Children categories

94. Education and Training Services (7)

94. Education and Training Services
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Diseases affecting day-care workers & teachers
2. Hazards & precautions for particular classes
3. Summary of hazards in colleges & universities
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

95. Emergency and Security Services (9)

95. Emergency and Security Services
Chapter Editor: Tee L. Guidotti
Table of Contents
Tables and Figures
Tables
Click a link below to view table in article context.
1. Recommendations & criteria for compensation
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

96. Entertainment and the Arts (31)

96. Entertainment and the Arts
Chapter Editor: Michael McCann
Table of Contents
Tables and Figures
Arts and Crafts
Performing and Media Arts
Entertainment
Tables
Click a link below to view table in article context.
1. Precautions associated with hazards
2. Hazards of art techniques
3. Hazards of common stones
4. Main risks associated with sculpture material
5. Description of fibre & textile crafts
6. Description of fibre & textile processes
7. Ingredients of ceramic bodies & glazes
8. Hazards & precautions of collection management
9. Hazards of collection objects
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

97. Health Care Facilities and Services (25)

97. Health Care Facilities and Services
Chapter Editor: Annelee Yassi
Table of Contents
Tables and Figures
Health Care: Its Nature and Its Occupational Health Problems
Annalee Yassi and Leon J. Warshaw
Social Services
Susan Nobel
Home Care Workers: The New York City Experience
Lenora Colbert
Occupational Health and Safety Practice: The Russian Experience
Valery P. Kaptsov and Lyudmila P. Korotich
Ergonomics and Health Care
Hospital Ergonomics: A Review
Madeleine R. Estryn-Béhar
Strain in Health Care Work
Madeleine R. Estryn-Béhar
Case Study: Human Error and Critical Tasks: Approaches for Improved System Performance
Work Schedules and Night Work in Health Care
Madeleine R. Estryn-Béhar
The Physical Environment and Health Care
Exposure to Physical Agents
Robert M. Lewy
Ergonomics of the Physical Work Environment
Madeleine R. Estryn-Béhar
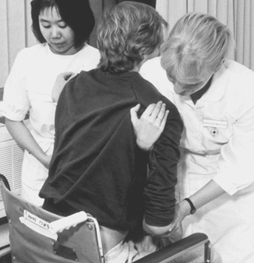
Prevention and Management of Back Pain in Nurses
Ulrich Stössel
Case Study: Treatment of Back Pain
Leon J. Warshaw
Health Care Workers and Infectious Disease
Overview of Infectious Diseases
Friedrich Hofmann
Prevention of Occupational Transmission of Bloodborne Pathogens
Linda S. Martin, Robert J. Mullan and David M. Bell
Tuberculosis Prevention, Control and Surveillance
Robert J. Mullan
Chemicals in the Health Care Environment
Overview of Chemical Hazards in Health Care
Jeanne Mager Stellman
Managing Chemical Hazards in Hospitals
Annalee Yassi
Waste Anaesthetic Gases
Xavier Guardino Solá
Health Care Workers and Latex Allergy
Leon J. Warshaw
The Hospital Environment
Buildings for Health Care Facilities
Cesare Catananti, Gianfranco Damiani and Giovanni Capelli
Hospitals: Environmental and Public Health Issues
M.P. Arias
Hospital Waste Management
M.P. Arias
Managing Hazardous Waste Disposal Under ISO 14000
Jerry Spiegel and John Reimer
Tables
Click a link below to view table in article context.
1. Examples of health care functions
2. 1995 integrated sound levels
3. Ergonomic noise reduction options
4. Total number of injuries (one hospital)
5. Distribution of nurses’ time
6. Number of separate nursing tasks
7. Distribution of nurses' time
8. Cognitive & affective strain & burn-out
9. Prevalence of work complaints by shift
10. Congenital abnormalities following rubella
11. Indications for vaccinations
12. Post-exposure prophylaxis
13. US Public Health Service recommendations
14. Chemicals’ categories used in health care
15. Chemicals cited HSDB
16. Properties of inhaled anaesthetics
17. Choice of materials: criteria & variables
18. Ventilation requirements
19. Infectious diseases & Group III wastes
20. HSC EMS documentation hierarchy
21. Role & responsibilities
22. Process inputs
23. List of activities
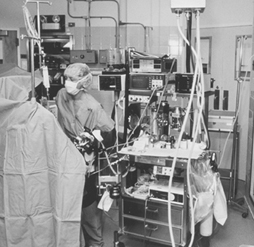
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

98. Hotels and Restaurants (4)

98. Hotels and Restaurants
Chapter Editor: Pam Tau Lee
Table of Contents

99. Office and Retail Trades (7)
99. Office and Retail Trades
Chapter Editor: Jonathan Rosen
Table of Contents
Tables and Figures
The Nature of Office and Clerical Work
Charles Levenstein, Beth Rosenberg and Ninica Howard
Professionals and Managers
Nona McQuay
Offices: A Hazard Summary
Wendy Hord
Bank Teller Safety: The Situation in Germany
Manfred Fischer
Telework
Jamie Tessler
The Retail Industry
Adrienne Markowitz
Case Study: Outdoor Markets
John G. Rodwan, Jr.
Tables
Click a link below to view table in article context.
1. Standard professional jobs
2. Standard clerical jobs
3. Indoor air pollutants in office buildings
4. Labour statistics in the retail industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

100. Personal and Community Services (6)
100. Personal and Community Services
Chapter Editor: Angela Babin
Table of Contents
Tables and Figures
Indoor Cleaning Services
Karen Messing
Barbering and Cosmetology
Laura Stock and James Cone
Laundries, Garment and Dry Cleaning
Gary S. Earnest, Lynda M. Ewers and Avima M. Ruder
Funeral Services
Mary O. Brophy and Jonathan T. Haney
Domestic Workers
Angela Babin
Case Study: Environmental Issues
Michael McCann
Click a link below to view table in article context.
1. Postures observed during dusting in a hospital
2. Dangerous chemicals used in cleaning
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

101. Public and Government Services (12)

101. Public and Government Services
Chapter Editor: David LeGrande
Table of Contents
Tables and Figurs
Occupational Health and Safety Hazards in Public and Governmental Services
David LeGrande
Case Report: Violence and Urban Park Rangers in Ireland
Daniel Murphy
Inspection Services
Jonathan Rosen
Postal Services
Roxanne Cabral
Telecommunications
David LeGrande
Hazards in Sewage (Waste) Treatment Plants
Mary O. Brophy
Domestic Waste Collection
Madeleine Bourdouxhe
Street Cleaning
J.C. Gunther, Jr.
Sewage Treatment
M. Agamennone
Municipal Recycling Industry
David E. Malter
Waste Disposal Operations
James W. Platner
The Generation and Transport of Hazardous Wastes: Social and Ethical Issues
Colin L. Soskolne
Tables
Click a link below to view table in article context.
1. Hazards of inspection services
2. Hazardous objects found in domestic waste
3. Accidents in domestic waste collection (Canada)
4. Injuries in the recycling industry
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

102. Transport Industry and Warehousing (18)

102. Transport Industry and Warehousing
Chapter Editor: LaMont Byrd
Table of Contents
Tables and Figures
General Profile
LaMont Byrd
Case Study: Challenges to Workers’ Health and Safety in the Transportation and Warehousing Industry
Leon J. Warshaw
Air Transport
Airport and Flight Control Operations
Christine Proctor, Edward A. Olmsted and E. Evrard
Case Studies of Air Traffic Controllers in the United States and Italy
Paul A. Landsbergis
Aircraft Maintenance Operations
Buck Cameron
Aircraft Flight Operations
Nancy Garcia and H. Gartmann
Aerospace Medicine: Effects of Gravity, Acceleration and Microgravity in the Aerospace Environment
Relford Patterson and Russell B. Rayman
Helicopters
David L. Huntzinger
Road Transport
Truck and Bus Driving
Bruce A. Millies
Ergonomics of Bus Driving
Alfons Grösbrink and Andreas Mahr
Motor Vehicle Fuelling and Servicing Operations
Richard S. Kraus
Case Study: Violence in Gasoline Stations
Leon J. Warshaw
Rail Transport
Rail Operations
Neil McManus
Case Study: Subways
George J. McDonald
Water Transport
Water Transportation and the Maritime Industries
Timothy J. Ungs and Michael Adess
Storage
Storage and Transportation of Crude Oil, Natural Gas, Liquid Petroleum Products and Other Chemicals
Richard S. Kraus
Warehousing
John Lund
Case Study: US NIOSH Studies of Injuries among Grocery Order Selectors
Tables
Click a link below to view table in article context.
1. Bus driver seat measurements
2. Illumination levels for service stations
3. Hazardous conditions & administration
4. Hazardous conditions & maintenance
5. Hazardous conditions & right of way
6. Hazard control in the Railway industry
7. Merchant vessel types
8. Health hazards common across vessel types
9. Notable hazards for specific vessel types
10. Vessel hazard control & risk-reduction
11. Typical approximate combustion properties
12. Comparison of compressed & liquified gas
13. Hazards involving order selectors
14. Job safety analysis: Fork-lift operator
15. Job safety analysis: Order selector
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Overview of Infectious Diseases
Infectious diseases play a significant part in worldwide occurrences of occupational disease in HCWs. Since reporting procedures vary from country to country, and since diseases considered job-related in one country may be classified as non-occupational elsewhere, accurate data concerning their frequency and their proportion of the overall number of occupational diseases among HCWs are difficult to obtain. The proportions range from about 10% in Sweden (Lagerlöf and Broberg 1989), to about 33% in Germany (BGW 1993) and nearly 40% in France (Estryn-Béhar 1991).
The prevalence of infectious diseases is directly related to the efficacy of preventive measures such as vaccines and post-exposure prophylaxis. For example, during the 1980s in France, the proportion of all viral hepatitides fell to 12.7% of its original level thanks to the introduction of vaccination against hepatitis B (Estryn-Béhar 1991). This was noted even before hepatitis A vaccine became available.
Similarly, it may be presumed that, with the declining immunization rates in many countries (e.g., in the Russian Federation and Ukraine in the former Soviet Union during 1994-1995), cases of diphtheria and poliomyelitis among HCWs will increase.
Finally, occasional infections with streptococci, staphylococci and Salmonella typhi are being reported among health care workers.
Epidemiological Studies
The following infectious diseases—listed in order of frequency—are the most important in worldwide occurrences of occupational infectious diseases in health care workers:
- hepatitis B
- tuberculosis
- hepatitis C
- hepatitis A
- hepatitis, non A-E.
Also important are the following (not in order of frequency):
- varicella
- measles
- mumps
- rubella
- Ringelröteln (parvovirus B 19 virus infections)
- HIV/AIDS
- hepatitis D
- EBV hepatitis
- CMV hepatitis.
It is very doubtful that the very many cases of enteric infection (e.g., salmonella, shigella, etc.) often included in the statistics are, in fact, job-related, since these infections are transmitted faecally/orally as a rule.
Much data is available concerning the epidemiological significance of these job-related infections mostly in relation to hepatitis B and its prevention but also in relation to tuberculosis, hepatitis A and hepatitis C. Epidemiological studies have also dealt with measles, mumps, rubella, varicella and Ringenröteln. In using them, however, care must be taken to distinguish between incidence studies (e.g., determination of annual hepatitis B infection rates), sero-epidemiological prevalence studies and other types of prevalence studies (e.g., tuberculin tests).
Hepatitis B
The risk of hepatitis B infections, which are primarily transmitted through contact with blood during needlestick injuries, among HCWs, depends on the frequency of this disease in the population they serve. In northern, central and western Europe, Australia and North America it is found in about 2% of the population. It is encountered in about 7% of the population in southern and south-eastern Europe and most parts of Asia. In Africa, the northern parts of South America and in eastern and south-eastern Asia, rates as high as 20% have been observed (Hollinger 1990).
A Belgian study found that 500 HCWs in northern Europe became infected with hepatitis B each year while the figure for southern Europe was 5,000 (Van Damme and Tormanns 1993). The authors calculated that the annual case rate for western Europe is about 18,200 health care workers. Of these, about 2,275 ultimately develop chronic hepatitis, of whom some 220 will develop cirrhosis of the liver and 44 will develop hepatic carcinoma.
A large study involving 4,218 HCWs in Germany, where about 1% of the population is positive for hepatitis B surface antigen (HBsAg), found that the risk of contracting hepatitis B is approximately 2.5 greater among HCWs than in the general population (Hofmann and Berthold 1989). The largest study to date, involving 85,985 HCWs worldwide, demonstrated that those in dialysis, anaesthesiology and dermatology departments were at greatest risk of hepatitis B (Maruna 1990).
A commonly overlooked source of concern is the HCW who has a chronic hepatitis B infection. More than 100 instances have been recorded worldwide in which the source of the infection was not the patient but the doctor. The most spectacular instance was the Swiss doctor who infected 41 patients (Grob et al. 1987).
While the most important mechanism for transmitting the hepatitis B virus is an injury by a blood-contaminated needle (Hofmann and Berthold 1989), the virus has been detected in a number of other body fluids (e.g., male semen, vaginal secretions, cerebrospinal fluid and pleural exudate) (CDC 1989).
Tuberculosis
In most countries around the world, tuberculosis continues to rank first or second in importance of work-related infections among HCWs (see the article “Tuberculosis prevention, control and surveillance”). Many studies have demonstrated that although the risk is present throughout the professional life, it is greatest during the period of training. For example, a Canadian study in the 1970s demonstrated the tuberculosis rate among female nurses to be double that of women in other professions (Burhill et al. 1985). And, in Germany, where the tuberculosis incidence ranges around 18 per 100,000 for the general population, it is about 26 per 100,000 among health care workers (BGW 1993).
A more accurate estimate of the risk of tuberculosis may be obtained from epidemiological studies based on the tuberculin test. A positive reaction is an indicator of infection by Mycobacterium tuberculosis or other mycobacteria or a prior inoculation with the BCG vaccine. If that inoculation was received 20 or more years earlier, it is presumed that the positive test indicates at least one contact with tubercle bacilli.
Today, tuberculin testing is done by means of the patch test in which the response is read within five to seven days after the application of the “stamp”. A large-scale German study based on such skin tests showed a rate of positives among health professionals that was only moderately higher than that among the general population (Hofmann et al. 1993), but long-range studies demonstrate that a greatly heightened risk of tuberculosis does exist in some areas of health care services.
More recently, anxiety has been generated by the increasing number of cases infected with drug-resistant organisms. This is a matter of particular concern in designing a prophylactic regimen for apparently healthy health care workers whose tuberculin tests “converted” to positive after exposure to patients with tuberculosis.
Hepatitis A
Since the hepatitis A virus is transmitted almost exclusively through faeces, the number of HCWs at risk is substantially smaller than for hepatitis B. An early study conducted in West Berlin showed that paediatric personnel were at greatest risk of this infection (Lange and Masihi 1986). These results were subsequently confirmed by a similar study in Belgium (Van Damme et al. 1989). Similarly, studies in Southwest Germany showed increase risk to nurses, paediatric nurses and cleaning women (Hofmann et al. 1992; Hofmann, Berthold and Wehrle 1992). A study undertaken in Cologne, Germany, revealed no risk to geriatric nurses in contrast to higher prevalence rates among the personnel of child care centres. Another study showed increased risk of hepatitis A among paediatric nurses in Ireland, Germany and France; in the last of these, greater risk was found in workers in psychiatric units treating children and youngsters. Finally, a study of infection rates among handicapped people disclosed higher levels of risk for the patients as well as the workers caring for them (Clemens et al. 1992).
Hepatitis C
Hepatitis C, discovered in 1989, like hepatitis B, is primarily transmitted through blood introduced via needle puncture wounds. Until recently, however, data relating to its threat to HCWs have been limited. A 1991 New York study of 456 dentists and 723 controls showed an infection rate of 1.75% among the dentists compared with 0.14% among the controls (Klein et al. 1991). A German research group demonstrated the prevalence of hepatitis C in prisons and attributed it to the large number of intravenous drug users among the inmates (Gaube et al. 1993). An Austrian study found 2.0% of 294 health care personnel to be seropositive for hepatitis C antibodies, a figure thought to be much higher than that among the general population (Hofmann and Kunz 1990). This was confirmed by another study of HCWs conducted in Cologne, Germany (Chriske and Rossa 1991).
A study in Freiburg, Germany, found that contact with handicapped residents of nursing homes, particularly those with infantile cerebral paresis and trisomia-21, patients with haemophilia and those dependent on drugs administered intravenously presented a particular risk of hepatitis C to workers involved in their care. A significantly increased prevalence rate was found in dialysis personnel and the relative risk to all health care workers was estimated to be 2.5% (admittedly calculated from a relatively small sample).
A possible alternative path of infection was demonstrated in 1993 when a case of hepatitis C was shown to have developed after a splash into the eye (Sartori et al. 1993).
Varicella
Studies of the prevalence of varicella, an illness particularly grave in adults, have consisted of tests for varicella antibodies (anti VZV) conducted in Anglo-Saxon countries. Thus, a seronegative rate of 2.9% was found among 241 hospital employees aged 24 to 62, but the rate was 7.5% for those under the age of 35 (McKinney, Horowitz and Baxtiola 1989). Another study in a paediatric clinic yielded a negative rate of 5% among 2,730 individuals tested in the clinic, but these data become less impressive when it is noted that the serological tests were performed only on persons without a history of having had varicella. A significantly increased risk of varicella infection for paediatric hospital personnel, however, was demonstrated by a study conducted in Freiburg, which found that, in a group of 533 individuals working in hospital care, paediatric hospital care and administration, evidence of varicella immunity was present in 85% of persons younger than 20 years.
Mumps
In considering risk levels of mumps infection, a distinction must be made between countries in which mumps immunization is mandatory and those in which these inoculations are voluntary. In the former, nearly all children and young people will have been immunized and, therefore, mumps poses little risk to health care workers. In the latter, which includes Germany, cases of mumps are becoming more frequent. As a result of lack of immunity, the complications of mumps have been increasing, particularly among adults. A report of an epidemic in a non-immune Inuit population on St. Laurance Island (located between Siberia and Alaska) demonstrated the frequency of such complications of mumps as orchitis in men, mastitis in women and pancreatitis in both sexes (Philip, Reinhard and Lackman 1959).
Unfortunately, epidemiological data on mumps among HCWs are very sparse. A 1986 study in Germany showed that the rate of mumps immunity among 15 to 10 year-olds was 84% but, with voluntary rather than mandatory inoculation, one may presume that this rate has been declining. A 1994 study involving 774 individuals in Freiburg indicated a significantly increased risk to employees in paediatric hospitals (Hofmann, Sydow and Michaelis 1994).
Measles
The situation with measles is similar to that with mumps. Reflecting its high degree of contagiousness, risks of infection among adults emerge as their immunization rates fall. A US study reported an immunity rate of over 99% (Chou, Weil and Arnmow 1986) and two years later 98% of a cohort of 163 nursing students were found to have immunity (Wigand and Grenner 1988). A study in Freiburg yielded rates of 96 to 98% among nurses and paediatric nurses while the rates of immunity among non-medical personnel were only 87 to 90% (Sydow and Hofman 1994). Such data would support a recommendation that immunization be made mandatory for the general population.
Rubella
Rubella falls between measles and mumps with respect to its contagiousness. Studies have shown that about 10% of HCWs are not immune (Ehrengut and Klett 1981; Sydow and Hofmann 1994) and, therefore, at high risk of infection when exposed. Although generally not a serious illness among adults, rubella may be responsible for devastating effects on the foetus during the first 18 weeks of pregnancy: abortion, stillbirth or congenital defects (see table 1) (South, Sever and Teratogen 1985; Miller, Vurdien and Farrington 1993). Since these may be produced even before the woman knows that she is pregnant and, since health care workers, particularly those in contact with paediatric patients, are likely to be exposed, it is especially important that inoculation be urged (and perhaps even required) for all female health care workers of child-bearing age who are not immune.
Table 1. Congenital abnormalities following rubella infection in pregnancy
|
Studies by South, Sever and Teratogen (1985) |
|||||
|
Week of pregnancy |
<4 |
5–8 |
9–12 |
13–16 |
>17 |
|
Deformity rate (%) |
70 |
40 |
25 |
40 |
8 |
|
Studies by Miller, Vurdien and Farrington (1993) |
|||||
|
Week of pregnancy |
<10 |
11–12 |
13–14 |
15–16 |
>17 |
|
Deformity rate (%) |
90 |
33 |
11 |
24 |
0 |
HIV/AIDS
During the 1980s and 1990s, HIV seroconversions (i.e., a positive reaction in an individual previously found to have been negative) became a minor occupational risk among HCWs, although clearly not one to be ignored. By early 1994, reports of some 24 reliably documented cases and 35 possible cases were collected in Europe (Pérez et al. 1994) with an additional 43 documented cases and 43 possible cases were reported in the US (CDC 1994a). Unfortunately, except for avoiding needlesticks and other contacts with infected blood or body fluids, there are no effective preventive measures. Some prophylactic regimens for individuals who have been exposed are recommended and described in the article “Prevention of occupational transmission of bloodborne pathogens”.
Other infectious diseases
The other infectious diseases listed earlier in this article have not yet emerged as significant hazards to HCWs either because they have not been recognized and reported or because their epidemiology has not yet been studied. Sporadic reports of single and small clusters of cases suggest that the identification and testing of serological markers should be explored. For example, a 33-month study of typhus conducted by the Centers for Disease Control (CDC) revealed that 11.2% of all sporadic cases not associated with outbreaks occurred in laboratory workers who had examined stool specimens (Blazer et al. 1980).
The future is clouded by two simultaneous problems: the emergence of new pathogens (e.g., new strains such as hepatitis G and new organisms such as the Ebola virus and the equine morbillivirus recently discovered to be fatal to both horses and humans in Australia) and the continuing development of drug resistance by well-recognized organisms such as the tuberculus bacillus. HCWs are likely to be the first to be systematically exposed. This makes their prompt and accurate identification and the epidemiological study of their patterns of susceptibility and transmission of the utmost importance.
Prevention of Infectious Diseases among Health Care Workers
The first essential in the prevention of infectious disease is the indoctrination of all HCWs, support staff as well as health professionals, in the fact that health care facilities are “hotbeds” of infection with every patient representing a potential risk. This is important not only for those directly involved in diagnostic or therapeutic procedures, but also those who collect and handle blood, faeces and other biological materials and those who come in contact with dressings, linens, dishes and other fomites. In some instances, even breathing the same air may be a possible hazard. Each health care facility, therefore, must develop a detailed procedure manual identifying these potential risks and the steps needed to eliminate, avoid or control them. Then, all personnel must be drilled in following these procedures and monitored to ensure that they are being properly performed. Finally, all failures of these protective measures must be recorded and reported so that revision and/or retraining may be undertaken.
Important secondary measures are the labelling of areas and materials which may be especially infectious and the provision of gloves, gowns, masks, forceps and other protective equipment. Washing the hands with germicidal soap and running water (wherever possible) will not only protect the health care worker but also will minimize the risk of his or her transmitting the infection to co-workers and other patients.
All blood and body fluid specimens or splashes and materials stained with them must be handled as though they are infected. The use of rigid plastic containers for the disposal of needles and other sharp instruments and diligence in the proper disposal of potentially infectious wastes are important preventive measures.
Careful medical histories, serological testing and patch testing should be performed prior to or as soon as health care workers report for duty. Where advisable (and there are no contraindications), appropriate vaccines should be administered (hepatitis B, hepatitis A and rubella appear to be the most important) (see table 2). In any case, seroconversion may indicate an acquired infection and the advisability of prophylactic treatment.
Table 2. Indications for vaccinations in health service employees.
|
Disease |
Complications |
Who should be vaccinated? |
|
Diptheria |
In the event of an epidemic, all employees without |
|
|
Hepatitis A |
Employees in the paediatric field as well as in infection |
|
|
Hepatitis B |
All seronegative employees with possibility of contact |
|
|
Influenza |
Regularly offered to all employees |
|
|
Measles |
Encephalitis |
Seronegative employees in the paediatric field |
|
Mumps |
Meningitis |
Seronegative employees in the paediatric field |
|
Rubella |
Embryopathy |
Seronegative employees in paediatry/midwifery/ |
|
Poliomyelitis |
All employees, e.g., those involved in vaccination |
|
|
Tetanus |
Employees in gardening and technical fields obligatory, |
|
|
Tuberculosis |
In all events employees in pulmonology and lung surgery |
|
|
Varicellas |
Foetal risks |
Seronegative employees in paediatry or at least in the |
Prophylactic therapy
In some exposures when it is known that the worker is not immune and has been exposed to a proven or highly suspected risk of infection, prophylactic therapy may be instituted. Especially if the worker presents any evidence of possible immunodeficiency, human immunoglobulin may be administered. Where specific “hyperimmune” serum is available, as in mumps and hepatitis B, it is preferable. In infections which, like hepatitis B, may be slow to develop, or “booster” doses are advisable, as in tetanus, a vaccine may be administered. When vaccines are not available, as in meningococcus infections and plague, prophylactic antibiotics may be used either alone or as a supplement to immune globulin. Prophylactic regimens of other drugs have been developed for tuberculosis and, more recently, for potential HIV infections, as discussed elsewhere in this chapter.
Rail Operations
Railroads provide a major mode of transportation around the world. Today, even with competition from road and airborne transport, rail remains an important means of land-based movement of bulk quantities of goods and materials. Railroad operations are carried out in an enormously wide variety of terrains and climates, from Arctic permafrost to equatorial jungle, from rainforest to desert. The roadbed of partly crushed stone (ballast) and track consisting of steel rails and ties of wood, concrete or steel are common to all railroads. Ties and ballast maintain the position of the rails.
The source of power used in railroad operations worldwide (steam, diesel-electric and current electricity) spans the history of development of this mode of transportation.
Administration and Train Operations
Administration and train operations create the public profile of the railroad industry. They ensure that goods move from origin to destination. Administration includes office personnel involved in business and technical functions and management. Train operations include dispatchers, rail traffic control, signal maintainers, train crews and yard workers.
Dispatchers ensure that a crew is available at the appropriate point and time. Railroads operate 24 hours per day, 7 days per week throughout the year. Rail traffic control personnel coordinate train movements. Rail traffic control is responsible for assigning track to trains in the appropriate sequence and time. This function is complicated by single sets of track that must be shared by trains moving in both directions. Since only one train can occupy a particular section of track at any time, rail traffic control must assign occupancy of the main line and sidings, in a manner that assures safety and minimizes delay.
Signals provide visual cues to train operators, as well as to drivers of road vehicles at level train crossings. For train operators, signals must provide unambiguous messages about the status of the track ahead. Signals today are used as an adjunct to rail traffic control, the latter being conducted by radio on channels received by all operating units. Signal maintainers must ensure operation of these units at all times, which can sometimes involve working alone in remote areas in all weather at any time, day or night.
Yard workers’ duties include ensuring that the rolling stock is prepared to receive cargo, which is an increasingly important function in this era of quality management. Tri-level automobile transporter cars, for example, must be cleaned prior to use and readied to accept vehicles by moving chocks to appropriate positions. The distance between levels in these cars is too short for the average male to stand upright, so that work is done in a hunched over position. Similarly, the handholds on some cars force yard workers to assume an awkward posture during shunting operations.
For long runs, a train crew operates the train between designated transfer points. A replacement crew takes over at the transfer point and continues the journey. The first crew must wait at the transfer point for another train to make the return trip. The combined trips and the wait for the return train can consume many hours.
A train trip on single track can be very fragmented, in part because of problems in scheduling, track work and the breakdown of equipment. Occasionally a crew returns home in the cab of a trailing locomotive, in the caboose (where still in use) or even by taxi or bus.
The train crew’s duties may include dropping off some cars or picking up additional ones en route. This could occur at any hour of the day or night under any imaginable weather conditions. The assembly and disassembly of trains are the sole duties of some train crews in yards.
On occasion there is a failure of one of the knuckles that couple cars together or a break in a hose that carries braking system air between cars. This necessitates investigative work by one of the train crew and repair or replacement of the defective part. The spare knuckle (about 30 kg) must be carried along the roadbed to the repair point, and the original removed and replaced. Work between cars must reflect careful planning and preparation to ensure that the train does not move during the procedure.
In mountainous areas, breakdown may occur in a tunnel. The locomotive must maintain power above idle under these conditions in order to keep the braking functional and to prevent train runaway. Running the engine in a tunnel could cause the tunnel to fill with exhaust gases (nitrogen dioxide, nitric oxide, carbon monoxide and sulphur dioxide).
Table 1 summarizes potential hazardous conditions associated with administration and train operations.
Table 1. Hazardous conditions associated with administration and train operations.
|
Conditions |
Affected groups |
Comments |
|
Exhaust emissions |
Train crew, supervisors, technical advisors |
Emissions primarily include nitrogen dioxide, nitric oxide, carbon monoxide, sulphur dioxide and particulates containing polycyclic aromatic hydrocarbons (PAHs). Potential for exposure is most likely in unventilated tunnels. |
|
Noise |
Train crew, supervisors, technical advisors |
In-cab noise could exceed regulated limits. |
|
Whole-body vibration |
Train crew |
Structure-borne vibration transmitted through the floor and seats in the cab originates from the engine and motion along the track and over gaps between rails. |
|
Electromagnetic fields |
Train crew, signal maintainers |
AC and DC fields are possible, depending on design of power unit and traction motors. |
|
Radio-frequency fields |
Users of two-way radios |
Effects on humans are not fully established. |
|
Weather |
Train crew, yard workers, signal maintainers |
Ultraviolet energy can cause sunburn, skin cancer and cataracts. Cold can cause cold stress and frostbite. Heat can cause heat stress. |
|
Shiftwork |
Dispatchers, rail traffic control, train crews, signal maintainers |
Train crews can work irregular hours; remuneration is often based on travelling a fixed distance within a time period. |
|
Musculoskeletal injury |
Train crew, yard workers |
Ankle injury can occur during disembarkment from moving equipment. Shoulder injury can occur during embarkment onto moving equipment. Injury can occur at various sites while carrying knuckles on rough terrain. Work is performed in awkward postures. |
|
Video displays units |
Management, administrative and technical staff, dispatchers, rail traffic control |
Effective use of computerized workstations depends on application of visual and office ergonomic principles. |
|
Rundown accidents |
All workers |
Rundown can occur when the individual stands on an active track and fails to hear approach of trains, track equipment and moving cars. |
Maintenance of Rolling Stock and Track Equipment
Rolling stock includes locomotives and railcars. Track equipment is specialized equipment used for track patrol and maintenance, construction and rehabilitation. Depending on the size of the railroad, maintenance can range from onsite (small-scale repairs) to complete stripdown and rebuilding. Rolling stock must not fail in operation, since failure carries serious adverse safety, environmental and business consequences. If a car carries a hazardous commodity, the consequences that can arise from failure to find and repair a mechanical defect can be enormous.
Larger rail operations have running shops and centralized stripdown and rebuild facilities. Rolling stock is inspected and prepared for the trip at running shops. Minor repair is performed on both cars and locomotives.
Railcars are rigid structures that have pivot points near each end. The pivot point accepts a vertical pin located in the truck (the wheels and their support structure). The body of the car is lifted from the truck for repairs. Minor repair can involve the body of the car or attachments or brakes or other parts of the truck. Wheels may require machining on a lathe to remove flat spots.
Major repair could include removal and replacement of damaged or corroded metal sheeting or frame and abrasive blasting and repainting. It could also include removal and replacement of wooden flooring. Trucks, including wheel-axle sets and bearings, may require disassembly and rebuilding. Rehabilitation of truck castings involves build-up welding and grinding. Rebuilt wheel-axle sets require machining to true the assembly.
Locomotives are cleaned and inspected prior to each trip. The locomotive may also require mechanical service. Minor repairs include oil changes, work on brakes and servicing of the diesel engine. Removal of a truck for wheel truing or evening may also be needed. Operation of the engine may be required in order to position the locomotive inside the service building or to remove it from the building. Prior to re-entry into service the locomotive could require a load test, during which the engine is operated at full throttle. Mechanics work in close proximity to the engine during this procedure.
Major servicing could involve complete stripdown of the locomotive. The diesel engine and engine compartment, compressor, generator and traction motors require thorough degreasing and cleaning owing to heavy service and contact of fuel and lubricants with hot surfaces. Individual components may then be stripped and rebuilt.
Traction motor casings may require build-up welding. Armatures and rotors may need machining in order to remove old insulation, then be repaired and impregnated with a solution of varnish.
Track maintenance equipment includes trucks and other equipment that can operate on road and rail, as well as specialized equipment that operates only on rail. The work may include highly specialized units, such as track inspection units or rail-grinding machines, which may be “one of a kind”, even in large railroad companies. Track maintenance equipment may be serviced in garage settings or in field locations. The engines in this equipment may produce considerable exhaust emissions due to long periods between service and lack of familiarity of mechanics. This can have major pollution consequences during operation in confined spaces, such as tunnels and sheds and enclosing formations.
Table 2 summarizes potential hazardous conditions associated with maintenance of rolling stock and track equipment as well as transportation accidents.
Table 2. Hazardous conditions associated with maintenance and transportation accidents.
|
Conditions |
Affected groups |
Comments |
|
Skin contamination with waste oils and lubricants |
Diesel mechanics, traction motor mechanics |
Decomposition of hydrocarbons in contact with hot surfaces can produce polycyclic aromatic hydrocarbons (PAHs). |
|
Exhaust emissions |
All workers in diesel shop, wash facility, refuelling area, load test area |
Emissions primarily include nitrogen dioxide, nitric oxide, carbon monoxide, sulphur dioxide and particulates containing (PAHs). Potential for exposure most likely where exhaust emissions are confined by structures. |
|
Welding emissions |
Welders, tackers, fitters, operators of overhead cranes |
Work primarily involves carbon steel; aluminium and stainless steel are possible. Emissions include shield gases and fluxes, metal fumes, ozone, nitrogen dioxide, visible and ultraviolet energy. |
|
Brazing emissions |
Electricians working on traction motors |
Emission include cadmium end lead in solder. |
|
Thermal decomposition products from coatings |
Welders, tackers, fitters, grinders, operators of overhead cranes |
Emissions can include carbon monoxide, inorganic pigments containing lead and other chromates, decomposition products from paint resins. PCBs may have been used prior to 1971. PCBs can form furans and dioxins when heated. |
|
Cargo residues |
Welders, fitters, tackers, grinders, mechanics, strippers |
Residues reflect service in which car was used; cargoes could include heavy metal concentrates, coal, sulphur, lead ingots, etc. |
|
Abrasive blasting dust |
Abrasive blaster, bystanders |
Dust can contain cargo residues, blast material, paint dust. Paint applied prior to 1971 may contain PCBs. |
|
Solvent vapours |
Painter, bystanders |
Solvent vapours can be present in paint storage and mixing areas and paint booth; flammable mixtures may develop inside confined spaces, such as hoppers and tanks, during spraying. |
|
Paint aerosols |
Painter, bystanders |
Paint aerosols contain sprayed paint plus diluent; solvent in droplets and vapour can form flammable mixtures; resin system can include isocyanates, epoxys, amines, peroxides and other reactive intermediates. |
|
Confined spaces |
All shop workers |
Interior of some railcars, tanks and hoppers, nose of locomotive, ovens, degreasers, varnish impregnator, pits, sumps and other enclosed and partially enclosed structures |
|
Noise |
All shop workers |
Noise generated by many sources and tasks can exceed regulated limits. |
|
Hand-arm vibration |
Users of powered hand tools and hand-held equipment |
Vibration is transmitted through hand grips. |
|
Electromagnetic fields |
Users of electrical welding equipment |
AC and DC fields are possible, depending on design of the unit. |
|
Weather |
Outside workers |
Ultraviolet energy can cause sunburn, skin cancer and cataracts. Cold can cause cold stress and frostbite. Heat can cause heat stress. |
|
Shiftwork |
All workers |
Crews can work irregular hours. |
|
Musculoskeletal injury |
All workers |
Ankle injury can occur during disembarkment from moving equipment. Shoulder injury can occur during embarkment onto moving equipment or climbing onto cars. Work is performed in awkward posture especially when welding, burning, cutting and operating powered hand tools. |
|
Rundown accidents |
All workers |
Rundown can occur when the individual stands on active track and fails to hear approach of track equipment and moving cars. |
Maintenance of Track and Right of Way
Maintenance of track and right of way primarily involves work in the outdoor environment in conditions associated with the outdoors: sun, rain, snow, wind, cold air, hot air, blowing sand, biting and stinging insects, aggressive animals, snakes and poisonous plants.
Track and right-of-way maintenance can include track patrol, as well as the maintenance, rehabilitation and replacement of buildings and structures, track and bridges, or service functions, such as snowplowing and herbicide application, and may involve local operating units or large, specialized work gangs that deal with replacement of rails, ballast or ties. Equipment is available to almost completely mechanize each of these activities. Small-scale work, however, could involve small, powered equipment units or even be a completely manual activity.
In order to carry out maintenance of operating lines, a block of time must be available during which the work can occur. The block could become available at any time of day or night, depending on train scheduling, especially on a single-track main line. Thus, time pressure is a main consideration during this work, since the line must be returned to service at the end of the assigned block of time. Equipment must proceed to the site, the work must be completed, and the track vacated within the set period.
Ballast replacement and tie and rail replacement are complex tasks. Ballast replacement first involves removal of contaminated or deteriorated material in order to expose the track. A sled, a plow-like unit that is pulled by a locomotive, or an undercutter performs this task. The undercutter uses a continuous toothed chain to pull ballast to the side. Other equipment is used to remove and replace rail spikes or tie clips, tie plates (the metal plate on which the rail sits on the tie) and ties. Continuous rail is akin to a noodle of wet spaghetti that can flex and whip and that is easily moved vertically and laterally. Ballast is used to stabilize the rail. The ballast train delivers new ballast and pushes it into position. Labourers walk along with the train and systematically open chutes located at the bottom of the cars in order to enable ballast to flow.
After the ballast is dropped, a tamper uses hydraulic fingers to pack the ballast around and under the ties and lifts the track. A spud liner drives a metal spike into the roadbed as an anchor and moves the track into the desired position. The ballast regulator grades the ballast to establish the final contours of the roadbed and sweeps clean the surface of the ties and rails. Considerable dust is generated during ballast dumping, regulating and sweeping.
There are a variety of settings in which track work can take place—open areas, semi-enclosed areas such as cuts, and hill and cliff faces and confined spaces, such as tunnels and sheds. These have a profound influence on working conditions. Enclosed spaces, for example, will confine and concentrate exhaust emissions, ballast dust, dust from grinding, fumes from thermite welding, noise and other hazardous agents and conditions. (Thermite welding uses powdered aluminium and iron oxide. Upon ignition the aluminium burns intensely and converts the iron oxide to molten iron. The molten iron flows into the gap between the rails, welding them together end to end.)
Switching structures are associated with track. The switch contains moveable, tapered rails (points) and a wheel guide (frog). Both are manufactured from specially hardened steel containing a high level of manganese and chromium. The frog is an assembled structure containing several pieces of specially bent rail. The self-locking nuts which are used to bolt together these and other track structures may be cadmium-plated. Frogs are built up by welding and are ground during refurbishing, which can occur onsite or in shop facilities.
Bridge repainting is also an important part of right-of-way maintenance. Bridges often are situated in remote locations; this can considerably complicate provision of personal hygiene facilities which are needed to prevent contamination of individuals and the environment.
Table 3 summarizes the hazards of track and right-of-way maintenance.
Transportation Accidents
Possibly the greatest single concern in rail operations is the transportation accident. The large quantities of material that could be involved could cause serious problems of exposure of personnel and the environment. No amount of preparation for a worst-case accident is ever enough. Therefore, minimizing risk and the consequences of an accident are imperative. Transportation accidents occur for a variety of reasons: collisions at level crossings, obstruction of the track, failure of equipment and operator error.
The potential for such accidents can be minimized through conscientious and ongoing inspection and maintenance of track and right-of-way and equipment. The impact of a transportation accident involving a train carrying mixed cargo can be minimized through strategic positioning of cars that carry incompatible freight. Such strategic positioning, however, is not possible for a train hauling a single commodity. Commodities of particular concern include: pulverized coal, sulphur, liquefied petroleum (fuel) gases, heavy metal concentrates, solvents and process chemicals.
All of the groups in a rail organization are involved in transportation accidents. Rehabilitation activities can literally involve all groups working simultaneously at the same location on the site. Thus, coordination of these activities is extremely important, so that the actions of one group do not interfere with those of another.
Hazardous commodities generally remain contained during such accidents because of the attention given to crashproofing in the design of shipping containers and bulk rail cars. During an accident, the contents are removed from the damaged car by emergency response crews that represent the shipper. Equipment maintainers repair the damage to the extent possible and put the car back on the track, if possible. However, the track under the derailed car may have been destroyed. If so, repair or replacement of track occurs next, using prefabricated sections and techniques similar to those described above.
In some situations, loss of containment occurs and the contents of the car or shipping container spill onto the ground. If substances are shipped in quantities sufficient to require placarding because of transportation laws, they are readily identifiable on shipping manifests. However, highly hazardous substances that are shipped in smaller quantities than mandated for listing in a shipping manifest can escape identification and characterization for a considerable period. Containment at the site and collection of the spilled material are the responsibility of the shipper.
Railway personnel can be exposed to materials that remain in snow, soil or vegetation during rehabilitation efforts. The severity of exposure depends on the properties and quantity of the substance, the geometry of the site and weather conditions. The situation could also pose fire, explosion, reactivity and toxic hazards to humans, animals and the surrounding environment.
At some point following the accident, the site must be cleared so that the track can be put back into service. Transfer of cargo and repair of equipment and track may still be required. These activities could be dramatically complicated by the loss of containment and the presence of spilled material. Any action taken to address this type of situation requires considerable prior planning that includes input from specialized knowledgeable professionals.
Hazards and Precautions
Table 1, table 2 and table 3 summarize the hazardous conditions associated with the various groups of workers involved in railroad operations. Table 4 summarizes the types of precautions used to control these hazardous conditions.
Table 3. Hazardous conditions associated with maintenance on track and right of way.
|
Condition |
Affected group(s) |
Comments |
|
Exhaust emissions |
All workers |
Emissions include nitrogen dioxide, nitric oxide, carbon monoxide, sulphur dioxide and particulates containing polycyclic aromatic hydrocarbons (PAHs). Potential for exposure is most likely in unventilated tunnels and other circumstances where exhaust is confined by structures. |
|
Ballast dust/spilled cargo |
Track equipment operators, labourers |
Depending on the source, ballast dust can contain silica (quartz), heavy metals or asbestos. Track work around operations that produce and handle bulk commodities can cause exposure to these products: coal, sulphur, heavy metal concentrates, etc. |
|
Welding, cutting and grinding emissions |
Field and shop welders |
Welding primarily involves hardened steel; emissions can include shield gases and fluxes, metal fumes, ozone, nitrogen dioxide, carbon monoxide, ultraviolet and visible energy. Exposure to manganese and chromium can occur during work involving rail; cadmium may occur in plated nuts and bolts. |
|
Abrasive blasting dust |
Abrasive blaster, bystanders |
Dust contains blast material and paint dust; paint likely contains lead and other chromates. |
|
Solvent vapours |
Painter, bystanders |
Solvent vapours can be present in paint storage and mixing areas; flammable mixtures could develop inside enclosed spray structure during spraying. |
|
Paint aerosols |
Painter, bystanders |
Paint aerosols contain sprayed paint plus diluent; solvent in droplets and vapour can form flammable mixture; resin system can include isocyanates, epoxys, amines, peroxides and other reactive intermediates. |
|
Confined spaces |
All workers |
Interior of tunnels, culverts, tanks, hoppers, pits, sumps and other enclosed and partially enclosed structures |
|
Noise |
All workers |
Noise generated by many sources and tasks can exceed regulated limits. |
|
Whole-body vibration |
Truck drivers, track equipment operators |
Structure-borne vibration transmitted through the floor and seat in the cab originates from the engine and motion along roads and track and over gaps between rails. |
|
Hand-arm vibration |
Users of powered hand tools and hand-held equipment |
Vibration transmitted through hand grips |
|
Electromagnetic fields |
Users of electrical welding equipment |
AC and DC fields are possible, depending on design of the unit. |
|
Radio-frequency fields |
Users of two-way radios |
Effects on humans not fully established |
|
Weather-related |
Outside workers |
Ultraviolet energy can cause sunburn, skin cancer and cataracts; cold can cause cold stress and frostbite; heat can cause heat stress. |
|
Shiftwork |
All workers |
Gangs work irregular hours due to problems in scheduling blocks of track time. |
|
Musculoskeletal injury |
All workers |
Ankle injury during disembark from moving equipment; shoulder injury during embark onto moving equipment; work in awkward posture, especially when welding and operating powered hand tools |
|
Rundown accident |
All workers |
Rundown can occur when the individual stands on active track and fails to hear approach of track equipment, trains and moving cars. |
Table 4. Railway industry approached to controlling hazardous conditions.
|
Hazardous conditions |
Comments/control measures |
|
Exhaust emissions |
Locomotives have no exhaust stack. Exhaust discharges vertically from the top surface. Cooling fans also located on the top of the locomotive can direct exhaust-contaminated air into the airspace of tunnels and buildings. In-cab exposure during normal transit through a tunnel does not exceed exposure limits. Exposure during stationary operations in tunnels, such as investigation of mechanical problems, rerailing of derailed cars or track repair, can considerably exceed exposure limits. Stationary operation in shops also can create significant overexposure.Track maintenance and construction equipment and heavy vehicles usually have vertical exhaust stacks. Low-level discharge or discharge through horizontal deflectors can cause overexposure. Small vehicles and portable gasoline-powered equipment discharge exhaust downward or have no stack. Proximity to these sources can cause overexposure. Control measures include:
|
|
Noise |
Control measures include:
|
|
Whole-body vibration |
Control measures include:
|
|
Electromagnetic fields |
Hazard not established below present limits. |
|
Radio-frequency fields |
Hazard not established below present limits. |
|
Weather |
Control measures include:
|
|
Shiftwork |
Arrange work schedules to reflect current knowledge about circadian rhythms. |
|
Musculoskeletal injury |
Control measures include:
|
|
Video display units |
Apply office ergonomic principles to selection and utilization of video display units. |
|
Rundown accidents |
Rail equipment is confined to the track. Unpowered rail equipment creates little noise when in motion. Natural features can block noise from powered rail equipment. Equipment noise can mask warning sound from the horn of an approaching train. During operations in rail yards, switching can occur under remote control with the result that all tracks could be live. Control measures include:
|
|
Ballast operations/ spilled cargo |
Wetting ballast prior to track work eliminates dust from ballast and cargo residues. Personal and respiratory protective equipment should be provided. |
|
Skin contamination by waste oils and lubricants |
Equipment should be cleaned prior to dismantling to remove contamination. Protective clothing, gloves and/or barrier creams should be used. |
|
Welding, cutting and brazing emissions, grinding dust |
Control measures include:
|
|
Thermal decomposition products from coatings |
Control measures include:
|
|
Cargo residues |
Control measures include:
|
|
Abrasive blasting dust |
Control measures include:
|
|
Solvent vapours, paint aerosols |
Control measures include:
|
|
Confined spaces |
Control measures include:
|
|
Hand-arm vibration |
Control measures include:
|
Zoos and Aquariums
Zoological gardens, wildlife parks, safari parks, bird parks and collections of aquatic wildlife share similar methods for the maintenance and handling of exotic species. Animals are held for exhibition, as an educational resource, for conservation and for scientific study. Traditional methods of caging animals and preparing aviaries for birds and tanks for water creatures remain common, but more modern, progressive collections have adopted different enclosures designed to meet more of the needs of particular species. The quality of space accorded to an animal is more important than the quantity, however, which has consequential beneficial effects on keeper safety. The danger to keepers is often related to the size and natural ferocity of the species attended, but many other factors can affect the danger.
The main animal groupings are mammals, birds, reptiles, amphibians, fish and invertebrates. Problem areas that are common to all the animal groups are toxins, diseases that are contractible from animals (zoonoses) and changing animal moods.
Mammals
Mammals’ varied forms and habits require a wide range of husbandry techniques. The largest land forms are herbivorous, such as elephants, and are limited in their ability to climb, jump, burrow or gnaw, so their control is similar to domestic forms. Remote control of gates can offer high degrees of safety. Large predators such as big cats and bears require enclosures with wide margins of safety, double entry doors and in-built catch-ups and crushes. Agile climbing and jumping species pose special problems to keepers, who lack comparable mobility. The use of electric shock fence wiring is now widespread. Capture and handling methods include corralling, nets, crushing, roping, sedation and immobilization with drugs injected by dart.
Birds
Few birds are too large to be restrained by gloved hands and nets. The largest flightless birds—ostriches and cassowaries—are strong and have a very dangerous kick; they require crating for restraint.
Reptiles
Large carnivorous reptile species have violent strike attack capability; many snakes do too. Captive specimens may seem docile and induce keeper complacency. An attacking large constricting snake can overwhelm and suffocate a panicking keeper of much greater weight. A few venomous snakes can “spit”; thus eye protection against them should be mandatory. Restraint and handling methods include nets, bags, hooks, grabs, nooses and drugs.
Amphibians
Only a large giant salamander or big toad can give an unpleasant bite; otherwise risks from amphibians are from toxin excretion.
Fish
Few fish specimens are hazardous except for venomous species, electric eels and bigger predatory forms. Careful netting minimizes risk. Electric and chemical stunning may be occasionally appropriate.
Invertebrates
Some lethal invertebrate species are kept which require indirect handling. Mis-identification and specimens hidden by camouflage and small size can endanger the unwary.
Toxins
Many animal species have evolved complex poisons for feeding or defence, and deliver them by biting, stinging, spitting and secretion. Delivered quantities may vary from the inconsequential to lethal doses. Worst case scenarios should be the model for accident anticipation procedures. Single keeper exposure to lethal species should not be practised. Husbandry must include risk evaluation, unambiguous warning signs, restriction of handling to those trained, maintenance of stocks of antidotes (if any) in close liaison with local trained medical practitioners, predetermination of handler reaction to antidotes and an efficient alarm system.
Zoonoses
A good animal health programme and personal hygiene will keep the risk from zoonoses very low. However, there are many which are potentially lethal, such as rabies, which is untreatable in later stages. Almost all are avoidable, and treatable if diagnosed correctly early enough. As with work elsewhere, the incidence of allergy-related illness is rising and it is best treated by non-exposure to the irritant when identified.
“Non-venomous” bites and scratches require careful attention, as even a bite which appears not to break skin can lead to rapid blood poisoning (septicaemia). Carnivore and monkey bites should be especially suspect. An extreme example is the bite of a komodo dragon; the microflora in its saliva are so virulent that bitten large prey that escapes an initial attack will rapidly die from shock and septicaemia.
Routine prophylaxis against tetanus and hepatitis may be appropriate for many staff.
Moods
Animals can give an infinite variety of responses, some very dangerous, to close human presence. Observable mood changes can alert keepers to danger, but few animals show signs readable by humans. Moods can be influenced by a combination of seen and unseen stimuli such as season, day length, time of day, sexual rhythms, upbringing, hierarchy, barometric pressure and high-frequency noise from electrical equipment. Animals are not production line machines; they may have predictable patterns of behaviour but all have the capacity to do the unexpected, against which even the most skilled attendant must guard.
Personal safety
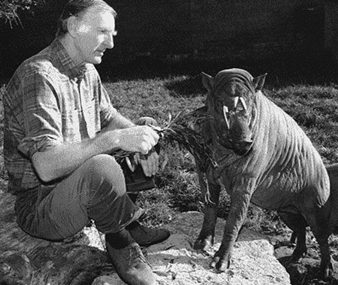
Risk appreciation should be taught by the skilled to the inexperienced. An undiminishing high level of caution will enhance personal safety, particularly, for example, when food is offered to larger carnivores. Animal responses will vary to different keepers, especially to those of different sex. An animal submissive to one person may attack another. The understanding and use of body language can enhance safety; animals naturally understand it better than humans. Voice tone and volume can calm or cause chaos (figure 1).
Figure 1. Handling animals with voice and body language.
Ken Sims
Clothing should be chosen with special care, avoiding bright, flapping material. Gloves may protect and reduce handling stress but are inappropriate for handling snakes because tactile sensitivity is reduced.
If keepers and other staff are expected to manage trespassing, violent or other problem visitors, they should be schooled in people management and have back-up on call to minimize risks to themselves.
Regulations
Despite the variety of potential risks from exotic species, the greater workplace hazards are conventional ones arising from plant and machinery, chemicals, surfaces, electricity and so on, so standard health and safety regulations must be applied with common sense and regard for the unusual nature of the work.
Prevention of Occupational Transmission of Bloodborne Pathogens
Prevention of occupational transmission of bloodborne pathogens (BBP) including the human immunodeficiency virus (HIV), hepatitis B virus (HBV) and more recently hepatitis C virus (HCV), has received significant attention. Although HCWs are the primary occupational group at risk of acquisition of infection, any worker who is exposed to blood or other potentially infectious body fluids during the performance of job duties is at risk. Populations at risk for occupational exposure to BBP include workers in health care delivery, public safety and emergency response workers and others such as laboratory researchers and morticians. The potential for occupational transmission of bloodborne pathogens including HIV will continue to increase as the number of persons who have HIV and other bloodborne infections and require medical care increases.
In the US, the Centers for Disease Control and Prevention (CDC) recommended in 1982 and 1983 that patients with the acquired immunodeficiency syndrome (AIDS) be treated according to the (now obsolete) category of “blood and body fluid precautions” (CDC 1982; CDC 1983). Documentation that HIV, the causative agent of AIDS, had been transmitted to HCWs by percutaneous and mucocutaneous exposures to HIV-infected blood, as well as the realization that the HIV infection status of most patients or blood specimens encountered by HCWs would be unknown at the time of the encounter, led CDC to recommend that blood and body fluid precautions be applied to all patients, a concept known as “universal precautions” (CDC 1987a, 1987b). The use of universal precautions eliminates the need to identify patients with bloodborne infections, but is not intended to replace general infection control practices. Universal precautions include the use of handwashing, protective barriers (e.g., goggles, gloves, gowns and face protection) when blood contact is anticipated and care in the use and disposal of needles and other sharp instruments in all health care settings. Also, instruments and other reusable equipment used in performing invasive procedures should be appropriately disinfected or sterilized (CDC 1988a, 1988b). Subsequent CDC recommendations have addressed prevention of transmission of HIV and HBV to public safety and emergency responders (CDC 1988b), management of occupational exposure to HIV, including the recommendations for the use of zidovudine (CDC 1990), immunization against HBV and management of HBV exposure (CDC 1991a), infection control in dentistry (CDC 1993) and the prevention of HIV transmission from HCWs to patients during invasive procedures (CDC 1991b).
In the US, CDC recommendations do not have the force of law, but have often served as the foundation for government regulations and voluntary actions by industry. The Occupational Health and Safety Administration (OSHA), a federal regulatory agency, promulgated a standard in 1991 on Occupational Exposure to Bloodborne Pathogens (OSHA 1991). OSHA concluded that a combination of engineering and work practice controls, personal protective clothing and equipment, training, medical surveillance, signs and labels and other provisions can help to minimize or eliminate exposure to bloodborne pathogens. The standard also mandated that employers make available hepatitis B vaccination to their employees.
The World Health Organization (WHO) has also published guidelines and recommendations pertaining to AIDS and the workplace (WHO 1990, 1991). In 1990, the European Economic Council (EEC) issued a council directive (90/679/EEC) on protection of workers from risks related to exposure to biological agents at work. The directive requires employers to conduct an assessment of the risks to the health and safety of the worker. A distinction is drawn between activities where there is a deliberate intention to work with or use biological agents (e.g., laboratories) and activities where exposure is incidental (e.g., patient care). Control of risk is based on a hierarchical system of procedures. Special containment measures, according to the classification of the agents, are set out for certain types of health facilities and laboratories (McCloy 1994). In the US, CDC and the National Institutes of Health also have specific recommendations for laboratories (CDC 1993b).
Since the identification of HIV as a BBP, knowledge about HBV transmission has been helpful as a model for understanding modes of transmission of HIV. Both viruses are transmitted via sexual, perinatal and bloodborne routes. HBV is present in the blood of individuals positive for hepatitis B e antigen (HBeAg, a marker for high infectivity) at a concentration of approximately 108 to 109 viral particles per millilitre (ml) of blood (CDC 1988b). HIV is present in blood at much lower concentrations: 103 to 104 viral particles/ml for a person with AIDS and 10 to 100/ml for a person with asymptomatic HIV infection (Ho, Moudgil and Alam 1989). The risk of HBV transmission to a HCW after percutaneous exposure to HBeAg-positive blood is approximately 100-fold higher than the risk of HIV transmission after percutaneous exposure to HIV-infected blood (i.e., 30% versus 0.3%) (CDC 1989).
Hepatitis
Hepatitis, or inflammation of the liver, can be caused by a variety of agents, including toxins, drugs, autoimmune disease and infectious agents. Viruses are the most common cause of hepatitis (Benenson 1990). Three types of bloodborne viral hepatitis have been recognized: hepatitis B, formerly called serum hepatitis, the major risk to HCWs; hepatitis C, the major cause of parenterally transmitted non-A, non-B hepatitis; and hepatitis D, or delta hepatitis.
Hepatitis B. The major infectious bloodborne occupational hazard to HCWs is HBV. Among US HCWs with frequent exposure to blood, the prevalence of serological evidence of HBV infection ranges between approximately 15 and 30%. In contrast, the prevalence in the general populations averages 5%. The cost-effectiveness of serological screening to detect susceptible individuals among HCWs depends on the prevalence of infection, the cost of testing and the vaccine costs. Vaccination of persons who already have antibodies to HBV has not been shown to cause adverse effects. Hepatitis B vaccine provides protection against hepatitis B for at least 12 years after vaccination; booster doses currently are not recommended. The CDC estimated that in 1991 there were approximately 5,100 occupationally acquired HBV infections in HCWs in the United States, causing 1,275 to 2,550 cases of clinical acute hepatitis, 250 hospitalizations and about 100 deaths (unpublished CDC data). In 1991, approximately 500 HCWs became HBV carriers. These individuals are at risk of long-term sequelae, including disabling chronic liver disease, cirrhosis and liver cancer.
The HBV vaccine is recommended for use in HCWs and public safety workers who may be exposed to blood in the workplace (CDC 1991b). Following a percutaneous exposure to blood, the decision to provide prophylaxis must include considerations of several factors: whether the source of the blood is available, the HBsAg status of the source and the hepatitis B vaccination and vaccine-response status of the exposed person. For any exposure of a person not previously vaccinated, hepatitis B vaccination is recommended. When indicated, hepatitis B immune globulin (HBIG) should be administered as soon as possible after exposure since its value beyond 7 days after exposure is unclear. Specific CDC recommendations are indicated in table 1 (CDC 1991b).
Table 1. Recommendation for post-exposure prophylaxis for percutaneous or permucosal exposure to hepatitis B virus, United States
|
Exposed person |
When source is |
||
|
HBsAg1 positive |
HBsAg negative |
Source not tested or |
|
|
Unvaccinated |
HBIG2´1 and initiate |
Initiate HB vaccine |
Initiate HB vaccine |
|
Previously Known |
No treatment |
No treatment |
No treatment |
|
Known non- |
HBIG´2 or HBIG´1 and |
No treatment |
If known high-risk source |
|
Response |
Test exposed for anti-HBs4 |
No treatment |
Test exposed for anti-HBs |
1 HBsAg = Hepatitis B surface antigen. 2 HBIG = Hepatitis B immune globulin; dose 0.06 mL/kg IM. 3 HB vaccine = hepatitis B vaccine. 4 Anti-HBs = antibody to hepatitis B surface antigen. 5 Adequate anti-HBs is ≥10 mIU/mL.
Table 2. Provisional US Public Health Service recommendations for chemoprophylaxis after occupational exposure to HIV, by type of exposure and source of material, 1996
|
Type of exposure |
Source material1 |
Antiretroviral |
Antiretroviral regimen3 |
|
Percutaneous |
Blood |
|
|
|
Mucous membrane |
Blood |
Offer |
ZDV plus 3TC, ± IDV5 |
|
Skin, increased risk7 |
Blood |
Offer |
ZDV plus 3TC, ± IDV5 |
1 Any exposure to concentrated HIV (e.g., in a research laboratory or production facility) is treated as percutaneous exposure to blood with highest risk. 2 Recommend—Postexposure prophylaxis (PEP) should be recommended to the exposed worker with counselling. Offer—PEP should be offered to the exposed worker with counselling. Not offer—PEP should not be offered because these are not occupational exposures to HIV. 3 Regimens: zidovudine (ZDV), 200 mg three times a day; lamivudine (3TC), 150 mg two times a day; indinavir (IDV), 800 mg three times a day (if IDV is not available, saquinavir may be used, 600 mg three times a day). Prophylaxis is given for 4 weeks. For full prescribing information, see package inserts. 4 Risk definitions for percutaneous blood exposure: Highest risk—BOTH larger volume of blood (e.g., deep injury with large diameter hollow needle previously in source patient’s vein or artery, especially involving an injection of source-patient’s blood) AND blood containing a high titre of HIV (e.g., source with acute retroviral illness or end-stage AIDS; viral load measurement may be considered, but its use in relation to PEP has not been evaluated). Increased risk—EITHER exposure to larger volume of blood OR blood with a high titre of HIV. No increased risk—NEITHER exposure to larger volume of blood NOR blood with a high titre of HIV (e.g., solid suture needle injury from source patient with asymptomatic HIV infection). 5 Possible toxicity of additional drug may not be warranted. 6 Includes semen; vaginal secretions; cerebrospinal, synovial, pleural, peritoneal, pericardial and amniotic fluids. 7 For skin, risk is increased for exposures involving a high titre of HIV, prolonged contact, an extensive area, or an area in which skin integrity is visibly compromised. For skin exposures without increased risk, the risk for drug toxicity outweighs the benefit of PEP.
Article 14(3) of EEC Directive 89/391/EEC on vaccination required only that effective vaccines, where they exist, be made available for exposed workers who are not already immune. There was an amending Directive 93/88/EEC which contained a recommended code of practice requiring that workers at risk be offered vaccination free of charge, informed of the benefits and disadvantages of vaccination and non-vaccination, and be provided a certificate of vaccination (WHO 1990).
The use of hepatitis B vaccine and appropriate environmental controls will prevent almost all occupational HBV infections. Reducing blood exposure and minimizing puncture injuries in the health care setting will reduce also the risk of transmission of other bloodborne viruses.
Hepatitis C. Transmission of HCV is similar to that of HBV, but infection persists in most patients indefinitely and more frequently progresses to long-term sequelae (Alter et al. 1992). The prevalence of anti-HCV among US hospital-based health care workers averages 1 to 2% (Alter 1993). HCWs who sustain accidental injuries from needlesticks contaminated with anti-HCV-positive blood have a 5 to 10% risk of acquiring HCV infection (Lampher et al. 1994; Mitsui et al. 1992). There has been one report of HCV transmission after a blood splash to the conjunctiva (Sartori et al. 1993). Prevention measures again consist of adherence to universal precautions and percutaneous injury prevention, since no vaccine is available and immune globulin does not appear to be effective.
Hepatitis D. Hepatitis D virus requires the presence of hepatitis B virus for replication; thus, HDV can infect persons only as a coinfection with acute HBV or as a superinfection of chronic HBV infection. HDV infection can increase the severity of liver disease; one case of occupationally acquired HDV infection hepatitis has been reported (Lettau et al. 1986). Hepatitis B vaccination of HBV-susceptible persons will also prevent HDV infection; however, there is no vaccine to prevent HDV superinfection of an HBV carrier. Other prevention measures consist of adherence to universal precautions and percutaneous injury prevention.
HIV
The first cases of AIDS were recognized in June of 1981. Initially, over 92% of the cases reported in the United States were in homosexual or bisexual men. However, by the end of 1982, AIDS cases were identified among injection drug users, blood transfusion recipients, haemophilia patients treated with clotting factor concentrates, children and Haitians. AIDS is the result of infection with HIV, which was isolated in 1985. HIV has spread rapidly. In the United States, for example, the first 100,000 AIDS cases occurred between 1981 and 1989; the second 100,000 cases occurred between 1989 and 1991. As of June 1994, 401,749 cases of AIDS had been reported in the United States (CDC 1994b).
Globally, HIV has affected many countries including those in Africa, Asia and Europe. As of 31 December 1994, 1,025,073 cumulative cases of AIDS in adults and children had been reported to the WHO. This represented a 20% increase from the 851,628 cases reported through December 1993. It was estimated that 18 million adults and about 1.5 million children have been infected with HIV since the beginning of the pandemic (late 1970s to early 1980s) (WHO 1995).
Although HIV has been isolated from human blood, breast milk, vaginal secretions, semen, saliva, tears, urine, cerebrospinal fluid and amniotic fluid, epidemiological evidence has implicated only blood, semen, vaginal secretions and breast milk in the transmission of the virus. The CDC has also reported on the transmission of HIV as the result of contact with blood or other body secretions or excretions from an HIV-infected person in the household (CDC 1994c). Documented modes of occupational HIV transmission include having percutaneous or mucocutaneous contact with HIV-infected blood. Exposure by the percutaneous route is more likely to result in infection transmission than is mucocutaneous contact.
There are a number of factors which may influence the likelihood of occupational bloodborne pathogen transmission, including: the volume of fluid in the exposure, the virus titre, the length of time of the exposure and the immune status of the worker. Additional data are needed to determine precisely the importance of these factors. Preliminary data from a CDC case-control study indicate that for percutaneous exposures to HIV-infected blood, HIV transmission is more likely if the source patient has advanced HIV disease and if the exposure involves a larger inoculum of blood (e.g., injury due to a large-bore hollow needle) (Cardo et al. 1995). Virus titre can vary between individuals and over time within a single individual. Also, blood from persons with AIDS, particularly in the terminal stages, may be more infectious than blood from persons in earlier stages of HIV infection, except possibly during the illness associated with acute infection (Cardo et al. 1995).
Occupational exposure and HIV infection
As of December 1996, CDC reported 52 HCWs in the United States who have seroconverted to HIV following a documented occupational exposure to HIV, including 19 laboratory workers, 21 nurses, six physicians and six in other occupations. Forty-five of the 52 HCWs sustained percutaneous exposures, five had mucocutaneous exposures, one had both a percutaneous and a mucocutaneous exposure and one had an unknown route of exposure. In addition, 111 possible cases of occupationally acquired infection have been reported. These possible cases have been investigated and are without identifiable non-occupational or transfusion risks; each reported percutaneous or mucocutaneous occupational exposures to blood or body fluids, or laboratory solutions containing HIV, but HIV seroconversion specifically resulting from an occupational exposure was not documented (CDC 1996a).
In 1993, the AIDS Centre at the Communicable Disease Surveillance Centre (UK) summarized reports of cases of occupational HIV transmission including 37 in the United States, four in the UK and 23 from other countries (France, Italy, Spain, Australia, South Africa, Germany and Belgium) for a total of 64 documented seroconversions after a specific occupational exposure. In the possible or presumed category there were 78 in the United States, six in the UK and 35 from other countries (France, Italy, Spain, Australia, South Africa, Germany, Mexico, Denmark, Netherlands, Canada and Belgium) for a total of 118 (Heptonstall, Porter and Gill 1993). The number of reported occupationally acquired HIV infections is likely to represent only a portion of the actual number due to under-reporting and other factors.
HIV post-exposure management
Employers should make available to workers a system for promptly initiating evaluation, counselling and follow-up after a reported occupational exposure that may place a worker at risk of acquiring HIV infection. Workers should be educated and encouraged to report exposures immediately after they occur so that appropriate interventions can be implemented (CDC 1990).
If an exposure occurs, the circumstances should be recorded in the worker’s confidential medical record. Relevant information includes the following: date and time of exposure; job duty or task being performed at the time of exposure; details of exposure; description of source of exposure, including, if known, whether the source material contained HIV or HBV; and details about counselling, post-exposure management and follow-up. The source individual should be informed of the incident and, if consent is obtained, tested for serological evidence of HIV infection. If consent cannot be obtained, policies should be developed for testing source individuals in compliance with applicable regulations. Confidentiality of the source individual should be maintained at all times.
If the source individual has AIDS, is known to be HIV seropositive, refuses testing or the HIV status is unknown, the worker should be evaluated clinically and serologically for evidence of HIV infection as soon as possible after the exposure (baseline) and, if seronegative, should be retested periodically for a minimum of 6 months after exposure (e.g., six weeks, 12 weeks and six months after exposure) to determine whether HIV infection has occurred. The worker should be advised to report and seek medical evaluation for any acute illness that occurs during the follow-up period. During the follow-up period, especially the first six to 12 weeks after the exposure, exposed workers should be advised to refrain from blood, semen or organ donation and to abstain from, or use measures to prevent HIV transmission, during sexual intercourse.
In 1990, CDC published a statement on the management of exposure to HIV including considerations regarding zidovudine (ZDV) post-exposure use. After a careful review of the available data, CDC stated that the efficacy of zidovudine could not be assessed due to insufficient data, including available animal and human data (CDC 1990).
In 1996, information suggesting that ZDV post-exposure prophylaxis (PEP) may reduce the risk for HIV transmission after occupational exposure to HIV-infected blood (CDC 1996a) prompted a US Public Health Service (PHS) to update a previous PHS statement on management of occupational exposure to HIV with the following findings and recommendations on PEP (CDC 1996b). Although failures of ZDV PEP have occurred (Tokars et al. 1993), ZDV PEP was associated with a decrease of approximately 79% in the risk for HIV seroconversion after percutaneous exposure to HIV-infected blood in a case-control study among HCWs (CDC 1995).
Although information about the potency and toxicity of antiretroviral drugs is available from studies of HIV-infected patients, it is uncertain to what extent this information can be applied to uninfected persons receiving PEP. In HIV-infected patients, combination therapy with the nucleosides ZDV and lamivudine (3TC) has greater antiretroviral activity than ZDV alone and is active against many ZDV-resistant HIV strains without significantly increased toxicity (Anon. 1996). Adding a protease inhibitor provides even greater increases in antiretroviral activity; among protease inhibitors, indinavir (IDV) is more potent than saquinavir at currently recommended doses and appears to have fewer drug interactions and short-term adverse effects than ritonavir (Niu, Stein and Schnittmann 1993). Few data exist to assess possible long-term (i.e., delayed) toxicity resulting from use of these drugs in persons not infected with HIV.
The following PHS recommendations are provisional because they are based on limited data regarding efficacy and toxicity of PEP and risk for HIV infection after different types of exposure. Because most occupational exposures to HIV do not result in infection transmission, potential toxicity must be carefully considered when prescribing PEP. Changes in drug regimens may be appropriate, based on factors such as the probable antiretroviral drug resistance profile of HIV from the source patient, local availability of drugs and medical conditions, concurrent drug therapy and drug toxicity in the exposed worker. If PEP is used, drug-toxicity monitoring should include a complete blood count and renal and hepatic chemical function tests at baseline and two weeks after starting PEP. If subjective or objective toxicity is noted, drug reduction or drug substitution should be considered, and further diagnostic studies may be indicated.
Chemoprophylaxis should be recommended to exposed workers after occupational exposures associated with the highest risk for HIV transmission. For exposures with a lower, but non-negligible risk, PEP should be offered, balancing the lower risk against the use of drugs having uncertain efficacy and toxicity. For exposures with negligible risk, PEP is not justified (see table 2 ). Exposed workers should be informed that knowledge about the efficacy and toxicity of PEP is limited, that for agents other than ZDV, data are limited regarding toxicity in persons without HIV infection or who are pregnant and that any or all drugs for PEP may be declined by the exposed worker.
PEP should be initiated promptly, preferably with 1 to 2 hours post-exposure. Although animal studies suggest that PEP probably is not effective when started later than 24 to 36 hours post-exposure (Niu, Stein and Schnittmann 1993; Gerberding 1995), the interval after which there is no benefit from PEP for humans is undefined. Initiating therapy after a longer interval (e.g., 1 to 2 weeks) may be considered for the highest risk exposures; even if infection is not prevented, early treatment of acute HIV infection may be beneficial (Kinloch-de-los et al. 1995).
If the source patient or the patient’s HIV status is unknown, initiating PEP should be decided on a case-by-case basis, based on the exposure risk and likelihood of infection in known or possible source patients.
Other Bloodborne Pathogens
Syphilis, malaria, babesiosis, brucellosis, leptospirosis, arboviral infections, relapsing fever, Creutzfeldt-Jakob disease, human T-lymphotropic virus type 1 and viral haemorrhagic fever have also been transmitted by the bloodborne route (CDC 1988a; Benenson 1990). Occupational transmission of these agents has only rarely been recorded, if ever.
Prevention of Transmission of Bloodborne Pathogens
There are several basic strategies which relate to the prevention of occupational transmission of bloodborne pathogens. Exposure prevention, the mainstay of occupational health, can be accomplished by substitution (e.g., replacing an unsafe device with a safer one), engineering controls (i.e., controls that isolate or remove the hazard), administrative controls (e.g., prohibiting recapping of needles by a two-handed technique) and use of personal protective equipment. The first choice is to “engineer out the problem”.
In order to reduce exposures to bloodborne pathogens, adherence to general infection control principles, as well as strict compliance with universal precaution guidelines, is required. Important components of universal precautions include the use of appropriate personal protective equipment, such as gloves, gowns and eye protection, when exposure to potentially infectious body fluids is anticipated. Gloves are one of the most important barriers between the worker and the infectious material. While they do not prevent needlesticks, protection for the skin is provided. Gloves should be worn when contact with blood or body fluids is anticipated. Washing of gloves in not recommended. Recommendations also advise workers to take precautions to prevent injuries by needles, scalpels and other sharp instruments or devices during procedures; when cleaning used instruments; during disposal of used needles; and when handling sharp instruments after procedures.
Percutaneous exposures to blood
Since the major risk of infection results from parenteral exposure from sharp instruments such as syringe needles, engineering controls such as resheathing needles, needleless IV systems, blunt suture needles and appropriate selection and use of sharps disposal containers to minimize exposures to percutaneous injuries are critical components of universal precautions.
The most common type of percutaneous inoculation occurs through inadvertent needlestick injury, many of which are associated with recapping of needles. The following reasons have been indicated by workers as reasons for recapping: inability to properly dispose of needles immediately, sharps disposal containers too far away, lack of time, dexterity problems and patient interaction.
Needles and other sharp devices can be redesigned to prevent a significant proportion of percutaneous exposures. A fixed barrier should be provided between hands and the needle after use. Worker’s hands should remain behind the needle. Any safety feature should be an integral part of the device. The design should be simple and little or no training should be required (Jagger et al. 1988).
Implementing safer needle devices must be accompanied by evaluation. In 1992, the American Hospital Association (AHA) published a briefing to assist hospitals with the selection, evaluation and adoption of safer needle devices (AHA 1992). The briefing stated that “because safer needle devices, unlike drugs and other therapies, do not undergo clinical testing for safety and efficacy before they are marketed, hospitals are essentially ‘on their own’ when it comes to selecting appropriate products for their specific institutional needs”. Included in the AHA document are guidance for the evaluation and adoption of safer needle devices, case studies of the use of safety devices, evaluation forms and listing of some, but not all, products on the US market.
Prior to implementation of a new device, health care institutions must ensure that there is an appropriate needlestick surveillance system in place. In order to accurately assess the efficacy of new devices, the number of reported exposures should be expressed as an incidence rate.
Possible denominators for reporting the number of needlestick injuries include patient days, hours worked, number of devices purchased, number of devices used and number of procedures performed. The collection of specific information on device-related injuries is an important component of the evaluation of the effectiveness of a new device. Factors to be considered in collecting information on needlestick injuries include: new product distribution, stocking and tracking; identification of users; removal of other devices; compatibility with other devices (especially IV equipment); ease of use; and mechanical failure. Factors which may contribute to bias include compliance, subject selection, procedures, recall, contamination, reporting and follow-up. Possible outcome measures include rates of needlestick injuries, HCW compliance, patient care complications and cost.
Finally, training and feedback from workers are important components of any successful needlestick prevention programme. User acceptance is a critical factor, but one that seldom receives enough attention.
Elimination or reduction of percutaneous injuries should result if adequate engineering controls are available. If HCWs, product evaluation committees, administrators and purchasing departments all work together to identify where and what safer devices are needed, safety and cost effectiveness can be combined. Occupational transmission of bloodborne pathogens is costly, both in terms of money and the impact on the employee. Every needlestick injury causes undue stress on the employee and may affect job performance. Referral to mental health professionals for supportive counselling may be required.
In summary, a comprehensive approach to prevention is essential to maintaining a safe and healthy environment in which to provide health care services. Prevention strategies include the use of vaccines, post-exposure prophylaxis and prevention or reduction of needlestick injuries. Prevention of needlestick injuries can be accomplished by improvement in the safety of needle-bearing devices, development of procedures for safer use and disposal and adherence to infection control recommendations.
Acknowledgements: The authors thank Mariam Alter, Lawrence Reed and Barbara Gooch for their manuscript review.
Subways
While railroad safety comes under the jurisdiction of national governments, which issue rules and policies for safety governance and enforcement, subways are usually governed by local public authorities, which in essence govern themselves.
Subway fares usually do not cover operating cost and, through subsidies, are kept at certain levels to maintain an affordable public transportation service. Subway and other city mass transit systems make city roads more accessible and reduce the pollution associated with urban automobile traffic.
Budget cuts that have become so common in many countries in recent years also affect mass transit systems. Preventive maintenance personnel and the upgrade of tracks, signals and rolling stock are the first to be affected. The controlling authorities are often unwilling or unable to enforce their own regulatory procedures on a rapid transit system abandoned by government subsidies. Inevitably in such circumstances, a transportation accident with catastrophic loss of life during the budget cuts results in a public outcry demanding improvements in safety.
While it is recognized that great variation exists in the design, construction and age of the physical facilities of the rapid transit properties in Canada, the United States and other countries, certain standard maintenance functions must be carried out to keep operating track, aerial and underground structures, passenger stations and related facilities in the safest possible condition.
Subway Operation and Maintenance
Subways differ from railroads in several basic ways:
- most subways run underground in tunnels
- subways run on electricity rather than diesel or steam (although there are also some electrical trains)
- subways run much more frequently than railroad trains
- graffiti removal is a major problem.
These factors influence the degree of risk for subway train operators and maintenance crews.
Collisions between subway trains on the same track and with maintenance crews on the track are a serious problem. These collisions are controlled by proper scheduling, central communications systems to alert subway train operators of problems and signal light systems indicating when operators can proceed safely. Breakdowns in these control procedures resulting in collisions can occur due to radio communication problems, broken or improperly placed signal lights that do not give operators adequate time to stop and fatigue problems from shift work and excessive overtime, resulting in inattention.
Maintenance crews patrol the subway tracks doing repairs to tracks, signal lights and other equipment, picking up rubbish and performing other duties. They face electrical hazards from the third rail carrying the electricity to operate the subways, fire and smoke hazards from burning rubbish and possible electrical fires, inhalation hazards from steel dust and other particulates in the air from the subway wheels and rails and the hazard of being hit by subway cars. Floods in subways can also create electrical shock and fire hazards. Because of the nature of subway tunnels, many of these hazardous situations are confined-space hazards.
Adequate ventilation to remove air contaminants, proper confined-space and other emergency procedures (e.g., evacuation procedures) for fires and floods and adequate communication procedures including radios and signal lights to notify subway train operators of the presence of maintenance crews on the tracks are essential to protect these crews. There should be frequent emergency spaces along subway walls or adequate space between tracks to allow maintenance crew members to avoid passing subway cars.
Graffiti removal from both the inside and outside of subway cars is a hazard in addition to regular painting and cleaning of cars. Graffiti removers often contained strong alkalis and hazardous solvents and can be a hazard both by skin contact and inhalation. Exterior graffiti removal is done by driving the cars through a car wash where the chemicals are sprayed on the exterior of the car. The chemicals are also applied by brushing and spraying inside subway cars. Applying hazardous graffiti removers inside cars could be a confined-space hazard.
Precautions include using the least toxic chemicals possible, proper respirator protection and other personal protective equipment and proper procedures to ensure that car operators know what chemicals are being used.
Parks and Botanical Gardens
The occupational safety and health hazards for those who work in parks and botanical gardens fall in the following general categories: environmental, mechanical, biological or chemical, vegetation, wildlife and caused by human beings. The risks differ depending on where the site is located. Urban, suburban, developed or undeveloped wildland will differ.
Environmental Hazards
As parks and garden personnel are found in all geographical areas and generally spend a great deal, if not all, of their working time outdoors, they are exposed to the widest variety and extremes of temperature and climatic conditions, with the resultant risks ranging from heat stroke and exhaustion to hypothermia and frostbite.
Those who work in urban areas may be in facilities where vehicular traffic is significant and may be exposed to toxic exhaust emissions such as carbon monoxide, unburned carbon particles, nitrous oxide, sulphuric acid, carbon dioxide and palladium (from the breakdown of catalytic converters).
Because some facilities are located in the higher elevations of mountainous regions, altitude sickness may be a risk if an employee is new to the area or is prone to high or low blood pressure.
Park area workers are usually called upon to perform search and rescue and disaster control activities during and following natural disasters such as earthquakes, hurricanes, flooding, volcanic eruptions and the like affecting their area, with all of the risks inherent in such events.
It is essential that all personnel be thoroughly trained in the potential environmental risks inherent in their areas and be provided with the proper clothing and equipment, such as adequate cold- or hot-weather gear, water and rations.
Mechanical Hazards
Personnel in parks and gardens are called upon to be thoroughly familiar with and operate an extremely wide variety of mechanical equipment, ranging from small hand tools and power tools and powered lawn and garden equipment (mowers, thatchers, rototillers, chainsaws, etc.) to heavy equipment such as small tractors, snow ploughs, trucks and heavy construction equipment. Additionally, most facilities have their own shops equipped with heavy power tools such as table saws, lathes, drill presses, air pressure pumps and so on.
Employees must be thoroughly trained in the operation, hazards and safety devices for all types of equipment they could potentially operate, and be provided and trained in the use of the appropriate personal protection equipment. Since some personnel may also be required to operate or ride the full range of motor vehicles, and fixed- or rotary-wing aircraft, they must be thoroughly trained and licensed, and regularly tested. Those that ride as passengers must have knowledge of the risks and training in safe operation of such equipment.
Biological and Chemical Hazards
Continuous, close contact with the general public is inherent in almost every occupation in park and garden work. The risk of contracting viral or bacterial diseases is always present. Additionally, the risk of contact with infected wildlife that carry rabies, psitticosis, Lyme disease and so on is present.
Park and botanical garden workers are exposed to various amounts and concentrations of pesticides, herbicides, fungicides, fertilizers and other agricultural chemicals, as well as toxic paints, thinners, varnishes, lubricants and so on used in maintenance and transport work and equipment.
With the proliferation of illegal drugs, it is becoming common for personnel in national parks and forests to come across illegal drug-manufacturing laboratories. The chemicals found in these can cause death or permanent neurological damage. Personnel in urban and rural areas may also encounter discarded drug paraphernalia such as used hypodermic syringes, needles, spoons and pipes. If any of these punctures the skin or enters the body, illness ranging from hepatitis to HIV could result.
Thorough training in the risks and preventive measures is essential; regular physical examinations should be provided and immediate medical attention sought if a person is so exposed. It is essential that the type and duration of exposure be recorded, if possible, to be given to the treating physician. Whenever illegal drug paraphernalia is encountered personnel should not touch it but rather should secure the area and refer the matter to trained law enforcement personnel.
Vegetation Hazards
Most types of vegetation pose no health risk. However, in wildland areas (and some urban and suburban park areas) poisonous plants such as poison ivy, poison oak and poison sumac can be found. Health problems ranging from a minor rash to a severe allergic reaction can result, depending on the susceptibility of the individual and the nature of the exposure.
It should be noted that roughly 22% of the total population suffers from allergic reactions of one form or another, ranging from mild to severe; an allergic individual may respond to only a few substances, or to many hundreds of different types of vegetation and animal life. Such reactions can result in death, in extreme cases, if immediate treatment is not found.
Prior to working in any environment with plant life, it should be determined whether an employee has any allergies to potential allergens and should take or carry appropriate medication.
Personnel should also be cognizant of plant life that is not safe to ingest, and should know the signs of ingestion illness and the antidotes.
Wildlife Hazards
Parks workers will encounter the full spectrum of wildlife that exists around the world. They must be familiar with the types of animals, their habits, the risks and, where necessary, the safe handling of the wildlife expected to be encountered. Wildlife ranges from urban domestic animals, such as dogs and cats, to rodents, insects and snakes, to wildland animals and bird species including bears, mountain lions, poisonous snakes and spiders, and so on.
Proper training in the recognition and handling of wildlife, including the diseases affecting such wildlife, should be provided. Appropriate medical response kits for poisonous snakes and insects should be available, along with training in how to use them. In remote wildland areas, it may be necessary to have personnel trained in the use of, and be equipped with, firearms for personal protection.
Human-caused Hazards
In addition to the aforementioned risk of contact with a visitor having a contagious illness, a major share of the risks faced by personnel who work in the parks, and to a lesser degree botanical gardens, are the result of either accidental or deliberate action of facilities visitors. Those risks range from the need of park employees to perform search and rescue activities for lost or injured visitors (some in the most remote and dangerous environments) to responding to acts of vandalism, drunkenness, fighting and other disruptive activities, including assault on park or garden employees. Additionally, the park or garden employee is at risk of vehicular accidents caused by visitors or others who are driving by or in the vicinity of the employee.
Approximately 50% of all wildland fires have a human cause, attributable to either arson or negligence, to which the park employee may be required to respond.
Wilful damage or destruction of public property is also, unfortunately, a risk the park or garden employee may well be required to respond to and repair, and, depending on the type of property and degree of damage, a significant safety risk may be present (i.e., damage to wilderness trails, foot bridges, interior doors, plumbing equipment and so on).
Personnel who work with the environment are, generally, sensitive and attuned to the outdoors and to preservation. As a result, many such personnel suffer from varying degrees of stress and related illnesses because of the unfortunate actions of some of those who visit their facilities. It is important, therefore, to be aware of the onset of stress and take remedial action. Classes in stress management are helpful for all such personnel.
Violence
Violence in the workplace is, unfortunately, becoming an increasing common risk and cause of injury. There are two general classes of violence: physical and psychological. The types of violence range from simple verbal threats to mass murder, as evidenced by the 1995 bombing of the US federal office building, Oklahoma City, Oklahoma. In 1997 a tribal police officer was killed while trying to serve a warrant on a Southwest Indian reservation. There is also a less discussed, but common, psychological violence that has been classed euphemistically as “office politics” that can have equally debilitating effects.
Physical. In the United States, attacks on federal, state and local governmental personnel who work in remote and semi-remote parks and recreation areas are not uncommon. The majority of these result in injury only, but some involve assaults with dangerous weapons. There have been instances where disgruntled members of the public have entered federal land-managing agencies’ offices brandishing firearms, threatened the employees and had to be restrained.
Such violence can result in injury ranging from minor to fatal. It can be inflicted by unarmed assault or the use of the widest variety of weapons, ranging from simple club and stick to handguns, rifles, knives, explosives and chemicals. It is not uncommon for such violence to be inflicted upon the vehicles and structures owned or used by the governmental agency that operates the park or recreational facility.
It is also not uncommon for disgruntled or dismissed employees to seek retaliation against current or former supervisors. It is also becoming common for outdoor recreation, forest and park employees to encounter persons growing and/or manufacturing illegal drugs in remote areas. Such persons do not hesitate to resort to violence to protect their perceived territory. Park and recreation personnel, particularly those involved in law enforcement, are required to deal with persons under the influence of drugs or alcohol who break the law and become violent when apprehended.
Psychological. Not as well publicized, but in some instances equally damaging, is psychological violence. Commonly called “office politics”, it has been in use probably since the beginning of civilization to gain status over co-workers, gain an advantage in the workplace and/or weaken a perceived opponent. It consists of destroying the credibility of another person or group, usually without that other person or group being aware that it is being done.
In some instances, it is done openly, through the media, legislative bodies and so on, in an attempt to gain political advantage (for example, destroying the credibility of a governmental agency in order to cut its funding).
This usually has a significant negative result on the morale of the individual or group involved and, in rare, extreme instances, can cause a recipient of the violence to take his or her own life.
It is not uncommon for victims of violence to suffer from post-traumatic stress disorder, which may affect them for years. It has the same effect as “shell shock” among military personnel who have experienced prolonged and intense combat. It may require extensive psychological counselling.
Protective measures. Because of the constantly increased risk of encountering violence in the workplace, it is essential that employees receive extensive training in the recognition and avoidance of potentially dangerous situations, including training in how to deal with persons who are violent or out of control.
- Where possible, additional security needs to be added to high-density occupancy areas.
- Employees who work away from a standard office or shop location should be provided with two-way radio communication to be able to summon help when needed.
- In some instances, it may be necessary to train employees in the use of firearms and arm them for self-protection.
- Each agency responsible for managing park or outdoor recreation areas should conduct an annual security survey of all its facilities to determine current risk and what measures are necessary to protect employees.
- Management at all levels needs to exercise extra vigilance to counter the psychological risk whenever it occurs, seek out and correct unfounded rumours and assure that all employees have accurate facts concerning the operation and future plans of their agency and workplace.
Post-incidence assistance. It is equally essential, not only for the affected employees or employers, but all agency employees as well, that any employee subjected to on-the-job violence be given not only prompt medical attention, but equally prompt psychological assistance and stress counselling. The effects of such violence can remain with the employee long after the physical wounds heal and can have a significant negative effect on his or her ability to function in the workplace.
As the population increases, the incidence of violence will increase. Preparation and prompt and effective response are, at present, the only remedies open to those at risk.
Conclusion
Because personnel are required to work in all types of environments, good health and physical fitness is essential. A consistent regimen of moderate physical training should be adhered to. Regular physical examinations, geared to the type of work to be performed, should be obtained. All personnel should be completely trained in types of work to be performed, the hazards involved and hazard avoidance.
Equipment should be maintained in sound operating condition.
All personnel expected to work in remote areas should carry two-way radio communication equipment and be in regular contact with a base station.
All personnel should have basic—and if possible, advanced—first aid training, including cardio-pulmonary resuscitation, in the event a visitor or co-worker is injured and medical help is not immediately available.
Tuberculosis Prevention, Control and Surveillance
Transmission of Mycobacterium tuberculosis is a recognized risk in health care facilities. The magnitude of the risk to HCWs varies considerably by the type of health care facility, the prevalence of TB in the community, the patient population served, the HCW’s occupational group, the area of the health care facility in which the HCW works and the effectiveness of TB infection-control interventions. The risk may be higher in areas where patients with TB are provided care before diagnosis and initiation of TB treatment and isolation precautions (e.g., in clinic waiting areas and emergency departments) or where diagnostic or treatment procedures that stimulate coughing are performed. Nosocomial transmission of M. tuberculosis has been associated with close contact with persons who have infectious TB and with the performance of certain procedures (e.g., bronchoscopy, endotracheal intubation and suctioning, open abscess irrigation and autopsy). Sputum induction and aerosol treatments that induce coughing may also increase the potential for transmission of M. tuberculosis. Personnel in health care facilities should be particularly alert to the need for preventing transmission of M. tuberculosis in those facilities in which immunocompromised persons (e.g., HIV-infected persons) work or receive care—especially if cough-inducing procedures, such as sputum induction and aerosolized pentamidine treatments, are being performed.
Transmission and Pathogenesis
M. tuberculosis is carried in airborne particles, or droplet nuclei, that can be generated when persons who have pulmonary or laryngeal TB sneeze, cough, speak or sing. The particles are an estimated 1 to 5 μm in size and normal air currents can keep them airborne for prolonged time periods and spread them throughout a room or building. Infection occurs when a susceptible person inhales droplet nuclei containing M. tuberculosis and these droplet nuclei traverse the mouth or nasal passages, upper respiratory tract and bronchi to reach the alveoli of the lungs. Once in the alveoli, the organisms are taken up by alveolar macrophages and spread throughout the body. Usually within two to ten weeks after initial infection with M. tuberculosis, the immune response limits further multiplication and spread of the tubercle bacilli; however, some of the bacilli remain dormant and viable for many years. This condition is referred to as latent TB infection. Persons with latent TB infection usually have positive purified protein derivative (PPD)-tuberculin skin-test results, but they do not have symptoms of active TB, and they are not infectious.
In general, persons who become infected with M. tuberculosis have approximately a 10% risk for developing active TB during their lifetimes. This risk is greatest during the first two years after infection. Immunocompromised persons have a greater risk for the progression of latent TB infection to active TB disease; HIV infection is the strongest known risk factor for this progression. Persons with latent TB infection who become co-infected with HIV have approximately an 8 to 10% risk per year for developing active TB. HIV-infected persons who are already severely immunosuppressed and who become newly infected with M. tuberculosis have an even greater risk for developing active TB.
The probability that a person who is exposed to M. tuberculosis will become infected depends primarily on the concentration of infectious droplet nuclei in the air and the duration of exposure. Characteristics of the TB patient that enhance transmission include:
- disease in the lungs, airways or larynx
- presence of cough or other forceful expiratory measures
- presence of acid-fast bacilli (AFB) in the sputum
- failure of the patient to cover the mouth and nose when coughing or sneezing
- presence of cavitation on chest radiograph
- inappropriate or short duration of chemotherapy
- administration of procedures that can induce coughing or cause aerosolization of M. tuberculosis (e.g., sputum induction).
Environmental factors that enhance the likelihood of transmission include:
- exposure in relatively small, enclosed spaces
- inadequate local or general ventilation that results in insufficient dilution and/or removal of infectious droplet nuclei
- recirculation of air containing infectious droplet nuclei.
Characteristics of the persons exposed to M. tuberculosis that may affect the risk for becoming infected are not as well defined. In general, persons who have been infected previously with M. tuberculosis may be less susceptible to subsequent infection. However, reinfection can occur among previously infected persons, especially if they are severely immunocompromised. Vaccination with Bacille of Calmette and Guérin (BCG) probably does not affect the risk for infection; rather, it decreases the risk for progressing from latent TB infection to active TB. Finally, although it is well established that HIV infection increases the likelihood of progressing from latent TB infection to active TB, it is unknown whether HIV infection increases the risk for becoming infected if exposed to M. tuberculosis.
Epidemiology
Several TB outbreaks among persons in health care facilities have been reported recently in the United States. Many of these outbreaks involved transmission of multidrug-resistant strains of M. tuberculosis to both patients and HCWs. Most of the patients and some of the HCWs were HIV-infected persons in whom new infection progressed rapidly to active disease. Mortality associated with those outbreaks was high (with a range of 43 to 93%). Furthermore, the interval between diagnosis and death was brief (with a range of median intervals of 4 to 16 weeks). Factors contributing to these outbreaks included delayed diagnosis of TB, delayed recognition of drug resistance and delayed initiation of effective therapy, all of which resulted in prolonged infectiousness, delayed initiation and inadequate duration of TB isolation, inadequate ventilation in TB isolation rooms, lapses in TB isolation practices and inadequate precautions for cough-inducing procedures and lack of adequate respiratory protection.
Fundamentals of TB infection control
An effective TB infection-control programme requires early identification, isolation and effective treatment of persons who have active TB. The primary emphasis of the TB infection-control plan should be on achieving these three goals. In all health care facilities, particularly those in which persons who are at high risk for TB work or receive care, policies and procedures for TB control should be developed, reviewed periodically and evaluated for effectiveness to determine the actions necessary to minimize the risk for transmission of M. tuberculosis.
The TB infection-control programme should be based on a hierarchy of control measures. The first level of the hierarchy, and that which affects the largest number of persons, is using administrative measures intended primarily to reduce the risk for exposing uninfected persons to persons who have infectious TB. These measures include:
- developing and implementing effective written policies and protocols to ensure the rapid identification, isolation, diagnostic evaluation and treatment of persons likely to have TB
- implementing effective work practices among HCWs in the health care facility (e.g., correctly wearing respiratory protection and keeping doors to isolation rooms closed)
- educating, training and counselling HCWs about TB
- screening HCWs for TB infection and disease.
The second level of the hierarchy is the use of engineering controls to prevent the spread and reduce the concentration of infectious droplet nuclei. These controls include:
- direct source control using local exhaust ventilation
- controlling direction of airflow to prevent contamination of air in areas adjacent to the infectious source
- diluting and removing contaminated air via general ventilation
- air cleaning via air filtration or ultraviolet germicidal irradiation (UVGI).
The first two levels of the hierarchy minimize the number of areas in the health care facility where exposure to infectious TB may occur, and they reduce, but do not eliminate, the risk in those few areas where exposure to M. tuberculosis can still occur (e.g., rooms in which patients with known or suspected infectious TB are being isolated and treatment rooms in which cough-inducing or aerosol-generating procedures are performed on such patients). Because persons entering such rooms may be exposed to M. tuberculosis, the third level of the hierarchy is the use of personal respiratory protective equipment in these and certain other situations in which the risk for infection with M. tuberculosis may be relatively higher.
Specific measures to reduce the risk for transmission of M. tuberculosis include the following:
1. Assigning to specific persons in the health care facility the supervisory responsibility for designing, implementing, evaluating and maintaining the TB infection-control programme.
2. Conducting a risk assessment to evaluate the risk for transmission of M. tuberculosis in all areas of the health care facility, developing a written TB infection-control programme based on the risk assessment and periodically repeating the risk assessment to evaluate the effectiveness of the TB infection-control programme. TB infection-control measures for each health care facility should be based on a careful assessment of the risk for transmission of M. tuberculosis in that particular setting. The first step in developing the TB infection-control programme should be to conduct a baseline risk assessment to evaluate the risk for transmission of M. tuberculosis in each area and occupational group in the facility. Appropriate infection-control interventions can then be developed on the basis of actual risk. Risk assessments should be performed for all inpatient and outpatient settings (e.g., medical and dental offices). Classification of risk for a facility, for a specific area and for a specific occupational group should be based on the profile of TB in the community, the number of infectious TB patients admitted to the area or ward, or the estimated number of infectious TB patients to whom HCWs in an occupational group may be exposed and the results of analysis of HCW PPD test conversions (where applicable) and possible person-to-person transmission of M. tuberculosis. Regardless of risk level, the management of patients with known or suspected infectious TB should not vary. However, the index of suspicion for infectious TB among patients, the frequency of HCW PPD skin testing, the number of TB isolation rooms and other factors will depend on the level of risk for transmission of M. tuberculosis in the facility, area or occupational group.
3. Developing, implementing and enforcing policies and protocols to ensure early identification, diagnostic evaluation and effective treatment of patients who may have infectious TB. A diagnosis of TB may be considered for any patient who has a persistent cough (i.e., a cough lasting for longer than 3 weeks) or other signs or symptoms compatible with active TB (e.g., bloody sputum, night sweats, weight loss, anorexia or fever). However, the index of suspicion for TB will vary in different geographic areas and will depend on the prevalence of TB and other characteristics of the population served by the facility. The index of suspicion for TB should be very high in geographic areas or among groups of patients in which the prevalence of TB is high. Appropriate diagnostic measures should be conducted and TB precautions implemented for patients in whom active TB is suspected.
4. Providing prompt triage for and appropriate management of patients in the outpatient setting who may have infectious TB. Triage of patients in ambulatory-care settings and emergency departments should include vigorous efforts to identify promptly patients who have active TB. HCWs who are the first points of contact in facilities that serve populations at risk for TB should be trained to ask questions that will facilitate identification of patients with signs and symptoms suggestive of TB. Patients with signs or symptoms suggestive of TB should be evaluated promptly to minimize the amount of time they are in ambulatory-care areas. TB precautions should be followed while the diagnostic evaluation is being conducted for these patients. TB precautions in the ambulatory-care setting should include placing these patients in a separate area apart from other patients and not in open waiting areas (ideally, in a room or enclosure meeting TB isolation requirements), giving these patients surgical masks to wear and instructing them to keep their masks on and giving these patients tissues and instructing them to cover their mouths and noses with the tissues when coughing or sneezing. Surgical masks are designed to prevent the respiratory secretions of the person wearing the mask from entering the air. When not in a TB isolation room, patients suspected of having TB should wear surgical masks to reduce the expulsion of droplet nuclei into the air. These patients do not need to wear particulate respirators, which are designed to filter the air before it is inhaled by the person wearing the mask. Patients suspected of having or known to have TB should never wear a respirator that has an exhalation valve, because the device would provide no barrier to the expulsion of droplet nuclei into the air.
5. Promptly initiating and maintaining TB isolation for persons who may have infectious TB and who are admitted to the inpatient setting. In hospitals and other inpatient facilities, any patient suspected of having or known to have infectious TB should be placed in a TB isolation room that has currently recommended ventilation characteristics (see below). Written policies for initiating isolation should specify the indications for isolation, the person(s) authorized to initiate and discontinue isolation, the isolation practices to follow, the monitoring of isolation, the management of patients who do not adhere to isolation practices and the criteria for discontinuing isolation.
6. Effectively planning arrangements for discharge. Before a TB patient is discharged from the health care facility, the facility’s staff and public health authorities should collaborate to ensure continuation of therapy. Discharge planning in the health care facility should include, at a minimum, a confirmed outpatient appointment with the provider who will manage the patient until the patient is cured, sufficient medication to take until the outpatient appointment and placement into case management (e.g., directly observed therapy (DOT)) or outreach programmes of the public health department. These plans should be initiated and in place before the patient’s discharge.
7. Developing, installing, maintaining and evaluating ventilation and other engineering controls to reduce the potential for airborne exposure to M. tuberculosis. Local exhaust ventilation is a preferred source control technique, and it is often the most efficient way to contain airborne contaminants because it captures these contaminants near their source before they can disperse. Therefore, the technique should be used, if feasible, wherever aerosol-generating procedures are performed. Two basic types of local exhaust devices use hoods: the enclosing type, in which the hood either partially or fully encloses the infectious source, and the exterior type, in which the infectious source is near but outside the hood. Fully enclosed hoods, booths or tents are always preferable to exterior types because of their superior ability to prevent contaminants from escaping into the HCW’s breathing zone. General ventilation can be used for several purposes, including diluting and removing contaminated air, controlling airflow patterns within rooms and controlling the direction of airflow throughout a facility. General ventilation maintains air quality by two processes: dilution and removal of airborne contaminants. Uncontaminated supply air mixes with the contaminated room air (i.e., dilution), which is subsequently removed from the room by the exhaust system. These processes reduce the concentration of droplet nuclei in the room air. Recommended general ventilation rates for health care facilities are usually expressed in number of air changes per hour (ACH).
This number is the ratio of the volume of air entering the room per hour to the room volume and is equal to the exhaust airflow (Q, in cubic feet per minute) divided by the room volume (V, in cubic feet) multiplied by 60 (i.e., ACH = Q / V x 60). For the purposes of reducing the concentration of droplet nuclei, TB isolation and treatment rooms in existing health care facilities should have an airflow of greater than 6 ACH. Where feasible, this airflow rate should be increased to at least 12 ACH by adjusting or modifying the ventilation system or by using auxiliary means (e.g., recirculation of air through fixed HEPA filtration systems or portable air cleaners). New construction or renovation of existing health care facilities should be designed so that TB isolation rooms achieve an airflow of at least 12 ACH. The general ventilation system should be designed and balanced so that air flows from less contaminated (i.e., more clean) to more contaminated (less clean) areas. For example, air should flow from corridors into TB isolation rooms to prevent spread of contaminants to other areas. In some special treatment rooms in which operative and invasive procedures are performed, the direction of airflow is from the room to the hallway to provide cleaner air during these procedures. Cough-inducing or aerosol-generating procedures (e.g., bronchoscopy and irrigation of tuberculous abscesses) should not be performed in rooms with this type of airflow on patients who may have infectious TB. HEPA filters may be used in a number of ways to reduce or eliminate infectious droplet nuclei from room air or exhaust. These methods include placement of HEPA filters in exhaust ducts discharging air from booths or enclosures into the surrounding room, in ducts or in ceiling- or wall-mounted units, for recirculation of air within an individual room (fixed recirculation systems), in portable air cleaners, in exhaust ducts to remove droplet nuclei from air being discharged to the outside, either directly or through ventilation equipment, and in ducts discharging air from the TB isolation room into the general ventilation system. In any application, HEPA filters should be installed carefully and maintained meticulously to ensure adequate functioning. For general use areas in which the risk for transmission of M. tuberculosis is relatively high, ultraviolet lamps (UVGI) may be used as an adjunct to ventilation for reducing the concentration of infectious droplet nuclei, although the effectiveness of such units has not been evaluated adequately. Ultraviolet (UV) units can be installed in a room or corridor to irradiate the air in the upper portion of the room, or they can be installed in ducts to irradiate air passing through the ducts.
8. Developing, implementing, maintaining and evaluating a respiratory protection programme. Personal respiratory protection (i.e., respirators) should be used by persons entering rooms in which patients with known or suspected infectious TB are being isolated, persons present during cough-inducing or aerosol-generating procedures performed on such patients and persons in other settings where administrative and engineering controls are not likely to protect them from inhaling infectious airborne droplet nuclei. These other settings include transporting patients who may have infectious TB in emergency transport vehicles and providing urgent surgical or dental care to patients who may have infectious TB before a determination has been made that the patient is non-infectious.
9. Educating and training HCWs about TB, effective methods for preventing transmission of M. tuberculosis and the benefits of medical screening programmes. All HCWs, including physicians, should receive education regarding TB that is relevant to persons in their particular occupational group. Ideally, training should be conducted before initial assignment and the need for additional training should be re-evaluated periodically (e.g., once a year). The level and detail of this education will vary according to the HCW’s work responsibilities and the level of risk in the facility (or area of the facility) in which the HCW works. However, the programme may include the following elements:
- the basic concepts of M. tuberculosis transmission, pathogenesis and diagnosis,
including information concerning the difference between latent TB infection and active
TB disease, the signs and symptoms of TB and the possibility of reinfection
- the potential for occupational exposure to persons who have infectious TB in the
health care facility, including information concerning the prevalence of TB in the
community and facility, the ability of the facility to properly isolate patients who have
active TB, and situations with increased risk for exposure to M. tuberculosis
- the principles and practices of infection control that reduce the risk for transmission of
M. tuberculosis, including information concerning the hierarchy of TB infection-control
measures and the written policies and procedures of the facility. Site-specific control
measures should be provided to HCWs working in areas that require control
measures in addition to those of the basic TB infection-control programme.
- the importance of proper maintenance for engineering controls (e.g., cleaning UVGI lamps and ensuring negative pressure in TB isolation rooms)
- the purpose of PPD skin testing, the significance of a positive PPD test result and the importance of participating in the skin-test programme
- the principles of preventive therapy for latent TB infection; these principles include the indications, use, effectiveness and the potential adverse effects of the drugs
- the HCW’s responsibility to seek prompt medical evaluation if a PPD test conversion
occurs or if symptoms develop that could be caused by TB. Medical evaluation will
enable HCWs who have TB to receive appropriate therapy and will help to prevent
transmission of M. tuberculosis to patients and other HCWs.
- the principles of drug therapy for active TB
- the importance of notifying the facility if the HCW is diagnosed with active TB so that contact investigation procedures can be initiated
- the responsibilities of the facility to maintain the confidentiality of the HCW while
ensuring that the HCW who has TB receives appropriate therapy and is non-
infectious before returning to duty
- the higher risks associated with TB infection in persons who have HIV infection or
other causes of severely impaired cell-mediated immunity, including (a) the more
frequent and rapid development of clinical TB after infection with M. tuberculosis, (b)
the differences in the clinical presentation of disease and (c) the high mortality rate associated with multiple drug resistant-TB in such persons
- the potential development of cutaneous anergy as immune function (as measured by CD4+ T-lymphocyte counts) declines
- information regarding the efficacy and safety of BCG vaccination and the principles of PPD screening among BCG recipients
- the facility’s policy on voluntary work reassignment options for immunocompromised HCWs.
10. Developing and implementing a programme for routine periodic counselling and screening of HCWs for active TB and latent TB infection. A TB counselling, screening and prevention programme for HCWs should be established to protect both HCWs and patients. HCWs who have positive PPD test results, PPD test conversions or symptoms suggestive of TB should be identified, evaluated to rule out a diagnosis of active TB and started on therapy or preventive therapy if indicated. In addition, the results of the HCW PPD screening programme will contribute to evaluation of the effectiveness of current infection-control practices. Because of the increased risk for rapid progression from latent TB infection to active TB in human immunodeficiency virus, HIV-infected or otherwise severely immunocompromised persons, all HCWs should know if they have a medical condition or are receiving a medical treatment that may lead to severely impaired cell-mediated immunity. HCWs who may be at risk for HIV infection should know their HIV status (i.e., they should be encouraged to voluntarily seek counselling and testing for HIV antibody status). Existing guidelines for counselling and testing should be followed routinely. Knowledge of these conditions allows the HCW to seek the appropriate preventive measures and to consider voluntary work reassignments.
11. ll HCWs should be informed about the need to follow existing recommendations for infection control to minimize the risk for exposure to infectious agents; implementation of these recommendations will greatly reduce the risk for occupational infections among HCWs. All HCWs should also be informed about the potential risks to severely immunocompromised persons associated with caring for patients who have some infectious diseases, including TB. It should be emphasized that limiting exposure to TB patients is the most protective measure that severely immunosuppressed HCWs can take to avoid becoming infected with M. tuberculosis. HCWs who have severely impaired cell-mediated immunity and who may be exposed to M. tuberculosis may consider a change in job-setting to avoid such exposure. HCWs should be advised of the legal option in many jurisdictions that severely immunocompromised HCWs can choose to transfer voluntarily to areas and work activities in which there is the lowest possible risk for exposure to M. tuberculosis. This choice should be a personal decision for HCWs after they have been informed of the risks to their health.
12. Employers should make reasonable accommodations (e.g., alternative job assignments) for employees who have a health condition that compromises cell-mediated immunity and who work in settings where they may be exposed to M. tuberculosis. HCWs who are known to be immunocompromised should be referred to employee health professionals who can individually counsel the employees regarding their risk for TB. Upon the request of the immunocompromised HCW, employers should offer, but not compel, a work setting in which the HCW would have the lowest possible risk for occupational exposure to M. tuberculosis.
13. All HCWs should be informed that immunosuppressed HCWs should have appropriate follow-up and screening for infectious diseases, including TB, provided by their medical practitioner. HCWs who are known to be HIV-infected or otherwise severely immunosuppressed should be tested for cutaneous anergy at the time of PPD testing. Consideration should be given to retesting, at least every 6 months, those immunocompromised HCWs who are potentially exposed to M. tuberculosis because of the high risk for rapid progression to active TB if they become infected.
14. Information provided by HCWs regarding their immune status should be treated confidentially. If the HCW requests voluntary job reassignment, the privacy of the HCW should be maintained. Facilities should have written procedures on confidential handling of such information.
15. Promptly evaluating possible episodes of M. tuberculosis transmission in health care facilities, including PPD skin-test conversions among HCWs, epidemiologically associated cases among HCWs or patients and contacts of patients or HCWs who have TB and who were not promptly identified and isolated. Epidemiological investigations may be indicated for several situations. These include, but are not limited to, the occurrence of PPD test conversions or active TB in HCWs, the occurrence of possible person-to-person transmission of M. tuberculosis and situations in which patients or HCWs with active TB are not promptly identified and isolated, thus exposing other persons in the facility to M. tuberculosis. The general objectives of the epidemiological investigations in these situations are as follows:
- to determine the likelihood that transmission of and infection with M. tuberculosis has occurred in the facility
- to determine the extent to which M. tuberculosis has been transmitted
- to identify those persons who have been exposed and infected, enabling them to receive appropriate clinical management
- to identify factors that could have contributed to transmission and infection and to implement appropriate interventions
- to evaluate the effectiveness of any interventions that are implemented and to ensure that exposure to and transmission of M. tuberculosis have been terminated.
16. Coordinating activities with the local public health department, emphasizing reporting and ensuring adequate discharge follow-up and the continuation and completion of therapy. As soon as a patient or HCW is known or suspected to have active TB, the patient or HCW should be reported to the public health department so that appropriate follow-up can be arranged and a community contact investigation can be performed. The health department should be notified well before patient discharge to facilitate follow-up and continuation of therapy. A discharge plan coordinated with the patient or HCW, the health department and the inpatient facility should be implemented.
Circuses and Amusement and Theme Parks
The common product shared between circuses and amusement and theme parks is creating and providing entertainment for the public’s enjoyment. Circuses can take place in a large temporary tent equipped with bleachers or in permanent buildings. Attending a circus is a passive activity in which the customer views the various animal, clown and acrobatic acts from a seated position. Amusement and theme parks, on the other hand, are locations where customers actively walk around the park and can participate in a wide variety of activities. Amusement parks can have many different types of rides, exhibits, games of skill, sales booths and stores, grandstand shows and other types of entertainment. Theme parks have exhibits, buildings and even small villages that illustrate the particular theme. Costume characters, who are actors dressed in costumes illustrating the theme—for example, historical costumes in historic villages or cartoon costumes for parks with a cartoon theme—will participate in shows or walk around among the visiting crowds. Local country fairs are another type of event where activities can include rides, animal and other side shows, such as fire-eating, and agricultural and farm animal exhibitions and competitions. The size of the operation can be as small as one person running a pony cart ride in a parking lot, or as large as a major theme park employing thousands. The larger the operation, the more background services that can be present, including parking lots, sanitation facilities, security and other emergency services and even hotels.
Occupations vary widely as do the levels of skills required for individual tasks. People employed in these activities include ticket sellers, acrobatic performers, animal handlers, food service workers, engineers, costume characters and ride operators, among a long list of other workers. The occupational safety and health risks include many of those found in general industry and others that are unique to circuses and amusement and theme park operations. The following information provides a review of entertainment-related hazards and precautions found within this segment of the industry.
Acrobatics and Stunts
Circuses, in particular, have many acrobatic and stunt acts, including high-wire tightrope walking and other aerial acts, gymnastic acts, fire-juggling acts and displays of horsemanship. Amusement and theme parks can also have similar activities. Hazards include falls, misjudged clearances, improperly inspected equipment and physical fatigue due to multiple daily shows. Typical accidents involve muscular, tendon and skeletal injuries.
Precautions include the following: Performers should receive comprehensive physical conditioning, proper rest and a good diet, and show schedules should be rotated. All equipment, props, rigging, safety devices and blocking should be carefully reviewed before each performance. Show personnel should not perform when they are ill, injured or taking medication which may affect required abilities to safely meet the needs of the show.
Animal Handling
Animals are most commonly found in circuses and county fairs, although they can also be found in activities such as pony rides in amusement parks. Animals are found in circuses in wild-animal training acts, for example, with lions and tigers, horse riding acts and other trained animal acts. Elephants are used as show performers, rides, exhibits and work animals. In country fairs, farm animals such as pigs, cattle and horses are exhibited in competitions. In some places, exotic animals are displayed in cages and in such acts as snake handling. Hazards include the unpredictable characteristics of animals combined with the potential for animal handlers to become overly confident and let their guard down. Serious injury and death are possible in this occupation. Elephant handling is considered one of the most dangerous professions. Some estimates indicate there are approximately 600 keepers in the United States and Canada. During the course of an average year there will be one elephant handler killed. Venomous snakes, if used in snake-handling acts, can also be very dangerous, with possible fatalities from snake bites.
Precautions include intense and ongoing animal-handling training. It must be instilled in employees to remain on their guard at all times. The use of protected contact systems is recommended where keepers work alongside animals capable of causing serious injury or death. Protected contact systems always separate the animal handler and the animal by means of bars or closed-off areas. When animals perform on stage to live audiences, noise and other stimuli conditioning must be a part of the required safety training. With venomous reptiles, proper anti-venom antidotes and protective equipment such as gloves, leg guards, snake pincers and carbon dioxide bottles should be available. Care and feeding of animals when they are not being exhibited also requires careful attention on the part of the animal caretakers to prevent injury.
Costume Characters
Costume characters acting the role of cartoon figures or historical period characters often wear heavy and bulky costumes. They can act on stages or mingle with the crowds. Hazards are back and neck injuries associated with wearing such costumes with uneven weight distribution (figure 1). Other exposures are fatigue, heat-related problems, crowd pushing and hitting. See also “Actors”.
Figure 1. Worker wearing a heavy costume.
William Avery
Precautions include the following: Costumes should be correctly fitted to the individual. The weight load, especially above the shoulders, should be kept at a minimum. Costume characters should drink plenty of water during periods of warm weather. Interaction with the public should be of short duration because of the stress of such work. Character duties should be rotated, and non-costumed escorts should be with characters at all times to manage crowds.
Fireworks
Fireworks displays and pyrotechnics special effects can be a common activity (figure 2). Hazards can involve accidental discharge, non-planned explosions and fire.
Figure 2. Loading pyrotechnics for fireworks show.
William Avery
Precautions include the following: Only appropriately trained and licensed pyrotechnicians should detonate explosives. Storage, transportation and detonation procedures must be followed (figure 3). Applicable codes, laws and ordinances in the jurisdiction where operating must be adhered to. Pre-approved personal safety equipment and fire extinguishing equipment must be at the detonation site where there is immediate access.
Figure 3. Bunker storage for fireworks.
William Avery
Food Service
Food can be bought at circuses and amusement and theme parks from individuals with trays of food, at vendor carts, booths, or even restaurants. Hazards common to food service operations at these events involve serving large captive audiences during high periods of demand in a very short period of time. Falls, burns, cuts and repetitive motion trauma are not uncommon in this occupational classification. Carrying food around on trays can involve back injuries. The risks are increased during periods of high volume. A common example of injury occurring in high-volume food service areas is repetitive motion trauma that can result in tendinitis and carpal tunnel syndrome. One example of a job description where such injuries occur is an ice-cream scooper.
Precautions include the following: Increased staffing during high-volume periods is essential to the safety of the operation. Specific duties such as mopping, sweeping and cleaning should be addressed. Precautions for repetitive motion trauma: regarding the example given above, using softer ice cream can make scooping less strenuous, employees can be regularly rotated, scoops can be warmed to promote easier penetration of the ice cream and the use of ergonomically designed handles should be considered.
Scenery, Props and Exhibits
Stage shows, exhibits, booths, artificial scenery and buildings must be built. Hazards include many of the same hazards as found in construction, including electrocution, severe lacerations, and eye and other injuries associated with the use of power tools and equipment. The outdoor building and use of props, scenery and exhibits increases the potential hazards such as collapse if construction is inadequate. Handling of these components can result in falls and back and neck injuries (see also “Scenery shops” in this chapter).
Precautions include the following: The manufacturer’s warnings, safety equipment recommendations and safe operating instructions for power tools and machinery must be followed. The weight of props and their sections should be minimized to reduce the possibility of lifting-associated injuries. Props, scenery and exhibits designed for outdoor use must be reviewed for wind load ratings and other outdoor exposures. Props designed for use with live loads should be appropriately rated and the built-in safety factor verified. Fire rating of the material should be considered based on the intended use, and any fire regulations that may be applicable must be followed.
Ride Operators and Maintenance Personnel
There are a wide variety of amusement park rides, including Ferris wheels, roller coasters, water flume rides, looping boats and aerial tramways. Ride operators and maintenance personnel work in areas and under conditions where there are increased risks of serious injury. The exposures include electrocution, being struck by equipment and caught in or between equipment and machinery. Besides the rides, ride and maintenance personnel must also operate and maintain the associated electrical power plants and transformers.
Precautions include an effective programme that can reduce the potential for serious injury in a lock out, tag out and block out procedure. This programme should include: personally assigned padlocks with single keys; written procedures for working on electrical circuitry, machinery, hydraulics, compressed air, water and other sources of possible energy release; and tests to ensure that the energy supply has been shut off. When more than one person is working on the same piece of equipment, each person should have and use his or her own lock.
Travelling Shows
Circuses and many amusement rides can travel from one location to another. This can be by truck for small operations, or by train for large circuses. Hazards include falls, severed body parts and possible death during erection, dismantling or transportation of equipment (figure 4). A particular problem is expedited work procedures, resulting in skipping time-consuming safety procedures, in an effort to meet play date deadlines.
Figure 4. Erecting an amusement park ride with a crane.
William Avery
Precautions include the following: Employees must be well trained, exercise caution and follow manufacturer’s safety instructions for assembly, dismantling, loading, unloading and transportation of the equipment. When animals are used, such as an elephant to pull or push heavy equipment, additional safety precautions are required. Equipment such as cables, ropes, hoists, cranes and fork-lifts should be inspected before each use. Over-the-road drivers must follow highway transportation safety guidelines. Employees will require additional training in safety and emergency procedures for train operations where animals, personnel and equipment travel together.
Bullfighting and Rodeos
Bullfighting, or the corrida as it is commonly called, is popular in Spain, Spanish-speaking countries in Latin America (especially Mexico), southern France and Portugal. It is highly ritualized, with pageants, well-defined ceremonies and colourful traditional costumes. Matadors are highly respected and often begin their training at an early age in an informal apprenticeship system.
Rodeos, on the other hand, are a more recent sports event. They are an outgrowth of skills contests between cowboys illustrating their everyday activities. Today, rodeos are formalized sports events popular in the western United States, western Canada and Mexico. Professional rodeo cowboys (and some cowgirls) travel the rodeo circuit from one rodeo to another. The most common rodeo events are bronco riding, bull riding, steer wrestling (bulldogging) and calf roping.
Bullfights. Participants in a bullfight include the matadors, their assistants (the banderilleros and picadors) and the bulls. When the bull first enters the arena from the bull pen gate, the matador attracts its attention with a series of passes with his large cape. The bull is attracted by the movement of the cape, not the colour, since bulls are colour-blind. The matador’s reputation is based on how close he gets to the horns of the bull. These fighting bulls have been bred and trained for centuries for their aggressiveness. The next part of the bullfight involves the weakening of the bull by mounted picadors placing lances in the bull, and then banderilleros, working on foot, placing barbed sticks called banderillas in the bull’s shoulder in order to lower the bull’s head for the kill.
The final stage of the fight involves the matador trying to kill the bull by inserting his sword blade between the shoulder blades of the bull into the aorta. This stage involves many formalized passes with the cape before the final kill. The greater the risks taken by the matador, the greater the acclaim, and of course the greater the risk of being gored (see figure 1). Bullfighters generally receive at least one goring per season, which could involve as many as 100 bullfights per year per matador.
Figure 1. Bullfighting.
El Pais
The primary hazard facing the matadors and their assistants is being gored or even killed by the bull. Another potential hazard is tetanus from being gored. One epidemiological study in Madrid, Spain, indicated that only 14.9% of bullfighting professionals had complete anti-tetanus vaccination, while 52.5% had suffered occupational injuries (Dominguez et al. 1987). Few precautions are taken. The mounted picadors wear steel leg armour. Otherwise, the bullfighting professionals depend on the training and skills of themselves and their horses. One essential precaution is adequate planning for onsite emergency medical care (see “Motion picture and television production” in this chapter).
Rodeos. The most hazardous common rodeo events are bronco or bull riding and steer wrestling. In bronco or bull riding, the purpose is to stay on the bucking animal for a predetermined time. Bronco riding can be either bareback or with a saddle. In steer wrestling, a rider on horseback attempts to throw the steer to the ground by diving off the horse, grabbing the bull by its horns and wrenching it to the ground. Calf roping involves roping a calf from horseback, jumping off the horse and then hog-tying the front and back legs of the calf together in the shortest possible time.
Besides the rodeo contestants, those at risk include the pickup riders or outriders, whose role is to rescue the thrown rider and capture the animal, and the rodeo clowns, whose job is to distract the animal, especially bulls, to give the thrown rider a chance to escape (figure 2). They do this while on foot and dressed in a colourful costume to attract the animal’s attention. Hazards include being trampled, being gored by the bull’s horns, injuries from being bucked off, knee injuries from jumping off the horse, elbow injuries in bronco and bull riders from holding on to the animal with one hand and facial injuries from bulls tossing their heads back. Injuries also occur from bronco or bull riders being smashed against the sides of the chute while waiting for the gate to open and the animal to be released. Severe injuries and fatalities are not infrequent. Bull riders sustain 37% of all rodeo-related injuries (Griffin et al. 1989). In particular, brain and spinal cord injuries are of concern (MMWR 1996). One study of 39 professional rodeo cowboys showed a total of 76 elbow abnormalities in 29 bronco and bull riders (Griffin et al. 1989). They concluded that the injuries were a result of constant hyperextension of the arm gripping the animal, as well as injuries in falls.
Figure 2. Rodeo clown distracting a bull from a fallen rider.
Dan Hubbell
The main way of preventing injuries lies in the skills of the rodeo cowboys, pickup riders and rodeo clowns. Well-trained horses are also essential. Taping elbows and wearing elbow pads has also been recommended for bronco and bull riding. Safety vests, mouth guards and safety helmets are rare, but becoming more accepted. Face masks have occasionally been used for bull riding. As in bullfighting, an essential precaution is adequate planning for on-site emergency medical care.
In both rodeos and bullfighting, of course, the animal keepers, feeders and so on are also at risk. For more information on this aspect, see “Zoos and aquariums” in this chapter.
Professional Sports
Sports activities involve a great number of injuries. Precautions, conditioning and safety equipment, when used properly, will minimize sports injuries.
In all sports, conditioning year round is encouraged. Bone, ligaments and muscles respond in a physiological fashion by gaining both size and strength (Clare 1990). This increases the athlete’s agility to avoid any injurious physical contact. All sports requiring weightlifting and strengthening should be under the supervision of a strength coach.
Contact Sports
Contact sports such as American football and hockey are particularly dangerous. The aggressive nature of football requires the player to strike or tackle the opposing player. The focus of the game is to possess the ball with the intent of physically striking anyone in one’s path. The equipment should be well-fitting and offer adequate protection. (figure 1). The helmet with appropriate face mask is standard and is critical in this sport (figure 2). It should not slide or twist and the straps should be applied snugly (American Academy of Orthopedic Surgeons 1991).
Figure 1. Snug fitting football pads.
MISSING
Source: American Academy of Orthopedic Surgeons 1991
Figure 2. American football helmet.
MISSING
Source: Clare 1990
Unfortunately, the helmet is sometimes used in an unsafe manner whereby the player “spears” an opponent. This can lead to cervical spine injuries and possible paralysis. It can also lead to careless play in sports like hockey, when players feel they can be more free with the use of their stick and risk slashing the face and body of the opponent.
Knee injuries are quite common in football and basketball. In minor injuries, an elastic “sleeve” (figure 3) which provides compressive support may be useful. The ligaments and cartilage of the knee are prone to stress as well as impact trauma. The classic combination of cartilage and ligamentous insult was first described by O’Donoghue (1950). An audible “pop” may be heard and felt, followed by swelling, if there are ligament injuries. Surgical intervention may be needed before the player may resume activities. A derotational brace may be worn post-operatively and by players with partial tear of the anterior cruciate ligament but with enough intact fibres able to sustain their activities. These braces must be well padded to protect the injured extremity and other players (Sachare 1994a).
Figure 3. Patella cut-out sleeve.
Huie, Bruno and Norman Scott
In hockey, the velocity of both the players and the hard hockey puck warrants the use of protective padding and helmet (figure 4). The helmet should have a face shield to prevent facial and dental injuries. Even with helmets and protective padding to vital areas, severe injuries such as fractures of extremities and spine do occur in football and hockey.
Figure 4. Padded hockey gloves.
Huie, Bruno and Norman Scott
In both American football and hockey, a complete medical kit (which includes diagnostic instruments, resuscitation equipment, immobilization devices, medication, wound care supplies, spine board and stretcher) and emergency personnel should be available (Huie and Hershman 1994). If possible, all contact sports should have this available. Radiographs should be obtained of all injuries to rule out any fractures. Magnetic resonance imaging has been found to be very helpful in determining soft tissue injuries.
Basketball
Basketball is also a contact sport, but protective equipment is not worn. The focus of the player is to have possession of the ball and their intent is not to strike the opposing players. Injuries are minimized due to the player’s conditioning and speed in averting any hard contact.
The most common injury to the basketball player are ankle sprains. Evidence of ankle sprains has been noted in about 45% of players (Garrick 1977; Huie and Scott 1995). The ligaments involved are the deltoid ligament medially and the anterior talofibular, posterior talofibular, and calcaneofibular ligaments laterally. X rays should be obtained to rule out any fractures which may occur. These radiographs should include the entire lower leg to rule out a Maisonneuve fracture (VanderGriend, Savoie and Hughes 1991). In the chronically sprained ankle, use of a semi-rigid ankle stirrup will minimize further insult to the ligaments (figure 5).
Figure 5. Rigid ankle stirrup.
AirCast
Finger injuries may result in ruptures of the supporting ligamentous structures. This can result in a Mallet finger, Swann Neck deformity and Boutonierre deformity (Bruno, Scott and Huie 1995). These injuries are quite common and are due to direct trauma with the ball, other players and the backboard or rim. Prophylactic taping of ankles and fingers helps minimize any accidental twisting and hyperextension of the joints.
Facial injuries (lacerations) and fractures of the nose due to contact with opponents’ flailing arms or bony prominences, and contact with the floor or other stationary structures have been encountered. A clear light-weight protective mask may help in minimizing this type of injury.
Baseball
Baseballs are extremely hard projectiles. The player must always be cognizant of the ball not only for safety reasons but for the strategy of the game itself. Batting helmets for the offensive player, and chest protector and catcher’s mask/helmet (figure 6). for the defensive player are required protective equipment. The ball is hurled at times in excess of 95 mph, sometimes resulting in bone fractures. Any head injuries should have a full neurological work-up, and, if loss of consciousness is present, radiographs of the head should be taken.
Figure 6. Protective cather's mask.
MISSING
Huie, Bruno and Norman Scott
Soccer
Soccer can be a contact sport resulting in trauma to the lower extremity. Ankle injuries are very common. The protection that would minimize this would be taping and the use of a semi-rigid ankle stirrup. It has been found that the effectiveness of the taped ankle diminishes after about 30 minutes of vigorous activities. Tears of the anterior cruciate ligament of the knee are often encountered and most likely will require a reconstructive procedure if the player wishes to continue participating in this sport. Anterior medial tibial stress syndrome (shin splints) is extremely common. The hypothesis is that there may be an inflammation to the periosteal sleeve around the tibia. In extreme situations, a stress fracture may occur. The treatment requires rest for 3 to 6 weeks and the use of non-steroidal anti-inflammatory drugs (NSAID), but high-level and professional-level players tend to compromise the treatment once the symptoms diminish as early as 1 week and thus go back to the impact activity. Hamstring pulls and groin pulls are common in the athletes who do not permit enough time to warm and stretch the musculature of the legs. Direct trauma to the lower extremities, particularly the tibia, may be minimized with the use of anterior shin guards.
Skiing
Skiing as a sport does not require any protective equipment, although goggles are encouraged to prevent eye injuries and to filter out the sun’s glare off the snow. Ski boots offer a rigid support for the ankles and have a “quick-release” mechanism in the event of a fall. These mechanisms, although helpful, are susceptible to circumstances of the fall. During the winter season, many injuries to the knee resulting in ligament and cartilage damage are encountered. This is found in the novice as well as the seasoned skier. In professional downhill skiing, helmets are required to protect the head due to the velocity of the athlete and the difficulty of stopping in the event the trajectory and direction are miscalculated.
Martial Arts and Boxing
Martial arts and boxing are hard contact sports, with little or no protective equipment. The gloves used on the professional boxing level are, however, weighted, which increases their effectiveness. Head guards at the amateur level help soften the impact of the blow. As with skiing, conditioning is extremely important. Agility, speed and strength minimize the combatant’s injuries. The blocking forces are deflected more than absorbed. Fractures and soft tissue insults are very common in this sport. Similar to volleyball, the repetitive trauma to the fingers and carpal bones of the hand results in fractures, subluxation, dislocation and ligamentous disruptions. Taping and padding of the hand and wrist may provide some support and protection, but this is minimal. Studies have shown that long-term brain damage is a serious concern for boxers (Council on Scientific Affairs of the American Medical Association 1983). Half of a group of professional boxers with more than 200 fights each had neurological signs consistent with traumatic encephalopathy.
Horse Racing
Horse racing at the professional and amateur levels requires a riding helmet. These helmets offer some protection for head injuries from falls, but they offer no attachment for the neck or spine. Experience and common sense help minimize falls, but even seasoned riders can sustain serious injuries and possibly paralysis if they land on their head. Many jockeys today also wear protective vests since being trampled under horses’ hooves is a major risk in falls and has resulted in fatalities. In harness racing, where horses pull two-wheeled carts called sulkies, collisions between sulkies has resulted in multiple pile-ups and serious injuries. For hazards to stable hands and others involved in handling the horses, see the chapter Livestock rearing.
First Aid
As a general rule, immediate icing (figure 7), compression, elevation and NSAIDs following most injuries will suffice. Pressure dressings should be applied to any open wounds, followed by an evaluation and suturing. The player should be removed from the game immediately to prevent any blood-borne contamination to other players (Sachare 1994b). Any head trauma with loss of consciousness should have a mental status and neurological work-up.
Figure 7. Cold compressive therapy.
MISSING
AirCast
Physical Fitness
Professional athletes with asymptomatic or symptomatic cardiac conditions may be hesitant in disclosing their pathology. In recent years, several professional athletes have been found to have cardiac problems that resulted in their deaths. The economic incentives of playing professional-level sports may inhibit athletes from disclosing their conditions for fear of disqualifying themselves from strenuous activities. Carefully obtained past medical and family histories followed by EKG and treadmill stress tests prove to be valuable in detecting those who are at risk. If a player is identified as a risk and still wishes to continue competing regardless of the medical-legal issues, emergency resuscitative equipment and trained personnel must be present at all practices and games.
Referees are present not only to keep the flow of the game going but to protect the players from hurting themselves and others. Referees, for the most part, are objective and have the authority to suspend any activity should an emergency condition arise. As with all competitive sports, emotion and adrenaline are flowing high; the referees are present to help the players harness these energies in a positive fashion.
Proper conditioning, warm-up and stretching prior to engaging in any competitive activity is vital to the prevention of strains and sprains. This procedure enables the muscles to perform at peak efficiency and minimizes the possibilities of strains and sprains (micro-tears). Warm-ups may very well be a simple jog or callisthenics for about 3 to 5 minutes followed by gentle stretching out of the extremities for an additional 5 to 10 minutes. With the muscle at its peak efficiency, the athlete may be able to quickly manoeuvre away from a threatening position.
More...
Sex Industry
The sex industry is a major industry both in developing countries, where it is a major source of foreign currency, and in industrialized countries. The two main divisions of the sex industry are (1) prostitution, which involves the direct exchange of a sexual service for money or other means of economic compensation and (2) pornography, which involves the performance of sex-related tasks, sometimes involving two or more people, for still photographs, in motion pictures and videotapes, or in a theatre or nightclub, but does not include direct sexual activity with the paying client. The line between prostitution and pornography is not very clear, however, as some prostitutes restrict their work to erotic acting and dance for private clients, and some workers in the pornography industry go beyond display to engaging in direct sexual contact with members of the audience, for example, in strip- and lap-dancing clubs.
The legal status of prostitution and pornography varies from one country to another, ranging from complete prohibition of the sex-money exchange and the businesses in which it takes place, as in the United States; to decriminalization of the exchange itself but prohibition of the businesses, as in many European countries; to toleration of both independent and organized prostitution, for example, in the Netherlands; to regulation of the prostitute under public health law, but prohibition for those who fail to comply, as in a number of Latin American and Asian countries. Even where the industry is legal, governments have remained ambivalent and few, if any, have attempted to use occupational safety and health regulations to protect the health of sex workers. However, since the early 1970s, both prostitutes and erotic performers have been organizing in many countries (Delacoste and Alexander 1987; Pheterson 1989), and have increasingly addressed the issue of occupational safety as they attempt to reform the legal context of their work.
A particularly controversial aspect of sex work is the involvement of young adolescents in the industry. There is not enough space to discuss this at any length here, but it is important that solutions to the problems of adolescent prostitution be developed in the context of responses to child labour and poverty, in general, and not as an isolated phenomenon. A second controversy has to do with the extent to which adult sex work is coerced or the result of individual decision. For the vast majority of sex workers, it is a temporary occupation, and the average worklife, worldwide, is from 4 to 6 years, including some who work only for a few days or intermittently (e.g., between other jobs), and others who work for 35 years or more. The primary factor in the decision to do sex work is economics, and in all countries, work in the sex industry pays much better than other work for which extensive training is not required. Indeed, in some countries, the higher-paid prostitutes earn more than some physicians and attorneys. It is the conclusion of the sex workers’ rights movement that it is difficult to establish issues like consent and coercion when the work itself is illegal and heavily stigmatized. The important thing is to support sex workers’ ability to organize on their own behalf, for example, in trade unions, professional associations, self-help projects and political advocacy organizations.
Hazards and Precautions
Sexually transmitted diseases (STDs). The most obvious occupational hazard for sex workers, and the one which has received the most attention historically, is STDs, including syphilis and gonorrhoea, chlamydia, genital ulcer disease, trichomonas and herpes, and, more recently, the human immunodeficiency virus (HIV) and AIDS.
In all countries, the risk of infection with HIV and other STDs is greatest among the lowest-income sex workers, whether on the street in the industrial countries, in low-income brothels in Asia and Latin America or in residential compounds in impoverished communities in Africa.
In industrialized countries, studies have found HIV infection among female prostitutes to be associated with injecting drug use by either the prostitute or her ongoing personal partner, or with the prostitute’s use of “crack”, a smokeable form of cocaine—not with the number of clients or with prostitution per se. There have been few if any studies of pornography workers, but it is likely to be similar. In developing countries, the primary factors are less clear, but may include a higher prevalence of untreated conventional STDs, which some researchers think facilitate transmission of HIV, and a reliance on informal street vendors or poorly equipped clinics for treatment of STDs, if treatment involves injections with unsterile needles. Injection of recreational drugs is also associated with HIV infection in some developing countries (Estébanez, Fitch and Nájera 1993). Among male prostitutes, HIV infection is more often associated with homosexual activity, but is also associated with injecting drug use and sex in the context of drug dealing.
Precautions involve the consistent use of latex or polyurethane condoms for fellatio and vaginal or anal intercourse, where possible with lubricants (water-based for latex condoms, water or oil-based for polyurethane condoms), latex or polyurethane barriers for cunnilingus and oral-anal contact and gloves for hand-genital contact. While condom use has been increasing among prostitutes in most countries, it is still the exception in the pornography industry. Women performers sometimes use spermicides to protect themselves. However, while the spermicide nonoxynol-9 has been shown to kill HIV in the laboratory, and reduces the incidence of conventional STD in some populations, its efficacy for HIV prevention in actual use is far less clear. Moreover, the use of nonoxynol-9 more than once a day has been associated with significant rates of vaginal epithelial disruption (which could increase the female sex worker’s vulnerability to HIV infection) and sometimes an increase in vaginal yeast infections. No one has studied its use for anal sex.
Access to sex worker–sensitive health care is also important, including care for other health problems, not just STDs. Traditional public health approaches that involve mandatory licensing or registration, and regular health examinations, have not been effective in reducing the risk of infection for the workers, and are contrary to World Health Organization policies that oppose mandatory testing.
Injuries. Although there have not been any formal studies of other occupational hazards, anecdotal evidence suggests that repetitive stress injuries involving the wrist and shoulder are common among prostitutes who do “hand jobs”, and jaw pain is sometimes associated with performing fellatio. In addition, street prostitutes and erotic dancers may develop foot, knee and back problems related to working in high heels. Some prostitutes have reported chronic bladder and kidney infections, due to working with a full bladder or not knowing how to position oneself to prevent deep penetration during vaginal intercourse. Finally, some groups of prostitutes are very vulnerable to violence, especially in countries where the laws against prostitution are heavily enforced. The violence includes rape and other sexual assault, physical assault and murder, and is committed by police, clients, sex work business managers and domestic partners. The risk of injury is greatest among younger, less experienced prostitutes, especially those who begin working during adolescence.
Precautions include ensuring that sex workers are trained in the least stressful way to perform different sexual acts to prevent repetitive stress injuries and bladder infections, and self-defence training to reduce vulnerability to violence. This is particularly important for young sex workers. In the case of violence, another important remedy is to increase the willingness of police and prosecuting attorneys to enforce the laws against rape and other violence when the victims are sex workers.
Alcohol and drug use. When prostitutes work in bars and nightclubs, they are often required by management to encourage clients to drink, as well as to drink with clients, which can be a serious hazard for individuals who are vulnerable to alcohol addiction. In addition, some begin to use drugs (e.g., heroin, amphetamines and cocaine) to help deal with the stress of their work, while others used drugs prior to beginning sex work, and turned to sex work in order to pay for their drugs. With injecting drug use, vulnerability to HIV infection, hepatitis and a range of bacterial infections increases if drug users share needles.
Precautions include workplace regulations to ensure that prostitutes can drink non-alcoholic beverages when with clients, the provision of sterile injection equipment and, where possible, legal drugs to sex workers who inject drugs, and increasing access to drug and alcohol addiction treatment programmes.
Nightlife Entertainment
This grouping of extremely varied and miscellaneous entertainment occupations includes work locations such as bars, nightclubs, discotheques, dancehalls, topless bars, go-go clubs, casinos, bingo and gambling parlours, and pool halls, as well as cinema theatres. Occupations include bartenders, waiters, hostess/host, card dealers, bouncers (security personnel), musicians, dancers, strippers and movie projectionists. Hotels and restaurants often have night entertainment venues within them. There are several categories of hazards common to almost all nightlife entertainment workers.
Shiftwork. Entertainment workers such as bartenders may have routine nightshifts, while musicians working in a club may have irregular shifts. Various physiological, psychological and social effects are associated with nightshift or irregular shiftwork. Often bartenders and cocktail waitresses work shifts that are 10 to 14 hours long.
Violence. Workplace violence is a major problem in establishments that serve alcohol, as well as in gambling enterprises. The United States National Institute for Occupational Safety and Health studied homicide rates among workers in the United States during 1980–1989. They found bartenders to be ranked the eighth highest occupational group, with a homicide rate of 2.1 per 100,000, compared to the average homicide rate of 0.7 homicides per 100,000 for all workers. The exchange of money with the public, often working alone or in small numbers and working late at night or early in the morning, as well as working in high-crime areas, were all found to be factors related to the high rate. Preventive measures for lowering the violence rate include increasing the visibility of the workplace, such as by installing better lighting. The amounts of cash on hand should be minimized and signs posted which clearly indicate that little or no cash in on hand. Silent alarms and hidden cameras can be installed and workers can be trained in non-violent response techniques for emergencies, such as robberies. Arrangements can be made for having routine police checks on workers’ safety, and workers may even be provided bullet-proof barriers and vests if needed.
Fire Safety. Many smaller nightclubs, dancehalls, movie theatres and bars may not meet with local assembly, building or fire code requirements. There have been several high-profile fatal fires in urban clubs, which are often more crowded than permissible by law. Adherence to fire and assembly codes, a fire safety and emergency programme and availability of fire extinguishers and training in their use, as well as other emergency procedures, can reduce risks (Malhotra 1984).
Second-hand smoke. In many locations where there is nightlife entertainment, second-hand cigarette smoke is a significant hazard. The risk of lung cancer and heart disease is increased with exposure to cigarette smoke in the workplace (NIOSH 1991). The risk of laryngeal cancer, also associated with tobacco use, is elevated in bartenders and food servers. Often, smaller bars and night entertainment clubs do not have adequate ventilation for cigarette smoke. In many countries, efforts are being made to regulate exposure to second-hand smoke; but such governmental restriction are not universal. Ventilation and air cleaning devices, such as electrostatic precipitators, as well as the restriction of smoking will decrease exposure.
Alcohol and drug abuse. Working in certain occupations has been found to be correlated to increased alcohol consumption, and one suggestive study has found that death from liver cirrhosis, a disease associated with alcohol consumption, is elevated among waiters, bartenders and musicians (Olkinuora 1984). In nightlife entertainment work there is easy access to alcohol and a social pressure to drink. Often there is isolation from a usual homelife because of working during the night shift or because of touring through different locations. Poor management and lack of supervision can contribute to the problem. Performance anxiety (in the case of musicians), or the need to stay awake during night shift, as well as the fact that patrons may be apt to abuse drugs, can also increase the risks for drug abuse among workers in the nightlife environment. The risks for alcohol and drug abuse intervention programmes can be decreased by well-designed training programmes which assist workers dealing with these problems.
Noise. Excessive noise exposure can be a problem in bars and restaurants. While the problem of noise is obvious in discotheques and music clubs which feature excessively high sound levels, noise overexposure can also be a problem in bars and other locations in which there is only pre-recorded or jukebox music, which can also be played very loudly. Sound levels of over 100 decibels (dB) are common in discos (Tan, Tsang and Wong 1990). One survey of 55 nightclubs in New Jersey in the United States revealed noise levels from 90 to 107 dB. Placement of speakers and jukeboxes away from work stations can reduce worker exposure, and acoustic baffling and barriers can also help. In some cases a general reduction in volume may be possible. If possible, wearing ear plugs can reduce worker exposure.
Dermatitis. Nightlife workers share many skin problems with food handlers. Skin infections, such as candidiasis of the hands, can arise from extensive contact with soiled glassware, washing and cleaning fluids and water. Automatic dish- and glass-washing equipment can address this problem. Food sensitivities are also known, such as contact dermatitis in a bartender with a sensitivity to lemon and lime peels (Cardullo, Ruszkowski and Deleo 1989). Bartenders have developed eczema from handling mint. Other specific sensitivities leading to dermatitis have been reported, such as dermatitis in a professional blackjack dealer who developed a sensitivity to chromate salts used in the green dye for the felt on gaming tables (Fisher 1976).
Musculoskeletal problems. Repetitive motion injuries and other problems associated with workplace design can be found among nightlife workers. For example, musicians and dancers are prone to specific musculoskeletal problems, as discussed elsewhere in this chapter. Bartenders who continually wash glassware and card dealers who must shuffle and deal cards for games in casinos have been found to suffer from carpal tunnel syndrome. More frequent breaks during shifts, in addition to job and task redesign, may reduce these hazards. Bartenders, cocktail waitresses, casino dealers and food servers often must stand for their entire workshift, which may be 10 to 12 hours long. Excessive standing can result in back strain and other circulatory and musculoskeletal problems. Corrugated rubber floor mats and comfortable, supportive shoes can lessen the strain.
Film projection booths. Projection booths are small and problems of excessive heat can arise. Older film projection booths use a carbon arc light source to project images, while more modern booths employ xenon lamps. In either case, ultraviolet (UV) radiation and ozone gas exposure can occur. Levels of ozone that ranged from 0.01 to 0.7 parts per million have been reported. The ozone is generated by the UV radiation, which ionizes oxygen found in the air. (Maloy 1978). In addition, use of carbon arc light sources is associated with rare earth metal fumes, carbon dioxide, carbon monoxide, ozone, electromagnetic radiation (EMF) and heat exposures. Local exhaust ventilation is required.
Special effects. Many different special effects can be used in clubs and discotheques, including, various smokes and fogs, laser light shows and even pyrotechnics. Adequate training in laser operation and safety and other special effects is necessary. UV light emitted from “black” lights may pose additional hazards, especially to strippers and go-go dancers (Schall et al. 1969). It has been suggested that a glass barrier between the black light and the performers would help decrease the hazards. These effects are described in more detail in other articles in this chapter.
Environmental Protection and Public Health Issues
Visual Arts
The visual arts produce a wide range of potential environmental problems and raise a number of public health issues. The visual arts use a broad range of chemicals and techniques which can create air and water pollution problems similar to that of the comparable industrial processes, only on a much smaller scale.
Hazardous waste produced by artists can include: (1) toxic and extremely toxic wastes, including solvents, lead compounds, chromates and cyanide solutions; (2) flammable waste, including flammable and combustible liquids (e.g., rags soaked with oil and turpentine), oxidizing substances such as potassium chlorate and dichromates, and ignitable compressed gases; (3) corrosive waste, including acids with a pH less than 2 and alkalis with a pH greater than 12; and (4) reactive wastes, such as organic peroxides, cyanide solutions and sulphide solutions. Artists and artisans are less likely, however, to know how to dispose of this waste or even to know what is hazardous. The most common method of waste disposal for artists is pouring down the sink or onto the ground, tossing in the garbage or evaporation. Although the individual amounts of pollutants are small, cumulatively they can result in significant pollution.
In the United States and Canada and many other countries, artists working in their homes are usually exempted from industrial hazardous waste regulations under a household hazardous waste exemption. Many localities, however, do provide special household hazardous waste days when households can bring their hazardous waste to a central site for collection. However, even in countries which do regulate artists as small businesses, there is little enforcement of hazardous waste regulations for these cottage industries.
Types of waste management methods available include many of the same ones used by industry, including source reduction, waste separation and concentration, recycling, energy and material recovery, incineration or treatment, and secure land disposal. Some of these methods are more available to artists than others.
The best way of managing hazardous waste is to actually eliminate or minimize its production by substituting materials which are less toxic—for example, using lead-free glazes instead of leaded glazes in pottery and enamelling, and using water-based screen printing inks and other coating materials instead of solvent-based ones.
Separating hazardous materials from non-hazardous materials—for example, separating solvent-based paints and water-based paints—can be a simple method to reduce the amount of hazardous waste and prevent it from contaminating regular garbage.
Traditional industrial methods of concentration, such as evaporation of large volumes of photographic wastes, are usually not feasible for artists.
Recycling can involve the reusing of materials (such as solvents used for oil painting cleanup) by the individual, or the passing of unwanted materials to someone else who can use them. Large printmaking facilities, which generate many solvent- or oil-soaked rags, can contract for laundering and reuse them.
Treatment can involve several processes. The most common one used by artists is neutralization of acids or alkaline solutions. Incineration is usually restricted to burning wood dust. Evaporation of solvents is also commonly done. This reduces the amount of hazardous waste potentially contaminating water supplies, although it does contaminate the atmosphere to some degree.
The least favourable option is secure land disposal in a proper hazardous waste disposal site. This is usually not a viable option for artists, especially in developing countries.
A public health issue that is common to many of the visual arts is the problem of the exposure of children to toxic chemicals found in many art materials, including those intended for use by children. Examples include solvents in permanent felt-tip markers and lead in ceramic glazes. Children and other family members can be exposed to hazardous substances and conditions in the home.
A widespread problem in many countries is lead poisoning, including fatalities from cooking and storing food in containers that have been made with lead-containing pottery glazes. In the commercial industry, the problem of lead leaching from glazed pottery has been mostly eliminated through government regulations and good quality control. The World Health Organization has standards for lead and cadmium leaching from pottery intended for food and drink use. The cost of the testing required, however, is not feasible for craft potters, and therefore craft potters should use only lead-free glazes for food and drink containers.
Performing and Media Arts
Theatres, scenery shops and motion picture and television production areas also can produce hazardous waste, since they use many of the same chemicals as are used in the visual arts. The same solutions apply. In particular, the widespread shift from solvent-based paints to water-based paints has greatly decreased the amount of solvent pollution.
One of the main public health issues for theatres (and other places of public assembly) is fire safety. Many theatres and other performance spaces, especially small, non-commercial ones, do not meet applicable fire codes and are dangerously overcrowded. There have been many disastrous fires with numerous fatalities in the performing arts. The use of fogs and smokes for special effects in theatre and opera can also pose the risk of asthma attacks in asthmatic audience members in the front of the theatre if the building does not have adequate exhaust ventilation to prevent the fog or smoke from affecting the audience.
Entertainment Industry
Entertainment industries such as amusement and theme parks can face all the solid waste and other pollution problems of a small town. Zoos, circuses and other types of entertainment involving animals can have many of the same pollution problems as livestock raising, but on a smaller scale.
A public health concern at all entertainment events where food is sold is the possibility of developing salmonella poisoning, hepatitis or other diseases if there are not adequate public health controls.
Crowd control is another major public health concern in many large entertainment events, such as certain types of popular concerts and sports events. Widespread use of drugs and alcohol, overcrowding, allowing extensive standing room (festival seating) and lack of adequate preplanning have led to many incidents involving riots and panic, with resulting multiple injuries and fatalities. In addition, lack of adequate construction standards has caused fires and collapses of seating areas in several countries. There is a need for better regulations and provision of proper crowd control measures in these situations.
Visitors to parks and zoos can also present hazards to themselves. There have been many incidents where zoo visitors have been maimed or killed after entering animal enclosures. Visitors who get too close to wild animals in the parks have also experienced attacks, many of which have been fatal. The problems of inexperienced parks visitors getting lost, caught in storms, or falling from mountains is also a constant public health risk which can use up extensive resources for rescue.
The sex industry, especially prostitution, is particularly infamous for the possibility of patrons being robbed and possibly contracting sexually transmitted diseases. This is particularly true in countries where prostitution is not legally controlled. Criminal activities are often associated with prostitution.
Health Care: Its Nature and its Occupational Health Problems
Health care is a labour intensive industry and, in most countries, health care workers (HCWs) constitute a major sector of the workforce. They comprise a wide range of professional, technical and support personnel working in a large variety of settings. In addition to health professionals, laboratory technicians, pharmacists, social workers and others involved in clinical services, they include administrative and clerical personnel, housekeeping and dietary staff, laundry workers, engineers, electricians, painters and maintenance workers who repair and refurbish the building and the equipment it contains. In contrast with those providing direct care, these support workers usually have only casual, incidental contact with patients.
HCWs represent diverse educational, social and ethnic levels and are usually predominantly female. Many, particularly in home care, are employed in entry-level positions and require considerable basic training. Table 1 lists samples of health care functions and associated occupations.
Table 1. Examples of health care functions and associated occupations
|
Functions |
Occupational category * |
Specific occupations |
|
Direct patient care |
Health-diagnosing occupations |
Physicians |
|
Technical support |
Health technicians |
Clinical laboratory technicians |
|
Services |
Health services |
Dental assistants |
|
Administrative support |
Clerical services |
Billing clerks |
|
Research |
Scientific occupations |
Scientists and research |
* Occupational categories are, in part, adapted from those used by the US Department of Labor, Bureau of Labor Statistics.
A segment of the health sector (unfortunately, often too small and under-resourced in most communities) is devoted to direct and indirect preventive services. The major focus of the health care industry, however, is the diagnosis, treatment and care of the sick. This creates a special set of dynamics, for the sick exhibit varying levels of physical and emotional dependencies that set them apart from the customers in such personal services industries as, for example, retail trade, restaurants and hotels. They require, and traditionally receive, special services and considerations, often on an emergency basis, provided frequently at the expense of the HCWs’ personal comfort and safety.
Reflecting their size and numbers of employees, acute and long-term care facilities constitute perhaps the most prominent elements in the health care industry. They are supplemented by outpatient clinics, “surgicenters” (facilities for outpatient surgery), clinical and pathological laboratories, pharmacies, x-ray and imaging centres, ambulance and emergency care services, individual and group offices, and home care services. These may be located within a hospital or operated elsewhere under its aegis, or they may be free-standing and operated independently. It should be noted that there are profound differences in the way health services are delivered, ranging from the well-organized, “high tech” care available in urban centres in developed countries to the underserved areas in rural communities, in developing countries and in inner-city enclaves in many large cities.
Superimposed on the health care system is a massive educational and research establishment in which students, faculty, researchers and support staffs often come in direct contact with patients and participate in their care. This comprises schools of medicine, dentistry, nursing, public health, social work and the variety of technical disciplines involved in health care.
The health care industry has been undergoing profound changes during the past few decades. Ageing of the population, especially in developed countries, has amplified the use of nursing homes, domiciliary facilities and home care services. Scientific and technological developments have not only led to the creation of new types of facilities staffed by new classes of specially-trained personnel, but they have also de-emphasized the role of the acute care hospital. Now, many services requiring inpatient care are being provided on an ambulatory basis. Finally, fiscal constraints dictated by the continuing escalation of health care costs have been reconfiguring the health care industry, at least in developing countries, resulting in pressure for cost-containment to be achieved through changes in the organization of health care services.
HCWs who are in direct contact with the sick, wherever they work, are exposed to a number of unique hazards. They face the risk of acquiring infections from the patients they serve, as well as the risk of musculoskeletal injuries when lifting, transferring or restraining them. Support staff not directly involved in patient care (e.g., laundry and housekeeping and materials handling workers) are not only routinely exposed to chemicals, such as cleaning agents and disinfectants of industrial strength, but are also exposed to biological hazards from contaminated linens and wastes (see figure 1). There is also the ethos of health care which, especially in emergency situations, requires HCWs to put the safety and comfort of their patients above their own. Coping with the stress of therapeutic failures, death and dying often takes its toll in worker burnout. All this is compounded by shift work, deliberate or inadvertent understaffing and the necessity of catering to the sometimes unreasonable demands from patients and their families. Finally, there is the threat of abuse and violence from patients, particularly when the job requires them to work alone or takes them into unsafe areas. All these are described in greater detail in other articles in this chapter and elsewhere in this Encyclopaedia.
Figure 1. Handling contaminated biological material
Health Sciences Centre, Winnipeg, Manitoba, Canada
The US National Institute for Occupational Safety and Health (NIOSH) reported that needle punctures, musculoskeletal sprains and back injuries probably were the most common injuries in the health care industry (Wugofski 1995). The World Health Organization (WHO) Conference on Occupational Hazards in 1981 identified as its five main areas of concern:
- cuts, lacerations and fractures
- back injuries
- lack of personal safety equipment
- poor maintenance of mechanical and electrical systems
- assault by patients.
Are they health care workers, too?
Often overlooked when considering the safety and well-being of health care workers are students attending medical, dental, nursing and other schools for health professionals and volunteers serving pro bono in healthcare facilities. Since they are not “employees” in the technical or legal sense of the term, they are ineligible for workers’ compensation and employment-based health insurance in many jurisdictions. Health care administrators have only a moral obligation to be concerned about their health and safety.
The clinical segments of their training bring medical, nursing and dental students into direct contact with patients who may have infectious diseases. They perform or assist in a variety of invasive procedures, including taking blood samples, and often do laboratory work involving body fluids and specimens of urine and faeces. They are usually free to wander about the facility, entering areas containing potential hazards often, since such hazards are rarely posted, without an awareness of their presence. They are usually supervised very loosely, if at all, while their instructors are often not very knowledgeable, or even interested, in matters of safety and health protection.
Volunteers are rarely permitted to participate in clinical care but they do have social contacts with patients and they usually have few restrictions with respect to areas of the facility they may visit.
Under normal circumstances, students and volunteers share with health care workers the risks of exposure to potentially harmful hazards. These risks are exacerbated at times of crisis and in emergencies when they step into or are ordered into the breech. Clearly, even though it may not be spelled out in laws and regulations or in organizational procedure manuals, they are more than entitled to the concern and protection extended to “regular” health care workers.
Leon Warshaw
Biological Hazards
Biological hazards, which pose a risk for infectious disease, are common throughout the world, but they are particularly problematic in developing countries. While the hepatitis B virus (HBV) is a nearly universal threat to HCWs, it is particularly important in African and Asian countries where this virus is endemic. As discussed later in this chapter, the risk of HBV transmission after percutaneous exposure to hepatitis B surface antigen (HBsAg) positive blood is approximately 100-fold higher than the risk of transmitting the human immunodeficiency virus (HIV) through percutaneous exposure to HIV-infected blood (i.e., 30% versus 0.3%). Nonetheless, there has indeed been an evolution of concern regarding parenteral exposure to blood and body fluids from the pre-HIV to the AIDS era. McCormick et al. (1991) found that the annual reported incidents of injuries from sharp instruments increased more than threefold during a 14-year period and among medical house officers the reported incidents increased ninefold. Overall, nurses incur approximately two-thirds of the needlestick injuries reported. Yassi and McGill (1991) also noted that nursing staff, particularly nursing students, are at highest risk for needlestick injuries, but they also found that approximately 7.5% of medical personnel reported exposures to blood and body fluids, a figure that is probably low because of underreporting. These data were consistent with other reports which indicated that, while there is increased reporting of needlesticks reflecting concerns about HIV and AIDS, certain groups continue to underreport. Sterling (1994) concludes that underreporting of needlestick injuries ranges from 40 to 60%.
Certain risk factors clearly enhance the likelihood of transmission of bloodborne diseases; these are discussed in the article “Prevention of occupational transmission of bloodborne pathogens”. Frequent exposure has indeed been associated with high seroprevalence rates of hepatitis B among laboratory workers, surgeons and pathologists. The risk of hepatitis C is also increased. The trend towards greater attention to prevention of needlestick injuries is, however, also noteworthy. The adoption of universal precautions is an important advance. Under universal precautions, it is assumed that all blood-containing fluid is potentially infectious and that appropriate safeguards should always be invoked. Safe disposal containers for needles and other sharp instruments are increasingly being placed in conveniently accessible locations in treatment areas, as illustrated in figure 2. The use of new devices, such as the needle-less access system for intravenous treatment and/or blood sampling has been shown to be a cost-effective method of reducing needlestick injuries (Yassi and McGill 1995).
Figure 2. Disposal container for sharp instruments and devices
Health Sciences Centre, Winnipeg, Manitoba, Canada
Blood and body fluids are not the only source of infection for HCWs. Tuberculosis (TB) is also on the rise again in parts of the world where previously its spread had been curtailed and, as discussed later in this chapter, is a growing occupational health concern. In this, as in other nosocomial infections, such concern is heightened by the fact that so many of the organisms involved have become drug-resistant. There is also the problem of new outbreaks of deadly infectious agents, such as the Ebola virus. The article “Overview of infectious diseases” summarizes the major infectious disease risks for HCWs.
Chemical Hazards
HCWs are exposed to a wide variety of chemicals, including disinfectants, sterilants, laboratory reagents, drugs and anaesthetic agents, to name just a few of the categories. Figure 3 shows a storage cabinet in an area of a large hospital where prosthetics are fabricated and clearly illustrates the vast array of chemicals that are present in health care facilities. Some of these substances are highly irritating and may also be sensitizing. Some disinfectants and antiseptics also tend to be quite toxic, also with irritating and sensitizing propensities that may induce skin or respiratory tract disease. Some, like formaldehyde and ethylene oxide, are classified as mutagens, teratogens and human carcinogens as well. Prevention depends on the nature of the chemical, the maintenance of the apparatus in which it is used or applied, environmental controls, worker training and, in some instances, the availability of correct personal protective equipment. Often such control is straightforward and not very expensive. For example, Elias et al. (1993) showed how ethylene oxide exposure was controlled in one health care facility. Other articles in this chapter address chemical hazards and their management.
Figure 3. Storage cabinet for hazardous chemicals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Physical Hazards and the Building Environment
In addition to the specific environmental contaminants faced by HCWs, many health care facilities also have documented indoor air quality problems. Tran et al. (1994), in studying symptoms experienced by operating room personnel, noted the presence of the “sick building syndrome” in one hospital. Building design and maintenance decisions are, therefore, extremely important in health care facilities. Particular attention must be paid to correct ventilation in specific areas such as laboratories, operating rooms and pharmacies, the availability of hoods and avoidance of the insertion of chemical-laden fumes into the general air-conditioning system. Controlling the recirculation of air and using special equipment (e.g., appropriate filters and ultraviolet lamps) is needed to prevent the transmission of air-borne infectious agents. Aspects of the construction and planning of health care facilities are discussed in the article “Buildings for health care facilities”.
Physical hazards are also ubiquitous in hospitals (see “Exposure to physical agents” in this chapter). The wide variety of electrical equipment used in hospitals can present an electrocution hazard to patients and staff if not properly maintained and grounded (see figure 4). Especially in hot and humid environments, heat exposure may present a problem to workers in such areas as laundries, kitchens and boiler rooms. Ionizing radiation is a special concern for staff in diagnostic radiology (i.e., x ray, angiography, dental radiography and computerized axial tomography (CAT) scans) as well as for those in therapeutic radiology. Controlling such radiation exposures is a routine matter in designated departments where there is careful supervision, well-trained technicians and properly shielded and maintained equipment, but it can be a problem when portable equipment is used in emergency rooms, intensive care units and operating rooms. It can also be a problem to housekeeping and other support staff whose duties take them into areas of potential exposure. In many jurisdictions these workers have not been properly trained to avoid this hazard. Exposure to ionizing radiation may also present a problem in diagnostic and therapeutic nuclear medicine units and in preparing and distributing doses of radioactive pharmaceuticals. In some cases, however, radiation exposure remains a serious problem (see the article “Occupational health and safety practice: The Russian experience” in this chapter).
Figure 4. Electrical equipment in hospital
Health Sciences Centre, Winnipeg, Manitoba, Canada
Contradicting the prevailing impression of hospitals as quiet workplaces, Yassi et al. (1991) have documented the surprising extent of noise-induced hearing loss among hospital workers (see table 2). The article “Ergonomics of the physical work environment” in this chapter offers useful recommendations for controlling this hazard, as does table 3.
Table 2. 1995 integrated sound levels
|
Area monitored |
dBA (lex) Range |
|
Cast room |
76.32 to 81.9 |
|
Central energy |
82.4 to 110.4 |
|
Nutrition and food services (main kitchen) |
|
|
Housekeeping |
|
|
Laundry |
|
|
Linen service |
76.3 to 91.0 |
|
Mailroom |
|
|
Maintenance |
|
|
Materials handling |
|
|
Print shop |
|
|
Rehabilitation engineering |
|
Note: “Lex” means the equivalent sound level or the steady sound level in dBA which, if present in a workplace for 8 hours, would contain the same acoustic energy.
Table 3. Ergonomic noise reduction options
|
Work area |
Process |
Control options |
|
Central energy |
General area |
Enclose the source |
|
Dietetics |
Pot washer |
Automate process |
|
Housekeeping |
Burnishing |
Purchasing criteria |
|
Laundry |
Dryer/washer |
Isolate and reduce vibration |
|
Mailroom |
Tuberoom |
Purchasing criteria |
|
Maintenance |
Various equipment |
Purchasing criteria |
|
Materiel handling and |
Carts |
Maintenance |
|
Print shop |
Press operator |
Maintenance |
|
Rehabilitation |
Orthotics |
Purchasing criteria |
By far the most common and most costly type of injury faced by HCWs is back injury. Nurses and attendants are at greatest risk of musculoskeletal injuries due to the large amount of patient lifting and transferring that their jobs require. The epidemiology of back injury in nurses was summarized by Yassi et al. (1995a) with respect to one hospital. The pattern they observed mirrors those that have been universally reported. Hospitals are increasingly turning to preventive measures which may include staff training and the use of mechanical lifting devices. Many are also providing up-to-date diagnostic, therapeutic and rehabilitation health services that will minimize lost time and disability and are cost-effective (Yassi et al. 1995b). Hospital ergonomics has taken on increasing importance and, therefore, is the subject of a review article in this chapter. The specific problem of the prevention and management of back pain in nurses as one of the most important problems for this cohort of HCWs is also discussed in the article “Prevention and management of back pain in nurses” in this chapter. Table 4 lists the total number of injuries in a one-year period.
Table 4. Total number of injuries, mechanism of injury and nature of industry (one hospital, all departments), 1 April 1994 to 31 March 1995
|
Nature of injury sustained |
Total |
||||||||||||
|
Mechanism |
Blood/ |
Cut/ |
Bruise/ |
Sprain/ |
Fracture/ |
Burn/ |
Human |
Broken |
Head- |
Occupa- |
Other3 |
Un- |
|
|
Exertion |
|||||||||||||
|
Transferring |
105 |
105 |
|||||||||||
|
Lifting |
83 |
83 |
|||||||||||
|
Assisting |
4 |
4 |
|||||||||||
|
Turning |
27 |
27 |
|||||||||||
|
Breaking fall |
28 |
28 |
|||||||||||
|
Pushing |
1 |
25 |
26 |
||||||||||
|
Lifting |
1 |
52 |
1 |
54 |
|||||||||
|
Pulling |
14 |
14 |
|||||||||||
|
Combination- |
38 |
38 |
|||||||||||
|
Other |
74 |
74 |
|||||||||||
|
Fall |
3 |
45 |
67 |
3 |
1 |
119 |
|||||||
|
Struck/ |
66 |
76 |
5 |
2 |
2 |
1 |
152 |
||||||
|
Caught in/ |
13 |
68 |
8 |
1 |
1 |
91 |
|||||||
|
Exp. |
3 |
1 |
4 |
19 |
16 |
12 |
55 |
||||||
|
Staff abuse |
|||||||||||||
|
Patient |
16 |
11 |
51 |
28 |
8 |
3 |
1 |
2 |
120 |
||||
|
Spill/splashes |
80 |
1 |
81 |
||||||||||
|
Drug/ |
2 |
2 |
|||||||||||
|
Exp. |
5 |
5 |
10 |
||||||||||
|
Needlesticks |
159 |
22 |
181 |
||||||||||
|
Scalpel cuts |
34 |
14 |
48 |
||||||||||
|
Other5 |
3 |
1 |
29 |
1 |
6 |
40 |
|||||||
|
Unknown (no |
8 |
8 |
|||||||||||
|
Total |
289 |
136 |
243 |
558 |
5 |
33 |
8 |
7 |
19 |
25 |
29 |
8 |
1,360 |
1 No blood/body fluid. 2 This includes rashes/dermatitis/work-related illness/burning eyes, irritated eyes. 3 Exposure to chemical or physical agents but with no documented injuries affects. 4 Accident not reported. 5 Exposure to cold/heat, unknown.
In discussing musculoskeletal and ergonomic problems, it is important to note that while those engaged in direct patient care may be at greatest risk (see figure 5) many of the support personnel in hospital must contend with similar ergonomic burdens (see figure 6 and figure 7). The ergonomic problems facing hospital laundry workers have been well-documented (Wands and Yassi 1993) (see figure 8, figure 9 and figure 10) and they also are common among dentists, otologists, surgeons and especially microsurgeons, obstetricians, gynaecologists and other health personnel who often must work in awkward postures.
Figure 5. Patient lifting is an ergonomic hazard in most hospitals
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 6. Overhead painting: A typical ergonomic hazard for a tradesworker
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 7. Cast-making involves many ergonomic stresses
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 8. Laundry work such as this can cause repetitive stress injury to the upper limbs
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 9. This laundry task requires working in an awkward position
Health Sciences Centre, Winnipeg, Manitoba, Canada
Figure 10. A poorly designed laundry operation can cause back strain
Health Sciences Centre, Winnipeg, Manitoba, Canada
Organizational Problems
The article “Strain in health care work” contains a discussion of some of the organizational problems in hospitals and a summary of the principal findings of Leppanen and Olkinuora (1987), who reviewed Finnish and Swedish studies of stress among HCWs. With the rapid changes currently under way in this industry, the extent of alienation, frustration and burnout among HCWs is considerable. Added to that is the prevalence of staff abuse, an increasingly troublesome problem in many facilities (Yassi 1994). While it is often thought that the most difficult psychosocial problem faced by HCWs is dealing with death and dying, it is being recognized increasingly that the nature of the industry itself, with its hierarchical structure, its growing job insecurity and the high demands unsupported by adequate resources, is the cause of the variety of stress-related illness faced by HCWs.
The Nature of the Health Care Sector
In 1976, Stellman wrote, “If you ever wondered how people can manage to work with the sick and always stay healthy themselves, the answer is that they can’t” (Stellman 1976). The answer has not changed, but the potential hazards have clearly expanded from infectious diseases, back and other injuries, stress and burnout to include a large variety of potentially toxic environmental, physical and psychosocial exposures. The world of the HCW continues to be largely unmonitored and largely unregulated. None the less, progress is being made in addressing occupational health and safety hazards in hospitals. The International Commission on Occupational Health (ICOH) has a sub-committee addressing this problem, and several international conferences have been held with published proceedings that offer useful information (Hagberg et al. 1995). The US Centers for Disease Control and Prevention (CDC) and NIOSH have proposed guidelines to address many of the problems of the health care industry discussed in this article (e.g., see NIOSH 1988). The number of articles and books addressing health and safety issues for HCWs has been growing rapidly, and good overviews of health and safety in the US health care industry have been published (e.g., Charney 1994; Lewy 1990; Sterling 1994). The need for systematic data collection, study and analysis regarding hazards in the health care industry and the desirability of assembling interdisciplinary occupational health teams to address them have become increasingly evident.
When considering occupational health and safety in the health care industry, it is crucial to appreciate the enormous changes currently taking place in it. Health care “reform”, being instituted in most of the developed countries of the world, is creating extraordinary turbulence and uncertainty for HCWs, who are being asked to absorb rapid changes in their work tasks often with greater exposure to risks. The transformation of health care is spurred, in part, by advances in medical and scientific knowledge, the development of innovative technological procedures and the acquisition of new skills. It is also being driven, however, and perhaps to an even greater extent, by concepts of cost-effectiveness and organizational efficiency, in which “downsizing” and “cost control” have often seemed to become goals in themselves. New institutional incentives are being introduced at different organizational levels in different countries. The contracting out of jobs and services that had traditionally been carried out by a large stable workforce is now increasingly becoming the norm. Such contracting out of work is reported to have helped the health administrators and politicians achieve their long-term goal of making the process of health care more flexible and more accountable. These changes have also brought changes in roles that were previously rather well-defined, undermining the traditional hierarchical relationships among planners, administrators, physicians and other health professionals. The rise of investor-owned health care organizations in many countries has introduced a new dynamic in the financing and management of health services. In many situations, HCWs have been forced into new working relationships that involve such changes as downgrading services so that they can be performed by less-skilled workers at lower pay, reduced staffing levels, staff redeployments involving split shifts and part-time assignments. At the same time, there has been a slow but steady growth in the numbers of such physician surrogates as physician assistants, nurse practitioners, midwives and psychiatric social workers who command lower rates of pay than the physicians they are replacing. (The ultimate social and health costs both to HCWs and to the public, as patients and payers, is still to be determined.)
A growing trend in the US that is also emerging in the UK and northern European countries is “managed care”. This generally involves the creation of organizations paid on a per capita basis by insurance companies or government agencies to provide or contract for the provision of a comprehensive range of health services to a voluntarily-enrolled population of subscribers. Their aim is to reduce the costs of health care by “managing” the process: using administrative procedures and primary care physicians as “gatekeepers” to control the utilization of expensive in-patient hospital days, reducing referrals to high-priced specialists and use of costly diagnostic procedures, and denying coverage for expensive new forms of “experimental” treatment. The growing popularity of these managed care systems, fuelled by aggressive marketing to employer- and government-sponsored groups and individuals, has made it difficult for physicians and other health care providers to resist becoming involved. Once engaged, there is a variety of financial incentives and disincentives to influence their judgement and condition their behaviour. The loss of their traditional autonomy has been particularly painful for many medical practitioners and has had a profound influence on their patterns of practice and their relationships with other HCWs.
These rapid changes in the organization of the health care industry are having profound direct and indirect effects on the health and safety of HCWs. They affect the ways health services are organized, managed, delivered and paid for. They affect the ways HCWs are trained, assigned and supervised and the extent to which considerations of their health and safety are addressed. This should be kept in mind as the various occupational health hazards faced by HCWs are discussed in this chapter. Finally, although it may not appear to be directly relevant to the content of this chapter, thought should be given to the implications of the well-being and performance of HCWs to the quality and effectiveness of the services they provide to their patients.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."