Children categories

94. Education and Training Services (7)

94. Education and Training Services
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Diseases affecting day-care workers & teachers
2. Hazards & precautions for particular classes
3. Summary of hazards in colleges & universities
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

95. Emergency and Security Services (9)

95. Emergency and Security Services
Chapter Editor: Tee L. Guidotti
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Recommendations & criteria for compensation
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

96. Entertainment and the Arts (31)

96. Entertainment and the Arts
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Arts and Crafts
Performing and Media Arts
Entertainment
Tables
Click a link below to view table in article context.
1. Precautions associated with hazards
2. Hazards of art techniques
3. Hazards of common stones
4. Main risks associated with sculpture material
5. Description of fibre & textile crafts
6. Description of fibre & textile processes
7. Ingredients of ceramic bodies & glazes
8. Hazards & precautions of collection management
9. Hazards of collection objects
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

97. Health Care Facilities and Services (25)

97. Health Care Facilities and Services
Chapter Editor: Annelee Yassi
Table of Contents
Tables and Figures
Health Care: Its Nature and Its Occupational Health Problems
Annalee Yassi and Leon J. Warshaw
Social Services
Susan Nobel
Home Care Workers: The New York City Experience
Lenora Colbert
Occupational Health and Safety Practice: The Russian Experience
Valery P. Kaptsov and Lyudmila P. Korotich
Ergonomics and Health Care
Hospital Ergonomics: A Review
Madeleine R. Estryn-Béhar
Strain in Health Care Work
Madeleine R. Estryn-Béhar
Case Study: Human Error and Critical Tasks: Approaches for Improved System Performance
Work Schedules and Night Work in Health Care
Madeleine R. Estryn-Béhar
The Physical Environment and Health Care
Exposure to Physical Agents
Robert M. Lewy
Ergonomics of the Physical Work Environment
Madeleine R. Estryn-Béhar
Prevention and Management of Back Pain in Nurses
Ulrich Stössel
Case Study: Treatment of Back Pain
Leon J. Warshaw
Health Care Workers and Infectious Disease
Overview of Infectious Diseases
Friedrich Hofmann
Prevention of Occupational Transmission of Bloodborne Pathogens
Linda S. Martin, Robert J. Mullan and David M. Bell
Tuberculosis Prevention, Control and Surveillance
Robert J. Mullan
Chemicals in the Health Care Environment
Overview of Chemical Hazards in Health Care
Jeanne Mager Stellman
Managing Chemical Hazards in Hospitals
Annalee Yassi
Waste Anaesthetic Gases
Xavier Guardino Solá
Health Care Workers and Latex Allergy
Leon J. Warshaw
The Hospital Environment
Buildings for Health Care Facilities
Cesare Catananti, Gianfranco Damiani and Giovanni Capelli
Hospitals: Environmental and Public Health Issues
M.P. Arias
Hospital Waste Management
M.P. Arias
Managing Hazardous Waste Disposal Under ISO 14000
Jerry Spiegel and John Reimer
Tables
Click a link below to view table in article context.
1. Examples of health care functions
2. 1995 integrated sound levels
3. Ergonomic noise reduction options
4. Total number of injuries (one hospital)
5. Distribution of nurses’ time
6. Number of separate nursing tasks
7. Distribution of nurses' time
8. Cognitive & affective strain & burn-out
9. Prevalence of work complaints by shift
10. Congenital abnormalities following rubella
11. Indications for vaccinations
12. Post-exposure prophylaxis
13. US Public Health Service recommendations
14. Chemicals’ categories used in health care
15. Chemicals cited HSDB
16. Properties of inhaled anaesthetics
17. Choice of materials: criteria & variables
18. Ventilation requirements
19. Infectious diseases & Group III wastes
20. HSC EMS documentation hierarchy
21. Role & responsibilities
22. Process inputs
23. List of activities
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

98. Hotels and Restaurants (4)

98. Hotels and Restaurants
Chapter Editor: Pam Tau Lee
Table of Contents

99. Office and Retail Trades (7)
99. Office and Retail Trades
Chapter Editor: Jonathan Rosen
Table of Contents
Tables and Figures
The Nature of Office and Clerical Work
Charles Levenstein, Beth Rosenberg and Ninica Howard
Professionals and Managers
Nona McQuay
Offices: A Hazard Summary
Wendy Hord
Bank Teller Safety: The Situation in Germany
Manfred Fischer
Telework
Jamie Tessler
The Retail Industry
Adrienne Markowitz
Case Study: Outdoor Markets
John G. Rodwan, Jr.
Tables
Click a link below to view table in article context.
1. Standard professional jobs
2. Standard clerical jobs
3. Indoor air pollutants in office buildings
4. Labour statistics in the retail industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

100. Personal and Community Services (6)
100. Personal and Community Services
Chapter Editor: Angela Babin
Table of Contents
Tables and Figures
Indoor Cleaning Services
Karen Messing
Barbering and Cosmetology
Laura Stock and James Cone
Laundries, Garment and Dry Cleaning
Gary S. Earnest, Lynda M. Ewers and Avima M. Ruder
Funeral Services
Mary O. Brophy and Jonathan T. Haney
Domestic Workers
Angela Babin
Case Study: Environmental Issues
Michael McCann
Click a link below to view table in article context.
1. Postures observed during dusting in a hospital
2. Dangerous chemicals used in cleaning
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

101. Public and Government Services (12)

101. Public and Government Services
Chapter Editor: David LeGrande
Table of Contents
Tables and Figurs
Occupational Health and Safety Hazards in Public and Governmental Services
David LeGrande
Case Report: Violence and Urban Park Rangers in Ireland
Daniel Murphy
Inspection Services
Jonathan Rosen
Postal Services
Roxanne Cabral
Telecommunications
David LeGrande
Hazards in Sewage (Waste) Treatment Plants
Mary O. Brophy
Domestic Waste Collection
Madeleine Bourdouxhe
Street Cleaning
J.C. Gunther, Jr.
Sewage Treatment
M. Agamennone
Municipal Recycling Industry
David E. Malter
Waste Disposal Operations
James W. Platner
The Generation and Transport of Hazardous Wastes: Social and Ethical Issues
Colin L. Soskolne
Tables
Click a link below to view table in article context.
1. Hazards of inspection services
2. Hazardous objects found in domestic waste
3. Accidents in domestic waste collection (Canada)
4. Injuries in the recycling industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

102. Transport Industry and Warehousing (18)

102. Transport Industry and Warehousing
Chapter Editor: LaMont Byrd
Table of Contents
Tables and Figures
General Profile
LaMont Byrd
Case Study: Challenges to Workers’ Health and Safety in the Transportation and Warehousing Industry
Leon J. Warshaw
Air Transport
Airport and Flight Control Operations
Christine Proctor, Edward A. Olmsted and E. Evrard
Case Studies of Air Traffic Controllers in the United States and Italy
Paul A. Landsbergis
Aircraft Maintenance Operations
Buck Cameron
Aircraft Flight Operations
Nancy Garcia and H. Gartmann
Aerospace Medicine: Effects of Gravity, Acceleration and Microgravity in the Aerospace Environment
Relford Patterson and Russell B. Rayman
Helicopters
David L. Huntzinger
Road Transport
Truck and Bus Driving
Bruce A. Millies
Ergonomics of Bus Driving
Alfons Grösbrink and Andreas Mahr
Motor Vehicle Fuelling and Servicing Operations
Richard S. Kraus
Case Study: Violence in Gasoline Stations
Leon J. Warshaw
Rail Transport
Rail Operations
Neil McManus
Case Study: Subways
George J. McDonald
Water Transport
Water Transportation and the Maritime Industries
Timothy J. Ungs and Michael Adess
Storage
Storage and Transportation of Crude Oil, Natural Gas, Liquid Petroleum Products and Other Chemicals
Richard S. Kraus
Warehousing
John Lund
Case Study: US NIOSH Studies of Injuries among Grocery Order Selectors
Tables
Click a link below to view table in article context.
1. Bus driver seat measurements
2. Illumination levels for service stations
3. Hazardous conditions & administration
4. Hazardous conditions & maintenance
5. Hazardous conditions & right of way
6. Hazard control in the Railway industry
7. Merchant vessel types
8. Health hazards common across vessel types
9. Notable hazards for specific vessel types
10. Vessel hazard control & risk-reduction
11. Typical approximate combustion properties
12. Comparison of compressed & liquified gas
13. Hazards involving order selectors
14. Job safety analysis: Fork-lift operator
15. Job safety analysis: Order selector
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Overview of Chemical Hazards in Health Care
Exposure to potentially hazardous chemicals is a fact of life for health care workers. They are encountered in the course of diagnostic and therapeutic procedures, in laboratory work, in preparation and clean-up activities and even in emanations from patients, to say nothing of the “infrastructure” activities common to all worksites such as cleaning and housekeeping, laundry, painting, plumbing and maintenance work. Despite the constant threat of such exposures and the large numbers of workers involved—in most countries, health care invariably is one of the most labour-intensive industries—this problem has received scant attention from those involved in occupational health and safety research and regulation. The great majority of chemicals in common use in hospitals and other health care settings are not specifically covered under national and international occupational exposure standards. In fact, very little effort has been made to date to identify the chemicals most frequently used, much less to study the mechanisms and intensity of exposures to them and the epidemiology of the effects on the health care workers involved.
This may be changing in the many jurisdictions in which right-to-know laws, such as the Canadian Workplace Hazardous Materials Information Systems (WHMIS) are being legislated and enforced. These laws require that workers be informed of the name and nature of the chemicals to which they may be exposed on the job. They have introduced a daunting challenge to administrators in the health care industry who must now turn to occupational health and safety professionals to undertake a de novo inventory of the identity and location of the thousands of chemicals to which their workers may be exposed.
The wide range of professions and jobs and the complexity of their interplay in the health care workplace require unique diligence and astuteness on the part of those charged with such occupational safety and health responsibilities. A significant complication is the traditional altruistic focus on the care and well-being of the patients, even at the expense of the health and well-being of those providing the services. Another complication is the fact that these services are often required at times of great urgency when important preventive and protective measures may be forgotten or deliberately disregarded.
Categories of Chemical Exposures in the Health Care Setting
Table 1 lists the categories of chemicals encountered in the health care workplace. Laboratory workers are exposed to the broad range of chemical reagents they employ, histology technicians to dyes and stains, pathologists to fixative and preservative solutions (formaldeyde is a potent sensitizer), and asbestos is a hazard to workers making repairs or renovations in older health care facilities.
Table 1. Categories of chemicals used in health care
|
Types of chemicals |
Locations most likely to be found |
|
Disinfectants |
Patient areas |
|
Sterilants |
Central supply |
|
Medicines |
Patient areas |
|
Laboratory reagents |
Laboratories |
|
Housekeeping/maintenance chemicals |
Hospital-wide |
|
Food ingredients and products |
Kitchen |
|
Pesticides |
Hospital-wide |
Even when liberally applied in combating and preventing the spread of infectious agents, detergents, disinfectants and sterilants offer relatively little danger to patients whose exposure is usually of brief duration. Even though individual doses at any one time may be relatively low, their cumulative effect over the course of a working lifetime may, however, constitute a significant risk to health care workers.
Occupational exposures to drugs can cause allergic reactions, such as have been reported over many years among workers administering penicillin and other antibiotics, or much more serious problems with such highly carcinogenic agents as the antineoplastic drugs. The contacts may occur during the preparation or administration of the dose for injection or in cleaning up after it has been administered. Although the danger of this mechanism of exposure had been known for many years, it was fully appreciated only after mutagenic activity was detected in the urine of nurses administering antineoplastic agents.
Another mechanism of exposure is the administration of drugs as aerosols for inhalation. The use of antineoplastic agents, pentamidine and ribavarin by this route has been studied in some detail, but there has been, as of this writing, no report of a systematic study of aerosols as a source of toxicity among health care workers.
Anaesthetic gases represent another class of drugs to which many health care workers are exposed. These chemicals are associated with a variety of biological effects, the most obvious of which are on the nervous system. Recently, there have been reports suggesting that repeated exposures to anaesthetic gases may, over time, have adverse reproductive effects among both male and female workers. It should be recognized that appreciable amounts of waste anaesthetic gases may accumulate in the air in recovery rooms as the gases retained in the blood and other tissues of patients are eliminated by exhalation.
Chemical disinfecting and sterilizing agents are another important category of potentially hazardous chemical exposures for health care workers. Used primarily in the sterilization of non-disposable equipment, such as surgical instruments and respiratory therapy apparatus, chemical sterilants such as ethylene oxide are effective because they interact with infectious agents and destroy them. Alkylation, whereby methyl or other alkyl groups bind chemically with protein-rich entities such as the amino groups in haemoglobiin and DNA, is a powerful biological effect. In intact organisms, this may not cause direct toxicity but should be considered potentially carcinogenic until proven otherwise. Ethylene oxide itself, however, is a known carcinogen and is associated with a variety of adverse health effects, as discussed elsewhere in the Encyclopaedia. The potent alkylation capability of ethylene oxide, probably the most widely-used sterilant for heat-sensitive materials, has led to its use as a classic probe in studying molecular structure.
For years, the methods used in the chemical sterilization of instruments and other surgical materials have carelessly and needlessly put many health care workers at risk. Not even rudimentary precautions were taken to prevent or limit exposures. For example, it was the common practice to leave the door of the sterilizer partially open to allow the escape of excess ethylene oxide, or to leave freshly-sterilized materials uncovered and open to the room air until enough had been assembled to make efficient use of the aerator unit.
The fixation of metallic or ceramic replacement parts so common in dentistry and orthopaedic surgery may be a source of potentially hazardous chemical exposure such as silica. These and the acrylic resins often used to glue them in place are usually biologically inert, but health care workers may be exposed to the monomers and other chemical reactants used during the preparation and application process. These chemicals are often sensitizing agents and have been associated with chronic effects in animals. The preparation of mercury amalgam fillings can lead to mercury exposure. Spills and the spread of mercury droplets is a particular concern since these may linger unnoticed in the work environment for many years. The acute exposure of patients to them appears to be entirely safe, but the long-term health implications of the repeated exposure of health care workers have not been adequately studied.
Finally, such medical techniques as laser surgery, electro-cauterization and use of other radiofrequency and high-energy devices can lead to the thermal degradation of tissues and other substances resulting in the formation of potentially toxic smoke and fumes. For example, the cutting of “plaster” casts made of polyester resin impregnated bandages has been shown to release potentially toxic fumes.
The hospital as a “mini-municipality”
A listing of the varied jobs and tasks performed by the personnel of hospitals and other large health care facilities might well serve as a table of contents for the commercial listings of a telephone directory for a sizeable municipality. All of these entail chemical exposures intrinsic to the particular work activity in addition to those that are peculiar to the health care environment. Thus, painters and maintenance workers are exposed to solvents and lubricants. Plumbers and others engaged in soldering are exposed to fumes of lead and flux. Housekeeping workers are exposed to soaps, detergents and other cleansing agents, pesticides and other household chemicals. Cooks may be exposed to potentially carcinogenic fumes in broiling or frying foods and to oxides of nitrogen from the use of natural gas as fuel. Even clerical workers may be exposed to the toners used in copiers and printers. The occurrence and effects of such chemical exposures are detailed elsewhere in this Encyclopaedia.
One chemical exposure that is diminishing in importance as more and more HCWs quit smoking and more health care facilities become “smoke-free” is “second hand” tobacco smoke.
Unusual chemical exposures in health care
Table 2 presents a partial listing of the chemicals most commonly encountered in health care workplaces. Whether or not they will be toxic will depend on the nature of the chemical and its biological proclivities, the manner, intensity and duration of the exposure, the susceptibilities of the exposed worker, and the speed and effectiveness of any countermeasures that may have been attempted. Unfortunately, a compendium of the nature, mechanisms, effects and treatment of chemical exposures of health care workers has not yet been published.
There are some unique exposures in the health care workplace that substantiate the dictum that a high level of vigilance is necessary to protect workers fully from such risks. For example, it was recently reported that health care workers had been overcome by toxic fumes emanating from a patient under treatment from a massive chemical exposure. Cases of cyanide poisoning arising from patient emissions have also been reported. In addition to the direct toxicity of waste anaesthetic gases to anaesthetists and other personnel in operating theatres, there is the often unrecognized problem created by the frequent use in such areas of high-energy sources which can transform the anaesthetic gases to free radicals, a form in which they are potentially carcinogenic.
Table 2. Chemicals cited Hazardous Substances Database (HSDB)
The following chemicals are listed in the HSDB as being used in some area of the health care environment. The HSDB is produced by the US National Library of Medicine and is a compilation of more than 4,200 chemicals with known toxic effects in commercial use. Absence of a chemical from the list does not imply that it is not toxic, but that it is not present in the HSDB.
|
Use list in the HSDB |
Chemical name |
CAS number* |
|
Disinfectants; antiseptics |
benzylalkonium chloride |
0001-54-5 |
|
Sterilants |
beta-propiolactone |
57-57-8 |
|
Laboratory reagents: |
2,4-xylidine (magenta-base) |
3248-93-9 |
* Chemical Abstracts identification number.
Water Transportation and the Maritime Industries
The very definition of the maritime setting is work and life that takes place in or around a watery world (e.g., ships and barges, docks and terminals). Work and life activities must first accommodate the macro-environmental conditions of the oceans, lakes or waterways in which they take place. Vessels serve as both workplace and home, so most habitat and work exposures are coexistent and inseparable.
The maritime industry comprises a number of sub-industries, including freight transportation, passenger and ferry service, commercial fishing, tankships and barge shipping. Individual maritime sub-industries consist of a set of merchant or commercial activities that are characterized by the type of vessel, targeted goods and services, typical practices and area of operations, and community of owners, operators and workers. In turn, these activities and the context in which they take place define the occupational and environmental hazards and exposures experienced by maritime workers.
Organized merchant maritime activities date back to the earliest days of civilized history. The ancient Greek, Egyptian and Japanese societies are examples of great civilizations where the development of power and influence was closely associated with having an extensive maritime presence. The importance of maritime industries to development of national power and prosperity has continued into the modern era.
The dominant maritime industry is water transportation, which remains the primary mode of international trade. The economies of most countries with ocean borders are heavily influenced by the receipt and export of goods and services by water. However, national and regional economies heavily dependent on the transport of goods by water are not limited to those which border oceans. Many countries removed from the sea have extensive networks of inland waterways.
Modern merchant vessels may process materials or produce goods as well as transport them. Globalized economies, restrictive land use, favourable tax laws and technology are among the factors which have spurred the growth of vessels that serve as both factory and means of transportation. Catcher-processor fishing vessels are a good example of this trend. These factory ships are capable of catching, processing, packaging and delivering finished sea food products to regional markets, as discussed in the chapter Fishing industry.
Merchant Transport Vessels
Similar to other transport vehicles, the structure, form and function of vessels closely parallel the vessel’s purpose and major environmental circumstances. For example, craft that transport liquids short distances on inland waterways will differ substantially in form and crew from those that carry dry bulk on trans-oceanic voyages. Vessels can be free moving, semi-mobile or permanently fixed structures (e.g., offshore oil-drilling rigs) and be self-propelled or towed. At any given time, existing fleets are comprised of a spectrum of vessels with a wide range of original construction dates, materials and degrees of sophistication.
Crew size will depend on the typical duration of trip, vessel purpose and technology, expected environmental conditions and sophistication of shore facilities. Larger crew size entails more extensive needs and elaborate planning for berthing, dining, sanitation, health care and personnel support. The international trend is toward vessels of increasing size and complexity, smaller crews and expanding reliance on automation, mechanization and containerization. Table 1 provides a categorization and descriptive summary of merchant vessel types.
Table 1. Merchant vessel types.
|
Vessel types |
Description |
Crew size |
|
Freight ships |
||
|
Bulk carrier
Break bulk
Container
Ore, bulk, oil (OBO)
Vehicle
Roll-on roll- off (RORO) |
Large vessel (200-600 feet (61-183 m)) typified by large open cargo holds and many voids; carry bulk cargoes such as grain and ore; cargo is loaded by chute, conveyor or shovel
Large vessel (200-600 feet (61-183 m)); cargo carried in bales, pallets, bags or boxes; expansive holds with between decks; may have tunnels
Large vessel (200-600 (61-183 m)) with open holds; may or may not have booms or cranes to handle cargo; containers are 20-40 feet (6.1-12.2 m) and stackable
Large vessel (200-600 feet (61-183 m)); holds are expansive and shaped to hold bulk ore or oil; holds are water tight, may have pumps and piping; many voids
Large vessel (200-600 feet (61-183 m)) with big sail area; many levels; vehicles can be self loading or boomed aboard
Large vessel (200-600 feet (61-183 m)) with big sail area; many levels; can carry other cargo in addition to vehicles |
25-50
25-60
25-45
25-55
25-40
25-40 |
|
Tank ships |
||
|
Oil
Chemical
Pressurized |
Large vessel (200-1000 feet (61-305 m)) typified by stern house piping on deck; may have hose handling booms and large ullages with many tanks; can carry crude or processed oil, solvents and other petroleum products
Large vessel (200-1000 feet (61-305 m)) similar to oil tankship, but may have additional piping and pumps to handle multiple cargoes simultaneously; cargoes can be liquid, gas, powders or compressed solids
Usually smaller (200-700 feet (61-213.4 m)) than typical tankship, having fewer tanks, and tanks which are pressurized or cooled; can be chemical or petroleum products such as liquid natural gas; tanks are usually covered and insulated; many voids, pipes and pumps |
25-50
25-50
15-30
|
|
Tug boats |
Small to mid-size vessel (80-200 feet (24.4-61 m)); harbour, push boats, ocean going |
3-15 |
|
Barge |
Mid-size vessel (100-350 feet (30.5-106.7 m)); can be tank, deck, freight or vehicle; usually not manned or self-propelled; many voids |
|
|
Drillships and rigs |
Large, similar profile to bulk carrier; typified by large derrick; many voids, machinery, hazardous cargo and large crew; some are towed, others self propelled |
40-120 |
|
Passenger |
All sizes (50-700 feet (15.2-213.4 m)); typified by large number of crew and passengers (up to 1000+) |
20-200 |
Morbidity and Mortality in the Maritime Industries
Health care providers and epidemiologists are often challenged to distinguish adverse health states due to work-related exposures from those due to exposures outside the workplace. This difficulty is compounded in the maritime industries because vessels serve as both workplace and home, and both exist in the greater environment of the maritime milieu itself. The physical boundaries found on most vessels result in close confinement and sharing of workspaces, engine-room, storage areas, passageways and other compartments with living spaces. Vessels often have a single water, ventilation or sanitation system that serves both work and living quarters.
The social structure aboard vessels is typically stratified into vessel officers or operators (ship’s master, first mate and so on) and remaining crew. Ship officers or operators are generally relatively more educated, affluent and occupationally stable. It is not uncommon to find vessels with crew members of an entirely different national or ethnic background from that of the officers or operators. Historically, maritime communities are more transient, heterogeneous and somewhat more independent than non-maritime communities. Work schedules aboard ship are often more fragmented and intermingled with non-work time than are land-based employment situations.
These are some reasons why it is difficult to describe or quantify health problems in the maritime industries, or to correctly associate problems with exposures. Data on maritime worker morbidity and mortality suffer from being incomplete and not representative of entire crews or sub-industries. Another shortfall of many data sets or information systems that report on the maritime industries is the inability to distinguish among health problems due to work, vessel or macro-environmental exposures. As with other occupations, difficulties in capturing morbidity and mortality information is most obvious with chronic disease conditions (e.g., cardiovascular disease), particularly those with a long latency (e.g., cancer).
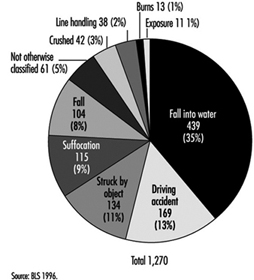
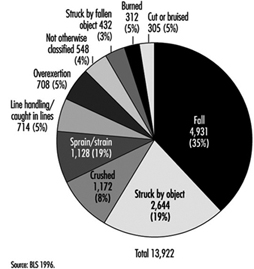
Review of 11 years (1983 to 1993) of US maritime data demonstrated that half of all fatalities due to maritime injuries, but only 12% of non-fatal injuries, are attributed to the vessel (i.e., collision or capsizing). The remaining fatalities and non-fatal injuries are attributed to personnel (e.g., mishaps to an individual while aboard ship). Reported causes of such mortality and morbidity are described in figure 1 and figure 2 respectively. Comparable information on non-injury-related mortality and morbidity is not available.
Figure 1. Causes of leading fatal unintentional injuries attributed to personal reasons (US maritime industries 1983-1993).
Figure 2. Causes of leading non-fatal unintentional injuries attributed to personal reasons (US maritime industries 1983-1993).
Combined vessel and personal US maritime casualty data reveal that the highest proportion (42%) of all maritime fatalities (N = 2,559), occurred among commercial fishing vessels. The next highest were among towboats/barges (11%), freight ships (10%) and passenger vessels (10%).
Analysis of reported work-related injuries for the maritime industries shows similarities to patterns reported for the manufacturing and construction industries. Commonalities are that most injuries are due to falls, being struck, cuts and bruises or muscular strains and overuse. Caution is needed when interpreting these data, however, as there is reporting bias: acute injuries are likely to be over-represented and chronic/latent injuries, which are less obviously connected to work, under-reported.
Occupational and Environmental Hazards
Most health hazards found in the maritime setting have land-based analogs in the manufacturing, construction and agricultural industries. The difference is that the maritime environment constricts and compresses available space, forcing close proximity of potential hazards and the intermingling of living quarters and workspaces with fuel tanks, engine and propulsion areas, cargo and storage spaces.
Table 2 summaries health hazards common across different vessel types. Health hazards of particular concern with specific vessel types are highlighted in table 3. The following paragraphs of this section expand discussion of selected environmental, physical and chemical, and sanitation health hazards.
Table 2. Health hazards common across vessel types.
|
Hazards |
Description |
Examples |
|
Mechanical |
Unguarded or exposed moving objects or their parts, which strike, pinch, crush or entangle. Objects can be mechanized (e.g., fork-lift) or simple (hinged door). |
Winches, pumps, fans, drive shafts, compressors, propellers, hatches, doors, booms, cranes, mooring lines, moving cargo |
|
Electrical |
Static (e.g., batteries) or active (e.g., generators) sources of electricity, their distribution system (e.g., wiring) and powered devices (e.g., motors), all of which can cause direct electrical-induced physical injury |
Batteries, vessel generators, dockside electrical sources, unprotected or ungrounded electric motors (pumps, fans, etc.), exposed wiring, navigation and communication electronics |
|
Thermal |
Heat- or cold-induced injury |
Steam pipes, cold storage spaces, power plant exhaust, cold- or warm-weather exposure above deck |
|
Noise |
Adverse auditory and other physiological problems due to excessive and prolonged sound energy |
Vessel propulsion system, pumps, ventilation fans, winches, steam-powered devices, conveyor belts |
|
Fall |
Slips, trips and falls resulting in kinetic-energy-induced injuries |
Steep ladders, deep vessel holds, missing railings, narrow gangways, elevated platforms |
|
Chemical |
Acute and chronic disease or injury resulting from exposure to organic or inorganic chemicals and heavy metals |
Cleaning solvents, cargo, detergents, welding, rusting/corrosion processes, refrigerants, pesticides, fumigants |
|
Sanitation |
Disease related to unsafe water, poor food practices or improper waste disposal |
Contaminated potable water, food spoilage, deteriorated vessel waste system |
|
Biologic |
Disease or illness causes by exposure to living organisms or their products |
Grain dust, raw wood products, cotton bales, bulk fruit or meat, seafood products, communicable disease agents |
|
Radiation |
Injury due to non-ionizing radiation |
Intense sunlight, arc welding, radar, microwave communications |
|
Violence |
Interpersonal violence |
Assault, homicide, violent conflict among crew |
|
Confined space |
Toxic or anoxic injury resulting from entering an enclosed space with limited entry |
Cargo holds, ballast tanks, crawl spaces, fuel tanks, boilers, storage rooms, refrigerated holds |
|
Physical work |
Health problems due to overuse, disuse or unsuitable work practices |
Shovelling ice in fish tanks, moving awkward cargo in restricted spaces, handling heavy mooring lines, prolonged stationary watch standing |
Table 3. Notable physical and chemical hazards for specific vessel types.
|
Vessel Types |
Hazards |
|
Tank vessels |
Benzene and various hydrocarbon vapours, hydrogen sulphide off-gassing from crude oil, inert gases used in tanks to create oxygen-deficient atmosphere for explosion control, fire and explosion due to combustion of hydrocarbon products |
|
Bulk cargo vessels |
Pocketing of fumigants used on agricultural products, personnel entrapment/suffocation in loose or shifting cargo, confined space risks in conveyor or man tunnels deep in vessel, oxygen deficiency due to oxidation or fermentation of cargo |
|
Chemical carriers |
Venting of toxic gases or dusts, pressurized air or gas release, leakage of hazardous substances from cargo holds or transfer pipes, fire and explosion due to combustion of chemical cargoes |
|
Container ships |
Exposure to spills or leakage due to failed or improperly stored hazardous substances; release of agricultural inerting gases; venting from chemical or gas containers; exposure to mislabeled substances that are hazardous; explosions, fire or toxic exposures due to mixing of separate substances to form a dangerous agent (e.g., acid and sodium cyanide) |
|
Break bulk vessels |
Unsafe conditions due to shifting of cargo or improper storage; fire, explosion or toxic exposures due to mixing of incompatible cargoes; oxygen deficiency due to oxidation or fermentation of cargoes; release of refrigerant gases |
|
Passenger ships |
Contaminated potable water, unsafe food preparation and storage practices, mass evacuation concerns, acute health problems of individual passengers |
|
Fishing vessels |
Thermal hazards from refrigerated holds, oxygen deficiency due to decomposition of seafood products or use of antioxidant preservatives, release of refrigerant gases, entanglement in netting or lines, contact with dangerous or toxic fish or sea animals |
Environmentalhazards
Arguably the most characteristic exposure defining the maritime industries is the pervasive presence of the water itself. The most variable and challenging of water environments is the open ocean. Oceans present constantly undulating surfaces, extremes of weather and hostile travel conditions, which combine to cause constant motion, turbulence and shifting surfaces and can result in vestibular disturbances (motion sickness), object instability (e.g., swinging latches and sliding gear) and the propensity to fall.
Humans have limited capability to survive unaided in open water; drowning and hypothermia are immediate threats upon immersion. Vessels serve as platforms that permit the human presence at sea. Ships and other water craft generally operate at some distance from other resources. For these reasons, vessels must dedicate a large proportion of total space to life support, fuel, structural integrity and propulsion, often at the expense of habitability, personnel safety and human factor considerations. Modern supertankers, which provide more generous human space and liveability, are an exception.
Excessive noise exposure is a prevalent problem because sound energy is readily transmitted through a vessel’s metallic structure to nearly all spaces, and limited noise attenuation materials are used. Excessive noise can be nearly continuous, with no available quiet areas. Sources of noise include the engine, propulsion system, machinery, fans, pumps and the pounding of waves on the vessel hull.
Mariners are an identified risk group for developing skin cancers, including malignant melanoma, squamous cell carcinoma and basal cell carcinoma. The increased risk is due to excess exposure to direct and water-surface-reflected ultraviolet solar radiation. Body areas of particular risk are exposed parts of the face, neck, ears and forearms.
Limited insulation, inadequate ventilation, internal sources of heat or cold (e.g., engine rooms or refrigerated spaces) and metallic surfaces all account for potential thermal stress. Thermal stress compounds physiological stress from other sources, resulting in reduced physical and cognitive performance. Thermal stress that is not adequately controlled or protected against can result in heat- or cold-induced injury.
Physical and chemical hazards
Table 3 highlights hazards unique or of particular concern to specific vessel types. Physical hazards are the most common and pervasive hazard aboard vessels of any type. Space limitations result in narrow passageways, limited clearance, steep ladders and low overheads. Confined vessel spaces means that machinery, piping, vents, conduits, tanks and so forth are squeezed in, with limited physical separation. Vessels commonly have openings that allow direct vertical access to all levels. Inner spaces below the surface deck are characterized by a combination of large holds, compact spaces and hidden compartments. Such physical structure places crew members at risk for slips, trips and falls, cuts and bruises, and being struck by moving or falling objects.
Constricted conditions result in being in close proximity to machinery, electrical lines, high-pressure tanks and hoses, and dangerously hot or cold surfaces. If unguarded or energized, contact can result in burns, abrasions, lacerations, eye damage, crushing or more serious injury.
Since vessels are basically a composite of spaces housed within a water-tight envelope, ventilation can be marginal or deficient in some spaces, creating a hazardous confined space situation. If oxygen levels are depleted or air is displaced, or if toxic gases enter these confined spaces, entry can be life threatening.
Refrigerants, fuels, solvents, cleaning agents, paints, inert gases and other chemical substances are likely to be found on any vessel. Normal ship activities, such as welding, painting and trash burning can have toxic effects. Transport vessels (e.g., freight ships, container ships and tank ships) can carry a host of biological or chemical products, many of which are toxic if inhaled, ingested or touched with the bare skin. Others can become toxic if allowed to degrade, become contaminated or mix with other agents.
Toxicity can be acute, as evidenced by dermal rashes and ocular burns, or chronic, as evidenced by neurobehavioural disorders and fertility problems or even carcinogenic. Some exposures can be immediately life-threatening. Examples of toxic chemicals carried by vessels are benzene-containing petrochemicals, acrylonitrile, butadiene, liquefied natural gas, carbon tetrachloride, chloroform, ethylene dibromide, ethylene oxide, formaldehyde solutions, nitropropane, o-toluidine and vinyl chloride.
Asbestos remains a hazard on some vessels, principally those constructed prior to the early 1970s. The thermal insulation, fire protection, durability and low cost of asbestos made this a preferred material in ship building. The primary hazard of asbestos occurs when the material becomes airborne when it is disturbed during renovations, construction or repair activities.
Sanitation and communicable disease hazards
One of the realities aboard ship is that the crew is often in close contact. In the work, recreation and living environments, crowding is often a fact of life that heightens the requirement for maintaining an effective sanitation programme. Critical areas include: berthing spaces, including toilet and shower facilities; food service and storage areas; laundry; recreation areas; and, if present, the barbershop. Pest and vermin control is also of critical importance; many of these animals can transmit disease. There are many opportunities for insects and rodents to infest a vessel, and once entrenched they are very difficult to control or eradicate, especially while underway. All vessels must have a safe and effective pest control programme. This requires training of individuals for this task, including annual refresher training.
Berthing areas must be kept free of debris, soiled laundry and perishable food. Bedding should be changed at least weekly (more often if soiled), and adequate laundry facilities for the size of the crew should be available. Food service areas must be rigorously maintained in a sanitary manner. The food service staff must receive training in proper techniques of food preparation, storage and galley sanitation, and adequate storage facilities must be provided aboard ship. The staff must adhere to recommended standards to ensure that food is prepared in a wholesome manner and is free of chemical and biological contamination. The occurrence of a food-borne disease outbreak aboard a vessel can be serious. A debilitated crew cannot carry out its duties. There may be insufficient medication to treat the crew, especially underway, and there may not be competent medical staff to care for the ill. In addition, if the ship is forced to change its destination, there may be significant economic loss to the shipping company.
The integrity and maintenance of a vessel’s potable water system is also of vital importance. Historically, water-borne outbreaks aboard ship have been the most common cause of acute disability and death among crews. Therefore, the potable water supply must come from an approved source (wherever possible) and be free from chemical and biological contamination. Where this is not possible, the vessel must have the means to effectively decontaminate the water and render it potable. A potable water system must be protected against contamination by every known source, including cross-contaminations with any non-potable liquids. The system also must be protected from chemical contamination. It must be cleaned and disinfected periodically. Filling the system with clean water containing at least 100 parts per million (ppm) of chlorine for several hours and then flushing the entire system with water containing 100 ppm chlorine is effective disinfection. The system should then be flushed with fresh potable water. A potable water supply must have at least 2 ppm residual of chlorine at all times, as documented by periodic testing.
Communicable disease transmission aboard ship is a serious potential problem. Lost work time, the cost of medical treatment and the possibility of having to evacuate crew members make this an important consideration. Besides the more common disease agents (e.g., those that cause gastroenteritis, such as Salmonella, and those that cause upper respiratory disease, such as the influenza virus), there has been a re-emergence of disease agents that were thought to be under control or eliminated from the general population. Tuberculosis, highly pathogenic strains of Escherichia coli and Streptococcus, and syphilis and gonorrhoea have reappeared in increasing incidence and/or virulence.
In addition, previously unknown or uncommon disease agents such as the HIV virus and the Ebola virus, which are not only highly resistant to treatment, but highly lethal, have appeared. It is therefore important that assessment be made of appropriate crew immunization for such diseases as polio, diphtheria, tetanus, measles, and hepatitis A and B. Additional immunizations may be required for specific potential or unique exposures, since crew members may have occasion to visit a wide variety of ports around the world and at the same time come in contact with a number of disease agents.
It is vital that crew members receive periodic training in the avoidance of contact with disease agents. The topic should include blood-borne pathogens, sexually transmitted diseases (STDs), food- and water-borne diseases, personal hygiene, symptoms of the more common communicable diseases and appropriate action by the individual on discovering these symptoms. Communicable disease outbreaks aboard ship can have a devastating effect on the vessel’s operation; they can result in a high level of illness among the crew, with the possibility of serious debilitating disease and in some cases death. In some instances, vessel diversion has been required with resultant heavy economic losses. It is in the best interest of the vessel owner to have an effective and efficient communicable disease programme.
Hazard Control and Risk Reduction
Conceptually, the principles of hazard control and risk reduction are similar to other occupational settings, and include:
- hazard identification and characterization
- inventory and analysis of exposures and at-risk populations
- hazard elimination or control
- personnel monitoring and surveillance
- disease/injury prevention and intervention
- programme evaluation and adjustment (see table 4).
Table 4. Vessel hazard control & risk-reduction.
|
Topics |
Activities |
|
Programme development and evaluation |
Identify hazards, shipboard and dockside. |
|
Hazard identification |
Inventory shipboard chemical, physical, biological, and environmental hazards, in both work and living spaces (e.g., broken railings, use and storage of cleaning agents, presence of asbestos). |
|
Assessment of exposure |
Understand work practices and job tasks (prescribed as well as those actually done). |
|
Personnel at risk |
Review work logs, employment records and monitoring data of entire ship’s complement, both seasonal and permanent. |
|
Hazard control and |
Know established and recommended exposure standards (e.g., NIOSH, ILO, EU). |
|
Health surveillance |
Develop health information gathering and reporting system for all injuries and illnesses (e.g., maintain a ship’s daily binnacle). |
|
Monitor crew health |
Establish occupational medical monitoring, determine performance standards, and establish fitness-for-work criteria (e.g., pre-placement and periodic pulmonary testing of crew handling grain). |
|
Hazard control and risk reduction effectiveness |
Devise and set priorities for goals (e.g., reduce shipboard falls). |
|
Programme evolution |
Modify prevention and control activities based on changing circumstances and prioritization. |
To be effective, however, the means and methods to implement these principles must be tailored to the specific maritime arena of interest. Occupational activities are complex and take place in integrated systems (e.g., vessel operations, employee/employer associations, commerce and trade determinants). The key to prevention is to understand these systems and the context in which they take place, which requires close cooperation and interaction between all organizational levels of the maritime community, from general deck hand through vessel operators and company upper management. There are many government and regulatory interests that impact the maritime industries. Partnerships between government, regulators, management and workers are essential for meaningful programmes for improving the health and safety status of the maritime industries.
The ILO has established a number of Conventions and Recommendations relating to shipboard work, such as the Prevention of Accidents (Seafarers) Convention, 1970 (No. 134), and Recommendation, 1970 (No. 142), the Merchant Shipping (Minimum Standards) Convention, 1976 (No. 147), the Merchant Shipping (Improvement of Standards) Recommendation, 1976 (No. 155), and the Health Protection and Medical Care (Seafarers) Convention, 1987 (No. 164). The ILO has also published a Code of Practice regarding the prevention of accidents at sea (ILO 1996).
Approximately 80% of vessel casualties are attributed to human factors. Similarly, the majority of reported injury-related morbidity and mortality have human factor causes. Reduction in maritime injury and death requires successful application of principles of human factors to work and life activities aboard vessels. Successful application of human factors principles means that vessel operations, vessel engineering and design, work activities, systems and management policies are developed that integrate human anthropometrics, performance, cognition and behaviours. For example, cargo loading/unloading presents potential hazards. Human factor considerations would highlight the need for clear communication and visibility, ergonomic matching of worker to task, safe separation of workers from moving machinery and cargo and a trained workforce, well acquainted with work processes.
Prevention of chronic diseases and adverse health states with long latency periods is more problematic than injury prevention and control. Acute injury events generally have readily recognized cause-effect relationships. Also, the association of injury cause and effect with work practices and conditions is usually less complicated than for chronic diseases. Hazards, exposures and health data specific to the maritime industries are limited. In general, health surveillance systems, reporting and analyses for the maritime industries are less developed than those for many of their land-based counterparts. The limited availability of chronic or latent disease health data specific to maritime industries hinders development and application of targeted prevention and control programmes.
Are They Health Care Workers, Too?
Often overlooked when considering the safety and well-being of health care workers are students attending medical, dental, nursing and other schools for health professionals and volunteers serving pro bono in healthcare facilities. Since they are not “employees” in the technical or legal sense of the term, they are ineligible for workers’ compensation and employment-based health insurance in many jurisdictions. Health care administrators have only a moral obligation to be concerned about their health and safety.
The clinical segments of their training bring medical, nursing and dental students into direct contact with patients who may have infectious diseases. They perform or assist in a variety of invasive procedures, including taking blood samples, and often do laboratory work involving body fluids and specimens of urine and faeces. They are usually free to wander about the facility, entering areas containing potential hazards often, since such hazards are rarely posted, without an awareness of their presence. They are usually supervised very loosely, if at all, while their instructors are often not very knowledgeable, or even interested, in matters of safety and health protection.
Volunteers are rarely permitted to participate in clinical care but they do have social contacts with patients and they usually have few restrictions with respect to areas of the facility they may visit.
Under normal circumstances, students and volunteers share with health care workers the risks of exposure to potentially harmful hazards. These risks are exacerbated at times of crisis and in emergencies when they step into or are ordered into the breech. Clearly, even though it may not be spelled out in laws and regulations or in organizational procedure manuals, they are more than entitled to the concern and protection extended to “regular” health care workers.
Managing Chemical Hazards in Hospitals
The vast array of chemicals in hospitals, and the multitude of settings in which they occur, call for a systematic approach to their control. A chemical-by-chemical approach to prevention of exposures and their deleterious outcome is simply too inefficient to handle a problem of this scope. Moreover, as noted in the article “Overview of chemical hazards in health care”, many chemicals in the hospital environment have been inadequately studied; new chemicals are constantly being introduced and for others, even some that have become quite familiar (e.g., gloves made of latex), new hazardous effects are only now becoming manifest. Thus, while it is useful to follow chemical-specific control guidelines, a more comprehensive approach is needed whereby individual chemical control policies and practices are superimposed on a strong foundation of general chemical hazard control.
The control of chemical hazards in hospitals must be based on classic principles of good occupational health practice. Because health care facilities are accustomed to approaching health through the medical model, which focuses on the individual patient and treatment rather than on prevention, special effort is required to ensure that the orientation for handling chemicals is indeed preventive and that measures are principally focused on the workplace rather than on the worker.
Environmental (or engineering) control measures are the key to prevention of deleterious exposures. However, it is necessary to train each worker correctly in appropriate exposure prevention techniques. In fact, right-to-know legislation, as described below, requires that workers be informed of the hazards with which they work, as well as of the appropriate safety precautions. Secondary prevention at the level of the worker is the domain of medical services, which may include medical monitoring to ascertain whether health effects of exposure can be medically detected; it also consists of prompt and appropriate medical intervention in the event of accidental exposure. Chemicals that are less toxic must replace more toxic ones, processes should be enclosed wherever possible and good ventilation is essential.
While all means to prevent or minimize exposures should be implemented, if exposure does occur (e.g., a chemical is spilled), procedures must be in place to ensure prompt and appropriate response to prevent further exposure.
Applying the General Principles of Chemical Hazard Control in the Hospital Environment
The first step in hazard control is hazard identification. This, in turn, requires a knowledge of the physical properties, chemical constituents and toxicological properties of the chemicals in question. Material safety data sheets (MSDSs), which are becoming increasingly available by legal requirement in many countries, list such properties. The vigilant occupational health practitioner, however, should recognize that the MSDS may be incomplete, particularly with respect to long-term effects or effects of low-dose chronic exposure. Hence, a literature search may be contemplated to supplement the MSDS material, when appropriate.
The second step in controlling a hazard is characterizing the risk. Does the chemical pose a carcinogenic risk? Is it an allergen? A teratogen? Is it mainly short-term irritancy effects that are of concern? The answer to these questions will influence the way in which exposure is assessed.
The third step in chemical hazard control is to assess the actual exposure. Discussion with the health care workers who use the product in question is the most important element in this endeavour. Monitoring methods are necessary in some situations to ascertain that exposure controls are functioning properly. These may be area sampling, either grab sample or integrated, depending on the nature of the exposure; it may be personal sampling; in some cases, as discussed below, medical monitoring may be contemplated, but usually as a last resort and only as back-up to other means of exposure assessment.
Once the properties of the chemical product in question are known, and the nature and extent of exposure are assessed, a determination could be made as to the degree of risk. This generally requires that at least some dose-response information be available.
After evaluating the risk, the next series of steps is, of course, to control the exposure, so as to eliminate or at least minimize the risk. This, first and foremost, involves applying the general principles of exposure control.
Organizing a Chemical Control Programme in Hospitals
The traditional obstacles
The implementation of adequate occupational health programmes in health care facilities has lagged behind the recognition of the hazards. Labour relations are increasingly forcing hospital management to look at all aspects of their benefits and services to employees, as hospitals are no longer tacitly exempt by custom or privilege. Legislative changes are now compelling hospitals in many jurisdictions to implement control programmes.
However, obstacles remain. The preoccupation of the hospital with patient care, emphasizing treatment rather than prevention, and the staff’s ready access to informal “corridor consultation”, have hindered the rapid implementation of control programmes. The fact that laboratory chemists, pharmacists and a host of medical scientists with considerable toxicological expertise are heavily represented in management has, in general, not served to hasten the development of programmes. The question may be asked, “Why do we need an occupational hygienist when we have all these toxicology experts?” To the extent that changes in procedures threaten to have an impact on the tasks and services provided by these highly skilled personnel, the situation may be made worse: “We cannot eliminate the use of Substance X as it is the best bactericide around.” Or, “If we follow the procedure that you are recommending, patient care will suffer.” Moreover, the “we don’t need training” attitude is commonplace among the health care professions and hinders the implementation of the essential components of chemical hazard control. Internationally, the climate of cost constraint in health care is clearly also an obstacle.
Another problem of particular concern in hospitals is preserving the confidentiality of personal information about health care workers. While occupational health professionals should need only to indicate that Ms. X cannot work with chemical Z and needs to be transferred, curious clinicians are often more prone to push for the clinical explanation than their non-health care counterparts. Ms. X may have liver disease and the substance is a liver toxin; she may be allergic to the chemical; or she may be pregnant and the substance has potential teratogenic properties. While the need to alter the work assignment of particular individuals should not be routine, the confidentiality of the medical details should be protected if it is necessary.
Right-to-know legislation
Many jurisdictions around the world have implemented right-to-know legislation. In Canada, for example, WHMIS has revolutionized the handling of chemicals in industry. This country-wide system has three components: (1) the labelling of all hazardous substances with standardized labels indicating the nature of the hazard; (2) the provision of MSDSs with the constituents, hazards and control measures for each substance; and (3) the training of workers to understand the labels and the MSDSs and to use the product safely.
Under WHMIS in Canada and OSHA’s Hazard Communications requirements in the United States, hospitals have been required to construct inventories of all chemicals on the premises so that those that are “controlled substances” can be identified and addressed according to the legislation. In the process of complying with the training requirements of these regulations, hospitals have had to engage occupational health professionals with appropriate expertise and the spin-off benefits, particularly when bipartite train-the-trainer programmes were conducted, have included a new spirit to work cooperatively to address other health and safety concerns.
Corporate commitment and the role of joint health and safety committees
The most important element in the success of any occupational health and safety programme is corporate commitment to ensure its successful implementation. Policies and procedures regarding the safe handling of chemicals in hospitals must be written, discussed at all levels within the organization and adopted and enforced as corporate policy. Chemical hazard control in hospitals should be addressed by general as well as specific policies. For example, there should be a policy on responsibility for the implementation of right-to-know legislation that clearly outlines each party’s obligations and the procedures to be followed by individuals at each level of the organization (e.g., who chooses the trainers, how much work time is allowed for preparation and provision of training, to whom should communication regarding non-attendance be communicated and so on). There should be a generic spill clean-up policy indicating the responsibility of the worker and the department where the spill occurred, the indications and protocol for notifying the emergency response team, including the appropriate in-hospital and external authorities and experts, follow-up provisions for exposed workers and so on. Specific policies should also exist regarding the handling, storage and disposal of specific classes of toxic chemicals.
Not only is it essential that management be strongly committed to these programmes; the workforce, through its representatives, must also be actively involved in the development and implementation of policies and procedures. Some jurisdictions have legislatively mandated joint (labour-management) health and safety committees that meet at a minimum prescribed interval (bimonthly in the case of Manitoba hospitals), have written operating procedures and keep detailed minutes. Indeed in recognizing the importance of these committees, the Manitoba Workers’ Compensation Board (WCB) provides a rebate on WCB premiums paid by employers based on the successful functioning of these committees. To be effective, the members must be appropriately chosen—specifically, they must be elected by their peers, knowledgeable about the legislation, have appropriate education and training and be allotted sufficient time to conduct not only incident investigations but regular inspections. With respect to chemical control, the joint committee has both a pro-active and a re-active role: assisting in setting priorities and developing preventive policies, as well as serving as a sounding board for workers who are not satisfied that all appropriate controls are being implemented.
The multidisciplinary team
As noted above, the control of chemical hazards in hospitals requires a multidisciplinary endeavour. At a minimum, it requires occupational hygiene expertise. Generally hospitals have maintenance departments that have within them the engineering and physical plant expertise to assist a hygienist in determining whether workplace alterations are necessary. Occupational health nurses also play a prominent role in evaluating the nature of concerns and complaints, and in assisting an occupational physician in ascertaining whether clinical intervention is warranted. In hospitals, it is important to recognize that numerous health care professionals have expertise that is quite relevant to the control of chemical hazards. It would be unthinkable to develop policies and procedures for the control of laboratory chemicals without the involvement of lab chemists, for example, or procedures for handling anti-neoplastic drugs without the involvement of the oncology and pharmacology staff. While it is wise for occupational health professionals in all industries to consult with line staff prior to implementing control measures, it would be an unforgivable error to fail to do so in health care settings.
Data collection
As in all industries, and with all hazards, data need to be compiled both to help in priority setting and in evaluating the success of programmes. With respect to data collection on chemical hazards in hospitals, minimally, data need to be kept regarding accidental exposures and spills (so that these areas can receive special attention to prevent recurrences); the nature of concerns and complaints should be recorded (e.g., unusual odours); and clinical cases need to be tabulated, so that, for example, an increase in dermatitis from a given area or occupational group could be identified.
Cradle-to-grave approach
Increasingly, hospitals are becoming cognizant of their obligation to protect the environment. Not only the workplace hazardous properties, but the environmental properties of chemicals are being taken into consideration. Moreover, it is no longer acceptable to pour hazardous chemicals down the drain or release noxious fumes into the air. A chemical control programme in hospitals must, therefore, be capable of tracking chemicals from their purchase and acquisition (or, in some cases, synthesis on site), through the work handling, safe storage and finally to their ultimate disposal.
Conclusion
It is now recognized that there are thousands of potentially very toxic chemicals in the work environment of health care facilities; all occupational groups may be exposed; and the nature of the exposures are varied and complex. Nonetheless, with a systematic and comprehensive approach, with strong corporate commitment and a fully informed and involved workforce, chemical hazards can be managed and the risks associated with these chemicals controlled.
Social Services
Overview of the Social Work Profession
Social workers function in a wide variety of settings and work with many different kinds of people. They work in community health centres, hospitals, residential treatment centres, substance-abuse programmes, schools, family service agencies, adoption and foster care agencies, day-care facilities and public and private child welfare organizations. Social workers often visit homes for interviews or inspections of home conditions. They are employed by businesses, labour unions, international aid organizations, human rights agencies, prisons and probation departments, agencies for the ageing, advocacy organizations, colleges and universities. They are increasingly entering politics. Many social workers have full- or part-time private practices as psychotherapists. It is a profession that seeks to “improve social functioning by the provision of practical and psychological help to people in need” (Payne and Firth-Cozens 1987).
Generally, social workers with doctorates work in community organization, planning, research, teaching or combined areas. Those with bachelor’s degrees in social work tend to work in public assistance and with the elderly, mentally retarded and developmentally disabled; social workers with master’s degrees are usually found in mental health, occupational social work and medical clinics (Hopps and Collins 1995).
Hazards and Precautions
Stress
Studies have shown that stress in the workplace is caused, or contributed to, by job insecurity, poor pay, work overload and lack of autonomy. All of these factors are features of the work life of social workers in the late 1990s. It is now accepted that stress is often a contributing factor to illness. One study has shown that 50 to 70% of all medical complaints among social workers are linked to stress (Graham, Hawkins and Blau 1983).
As the social work profession has attained vendorship privileges, managerial responsibilities and increased numbers in private practice, it has become more vulnerable to professional liability and malpractice suits in countries such as the United States which permit such legal actions, a fact which contributes to stress. Social workers are also increasingly dealing with bioethical issues—those of life and death, of research protocols, of organ transplantation and of resource allocation. Often there is inadequate support for the psychological toll confronting these issues can take on involved social workers. Increased pressures of high caseloads as well as increased reliance on technology makes for less human contact, a fact which is likely true for most professions, but particularly difficult for social workers whose choice of work is so related to having face to face contact.
In many countries, there has been a shift away from government-funded social programmes. This policy trend directly affects the social work profession. The values and goals generally held by social workers—full employment, a “safety net” for the poor, equal opportunity for advancement—are not supported by these current trends.
The movement away from spending on programmes for the poor has produced what has been called an “upside-down welfare state” (Walz, Askerooth and Lynch 1983). One result of this, among others, has been increased stress for social workers. As resources decline, demand for services is on the rise; as the safety net frays, frustration and anger must rise, both for clients and for social workers themselves. Social workers may increasingly find themselves in conflict over respecting the values of the profession versus meeting statutory requirements. The code of ethics of the US National Association of Social Workers, for example, mandates confidentiality for clients which may be broken only when it is for “compelling professional reasons”. Further, social workers are to promote access to resources in the interest of “securing or retaining social justice”. The ambiguity of this could be quite problematic for the profession and a source of stress.
Violence
Work-related violence is a major concern for the profession. Social workers as problem-solvers on the most personal level are particularly vulnerable. They work with powerful emotions, and it is the relationship with their clients which becomes the focal point for expression of these emotions. Often, an underlying implication is that the client is unable to manage his or her own problems and needs the help of social workers to do so. The client may, in fact, be seeing social workers involuntarily, as, for example, in a child welfare setting where parental abilities are being evaluated. Cultural mores might also interfere with accepting offers of help from someone of another cultural background or sex (the preponderence of social workers are women) or outside of the immediate family. There may be language barriers, necessitating the use of translators. This can be distracting at least or even totally disruptive and may present a skewed picture of the situation at hand. These language barriers certainly affect the ease of communication, which is essential in this field. Further, social workers may work in locations which are in high-crime areas, or the work might take them into the “field” to visit clients who live in those areas.
Application of safety procedures is uneven in social agencies, and, in general, insufficient attention has been paid to this area. Prevention of violence in the workplace implies training, managerial procedures and modifications of the physical environment and/or communication systems (Breakwell 1989).
A curriculum for safety has been suggested (Griffin 1995) which would include:
- training in constructive use of authority
- crisis intervention
- field and office safety
- physical plant set-up
- general prevention techniques
- ways to predict potential violence.
Other Hazards
Because social workers are employed in such a variety of settings, they are exposed to many of the hazards of the workplace discussed elsewhere in this Encyclopaedia. Mention should be made, however, that these hazards include buildings with poor or unclean air flow (“sick buildings”) and exposures to infection. When funding is scarce, maintenance of physical plants suffers and risk of exposure increases. The high percentage of social workers in hospital and out-patient medical settings suggests vulnerability to infection exposure. Social workers see patients with conditions like hepatitis, tuberculosis and other highly contagious diseases as well as human immunodeficiency virus (HIV) infection. In response to this risk for all health workers, training and measures for infection control are necessary and have been mandated in many countries. The risk, however, persists.
It is evident that some of the problems faced by social workers are inherent in a profession which is so centred on lessening human suffering as well as one which is so affected by changing social and political climates. At the end of the twentieth century, the profession of social work finds itself in a state of flux. The values, ideals and rewards of the profession are also at the heart of the hazards it presents to its practitioners.
Waste Anaesthetic Gases
The use of inhaled anaesthetics was introduced in the decade of 1840 to 1850. The first compounds to be used were diethyl ether, nitrous oxide and chloroform. Cyclopropane and trichloroethylene were introduced many years later (circa 1930-1940), and the use of fluoroxene, halothane and methoxiflurane began in the decade of the 1950s. By the end of the 1960s enflurane was being used and, finally, isoflurane was introduced in the 1980s. Isoflurane is now considered the most widely used inhalation anaesthetic even though it is more expensive than the others. A summary of the physical and chemical characteristics of methoxiflurane, enflurane, halothane, isoflurane and nitrous oxide, the most commonly used anaesthetics, is shown in table 1 (Wade and Stevens 1981).
Table 1. Properties of inhaled anaesthetics
|
Isoflurane, |
Enflurane, |
Halothane, |
Methoxyflurane, |
Dinitrogen oxide, |
|
|
Molecular weight |
184.0 |
184.5 |
197.4 |
165.0 |
44.0 |
|
Boiling point |
48.5°C |
56.5°C |
50.2°C |
104.7°C |
— |
|
Density |
1.50 |
1.52 (25°C) |
1.86 (22°C) |
1.41 (25°C) |
— |
|
Vapour pressure at 20 °C |
250.0 |
175.0 (20°C) |
243.0 (20°C) |
25.0 (20°C) |
— |
|
Smell |
Pleasant, sharp |
Pleasant, like ether |
Pleasant, sweet |
Pleasant, fruity |
Pleasant, sweet |
|
Separation coefficients: |
|||||
|
Blood/gas |
1.40 |
1.9 |
2.3 |
13.0 |
0.47 |
|
Brain/gas |
3.65 |
2.6 |
4.1 |
22.1 |
0.50 |
|
Fat/gas |
94.50 |
105.0 |
185.0 |
890.0 |
1.22 |
|
Liver/gas |
3.50 |
3.8 |
7.2 |
24.8 |
0.38 |
|
Muscle/gas |
5.60 |
3.0 |
6.0 |
20.0 |
0.54 |
|
Oil/gas |
97.80 |
98.5 |
224.0 |
930.0 |
1.4 |
|
Water/gas |
0.61 |
0.8 |
0.7 |
4.5 |
0.47 |
|
Rubber/gas |
0.62 |
74.0 |
120.0 |
630.0 |
1.2 |
|
Metabolic rate |
0.20 |
2.4 |
15–20 |
50.0 |
— |
All of them, with the exception of nitrous oxide (N2O), are hydrocarbons or chlorofluorinated liquid ethers that are applied by vapourization. Isoflurane is the most volatile of these compounds; it is the one that is metabolized at the lowest rate and the one that is least soluble in blood, in fats and in the liver.
Normally, N2O, a gas, is mixed with a halogenated anaesthetic, although they are sometimes used separately, depending on the type of anaesthesia that is required, the characteristics of the patient and the work habits of the anaesthetist. The normally used concentrations are 50 to 66% N2O and up to 2 or 3% of the halogenated anaesthetic (the rest is usually oxygen).
The anaesthesia of the patient is usually started by the injection of a sedative drug followed by an inhaled anaesthetic. The volumes given to the patient are in the order of 4 or 5 litres/minute. Parts of the oxygen and of the anaesthetic gases in the mixture are retained by the patient while the remainder is exhaled directly into the atmosphere or is recycled into the respirator, depending among other things on the type of mask used, on whether the patient is intubated and on whether or not a recycling system is available. If recycling is available, exhaled air can be recycled after it is cleaned or it can be vented to the atmosphere, expelled from the operating room or aspirated by a vacuum. Recycling (closed circuit) is not a common procedure and many respirators do not have exhaust systems; all the air exhaled by the patient, including the waste anaesthetic gases, therefore, ends up in the air of the operating room.
The number of workers occupationally exposed to waste anaesthetic gases is high, because it is not only the anaesthetists and their assistants who are exposed, but all the other people who spend time in operating rooms (surgeons, nurses and support staff), the dentists who perform odontological surgery, the personnel in delivery rooms and intensive care units where patients may be under inhaled anaesthesia and veterinary surgeons. Similarly, the presence of waste anaesthetic gases is detected in recovery rooms, where they are exhaled by patients who are recovering from surgery. They are also detected in other areas adjacent to operating rooms because, for reasons of asepsis, operating rooms are kept at positive pressure and this favours the contamination of surrounding areas.
Health Effects
Problems due to the toxicity of anaesthetic gases were not seriously studied until the 1960s, even though a few years after the use of inhaled anaesthetics became common, the relationship between the illnesses (asthma, nephritis) that affected some of the first professional anaesthetists and their work as such was already suspected (Ginesta 1989). In this regard the appearance of an epidemiological study of more than 300 anaesthetists in the Soviet Union, the Vaisman (1967) survey, was the starting point for several other epidemiological and toxicological studies. These studies—mostly during the 1970s and the first half of the 1980s—focused on the effects of anaesthetic gases, in most cases nitrous oxide and halothane, on people occupationally exposed to them.
The effects observed in most of these studies were an increase in spontaneous abortions among women exposed during or before pregnancy, and among women partners of exposed men; an increase in congenital malformations in children of exposed mothers; and the occurrence of hepatic, renal and neurological problems and of some types of cancer in both men and women (Bruce et al. 1968, 1974; Bruce and Bach 1976). Even though the toxic effects of nitrous oxide and of halothane (and probably its substitutes as well) on the body are not exactly the same, they are commonly studied together, given that exposure generally occurs simultaneously.
It appears likely that there is a correlation between these exposures and an increased risk, particularly for spontaneous abortions and congenital malformations in children of women exposed during pregnancy (Stoklov et al. 1983; Spence 1987; Johnson, Buchan and Reif 1987). As a result, many of the people exposed have expressed great concern. Rigorous statistical analysis of these data, however, casts doubt on the existence of such a relationship. More recent studies reinforce these doubts while chromosomal studies yield ambiguous results.
The works published by Cohen and colleagues (1971, 1974, 1975, 1980), who carried out extensive studies for the American Society of Anaesthetists (ASA), constitute a fairly extensive series of observations. Follow-up publications criticized some of the technical aspects of the earlier studies, particularly with respect to the sampling methodology and, especially, the proper selection of a control group. Other deficiencies included lack of reliable information on the concentrations to which the subjects had been exposed, the methodology for dealing with false positives and the lack of controls for factors such as tobacco and alcohol use, prior reproductive histories and voluntary infertility. Consequently, some of the studies are now even considered invalid (Edling 1980; Buring et al. 1985; Tannenbaum and Goldberg 1985).
Laboratory studies have shown that exposure of animals to ambient concentrations of anaesthetic gases equivalent to those found in operating rooms does cause deterioration in their development, growth and adaptive behaviour (Ferstandig 1978; ACGIH 1991). These are not conclusive, however, since some of these experimental exposures involved anaesthetic or subanaesthetic levels, concentrations significantly higher than the levels of waste gases usually found in operating room air (Saurel-Cubizolles et al. 1994; Tran et al. 1994).
Nevertheless, even acknowledging that a relationship between the deleterious effects and exposures to waste anaesthetic gases has not been definitively established, the fact is that the presence of these gases and their metabolites is readily detected in the air of operating rooms, in exhaled air and in biological fluids. Accordingly, since there is concern about their potential toxicity, and because it is technically feasible to do so without inordinate effort or expense, it would be prudent to take steps to eliminate or reduce to a minimum the concentrations of waste anaesthetic gases in operating rooms and nearby areas (Rosell, Luna and Guardino 1989; NIOSH 1994).
Maximum Allowable Exposure Levels
The American Conference of Governmental Industrial Hygienists (ACGIH) has adopted a threshold limit value-time weighted average (TLV-TWA) of 50 ppm for nitrous oxide and halothane (ACGIH 1994). The TLV-TWA is the guideline for the production of the compound, and the recommendations for operating rooms are that its concentration be kept lower, at a level below 1 ppm (ACGIH 1991). NIOSH sets a limit of 25 ppm for nitrous oxide and of 1 ppm for halogenated anaesthetics, with the additional recommendation that when they are used together, the concentration of halogenated compounds be reduced to a limit of 0.5 ppm (NIOSH 1977b).
With regard to values in biological fluids, the recommended limit for nitrous oxide in urine after 4 hours of exposure at average ambient concentrations of 25 ppm ranges from 13 to 19 μg/L, and for 4 hours of exposure at average ambient concentrations of 50 ppm, the range is 21 to 39 μg/L (Guardino and Rosell 1995). If exposure is to a mixture of a halogenated anaesthetic and nitrous oxide, the measurement of the values from nitrous oxide is used as the basis for controlling exposure, because as higher concentrations are used, quantification becomes easier.
Analytical Measurement
Most of the procedures described for measuring residual anaesthetics in air are based on the capture of these compounds by adsorption or in an inert bag or container, later to be analysed by gas chromatography or infrared spectroscopy (Guardino and Rosell 1985). Gas chromatography is also employed to measure nitrous oxide in urine (Rosell, Luna and Guardino 1989), while isoflurane is not readily metabolized and is therefore seldom measured.
Common Levels of Residual Concentrations in the Air of Operating Rooms
In the absence of preventive measures, such as the extraction of residual gases and/or introducing an adequate supply of new air into the operating suite, personal concentrations of more than 6,000 ppm of nitrous oxide and 85 ppm of halothane have been measured (NIOSH 1977). Concentrations of up to 3,500 ppm and 20 ppm, respectively, in the ambient air of operating rooms, have been measured. The implementation of corrective measures can reduce these concentrations to values below the environmental limits cited earlier (Rosell, Luna and Guardino 1989).
Factors that Affect the Concentration of Waste Anaesthetic Gases
The factors which most directly affect the presence of waste anaesthetic gases in the environment of the operating room are the following.
Method of anaesthesia. The first question to consider is the method of anaesthesia, for example, whether or not the patient is intubated and the type of face mask being used. In dental, laryngeal or other forms of surgery in which intubation is precluded, the patient’s expired air would be an important source of emissions of waste gases, unless equipment specifically designed to trap these exhalations is properly placed near the patient’s breathing zone. Accordingly, dental and oral surgeons are considered to be particularly at risk (Cohen, Belville and Brown 1975; NIOSH 1977a), as are veterinary surgeons (Cohen, Belville and Brown 1974; Moore, Davis and Kaczmarek 1993).
Proximity to the focus of emission. As is usual in industrial hygiene, when the known point of emission of a contaminant exists, proximity to the source is the first factor to consider when dealing with personal exposure. In this case, the anaesthetists and their assistants are the persons most directly affected by the emission of waste anaesthetic gases, and personal concentrations have been measured in the order of two times the average levels found in the air of operating rooms (Guardino and Rosell 1985).
Type of circuit. It goes without saying that in the few cases in which closed circuits are used, with reinspiration after the cleansing of the air and the resupply of oxygen and the necessary anaesthetics, there will be no emissions except in the case of equipment malfunction or if a leak exists. In other cases, it will depend on the characteristics of the system used, as well as on whether or not it is possible to add an extraction system to the circuit.
The concentration of anaesthetic gases. Another factor to take into account is the concentrations of the anaesthetics used since, obviously, those concentrations and the amounts found in the air of the operating room are directly related (Guardino and Rosell 1985). This factor is especially important when it comes to surgical procedures of long duration.
Type of surgical procedures. The duration of the operations, the time elapsed between procedures done in the same operating room and the specific characteristics of each procedure—which often determine which anaesthetics are used—are other factors to consider. The duration of the operation directly affects the residual concentration of anaesthetics in the air. In operating rooms where procedures are scheduled successively, the time elapsed between them also affects the presence of residual gases. Studies done in large hospitals with uninterrupted use of the operating rooms or with emergency operating rooms that are used beyond standard work schedules, or in operating rooms used for prolonged procedures (transplants, laryngotomies), show that substantial levels of waste gases are detected even before the first procedure of the day. This contributes to increased levels of waste gases in subsequent procedures. On the other hand, there are procedures that require temporary interruptions of inhalation anaesthesia (where extracorporeal circulation is needed, for example), and this also interrupts the emission of waste anaesthetic gases into the environment (Guardino and Rosell 1985).
Characteristics specific to the operating room. Studies done in operating rooms of different sizes, design and ventilation (Rosell, Luna and Guardino 1989) have demonstrated that these characteristics greatly influence the concentration of waste anaesthetic gases in the room. Large and non-partitioned operating rooms tend to have the lowest measured concentrations of waste anaesthetic gases, while in small operating rooms (e.g., paediatric operating rooms) the measured concentrations of waste gases are usually higher. The general ventilation system of the operating room and its proper operation is a fundamental factor for the reduction of the concentration of waste anaesthetics; the design of the ventilation system also affects the circulation of waste gases within the operating room and the concentrations in different locations and at various heights, something that can be easily verified by carefully taking samples.
Characteristics specific to the anaesthesia equipment. The emission of gases into the environment of the operating room depends directly on the characteristics of the anaesthesia equipment used. The design of the system, whether it includes a system for the return of excess gases, whether it can be attached to a vacuum or vented out of the operating room, whether it has leaks, disconnected lines and so on are always to be considered when determining the presence of waste anaesthetic gases in the operating room.
Factors specific to the anaesthetist and his or her team. The anaesthetist and his or her team are the last element to consider, but not necessarily the least important. Knowledge of the anaesthesia equipment, of its potential problems and the level of maintenance it receives—both by the team and by the maintenance staff in the hospital—are factors that affect very directly the emission of waste gases into the air of the operating room (Guardino and Rosell 1995). It has been clearly shown that, even when using adequate technology, the reduction of the ambient concentrations of anaesthetic gases cannot be achieved if a preventive philosophy is absent from the work routines of anaesthetists and their assistants (Guardino and Rosell 1992).
Preventive Measures
The basic preventive actions required to reduce occupational exposure to waste anaesthetic gases effectively can be summarized in the following six points:
- Anaesthetic gases should be thought of as occupational hazards. Even if from a scientific standpoint it has not been conclusively shown that anaesthetic gases have a serious deleterious effect on the health of people who are occupationally exposed, there is a high probability that some of the effects mentioned here are directly related to the exposure to waste anaesthetic gases. For that reason it is a good idea to consider them toxic occupational hazards.
- Scavenger systems should be used for waste gases. Scavenger systems are the most effective technical hardware for the reduction of waste gases in the air of the operating room (NIOSH 1975). These systems must fulfil two basic principles: they must store and/or adequately eliminate the whole volume of air expired by the patient, and they must be designed to guarantee that neither the respiration of the patient nor the proper functioning of the anaesthesia equipment will be affected—with separate safety devices for each function. The techniques most commonly employed are: a direct connection to a vacuum outlet with a flexible regulating chamber that allows for the discontinuous emission of gases of the respiratory cycle; directing the flow of the gases exhaled by the patient to the vacuum without a direct connection; and directing the flow of gases coming from the patient to the return of the ventilation system installed in the operating room and expelling these gases from the operating room and from the building. All these systems are technically easy to implement and very cost-efficient; the use of installed respirators as part of the design is recommended. In cases where systems that eliminate waste gases directly cannot be used because of the special characteristics of a procedure, localized extraction can be employed near the source of emission as long as it does not affect the general ventilation system or the positive pressure in the operating room.
- General ventilation with a minimum of 15 renewals/hour in the operating room should be guaranteed. The general ventilation of the operating room should be perfectly regulated. It should not only maintain positive pressure and respond to the thermohygrometric characteristics of the ambient air, but should also provide a minimum of 15 to 18 renewals per hour. Also, a monitoring procedure should be in place to ensure its proper functioning.
- Preventive maintenance of the anaesthesia circuit should be planned and regular. Preventive maintenance procedures should be set up that include regular inspections of the respirators. Verifying that no gases are being emitted to the ambient air should be part of the protocol followed when the equipment is first turned on, and its proper functioning with regard to the safety of the patient should be checked. The proper functioning of the anaesthesia circuit should be verified by checking for leaks, periodically replacing filters and checking the safety valves.
- Environmental and biological controls should be used. The implementation of environmental and biological controls provides information not only about the correct functioning of the various technical elements (extraction of gases, general ventilation) but also about whether the working procedures are adequate for curtailing the emission of waste gases into the air. Today these controls do not present technical problems and they can be implemented economically, which is why they are recommended.
- Education and training of the exposed personnel is crucial. Achieving an effective reduction of occupational exposure to waste anaesthetic gases requires educating all operating room personnel about the potential risks and training them in the required procedures. This is particularly applicable to anaesthetists and their assistants who are most directly involved and those responsible for the maintenance of the anaesthesia and air-conditioning equipment.
Conclusion
Although not definitively proven, there is enough evidence to suggest that exposures to waste anaesthetic gases may be harmful to HCWs. Stillbirths and congenital malformations in infants born to female workers and to the spouses of male workers represent the major forms of toxicity. Since it is technically feasible at a low cost, it is desirable to reduce the concentration of these gases in the ambient air in operating rooms and adjacent areas to a minimum. This requires not only the use and correct maintenance of anaesthesia equipment and ventilation/air conditioning systems but also the education and training of all personnel involved, especially anaesthetists and their assistants, who generally are exposed to higher concentrations. Given the work conditions peculiar to operating rooms, indoctrination in the correct work habits and procedures is very important in trying to reduce the amounts of anaesthetic waste gases in the air to a minimum.
Home Care Workers: The New York City Experience
Massive use of home care workers in New York City began in 1975 as a response to the needs of the growing population of chronically ill and frail elderly and as an alternative to more expensive care in nursing homes, many of which had long lists of such people waiting for admission. Additionally, it allowed for more personal assistance at a time when nursing homes were perceived as impersonal and uncaring. It also provided entry-level employment to unskilled individuals, mostly women, many of whom were recipients of welfare.
Initially, these workers were employees of the City’s Department of Human Resources but, in 1980, this service was “privatized” and they were recruited, trained and employed by non-profit, community-based social agencies and traditional health care organizations such as hospitals which had to be certified by the State of New York as providers of home care services. The workers are categorized as home makers, personal care workers, health aides, home care attendants and housekeepers, depending on their levels of skills and the kinds of services they provide. Which of these services a particular client uses depends on an evaluation of that person’s health status and needs which is conducted by a licensed health professional, such as a physician, nurse or social worker.
The Home Care Workforce
Home care workers in New York City present a conglomerate of characteristics that provide a unique profile. A recent survey by Donovan, Kurzman and Rotman (1993) found that 94% are female with an average age of 45. About 56% were not born within the continental US and about 51% never completed high school. Only 32% were identified as married, 33% were separated or divorced and 26% were single, while 86% have children, 44% with children under 18 years of age. According to the survey, 63% live with their children and 26% live with a spouse.
The median family income for this group in 1991 was $12,000 per year. In 81% of these families, the home care worker was the primary breadwinner. In 1996, the annual salary of full-time home care workers’ ranged between $16,000 and $28,000; part-time workers earned less.
Such low earnings represent significant economic hardship to the survey respondents: 56% said they could not afford adequate housing; 61% reported being unable to afford furniture or household equipment; 35% said they lacked funds to purchase enough food for their families; and 36% were ineligible for Medicare and unable to afford needed medical care for themselves and their families. As a group, their financial status will inevitably worsen as cuts in government funding force curtailment of the amount and intensity of home care services being provided.
Home Care Services
The services provided by home care workers depend on the needs of the clients being served. Those with greater disability require assistance with the “basic activities of daily living”, which consist of bathing, dressing, toileting, transferring (moving in or out of bed and chairs) and feeding. Those with higher levels of functional capacity need help with the “instrumental activities of daily living”, which comprise housekeeping (cleaning, bed making, dishwashing, and so forth), shopping, food preparation and serving, laundry, using public or private transportation and managing finances. Home care workers may give injections, dispense medications and provide such treatments as passive exercise and massage as prescribed by the client’s physician. A most appreciated service is companionship and assisting the client to participate in recreational activities.
The difficulty of the home care worker’s job is directly related to the home environment and, in addition to physical status, the behaviour of the client and any family members who may be on the scene. Many clients (and the workers as well) live in poor neighbourhoods where crime rates are high, public transportation often marginal and public services substandard. Many live in deteriorated housing with no or non-functioning elevators, dark and dirty stairwells and hallways, lack of heat and hot water, dilapidated plumbing and poorly functioning household appliances. Commuting to and from the client’s home may be arduous and time-consuming.
Many of the clients may have very low levels of functional capacity and require assistance at every turn. Clients’ muscle weakness and lack of coordination, loss of vision and hearing and incontinence of bladder and/or bowels add to the burden of care. Mental difficulties such as senile dementia, anxiety and depression and difficulties in communication because of memory loss and language barriers may also magnify the difficulty. Finally, abusive and demanding behaviour on the part of both clients and their family members may sometimes escalate into acts of violence.
Home Care Work Hazards
Work hazards commonly encountered by home care workers include:
- working alone without assistance
- lack of education and training and remote, if any, supervision
- working in substandard housing in high risk neighbourhoods
- back pain and musculoskeletal injuries incurred while lifting, transferring and supporting clients who may be heavy, weak and poorly coordinated
- violence in the home and in the neighbourhood
- infectious diseases (the health care worker may not have been fully informed of the client’s medical status; recommended gloves, gowns and masks may not be available)
- household chemicals and cleaning supplies (often incorrectly labelled and stored)
- sexual harassment
- work stress.
Stress is probably the most ubiquitous hazard. It is compounded by the fact the worker is usually alone in the home with the client with no simple way to report trouble or summon assistance. Stress is being exacerbated as cost-containment efforts are reducing the hours of service allowed for individual clients.
Prevention Strategies
A number of strategies have been suggested to promote occupational health and safety for home care workers and to improve their lot. They include:
- development and promulgation of standards of practice for home care accompanied by improved education and training so that home care workers can meet them
- education and training in the recognition and avoidance of chemical and other hazards in the home
- training in lifting, carrying and giving physical support to clients as needed in the course of providing services
- preliminary needs assessment of clients supplemented by inspections of their homes so that potential hazards can be identified and eliminated or controlled and needed materials and equipment can be procured
- periodic meetings with supervisors and other home care workers to compare notes and receive instruction. Videotapes may be developed and used for skills demonstrations. The meetings may be supplemented by telephone networks through which workers may communicate with each other to exchange information and alleviate any feelings of isolation.
- establishment of a health and safety committee within each agency to review work-related accidents and problems and develop appropriate preventive interventions
- establishment of an Employee Assistance Programme (EAP) through which the workers may receive counselling for their own psychosocial problems both on- and off-the-job.
Educational and training sessions should be conducted during working hours at a place and time convenient for the workers. They should be supplemented by the distribution of instructional materials designed for the low educational levels of most of the workers and, when necessary, they should be multilingual.
Case study: Violence in health care work
A psychotic patient in his thirties had been forcibly committed to a large psychiatric hospital in the suburbs of a city. He was not regarded as having violent tendencies. After a few days he escaped from his secure ward. The hospital authorities were informed by his relatives that he had returned to his own house. As was routine an escort of three male psychiatric nurses set out with an ambulance to bring the patient back. En route they stopped to pick up a police escort as was routine in such cases. When they arrived at the house, the police escort waited outside, in case a violent incident developed. The three nurses entered and were informed by the relatives that the patient was sitting in an upstairs bedroom. When approached and quietly invited to come back to hospital for treatment the patient produced a kitchen knife which he had hidden. One nurse was stabbed in the chest, another a number of times in the back and the third in the hand and the arm. All three nurses survived but had to spend time in hospital. When the police escort entered the bedroom the patient quietly surrendered the knife.
Daniel Murphy
Health Care Workers and Latex Allergy
With the advent of the universal precautions against bloodborne infections which dictate the use of gloves whenever HCWs are exposed to patients or materials that might be infected with hepatitis B or HIV, the frequency and severity of allergic reactions to natural rubber latex (NRL) have zoomed upward. For example, the Department of Dermatology at the Erlangen-Nuremberg University in Germany reported a 12-fold increase in the number of patients with latex allergy between 1989 and 1995. More serious systemic manifestations increased from 10.7% in 1989 to 44% in 1994-1995 (Hesse et al. 1996).
It seems ironic that so much difficulty is attributable to rubber gloves when they were intended to protect the hands of nurses and other HCWs when they were originally introduced toward the end of the nineteenth century. This was the era of antiseptic surgery in which instruments and operative sites were bathed in caustic solutions of carbolic acid and bichloride of mercury. These not only killed germs but they also macerated the hands of the surgical team. According to what has become a romantic legend, William Stewart Halsted, one of the surgical “giants” of the time who is credited with a host of contributions to the techniques of surgery, is said to have “invented” rubber gloves around 1890 to make it more pleasant to hold hands with Caroline Hampton, his scrub nurse, whom he later married (Townsend 1994). Although Halsted may be credited with introducing and popularizing the use of rubber surgical gloves in the United States, many others had a hand in it, according to Miller (1982) who cited a report of their use in the United Kingdom published a half century earlier (Acton 1848).
Latex Allergy
Allergy to NRL is succinctly described by Taylor and Leow (see the article “Rubber contact dermatitis and latex allergy” in the chapter Rubber industry) as “an immunoglobulin E-mediated, immediate, Type I allergic reaction, most always due to NRL proteins present in medical and non-medical latex devices. The spectrum of clinical signs ranges from contact urticaria, generalized urticaria, allergic rhinitis, allergic conjunctivitis, angioedema (severe swelling) and asthma (wheezing) to anaphylaxis (severe, life-threatening allergic reaction)”. Symptoms may result from direct contact of normal or inflamed skin with gloves or other latex-containing materials or indirectly by mucosal contact with or inhalation of aerosolized NRL proteins or talcum powder particles to which NRL proteins have adhered. Such indirect contact can cause a Type IV reaction to the rubber accelerators. (Approximately 80% of “latex glove allergy” is actually a Type IV reaction to the accelerators.) The diagnosis is confirmed by patch, prick, scratch or other skin sensitivity tests or by serological studies for the immune globulin. In some individuals, the latex allergy is associated with allergy to certain foods (e.g., banana, chestnuts, avocado, kiwi and papaya).
While most common among health care workers, latex allergy is also found among employees in rubber manufacturing plants, other workers who habitually use rubber gloves (e.g., greenhouse workers (Carillo et al. 1995)) and in patients with a history of multiple surgical procedures (e.g., spina bifida, congenital urogenital abnormalities, etc.) (Blaycock 1995). Cases of allergic reactions after the use of latex condoms have been reported (Jonasson, Holm and Leegard 1993), and in one case, a potential reaction was averted by eliciting a history of an allergic reaction to a rubber swimming cap (Burke, Wilson and McCord 1995). Reactions have occurred in sensitive patients when hypodermic needles used to prepare doses of parenteral medications picked up NRL protein as they were pushed through the rubber caps on the vials.
According to a recent study of 63 patients with NRL allergy, it took an average of 5 years of working with latex products for the first symptoms, usually a contact urticaria, to develop. Some also had rhinitis or dyspnoea. It took, on average, an additional 2 years for the appearance of lower respiratory tract symptoms (Allmeers et al. 1996).
Frequency of latex allergy
To determine the frequency of NRL allergy, allergy tests were performed on 224 employees at the University of Cincinnati College of Medicine, including nurses, laboratory technicians, physicians, respiratory therapists, housekeeping and clerical workers (Yassin et al. 1994). Of these, 38 (17%) tested positive to latex extracts; the incidence ranged from 0% among housekeeping workers to 38% among dental staff. Exposure of these sensitized individuals to latex caused itching in 84%, a skin rash in 68%, urticaria in 55%, lachrymation and ocular itching in 45%, nasal congestion in 39% and sneezing in 34%. Anaphylaxis occurred in 10.5%.
In a similar study at the University of Oulo in Finland, 56% of 534 hospital employees who used protective latex or vinyl gloves on a daily basis had skin disorders related to the usage of the gloves (Kujala and Reilula 1995). Rhinorrhoea or nasal congestion was present in 13% of workers who used powdered gloves. The prevalence of both skin and respiratory symptoms was significantly higher among those who used the gloves for more than 2 hours a day.
Valentino and colleagues (1994) reported latex induced asthma in four health care workers in an Italian regional hospital, and the Mayo Medical Center in Rochester Minnesota, where 342 employees who reported symptoms suggestive of latex allergy were evaluated, recorded 16 episodes of latex-related anaphylaxis in 12 subjects (six episodes occurred after skin testing) (Hunt et al. 1995). The Mayo researchers also reported respiratory symptoms in workers who did not wear gloves but worked in areas where large numbers of gloves were being used, presumably due to air-borne talcum powder/latex protein particles.
Control and Prevention
The most effective preventive measure is modification of standard procedures to replace the use of gloves and equipment made with NRL with similar items made of vinyl or other non-rubber materials. This requires involvement of the purchasing and supply departments, which should also mandate the labelling of all latex-containing items so that they may be avoided by individuals with latex sensitivity. This is important not only to the staff but also to patients who may have a history suggestive of latex allergy. Aerosolized latex, from latex powder, is also problematic. HCWs who are allergic to latex and who do not use latex gloves may still be affected by the powdered latex gloves used by co-workers. A significant problem is presented by the wide variation in content of latex allergen among gloves from different manufacturers and, indeed, among different lots of gloves from the same manufacturer.
Glove manufacturers are experimenting with gloves using formulations with smaller amounts of NRL as well as coatings that will obviate the need for talcum powder to make the gloves easy to put on and take off. The goal is to provide comfortable, easy to wear, non-allergenic gloves that still provide effective barriers to the transmission of the hepatitis B virus, HIV and other pathogens.
A careful medical history with a particular emphasis on prior latex exposures should be elicited from all health care workers who present symptoms suggestive of latex allergy. In suspect cases, evidence of latex sensitivity may be confirmed by skin or serological testing. Since there is evidently a risk of provoking an anaphylactic reaction, the skin testing should only be performed by experienced medical personnel.
At the present time, allergens for desensitization are not available so that the only remedy is avoidance of exposure to products containing NRL. In some instances, this may require a change of job. Weido and Sim (1995) at the University of Texas Medical Branch at Galveston suggest advising individuals in high-risk groups to carry self-injectable epinephrine to use in the event of a systemic reaction.
Following the appearance of several clusters of latex allergy cases in 1990, the Mayo Medical Center in Rochester, Minnesota, formed a multidisciplinary work group to address the problem (Hunt et al. 1996). Subsequently, this was formalized in a Latex Allergy Task Force with members from the departments of allergy, preventive medicine, dermatology and surgery as well as the Director of Purchasing, the Surgical Nursing Clinical Director and the Director of Employee Health. Articles on latex allergy were published in staff newsletters and information bulletins to educate the 20,000 member workforce to the problem and to encourage those with suggestive symptoms to seek medical consultation. A standardized approach to testing for latex sensitivity and techniques for quantifying the amount of latex allergen in manufactured products and the amount and particle size of air-borne latex allergen were developed. The latter proved to be sufficiently sensitive to measure the exposure of individual workers while performing particular high-risk tasks. Steps were initiated to monitor a gradual transition to low-allergen gloves (an incidental effect was a lowering of their cost by concentrating glove purchases among the fewer vendors who could meet the low allergen requirements) and to minimize exposures of staff and patients with known sensitivity to NLR.
To alert the public to the risks of NLR allergy, a consumer group, the Delaware Valley Latex Allergy Support Network has been formed. This group has created an Internet website (http://www.latex.org) and maintains a toll-free telephone line (1-800 LATEXNO) to provide up-to-date factual information about latex allergy to persons with this problem and those who care for them. This organization, which has a Medical Advisory Group, maintains a Literature Library and a Product Center and encourages the exchange of experiences among those who have had allergic reactions.
Conclusion
Latex allergies are becoming an increasingly important problem among health care workers. The solution lies in minimizing contact with latex allergen in their work environment, especially by substituting non-latex surgical gloves and appliances.
Case Study: Violence in Health Care Work
A psychotic patient in his thirties had been forcibly committed to a large psychiatric hospital in the suburbs of a city. He was not regarded as having violent tendencies. After a few days he escaped from his secure ward. The hospital authorities were informed by his relatives that he had returned to his own house. As was routine an escort of three male psychiatric nurses set out with an ambulance to bring the patient back. En route they stopped to pick up a police escort as was routine in such cases. When they arrived at the house, the police escort waited outside, in case a violent incident developed. The three nurses entered and were informed by the relatives that the patient was sitting in an upstairs bedroom. When approached and quietly invited to come back to hospital for treatment the patient produced a kitchen knife which he had hidden. One nurse was stabbed in the chest, another a number of times in the back and the third in the hand and the arm. All three nurses survived but had to spend time in hospital. When the police escort entered the bedroom the patient quietly surrendered the knife.
Occupational Health and Safety Practice: The Russian Experience
The work of people in the medical profession has great social value, and in recent years the urgent problem of the labour conditions and the state of health of HCWs has been studied actively. However, the nature of this work is such that any preventive and ameliorating measures cannot eliminate or reduce the main source of the hazards in the work of physicians and other HCWs: contact with a sick patient. In this respect the problem of prevention of occupational illness in medical workers is rather complicated.
In many cases the diagnostic and medical equipment and the methods of treatment used in medical institutions can affect the health of HCWs. Therefore, it is necessary to follow hygienic standards and precautionary measures to control the levels of exposure to unfavourable factors. Studies carried out in a number of Russian medical institutions have revealed that the labour conditions at many workplaces were not optimum and could induce the deterioration of the health of medical and support personnel, and sometimes cause the development of occupational diseases.
Among the physical factors that can substantially affect the health of medical personnel in the Russian Federation, ionizing radiation should be ranked as one of the first. Tens of thousands of Russian medical workers encounter sources of ionizing radiation at work. In the past, special laws were adopted to limit the doses and levels of irradiation at which specialists could work for a long period without health risk. In recent years x-ray control procedures were extended to cover not only radiologists, but surgeons, anaesthetists, traumatologists, rehabilitation specialists and mid-level personnel. The levels of radiation at worksites and the x-ray doses received by these individuals sometimes are even higher than the doses received by the radiologists and radiology laboratory assistants.
Instruments and equipment generating non-ionizing radiation and ultrasound are also widespread in modern medicine. Since many physiotherapy procedures are used precisely because of the therapeutic benefits of such treatment, the same biological effects may be hazardous to those involved in administering them. Persons encountering instruments and machines generating non-ionizing radiation are often reported to have functional disturbances in the nervous and cardiovascular systems.
Studies of working conditions where ultrasound is used for diagnostic or therapeutic procedures revealed that the personnel were exposed during as much as 85 to 95% of their working day to levels of high frequency, low intensity ultrasound comparable to the exposures experienced by operators of industrial ultrasonic defectoscopy. They experienced such impairments of the peripheral neuro-vascular system as angiodistonic syndrome, vegetative polyneuritis, vegetative vascular malfunction and so on.
Noise is rarely reported as a substantial factor of occupational risk in the work of Russian medical personnel, except at dental institutions. When using high-speed drills (200,000 to 400,000 rev/min) the maximum energy of the sound falls at a frequency of 800 Hz. The noise levels at a distance of 30 cm from the drill placed in the mouth of the patient vary from 80 to 90 dBA. One-third of the whole sound spectrum falls within the range most harmful to the ear (i.e., between 1000 and 2000 Hz).
Many noise sources gathered in one place can generate levels exceeding permissible limits. To create optimum conditions it is recommended that anaesthetizing machines, respiratory equipment and artificial blood circulation pumps be taken out of operating rooms.
In surgery departments, especially in operating rooms and in rehabilitation and intensive care departments, as well as in some other special rooms, it is necessary to maintain the required parameters of temperature, humidity and air circulation. The optimal layout of modern medical institutions and the installation of ventilation and air-conditioning plants provide the favourable microclimate.
However, in operating suites built without optimal planning, occlusive clothing (i.e., gowns, masks, caps and gloves) and exposure to heat from lighting and other equipment lead many surgeons and other members of the operating teams to complain of “overheating”. Perspiration is mopped from surgeons’ brows lest it interfere with their vision or contaminate the tissues in the surgical field.
As a result of the introduction into medical practice of treatment in hyperbaric chambers, physicians and nurses now are often exposed to heightened atmospheric pressure. In most cases this affects surgical teams performing operations in such chambers. Exposure to conditions of increased atmospheric pressure is believed to lead to unfavourable changes in a number of body functions, depending on the level of the pressure and the duration of the exposure.
Working posture is also of great importance for physicians. Although most tasks are performed in sitting or standing positions, some activities require long periods in awkward and uncomfortable positions. This is particularly the case with dentists, otologists, surgeons (especially microsurgeons), obstetricians, gynaecologists and physiotherapists. Work requiring long periods of standing in one position has been associated with the development of varicose veins in the legs and haemorrhoids.
Continual, intermittent or casual exposure to potentially hazardous chemicals used in medical institutions also can affect medical personnel. Among these chemicals, inhalation anaesthetics are considered to have the most unfavourable influence on humans. These gases can accumulate in large amounts not only in operating and delivery rooms but also in pre-op areas where anaesthesia is induced and in recovery rooms where they are exhaled by patients coming out of anaesthesia. Their concentration depends on the content of the gas mixtures being administered, the type of equipment being used and the duration of the procedure. Concentrations of anaesthetic gases in the breathing zones of surgeons and anaesthetists in the operating room have been found ranging from 2 to 14 times the maximum allowable concentration (MAC). Exposure to anaesthetic gases has been associated with impaired reproductive capacity of both male and female anaesthetists and abnormalities in the foetuses of pregnant female anaesthetists and the spouses of male anaesthetists (see chapter Reproductive system and the article “Waste anaesthetic gases" in this chapter).
In the treatment rooms where many injections are performed, the concentration of a medicine in the respiration zone of nurses can exceed permissible levels. Airborne drug exposure can happen when washing and sterilizing syringes, removing air bubbles from a syringe, and while dispensing aerosol therapy.
Among chemicals which could affect the health of medical personnel are hexachlorophene (possibly causing teratogenic effects), formalin (an irritant, sensitizer and carcinogen), ethylene oxide (which has toxic, mutagenic and carcinogenic characteristics), antibiotics that cause allergies and suppressed immune response, vitamins and hormones. There is also the possibility of exposure to industrial chemicals used in cleaning and maintenance work and as insecticides.
Many of the drugs used in the treatment of cancer are themselves mutagenic and carcinogenic. Special training programmes have been developed to prevent workers involved in preparing and administering them from exposure to such cytotoxic agents.
One of the features of job assignments of medical workers of many specialties is contact with infected patients. Any infectious disease incurred as a result of such contact is considered to be an occupational one. Viral serum hepatitis has proved to be the most dangerous for the staff of medical institutions. Viral hepatitis infections of laboratory assistants (from examining blood samples), staff members of haemodialysis departments, pathologists, surgeons, anaesthetists and other specialists who had occupational contact with the blood of infected patients have been reported (see the article “Prevention of occupational transmission of bloodborne pathogens” in this chapter).
There has apparently been no recent improvement in the health status of HCWs in the Russian Federation. The proportion of cases of work-related, temporary disability remained at the level of 80 to 96 per 100 working doctors and 65 to 75 per 100 mid-level medical workers. Although this measure of work loss is quite high, it should also be noted that self-treatment and informal, unreported treatment are widespread among HCWs, which means that many cases are not captured by the official statistics. This was confirmed by a survey among physicians which found that 40% of the respondents were ill four times a year or more but did not apply to a practising physician for medical care and did not submit a disability form. These data were corroborated by medical examinations which found evidence of disability in 127.35 cases per 100 workers examined.
Morbidity also increases with age. In these examinations, it was six times more frequent among HCWs with 25 years of service than among those with less than 5 years of service. The most common diseases included circulatory impairments (27.9%), diseases of the digestive organs (20.0%) and musculoskeletal disorders (20.72%). Except for the last, most of the cases were non-occupational in origin.
Sixty per cent of doctors and 46% of mid-level personnel were found to have chronic diseases. Many of these were directly associated with job assignments.
Many of the observed diseases were directly associated with job assignments of those examined. Thus, microsurgeons working in an awkward posture were found to have frequent osteochondroses; chemotherapists were found to suffer frequently from chromosome abnormalities and anaemia; nurses who were in contact with a large variety of medicines suffered various allergic diseases, ranging from dermatoses to bronchial asthma and immunodeficiency.
In Russia, health problems of medical workers were first addressed in the 1920s. In 1923 a special scientific-consultative bureau was founded in Moscow; the results of its studies were published in five collections entitled Labour and Life of Medical Workers of Moscow and Moscow Province. Since that time other studies have appeared devoted to this problem. But this work has been carried on in the most fruitful way only since 1975, when the Laboratory of Labour Hygiene of Medical Workers was established in the RAMS Institute of Occupational Health, which coordinated all the studies of this problem. After analysis of the then-current situation, research was directed at:
- studies of the features of labour processes in the main medical specialties
- assessment of the factors of the occupational environment
- analysis of the morbidity of medical workers
- elaboration of measures for optimization of labour conditions, reduction of fatigue and prevention of morbidity.
Based on the studies carried out by the Laboratory and other institutions, a number of recommendations and suggestions were prepared, aimed at reduction and prevention of the occupational diseases of medical workers.
Instructions were established for pre-employment and periodic medical examinations of health care workers. The aim of these examinations was to determine the fitness of the worker for the job and to prevent common and occupational diseases as well as occupational accidents. A list of hazardous and dangerous factors in the work of medical personnel was prepared which included recommendations for frequency of examinations, the range of specialists to take part in the examinations, the number of laboratory and functional studies as well as a list of medical contra-indications for work with a specific hazardous occupational factor. For every studied group there was a list of occupational diseases, enumerating the nosological forms, approximate list of job assignments and hazardous factors which can cause the respective occupational conditions.
In order to control the working conditions in treatment and prevention institutions, a Certificate of Sanitary and Technical Conditions of Labour in the health care institutions was developed. The certificate can be used as a guide for conducting sanitary measures and improvement of labour safety. For an institution to complete the certificate, it is necessary to carry out a study, with the help of specialists in sanitary service and other respective organizations, of the general situation in the departments, rooms and wards, to measure the levels of health and safety hazards.
Departments of hygiene of the preventive medicine institutions have been established in the modern centres of sanitary-epidemic inspections. The mission of these departments includes perfecting measures for the prevention of nosocomial infections and their complications in hospitals, creating optimal conditions for treatment and protecting the safety and health of HCWs. Public health doctors and their assistants conduct the preventive monitoring of design and construction of buildings for health care institutions. They see to the compliance of the new premises with the climate conditions, required arrangement of worksites, comfortable labour conditions and systems of rest and nutrition during the work shifts (see the article “Buildings for health care facilities” in this chapter). They also control technical documentation for the new equipment, technological procedures and chemicals. The routine sanitary inspection includes the monitoring of the occupational factors at the worksites and accumulation of the received data in the above-mentioned Certificate of Sanitary and Technical Conditions of Labour. Quantitative measurement of working conditions and prioritization of health improvement measures are established according to hygienic criteria for assessments of labour conditions which are based on indicators of the hazard and danger of labour environment factors and the heaviness and intensity of the working process. The frequency of laboratory studies is determined by the specific needs of each case. Each study usually includes measurement and analysis of microclimate parameters; measurement of indicators of air environment (e.g., content of bacteria and hazardous substances); assessment of the effectiveness of ventilation systems; assessment of the levels of natural and artificial illumination; and measurement of noise levels, ultrasound, ionizing radiation and so on. It is also recommended that time-keeping monitoring of the exposures of the unfavourable factors be conducted, based on the guideline documents.
According to instructions of the Russian government, and in keeping with current existing practice, the hygienic and medical standards should be revised following the accumulation of new data.
More...
Case Study: Human Error and Critical Tasks: Approaches for Improved System Performance
Health error and critical tasks in remote afterloading brachytherapy: Approaches for improved system performance
Remote afterloading btachytherapy (RAB) is a medical process used in the treatment of cancer. RAB uses a computer-controlled device to remotely insert and remove radioactive sources, close to a target (or tumour) in the body. Problems related to the dose delivered during RAB have been reported and attributed to human error (Swann-D'Emilia, Chu and Daywalt 1990). Callan et al. (1995) evaluated human error and critical tasks associated with RAB in 23 sites in the United States. Evaluation included six phases:
Phase 1: Functions and tasks. Preparation for treatment was considered to be the most difficult task, as it was responsible for the greatest cognitive strain. In addition, distractions had the greatest effect on preparation.
Phase 2: Human-system interferences. Personnel were often unfamiliar with interfaces they used infrequently. Operators were unable to see control signals or essential information from their workstations. In many cases, information on the state of the system was not given to the operator.
Phase 3: Procedures and practices. Because procedures used to move from one operation to the next, and those used to transmit information and equipment between tasks, were not well defined, essential information could be lost. Verification procedures were often absent, poorly constructed or inconsistent.
Phase 4: Training policies. The study revealed the absence of formal training programmes at most sites.
Phase 5: Organizational support structures. Communication during RAB was particularly subject to error. Quality-control procedures were inadequate.
Phase 6: Identification and classification or circumstances favouring human error. In all, 76 factors favouring human error were identified and categorized. Alternative approaches were identified and evaluated.
Ten critical tasks were subject to error:
- patient scheduling, identification and tracking
- applicator placement stabilization
- large volume localization
- dwell position localization
- dosimetry
- treatment set-up
- treatment plan entry
- source exchange
- source calibration
- record-keeping and routine quality assurance
Treatment was the function associated with the greatest number of errors. Thirty treatment-related errors were analysed and errors were found to occur during four or five treatment sub-tasks. The majority of errors occurred during treatment delivery. The second-highest number of errors were associated with the planning of treatment and were related to the calculation of dose. Improvements of eqiupment and documentation are under way, in collaboration with manufacturers.
Buildings for Health Care Facilities
The health maintenance and enhancement, the safety and the comfort of people in health care facilities are seriously affected if specific building requirements are not met. Health care facilities are rather unique buildings, in which heterogeneous environments coexist. Different people, several activities in each environment and many risk factors are involved in the pathogenesis of a broad spectrum of diseases. Functional organization criteria classify health care facility environments as follows: nursing units, operating theatres, diagnostic facilities (radiology unit, laboratory units and so on), outpatients’ departments, administration area (offices), dietary facilities, linen services, engineering services and equipment areas, corridors and passages. The group of people which attends a hospital is composed of health personnel, staff personnel, patients (long-stay inpatients, acute inpatients and outpatients) and visitors. The processes include health care specific activities—diagnostic activities, therapeutic activities, nursing activities—and activities common to many public buildings—office work, technological maintenance, food preparation and so on. The risk factors are physical agents (ionizing and non-ionizing radiation, noise, lighting and microclimatic factors), chemicals (e.g., organic solvents and disinfectants), biological agents (viruses, bacteria, fungi and so on), ergonomics (postures, lifting and so on) and psychological and organizational factors (e.g., environmental perceptions and work hours). The illnesses related to the above-mentioned factors range from environmental annoyance or discomfort (e.g., thermal discomfort or irritative symptoms) to severe diseases (e.g., hospital-acquired infections and traumatic accidents). In this perspective, the risk assessment and control require an interdisciplinary approach involving physicians, hygienists, engineers, architects, economists and so on and fulfilment of preventive measures in the building planning, design, construction and management tasks. Specific building requirements are extremely important among these preventive measures, and, according to the guidelines for healthy buildings introduced by Levin (1992), they should be classified as follows:
- site planning requirements
- architectural design requirements
- requirements for building materials and furnishings
- requirements for heating, ventilation and air-conditioning systems and for microclimatic conditions.
This article focuses on general hospital buildings. Obviously, adaptations would be required for specialty hospitals (e.g., orthopaedic centres, eye and ear hospitals, maternity centres, psychiatric institutions, long-term care facilities and rehabilitation institutes), for ambulatory care clinics, emergency/urgent care facilities and offices for individual and group practices. These will be determined by the numbers and types of patients (including their physical and mental status) and by the number of HCWs and the tasks they perform. Considerations promoting the safety and well-being of both patients and staff that are common to all health care facilities include:
- ambience, including not only decoration, lighting and noise control but also partitioning and placement of furniture and equipment that avoid entrapment of workers with potentially violent patients and visitors
- ventilation systems that minimize exposure to infectious agents and potentially toxic chemicals and gases
- storage facilities for clothing and effects of patients and their visitors that minimize potential contamination
- lockers, changing rooms, wash-up facilities and rest rooms for staff
- conveniently-located hand-washing facilities in each room and treatment area
- doorways, elevators and toilets that accommodate wheel chairs and stretchers
- storage and filing areas designed to minimize workers’ stooping, bending, reaching and heavy lifting
- automatic and worker-controlled communication and alarm systems
- mechanisms for collection, storage and disposition of toxic wastes, contaminated linens and clothing and so on.
Site Planning Requirements
The health care facility site must be chosen following four main criteria (Catananti and Cambieri 1990; Klein and Platt 1989; Decree of the President of Ministers Council 1986; Commission of the European Communities 1990; NHS 1991a, 1991b):
- Environmental factors. The terrain should be as level as possible. Ramps, escalators and elevators can offset sides of hills, but they hinder the access of elderly and handicapped people, adding both a higher cost to the project and an extra burden to fire departments and evacuation teams. Heavy wind sites should be avoided, and the area should be far from sources which create pollution and noise (especially factories and landfills). Radon and radon daughters levels should be assessed, and measures to reduce exposure should be taken. In colder climates, consideration should be given to embedding snow-melting coils in sidewalks, entrance ways and parking areas to minimize falls and other accidents.
- Geological configuration. Earthquake-prone areas should be avoided, or at least anti-seismic construction criteria must be followed. The site must be chosen following an hydrogeological assessment, to avoid water infiltrations into the foundations.
- Urbanistic factors. The site should be easily accessible to potential users, ambulances and service vehicles for goods supply and waste disposal. Public transportation and utilities (water, gas, electricity and sewers) should be available. Fire departments should be nearby, and fire-fighters and their apparatus should find ready access to all parts of the facility.
- Space availability. The site should allow some scope for expansion and provision of adequate car parking.
Architectural Design
Health care facilities architectural design usually follows several criteria:
- class of the health care facility: hospital (acute-care hospital, community hospital, rural hospital), large or small health care centre, nursing homes (extended care facilities, skilled nursing homes, residential care homes), general medical practice premise (NHS 1991a; NHS 1991b; Kleczkowski, Montoya-Aguilar and Nilsson 1985; ASHRAE 1987)
- catchment area dimensions
- management issues: costs, flexibility (susceptibility to adaptation)
- ventilation provided: an air-conditioned building is compact and deep with as small an amount of external walls as possible, to reduce the heat transfer between outside and inside; a naturally ventilated building is long and thin, to maximize exposure to breezes and to minimize internal distances from windows (Llewelyn-Davies and Wecks 1979)
- building/area ratio
- environmental quality: safety and comfort are extremely relevant targets.
The listed criteria lead health care facilities planners to choose the best building shape for each situation, ranging essentially from an extended horizontal hospital with scattered buildings to a monolithic vertical or horizontal building (Llewelyn-Davies and Wecks 1979). The first case (a preferable format for low-density buildings) is normally used for hospitals up to 300 beds, because of its low costs in construction and management. It is particularly considered for small rural hospitals and community hospitals (Llewelyn-Davies and Wecks 1979). The second case (usually preferred for high-density buildings) becomes cost-effective for hospitals with more than 300 beds, and it is advisable for acute-care hospitals (Llewelyn-Davies and Wecks 1979). The internal space dimensions and distribution have to cope with many variables, among which one can consider: functions, processes, circulation and connections to other areas, equipment, predicted workload, costs, and flexibility, convertibility and susceptibility of shared use. Compartments, exits, fire alarms, automatic extinction systems and other fire prevention and protection measures should follow local regulations. Furthermore, several specific requirements have been defined for each area in health care facilities:
1. Nursing units. Internal layout of nursing units usually follows one of the following three basic models (Llewelyn-Davies and Wecks 1979): an open ward (or “Nightingale” ward)—a broad room with 20 to 30 beds, heads to the windows, ranged along both walls; the “Rigs” layout—in this model beds were placed parallel to the windows, and, at first, they were in open bays on either side of a central corridor (as at Rigs Hospital in Copenhagen), and in later hospitals the bays were often enclosed, so that they became rooms with 6 to 10 beds; small rooms, with 1 to 4 beds. Four variables should lead the planner to choose the best layout: bed need (if high, an open ward is advisable), budget (if low, an open ward is the cheapest one), privacy needs (if considered high, small rooms are unavoidable) and intensive care level (if high, the open ward or Rigs layout with 6 to 10 beds are advisable). The space requirements should be at least: 6 to 8 square metres (sqm) per bed for open wards, inclusive of circulation and ancillary rooms (Llewelyn-Davies and Wecks 1979); 5 to 7 sqm/bed for multiple bedrooms and 9 sqm for single bedrooms (Decree of the President of Ministers Council 1986; American Institute of Architects Committee on Architecture for Health 1987). In open wards, toilet facilities should be close to patients’ beds (Llewelyn-Davies and Wecks 1979). For single and multiple bedrooms, handwashing facilities should be provided in each room; lavatories may be omitted where a toilet room is provided to serve one single-bed room or one two-bed room (American Institute of Architects Committee on Architecture for Health 1987). Nursing stations should be large enough to accommodate desks and chairs for record keeping, tables and cabinets for preparation of drugs, instruments and supplies, chairs for sit-down conferences with physicians and other staff members, a wash-up sink and access to a staff toilet.
2. Operating theatres. Two main classes of elements should be considered: operating rooms and service areas (American Institute of Architects Committee on Architecture for Health 1987). Operating rooms should be classified as follows:
- general operating room, needing a minimum clear area of 33.5 sqm.
- room for orthopaedic surgery (optional), needing enclosed storage space for splints and traction equipment
- room for cardiovascular surgery (optional), needing a minimum clear area of 44 sqm. In the clear area of the surgical suite, nearby the operating room, an additional pump room should be designed, where extracorporeal pump supplies and accessories are stored and serviced.
- room for endoscope procedures, needing a minimum clear area of 23 sqm
- rooms for waiting patients, induction of anaesthesia and recovery from anaesthesia.
Service areas should include: sterilizing facility with high-speed autoclave, scrub facilities, medical gas storage facilities and staff clothing change areas.
3. Diagnostic facilities: Each radiology unit should include (Llewelyn-Davies and Wecks 1979; American Institute of Architects Committee on Architecture for Health 1987):
- appointment desk and waiting areas
- diagnostic radiographic rooms, needing 23 sqm for fluoroscopic procedures and about 16 sqm for radiographic ones, plus a shielded control area, and rigid support structures for ceiling-mounted equipment (where necessary)
- dark room (where necessary), needing almost 5 sqm and appropriate ventilation for the developer
- contrast media preparation area, clean-up facilities, film quality control area, computer area and film storage area
- viewing area where films can be read and reports dictated.
The wall thickness in a radiology unit should be 8 to 12 cm (poured concrete) or 12 to 15 cm (cinder block or bricks). The diagnostic activities in health care facilities may require tests in haematology, clinical chemistry, microbiology, pathology and cytology. Each laboratory area should be provided with work areas, sample and material storage facilities (refrigerated or not), specimen collection facilities, facilities and equipment for terminal sterilization and waste disposal, and a special facility for radioactive material storage (where necessary) (American Institute of Architects Committee on Architecture for Health 1987).
4. Outpatient departments. Clinical facilities should include (American Institute of Architects Committee on Architecture for Health 1987): general-purpose examination rooms (7.4 sqm), special-purpose examination rooms (varying with the specific equipment needed) and treatment rooms (11 sqm). In addition, administrative facilities are needed for the admittance of outpatients.
5. Administration area (offices). Facilities such as common office building areas are needed. These include a loading dock and storage areas for receiving supplies and equipment and dispatching materials not disposed of by the separate waste removal system.
6. Dietary facilities (optional). Where present, these should provide the following elements (American Institute of Architects Committee on Architecture for Health 1987): a control station for receiving and controlling food supplies, storage spaces (including cold storage), food preparation facilities, handwashing facilities, facility for assembling and distributing patients’ meals, dining space, dishwashing space (located in a room or an alcove separated from the food preparation and serving area), waste storage facilities and toilets for dietary staff.
7. Linen services (optional). Where present, these should provide the following elements: a room for receiving and holding soiled linen, a clean-linen storage area, a clean-linen inspection and mending area and handwashing facilities (American Institute of Architects Committee on Architecture for Health 1987).
8. Engineering services and equipment areas. Adequate areas, varying in size and characteristics for each health care facility, have to be provided for: boiler plant (and fuel storage, if necessary), electrical supply, emergency generator, maintenance workshops and stores, cold-water storage, plant rooms (for centralized or local ventilation) and medical gases (NHS 1991a).
9. Corridors and passages. These have to be organized to avoid confusion for visitors and disruptions in the work of hospital personnel; circulation of clean and dirty goods should be strictly separated. Minimum corridor width should be 2 m (Decree of the President of Ministers Council 1986). Doorways and elevators must be large enough to allow easy passage of stretchers and wheelchairs.
Requirements for Building Materials and Furnishings
The choice of materials in modern health care facilities is often aimed to reduce the risk in accidents and fire occurrence: materials must be non-inflammable and must not produce noxious gases or smokes when burnt (American Institute of Architects Committee on Architecture for Health 1987). Trends in hospital floor-covering materials have shown a shift from stone materials and linoleum to polyvinyl chloride (PVC). In operating rooms, in particular, PVC is considered the best choice to avoid electrostatic effects that may cause explosion of anaesthetic flammable gases. Up to some years ago, walls were painted; today, PVC coverings and fibreglass wallpaper are the most used wall finishes. False ceilings are today built mainly from mineral fibres instead of gypsum board; a new trend appears to be that of using stainless steel ceilings (Catananti et al. 1993). However, a more complete approach should consider that each material and furnishing may cause effects in the outdoor and indoor environmental systems. Accurately chosen building materials may reduce environmental pollution and high social costs and improve the safety and comfort of building occupants. At the same time, internal materials and finishes may influence the functional performance of the building and its management. Besides, the choice of materials in hospitals should also consider specific criteria, such as ease of cleaning, washing and disinfecting procedures and susceptibility to becoming a habitat for living beings. A more detailed classification of criteria to be considered in this task, derived from the European Community Council Directive No. 89/106 (Council of the European Communities 1988), is shown in table 1 .
Table 1. Criteria and variables to be considered in the choice of materials
|
Criteria |
Variables |
|
Functional performance |
Static load, transit load, impact load, durability, construction requirements |
|
Safety |
Collapse risk, fire risk (reaction to fire, fire resistance, flammability), static electric charge (explosion risk), disperse electric power (electric shock risk), sharp surface (wound risk), poisoning risk (hazardous chemical emission), slip risk, radioactivity |
|
Comfort and pleasantness |
Acoustic comfort (features related to noise), optical and visual comfort (features related to light), tactile comfort (consistence, surface), hygrothermal comfort (features related to heat), aesthetics, odour emissions, indoor air quality perception |
|
Hygienicity |
Living beings habitat (insects, moulds, bacteria), susceptibility to stains, susceptibility to dust, easiness in cleaning, washing and disinfecting, maintenance procedures |
|
Flexibility |
Susceptibility to modifications, conformational factors (tile or panel dimensions and morphology) |
|
Environmental impact |
Raw material, industrial manufacturing, waste management |
|
Cost |
Material cost, installation cost, maintenance cost |
Source: Catananti et al. 1994.
On the matter of odour emissions, it should be observed that a correct ventilation after floor or wall-coverings installation or renovation work reduces exposure of personnel and patients to indoor pollutants (especially volatile organic compounds (VOCs)) emitted by building materials and furnishings.
Requirements for Heating, Ventilation and Air-Conditioning Systems and for Microclimatic Conditions
The control of microclimatic conditions in health care facilities areas may be carried out by heating, ventilation and/or air-conditioning systems (Catananti and Cambieri 1990). Heating systems (e.g., radiators) permit only temperature regulation and may be sufficient for common nursing units. Ventilation, which induces changes of air speed, may be natural (e.g., by porous building materials), supplementary (by windows) or artificial (by mechanical systems). The artificial ventilation is especially recommended for kitchens, laundries and engineering services. Air-conditioning systems, particularly recommended for some health care facility areas such as operating rooms and intensive-care units, should guarantee:
- the control of all microclimatic factors (temperature, relative humidity and air speed)
- the control of air purity and concentration of micro-organisms and chemicals (e.g., anaesthetic gases, volatile solvents, odours and so on). This target may be achieved by adequate air filtration and air changes, right pressure relationships among adjacent areas and laminar airflow.
General requirements of air-conditioning systems include outdoor intake locations, air filter features and air supply outlets (ASHRAE 1987). Outdoor intake locations should be far enough, at least 9.1 m, from pollution sources such as exhaust outlets of combustion equipment stacks, medical-surgical vacuum systems, ventilation exhaust outlets from the hospital or adjoining buildings, areas that may collect vehicular exhaust and other noxious fumes, or plumbing vent stacks. Besides, their distance from ground level should be at least 1.8 m. Where these components are installed above the roof, their distance from roof level should be at least 0.9 m.
Number and efficiency of filters should be adequate for the specific areas supplied by air conditioning systems. For example, two filter beds of 25 and 90% efficiency should be used in operating rooms, intensive-care units and transplant organ rooms. Installation and maintenance of filters follow several criteria: lack of leakage between filter segments and between the filter bed and its supporting frame, installation of a manometer in the filter system in order to provide a reading of the pressure so that filters can be identified as expired and provision of adequate facilities for maintenance without introducing contamination into the air flow. Air supply outlets should be located on the ceiling with perimeter or several exhaust inlets near the floor (ASHRAE 1987).
Ventilation rates for health care facility areas permitting air purity and comfort of occupants are listed in table 2 .
Table 2. Ventilation requirements in health care facilities areas
|
Areas |
Pressure relationships to adjacent areas |
Minimum air changes of outdoor air per hour supplied to room |
Minimum total air changes per hour supplied to room |
All air exhausted directly to outdoors |
Recirculated within room units |
|
Nursing units |
|||||
|
Patient room |
+/– |
2 |
2 |
Optional |
Optional |
|
Intensive care |
P |
2 |
6 |
Optional |
No |
|
Patient corridor |
+/– |
2 |
4 |
Optional |
Optional |
|
Operating theatres |
|||||
|
Operating room (all outdoor system) |
P |
15 |
15 |
Yes1 |
No |
|
Operating room (recirculating system) |
P |
5 |
25 |
Optional |
No2 |
|
Diagnostic facilities |
|||||
|
X ray |
+/– |
2 |
6 |
Optional |
Optional |
|
Laboratories |
|||||
|
Bacteriology |
N |
2 |
6 |
Yes |
No |
|
Clinical chemistry |
P |
2 |
6 |
Optional |
No |
|
Pathology |
N |
2 |
6 |
Yes |
No |
|
Serology |
P |
2 |
6 |
Optional |
No |
|
Sterilizing |
N |
Optional |
10 |
Yes |
No |
|
Glasswashing |
N |
2 |
10 |
Yes |
Optional |
|
Dietary facilities |
|||||
|
Food preparation centres3 |
+/– |
2 |
10 |
Yes |
No |
|
Dishwashing |
N |
Optional |
10 |
Yes |
No |
|
Linen service |
|||||
|
Laundry (general) |
+/– |
2 |
10 |
Yes |
No |
|
Soiled linen sorting and storage |
N |
Optional |
10 |
Yes |
No |
|
Clean linen storage |
P |
2 (Optional) |
2 |
Optional |
Optional |
P = Positive. N = Negative. +/– = Continuous directional control not required.
1 For operating rooms, use of 100% outside air should be limited to these cases where local codes require it, only if heat recovery devices are used; 2 recirculating room units meeting the filtering requirement for the space may be used; 3 food preparation centres shall have ventilation systems that have an excess of air supply for positive pressure when hoods are not in operation. The number of air changes may be varied to any extent required for odour control when the space is not in use.
Source: ASHRAE 1987.
Specific requirements of air-conditioning systems and microclimatic conditions regarding several hospital areas are reported as follows (ASHRAE 1987):
Nursing units. In common patient rooms a temperature (T) of 24 °C and a 30% relative humidity (RH) for winter and a T of 24 °C with 50% RH for summer are recommended. In intensive-care units a variable range temperature capability of 24 to 27 °C and a RH of 30% minimum and 60% maximum with a positive air pressure are recommended. In immunosuppressed patient units a positive pressure should be maintained between patient room and adjacent area and HEPA filters should be used.
In full-term nursery a T of 24 °C with RH from 30% minimum to 60% maximum is recommended. The same microclimatic conditions of intensive-care units are required in special-care nursery.
Operating theatres. Variable temperature range capability of 20 to 24 °C with RH of 50% minimum and 60% maximum and positive air pressure are recommended in operating rooms. A separate air-exhaust system or special vacuum system should be provided in order to remove anaesthetic gas traces (see “Waste anaesthetic gases” in this chapter).
Diagnostic facilities. In the radiology unit, fluoroscopic and radiographic rooms require T of 24 to 27 °C and RH of 40 to 50%. Laboratory units should be supplied with adequate hood exhaust systems to remove dangerous fumes, vapours and bioaerosols. The exhaust air from the hoods of the units of clinical chemistry, bacteriology and pathology should be discharged to the outdoors with no recirculation. Also, the exhaust air from infectious disease and virology laboratories requires sterilization before being exhausted to the outdoors.
Dietary facilities. These should be provided with hoods over the cooking equipment for removal of heat, odours and vapours.
Linen services. The sorting room should be maintained at a negative pressure in relation to adjoining areas. In the laundry processing area, washers, flatwork ironers, tumblers, and so on should have direct overhead exhaust to reduce humidity.
Engineering services and equipment areas. At work stations, the ventilation system should limit temperature to 32 °C.
Conclusion
The essence of specific building requirements for health care facilities is the accommodation of external standard-based regulations to subjective index-based guidelines. In fact, subjective indices, such as Predicted Mean Vote (PMV) (Fanger 1973) and olf, a measure of odour (Fanger 1992), are able to make predictions of the comfort levels of patients and personnel without neglecting the differences related to their clothing, metabolism and physical status. Finally, the planners and architects of hospitals should follow the theory of “building ecology” (Levin 1992) which describes dwellings as a complex series of interactions among buildings, their occupants and the environment. Health facilities, accordingly, should be planned and built focusing on the whole “system” rather than any particular partial frames of reference.
General Profile
Hotels and restaurants are found in every country. The economy of hotels and restaurants is intimately tied to the tourism industry, to business travel and to conventions. In many countries, the tourism industry is a major part of the overall economy.
The primary function of a restaurant is to provide food and drink to people outside the home. Types of restaurants include restaurants (which are often costly) with dining rooms and extensive serving staffs; smaller, “family-style” restaurants and cafes which often service the local community; “diners”, or restaurants where serving short-order meals at counters is the major feature; fast food restaurants, where people line up at counters to place their orders and where meals are available in a few minutes, often for taking out to eat elsewhere; and cafeterias, where people go through serving lines and make their selections from a variety of already prepared foods, which are usually displayed in cases. Many restaurants have separate bar or lounge areas, where alcoholic beverages are served, and many larger restaurants have special banquet rooms for groups of people. Street vendors serving food from carts and stalls are common in most countries, often as part of the informal sector of the economy.
The primary function of a hotel is to provide lodging for guests. Types of hotels range from basic overnight facilities, such as inns and motels that cater to business travellers and tourists, to elaborate luxury complexes, such as resorts, spas and convention hotels. Many hotels offer auxiliary services such as restaurants, bars, laundries, health and fitness clubs, beauty salons, barber shops, business centres and gift shops.
Restaurants and hotels can be individually or family-owned and operated, owned by partnerships or owned by large corporate entities. Many corporations do not actually own individual restaurants or hotels in the chain but rather grant a franchise of a name and style to local owners.
The restaurant workforce can include chefs and other kitchen staff, waiters and head waiters, table busing staff, bartenders, a cashier and coatroom personnel. Larger restaurants have staffs which can be highly specialized in their job functions.
The workforce in large a hotel typically will include reception clerks, door and bell persons, security personnel, parking and garage staff, housekeepers, laundry workers, maintenance personnel, kitchen and restaurant workers and office staff.
Most hotel jobs are “blue collar” and require minimal language and literacy skills. Women and immigrant workers comprise the bulk of the workforce in most hotels in developed countries today. In developing countries, hotels tend to be staffed by local residents. Because hotel occupancy levels tend to be seasonal, there is usually a small group of full-time employees with a sizeable number of part-time and seasonal workers. Salaries tend to be in the middle to low income range. As a result of these factors, employee turnover is relatively high.
In restaurants, workforce characteristics are similar, although men comprise a larger proportion of the workforce in restaurants than in hotels. In many countries salaries are low, and the staff waiting on and busing tables may depend on gratuities for a major portion of their income. In many places, a service charge is automatically added to the bill. In fast food restaurants, the workforce are often teenagers and the pay is at the minimum wage.
Storage and Transportation of Crude Oil, Natural Gases, Liquid Petroleum Products and Other Chemicals
Pipelines, marine vessels, tank trucks, rail tank cars and so forth are used to transport crude oils, compressed and liquefied hydrocarbon gases, liquid petroleum products and other chemicals from their point of origin to pipeline terminals, refineries, distributors and consumers.
Crude oils and liquid petroleum products are transported, handled and stored in their natural liquid state. Hydrocarbon gases are transported, handled and stored in both the gaseous and liquid states and must be completely confined in pipelines, tanks, cylinders or other containers prior to use. The most important characteristic of liquefied hydrocarbon gases (LHGs) is that they are stored, handled and shipped as liquids, taking up a relatively small amount of space and then expanding into a gas when used. For example, liquefied natural gas (LNG) is stored at –162°C, and when it is released the difference in storage and atmospheric temperatures causes the liquid to expand and gasify. One gallon (3.8 l) of LNG converts to approximately 2.5 m3 of natural gas at normal temperature and pressure. Because liquefied gas is much more “concentrated” than compressed gas, more useable gas can be transported and provided in the same size container.
Pipelines
It is generally the case that all crude oils, natural gas, liquefied natural gas, liquefied petroleum gas (LPG) and petroleum products flow through pipelines at some time in their migration from the well to a refinery or gas plant, then to a terminal and eventually to the consumer. Aboveground, underwater and underground pipelines, varying in size from several centimetres to a metre or more in diameter, move vast amounts of crude oil, natural gas, LHGs and liquid petroleum products. Pipelines run throughout the world, from the frozen tundra of Alaska and Siberia to the hot deserts of the Middle East, across rivers, lakes, seas, swamps and forests, over and through mountains and under cities and towns. Although the initial construction of pipelines is difficult and expensive, once they are built, properly maintained and operated, they provide one of the safest and most economical means of transporting these products.
The first successful crude-oil pipeline, a 5-cm-diameter wrought iron pipe 9 km long with a capacity of about 800 barrels a day, was opened in Pennsylvania (US) in 1865. Today, crude oil, compressed natural gas and liquid petroleum products are moved long distances through pipelines at speeds from 5.5 to 9 km per hour by large pumps or compressors located along the route of the pipeline at intervals ranging from 90 km to over 270 km. The distance between pumping or compressor stations is determined by the pump capacity, viscosity of the product, size of the pipeline and the type of terrain crossed. Regardless of these factors, pipeline pumping pressures and flow rates are controlled throughout the system to maintain a constant movement of product within the pipeline.
Types of pipelines
The four basic types of pipelines in the oil and gas industry are flow lines, gathering lines, crude trunk pipelines and petroleum product trunk pipelines.
- Flow lines. Flow lines move crude oil or natural gas from producing wells to producing field storage tanks and reservoirs. Flow lines may vary in size from 5 cm in diameter in older, lower-pressure fields with only a few wells, to much larger lines in multi-well, high-pressure fields. Offshore platforms use flow lines to move crude and gas from wells to the platform storage and loading facility. A lease line is a type of flow line which carries all of the oil produced on a single lease to a storage tank.
- Gathering and feeder lines. Gathering lines collect oil and gas from several locations for delivery to central accumulating points, such as from field crude oil tanks and gas plants to marine docks. Feeder lines collect oil and gas from several locations for delivery direct into trunk lines, such as moving crude oil from offshore platforms to onshore crude trunk pipelines. Gathering lines and feeder lines are typically larger in diameter than flow lines.
- Crude trunk pipelines. Natural gas and crude oil are moved long distances from producing areas or marine docks to refineries and from refineries to storage and distribution facilities by 1- to 3-m- or larger-diameter trunk pipelines.
- Petroleum product trunk pipelines. These pipelines move liquid petroleum products such as gasoline and fuel oil from refineries to terminals, and from marine and pipeline terminals to distribution terminals. Product pipelines may also distribute products from terminals to bulk plants and consumer storage facilities, and occasionally from refineries direct to consumers. Product pipelines are used to move LPG from refineries to distributor storage facilities or large industrial users.
Regulations and standards
Pipelines are constructed and operated to meet safety and environmental standards established by regulatory agencies and industry associations. Within the United States, the Department of Transportation (DOT) regulates the operation of pipelines, the Environmental Protection Agency (EPA) regulates spills and releases, the Occupational Safety and Health Administration (OSHA) promulgates standards covering worker health and safety, and the Interstate Commerce Commission (ICC) regulates common carrier pipelines. A number of industry organizations, such as the American Petroleum Institute and the American Gas Association, also publish recommended practices covering pipeline operations.
Pipeline construction
Pipeline routes are planned using topographic maps developed from aerial photogrammetric surveys, followed by actual ground surveying. After planning the route, obtaining right-of-way and permission to proceed, base camps are established and a means of access for construction equipment is required. Pipelines can be constructed working from one end to another or simultaneously in sections which are then connected.
The first step in laying pipeline is to construct a 15- to 30-m-wide service road along the planned route to provide a stable base for the pipe-laying and pipe-joining equipment and for underground pipeline excavation and backfill equipment. The pipe sections are laid on the ground alongside the service road. The ends of the pipe are cleaned, the pipe is bent horizontally or vertically, as necessary, and the sections are held in position by chocks above the ground and joined by multi-pass electrical arc-welding. The welds are checked visually and then with gamma radiation to assure that no defects are present. Each connected section is then coated with liquid soap and air-pressure tested to detect leaks.
The pipeline is cleaned, primed and coated with a hot, tar-like material to prevent corrosion and wrapped in an outer layer of heavy paper, mineral wool or plastic. If the pipe is to be buried, the bottom of the trench is prepared with a sand or gravel bed. The pipe may be weighed down by short, concrete sleeves to prevent its lifting out of the trench from groundwater pressure. After the underground pipeline is placed in the trench, the trench is backfilled and the surface of the ground returned to normal appearance. After coating and wrapping, aboveground piping is lifted up onto prepared stanchions or casements, which may have various design features such as anti-earthquake shock absorption. Pipelines may be insulated or have heat trace capabilities to keep products at desired temperatures throughout transport. All pipeline sections are hydrostatically tested prior to entering gas or liquid hydrocarbon service.
Pipeline operations
Pipelines may be either privately owned and operated, carrying only the owner’s products, or they may be common carriers, required to carry any company’s products provided that the pipeline’s product requirements and tariffs are met. The three major pipeline operations are pipeline control, pumping or compressor stations and delivery terminals. Storage, cleaning, communication and shipment are also important functions.
- Pipeline control. Regardless of the product being transported, the size and length of the pipeline or the terrain, pipeline pumping stations, pressures and flow rates are completely controlled in order to ensure appropriate flow rates and continuous operations. Typically an operator and computer control the pumps, valves, regulators and compressors throughout the pipeline system from a central location.
- Oil pumping and gas compressor stations. Crude oil and petroleum products pumping stations and gas compressor stations are located at wellheads and along the pipeline route as needed to maintain pressure and volume. Pumps are driven by electric motors or diesel engines, and turbines may be powered by fuel oil, gas or steam. Many of these stations are automatically controlled and not staffed at most times. Pumps, with and without vapour return lines or pressure equalizing lines, are commonly used in smaller pipelines for transport of LNG, LPG and compressed natural gas (CNG). Pressure drop detectors are installed to signal any leaks in pipelines, and excess flow valves or other flow limiting devices are used to minimize the rate of flow in case of a pipeline leak. Storage vessels and reservoirs may be isolated from main pipelines by manually operated or remote control valves or fusible link valves.
- Pipeline product storage. Crude and petroleum product pipeline terminals have breakout storage tanks to which shipments may be diverted, where they are held until required by a refinery, terminal or user (see figure 1). Other tanks at pipeline pumping stations contain fuel for operating diesel-driven pump motors or for running electrical generators. Because gas fields produce continuously and gas pipelines operate continuously, during times of reduced demand, such as summertime, liquefied natural and petroleum gases are stored underground in natural caverns or salt domes until needed.
- Pipeline cleaning. Pipelines are cleaned on a scheduled basis or as necessary in order to continue flow by reducing friction and maintaining as large a diameter interior as possible. A special cleaning device, called a pig or go-devil, is placed into the pipeline and pushed along by the flow of oil from one pumping station to the next. As the pig passes through the pipeline it scrapes off any dirt, wax or other deposits which have built up inside the pipeline walls. When it reaches a pumping station, the pig is removed, cleaned and reinserted into the pipeline to travel to the next station.
- Communications. It is important that there be communication and agreement concerning schedules, pumping rates and pressures and emergency procedures between pipeline stations and operators and those shipping and receiving crude oil, gas and petroleum products. Some pipeline companies have private telephone systems which transmit the signal along the pipeline, while others use radios or public telephones. Many pipelines use ultra-high-frequency microwave transmitter systems for computer communications between control centres and pumping stations.
- Petroleum product shipment. Petroleum products may be shipped a number of different ways on pipelines. A company operating a refinery may blend a specific grade of its own gasoline with appropriate additives (additize) and ship a batch through a pipeline directly to its own terminal for distribution to its customers. Another method is for a refinery to produce a batch of gasoline, called a frangible or specification product, which is blended to meet a common carrier pipeline company’s product specifications. The gasoline is placed into the pipeline for delivery to any company’s terminals which are connected to the pipeline system. In a third method, products are shipped by companies to each other’s terminals and exchanged in order to avoid extra transportation and handling. Frangible and exchange products are usually blended and additized at the terminal which receives the product from the pipeline, to meet the specific requirements of each company operating from the terminal. Finally, some products are delivered by pipeline from terminals and refineries direct to large commercial consumers—jet fuel to airports, gas to gas distribution companies and fuel oil to electric generating plants.
- Product receipt and delivery. Pipeline operators and terminal operators should jointly establish programmes to provide for the safe receipt and transfer of products and to coordinate actions in case an emergency occurs on the pipeline or at the terminal during shipment which requires shutdown or diversion of product.
Figure 1. A terminal operator transfers product the Pasagoula Refinery into holding tanks in the Deraville Terminal near Atlanta, Georgia, US.
American Petroleum Institute
Instructions for receiving pipeline deliveries should include verification of the availability of the storage tanks to hold the shipment, opening and aligning tank and terminal valves in anticipation of delivery, checking to assure that the proper tank is receiving product immediately after the start of delivery, conducting required sampling and testing of batches at the start of delivery, performing batch changes and tank switches as required, monitoring receipts to assure that overfills do not occur and maintaining communications between the pipeline and the terminal. The use of written communications between terminal workers, especially when shift changes occur during product transfer, should be considered.
Batch shipments and interface
Although pipelines originally were used to move only crude oil, they evolved into carrying all types and different grades of liquid petroleum products. Because petroleum products are transported in pipelines by batches, in succession, there is commingling or mixing of the products at the interfaces. The product intermix is controlled by one of three methods: downgrading (derating), using liquid and solid spacers for separation or reprocessing the intermix. Radioactive tracers, colour dyes and spacers may be placed into the pipeline to identify where the interfaces occur. Radioactive sensors, visual observation or gravity tests are conducted at the receiving facility to identify different pipeline batches.
Petroleum products are normally transported through pipelines in batch sequences with compatible crude oils or products adjoining one another. One method of maintaining product quality and integrity, downgrading or derating, is accomplished by lowering the interface between the two batches to the level of the least affected product. For example, a batch of high-octane premium gasoline is typically shipped immediately before or after a batch of lower-octane regular gasoline. The small quantity of the two products which has intermixed will be downgraded to the lower octane rating regular gasoline. When shipping gasoline before or after diesel fuel, a small amount of diesel interface is allowed to blend into the gasoline, rather than blending gasoline into the diesel fuel, which could lower its flashpoint. Batch interfaces are typically detected by visual observation, gravitometers or sampling.
Liquid and solid spacers or cleaning pigs may be used to physically separate and identify different batches of products. The solid spacers are detected by a radioactive signal and diverted from the pipeline into a special receiver at the terminal when the batch changes from one product to another. Liquid separators may be water or another product that does not commingle with either of the batches it is separating and is later removed and reprocessed. Kerosene, which is downgraded (derated) to another product in storage or is recycled, can also be used to separate batches.
A third method of controlling the interface, often used at the refinery ends of pipelines, is to return the interface to be reprocessed. Products and interfaces which have been contaminated with water may also be returned for reprocessing.
Environmental protection
Because of the large volumes of products which are transported by pipelines on a continuous basis, there is opportunity for environmental damage from releases. Depending on company and regulatory safety requirements and the pipeline’s construction, location, weather, accessibility and operation, a considerable amount of product may be released should a break in the line or leak occur. Pipeline operators should have emergency response and spill contingency plans prepared and have containment and clean-up materials, personnel and equipment available or on call. Simple field solutions such as building earth dykes and drainage ditches can be quickly implemented by trained operators to contain and divert spilled product.
Maintaining pipelines and worker health and safety
The first pipelines were made of cast iron. Modern trunk pipelines are constructed of welded, high-strength steel, which can withstand high pressures. Pipe walls are periodically tested for thickness to determine whether internal corrosion or deposits have occurred. Welds are checked visually and with gamma radiation to assure that no defects are present.
Plastic pipe may be used for low-pressure, small-diameter flow lines and gathering lines in gas and crude-oil-producing fields, since plastic is light in weight and easy to handle, assemble and move.
When a pipeline is separated by cutting, spreading flanges, removing a valve or opening the line, an electrostatic arc may be created by impressed cathodic protection voltage, corrosion, sacrificial anodes, nearby high-voltage power lines or stray ground currents. This should be minimized by grounding (earthing) the pipe, de-energizing the cathodic rectifiers closest to both sides of the separation and connecting a bonding cable to each side of the piping prior to starting work. As additional pipeline sections, valves and so on are added to an existing line, or during construction, they should first be bonded to the pipelines in place.
Work on pipelines should cease during electrical storms. Equipment used to lift and place pipe should not be operated within 3 m of high-voltage electric lines. Any vehicles or equipment working in the vicinity of high-voltage lines should have trailing grounding straps attached to the frames. Temporary metal buildings should also be grounded.
Pipelines are specially coated and wrapped to prevent corrosion. Cathodic electrical protection may also be required. After the pipeline sections are coated and insulated, they are joined by special clamps connected to metallic anodes. The pipeline is subjected to a grounded source of direct current of sufficient capacity so that the pipeline acts as a cathode and does not corrode.
All pipeline sections are hydrostatically tested prior to entering gas or liquid hydrocarbon service and, depending on regulatory and company requirements, at regular intervals during the life of the pipeline. Air must be eliminated from pipelines prior to hydrostatic testing, and hydrostatic pressure built up and reduced at safe rates. Pipelines are regularly patrolled, usually by aerial surveillance, to visually detect leaks, or monitored from the control centre to detect a drop in flow rate or pressure, which would signify that a break in the pipeline has occurred.
Pipeline systems are provided with warning and signalling systems to alert operators so they may take corrective action in an emergency. Pipelines may have automatic shutdown systems which activate emergency pressure valves upon sensing increased or reduced pipeline pressure. Manually or automatically operated isolation valves are typically located at strategic intervals along pipelines, such as at pumping stations and at both sides of river crossings.
An important consideration when operating pipelines is to provide a means of warning contractors and others who may be working or conducting excavations along the pipeline route, so that the pipeline is not inadvertently ruptured, breached or punctured, resulting in a vapour or gas explosion and fire. This is usually done by regulations which require construction permits or by pipeline companies and associations providing a central number which contractors can call prior to excavation.
Because crude oil and flammable petroleum products are transported in pipelines, the possibility exists for fire or explosion in case of a line break or release of vapour or liquid. Pressure should be reduced to a safe level before working on high-pressure pipelines. Combustible gas testing should be conducted and a permit issued prior to repair or maintenance involving hot work or hot tapping on pipelines. The pipeline should be cleared of flammable liquids and vapours or gas prior to starting work. If a pipeline cannot be cleared and an approved plug is used, safe work procedures should be established and followed by qualified workers. The line should be vented a safe distance from the hot work area to relieve any build-up of pressure behind the plug.
Proper safety procedures should be established and followed by qualified workers when hot tapping pipelines. If welding or hot tapping is conducted in an area where a spill or leak has occurred, the outside of the pipe should be cleaned of liquid, and contaminated soil should be removed or covered to prevent ignition.
It is very important to notify operators at the nearest pumping stations on each side of the operating pipeline where maintenance or repair is to be performed, in case shutdown is required. When crude oil or gas is being pumped into pipelines by producers, the pipeline operators must provide specific instructions to the producers as to actions to take during repair, maintenance or in an emergency. For example, prior to tie-in of production tanks and lines to pipelines, all gate valves and bleeders for the tanks and lines involved in the tie-in should be closed and locked or sealed until the operation is completed.
Normal safety precautions concerning pipe and materials handling, toxic and hazardous exposures, welding and excavation apply during pipeline construction. Workers clearing right-of-way should protect themselves from climatic conditions; poisonous plants, insects and snakes; falling trees and rocks; and so on. Excavations and trenches should be sloped or shored to prevent collapse during underground pipeline construction or repair (see the article “Trenching” in the chapter Construction). Workers should follow safe work practices when opening and de-energizing electrical transformers and switches.
Pipeline operating and maintenance personnel often work alone and are responsible for long stretches of pipeline. Atmospheric testing and the use of personal and respiratory protective equipment is needed to determine oxygen and flammable vapour levels and protect against toxic exposures to hydrogen sulphide and benzene when gauging tanks, opening lines, cleaning spills, sampling and testing, shipping, receiving and performing other pipeline activities. Workers should wear dosimeters or film badges and avoid exposure when working with density gauges, source holders or other radioactive materials. The use of personal and respiratory protective equipment should be considered for exposure to burns from the hot protective tar used in pipe-coating operations and from toxic vapours which contain polynuclear aromatic hydrocarbons.
Marine Tankers and Barges
The majority of the world’s crude oil is transported by tankers from producing areas such as the Middle East and Africa to refineries in consumer areas such as Europe, Japan and the United States. Oil products were originally transported in large barrels on cargo ships. The first tanker ship, which was built in 1886, carried about 2,300 SDWT (2,240 pounds per ton) of oil. Today’s supertankers can be over 300 m long and carry almost 200 times as much oil (see figure 2). Gathering and feeder pipelines often end at marine terminals or offshore platform loading facilities, where the crude oil is loaded into tankers or barges for transport to crude trunk pipelines or refineries. Petroleum products also are transported from refineries to distribution terminals by tanker and barge. After delivering their cargoes, the vessels return in ballast to loading facilities to repeat the sequence.
Figure 2. SS Paul L. Fahrney oil tanker.
American Petroleum Institute
Liquefied natural gas is shipped as a cryogenic gas in specialized marine vessels with heavily insulated compartments or reservoirs (see figure 3). At the delivery port, the LNG is off-loaded to storage facilities or regasification plants. Liquefied petroleum gas may be shipped both as a liquid in uninsulated marine vessels and barges and as a cryogenic in insulated marine vessels. Additionally, LPG in containers (bottled gas) may be shipped as cargo on marine vessels and barges.
Figure 3. LNG Leo tanker loading at Arun, Sumatra, Indonesia.
American Petroleum Institute
LPG and LNG marine vessels
The three types of marine vessels used for transport of LPG and LNG are:
- vessels with reservoirs pressurized up to 2 mPa (LPG only)
- vessels with heat-insulated reservoirs and a reduced pressure of 0.3 to 0.6 mPa (LPG only)
- cryogenic vessels with heat-insulated reservoirs pressurized close to atmospheric pressure (LPG and LNG).
Shipment of LHGs on marine vessels requires constant safety awareness. Transfer hoses must be suitable for the correct temperatures and pressures of the LHGs being handled. To prevent a flammable mixture of gas vapour and air, inert gas (nitrogen) blanketing is provided around reservoirs, and the area is continually monitored to detect leaks. Before loading, storage reservoirs should be inspected to ensure that they are free of contaminants. If reservoirs contain inert gas or air, they should be purged with LHG vapour prior to loading the LHG. Reservoirs should be constantly inspected to ensure integrity, and safety valves should be installed to relieve the LHG vapour generated at maximum heat load. Marine vessels are provided with fire suppression systems and have comprehensive emergency response procedures in place.
Crude oil and petroleum products marine vessels
Oil tankers and barges are vessels designed with the engines and quarters at the rear of the vessel and the remainder of the vessel divided into special compartments (tanks) to carry crude oil and liquid petroleum products in bulk. Cargo pumps are located in pump rooms, and forced ventilation and inerting systems are provided to reduce the risk of fires and explosions in pump rooms and cargo compartments. Modern oil tankers and barges are built with double hulls and other protective and safety features required by the United States Oil Pollution Act of 1990 and the International Maritime Organization (IMO) tanker safety standards. Some new ship designs extend double hulls up the sides of the tankers to provide additional protection. Generally, large tankers carry crude oil and small tankers and barges carry petroleum products.
- Supertankers. Ultra-large and very large crude carriers (ULCCs and VLCCs) are restricted by their size and draft to specific routes of travel. ULCCs are vessels whose capacity is over 300,000 SDWTs, and VLCCs have capacities ranging from 160,000 to 300,000 SDWTs. Most large crude carriers are not owned by oil companies, but are chartered from transportation companies which specialize in operating these super-sized vessels.
- Oil tankers. Oil tankers are smaller than VLCCs, and, in addition to ocean travel, they can navigate restricted passages such as the Suez and Panama Canals, shallow coastal waters and estuaries. Large oil tankers, which range from 25,000 to 160,000 SDWTs, usually carry crude oil or heavy residual products. Smaller oil tankers, under 25,000 SDWT, usually carry gasoline, fuel oils and lubricants.
- Barges. Barges operate mainly in coastal and inland waterways and rivers, alone or in groups of two or more, and are either self-propelled or moved by tugboat. They may carry crude oil to refineries, but more often are used as an inexpensive means of transporting petroleum products from refineries to distribution terminals. Barges are also used to off-load cargo from tankers offshore whose draft or size does not allow them to come to the dock.
Barge and ship loading and unloading
Vessel-to-shore procedures, safety checklists and guidelines should be established and agreed upon by terminal and marine vessel operators. The International Safety Guide for Oil Tankers and Terminals (International Chamber of Shipping 1978) contains information and samples of checklists, guidelines, permits and other procedures covering safe operations when loading or unloading vessels, which may be used by vessel and terminal operators.
Although marine vessels sit in water and are thereby intrinsically grounded, there is a need to provide protection from static electricity which can build up during loading or unloading. This is accomplished by bonding or connecting metal objects on the dock or loading/unloading apparatus to the metal of the vessel. Bonding is also accomplished by use of conductive loading hose or piping. An electrostatic spark of ignitable intensity may also be generated when lowering equipment, thermometers or gauging devices into compartments immediately after loading; enough time must be allowed for the static charge to dissipate.
Ship-to-shore electric currents, which are different from static electricity, may be generated by cathodic protection of the vessel’s hull or dock, or by galvanic potential differences between the vessel and the shore. These currents also build up in metal loading/unloading apparatus. Insulating flanges may be installed within the length of the loading arm and at the point where flexible hoses connect to the shore pipeline system. When the connections are broken, there is no opportunity for a spark to jump from one metal surface to another.
All vessels and terminals need mutually agreed upon emergency response procedures in case of a fire or release of product, vapour or toxic gas. These must cover emergency operations, stopping product flow and emergency removal of a vessel from the dock. The plans should consider communications, fire-fighting, vapour cloud mitigation, mutual aid, rescue, clean-up and remediation measures.
Fire protection portable equipment and fixed systems should be in accord with government and company requirements and appropriate to the size, function, exposure potential and value of the dock and wharf facilities. The International Safety Guide for Oil Tankers and Terminals (International Chamber of Shipping 1978) contains a sample fire notice which may be used as a guide by terminals for dock fire prevention.
Marine vessel health and safety
In addition to the usual maritime working hazards, transporting crude oil and flammable liquids by marine vessel creates a number of special health, safety and fire prevention situations. These include surging and expansion of liquid cargo, flammable vapour hazards during transport and when loading and unloading, possibility of pyrophoric ignition, toxic exposures to materials such as hydrogen sulphide and benzene and safety considerations when venting, flushing and cleaning compart-ments. The economics of operating modern tankers requires them to be at sea for extended periods of time with only short intervals in port to load or unload cargo. This, together with the fact that tankers are highly automated, creates unique mental and physical demands on the few crew members used to operate the vessels.
Fire and explosion protection
Emergency plans and procedures should be developed and implemented that are appropriate for the type of cargo on board and other potential hazards. Fire-fighting equipment must be supplied. Response team members who have shipboard fire-fighting, rescue and spill clean-up responsibilities should be trained, drilled and equipped to handle potential emergencies. Water, foam, dry chemicals, halon, carbon dioxide and steam are used as cooling, inhibiting and smothering fire-fighting agents aboard marine vessels, although halon is being phased out due to environmental concerns. The requirements for vessel fire-fighting equipment and systems are established by the country under whose flag the vessel sails and by company policy, but usually follow the recommendations of the 1974 International Convention for the Safety of Life at Sea (SOLAS).
Strict control of flames or naked lights, lighted smoking materials and other sources of ignition, such as welding or grinding sparks, electrical equipment and unprotected light bulbs, is required on vessels at all times to reduce the risk of fire and explosion. Prior to conducting hot work on board marine vessels, the area should be examined and tested to assure that conditions are safe, and permits should be issued for each specific task allowed.
One method of preventing explosions and fires in the vapour space of cargo compartments is to maintain the level of oxygen below 11% by making the atmosphere inert with a noncombustible gas. Sources for inert gas are exhaust gases from the vessel’s boilers or an independent gas generator or a gas turbine fitted with an afterburner. The 1974 SOLAS Convention implies that vessels carrying cargo with flashpoints below 60°C should have compartments fitted with inert systems. Vessels using inert gas systems should maintain cargo compartments in non-flammable conditions at all times. Inert gas compartments should be constantly monitored to assure safe conditions and should not be allowed to become flammable, because of the danger of ignition from pyrophoric deposits.
Confined spaces
Confined spaces on marine vessels, such as cargo compartments, paint lockers, pump rooms, fuel tanks and spaces between double hulls, must be treated the same as any confined space for entry, hot work and cold work. Tests for oxygen content, flammable vapours and toxic substances, in that order, must be conducted prior to entering confined spaces. A permit system should be established and followed for all confined space entry, safe (cold) work and hot work, which indicates safe exposure levels and required personal and respiratory protective equipment. In waters of the United States, these tests may be conducted by qualified individuals called “marine chemists”.
Compartments on marine vessels such as cargo tanks and pump rooms are confined spaces; when cleaning those which have been made inert or have flammable vapour, toxic or unknown atmospheres, they should be tested, and special safety and respiratory protection procedures should be followed. After crude oil has been unloaded, a small amount of residue, called clingage, remains on the interior surfaces of the compartments, which may then be washed and filled with water for ballast. One method of reducing the amount of residue is to install fixed equipment which removes up to 80% of the clingage by washing down the sides of inerted compartments with crude oil during unloading.
Pumps, valves and equipment
A work permit should be issued and safe work procedures followed, such as bonding, draining and vapour freeing, flammable vapour and toxic exposure testing, and providing stand-by fire protection equipment when operations, maintenance or repair requires opening cargo pumps, lines, valves or equipment on board marine vessels.
Toxic exposures
There is an opportunity for vented gases such as flue gas or hydrogen sulphide to reach the decks of vessels, even from specially designed vent systems. Testing should be continuously conducted to determine inert gas levels on all vessels and hydrogen sulphide levels on vessels which contain or previously carried sour crude oil or residual fuel. Tests should be conducted for benzene exposure on vessels carrying crude oil and gasoline. Inert gas scrubber effluent water and condensate water is acidic and corrosive; PPE should be used when contact is possible.
Environmental protection
Marine vessels and terminals should establish procedures and provide equipment to protect the environment from spills on water and land, and from releases of vapour to the air. The use of large vapour recovery systems at marine terminals is growing. Care must be taken to comply with air pollution requirements when vessels vent compartments and enclosed spaces. Emergency response procedures should be established, and equipment and trained personnel should be available to respond to spills and releases of crude oil and flammable and combustible liquids. A responsible person should be designated to ensure that notifications are made to both the company and the appropriate authorities should a reportable spill or release occur.
In the past, the oil-contaminated ballast water and tank washings were flushed out of the compartments at sea. In 1973, the International Convention for Prevention of Pollution from Ships established requirements that before the water is discharged at sea, the oily residue must be separated and retained on board for eventual onshore processing. Modern tankers have segregated ballast systems, with different lines, pumps and tanks than those used for cargo (in accordance with international recommen-dations), so that there is no possibility of contamination. Older vessels still carry ballast in cargo tanks, so special procedures, such as pumping oily water into designated onshore tanks and processing facilities, must be followed when discharging ballast in order to prevent pollution.
Motor Vehicle and Railroad Transport of Petroleum Products
Crude oil and petroleum products were initially transported by horse-drawn tank wagons, then by railroad tank cars and finally by motor vehicles. Following receipt at terminals from marine vessels or pipelines, bulk liquid petroleum products are delivered by non-pressure tank trucks or rail tank cars directly to service stations and consumers or to smaller terminals, called bulk plants, for redistribution. LPG, gasoline anti-knock compounds, hydrofluoric acid and many other products, chemicals and additives used in the oil and gas industry are transported in pressure tank cars and tank trucks. Crude oil may also be transported by tank truck from small producing wells to gathering tanks, and by tank truck and railroad tank car from storage tanks to refineries or main pipelines. Packaged petroleum products in bulk bins or drums and pallets and cases of smaller containers are carried by package truck or railroad box car.
Government regulations
Transportation of petroleum products by motor vehicle or railroad tank car is regulated by government agencies throughout most of the world. Agencies such as the US DOT and the Canadian Transport Commission (CTC) have established regulations governing the design, construction, safety devices, testing, preventive maintenance, inspection and operation of tank trucks and tank cars. Regulations governing railroad tank car and tank truck operations typically include tank pressure and pressure relief device testing and certification before being placed into initial service and at regular intervals thereafter. The Association of American Railroads and the National Fire Protection Association (NFPA) are typical of organizations which publish specifications and requirements for the safe operation of tank cars and tank trucks. Most governments have regulations or adhere to United Nations Conventions which require the identification of and information concerning hazardous materials and petroleum products which are shipped in bulk or in containers. Railroad tank cars, tank trucks and package trucks are placarded to identify any hazardous products being transported and to provide emergency response information.
Railroad tank cars
Railroad tank cars are constructed of carbon steel or aluminium and may be pressurized or unpressurized. Modern tank cars can hold up to 171,000 l of compressed gas at pressures up to 600 psi (1.6 to 1.8 mPa). Non-pressure tank cars have evolved from small wooden tank cars of the late 1800s to jumbo tank cars which transport as much as 1.31 million litres of product at pressures up to 100 psi (0.6 mPa). Non-pressure tank cars may be individual units with one or multiple compartments or a string of interconnected tank cars, called a tank train. Tank cars are loaded individually, and entire tank trains can be loaded and unloaded from a single point. Both pressure and non-pressure tank cars may be heated, cooled, insulated and thermally protected against fire, depending on their service and the products transported.
All railroad tank cars have top- or bottom-liquid or vapour valves for loading and unloading and hatch entries for cleaning. They are also equipped with devices intended to prevent the increase of internal pressure when exposed to abnormal con-ditions. These devices include safety relief valves held in place by a spring which can open to relieve pressure and then close; safety vents with rupture discs that burst open to relieve pressure but cannot reclose; or a combination of the two devices. A vacuum relief valve is provided for non-pressure tank cars to prevent vacuum formation when unloading from the bottom. Both pressure and non-pressure tank cars have protective housings on top surrounding the loading connections, sample lines, thermometer wells and gauging devices. Platforms for loaders may or may not be provided on top of cars. Older non-pressure tank cars may have one or more expansion domes. Fittings are provided on the bottom of tank cars for unloading or cleaning. Head shields are provided on the ends of tank cars to prevent puncture of the shell by the coupler of another car during derailments.
LNG is shipped as a cryogenic gas in insulated tank truck and rail pressure tank cars. Pressure tank trucks and rail tank cars for LNG transport have a stainless steel inner reservoir suspended in an outer reservoir of carbon steel. The annular space is a vacuum filled with insulation to maintain low temperatures during shipment. To prevent gas from igniting back to the tanks, they are equipped with two independent, remotely controlled fail-safe emergency shut-off valves on the filling and discharge lines and have gauges on both the inside and outside reservoirs.
LPG is transported on land in specially designed rail tank cars (up to 130 m3 capacity) or tank trucks (up to 40 m3 capacity). Tank trucks and rail tank cars for LPG transport are typically uninsulated steel cylinders with spherical bottoms, equipped with gauges, thermometers, two safety relief valves, a gas level meter and maximum fill indicator and baffles.
Rail tank cars transporting LNG or LPG should not be overloaded, since they may sit on a siding for some period of time and be exposed to high ambient temperatures, which could cause overpressure and venting. Bond wires and grounding cables are provided at rail and tank truck loading racks to help neutralize and dissipate static electricity. They should be connected before operations commence and not disconnected until operations are complete and all valves are closed. Truck and rail loading facilities are typically protected by fire water spray or mist systems and fire extinguishers.
Tank trucks
Petroleum products and crude oil tank trucks are typically constructed of carbon steel, aluminium or a plasticized fibreglass material, and vary in size from 1,900-l tank wagons to jumbo 53,200-l tankers. The capacity of tank trucks is governed by regulatory agencies, and usually is dependent upon highway and bridge capacity limitations and the allowable weight per axle or total amount of product allowed.
There are pressurized and non-pressurized tank trucks, which may be non-insulated or insulated depending on their service and the products transported. Pressurized tank trucks are usually single compartment, and non-pressurized tank trucks may have single or multiple compartments. Regardless of the number of compartments on a tank truck, each compartment must be treated individually, with its own loading, unloading and safety-relief devices. Compartments may be separated by single or double walls. Regulations may require that incompatible products and flammable and combustible liquids carried in different compartments on the same vehicle be separated by double walls. When pressure testing compartments, the space between the walls should also be tested for liquid or vapour.
Tank trucks have either hatches which open for top loading, valves for closed top- or bottom-loading and unloading, or both. All compartments have hatch entries for cleaning and are equipped with safety relief devices to mitigate internal pressure when exposed to abnormal conditions. These devices include safety relief valves held in place by a spring which can open to relieve pressure and then close, hatches on non-pressure tanks which pop open if the relief valves fail and rupture discs on pressurized tank trucks. A vacuum relief valve is provided for each non-pressurized tank truck compartment to prevent vacuum when unloading from the bottom. Non-pressurized tank trucks have railings on top to protect the hatches, relief valves and vapour recovery system in case of a rollover. Tank trucks are usually equipped with breakaway, self-closing devices installed on compartment bottom loading and unloading pipes and fittings to prevent spills in case of damage in a rollover or collision.
Rail tank car and tank truck loading and unloading
While railroad tank cars are almost always loaded and unloaded by workers assigned to these specific duties, tank trucks may be loaded and unloaded by either loaders or drivers. Tank cars and tank trucks are loaded at facilities called loading racks, and may be top loaded through open hatches or closed connections, bottom loaded through closed connections, or a combination of both.
Loading
Workers who load and unload crude oil, LPG, petroleum products, and acids and additives used in the oil and gas industry, should have a basic understanding of the characteristics of the products handled, their hazards and exposures and the operating procedures and work practices needed to perform the job safely. Many government agencies and companies require the use and completion of inspection forms upon receipt and shipment and prior to loading and unloading railroad tank cars and tank trucks. Tank trucks and railroad tank cars may be loaded through open hatches on the top or through fittings and valves at the top or bottom of each tank or compartment. Closed connections are required when pressure loading and where vapour recovery systems are provided. If loading systems do not activate for any reason (such as improper operation of the vapour recovery system or a fault in the grounding or bonding system), by-pass should not be attempted without approval. All hatches should be closed and securely latched during transit.
Workers should follow safe work practices to avoid slips and falls when top loading. If loading controls use pre-set meters, loaders must be careful to load the correct products into the assigned tanks and compartments. All compartment hatches should be shut when bottom loading, and when top loading, only the compartment being loaded should be open. When top loading, splash loading should be avoided by placing the loading tube or hose close to the bottom of the compartment and starting to load slowly until the opening is submerged. During manual top loading operations, loaders should remain in attendance, not tie down the loading shut-off (deadman) control and not overfill the compartment. Loaders should avoid exposures to product and vapour by standing upwind and averting the head when top loading through open hatches and by wearing protective equipment when handling additives, obtaining samples and draining hoses. Loaders should be aware of and follow prescribed response actions in case of a hose or line rupture, spill, release, fire or other emergency.
Unloading and delivery
When unloading tank cars and tank trucks, it is important first to assure that each product is unloaded into the proper designated storage tank and that the tank has sufficient capacity to hold all of the product being delivered. Although valves, fill pipes, lines and fill covers should be colour coded or otherwise marked to identify the product contained, the driver should still be responsible for product quality during delivery. Any misdelivery of product, mixing or contamination should be immediately reported to the recipient and to the company to prevent serious consequences. When drivers or operators are required to additize products or obtain samples from storage tanks following delivery to assure product quality or for any other reason, all safety and health provisions specific to the exposure should be followed. Persons engaged in delivery and unloading operations should remain in the vicinity at all times and know what to do in an emergency, including notification, stopping product flow, cleaning spills and when to leave the area.
Pressurized tanks may be unloaded by compressor or pump, and unpressurized tanks by gravity, vehicle pump or recipient pump. Tank trucks and tank cars which carry lubrication or industrial oils, additives and acids are sometimes unloaded by pressurizing the tank with an inert gas such as nitrogen. Tank cars or tank trucks may need to be heated using steam or electric coils in order to unload heavy crude oils, viscous products and waxes. All of these activities have inherent dangers and exposures. Where required by regulation, unloading should not commence until the vapour recovery hoses have been connected between the delivery tank and the storage tank. When delivering petroleum products to residences, farms and commercial accounts, drivers should gauge any tank which is not equipped with a vent alarm in order to prevent an overfill.
Loading-rack fire protection
Fires and explosions at top and bottom tank car and tank truck loading racks may occur from causes such as electrostatic build-up and incendiary spark discharge in a flammable atmosphere, unauthorized hot work, flashback from a vapour recovery unit, smoking or other unsafe practices.
Sources of ignition, such as smoking, running internal combustion engines and hot work activity, should be controlled at the loading rack at all times, and particularly during loading or other operations when a spill or release may occur. Loading racks may be equipped with portable fire extinguishers and manually or automatically operated foam, water or dry chemical fire extinguishing systems. If vapour recovery systems are in use, flame arrestors should be provided to prevent flashback from the recovery unit to the loading rack.
Drainage should be provided at loading racks to divert product spills away from the loader, tank truck or tank car and the loading rack pad. Drains should be provided with fire traps to prevent migration of flames and vapours through sewer systems. Other loading-rack safety considerations include emergency shut-down controls placed at loading spots and other strategic locations in the terminal and automatic pressure-sensing valves which stop product flow to the rack in case of a leak in the product lines. Some companies have installed automatic brake lock systems on their tank truck fill connections, which lock the brakes and will not allow the truck to be moved from the rack until the fill lines have been disconnected.
Electrostatic ignition hazards
Some products such as intermediate distillates and low-vapour-pressure fuels and solvents tend to accumulate electrostatic charges. When loading tank cars and tank trucks, there is always an opportunity for electrostatic charges to be generated by friction as product goes through lines and filters and by splash loading. This can be mitigated by designing loading racks to allow for relaxation time in piping downstream from pumps and filters. Compartments should be checked to assure that they do not contain any unbonded or floating objects which could act as static accumulators. Bottom loaded compartments may be provided with internal cables to help dissipate electrostatic charges. Sample containers, thermometers or other items should not be lowered into compartments until a waiting period of at least 1 minute has elapsed, to allow any electrostatic charge which has accumulated in the product to dissipate.
Bonding and grounding are important considerations in dissipating electrostatic charges which build up during loading operations. By keeping the fill pipe in contact with the metal side of the hatch when top loading, and through the use of metal loading arms or conductive hose when loading through closed connections, the tank truck or tank car is bonded to the loading rack, maintaining the same electrical charge between the objects so that a spark is not created when the loading tube or hose is removed. The tank car or tank truck may also be bonded to the loading rack by use of a bonding cable, which carries any accumulated charge from a terminal on the tank to the rack, where it is then grounded by a grounding cable and rod. Similar bonding precautions are needed when unloading from tank cars and tank trucks. Some loading racks are provided with electronic connectors and sensors which will not allow loading pumps to activate until a positive bond is achieved.
During cleaning, maintenance or repair, pressurized LPG tank cars or tank trucks are usually opened to the atmosphere, allowing air to enter the tank. In order to prevent combustion from electrostatic charges when loading these cars for the first time after such activities, it is necessary to reduce the oxygen level below 9.5% by blanketing the tank with inert gas, such as nitrogen. Precautions are needed to prevent liquid nitrogen from entering the tank if the nitrogen is provided from portable containers.
Switch loading
Switch loading occurs when intermediate- or low-vapour-pressure products such as diesel fuel or fuel oil are loaded into a tank car or tank truck compartment which previously contained a flammable product such as gasoline. The electrostatic charge generated during loading can discharge in an atmosphere which is within the flammable range, with a resultant explosion and fire. This hazard can be controlled when top loading by lowering the fill tube to the bottom of the compartment and loading slowly until the end of the tube is submerged to avoid splash loading or agitation. Metal to metal contact should be maintained during loading in order to provide a positive bond between the loading tube and the tank hatchway. When bottom loading, initial slow fill or splash deflectors are used to reduce static build-up. Prior to switch loading, tanks which cannot be drained dry may be flushed out with a small amount of the product to be loaded, to remove any flammable residue in sumps, lines, valves and onboard pumps.
Shipping products by rail box cars and package vans
Petroleum products are shipped by motor truck package vans and railroad box cars in metal, fibre and plastic containers of various sizes, from 55-gallon (209-l) drums to 5-gallon (19-l) pails and from 2-1/2-gallon (9.5-l) to 1-quart (.95-l) containers, in corrugated boxes, usually on pallets. Many industrial and commercial petroleum products are shipped in large metal, plastic or combination intermediate bulk containers ranging in size from 380 to over 2,660 l capacity. LPG is shipped in large and small pressure containers. In addition, samples of crude oil, finished products and used products are shipped by mail or express freight carrier to laboratories for assay and analysis.
All of these products, containers and packages have to be handled in accordance with government regulations for hazardous chemicals, flammable and combustible liquids and toxic materials. This requires the use of hazardous materials manifests, shipping documents, permits, receipts and other regulatory requirements, such as marking the outsides of packages, containers, motor trucks and box cars with proper identification and a hazard warning label. Proper utilization of tank trucks and tank cars is important to the petroleum industry. Because storage capacity is finite, delivery schedules need to be met, from the delivery of crude oil to keep refineries running to the delivery of gasoline to service stations, and from the delivery of lubricants to commercial and industrial accounts to the delivery of heating oil to homes.
LPG is supplied to consumers by bulk tank trucks which pump directly into smaller onsite storage tanks, both above ground and below ground (e.g., service stations, farms, commercial and industrial consumers). LPG is also delivered to consumers by truck or van in containers (gas cylinders or bottles). LNG is delivered in special cryogenic containers which have an inner fuel tank surrounded by insulation and an outer shell. Similar containers are provided for vehicles and appliances which use LNG as a fuel. Compressed natural gas is normally delivered in conventional compressed gas cylinders, such as those used on industrial lift trucks.
In addition to the normal safety and health precautions required in rail car and package trucking operations, such as moving and handling heavy objects and operating industrial trucks, workers should be familiar with the hazards of the products they are handling and delivering, and know what to do in case of a spill, release or other emergency. For example, intermediate bulk containers and drums should not be dropped out of box cars or from the tailgates of trucks onto the ground. Both companies and government agencies have established special regulations and requirements for drivers and operators who are involved in the transport and delivery of flammable and hazardous petroleum products.
Tank truck and package van drivers often work alone and may have to travel great distances for a number of days to deliver their loads. They work both day and night and in all sorts of weather conditions. Manoeuvring super-sized tank trucks into service stations and customer locations without hitting parked vehicles or fixed objects requires patience, skill and experience. Drivers should have the physical and mental characteristics required for this work.
Driving tank trucks is different from driving package vans in that the liquid product tends to shift forward as the truck stops, backwards as the truck accelerates and from side to side as the truck turns. Tank truck compartments should be fitted with baffles which restrict the movement of product during transport. Considerable skill is required by drivers to overcome the inertia created by this phenomenon, called “mass in motion”. Occasionally, tank truck drivers are required to pump out storage tanks. This activity requires special equipment, including suction hose and transfer pumps, and safety precautions, such as bonding and grounding to dissipate electrostatic build-up and to prevent any release of vapours or liquids.
Motor vehicle and rail car emergency response
Drivers and operators should be familiar with notification requirements and emergency response actions in case of a fire or a release of product, gas or vapour. Product identification and hazard warning placards in compliance with industry, association or national marking standards are posted on trucks and rail cars to allow emergency responders to determine the precautions needed in case of a spill or release of vapour, gas or product. Motor vehicle drivers and train operators may also be required to carry material safety data sheets (MSDSs) or other documentation describing the hazards and precautions for handling the products being transported. Some companies or government agencies require that vehicles transporting flammable liquids or hazardous materials carry first aid kits, fire extinguishers, spill clean-up materials and portable hazard warning devices or signals to alert motorists if the vehicle is stopped alongside a highway.
Special equipment and techniques are required if a tank car or tank truck needs to be emptied of product as the result of an accident or rollover. Removal of product through fixed piping and valves or by using special knock-out plates on tank truck hatches is preferred; however, under certain conditions holes may be drilled in tanks using prescribed safe work procedures. Regardless of the method of removal, tanks should be grounded and a bond connection provided between the tank being emptied and the receiving tank.
Cleaning tank cars and tank trucks
Entering a tank car or tank truck compartment for inspection, cleaning, maintenance or repair is a hazardous activity requiring that all ventilation, testing, gas freeing and other confined-space entry and permit system requirements be followed in order to assure a safe operation. Cleaning tank cars and tank trucks is not any different from cleaning petroleum-product storage tanks, and all the same safety and health exposure precautions and procedures apply. Tank cars and tank trucks may contain residue of flammable, hazardous or toxic materials in sumps and unloading piping, or have been unloaded using an inert gas, such as nitrogen, so that what may appear to be a clean, safe space is not. Tanks which have contained crude oil, residues, asphalt or high-melting-point products may need to be steam or chemically cleaned prior to ventilation and entry, or may have a pyrophoric hazard. Ventilating tanks to free them from vapours and toxic or inert gases may be accomplished by opening the lowest and furthest valve or connection on each tank or compartment and placing an air eductor at the furthest top opening. Monitoring should be performed prior to entry without respiratory protection to assure that all of the corners and low spots in the tank, such as sumps, have been thoroughly vented, and ventilation should continue while working in the tank.
Aboveground Tank Storage of Liquid Petroleum Products
Crude oil, gas, LNG and LPG, processing additives, chemicals and petroleum products are stored in aboveground and underground atmospheric (non-pressure) and pressure storage tanks. Storage tanks are located at the ends of feeder lines and gathering lines, along truck pipelines, at marine loading and unloading facilities and in refineries, terminals and bulk plants. This section covers aboveground atmospheric storage tanks in refinery, terminal and bulk plant tank farms. (Information concerning aboveground pressure tanks is covered below, and information concerning underground tanks and small aboveground tanks is in the article “Motor vehicle fuelling and servicing operations”.)
Terminals and bulk plants
Terminals are storage facilities which generally receive crude oil and petroleum products by trunk pipeline or marine vessel. Terminals store and redistribute crude oil and petroleum products to refineries, other terminals, bulk plants, service stations and consumers by pipelines, marine vessels, railroad tank cars and tank trucks. Terminals may be owned and operated by oil companies, pipeline companies, independent terminal operators, large industrial or commercial consumers or petroleum product distributors.
Bulk plants are usually smaller than terminals and typically receive petroleum products by rail tank car or tank truck, normally from terminals but occasionally direct from refineries. Bulk plants store and redistribute products to service stations and consumers by tank truck or tank wagon (small tank trucks of approximately 9,500 to 1,900 l capacity). Bulk plants may be operated by oil companies, distributors or independent owners.
Tank farms
Tank farms are groupings of storage tanks at producing fields, refineries, marine, pipeline and distribution terminals and bulk plants which store crude oil and petroleum products. Within tank farms, individual tanks or groups of two or more tanks are usually surrounded by enclosures called berms, dykes or fire walls. These tank farm enclosures may vary in construction and height, from 45-cm earth berms around piping and pumps inside dykes to concrete walls that are taller than the tanks they surround. Dykes may be built of earth, clay or other materials; they are covered with gravel, limestone or sea shells to control erosion; they vary in height and are wide enough for vehicles to drive along the top. The primary functions of these enclosures are to contain, direct and divert rain water, physically separate tanks to prevent the spread of fire in one area to another, and to contain a spill, release, leak or overflow from a tank, pump or pipe within the area.
Dyke enclosures may be required by regulation or company policy to be sized and maintained to hold a specific amount of product. For example, a dyke enclosure may need to contain at least 110% of the capacity of the largest tank therein, allowing for the volume displaced by the other tanks and the amount of product remaining in the largest tank after hydrostatic equilibrium is reached. Dyke enclosures may also be required to be constructed with impervious clay or plastic liners to prevent spilled or released product from contaminating soil or groundwater.
Storage tanks
There are a number of different types of vertical and horizontal aboveground atmospheric and pressure storage tanks in tank farms, which contain crude oil, petroleum feedstocks, intermediate stocks or finished petroleum products. Their size, shape, design, configuration, and operation depend on the amount and type of products stored and company or regulatory requirements. Aboveground vertical tanks may be provided with double bottoms to prevent leakage onto the ground and cathodic protection to minimize corrosion. Horizontal tanks may be constructed with double walls or placed in vaults to contain any leakage.
Atmospheric cone roof tanks
Cone roof tanks are aboveground, horizontal or vertical, covered, cylindrical atmospheric vessels. Cone roof tanks have external stairways or ladders and platforms, and weak roof to shell seams, vents, scuppers or overflow outlets; they may have appurtenances such as gauging tubes, foam piping and chambers, overflow sensing and signalling systems, automatic gauging systems and so on.
When volatile crude oil and flammable liquid petroleum products are stored in cone roof tanks there is an opportunity for the vapour space to be within the flammable range. Although the space between the top of the product and the tank roof is normally vapour rich, an atmosphere in the flammable range can occur when product is first put into an empty tank or as air enters the tank through vents or pressure/vacuum valves when product is withdrawn and as the tank breathes during temperature changes. Cone roof tanks may be connected to vapour recovery systems.
Conservation tanks are a type of cone roof tank with an upper and lower section separated by a flexible membrane designed to contain any vapour produced when the product warms up and expands due to exposure to sunlight in the daytime and to return the vapour to the tank when it condenses as the tank cools down at night. Conservation tanks are typically used to store aviation gasoline and similar products.
Atmospheric floating roof tanks
Floating roof tanks are aboveground, vertical, open top or covered cylindrical atmospheric vessels that are equipped with floating roofs. The primary purpose of the floating roof is to minimize the vapour space between the top of the product and the bottom of the floating roof so that it is always vapour rich, thus precluding the chance of a vapour-air mixture in the flammable range. All floating roof tanks have external stairways or ladders and platforms, adjustable stairways or ladders for access to the floating roof from the platform, and may have appurtenances such as shunts which electrically bond the roof to the shell, gauging tubes, foam piping and chambers, overflow sensing and signalling systems, automatic gauging systems and so on. Seals or boots are provided around the perimeter of floating roofs to prevent product or vapour from escaping and collecting on the roof or in the space above the roof.
Floating roofs are provided with legs which may be set in high or low positions depending on the type of operation. Legs are normally maintained in the low position so that the greatest possible amount of product can be withdrawn from the tank without creating a vapour space between the top of the product and the bottom of the floating roof. As tanks are brought out of service prior to entry for inspection, maintenance, repair or cleaning, there is a need to adjust the roof legs into the high position to allow room to work under the roof once the tank is empty. When the tank is returned to service, the legs are readjusted into the low position after it is filled with product.
Aboveground floating roof storage tanks are further classified as external floating roof tanks, internal floating roof tanks or covered external floating roof tanks.
External (open top) floating roof tanks are those with floating covers installed on open-top storage tanks. External floating roofs are usually constructed of steel and provided with pontoons or other means of flotation. They are equipped with roof drains to remove water, boots or seals to prevent vapour releases and adjustable stairways to reach the roof from the top of the tank regardless of its position. They may also have secondary seals to minimize release of vapour to the atmosphere, weather shields to protect the seals and foam dams to contain foam in the seal area in case of a fire or seal leak. Entry onto external floating roofs for gauging, maintenance or other activities may be considered confined-space entry, depending on the level of the roof below the top of the tank, the products contained in the tank and government regulations and company policy.
Internal floating roof tanks usually are cone roof tanks which have been converted by installing buoyant decks, rafts or internal floating covers inside the tank. Internal floating roofs are typically constructed of various types of sheet metal, aluminium, plastic or metal-covered plastic expanded foam, and their construction may be of the pontoon or pan type, solid buoyant material, or a combination of these. Internal floating roofs are provided with perimeter seals to prevent vapour from escaping into the portion of the tank between the top of the floating roof and the exterior roof. Pressure/vacuum valves or vents are usually provided at the top of the tank to control any hydrocarbon vapours which may accumulate in the space above the internal floater. Internal floating roof tanks have ladders installed for access from the cone roof to the floating roof. Entry onto internal floating roofs for any purpose should be considered confined-space entry.
Covered (external) floating roof tanks are basically external floating roof tanks that have been retrofitted with a geodesic dome, snow cap or similar semi-fixed cover or roof so that the floating roof is no longer open to the atmosphere. Newly constructed covered external floating roof tanks may incorporate typical floating roofs designed for internal floating roof tanks. Entry onto covered external floating roofs for gauging, maintenance or other activities may be considered confined-space entry, depending on the construction of the dome or cover, the level of the roof below the top of the tank, the products contained in the tank and government regulations and company policy.
Pipeline and marine receipts
An important safety, product quality and environmental concern in tank storage facilities is to prevent intermixing of products and overfilling tanks by developing and implementing safe operating procedures and work practices. Safe operation of storage tanks depends on receiving product into tanks within their defined capacity by designating receiving tanks prior to delivery, gauging tanks to determine the available capacity and ensuring that valves are properly aligned and that only the receiving tank inlet is opened, so the correct amount of product is delivered into the assigned tank. Drains in dyke areas surrounding tanks receiving product should normally be kept closed during receipt in case an overfill or spill occurs. Overfill protection and prevention can be accomplished by a variety of safe operating practices, including manual controls and automatic detection, signalling and shut-down systems and a means of communication, all of which should be mutually understood and acceptable to product transfer personnel at the pipeline, marine vessel and terminal or refinery.
Government regulations or company policy may require that automatic product level detection devices and signal and shut-down systems be installed on tanks receiving flammable liquids and other products from trunk pipelines or marine vessels. Where such systems are installed, electronic system integrity tests should be conducted on a regular basis or prior to product transfer, and if the system fails, transfers should follow manual receipt procedures. Receipts should be monitored manually or automatically, onsite or from a remote control location, to ensure that operations are proceeding as planned. Upon completion of transfer, all valves should be returned to normal operating position or set for the next receipt. Pumps, valves, pipe connections, bleeder and sample lines, manifold areas, drains and sumps should be inspected and maintained to assure good condition and to prevent spills and leakage.
Tank gauging and sampling
Tank storage facilities should establish procedures and safe work practices for gauging and sampling crude oil and petroleum products which take into consideration the potential hazards involved with each product stored and each type of tank in the facility. Although tank gauging is often done using automatic mechanical or electronic devices, manual gauging should be performed at scheduled intervals to assure the accuracy of the automatic systems.
Manual gauging and sampling operations usually require the operator to climb to the top of the tank. When gauging floating roof tanks, the operator then has to descend onto the floating roof unless the tank is fitted with gauging and sampling tubes that are accessible from the platform. With cone roof tanks, the gauger must open a roof hatch in order to lower the gauge into the tank. Gaugers should be aware of the confined-space entry requirements and potential hazards when entering onto covered floating roofs or down upon open-top floating roofs which are below established height levels. This may require the use of monitoring devices, such as oxygen, combustible gas and hydrogen sulphide detectors and personal and respiratory protective equipment.
Product temperatures and samples may be taken at the same time as manual gauging is conducted. Temperatures may also be recorded automatically and samples obtained from built-in sample connections. Manual gauging and sampling should be restricted while tanks are receiving product. Following the completion of receipt, a relaxation period of from 30 minutes to 4 hours, depending on the product and company policy, should be required to allow any electrostatic build-up to dissipate before conducting manual sampling or gauging. Some companies require that communications or visual contact be established and maintained between gaugers and other facility personnel when descending upon floating roofs. Entry onto tank roofs or platforms for gauging, sampling or other activities should be restricted during thunderstorms.
Tank venting and cleaning
Storage tanks are taken out of service for inspection, testing, maintenance, repair, retrofitting and tank cleaning as needed or at regular intervals dependent on government regulations, company policy and operating service requirements. Although tank venting, cleaning and entry is a potentially hazardous operation, this work can be accomplished without incident, provided that proper procedures are established and safe work practices followed. Without such precautions, injury or damage can occur from explosions, fires, lack of oxygen, toxic exposures and physical hazards.
Preliminary preparations
A number of preliminary preparations are required after it has been decided that a tank needs to be taken out of service for inspection, maintenance or cleaning. These include: scheduling storage and supply alternatives; reviewing the tank history to determine whether it has ever contained leaded product or has previously been cleaned and certified lead free; determining the amount and type of products contained and how much residue will remain in the tank; inspecting the outside of the tank, the surrounding area and the equipment to be used for product removal, vapour freeing and cleaning; assuring that personnel are trained, qualified and familiar with facility permit and safety procedures; assigning job responsibilities in accordance with the facility’s confined-space entry and hot- and safe-work permit requirements; and holding a meeting between terminal and tank cleaning personnel or contractors before tank cleaning or construction starts.
Control of ignition sources
After the removal of all available product from the tank through fixed piping, and before any water draws or sample lines are opened, all sources of ignition should be removed from the surrounding area until the tank is declared vapour free. Vacuum trucks, compressors, pumps and other equipment which is electrically or motor driven should be located upwind, either on top of or outside the dyke area, or, if inside the dyke area, at least 20 m from the tank or any other sources of flammable vapours. Tank preparation, venting and cleaning activities should cease during electrical storms.
Removing residue
The next step is to remove as much remaining product or residue in the tank as possible through pipeline and waterdraw connections. A safe-work permit may be issued for this work. Water or distillate fuel may be injected into the tank through fixed connections to help float product out of the tank. Residue removed from tanks that have contained sour crude should be kept wet until disposal to avoid spontaneous combustion.
Isolating the tank
After all available product has been removed through fixed piping, all piping connected to the tank, including product lines, vapour recovery lines, foam piping, sample lines and so on, should be disconnected by closing the valves nearest the tank and inserting blinds in the lines on the tank side of the valve to prevent any vapours from entering the tank from the lines. The portion of piping between the blinds and the tank should be drained and flushed. Valves outside the dyke area should be closed and locked or tagged. Tank pumps, internal mixers, cathodic protection systems, electronic gauging and level detection systems and so on should be disconnected, de-energized and locked or tagged out.
Vapour freeing
The tank is now ready to be made vapour free. Intermittent or continuous vapour testing should be conducted and work in the area restricted during tank ventilation. Natural ventilation, through opening the tank to the atmosphere, is not usually preferred, since it is neither as fast nor as safe as forced ventilation. There are a number of methods of mechanically venting a tank, depending on its size, construction, condition and internal configuration. In one method, cone roof tanks may be vapour freed by placing an eductor (a portable ventilator) at a hatch on the top of the tank, starting it slowly while a hatch at the bottom of the tank is opened and then setting it on high speed to draw air and vapours through the tank.
A safe- or hot-work permit should be issued covering ventilation activities. All blowers and eductors should be securely bonded to the tank shell to prevent electrostatic ignition. For safety purposes, blowers and eductors should preferably be operated by compressed air; however, explosion-proof electric- or steam-driven motors have been used. Internal floating roof tanks may need to have the portions above and below the floating roof vented separately. If vapours are discharged from a bottom hatch, a vertical tube at least 4 m above ground level and no lower than the surrounding dyke wall is needed in order to prevent vapours from collecting at low levels or reaching a source of ignition before dissipating. If necessary, vapours may be directed to the facility vapour recovery system.
As ventilation progresses, the remaining residue can be washed down and removed through the open bottom hatch by water and suction hoses, both of which should be bonded to the tank shell to prevent electrostatic ignition. Tanks which have contained sour crude oil or high-sulphur residual products may generate spontaneous heat and ignite as they dry out during ventilation. This should be avoided by wetting the inside of the tank with water to blanket the deposits from air and prevent a rise in temperature. Any iron sulphide residue should be removed from the open hatch to prevent ignition of vapours during ventilation. Workers engaged in washdown, removal and wetting activities should wear appropriate personal and respiratory protection.
Initial entry, inspection and certification
An indication of the progress being made in vapour freeing the tank can be obtained by monitoring vapours at the point of eduction during ventilation. Once it appears that the flammable vapour level is below that established by regulatory agencies or company policy, entry can be made into the tank for inspection and testing purposes. The entrant should wear appropriate personal and air-supplied respiratory protection; after testing the atmosphere at the hatch and obtaining an entry permit, the worker may enter the tank to continue testing and inspection. Checks for obstructions, falling roofs, weak supports, holes in the floor and other physical hazards should be conducted during the inspection.
Cleaning, maintenance and repair
As ventilation continues and the vapour levels in the tank drop lower, permits may be issued allowing entry by workers with appropriate personal and respiratory equipment, if needed, to start cleaning the tank. Monitoring for oxygen, flammable vapours and toxic atmospheres should continue, and if the levels inside the tank exceed those established for entry, the permit should automatically expire and the entrants should immediately leave the tank until the safe level is again achieved and the permit is reissued. Ventilation should continue during cleaning operations as long as any residue or sludge remains in the tank. Only low-voltage lighting or approved flashlights should be used during inspection and clean-up.
After tanks have been cleaned and dried, a final inspection and testing should be conducted before maintenance, repair or retrofitting work is started. Careful inspection of sumps, wells, floor plates, floating roof pontoons, supports and columns is needed to assure that no leaks have developed which allowed product to enter these spaces or seep beneath the floor. Spaces between foam seals and weather shields or secondary containment should also be inspected and tested for vapours. If the tank has previously contained leaded gasoline, or if no tank history is available, a lead-in-air test should be conducted and the tank certified lead free before workers are allowed inside without air-supplied respiratory equipment.
A hot-work permit should be issued covering welding, cutting and other hot work, and a safe-work permit issued to cover other repair and maintenance activities. Welding or hot work can create toxic or noxious fumes inside the tank, requiring monitoring, respiratory protection and continued ventilation. When tanks are to be retrofitted with double bottoms or internal floating roofs, a large hole is often cut into the side of the tank to provide unrestricted access and avoid the need for confined-space entry permits.
Blast cleaning and painting the outside of tanks usually follows tank cleaning and is completed before the tank is returned to service. These activities, together with cleaning and painting tank farm piping, may be performed while tanks and pipes are in service, by implementing and following prescribed safety procedures, such as conducting monitoring for hydrocarbon vapours and stopping blast cleaning while nearby tanks are receiving flammable liquid products. Blast cleaning with sand has the potential for hazardous exposure to silica; therefore, many government agencies and companies require the use of special non-toxic blast cleaning materials or grit, which may be collected, cleaned and recycled. Special vacuum collection blast cleaning devices may be used in order to avoid contamination when cleaning leaded paint from tanks and piping. Following blast cleaning, spots in the tank walls or piping suspected of having leaks and seeps should be tested and repaired before being painted.
Returning the tank to service
In preparation for return to service upon completion of tank cleaning, inspection, maintenance or repair, the hatches are closed, all blinds are removed and the piping is reconnected to the tank. Valves are unlocked, opened and aligned, and mechanical and electrical devices are reactivated. Many government agencies and companies require tanks to be hydrostatically tested to assure that there are no leaks before they are returned to service. Since a considerable amount of water is required to obtain the necessary pressure head for an accurate test, a water bottom topped with diesel fuel is often used. Upon completion of the testing, the tank is emptied and made ready to receive product. After receipt is completed and a relaxation time has elapsed, the legs on floating roof tanks are reset into the low position.
Fire protection and prevention
Whenever hydrocarbons are present in closed containers such as storage tanks in refineries, terminals and bulk plants, the potential exists for release of liquids and vapours. These vapours could mix with air in the flammable range and, if subjected to a source of ignition, cause an explosion or fire. Regardless of the capability of fire protection systems and personnel in the facility, the key to fire protection is fire prevention. Spills and releases should be stopped from entering sewers and drainage systems. Small spills should be covered with wet blankets, and larger spills with foam, to prevent vapours from escaping and mixing with air. Sources of ignition in areas when hydrocarbon vapours may be present should be eliminated or controlled. Portable fire extinguishers should be carried on service vehicles and located at accessible and strategic positions throughout the facility.
The establishment and implementation of safe work procedures and practices such as hot- and safe- (cold-) work permit systems, electrical classification programmes, lockout/tagout programmes, and employee and contractor training and education is critical to preventing fires. Facilities should develop preplanned emergency procedures, and employees should be knowledgeable in their responsibilities for reporting and responding to fires and evacuation. Telephone numbers of responsible persons and agencies to be notified in case of an emergency should be posted at the facility and a means of communication provided. Local fire departments, emergency response, public safety and mutual aid organizations should also be aware of the procedures and familiar with the facility and its hazards.
Hydrocarbon fires are controlled by one or a combination of methods, as follows:
- Removing fuel. One of the best and easiest methods of controlling and extinguishing a hydrocarbon fire is to shut off the source of fuel by closing a valve, diverting product flow or, if a small amount of product is involved, controlling exposures while allowing the product to burn away. Foam may also be used to cover hydrocarbon spills to prevent vapours from being emitted and mixing with the air.
- Removing oxygen. Another method is to shut off the supply of air or oxygen by smothering fires with foam or water fog, or by using carbon dioxide or nitrogen to displace air in enclosed spaces.
- Cooling. Water fog, mist or spray and carbon dioxide may be used to extinguish certain petroleum product fires by cooling the temperature of the fire below the product’s ignition temperature and by stopping vapours from forming and mixing with air.
- Interrupting combustion. Chemicals such as dry powders and halon extinguish fires by interrupting the chemical reaction of the fire.
Storage tank fire protection
Storage tank fire protection and prevention is a specialized science which depends on the interrelationship of tank type, condition and size; product and amount stored in the tank; tank spacing, dyking and drainage; facility fire protection and response capabilities; outside assistance; and company philosophy, industry standards and government regulations. Storage tank fires may be easy or very difficult to control and extinguish, depending primarily on whether the fire is detected and attacked during its initial inception. Storage tank operators should refer to the numerous recommended practices and standards developed by organizations such as the American Petroleum Institute (API) and the US National Fire Protection Association (NFPA), which cover storage tank fire prevention and protection in great detail.
If open-top floating roof storage tanks are out of round or if the seals are worn or not tight against the tank shells, vapours can escape and mix with air, forming flammable mixtures. In such situations, when lightning strikes, fires may occur at the point where the roof seals meet the shell of the tank. If detected early, small seal fires can often be extinguished by a hand-carried dry powder extinguisher or with foam applied from a foam hose or foam system.
If a seal fire cannot be controlled with hand extinguishers or hose streams, or if a large fire is in progress, foam may be applied onto the roof through fixed or semi-fixed systems or by large foam monitors. Precautions are necessary when applying foam onto the roofs of floating roof tanks; if too much weight is placed on the roof, it may tilt or sink, allowing a large surface area of product to be exposed and become involved in the fire. Foam dams are used on floating roof tanks to trap foam in the area between the seals and the tank shell. As the foam settles, water drains out under the foam dams and should be removed through the tank roof drain system to avoid overweighing and sinking the roof.
Depending on government regulations and company policy, storage tanks may be provided with fixed or semi-fixed foam systems which include: piping to the tanks, foam risers and foam chambers on the tanks; subsurface injection piping and nozzles inside the bottom of tanks; and distribution piping and foam dams on the tops of tanks.With fixed systems, foam-water solutions are generated in centrally located foam houses and pumped to the tank through a piping system. Semi-fixed foam systems typically use portable foam tanks, foam generators and pumps which are brought to the tank involved, connected to a water supply and connected to the tank’s foam piping.
Water-foam solutions may also be centrally generated and distributed within the facility through a system of piping and hydrants, and hoses would be used to connect the nearest hydrant to the tank’s semi-fixed foam system. Where tanks are not provided with fixed or semi-fixed foam systems, foam may be applied onto the tops of tanks, using foam monitors, fire hoses and nozzles. Regardless of the method of application, in order to control a fully involved tank fire, a specific amount of foam must be applied using special techniques at a specific concentration and rate of flow for a minimum amount of time depending primarily on the size of the tank, the product involved and the surface area of the fire. If there is not enough foam concentrate available to meet the required application criteria, the possibility of control or extinguishment is minimal.
Only trained and knowledgeable fire-fighters should be allowed to use water to fight liquid petroleum tank fires. Instantaneous eruptions, or boil-overs, can occur when water turns into steam upon direct application onto tank fires involving crude or heavy petroleum products. As water is heavier than most hydrocarbon fuels, it will sink to the bottom of a tank and, if enough is applied, fill the tank and push the burning product up and over the top of the tank.
Water is typically used to control or extinguish spill fires around the outside of tanks so that valves can be operated to control product flow, to cool the sides of involved tanks to prevent boiling liquid–expanding vapour explosions (BLEVEs—see the section “Fire hazards of LHGs” below) and to reduce the effect of heat and flame impingement on adjacent tanks and equipment. Because of the need for specialized training, materials and equipment, rather than allow employees to attempt to extinguish tank fires, many terminals and bulk plants have established a policy to remove as much product as possible from the involved tank, protect adjacent structures from heat and flame and allow the remaining product in the tank to burn under controlled conditions until the fire burns out.
Terminal and bulk plant health and safety
Storage tank foundations, supports and piping should be regularly inspected for corrosion, erosion, settling or other visible damage to prevent loss or degradation of product. Tank pressure/vacuum valves, seals and shields, vents, foam chambers, roof drains, water draw-off valves and overfill detection devices should be inspected, tested and maintained on a regular schedule, including removal of ice in the winter. Where flame arrestors are installed on tank vents or in vapour recovery lines, they have to be inspected and cleaned regularly and kept free of frost in the winter to ensure proper operation. Valves on tank outlets which close automatically in case of fire or drop in pressure should be checked for operability.
Dyke surfaces should drain or slope away from tanks, pumps and piping to remove any spilled or released product to a safe area. Dyke walls should be maintained in good condition, with drain valves kept closed except when draining water and dyke areas excavated as needed to maintain design capacity. Stairways, ramps, ladders, platforms and railings to loading racks, dykes and tanks should be maintained in a safe condition, free of ice, snow and oil. Leaking tanks and piping should be repaired as soon as possible. The use of victaulic or similar couplings on piping within dyked areas which could be exposed to heat should be discouraged to prevent lines from opening during fires.
Safety procedures and safe work practices should be established and implemented, and training or education provided, so that terminal and bulk plant operators, maintenance personnel, tank truck drivers and contractor personnel can work safely. These should include, as a minimum, information concerning the basics of hydrocarbon fire ignition, control and extinguishment; hazards and protection from exposures to toxic substances such as hydrogen sulphide and polynuclear aromatics in crude oil and residual fuels, benzene in gasoline and additives such as tetraethyl lead and methyl-tert-butyl ether (MTBE); emergency response actions; and normal physical and climatic hazards associated with this activity.
Asbestos or other insulation may be present in the facility as protection for tanks and piping. Appropriate safe-work and personal protective measures should be established and followed for handling, removing and disposing of such materials.
Environmental protection
Terminal operators and employees should be aware of and comply with government regulations and company policies covering environmental protection of ground and surface water, soil and air from pollution by petroleum liquids and vapours, and for handling and removing hazardous waste.
- Water contamination. Many terminals have oil/water separators to handle contaminated water from tank containment areas, run-off from loading racks and parking areas and water drained from tanks and open-top tank roofs. Terminals may be required to meet established water quality standards and obtain permits before discharging water.
- Air pollution. Air pollution prevention includes minimizing releases of vapours from valves and vents. Vapour recovery units collect vapours from loading racks and marine docks, even when tanks are vented prior to entry. These vapours are either processed and returned to storage as liquids or burned.
- Spills on land and water. Government agencies and companies may require that oil storage facilities have spill prevention control and counter-measure plans, and that personnel be trained and aware of the potential hazards, notifications to be made and the actions to take in case of a spill or release. In addition to handling spills within the terminal facility, personnel are often trained and equipped to respond to offsite emergencies, such as a tank truck rollover.
- Sewage and hazardous waste. Terminals may be required to meet regulatory requirements and obtain permits for discharge of sewage and oily waste to public or privately owned treatment works. Various government requirements and company procedures may apply to the onsite storage and handling of hazardous waste such as asbestos insulation, tank cleaning residue and contaminated product. Workers should be trained in this activity and be made aware of the potential hazards from exposures which could occur.
LHG Storage and Handling
Bulk storage tanks
LHGs are stored in large bulk storage tanks at the point of process (gas and oil fields, gas plants and refineries) and at the point of distribution to the consumer (terminals and bulk plants). The two most commonly used methods of bulk storage of LHGs are:
- Under high pressure at ambient temperature. LHG is stored in steel pressure tanks (at 1.6 to 1.8 mPa) or in underground impermeable rock or salt formations.
- Under pressure close to atmospheric at low temperature. LHG is stored in thin-walled, heat-insulated steel storage tanks; in reinforced concrete tanks above and below ground; and in underground cryogenic storage tanks. Pressure is maintained close to atmospheric (0.005 to 0.007 mPa) at a temperature of –160°C for LNG stored in cryogenic underground storage tanks.
LPG bulk storage vessels are either cylindrically (bullet) shaped horizontal tanks (40 to 200 m3) or spheres (up to 8,000 m3). Refrigerated storage is typical for storage in excess of 2,400 m3. Both horizontal tanks, which are fabricated in shops and transported to the storage site, and spheres, which are built onsite, are designed and constructed in accordance with rigid specifications, codes and standards.
The design pressure of storage tanks should not be less than the vapour pressure of the LHG to be stored at the maximum service temperature. Tanks for propane-butane mixtures should be designed for 100% propane pressure. Consideration should be given to additional pressure requirements resulting from the hydrostatic head of the product at maximum fill and the partial pressure of non-condensible gases in the vapour space. Ideally, liquefied hydrocarbon gas storage vessels should be designed for full vacuum. If not, vacuum relief valves must be provided. Design features should also include pressure relief devices, liquid level gauges, pressure and temperature gauges, internal shut-off valves, back flow preventers and excess flow check valves. Emergency fail-safe shut-down valves and high level signals may also be provided.
Horizontal tanks are either installed aboveground, placed on mounds or buried underground, typically downwind from any existing or potential sources of ignition. If the end of a horizontal tank ruptures from over-pressurization, the shell will be propelled in the direction of the other end. Therefore, it is prudent to place an aboveground tank so that its length is parallel to any important structure (and so that neither end points toward any important structure or equipment). Other factors include tank spacing, location, and fire prevention and protection. Codes and regulations specify minimum horizontal distances between pressurized liquefied hydrocarbon gas storage vessels and adjoining properties, tanks and important structures as well as potential sources of ignition, including processes, flares, heaters, power transmission lines and transformers, loading and unloading facilities, internal combustion engines and gas turbines.
Drainage and spill containment are important considerations in designing and maintaining liquid hydrocarbon gas tank storage areas in order to direct spills to a location where they will minimize risk to the facility and surrounding areas. Dyking and impounding may be used where spills present a potential hazard to other facilities or to the public. Storage tanks are not usually dyked, but the ground is graded so that vapours and liquids do not collect underneath or around the storage tanks, in order to keep burning spills from impinging upon storage tanks.
Cylinders
LHGs for use by consumers, either LNG or LPG, are stored in cylinders at temperatures above their boiling points at normal temperature and pressure. All LNG and LPG cylinders are provided with protective collars, safety valves and valve caps. The basic types of consumer cylinders in use are:
- vapour withdrawal (1/2 to 50 kg) cylinders used by consumers, with larger ones usually refillable on an exchange basis with the supplier
- liquid withdrawal cylinders for dispensing into small consumer-owned refillable cylinders
- motor vehicle fuel cylinders, including vehicle cylinders (40 kg) permanently installed as fuel tanks on motor vehicles and filled and used in the horizontal position, and industrial truck cylinders designed to be stored, filled and handled in the upright position, but used in the horizontal position.
Properties of hydrocarbon gases
According to the NFPA, flammable (combustible) gases are those which burn in the normal concentrations of oxygen in air. The burning of flammable gases is similar to flammable hydrocarbon liquid vapours, as a specific ignition temperature is needed to initiate the burning reaction, and each will burn only within a certain defined range of gas-air mixtures. Flammable liquids have a flashpoint, which is the temperature (always below the boiling point) at which they emit sufficient vapours for combustion. There is no apparent flashpoint for flammable gases, since they are normally at temperatures above their boiling points, even when liquefied, and are therefore always at temperatures well in excess of their flashpoints.
The NFPA (1976) defines compressed and liquefied gases as follows:
- “Compressed gases are those which at all normal atmospheric temperatures inside their containers, exist solely in the gaseous state under pressure.”
- “Liquefied gases are those which at normal atmospheric temperatures inside their containers, exist partly in the liquid state and partly in the gaseous state, and are under pressure as long as any liquid remains in the container.”
The major factor which determines the pressure inside the vessel is the temperature of the liquid stored. When exposed to the atmosphere, the liquefied gas very rapidly vaporizes, travelling along the ground or water surface unless dispersed into the air by wind or mechanical air movement. At normal atmospheric temperatures, about one-third of the liquid in the container will vaporize.
Flammable gases are further classified as fuel gas and industrial gas. Fuel gases, including natural gas (methane) and LPGs (propane and butane), are burned with air to produce heat in ovens, furnaces, water heaters and boilers. Flammable industrial gases, such as acetylene, are used in processing, welding, cutting and heat-treating operations. The differences in combustion properties of LNG and LPGs are shown in table 1.
Table 1. Typical approximate combustion properties of liquified hydrocarbon gases.
|
Type gas |
Flammable range |
Vapour pressure |
Normal init. boiling |
Weight (pounds/gal) |
BTU per ft3 |
Specific gravity |
|
LNG |
4.5–14 |
1.47 |
–162 |
3.5–4 |
1,050 |
9.2–10 |
|
LPG (propane) |
2.1–9.6 |
132 |
–46 |
4.24 |
2,500 |
1.52 |
|
LPG (butane) |
1.9–8.5 |
17 |
–9 |
4.81 |
3,200 |
2.0 |
Safety hazards of LPG and LNG
The safety hazards applicable to all LHGs are associated with flammability, chemical reactivity, temperature and pressure. The most serious hazard with LHGs is the unplanned release from containers (canisters or tanks) and contact with an ignition source. Release can occur by failure of the container or valves for a variety of reasons, such as overfilling a container or from overpressure venting when the gas expands due to heating.
The liquid phase of LPG has a high coefficient of expansion, with liquid propane expanding 16 times and liquid butane 11 times as much as water with the same rise in temperature. This property must be considered when filling containers, as free space must be left for the vapour phase. The correct quantity to be filled is determined by a number of variables, including the nature of the liquefied gas, temperature at time of filling and expected ambient temperatures, size, type (insulated or uninsulated) and location of container (above or below ground). Codes and regulations establish allowable quantities, known as “filling densities”, which are specific for individual gases or families of similar gases. Filling densities may be expressed by weight, which are absolute values, or by liquid volume, which must always be temperature corrected.
The maximum amount that LPG pressure containers should be filled with liquid is 85% at 40 ºC (less at higher temperatures). Because LNG is stored under low temperatures, LNG containers may be liquid filled from 90% to 95%. All containers are provided with overpressure relief devices which normally discharge at pressures relating to liquid temperatures above normal atmospheric temperatures. As these valves cannot reduce the internal pressure to atmospheric, the liquid will always be at a temperature above its normal boiling point. Pure compressed and liquefied hydrocarbon gases are non-corrosive to steel and most copper alloys. However, corrosion can be a serious problem when sulphur compounds and impurities are present in the gas.
LPGs are 1-1/2 to 2 times heavier than air and, when released in air, tend to quickly disperse along the ground or water surface and collect in low areas. However, as soon as the vapour is diluted by air and forms a flammable mixture, its density is essentially the same as air, and it disperses differently. Wind will significantly reduce the dispersion distance for any size of leak. LNG vapours react differently from LPG. Because natural gas has a low vapour density (0.6), it will mix and disperse rapidly in open air, reducing the chance of forming a flammable mixture with air. Natural gas will collect in enclosed spaces and form vapour clouds which could be ignited. Figure 4 indicates how a liquefied natural gas vapour cloud spreads downwind in different spill situations.
Figure 4. Extension of LNG vapour cloud downwind from different spills (wind speed 8.05 km/h).
Although LHG is colourless, when released in air its vapours will be noticeable due to the condensation and freezing of water vapour contained in the atmosphere which is contacted by the vapour. This may not occur if the vapour is near ambient temperature and its pressure is relatively low. Instruments are available which can detect the presence of leaking LHG and signal an alarm at levels as low as 15 to 20% of the lower flammable limit (LFL). These devices may also stop all operations and activate suppression systems, should the concentrations of gas reach 40 to 50% of the LFL. Some industrial operations provide forced ventilation to keep leaking fuel-air concentrations below the lower flammable limit. Heater and furnace burners may also have devices which automatically stop the flow of gas if the flame is extinguished.
LHG leakage from tanks and containers may be minimized by the use of limiting and flow control devices. When decompressed and released, LHG will flow out of containers with a low negative pressure and low temperature. The auto refrigeration temperature of the product at the lower pressure must be considered when selecting materials of construction for containers and valves, to prevent metal embrittlement followed by rupture or failure due to exposure to low temperatures.
LHG can contain water in both its liquid and gaseous phases. Water vapour can saturate gas in a specific amount at a given temperature and pressure. If the temperature or pressure changes, or the water vapour content exceeds the evaporation limits, the water condenses. This can create ice plugs in valves and regulators and form hydrocarbon hydrate crystals in pipelines, devices and other apparatus. These hydrates can be decomposed by heating the gas, lowering the gas pressure or introducing materials, such as methanol, which reduce the water vapour pressure.
There are differences in the characteristics of compressed and liquefied gases which must be considered from safety, health and fire aspects. As an example, the differences in the characteristics of compressed natural gas and LNG are illustrated in table 2.
Table 2. Comparison of characteristics of compressed and liquified gas.
|
Type gas |
Flammable range |
Heat release rate (BTU/gal) |
Storage condition |
Fire risks |
Health risks |
|
Compressed natural gas |
5.0–15 |
19,760 |
Gas at 2,400 to 4,000 psi |
Flammable gas |
Asphyxiant; overpressure |
|
LNG |
4.5–14 |
82,450 |
Liquid at 40–140 psi |
Flammable gas 625:1 expansion ratio; BLEVE |
Asphyxiant; cryogenic liquid |
Health hazards of LHGs
The primary occupational injury concern in handling LHGs is the potential hazard of frostbite to the skin and eyes from contact with liquid during handling and storage activities including sampling, measuring, filling, receiving and delivery. As with other fuel gases, when improperly burned, compressed and liquefied hydrocarbon gases will emit undesirable levels of carbon monoxide.
Under atmospheric pressures and low concentrations, compressed and liquefied hydrocarbon gases are normally non-toxic, but they are asphyxiants—they will displace oxygen (air) if released in enclosed or confined spaces. Compressed and liquefied hydrocarbon gases may be toxic if they contain sulphur compounds, especially hydrogen sulphide. Because LHGs are colourless and odourless, safeguards include adding odourants, such as mercaptans, to consumer fuel gases to aid in leak detection. Safe work practices should be implemented to protect workers from exposure to mercaptans and other additives during storage and injection. Exposure to LPG vapours in concentrations at or above the LFL may cause a general central nervous system depression similar to anaesthesia gases or intoxicants.
Fire hazards of LHGs
Failure of liquefied gas (LNG and LPG) containers constitutes a more severe hazard than failure of compressed gas containers, as they release greater quantities of gas. When heated, liquefied gases react differently from compressed gases, because they are two-phase (liquid-vapour) products. As the temperature rises, the vapour pressure of the liquid is increased, resulting in increased pressure inside the container. The vapour phase first expands, followed by expansion of the liquid, which then compresses the vapour. The design pressure for LHG vessels is therefore assumed to be near that of the gas pressure at maximum possible ambient temperature.
When a liquefied gas container is exposed to fire, a serious condition can occur if the metal in the vapour space is allowed to heat. Unlike the liquid phase, the vapour phase absorbs little heat. This allows the metal to heat rapidly until a critical point is reached at which an instantaneous, catastrophic explosive failure of the container occurs. This phenomenon is known as a BLEVE. The magnitude of a BLEVE depends on the amount of liquid vaporizing when the container fails, the size of the pieces of exploded container, the distance they travel and the areas they impact. Uninsulated LPG containers may be protected against a BLEVE by applying cooling water to those areas of the container which are in the vapour phase (not in contact with LPG).
Other more common fire hazards associated with compressed and liquefied hydrocarbon gases include electrostatic discharge, combustion explosions, large open-air explosions and small leaks from pump seals, containers, valves, pipes, hoses and connections.
- Electrostatic charges may be generated when LHG is shipped in pipelines, when loaded and unloaded, in blending and filtering and during tank cleaning.
- Combustion explosions result when escaping gas or vapour is contained in a confined space or structure and combines with air to create a flammable mixture. When this flammable mixture contacts a source of ignition, it burns instantaneously and rapidly, producing extreme heat. The very hot air expands quickly, causing a considerable rise in pressure. If the space or structure is not strong enough to contain this pressure, a combustion explosion occurs.
- Flammable gas fires result when there is no confinement of the escaping gas or vapours, or ignition occurs when only a small amount of gas has been released.
- Large open-air explosions occur when a massive failure of a container releases a large vapour cloud of gas which is ignited before it disperses.
Controlling sources of ignition in hazardous areas is essential for the safe handling of compressed and liquefied hydrocarbon gases. This may be accomplished by establishing a permit system to authorize and control hot work, smoking, operation of motor vehicles or other internal combustion engines, and the use of open flames in areas where compressed and liquefied hydrocarbon gas is transported, stored and handled. Other safeguards include the use of properly classified electrical equipment and bonding and grounding systems to neutralize and dissipate static electricity.
The best means of reducing the fire hazard of leaking compressed or liquefied hydrocarbon gas is to stop the release, or shut off the flow of product, if possible. Although most LHGs will vaporize upon contact with air, lower vapour pressure LPGs, such as butane, and even some higher vapour pressure LPGs, such as propane, will pool if ambient temperatures are low. Water should not be applied to these pools, as it will create turbulence and increase the rate of vaporization. Vaporization from pool spills can be controlled by the careful application of foam. Water, if correctly applied against a leaking valve or small rupture, can freeze upon contact with the cold LHG and block the leak. LHG fires require controlling heat impingement upon storage tanks and containers by the application of cooling water. While compressed and liquefied hydrocarbon gas fires can be extinguished by the use of water spray and dry powder extinguishers, it is often more prudent to allow controlled burning so that a combustible explosive vapour cloud does not form and re-ignite should the gas continue to escape after the fire is extinguished.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."