.
Building orientation can result in high day-time lighting levels that disturb patients’ rest. For example, in geriatric wards, beds furthest from the windows received 1,200 lux, while those nearest the windows received 5,000 lux. The only window shading available in these rooms were solid window blinds and nurses were unable to dispense care in four-bed rooms when these were drawn. In some cases, nurses stuck paper on the windows to provide patients with some relief.
The lighting in some intensive-care units is too intense to allow patients to rest (Meyer et al. 1994). The effect of lighting on patients’ sleep has been studied in neonatology wards by North American and German nurses (Oëler 1993; Boehm and Bollinger 1990).
In one hospital, surgeons disturbed by reflections from white tiles requested the renovation of the operating theatre. Lighting levels outside the shadow-free zone (15,000 to 80,000 lux) were reduced. However, this resulted in levels of only 100 lux at the instrument nurses’ work surface, 50 to 150 lux at the wall unit used for equipment storage, 70 lux at the patients’ head and 150 lux at the anaesthetists’ work surface. To avoid generating glare capable of affecting the accuracy of surgeons’ movements, lamps were installed outside of surgeons’ sight-lines. Rheostats were installed to control lighting levels at the nurses’ work surface between 300 and 1,000 lux and general levels between 100 and 300 lux.
Construction of a hospital with extensive natural lighting
In 1981, planning for the construction of Saint Mary’s Hospital on the Isle of Wight began with a goal of halving energy costs (Burton 1990). The final design called for extensive use of natural lighting and incorporated double-pane windows that could be opened in the summer. Even the operating theatre has an outside view and paediatric wards are located on the ground floor to allow access to play areas. The other wards, on the second and third (top) floors, are equipped with windows and ceiling lighting. This design is quite suitable for temperate climates but may be problematic where ice and snow inhibit overhead lighting or where high temperatures may lead to a significant greenhouse effect.
Architecture and Working Conditions
Flexible design is not multi-functionality
Prevailing concepts from 1945 to 1985, in particular the fear of instant obsolescence, were reflected in the construction of multi-purpose hospitals composed of identical modules (Games and Taton-Braen 1987). In the United Kingdom this trend led to the development of the “Harnes system”, whose first product was the Dudley Hospital, built in 1974. Seventy other hospitals were later built on the same principles. In France, several hospitals were constructed on the “Fontenoy” model.
Building design should not prevent modifications necessitated by the rapid evolution of therapeutic practice and technology. For example, partitions, fluid circulation subsystems and technical duct-work should all be capable of being easily moved. However, this flexibility should not be construed as an endorsement of the goal of complete multi-functionality—a design goal which leads to the construction of facilities poorly suited to any speciality. For example, the surface area needed to store machines, bottles, disposable equipment and medication is different in surgical, cardiology and geriatric wards. Failure to recognize this will lead to rooms being used for purposes they were not designed for (e.g., bathrooms being used for bottle storage).
The Loma Linda Hospital in California (United States) is an example of better hospital design and has been copied elsewhere. Here, nursing and technical medicine departments are located above and below technical floors; this “sandwich” structure permits easy maintenance and adjustment of fluid circulation.
Unfortunately, hospital architecture does not always reflect the needs of those who work there, and multi-functional design has been responsible for reported problems related to physical and cognitive strain. Consider a 30-bed ward composed of one- and two-bed rooms, in which there is only one functional area of each type (nursing station, pantry, storage of disposable materials, linen or medication), all based on the same all-purpose design. In this ward, the management and dispensation of care obliges nurses to change location extremely frequently, and work is greatly fragmented. A comparative study of ten wards has shown that the distance from the nurses’ station to the farthest room is an important determinant of both nurses’ fatigue (a function of the distance walked) and the quality of care (a function of the time spent in patients’ rooms) (Estryn-Béhar and Hakim-Serfaty 1990).
This discrepancy between the architectural design of spaces, corridors and materials, on the one hand, and the realities of hospital work, on the other, has been characterized by Patkin (1992), in a review of Australian hospitals, as an ergonomic “debacle”.
Preliminary analysis of the spatial organization in nursing areas
The first mathematical model of the nature, purposes and frequency of staff movements, based on the Yale Traffic Index, appeared in 1960 and was refined by Lippert in 1971. However, attention to one problem in isolation may in fact aggravate others. For example, locating a nurses’ station in the centre of the building, in order to reduce the distances walked, may worsen working conditions if nurses must spend over 30% of their time in such windowless surroundings, known to be a source of problems related to lighting, ventilation and psychological factors (Estryn-Béhar and Milanini 1992).
The distance of the preparation and storage areas from patients is less problematic in settings with a high staff-patient ratio and where the existence of a centralized preparation area facilitates the delivery of supplies several times per day, even on holidays. In addition, long waits for elevators are less common in high-rise hospitals with over 600 beds, where the number of elevators is not limited by financial constraints.
Research on the design of specific but flexible hospital units
In the United Kingdom in the late 1970s, the Health Ministry created a team of ergonomists to compile a database on ergonomics training and on the ergonomic layout of hospital work areas (Haigh 1992). Noteworthy examples of the success of this programme include the modification of the dimensions of laboratory furniture to take into account the demands of microscopy work and the redesign of maternity rooms to take into account nurses’ work and mothers’ preferences.
Cammock (1981) emphasized the need to provide distinct nursing, public and common areas, with separate entrances for nursing and public areas, and separate connections between these areas and the common area. Furthermore, there should be no direct contact between the public and nursing areas.
The Krankenanstalt Rudolfsstiftung is the first pilot hospital of the “European Healthy Hospitals” project. The Viennese pilot project consists of eight sub-projects, one of which, the “Service Reorganization” project, is an attempt, in collaboration with ergonomists, to promote functional reorganization of available space (Pelikan 1993). For example, all the rooms in an intensive care unit were renovated and rails for patient lifts installed in the ceilings of each room.
A comparative analysis of 90 Dutch hospitals suggests that small units (floors of less than 1,500 m2) are the most efficient, as they allow nurses to tailor their care to the specifics of patients’ occupational therapy and family dynamics (Van Hogdalem 1990). This design also increases the time nurses can spend with patients, since they waste less time in changes of location and are less subject to uncertainty. Finally, the use of small units reduces the number of windowless work areas.
A study carried out in the health administration sector in Sweden reported better employee performance in buildings incorporating individual offices and conference rooms, as opposed to an open plan (Ahlin 1992). The existence in Sweden of an institute dedicated to the study of working conditions in hospitals, and of legislation requiring consultation with employee representatives both before and during all construction or renovation projects, has resulted in the regular recourse to participatory design based on ergonomic training and intervention (Tornquist and Ullmark 1992).
Architectural design based on participatory ergonomics
Workers must be involved in the planning of the behavioural and organizational changes associated with the occupation of a new work space. The adequate organization and equipping of a workplace requires taking into account the organizational elements that require modification or emphasis. Two detailed examples taken from two hospitals illustrate this.
Estryn-Béhar et al. (1994) report the results of the renovation of the common areas of a medical ward and a cardiology ward of the same hospital. The ergonomics of the work performed by each profession in each ward was observed over seven entire workdays and discussed over a two-day period with each group. The groups included representatives of all occupations (department heads, supervisors, interns, nurses, nurses’ aides, orderlies) from all the shifts. One entire day was spent developing architectural and organizational proposals for each problem noted. Two more days were spent on the simulation of characteristic activities by the entire group, in collaboration with an architect and an ergonomist, using modular cardboard mock-ups and scale models of objects and people. Through this simulation, representatives of the various occupations were able to agree on distances and the distribution of space within each ward. Only after this process was concluded was the design specification drawn up.
The same participatory method was used in a cardiac intensive-care unit in another hospital (Estryn-Béhar et al. 1995a, 1995b). It was found that four types of virtually incompatible activities were conducted at the nursing station:
- care preparation, requiring the use of a drain-board and sink
- decontamination, which also used the sink
- meeting, writing and monitoring; the area used for these activities was also sometimes used for the preparation of care
- clean-equipment storage (three units) and waste storage (one unit).
These zones overlapped, and nurses had to cross the meeting-writing-monitoring area to reach the other areas. Because of the position of the furniture, nurses had to change direction three times to get to the drain-board. Patient rooms were laid out along a corridor, both for regular intensive care and highly intensive care. The storage units were located at the far end of the ward from the nursing station.
In the new layout, the station’s longitudinal orientation of functions and traffic is replaced with a lateral one which allows direct and central circulation in a furniture-free area. The meeting-writing-monitoring area is now located at the end of the room, where it offers a calm space near windows, while remaining accessible. The clean and dirty preparation areas are located by the entrance to the room and are separated from each other by a large circulation area. The highly intensive care rooms are large enough to accommodate emergency equipment, a preparation counter and a deep washbasin. A glass wall installed between the preparation areas and the highly intensive care rooms ensures that patients in these rooms are always visible. The main storage area was rationalized and reorganized. Plans are available for each work and storage area.
Architecture, ergonomics and developing countries
These problems are also found in developing countries; in particular, renovations there frequently involve the elimination of common rooms. The performance of ergonomic analysis would identify existing problems and help avoid new ones. For example, the construction of wards comprised of only one- or two-bed rooms increases the distances that personnel must travel. Inadequate attention to staffing levels and the layout of nursing stations, satellite kitchens, satellite pharmacies and storage areas may lead to significant reductions in the amount of time nurses spend with patients and may render work organization more complex.
Furthermore, the application in developing countries of the multi-functional hospital model of developed countries does not take into account different cultures’ attitudes toward space utilization. Manuaba (1992) has pointed out that the layout of developed countries’ hospital rooms and the type of medical equipment used is poorly suited to developing countries, and that the rooms are too small to comfortably accommodate visitors, essential partners in the curative process.
Hygiene and Ergonomics
In hospital settings, many breaches of asepsis can be understood and corrected only by reference to work organization and work space. Effective implementation of the necessary modifications requires detailed ergonomic analysis. This analysis serves to characterize the interdependencies of team tasks, rather than their individual characteristics, and identify discrepancies between real and nominal work, especially nominal work described in official protocols.
Hand-mediated contamination was one of the first targets in the fight against nosocomial infections. In theory, hands should be systemtically washed on entering and leaving patients’ rooms. Although initial and ongoing training of nurses emphasizes the results of descriptive epidemiological studies, research indicates persistent problems associated with hand-washing. In a study conducted in 1987 and involving continuous observation of entire 8-hour shifts in 10 wards, Delaporte et al. (1990) observed an average of 17 hand-washings by morning-shift nurses, 13 by afternoon-shift nurses and 21 by night-shift nurses.
Nurses washed their hands one-half to one-third as often as is recommended for their number of patient contacts (without even considering care-preparation activities); for nurses’ aides, the ratio was one-third to one-fifth. Hand-washing before and after each activity is, however, clearly impossible, in terms of both time and skin damage, given the atomization of activity, number of technical interventions and frequency of interruptions and attendant repetition of care that personnel must cope with. Reduction of work interruptions is thus essential and should take precedence over simply reaffirming the importance of hand-washing, which, in any event, cannot be performed over 25 to 30 times per day.
Similar patterns of hand-washing were found in a study based on observations collected over 14 entire workdays in 1994 during the reorganization of the common areas of two university hospital wards (Estryn-Béhar et al. 1994). In every case, nurses would have been incapable of dispensing the required care if they had returned to the nursing station to wash their hands. In short-term-stay units, for example, almost all the patients have blood samples drawn and subsequently receive oral and intravenous medication at virtually the same time. The density of activities at certain times also renders appropriate hand-washing impossible: in one case, an afternoon-shift nurse responsible for 13 patients in a medical ward entered patients’ rooms 21 times in one hour. Poorly organized information provision and transmission structures contributed to the number of visits he was obliged to perform. Given the impossibility of washing his hands 21 times in one hour, the nurse washed them only when dealing with the most fragile patients (i.e., those suffering from pulmonary failure).
Ergonomically based architectural design takes several factors affecting hand-washing into account, especially those concerning the location and access to wash-basins, but also the implementation of truly functional “dirty” and “clean” circuits. Reduction of interruptions through participatory analysis of organization helps to make hand-washing possible.
Ergonomics of Bus Driving
Bus driving is characterized by psychological and physical stresses. Most severe are the stresses of traffic in big cities, because of the heavy traffic and frequent stops. In most transit companies, the drivers must, in addition to driving responsibilities, handle tasks such as selling tickets, observing passenger loading and unloading and providing information to passengers.
Psychological stresses result from the responsibility for the safe transport of passengers, scant opportunity to communicate with colleagues and the time pressure of holding to a fixed schedule. Rotating shift work is also psychologically and physically stressful. Ergonomic shortcomings in the driver’s workstation increase physical stresses.
Numerous studies of the activity of bus drivers have shown that the individual stresses are not great enough to cause an immediate health hazard. But the sum of the stresses and the resulting strain leads to bus drivers having more frequent health problems than other workers. Especially significant are diseases of the stomach and digestive tract, of the motor system (especially the spine) and of the cardiovascular system. This results in drivers often not reaching retirement age, but rather having to quit driving early for health reasons (Beiler and Tränkle 1993; Giesser-Weigt and Schmidt 1989; Haas, Petry and Schühlein 1989; Meifort, Reiners and Schuh 1983; Reimann 1981).
In order to achieve more effective occupational safety in the field of commercial driving, technical as well as organizational measures are necessary. An important work practice is the arranging of shift schedules so that the stress on the drivers is minimized and their personal desires are also taken into account to the extent possible. Informing the personnel of and motivating them to health-conscious conduct (e.g., proper diet, adequate movement within and outside of the workstation) can play an important role in promoting health. An especially necessary technical measure is the ergonomically optimal design of the driver’s workstation. In the past, the requirements of the driver’s workstation were considered only after other requirements, such as design of the passenger area. Ergonomic design of the driver’s workstation is a necessary component of driver safety and health protection. In recent years, research projects on, among other things, the ergonomically optimal driver’s workstation were conducted in Canada, Sweden, Germany and the Netherlands (Canadian Urban Transit Association 1992; Peters et al. 1992; Wallentowitz et al. 1996; Streekvervoer Nederland 1991). The results of the interdisciplinary project in Germany resulted in a new, standardized driver’s workstation (Verband Deutscher Verkehrsunternehmen 1996).
The driver’s workstation in buses is normally designed in the form of a half-open cabin. The measurements of the driver’s cabin and the adjustments that can be made to the seat and steering wheel must fall within a range that is applicable to all drivers. For central Europe, this means a body-size range of 1.58 to 2.00 m. Special proportions, such as being overweight and having long or short limbs, should also be taken into account in the design.
The adjustability and the ways of adjusting the driver’s seat and steering wheel should be coordinated so that all drivers within the design range can find positions for their arms and legs that are comfortable and ergonomically healthy. For this purpose, the optimal seat placement has a back incline about 20°, which is further from the vertical than has previously been the norm in commercial vehicles. Furthermore, the instrument panel should also be adjustable for optimal access to adjustment levers and for good visibility of the instruments. This can be coordinated with the steering wheel adjustment. Using a smaller steering wheel also improves spatial relations. The steering wheel diameter now in general use apparently comes from a time when power steering was not common in buses. See figure 1.
Figure 1. Ergonomically optimized and unified driver's workstation for busses in Germany.
Courtesy of Erobus GmbH, Mannheim, Germany
The instrument panel with the controls can be adjusted in coordination with the steering wheel.
Since stumbling and falling are the most common causes of workplace accidents among drivers, particular attention should be paid to the design of the entrance to the driver’s workstation. Anything that can be stumbled on should be avoided. Steps in the entrance area must be of equal height and have adequate step depth.
The driver’s seat should have a total of five adjustments: seat length and height settings, seat back angle, seat bottom angle and seat depth. Adjustable lumbar support is strongly advised. To the extent that it is not already legally required, equipping the driver’s seat with a three-point seat-belt and head rest are recommended. Since experience shows that manually adjusting to the ergonomically right position is time-consuming, in the future some way of electronically storing the adjustment functions listed in table 1 should be used, allowing for quickly and easily refinding the individual seating adjustment (e.g., by entering it onto an electronic card).
Table 1. Bus driver seat measurements and seat adjustment ranges.
|
Component |
Measurement/ |
Standard value |
Adjustment range |
Memorized |
|
Entire seat |
Horizontal |
— |
≥ 200 |
Yes |
|
Vertical |
— |
≥ 100 |
Yes |
|
|
Seat surface |
Seat surface depth |
— |
390–450 |
Yes |
|
Seat surface width (total) |
Min. 495 |
— |
— |
|
|
Seat surface width (flat part, in pelvic area) |
430 |
— |
— |
|
|
Side upholstering in pelvic area (crosswise) |
40–70 |
— |
— |
|
|
Depth of seat recess |
10–20 |
— |
— |
|
|
Seat surface slope |
— |
0–10° (rising toward front) |
Yes |
|
|
Seatback |
Seatback height |
|||
|
Min. height |
495 |
— |
— |
|
|
Max. height |
640 |
— |
— |
|
|
Seatback width (total)* |
Min. 475 |
— |
— |
|
|
Seatback width (flat part) |
||||
|
—lumbar area (lower) |
340 |
— |
— |
|
|
—shoulder area (upper) |
385 |
— |
— |
|
|
Seatback |
Side upholstering* (side depth) |
|||
|
—lumbar area (lower) |
50 |
— |
— |
|
|
—shoulder area (upper) |
25 |
— |
— |
|
|
Seatback slope (to vertical) |
— |
0°–25° |
Yes |
|
|
Headrest |
Height of headrest upper edge above seat surface |
— |
Min. 840 |
— |
|
Height of headrest itself |
Min. 120 |
— |
— |
|
|
Width of headrest |
Min. 250 |
— |
— |
|
|
Lumbar pad |
Forward arch of lumbar support from lumbar surface |
— |
10–50 |
— |
|
Height of lumbar support lower edge over seat surface |
— |
180–250 |
— |
– Not applicable
* The width of the lower part of the backrest should correspond approximately to the width of the seat surface and grow narrower as it goes up.
** The side upholstering of the seat surface applies only to the recess area.
Stress through whole-body vibrations in the driver’s workstation is low in modern buses compared to other commercial vehicles, and it falls well below the international standards. Experience shows that driver’s seats in buses are often not optimally adjusted to the vehicle’s actual vibration. An optimal adaptation is advised to avoid certain frequency ranges causing an increase in whole-body vibration on the driver, which can interfere with productivity.
Noise levels that are a hazard to hearing are not anticipated in the bus driver’s workstation. High-frequency noise can be irritating and should be eliminated because it could interfere with the drivers’ concentration.
All adjustment and service components in the driver’s workstation should be arranged for comfortable access. A large number of adjustment components are often required due to the amount of equipment added to the vehicle. For this reason, switches should be grouped and consolidated according to use. Frequently used service components such as door openers, bus stop brakes and windshield wipers should be placed in the main access area. Less frequently used switches can be located outside the main access area (e.g., on a side console).
Analyses of visual movements have shown that driving the vehicle in traffic and observing the loading and unloading of passengers at the stops is a serious burden on the driver’s attention. Thus, the information conveyed by instruments and indicator lights in the vehicle should be limited to those absolutely necessary. Vehicle computerized electronics offer the possibility of eliminating numerous instruments and indicator lights, and instead installing a liquid crystal display (LCD) in a central location to convey information, as shown in the instrument panel in figure 2 and figure 3.
Figure 2. View of an instrument panel.
Courtesy of Erobus GmbH, Mannheim, Germany
With the exception of the speedometer and a few legally required indicator lights, the functions of the instrument and indicator displays have been assumed by a central LCD display.
Figure 3. Illustration of an instrument panel with legend.
With the proper computer software, the display will show only a selection of information that is needed for the particular situation. In the case of malfunction, a description of the problem and brief instructions in clear text, rather than in difficult-to- understand pictograms, can provide the driver with important assistance. A hierarchy of malfunction notifications can also be established (e.g., “advisory” for less significant malfunctions, “alarm” when the vehicle must be stopped immediately).
Heating systems in buses often heat the interior with warm air only. For real comfort, however, a higher proportion of radiant heat is desirable (e.g., by heating the side walls, whose surface temperature often lies significantly below the interior air temperature). This, for example, can be achieved by circulating warm air through perforated wall surfaces, which thereby will also have the right temperature. Large window surfaces are used in the driver’s area in buses to improve visibility and also for appearance. These can lead to a significant warming of the inside by sun rays. The use of air conditioning is thus advisable.
The air quality of the driver’s cabin depends heavily on the quality of the outside air. Depending on the traffic, high concentrations of harmful substances, such as carbon monoxide and diesel motor emissions, can briefly occur. Providing fresh air from less-used areas, such as the roof instead of the vehicle front, lessens the problem significantly. Fine-particle filters should also be used.
In most transit companies, an important part of the driving personnel’s activity consists of selling tickets, operating devices to provide information to passengers and communicating with the company. Until now, separate devices, located in the available work space and often hard for the driver to reach, have been used for these activities. An integrated design should be sought from the start that arranges the devices in an ergonomically convenient manner in the driver’s area, especially the input keys and display panels.
Finally, the assessment of the driver’s area by the drivers, whose personal interests should be taken into account, is of great importance. Supposedly minor details, such as placement of the driver’s bag or storage lockers for personal effects, are important for driver satisfaction.
Firefighting Hazards
We thank the Edmonton Fire-fighters’ Union for their interest and generous support of the development of this chapter. The “Edmonton Sun” and the “Edmonton Journal” graciously allowed their news photographs to be used in the articles on firefighting. Ms. Beverly Cann of the Manitoba Federation of Labour Occupational Health Centre contributed invaluable advice on the article on paramedical personnel and ambulance attendants.
Fire-brigade personnel may be engaged on a full-time, part-time, paid-on-call or unpaid, volunteer basis—or on a combination of these systems. The type of organization employed will, in most cases, depend on the size of the community, the value of the property to be protected, the types of fire risk and the number of calls typically answered. Cities of any appreciable size require regular fire brigades with full crews on duty equipped with the appropriate apparatus.
Smaller communities, residential districts and rural areas having few fire calls usually depend upon volunteer or paid-on-call fire-fighters for either full staffing of their firefighting apparatus or to assist a skeleton force of full-time regulars.
Although there are a great many efficient, well equipped volunteer fire departments, full-time, paid fire departments are essential in larger communities. A call or volunteer organization does not lend itself as readily to the continuous fire-prevention inspection work that is an essential activity of modern fire departments. Using volunteer and call systems, frequent alarms may call out workers who hold other jobs, causing a loss of time with seldom any direct benefit to employers. Where full-time fire-fighters are not employed, the volunteers must come to a central fire hall before response can be made to a call, causing a delay. Where there are only a few regulars, a supplementary group of well-trained call or volunteer fire-fighters should be provided. There should be a reserve arrangement that make assistance available for the response of neighbouring departments on a mutual-aid basis.
Firefighting is a highly unusual occupation, in that it is perceived of as dirty and dangerous but is indispensable and even prestigious. Fire-fighters enjoy public admiration for the essential work that they do. They are well aware of the hazards. Their work involves intermittent periods of exposure to extreme physical and psychological stress on the job. Fire-fighters are also exposed to serious chemical and physical hazards, to a degree unusual in the modern workforce.
Hazards
Occupational hazards experienced by fire-fighters may be categorized as physical (mostly unsafe conditions, thermal stress and ergonomic stress), chemical and psychological. The level of exposure to hazards that may be experienced by a fire-fighter in a given fire depends on what is burning, the combustion characteristics of the fire, the structure that is on fire, the presence of non-fuel chemicals, the measures taken to control the fire, the presence of victims that require rescue and the position or line of duty held by the fire-fighter while fighting the fire. The hazards and levels of exposure experienced by the first fire-fighter to enter a burning building are also different from those of the fire-fighters who enter later or who clean up after the flames are extinguished. There is usually rotation among the active firefighting jobs in each team or platoon, and a regular transfer of personnel between fire halls. Fire-fighters may also have special rank and duties. Captains accompany and direct the crews but are still actively involved in fighting the fire on site. Fire chiefs are the heads of the fire service and are called out only in the worst fires. Individual fire-fighters may still experience unusual exposures in particular incidents, of course.
Physical hazards
There are many physical dangers in firefighting that can lead to serious physical injury. Walls, ceilings and floors can collapse abruptly, trapping fire-fighters. Flashovers are explosive eruptions of flame in a confined space that occur as a result of the sudden ignition of flammable gas products driven out of burning or hot materials and combined with superheated air. Fire situations that lead to flashovers may engulf the fire-fighter or cut off escape routes. The extent and number of injuries can be minimized by intensive training, job experience, competency and good physical fitness. However, the nature of the job is such that fire-fighters may be placed in dangerous situations by miscalculation, circumstance or during rescues.
Some fire departments have compiled computerized databases on structures, materials and potential hazards likely to be encountered in the district. Quick access to these databases assists the crew in responding to known hazards and anticipating possibly dangerous situations.
Thermal hazards
Heat stress during firefighting may come from hot air, radiant heat, contact with hot surfaces or endogenous heat that is produced by the body during exercise but which cannot be cooled during the fire. Heat stress is compounded in firefighting by the insulating properties of the protective clothing and by physical exertion, which result in heat production within the body. Heat may result in local injury in the form of burns or generalized heat stress, with the risk of dehydration, heat stroke and cardiovascular collapse.
Hot air by itself is not usually a great hazard to the fire-fighter. Dry air does not have much capacity to retain heat. Steam or hot, wet air can cause serious burns because much more heat energy can be stored in water vapour than in dry air. Fortunately, steam burns are not common.
Radiant heat is often intense in a fire situation. Burns may occur from radiant heat alone. Fire-fighters may also show skin changes characteristic of prolonged exposure to heat.
Chemical hazards
Over 50% of fire-related fatalities are the result of exposure to smoke rather than burns. One of the major contributing factors to mortality and morbidity in fires is hypoxia because of oxygen depletion in the affected atmosphere, leading to loss of physical performance, confusion and inability to escape. The constituents of smoke, singly and in combination, are also toxic. Figure 1 shows a fire-fighter using self-contained breathing apparatus (SCBA) rescuing an unprotected fire-fighter who was trapped in a very smoky fire in a tire warehouse. (The fire-fighter being rescued ran out of air, took off his SCBA to breathe as best he could, and was fortunate enough to be rescued before it was too late.)
Figure 1. Fire-fighter rescuing another fire-fighter who was trapped in the toxic smoke from a fire in a tire warehouse.
All smoke, including that from simple wood fires, is hazardous and potentially lethal with concentrated inhalation. Smoke is a variable combination of compounds. The toxicity of smoke depends primarily on the fuel, the heat of the fire and whether or how much oxygen is available for combustion. Fire-fighters on the scene of a fire are frequently exposed to carbon monoxide, hydrogen cyanide, nitrogen dioxide, sulphur dioxide, hydrogen chloride, aldehydes and organic compounds such as benzene. Different gas combinations present different degrees of hazard. Only carbon monoxide and hydrogen cyanide are commonly produced in lethal concentrations in building fires.
Carbon monoxide is the most common, characteristic and serious acute hazard of firefighting. Carboxyhaemoglobin accumulates rapidly in the blood with duration of exposure, as a result of the affinity of carbon monoxide for haemoglobin. High levels of carboxyhaemoglobin may result, particularly when heavy exertion increases minute ventilation and therefore delivery to the lung during unprotected firefighting. There is no apparent correlation between the intensity of smoke and the amount of carbon monoxide in the air. Fire-fighters should particularly avoid cigarette smoking during the clean-up phase, when burning material is smouldering and therefore burning incompletely, as this adds to the already elevated levels of carbon monoxide in the blood. Hydrogen cyanide is formed from the lower temperature combustion of nitrogen-rich materials, including natural fibres such as wool and silk, as well as common synthetics such as polyurethane and polyacrylonitrile.
Light-molecular-weight hydrocarbons, aldehydes (such as formaldehyde) and organic acids may be formed when hydrocarbon fuels burn at lower temperatures. The oxides of nitrogen are also formed in quantity when temperatures are high, as a consequence of the oxidation of atmospheric nitrogen, and in lower temperature fires where the fuel contains significant nitrogen. When the fuel contains chlorine, hydrogen chloride is formed. Polymeric plastic materials pose particular hazards. These synthetic materials were introduced into building construction and furnishings in the 1950s and thereafter. They combust into particularly hazardous products. Acrolein, formaldehyde and volatile fatty acids are common in smouldering fires of several polymers, including polyethylene and natural cellulose. Cyanide levels increase with temperature when polyurethane or polyacrylonitriles are burned; acrylonitrile, acetonitrile pyridine and benzonitrile occur in quantity above 800 but below 1,000 °C. Polyvinyl chloride has been proposed as a desirable polymer for furnishings because of its self-extinguishing characteristics due to the high chlorine content. Unfortunately, the material produces large quantities of hydrochloric acid and, sometimes, dioxins when fires are prolonged.
Synthetic materials are most dangerous during smouldering conditions, not in conditions of high heat. Concrete retains heat very efficiently and may act as a “sponge” for trapped gases that are then released from the porous material, releasing hydrogen chloride or other toxic fumes long after a fire has been extinguished.
Psychological hazards
A fire-fighter enters a situation that others are fleeing, walking into immediate personal danger greater than in almost any other civilian occupation. There is much that can go wrong in any fire, and the course of a serious fire is often unpredictable. Besides personal security, the fire-fighter must be concerned with the safety of others threatened by the fire. Rescuing victims is an especially stressful activity.
The professional life of a fire-fighter is more than an endless round of anxious waiting punctuated by stressful crises, however. Fire-fighters enjoy the many positive aspects of their work. Few occupations are so respected by the community. Job security is largely assured in urban fire departments once a fire-fighter is hired, and the pay usually compares well with other jobs. Fire-fighters also enjoy a strong sense of team membership and group bonding. These positive aspects of the job offset the stressful aspects and tend to protect the fire-fighter against the emotional consequences of repeated stress.
At the sound of an alarm, a fire-fighter experiences a degree of immediate anxiety because of the inherent unpredictability of the situation he or she is about to encounter. The psychological stress experienced at this moment is as great and perhaps greater than any of the stresses that follow during the course of responding to an alarm. Physiological and biochemical indicators of stress have shown that fire-fighters on duty have sustained psychological stress that reflects subjectively perceived patterns of psychological stress and activity levels at the station.
Health Risks
The acute hazards of firefighting include trauma, thermal injury and smoke inhalation. The chronic health effects that follow recurrent exposure have not been so clear until recently. This uncertainty has led to a patchwork of employment and workers’ compensation board policies. The occupational risks of fire-fighters have received a great deal of attention because of their known exposure to toxic agents. A large body of literature has developed on the mortality experience of fire-fighters. This literature has grown with the addition of several substantial studies in recent years, and a sufficient database is now available to describe certain patterns in the literature.
The critical compensation issue is whether a general presumption of risk can be made for all fire-fighters. This means that one must decide whether all fire-fighters can be assumed to have an elevated risk of a particular disease or injury because of their occupation. To satisfy the usual compensation standard of proof that the occupational cause must be more likely than not responsible for the outcome (giving the benefit of the doubt to the claimant), a general presumption of risk requires a demonstration that the risk associated with occupation must be at least as great as the risk in the general population. This can be demonstrated if the usual measure of risk in epidemiological studies is at least double the expected risk, making allowances for uncertainty in the estimate. Arguments against presumption in the specific, individual case under consideration are called “rebuttal criteria”, because they can be used to question, or rebut, the application of the presumption in an individual case.
There are a number of unusual epidemiological characteristics that influence the interpretation of studies of fire-fighters and their occupational mortality and morbidity. Fire-fighters do not show a strong “healthy worker effect” in most cohort mortality studies. This may suggest an excess mortality from some causes compared to the rest of the healthy, fit workforce. There are two types of healthy worker effect that may conceal excess mortality. One healthy worker effect operates at the time of hire, when new workers are screened for firefighting duty. Because of the strenuous fitness requirements for duty, this effect is very strong and might be expected to have an effect of reducing mortality from cardiovascular disease, especially in the early years following hire, when few deaths would be expected anyway. The second healthy worker effect occurs when workers become unfit following employment due to obvious or subclinical illness and are reassigned to other duties or are lost to follow-up. Their relative high contribution to total risk is lost by undercount. The magnitude of this effect is not known but there is a strong evidence that this effect occurs among fire-fighters. This effect would not be apparent for cancer because, unlike cardiovascular disease, the risk of cancer has little to do with fitness at the time of hire.
Lung Cancer
Lung cancer has been the most difficult cancer site to evaluate in epidemiological studies of fire-fighters. A major issue is whether the large-scale introduction of synthetic polymers into building materials and furnishings after about 1950 increased the risk of cancer among fire-fighters because of exposure to the combustion products. Despite the obvious exposure to carcinogens inhaled in smoke, it has been difficult to document an excess in mortality from lung cancer big enough and consistent enough to be compatible with occupational exposure.
There is evidence that work as a fire-fighter contributes to risk of lung cancer. This is seen mostly among fire-fighters who had the highest exposure and who worked the longest time. The added risk may be superimposed on a greater risk from smoking.
Evidence for an association between firefighting and lung cancer suggests that the association is weak and does not attain the attributable risk required to conclude that a given association is “more likely than not” due to occupation. Certain cases with unusual characteristics may warrant this conclusion, such as cancer in a relatively young non-smoking fire-fighter.
Cancer at Other Sites
Other cancer sites have been shown recently to be more consistently associated with firefighting than lung cancer.
The evidence is strong for an association with genito-urinary cancers, including kidney, ureter and bladder. Except for bladder, these are rather uncommon cancers, and the risk among fire-fighters appears to be high, close to or in excess of a doubled relative risk. One could therefore consider any such cancer to be work-related in a fire-fighter unless there is a convincing reason to suspect otherwise. Among the reasons one might doubt (or rebut) the conclusion in an individual case would be heavy cigarette smoking, prior exposure to occupational carcinogens, schistosomiasis (a parasitic infection—this applies to bladder only), analgesic abuse, cancer chemotherapy and urologic conditions that result in stasis and prolonged residence time of urine in the urinary tract. These are all logical rebuttal criteria.
Cancer of the brain and central nervous system has shown highly variable findings in the extant literature, but this is not surprising since the numbers of cases in all reports are relatively small. It is unlikely that this association will be clarified any time soon. It is therefore reasonable to accept a presumption of risk for fire-fighters on the basis of current evidence.
The increased relative risks for lymphatic and haematopoietic cancers appear to be unusually high. However, the small numbers of these relatively rare cancers make it difficult to evaluate the significance of the association in these studies. Because they are individually rare, epidemiologists group them together in order to make statistical generalizations. The interpretation is even more difficult because grouping these very different cancers together makes little sense medically.
Heart Disease
There is no conclusive evidence for an increased risk of death overall from heart disease. Although a single large study has shown an excess of 11%, and a smaller study confined to ischemic heart disease suggested a significant excess of 52%, most studies cannot conclude that there is a consistently increased population risk. Even if the higher estimates are correct, the relative risk estimates still fall far short of what would be required to make a presumption of risk in the individual case.
There is some evidence, primarily from clinical studies, to suggest a risk of sudden cardiac decompensation and risk of a heart attack with sudden maximal exertion and following exposure to carbon monoxide. This does not seem to translate into an excess risk of fatal heart attacks later in life, but if a fire-fighter did have a heart attack during or within a day after a fire it would be reasonable to call it work-related. Each case must therefore be interpreted with a knowledge of individual characteristics, but the evidence does not suggest a generally elevated risk for all fire-fighters.
Aortic Aneurysm
Few studies have accumulated sufficient deaths among fire-fighters from this cause to achieve statistical significance. Although one study conducted in Toronto in 1993 suggests an association with work as a fire-fighter, it should be considered an unproven hypothesis at present. Should it be ultimately confirmed, the magnitude of risk suggests that it would merit acceptance on a schedule of occupational diseases. Rebuttal criteria would logically include severe atherosclerosis, connective tissue disease and associated vasculitis and a history of thoracic trauma.
Lung Disease
Unusual exposures, such as intense exposure to the fumes of burning plastics, can certainly cause severe lung toxicity and even permanent disability. Ordinary firefighting may be associated with short-term changes similar to asthma, resolving over days. This does not appear to result in an increased lifetime risk of dying from chronic lung disease unless there has been an unusually intense exposure (the risk of dying from the consequences of smoke inhalation) or smoke with unusual characteristics (particularly involving burning polyvinyl chloride (PVC)).
Chronic obstructive pulmonary disease has been extensively studied among fire-fighters. The evidence does not support an association with firefighting, and therefore there can be no presumption. An exception may be in rare cases when a chronic lung disease follows an unusual or severe acute exposure and there is a compatible history of medical complications.
A general presumption of risk is not easily or defensibly justified in situations of weak associations or when diseases are common in the general population. A more productive approach may be to take the claims on a case-by-case basis, examining individual risk factors and overall risk profile. A general presumption of risk is more easily applied to unusual disorders with high relative risks, particularly when they are unique to or characteristic of certain occupations. Table 1 presents a summary of specific recommendations, with criteria that could be used to rebut, or question, presumption in the individual case.
Table 1. Summary of recommendations, with rebuttal criteria and special considerations, for compensation decisions.
|
|
Risk estimate (approximate) |
Recommendations |
Rebuttal criteria |
|
Lung cancer |
150 |
A NP |
- Smoking, previous occupational carcinogens |
|
Cardiovascular disease |
<150 |
NA NP |
+ Acute event at or soon following exposure |
|
Aortic aneurysm |
200 |
A P |
- Atherosclerosis (advanced), connective tissue disorders, history of thoracic trauma |
|
Cancers of genitourinary tract
|
>200
|
A P |
+ Occupational carcinogens - Heavy cigarette smoking, previous occupational carcinogens, schistosomiasis (bladder only), analgesic abuse, cancer chemotherapy (chlornaphazine), conditions resulting in urinary stasis / Coffee consumption, artificial sweeteners |
|
Brain cancer |
200
|
A P |
- Heritable neoplasms (rare), previous vinyl chloride exposure, radiation to head / Trauma, family history, smoking |
|
Cancers of lymphatic and haematopoietic system |
200 |
A
P |
- Ionizing radiation, previous occupational carcinogens (benzene), immunosuppressed state, cancer chemotherapy + Hodgkin’s disease |
|
Cancer of colon and rectum |
A NP NA NP |
A NP |
+ Low risk profile - Familial syndromes, ulcerative colitis / Other occupational exposures |
|
Acute lung disease |
NE NE |
A P |
Circumstances of case |
|
Chronic lung disease (COPD) |
NE NE |
NA NP |
+ Sequela of severe acute exposure, followed by recovery - Smoking, protease deficiency |
A = epidemiological association but not sufficient for presumption of association with firefighting. NA = no consistent epidemiological evidence for association. NE = Not established. P = presumption of association with firefighting; risk exceeds doubling over general population. NP = no presumption; risk does not exceed doubling over general population. + = suggests increased risk due to firefighting. - = suggests increased risk due to exposures unrelated to firefighting. / = no likely contribution to risk.
Injuries
Injuries associated with firefighting are predictable: burns, falls and being struck by falling objects. Mortality from these causes is markedly increased among fire-fighters compared to other workers. Jobs in firefighting have a high risk of burns, especially, include those involving early entry and close-in firefighting, such as holding the nozzle. Burns are also more commonly associated with basement fires, recent injury before the incident and training outside the fire department of present employment. Falls tend to be associated with SCBA use and assignment to truck companies.
Ergonomics
Firefighting is a very strenuous occupation and is often performed under extreme environmental conditions. The demands of firefighting are sporadic and unpredictable, characterized by long periods of waiting between bouts of intense activity.
Fire-fighters maintain their level of exertion at a relatively constant, intense level once active firefighting begins. Any additional burden in the form of an encumbrance by protective equipment or victim rescue, however necessary for protection, reduces performance because fire-fighters are already exerting themselves to the maximum. The use of personal protection equipment has imposed new physiological demands on fire-fighters but has removed others by reducing exposure levels.
A great deal is known about the exertion characteristics of fire-fighters as a result of many careful studies on the ergonomics of firefighting. Fire-fighters adjust their levels of exertion in a characteristic pattern during simulated fire conditions, as reflected by heart rate. Initially, their heart rate increases rapidly to 70 to 80% of maximal within the first minute. As firefighting progresses, they maintain their heart rates at 85 to 100% maximal.
The energy requirements for firefighting are complicated by the severe conditions encountered in many inside fires. The metabolic demands of coping with retained body heat, heat from the fire and fluid loss through sweating add to the demands of physical exertion.
The most demanding activity known is building search and victim rescue by the “lead hand” (first fire-fighter to enter building), resulting in the highest average heart rate of 153 beats/minute and highest rise in rectal temperature of 1.3 °C. Serving as “secondary help” (entering a building at a later time to fight the fire or to conduct additional searches and rescues) is next most demanding, followed by exterior firefighting and serving as crew captain (directing the firefighting, usually at some distance from the fire). Other demanding tasks, in decreasing order of energy costs, are climbing ladders, dragging the fire hose, carrying a travelling ladder and raising a ladder.
During firefighting, core body temperature and heart rate follow a cycle over a period of minutes: they both increase slightly in response to work in preparation for entry, then both increase more as a result of environmental heat exposure and subsequently increase more steeply as a result of high work loads under conditions of heat stress. After 20 to 25 minutes, the usual length of time allowed for interior work by the SCBA used by fire-fighters, the physiological stress remains within limits tolerable by a healthy individual. However, in extended firefighting involving multiple re-entries, there is insufficient time between SCBA air bottle changes to cool off, leading to a cumulative rise in core temperature and an increasing risk of heat stress.
Personal Protection
Fire-fighters exert themselves to maximal levels while fighting fires. Under fire conditions, physical demands are complicated by the metabolic demands of coping with heat and loss of fluids. The combined effect of internally generated heat during work and of external heat from the fire may result in markedly increased body temperatures that climb to unusually high levels in an intense firefighting situation. Half-hour interval breaks to change SCBAs are not enough to arrest this climb in temperature, which can reach dangerous levels in prolonged firefighting. Although essential, personal protection, particularly SCBAs, imposes a considerable additional energy burden on the fire-fighter. The protective clothing also becomes much heavier when it gets wet.
The SCBA is an effective personal protection device that prevents exposure to the products of combustion when used properly. Unfortunately, it is often used only during the “knockdown” phase, when the fire is being actively fought, and not during the “overhaul” phase, when the fire is over but the debris is being examined and embers and smouldering flames are being extinguished.
Fire-fighters tend to judge the level of hazard they face by the intensity of smoke and decide whether to use an SCBA solely on the basis of what they see. This may be very misleading, after the flames are extinguished. While the fire scene may appear to be safe at this stage, it can still be dangerous.
The additional burden or energy cost of using personal protective equipment has been a major area of emphasis in occupational health research on firefighting. This undoubtedly reflects the degree to which firefighting is an extreme case of a matter of general interest, the implications for performance of using personal protection.
Although fire-fighters are obliged to use several forms of personal protection in their work, it is respiratory protection that is most problematic and which has received the most attention. A 20% decrement has been found in work performance imposed by carrying an SCBA, which is a substantial restraint under extreme and dangerous conditions. Investigations have identified several factors of importance in evaluating the physiological demands imposed by respirators in particular, among them the characteristics of the respirator, physiological characteristics of the user and the interactive effects with other personal protection and with environmental conditions.
The fire-fighter’s typical “turnout” gear may weigh 23 kg and imposes a high energy cost. Chemical protective clothing (17 kg), as used for clean-up of spills, is the next most demanding gear to wear, followed by the use of SCBA gear while wearing light clothing, which is only slightly more demanding than wearing light, flame-resistant clothing with a low-resistance mask. The firefighting apparatus has been associated with significantly greater retention of internally generated heat and rise in body temperature.
Fitness
Numerous studies have evaluated the physiological characteristics of fire-fighters, usually in the context of other studies to determine the response to firefighting-related demands.
Studies of the fitness of fire-fighters have shown fairly consistently that most fire-fighters are as or somewhat more fit than the general adult male population. They are not, however, necessarily fit to an athletically trained level. Fitness and health maintenance programmes have been developed for fire-fighters but have not been convincingly evaluated for their effectiveness.
The entrance of female applicants into firefighting has caused a re-evaluation of performance tests and studies comparing the sexes. In studies of trained individuals capable of achieving their potential maximum performance, rather than typical applicants, women demonstrated lower scores on average than men in all performance items, but a subgroup of women performed nearly as well in some tasks. The overall difference in performance was attributed primarily to lower absolute lean body weight, which correlated most strongly and consistently with performance differences. The most difficult tests for women were the stair-climbing exercises.
Musicians
The musician relies on the skilled use of the muscles, nerves and bones (neuromusculoskeletal system). Playing an instrument requires finely controlled repetitive motions and often entails working in unnatural postures for extended periods of practice and performance (figure 1). These demands on the body can result in specific types of health problems. In addition, adverse working conditions, such as excessive sound exposure levels, prolonged periods of performance without rest, and inadequate preparation for new and difficult repertoire or instruments may affect the health of musicians in all age groups and at all levels of performing ability. Recognition of these hazards, accurate diagnosis and early treatment will prevent occupational disabilities that may interfere with, interrupt or end careers.
Figure 1. Orchestra.
Neuromusculoskeletal Problems
Studies from the United States, Australia and Canada suggest that around 60% of musicians will face career-threatening injuries during their working lifetime. Clinical cross-sectional studies have examined the prevalence of muscle-tendon disorders, of peripheral nerve entrapment syndromes and motor control problems. These studies have revealed several common diagnoses, which include various overuse syndromes, including strain of the muscles and connective tissue which control the bending and extending motions in the wrist and fingers. These syndromes result from the repetitive forceful movement of the muscle-tendon units. Other common diagnoses relate to pain in body parts which are involved in prolonged strain from awkward and imbalanced postures while playing musical instruments. Playing the instruments in the groups described below involves putting pressure on the branches of the nerves in the wrist and forearm, the shoulders, arm and neck. Occupational cramp or muscle spasms (focal dystonia) are also common problems which often can affect performers at the pinnacle of their careers.
String instruments: Violin, viola, cello, bass, harp, classical guitar and electric guitar
Health problems in musicians who play string instruments often are caused by the manner in which the musician supports the instrument and the posture assumed while sitting or standing and playing. For example, most violinists and violists support their instruments between the left shoulder and chin. Often the musician’s left shoulder will be elevated and the left chin and jaw will bear down in order to allow the left hand to move over the fingerboard. Elevating a joint and bearing down at the same time leads to a state of static contraction which promotes neck and shoulder pain, temporomandibular joint disorders involving the nerves and muscles of the jaw, and thoracic outlet syndrome, which can include pain or numbness in the neck, shoulder and upper chest area. Prolonged static sitting postures, particularly while assuming a bent posture, promote pain in the large muscle groups which support posture. Static twisting rotation of the spine is often required to play the string bass, harp and classical guitar. Heavy electric guitars are usually supported by a strap over the left neck and shoulder, contributing to pressure on the nerves of the shoulder and upper arm (the brachial plexus) and thus to pain. These problems of posture and support contribute to the development of strain and pressure of the nerves and muscles of the wrist and fingers by promoting their faulty alignment. For example, the left wrist may be used for excessive repetitive bending motions which result in strain of the extensor muscles of the wrist and fingers and the development of carpal tunnel syndrome. Pressure on the nerves of the shoulder and arm (lower trunks of the brachial plexus) may contribute to problems with the elbow, such as a double crush syndrome and ulnar neuropathy.
Keyboard instruments: Piano, harpsichord, organ, synthesizers and electronic keyboards
Playing a keyboard instrument requires assuming a similar posture to that of typing. Often the forward and downward orientation of the head to look at the keys and hands and repetitive upward movement to look at the music causes pain in the nerves and muscles of the neck and back. The shoulders will often be rounded, combined with a forward head poking posture and a shallow breathing pattern. A condition known as thoracic outlet syndrome can develop from chronic compression of the nerves and blood vessels that pass between the muscles in the neck, shoulder and rib cage. In addition, a musician’s tendency to bend the wrists and curl the fingers while keeping the hand/finger joints flat places excessive strain on the wrist and finger muscles in the forearm. Additionally, the repeated use of the thumb kept in a position under the hand strains the thumb muscles which extend and binds the finger extensor muscles across the back of the hand. The high repetitive force needed to play large chords or octaves may strain the capsule of the wrist joint and result in ganglion formation. Prolonged co-contraction of the muscles that turn and move the arms up and down can lead to nerve entrapment syndromes. Muscle spasms and cramps (focal dystonia) are common among this group of instrumentalists, sometimes requiring long periods of neuromuscular retraining to correct movement patterns which can lead to these difficulties.
Wind and brass instruments: Flute, clarinet, oboe, saxophone, bassoon, trumpet, french horn, trombone, tuba and bagpipes
A musician who plays one of these instruments will vary his or her posture according to the need to control airflow since posture will control the area from which diaphragmatic and intercostal breath is drawn. Playing these instruments depends on the way the mouthpiece is held (the embouchure) which is controlled by the facial and pharyngeal muscles. The embouchure controls sound production of vibrating reeds or the mouthpiece. Posture also affects how the musician supports the instrument while sitting or standing and in operating the keys or valves of the instrument that govern the pitch of the note played by the fingers. For example, the traditional French open-holed flute requires sustained adduction and flexion (bending forward) of the left shoulder, sustained abduction (drawing away) of the right shoulder and rotation of the head and neck to the left in slight movement. The left wrist is often held in an extremely bent position while the hand is also extended in order to support the instrument by the curled left index finger and both thumbs, counter balanced by the right little finger. This promotes strain of the forearm muscles and the muscles which permit extension of the fingers and thumbs. The tendency to project the head and neck forward and use shallow breathing increases the chances of developing thoracic outlet syndrome.
Percussion instruments: Drums, timpani, cymbals, xylophone, marimba, tabla and taiko
The use of sticks, mallets and bare hands to strike various percussion instruments results in rapid pulling back of the wrists and fingers at impact. The impulse vibration caused by striking the instrument is transmitted up the hand and arm and contributes to repetitive strain injuries of the muscle-tendon units and the peripheral nerves. Biomechanical factors, such as the amount of force used, the repetitive nature of the playing and static load placed on the muscles can add to the injuries. Carpal tunnel syndrome and nodule formation in tendon sheaths are common in this group of musicians.
Hearing Loss
The risk of hearing loss from music exposure depends on the intensity and duration of exposure. It is not uncommon to have exposure levels of 100 dB during a quiet passage of orchestral music, with peak values of 126 dB measured at the shoulder of an instrumentalist in the middle of the orchestra. At the position of the conductor or teacher, levels of 110 dB in an orchestra or band are common. Exposure levels for pop/rock and jazz musicians may be significantly higher, depending on the physical acoustics of the stage or pit, amplification system and placement of speakers or other instruments. The average duration of exposure may be approximately 40 hours per week, but many professional musicians will perform 60 to 80 hours per week on occasion. Hearing loss among musicians is far more common than expected, with approximately 89% of professional musicians who were found to have suffered musculoskeletal injuries also showing an abnormal hearing test result, with a hearing loss in the 3 to 6 KHz region.
Personal ear protection can be used but it must be adapted for each instrument type (Chasin and Chong 1992). By inserting an acoustic attenuator or filter into custom-moulded earplugs, the intensity of higher frequency sounds transmitted by ordinary earplugs is reduced to a flat attenuation as measured at the eardrum, which should be less damaging to the ear. The use of a tuned or adjustable vent in a custom earplug will allow the lower frequencies and some harmonic energy to pass through the earplug unattenuated. Earplugs can be designed to provide a slight amplification to alter perception of the singer’s voice, thus allowing the artist to reduce the risk of vocal strain. Depending on the psycho-acoustical nature of the instrument and surrounding music exposures, substantial reduction in risk for the development of hearing loss can be obtained. Improvement in the perception of the relative intensity of the musician’s own performance may reduce the risk of repetitive strain injuries by a relative reduction of the force of repetitive movements.
There are practical strategies for reducing the exposure of musicians that do not interfere with music production (Chasin and Chong 1995). Loudspeaker enclosures can be elevated above floor level, which results in minimal loss of low-frequency sound energy, while preserving sufficient loudness for the musician to perform at a lower intensity level. Musicians who play high-intensity, highly directional instruments such as trumpets and trombones should be on risers so that the sound passes above the other musicians, thereby lowering its impact. There should be 2 m of unobstructed floor space in front of the orchestra. Small stringed instruments should always have at least 2 m of unobstructed space above them.
Prevention and Management of Back Pain in Nurses
Epidemiology
The significance of back pain among instances of disease in developed industrial societies is currently on the rise. According to data provided by the National Center for Health Statistics in the United States, chronic diseases of the back and of the vertebral column make up the dominant group among disorders affecting employable individuals under 45 in the US population. Countries such as Sweden, which have at their disposal traditionally good occupational accident statistics, show that musculoskeletal injuries occur twice as frequently in the health services as in all other fields (Lagerlöf and Broberg 1989).
In an analysis of accident frequency in a 450-bed hospital in the United States, Kaplan and Deyo (1988) were able to demonstrate an 8 to 9% yearly incidence of injury to lumbar vertebrae in nurses, leading on average to 4.7 days of absence from work. Thus of all employee groups in hospitals, nurses were the one most afflicted by this condition.
As is clear from a survey of studies done in the last 20 years (Hofmann and Stössel 1995), this disorder has become the object of intensive epidemiological research. All the same, such research—particularly when it aims at furnishing internationally comparable results—is subject to a variety of methodological difficulties. Sometimes all employee categories in the hospital are investigated, sometimes simply nurses. Some studies have suggested that it would make sense to differentiate, within the group “nurses”, between registered nurses and nursing aides. Since nurses are predominantly women (about 80% in Germany), and since reported incidence and prevalence rates regarding this disorder do not differ significantly for male nurses, gender-related differentiation would seem to be of less importance to epidemiological analyses.
More important is the question of what investigative tools should be used to research back pain conditions and their gradations. Along with the interpretation of accident, compensation and treatment statistics, one frequently finds, in the international literature, a retrospectively applied standardized questionnaire, to be filled out by the person tested. Other investigative approaches operate with clinical investigative procedures such as orthopaedic function studies or radiological screening procedures. Finally, the more recent investigative approaches also use biomechanical modelling and direct or video-taped observation to study the pathophysiology of work performance, particularly as it involves the lumbo-sacral area (see Hagberg et al. 1993 and 1995).
An epidemiological determination of the extent of the problem based on self-reported incidence and prevalence rates, however, poses difficulties as well. Cultural-anthropological studies and comparisons of health systems have shown that perceptions of pain differ not only between members of different societies but also within societies (Payer 1988). Also, there is the difficulty of objectively grading the intensity of pain, a subjective experience. Finally, the prevailing perception among nurses that “back pain goes with the job” leads to under-reporting.
International comparisons based on analyses of governmental statistics on occupational disorders are unreliable for scientific evaluation of this disorder because of variations in the laws and regulations related to occupational disorders among different countries. Further, within a single country, there is the truism that such data are only as reliable as the reports upon which they are based.
In summary, many studies have determined that 60 to 80% of all nursing staff (averaging 30 to 40 years in age) have had at least one episode of back pain during their working lives. The reported incidence rates usually do not exceed 10%. When classifying back pain, it has been helpful to follow the suggestion of Nachemson and Anderson (1982) to distinguish between back pain and back pain with sciatica. In an as-yet unpublished study a subjective complaint of sciatica was found to be useful in classifying the results of subsequent CAT scans (computer assisted tomography) and magnetic resonance imaging (MRI).
Economic Costs
Estimates of the economic costs differ greatly, depending, in part, on the possibilities and conditions of diagnosis, treatment and compensation available at the particular time and/or place. Thus, in the US for 1976, Snook (1988b) estimated that the costs of back pain totalled US$14 billion, while a total cost of US$25 billion was calculated for 1983. The calculations of Holbrook et al. (1984), which estimated 1984 costs to total just under US$16 billion, appear to be most reliable. In the United Kingdom, costs were estimated to have risen by US$2 billion between 1987 and 1989 according to Ernst and Fialka (1994). Estimates of direct and indirect costs for 1990 reported by Cats-Baril and Frymoyer (1991) indicate that the costs of back pain have continued to increase. In 1988 the US Bureau of National Affairs reported that chronic back pain generated costs of US$80,000 per chronic case per year.
In Germany, the two largest workers’ accident insurance funds (Berufsgenossenschaften) developed statistics showing that, in 1987, about 15 million work days were lost because of back pain. This corresponds to roughly one-third of all missed work days annually. These losses appear to be increasing at a current average cost of DM 800 per lost day.
It may therefore be said, independently of national differences and vocational groups, that back disorders and their treatment represent not simply a human and a medical problem, but also an enormous economic burden. Accordingly, it seems advisable to pay special attention to the prevention of these disorders in particularly burdened vocational groups such as nursing.
In principle one should differentiate, in research concerning the causes of work-related disorders of the lower back in nurses, between those attributed to a particular incident or accident and those whose genesis lacks such specificity. Both may give rise to chronic back pain if not properly treated. Reflecting their presumed medical knowledge, nurses are much more prone to use self-medication and self-treatment, without consulting a physician, than other groups in the working population. This is not always a disadvantage, since many physicians either do not know how to treat back problems or give them short shrift, simply prescribing sedatives and advising heat applications to the area. The latter reflects the oft-repeated truism that “backaches come with the job”, or the tendency to regard workers with chronic back complaints as malingerers.
Detailed analyses of work accident occurrences in the area of spinal disorders have only just begun to be made (see Hagberg et al. 1995). This is also true of the analysis of so-called near-accidents, which can provide a particular sort of information concerning the precursor conditions of a given work accident.
The cause of low back disorders has been attributed by the majority of the studies to the physical demands of the work of nursing, i.e., lifting, supporting and moving of patients and handling heavy and/or bulky equipment and materials, often without ergonomic aids or the help of additional personnel. These activities are often conducted in awkward body positions, where footing is uncertain, and when, out of wilfulness or dementia, the nurse’s efforts are resisted by the patient. Trying to keep a patient from falling often results in injury to the nurse or the attendant. Current research, however, is characterized by a strong tendency to speak in terms of multicausality, whereby both the biomechanical basis of demands made upon the body and the anatomical preconditions are discussed.
In addition to faulty biomechanics, injury in such situations can be pre-conditioned by fatigue, muscular weakness (especially of the abdominals, back extensors and quadriceps), diminished flexibility of joints and ligaments and various forms of arthritis. Excessive psychosocial stress can contribute in two ways: (1) prolonged unconscious muscular tension and spasm leading to muscular fatigue and proneness to injury, and (2) irritation and impatience which prompts injudicious attempts to work hurriedly and without waiting for assistance. Enhanced ability to cope with stress and the availability of social support in the workplace are helpful (Theorell 1989; Bongers et al. 1992) when work-related stressors cannot be eliminated or controlled.
Diagnosis
Certain risk situations and dispositions may be added to the risk factors deriving from the biomechanics of the forces acting on the spine and from the anatomy of the support and movement apparatus, ones which are attributable to the work environment. Even though current research is not clear on this point, there is still some indication that the increased and recurrent incidence of psychosocial stress factors in nursing work has the capacity to reduce the threshold of sensitivity to physically burdensome activities, thus contributing to an increased level of vulnerability. In any case, whether such stress factors exist appears to be less decisive in this connection than how nursing staff manages them in a demanding situation and whether they can count on social support in the workplace (Theorell 1989; Bongers et al. 1992).
The proper diagnosis of low back pain requires a complete medical and a detailed occupational history including accidents resulting in injury or near-misses and prior episodes of back pain. The physical examination should include evaluation of gait and posture, palpation for areas of tenderness and evaluation of muscle strength, range of motion and joint flexibility. Complaints of weakness in the leg, areas of numbness and pain that radiate below the knee are indications for neurological examination to seek evidence of spinal cord and/or peripheral nerve involvement. Psychosocial problems may be disclosed through judicious probing of emotional status, attitudes and pain tolerance.
Radiological studies and scans are rarely helpful since, in the vast majority of cases, the problem lies in the muscles and ligaments rather than the bony structures. In fact, bony abnormalities are found in many individuals who have never had back pain; ascribing the back pain to such radiological findings as disc space narrowing or spondylosis may lead to needlessly heroic treatment. Myelography should not be undertaken unless spinal surgery is contemplated.
Clinical laboratory tests are useful in assessing general medical status and may be helpful in disclosing systemic diseases such as arthritis.
Treatment
Various modes of management are indicated depending on the nature of the disorder. Besides ergonomic interventions to enable the return of injured workers to the workplace, surgical, invasive-radiological, pharmacological, physical, physiotherapeutic and also psychotherapeutic management approaches may be necessary—sometimes in combination (Hofmann et al. 1994). Again, however, the vast majority of cases resolve regardless of the therapy offered. Treatment is discussed further in the Case Study: Treatment of Back Pain.
Prevention in the Work Environment
Primary prevention of back pain in the workplace involves the application of ergonomic principles and the use of technical aids, coupled with physical conditioning and training of the workers.
Despite the reservations frequently held by nursing staff regarding the use of technical aids for the lifting, positioning and moving of patients, the importance of ergonomic approaches to prevention is increasing (see Estryn-Béhar, Kaminski and Peigné 1990; Hofmann et al. 1994).
In addition to the major systems (permanently installed ceiling lifters, mobile floor lifters), a series of small and simple systems has been introduced noticeably into nursing practice (turntables, walking girdles, lifting cushions, slide boards, bed ladders, anti-slide mats and so on). When using these aids it is important that their actual use fits in well with the care concept of the particular area of nursing in which they are used. Wherever the use of such lifting aids stands in contradiction to the care concept practised, acceptance of such technical lifting aids by nursing staff tends to be low.
Even where technical aids are employed, training in techniques of lifting, carrying and supporting are essential. Lidström and Zachrisson (1973) describe a Swedish “Back School” in which physiotherapists trained in communication conduct classes explaining the structure of the spine and its muscles, how they work in different positions and movements and what can go wrong with them, and demonstrating appropriate lifting and handling techniques that will prevent injury. Klaber Moffet et al. (1986) describe the success of a similar programme in the UK. Such training in lifting and carrying is particularly important where, for one reason or another, use of technical aids is not possible. Numerous studies have shown that training in such techniques must constantly be reviewed; knowledge gained through instruction is frequently “unlearned” in practice.
Unfortunately, the physical demands presented by patients’ size, weight, illness and positioning are not always amenable to nurses’ control and they are not always able to modify the physical environment and the way their duties are structured. Accordingly, it is important for institutional managers and nursing supervisors to be included in the educational programme so that, when making decisions about work environments, equipment and job assignments, factors making for “back friendly” working conditions can be considered. At the same time, deployment of staff, with particular reference to nurse-patient ratios and the availability of “helping hands”, must be appropriate to the nurses’ well-being as well as consistent with the care concept, as hospitals in the Scandinavian countries seem to have managed to do in exemplary fashion. This is becoming ever more important where fiscal constraints dictate staff reductions and cut-backs in equipment procurement and maintenance.
Recently developed holistic concepts, which see such training not simply as instruction in bedside lifting and carrying techniques but rather as movement programmes for both nurses and patients, could take the lead in future developments in this area. Approaches to “participatory ergonomics” and programmes of health advancement in hospitals (understood as organizational development) must also be more intensively discussed and researched as future strategies (see article “Hospital ergonomics: A review”).
Since psychosocial stress factors also exercise a moderating function in the perception and mastering of the physical demands made by work, prevention programmes should also ensure that colleagues and superiors work to ensure satisfaction with work, avoid making excessive demands on the mental and physical capacities of workers and provide an appropriate level of social support.
Preventive measures should extend beyond professional life to include work in the home (housekeeping and caring for small children who have to be lifted and carried are particular hazards) as well as in sports and other recreational activities. Individuals with persistent or recurrent back pain, however it is acquired, should be no less diligent in following an appropriate preventive regimen.
Rehabilitation
The key to a rapid recovery is early mobilization and a prompt resumption of activities with the limits of tolerance and comfort. Most patients with acute back injuries recover fully and return to their usual work without incident. Resumption of an unrestricted range of activity should not be undertaken until exercises have fully restored muscle strength and flexibility and banished the fear and temerity that make for recurrent injury. Many individuals exhibit a tendency to recurrences and chronicity; for these, physiotherapy coupled with exercise and control of psychosocial factors will often be helpful. It is important that they return to some form of work as quickly as possible. Temporary elimination of more strenuous tasks and limitation of hours with a graduated return to unrestricted activity will promote a more complete recovery in these cases.
Fitness for work
The professional literature attributes only a very limited prognostic value to screening done before employees start work (US Preventive Services Task Force 1989). Ethical considerations and laws such as the Americans with Disabilities Act mitigate against pre-employment screening. It is generally agreed that pre-employment back x rays have no value, particularly when one considers their cost and the needless exposure to radiation. Newly-hired nurses and other health workers and those returning from an episode of disability due to back pain should be evaluated to detect any predisposition to this problem and provided with access to educational and physical conditioning programmes that will prevent it.
Conclusion
The social and economic impact of back pain, a problem particularly prevalent among nurses, can be minimized by the application of ergonomic principles and technology in the organization of their work and its environment, by physical conditioning that enhances the strength and flexibility of the postural muscles, by education and training in the performance of problematic activities and, when episodes of back pain do occur, by treatment that emphasizes a minimum of medical intervention and a prompt return to activity.
More...
Motor Vehicle Fueling and Servicing Operations
Petroleum-based fuels and lubricants are sold directly to consumers at full-service and self-service (with or without repair bays) service stations, car washes, automotive service centres, motor vehicle agencies, truck stops, repair garages, automotive parts stores and convenience stores. Service station attendants, mechanics and other employees who fuel, lubricate and service motor vehicles should be aware of the physical and chemical hazards of the petroleum fuels, lubricants, additives and waste products they come into contact with and follow appropriate safe work procedures and personal protection measures. The same physical and chemical hazards and exposures are present at commercial facilities, such as those operated by motor truck fleets, automobile rental agencies and bus companies for fuelling and servicing their own vehicles.
Because they are the facilities where motor fuels are delivered direct to the user’s vehicle, service stations, particularly those where drivers fuel their own vehicles, are where employees and the general public are most likely to come into direct contact with hazardous petroleum products. Other than those drivers who change their own oil and lubricate their own vehicles, the likelihood of contact with lubricants or used oil by motorists, except for incidental contact when checking fluid levels, is very small.
Service Station Operations
Fuel island area and dispensing system
Employees should be aware of the potential fire, safety and health hazards of gasoline, kerosene, diesel and other fuels dispensed at service stations. They should also be aware of suitable precautions. These include: safe dispensing of fuels into vehicles and containers, clean-up and disposal of spills, fighting incipient fires and draining fuels safely. Service stations should provide fuel-dispenser pumps which operate only when the fuel-hose nozzles are removed from the dispensers’ brackets and the switches are manually or automatically activated. Fuel-dispensing devices should be mounted on islands or protected against collision damage by barriers or curbs. Dispensing equipment, hoses and nozzles should be inspected regularly for leaks, damage and malfunctions. Safety features may be installed on fuel dispensers such as emergency breakaway devices on hoses, which retain liquid on each side of the break point, and impact valves with fusible links at the base of dispensers, which close automatically in event of severe impact or fire.
Government regulations and company policies may require that signs be posted in dispensing areas similar to the following signs, which are required in the United States:
- “No Smoking—Shut off engine”
- “WARNING: It is unlawful and dangerous to dispense gasoline into unapproved containers”
- “Federal Law prohibits the introduction of any gasoline containing lead or phosphorus into any motor vehicle labelled UNLEADED GASOLINE ONLY”
- “UNLEADED GASOLINE”, posted at unleaded gasoline dispensers and “CONTAINS LEAD ANTIKNOCK COMPOUNDS”, posted at leaded gasoline dispensers.
Fuelling vehicles
Service station employees should know where the fuel dispenser pump emergency shut-off switches are located and how to activate them, and should be aware of potential hazards and procedures for safely dispensing fuel into vehicles, such as the following:
- Vehicle engines should be shut off and smoking prohibited while fuelling to reduce the hazards of accidental vehicle movement, spills and fuel vapour ignition.
- When fuel is dispensed, the nozzle should be inserted into the vehicle’s fill pipe and contact between the nozzle and the fill pipe maintained to provide for an electric bond until the delivery has been completed. Nozzles should not be blocked open with fuel caps or other objects. Where allowed, approved latches should be used to hold open automatic nozzles.
- Vehicles such as cement mixers and recreation vehicles with auxiliary internal combustion engines should not be fuelled until both the vehicle’s engines and auxiliary engines are shut off. Care should be taken when fuelling recreational or other vehicles equipped with gas-fired stoves, refrigerators and water heaters to ensure that fuel vapours are not ignited by pilot lights. Employees should not fuel trucks while standing on the side rail, truck bed or fuel tank.
- Fuel tanks on motorcycles, motor bicycles, fork-lift trucks and similar vehicles should not be filled while the engine is running or when anyone is seated on the vehicle. The tanks should be filled at a slow rate to prevent fuel spills that could run onto hot engines and start fires.
- After fuelling, hose nozzles should be promptly replaced on the dispensers, pumps turned off and caps replaced on fill pipes or containers.
Filling portable fuel containers
Service stations should establish procedures such as the following for safely dispensing fuel into portable containers:
- Where required by government regulation or company policies, fuel should be dispensed only into approved, properly identified and labelled portable containers, with or without dispensing spouts, nozzles or hoses and equipped with vents and screw tops or self-closing gravity, spring action or combination fusible link covers designed to provide pressure relief.
- Containers should be placed on the ground and filled slowly to avoid splash filling and overfills and to provide for grounding (earthing). Containers should not be filled while in a vehicle or in the bed of a truck, particularly one with a plastic liner, as proper grounding cannot be achieved. Bonding wires and clamps should be provided and used, or contact should be maintained between dispenser nozzles and containers to provide a bond while filling, and between container spouts or funnels and tanks during refuelling from containers.
- When pouring fuel from containers which do not have built-in spouts, funnels should be used to minimize spillage and avoid splash filling.
- Portable containers which contain fuel or vapours should be properly stored in approved storage cabinets or rooms away from sources of heat and ignition.
Storage tanks, fill pipes, fill caps and vents
Service station underground and aboveground storage-tank gauge and fill-caps should be kept closed except when filling and gauging to minimize release of fuel vapours. When tank-gauge openings are located inside buildings, spring-loaded check valves or similar devices should be provided to protect each of the openings against fluid overflow and possible vapour release. Storage-tank vents should be located in accordance with government regulations and company policy. Where venting to open air is permitted, vent-pipe openings from both underground and aboveground storage tanks should be located at a high level so that flammable vapours are directed away from potential sources of ignition and will not enter windows or air intakes or doors or become trapped under eaves or overhangs.
Improper mixing of different products during deliveries may be caused by lack of identification or improper colour coding or markings on storage tanks. Storage-tank covers, fill pipes, caps and fill-box rims or pads should be properly identified as to products and grades so as to reduce the potential of a delivery into the wrong tank. Identification symbols and colour coding should conform to government regulations, company policies or industry standards, such as the American Petroleum Institute’s (API) Recommended Practice 1637, Using the API Color Symbol System to Mark Equipment and Vehicles for Product Identification at Service Stations and Distribution Terminals. A chart indicating the symbols or colour codes in use should be available at the service station during deliveries.
Delivery of fuel to service stations
Service stations should establish and implement procedures such as the following, for the safe delivery of fuel into aboveground and underground service station storage tanks:
Prior to delivery
- Vehicles and other objects should be moved from the area where the delivery tank truck and delivery hoses will be located.
- Delivery tank trucks should be positioned away from traffic areas, and vehicles should be restricted from driving near the unloading area or over hoses by the use of traffic cones or barriers.
- Receiving storage tanks should be gauged prior to delivery to determine if there is sufficient capacity, and checked to see if any water is in the tank.
- Drivers should assure that fuel is delivered into the correct tanks, that gauge caps are replaced before starting delivery and that all tank openings not being used for delivery are covered.
- Where required by company policies or government regulation, the tank truck vapour recovery system should be connected to the receiving storage tank prior to starting delivery.
During delivery
- Drivers should monitor the area near the receiving tank’s vents for potential ignition sources and check that the vents operate properly during delivery.
- Drivers should remain where they can observe the delivery and be able to stop delivery or take other appropriate action in event of an emergency, such as ejection of liquid from vents or if an overfill device or tank vent alarm activates.
After delivery
- Storage tanks may be gauged after delivery to verify that specific tanks have received the correct products and the proper amount of products as indicated on the delivery ticket or record. Samples may be taken from the tanks after delivery for quality-control purposes.
- After delivery, spill containment devices should be drained if necessary and the correct fill and gauge caps and storage tank covers replaced on the proper tanks.
Other Service Station Functions
Storage of flammable and combustible liquids
Government regulations and company policies may control the storage, handling and dispensing of flammable and combustible liquids and automotive chemicals such as paints, starter fluids, antifreeze, battery acids, window washer fluids, solvents and lubricants in service stations. Service stations should store aerosols and flammable liquids in closed containers in approved, well-ventilated areas, away from sources of heat or ignition, in appropriate flammable liquid rooms, lockers or cabinets, or in separate, outside buildings.
Electrical safety and lighting
Service station employees should be familiar with electrical safety fundamentals applicable to service stations, such as the following:
- Lighting and electrical installations, equipment and fixtures of the proper electrical classification should be provided and maintained in accordance with codes and regulations and should not be replaced by equipment of lesser classification.
- Electric tools, water coolers, ice machines, refrigerators and similar electrical equipment should be properly grounded (earthed). Portable lights should be protected against breakage to minimize the chance that a spark might ignite flammable vapours in case bulbs break.
Adequate illumination should be provided at appropriate locations in service stations to reduce the potential for accidents and injuries. Government regulations, company policies or voluntary standards may be used to determine appropriate illumination levels. See table 1.
Table 1. Illumination levels for service station areas.
|
Service station area |
Suggested foot candles |
|
Active traffic areas |
20 |
|
Storage areas and stockrooms |
10–20 |
|
Washrooms and waiting areas |
30 |
|
Dispenser islands, work benches and cashier areas |
50 |
|
Service, repair, lubrication and washing areas |
100 |
|
Offices |
100–150 |
Source: ANSI 1967.
Lockout/tagout
Service stations should establish and implement lockout/tagout procedures to prevent the release of potentially hazardous energy while performing maintenance, repair and service work on electrical, mechanical, hydraulic and pneumatic powered tools, equipment, machinery and systems such as lifts, hoists and jacks, lubrication equipment, fuel-dispenser pumps and compressors. Safe work procedures to prevent the accidental start-up of vehicle engines during servicing or repair should include disconnecting the battery or removing the key from the ignition.
Service station fluids
Fluid and coolant levels
Before working under a hood (bonnet), employees should assure that it will stay open by testing the tension or using a rod or brace. Employees should exercise caution when checking vehicle engine fluids to avoid burns from exhaust manifolds and to prevent contact between dipsticks and electrical terminals or wires; care is also necessary when checking transmission fluid levels (since the engine must be running). Employees should follow safe work procedures when opening radiators, such as allowing pressurized radiators to cool and covering radiator caps with a heavy cloth when opening, using PPE and standing with face turned away from radiators so as to not inhale any escaping steam or vapours.
Antifreeze and window washer fluids
Employees servicing vehicles should be aware of the hazards of both glycol and alcohol antifreezes and window washer fluid concentrates and how to safely handle them. This includes precautions such as storing alcohol-based products in tightly closed drums or packaged containers, in separate rooms or lockers, away from all heating equipment, and providing containment to prevent contamination of drains and ground in the event of a spill or leak of glycol-type antifreeze. Antifreeze or washer fluid should be dispensed from upright drums by using tightly connected hand pumps equipped with drip returns, rather than by using faucets or valves on horizontal drums, which may leak or be knocked open or broken off, causing spills. Air pressure should not be used to pump antifreeze or washer fluid concentrates from drums. Empty portable antifreeze and washer fluid concentrate containers should be completely drained prior to disposal, and applicable regulations governing the disposal of glycol antifreeze solutions should be followed.
Lubrication
Service stations should ensure that employees are aware of the characteristics and uses of the different fuels, oils, lubricants, greases, automotive fluids and chemicals available in the facility and their correct selection and application. The proper tools should be used to remove crankcase, transmission and differential drains, test plugs and oil filters so as to not damage vehicles or equipment. Pipe wrenches, extenders and chisels should be used only by employees who know how to safely remove frozen or rusted plugs. Because of the potential hazards involved, high-pressure lubricating equipment should not be started until the nozzles are set firmly against grease fittings. If testing is to be done prior to use, the nozzle should be aimed into an empty drum or similar receptacle, and not into a hand-held rag or cloth.
Lift operations
Employees working in and around vehicle service areas should be aware of unsafe conditions and follow safe work practices such as not standing in front of vehicles while they are being driven into service bays, over lubrification pits or onto lifts, or when vehicles are being lifted.
- Vehicles should be properly aligned on two-rail, free-wheel or frame-contact lifts, since an off-centre position may cause a vehicle to fall.
- Lifts should not be raised until occupants have left the vehicles and a check of overhead clearance has been made.
- Once the vehicle is in position, the emergency stop device should be set so the lift will not fall in the event of a pressure drop. If a lift is in a position where the emergency stop device cannot be engaged, blocks or safety stands should be placed under the lift or vehicle.
- A hydraulic lift may be equipped with a low-oil control valve, which prevents operation if the oil in the supply tank falls below a minimum level, since the lift can drop accidentally under those conditions.
When wheel-bearing lubrication, brake repair, tyre changing or other services are performed on free-wheel or frame-contact lifts, vehicles should be raised slightly above the floor to allow employees to work from a squatting position, to reduce the possibility of back strain. After vehicles are raised, the wheels should be blocked to prevent rolling, and safety stands should be placed underneath for support in case of jack or lift failure. When removing wheels from vehicles on drive-on lifts, the vehicles should be blocked securely to prevent rolling. If jacks or stands are used to lift and support vehicles, they should be of the proper capacity, placed at appropriate lift points on the vehicles and checked for stability.
Servicing tyres
Employees should be aware of how to safely check pressures and inflate tyres; tyres should be inspected for excessive wear, maximum tyre pressures should not be exceeded, and the worker should stand or kneel to the side and turn the face when inflating tyres. Employees should be aware of hazards and follow safe work practices when servicing wheels with multi-piece and single-piece rims and lock-ring-rim wheels on trucks and trailers. When repairing tyres with flammable or toxic patching compounds or liquids, precautions such as controlling ignition sources, using PPE and providing adequate ventilation, should be observed.
Parts cleaning
Service station employees should be aware of the fire and health hazards of using gasoline or low-flashpoint solvents to clean parts and should follow safe practices such as using approved solvents with a flashpoint above 60ºC. Parts washers should have a protective cover that is kept closed when the washer is not in use; when the washer is open, there should be a hold-open device such as fusible links, which allows the cover to close automatically in case of fire.
Employees should take precautions so that gasoline or other flammable liquids do not contaminate the cleaning solvent and lower its flashpoint to create a fire hazard. Contaminated cleaning solvent should be removed and placed in approved containers for proper disposal or recycling. Employees who clean parts and equipment using cleaning solvents should avoid skin and eye contact and use appropriate PPE. Solvents should not be used for hand-washing and other personal hygiene.
Compressed air
Safe work practices should be established by service stations for the operation of air compressors and the use of compressed air. The air hoses should be used only for inflating tyres and for lubrication, maintenance and auxiliary services. Employees should be aware of the hazards of pressurizing fuel tanks, air horns, water tanks and other non-air pressure containers. Compressed air should not be used for cleaning or to blow residue from vehicle brake systems, since many brake linings, especially on older model vehicles, contain asbestos. Safer methods such as cleaning with vacuums or liquid solutions should be used.
Storage battery service and handling
Service stations should establish procedures to ensure that storage, handling and disposal of batteries and battery electrolyte fluids follow government regulations and company policies. Employees should be aware of the hazards of electrical short circuits when charging, removing, installing or handling batteries; disconnect the ground (negative) cable first before removing batteries; and reconnect the ground (negative) cable last when installing batteries. When removing and replacing batteries, a carrier may be used to facilitate lifting and to avoid touching the battery.
Employees should be aware of safe practices such as the following for handling battery solution:
- Containers of electrolyte solution should be stored at temperature ranges between 16 and
32ºC in safe areas where they cannot overturn. Any electrolyte solution spilled on the batteries or in the filling area should be flushed with water. Baking soda (sodium bicarbonate) may be used on spills, since it is an effective neutralizer for battery electrolyte solution.
- New batteries should be placed on the floor or work table when being filled with electrolyte solution, and the caps should be replaced prior to installation. New batteries should not be filled when they are inside vehicles.
- Face shields and chemical goggles, aprons and gloves may be used to minimize exposure to battery solution. Battery solution should be handled and dispensed where a supply of potable water or eye wash fluid is available, in case the battery solution spills or contacts an employee’s skin or eyes. Do not use neutralizing solutions on skin or eyes.
- When servicing batteries, corrosive particles which accumulate around the terminals should be brushed away, washed with clean water, neutralized with baking soda or other similar agents and prevented from contacting eyes or clothing.
Employees should check fluid levels in batteries prior to charging and periodically check them during charging to determine whether batteries are overheating. Chargers should be turned off before disconnecting cables from batteries, to avoid creating sparks which may ignite hydrogen gas generated during the charge. When “quick charging” batteries are installed in vehicles, the vehicles should be moved away from the fuel-dispensing islands, and the battery ground (negative) cables should be disconnected before connecting the charger units. If the batteries are located within passenger compartments or under vehicle floorboards, they should be removed before charging.
Employees should be familiar with the hazards and safe procedures to “jump start” vehicles that have dead batteries, in order to avoid electrical system damage or injury from exploding batteries if the jumper cables are hooked up incorrectly. Employees should never jump start or charge frozen batteries.
Driving vehicles and towing
Employees should be trained, qualified and have proper motor vehicle operator’s licences to drive customer or company vehicles, service trucks or towing equipment either on or off the premises. All vehicles should be operated in compliance with government regulations and company policies. Operators should check the vehicle’s brakes immediately, and vehicles with faulty brakes should not be driven. Employees operating tow trucks should be familiar with safe operating procedures, such as operating the hoist, checking the transmission and frame of the vehicle to be towed and not exceeding the tow truck’s maximum lifting capacity.
Confined spaces in service stations
Service station employees should be aware of the hazards associated with entry into confined spaces such as aboveground and underground tanks, sumps, pump pits, waste containment tanks, septic tanks and environmental collection wells. Unauthorized entry should not be allowed, and confined-space entry permit procedures should be established that apply to both employee and contractor entrants.
Emergency procedures
Service stations should develop emergency procedures, and employees should know how to sound the alarms, how to notify authorities of emergencies when and how to evacuate and what appropriate response actions should be taken (such as shutting off emergency switches in the event of spills or fires in the dispensing pump areas). Service stations may establish security programmes to familiarize employees with robbery and violence prevention, depending on the service station’s location, hours of operation and potential threats.
Service Station Health and Safety
Fire protection
Gasoline vapours are heavier than air and may travel long distances to reach sources of ignition when released during fuel filling, spills, overflows or repairs. Proper ventilation should be provided in enclosed areas to allow for dissipation of gasoline vapours. Fires may occur from spills and overflows when fuelling or servicing vehicles or delivering product into service station tanks, particularly if smoking is not restricted or if vehicle engines remain running during fuelling. To avoid fires, vehicles should be pushed away from spill areas or the spilled gasoline should be cleaned from under or around vehicles before starting their engines. Vehicles should not be permitted to enter or drive through spills.
Employees should be aware of other causes of fires in service stations, such as improper handling, transfer and storage of flammable and combustible liquids, accidental releases during fuel system repairs, electrostatic discharge when changing filters on gasoline dispensers and the use of improper or unprotected work lights. Draining gasoline from vehicle fuel tanks could be very hazardous due to the potential for release of fuel and vapours, especially in enclosed service areas when sources of ignition may be present.
Hot-work permits should be issued when work other than vehicle repair and servicing is performed which introduces sources of ignition in areas where flammable vapours may be present. Employees should be aware that carburettor priming should not be attempted while vehicle engines are running or being turned over with their starters, since flashbacks could ignite the fuel vapours. Employees should follow safe procedures, such as using starter fluid and not gasoline for priming carburettors and using clamps to hold the chokes open while attempting to start the engine.
Although government regulations or company policies may require the installation of fixed fire-protection systems, fire extinguishers are usually the primary means of fire protection in service stations. Service stations should provide fire extinguishers of the proper classification for the expected hazards. Fire extinguishers and fixed fire protection systems should be regularly inspected, maintained and serviced, and employees should know when, where and how to use the fire extinguishers and how to activate the fixed systems.
Service stations should install fuel-dispenser emergency shut-down controls at clearly identified and accessible locations and ensure that employees know the purpose, location and operation of these controls. To prevent spontaneous combustion, oily rags should be kept in covered metal containers until they are recycled or discarded.
Safety
Employee injuries at service stations may result from improper use of tools, equipment and ladders; not wearing PPE; falling or tripping; working in awkward positions; and lifting or carrying cases of materials incorrectly. Injuries and accidents may also occur from not following safe practices when working on hot radiators, transmissions, engines and exhaust systems, servicing tyres and batteries, and working with lifts, jacks, electrical equipment and machinery; from robbery and assault; and from improper use of or exposure to automotive cleaners, solvents and chemicals.
Service stations should develop and implement programmes to prevent accidents and incidents which can be attributed to problems associated with service station physical conditions, such as poor maintenance, storage and housekeeping practices. Other factors contributing toward accidents in service stations include employees’ lack of attention, training or skills, which may result in the improper use of equipment, tools, automotive parts, supplies and maintenance materials. Figure 1 provides a safety checklist.
Figure 1. Service station safety and health checklist.
Robberies are a major safety hazard in service stations. Appropriate precautions and training are discussed in the accompanying box and elsewhere in this Encyclopaedia.
Health
Employees should be aware of health hazards associated with working in service stations, such as the following:
Carbon monoxide. Internal combustion engine exhaust gases contain carbon monoxide, a highly toxic, odourless and colourless gas. Employees should be aware of the dangers of exposure to carbon monoxide, particularly when vehicles are inside service bays, garages or car washes with their engines running. Vehicle exhaust gases should be piped outside through flexible hoses, and ventilation should be provided to assure an adequate supply of fresh air. Fuel oil appliances and heaters should be checked to assure that carbon monoxide is not vented to inside areas.
Toxicity of petroleum fuels. Employees who come in contact with gasoline, diesel fuel, heating oil or kerosene should be aware of the potential hazards of exposure and know how to handle these fuels safely. Inhaling sufficient concentrations of petroleum fuel vapours for extended periods of time may result in mild intoxication, anaesthesia or more serious conditions. Short exposure to high concentrations will cause dizziness, headaches and nausea, and irritate the eyes, nose and throat. Gasoline, solvents or fuel oils should never be siphoned from containers or tanks by mouth, since the toxicity of low viscosity liquid hydrocarbons aspired directly into the lungs is 200 times greater than if they are ingested. Aspiration into the lungs may cause pneumonia with extensive pulmonary oedema and haemorrhage, leading to serious injury or death. Vomiting should not be induced. Immediate medical assistance should be sought.
Benzene. Service station employees should be aware of the potential hazards of benzene, which is found in gasoline, and avoid inhaling gasoline vapours. Although gasoline contains benzene, low-level exposure to gasoline vapours is unlikely to cause cancer. Numerous scientific studies have shown that service station employees are not exposed to excessive levels of benzene during the course of their normal work activities; however, there is always the possibility that overexposure could occur.
Dermatitis hazards. Employees who handle and come into contact with petroleum products as part of their jobs should be aware of the hazards of dermatitis and other skin disorders and the personal hygiene and personal protective measures needed to control exposure. If eye contact with gasoline, lubricants or antifreeze occurs, the eyes should be flushed with clean, lukewarm potable water, and medical assistance should be provided.
Lubricants, used motor oil and automotive chemicals. Employees who change oil and other motor vehicle fluids, including antifreeze, should be aware of the hazards and know how to minimize exposure to products such as gasoline in used motor oil, glycol in antifreeze and other contaminants in transmission fluids and gear lubricants by the use of PPE and good hygiene practices. If high-pressure lubricating guns are discharged against an employee’s body, the affected area should be examined immediately to see if petroleum products have penetrated the skin. These injuries cause little pain or bleeding, but involve almost instant separation of the skin tissues and possible deeper damage, which should receive immediate medical attention. The attending physician should be informed of the cause and the product involved in the injury.
Welding. Welding, besides being a fire hazard, can involve exposure to lead pigments from welding on car exteriors, as well as metal fumes and welding gases. Local exhaust ventilation or respiratory protection is needed.
Spray painting and auto body fillers. Spray painting can involve exposure to solvent vapours and pigment particulates (e.g., lead chromate). Auto body fillers often are epoxy or polyester resins and can involve skin and respiratory hazards. Drive-in spray booths for spray painting, local exhaust ventilation and skin and eye protection are recommended while using auto body fillers.
Storage batteries. Batteries contain corrosive electrolyte solutions of sulphuric acid that can cause burns and other injuries to the eyes or skin. Exposure to battery solution should be minimized by the use of PPE, including rubber gloves and eye protection. Employees should immediately flush electrolyte solution from the eyes or skin with clean potable water or eye wash fluid for at least 15 minutes and seek immediate medical attention. Employees should thoroughly wash their hands after servicing batteries and keep their hands away from the face and eyes. Employees should be aware that overcharging batteries can create explosive and toxic quantities of hydrogen gas. Because of the potential harmful effects of exposure to lead, used storage batteries should be properly disposed of or recycled in accordance with government regulations or company policies.
Asbestos. Employees who check and service brakes should be aware of the hazards of asbestos, know how to recognize whether brake shoes contain asbestos and take appropriate protective measures to reduce exposure and contain waste for proper disposal (see figure 2).
Figure 2. Portable enclosure for preventing exposure to asbestos dust from brake drums It is equipped with an enclosed compressed-air gun with a cotton sleeve and is connected to a HEPA vacuum cleaner.
Courtesy of Nilfisk of America, Inc.
Personal protective equipment (PPE)
Injuries to employees may occur from contact with automotive fuels, solvents and chemicals or from chemical burns caused by exposure to battery acids or caustic solutions. Service station employees should be familiar with the need to use and wear PPE such as the following:
- Work shoes with oil- and slip-resistant soles should be worn for general work in service stations, and approved protective-toe safety shoes with oil/slip-resistant soles should be worn where there is a danger of foot injuries due to rolling or falling objects or equipment.
- Safety goggles and respiratory protection should be used for protection against exposures to chemicals, dust or steam, such as when painting or working around batteries and radiators. Industrial safety glasses or face shields with goggles should be worn when the potential exists for exposure to impact materials, such as working with grinders or wire buffers, repairing or mounting tyres, or replacing exhaust systems. Welding glasses should be worn when cutting or welding to prevent flash burns and injuries from particles.
- Impervious gloves, aprons, footwear, face shields and chemical goggles should be worn when handling automotive chemicals and solvents, battery acid and caustic solutions and when cleaning up chemical or fuel spills. Leather work gloves should be worn when handling sharp objects such as broken glass, motor vehicle parts or tyre rims and while emptying trash cans.
- Head protection may be needed when working beneath vehicles in pits or changing overhead signage or lights and in other areas where a potential exists for injury to the head.
- Employees working on vehicles should not wear rings, wristwatches, bracelets or long chains, since the jewellery may contact the vehicle’s moving parts or electrical system and cause injury.
To prevent fires, dermatitis or chemical burns to the skin, clothing that is soaked with gasoline, antifreeze or oil should be immediately removed in an area or room with good ventilation and where no sources of ignition, such as electric heaters, engines, cigarettes, lighters or electric hand dryers, are present. The affected areas of the skin should then be thoroughly washed with soap and warm water to remove all traces of contamination. Clothing should be air dried outside or in well-ventilated areas away from sources of ignition before laundering to minimize contamination of wastewater systems.
Service Station Environmental Issues
Storage tank inventory control
Service stations should maintain and reconcile accurate inventory records on all gasoline and fuel oil storage tanks on a regular basis to control losses. Manual stick gauging may be used to provide a check of the integrity of underground storage tanks and connecting pipes. Where automatic gauging or leak detection equipment is installed, its accuracy should be verified regularly by manual stick gauging. Any storage tank or system suspected of leaking should be investigated, and if leakage is detected, the tank should be made safe or emptied and repaired, removed or replaced. Service station employees should be aware that leaking gasoline can travel long distances underground, contaminate water supplies, enter sewer and drainage systems and cause fires and explosions.
Handling and disposal of waste materials
Waste lubricants and automotive chemicals, used motor oil and solvents, spilled gasoline and fuel oil and glycol-type antifreeze solutions should be drained into approved, properly labelled tanks or containers and stored until disposed of or recycled in accordance with government regulations and company policies.
Because engines with worn cylinders or other defects may allow small amounts of gasoline to enter their crankcases, precautions are needed to prevent vapours which could be released from tanks and containers with crankcase drainings from reaching sources of ignition.
Used oil filters and transmission fluid filters should be drained of oil prior to disposal. Used fuel filters which have been removed from vehicles or fuel dispenser pumps should be drained into approved containers and stored in well-ventilated locations away from sources of ignition until dry before disposal.
Used battery-electrolyte containers should be thoroughly rinsed with water before discarding or recycling. Used batteries contain lead and should be properly disposed of or recycled.
Cleaning large spills may require special training and PPE. Recovered spilled fuel may be returned to the terminal or bulk plant or otherwise disposed of according to government regulations or company policy. Lubricants, used oil, grease, antifreeze, spilled fuel and other materials should not be swept, washed or flushed into floor drains, sinks, toilets, sewers, sumps or other drains or the street. Accumulated grease and oil should be removed from floor drains and sumps to prevent these materials from flowing into sewers. Asbestos dust and used asbestos brake linings should be handled and disposed of according to government regulations and company policies. Employees should be aware of the environmental impact and potential health, safety and fire hazards of these wastes.
Law Enforcement
Law enforcement is difficult, stressful, demanding work. There is evidence that much of the work is sedentary, but the small part of the work which is not sedentary is physically demanding. This is also the part of the work which is often the most critical. In this respect, police work has been likened to the work of a lifeguard at a swimming pool. Most of the time, the lifeguard is watching from the water’s edge, but when it is necessary to intervene the emotional and physical demands are extreme and there is usually no warning. Unlike the lifeguard, the police officer may be exposed to attack with a knife or a gun, and may be exposed to intentional violence from some members of the public. Routine activities include patrolling streets, subways, country roads, parks and many other areas. Patrols may be carried out on foot, in vehicles (such as automobiles, helicopters or snowmobiles) and sometimes on horseback. There is a need for constant vigilance and, in many parts of the world, there is the constant threat of violence. Police officers may be called upon to provide assistance to the public in cases of robbery, riot, assault or domestic disputes. They may be involved in crowd control, search and rescue, or assistance to the public in the event of natural disaster. There is an episodic need to chase criminals on foot or in a vehicle, to grapple with, tackle and control criminals and, occasionally, to resort to the use of a lethal weapon. Routine activities can escalate to life-threatening violence with little or no warning. Some police officers work undercover, sometimes for prolonged periods. Others, particularly forensic specialists, are exposed to toxic chemicals. Almost all are exposed to biohazard risk from blood and body fluids. Police officers usually work shifts. Often their shifts are extended by administrative work or court appearances. The actual physical demands of police work and the physical tasks of policing have been extensively studied and are remarkably similar in different police forces and different geographical locations. The question of whether any specific medical condition may be attributable to the occupation of policing is controversial.
Violence
Violence is, unfortunately, a reality of police work. In the United States the homicide rate for police is more than double that for the general population. Work-related violent assault is common among police officers. The particular activities that are likely to result in violent conflict have been the subject of much recent research. The notion that domestic dispute calls were particularly dangerous has been seriously questioned (Violanti, Vena and Marshall 1986). More recently, the activities most likely to result in the assault of a police officer were ranked as follows: First, arresting/controlling suspects; second, robbery in progress; and third, domestic dispute.
The type of violence to which police officers are exposed varies from one country to another. Firearms are more common in the United States than Britain or Western Europe. Countries where political unrest is recent may see police officers exposed to attack from large-calibre or automatic-fire weaponry of a military type. Knife wounds are encountered everywhere, but large-blade knives, particularly machetes, seem more common in tropical countries.
Police officers must maintain a high level of physical fitness. Police training must include training in the physical control of suspects where necessary, as well as training in the use of firearms and other types of tools such as CS gas, pepper spray or hand-held batons. Personal protective equipment such as the “bullet proof” vest is necessary in some communities. Similarly, a communication system that allows the police officer to summon assistance is often important. The most important training, however, must be in the prevention of violence. Current police theory underscores the idea of community policing, with the police officer an integral part of the community. It is to be hoped that as this approach replaces the philosophy of armed military incursion into the community, the need for weaponry and for armour will be reduced.
The sequelae of violence need not be physical. Violent encounters are exceedingly stressful. This stress is particularly likely if the incident has resulted in serious injury, bloodshed or death. Particularly important is the assessment for post-traumatic stress disorder (PTSD) after such incidents.
Emotional and Psychological Stress
It is apparent that police work is stressful. For many police officers the excess of paperwork, as opposed to active law enforcement, is seen as a major stressor. The combination of shiftwork and the uncertainty about what may happen during the shift provides a powerfully stressful situation. In times of fiscal restraint, these stressors are often dramatically amplified by inadequate staffing and inadequate equipment. Situations where there is a potential for violence are stressful in themselves; the stress is dramatically increased where staffing is such that there is inadequate back-up, or when the police officer is seriously overworked.
In addition, the high stress levels which may result from police work have been blamed for marital difficulties, alcohol abuse and suicides among police officers. Much of the data supporting such associations are variable from one geographic region to another. Nevertheless, these problems may well result from the occupation of police work in some cases.
The need for constant vigilance for evidence of stress-related problems or post-traumatic stress disorder cannot be overemphasized. Stress-related disease may manifest as behavioural problems, marital or family problems or, sometimes, as alcohol or substance abuse.
Atherosclerotic Heart Disease
There have been numerous studies suggesting that atherosclerotic disease is more common among police officers (Vena et al. 1986; Sparrow, Thomas and Weiss 1983); there are also studies suggesting that this is not the case. It has been suggested that the increase in the prevalence of heart disease among police officers was almost entirely due to the increased risk of acute myocardial infarction.
This is intuitively satisfying since it is well known that sudden exertion, in the face of underlying heart disease, is an important risk factor for sudden death. The functional job analysis for a general-duty constable clearly indicates that a police officer may be expected, in the course of duty, to go from the sedentary state to maximal exertion with little or no warning and with no preparation. Indeed, much police work is sedentary, but, when required, the police officer is expected to run and chase, to grapple and tackle, and to forcibly subdue a suspect. It is therefore not unexpected that even if the rate of underlying coronary disease is not much different among police officers than the rest of the population, the risk of suffering an acute myocardial infarction, because of the nature of the work, may well be higher (Franke and Anderson 1994).
The demographics of the police population must be considered when assessing the risks for heart disease. Heart disease is most commonly found among middle-aged men, and this group makes up a very large proportion of police officers. Women, who have a significantly lower rate of heart disease during their premenopausal years, are significantly under-represented in the demographics of most police forces.
If one is to effectively reduce the risk of cardiac disease in police officers, the regular assessment of the police officer, by a physician knowledgeable about police work and the potential cardiac risks that are associated with police work, is essential (Brown and Trottier 1995). The periodic health assessment must include health education and counselling about cardiac risk factors. There is good evidence that work-based health promotion programmes have a salutary effect on employee health and that the modification of cardiac risk factors reduces the risks of cardiac death. Smoking cessation programmes, nutritional advice, hypertension awareness and cholesterol monitoring and modification are all appropriate activities that will help modify risk factors for cardiac disease among police officers. Regular exercise may be particularly important in police work. The generation of a work environment that educates the worker about positive nutritional and lifestyle choices and that encourages such choices is likely to be beneficial.
Lung Disease in Police Work
The evidence suggests that the prevalence of lung disease in police work is lower than in the general population. There is, however, evidence of an increased rate of cancer of the respiratory system. The majority of police officers are not routinely exposed to inhaled toxins at a rate any greater than other residents of the communities they police. There are exceptions to this general rule, however, the most notable exception being police officers working in forensic identification. There is good evidence that these individuals may suffer from an increased prevalence of respiratory symptoms and, possibly, occupational asthma (Souter, van Netten and Brands 1992; Trottier, Brown and Wells 1994). Cyanoacrylate, used in uncovering latent fingerprints, is a known respiratory sensitizer. In addition to this, there are a large number of chemical carcinogens routinely used in this type of work. For these reasons it is recommended that police officers who work in forensic identification, particularly those who do fingerprint work, should undergo annual chest x ray and spirometry. Similarly, periodic health assessment of these officers must include a careful assessment of the respiratory system.
Even though the practice of smoking cigarettes is becoming less common, a significant number of police officers continue to smoke. This may be the reason why some studies have shown an increased risk of lung and laryngeal cancers among police officers. Smoking is, of course, a major risk factor for cardiac disease. It is also the leading cause of lung cancer. When a police officer gets lung cancer the question frequently asked is whether the cancer is due to occupational exposure, in particular to the carcinogens known to be present in fingerprint powders. If the police officer smokes, it will be impossible to confidently assign blame to any occupational exposure. In summary, respiratory disease is not normally an occupational hazard of police work except for forensic identification workers.
Cancer
There is some evidence that police officers suffer a somewhat higher risk of cancer than expected in the general population. In particular, the risk of digestive tract cancers such as cancer of the oesophagus, cancer of the stomach and cancer of the large bowel is reported to be elevated among police officers. There may be an increased risk of cancer of the lung and larynx. The risk of cancer among police officers working in forensic identification and forensic laboratory work has been briefly discussed above. The controversial issue of testicular cancer associated with the use of police “radar” to detect speeders must also be addressed.
The data suggesting an increase in the risk of cancer of the digestive tract among police officers is scant, but it is a question that must be seriously examined. In the case of lung and oesophageal cancer, it is difficult to see how the activities of police work would be expected to increase the risk. Smoking, of course, is known to increase the risk of both lung and oesophageal cancer, and significant numbers of police officers are known to continue to smoke cigarettes. Another substance known to increase the risk of oesophageal cancer is alcohol, particularly whisky. Police work is known to be exceedingly stressful, and there have been some studies that suggest police officers may sometimes use alcohol to relieve the tension and stress of their work.
The same research that demonstrated an increased risk of cancers of the digestive tract also demonstrated a peculiar increase in the incidence of cancers of the lymphatic and haemopoietic systems in some police officers. The increased risk was restricted to one group and the overall risk was not elevated. Given this very peculiar distribution, and the small numbers, this finding may well turn out to be a statistical aberration.
The risk of cancer among police officers involved in forensic identification work and forensic laboratory work has been discussed. The expected toxicities of chronic low-level exposure to various chemicals are determined by the level of exposure and the use of personal protective equipment. Based on these exposures a periodic health examination has been developed, performed annually and tailored to risks specific for these exposures.
Recent work has suggested a possible increase in the risk of skin cancer, including melanoma, among police officers. Whether this is due to the amount of sun exposure experienced by some police officers who work out of doors is purely speculative.
The question of cancer resulting from exposure to microwaves from “police radar” units has created much controversy. There is certainly some evidence that there may be clustering of certain kinds of cancers among police officers exposed (Davis and Mostofi 1993). The particular concern is about exposure from hand-held units. Alternatively, recent work with large populations refutes any risk of carcinogenicity from exposure to these units. Testicular cancer, in particular, has been reported to be associated with such exposure. The circumstance said to pose the greatest risk is that where the hand-held unit is turned on and resting on the lap of the police officer. This could result in considerable cumulative exposure of the testes over the long term. Whether such exposure causes cancer remains unproven. In the meantime it is recommended that police radar units be mounted outside the police car, be directed away from the police officer, not be used inside the car, be turned off when not in use and be tested regularly for microwave leakage. In addition the periodic examination of police officers should include careful palpation of the testes.
Back Pain
Low-back pain is a major cause of absenteeism throughout the Western world. It is a condition most common among middle-aged males. The factors which predispose to chronic low-back pain are multiple and some, such as the correlation to smoking, seem intuitively difficult to comprehend.
With respect to the occupation of driving, there is ample evidence that individuals who drive for a living are at a dramatically increased risk of low-back pain. This observation includes police officers for whom driving plays a significant part in their daily work. The majority of police cars continue to be equipped with the seats that were installed at the time of their manufacture. Various back supports and prosthetic devices are available which may improve the support of the lumbar spine, but the problem remains.
There is evidence that physical confrontation may play a role in the development of back pain. Motor vehicle accidents, particularly in police vehicles, may play a part. Some police equipment, such as thick leather belts festooned with heavy equipment, may also play a role.
It is important to remember that stress may precipitate or exacerbate back pain and that back pain, as a reason for sick-leave, may be perceived by some police officers as more acceptable than the need to recover from emotional trauma.
There is no doubt that specific exercises designed to maintain flexibility and strengthen the muscles of the back can significantly improve function and symptoms. Numerous classification systems of back pain have been promulgated. These different patterns of pain have distinct approaches of active intervention through specific muscle strengthening programmes. It is important that specific symptom patterns be sought out among police officers and that appropriate intervention and treatment be initiated. This requires periodic assessment by physicians knowledgeable in this clinical syndrome and capable of early effective intervention. It is equally important that a good level of overall fitness be maintained in order to avoid disability from this common chronic, costly syndrome.
Biohazard Risks
There are reports of police officers said to have contracted AIDS from their work. In May 1993 the US Federal Bureau of Investigations reported that there had been seven cases of police officers contacting AIDS through their work over 10 years (Bigbee 1993). Let us begin by noting that this is a surprisingly small number of cases over a 10-year period in the entire United States. Let us next observe that there was some controversy about whether these cases were all to be considered job-related. Nevertheless, it is clearly possible to become infected with HIV as a result of police work.
Since there is no cure for AIDS, and no vaccine that prevents the disease, the best defence a police officer has against this infection is prevention. Latex gloves should be worn, whenever possible, any time that contact with blood or blood-contaminated evidence is foreseen. This is especially important if there are any skin breaks on the hands.
Any open sores or cuts that a police officer has sustained must be kept covered with an occlusive dressing while on duty. Needles should be handled with extreme care, and needles or syringes must be transported in a sharps container that can effectively prevent the needle from penetrating through the container. Sharp edges must be avoided and sharp exhibits handled with extreme care, particularly when contaminated with fresh blood. Where possible, such exhibits should be picked up with instruments rather than by hand.
Latex gloves and a barrier mask should be used if resuscitation attempts are undertaken, and latex gloves must always be worn when rendering first aid. It is important to bear in mind, however, that the risk of becoming infected with HIV from resuscitation procedures is very remote.
There are also some traditional techniques in policing that must be avoided. “Pat down” searches are dangerous to the police officer. There are numerous cases of police officers suffering needle stick injuries from this type of procedure. Also dangerous is searching containers, bags or even pockets by rummaging through them. All containers must be emptied into a flat surface and their contents examined in plain view. Similarly sweep searches under car seats and between seats and backs of couches and chairs must not be performed. It is preferable to dismantle furniture rather than have police officers putting their hands blindly in places where needles and syringes may be hidden. Latex gloves do not protect from needlestick injury.
Eye protection and face masks may be appropriate in circumstances where spatter of body fluid such as saliva or blood can reasonably be foreseen. There must be a system in place for the safe disposal of personal protective equipment. There must be a facility for police officers to wash their hands. Given the fact that few patrol cars have running water and sinks, prepackaged washing solutions for cleaning skin should be provided. Lastly, the question of what should be done for a police officer who, in spite of all the best precautions, suffers a percutaneous exposure to HIV should be asked. After appropriate wound care the first step is to try to determine whether the source of the exposure is truly HIV positive. This is not always possible. Secondly, it is imperative that the police officer be educated about the true risks of infection. Many non-medical personnel assume that the risk is much higher than it really is. Thirdly, the police officer must be informed of the need to retest for at least six months and possibly nine months in order to ensure that the officer has not been infected. Steps must be taken to prevent potential infection of the officer’s sexual partner(s) for at least six months. Lastly, the question of post-exposure prophylaxis must be discussed. There is increasing evidence that prophylaxis with antiviral drugs may be helpful in reducing the risk of seroconversion after percutaneous exposure. These are discussed elsewhere in the Encyclopaedia. In addition, the area of prophylaxis is under intense research scrutiny so that current references must be consulted to assure the most appropriate approach.
There are numerous case reports of occupationally acquired hepatitis among law enforcement personnel. The quantitative risk is not dramatically high when compared to other occupations. Nevertheless it is a real risk and must be seen as a possible occupational disease. The preventive approach to HIV infection that was outlined above applies equally well to the blood-borne disease hepatitis B. Given the fact that hepatitis B is so much more contagious than AIDS, and more likely to cause disease or death in the short term, this disease ought to be an even more compelling reason for following universal precautions.
There is an effective vaccine against hepatitis B. All police officers regardless of whether they are involved in forensics or general-duty policing, should be vaccinated against hepatitis B. Other conditions, including hepatitis C, tuberculosis and airborne pathogens, may also be encountered by police officers.
Singers
The term singer applies to any person whose career, avocation or livelihood relies heavily on the use of his or her voice in a musical context rather than ordinary speech. Unlike percussionists, pianists or violinists, the singer is the instrument. Hence, the well-being of a singer depends not only on the health of his or her larynx (where the sound originates) or vocal tract (where the sound is modified), but also on proper functioning and maximal coordination of most mind and body systems.
Of the many styles of singing documented throughout the world, some reflect a unique liturgical, cultural, linguistic, ethnic or geo-political heritage, while others are more universal in nature. Among the common styles of singing in the United States and Western world are: traditional classical (including oratorio, opera, art songs and so on), barbershop, jazz, musical theatre (Broadway), choral, gospel, folk, country (and western), popular, rhythm and blues, rock ’n’ roll (including heavy metal, alternative rock and so on) and others. Each style of delivery has its typical settings, patterns, habits and associated risk factors.
Vocal Problems
Unlike non-singers, who may not be significantly hindered by vocal problems, for the classical singer, the effect of subtle vocal impairment can be devastating. Even within that category of trained singers, vocal impairment is much more debilitating for the higher voice classifications (sopranos and tenors) than for lower classifications (mezzo sopranos, altos, baritones and basses). On the other hand, some vocal performers (pop, gospel or rock, for example) go to great lengths to achieve a unique trademark and enhance their marketability by inducing vocal pathologies which often yield a breathy, husky, muffled diplophonic (simultaneous multiple pitches) quality. Owing, in part, to their impairment, they tend to sing with great effort, struggling particularly to produce the high notes. To many listeners, this struggle adds a dramatic effect, as if the singer is sacrificing his or her self while engaging in the artistic process.
The prevalence of occupation-related injuries in general, and voice disorders in particular, among singers is not well documented in the literature. This author estimates that on the average, between 10 and 20% of singers in the United States sustain some form of chronic voice disorder. However, the incidence of vocal injury varies significantly with many factors. Because many singers must adhere to specific artistic/aesthetic criteria, performance practices, popular (consumer) demands, financial constraints and social pressures, they often stretch their vocal capabilities and endurance to the limits. Furthermore, singers generally tend to deny, trivialize or ignore warning signs and even diagnoses of vocal injury (Bastian, Keidar and Verdolini-Marston 1990).
The most common problems among singers are benign mucosal disorders. The mucosa is the outer layer, or cover, of the vocal folds (commonly called vocal cords) (Zeitels 1995). Acute problems can include laryngitis and transient vocal fold swelling (oedema). Chronic mucosal lesions include vocal fold swellings, nodules (“calluses”), polyps, cysts, sub-mucosal haemorrhage (bleeding), capillary ectasia (widening), chronic laryngitis, leukoplakia (white spots or patches), mucosal tears and glottic sulci (deep furrows in the tissue). Although these disorders can be exacerbated by smoking and excessive alcohol consumption, it is important to note that these benign mucosal lesions are typically related to the amount and manner of voice use, and are the product of vibratory trauma (Bastian 1993).
Causes of Vocal Problems
In looking at the causes of vocal problems in singers, one should distinguish between intrinsic and extrinsic factors. Intrinsic factors are those related to personality, vocal behaviour (including speaking) on and off stage, vocal technique, and intake habits (primarily if substance abuse, improper medication, malnutrition and/or dehydration is involved). Extrinsic factors are related to environmental pollutants, allergies and so on. Based on clinical experience, intrinsic factors tend to be most important.
Vocal injury is usually a cumulative process of misuse and/or overuse during the singer’s productive (performance-related) and/or non-productive (domestic, social) activities. It is difficult to ascertain how much of the damage is attributable directly to the former versus the latter. Performance risk factors can include unreasonably long dress rehearsals requiring full-voice singing, performing with an upper-respiratory infection in the absence of a replacement and excessive singing. Most vocalists are advised not to sing for more than about 1.5 hours (net) per day. Unfortunately, many singers do not respect the limitations of their apparatus. Some tend to get caught up in the exploratory excitement of new technical skills, new means of artistic expression, new repertoire and so on, and practice 4, 5 or 6 hours daily. Even worse is the beating of the voice into shape when distress signals of injury (such as loss of high notes, inability to sing softly, breathy delay in sound initiation, unstable vibrato and increased phonatory effort) are manifested. The culpability of vocal overtaxing is shared with other taskmasters such as the booking agent who squeezes multiple performances into an impossible time frame, and the recording agent who leases the studio for 12 consecutive hours during which the singer is expected to record a complete CD sound track from start to finish.
Although every singer may encounter acute episodes of voice problems at some point in his or her career, it is generally believed that those singers who are musically literate and can adjust the musical score to their voice limitations, and those who have had proper voice training, are less likely to encounter severe problems of a chronic nature than their untrained peers, who often learn their repertoire by rote, repeatedly imitating or singing along with demo tapes or recordings of other performers. In doing so, they frequently sing in a key, range or style unsuitable for their voices. Singers who lend themselves to periodic tutelage and maintenance by proficient voice experts are less likely to resort to faulty compensatory vocal manoeuvres if confronted by physical impairment, and are more inclined to establish a reasonable balance between artistic demands and vocal longevity. A good teacher is aware of the normal (expected) capabilities of each instrument, can usually distinguish between technical and physical limitations, and often is the first to detect warning signs of vocal impairment.
Sound amplification can also create problems for singers. Many rock groups, for example, amplify not only the singer, but the entire band. When the noise level interferes with auditory feedback, the singer is often unaware that he or she is singing too loudly and using faulty technique. This may contribute significantly to the development and exacerbation of vocal pathology.
Non-performance factors can also be important. Singers must realize that they do not have separate laryngeal mechanisms for singing and speaking. Although most professional singers spend much more time talking than singing, speaking technique is commonly discarded or rejected, which can adversely affect their singing.
Many of today’s singers must travel regularly from one performance venue to another, on trains, tour buses or airplanes. Ongoing touring requires not only psychological adaptation, but also physical adjustments on many levels. In order for singers to function optimally, they must receive adequate quality and quantity of sleep. Radical rapid changes in time zones causes jet lag, which forces singers to remain awake and alert when their internal clock is cueing various body systems to shut down for sleep, and conversely, to sleep when their brain systems are aroused to plan and execute normal daytime activities. Such interruption may result in a host of debilitating symptoms, including chronic insomnia, headaches, sluggishness, dizziness, irritability and forgetfulness (Monk 1994). Aberrant sleep patterns are also a common problem among those singers who perform late at night. These abnormal sleep patterns are all too often mismanaged with alcohol or recreational, prescription or over-the-counter (OTC) drugs (most of which adversely affect the voice). Frequent and/or prolonged confinement to a closed cabin of a motor vehicle, train or aircraft may create additional problems. Inhalation of poorly filtered (often recycled), contaminated, dehumidified (dry) air (Feder 1984), according to many singers, can cause respiratory discomfort, tracheitis, bronchitis or laryngitis that may linger on for hours or even days following a trip.
Owing to environmental instability and hectic scheduling, many singers develop erratic, unhealthful eating habits. In addition to reliance on restaurant food and unpredictable changes in meal times, many singers eat the main meal of the day after their performance, usually late at night. Particularly for the overweight singer, and especially if spicy, greasy or acidic foods, alcohol or coffee were consumed, lying down soon after having filled the stomach is likely to result in gastroesophageal reflux. Reflux is the retrograde flow of acids from the stomach up the oesophagus and into the throat and larynx. The resulting symptoms can be devastating to the singer. Eating disorders are quite common among singers. In the operatic and classical realm, overeating and obesity are quite common. In the musical theatre and pop domain, particularly among young females, reportedly one-fifth of all singers have encountered some form of eating disorder, such as anorexia or bulimia. The latter involves various purging methods, of which vomiting is thought to be particularly hazardous to the voice.
A detrimental factor to voice production is exposure to pollutants, such as formaldehyde, solvents, paints and dusts, and allergens, such as tree, grass or weed pollens, dust, mould spores, animal danders and perfumes (Sataloff 1996). Such exposure may occur on and off stage. In their work milieu, singers can be exposed to these and other pollutants associated with vocal symptoms, including cigarette smoke and theatrical smoke and fog effects. Singers use a greater percentage of their vital capacity than ordinary speakers. Furthermore, during intense aerobic activity (such as dancing), the number of breathing cycles per minute increases, and mouth breathing prevails. This results in the inhalation of larger amounts of cigarette smoke and fogs during performances.
Treatment of Vocal Problems
Two major issues in the treatment of vocal problems of singers are self-medication and improper treatment by physicians who are not knowledgeable about the voice and its problems. Sataloff (1991, 1995) surveyed the potential side effects associated with medications commonly used by singers. Whether recreational, prescription, over the counter or food supplements, most drugs are likely to have some effect on phonatory function. In an attempt to control “allergies”, “phlegm” or “sinus congestion”, the self-medicating singer will ultimately ingest something that will damage the vocal system. Likewise, the physician who keeps prescribing steroids to reduce chronic inflammation caused by abusive vocal habits and ignores the underlying causes will eventually hurt the singer. Vocal dysfunction resulting from poorly indicated or ill-performed phonosurgery has been documented (Bastian 1996). To avoid injuries secondary to treatment, singers are advised to know their instruments, and consult only with health care professionals who understand and have experience and expertise managing the vocal problems of singers, and who possess the patience to educate and empower singers.
Case Study: Treatment of Back Pain
Most episodes of acute back pain respond promptly to several days of rest followed by the gradual resumption of activities within the limits of pain. Non-narcotic analgesics and non-steroidal anti-inflammatory drugs may be helpful in relieving pain but do not shorten the course. (Since some of these drugs affect alertness and reaction time, they should be used with caution by individuals who drive vehicles or have assignments where momentary lapses may result in harm to patients.) A variety of forms of physiotherapy (e.g., local applications of heat or cold, diathermy, massage, manipulation, etc.) often provide short periods of transient relief; they are particularly useful as a prelude to graded exercises that will promote the restoration of muscle strength and relaxation as well as flexibility. Prolonged bed rest, traction and the use of lumbar corsets tend to delay recovery and often lengthen the period of disability (Blow and Jayson 1988).
Chronic, recurrent back pain is best treated by a secondary prevention regimen. Getting enough rest, sleeping on a firm mattress, sitting in straight chairs, wearing comfortable, well-fitted shoes, maintaining good posture and avoiding long periods of standing in one position are important adjuncts. Excessive or prolonged use of medications increase the risk of side effects and should be avoided. Some cases are helped by the injection of “trigger points”, localized tender nodules in muscles and ligaments, as originally advocated in the seminal report by Lange (1931).
Exercise of key postural muscles (upper and lower abdominal, back, gluteal and thigh muscles) is the mainstay of both chronic care and prevention of back pain. Kraus (1970) has formulated a regimen that features strengthening exercises to correct muscle weakness, relaxing exercises to relief tension, spasticity and rigidity, stretching exercises to minimize contractures and exercises to improve balance and coordination. These exercises, he cautions, should be individualized on the basis of examination of the patient and functional tests of muscle strength, holding power and elasticity (e.g., the Kraus-Weber tests (Kraus 1970)). To avoid adverse effects of exercise, each session should include warm-up and cool-down exercises as well as limbering and relaxing exercises, and the number, duration and intensity of the exercises should be increased gradually as conditioning improves. Simply giving the patient a printed exercise sheet or booklet is not enough; initially, he or she should be given individual instruction and observed to be sure that the exercises are being done correctly.
In 1974, the YMCA in New York introduced the “Y’s Way to a Healthy Back Program”, a low-cost course of exercise training based on the Kraus exercises; in 1976 it became a national programme in the US and, later, it was established in Australia and in several European countries (Melleby 1988). The twice-a-week, six week programme is given by specially-trained YMCA exercise instructors and volunteers, mainly in urban YMCAs (arrangements for courses at the worksite have been made by a number of employers), and it emphasizes the indefinite continuation of the exercises at home. Approximately 80% of the thousands of individuals with chronic or recurrent back pain who have participated in this program have reported elimination or improvement in their pain.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."