Children categories

14. First Aid and Emergency Medical Services (2)

14. First Aid and Emergency Medical Services
Chapter Editor: Antonio J. Dajer
Table of Contents
Tables
First Aid
Antonio J. Dajer
Traumatic Head Injuries
Fengsheng He
Tables
Click a link below to view table in article context.

15. Health Protection and Promotion (25)

15. Health Protection and Promotion
Chapter Editors: Jacqueline Messite and Leon J. Warshaw
Table of Contents
Figures and Tables
Health Protection and Promotion in the Workplace: An Overview
Leon J. Warshaw and Jacqueline Messite
Worksite Health Promotion
Jonathan E. Fielding
Health Promotion in the Workplace: England
Leon Kreitzman
Health Promotion in Small Organizations: The US experience
Sonia Muchnick-Baku and Leon J. Warshaw
Role of the Employee Health Service in Preventive Programmes
John W.F. Cowell
Health Improvement Programmes at Maclaren Industries, Inc.: A Case Study
Ian M.F. Arnold and Louis Damphousse
Role of the Employee Health Service in Prevention Programmes: A Case Study
Wayne N. Burton
Worksite Health Promotion in Japan
Toshiteru Okubo
Health Risk Appraisal
Leon J. Warshaw
Physical Training and Fitness Programmes: An Organizational Asset
James Corry
Worksite Nutrition Programmes
Penny M. Kris-Etherton and John W. Farquhar
Smoking Control in the Workplace
Jon Rudnick
Smoking Control Programmes at Merrill Lynch and Company, Inc.: A Case Study
Kristan D. Goldfein
Cancer Prevention and Control
Peter Greenwald and Leon J. Warshaw
Women’s Health
Patricia A. Last
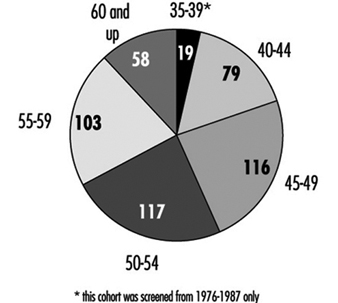
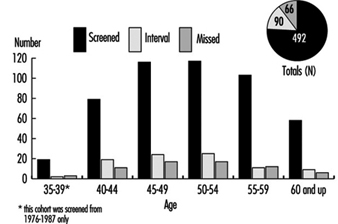
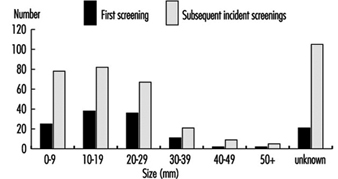
Mammography Programme at Marks and Spencer: A Case Study
Jillian Haslehurst
Worksite Strategies to Improve Maternal and Infant Health: Experiences of US Employers
Maureen P. Corry and Ellen Cutler
HIV/AIDS Education
B.J. Stiles
Health Protection and Promotion: Infectious Diseases
William J. Schneider
Protecting the Health of the Traveller
Craig Karpilow
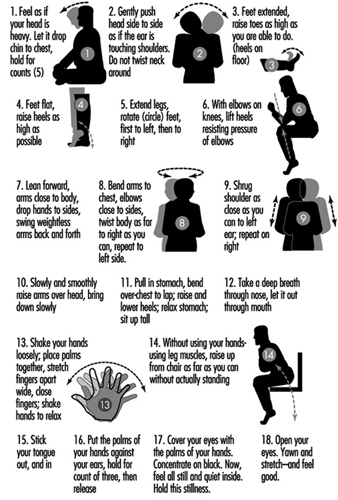
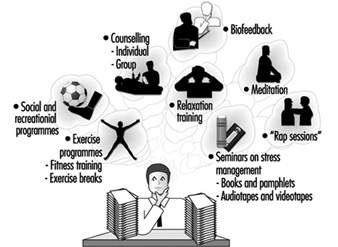
Stress Management Programmes
Leon J. Warshaw
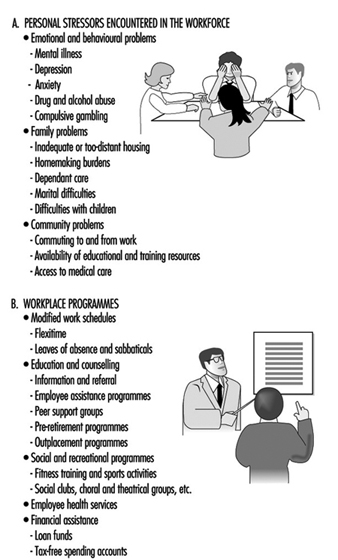
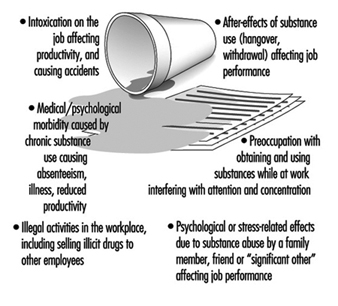
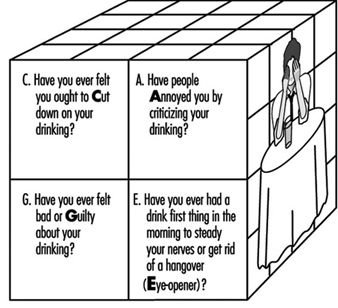
Alcohol and Drug Abuse
Sheila B. Blume
Employee Assistance Programmes
Sheila H. Akabas
Health in the Third Age: Pre-retirement Programmes
H. Beric Wright
Outplacement
Saul G. Gruner and Leon J. Warshaw
Tables
Click a link below to view table in the article context.
1. Health-related activities by workforce size
2. Breast & cervical cancer screening rates
3. Themes of “World No-Tobacco Days”
4. Screening for neoplastic diseases
5. Health insurance benefits
6. Services provided by the employer
7. Substances capable of producing dependence
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

16. Occupational Health Services (16)

16. Occupational Health Services
Chapter Editors: Igor A. Fedotov, Marianne Saux and Jorma Rantanen
Table of Contents
Figures and Tables
Standards, Principles and Approaches in Occupational Health Services
Jorma Rantanen and Igor A. Fedotov
Occupational Health Services and Practice
Georges H. Coppée
Medical Inspection of Workplaces and Workers in France
Marianne Saux
Occupational Health Services in Small-Scale Enterprises
Jorma Rantanen and Leon J. Warshaw
Accident Insurance and Occupational Health Services in Germany
Wilfried Coenen and Edith Perlebach
Occupational Health Services in the United States: Introduction
Sharon L. Morris and Peter Orris
Governmental Occupational Health Agencies in the United States
Sharon L. Morris and Linda Rosenstock
Corporate Occupational Health Services in the United States: Services Provided Internally
William B. Bunn and Robert J. McCunney
Contract Occupational Health Services in the United States
Penny Higgins
Labour Union-Based Activities in the United States
Lamont Byrd
Academic-Based Occupational Health Services in the United States
Dean B. Baker
Occupational Health Services in Japan
Ken Takahashi
Labour Protection in the Russian Federation: Law and Practice
Nikolai F. Izmerov and Igor A. Fedotov
The Practice of Occupational Health Service in the People’s Republic of China
Zhi Su
Occupational Safety and Health in the Czech Republic
Vladimír Bencko and Daniela Pelclová
Practising Occupational Health in India
T. K. Joshi
Tables
Click a link below to view table in article context.
1. Principles for occupational health practice
2. Doctors with specialist knowledge in occ. medicine
3. Care by external occupational medical services
4. US unionized workforce
5. Minimum requirements, in-plant health
6. Periodic examinations of dust exposures
7. Physical examinations of occupational hazards
8. Results of environmental monitoring
9. Silicosis & exposure, Yiao Gang Xian Tungsten Mine
10. Silicosis in Ansham Steel company
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Smoking Control Programmes at Merrill Lynch and Company, Inc.: A Case Study
In 1990, the US Government demonstrated strong support for workplace health promotion programs with the publication of Healthy People 2000, setting forth the National Health Promotion and Disease Prevention Objectives for the Year 2000 (US Public Health Service 1991). One of these objectives calls for an increase in the percentage of worksites offering health promotion activities for their employees by the year 2000, “preferably as part of a comprehensive employee health promotion program” (Objective 8.6). Two objectives specifically include efforts to prohibit or severely restrict smoking at work by increasing the percentage of worksites with a formal smoking policy (Objective 3.11) and by enacting comprehensive state laws on clean indoor air (Objective 3.12).
In response to these objectives and employee interest, Merrill Lynch and Company, Inc. (hereafter called Merrill Lynch) launched the Wellness and You program for employees at headquarters locations in New York City and in the state of New Jersey. Merrill Lynch is a US-based, global financial management and advisory company, with a leadership position in businesses serving individuals as well as corporate and institutional clients. Merrill Lynch’s 42,000 employees in more than 30 countries provide services including securities underwriting, trading and brokering; investment banking; trading of foreign exchange, commodities and derivatives; banking and lending; and insurance sales and underwriting services. The employee population is diverse in terms of ethnicity, nationality, educational achievement and salary level. Nearly half of the employee population is headquartered in the New York City metropolitan area (includes part of New Jersey) and in two service centers in Florida and Colorado.
Merrill Lynch’s Wellness and You Program
The Wellness and You program is based in the Health Care Services Department and is managed by a doctorate-level health educator who reports to the medical director. The core wellness staff consists of the manager and a full-time assistant, and is supplemented by staff physicians, nurses and employee assistance counselors as well as outside consultants as needed.
In 1993, its initial year, over 9,000 employees representing approximately 25% of the workforce participated in a variety of Wellness and You activities, including the following:
- self-help and written information programmes, including the distribution of pamphlets on a diversity of health topics and a Merrill Lynch personal health guide designed to encourage employees to get the tests, immunizations, and guidance they need to stay healthy
- educational seminars and workshops on topics of broad interest such as smoking cessation, stress management, AIDS, and Lyme disease
- comprehensive screening programmes to identify employees at risk for cardiovascular disease, skin cancer, and breast cancer. These programmes were provided by outside contractors on company premises either in health services clinics or mobile van units
- ongoing programmes, including aerobic exercise in the company cafeteria and personal weight management classes in company conference rooms
- clinical care, including influenza immunizations, dermatology services, periodic health examinations and nutritional counselling in the employee health services clinics.
In 1994, the program expanded to include an onsite gynecology screening program comprising of Pap smears and pelvic and breast examinations; and a worldwide emergency medical assistance program to help American employees locate an English-speaking doctor anywhere in the world. In 1995, wellness programs will be extended to service offices in Florida and Colorado and will reach approximately half of the entire workforce. Most services are offered to employees free of charge or at nominal cost.
Smoking Control Programs at Merrill Lynch
Anti-smoking programs have gained a prominent place in the workplace wellness arena in recent years. In 1964, the US Surgeon General identified smoking as the single cause of the greater part of preventable disease and premature death (US Department of Health, Education, and Welfare 1964). Since then, research has demonstrated that the health risk from inhaling tobacco smoke is not limited to the smoker, but includes those who inhale second-hand smoke (US Department of Health and Human Services 1991). Consequently, many employers are taking steps to limit or curtail smoking by employees out of concern for employee health as well as their own “bottom lines”. At Merrill Lynch, Wellness and You includes three types of smoking cessation effort: (1) the distribution of written material, (2) smoking cessation programs, and (3) restrictive smoking policies.
Written materials
The wellness program maintains a wide selection of quality educational materials to provide information, assistance and encouragement to employees to improve their health. Self-help materials such as pamphlets and audiotapes designed to educate employees about the harmful effects of smoking and about the benefits of quitting are available in the health care clinic waiting rooms and through interoffice mail by request.
Written materials also are distributed at health fairs. Often these health fairs are sponsored in conjunction with national health initiatives so as to capitalize on existing media attention. For example, on the third Thursday of each November, the American Cancer Society sponsors the Great American Smokeout. This national campaign, designed to encourage smokers to give up cigarettes for 24 hours, is well publicized throughout the United States by television, radio and newspapers. The idea is that if smokers can prove to themselves that they can quit for the day, they might quit for good. In 1993’s Smokeout, 20.5% of smokers in the United States (9.4 million) stopped smoking or reduced the number of cigarettes they smoked for the day; 8 million of them reported continuing not to smoke or reducing their smoking one to ten days later.
Each year, members of Merrill Lynch’s medical department set up quit-smoking booths on the day of the Great American Smokeout at home office locations. Booths are stationed in high-traffic locations (lobbies and cafeterias) and provide literature, “survival kits” (containing chewing gum, cinnamon sticks, and self-help materials), and quit-smoking pledge cards to encourage smokers to quit smoking at least for the day.
Smoking cessation programs
Since no single smoking cessation program works for everyone, employees at Merrill Lynch are offered a variety of options. These include self-help written materials (“quit kits”), group programs, audiotapes, individual counseling and physician intervention. Interventions range from education and classic behavior modification to hypnosis, nicotine replacement therapy (e.g., “the patch” and nicotine chewing gum), or a combination. Most of these services are available to employees free of charge and some programs, such as group interventions, have been subsidized by the firm’s benefits department.
Non-smoking policies
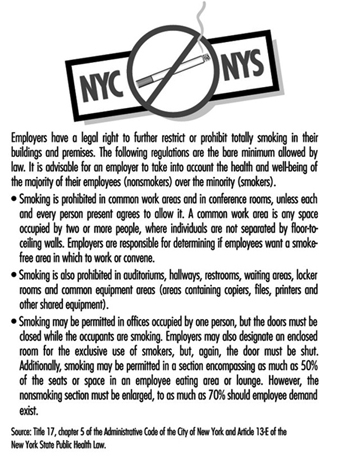
In addition to smoking cessation efforts aimed at individuals, smoking restrictions are becoming increasingly common in the workplace. Many jurisdictions in the United States, including the states of New York and New Jersey, have enacted strict workplace smoking laws that, for the most part, limit smoking to private offices. Smoking in common work areas and conference rooms is permitted, but only if each and every person present agrees to allow it. The statutes typically mandate that non-smokers’ preferences receive priority even to the point of banning smoking entirely. Figure 1 summarizes the city and state regulations applicable in New York City.
Figure 1. Summary of city and state restrictions on smoking in New York.
In many offices, Merrill Lynch has implemented smoking policies which extend beyond the legal requirements. Most headquarters cafeterias in New York City and in New Jersey have gone smoke-free. In addition, total smoking bans have been implemented in some office buildings in New Jersey and Florida, and in certain work areas in New York City.
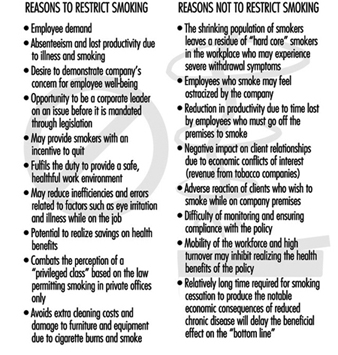
There seems to be little debate about the adverse health effects of tobacco exposure. However, other issues should be considered in developing a corporate smoking policy. Figure 2 outlines many of the reasons why a company may or may not elect to restrict smoking beyond the legal requirements.
Figure 2. Reasons for and against restricting smoking in the workplace.
Evaluation of Smoking Cessation Programs and Policies
Given the relative youth of the Wellness and You program, no formal evaluation has yet been conducted to determine the effect of these efforts on employee morale or smoking habits. However, some studies suggest that worksite smoking restrictions are favored by a majority of employees (Stave and Jackson 1991), result in decreased cigarette consumption (Brigham et al. 1994; Baile et al. 1991; Woodruff et al. 1993), and effectively increase smoking cessation rates (Sorensen et al. 1991).
Cancer Prevention and Control
Within the next decade, it is predicted, cancer will become the leading cause of death in many developed countries. This reflects not so much an increase in the incidence of cancer but rather a decrease in mortality due to cardiovascular disease, currently topping the mortality tables. Equally with its high mortality rate, we are disturbed by the specter of cancer as a “dread” disease: one associated with a more or less rapid course of disability and a high degree of suffering. This somewhat fearsome picture is being made easier to contemplate by our growing knowledge of how to reduce risk, by techniques permitting early detection and by new and powerful achievements in the field of therapy. However, the latter may be associated with physical, emotional and economic costs for both the patients and those concerned about them. According to the US National Cancer Institute (NCI), a significant reduction in cancer morbidity and mortality rates is possible if current recommendations relating to use of tobacco, dietary changes, environmental controls, screening and state-of-the-art treatment are effectively applied.
To the employer, cancer presents significant problems entirely apart from the responsibility for possible occupational cancer. Workers with cancer may have impaired productivity and recurrent absenteeism due both to the cancer itself and the side effects of its treatment. Valuable employees will be lost through prolonged periods of disability and premature death, leading to the considerable cost of recruiting and training replacements.
There is a cost to the employer even when it is a spouse or other dependant rather than the healthy employee who develops the cancer. The caregiving burden may lead to distraction, fatigue and absenteeism which tax that employee’s productivity, and the often considerable medical expenses increase the cost of employer-sponsored health insurance. It is entirely appropriate, therefore, that cancer prevention should be a major focus of worksite wellness programs.
Primary Prevention
Primary prevention involves avoidance of smoking and modifying other host factors that may influence the development of cancer, and identifying potential carcinogens in the work environment and eliminating or at least limiting workers’ exposure to them.
Controlling exposures
Potential as well as proven carcinogens are identified through basic scientific research and by epidemiological studies of exposed populations. The latter involves industrial hygiene measurements of the frequency, magnitude and duration of the exposures, coupled with comprehensive medical surveillance of the exposed workers, including analysis of causes of disability and death. Controlling exposures involves the elimination of these potential carcinogens from the workplace or, when that is not possible, minimizing exposure to them. It also involves the proper labeling of such hazardous materials and continuing education of workers with respect to their handling, containment and disposal.
Smoking and cancer risk
Approximately one-third of all cancer deaths and 87% of all lung cancers in the US are attributable to smoking. Tobacco use is also the principal cause of cancers of the larynx, oral cavity and oesophagus and it contributes to the development of cancers of the bladder, pancreas, kidney, and uterine cervix. There is a clear dose-response relationship between lung cancer risk and daily cigarette consumption: those who smoke more than 25 cigarettes a day have a risk that is about 20 times greater than that of non-smokers.
Experts believe that the involuntary intake of the tobacco smoke emitted by smokers (“environmental tobacco smoke”) is a significant risk factor for lung cancer in non-smokers. In January 1993, the US Environmental Protection Agency (EPA) classified environmental tobacco smoke as a known human carcinogen which, it estimated, is responsible for approximately 3,000 lung cancer deaths annually among US non-smokers.
The 1990 US Surgeon General’s report on the health benefits of smoking cessation provides clear evidence that quitting smoking at any age is beneficial to one’s health. For example, five years after quitting, former smokers experience a diminished risk for lung cancer; their risk, however, remains higher than that of non-smokers for as long as 25 years.
The elimination of tobacco exposure by employer-sponsored/ labor union-sponsored smoking cessation programs and worksite policies enforcing a smoke-free working environment represent a major element in most worksite wellness programs.
Modifying host factors
Cancer is an aberration of normal cell division and growth in which certain cells divide at abnormal rates and grow abnormally, sometimes migrating to other parts of the body, affecting the form and function of involved organs, and ultimately causing death of the organism. Recent, continuing biomedical advances are providing increasing knowledge of the carcinogenesis process and are beginning to identify the genetic, humoral, hormonal, dietary and other factors that may accelerate or inhibit it—thus leading to research on interventions that have the potential to identify the early, precancerous process and so to help restore the normal cellular growth patterns.
Genetic factors
Epidemiologists continue to accumulate evidence of familial variations in the frequency of particular types of cancer. These data have been bolstered by molecular biologists who have already identified genes that appear to control steps in cellular division and growth. When these “tumor suppressor” genes are damaged by naturally-occurring mutations or the effects of an environmental carcinogen, the process may go out of control and a cancer is initiated.
Heritable genes have been found in patients with cancer and members of their immediate families. One gene has been associated with a high risk of colon cancer and endometrial or ovarian cancer in women; another with a high risk of breast and ovarian cancer; and a third with a form of malignant melanoma. These discoveries led to a debate about the ethical and sociological issues surrounding DNA testing to identify individuals carrying these genes with the implication that they then might be excluded from jobs involving possible exposure to potential or actual carcinogens. After studying this question, the National Advisory Council for Human Genome Research (1994), raising issues to do with the reliability of the testing, the present effectiveness of potential therapeutic interventions, and the likelihood of genetic discrimination against those found to be at high risk, concluded that “it is premature to offer DNA testing or screening for cancer predisposition outside a carefully monitored research environment”.
Humoral factors
The value of the prostate specific antigen (PSA) test as a routine screening test for prostatic cancer in older men has not been scientifically demonstrated in a clinical trial. However, in some instances, it is being offered to male workers, sometimes as a token of gender equity to balance the offering of mammography and cervical Pap smears to female workers. Clinics providing routine periodic examinations are offering the PSA test as a supplement to and, sometimes, even as a replacement for the traditional digital rectal examination as well as the recently introduced rectal ultrasound examination. Although its use appears to be valid in men with prostatic abnormalities or symptoms, a recent multinational review concludes that measurement of PSA should not be a routine procedure in screening healthy male populations (Adami, Baron and Rothman 1994).
Hormonal factors
Research has implicated hormones in the genesis of some cancers and they have been used in the treatment of others. Hormones, however, do not appear to be an appropriate item to emphasize in workplace health promotion programs. A possible exception would be warnings of their potential carcinogenic hazard in certain cases when recommending hormones for the treatment of menopausal symptoms and the prevention of osteoporosis.
Dietary factors
Researchers have estimated that approximately 35% of all cancer mortality in the US may be related to diet. In 1988, the US Surgeon General’s Report on Nutrition and Health indicated that cancers of the lung, colon-rectum, breast, prostate, stomach, ovary and bladder may be associated with diet. Research indicates that certain dietary factors—fat, fiber, and micronutrients such as beta-carotene, vitamin A, vitamin C, vitamin E and selenium—may influence cancer risk. Epidemiological and experimental evidence indicates that modulation of these factors in the diet can reduce the occurrence of some types of cancer.
Dietary fat
Associations between excess intake of dietary fat and the risk of various cancers, particularly cancers of the breast, colon and prostate, have been demonstrated in both epidemiological and laboratory studies. International correlational studies have shown a strong association between the incidence of cancers at these sites and total dietary fat intake, even after adjusting for total caloric intake.
In addition to the amount of fat, the type of fat consumed may be an important risk factor in cancer development. Different fatty acids may have various site-specific tumor-promoting or tumor-inhibiting properties. Intake of total fat and saturated fat has been strongly and positively associated with colon, prostate, and post-menopausal breast cancers; intake of polyunsaturated vegetable oil has been positively associated with post-menopausal breast and prostate cancers, but not with colon cancer. Conversely, consumption of highly polyunsaturated omega-3 fatty acids found in certain fish oils may not affect or may even decrease the risk of breast and colon cancers.
Dietary fiber
Epidemiological evidence suggests that the risk of certain cancers, particularly colon and breast cancers, may be lowered by increased intake of dietary fiber and other dietary constituents associated with high intakes of vegetables, fruits, and whole grains.
Micronutrients
Epidemiological studies generally show an inverse relationship between cancer incidence and intake of foods high in several nutrients having antioxidant properties, such as beta-carotene, vitamin C (ascorbic acid), and vitamin E (alpha-tocopherol). A number of studies have shown that low intakes of fruits and vegetables are associated with increased risk of lung cancer. Deficiencies of selenium and zinc have also been implicated in increased cancer risk.
In a number of studies in which the use of antioxidant supplements was shown to reduce the expected number of serious heart attacks and strokes, the data on cancer were less clear. However, results from the Alpha-Tocopherol, Beta-Carotene (ATBC) Lung Cancer Prevention clinical trial, conducted by the NCI in collaboration with the National Public Health Institute of Finland, indicated that vitamin E and beta-carotene supplements did not prevent lung cancer. Vitamin E supplementation also resulted in 34% fewer prostate cancers and 16% fewer colorectal cancers, but those subjects taking beta-carotene had 16% more lung cancers, which was statistically significant, and had slightly more cases of other cancers than those taking vitamin E or the placebo. There was no evidence that the combination of vitamin E and beta-carotene was better or worse than either supplement alone. The researchers have not yet determined why those taking beta-carotene in the study were observed to have more lung cancers. These results suggest the possibility that a different compound or compounds in foods which have high levels of beta-carotene or vitamin E may be responsible for the protective effect observed in epidemiological studies. The researchers also speculated that the length of time of supplementation may have been too short to inhibit the development of cancers in long-term smokers. Further analyses of the ATBC study, as well as results from other trials in progress, will help resolve some of the questions that have arisen in this trial, particularly the question of whether large doses of beta-carotene may be harmful to smokers.
Alcohol
Excessive use of alcoholic beverages has been associated with cancer of the rectum, pancreas, breast and liver. There is also strong evidence supporting a synergistic association of alcohol consumption and tobacco use with increased risk of cancer of the mouth, pharynx, oesophagus and larynx.
Dietary recommendations
Based on the compelling evidence that diet is related to cancer risk, the NCI has developed dietary guidelines that include the following recommendations:
- Reduce fat intake to 30% or less of calories.
- Increase fibre intake to 20 to 30 grams per day, with an upper limit of 35 grams.
- Include a variety of vegetables and fruits in the daily diet.
- Avoid obesity.
- Consume alcoholic beverages in moderation, if at all.
- Minimize consumption of salt-cured (packed in salt), salt-pickled (soaked in brine), or smoked foods (associated with increased incidence of stomach and oesophageal cancer).
These guidelines are intended to be incorporated into a general dietary regimen that can be recommended for the entire population.
Infectious diseases
There is increasing knowledge of the association of certain infectious agents with several types of cancer: for example, the hepatitis B virus with liver cancer, the human papillomavirus with cervical cancer, and the Epstein-Barr virus with Burkitt’s lymphoma. (The frequency of cancer among patients with AIDS is attributable to the patient’s immunodeficiency and is not a direct carcinogenic effect of the HIV agent.) A vaccine for hepatitis B is now available that, when given to children, ultimately will reduce their risk for liver cancer.
Worksite Cancer Prevention
To explore the potential of the workplace as an arena for the promotion of a broad set of cancer prevention and control behaviors, the NCI is sponsoring the Working Well Project. This project is designed to determine whether worksite-based interventions to reduce tobacco use, achieve cancer preventive dietary modifications, increase screening prevalence and reduce occupational exposure can be developed and implemented in a cost-effective way. It was initiated in September 1989 at the following four research centers in the United States.
- M.D. Anderson Cancer Center, Houston, Texas
- University of Florida, Gainesville, Florida
- Dana Farber Cancer Institute, Boston, Massachusetts
- Miriam Hospital/Brown University, Providence, Rhode Island
The project involves approximately 21,000 employees at 114 different worksites around the United States. Most of the selected worksites are involved predominantly in manufacturing; other types of worksites in the project included fire stations and newspaper printers. Tobacco reduction and dietary modification were areas of intervention included in all of the worksites; however, each site maximized or minimized particular intervention programs or included additional options to meet the climatic and socioeconomic conditions of the geographic area. The centers in Florida and Texas, for example, included and emphasized skin cancer screening and the use of sun screens because of increased exposure to the sun in those geographic regions. The centers in Boston and Texas offered programs that emphasized the relationship between cancer and tobacco use. The Florida centre enhanced the diet modification intervention with supplies of fresh citrus fruits, readily available from the state’s farming and fruit industry. Management-employee consumer boards also were established at the worksites of the Florida centre to work with the food service to ensure that the cafeterias offered fresh vegetable and fruit selections. Several of the worksites participating in the project offered small prizes—gift certificates or cafeteria lunches—for continued participation in the project or for achievement of a desired goal, such as smoking cessation. Reduction of exposure to occupational hazards was of special interest at those worksites where diesel exhaust, solvent use or radiation equipment were prevalent. The worksite-based programs included:
- group activities to generate interest, such as taste testing of various foods
- directed group activities, such as quit-smoking contests
- medical/scientific-based demonstrations, such as
 testing, to verify the effect of smoking on the respiratory system
testing, to verify the effect of smoking on the respiratory system - seminars on business practices and policy development aimed at significantly reducing or eliminating occupational exposure to potentially or actually dangerous or toxic materials
- computer-based self-help and self-assessment programmes on cancer risk and prevention
- manuals and self-help classes to help reduce or eliminate tobacco use, achieve dietary modifications, and increase cancer screening.
Cancer education
Worksite health education programs should include information about signs and symptoms that are suggestive of early cancer—for example, lumps, bleeding from the rectum and other orifices, skin lesions that do not appear to heal—coupled with advice to seek evaluation by a physician promptly. These programs might also offer instruction, preferably with supervised practice, in self-examination of the breast.
Cancer screening
Screening for precancerous lesions or early cancer is carried out with a view to their earliest possible detection and removal. Educating individuals about the early signs and symptoms of cancer so that they may seek the attention of a physician is an important part of screening.
A search for early cancer should be included in every routine or periodic medical examination. In addition, mass screenings for particular types of cancer may be carried out in the workplace or in a community facility near the worksite. Any acceptable and justifiable screening of an asymptomatic population for cancer should meet the following criteria:
- The disease in question should represent a substantial burden at the public health level and should have a prevalent, asymptomatic, nonmetastatic phase.
- The asymptomatic, nonmetastatic phase should be recognizable.
- The screening procedure should have reasonable specificity, sensitivity and predictive values; it should be of low risk and low cost, and be acceptable to both the screener and the person being screened.
- Early detection followed by appropriate treatment should offer a substantially greater potential for cure than exists in cases in which discovery was delayed.
- Treatment of lesions detected by screening should offer improved outcomes as measured in cause-specific morbidity and mortality.
The following additional criteria are particularly relevant in the workplace:
- Employees (and their dependants, when involved in the programme) should be informed of the purpose, nature and potential results of the screening, and a formal “informed consent” should be obtained.
- The screening programme should be conducted with due consideration for the comfort, dignity and privacy of the individuals consenting to be screened and should involve minimal interference with working arrangements and production schedules.
- Screening results should be conveyed promptly and privately, with copies forwarded to personal physicians designated by the workers. Counselling by trained health professionals should be available to those seeking clarification of the screening report.
- The individuals screened should be informed of the possibility of false negatives and warned to seek medical evaluation of any signs or symptoms developing soon after the screening exercise.
- A prearranged referral network should be in place to which those with positive results who are not able or do not wish to consult their personal physicians may be referred.
- The costs of the necessary confirmatory examinations and the costs of treatment should be covered by health insurance or otherwise be affordable.
- A prearranged follow-up system should be in place to be sure that positive reports have been promptly confirmed and proper interventions arranged.
A further final criterion is of fundamental importance: the screening exercise should be conducted by properly skilled and accredited health professionals using state-of-the-art equipment and interpretation and analysis of the results should be of the highest possible quality and accuracy.
In 1989 the US Preventive Services Task Force, a panel of 20 experts from medicine and other related fields drawing upon hundreds of “advisors” and others from the United States, Canada and the United Kingdom, assessed the effectiveness of some 169 preventive interventions. Its recommendations with respect to screening for cancer are summarized in table 1. Reflecting the Task Force’s somewhat conservative attitude and rigorously applied criteria, these recommendations may differ from those advanced by other groups.
Table 1. Screening for neoplastic diseases.
|
Types of cancer |
Recommendations of the US Preventive Services Task Force* |
|
Breast |
All women over age 40 should receive an annual clinical breast examination. Mammography every one to two years is recommended for all women beginning at age 50 and continuing until age 75 unless pathology has been detected. It may be prudent to begin mammography at an earlier age for women at high risk for breast cancer. Although the teaching of breast self-examination is not specifically recommended at this time, there is insufficient evidence to recommend any change in current breast self- examination practices (i.e., those who are now teaching it should continue the practice). |
|
Colorectal |
There is insufficient evidence to recommend for or against fecal occult blood testing or sigmoidoscopy as effective screening tests for colorectal cancer in asymptomatic individuals. There are also insufficient grounds for discontinuing this form of screening where it is currently practiced or for withholding it from persons who request it. It may be clinically prudent to offer screening to persons aged 50 or older with known risk factors for colorectal cancer. |
|
Cervical |
Regular Papanicolaou (Pap) testing is recommended for all women who are or have been sexually active. Pap smears should begin with the onset of sexual activity and should be repeated every one to three years at the physician’s discretion. They may be discontinued at age 65 if previous smears have been consistently normal. |
|
Prostate |
There is insufficient evidence to recommend for or against routine digital rectal examination as an effective screening test for prostate cancer in asymptomatic men. Transrectal ultrasound and serum tumor markers are not recommended for routine screening in asymptomatic men. |
|
Lung |
Screening asymptomatic persons for lung cancer by performing routine chest radiography or sputum cytology is not recommended. |
|
Skin |
Routine screening for skin cancer is recommended for persons at high risk. Clinicians should advise all patients with increased outdoor exposure to use sunscreen preparations and other measures to protect from ultraviolet rays. Currently there is no evidence for or against advising patients to perform skin self-examination. |
|
Testicular |
Periodic screening for testicular cancer by testicular examination is recommended for men with a history of cryptorchidism, orchiopexy, or testicular atrophy. There is no evidence of clinical benefit or harm to recommend for or against routine screening of other men for testicular cancer. Currently there is insufficient evidence for or against counseling patients to perform periodic self-examination of the testicles. |
|
Ovarian |
Screening of asymptomatic women for ovarian cancer is not recommended. It is prudent to examine the adnexa when performing gynecologic examinations for other reasons. |
|
Pancreatic |
Routine screening for pancreatic cancer in asymptomatic persons is not recommended. |
|
Oral |
Routine screening of asymptomatic persons for oral cancer by primary care clinicians is not recommended. All patients should be counseled to receive regular dental examinations, to discontinue the use of all forms of tobacco, and to limit consumption of alcohol. |
Source: Preventive Services Task Force 1989.
Screening for breast cancer
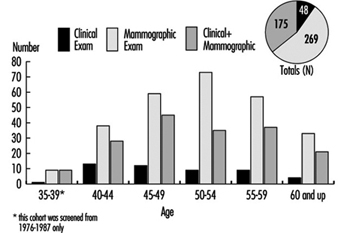
There is a general consensus among experts that screening with mammography combined with clinical breast examination every one to two years will save lives among women aged 50 to 69, reducing breast cancer deaths in this age group by up to 30%. Experts have not reached agreement, however, on the value of breast cancer screening with mammography for asymptomatic women aged 40 to 49. The NCI recommends that women in this age group should be screened every one to two years and that women at increased risk for breast cancer should seek medical advice about whether to begin screening before age 40.
The female population in most organizations may be too small to warrant the installation of mammography equipment onsite. Accordingly, most programs sponsored by employers or labor unions (or both) rely on contracts with providers who bring mobile units to the workplace or on providers in the community to whom participating female employees are referred either during working hours or on their own time. In making such arrangements, it is essential to be sure that the equipment meets standards for x-ray exposure and safety such as those promulgated by the American College of Radiology, and that the quality of the films and their interpretation is satisfactory. Further, it is imperative that a referral resource be prearranged for those women who will require a small needle aspiration or other confirmatory diagnostic procedures.
Screening for cervical cancer
Scientific evidence strongly suggests that regular screening with Pap tests will significantly decrease mortality from cervical cancer among women who are sexually active or who have reached the age of 18. Survival appears to be directly related to the stage of the disease at diagnosis. Early detection, using cervical cytology, is currently the only practical means of detecting cervical cancer in localized or premalignant stages. The risk of developing invasive cervical cancer is three to ten times greater in women who have never been screened than in those who have had Pap tests every two or three years.
Of particular relevance to the cost of workplace screening programs is the fact that cervical cytology smears can be obtained quite efficiently by properly trained nurses and do not require the involvement of a physician. Perhaps of even greater importance is the quality of the laboratory to which they are sent for interpretation.
Screening for colorectal cancer
It is generally agreed that early detection of precancerous colorectal polyps and cancers by periodic tests for fecal blood, as well as digital rectal and sigmoidoscopic examinations, and their timely removal, will reduce mortality from colorectal cancer among individuals aged 50 and over. The examination has been made less uncomfortable and more reliable with the replacement of the rigid sigmoidoscope by the longer, flexible fibreoptic instrument. There remains, however, some disagreement as to which tests should be relied upon and how often they should be applied.
Pros and cons of screening
There is general agreement about the value of cancer screening in individuals at risk because of family history, prior occurrence of cancer, or known exposure to potential carcinogens. But there appear to be justifiable concerns about the mass screening of healthy populations.
Advocates of mass screening for the detection of cancer are guided by the premise that early detection will be followed by improvements in morbidity and mortality. This has been demonstrated in some instances, but is not always the case. For example, although it is possible to detect lung cancer earlier by use of chest x rays and sputum cytology, this has not led to any improvement in treatment outcomes. Similarly, concern has been expressed that increasing the lead time for treatment of early prostatic cancers may not only be without benefit but may, in fact, be counterproductive in view of the longer period of well-being enjoyed by patients whose treatment is delayed.
In planning mass screening programs, consideration must also be given to the impact on the well-being and pocketbooks of patients with false positives. For example, in several series of cases, 3 to 8% of women with positive breast screenings had unnecessary biopsies for benign tumors; and in one experience with the fecal blood test for colorectal cancer, nearly one-third of those screened were referred for diagnostic colonoscopy, and most of them showed negative results.
It is clear that additional research is needed. To assess the efficacy of screening, the NCI has launched a major study, the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trials (PLCO) to evaluate early detection techniques for these four cancer sites. Enrolment for the PLCO began in November 1993, and will involve 148,000 men and women, aged 60 to 74 years, randomized to either the intervention or the control group. In the intervention group, men will be screened for lung, colorectal and prostatic cancer while women will be screened for lung, colorectal and ovarian cancer; those assigned to the control group will receive their usual medical care. For lung cancer, the value of an annual single-view chest x ray will be studied; for colorectal cancer, annual fibreoptic sigmoidoscopy will be performed; for prostate cancer, digital rectal examination and a blood test for PSA will be done; and for ovarian cancer, yearly physical and transvaginal ultrasound examinations will be supplemented by an annual blood test for the tumor marker known as CA-125. At the end of 16 years and the expenditure of US$ 87.8 million, it is hoped that solid data will be obtained about how screening may be used to obtain early diagnoses that may extend lives and reduce mortality.
Treatment and Continuing Care
Treatment and continuing care comprise efforts to enhance the quality of life for those in whom a cancer has taken hold and for those involved with them. Occupational health services and employee assistance programs sponsored by employers and unions can provide useful counsel and support to workers being treated for cancer or who have a dependant receiving treatment. This support can include explanations of what is going on and what to expect, information that is sometimes not provided by oncologists and surgeons; guidance in referrals for second opinions; and consultations and assistance with regard to access to centers of highly specialized care. Leaves of absence and modified work arrangements may make it possible for workers to remain productive while in treatment and to return to work earlier when a remission is achieved. In some workplaces, peer support groups have been formed to provide an exchange of experiences and mutual support for workers facing similar problems.
Conclusion
Programs for the prevention and detection of cancer can make a meaningful contribution to the well-being of the workers involved and their dependants and yield a significant return to the employers and labor unions that sponsor them. As with other preventive interventions, it is necessary that these programs be properly designed and carefully implemented and, since their benefits will accrue over many years, they should be continued on a steady basis.
Women's Health
There is a common misperception that, outside of reproductive differences, female and male workers will be similarly affected by workplace health hazards and attempts to control them. While women and men do suffer from many of the same disorders, they differ physically, metabolically, hormonally, physiologically and psychologically. For example, women’s smaller average size and muscle mass dictate special attention to the fitting of protective clothing and devices and the availability of properly designed hand tools, while the fact that their body mass is usually smaller than that of men makes them more susceptible, on average, to the effects of alcohol abuse on the liver and the central nervous system.
They also differ in the types of job they hold, in the social and economic circumstances that influence their lifestyles, and in their participation in and response to health promotion activities. Although there have been some recent changes, women are still more likely to be found in jobs that are stultifyingly routine and in which they are exposed to repetitive injury. They suffer from pay inequity and are much more likely than men to be burdened with homemaking responsibilities and the care of children and elderly dependants.
In industrialized countries women have a longer life expectancy than men; this applies to every age group. At age 45, a Japanese woman may expect to live on average another 37.5 years, and a 45-year-old Scottish woman another 32.8 years, with women from most of the other countries of the developed world falling between these limits. These facts lead to an assumption that women are, therefore, healthy. There is a lack of awareness that these “extra” years are frequently marred by chronic illness and disability much of which is preventable. Many women know far too little about the health risks they face and, therefore, about the measures they can take to control those risks and protect themselves against serious disease and injury. For example, many women are rightfully concerned about breast cancer but ignore the fact that heart disease is by far the major cause of death in women and that, owing primarily to the increase in their cigarette smoking—which is also a major risk factor for coronary artery disease—the incidence of lung cancer among women is increasing.
In the United States, a 1993 national survey (Harris et al. 1993), involving interviews of more than 2,500 adult women and 1,000 adult men, confirmed that women suffer from serious health problems and that many do not receive the care they need. Between three and four out of ten women, the survey found, are at risk for undetected treatable disease because they are not receiving appropriate clinical preventive services, largely because they lack health care insurance or because their doctors never suggested that appropriate tests were available and should be sought. Furthermore, a substantial number of the American women surveyed were not happy with their personal physicians: four out of ten (twice the proportion of men) said their physicians “spoke down” to them and 17% (compared to 10% of men) had been told that their symptoms were “all in the head”.
While overall rates of mental illness are roughly the same for men and women, the patterns are different: women suffer more from depression and anxiety disorders while drug and alcohol abuse and antisocial personality disorders are more common among men (Glied and Kofman 1995). Men are more likely to seek and receive care from mental health specialists while women are more often treated by primary care physicians, many of whom lack the interest if not the expertise to treat mental health problems. Women, especially older women, receive a disproportionate share of the prescriptions for psychotropic drugs, so that concern has arisen that these drugs are possibly being overutilized. All too often, difficulties stemming from inordinate levels of stress or from problems that are preventable and treatable are explained away by health professionals, family members, supervisors and co-workers, and even by women themselves, as being reflective of the “time of the month” or “change of life”, and, therefore, go untreated.
These circumstances are compounded by the assumption that women—young and old alike—know all there is to know about their bodies and how they function. This is far from the truth. There exists widespread ignorance and uncritically accepted misinformation. Many women feel ashamed to reveal their lack of knowledge and are being needlessly worried by symptoms that are in fact either “normal” or simply explained.
As women constitute some 50% of the workforce in a large section of the employment arena, and considerably more in some service industries, the consequences of their preventable and correctable health problems levy a significant and avoidable toll on their well-being and productivity and on the organization as well. That toll may be considerably reduced by a worksite health promotion program designed for women.
Worksite Health Promotion for Women
A good deal of health information is provided by newspapers and magazines and on television but much of that is incomplete, sensationalized or geared to the promotion of particular products or services. Too often, in reporting on current medical and scientific advances, the media raise more questions than they answer and even cause needless anxiety. Health care professionals in hospitals, clinics and private offices often fail to make sure that their patients are properly educated about the problems they present, to say nothing of taking the time to inform them about important health issues unrelated to their symptoms.
A properly designed and administered worksite health promotion program should provide accurate and complete information, opportunities to ask questions either in group or individual sessions, clinical preventive services, access to a variety of health promotion activities and counseling about adjustments that may prevent or minimize distress and disability. The worksite offers an ideal venue for the sharing of health experiences and information, particularly when they are relevant to circumstances encountered on the job. One can also take advantage of the peer pressure that is present in the workplace to provide workers with additional motivation for participating and persisting in health promoting activities and in maintaining a healthful lifestyle.
There is a variety of approaches to programming for women. Ernst and Young, the large accounting firm, offered its London employees a series of Health Seminars for Women conducted by an outside consultant. They were attended by all grades of staff and were well received. The women who attended were secure in the format of the presentations. As an outsider, the consultant posed no threat to their employment status, and together they cleared up many areas of confusion about women’s health.
Marks and Spencer, a major retailer in the United Kingdom, conducts a program through its in-house medical department using outside resources to provide services to employees in their many regional worksites. They offer screening examinations and individual advice to all their staff, together with an extensive range of health literature and videotapes, many of which are produced in-house.
Many companies use independent health advisers outside the company. An example in the United Kingdom is the service provided by the BUPA (British United Provident Association) Medical Centers, who see many thousands of women through their network of 35 integrated but geographically scattered units, supplemented by their mobile units. Most of these women are referred through their employers’ health promotion programs; the remainder come independently.
BUPA was probably the first, at least in the United Kingdom, to establish a women’s health centre dedicated to preventive services exclusively for women. Hospital-based and free-standing women’s health centers are becoming more common and are proving attractive to women who have not been well served by the prevailing health care system. In addition to providing prenatal and obstetrical care, they tend to offer broad-ranging primary care, with most placing particular emphasis on preventive services.
The National Survey of Women’s Health Centers, conducted in 1994 by researchers from the Johns Hopkins School of Hygiene and Public Health with support from the Commonwealth Foundation (Weisman 1995), estimated that there are 3,600 women’s health centers in the United States, of which 71% are reproductive health centers providing primarily routine outpatient gynaecological examinations, Pap tests and family planning services. They also provide pregnancy tests, abortion counseling (82%) and abortions (50%), screening and treatment for sexually transmitted diseases, breast examinations and blood pressure checks.
Twelve per cent are primary care centers (these include women’s college health services) which provide basic well-woman and preventive care including periodic physical examinations, routine gynaecological examinations and Pap tests, diagnosis and treatment of menstrual problems, menopausal counseling and hormone replacement therapy, and mental health services, including drug and alcohol abuse counseling and treatment.
Breast centers constitute 6% of the total (see below), while the remainder are centers providing various combinations of services. Many of these centers have demonstrated interest in contracting to provide services to female employees of nearby organizations as part of their worksite health promotion programs.
Regardless of the venue, the success of worksite health promotion programming for women hinges not only on the reliability of the information and services offered but, more important, on the manner in which they are presented. The programs must be sensitized to women’s attitudes and aspirations as well as to their concerns and, while being supportive, they should be free of the condescension with which these problems are so often addressed.
The remainder of this article will focus on three categories of problems regarded as particularly important health concerns for women—menstrual disorders, cervical and breast cancer and osteoporosis. However, in addressing other health categories, the worksite health promotion program should ensure that any other problems of particular relevance for women will not be overlooked.
Menstrual Disorders
For the great majority of women, menstruation is a “natural” process that presents few difficulties. The menstrual cycle may be disturbed by a variety of conditions which may cause discomfort or concern for the employee. These may lead her to take sick absence on a regular basis, often reporting a “cold” or “sore throat” rather than a menstrual problem, especially if the absence certificate is to be submitted to a male manager. However, the absence pattern is obvious and referral to a qualified health professional may resolve the problem rapidly. Menstrual problems that may affect the workplace include amenorrhoea, menorrhagia, dysmenorrhoea, the premenstrual syndrome (PMS) and menopause.
Amenorrhoea
While amenorrhoea may create concern, it does not ordinarily affect work performance. The most common cause of amenorrhoea in younger women is pregnancy and in older women it is menopause or a hysterectomy. However, it may also be attributable to the following circumstances:
- Poor nutrition or underweight. The reason for poor nutrition may be socioeconomic in that little food is available or affordable, but it may also be the result of self-starvation related to eating disorders such as anorexia nervosa or bulimia.
- Excessive exercise. In many developed countries. women train excessively in physical fitness or sports programmes. Even though their food intake may be adequate, they may have amenorrhoea.
- Medical conditions. Problems arising from hypothyroidism or other endocrine disorders, tuberculosis, anaemia from any cause and certain serious, life-threatening diseases can all cause amenorrhoea.
- Contraceptive measures. Medications containing progesterone only will commonly lead to amenorrhoea. It should be noted that sterilization without цphorectomy does not cause a woman’s periods to stop.
Menorrhagia
In the absence of any objective measure of menstrual flow, it is commonly accepted that any flow of menses which is heavy enough to interfere with a woman’s normal day-to-day activities, or which leads to anemia, is excessive. When the flow is heavy enough to overwhelm the normal circulating anti-clotting factor, the woman with “heavy periods” may complain of passing clots. Inability to control the blood flow by any normal sanitary protection can lead to considerable embarrassment in the workplace and may lead to a pattern of regular, monthly one- or two-day absences.
Menorrhagia may be caused by uterine fibroids or polyps. It can also be caused by an intrauterine contraceptive device (IUD) and, rarely, it may be the first indication of a severe anemia or other serious blood disorder such as leukaemia.
Dysmenorrhoea
Although the vast majority of menstruating women experience some discomfort at the time of menstruation, only a few have pain sufficient to interfere with normal activity and, thus, require referral for medical attention. Again, this problem may be suggested by a pattern of regular monthly absences. Such difficulties associated with menstruation may for certain practical purposes be classified thus:
- Primary dysmenorrhoea. Young women with no evidence of disease may suffer pain on the day before or on the first day of their period that is serious enough to induce them to take time off from work. Although no cause has been found, it is known to be associated with ovulation and, hence, can be prevented by the oral contraceptive pill or by other medication which prevents ovulation.
- Secondary dysmenorrhoea. The onset of painful periods in a woman in her middle thirties or later suggests pelvic pathology and should be fully investigated by a gynaecologist.
It should be noted that some over-the-counter or prescribed analgesics taken for dysmenorrhoea may cause drowsiness and can present a problem for women working in jobs that require alertness to occupational hazards.
Premenstrual syndrome
Premenstrual syndrome (PMS), a combination of physical and psychological symptoms experienced by a relatively small percentage of women during the seven or ten days prior to menstruation, has developed its own mythology. It has falsely been credited as the cause of women’s so-called emotionalism and “flightiness”. According to some men, all women suffer from it, while ardent feminists claim that no women have it. In the workplace, it has improperly been cited as a rationale for keeping women out of positions requiring decision making and the exercise of judgment, and it has served as a convenient excuse for denying women promotion to managerial and executive levels. It has been blamed for women’s problems with interpersonal relations and, indeed, in England it has provided the grounds for pleas of temporary insanity that enabled two separate female defendants to escape charges of murder.
The physical symptoms of PMS may include abdominal distention, breast tenderness, constipation, sleeplessness, weight gain due to increased appetite or to sodium and fluid retention, fine-movement clumsiness and inaccuracy in judgment. The emotional symptoms include excessive crying, temper tantrums, depression, difficulty in making decisions, an inability to cope in general and a lack of confidence. They always occur in the premenstrual days, and are always relieved by the onset of the period. Women taking the combined oral contraceptive pill and those who have had oophorectomies rarely get PMS.
The diagnosis of PMS is based on the history of its temporal relationship to menstrual periods; in the absence of definitive causes, there are no diagnostic tests. Its treatment, the intensity of which is determined by the intensity of the symptoms and their effect on normal activities, is empirical. Most cases respond to simple self-help measures which include abolishing caffeine from the diet (tea, coffee, chocolate and most cola soft drinks all contain significant amounts of caffeine), frequent small feedings to minimize any tendency to hypoglycemia, restricting sodium intake to minimize fluid retention and weight gain, and regular moderate exercise. When these fail to control the symptoms, physicians may prescribe mild diuretics (for two to three days only) that control sodium and fluid retention and/or oral hormones that modify ovulation and the menstrual cycle. In general, PMS is treatable and should not represent a significant problem to women in the workplace.
Menopause
Menopause reflecting ovarian failure may occur in women in their thirties or may be postponed to well beyond the age of 50; by the age of 48, about half of all women will have experienced it. The actual time of the menopause is influenced by general health, nutrition and familial factors.
The symptoms of the menopause are diminished frequency of periods usually coupled with scanty menstrual flow, hot flushes with or without night sweats, and a diminution in vaginal secretions, which may cause pain during sexual intercourse. Other symptoms frequently attributed to the menopause include depression, anxiety, tearfulness, lack of confidence, headaches, changes in skin texture, loss of sexual interest, urinary difficulties and sleeplessness. Interestingly, a controlled study involving a symptom questionnaire administered to both men and women showed that a significant portion of these complaints were shared by men of the same age (Bungay, Vessey and McPherson 1980).
The menopause, coming as it does at about the age of 50, may coincide with what has been called the “mid-life transition” or the “mid-life crisis”, terms coined to denote collectively the experiences which seem to be shared by both men and women in their middle years (if anything, they appear to be more common among men). These include loss of purpose, dissatisfaction with one’s job and with life in general, depression, waning interest in sexual activity and a tendency to diminished social contacts. It may be precipitated by the loss of spouse or partner through separation or death or, as regards one’s job, by failure to win an expected promotion or by separation, whether by termination or voluntary retirement. In contrast to menopause, there is no known hormonal basis for the mid-life transition.
Particularly in women, this period may be associated with the “empty nest syndrome,” the sense of purposelessness that may be felt when, their children having left the home, their whole perceived raison d’être seems to have been lost. In such cases, the job and the social contacts in the workplace often provide a stabilizing, therapeutic influence.
Like many of the other “female problems,” menopause has developed its own mythology. Preparatory education debunking these myths supplemented by sensitive supportive counseling will go far to preventing significant dislocations. Continuing to work and maintaining her satisfactory performance on the job may be of crucial value in sustaining a woman’s well-being at this time.
It is at this point that the advisability of hormone replacement therapy (HRT) needs to be considered. Currently the subject of some controversy, HRT was originally prescribed to control menopausal symptoms if they became excessively severe. While usually effective, the hormones commonly used often precipitated vaginal bleeding and, more important, they were suspected of being carcinogenic. As a result, they were prescribed only for limited periods of time, just long enough to control the troublesome menopausal symptoms.
HRT has no effect on the symptoms of the mid-life transition. However, if a woman’s flushes are controlled and she can get a good night’s sleep because her night sweats are prevented, or if she can respond to lovemaking more enthusiastically because it is no longer painful, then some of her other problems may be resolved.
Today, the value of long-term HRT is increasingly being recognized in maintaining the integrity of bone in women with osteoporosis (see below) and in reducing the risk of coronary heart disease, now the highest-ranking cause of death among women in industrialized countries. Newer hormones, combinations and sequences of administration may eliminate the occurrence of planned vaginal bleeding and there appears to be little or no risk of carcinogenesis, even among women with a history of cancer. However, because many physicians are strongly biased for or against HRT, women need to be educated about its benefits and disadvantages so that they can participate confidently in the decision about whether to use it or not.
Recently, calling to mind the millions of women “baby boomers” (children born after the Second World War) who will be reaching the age of menopause within the next decade, the American College of Obstetricians and Gynecologists (ACOG) warned that staggering increases in osteoporosis and heart disease could result unless women are better educated about menopause and the interventions designed to prevent disease and disability and to prolong and enhance their lives after menopause (Voelker 1995). ACOG president William C. Andrews, MD, has proposed a three-pronged program that includes a massive campaign to educate physicians about the menopause, a “perimenopausal visit” to a physician by all women over the age of 45 for a personal risk assessment and in-depth counseling, and involvement of the news media in educating women and their families about the symptoms of menopause and the benefits and risks of treatments like HRT before women reach menopause. The worksite health promotion program can make a major contribution to such an educational effort.
Screening for Cervical and Breast Disease
With regard to women’s needs, a health promotion program should either provide or, at least, recommend periodic screening for cervical and breast cancer.
Cervical disease
Regular screening for precancerous cervical changes by means of the Pap test is a well-established practice. In many organizations, it is made available in the workplace or in a mobile unit brought to it, eliminating the need for female employees to spend time traveling to a facility in the community or visiting their personal physicians. The services of a physician are not required in the administration of this procedure: satisfactory smears may be taken by a well-trained nurse or technician. More important is the quality of the reading of the smears and the integrity of the procedures for record-keeping and reporting of the results.
Breast cancer
Although breast screening by mammography is widely practiced in almost all developed countries, it has been established on a national basis only within the United Kingdom. Currently, over a million women in the United Kingdom are screened, with each woman aged 50 to 64 having a mammogram every three years. All the examinations, including any further diagnostic studies needed to clarify abnormalities in the initial films, are free of charge to the participants. The response to the offer of this three-year cycle of mammography has been over 70%. Reports for the 1993-1994 period (Patnick 1995) show a rate of 5.5% for referral to further assessment; 5.5 women per 1,000 women screened were discovered to have breast cancer. The positive predictive value for surgical biopsy was 70% in this program, compared to some 10% in programs reported elsewhere in the world.
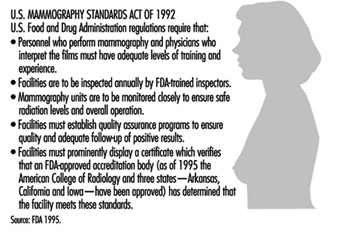
The critical issues in mammography are the quality of the procedure, with particular emphasis on minimizing radiation exposure, and the accuracy of the interpretation of the films. In the United States, the Food and Drug Administration (FDA) has promulgated a set of quality regulations proposed by the American College of Radiology that, commencing October 1, 1994, must be observed by the more than 10,000 medical units taking or interpreting mammograms around the country (Charafin 1994). In accordance with the national Mammography Standards Act (enacted in 1992), all mammography facilities in the United States (except those operated by the Department of Veterans Affairs, which is developing its own standards) had to be certified by the FDA as of this date. These regulations are summarized in figure 1.
Figure 1. Mammography quality standards in the United States.
A recent phenomenon in the United States is the increase in the number of breast or breast health centers, 76% of which have appeared since 1985 (Weisman 1995). They are predominantly hospital-affiliated (82%); the others are primarily profit-making enterprises owned by physician groups. About a fifth maintain mobile units. They provide outpatient screening and diagnostic services including physical breast examinations, screening and diagnostic mammography, breast ultrasound, fine-needle biopsy and instruction in breast self-examination. Slightly more than one-third also offer treatment for breast cancer. While primarily focused on attracting self-referrals and referrals by community physicians, many of these centers are making an effort to contract with employer- or labor union-sponsored health promotion programs to provide breast screening services to their female participants.
Introducing such screening programs into the workplace can generate considerable anxiety among some women, particularly those with personal or family histories of cancer and those found to have “abnormal” (or inconclusive) results. The possibility of such non-negative results should be carefully explained in presenting the program, along with the assurance that arrangements are in place for the additional examinations needed to explain and to act upon them. Supervisors should be educated to sanction absences by these women when the necessary follow-up procedures cannot be expeditiously arranged outside of working hours.
Osteoporosis
Osteoporosis is a metabolic bone disorder, much more prevalent in women than in men, that is characterized by a gradual decline in bone mass leading to susceptibility to fractures which may result from seemingly innocuous movements and accidents. It represents an important public health problem in most developed countries.
The most common sites for fractures are the vertebrae, the distal portion of the radius and the upper portion of the femur. All fractures at these sites in older individuals should cause one to suspect osteoporosis as a contributing cause.
While such fractures usually occur later in life, after the individual has left the workforce, osteoporosis is a desirable target for worksite health promotion programs for a number of reasons: (1) the fractures may involve retirees and add significantly to their medical care costs, for which the employer may be responsible; (2) the fractures may involve the elderly parents or in-laws of current employees, creating a dependant-care burden that can compromise their attendance and work performance; and (3) the workplace presents an opportunity to educate younger people about the eventual danger of osteoporosis and to urge them to initiate the lifestyle changes that can slow its progress.
There are two types of primary osteoporosis:
- Post-menopausal, which is related to loss of oestrogens and, hence, is more prevalent in women than in men (ratio = 6:1). It is commonly found in the 50-to-70 age group and is associated with vertebral fractures and Colles fractures (of the wrist).
- Involutional, which occurs mainly in those over the age of 70 and is only twice as common among women than in men. It is thought to be due to age-related changes in vitamin D synthesis and is associated chiefly with vertebral and femoral fractures.
Both types may be present simultaneously in women. In addition, in a small percentage of cases, osteoporosis has been attributed to a variety of secondary causes including: hyperparathyroidism; the use of corticosteroids, L-thyroxine, aluminum-containing antacids and other drugs; prolonged bed rest; diabetes mellitus; the use of alcohol and tobacco; and rheumatoid arthritis.
Osteoporosis may be present for years and even decades before fractures result. It can be detected by well-standardized x-ray measurements of bone density, calibrated for age and sex, and supplemented by laboratory evaluation of calcium and phosphorus metabolism. Unusual radiolucency of bone in conventional x rays may be suggestive, but such osteopenia usually cannot be reliably detected until more than 30% of the bone is lost.
It is generally agreed that screening asymptomatic individuals for osteoporosis should not be employed as a routine procedure, especially in worksite health promotion programs. It is costly, not very reliable except in the most well-staffed facilities, involves exposure to radiation and, most important, does not identify those women with osteoporosis who are most likely to have fractures.
Accordingly, although everyone is subject to some degree of bone loss, the prevention program for osteoporosis is focused on those individuals who are at higher risk for its more rapid progression and who are therefore more susceptible to fractures. A special problem is that although the earlier in life the preventive measures are started, the more effective they are, it is nonetheless difficult to motivate younger people to adopt lifestyle changes in the hope of avoiding a health problem that may develop at what many of them consider to be a very remote age of life. A saving grace is that many of the recommended changes are also useful in the prevention of other problems as well as in promoting general health and well-being.
Some risk factors for osteoporosis cannot be changed. They include:
- Race. On average, Whites and Orientals have lower bone density than Blacks matched age for age and are therefore at greater risk.
- Sex. Women have less dense bones than men when matched for age and race and therefore are at greater risk.
- Age. All people lose bone mass with age. The stronger the bones are in youth, the less likely is it that the loss will reach potentially dangerous levels in old age.
- Family history. There is some evidence of a genetic component in the attainment of peak bone mass and the rate of subsequent bone loss; thus, a family history of suggestive fractures in family members may represent an important risk factor.
The fact that these risk factors cannot be altered makes it important to give attention to those that can be modified. Among the measures that may be taken to delay the onset of osteoporosis or to diminish its severity, the following may be mentioned:
- Diet. If adequate amounts of calcium and vitamin D are not present in the diet, supplementation is recommended. This is particularly important for people with lactose intolerance who tend to avoid milk and milk products, the major sources of dietary calcium, and is most effective if maintained from childhood until the thirties as peak bone density is being achieved. Calcium carbonate, the most commonly used form of calcium supplementation, frequently causes side effects such as constipation, rebound hyperacidity, abdominal bloating and other gastrointestinal symptoms. Accordingly, many people substitute preparations of calcium citrate which, despite a significantly lower content of elemental calcium, is better absorbed and has fewer side-effects. The amounts of vitamin D present in the usual multivitamin preparation suffice for slowing the bone loss of osteoporosis. Women should be cautioned against excessive doses, which may lead to hypervitaminosis D, a syndrome that includes acute renal failure and increased resorption of bone.
- Exercise. Regular moderate weight-bearing exercise-for example, 45 to 60 minutes of walking at least three times a week-is advisable.
- Smoking. Women who smoke have their menopause on average two years earlier than non-smokers. Without hormone replacement, the earlier menopause will accelerate post-menopausal bone loss. This is another important reason to counter the current trend to increased cigarette smoking among women.
- Hormone replacement therapy. If oestrogen replacement is undertaken, it should be started early in the progress of the menopausal changes since the rate of bone loss is greatest during the first few years after menopause. Because bone loss is resumed after the discontinuation of oestrogen therapy, it should be maintained indefinitely.
Once osteoporosis is diagnosed, treatment is aimed at circumventing further bone loss by following all of the above recommendations. Some recommend using calcitonin, which has been shown to increase total body calcium. However, it must be given parenterally; it is expensive; and there is yet no evidence that it retards or reverses the loss of calcium in the bone or reduces the occurrence of fractures. Biphosphonates are gaining ground as anti-resorptive agents.
It must be remembered that osteoporosis sets the stage for fractures but it does not cause them. Fractures are caused by falls or sudden injudicious movements. While the prevention of falls should be an integral part of every worksite safety program, it is particularly important for individuals who may have osteoporosis. Thus, the health promotion program should include education about safeguarding the environment in both the workplace and in the home (e.g., eliminating or taping down trailing electrical wires, painting the edges of steps or irregularities in the floor, tacking down slippery rugs and promptly drying up any wet spots) as well as sensitizing individuals to such hazards as insecure footwear and seats that are difficult to get out of because they are too low or too soft.
Women’s Health and Their Work
Women are in the paid workforce to stay. In fact, they are the mainstay of many industries. They should be treated as equal to men in every respect; only some aspects of their health experience are different. The health promotion program should inform women about these differences and empower them to seek the kind and quality of health care they need and deserve. Organizations and those who manage them should be educated to understand that most women do not suffer from the problems described in this article, and that, for the small proportion of women who do, prevention or control is possible. Except in rare instances, no more frequent than among men with similar health problems, these problems do not constitute barriers to good attendance and effective work performance.
Many women managers get to their high positions not only because their work is excellent, but because they experience none of the problems of female health that have been outlined above. This can make some of them intolerant and unsupportive of other women who do have such difficulties. One major area of resistance to women’s status in the workplace, it appears, can be women themselves.
A worksite health promotion program that embodies a focus on women’s health issues and problems and addresses them with appropriate sensitivity and integrity can have an important positive impact for good, not only for the women in the workforce, but also for their families, the community and, most important, the organization.
Mammography Programme at Marks and Spencer: A Case Study
This case study describes the mammography program at Marks and Spencer, the first to be offered by an employer on a nationwide scale. Marks and Spencer is an international retail operation with 612 stores worldwide, the majority being in the United Kingdom, Europe and Canada. In addition to a number of international franchise operations, the company owns Brooks Brothers and Kings Super Markets in the United States and D’Allaird’s in Canada and pursues extensive financial activities.
The company employs 62,000 people, the majority of whom work in 285 stores in the United Kingdom and the Republic of Ireland. The company’s reputation as a good employer is legendary and its policy of good human relations with staff has included the provision of comprehensive, high-quality health and welfare programs.
Although a treatment service is provided at some work locations, this need is largely met by community-based primary care physicians. The company health policy emphasizes the early detection and prevention of disease. A number of innovative screening programs have consequently been developed over the past 20 years, many of which have predated similar projects in the National Health Service (NHS). Over 80% of the workforce is female, a fact that has influenced the choice of screening programs, which include cervical cytology, ovarian cancer screening and mammography.
Breast Cancer Screening
In the mid-1970s the New York HIP study (Shapiro 1977) proved that mammography was capable of detecting impalpable breast cancers with the expectation that earlier detection would reduce mortality. To an employer of large numbers of middle-aged women, the appeal of mammography was obvious and a screening program was introduced in 1976 (Hutchinson and Tucker 1984; Haslehurst 1986). At that time there was virtually no access to reliable high-quality mammography in the public sector and that available in private health care organizations was of variable quality and expensive. The first task therefore was to ensure access to a uniformly high quality and this challenge was met by using mobile screening units, each equipped with a waiting area, examination cubicle and mammography equipment.
Centralized administration and film processing allowed continuous checks on all aspects of quality and allowed film interpretation to be undertaken by an experienced group of mammographers. There was, however, a disadvantage in that the radiographer was not able to immediately examine the developed film to verify that there were no technical errors so that if there had been any, the employee could be recalled or other arrangements made for the necessary repeat examination.
Compliance has always been exceptionally high and has remained over 80% for all age groups. Doubtless this is due peer group pressure, the easy availability of the service at or near the worksite and, until recently, a lack of mammography facilities in the NHS.
Women are invited to join the screening program and attendance is entirely voluntary. Prior to screening, short educational sessions are carried out by the company doctor or nurse, both of whom are available to answer queries and give explanations. Common anxieties include concern about radiation dosage and worry that the compression of the breast may cause pain. Women who are recalled for further tests are seen during working hours and fully recompensed for travel expenses for themselves and a companion.
Three modalities were used for the first five years of the program: clinical examination by a highly trained nurse-practitioner, thermography and mammography. Thermography was a time-consuming examination with a high rate of false positives and made no contribution to the cancer detection rate; accordingly it was discontinued in 1981. Although of limited value in cancer detection, clinical examination, which includes a detailed review of personal and family history, provides invaluable information to the radiologist and allows the client time to discuss her fears and other health issues with a sympathetic health professional. Mammography is the most sensitive of the three tests. Cranio-caudal and lateral oblique views are taken at the initial examination with single views only at the interval check. Single reading of films is the norm, though double reading is used for difficult cases and as a random quality check. Figure 1 shows the contribution of clinical examination and mammography to the total cancer detection rate. Of the 492 cases of cancer found, 10% were detected by clinical examination alone, 54% by mammography alone, and 36% were noted by clinical examination and mammography.
Figure 1. Screening for breast cancer. Contribution of clinical examination and mammography to cancer detection, by age group.
Women aged 35 to 70 were offered screening when the program was first introduced but the low cancer detection rate and high incidence of benign breast disease among those in the 35 to 39 age group led to withdrawal of the service in 1987 from these women. Figure 19 shows the numbers of screen-detected cancers by age group.
Figure 2. Age distribution of screen-detected cancers.
Similarly, the screening interval has changed from a yearly interval (reflecting initial enthusiasm) to a two-year gap. Figure 3 shows the number of screen-detected cancers by age group with the corresponding numbers of interval tumors and missed tumors. Interval cases are defined as those occurring after a truly negative screen during the time between routine tests. Missed cases are defined as those cancers which can be seen retrospectively on the films but were not identified at the time of the screening test.
Figure 3. Number of screen-detected cancers, interval cancers and missed cancers, by age group.
Among the screened population, 76% of breast cancers were detected at screening with a further 14% of cases occurring during the interval between examinations. The interval cancer rate will be carefully monitored to ensure that it does not rise to an unacceptably high level.
The survival benefit of screening women under the age of 50 remains unproven although it is agreed that smaller cancers are detected and this allows some women to choose between mastectomy or breast conservation therapy—a choice valued highly by many. Figure 4 shows the sizes of screen-detected cancers, the majority being under two centimeters in size and node negative.
Figure 4. Sizes of screen-detected cancers.
Impact of the Forrest Report
In the late 1980s, Professor Sir Patrick Forrest recommended that regular breast screening be made available to women over the age of 50 via the NHS (i.e., with no charge at the point of delivery of the service) (Forrest 1987). His most important recommendation was that the service should not start until specialist staff had been fully trained in the multidisciplinary approach to breast care diagnosis. Such staff was to include radiologists, nurse counselors and breast physicians. Since 1990, the United Kingdom has had an outstanding breast screening and assessment service for women over 50.
Coincidentally with this national development, Marks and Spencer reviewed its data and a major flaw in the program became apparent. The recall rate following routine screening was in excess of 8% for women over fifty and 12% for younger women. Analysis of the data showed that common reasons for recall were technical problems, such as malpositioning, processing errors, difficulties with grid lines or a need for further views. Additionally, it was clear that the use of ultrasonography, specialized mammography and fine needle aspiration cytology could cut the recall and referral rate even further. An initial study confirmed these impressions, and it was decided to redefine the screening protocol so that clients who needed further tests were not referred back to their family practitioners, but were retained within the screening program until a definitive diagnosis was made. Most of these women were returned to a schedule of routine recall after the further investigations and this reduced the formal surgical referral rate to a minimum.
Instead of duplicating the service provided by the National Health Service, a policy of partnership was developed which allowed Marks and Spencer to draw upon the expertise of the public sector while company funding is used to improve service for all. The breast screening program is now delivered by a number of providers: about half the requirement is met by the original mobile service but employees at the larger city stores now receive routine screening at specialist centers, which may either be in the private or public sectors. This cooperation with the National Health Service has been an exciting and challenging development and has helped to improve the overall standards of breast diagnosis and care for the entire population. By marrying together both private worksite and public sector programs it is possible to deliver an exceptionally high quality service to a widely distributed population.
Worksite Strategies to Improve Maternal and Infant Health: Experiences of US Employers
There is a growing awareness among public and private sector employers in the United States that healthy birth outcomes, productivity and the organization’s economic status are connected. Concurrently, there is heightened concern about occupational reproductive health hazards. Never before have employers had better reasons to improve maternal and infant health among employees and their families. Rising health care costs, changing workforce demographics, and increasing evidence that healthy employees lead to productivity gains, are compelling reasons to make maternal and infant health an addition to their health education and promotion programs.
A maternal and infant health strategy is a term broadly used to define any thoughtfully planned employer-sponsored or union-sponsored initiative that promotes the health and well-being of women, before, during, and after pregnancy, and supports the health of infants during the first year of life as well. There is no single solution or approach to improving maternal and infant health. Rather, for most employers, the effort is a combination of the following activities, custom-fit to meet the environment that makes their workplace unique.
Health Care Benefits
It is helpful to view maternal and infant health care benefits as a continuum of care that provides reproductive health awareness and family planning counseling and services throughout the reproductive life span. The benefits listed in table 1 represent those a health insurance plan should cover because of their significance in improving maternal and infant health.
Table 1. Health insurance benefits.
|
Pre-pregnancy |
Pregnancy |
Post-pregnancy |
Infancy |
|
Annual preconception or interconception care visit (includes family planning services) Genetic counseling and testing Prescription drug plan Substance abuse treatment |
Genetic counseling and testing Prenatal care–should be offered with no deductibles or copayments Labor and delivery at a hospital or birthing centre should be offered with no deductibles or copayments
|
Postpartum care Prescription drug plan Home health care services Substance abuse treatment |
Normal newborn nursery care Neonatal intensive care–no pre-existing conditions exclusions for newborns Prescription drug plan Home health care services |
Source: March of Dimes Birth Defects Foundation 1994.
Benefits design
While many American health care plans provide coverage for preconception and prenatal care, there are a number of reasons why it may be difficult for some women to obtain high quality, affordable care. For example, some providers require payment in advance for prenatal care and delivery services, yet most insurers will not make payment until after delivery. Other barriers to accessing proper care include high deductible fees or copayments, inconvenient office hours, lack of coverage for dependants, and geographic inaccessibility. Employers cannot eliminate all of these barriers, but it would represent an excellent beginning to help remove the burdens of upfront payments and high deductible fees and to offer assistance to the employee in finding acceptance by a suitable provider of prenatal care.
At Texas Instruments (TI), the goal is to make prenatal care affordable regardless of an employee’s income level or health care provider. Mothers seeking prenatal care inside the TI network pay only 10% of an upfront negotiated fee, a single charge that covers prenatal care services and both uncomplicated deliveries and Caesarean sections.
The Haggar Apparel Company pays 100% of the cost of prenatal care upfront if an employee or dependant accesses prenatal care in the first trimester of pregnancy. The Home Depot (a retailer of builder’s wares and related merchandise) waives the expectant mother’s hospital deductible fee if prenatal care visits begin in the first trimester.
While many plans provide for adequate care for a newborn’s first few days of life, coverage for the infant’s ongoing preventive care after leaving the hospital, frequently referred to as well-baby care, is often inadequate or nonexistent.
At the First National Bank of Chicago, expectant mothers who are enrolled in the indemnity plan and who complete a prenatal education program by the end of their fourth month of pregnancy have the $400 deductible charge waived from their newborn’s first year health insurance coverage. The Monfort Company, a beef packing plant in Greeley, Colorado, totally covers well-baby care up to age three.
Benefits-related Services and Employee Programs
Table 2 lists benefits-related services and programs that are considered important supportive features to a maternal and infant health strategy. These services and programs may be provided directly by the employer, either in the workplace or a nearby location, or under a contract with an outside agency or vendor, depending on the structure, location and size of the organization and may be administered by the benefits, employee health, health promotion or employee assistance department, for example.
Few companies can offer all of these components; however, the more complete and comprehensive the strategy, the better the chance of improving the health of mothers and babies.
Table 2. Other benefits-related services provided by the employer.
|
SERVICES |
|||
|
Pre-pregnancy |
Pregnancy |
Post-pregnancy |
Infancy |
|
|
||
|
PROGRAMMES |
|||
|
Pre-pregnancy |
Pregnancy |
Post-pregnancy |
Infancy |
|
|
|
|
Source: March of Dimes Birth Defects Foundation 1994.
Pre-pregnancy and pregnancy period
Maternity management programs are gaining popularity because they offer attractive features to both the expectant parents and the employer. While not designed to replace prenatal care delivered by a health care professional, maternity management is a benefit-related service that provides personalized advice and support customized to a mother’s needs and risk levels.
Levi Strauss & Company, one of the nation’s largest clothing and apparel producers, offers a maternity management program administered by an insurance company. Employees are encouraged to access the program as soon as they are pregnant and they will receive $100 cash for calling the toll-free maternity management number. In 1992, costs for newborns whose mothers participated in the program were nearly 50% lower than for those whose mothers who did not.
The First National Bank of Chicago offers the March of Dimes Babies and You prenatal health promotion program as part of its maternal and infant health strategy. This program is described below and in the case study on p. 15.23 above.
Babies and You: A prenatal health promotion program
The March of Dimes’ Babies and You prenatal health promotion program was developed in 1982 in partnership with maternal and infant health care specialists throughout the country. Extensively field-tested by March of Dimes chapters and worksites, the program is continuously updated and enhanced.
Babies and You educates adults about how to practice healthy lifestyle behaviors before and during pregnancy, motivates women to get early and regular prenatal care, and influences employers to implement strategies that support healthy pregnancy outcomes.
Prenatal health promotion activities should be reaching male as well as female employees, partners, other family members and friends. Babies and You is adaptable to the unique needs of any given workforce. Consideration is given to the educational level, culture and language of prospective participants, as well as to any worksite restrictions and available community resources.
Because employers are at different stages in their health promotion activities, Babies and You offers three levels of implementation: an information campaign, educational seminars, and training of health professionals (see box). The most popular topics for informational materials and educational seminars are preconception and prenatal care, fetal development, genetics, the male role in pregnancy, nutrition during pregnancy, and parenting. The topics covered in the prenatal programs of 31 companies surveyed by the New York Business Group on Health found the dominant themes to be understanding what goes on during pregnancy and delivery; timely care by qualified health professionals; practicing healthy behaviors related to pregnancy and avoidance of hazards that might affect mother and/or fetus; care of the newborn; and maintaining satisfactory family and work relationships (Duncan, Barr and Warshaw 1992).
BABIES AND YOU: Levels of Implementation
Level I Informational Campaign is designed to create awareness at the worksite about the importance of early and regular prenatal care. To sustain this level of implementation, a variety of print and audiovisual materials is available from the March of Dimes.
Level II Educational Seminars are delivered at the worksite by March of Dimes volunteer health professionals. Fourteen different seminar topics are available to choose from, including: preconception care, prenatal care, nutrition, exercise and pregnancy, pregnancy after 35, stress and pregnancy, pregnancy complications, well-baby care, male role in pregnancy, and breastfeeding.
Level III Training of Health Professionals allows a worksite to establish Babies and You as an on-going component of its wellness activities. The March of Dimes provides a one-day training on program delivery and implementation to on-site health professionals such as occupational health nurses, benefits managers, medical directors and health promotion specialists.
But no matter what level of Babies and You a worksite chooses to implement, there are eight goals of a successful prenatal health promotion effort that this program strives to achieve:
- Management commitment
- Inter-departmental program planning
- Employee input
- The offering of incentives
- Supportive benefits and policies
- Establishment of communications channels
- Access to community resources
- Evaluation
Post-pregnancy and infancy period
In addition to implementing health promotion programs and other services that focus on a mother’s health before and during pregnancy, many employers also offer programs that support parents and infants after pregnancy, during the critical first twelve months and beyond. Maternity disability benefits, lactation programs, dependant care reimbursement accounts (e.g., pre-tax set-asides of earnings that employees may draw on to pay for dependant care expenses), parenting classes and onsite child care are just a few of the benefits and programs now offered.
For example, to maintain goodwill with its employees, Lancaster Laboratories, based in Lancaster, Pennsylvania, and providing contract laboratory research and consulting to the environmental, food and pharmaceutical industries, continues to provide health care insurance benefits during both maternity disability leave and unpaid parental leave whether or not the employee plans to return to work after having given birth. This family-supportive management approach has gotten results: in an industry where a 27% turnover rate is the norm, the rate at Lancaster is only 8% (March of Dimes 1994).
Lactation programs also are easy and beneficial for employers to implement. The health benefits of breastfeeding extend beyond the child’s own. A recent study shows that improving an infant’s health through breastfeeding has a direct effect on employee productivity. Healthier infants mean mothers and fathers miss significantly fewer days of work to care for a sick child (Ryan and Martinez 1989). Offering a lactation program simply requires providing onsite space and equipment for pumping and storing breast milk.
The Los Angeles Department of Water and Power was able to quantify some benefits of its lactation program: for example, 86% of participants state that the program eased their transition back to work; 71% report taking less time off since participating; and program participants have a 2% turnover rate (March of Dimes 1994).
Employer Policies
There are many workplace policies that employers can initiate to create a maternal and infant-health supportive culture. Instituting new policies and changing old ones can send an important message to employees about the company’s corporate culture.
Some policies affect the health of all workers, like creating a smoke-free environment. Others focus on selected groups, such as those that address occupational reproductive health hazards and which are targeted to meet the needs of men and women who are planning to have a child. Still more, including flexible work policies, support pregnant women in scheduling prenatal visits and ease the burden of parents with infants and small children. Finally, policies relating to modifying work assignments when needed during pregnancy and resolving questions of disability and its duration help to protect the health of the pregnant worker while minimizing interference with her work assignments.
When the Warner-Lambert Company, a leader in the pharmaceutical, consumer health care and confectionary products industries, initiated its maternity management and prenatal education programs, the company also introduced comprehensive guidelines for managing reproductive health. The guidelines encourage employees to complete questionnaires assessing the potential of reproductive health hazards in their jobs or worksites. If necessary, a Warner-Lambert safety engineer will conduct an assessment to determine what, if any, control of workplace hazards or job restrictions may be necessary.
In addition to reproductive health hazards policies, a number of employers offer flexible family leave policies. For example, at AT&T, the communications giant, employees can take up to 12 months of unpaid leave to care for a newborn or adopted child. More than 50% of the employees who have taken advantage of this leave policy since 1990 returned to work within three months. Within six months, 82% of the employees were back at work (March of Dimes 1994).
And at PepsiCo Inc., the large beverage and food conglomerate based in Purchase, New York, fathers of newborns can take up to eight weeks of paid leave and an additional eight weeks of unpaid leave with a guarantee of the same or a comparable job when they return (March of Dimes 1994).
Designing a Maternal and Infant Health Strategy to Meet Business Needs
Any sustainable employer-based maternal and infant health strategy, in addition to being acceptable to employees, must meet sound business objectives. Depending on a company’s objectives, different benefits, employee programs, or policies may take priority. The following steps are useful in developing a preliminary strategy:
- Document existing benefits, programmes, and policies that support maternal and infant health in order to create the foundation of a formal strategy.
- Find out about community resources available to assist the company’s efforts.
- Prepare a prioritized list of preliminary maternal and infant health initiatives which includes changes or introductions in benefits, programmes, or policies.
- Gain preliminary support from top management before taking the next step.
- Assess perceived needs and test proposed strategies with employees to validate preliminary recommendations.
- Develop a formal maternal and infant health strategy by articulating a mission, outlining objectives, allocating the resources needed, identifying potential obstacles and key players, preparing an implementation timetable and gaining necessary support at all levels of the company.
Implementing maternal and infant health initiatives
The next step is to implement the benefits, programs and policies that are part of the strategy. The implementation process typically includes the following steps:
- Assign responsibility for implementation.
- Select quality measurements by which to manage the programme.
- Evaluate and select vendors.
- Review incentives and other methods to increase employee participation.
- Communicate initiatives to employees and family members.
Managing the success of a maternal and infant health strategy
After implementation, an employer’s maternal and infant health strategy should be reviewed for effectiveness in meeting original objectives and business needs. Evaluation and feedback are essential and help to ensure that the maternal and infant health initiatives are meeting both the employer’s and employees’ needs.
Mother and Child Health in France
Shortly after World War II, France instituted Protection maternelle et infantile (PMI), a nationwide system through which public and private health professionals, in collaboration with social services, provide basic preventive health, medical, social and educational services to pregnant women, infants and children through to the age of six.
For the most part, families and private physicians arrange individually for preconception counseling, family planning, early and regular prenatal care and preventive health examinations and vaccinations for children up to the age of six. Participation in the program is encouraged through 100% reimbursement by national health insurance (in order to qualify for this coverage, women must register their pregnancies by the 15th week of gestation), monthly (family) allowance payments from a woman’s fourth month of gestation through to the child’s third month of life as an incentive for compliance with the national guidelines for preventive care, and a continuing program of information and education.
Women not able to participate in care via the private sector are covered by 96 locally controlled PMI centers, one in each French département. In addition to providing free neighborhood health clinics, these centers identify and target for intervention pregnant women and children at risk, conduct home visits and monitor the progress of all women and infants to ensure that the preventive services called for in the national guidelines are received.
The employers’ role in this system is regulated by law. They provide pregnant women with:
- Job changes; flexible hours to ease commuting burdens and rest periods in order to reduce the stress and fatigue that may lead to premature delivery
- Maternity leave with job security for mothers who bear or adopt children to promote bonding and healthy child development (a maternity benefit amounting to 84% of the salary, is paid by social security up to a ceiling)
- Part-time work arrangements and unpaid parental leave with job security to enable parents to balance child care and work responsibilities (a national parental allowance helps to offset the cost of the unpaid leave) (Richardson 1994)
Conclusion
The need to address maternal and infant health in the American workplace will increase as more and more women enter the labor force and as family and workplace issues become inseparable. Forward-thinking companies have already recognized this and are developing innovative approaches. Employers are in a unique and powerful position to influence change and become leaders in promoting healthy mothers and babies.
HIV/AIDS Education
As the epidemic of HIV infection worsens and spreads, increasing numbers of workplaces, labour unions, employers and employees are being affected by the threat of HIV infection and AIDS (collectively to be termed HIV/AIDS). The effects are often particular and highly visible; they can also be insidious and somewhat hidden. Over the relatively brief lifetime of the HIV epidemic, the direct and indirect consequences of AIDS for the business sector and for the workplace in general (as distinguished from its health care aspect), remain for the most part a peripherally acknowledged component of the severity and magnitude of AIDS.
The attitudes and opinions of employees about AIDS are of pivotal importance, and must be assessed if a workplace programme is to be planned and managed effectively. Employee ignorance and misinformation can represent major obstacles to an educational programme, and if misjudged or handled poorly, can lead to distrust and disruption, and can aggravate already-prevalent biases and fears about AIDS.
In the United States, “AIDS has generated more individual lawsuits across a broad range of health issues than any other disease in history”, notes Lawrence Gostin of the HIV Litigation Project. A 1993 national survey of employee attitudes about AIDS by the National Leadership Coalition on AIDS reports that many working Americans continue to hold negative and potentially discriminatory attitudes toward HIV-infected co-workers, and the survey finds that most employees either don’t know how their employers would react to HIV- or AIDS-related situations in their workplaces, or they think that their employer would dismiss an employee with HIV infection at the first sign of illness. Discriminating against employees based solely on disability is expressly forbidden in the United States by the Americans with Disabilities Act (ADA), which includes under its protection people with HIV infection and AIDS. The Americans with Disabilities Act requires employers of more than 15 people to make “reasonable accommodations”, or adjustments in the job for their employees with disabilities, including HIV infection and AIDS.
For example, 32% of working Americans in the survey thought an employee with HIV infection would be fired or placed on disability leave at the first sign of illness. Clearly, if an employer moved to dismiss an employee with HIV infection solely on the basis of the diagnosis alone, that employer would be breaking the law. Such widespread employee ignorance of an employer’s legal responsibilities clearly makes employers—and by extension, their managers and employees—vulnerable to potentially costly discrimination lawsuits, work disruptions and employee morale and productivity problems.
Misperceptions about the epidemic can also fuel discriminatory attitudes and behaviour among managers and employees and can place an employer at risk. For example, 67% of workers surveyed thought that their colleagues would be uncomfortable working with someone with HIV infection. Left unchecked, such attitudes and the sorts of behaviour consistent with them can place an employer at considerable risk. Managers may erroneously assume that discriminatory treatment against those with HIV infection or AIDS, or those perceived as being infected, is acceptable.
HIV/AIDS Management Challenges
The medical, legal, financial, and workplace developments arising from the epidemic pose a host of challenges for people with HIV infection and AIDS, their families, their unions and their employers. Labour leaders, business executives, human resource professionals and front-line managers face increasingly complicated duties, including controlling costs, protecting the confidentiality of employees’ medical information and providing “reasonable accommodations” to their employees with HIV infection and AIDS, in addition to protecting people with HIV infection and AIDS and those perceived as having the illness from discrimination in hiring and promotion. People infected with HIV are remaining at work longer, so that employers need to plan how best to manage HIV-infected employees fairly and effectively over a longer period of time, and often with little or no training or guidance. Effectively managing employees with AIDS requires keeping abreast of emerging health care options, health insurance and health care costs, and legal and regulatory requirements, shaping effective “reasonable accommodations”, and managing concerns about confidentiality and privacy, discrimination issues, employee fears, harassment of infected workers, customer concerns, work disruptions, lawsuits, declines in worker productivity and morale—all the while maintaining a productive and profitable workplace and meeting business goals.
That is a large and somewhat complex set of expectations, a fact that underscores one of the essential needs in setting about to provide workplace education, namely, to start with managers and to train and motivate them to view AIDS in the workplace as part of long-term strategies and goals.
Amid the barrage of questions and concerns about the epidemic and how to manage its impact on the workplace, employers can take cost-effective steps to minimize risk, cut health care costs, protect their company’s future and, most important, save lives.
Step one: Establish a workplace HIV/AIDS policy
The first step toward effectively managing the workplace issues arising from the HIV epidemic is to put in place a sound workplace policy. Such a policy must set forth clearly the ways a business will deal with the host of complex but manageable challenges generated by HIV/AIDS. (“A sound workplace policy that accounts for an employer’s responsibilities to infected and affected workers will help keep a business from becoming a test case,” says Peter Petesch, a Washington, DC–based labour lawyer interested in the issue of AIDS and its workplace ramifications.)
Of course, a workplace policy itself will not remove the difficulties inherent in managing an employee with a fatal and often stigmatized illness. Nonetheless, a written workplace policy goes a long way towards preparing a company for its efforts to manage AIDS by minimizing risks and protecting its workforce. An effective written policy will include among its aims the need to
- Set a consistent internal standard for a company’s entire HIV/AIDS programme.
- Standardize a company’s position and communications about HIV/AIDS.
- Establish a precedent and standards for employee behaviour.
- Inform all employees where they can go for information and assistance.
- Instruct supervisors how to manage AIDS in their work groups.
Effective HIV/AIDS policies should cover and provide guidance on compliance with the law, nondiscrimination, confidentiality and privacy, safety, performance standards, reasonable accommodation, co-worker concerns and employee education. In order to be effective, a policy must be communicated to employees at every level of the company. Moreover, it is crucial to have the outspoken, highly visible support of upper-level management and executives, including the chief executive, in reinforcing the urgency and importance of the messages outlined above. Without this level of commitment, a policy that exists just “on paper” runs the risk of being simply a lion with no teeth.
There are two general approaches to developing HIV/AIDS policies:
- The life-threatening illness approach. Some employers choose to develop their HIV/AIDS policy as part of the continuum of all life-threatening illnesses or disabilities. These policies usually state that HIV/AIDS will be handled as are all other long-term illnesses—compassionately, sensibly and without discrimination.
- The HIV/AIDS-specific approach. This approach to policy development specifically acknowledges and addresses HIV/AIDS as a major health issue with potential impact on the workplace. In addition to the policy statement itself, this approach often includes an educational component asserting that HIV/AIDS is not transmitted through casual workplace contact, and that employees with HIV infection or AIDS do not pose a health risk to co-workers or customers.
Step two: Train managers and supervisors
Managers and supervisors should be thoroughly familiarized with the employer’s workplace HIV/AIDS policy guidelines. One should ensure that every level of management is supplied with clear and consistent guidance on the medical facts and the minimal risk of transmission in the general workplace. In countries with anti-discrimination laws, managers must also be thoroughly familiar with their requirements (e.g., the Americans with Disabilities Act and its reasonable accommodation requirements, nondiscrimination, confidentiality and privacy, workplace safety and employee performance standards in the United States).
Also, all managers must be prepared to field questions and concerns from employees about HIV/AIDS and the workplace. Often the front-line managers are the first ones called on to provide information and referrals to other sources of information and to provide in-depth answers to employee questions about why they should be concerned about HIV infection and AIDS and about how they are expected to behave. Managers should be educated and prepared before employee education programmes are instituted.
Step three: Educate employees
Workplace-based education programmes are inexpensive and cost-effective ways to minimize risk, protect workers’ lives, save money on health care costs and save lives. MacAllister Booth, CEO of the Polaroid Corporation, recently said that the AIDS education and training for all Polaroid employees cost less than the treatment costs of one case of AIDS.
Workplace wellness programmes and health promotion are already an established part of the world of work for more and more workers, particularly among labour organizations and larger businesses. Campaigns to reduce medical costs and days missed due to preventable illnesses have focussed on the importance of stopping smoking and of exercising and following a healthier diet. Building on efforts to increase the safety of workplaces and the health of the workforce, workplace wellness programmes are already established as cost-effective and appropriate venues for health information for employees. HIV/AIDS education programmes can be integrated into these ongoing health promotion efforts.
Further, studies have shown that many employees trust their employers to provide accurate information about a broad range of topics, including health education. Working people are concerned about AIDS, many lack understanding of the medical and legal facts about the epidemic, and they want to learn more about it.
According to a study by the New York Business Group on Health (Barr, Waring and Warshaw 1991), employees generally have a positive opinion of employers who provide information about AIDS and—depending on the type of programme offered—found the employer to be a more credible source of information than either the media or the government. Further, according to the National Leadership Coalition on AIDS’ survey of working American’s attitudes about AIDS, 96% of employees who received AIDS education at work supported workplace-based HIV/AIDS education.
Ideally, attendance at employee education sessions should be mandatory, and the programme should last at least one and a half hours. The session should be conducted by a trained educator, and should present materials in an objective and nonjudgemental way. The programme should also allow for a question-and-answer period and provide referrals for confidential assistance. Initiatives taken with regard to AIDS in the workplace should be ongoing, not one-shot events, and are more effective when linked with such public acknowledgements of the importance of the problem as World AIDS Day observances. Finally, one of the most effective methods for discussing AIDS with employees is to invite a person living with HIV infection or AIDS to address the session. Hearing first-hand how someone lives and works with HIV infection or AIDS has been shown to have a positive impact on the effectiveness of the session.
A thorough workplace AIDS education programme should include a presentation of these matters:
- the medical facts— how HIV is and is not transmitted, emphasizing that it cannot be spread through casual contact and is virtually impossible to contract in the workplace
- the legal facts, including employer responsibilities, especially the importance of confidentiality and privacy and of providing reasonable accommodations
- the psychosocial issues, including how to respond to a co-worker with HIV/AIDS, and what it is like to live and work with HIV/AIDS
- guidelines on company policies, benefits and information
- information for employees to take home to their families to teach them how to protect themselves
- information on community resources and places to go for anonymous testing.
Studies caution that attitudes about AIDS can be negatively reinforced if an education or training session is too brief and not sufficiently thorough and interactive. Similarly, simply handing out a brochure has been shown to increase anxiety about AIDS. In a brief, cursory session, attendees have been found to absorb some of the facts, but to leave with unresolved anxieties about the transmission of HIV, anxieties which have, in fact, been aroused by the introduction of the subject. Thus it is important to allow sufficient time in a training session for in-depth discussion, questions and answers, and referrals to other sources of confidential information. Optimally, a training session should be compulsory because the stigma still associated with HIV infection and AIDS will prevent many from attending a voluntary session.
Some Union Responses to HIV/AIDS
Some leading examples of union HIV/AIDS education and policy initiatives include the following:
- The Seafarers International Union established an HIV/AIDS education programme as a mandatory component of the curriculum for merchant marine students at its Lundeberg School of Seamanship in Piney Point, Maryland. Individuals wishing to enter the industry may attend a 14-week training course at the school, and those already working in the industry attend no-cost classes to upgrade their skills and to obtain high-school equivalency diplomas or associate degrees. The Seafarers educational seminars about HIV/AIDS last two hours, and this comprehensive approach is based on the recognition that a thorough training is necessary to meet the needs of a workforce which travels abroad and operates in a self-contained environment. The HIV prevention course is part of a programme that covers employment practices, workplace health and safety, and the containment of health care costs. The education is supplemented by the showing of a variety of AIDS videotapes in the closed circuit television system in the Lundeberg school, publication of articles in the school newspaper and the distribution of brochures at Union Halls in each port. Free condoms are also made available.
- The Service Employees International Union (SEIU) became involved in AIDS-related activities in 1984 when fear of AIDS transmission first arose among its members working at San Francisco General Hospital. To assure that health care workers would be able to continue to provide compassionate care to their patients, it was critically important that irrational fear be confronted with factual information and that adequate safety precautions be implemented at the same time. This crisis led to the establishment of the SEIU’s AIDS Program, a model for peer-oriented efforts, in which members work with each other to resolve educational and emotional support needs. The programme includes monitoring infection control procedures in hospitals, responding to individual requests from union members to design and conduct AIDS training programmes and encouraging hospital management coordination with the SEIU on AIDS-related concerns.
- A significant benefit of the SEIU approach to HIV/AIDS has been the development of scientifically-based policies and member education programmes that demonstrate genuine concern for all involved in the epidemic, including the health care worker, the patient and the public. The union actively promotes AIDS awareness on the national and international levels at conferences and meetings, a focus which has positioned the SEIU at the forefront of educating newly arrived immigrant workers about HIV prevention and about workplace safety with respect to all blood-borne pathogens. This educational effort takes into account the primary or preferred languages and cultural differences among its target audience.
Conclusion
Although the unions and companies responding constructively to the day-to-day workplace challenges of HIV/AIDS are in the minority, many have provided the models and a growing body of knowledge that is readily available to help others effectively address HIV as a workplace concern. The insight and experience gained over the past ten years demonstrate that well-planned AIDS policies, workplace standards and practices, leadership and ongoing labour, management and employee education are effective methods for addressing these challenges.
As trade unionists, industry groups and business associations recognize the growing consequences of AIDS for their sectors, new groups are forming to address the particular relevance of AIDS to their interests. The Thai Business Coalition on AIDS was launched in 1993, and appears likely to stimulate similar developments in other Pacific Rim countries. Several business and trade groups in Central and Southern Africa are taking the initiative in providing workplace education, and similar undertakings have become visible in Brazil and in the Caribbean.
The World Development Report (1993) was devoted to “Investing in Health” and examined the interplay between human health, health policy and economic development. The report provided a number of examples of the threat which AIDS poses to development strategies and accomplishments. This report indicates that there is a growing opportunity to utilize the skills and resources of global finance and development, working in closer harmony with public health leaders around the world, to form more effective action plans for confronting the economic and business challenges stemming from AIDS (Hammer 1994).
Unions and employers find that implementing AIDS policies and employee education programmes before confronting a case of HIV helps reduce workplace disruptions, saves money by protecting the health of the workforce, averts costly legal battles, and prepares managers and employees to respond constructively to the challenges of AIDS in the workplace. The tools needed to manage the multiple and complex day-to-day issues associated with the disease are readily accessible and inexpensive. Finally, they can save lives and money.
Health Protection and Promotion: Infectious Diseases
Prevention and control of infectious diseases is a central responsibility of the employee health service in areas where they are endemic, where work entails exposure to particular infectious agents to which the population may be singularly susceptible, and where community health services are deficient. In such circumstances, the medical director must act as the public health officer for the workforce, a duty that requires attention to sanitation, potable food and water, potential vectors of infection, appropriate immunization when available, as well as early detection and prompt treatment of infections when they occur.
In well-developed urban areas where employees are relatively healthy, concern over infectious diseases is usually eclipsed by other problems, but prevention and control of infectious diseases remain, nonetheless, important responsibilities of the employee health service. By virtue of their prevalence among all age groups (obviously including those most likely to be employed) and because of their fundamental capacity to be spread through the close contacts characteristic of the typical work environment, infectious diseases are an appropriate target for any employee health promotion programme. However, the efforts of employee health units to respond to the problem they pose are not often discussed. In part, this lack of attention may be attributed to the view that such efforts are a matter of routine, taking the form, say, of seasonal influenza immunization programmes. Additionally, they may be overlooked because they are activities not necessarily associated with broad health promotion initiatives but, instead, are woven into the fabric of the comprehensive employee health programme. For example, the individual counselling and treatment of employees undergoing periodic health evaluation often includes ad hoc health promotion interventions directed at infectious illnesses. Nonetheless, all these represent meaningful activities which, with or without formal designation as a “programme”, may be combined into a cohesive strategy for the prevention and control of infectious diseases.
These activities may be divided among a number of components: dissemination of information and employee education; immunizations; response to outbreaks of infection; protecting the health of travellers; reaching family members; and keeping up-to-date. To illustrate how these may be integrated into a comprehensive employee health programme serving a large urban, largely white-collar workforce, this article will describe the programme at J.P. Morgan and Company, Inc., based in New York City. While it has unique features, it is not dissimilar from those maintained by many large organizations.
J.P. Morgan & Company, Inc.
J.P. Morgan & Company, Inc., is a corporation providing diverse financial services throughout the world. Headquartered in New York City, where approximately 7,500 of its 16,500 employees are based, it maintains offices of various sizes elsewhere in the United States and Canada and in major cities of Europe, Asia, Latin America and Australia.
In-house medical departments were present in each of its immediate parent organizations from the early part of this century and, following the amalgamation of J.P. Morgan with Guaranty Trust Company, the employee health unit has evolved to provide not only standard occupational medical activities but a broad range of free services to employees, including periodic health evaluations, immunizations, outpatient primary care, health education and promotion and an employee assistance programme. The effectiveness of the medical department, which is based in New York City, is enhanced by the concentration of the bulk of Morgan’s workforce in a limited number of centrally located facilities.
Dissemination of Information
Dissemination of relevant information is usually the cornerstone of a health promotion programme and it is arguably the simplest approach whether resources are limited or abundant. Providing accurate, meaningful, and understandable information—modified as needed according to employees’ age, language, ethnicity and educational level—serves not only to educate but also to correct misconceptions, inculcate effective prevention strategies and direct employees to appropriate resources within or outside the worksite.
This information can take many forms. Written communications can be directed to employees at their workstations or to their homes, or can be distributed at central worksite locations. These may consist of bulletins or publications obtained from government or voluntary health agencies, pharmaceutical companies or commercial sources, among others or, if resources permit, they can be developed in-house.
Lectures and seminars can be even more effective particularly when they allow employees to pose questions about their individual concerns. On the other hand, they present the drawback of requiring accessibility and a greater time commitment on the part of both employer and staff; they also breach anonymity, which sometimes may be an issue.
HIV/AIDS
Our own experience with the dissemination of health information on HIV infection can be viewed as an example of this activity. The first cases of the illness were reported in 1981 and we first became aware of cases among our employees in 1985. In 1986, in large measure because of local media attention to the problem, the employees in one of our European offices (where no cases of the illness had yet surfaced) requested a programme on AIDS. The speakers included the corporate medical director and an expert on infectious diseases from a local university hospital. The audience consisted of almost 10% of that unit’s entire workforce of whom 80% were women. The emphasis of these and subsequent presentations was on transmission of the virus and on strategies for prevention. As one might assume from the composition of the audience, there was considerable concern about heterosexual spread.
The success of that presentation facilitated the development of a far more ambitious programme at the New York headquarters the following year. A newsletter and brochure anticipated the events with a brief discussion of the illness, posters and other advertisements were utilized to remind employees of the times and places of presentations, and managers strongly encouraged attendance. Because of the commitment of management and general concerns about the illness in the community, we were able to reach between 25 and 30% of the local workforce in the multiple presentations.
These sessions included a discussion by the corporate medical director, who acknowledged the presence of the illness among employees and noted that the corporation was committed to their continuing employment as long as they remained well enough to work effectively. He reviewed the corporation’s policy on life-threatening illnesses and noted the availability of confidential HIV testing through the medical department. An educational videotape on the illness was shown, followed by an expert speaker from the local municipal health department. A period of questions and answers followed and, at the close of the session, everyone was given a packet of information materials on HIV infection and prevention strategies.
The response to these sessions was very positive. At a time when other corporations were experiencing workplace disruptions over employees with HIV infections, Morgan had none. An independent survey of employees (and those of several other corporations with similar programmes) found that programme participants thoroughly appreciated the opportunity to attend such sessions and found the information provided was more helpful than that available to them from other sources (Barr, Waring and Warshaw 1991).
We held similar sessions on HIV infection in 1989 and 1991, but found that attendance diminished with time. We attributed this, in part, to perceived saturation with the subject and, in part, to the illness shifting its impact to the chronically unemployed (in our area); indeed, the number of employees newly infected with HIV who came to our attention dramatically declined after 1991.
Lyme disease
Meanwhile, Lyme disease, a bacterial illness transmitted by the bite of the deer tick in suburban and local vacation environments has become increasingly prevalent among our employees. A lecture on this subject supplemented by printed information attracted considerable attention when it was given in 1993. Points emphasized in this presentation included recognition of the illness, testing, treatment and, most important, prevention.
In general, programmes designed to disseminate information whether written or in lecture form, should be credible, easily understandable, practical and relevant. They should serve to elevate awareness, especially with regard to personal prevention and when and how to obtain professional attention. At the same time, they should serve to dissipate any inappropriate anxieties.
Immunization Programmes
Immunizations at the worksite address an important public health need and are likely to provide tangible benefits, not only to the individual recipients but to the organization as well. Many employers in the developed world who do not have an employee health service arrange for outside contractors to come to the worksite to provide a mass immunization programme.
Influenza.
While most immunizations provide protection for many years, influenza vaccine must be administered annually because of continuing changes in the virus and, to a lesser extent, waning patient immunity. Since influenza is a seasonal illness whose infectiousness is typically widespread in the winter months, the vaccine should be administered in the autumn. Those most in need of immunization are older employees and those with underlying illnesses or immune deficiencies, including diabetes and chronic lung, heart and kidney problems. Employees in health care institutions should be encouraged to be immunized not only because they are more likely to be exposed to persons with the infection, but also because their continuing ability to work is critical in the event of a serious outbreak of the illness. A recent study has shown that vaccination against influenza offers substantial health-related and economic benefits for healthy, working adults also. Since the morbidity associated with the illness can typically result in a week or more of disability, often involving multiple employees in the same unit at the same time, there is sufficient incentive for employers to prevent the resultant impact on productivity by offering this relatively innocuous and inexpensive form of immunization. This becomes especially important when public health authorities anticipate major changes in the virus and predict a major epidemic for a given season.
Probably, the main barrier to the success of influenza (or any other) immunization programmes is the reluctance of individuals to participate. To minimize their hesitation, it is important to educate employees on the need for and availability of the vaccine and to make the immunization readily accessible. Notices should go out through all available means, generically identifying all those in special need of immunization emphasizing the relative safety of the vaccine, and explaining the procedure through which it can be obtained.
Time and the inconvenience of travel to visit a personal physician are potent disincentives for many individuals; the most effective programmes will be those that provide immunizations at the worksite during working hours with minimum delays. Finally, cost, a major barrier, should either be held to a minimum or absorbed entirely by the employer or the group health insurance programme.
Contributing to employee acceptance of immunizations are such additional factors as community publicity and incentive programmes. We have found that media reports of a threatening influenza epidemic will regularly increase employee acceptance of the vaccine. In 1993, to encourage all employees to have their vaccination status evaluated and to receive needed immunizations, the medical department at Morgan offered those who accepted these services participation in a lottery in which company stock was the prize. The number of employees seeking immunization in this year was half again as great as the number seen during the same period in the prior year.
Diphtheria-tetanus.
Other immunizations advised for healthy adults of typical employment age are diphtheria-tetanus and, possibly measles, mumps, and rubella. Diphtheria-tetanus immunization is recommended every ten years throughout life, assuming that one has had a primary series of immunizations. With this interval, we find immune status most easily confirmed and the vaccine most easily administered during our employees’ periodic health evaluations (see below), although this can also be accomplished in a company-wide immunization campaign such as the one used in the incentive programme mentioned above.
Measles.
Public health authorities recommend measles vaccine for everyone born after 1956 who does not have documentation of two doses of measles vaccine on or after the first birthday, a history of measles confirmed by a physician, or laboratory evidence of measles immunity. This immunization can readily be administered during a pre-employment or pre-placement health evaluation or in a company-wide immunization campaign.
Rubella.
Public health authorities recommend that everyone have medical documentation of having received rubella vaccine or laboratory evidence of immunity to this illness. Adequate rubella immunization is especially important for health care workers, for whom it is likely to be mandated.
Again, adequate rubella immunity should be ascertained at the time of employment or, absent this possibility, through periodic immunization campaigns or during periodic health evaluations. Effective immunity can be conferred on persons in need of rubella or rubeola vaccine by administration of MMR (measles-mumps-rubella) vaccine. Serologic testing for immunity can be undertaken to identify the immune status of an individual prior to immunization, but this is not likely to be cost-effective.
Hepatitis B.
In so far as hepatitis B is transmitted through sexual intimacy and by direct contact with blood and other body fluids, initial immunization efforts were directed at populations with elevated risks, such as health professionals and those with multiple sexual partners. Additionally, the increased prevalence of the illness and carrier state in certain geographic areas such as the Far East and sub-Saharan Africa has given priority to immunization of all newborns there and of those who frequently travel to, or remain for extended periods in, those regions. More recently, universal immunization of all newborns in the United States and elsewhere has been proposed as a more effective strategy for reaching vulnerable individuals.
In the work environment, the focus of hepatitis B immunization has been on health care workers because of the risk of their exposure to blood. Indeed, in the United States, government regulation requires informing such personnel and other likely responders to health care emergencies of the advisability of being immunized against hepatitis B, in the context of a general discussion of universal precautions; immunization must then be provided.
Thus, in our setting at Morgan, information about hepatitis B immunization is conveyed in three contexts: in discussions on sexually transmitted diseases such as AIDS, in presentations to health care and emergency service personnel on the risks and precautions relevant to their health care work, and in interventions with individual employees and their families anticipating assignments in areas of the world where hepatitis B is most prevalent. The immunization is provided in conjunction with these programmes.
Hepatitis A.
This illness, typically transmitted by contaminated food or water, is much more prevalent in developing nations than in industrialized countries. Thus, protection efforts have been directed at travellers to areas of risk or those who have household contact or other very close contact with those newly diagnosed with the illness.
Now that a vaccine to protect against hepatitis A has become available, it is administered to travellers to developing countries and to close contacts of newly diagnosed, documented cases of hepatitis A. If there is insufficient time for antibody levels to develop prior to the departure of travellers, serum immune globulin may be administered simultaneously.
As an effective, safe hepatitis A vaccine is available, immunization efforts can be directed to a significantly larger target group. At a minimum, frequent travellers to and residents in endemic areas should receive this immunization, and food handlers should also be considered for immunization because of the risk of their transmitting the illness to large numbers of people.
Prior to any immunization, careful attention should be paid to possible contraindications, such as hypersensitivity to any vaccine component or, in the case of live vaccines such as measles, mumps, and rubella, immune deficiency or pregnancy, whether present or soon anticipated. Appropriate information on possible vaccine risks should be conveyed to the employee and signed consent forms obtained. The limited possibility of immunization-related reactions should be anticipated in any programme.
Those organizations with existing medical staffs can obviously utilize their own personnel to implement an immunization programme. Those without such personnel may arrange for immunizations to be provided by community physicians or nurses, hospitals or health agencies or by government health agencies.
Response to Outbreaks
Few events arouse as much interest and concern among employees in a particular work unit or an entire organization as awareness that a co-worker has a contagious illness. The essential response of the employee health service to such news is to identify and appropriately isolate those who are ill, both the source case and any secondary cases, while disseminating information about the illness that will allay the anxiety of those who believe that they may have been exposed. Some organizations, hoping to minimize potential anxiety, may limit this dissemination to possible contacts. Others, recognizing that the “grapevine” (informal communication among employees) will not only spread the news but will probably also convey misinformation that could unleash latent anxiety, will seize the event as a unique opportunity to educate the entire workforce about the potential for spread of the disease and how to prevent it. At Morgan, there have been several episodes of this type involving three different diseases: tuberculosis, rubella, and food-borne gastroenteritis.
Tuberculosis.
Tuberculosis is justifiably feared because of the potentially significant morbidity of the illness, especially with the increasing prevalence of multiple drug resistant bacteria. In our experience, the illness has been brought to our attention by news of the hospitalization and definitive diagnosis of the index cases; fortunately at Morgan, secondary cases have been rare and have been limited to skin test conversions only.
Typically with such cases, public health authorities are notified, following which contacts are encouraged to undergo baseline tuberculin skin testing or chest x-rays; the skin tests are repeated ten to twelve weeks later. For those whose skin tests convert from negative to positive in the follow-up testing, chest x-rays are obtained. If the x-ray is positive, employees are referred for definitive treatment; if negative, isoniazid prophylaxis is prescribed.
During each stage of the process, informational sessions are held on both a group and individual basis. Anxiety is typically disproportionate to risk, and reassurance, as well as the need for prudent follow-up, are the primary targets of the counselling.
Rubella.
Morgan’s cases of rubella have been identified on visits to the employee health unit. To avoid further contact, the employees are sent home even if there is only a clinical suspicion of the illness. Following serologic confirmation, usually within 48 hours, epidemiological surveys are conducted to identify other cases while information about the occurrence is disseminated. Although the major targets of these programmes are female employees who may be pregnant and who might have been exposed, the outbreaks have served as an opportunity to verify the immune status of all employees and to offer vaccine to all those who might need it. Again, local public health authorities are advised of these occurrences and their expertise and assistance are utilized in addressing organizational needs.
Food-borne infection.
A single experience with a food-related illness outbreak occurred at Morgan several years ago. It was due to staphylococcal food poisoning which was traced to a food handler with a skin lesion on one of his hands. Over fifty employees who utilized the in-house dining facilities developed a self-limited illness which was characterized by nausea, vomiting and diarrhoea, appearing approximately six hours after ingesting the offending cold duck salad, and resolving within 24 hours.
In this instance, the thrust of our health education efforts was to sensitize the food handlers themselves to the signs and symptoms of illness that should influence them to leave their work and seek medical attention. Certain managerial and procedural changes were also implemented:
- making supervisors aware of their responsibility to assure that workers with signs of illness receive medical scrutiny
- holding periodic educational sessions for all food service employees to remind them of appropriate precautions
- assuring that disposable gloves are used.
Recently, two neighbouring organizations also experienced food-related illness outbreaks. In one, hepatitis A was transmitted to a number of employees by a food handler in the company dining room; in the other, a number of employees developed salmonella food poisoning after consuming a dessert prepared with raw eggs in a restaurant off the premises. In the first instance, the organization’s educational efforts were directed at the food handlers themselves; in the second, information on various foods prepared from raw eggs—and the potential hazard that this entailed—was shared with the entire workforce.
Individual Interventions
While the three experiences described above follow the typical health promotion format of reaching out to the entire employee population or, at least, to a substantial subset, much of the health promotion activities of organizations like Morgan with respect to infectious diseases takes place on a one-on-one basis. These include interventions that are made possible by pre-placement, periodic, or retirement health evaluations, inquiries about international travel, and incidental visits to the employee health service.
Pre-placement examinations.
Individuals examined at the time of employment are typically young and healthy and are unlikely to have had recent medical attention. They are often in need of such immunizations as measles, rubella, or diphtheria-tetanus. Additionally, those scheduled to be placed in areas of potential disease transmission such as in health or food services receive appropriate counselling about the precautions that they should observe.
Periodic medical examinations.
Similarly, the periodic health evaluation provides the opportunity to review immunization status and to discuss the risks that may be associated with specific chronic illnesses and the precautions that should be undertaken. Examples of the latter include the need for annual influenza immunization for individuals with diabetes or asthma and instruction for diabetics on the appropriate care of the feet to avoid local infection.
Recently reported news about infectious diseases should be discussed, particularly with those with known health problems. For example, news of outbreaks of an E. coli infection attributed to eating inadequately cooked ground meat would be of importance to all, while the danger of contracting cryptosporidiosis from swimming in public pools would be especially relevant to those with HIV disease or other immune deficiencies.
Pre-retirement examinations.
Employees who are examined in relation to retirement should be urged to obtain pneumococcal immunization and advised about annual influenza immunization.
Pre-travel protection.
The increasing globalization of work assignments coupled with the heightened interest in international travel for pleasure have contributed to a continuing expansion of the population needing protection against infectious diseases not likely to be encountered at home. A pre-travel encounter should include a medical history to reveal any individual health vulnerabilities that may increase the risks associated with the anticipated travel or assignment. A good—and not uncommon—example of this is the pregnant woman considering travel to an environment with chloroquine-resistant malaria, since the alternative forms of malaria prophylaxis may be contraindicated during pregnancy.
Comprehensive information on the infectious illnesses prevalent in the areas to be visited should be provided. This should include methods of transmission of the relevant illnesses, avoidance and prophylactic techniques, and typical symptoms and strategies for obtaining medical attention if they develop. And, of course, indicated immunizations should be provided.
Visits to the employee health service.
In most occupational health settings, employees may receive first aid and treatment for symptoms of illness; in some, as at Morgan, a broad range of primary care services is available. Each encounter offers an opportunity for preventive health interventions and counselling. This includes providing immunizations at appropriate intervals and alerting employee-patients about health precautions relative to any underlying illness or potential exposure. A particular advantage of this situation is that the very fact that the employee has sought this attention suggests that he or she may be more receptive to the advice given than may be the case when the same information is received in a broad educational campaign. The health professional should capitalize on this opportunity by ensuring that appropriate information and necessary immunizations or prophylactic medications are provided.
Reaching family members.
Although the main thrust of occupational health is to assure the health and well-being of the employee, there are many reasons to see that effective health promotion efforts are conveyed to the employee’s family as well. Obviously, most of the objectives noted earlier are equally applicable to other adult members of the household and, while the direct services of the occupational health unit are generally not available to family members, the information can be conveyed home through newsletters and brochures and by word of mouth.
An additional consideration is the health of children, especially in view of the importance of early childhood immunizations. It has been recognized that these immunizations are often overlooked, at least in part, not only by the economically disadvantaged, but even by the children of more affluent US corporate employees. Seminars on well-baby care and printed information on this subject, provided either by the employer or by the employer’s health insurance carrier may serve to minimize this deficiency. Additionally, modifying health insurance coverage to include such “preventive” measures as immunizations should also serve to encourage appropriate attention to this matter.
Keeping Abreast
Although the introduction of antibiotics in the middle of the twentieth century led some to believe that infectious diseases would soon be eliminated, actual experience has been very different. Not only have new infectious diseases appeared (e.g., HIV and Lyme disease), but more infectious agents are developing resistance to formerly effective medications (e.g., malaria and tuberculosis). It is imperative, therefore, that occupational health professionals keep their knowledge of developments in the field of infectious diseases and their prevention current. Although there are many ways of doing this, periodic reports and bulletins emanating from the World Health Organization and national health agencies such as the US Centers for Disease Control and Prevention are particularly useful.
Conclusion
High among employers’ responsibilities for the health of the workforce is the prevention and control of infectious diseases among employees. This includes identification, isolation and appropriate treatment of individuals with infections together with prevention of their spread to co-workers and dependants and allaying the anxieties of those concerned about potential contact. It also involves education and appropriate protection of employees who may encounter infectious diseases while at work or in the community. The employee health service, as illustrated by the above description of activities of the medical department at J.P. Morgan and Company, Inc., in New York City, may play a central role in meeting this responsibility, resulting in benefit to individual employees, the organization as a whole and the community.
Protecting the Health of the Traveller
In this era of multinational organizations and ever-expanding international trade, employees are being increasingly called upon to undertake travel for business reasons. At the same time, more employees and their families are spending their holidays in travel to distant places around the world. While for most people such travel is usually exciting and enjoyable, it is often burdensome and debilitating and, especially for those who are not properly prepared, it can be hazardous. Although life-threatening situations may conceivably be encountered, most of the problems associated with travel are not serious. For the holiday traveller, they bring anxiety, discomfort and inconvenience along with the disappointment and added expense involved in shortening a trip and making new travel arrangements. For the business person, travel difficulties may ultimately affect the organization adversely on account of the impairment of his or her work performance in negotiations and other dealings, to say nothing of the cost of having to abort the mission and sending someone else to complete it.
This article will outline a comprehensive travel protection programme for individuals making short-term business trips and it will briefly describe steps that may be taken to circumvent the more frequently encountered travel hazards. (The reader may consult other sources—e.g., Karpilow 1991—for information on programmes for individuals on long-term expatriate assignments and on programmes for whole units or groups of employees dispatched to workstations in distant locales).
A Comprehensive Travel Protection Programme
Occasional seminars on managing the hazards of travel are a feature of many worksite health promotion programmes, especially in organizations where a sizeable proportion of employees travels extensively. In such organizations, there often is an in-house travel department which may be given the responsibility of arranging the sessions and procuring the pamphlets and other literature that may be distributed. For the most part, however, educating the prospective traveller and providing any services that may be needed are conducted on an individual rather than a group basis
Ideally, this task is assigned to the medical department or employees’ health unit, where, it is to be hoped, a knowledgeable medical director or other health professional will be available. The advantages of maintaining in-house medical unit staff, apart from convenience, is their knowledge of the organization, its policies and its people; the opportunity for close collaboration with other departments that may be involved (personnel and travel, for example); access to medical records containing health histories of those assigned to travel assignments, including details of any prior travel misadventures; and, at least, a general knowledge of the kind and intensity of work to be accomplished during the trip.
Where such an in-house unit is lacking, the travelling individual may be referred to one of the “travel clinics” that are maintained by many hospitals and private medical groups in the community. The advantages of such clinics include medical staff specializing in the prevention and treatment of the diseases of travellers, current information about conditions in the areas to be visited and fresh supplies of any vaccines that may be indicated.
A number of elements should be included if the travel protection programme is to be truly comprehensive. These are considered under the following heads.
An established policy
Too often, even when a trip has been scheduled for some time, the desired steps to protect the traveller are taken on an ad hoc, last-minute basis or, sometimes, neglected entirely. Accordingly, an established written policy is a key element in any travel protection programme. Since many business travellers are high-level executives, this policy should be promulgated and supported by the chief executive of the organization so that its provisions can be enforced by all of the departments involved in travel assignments and arrangements, which may be headed by managers of lower rank. In some organizations, the policy expressly prohibits any business trip if the traveler has not received a medical “clearance”. Some policies are so detailed that they designate minimal height and weight criteria for authorizing the booking of more expensive business-class seating instead of the much more crowded seats in the economy or tourist sections of commercial aircraft, and specify the circumstances under which a spouse or family members may accompany the traveller.
Planning the trip
The medical director or responsible health professional should be involved in planning the itinerary in conjunction with the travel agent and the individual to whom the traveller reports. The considerations to be addressed include (1) the importance of the mission and its ramifications (including obligatory social activities), (2) the exigencies of travel and conditions in the parts of the world to be visited, and (3) the physical and mental condition of the traveller along with his or her capacity to withstand the rigours of the experience and continue to perform adequately. Ideally, the traveller will also be involved in such decisions as to whether the trip should be postponed or cancelled, whether the itinerary should be shortened or otherwise modified, whether the mission (i.e., with respect to number of people visited or number or duration of meetings, etc.) should be modified, whether the traveller should be accompanied by an aide or assistant, and whether periods of rest and relaxation should be built into the itinerary.
Pre-travel medical consultation
If a routine periodic medical examination has not been performed recently, a general physical examination and routine laboratory tests, including an electrocardiogram, should be performed. The purpose is to ensure that the employee’s health will not be adversely affected either by the rigours of transit per se or by other circumstances encountered during the trip. The status of any chronic diseases needs to be determined and modifications advised for those with such conditions as diabetes, autoimmune diseases or pregnancy. A written report of the findings and recommendations should be prepared to be made available to any physicians consulted for problems arising en route. This examination also provides a baseline for evaluating potential illness when the traveller returns.
The consultation should include a discussion of the desirability of immunizations, including a review of their potential side-effects and the differences between those that are required and those that are only recommended. An inoculation schedule individualized for the traveler’s needs and departure date should be developed and the necessary vaccines administered.
Any medications being taken by the traveller should be reviewed and prescriptions provided for adequate supplies, including allowances for spoilage or loss. Modifications of timing and dosage must be prepared for travellers crossing several time zones (e.g., for those with insulin-dependent diabetes). Based on the work assignment and mode of transport, medications should be prescribed for the prevention of certain specific diseases, including (but not limited to) malaria, traveller’s diarrhoea, jet lag and high altitude sickness. In addition, medications should be prescribed or supplied for on-the-trip treatment of minor illnesses such as upper respiratory infections (particularly nasal congestion and sinusitis), bronchitis, motion sickness, dermatitis and other conditions that may be reasonably anticipated.
Medical kits
For the traveller who does not wish to spend valuable time searching for a pharmacy in case of need, a kit of medications and supplies may be invaluable. Even if the traveller may be able to find a pharmacy, the pharmacist’s knowledge of the traveller’s special condition may be limited, and any language barrier may result in serious lapses in communication. Further, the medication offerred may not be safe and effective. Many countries do not have strict drug labelling laws and quality assurance regulations are sometimes non-existent. The expiration dates of medications are often ignored by small pharmacies and the high temperatures in tropical climates may inactivate certain medications that are stored on shelves in hot shops.
While commercial kits stocked with routine medications are available, the contents of any such kit should be customized to meet the traveller’s specific needs. Among those most likely to be needed, in addition to medications prescribed for specific health problems, are drugs for motion sickness, nasal congestion, allergies, insomnia and anxiety; analgesics, antacids and laxatives, as well as medication for haemorrhoids, menstrual discomfort and nocturnal muscle cramps. The kit may furthermore contain antiseptics, bandages and other surgical supplies.
Travellers should carry either letters signed by a physician on letterhead stationery or else prescription blanks listing the medications being carried and indicating the conditions for which they have been prescribed. This may save the traveller from embarrassing and potentially long delays at international ports of entry where customs agents are especially diligent in looking for illicit drugs.
The traveller should also carry either an extra pair of eyeglasses or contact lenses with adequate supplies of cleansing solutions and other necessary appurtenances. (Those going to excessively dirty or dusty areas should be encouraged to wear eyeglasses rather than contact lenses). A copy of the user’s lens prescription will facilitate the procurement of replacement glasses should the traveller’s pair be lost or damaged.
Those who travel frequently should have their kits checked before each trip to make sure that the contents have been adjusted to the particular itinerary and are not outdated.
Medical records
In addition to notes confirming the appropriateness of the medications being carried, the traveller should carry a card or letter summarizing any significant medical history, findings on his or her pre-travel health assessment and copies of a recent electrocardiogram and any relevant laboratory data. A record of the traveller’s most recent immunizations may obviate the necessity of submitting to mandatory inoculation at the port of entry. The record should also contain the name, address, telephone and fax numbers of a physician who can supply additional information about the traveller should it be required (a Medic-Alert type of badge or bracelet can be useful in this regard).
A number of vendors can supply medical record cards with microfilm chips containing travellers’ complete medical files. While often convenient, the foreign physician may lack access to the microfilm viewer or a hand lens powerful enough to read them. There is also the problem of making sure that the information is up-to-date.
Immunizations
Some countries require all arriving travellers to be vaccinated for certain diseases, such as cholera, yellow fever or plague. While the World Health Organization has recommended that only vaccination for yellow fever be required, a number of countries still require cholera immunization. In addition to protecting travellers, the required immunizations are also intended to protect their citizens from diseases that may be carried by travellers.
Recommended immunizations are intended to prevent travellers from contracting endemic diseases. This list is much longer than the “required” list and is enlarging annually as new vaccines are developed to combat new and rapidly advancing diseases. The desirability of a specific vaccine also changes frequently in accord with the amount and virulence of the disease in the particular area. For this reason, current information is essential. This may be obtained from the World Health Organization; from government agencies such as the US Centers for Disease Control and Prevention; the Canada Health and Welfare Department; or from the Commonwealth Department of Health in Sydney, Australia. Similar information, usually derived from such sources, may be obtained from local voluntary and commercial organizations; it is also available in periodically updated computer software.
Immunizations recommended for all travellers include diphtheria-tetanus, polio, measles (for those born after 1956 and without a physician-documented episode of measles), influenza and hepatitis B (particularly if the work assignment may involve exposure to this hazard).
The amount of time available for departure may influence the immunization schedule and dosage. For example, for the individual who has never been immunized against typhoid, two injections, four weeks apart, should produce the highest antibody titre. If there is not enough time, those who have not been previously inoculated may be given four pills of the newly developed oral vaccine on alternate days; this will be considerably more effective than a single dose of the injected vaccine. The oral vaccine regimen may also be used as a booster for individuals who have previously received the injections.
Health Insurance and Repatriation Coverage
Many national and private health insurance programmes do not cover individuals who receive health services while outside of the specified area. This can cause embarrassment, delays in receiving needed care and high out-of-pocket expenses for individuals who incur injuries or acute illnesses while on a trip. It is prudent, therefore, to verify that the traveller’s current health insurance will cover him or her throughout the trip. If not, procurement of temporary health insurance covering the entire period of the trip should be advised.
Under certain circumstances, particularly in undeveloped areas, lack of adequate modern facilities and concern over the quality of the available care may dictate medical evacuation. The traveller may be returned to his or her home city or, when the distance is too great, to an acceptable urban medical centre en route. A number of companies provide emergency evacuation services around the world; some, however, are available only in more limited areas. Since such situations are usually quite urgent and stressful for all those involved, it is wise to make preliminary stand-by arrangements with a company that serves the areas to be visited and, since such services may be quite expensive, to confirm that they are covered by the traveller’s health insurance programme.
Post-travel Debriefing
A medical consultation soon after return is a desirable follow-up to the trip. It provides for a review of any health problems that may have arisen and the proper treatment of any that may not have entirely cleared up. It also provides for a debriefing on the circumstances encountered en route that can lead to more appropriate recommendations and arrangements if the trip is to be repeated or undertaken by others.
Coping with the Hazards of Travel
Travel almost always entails exposure to health hazards that, at the least, present inconvenience and annoyance and can lead to serious and disabling illnesses or worse. For the most part, they can be circumvented or controlled, but this usually requires a special effort on the part of the traveller. Sensitizing the traveller to recognize them and providing the information and training required to cope with them is the major thrust of the travel protection programme. The following represent some of the hazards most commonly encountered during travel.
Jet lag.
Rapid passage across time zones can disrupt the physiological and psychological rhythms—the circadian rhythms—that regulate the organism’s functions. Known as “jet lag” because it occurs almost exclusively during air travel, it can cause sleep disturbances, malaise, irritability, reduced mental and physical performance, apathy, depression, fatigue, loss of appetite, gastric distress and altered bowel habits. As a rule, it takes several days before a traveller’s rhythms adapt to the new location. Consequently, it is prudent for travellers to book long-distance flights several days prior to the start of important business or social engagements so as to allow themselves a period during which they can recover their energy, alertness and work capacities (this also applies to the return flight). This is particularly important for older travellers, since the effects of jet lag seem to increase with age.
A number of approaches to minimizing jet lag have been employed. Some advocate the “jet lag diet,” alternating feasting and fasting of carbohydrates or high protein foods for three days prior to departure. Others suggest eating a high carbohydrate dinner prior to departure, limiting food intake during the flight to salads, fruit plates and other light dishes, drinking a good deal of fluids before and during the trip (enough on the plane to require the hourly use of the rest room) and avoidance of all alcoholic beverages. Others recommend the use of a head-mounted light that suppresses the secretion of melatonin by the pineal gland, the excess of which has been linked to some of the symptoms of jet lag. More recently, small doses of melatonin in tablet form (1 mg or less—larger doses, popular for other purposes, produce drowsiness) taken on a prescibed schedule several days before and after the trip, have been found useful in minimizing jet lag. While these may be helpful, adequate rest and a relaxed schedule until the readjustment has been completed are most reliable.
Air travel.
In addition to jet lag, travel by air can be difficult for other reasons. Getting to and through the airport can be a source of anxiety and irritation, especially when one has to cope with traffic congestion, heavy or bulky luggage, delayed or cancelled flights and dashing through terminals to make connecting flights. Long periods of confinement in narrow seats with insufficient leg room are not only uncomfortable but may precipitate attacks of phlebitis in the legs. Most passengers in well-maintained modern aircraft will have no difficulty breathing since cabins are pressurized to maintain a simulated altitude below that of 8,000 feet above sea level. Cigarette smoke may be annoying for those seated in or near the smoking sections of planes that have not been designated as smoke-free.
These problems can be minimized by such steps as prearranging transfers to and from the airports and assistance with baggage, providing electric carts or wheel chairs for those for whom the long walk between the terminal entrance and the gate may be troublesome, eating lightly and avoiding alcoholic beverages during the flight, drinking plenty of fluids to combat the tendency toward dehydration and getting out of one’s seat and walking about the cabin frequently. When the lattermost alternative is not feasible, performing stretching and relaxing exercises like those demonstrated in figure 1 is essential. Eye shades may be helpful in trying to sleep during the flight, while wearing ear plugs throughout the flight has been shown to decrease stress and fatigue.
Figure 1. Exercises to be performed during long airplane trips.
In some 25 countries, including Argentina, Australia, India, Kenya, Mexico, Mozambique and New Zealand, arriving aircraft cabins are required to be sprayed with insecticides before passengers are allowed to leave the plane The purpose is to prevent disease-bearing insects from being brought into the country. Sometimes, the spraying is cursory but often it is quite thorough, taking in the entire cabin, including the seated passengers and crew. Travellers who find the hydrocarbons in the spray annoying or irritating should cover their faces with a damp cloth and practice relaxation breathing exercises.
The United States objects to this practice. Transportation Secretary Federico F. Peña has proposed that all airlines and travel agencies be required to notify passengers when they will be sprayed, and the Transportation Department plans to bring this controversial issue before the International Civil Aviation Association and to cosponsor a World Health Organization symposium on this question (Fiorino 1994).
Mosquitoes and other biting pests.
Malaria and other arthropod-borne diseases (e.g., yellow fever, viral encephalitis, dengue fever, filariasis, leishmaniasis, onchocercosis, trypanosomiasis and Lyme disease) are endemic in many parts of the world. Keeping from getting bitten is the first line of defence against these diseases.
Insect repellents containing “DEET” (N,N-diethyl-meta-toluamide) may be used on the skin and/or clothing. Because DEET can be absorbed through the skin and may cause neurological symptoms, preparations with a DEET concentration over 35% are not recommended, especially for infants. Hexanediol is a useful alternative for those who may be sensitive to DEET. Skin-So-Soft®, the commercially available moisturizer, needs to be reapplied every twenty minutes or so to be an effective repellent.
All persons travelling in areas where insect-borne diseases are endemic should wear long-sleeve shirts and long trousers, especially after dusk. In hot climates, wearing loose-fitting thin cotton or linen garments is actually cooler than leaving the skin exposed. Perfumes and scented cosmetics, soaps and lotions that may attract insects should be avoided. Lightweight mesh jackets, hoods and face guards are particularly helpful in highly infested areas. Mosquito bed netting and window screens are important adjuncts. (Before retiring, it is important to spray the inside of the bednetting in case undesirable insects have become trapped in it.)
Protective clothing and nets may be treated with a DEET-containing repellent or with permethrin, an insecticide available in both spray and liquid formulations.
Malaria.
Despite decades of mosquito eradication efforts, malaria remains endemic in most tropical and subtropical regions of the world. Because it is so dangerous and debilitating, the mosquito control efforts described above should be supplemented by prophylactic use of one or more antimalarial drugs. While a number of fairly effective antimalarials have been developed, some strains of the malaria parasite have become highly resistant to some if not all of the currently used drugs. For example, chloroquine, traditionally the most popular, is still effective against strains of malaria in certain parts of the world but is useless in many other areas. Proguanil, mefloquine and doxycycline are currently most commonly used for chloroquine-resistant strains of malaria. Maloprim, fansidar and sulfisoxazole are also used in certain areas. A prophylactic regimen is started prior to entering the malarious area and continued for some time after leaving it.
The choice of the drug is based on “up to the minute” recommendations for the particular areas to be visited by the traveller. The potential side-effects should also be considered: for example, fansidar is contraindicated during pregnancy and lactation, while mefloquine should not be used by airline pilots or others in whom central nervous system side-effects could impair performance and affect the safety of others, nor by those taking beta-blockers or calcium-channel blockers or other drugs that alter cardiac conduction.
Contaminated water.
Contaminated tap water may be a problem all over the world. Even in modern urban centers, defective pipes and faulty connections in older or poorly maintained buildings may allow the spread of infection. Even bottled water may not be safe, particularly if the plastic seal on the cap is not intact. Carbonated beverages are generally safe to drink provided they have not been allowed to go flat.
Water can be disinfected by heating it to 62ºC for 10 minutes or by adding iodine or chlorine after filtering to remove parasites and worm larvae and then allowing it to stand for 30 minutes.
Water filtration units sold for camping trips are usually not appropriate for areas where the water is suspect since they do not inactivate bacteria and viruses. So-called “Katadyn” filters are available in individual units and filter out organisms larger than 0.2 microns but must be followed by iodine or chlorine treatment to remove viruses. The more recently developed “PUR” filters combine 1.0 micron filters with exposure to a tri-iodine resin matrix that eliminates bacteria, parasites and viruses in a single process.
In areas where the water may be suspect, the traveller should be advised not to use ice or iced drinks and to avoid brushing the teeth with water that has not been purified.
Another important precaution is to avoid swimming or dangling limbs in fresh-water lakes or streams harboring the snails carrying the parasites that cause schistosomiasis (bilharzia).
Contaminated food.
Food may be contaminated at the source by the use of “night soil” (human body wastes) as a fertilizer, in passage by a lack of refrigeration and exposure to flies and other insects, and in preparation by poor hygiene on the part of cooks and food handlers. In this respect, the food prepared by a street vendor where one can see what is being cooked and how it is being prepared may be safer than the “four star” restaurant where the posh ambience and clean uniforms worn by the staff may hide lapses in the storage, preparation and serving of the food. The old adage, “If you can’t boil it or peel it yourself, don’t eat it” is probably the best advice one can give the traveller.
Traveller’s diarrhoea.
Travellers’ diarrhoea is encountered worldwide in modern urban centres as well as in undeveloped areas. While most cases are attributed to organisms in food and drink, many are simply the result of strange foods and food preparation, dietary indiscretions and fatigue. Some cases may also follow bathing or showering in unsafe water or swimming in contaminated lakes, streams and pools.
Most cases are self-limited and respond promptly to such simple measures as maintaining an adequate fluid intake, a light bland diet and rest. Simple medications such as attapulgite (a clay product that acts as an absorbent), bismuth subsalicylate and anti-motility agents such as loperamide or reglan may help to control the diarrhoea. However, when the diarrhoea is unusually severe, lasts more than three days, or is accompanied by repeated vomiting or fever, medical attention and the use of appropriate antibiotics are advisable. Selection of the antibiotic of choice is guided by laboratory identification of the offending organism or, if that is not feasible, by an analysis of the symptoms and epidemiological information about the prevalence of particular infections in the areas visited. The traveller should be provided with a pamphlet such as the one developed by the World Health Organization (figure 2) that explains what to do in simple, non-alarming language.
Prophylactic use of antibiotics has been suggested before one enters an area where water and food are suspect, but this is generally frowned upon since the antibiotics themselves may cause symptoms and taking them in advance may lead the traveller to ignore or become lax towards the precautions that have been advised.
Figure 2. A sample of a World Health Organization educational pamphlet on traveller’s diarrhoea.
MISSING
In some cases, the onset of the diarrhoea may not occur until after the return home. This is particularly suggestive of parasitic disease and is an indication that the appropriate laboratory tests be made to determine whether such an infection exists.
Altitude sickness.
Travellers to mountainous regions such as Aspen, Colorado, Mexico City or La Paz, Bolivia, may have difficulty with the altitude, particularly those with coronary artery disease, congestive heart failure or lung diseases such as emphysema, chronic bronchitis or asthma. When mild, altitude sickness may cause fatigue, headache, exertional dyspnoea, insomnia or nausea. These symptoms generally subside after a few days of diminished physical activity and rest.
When more severe, these symptoms may progress to respiratory distress, vomiting and blurred vision. When this occurs, the traveller should seek medical attention and get to a lower altitude as quickly as possible, perhaps meanwhile even inhaling supplementary oxygen.
Crime and civil unrest.
Most travellers will have the sense to avoid war zones and areas of civil unrest. However, while in strange cities, they may unwittingly stray into neighbourhoods where violent crime is prevalent and where tourists are popular targets. Instructions on safeguarding jewelry and other valuables, and maps showing safe routes from the airport to the centre of the city and which areas to shun, may be helpful in avoiding being victimized.
Fatigue.
Simple fatigue is a frequent cause of discomfort and impaired performance. A good deal of the difficulty attributed to jet lag is often the result of the rigours of travel in planes, buses and automobiles, poor sleep in strange beds and strange surroundings, overeating and alcohol consumption, and schedules of business and social engagements that are too full and demanding.
The business traveller is often bedevilled by the volume of work to clear up prior to departure as well as in preparing for the trip, to say nothing of catching up after the return home. Teaching the traveller to prevent the accumulation of undue fatigue while educating the executive to whom he or she reports to consider this ubiquitous hazard in laying out the assignment is often a key element in the travel protection programme.
Conclusion
With the increase in travel to strange and distant places for business and for pleasure, protecting the health of the traveller has become an important element in the worksite health promotion programme. It involves sensitizing the traveller to the hazards that will be encountered and providing the information and the tools needed to circumvent them. It includes medical services such as the pre-travel consultations, immunizations and provisions of medications that are likely to be needed en route. Participation by the organization’s management is also important in developing reasonable expectations for the mission, and making suitable travel and living arrangements for the trip. The goal is successful completion of the mission and the safe return of a healthy, travelling employee.
Stress Management Programmes
The essential mission of occupational health and safety is to protect and enhance the health, well-being and productivity of workers, individually and collectively. That mission cannot be accomplished without an understanding of stress and the mechanisms through which it affects individuals and organizations, and without a well-planned programme that will both alleviate its deleterious effects and, more important, prevent them.
Stress is an inescapable ingredient of the lives of all people everywhere. It stems from—and simultaneously affects—individuals’ inner sense of well-being; their relationships with family, friends, co-workers and strangers; and their capacity to function in the home, the workplace and the community. When excessive, it leads to physical or psychological symptoms and, when prolonged, it may lead to disability and disease. It modifies individuals’ perceptions, feelings, attitudes and behaviour and affects the organizations whose activities they direct or carry out. The subject of stress is covered extensively elsewhere in this Encyclopaedia.
Designing a Stress Management Programme
The effective workplace stress management programme will contain a number of overlapping elements operating concurrently. Some are formalized under the designation of a stress management programme while others are simply part of general organizational management even when they are explicitly aimed at controlling stress. Some of these are aimed at employees individually and in groups; others are aimed at stressors arising in the workplace; and still others address the stressors impinging on the organization as an entity in itself which inevitably filter down to affect some or all of the employees. The elements of a workplace stress management programme will be examined under the following headings.
1. Managing stress-related symptoms. This element deals with individuals already suffering from the effects of stress. Labelled the “medical model,” it attempts to identify individuals with signs and symptoms and to persuade them to come forward voluntarily or accept referral to professionals able to evaluate their problems, diagnose the causes and offer appropriate treatment. It may be based in the employee health service or in the employee assistance programme, or it may be associated with any other counselling services provided by the organization. The services may cover a broad range extending from one-on-one interviews and examinations to telephone “hot-lines” for emergency situations to comprehensive centres with multidisciplinary staffs of qualified professionals. It may be served by full- or part-time professionals or by contractual or casual referral arrangements with professionals who come to the worksite or are based in nearby facilities in the community. Some units deal with any and all problems, while others may more or less focus on such specific stress-related syndromes as hypertension, backache, alcoholism, drug abuse or family problems. The contributions of these service elements to the stress management programme are based on the following capabilities:
- An awareness that many recurrent or persistent somatic complaints such as muscular aches and pains, backache, headache, gastrointestinal upsets, and so on, are attributable to stress. Instead of simply providing palliative medications and advice, the alert health professional or counsellor will recognize the pattern and direct attention to the stressors that are actually responsible.
- Recognition that when a number of employees in a particular unit or area of the workplace present such functional complaints, a search should be initiated for a causative factor in the work environment which may prove to be a controllable stressor.
- Reaching out to individuals involved in or witnessing a cataclysmic occurrence such as a fatal accident, or an episode of violence.
- Seizing the opportunity to stay a disciplinary action faced by an employee because of inadequate performance or aberrant behaviour pending an opportunity to lower the stress level and restore his or her normal equanimity and work capacity.
2. Reducing individual vulnerability. The most common elements in stress management programmes are those that help individuals to cope with stress by reducing their vulnerability. These include series of seminars and workshops, supplemented by audiotapes or videotapes and pamphlets or other publications that educate employees to cope with stress more effectively. Their common denominators are these:
- Training in self-awareness and problem analysis to detect signs of increasing stress and identify the stressors that are responsible
- Assertiveness training enabling workers to become more dynamic in dealing with them
- Techniques that will reduce stress to more tolerable levels
Some of the tools they employ are listed in figure 1. For those not familiar with the term, “rap sessions” are meetings of groups of employees, with or without supervisors being present, in which experiences and problems are discussed and complaints freely ventilated. They are analogous to the shop meetings held under union auspices.
Figure 1. Some approaches to reducing vulnerability.
3. Interpersonal relations in the workplace. Organizations are being increasingly made aware of stressors emanating from the diversity of the workforce and the interpersonal problems they often present. Prejudice and bigotry do not stop at the gates of the worksite and are often compounded by insensitive or discriminatory behaviour on the part of managers and supervisors. Sexual and racial bias may take the form of harassment and may even be expressed in or evoke acts of violence. When rampant, such attitudes demand prompt correction through enunciation of an explicit policy that includes disciplinary actions against those who are guilty, coupled with protecting victims emboldened to complain against reprisals.
4. Managing job-related stressors. It is the organization’s responsibility to minimize job-related stressors that may have an adverse effect on employees’ capacity to function effectively. It is most important to ensure that supervisors and managers on all levels receive appropriate training to recognize and to deal promptly and effectively with the “people problems” that will inevitably arise in the workplace.
5. Managing the organization’s stress. The organization as an entity is exposed to stressors which, if not properly managed, filter down through the workforce, inevitably impinging on employees on all levels. This state of affairs requires the establishment of challenging but attainable goals and objectives, early identification and assessment of potential stressors that may thwart those plans, coordination of the organization’s capacities to deal with them and the communication of the results of those efforts to the workforce. The last-mentioned need is particularly critical at times of economic stringency, when employee collaboration and optimal productivity are especially important in dealing with such crises as changes in top management, threatened mergers and takeovers, plant closings or relocations. and downsizing.
6. Helping to manage personal stressors. While the management of stressors arising in the home and in the community is fundamentally a problem for the individual, employers are discovering that the stress they generate is inevitably brought into the workplace where, either on their own or in conjunction with job-related stressors, they often affect employees’ well-being and compromise their work performance. Accordingly, employers are finding it expedient (and in some instances, necessary) to establish programmes designed to assist employees to cope with stressors of this sort. A list of the most common personal stressors and workplace programmes aimed at them is presented in figure 2.
Figure 2. Stressors in the workplace and workplace programmes to help with them.
Basic Principles of the Programme
In establishing a worksite stress management programme, some basis principles must be emphasized.
First, it must be remembered that there are no boundaries between stress arising in the workplace, in the home and in the community. Each individual presents a unique composite of all of the factors which are carried wherever he or she may go. This means that while the programme must focus on those problems arising in the workplace, it must recognize that these continue to affect the worker’s outside life, nor can it ignore those originating off the job. Indeed, it has been shown that work itself and the support derived from co-workers and the organization may have a therapeutic value in dealing with personal and family problems. In fact, the loss of this support probably accounts for much of the disability associated with retirement, even when it is voluntary.
Second, stress is highly “contagious”. It not only affects particular individuals but also those about them with whom they must relate and collaborate. Thus, dealing with stress is simultaneously therapeutic and preventive.
Third, coping with stress is inherently an individual responsibility. Troubled employees can be identified and offered counselling and guidance. They can be given support and encouragement and taught to improve their coping skills. When necessary, they can be referred to qualified health professionals in the community for more intensive or prolonged therapy. But, in the last analysis, all this requires the consent and participation of the individual which, in turn, depends on the structure of the programme, its status in the organization, the competence of its staff and the reputations they earn, and its accessibility. Perhaps the most important determinant of programme success is the establishment of and strict adherence to a policy of observing the confidentiality of personal information.
Fourth, control of workplace stress is fundamentally a managerial responsibility. The programme must be based on an explicit organizational policy that places high value on employee’s health and well-being. And that policy must be reflected in the day-to-day operations by the attitudes and behaviour of managers on all levels,
Fifth, employee involvement in the programme’s design and operation and, particularly, in identifying stressors and devising ways to control them is an important ingredient of programme success. This is facilitated in many workplaces where safety and health joint labour-management committees function or where worker participation in managerial decision-making is encouraged.
Finally, a successful stress management programme requires an intimate understanding of the employees and the environment in which they work. It is most successful when stress-related problems are identified and resolved before any damage is done.
Conclusion
The essential mission of occupational health and safety is to protect and enhance the health, well-being and productivity of workers, individually and collectively. That mission cannot be accomplished without an understanding of stress and the mechanisms through which it affects individuals and organizations, and a well-planned programme that will both alleviate its deleterious effects and, more important, prevent them.
Alcohol and Drug Abuse
Introduction
Throughout history human beings have sought to alter their thoughts, feelings and perceptions of reality. Mind-altering techniques, including reduction of sensory input, repetitive dancing, sleep deprivation, fasting and prolonged meditation have been employed in many cultures. However, the most popular method for producing mood and perception changes has been the use of mind-altering drugs. Of the 800,000 species of plants on earth, about 4,000 are known to produce psychoactive substances. Approximately 60 of these have been used consistently as stimulants or intoxicants (Malcolm 1971). Examples are coffee, tea, the opium poppy, coca leaf, tobacco and Indian hemp, as well as those plants from which beverage alcohol is fermented. In addition to naturally occurring substances, modern pharmaceutical research has produced a range of synthetic sedatives, opiates and tranquillizers. Both plant-derived and synthetic psychoactive drugs are commonly used for medical purposes. Several traditional substances are also employed in religious rites and as part of socialization and recreation. In addition, some cultures have incorporated drug use into customary workplace practices. Examples include the chewing of coca leaves by Peruvian Indians in the Andes and the smoking of cannabis by Jamaican sugar cane workers. The use of moderate amounts of alcohol during farm labour was an accepted practice in the past in some Western societies, for example in the United States in the eighteenth century and the early nineteenth century. More recently, it was customary (and even required by some unions) for employers of battery burners (workers who incinerate discarded storage batteries to salvage their lead content) and house painters using lead-based paints to provide each worker with a daily bottle of whisky to be sipped during the work day in the belief—an erroneous one—that it would prevent lead poisoning. In addition, drinking has been a traditional part of certain occupations, as, for example, among brewery and distillery salespeople. These sales representatives are expected to accept the hospitality of the tavern owner on completing their order-taking.
Customs that dictate alcohol use persist in other work too, such as the “three martini” business lunch, and the expectation that groups of workers will stop at the neighbourhood pub or tavern for a few convivial rounds of drinks at the end of the work day. This latter practice poses a particular hazard for those who then drive home.
Mild stimulants also remain in use in contemporary industrial settings, institutionalized as coffee and tea breaks. However, several historical factors have combined to make the use of psychoactive substances at the workplace a major social and economic problem in contemporary life. The first of these is the trend towards employing increasingly sophisticated technology in today’s workplace. Modern industry requires alertness, unimpaired reflexes and accurate perception on the part of workers. Impairments in these areas can cause serious accidents on one hand and can interfere with the accuracy and efficiency of work on the other. A second important trend is the development of more powerful psychoactive drugs and more rapid means of drug administration. Examples are the intranasal or intravenous administration of cocaine and the smoking of purified cocaine (“freebase” or “crack” cocaine). These methods, delivering much more powerful cocaine effects than the traditional chewing of coca leaves, have greatly increased the dangers of cocaine use on the job.
Effects of Alcohol and Other Drug Usein the Workplace
Figure 1 summarizes the various ways in which the use of psychoactive substances can influence the functioning of employees in the workplace. Intoxication (the acute effects of drug ingestion) is the most obvious hazard, accounting for a wide variety of industrial accidents, for example vehicle crashes due to alcohol-impaired driving. In addition, the impaired judgement, inattention and dulled reflexes produced by alcohol and other drugs also interferes with productivity at every level, from the board room to the production line. Furthermore, workplace impairment due to drug and alcohol use often lasts beyond the period of intoxication. The alcohol-related hangover may produce headache, nausea and photophobia (light sensitivity) for 24 to 48 hours after the last drink. Workers suffering from alcohol dependence may also undergo alcohol withdrawal symptoms on the job, with shaking, sweating and gastrointestinal disturbances. Heavy cocaine use is characteristically followed by a withdrawal period of depressed mood, low energy and apathy, all of which interfere with work. Both intoxication and the after-effects of drug and alcohol use also characteristically lead to lateness and absenteeism. In addition, the chronic use of psychoactive substances is implicated in a wide range of health problems that increase society’s medical costs and time lost from work. Cirrhosis of the liver, hepatitis, AIDS and clinical depression are examples of such problems.
Figure 1. Ways in which alcohol/drug use can cause problems in the workplace.
Workers who become heavy, frequent users of alcohol or other drugs (or both) may develop a dependency syndrome, which characteristically includes a preoccupation with obtaining the drug or the money needed to buy it. Even before other drug or alcohol-induced symptoms begin to interfere with work, this preoccupation may already have started to impair productivity. Furthermore, as a result of the need for money, the employee may resort to stealing items from the workplace or selling drugs on the job, creating another set of serious problems. Finally, the close friends and family members of drug and alcohol abusers (often referred to as “significant others”) are also affected in their ability to work by anxiety, depression and a variety of stress-related symptoms. These effects may even carry over into later generations in the form of residual work problems in adults whose parents suffered from alcoholism (Woodside 1992). Health expenditures for employees with serious alcohol problems are about twice as high as health costs for other employees (Institute for Health Policy 1993). Health costs for members of their families are also increased (Children of Alcoholics Foundation 1990).
Costs to Society
For the above reasons and others, drug and alcohol use and abuse have created a major economic burden on many societies. For the United States, the societal cost estimated for the year 1985 was US$70.3 billion (thousand millions) of for alcohol and $44 billion for other drugs. Of the total alcohol-related costs, $27.4 billion (about 39% of the total) was attributed to lost productivity. The corresponding figure for other drugs was $6 billion (about 14% of the total) (US Department of Health and Human Services 1990). The remainder of the cost accruing to society as a result of drug and alcohol abuse includes the costs for the treatment of medical problems (including AIDS and alcohol-related birth defects), vehicle crashes and other accidents, crime, property destruction, incarceration and the social welfare costs of family support. Although some of these costs may be attributed to the socially acceptable use of psychoactive substances, the vast majority are associated with drug and alcohol abuse and dependence.
Drug and Alcohol Use, Abuse and Dependence
A simple way to categorize the patterns of use of psychoactive substances is to distinguish among non-hazardous use (use in socially accepted patterns that neither create harm nor involve a high risk of harm), drug and alcohol abuse (use in high risk or harm-producing ways) and drug and alcohol dependence (use in a pattern characterized by signs and symptoms of the dependence syndrome).
Both the International Classification of Diseases, 10th edition (ICD-10) and the Diagnostic and Statistical Manual of the American Psychiatric Association, 4th edition (DSM-IV) specify diagnostic criteria for drug and alcohol-related disorders. The DSM-IV uses the term abuse to describe patterns of drug and alcohol use that cause impairment or distress, including interference with work, school, home or recreational activities. This definition of the term is also meant to imply recurrent use in physically hazardous situations, such as repeatedly driving while impaired by drugs or alcohol, even if no accident has yet occurred. The ICD-10 uses the term harmful use instead of abuse and defines it as any pattern of drug or alcohol use that has caused actual physical or psychological harm in an individual who does not meet the diagnostic criteria for drug or alcohol dependence. In some cases drug and alcohol abuse is an early or prodromal stage of dependence. In others, it constitutes an independent pattern of pathological behaviour.
Both the ICD-10 and the DSM-IV use the term psychoactive substance dependence to describe a group of disorders in which there is both interference with functioning (in job, family and social arenas) and an impairment in the individual’s ability to control the use of the drug. With some substances, a physiological dependence develops, with increased tolerance to the drug (higher and higher doses required to obtain the same effects) and a characteristic withdrawal syndrome when use of the drug is abruptly discontinued.
A definition recently prepared by the American Society of Addiction Medicine and the National Council on Alcoholism and Drug Dependence of the United States describes the features of alcoholism (a term usually employed as a synonym for alcohol dependence) as follows:
Alcoholism is a primary, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking, most notably denial. Each of these symptoms may be continuous or periodic. (Morse and Flavin 1992)
The definition then goes on to explain the terms used, for example, that the qualification “primary” implies that alcoholism is a discrete disease rather than a symptom of some other disorder, and that “impaired control” means that the affected person cannot consistently limit the duration of a drinking episode, the amount consumed or the resulting behaviour. “Denial” is described as referring to a complex of physiological, psychological and culturally-influenced manoeuvres that decrease the recognition of alcohol-related problems by the affected individual. Thus, it is common for persons suffering from alcoholism to regard alcohol as a solution to their problems rather than as a cause.
Drugs capable of producing dependence are commonly divided into several categories, as listed in table 1. Each category has both a specific syndrome of acute intoxication and a characteristic combination of destructive effects related to long-term heavy use. Although individuals often suffer from dependency syndromes relating to a single substance (e.g., heroin), patterns of multiple drug abuse and dependence are also common.
Table 1. Substances capable of producing dependence.
|
Category of drug |
Examples of general effects |
Comments |
|
Alcohol (e.g., beer, wine, spirits) |
Impaired judgement, slowed reflexes, impaired motor function, somnolence, coma-overdose may be fatal |
Withdrawal may be severe; danger to foetus if used excessively in pregnancy |
|
Depressants (e.g., sleeping medicines, sedatives, some tranquillizers) |
Inattention, slowed reflexes, depression, impaired balance, drowsiness, coma-overdose may be fatal |
Withdrawal may be severe |
|
Opiates (e.g., morphine, heroin, codeine, some prescription pain medications) |
Loss of interest, “nodding”-overdose may be fatal. Subcutaneous or intravenous abuse may spread Hepatitis B, C and HIV/AIDS via needle-sharing |
|
|
Stimulants (e.g., cocaine, amphetamines) |
Elevated mood, overactivity, tension/anxiety, rapid heartbeat, constriction of blood vessels |
Chronic heavy use may lead to paranoid psychosis. Use by injection may spread Hepatitis B, C and HIV/AIDS via needle-sharing |
|
Cannabis (e.g., marijuana, hashish) |
Distorted time sense, impaired memory, impaired coordination |
|
|
Hallucinogens (e.g., LSD (lysergic acid diethylamide), PCP (phencyclidine), mescaline) |
Inattention, sensory illusions, hallucinations, disorientation, psychosis |
Does not produce withdrawal symptoms but users may experience “flashbacks” |
|
Inhalants (e.g., hydrocarbons, solvents, gasoline) |
Intoxication similar to alcohol, dizziness, headache |
May cause long- term organ damage (brain, liver, kidney) |
|
Nicotine (e.g., cigarettes, chewing tobacco, snuff) |
Initial stimulant, later depressant effects |
May produce withdrawal symptoms. Implicated in causing a variety of cancers, cardiac and pulmonary diseases |
Drug and alcohol-related disorders often affect the employee’s family relationships, interpersonal functioning and health before obvious work impairments are noticed. Therefore, effective workplace programmes cannot be limited to efforts at achieving drug and alcohol abuse prevention on the job. These programmes must combine employee health education and prevention with adequate provisions for intervention, diagnosis and rehabilitation as well as long-term follow-up of affected employees after their reintegration into the workforce.
Approaches to Drug and Alcohol-relatedProblems in the Workplace
Concern over the serious productivity losses caused by drug and alcohol abuse and dependence have led to several related approaches on the part of governments, labour and industries. These approaches include so-called “drug-free workplace policies” (including chemical testing for drugs) and employee assistance programmes.
One example is the approach taken by the United States Military Services. In the early 1980s successful anti-drug policies and drug testing programmes were established in each branch of the US military. As a result of its programme, the US Navy reported a dramatic fall in the proportion of random urine tests of its personnel that were positive for illicit drugs. The positive test rates for those under age 25 fell from 47% in 1982, to 22% in 1984, to 4% in 1986 (DeCresce et al. 1989). In 1986 the President of the United States issued an executive order requiring that all federal government employees refrain from illegal drug use, whether on or off the job. As the largest single employer in the United States, with over two million civilian employees, the federal government thereby assumed the lead in developing a national drug-free workplace movement.
In 1987, following a fatal railway accident linked to marijuana abuse, the US Department of Transportation ordered a drug and alcohol testing programme for all transportation workers, including those in private industry. Managements in other work settings have followed suit, establishing a combination of supervision, testing, rehabilitation and follow-up in the workplace that has shown consistently successful results.
The case-finding, referral and follow-up component of this combination, the employee assistance programme (EAP), has become an increasingly common feature of employee health programmes. Historically, EAPs evolved from more narrowly-focused employee alcoholism programmes that had been pioneered in the United States during the 1920s and expanded more rapidly in the 1940s during and after the Second World War. Current EAPs are customarily established on the basis of a clearly enunciated company policy, often developed by joint agreement between management and labour. This policy includes rules of acceptable workplace behaviour (e.g., no alcohol or illicit drugs) and a statement that alcoholism and other drug and alcohol dependence are considered treatable diseases. It also includes a statement of confidentiality, guaranteeing the privacy of sensitive personal employee information. The programme itself conducts preventive education for all employees and special training for supervisory personnel in identifying job performance problems. Supervisors are not expected to learn to diagnose drug and alcohol-related problems. Rather, they are trained to refer employees who show problematic job performance to the EAP, where an assessment is made and a plan of treatment and follow-up is formulated, as appropriate. Treatment is usually provided by community resources outside the workplace. EAP records are kept confidentially as a matter of company policy, with reports relating only to the subject’s degree of cooperation and general progress released to management except in cases of imminent danger.
Disciplinary action is usually suspended as long as the employee cooperates with treatment. Self-referrals to the EAP are also encouraged. EAPs that help employees with a wide range of social, mental health and drug and alcohol-related problems are known as “broad-brush” programmes to distinguish them from programmes that focus only on drug and alcohol abuse.
There is no question of the appropriateness of employers’ prohibiting the use of alcohol and other drugs during working hours or in the workplace. However, the right of the employer to prohibit the use of such substances away from the workplace during off hours has been disputed. Some employers have said, “I don’t care what employees do off the job as long as they report on time and are able to perform adequately,” and some labour representatives have opposed such a prohibition as an intrusion on the worker’s privacy. Yet, as noted above, excess use of drugs or alcohol during off-hours can affect work performance. This is recognized by airlines when they prohibit all use of alcohol by air crews during a specified number of hours prior to flight time. Although the prohibitions of alcohol use by an employee before flying or driving a vehicle are generally accepted, blanket prohibitions of tobacco, alcohol or other drug use outside of the workplace have been more controversial.
Workplace drug testing programmes
Along with EAPs, increasing numbers of employers have also instituted workplace drug testing programmes. Some of these programmes test only for illicit drugs, while others include breath or urine testing for alcohol. Testing programmes may involve any of the following components:
- pre-employment testing
- random testing of employees in sensitive positions (e.g., nuclear reactor operators, pilots, drivers, operators of heavy machinery)
- testing “for cause” (e.g., after an accident or if a supervisor has good reason to suspect that the employee is intoxicated)
- testing as part of the follow-up plan for an employee returning to work after treatment for drug or alcohol abuse or dependence.
Drug testing programmes create special responsibilities for those employers who undertake them (New York Academy of Medicine 1989). This is discussed more fully under “Ethical Issues” in the Encyclopaedia. If employers rely on urine tests in making employment and disciplinary decisions in drug-related cases, the legal rights of both employers and employees must be protected by meticulous attention to collection and analysis procedures and to the interpretation of laboratory results. Specimens must be collected carefully and labelled immediately. Because drug users may attempt to evade detection by substituting a sample of drug-free urine for their own or by diluting their urine with water, the employer may require that the specimen be collected under direct observation. Because this procedure adds time and expense to the procedure it may be required only in special circumstances rather than for all tests. Once the specimen is collected, a chain-of-custody procedure is followed, documenting each movement of the specimen to protect it from loss or misidentification. Laboratory standards must ensure specimen integrity, with an effective programme of quality control in place, and staff qualifications and training must be adequate. The test used must employ a cut-off level for the determination of a positive result that minimizes the possibility of a false positive. Finally, positive results found by screening methods (e.g., thin-layer chromatography or immunological techniques) should be confirmed to eliminate false results, preferably by the techniques of gas chromatography or mass spectrometry, or both (DeCresce et al. 1989). Once a positive test is reported, a trained occupational physician (known in the United States as a medical review officer) is responsible for its interpretation, for example, ruling out prescribed medication as a possible reason for the test results. Performed and interpreted properly, urine testing is accurate and may be useful. However, industries must calculate the benefit of such testing in relationship to its cost. Considerations include the prevalence of drug and alcohol abuse and dependence in the prospective workforce, which will influence the value of pre-employment testing, and the proportion of the industry’s accidents, productivity losses and medical benefit costs related to the abuse of psychoactive substances.
Other methods of detecting drug and alcohol-related problems
Although urine testing is an established screening method for detecting drugs of abuse, there are other methods available to EAPs, occupational physicians and other health professionals. Blood alcohol levels may be estimated by means of breath testing. However, a negative chemical test of any kind does not rule out a drug or alcohol problem. Alcohol and some other drugs are metabolized rapidly and their aftereffects may continue to impair work performance even when the drugs are no longer detectable on a test. On the other hand, the metabolites produced by the human body after the ingestion of certain drugs may remain in the blood and urine for many hours after the drug’s effects and aftereffects have subsided. A positive urine test for drug metabolites therefore does not necessarily prove that the employee’s work is drug-impaired.
In making an assessment of employee drug and alcohol-related problems a variety of clinical screening instruments are used (Tramm and Warshaw 1989). These include pencil-and-paper tests, such as the Michigan Alcohol Screening Test (MAST) (Selzer 1971), the Alcohol Use Disorders Identification Test (AUDIT) developed for international use by the World Health Organization (Saunders et al. 1993), and the Drug Abuse Screening Test (DAST) (Skinner 1982). In addition, there are simple sets of questions that can be incorporated into history-taking, for example the four CAGE questions (Ewing 1984) illustrated in figure 2. All of these methods are used by EAPs to evaluate employees referred to them. Employees referred for job performance problems such as absences, lateness and decreased productivity on the job should additionally be evaluated for other mental health problems such as depression or compulsive gambling, which may also produce impairments in job performance and are often associated with drug and alcohol-related disorders (Lesieur, Blume and Zoppa 1986). With respect to pathological gambling, a paper-and-pencil screening test, the South Oaks Gambling Screen (SOGS) is available (Lesieur and Blume 1987).
Figure 2. The CAGE questions.
Treatment of Disorders Related to theUse of Drugs and Alcohol
Although each employee presents a unique combination of problems to the addiction treatment professional, the treatment of disorders related to drug and alcohol use usually consists of four overlapping phases: (1) identification of the problem and (as necessary) intervention, (2) detoxification and general health assessment, (3) rehabilitation, and (4) long-term follow-up.
Identification and intervention
The first phase of treatment involves confirming the presence of a problem caused by the use of drugs or alcohol (or both) and motivating the affected individual to enter treatment. The employee health programme or company EAP has the advantage of using the employee’s concern both for health and job security as motivational factors. Workplace programmes are also likely to understand the employee’s environment and his or her strengths and weaknesses, and can thus choose the most appropriate treatment facility for referral. An important consideration in making a referral for treatment is the nature and extent of workplace-based health insurance coverage for the treatment of drug and alcohol-induced disorders. Policies with coverage of the full range of inpatient and outpatient treatments offer the most flexible and effective options. In addition, the involvement of the employee’s family at the intervention stage is often helpful.
Detoxification and general health assessment
The second stage combines the appropriate treatment needed to help the employee attain a drug and alcohol-free state with a thorough evaluation of the patient’s physical, psychological, family, interpersonal and work-related problems. Detoxification involves a short period—several days to several weeks—of observation and treatment for the elimination of the drug of abuse, recovery from its acute effects, and control of any symptoms of withdrawal. While detoxification and the assessment activities are progressing, the patient and “significant others” are educated about the nature of drug and alcohol dependence and recovery. They and the patient are also introduced to the principles of self-help groups, where this modality is available, and the patient is motivated to continue in treatment. Detoxification may be carried out in an inpatient or outpatient setting, depending on the needs of the individual. Treatment techniques found useful include a variety of medications, augmented by counselling, relaxation training and other behavioural techniques. Pharmacological agents used in detoxification include drugs which can substitute for the drug of abuse to relieve withdrawal symptoms and then be gradually reduced in dosage until the patient is drug-free. Phenobarbital and the longer-acting benzodiazepines are often used this way to achieve detoxification in the case of alcohol and sedative drugs. Other medicines are used to relieve withdrawal symptoms without substituting a similarly-acting drug of abuse. For example, clonidine is sometimes used in the treatment of opiate withdrawal symptoms. Acupuncture has also been used as an aid in detoxification, with some positive results (Margolin et al. 1993).
Rehabilitation
The third phase of treatment combines helping the patient establish a stable state of ongoing abstinence from all substances of abuse (including those prescription drugs which may cause dependence) and treating whatever associated physical and psychological conditions accompany the drug-related disorder. Treatment may begin on an inpatient or intensive outpatient basis, but characteristically continues in an outpatient setting for a number of months. Group, individual and family counselling and behavioural techniques may be combined with psychiatric management, which may include medication. The goals include helping patients understand their patterns of drug or alcohol use, identifying triggers for relapse after past efforts at recovery, helping them to develop drug-free coping patterns in dealing with life problems, and helping them integrate into a clean and sober social support network in the community. In some cases of opiate dependence, long-term maintenance on a long-acting synthetic opiate (methadone) or an opiate receptor blocking drug (naltrexone) is the treatment of choice. Maintenance on a daily dose of methadone, a long-acting opiate, is recommended by some practitioners for individuals with long-term opiate addiction who are unwilling or unable to achieve drug-free status. Patients stably maintained on methadone over long periods are able to function successfully in the workforce. In many cases, such patients are eventually able to detoxify and become drug free. In these cases, maintenance is combined with counselling, social services and other rehabilitative treatment. Recovery is defined in terms of stable abstinence from all drugs other than the drug of maintenance.
Long-term follow-up
The final phase of treatment continues on an outpatient basis for a year or more after a stable remission is attained. The goal of long-term follow-up is preventing relapse and helping the patient internalize new patterns of coping with life problems. The EAP or employee health service can be a great help during the rehabilitation and follow-up phases by monitoring cooperation in treatment, encouraging the recovering employee to maintain abstinence and assisting him/her in readjusting to the workplace. Where self-help or peer assistance groups are available (for example, Alcoholics Anonymous or Narcotics Anonymous), these groups provide a life-long supportive programme for sustained recovery. Since drug or alcohol dependence is a chronic disorder in which there may be relapses, company policies often require follow-up and monitoring by the EAP for a year or more after abstinence is established. If an employee relapses the EAP usually re-evaluates the situation and a change in treatment plan may be instituted. Such relapses, if brief and followed by a return to abstinence, usually do not signal overall treatment failure. Employees who do not cooperate with treatment, deny their relapses in face of clear evidence or cannot maintain stable abstinence will continue to show poor work performance and may be terminated from employment on that basis.
Women and Substance Abuse
While social changes in some areas have narrowed the differences between men and women, substance abuse has traditionally been seen as a man’s problem. Substance abuse was felt to be incompatible with women’s role in society. Consequently, while men’s abuse ot substances could be excused, or even condoned, as an acceptable part of manhood, women’s abuse of substances attracted a negative stigma. While this latter fact may be claimed to have prevented many women from abusing drugs, it has also made it extremely difficult for substance-dependent women to seek assistance for their dependence in many societies.
Negative attitudes to women’s substance abuse, coupled with the reluctance of women to admit their abuse and dependence have resulted in scanty data being available specifically on women. Even in countries with considerable information about drug abuse and dependence, it is often hard to find data relating directly to women. In cases where studies have examined women’s role in substance abuse the approach has by no means been gender-specific, so that conclusions may have been clouded by viewing women’s involvement from a male perspective.
Another factor related to the concept of substance abuse as a male problem is the lack of services for women substance abusers. ... Where services, such as treatment and rehabilitation services, do exist, they frequently have an approach based on male role models of drug dependence. Where services are provided for women, it is clear that they must be accessible. This is not always easy when women’s drug dependence is stigmatized and when cost of treatment is beyond the means of the majority of women.
Quoted from: World Health Organization 1993.
Effectiveness of Workplace-based Programmes
An investment in workplace programmes to deal with drug and alcohol problems has been profitable in many industries. An example is a study of 227 employees of a large US manufacturing company who were referred for the treatment of alcoholism by the company’s EAP. Employees were randomly assigned to three treatment approaches: (1) mandatory inpatient care, (2) mandatory attendance at Alcoholics Anonymous (AA) or, (3) a choice of inpatient care, outpatient care or AA. At follow-up, two years later, only 13% of the employees had been discharged. Of the remainder, less than 15% had job problems and 76% were rated “good” or “excellent” by their supervisors. Time absent from work fell by more than a third. Although some differences were found between initial treatment approaches the two-year job outcomes were similar for all three (Walsh et al. 1991).
The US Navy has calculated that its inpatient drug and alcohol rehabilitation programmes have produced an overall ratio of financial benefit to cost of 12.9 to 1. This figure was calculated by comparing the cost of the programme with the costs that would have been incurred in replacing the successfully rehabilitated programme participants with new personnel (Caliber Associates 1989). The Navy found that the benefit to cost ratio was highest for those over 26 years of age (17.8 to 1) as compared to younger personnel (8.2 to 1) and found the greatest benefit for alcoholism treatment (13.8 to 1), versus other drug (10.3 to 1) or polydrug dependence treatment (6.8 to 1). Nevertheless, the programme produced financial savings in all categories.
In general, workplace-based programmes for the identification and rehabilitation of employees who suffer from alcohol and other drug problems have been found to benefit both employers and workers. Modified versions of EAP programmes have also been adopted by professional organizations, such as the medical societies, nursing associations and bar associations (associations of lawyers). These programmes receive confidential reports about possible signs of impairment in a professional from colleagues, families, clients or employers. Face-to-face intervention is performed by peers, and if treatment is required the programme makes the appropriate referral. It then monitors the recovery of the individual and helps the recovering professional deal with practice and licensing problems (Meek 1992).
Conclusion
Alcohol and other psychoactive drugs are significant causes of problems in the workplace in many parts of the world. Although the type of drug used and the route of administration may vary from place to place and with the type of industry, the abuse of drugs and alcohol creates health and safety hazards for users, for their families, for other workers and, in many cases, for the public. An understanding of the types of drug and alcohol problems that exist within a given industry and the intervention and treatment resources available in the community will allow rehabilitative programmes to be developed. Such programmes bring benefits to employers, employees, their families and the larger society in which these problems arise.
More...
Employee Assistance Programmes
Introduction
Employers may recruit workers and trade unions may enlist members, but both get human beings who bring to the workplace all the concerns, problems and dreams characteristic of the human condition. As the world of work has become increasingly conscious that the competitive edge in a global economy depends on the productivity of its work force, the key agents in the workplace—management and labour unions—have devoted significant attention to meeting the needs of those human beings. Employee Assistance Programmes (EAPs), and their parallel in unions, Membership Assistance Programmes (MAPs) (hereafter referred to jointly as EAPs), have developed in workplaces around the world. They constitute a strategic response to meeting the diverse needs of a working population and, more recently, to meeting the humanist agenda of organizations of which they are a part. This article will describe the origins, functions and organization of EAPs. It is written from the point of view of the social worker’s profession, which is the major profession driving this development in the United States and one which, because of its worldwide interconnections, appears to be playing a major role in establishing EAPs worldwide.
The extent of development of employee assistance programmes varies from country to country, reflecting, as David Bargal has pointed out (Bargal 1993), the differences in degree of industrialization, state of the professional training available for appropriate personnel, degree of unionization in the employment sector and societal commitment to social issues, among other variables. His comparison of EAP development in Australia, the Netherlands, Germany and Israel leads him to suggest that although industrialization may be a necessary condition to achieve a high rate of EAPs and MAPs in a country’s workplaces, it may not be sufficient. The existence of these programmes also is characteristic of a society with significant unionization, labour/management cooperation and a well-developed social service sector in which government plays a major role. Further, there is need for a professional culture, supported by an academic specialization that promotes and disseminates social services at the workplace. Bargal concludes that the greater the aggregate of these characteristics in a given nation, the more likely that there will be extensive availability of EAP services in its workplaces.
Diversity is also apparent among programmes within individual countries in relation to structure, staffing, focus and scope of programme. All EAP efforts, however, reflect a common theme. The parties in the workplace seek to provide services to remediate the problems that employees experience, often without causal relationship to their work, that interfere with employees’ productivity on the job and sometimes with their general well-being as well. Observers have noted an evolution in EAP activities. Although the initial impetus may be the control of alcoholism or drug abuse among workers, nevertheless, over time, interest in individual workers becomes more broadly based, and the workers themselves become only one element in a dual focus that embraces the organization as well.
This organizational focus reflects an understanding that many workers are “at risk” of being unable to maintain their work roles and that the “risk” is as much a function of the way the work world is organized as it is a reflection of the individual characteristics of any particular worker. For example, ageing workers are “at risk” if the workplace technology changes and they are denied retraining because of their age. Single parents and caretakers of the elderly are “at risk” if their work environment is so rigid that it does not provide time flexibility in the face of the illness of a dependant. A person with a disability is “at risk” when a job changes and accommodations are not offered to enable the individual to perform in keeping with the new requirements. Many other examples will occur to the reader. What is significant is that, in the matrix of being able to change the individual, the environment, or some combination thereof, it has become increasingly clear that a productive, economically successful work organization cannot be achieved without consideration of the interaction between organization and individual at a policy level.
Social work rests on a model of individual in environment. The evolving definition of “at risk” has enhanced the potential contribution of its practitioners. As Googins and Davidson have noted, the EAP is exposed to a range of problems and issues affecting not only individuals, but also families, the corporation and the communities in which they are located (Googins and Davidson 1993). When a social worker with an organizational and environmental outlook functions in the EAP, that professional is in a unique position to conceptualize interventions that promote not only the EAP’s role in delivery of individual service but in advising on organizational policy in the workplace as well.
History of EAP Development
The origin of social service delivery at the workplace dates back to the time of industrialization. In the craft workshops that marked an earlier period, work groups were small. Intimate relationships existed between the master craftsman and his journeymen and apprentices. The first factories introduced larger work groups and impersonal relationships between employer and employee. As problems that interfered with the workers’ performance became apparent, employers began to provide helping individuals, often called social or welfare secretaries, to assist workers recruited from rural settings, and sometimes new immigrants, with the process of adjusting to formalized workplaces.
This focus on using social workers and other human service providers to achieve acculturation of new populations to the demands of factory labour continues internationally to this day. Several nations, for example Peru and India, legally require that work settings that exceed a particular employment level provide a human service worker to be available to replace the traditional support structure that was left behind in the home or rural environment. These professionals are expected to respond to the needs presented by the newly recruited, largely displaced rural residents in relation to concerns of everyday living such as housing and nutrition as well as those involving illness, industrial accidents, death and burial.
As the challenges involved in maintaining a productive work force evolved, a different set of issues asserted itself, warranting a somewhat different approach. EAPs probably represent a discontinuity from the earlier welfare secretary model in that they are more clearly a programmatic response to the problems of alcoholism. Pressed by the need to maximize productivity during the Second World War, employers “attacked” the losses resulting from alcohol abuse among workers by establishing occupational alcoholism programmes in the major production centres of the Western Allies. The lessons learned from the effective efforts at containing alcoholism, and the concomitant improvement in the productivity of the workers involved, received recognition after the War. Since that time, there has been a slow but steady increase in service delivery programmes worldwide that make use of the employment site as an appropriate location and centre of support for remediating problems that are identified as causes of major drains in productivity.
This trend has been aided by the development of multinational corporations that tend to replicate an effective effort, or a legally required system, in all their corporate units. They have done so almost without regard to the programme’s relevance or cultural appropriateness to the particular country in which the unit is located. For example, South African EAPs resemble those in the United States, a state of affairs accountable in part by the fact that the earliest EAPs were established in the local outposts of multinational corporations that are headquartered in the United States. This cultural crossover has been positive in that it has fostered replication of the best of each country on a worldwide scale. An example is the sort of preventive action, in relation to sexual harassment or labour force diversity issues that have come to prominence in the United States, that has become the standard to which American corporate units around the world are expected to adhere. These provide models for some local firms to establish comparable initiatives.
Rationale for EAPs
EAPs may be differentiated by their stage of development, programme philosophy or definition of what problems are appropriate to address and what services are acceptable responses. Most observers would agree, however, that these occupational interventions are expanding in scope in the countries that have already established such services, and are incipient in those nations that have yet to establish such initiatives. As already indicated, one reason for expansion can be traced to the widespread understanding that drug and alcohol abuse in the workplace is a significant problem, costing lost time and high medical care expenses and seriously interfering with productivity.
But EAPs have grown in response to a wide array of changing conditions that cross national boundaries. Unions, pressed to offer benefits to maintain the loyalty of their members, have viewed EAPs as a welcome service. Legislation on affirmative action, family leave, worker’s compensation and welfare reform all involve the workplace in a human service outlook. The empowerment of working populations and the search for gender equity that are needed for employees to function effectively in the team environment of the modern production machine, are aims that are well served by the availability of destigmatized, universal social service delivery systems that can be established in the world of work. Such systems also help with the recruitment and retention of a quality labour force. EAPs have also filled the gap in community services that exists, and seems to be increasing, in many nations of the world. The spread of, and desire to contain HIV/AIDS, as well as the growing interest in prevention, wellness and safety in general, have each contributed support to the educational role of EAPs in the world’s workplaces.
EAPs have proven a valuable resource in helping workplaces respond to the pressure of demographic trends. Such changes as the increase in single parenthood, in the employment of mothers (whether of infants or of young children), and in the number of two-worker families have required attention. The ageing of the population and the interest in reducing welfare dependency through maternal employment—facts that are apparent in most industrialized countries—have involved the workplace in roles that require assistance from human service providers. And, of course, the ongoing problem of drug and alcohol abuse that has reached epidemic proportions in many countries, has been a major concern of work organizations. A survey examining public perception of the drug crisis in 1994 as compared with five years earlier found that 50% of respondents felt it was much greater, an additional 20% felt it was somewhat greater, only 24% considered it the same and the remaining 6% felt it had declined. While each of these trends varies from country to country, all exist across countries. Most are characteristic of the industrialized world where EAPs have already developed. Many can be observed in the developing countries that are experiencing any significant degree of industrialization.
Functions of EAPs
The establishment of an EAP is an organizational decision that represents a challenge to the existing system. It suggests that the workplace has not attended adequately to the needs of individuals. It confirms the mandate for employers and trade unions, in their own organizational interest, to respond to the broad social forces at work in society. It is an opportunity for organizational change. Though resistance may occur, as it does in all situations where systemic change is attempted, the trends described earlier provide many reasons why EAPs can be successful in their quest for offering both counselling and advocacy services to individuals and policy advice to the organization.
The kinds of functions EAPs serve reflect the presenting issues to which they seek to respond. Probably every programme extant deals with drug and alcohol abuse. Interventions in this connection usually include assessment, referral, training for supervisors and operation of support groups to maintain employment and encourage abstinence. The service agenda of most EAPs, however, is more broadranging. Programmes offer counselling to those experiencing marital problems or difficulties with children, those needing help with finding day care or those making decisions concerning elder care for a family member. Some EAPs have been asked to deal with work environment issues. Their response is to give help to families adjusting to relocation, to bank employees who experience robberies and need trauma debriefing, to disaster crews, or to health care workers accidentally exposed to HIV infection. Assistance in coping with “downsizing” is supplied, too, to both those laid off and the survivors of such lay-offs. EAPs may be called on to assist with organizational change to meet affirmative action goals or to serve as case managers in achieving accommodation and return to work for employees who become disabled. EAPs have been enlisted in preventive activities as well, including good nutrition and smoking cessation programmes, encouraging participation in exercise regimes or other parts of health promotion efforts, and offering educational initiatives that can range from parenting programmes to preparation for retirement.
Although these EAP responses are multifaceted, they typify EAPs as widespread as Hong Kong and Ireland. Studying a non-random sample of American employers, trade unions and contractors who deliver EAP drug and alcohol abuse services, for example, Akabas and Hanson (1991) found that plans in a variety of industries, with different histories and under various auspices, all conform to each other in important ways. The researchers, expecting that there would be a wide variety of creative responses to dealing with workplace needs, identified, on the contrary, an astounding uniformity of programme and practice. At an International Labour Organization (ILO) international conference convoked in Washington, D.C. to compare national initiatives, a similar degree of uniformity was confirmed throughout western Europe (Akabas and Hanson 1991).
Respondents in the surveyed work organizations in the United States agreed that legislation has had a significant impact on determining the components of their programmes and the rights and expectations of client populations. In general, programmes are staffed by professionals, more often social workers than professionals of any other discipline. They respond to a broad constituency of workers, and often their family members, with services that provide diverse care for a range of presenting problems in addition to their focus on rehabilitation of alcohol and drug abusers. Most programmes overcome general inattention by top management and inadequate training for and support from supervisors, to achieve penetration rates of between 3 and 5% of the total workers at the target site. The professionals who staff the EAP and MAP movements seem to agree that confidentiality and trust are the keys to effective service. They claim success in dealing with the problems of drug and alcohol abuse although they can point to few evaluative studies to confirm the efficacy of their intervention in relation to any aspect of service delivery.
Estimates suggest that there are as many as 10,000 EAPs now in operation in settings throughout the United States alone. Two main types of service delivery systems have evolved, the one directed by an inhouse staff and the other provided by an outside contractor that offers service to numerous work organizations (employers and trade unions) at the same time. There is a raging debate as to the relative merits of internal versus external programmes. Claims of increased protection of confidentiality, greater diversity of staff and clarity of role undiluted by other activities, are made for external programmes. Advocates of internal programmes point to the advantage conferred by their position within the organization with respect to effective intervention at the systems level and to the policy-making influence that they have gained as a result of their organizational knowledge and involvement. Since organization-wide initiatives are increasingly valued, internal programmes are probably better for those worksites that have sufficient demand (at least 1,000 employees) to warrant a full-time staffer. This arrangement allows, as Googins and Davidson (1993) point out, improved access to employees because of the varied services that can be offered and the opportunity it affords to exert influence on policymakers, and it facilitates collaboration and integration of the EAP function with others in the organization—all of these capabilities strengthen the authority and role of the EAP.
Work and Family Issues: A Case in Point
The interaction of EAPs, over time, with work and family issues provides an informative example of the evolution of EAPs and of their potential for individual and organizational impact. EAPs developed, historically speaking, parallel with the period during which women entered the labour market in increasing numbers, especially single mothers and mothers of infants and young children. These women often experienced tension between their family demands for dependant care—whether children or the elderly—and their job requirements in a work environment in which the roles of work and family were considered to be separate, and management was inhospitable to the need for flexibility with respect to work and family issues. Where there was an EAP, the women brought their problems to it. EAP staffers identified that women under stress became depressed and sometimes coped with this depression by drug and alcohol abuse. Early EAP responses involved counselling on drug and alcohol abuse, education about time management, and referral to child and elder care resources.
As the number of clients with similar presenting problems mounted, EAPs carried out needs assessments that pointed to the importance of moving from case to class, that is, they began to look for group rather than individual solutions, offering, for example, group sessions on coping with stress. But even this proved to be an inadequate approach to problem resolution. With an understanding that needs differ across the life cycle, EAPs began thinking about their client population in age-related cohorts that had different requirements. Young parents needed flexible leave to care for sick children and easy access to child care information. Those in their middle thirties to late forties were identified as the “sandwich generation”; at their time of life, the twofold demands of adolescent children and ageing relatives increased the need for an array of support services that included education, referral, leave, family counselling and abstinence assistance, among others. The mounting pressures experienced by ageing workers who face the onset of disability, the need to accommodate to a work world in which almost all one’s associates, including one’s supervisors, are younger than oneself, while planning for retirement and dealing with their frail elderly relatives (and sometimes with the parenting demands of the children of their children), create yet another set of burdens. The conclusion drawn from monitoring these individual needs and the service response to them was that what was required was a change in workplace culture that integrated the work and family lives of employees.
This evolution has led directly to the emergence of the EAP’s current role with respect to organizational change. During the process of meeting individual needs, it is probable that any given EAP has built up credibility within the system and is regarded by the key people as the source of knowledge about work and family issues. Likely, it has served an educational and informational role in response to questions raised by managers in numerous departments affected by the problems that occur when these two aspects of human life are experienced in conflict with each other. The EAP has probably collaborated with many organizational actors, including affirmative action officers, industrial relations experts, union representatives, training specialists, safety and health personnel, the medical department staff, risk managers and other human resource personnel, and fiscal workers, and line managers and supervisors.
A force field analysis, a technique suggested in the 1950s by Kurt Lewin (1951), provides a framework for defining the activities necessary to undertake to produce organizational change. The occupational health professional should understand where there will be support within the organization to resolve work and family issues on a systemic basis, and where there might be opposition to such a policy approach. A force field analysis should identify the key actors in the corporation, union or government agency who will influence change, and the analysis will summarize the promoting and restraining forces that will influence these actors in relation to work and family policy.
A sophisticated outcome of an organizational approach to work and family issues will have the EAP participating in a policy committee that establishes a statement of purpose for the organization. The policy should recognize the dual interests of its employees in being both productive workers and effective family participants. Expressed policy should indicate the organization’s commitment to establishing a flexible climate and work culture in which such dual roles can exist in harmony. Then an array of benefits and programmes may be specified to fulfil that commitment including, but not limited to, flexible work schedules, job sharing and part-time employment options, subsidized or onsite child care, an advice and referral service to assist with other child and eldercare needs, family leave with and without pay to cover demands deriving from illness of a relative, scholarships for children’s education and for employees’ own development, and individual counselling and group support systems for the variety of presenting problems experienced by family members. These manifold initiatives related to work and family issues would combine to allow a total individual and environmental response to the needs of workers and their work organizations.
Conclusions
There is ample experiential evidence to suggest that the provision of these benefits assists workers to their goal of productive employment. Yet these benefits have the potential to become costly programmes and they offer no guarantee that work will be performed in an effective and efficient manner as a result of their implementation. Like the EAPs that foster them, work and family benefits must be assessed for their contribution to the organization’s effectiveness as well as to the well-being of its many constituencies. The uniformity of development, described earlier, can be interpreted as support for the fundamental value of EAP services across work places, employers and nations. As the world of work becomes increasingly demanding in the era of a competitive global economy, and as the knowledge and skill that workers bring to the job becomes more important than their mere presence or physical strength, it seems safe to predict that EAPs will be called upon increasingly to provide guidance to organizations in fulfilling their humanist responsibilities to their employees or members. In such an individual and environmental approach to problem solving, it seems equally safe to predict that social workers will play a key role in service delivery.
Health in the Third Age: Pre-retirement Programmes
It is increasingly being recognized that the last third of life—the “third age”—requires as much thought and planning as do education and training (the “first age”) and career development and retraining (the “second age”). About 30 years ago, when the movement to address the needs of the retired began, the average male employee in the United Kingdom, and in many other developed countries as well, retired at the age of 65 as a rather worn-out worker with a limited life expectancy and, especially if he was a blue collar worker or labourer, with an inadequate pension or none at all.
This scene has been changing dramatically. Many people are retiring younger, voluntarily or at ages other than those dictated by mandatory retirement regulations; for some, early retirement is being forced upon them by illness and disability and by redundancy. At the same time, many others are electing to continue to work long past the “normal” retirement age, in the same job or in another career.
By and large, today’s retirees generally have better health and longer life expectancies. Indeed, in the United Kingdom, the over-80s are the fastest growing group in the population, while more and more people are living into their 90s. And with the surge of women into the workforce, a growing number of the retirees is female, many of whom, owing to longer life expectancies than their male counterparts, will be single or widowed.
For a time—two decades or longer for some—most retirees retain mobility, vigour and functional capacities honed by experience. Thanks to higher living standards and advances in medical care, this period continues to extend. Sadly, however, many live longer than their biological structures were designed for (i.e., some of their bodily systems give up efficient service while the rest struggle on), causing increasing medical and social dependency with ever fewer compensatory enjoyments. The goal of retirement planning is to enhance and extend enjoyment of the period of well-being and ensure to the extent possible the resources and support systems needed during the final decline. It goes beyond estate planning and the disposition of property and assets, although these are often important elements.
Thus, retirement today can offer immeasurable compensations and benefits. Those who retire in good health can expect to live another 20 to 30 years, enjoying potentially purposeful activity for at least two-thirds of this period. This is far too long to drift about doing nothing in particular or rotting away on some sunny “Costa Geriatrica”. And their ranks are being swelled by those who retire early by choice or, sadly, because of redundancy, and by women, too, more of whom are retiring as adequately pensioned workers expecting to remain purposefully active rather than to live as dependants.
Fifty years ago, pensions were inadequate and economic survival was a struggle for most of the elderly. Now, employer-provided pensions and general welfare benefits supplied by government agencies, although still inadequate for many, do allow a not too unreasonable existence. And, because the skilled workforce is shrinking in many industries while employers are recognizing that older workers are productive and often more reliable employees, opportunities for third-agers to get part-time employment are improving.
Further, the “retired” now form about a third of the population. Being sound in mind and limb, they are an important and potentially contributory segment of society which, as they recognize their importance and potential, can organize themselves to pull much more weight. An example in the United States is the American Association of Retired Persons (AARP), which offers to its 33 million members (not all of whom are retired, since membership in the AARP is open to anyone aged 50 or over) a broad range of benefits and exercises considerable political influence. At the first Annual General Meeting of the United Kingdom’s Pre-Retirement Association (PRA) in 1964, Lord Houghton, its president, a member of the Cabinet, said, “If only pensioners could get their act together, they could swing an election.” This has not yet happened, and probably never will in these terms, but it is now accepted in most developed countries that there is a “third age”, comprising a third of the population that has both expectations and needs along with an enormous potential for contributing to the benefit of its members and to the community as a whole.
And with this acceptance, there has been a growing realization that adequate provision and opportunity for this group is vital to social stability. Over the last few decades, politicians and governments have begun to respond through extension and improvement of the variety of “social security” and other welfare programmes. These responses have been handicapped both by fiscal exigencies and by bureaucratic rigidities.
Another, major, handicap has been the attitude of the pensioners themselves. Too many have accepted the stereotyped personal and social image of retirement as both the end of recognition as a useful or even deserving member of society and the expectation of being shunted into a backwater where one can be conveniently forgotten. Overcoming this negative image has been, and to a degree still is, the main objective of training for retirement.
As more and more retirees accomplished this transformation and looked to fulfil the needs that emerged, they became aware of the shortcomings of government programmes and began to look to employers to fill the gap. Thanks to accumulated savings and employer-provided pension programmes (many of which were shaped through collective bargaining with unions), they discovered financial resources that were often considerable. To enhance the value of their private pension schemes, employers and unions began to arrange for (and even offer) programmes providing advice and support in managing them.
In the United Kingdom, credit for this is largely due to the Pre-Retirement Association (PRA) which, with government support through the Department of Education (initially, this programme was shunted among the Departments of Health, Employment, and Education), is being accepted as the mainstream of retirement preparation.
And, as the thirst for such guidance and assistance has grown, a veritable industry of voluntary and for-profit organizations has come into existence to meet the demand. Some function quite altruistically; others are self-serving, and include insurance companies that wish to sell annuities and other insurance, investment firms that manage accumulated savings and pension income, real estate brokers selling retirement homes, operators of retirement communities seeking to sell memberships, charities that offer advice on the tax benefits of making contributions and bequests, and so on. These are supplemented by an army of publishers offering “how-to” books, magazines, audiotapes and videotapes, and by colleges and adult education organizations that offer seminars and courses on relevant topics.
While many of these providers focus primarily on coping with financial, social or family problems, recognition that well-being and productive living are dependent on being healthy has led to the increasing prominence of health education and health promotion programmes intended to avert, defer or minimize illness and disability. This is particularly the case in the United States, where employers’ financial commitment for the escalating costs of health care for retirees and their dependants has not only become a very weighty burden but now must be projected as a liability on the balance sheets included in corporation annual reports.
Indeed, some of the categorical voluntary health organizations (e.g., heart, cancer, diabetes, arthritis) produce educational materials specifically designed for employees approaching retirement age.
In short, the third age has arrived. Pre-retirement and retirement programmes offer opportunities both for maximizing personal and social well-being and function and for providing the necessary understanding, training and support.
Role of the Employer
Although far from universal, the main support and funding for pre-retirement programmes has come from employers (including local and central governments and the armed forces). In the United Kingdom, this was in large part due to the efforts of the PRA, which, early on, initiated company membership through which employees are provided with encouragement, advice and in-house courses. It has, in fact, not been difficult to convince commerce and industry that they have a responsibility far beyond the mere provision of pensions. Even there, as pension schemes and their tax implications have become more complicated, detailed explanations and personalized advice have become more important.
The workplace provides a convenient captive audience, making the presentation of programmes more efficient and less costly, while peer pressure enhances employee participation. The benefits to the employees and their dependants are obvious. The benefits to the employers are substantial, albeit more subtle: improved morale, the enhancement of the company’s image as a desirable employer, encouragement for retaining older employees with valuable experience, and retaining the good will of retirees, many of whom, thanks to profit-sharing and company-sponsored investment plans, are also shareholders. When workforce reductions are desired, employer-sponsored pre-retirement programmes are often presented to enhance the attractiveness of the “golden handshake,” a package of inducements for those accepting early retirement.
Similar benefits accrue to trade unions who offer such programmes as an adjunct to union-sponsored pension programmes: making union membership more attractive and enhancing good will and esprit de corps among union members. It should be noted that interest among the trade unions in the United Kingdom is only beginning to develop, primarily among the smaller and professional unions, like that of the airline pilots.
The employer may contract for a complete, “pre-packaged” programme or assemble one from the list of individual elements offered by organizations like the PRA, assorted adult educational institutions and the many investment, pension and insurance firms that offer retirement training courses as a commercial venture. Although generally of a high standard, the latter have to be monitored to be sure that they provide straightforward, objective information rather than promotion of the provider’s own products and services. The employer’s departments of personnel, pension and, where there is one, education, should be involved in assembling and presenting the programme.
The programmes may be given entirely in-house or at a conveniently located facility in the community. Some employers offer them during working hours but, more often, they are made available during lunch periods or after hours. The latter are more popular because they minimize interference with work schedules and they facilitate the attendance of spouses.
Some employers cover the entire cost of participation; others share it with the employees while some rebate all or part of the employee’s share on successful completion of the programme. While faculty should be available for answers to questions, participants are usually referred to appropriate experts when individualized personal consultations are needed. As a rule, these participants accept responsibility for any costs that may be required; sometimes, when the expert is affiliated with the programme, the employer may be able to negotiate reduced fees.
Pre-retirement Course
Philosophy
For many people, especially those who have been workaholics, separation from work is a wrenching experience. Work provides status, identity and association with other people. In many societies, we tend to be identified and to identify ourselves socially by the jobs we do. The work context that we are in, especially as we grow older, dominates our lives in terms of what we do, where we go and, particularly for professional people, our daily priorities. Separation from co-workers, and a sometimes unhealthy level of preoccupation with minor family and household affairs, indicate a need for developing a new frame of social reference.
Well-being and survival in retirement depend on understanding these changes and setting out to make the most of the opportunities they present. Central to such understanding is the concept of maintenance of health in the widest sense of the World Health Organization definition and a more modern acceptance of a holistic approach to medical problems. Establishment of and adherence to a healthful life style must be supplemented by properly managing finances, housing, activities and social relationships. Preserving financial resources for the time when increasing disability requires special care and assistance that may increase the cost of living is often more important than estate planning.
Organized courses which provide information and guidance may be considered the keystone of pre-retirement training. It is sensible for the course organizers to realize that the aim is not to provide all the answers but to delineate possible problem areas and point the way to the best solutions for each individual.
Topic areas
Pre-retirement programmes may include a variety of elements; the following briefly described topics are the most fundamental and should be assured a place among any programme’s discussions:
Vital statistics and demography.
Life expectancies at relevant ages—women live longer than men—and trends in family composition and their implications.
Understanding retirement.
The lifestyle, motivational and opportunity-based changes to be required over the next 20 to 30 years.
Health maintenance.
Understanding the physical and mental aspects of ageing and elements of the lifestyle that will promote optimal well-being and functional capacity (e.g., physical activity, diet and weight control, coping with failing vision and hearing, increased sensitivity to cold and hot weather, and use of alcohol, tobacco and other drugs). Discussions of this topic should include dealing with doctors and the health care system, periodic health screening and preventive interventions, and attitudes toward illness and disability.
Financial planning.
Understanding the company’s pension plan as well as potential social security and welfare benefits; managing investments to preserve resources and maximize income, including the investment of lump sum payments; managing home ownership and other properties, mortgages, and so on; continuation of employer/union-sponsored and other health insurance, including consideration of long-term care insurance, if available; how to select a financial advisor.
Domestic planning.
Estate planning and making a will; executing a living will (i.e., the setting forth of “medical directives” or naming a health care proxy) containing wishes about what treatments should or should not be administered in the event of potentially terminal illness and inability to participate in decision-making; relationships with spouse, children, grandchildren; coping with constriction of social contacts; role reversal in which the wife continues a career or outside activities while the husband takes more responsibility for cooking and homemaking.
Housing.
Home and garden may become too large, costly and burdensome as financial and physical resources shrink, or it may be too small as the retiree recreates an office or workshop in the home; with both spouses at home, it is helpful, if possible, to arrange for each to have his and her own territory to provide a modicum of privacy for activities and reflection; consideration of moving to another area or country or to a retirement community; availability of public transportation if automobile driving becomes imprudent or impossible; preparing for eventual frailty; assistance with homemaking and social contacts for the single person.
Possible activities.
How to find opportunities and training for new jobs, hobbies and volunteer activities; educational activities (e.g., completion of interrupted diploma and degree courses); travel (in the United States, Elderhostel, a voluntary organization, offers a large catalogue of year-round one-week or two-week adult education courses given at college campuses and vacation resorts throughout the United States and internationally).
Time management.
Developing a schedule of meaningful and enjoyable activities that balance individual and joint involvement; while new opportunities for “togetherness” are a benefit of retirement, it is important to realize the value of independent activities and to avoid “getting in each other’s way”; group activities including clubs, church and community organizations; recognizing the motivational value of ongoing paid or voluntary work commitments.
Organizing the course
The type, content and length of the course are usually determined by the sponsor on the basis of the available resources and expected costs, as well as the level of commitment and the interests of employee participants. Few courses will be able to cover all of the above topic areas in exhaustive detail, but the course should include some discussion of most (and preferably all) of them.
The ideal course, educators tell us, is of the day-release type (employees attend the course on company time) with about ten sessions in which participants can get to know each other and instructors can explore individual needs and concerns. Few companies can afford this luxury, but Pre-Retirement Associations (of which the United Kingdom has a network) and adult education centres run them successfully. The course may be presented as a short-term entity—as a two-day course which allows participants more discussion and more time for guidance in activities is probably the best compromise, rather than as a one-day course in which condensation requires more didactic than participative presentations—or it may involve a series of more or less brief sessions.
Who attends?
It is prudent that the course be open to spouses and partners; this may influence its location and timing.
Clearly, every employee facing retirement should be given the opportunity to attend, but the problem is the mix. Senior executives have very different attitudes, aspirations, experiences and resources than relatively junior executives and line staff. Widely differing educational and social backgrounds may inhibit the free-wheeling exchanges that make the courses so valuable to participants, particularly with respect to finances and post-retirement activities. Very large classes dictate a more didactic approach; groups of 10 to 20 facilitate valuable exchanges of concerns and experiences.
Employees in large companies which emphasize corporate identity, like IBM in the United States and Marks & Spencer in the United Kingdom, often find it difficult to fit into the wide world without the “big brother” aura to support them. This is particularly true of the separate services in the armed forces, at least in the United Kingdom and the United States. At the same time in such tightly-knit groups, employees sometimes find it difficult to express concerns that might be construed as company disloyalty. This does not appear as much of a problem when courses are given off-site or include employees of number of companies, a necessity when smaller organizations are involved. These “mixed” groups are often less formal and more productive.
Who teaches?
It is essential that the instructors have the knowledge and, especially, the communication skills required to make the course a useful and pleasurable experience. While the company’s personnel, medical and education departments may be involved, qualified consultants or academicians are often considered to be more objective. In some instances, qualified instructors recruited from among the company’s retirees can combine greater objectivity with knowledge of the company environment and culture. Since it is rare for any one individual to be expert in all of the issues involved, a course director supplemented by several specialists is usually desirable.
Supplemental materials
The course sessions are usually supplemented by workbooks, videotapes and other publications. Many programmes include subscriptions to pertinent books, periodicals, and newsletters, which are most effective when addressed to the home, where they may be shared by spouses and family members. Membership in national organizations, like PRA and AARP or their local counterparts, provides access to useful meetings and publications.
When is the course given?
Pre-retirement programmes generally begin about five years before the scheduled retirement date (recall that AARP membership becomes available at age 50, regardless of planned retirement age). In some companies, the course is repeated every one or two years, with employees invited to take it as often as they wish; in others, the curriculum is divided into segments given in successive years to the same group of participants with content varying as the retirement date approaches.
Course evaluation
The number of eligible employees electing to participate and the rate of drop-out are perhaps the best indicators of the utility of the course. However, a mechanism should be introduced so that participants can feed back their impressions of the course content and the quality of the instructors as a basis for making changes.
Caveats
Courses with uninspired presentations of largely irrelevant material are not likely to be very successful. Some employers use questionnaire surveys or conduct focus groups to probe the interests of potential participants.
An important point in the decision-making process is the state of employer/employee relations. When hostility is overt or just beneath the surface, employees are not likely to assign great value to anything the employer offers, especially if it is labelled “for your own good”. Employee acceptance can be enhanced by having one or more staff committees or union representatives involved in the design and planning.
Finally, as retirement approaches and becomes a way of life, circumstances change and new problems arise. Accordingly, periodic repetition of the course should be planned, both for those who might benefit from a rerun and those who are newly approaching the “third age”.
Post-retirement Activities
Many companies continue contact with retirees throughout their lives, often together with their surviving spouses, especially when employer-sponsored health insurance is continued. Periodic health screenings and health education and promotion programmes designed for “seniors” are provided and, when needed, access to individual consultations on health, financial, domestic and social problems is made available. An increasing number of larger companies subsidize pensioner clubs which may have more or less autonomy in programming.
Some employers make a point of rehiring retirees on a temporary or part-time basis when extra help is needed. Other examples from New York City include: the Equitable Life Assurance Society of the United States, which encourages retirees to volunteer their services to non-profit-making community agencies and educational institutions, paying them a modest stipend to offset commuting and incidental out-of-pocket expenses; the National Executive Service Corps, which arranges to provide the expertise of retired executives to companies and government agencies around the world; the International Ladies Garment Workers Union (ILGWU), which has instituted the “Friendly Visiting Program,” which trains retirees to provide companionship and useful services to members beset by problems of ageing. Similar activities are sponsored by pensioner clubs in the United Kingdom.
Except for employer/union-sponsored pensioner clubs, most post-retirement programmes are carried out by adult education organizations through their offerings of formal courses. In the United Kingdom, there are several nationwide pensioner groups like PROBUS which holds regular local meetings to provide information and social contacts to their members, and the PRA which offers individual and corporate membership for information, courses, tutors and general advice.
An interesting development in the United Kingdom, based on a similar organization in France, is the University of the Third Age, which is centrally coordinated with local groups in the larger towns. Its members, mostly professionals and academics, work to broaden their interests and extend their knowledge.
Through their regular intramural publications as well as in materials specifically prepared for retirees, many companies and unions provide information and advice, often spiced with anecdotes about retirees’ activities and experiences. Most developed countries have at least one or two general circulation magazines aimed at retirees: France’s Notre Temps has a large circulation among third agers and, in the United States, AARP’s Modern Maturity goes to its more than 33 million members. In the UK there are two monthly publications for the retired: Choice and SAGA Magazine. The European Commission is currently sponsoring a multi-language retirement workbook, Making the Most of Your Retirement.
Eldercare
In the many developed countries, employers are becoming increasingly aware of the impact of the problems faced by employees with elderly or disabled parents, in-laws and grandparents. Although some of these may be pensioners of other companies, their needs for support, attention, and direct services may be significant burdens for the employees who must contend with their own jobs and personal affairs. To ease those burdens and reduce the consequent distraction, fatigue, absenteeism and lost productivity, employers are offering “eldercare programmes” to these caregivers (Barr, Johnson and Warshaw 1992; US General Accounting Office 1994). These provide various combinations of education, information and referral programmes, modified work schedules and respite leaves, social support, and financial aid.
Conclusion
It is abundantly clear that demographic and social workforce trends in the developed countries are producing increasing awareness of the need for information, training and advice across the whole spectrum of “third age” problems. This awareness is being appreciated by employers and labour unions—and by politicians, as well—and is being translated into pre-retirement programmes and post-retirement activities which offer potentially great benefits to the ageing, their employers and unions, and society at large.
Outplacement
Outplacement is a professional consulting service that helps organizations plan and implement individual terminations or reductions in their workforces so as to minimize disruptions and avoid legal liability, and counsels terminated employees in order to minimize the trauma of separation while orienting them towards seeking alternative employment or new careers.
The economic downturn of the 1980s, which continues in the 1990s, has been characterized by a virtual pandemic of job terminations reflecting the closing down of obsolescent or unprofitable units, plants and businesses, the elimination of redundancies created by mergers, takeovers, consolidations and reorganizations, and the trimming of staff to reduce operating costs and produce a “lean and mean” workforce. Although less striking than in private industry thanks to the protection of civil service regulations and political pressures, the same phenomenon has also been seen in government organizations struggling to cope with budget deficits and a philosophy that less government is desirable.
For the terminated employees, job loss is a potent stressor and source of trauma, especially when the manner of dismissal is sudden and brutal. It generates anger, anxiety and depression and may cause decompensation in persons with marginal adjustment to chronic mental illness. Rarely, the anger may express itself in sabotage or violence aimed at the supervisors and managers responsible for the termination. Sometimes, the violence is directed at spouses and family members.
The trauma of job loss has also been associated with physical ailments ranging from headaches, gastrointestinal disturbances and other functional complaints to stress-related disorders such as heart attacks, bleeding peptic ulcers and colitis.
In addition to the financial impact of loss of earnings and, in the United States, loss of employer-sponsored health insurance, job loss also affects the health and well-being of the families of the terminated employees.
Employees who are not terminated are also affected. Despite employers’ reassurances, there often is concern over the possibility of additional layoffs (threatened job loss has been found to be an even more potent stressor than actual loss of the job). In addition, there is the stress of adjusting to changes in work load and job content as relationships with co-workers are reshuffled. “Downsizing”, or reduction in the size of a workforce, may also be traumatic to the employer. It may take significant time and effort to smooth out the resultant organizational disruptions and achieve the desired productive efficiency. Valuable employees not scheduled for termination may leave for other, ostensibly more secure jobs and better-organized firms. There is also the potential of legal liability stemming from discharged employees’ allegations of breach of contract or unlawful discrimination.
Outplacement—A Preventive Approach
Outplacement is a professional service offered to prevent, or at least minimize, the trauma of staff reduction for terminated employees, those who remain and the employer.
Not all discharged employees require assistance. For some, the termination precipitates an opportunity to seek new work that might provide welcome relief from a job that had become stultifying and offered little hope of advancement. For most, however, professional counselling in working through the almost inevitable disappointment and anger of dismissed employees and help in finding new jobs can facilitate the restoration of their sense of self-worth and their well-being. Even those who accept the lure of the “golden handshake” (a package of enhanced severance and retirement benefits) and leave voluntarily may benefit from help in making the necessary readjustments.
It is generally agreed that outplacement services are most inexpensively provided by in-house staff. However, even a large organization with a competent and well-functioning staff may not have had much experience with the sensitive work of downsizing and may be too busy planning the restructuring of the organization following the exodus to attend to the niceties that may be involved. Even hardened executives often find it difficult to deal with their erstwhile co-workers. Furthermore, the departing employees are more likely to give credibility to advice from a “neutral” resource.
Accordingly, the vast majority of organizations find it expedient to contract with an outplacement consultant or consulting firm. This neutrality is reinforced by having all possible outplacement contacts located offsite in separate quarters occupied even temporarily by the consultant(s).
Outplacement Process
The outplacement process for terminated employees needs to be individualized depending on their attitudes, capabilities and circumstances, and the nature of the job market locally or in other regions. For non-exempt production workers and first-line supervisors, it involves an inventory of the worker’s skills and, where there is a market for them, assistance in placement. Where no suitable jobs exist, it involves assessment of the potential for retraining, referral for retraining, and assistance in marketing the new skills. An unfortunate complication that is difficult to overcome arises when the pay scales for the available new jobs do not measure up to the earnings of the former employment.
For employees in managerial and “creative” positions, the process generally involves a number of phases that are frequently overlapping. These phases are considered under the following heads.
Leaving the past employer.
The object is to help the candidate through the stages of reaction, understanding and acceptance of his or her predicament. Occasionally, this may require the intervention of a mental health professional.
This usually involves a reevaluation of the termination event. To earn the candidate’s confidence and assist in establishing a desirable rapport, the consultant generally reviews the circumstances of the termination and makes certain that the candidate understands them and, furthermore, has received all of the monetary and other benefits to which he or she may be entitled.
This phase concludes when the candidate is able to deal constructively with the immediate problems and responsibilities and is ready to start preparing for the future with a positive attitude. Ideally, some measure of reconciliation has been established with the past employer and the candidate is willing to accept whatever support may be offered. Such support may include temporary use of an office with a business address and telephone, supplemented by the services of a secretary who can provide typing and photocopying services, take messages, confirm appointments, etc. Most candidates function more effectively from an business-like office environment than from their own homes. Also, the consultant helps formulate a mutually satisfactory reason for the termination and arrange a mutually acceptable response to requests for references from potential employers.
Preparation for new employment.
This phase is intended to provide the focus and structure for positive thinking and action. It involves a start of the recovery of self-confidence (which continues throughout the process) by building a personal data base of the candidate’s skills, abilities, knowledge and experience, and learning to communicate it in clear, functional terms. Simultaneously, the candidate begins to identify and confirm suitable job objectives and to consider the nature of the jobs for which his or her background might be particularly suitable. Through it all, the candidate acquires the knack of accumulating and organizing information that will highlight the range and depth of his or her experience and level of competence.
Résumé writing.
Here, the candidate learns to develop a flexible tool that will present his or her objectives, qualifications, and background, arouse the interest of potential employers, help obtain interviews, and serve as an aid during job interviews. Rather than being restricted to a fixed format, the résumé is varied to “package” skills and experiences to make them most attractive for particular job opportunities.
Assessing job opportunities.
The consultant guides the candidate to an assessment of the availability of potential jobs that might be suitable. This includes a survey of different industries, the job market in different localities, opportunities for growth and advancement, and likely earning potential. Experience indicates that about 80% of job opportunities are “hidden,” that is, they are not readily apparent on the basis of industry designation or job title. Where appropriate, the assessment also includes an appraisal of the potential of self-employment.
Job-hunting campaign.
This involves identifying and exploring existing and potential opportunities through direct approaches to potential employers and developing and making use of contacts and intermediaries. The campaign entails obtaining interviews with the “right” people on a right basis, and using letters both to obtain interviews and as a follow-up to interviews.
The consultant will, as part of enhancing the candidate’s job-hunting skills, improve his or her writing and interview techniques. Practice in letter writing is aimed at polishing a communication skill that is uniquely helpful in defining job opportunities, in identifying the “right” people and developing contacts with them, obtaining interviews with them and in following up on interviews. The candidate is further trained by interview coaching, which involves role playing and critiquing videotapes of practice interviews in order to maximize the effectiveness with which his or her personality, experience and desires are presented. The candidate’s chances of coming away from an interview, with, at least, an appointment for the next interview, if not an actual job offer, are by this means enhanced.
Negotiating compensation.
The consultant will help candidates overcome their dislike or even fear of discussing compensation in negotiating a potential position so that they can obtain the best compensation package possible under the existing circumstances, avoiding the possibility of over-selling or under-selling themselves or antagonizing the interviewer.
Control.
Within the limits of the consulting contract, regular contact with the candidate is maintained until a new position is maintained. This involves gathering and organizing information to track how the campaign is progressing and to ensure optimal use of time and effort. It will help the candidate to avoid errors of omission and provide a signal to correct errors of commission.
Following through.
When a new position is obtained, the candidate notifies the consultant and the old employer as well as other prospective employers with whom he or she may have been negotiating.
Follow-up.
Again, within the limits of the contract, the consultant maintains contact to assist the candidate’s adjustment to the new position to aid in overcoming any adverse factors and to encourage continuing career growth and development. Finally, at the close of the programme, the consultant provides the employer with an aggregate report of the results (personal and/or sensitive information is usually held confidential).
The organization
It is rare for the outplacement consultant to be involved in designating specifically which employees are to be separated and which will remain — that is a decision usually made by the organization’s top management, often in consultation with department heads and line supervisors and in the light of the structure envisioned for the revised organization. The consultant, however, does provide guidance on the planning, timing and staging of the downsizing process and on the communications with both those who will leave and those who will remain. Since the “grapevine” (i.e., rumors circulating in the workforce) is usually active, it is imperative that these communications be timely, complete and accurate. Proper communications will also help address potential allegations of discrimination. The consultant also often assists with public relations communications to the industry, customers and the community.
Caveats
The extent of downsizing during the last decade, at least in the United States, has given impetus to development of a veritable industry of outplacement consultants and firms. A number of search firms devoted to identifying candidates for job vacancies have taken up outplacement as a side-line. A variety of semiprofessionals, including former personnel directors, have become outplacement counsellors.
Until recently, there was no formally adopted code of practice and ethical standards. However, in 1992, the International Association of Outplacement Professionals (IAOP) sponsored the creation of the Outplacement Institute, membership in which requires meeting a set of criteria based on educational background and personal experience, evidence of continuing participation in programs of personal and professional development, and a commitment to uphold and observe the published IAOP Standards for Ethical Practice.
Conclusion
Reduction in the size of a workforce is, at best, a trying experience for the employees being terminated or forced into retirement, and for those remaining and for the organization as a whole. It is invariably traumatic. Outplacement is a professional consulting service designed to prevent or minimize the potential adverse effects and promote the health and well-being of those involved.
Standards, Principles and Approaches in Occupational Health Services
This article is based on the standards, principles and approaches embodied in the ILO Occupational Health Services Convention, 1985 (No. 161) and its accompanying Recommendation (No. 171); ILO Occupational Safety and Health Convention, 1981 (No. 155) and its accompanying Recommendation (No. 164); and the Working Document of the Twelfth Session of the Joint ILO/WHO Committee on Occupational Health, 5-7 April 1995.
The ILO Occupational Health Services Convention (No. 161) defines “occupational health services” as services entrusted with essentially preventive functions and responsible for advising the employer, the workers and their representatives in the undertaking on the requirements for establishing and maintaining a safe and healthy working environment which will facilitate optimal physical and mental health in relation to work and the adaptation of work to the capabilities of workers in the light of their state of physical and mental health.
Provision of occupational health services means carrying out activities in the workplace with the aim of protecting and promoting workers’ safety, health and well-being, as well as improving working conditions and the working environment. These services are provided by occupational health professionals functioning individually or as part of special service units of the enterprise or of external services.
Occupational health practice is broader and consists not only of the activities performed by the occupational health service. It is multidisciplinary and multisectoral activity involving in addition to occupational health and safety professionals other specialists both in the enterprise and outside, as well as competent authorities, the employers, workers and their representatives. Such involvement requires a well-developed and well-coordinated system at the workplace. The necessary infrastructure should comprise all the administrative, organizational and operative systems that are needed to conduct the occupational health practice successfully and ensure its systematic development and continuous improvement.
The most elaborate infrastructure for occupational health practice is described in the ILO Occupational Safety and Health Convention, 1981 (No. 155) and the Occupational Health Services Convention, 1985 (No. 161). The establishment of occupational health services according to the models advocated by the Convention No. 161 and its accompanying Recommendation No. 171 is one of the options. It is however evident that the most advanced occupational health services are in concordance with the ILO instruments. Other types of infrastructures may be used. Occupational medicine, occupational hygiene and occupational safety may be practised separately or together within the same occupational health service. The occupational health service may be a single integrated entity or a composite of different occupational health and safety units unified by a common concern for workers’ health and well-being.
Availability of Occupational Health Services
Occupational health services are unevenly distributed in the world (WHO 1995b). In the European Region, about half of the working population remains uncovered by competent occupational health services; the variation among countries is very wide, with coverage figures ranging between 5% and 90% of the workforce. The Central and Eastern European countries now in transition are having problems in providing services due to reorganization of their economic activities and the break-up of the large centralized industries into smaller units.
Lower coverage figures are found on other continents. Only a few countries (United States, Canada, Japan, Australia, Israel) show coverage figures comparable to those in Western Europe. In typical developing regions, the coverage by employee health services ranges from 5% to 10% at best, with services being found mainly in manufacturing enterprises, while some sectors of industry, agriculture, the self-employed, small-scale enterprises and the informal sector are usually not covered at all. Even in countries where coverage rates are high, there are gaps, with small-scale enterprises, certain mobile workers, construction, agriculture and the self-employed being underserved.
Thus, there is a universal need to increase the coverage of workers by occupational health services throughout the world. In a number of countries, intervention programmes to increase the coverage have demonstrated that it is possible to substantially improve the availability of occupational health services in a relatively short time and at a reasonable cost. Such interventions have been found to improve both the workers’ access to the services and the cost effectiveness of the services provided.
Policy Impact of International Instruments
The so-called work environment reform which took place in most of the industrialized countries in the 1970s and 1980s saw the production of important international instruments and guidelines. They reflected the responses of occupational health policies to the new needs of working life, and the achievement of an international consensus on the development of occupational safety and health.
The International Programme for the Improvement of Working Conditions and Environment (PIACT) was launched by the ILO in 1976 (Improving Working Conditions and Environment: An International Programme (PIACT) 1984; 71st Session of the International Labour Conference 1985). The ILO Occupational Safety and Health Convention, 1981 (No. 155), with its accompanying Recommendation (No. 164), and the ILO Occupational Health Services Convention, 1985 (No. 161) and its accompanying Recommendation (No. 171), amplified the impact of the ILO in the development of occupational safety and health. By 31 May 1995, 40 ratifications of these Conventions had been registered, but their practical impact was much wider than the number of ratifications, since many countries had implemented the principles embodied in these instruments, although they had not been able to ratify them.
Simultaneously, the WHO Global Strategy Health for All by the Year 2000 (HFA) (1981), first launched in 1979, was followed in the 1980s by introduction and implementation of regional and national HFA strategies in which workers’ health constituted an essential part. In 1987, WHO launched a Programme of Action for Workers’ Health, and in 1994 the WHO Collaborating Centres in Occupational Health developed the Global Strategy for Occupational Health for All (1995), which was endorsed by the WHO Executive Board (EB97.R6) and unanimously adopted by the World Health Assembly in May 1996 (WHA 49.12).
The most important features of the international consensus on occupational safety and health are:
- a focus on occupational health and safety for all workers irrespective of the sector of the economy, the type of employment (salaried worker or self-employed), the size of the enterprise or company (industry, public sector, services, agriculture and so on)
- the responsibility of governments for the establishment of appropriate infrastructures for occupational health practice through legislation, collective agreements or any other mechanism acceptable to the government after consultation with employers’ and workers’ representative organizations
- the liability of governments for the development and implementation of occupational safety and health policy in tripartite collaboration with employers’ and workers’ organizations
- the primary responsibility of the employer for the provision of occupational health services at the enterprise level, who must involve competent occupational health professionals to implement the provisions stipulated by the national legislation or the collective agreements
- the prevention of work accidents and occupational diseases and control of workplace hazards as well as the development of a work environment and work conducive to workers’ health are the main purpose of occupational health services.
The United Nations Summit on Environment and Development in Rio de Janeiro in 1993 touched on several aspects of human environment which have relevance to occupational health (WHO 1993). Its Agenda 21 contains elements on providing services for underserved workers and ensuring chemical safety at the workplace. The Rio Declaration emphasized peoples’ right to lead “healthy and productive lives in harmony with nature”, which would require work and working environment to meet certain minimum health and safety standards.
Such instruments and international programmes directly or indirectly stimulated the inclusion of the provision of occupational health services in the national Health for All by the Year 2000 programmes and other national development programmes. Thus, the international instruments have served as guidelines for the development of national legislation and programmes.
A significant role in the global development of occupational health has been played by the Joint ILO/WHO Committee on Occupational Health, which, in its twelve meetings held since 1950, has made important contributions toward the definition of concepts and their transfer into national and local practices.
Legislative Structures for Occupational Health Practice
Most countries have laws governing the provision of occupational health services, but the structure of the legislation, its content and the workers covered by it vary widely (Rantanen 1990; WHO 1989c). The more traditional laws consider occupational health services as a group of specialized and separate activities such as occupational health care, occupational safety and hygiene services, workplace health promotion programmes and so on. In many countries, instead of stipulating what might be regarded as programmes, the legislation stipulates the responsibility of employers to provide health risk assessments, health examinations of workers or other individual activities related to workers’ health and safety.
More recent laws reflecting international guidelines such as those contained in the ILO Convention on Occupational Health Services (No. 161) consider the occupational health service as an integrated, comprehensive, multidisciplinary team containing all the elements needed for the improvement of health at work, improvement of the working environment, promotion of workers’ health, and the overall development of the structural and managerial aspects of the workplace needed for health and safety.
The legislation usually delegates the authority to establish, implement and inspect occupational health services to such ministries or agencies as Labour, Health or Social Security (WHO 1990).
There are two main types of legislation regulating occupational health services:
One views the occupational health service as an integrated multidisciplinary service infrastructure and stipulates the objectives, activities, obligations and rights of the various partners, the conditions of operation, as well as the qualifications of its personnel. Examples include the European Union Framework Directive No. 89/391/EEC on Occupational Safety and Health (CEC 1989; Neal and Wright 1992), the Dutch ARBO Act (Kroon and Overeynder 1991) and the Finnish Act on Occupational Health Services (Translation of the Occupational Health Care Act and the Council of the State Decree No. 1009 1979). There are only a few examples of the organization of systems of occupational health services in the industrialized world that are in accord with this type of legislation, but their number is expected to grow with progressive implementation of the European Union Framework Directive (89/391/EEC).
The other type of legislation is found in most industrialized countries and is more fragmented. Instead of a single act stipulating the occupational health service as an entity, it involves a number of laws that simply oblige employers to carry out certain activities. These may be stipulated quite specifically or merely in general, leaving issues of their organization and conditions of operation open (WHO 1989c). In many developing countries, this legislation is applicable only to main industrial sectors, while large numbers of other sectors as well as agriculture, small-scale enterprises and the informal sector remain uncovered.
During the 1980s, particularly in industrialized countries, social and demographic developments such as ageing of the working population, increase in disability pensions and sickness absenteeism, and difficulty in controlling social security budgets led to some interesting reforms of national occupational health systems. These focused on the prevention of both short-term and long-term disability, preservation of working capacity, particularly of older workers, and reducing early retirement.
For example, the amendment of the Dutch ARBO Act (Kroon and Overeynder 1991) together with three other social laws aimed at the prevention of short- and long-term disability stipulated important new requirements for occupational health and safety services at the plant level. They included:
- minimum requirements for procedures, guidelines and facilities
- minimum requirements for the numbers, composition and competence of occupational health service teams, including such specialists as physicians with competence in occupational health, senior safety experts, occupational hygienists and management consultants
- requirements specifying the organization of services and their activities
- requirement of quality assurance systems, including appropriate audits
- requirement that the specialists working in the service be certified by appropriate authorities and that the service itself be certified on the basis of an external audit.
This new system will be implemented stepwise and should be mature before the end of the 1990s.
Amendments of the Finnish Act on Occupational Health Services in 1991 and 1994 introduced the maintenance of working capacity, particularly of ageing workers, as a new element in the legislation-based preventive activities of occupational health services. Implemented through the close collaboration of all the actors in the workplace (management, workers, health and safety services), it involves improvement and adaptation of work, working environment and equipment to the worker, improving and maintaining the physical and mental working capacity of the worker, and making the work organization more conducive to maintaining the work capacity of the worker. Currently, efforts are being directed at the development and evaluation of practical methods to achieve these goals.
The adoption in 1987 of the Single European Act gave new impetus to the occupational health and safety measures taken by the European Communities. This was the first time health and safety at work had been directly included in the EEC Treaty of 1957 and was done through the new Article 118a. Of significant importance to the level of protection is that directives adopted by the Member States under Article 118a lay down minimum requirements concerning health and safety at work. According to this principle, the Member States must raise their level of protection if it is lower than the minimum requirements set by the directives. Beyond this, they are entitled and encouraged to maintain and introduce more stringent protective measures than required by the directives.
June 1989 saw the adoption of the first and probably the most important Directive providing for minimum requirements concerning health and safety at work under Article 118a: Framework Directive 89/391/EEC on the introduction of measures to encourage improvements in the safety and health of workers at work. It is the core strategy on health and safety on which all subsequent directives will be built. The Framework Directive is to be supplemented by individual directives covering specific areas and also sets the general framework for future directives related to it.
The Framework Directive 89/391/EEC contains many features of the ILO Conventions Nos. 155 and 161 which the 15 countries of the European Union will implement in their national laws and practices. Main provisions that are relevant to occupational health practice include:
- the development of a coherent overall prevention policy at the enterprise level covering the working environment, technology, organization of work, working conditions and social relationships
- the responsibility of the employer to ensure the safety and health of workers in every aspect related to the work, including prevention of occupational hazards, provision of information and training, as well as provision of the necessary work organization, control measures and means that occupational health activities should be carried out in collaboration between employers and workers
- that workers should receive health surveillance adequate for the health risks they incur at work
- that workers have the right to receive all the necessary information concerning the safety and health risks as well as preventive and protective measures in respect of both the enterprise in general and each type of workstation and work practice
- that the planning and introduction of new technologies should be subject to consultation with the workers and/or their representatives, as regards the choice of equipment, working conditions and the working environment for the safety and health of workers
- that the general principles of prevention should include the elimination of occupational hazards; evaluation of hazards which cannot be avoided; combating the risks at the source; adapting the work to the individual, especially as regards the design of workplaces, the choice of equipment and working and production methods; adapting to technical progress; replacing dangerous substances by non-dangerous or less dangerous ones; giving collective protective measures priority over individual protective measures; giving appropriate instructions to the workers.
During the past years, a large amount of European Union legislation has been introduced, including a series of individual directives based on the principles formulated in the Framework Directive, some supplementing those which had been subject to technical harmonization measures in preparation, and others covering specific risks and high-risk sectors. Examples of the first group are directives concerning the minimum safety and health requirements for the workplace, for the use of work equipment by workers at work, for the use of personal protective equipment, for the manual handling of loads, for work with display screen equipment, for the provision of safety and health signs at work, and the implementation of the minimum safety and health requirements at temporary or mobile construction sites. The second group includes such directives as the protection of workers from the risks related to exposure to vinyl chloride monomer, metallic lead and its ionic compounds, asbestos at work, carcinogens at work, biological agents at work, the protection of workers by the banning of certain specified agents and/or certain work activities, and some others (Neal and Wright 1992; EC 1994).
Proposals have been made recently for the adoption of other directives (namely, the directives on physical agents, chemical agents, transport activities and workplaces, and work equipment) in order to consolidate some existing directives and rationalize the overall approach to the safety and health of workers in these fields (EC 1994).
Many new elements in the national legislation and practices respond to today’s emerging problems of working life and contain provisions for further development of occupational health infrastructures. This especially concerns programming, at the national and enterprise level, more comprehensive activities in respect of psychosocial, organizational and work capacity aspects and particular emphasis on the principle of participation. They also provide for the application of quality management systems, auditing and certification of both the competence of the experts and services to meet the requirements of occupational safety and health legislation. Thus, such national laws, by absorbing the substantive content of the ILO instruments, no matter whether the instruments are ratified or not, lead to the stepwise implementation of the objectives and principles embodied in the ILO Conventions Nos. 155 and 161 and in the WHO HFA Strategy.
Objectives of Occupational Health Practice
The objectives of occupational health practice that were originally defined in 1950 by the Joint ILO/WHO Committee on Occupational Health stated that:
Occupational health should aim at the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations; the prevention amongst workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological capabilities; and, to summarize: the adaptation of work to man and of each man to his job.
In 1959, based on discussions of the special ILO tripartite committee (representing governments, employers and workers), the Forty-third Session of the International Labour Conference adopted Recommendation No. 112 (ILO 1959) which defined an occupational health service as a service established in or near a place of employment for the purposes of:
- protecting the workers against any health hazard which may arise out of their work or the conditions in which it is carried on
- contributing towards the workers’ physical and mental adjustment, in particular by the adaptation of the work to the workers and their assignment to jobs for which they are suited
- contributing to the establishment and maintenance of the highest possible degree of physical and mental well-being of the workers.
In 1985, the ILO adopted new international instruments—the Occupational Health Services Convention (No. 161) and its accompanying Recommendation (No. 171) (ILO 1985a, 1985b)— which defined occupational health services as services entrusted with essentially preventive functions and responsible for advising the employer, the workers and their representatives in the undertaking on: the requirements for establishing and maintaining a safe and healthy working environment which will facilitate optimal physical and mental health in relation to work; and the adaptation of work to the capabilities of workers in light of their state of physical and mental health.
In 1980, the WHO/Euro Working Group on Evaluation of Occupational Health and Industrial Hygiene Services (WHO 1982) defined the ultimate goal of such services as “promoting conditions at work that guarantee the highest degree of quality of working life by protecting workers’ health, enhancing their physical, mental and social well-being, and preventing ill-health and accidents”.
The extensive survey of occupational health services in the 32 countries in the European Region carried out in 1985 by the WHO Regional Office for Europe (Rantanen 1990) identified the following principles as objectives of occupational health practice:
- protecting workers’ health against hazards at work (the protection and prevention principle)
- adapting work and the work environment to the capabilities of workers (the adaptation principle)
- enhancing the physical, mental and social well-being of workers (the health promotion principle)
- minimizing the consequences of occupational hazards, accidents and injuries, and occupational and work-related diseases (the cure and rehabilitation principle)
- providing general health care services for workers and their families, both curative and preventive, at the workplace or from nearby facilities (the general primary health care principle).
Such principles can still be considered to be relevant with respect to the new developments in countries’ policies and legislation. On the other hand, the formulation of objectives of occupational health practice as they stand on recent national laws and the development of new needs for working life seem to emphasize the following trends (WHO 1995a, 1995b; Rantanen, Lehtinen and Mikheev 1994):
- The scope of occupational health is expanding to cover not only health and safety but also psychological and social well-being and the ability to conduct socially and economically productive life.
- The full range of objectives extends beyond the scope of traditional occupational health and safety issues.
- The new principles go beyond the mere prevention and control of effects adverse to the health and safety of workers to the positive promotion of health, the improvement of the working environment and work organization.
Thus, there certainly exists a tendency for expansion of the scope of the objectives of occupational health practice towards new types of issues entailing social and economic consequences for workers.
Functions and Activities of Occupational Health Services
To protect and promote the health of workers, an occupational health service has to meet the special needs of the enterprise it serves and the workers employed in it. With the enormous range and scope of industrial, manufacturing, commercial, agricultural and other economic activities, it is not possible to lay down a detailed programme of activity or pattern of organization and conditions of operation for an occupational health service which should be suitable for all enterprises and in all circumstances. According to the ILO Occupational Safety and Health Convention (No. 155) and the ILO Occupational Health Services Convention (No. 161), the prime responsibility for health and safety of workers rests with the employers. The functions of an occupational health service are to protect and promote the health of workers, improve working conditions and the working environment and maintain the health of the enterprise as a whole by providing occupational health services to workers and expert advice to the employer on how to achieve the highest possible standards of health and safety in the interests of the particular working community of which it is a part.
ILO Convention No. 161 and its accompanying Recommendation No. 171 envisage occupational health services as multidisciplinary, comprehensive and, although essentially preventive, also allow for carrying out curative activities. The WHO documents calling for services for small-scale enterprises, the self-employed and agricultural workers encourage the provision of services by primary health care units (Rantanen, Lehtinen and Mikheev 1994). The documents described above and national laws and programmes recommend a stepwise implementation so that the occupational health activities can be adjusted to the national and local needs and the prevailing circumstances.
Ideally, an occupational health service should establish and act in accordance with a programme of activities adapted to the needs of the enterprise where it operates. Its functions should be adequate and appropriate to the occupational hazards and health risks of the enterprise it serves, with particular attention given to the problems specific to the branch of economic activity concerned. The following represent the basic functions and most typical activities of an occupational health service.
Preliminary orientation to the enterprise
If occupational health services have not been previously provided or when new occupational health service staff members are recruited, a preliminary orientation to the occupational safety and health situation of the enterprise is needed. This involves the following steps:
- Analysis of the type of production will indicate the types of hazards typical for the economic activity, work or occupation which therefore may be expected to be encountered in the enterprise and can help identify those that may call for special attention.
- Review of problems that have been identified by occupational health professionals, management, workers or other specialists, and occupational health measures that have previously been undertaken at the workplace will indicate the perception of the problems by the enterprise. This should include examination of reports of occupational health and safety activities, industrial hygiene measurements, biological monitoring data and so on.
- Review of the characteristics of the workforce (i.e., numbers by age, sex, ethnic background, family relations, occupational classifications, work history and, if available, related health issues) will help to identify vulnerable groups and those with special needs.
- Available data on occupational diseases and accidents and sickness absenteeism grouped, if possible, by department, occupation and type of work, causative factors and the type of injury or disease should be examined.
- Data on working methods, chemical substances handled at work, recent exposure measurements and the numbers of workers exposed to special hazards are needed for the identification of the priority problems.
- The knowledge by employees of occupational health problems, the extent of their training in emergency measures and first-aid, and the prospects for an effective occupational safety and health committee should be explored.
- Finally, pending plans for changes in production systems, installation of new facilities, machinery and equipment, introduction of new materials and changes in the organization of work should be examined as a basis for changing the occupational health practice in the future.
Surveillance of the working environment
The quality of the working environment through compliance with safety and health standards has to be ensured by surveillance at the workplace. According to ILO Convention No. 161, surveillance of the working environment is one of the main tasks of the occupational health services.
On the basis of the information obtained through the preliminary orientation to the enterprise, a walk-through survey of the workplace is conducted, preferably by a multidisciplinary occupational health team supplemented by employers’ and workers’ representatives. This should include interviews with managers, foremen and workers. When needed, special safety, hygiene, ergonomic or psychological checks can be performed.
Special checklists and guidelines are available and are recommended for such surveys. The observations may indicate a need for specific measurements or checks which should be performed by specialists in occupational hygiene, ergonomics, toxicology, safety engineering or psychology who may be members of the occupational health team of the enterprise or may have to be procured externally. Such special measurements or checks may be beyond the resources of small-scale enterprises, which would have to rely on observations made during the survey supplemented by qualitative or, in the best case, by semi-quantitative data as well.
As a basic checklist for the identification of potential health hazards, the List of Occupational Diseases (amended 1980) appended to the ILO Employment Injury Benefits Convention, 1964 (No. 121), may be recommended. It lists the major known causes of occupational diseases, and although its main purpose is to provide guidance for compensation of occupational diseases, it can also serve for their prevention. Hazards not mentioned in the list can be added according to national or local conditions.
The scope of surveillance of the working environment as defined by the ILO Occupational Health Services Recommendation (No. 171) is as follows:
- identification and evaluation of the environmental factors which may affect the workers’ health
- assessment of conditions of occupational hygiene and factors in the organization of work which may give rise to risks for the health of workers
- assessment of collective and personal protective equipment
- assessment where appropriate, by valid and generally accepted monitoring methods, of exposure of workers to hazardous agents
- assessment of control systems designed to eliminate or reduce exposure.
As a result of the walk-through survey a hazard inventory should be prepared, identifying each hazard inherent in the enterprise. This inventory is necessary for estimating a potential for exposure and suggesting control measures. For purposes of this inventory and to facilitate designing, implementing and evaluating of controls, hazards should be cross-classified by the risks they present for workers’ health with acute or chronic outcomes and by type of hazard (i.e., chemical, physical, biological, psychological or ergonomic).
The next step is a quantitative assessment of exposure, which is necessary for more exact health hazard evaluation. It consists of measuring the intensity or concentration, the variation in time, the total duration of exposure, as well as the number of workers exposed. Measurement and evaluation of exposure are usually conducted by occupational hygienists, ergonomists and specialists in injury control. They are based on the principles of environmental monitoring and should include, where necessary, ambient monitoring to collect data on exposure in a given working environment, and personal exposure monitoring of an individual worker or a group of workers (e.g., exposed to specific hazards). Measurement of exposure is necessary whenever hazards are suspected or reasonably predictable, and should be based on the completed hazard inventory combined with an assessment of work practices. Knowledge of potential effects caused by each hazard should be used to establish priorities for intervention.
The evaluation of health hazards in the workplace should be accomplished by considering the complete picture of exposures in comparison with established occupational exposure standards. Such standards are expressed in terms of permissible levels and exposure limits and are set up through numerous scientific studies correlating exposure with produced health effects. Some of them have become state standards and are legally enforceable according to national law and practice. Examples are Maximum Allowable Concentrations (MAKs in Germany, MACs in the East European countries) and Permissible Exposure Limits (PELs, United States). There are PELs for about 600 chemical substances commonly found in the workplace. There are also limits on time-weighted average exposure, short-term exposure limits (STELs), ceilings, and for some hard conditions that might result in skin absorption.
Surveillance in the working environment includes monitoring both the hazardous exposures and the health outcomes. If exposure to hazards is excessive, it should be controlled regardless of outcome, and the health of exposed workers should be evaluated. Exposure is considered excessive if it approaches or exceeds established limits such as those mentioned above.
Surveillance of the work environment provides information on the occupational health needs of the enterprise and indicates the priorities for preventive and control actions. Most of the instruments guiding occupational health services emphasize the need to carry out the surveillance before initiating services, periodically during the course of the activities, and always when substantial changes in work or the working environment have taken place.
The results obtained provide the necessary data to estimate whether preventive actions taken against health hazards are effective, as well as whether workers are placed in jobs adequate to their capacities. These data are also used by the occupational health service to ensure that reliable protection against exposures is maintained and to formulate advice on how to implement controls in order to improve the working environment. In addition, the accumulated information is used for epidemiological surveys, for the revision of permissible exposure levels, as well as for the evaluation of the effectiveness of the engineering control measures and other methods of various preventive programmes.
Informing employer, enterprise managementand workers about occupational health hazards
As information about potential workplace health hazards is obtained, it should be communicated to those responsible for implementing preventive and control measures as well as to the workers exposed to these hazards. The information should be as precise and quantitative as possible, describing the preventive measures being taken and explaining what the workers should do to ensure their effectiveness.
The ILO Occupational Health Services Recommendation, 1985 (No. 171) provides that in accordance with national law and practice, data resulting from surveillance of the working environ-ment should be recorded in an appropriate manner and be available to the employer, the workers and their representatives, or to the safety and health committee, where one exists. These data should be used on a confidential basis solely to provide guidance and advice on measures to improve the working en-vironment and the safety and health of workers. The competent authority should also have access to these data. They may be communicated to others by the occupational health service only with the agreement of the employer and the workers. Workers concerned should be informed in an adequate and appropriate manner of the results of the surveillance and should have the right to request the monitoring of the working environment.
Assessment of health risks
To assess occupational health risks, information from surveillance of the work environment is combined with information from other sources, such as epidemiological research on particular occupations and exposures, reference values like occupational exposure limits and available statistics. Qualitative (e.g., whether the substance is carcinogenic) and, where possible, quantitative (e.g., what is the degree of exposure) data may demonstrate that workers face health hazards and indicate a need for preventive and control measures.
The steps in an occupational health risk assessment include:
- identification of occupational health hazards (performed as a result of surveillance of the working environment)
- analysis of how the hazard may affect the worker (ways of entry and type of exposure, threshold limit values, dose-response relationships, adverse health effects it may cause and so on)
- identification of workers or group of workers exposed to specific hazards
- identification of individuals and groups with special vulnerabilities
- evaluation of available hazard prevention and control measures
- making conclusions and documenting the findings of the assessment
- periodic review and, if necessary, reassessment.
Surveillance of workers’ health
Due to limitations of a technological and economic nature, it is often not possible to eliminate all health hazards in the workplace. It is in these circumstances that surveillance of workers’ health plays a major role. It comprises many forms of medical evaluation of health effects developed as a result of workers’ exposure to occupational health hazards.
The main purposes of health examinations are to assess the fitness of a worker to carry out certain jobs, to assess any health impairment which may be related to the exposure to harmful agents inherent in the work process and to identify cases of occupational diseases in accordance with national legislation.
Health examinations cannot protect workers against health hazards and they cannot substitute for appropriate control measures, which have the first priority in the hierarchy of actions. Health examinations help to identify conditions which may make a worker more susceptible to the effects of hazardous agents or detect early signs of health impairment caused by these agents. They should be conducted in parallel with surveillance of the working environment, which provides information on potential exposure in the workplace and is used by occupational health professionals to assess results obtained through health surveillance of the exposed workers.
Health surveillance of workers may be passive and active
In case of passive health surveillance, ill or affected workers are required to consult occupational health professionals. Passive surveillance usually detects only symptomatic disease and requires that occupational health professionals be able to differentiate the effects of occupational exposures from the similar effects of non-occupational exposures.
In case of active health surveillance, occupational health professionals select and examine workers who are at high risk of work-related disease or injury. It may be conducted under many forms, including periodic medical examinations for all workers, medical examinations for workers exposed to specific health hazards, screening and biological monitoring of selected groups of workers. Specific forms of health surveillance depend largely upon possible health effects resulting from a particular occu-pational exposure. Active surveillance is more appropriate for workers with a history of multiple exposures and those at higher risk for disease or injury.
Details about health surveillance are given in the ILO Convention No. 161 and Recommendation No. 171. These instruments specify that surveillance of workers’ health should include, in the cases and under the conditions specified by the competent authority, all assessments necessary to protect the health of workers, which may include:
- health assessment of workers before their assignment to specific tasks which may involve a danger to their health or that of others
- health assessment at periodic intervals during employment which involves exposure to a particular hazard to health
- health assessment on resumption of work after a prolonged absence for health reasons, for the purposes of determining possible occupational causes, recommending appropriate action to protect the workers and determining the workers’ suitability for the job and needs for assignment and rehabilitation
- health assessment on and after termination of assignment involving hazards which might cause or contribute to future health impairment.
Evaluation of the health status of workers is of utmost importance when occupational health practice is initiated, when new workers are recruited, when new working practices are adopted, when new technologies are introduced, when special exposures are identified, and when individual workers display health characteristics that need follow-up. A number of countries have special regulations or guidelines specifying when and how health examinations should be carried out. Health examinations should be monitored and continuously developed to identify the work-related health effects at their earliest stage of development.
Pre-assignment (pre-employment) health examinations
This type of health assessment is carried out before the job placement of workers or their assignment to specific tasks which may involve a danger to their health or that of others. The purpose of this health assessment is to determine whether a person is physically and psychologically fit to perform a particular job and to ensure that his or her placement in this job will not represent a danger to his or her health or to the health of other workers. In most instances, a review of the medical history, a general physical examination and routine laboratory tests (e.g., simple blood count and urinalysis) will suffice, but in some cases the presence of a health problem or the unusual requirements of a particular job will require extensive functional examinations or diagnostic testing.
There are a number of health problems that may make a certain job hazardous for the worker or incur a risk for the public or other workers. For these reasons, it may be necessary, for example, to exclude workers with uncontrolled hypertension or unstable diabetes from certain hazardous jobs (e.g., air and sea pilots, drivers of public service and heavy goods vehicles, crane drivers). Colour blindness may justify an exclusion from jobs requiring colour discrimination for safety purpose (e.g., reading traffic signals). In jobs demanding a high standard of general fitness like deep-water diving, fire fighting, police service and aircraft piloting, only workers able to meet the performance requirements would be acceptable. A possibility that chronic diseases may be aggravated by the exposures involved in a particular job should also be considered. It is essential, therefore, that the examiner have a detailed knowledge of the job and the work environment and be aware that standardized job descriptions may be too superficial or even misleading.
After finishing a prescribed health assessment, the occupational physician should communicate the results in writing to both the worker and the employer. These conclusions communicated to the employer should contain no information of a medical nature. They should contain a conclusion about the fitness of the examined person for the proposed or held assignment and specify the kinds of jobs and the conditions of work which are medically contra-indicated either temporarily or permanently.
The pre-employment medical examination is important to the worker’s subsequent occupational history since it provides the necessary clinical information and laboratory data on the worker’s health status at the moment of entering the employment. It also represents an indispensable baseline for the subsequent evaluation of any changes in health status that may occur later on.
Periodic health examinations
These are performed at periodic intervals during employment which involves exposure to potential hazards that could not be entirely eliminated by preventive and control measures. The purpose of periodic health examinations is to monitor the health of workers during the course of their employment. It aims at verifying workers’ fitness in relation to their jobs and at detecting as early as possible any sign of ill-health which may be due to work. They are often supplemented by other examinations in accordance with the nature of hazards observed.
Their objectives include:
- identifying as early as possible any adverse health effects caused by work practices or exposures to potential hazards
- detecting the possible onset of an occupational disease
- verifying whether the health of an especially vulnerable or chronically ill worker is being adversely affected by the work or the work environment
- monitoring personal exposure with the help of biological monitoring
- checking the effectiveness of preventive and control measures
- identifying possible health effects of changes in the working practices, technology or substances used in the enterprise.
These objectives will determine the frequency, content and methods of the periodic health examinations, which may be conducted as frequently as every one to three months or every few years, depending on the nature of the exposure, the biological response expected, the opportunities for preventive measures and the feasibility of the examination method. They may be comprehensive or limited to just a few tests or determinations. Special guidelines on the purpose, frequency, content and methodology of these examinations are available in a number of countries.
Return-to-work health examinations
This type of health assessment is required to authorize the resumption of work after a long absence for health reasons. This health examination determines the workers’ suitability for the job, recommends appropriate actions to protect them against future exposures, and identifies whether there is a need for a reassignment or a special rehabilitation.
Similarly, when a worker changes jobs, the occupational physician is required to certify that the worker is fit to carry out the new duties. The objective of the examination, the need and the use of the results determine its content and methods and the context in which it is performed.
General health examinations
In many enterprises, general health examinations may be performed by the occupational health service. They are usually voluntary and may be available to the entire workforce or only to certain groups determined by age, length of employment, status in the organization and so on. They may be comprehensive or limited to screenings for particular diseases or health risks. Their objectives determine their frequency, contents and methods used.
Health examinations after the ending of service
This type of health assessment is performed after the termination of assignment involving hazards which could cause or contribute to future health impairment. The purpose of this health assessment is to make a final evaluation of workers’ health, compare it with previous medical examinations and to assess how the prior job assignments may have affected their health.
General observations
The general observations summarized below apply to all types of health examinations.
Health examinations of workers should be conducted by professionally qualified personnel trained in occupational health. These health professionals should be familiar with the exposures at work, physical requirements and other conditions of work in the enterprise and experienced in using appropriate medical examination techniques and instruments, as well as in keeping correct record forms.
The health examination is not a substitute for action to prevent or control hazardous exposures in the working environment. If prevention has been successful, fewer examinations are needed.
All data collected in connection with health examinations are confidential and should be recorded by the occupational health service in a personal confidential health files. Personal data relating to health assessments may be communicated to others only with the informed consent of the worker concerned. When the worker wishes the data to be forwarded to a personal physician, he or she provides formal permission for this.
Conclusions about the suitability of a worker for a particular job or about the health effects of the job should be communicated to the employer in a form that does not violate the principle of the confidentiality of personal health data.
Use of health examinations and their results for any kind of discrimination against workers cannot be tolerated and must be strictly prohibited.
Initiatives for preventive and control measures
Occupational health services are responsible not only for the identification and evaluation of potential risks for the health of workers but also for providing advice on preventive and control measures which will help to avoid risks.
After analysing the results of surveillance of the working environment, including where necessary workers’ personal exposure monitoring, and the results of workers’ health surveillance, including where necessary the results of biological monitoring, occupational health services should be in a position to assess possible connections between the exposure to occupational hazards and resulting health impairments and to propose appropriate control measures to protect workers’ health. These measures are recommended together with other technical services in the enterprise after consulting the enterprise management, employers, workers or their representatives.
Control measures should be adequate to prevent unnecessary exposure during normal operating conditions as well as during accident and emergencies. Planned modifications in work processes should also be taken into account, and recommendations should be adaptable to future needs.
Measures of control of health hazards are used to eliminate occupational exposure, minimize or in any case reduce it to permissible limits. They include primarily engineering, engineering controls in the work environment, changes in technology, substances and materials and as secondary preventive measures, human behaviour controls, personal protective equipment, integrated control and others.
The formulation of recommendations for control measures is a complicated process that includes the analysis of information on existing health risks in the enterprise and the consideration of occupational safety and health requirements and needs. For analysis of feasibility and costs versus benefits one should consider the fact that the investments made for health and safety may pay back during long periods in the future, but not necessarily immediately.
The ILO instruments include a requirement that the employers, workers and their representatives should cooperate and participate in the implementation of such recommendations. They are usually discussed by the safety and health committee at large-scale enterprises, or in smaller enterprises by the representatives of the employers and workers. It is important to document the proposed recommendations so that there can be a follow-up of their implementation. Such documentation should emphasize the responsibility of management for preventive and control actions at the enterprise.
Advisory role
Occupational health services have an important task to perform by providing advice to the enterprise management, the employers, the workers, and health and safety committees in their collective as well as individual capacities. This needs to be recognized and used in the decision-making processes as it often happens that occupational health professionals are not directly involved in the decision-making.
The ILO Occupational Health Services Convention (No. 161) and Recommendation (No. 171) promote the advisory role of occupational health professionals in the enterprise. To promote the adaptation of work to the workers and improve working conditions and environment, occupational health services should act as advisers on occupational health, hygiene, ergonomics, collective and individual protective equipment to the employers, the workers and their representatives in the enterprise, and to the safety and health committee, and should collaborate with other services already operating as advisers in these fields. They should advise on the planning and organization of work, the design of workplaces, on the choice, maintenance and condition of machinery and other equipment, as well as on the substances and materials used in the enterprise. They should also participate in the development of programmes for the improvement of working practices, as well as in the testing and evaluation of health aspects of new equipment.
Occupational health services should provide workers with personal advice concerning their health in relation to work.
Another important task is to provide advice and information related to the integration of workers who have been victims of work accidents or diseases in order to help them in their rapid rehabilitation, protect their working capacity, reduce absenteeism and restore a good psychosocial climate in the enterprise.
Educational and training activities are closely linked to the advisory task that occupational health professionals perform vis-à-vis the employers and workers. They are of particular importance when the modification of existing installations or the introduction of new equipment are envisaged, or when there may be changes in the layout of workplaces, workstations and in the organization of work. Such activities have an advantage when started at the right time because they provide for better consideration of human factors and ergonomic principles in the improvement of working conditions and environment.
Technical advisory services at the workplace constitute an important preventive function of occupational health services. They should give priority to the awareness of occupational hazards and to the involvement of the employers and workers in hazard control and the improvement of the working environment.
First aid services and emergency preparedness
The organization of first aid and emergency treatment is a tradi-tional responsibility of occupational health services. ILO Convention No. 161 and Recommendation No. 171 stipulate that the occupational health service should provide first aid and emergency treatment in cases of accident or indisposition of workers at the workplace and should collaborate in the organization of first aid.
This covers preparedness for accidents and acute health conditions in individual workers, as well as readiness for response in collaboration with other emergency services in cases of serious accidents affecting the entire enterprise. Training in first aid is a primary duty of occupational health services, and the personnel of these services are among the first to respond.
The occupational health service should make appropriate preliminary arrangements for ambulance services and with community fire, police and rescue units and local hospitals in order to avoid delays and confusion that may threaten the survival of critically injured or affected workers. These arrangements, supplemented by drills when feasible, are particularly important in preparing for major emergencies such as fire, explosions, toxic emissions and other catastrophes that may involve many individuals in the enterprise as well as in the neighbourhood and may result in a number of casualties.
Occupational health care, general preventiveand curative health services
Occupational health services may be involved in the diagnosis, treatment and rehabilitation of occupational injuries and diseases. The knowledge of occupational diseases and injuries coupled with the knowledge of the job, the working environment and occupational exposures present in the workplace enable the occupational health professionals to play a key role in the management of work-related health problems.
According to the scope of activities and as required by national legislation or based on national practice, occupational health services fall into three main categories:
- occupational health services with essentially preventive functions, including mainly workplace visits, health examinations and the provision of first-aid
- occupational health services with preventive functions supplemented by selective curative and general health care services
- occupational health services with a wide range of activities including both preventive and comprehensive curative and rehabilitation activities.
The ILO Occupational Health Services Recommendation (No. 171) promotes the provision of curative and general health care services as functions of occupational health services where they are found to be appropriate. Based on national legislation and practice, the occupational health service may undertake or participate in one or more of the following curative activities with regard to occupational illnesses:
- treatment of workers who have not stopped work or who have resumed work after an absence
- treatment of workers with occupational diseases or health impairments aggravated by work
- treatment of victims of occupational accidents and injuries
- medical aspects of vocational re-education and rehabilitation.
The provision of general preventive and curative health care services includes the prevention and treatment of non-occupational illnesses and other relevant primary health care services. Usually, general preventive health care services include immunizations, maternity and child care, general hygiene and sanitary services, whereas general curative health care services include conventional general-practitioner-level practice. Here, ILO Recommendation No. 171 prescribes that the occupational health service may, taking into account the organization of preventive medicine at the national level, fulfil the following functions:
- carry out immunizations in respect of biological hazards in the working environment
- take part in campaigns aimed at the protection of workers’ health
- collaborate with the health authorities within the framework of public health programmes.
Occupational health services set up by large enterprises, as well as those operating in remote or medically underserved areas, may be called upon to provide general non-occupational health care not only for workers but for their families as well. The extension of such services depends on the infrastructure of the health services in the community and on the capacity of the enterprises. When industrial enterprises are established in poorly developed areas, it may even be expedient to provide such services together with occupational health care.
In some countries, occupational health services provide ambulatory treatment during working hours which is normally provided by a general practitioner. It usually concerns simple forms of treatment, or it may be more comprehensive medical care if the enterprise has an agreement with the social security or other insurance institutions providing reimbursement of the cost of workers’ treatment.
Rehabilitation
The participation of occupational health services is particularly crucial in guiding workers’ rehabilitation and their return to work. This is becoming more and more important owing to a large number of occupational accidents in developing countries and the ageing of the working populations in industrialized societies. Rehabilitation services are usually provided by external units which may be free-standing or hospital-based and staffed by rehabilitation specialists, occupational therapists, vocational counsellors and so on.
There are some important aspects concerning the participation of occupational health services in the rehabilitation of injured workers.
First, the occupational health service may play an important role in seeing that workers recovering from injury or disease are referred to them promptly. It is greatly preferable, when practicable, for a worker to return to his or her original place of employment, and it is an important function of the occupational health service to maintain contact during the period of incapacity with those responsible for treatment during the acute stages in order to identify the time when a return to work can be envisaged.
Second, the occupational health service can facilitate an early return to work by collaborating with the rehabilitation unit in planning. Its knowledge of the job and work environment will be helpful in exploring the possibilities of modifying the original job (e.g., changes in work assignment, limited hours, rest periods, special equipment and so on) or arranging an alternative temporary substitute.
Finally, by following the worker’s progress, the occupational health service can keep management informed of the probable duration of absence or limited capacity, or the extent of any residual disability, so that arrangements for alternative staffing may be made with minimal impact on production schedules. On the other hand, the occupational health service maintains a link with the workers and often with their families, facilitating and better preparing their return to work.
Adaptation of work to the workers
To facilitate the adaptation of work to the workers and improve the working conditions and environment, occupational health services should advise the employer, the workers and the safety and health committee in the enterprise on matters of occupational health, occupational hygiene and ergonomics. Recommendations may include modifications of the job, the equipment and the working environment that will allow the worker to perform effectively and safely. This may involve reducing the physical workload for an ageing worker, providing special equipment for workers with sensory or locomotor impairments or fitting equipment or work practices to the anthropometric dimensions of the worker. The adaptations may be required temporarily in the case of workers recovering from an injury or disease. A number of countries have legal provisions requiring workplace adaptations.
Protection of vulnerable groups
The occupational health service is responsible for recommendations that will protect vulnerable groups of workers, such as those with hypersensitivities or chronic diseases and those with certain disabilities. This may include selection of a job that minimizes adverse effects, provision of special equipment or protective devices, prescription of sick leave and so on. The recommendations must be feasible in the light of the circumstances in a particular workplace, and workers may be required to undertake special training in appropriate working practices and the use of personal protective equipment.
Information, education and training
Occupational health services should play an active role in providing relevant information and organizing education and training in relation to work.
The ILO Occupational Health Services Convention (No. 161) and Recommendation (No. 171) provide for the participation of occupational health services in designing and implementing programmes of information, education and training in the field of occupational safety and health for the personnel of the enterprise. They should participate in the progressive and continuing training of all workers in the enterprise who contribute to occupational safety and health.
Occupational health professionals can help increase workers’ awareness of occupational hazards to which they are exposed, discuss with them existing health risks and advise workers on the protection of their health, including protective measures and proper use of personal protective equipment. Every contact with workers offers an opportunity to provide useful information and to encourage healthful behaviour in the workplace.
Occupational health services should provide all information on occupational hazards present in the enterprise as well as on safety and health standards relevant to the local situation. This information should be written in language understandable by the workers. It should be provided on a periodic basis and especially when new substances or equipment are being introduced or changes are being made in the working environment.
Education and training can play a key role in the improvement of working conditions and environment. Efforts to improve safety, health and welfare at work are often substantially limited due to lack of awareness, technical expertise and know-how. Education and training in specific fields of occupational safety and health and working conditions can facilitate both the diagnosis of problems and the implementation of solutions, and can therefore help overcome these limitations.
ILO Conventions Nos. 155 and 161 and their accompanying Recommendations emphasize the key role of education and training in the enterprise. Training is essential to fulfil the obligations of both the employers and the workers. Employers are responsible for the organization of in-plant occupational safety and health training, and workers and their representatives in the enterprise should fully cooperate with them in this respect.
Training in occupational safety and health should be organized as an integral part of the overall efforts for improving working conditions and environment, and occupational health services should play a major role in this respect. It should aim at solving various problems affecting the physical and mental well-being of workers and should address adaptation to technology and equipment, improvement of working environment, ergonomics, working time arrangements, the organization of work, job content and workers’ welfare.
Health promotion activities
There is some tendency, particularly in North America, to incorporate wellness promotion activities in the form of occupational health programmes. These programmes are, however, essentially general health promotion programmes that may include such elements as health education, stress management and assessment of health risks. They usually aim at changing personal health practices such as alcohol and drug abuse, smoking, diet and physical exercise, with a view to improving overall health status and reducing absenteeism. Although such programmes are supposed to improve productivity and reduce health care costs, they have not been properly evaluated so far. These programmes, designed as health promotion programmes, though valuable as such are not usually considered as occupational health programmes, but as public health services delivered in the workplace, because they focus attention and resources on personal health habits rather than on protection of workers against occupational hazards.
It should be recognized that the implementation of health promotion programmes is an important factor contributing to the improvement of the health of workers in the enterprise. In some countries, “health promotion in the workplace” is regarded as a separate discipline on its own and is carried out by completely independent groups of health workers other than occupational health professionals. In this case, their activities should be coordinated with the activities of the occupational health service, whose staff can ensure their relevance, feasibility and sustainable effect. The participation of occupational health services in the realization of health promotion programmes should not limit the performance of their main functions as specialized health services created to protect workers against harmful exposures and unhealthy working conditions in the workplace.
A very recent development in some countries (e.g., the Netherlands, Finland) is the establishment of occupational health promotion activity within occupational health services. Such activities aim at promotion and maintenance of work ability of workers by targeting early prevention and promotion actions to workers and their health, to work environment, and to work organization. The results of such activities are found to be highly positive.
Data collection and record-keeping
It is important that all medical contacts, evaluations, assessments and surveys be properly documented and the records safely stored so that, if necessary for follow-up health examinations, legal or research purposes, they may be retrieved years and even decades later.
The ILO Occupational Health Services Recommendation (No. 171) provides that occupational health services should record data on workers’ health in personal confidential files. These files should also contain information on jobs held by the workers, on exposure to occupational hazards involved in their work, and on the results of any assessment of workers’ exposure to these hazards. Personal data relating to health assessments may be communicated to others only with the informed consent of the worker concerned.
The conditions under which and time during which records containing workers’ health data should be kept, communicated or transferred, and the measures necessary to keep them confidential, especially when these data are computerized, are usually prescribed by national laws or regulations or by the competent authority, and governed by recognized ethical guidelines.
Research
According to the ILO Occupational Health Services Recommendation (No. 171), occupational health services, in consultation with the employers’ and workers’ representatives, should contribute to research within the limits of their resources by participating in studies in the enterprise or in the relevant branch of economic activity (e.g., to collect data for epidemiological purposes or participate in national research programmes). Occupational physicians involved in the implementation of research projects will therefore be bound by the ethical considerations applied to such projects by the World Medical Association (WMA) and the Council for International Organizations of Medical Sciences (CIOMS). Research in the working environment may involve healthy “volunteers”, and the occupational health service should fully inform them about the purpose and the nature of the research. Each participant should give individual consent to the participation in the project. The collective consent provided by the workers’ trade union in the enterprise is not enough. Workers must feel free to withdraw from the investigation at any time and the occupational health service should be responsible that they will not be subjected to undue pressure to remain within the project against their will.
Liaison and Communications
A successful occupational health service is necessarily involved in communications of many kinds.
Internal collaboration
The occupational health service is an integral part of the productive apparatus of the enterprise. It must closely coordinate its activities with occupational hygiene, occupational safety, health education and health promotion, and other services directly related to workers’ health, when these operate separately. In addition, it must collaborate with all services in the operation in the enterprise: personnel administration, finance, employee relations, planning and design, production engineering, plant maintenance and so on. There should be no obstacles in reaching out to any department in the enterprise when issues of worker health and safety are involved. At the same time, the occupational health service should be responsive to the needs and sensitive to the constraints of all other departments. And, if it does not report to a most senior executive, it must have the privilege of direct access to top management in cases when important recommendations relating to workers’ health are denied appropriate consideration.
In order to function effectively, the occupational health service needs the support of the enterprise management, the employer, workers and their representatives. The ILO instruments (ILO 1981a, 1981b, 1985a, 1985b) require the employer and the workers to cooperate and participate in the implementation of the organizational and other measures relating to occupational health services on an equitable basis.
The employer should collaborate with the occupational health service in achieving its objectives particularly by:
- providing general information about occupational health and safety in the enterprise
- providing information on any known or suspected factors that might affect the workers’ health
- providing the occupational health service with adequate resources in terms of facilities, equipment and supplies, and qualified staff
- providing appropriate authority to enable the occupational health service to perform its functions
- allowing free access to all parts and facilities of the enterprise (including separate plants and field units) and providing information about plans for changes in production equipment and supplies, as well as work processes and the organization of work, so that preventive measures can be taken before workers are exposed to any potential hazards
- giving prompt consideration to any recommendations made by the occupational health service for the control of occupational hazards and the protection of workers’ health, and ensuring their implementation
- safeguarding the professional independence of occupational health professionals, encouraging and, where possible, subsidizing their continuing education and training.
Where a special plant-level programme for occupational health activities is required, the collaboration between the employer and the occupational health service is crucial in the preparation of such a programme and the activity report.
Occupational health services are established to protect and promote workers’ health by preventing work injuries and occupational diseases. Many functions of occupational health services cannot be carried out without cooperation with workers. According to the ILO instruments, workers and their organizations should cooperate with occupational health services and provide support to these services in the execution of their duties (ILO, 1981a, 1981b, 1985a, 1985b). The workers should cooperate with occupational health services in particular by:
- informing the occupational health service about any known or suspected factors in the work and the work environment that may have adverse effects on their health
- assisting occupational health staff in performing their duties in the workplace
- participating in health examinations, surveys and other activities conducted by the occupational health service
- obeying health and safety rules and regulations
- maintaining safety equipment and personal protective devices as well as first aid supplies and emergency equipment, and learning to use them properly
- participating in health education and safety training exercises in the workplace
- reporting on the effectiveness of occupational safety and health measures
- participating in the organization, planning, implementation and evaluation of activities of occupational health services.
The ILO instruments recommend the collaboration between the employers and workers on matters of occupational safety and health (ILO 1981a,1981b,1985a,1985b). This collaboration is carried out in the occupational safety and health committee of the enterprises, which comprises the representatives of workers and the employer and constitutes a forum for the discussion of matters relating to occupational health and safety. The establishment of such a committee may be prescribed by legislation or collective agreements in enterprises with 50 or more workers. In smaller enterprises, its functions are intended to be fulfilled by less formal discussions between the workers’ safety delegates and the employer.
The committee has a broad range of functions (ILO 1981b) which may include:
- participating in decisions regarding the establishment, organization, staffing and operation of the occupational health service
- contributing to the occupational health and safety programme of the enterprise
- providing support to the occupational health service in the performance of its duties
- participating in the evaluation of the activities of the occupational health service and contributing to its reports submitted to subsidizing bodies, enterprise management and external authorities
- facilitating the communication of information on occupational health and safety matters between different services in the enterprise
- providing a forum for discussions and decisions on collaborative actions in the enterprise regarding matters of occupational safety and health
- evaluating the overall status of occupational health and safety in the enterprise.
The principle of workers’ participation in decisions concerning their own health and safety, on changes in jobs and working environments, and on safety and health activities is emphasized in recent guidelines on occupational health practice. It also requires that workers should have access to information on the activities of the enterprise concerning occupational safety and health and on any potential health hazard that they may encounter at the workplace. Accordingly, the principle of “right to know” and transparency principles have been established or strengthened by legislation in many countries.
External collaboration
Occupational health services should establish close relations with external services and institutions. Foremost among these are relationships with the public health care system of the country as a whole and the institutions and facilities in the local communities. This starts at the level of primary health care units and extends to the level of hospital-based specialized services, some of which may also be providing occupational health services. Such relationships are important when it is necessary to refer workers to specialized health services for appropriate evaluation and treatment of occupational injuries and diseases, and also to provide opportunities for mitigating the possible adverse effects of non-occupational health problems on attendance and work performance. Collaboration with public health as well as environmental health services is important. Inviting general practitioners and other health professionals to visit the occupational health service and familiarize themselves with the demands made on their patients by occupations or the hazards to which they are exposed will not only help to establish friendly relations, but also provide an opportunity to sensitize them to the particulars of occupational health issues that ordinarily would be ignored in their treatment of workers for whom they provide general health care services.
Rehabilitation institutes are a frequent collaborative partner, particularly in the case of workers with handicaps or chronic disabilities who may require special efforts to enhance and maintain their work capacities. Such collaboration is especially important in recommending temporary job modifications that will accelerate and facilitate the return to work of individuals recovering from serious injuries or illnesses, with occupational or non-occupational aetiology.
Emergency response organizations and first aid providers such as ambulance services, hospital outpatient and emergency clinics, poison control centres, police and fire brigades, and civic rescue organizations can ensure the expeditious treatment of acute injuries and illnesses and assist in planning for and response to major emergencies.
Appropriate links with social security and health insurance institutions can facilitate the administration of benefits and functioning of the workers’ compensation system.
The competent safety and health authorities and labour inspectorates are key collaborative partners for the occupational health services. In addition to expediting formal inspections, appropriate relationships may provide support for internal occupational health and safety activities and offer opportunities to input to the formulation of regulations and methods of enforcement.
Participation in professional societies and in activities of educational/training institutes and universities is valuable for arranging continuing education for professional staff members. Ideally, the time and expenses should be subsidized by the enterprise. In addition, the collegial contacts with occupational health professionals serving other enterprises can provide strategic information and insights and may lead to partnerships for meaningful data collection and research.
The kinds of collaboration described above should be initiated from the very beginning of the operation of the occupational health service and be continued and expanded as appropriate. They may not only facilitate achievement of the objectives of the occupational health service, but may also contribute to the community and public relations efforts of the enterprise.
Infrastructures for Occupational Health Services
Infrastructures for the provision of occupational health services are insufficiently developed in most parts of the world, including developed and developing countries. The need for occupational health services is particularly acute in the developing and newly industrialized countries, which contain eight out of ten of the world’s workers. If organized appropriately and effectively, such services would contribute significantly not only to workers’ health, but also to the overall socio-economic development, productivity, environmental health, and the well-being of countries, communities and families (WHO 1995b; Jeyaratnam and Chia 1994). Effective occupational health services can not only reduce avoidable-sickness absenteeism and work disability, but also help to control the costs of health care and social security. Thus, the development of the occupational health services covering all workers is fully justified with regard to both workers’ health and the economy.
Infrastructures for the provision of occupational health services should permit effective implementation of activities needed to meet the objectives of occupational health (ILO 1985a, 1985b; Rantanen, Lehtinen and Mikheev 1994; WHO 1989b). To allow the necessary flexibility, Article 7 of ILO Convention No. 161 provides that occupational health services may be organized as a service for a single undertaking or as a service common to a number of undertakings. Or, in accordance with national conditions and practice, occupational health services may be organized by the undertakings or groups of undertakings concerned, public authorities or official services, social security institutions, any other bodies authorized by the competent authority, or any combination of the above.
Some countries have regulations relating the organization of occupational health services to the size of the enterprise. For example, larger enterprises have to establish their own in-plant occupational health service while medium-sized and small enterprises are required to join group services. As a rule, legislation allows flexibility in the choice of structural models of occupational health services in order to meet local conditions and practices.
Models of Occupational Health Services
To meet the occupational health needs of enterprises which vary widely with respect to type of industry, size, type of activity, structure and so on, a number of different models of occupational health services have been developed (Rantanen, Lehtinen and Mikheev 1994; WHO 1989). In developing and newly industrialized countries, for example, where health care for the general population may be deficient, the occupational health service may provide primary non-occupational health care to the employees and their families as well. This has also been successfully implemented in Finland, Sweden and Italy (Rantanen 1990; WHO 1990). On the other hand, the high level of worker coverage in Finland has been made possible by organizing municipal health centres (PHC units) providing occupational health services for workers in small-scale enterprises, the self-employed and even small worksites operated by large enterprises that are scattered throughout the country.
In-plant (in-company) model
Many large industrial and non-industrial enterprises in both the private and public sectors have an integrated, comprehensive occupational health service on their premises that not only provides a full range of occupational health services, but may also provide non-occupational health services to workers and their families, and may carry out research. These units usually have multidisciplinary staff that may include not only occupational physicians and nurses, but also occupational hygienists, ergonomists, toxicologists, occupational physiologists, laboratory and x-ray technicians, and possibly physiotherapists, social workers, health educators, counsellors and industrial psychologists. Occupational hygiene and safety services may be provided by the staff of the occupational health service or by separate units of the enterprise. Such multidisciplinary units are usually afforded only by large (often multinational) enterprises and their quality of services and impact on health and safety is most convincing.
Smaller enterprises may have an in-plant unit that is staffed by one or more occupational health nurses and a part-time occupational physician who visits the unit for several hours a day or several times a week. A variant is the unit staffed by one or more occupational health nurses with an “on-call” physician who visits the unit only when summoned and usually provides “standing orders” which authorize the nurse to perform procedures and dispense medications that are normally the prerogative of licensed physicians only. In some instances in the United States and England, these units are operated and supervised by an external contractor such as a local hospital or a private entrepreneurial organization.
Due to various reasons, the occupational health staff may sometimes become more and more separated from the central operating structure of the enterprise, and, as result, the range of services it provides tends to shrink to first aid and treatment of acute occupational injuries and illnesses and the performance of routine medical examinations. Part-time and particularly on-call physicians often do not acquire the necessary familiarity with details of the kinds of jobs being performed or the working environment, and may not have enough contact with managers and the safety committee or do not have enough authority to effectively recommend appropriate preventive measures.
As part of the reductions in workforce seen at times of recession, some large enterprises are shrinking their occupational health services and, in some instances, eliminating them entirely. The latter may occur when an enterprise with an established occupational health service is acquired by an enterprise that had not maintained one. In such cases, the enterprise may contract with external resources to operate the in-plant facility and employ consultants on an ad hoc basis to provide such specialized services as occupational hygiene, toxicology and safety engineering. Some enterprises choose to retain an expert in occupational and environmental health to serve as an in-house medical director or manager to coordinate the services of the external providers, monitor their performance, and provide advice to top management on matters relating to employee health and safety and environmental concerns.
Group or inter-enterprise model
Sharing of occupational health services by groups of small or medium-sized enterprises has been widely used in industrialized countries such as Sweden, Norway, Finland, Denmark, the Netherlands, France and Belgium. This enables enterprises that are individually too small to have their own services, to enjoy the advantages of a well-staffed, well-equipped comprehensive service. The Slough Plan, organized some decades ago in an industrial community in England, pioneered this type of arrangement. In the 1980s, interesting experiments with regional occupational health centres organized in Sweden were found to be feasible and particularly useful for mid-sized enterprises, and some countries, such as Denmark, have made efforts to increase the size of the shared units to allow them to provide a broader range of services instead of splitting them into smaller monodisciplinary units.
A frequently encountered disadvantage of the group model compared to the in-plant model of larger enterprises is the distance between the worksite and the occupational health service. This is important not only in cases requiring first aid for more serious injuries (it is sometime more prudent to send such cases directly to a local hospital, bypassing the occupational health unit) but because more time is usually lost when workers are forced to go off the premises when seeking health services during working hours. Another problem arises when the participating enterprises are unable to contribute sufficient funds to sustain the unit which is forced to close down when the government or private foundation grants that may have subsidized its start-up are no longer available.
Industry-oriented (branch-specific) model
A variant of the group model is the joint use of an occupational health service by a number of enterprises in the same industry, trade or economic activity. Construction, food, agriculture, banking and insurance are examples of sectors that have made such arrangements in Europe; such models are found in Sweden, the Netherlands and France. The advantage of this model is the opportunity for the occupational health service to concentrate on the particular industry and accumulate special competence in addressing its problems. Such a model for the construction industry in Sweden provides sophisticated, high-quality, multidisciplinary services for the entire country and has been able to conduct research and develop programmes dealing with problems specific to that industry.
Hospital outpatient clinics
Hospital outpatient clinics and emergency rooms have traditionally provided services to injured or sick workers who seek care. A notable disadvantage is the lack of familiarity with occupational diseases on the part of the usual staff and attending physicians. In some instances, as noted above, occupational health services have made arrangements with local hospitals to provide certain specialized services and fill the gap either by collaborating in the care or educating the hospital staff about the kinds of cases that may be referred to them.
More recently, hospitals have begun to operate special occupational health clinics or services that are compared favourably to the large in-plant or group services described above. They are staffed by physicians specialized in occupational health who may also conduct research involving the kinds of problems they see. In Sweden, for example, there are eight regional clinics of occupational medicine, several of which are affiliated with a university or medical college, each providing services to enterprises in several communities. Several have a special unit to serve small enterprises.
A significant difference between the group services and the hospital-based activity is that in the case of the former, the participating enterprises usually share ownership of the occupational health service and have the decision-making authority over how it operates, while the latter operates as a private or public polyclinic that has a provider-customer relationship with the client enterprises. This limits, for example, the extent to which participation and collaboration between employers and workers can influence the operation of the unit.
Private health centres
The private health centre model is a unit usually organized by a group of physicians (it may be organized by a private entrepreneurial organization that employs the physicians) to provide several types of outpatient and sometimes also hospital-based health services. The larger centres often have a multidisciplinary staff and may offer occupational hygiene and physiotherapy services, while smaller units usually supply only medical services. As in the hospital clinic model, the provider-client relationship with participating enterprises may hinder implementation of the principle of employer and worker involvement in formulating policies and procedures.
In some countries, private health centres have been criticized for being too much oriented to curative clinical services provided by the physicians. Such criticism is justified in the case of smaller centres where the services are provided by general practitioners instead of health professionals experienced in occupational health practice.
Primary health care units
Primary health care units are usually organized by municipal or other local authorities or by the national health service, and usually provide both preventive services and primary health care. This is the model strongly recommended by the WHO as a means of providing services to small-scale enterprises and, particularly, to agricultural enterprises, the informal sector and the self-employed. Since general physicians and nurses usually lack specialization and experience in occupational health, the success of this model critically depends on how much training in occupational health and occupational medicine can be arranged for the health professionals.
An advantage of this model is its good coverage of the country and its location in the communities where the people it serves work and live. This is a particular advantage in serving agricul-tural workers and the self-employed.
A weakness is its concentration on general curative health services and treatment of emergencies with only limited ability to carry out surveillance of the working environment and to institute preventive measures needed in the workplace. Experience in Finland, where large primary health care units employ teams of trained specialists to provide occupational health services is, however, highly positive. Interesting new models for providing occupational health services by primary health care units have been tried in the Shanghai area of China.
Social security model
In Israel, Mexico, Spain and some African countries, for example, occupational health services are provided by special units organized and operated by the social security system. In Israel, this model is essentially similar in structure and operation to the group model, while elsewhere it is usually oriented more to curative health care. The specific feature of this model is that it is operated by the organization responsible for workers’ compensation for occupational injuries and diseases. While curative and rehabilitative services are provided, the emphasis on controlling social security costs has led to priority being given to preventive services.
Selecting a Model for Occupational Health Services
The primary decision of whether or not to have an occupational health service may be determined by law, by a labour-management contract, or by management’s concerns about employees’ health and safety. While many enterprises are motivated toward a positive decision by awareness of the value of an occupational health service in maintaining their productive apparatus, others are impelled by such economic considerations as controlling the costs of workers’ compensation benefits, avoidable sickness absenteeism and disability, early retirement for health reasons, regulatory penalties, litigation and so on.
The model for providing occupational health services may be dictated by laws or regulations which may be general or applicable only to certain industries. This is generally the case with the social security model, in which the client enterprises have no other option.
In most instances, the model selected is determined by such factors as the size of the workforce and its demographic characteristics, the kinds of work they do and the workplace hazards they encounter, the location of the worksite(s), the kind and quality of health services available in the community and, perhaps most important, the affluence of the enterprise and its ability to provide the requisite financial support. Sometimes, an enterprise will launch a minimal unit and enlarge and expand its activities as it proves its worth and earns the acceptance of the workers. Only a few comparative studies have been conducted so far on the operation of various models of occupational health services in different situations.
Occupational hygiene services
International instruments and guidelines strongly recommend the inclusion of occupational hygiene services in the multidisciplinary occupational health service. In some countries, however, occupational hygiene is traditionally carried out as a separate and independent activity. Under such circumstances, collaboration with other services involved in occupational safety and health activities is necessary.
Safety services
Safety services are traditionally carried out as a separate activity either by safety officers or safety engineers who are employees of the enterprise (ILO 1981a; Bird and Germain 1990) or by some form of consulting arrangement. In the in-plant safety service, the safety officer is often also the chief responsible for safety in the enterprise and represents the employer in such matters. Again, the modern trend is to integrate safety along with occupational hygiene and occupational health and other services involved in occupational health activities in order to form a multidisciplinary entity.
Where safety activities are carried out in parallel with those of occupational health and occupational hygiene, the collaboration is necessary particularly as regards the identification of accident hazards, risk assessment, planning and implementation of preventive and control measures, education and training of managers, supervisors and workers, and collecting, maintaining and registering records of accidents, and the operation of any control measures that are instituted.
Staffing of the Occupational Health Service
Traditionally, the occupational health service is staffed by an occupational health physician only, or a physician and a nurse who, perhaps with the addition of an industrial hygienist, may be designated as the “core” staff. The most recent provisions, however, require that whenever possible the occupational health staff should be multidisciplinary in composition.
The staff may be enlarged to a full multidisciplinary team depending on the model of the service, the nature of the industry and the types of work involved, the availability of the various specialists or of programmes for training them, and the extent of the available financial resources. When not actually on the staff, the supplementary staff positions may be filled in by external support services (WHO 1989a, 1989b). They may include safety engineers, mental health specialists (e.g., psychologists, counsellors), work physiologists, ergonomists, physiotherapists, toxicologists, epidemiologists and health educators. Most of these are rarely included in the full-time staff of the occupational health service and are involved on a part-time or an “as needed” basis (Rantanen 1990).
Since quantitative needs for occupational health staff vary widely depending on the enterprise in question, the organization model and the services provided by the occupational health service, as well as on the availability of support and parallel services, it is not possible to be categorical about the numerical size of the staff (Rantanen 1990; Rantanen, Lehtinen and Mikheev 1994). For example, 3,000 workers in one large enterprise require a smaller staff than would be needed to provide a similar range of services for 300 workplaces with 10 employees each. It has been noted, however, that at present in Europe, the usual proportion is one physician and two nurses to serve from 2,000 to 3,000 workers. The variation is wide, ranging from 1 per 500 to 1 per 5,000. In some countries, decisions on the staffing of the occupational health service is made by the employer on the basis of the kinds and volume of services provided, whereas in a number of countries the number and composition of occupational health staff are stipulated by legislation. For example, recent legislation in the Netherlands requires that the occupational health team must consist at least of a physician, a hygienist, a safety engineer and an expert in labour/organization relations (Ministerial Order on the Certification of SHW Services and Expertise Requirements for SHW Services 1993).
Many countries have formulated official or semi-official competence criteria for occupational physicians and nurses, but those for the other disciplines have not been established. The new European Union principles call for confirmation of the competence of all occupational health specialists, and some countries have established certification systems for them (CEC 1989; Ministerial Order on the Certification of SHW Services and Expertise Requirements for SHW Services 1993).
Training curricula for occupational health specialists are not well developed, apart from those for occupational physicians, nurses and, in some countries, occupational hygienists (Rantanen 1990). The establishment of curricula at all levels for all of the specialist categories, including programmes for basic, postgraduate and continuing education, has been encouraged. It is also deemed desirable to include training elements of occupational health at the level of basic education, not only in medical schools but also in other institutions such as technical universities, faculties of science and so on. In addition to the background in science and practical skills needed for occupational health practice, the training should include development of appropriate attitudes towards protection of workers’ health. Training in collaboration with specialists in other disciplines would enable a multidisciplinary approach. Training in collaboration with competent authorities and employers is also deemed necessary.
The professional identity of occupational health specialists needs to be supported on an equitable basis among the various disciplines. Strengthening their professional independence is crucial for efficient performance of their duties and may increase interest of other health professionals in developing lifelong careers in occupational health. It is important that the training curricula be reorganized while countries are developing new competence and certification criteria for occupational health specialists.
Infrastructures for Support Services
The majority of enterprises cannot afford the comprehensive multidisciplinary occupational health service needed for their occupational health and safety programmes. In addition to basic services provided for the enterprise, the occupational health service itself may need technical expertise in such areas as (Kroon and Overeynder 1991; CEC 1989; Rantanen, Lehtinen and Mikheev 1994):
- occupational hygiene (measurement and analysis)
- ergonomics
- information and advice about new problems and approaches to their solution
- organizational development
- psychology and stress management
- newer developments in control measures and equipment
- research support.
Countries have used different approaches to the organization of such services. For example, Finland has an Institute of Occupational Health with six regional institutes to supply expert support for front-line occupational health services. Most of the industrialized countries have such a national institute or a comparable structure with research, training, information and consultation services as its main functions; they are rare in the developing countries. Where such an institute does not exist, these services may be provided by university research groups, social security institutions, national health service systems, governmental occupational health and safety authorities and private consultants.
Experiences from industrialized countries have demonstrated the advisability of creating in each industrializing and newly developing country a special centre for occupational health research and development that can:
- provide support for policy development, evaluation and monitoring
- provide continuous scientific support for setting standards and occupational exposure limits
- develop and implement criteria for evaluating competence in the various occupational health disciplines
- provide and promote the creation of educational and training programmes to increase the number and competence of occupational health specialists
- provide information and advice on occupational health matters not only to those in the field but also to managers, labour unions, government agencies and the general public
- conduct or commission needed research in occupational health and safety.
When an individual institute is not able to supply all of the needed services, networking among several service units such as universities, research institutions and other such organizations may be needed.
Financing of Occupational Health Services
According to the ILO instruments, the primary responsibility for financing occupational health and safety services rests with the employer, with no charge being made to the workers. In some countries, however, there are modifications of these principles. For example, costs for the provision of occupational health services may be substantially subsidized by the social security institution. A case in point is Finland, where the primary financial responsibility is on the employer but 50% of the costs will be reimbursed by the social insurance institution provided there is evidence of compliance with the occupational health and safety regulations and the occupational safety and health committee of the enterprise confirms that the occupational health services have been properly provided.
In most countries, such national systems of reimbursement are available. In the community health centre model for the delivery of occupational health services, the start-up costs for facilities, equipment and personnel are met by the community, but operating costs are met by collecting fees from employers and from the self-employed.
The reimbursement or subsidy systems are intended to encourage the availability of services to enterprises with economic constraints, and particularly to small-scale enterprises which rarely can command adequate resources. The effectiveness of such a system is shown by the experience in Sweden in the 1980s, in which the allocation of substantial amounts of government financing to subsidize occupational health service for enterprises in general and particularly for small-scale enterprises increased the proportion of covered workers from 60% to over 80%.
Quality Systems and Evaluation of OccupationalHealth Services
The occupational health service should continually evaluate for itself its objectives, activities and results achieved as regards the protection of workers’ health and the improvement of the working environment. Many enterprises have arrangements for periodic independent audits by specialists in the organization or by external consultants. In some countries, there are governmental or private mechanisms for periodic recertification based on formal audit protocols. In some enterprises, periodic employee surveys provide useful indications of workers’ regard for the occupational health service and their satisfaction with the services it provides. To be truly valuable, there must be a feedback of the results of such surveys to participating employees, and evidence that appropriate actions are being taken to address any problems they disclose.
Many of the industrialized countries (e.g., the Netherlands and Finland) have initiated the use of the ISO 9000 series standards in developing quality systems for health services in general as well as for occupational health services. This is particularly appropriate because many client enterprises are applying such standards to their production processes. Some enterprises which have included their occupational health services in the application of Total Quality Management (also known as Continuous Quality Improvement) throughout their organizations have reported a positive experience in terms of improved quality and smoother operation of services.
In practice, the application of a programme of continuous quality improvement means that each department or unit of the enterprise analyses its functions and performance, and institutes any changes needed to bring their quality to an optimal level. The occupational health service should not only be a willing participant in this effort but should make itself available to ensure that considerations of workers’ health and safety are not overlooked in this process.
Evaluation of the quality of occupational health services not only serves the interests of the employers, workers and the competent authorities, but also the interests of the providers of the services as well. Several schemes for such evaluation have been developed in a number of countries. For practical purposes, the self-evaluation by the occupational health service staff itself may be the most practical, particularly when there is a health and safety committee to assess the results of such evaluation.
There is a growing interest in examining the economic aspects of occupational health and safety services and validating their cost-effectiveness, but few such studies have yet been reported.
Stepwise Development of Occupational Health Services
The ILO Occupational Health Services Convention, 1985 (No. 161) and its accompanying Recommendation (No. 171) encourage countries to develop progressively occupational health services for all workers, in all branches of economic activity and in all undertakings, including those in the public sector and the members of production cooperatives. Some countries have already developed well-organized services based on provisions stipulated by their legislation.
Starting with established services, there are three strategies for further development: extending the full spectrum of activities to cover more enterprises and more workers; expanding the content of occupational health services offering only core services; and stepwise expansion of both the content and the coverage.
There have been discussions of the minimum activities that should be provided by an occupational health service. In some countries, they are limited to health examinations conducted by specially authorized physicians. In 1989, the WHO/European Consultation on Occupational Health Services (WHO 1989b) proposed that the minimum should comprise the following core activities:
- assessment of occupational health needs
- preventive and control actions directed to the work environment
- preventive activities directed to the worker
- curative activities limited to first aid, diagnosis of occupational diseases, rehabilitation on return to work
- follow-up and evaluation of statistics of occupational injuries and diseases.
In practice, there exist a large number of workplaces around the world that have not yet been able to provide any services to their workers. Consequently, the first step for a national programme may be limited just to establishing occupational health services providing these core activities for those most in need.
Future Perspectives for Occupational Health Services Development
The future development of occupational health services depends on a number of factors in the world of work and on national economies and policies as well. The most important trends in industrialized countries include ageing of the workforce, increase of irregular employment patterns and working schedules, distant work (telework), mobile workplaces and the steady increase in small-scale enterprises and the self-employed. New technologies are introduced, new substances and materials are used, and new forms of work organization appear. There is pressure for simultaneously increasing productivity and quality, resulting in the need to maintain strong motivation for work in the face of the increasing tempo of change, and the need to learn new work practices and methods grows apace.
While measures to combat traditional occupational hazards have been successful, particularly in industrialized countries, these hazards are not likely to totally disappear in the near future and they will still represent danger even though for smaller populations of workers. Psychological and psychosocial problems are becoming dominant occupational hazards. The globalization of the world economy, the regionalization and the growth of multinational economies and enterprises are creating an internationally mobile workforce and resulting in the exportation of occupational hazards to areas in which protective regulations and constraints are weak or non-existent.
In response to these trends, the Second Meeting of the WHO Collaborating Centres in Occupational Health (the Network of 52 National Institutes of Occupational Health) held in October 1994 developed the Global Strategy on Occupational Health for All with particular relevance to future development of occupational health practice. With regard to further development of occupational health services, the following emerging issues will have to be met in the future:
- universal development of occupational health for all in order to equalize the conditions of work and health in all parts of the world
- developing better predictive methods for assessing in advance health risks of exposures and providing health and safety criteria for industrial planners, designers and engineers
- improving the integration of occupational health services with other services of the enterprise
- developing improved systems for providing occupational health services to small enterprises, agricultural workers and the self-employed
- accelerating and improving the assessment of the potential hazards introduced by new technologies, materials and substances
- strengthening the strategies and methodologies applicable in dealing with the psychosocial aspects of work, with special attention to controlling hazards and preventing their adverse effects
- improving the capability for preventing and controlling musculoskeletal disorders, cumulative strain injuries and occupational stress
- increasing attention to the needs of ageing workers and improving the methods for their adaptation to work and the maintenance of work capacities
- developing and enhancing programmes for maintaining the work capacities of the unemployed and facilitating their re-employment
- increasing the numbers and competence of professionals in many disciplines involved in occupational health and safety and recognizing the need for involvement of such new disciplines as the science of work organization, quality management and health economics.
To summarize, occupational health services will face formidable challenges during the next decade and beyond in addition to the economic, political and social pressures inherent in changing national and industrial configurations. They include the occupational health problems linked with new information technologies and automation, new chemical substances and new forms of physical energy, the hazards of new biotechnologies, relocation and international transfer of hazardous technologies, ageing of the workforce, the special problems of such vulnerable groups as the chronically ill and the handicapped, as well as the unemployment and relocations forced by job-seeking, and the appearance of new and hitherto unrecognized diseases that may affect the workforce.
Conclusions
Occupational health infrastructures are insufficiently developed to meet the needs of workers in all parts of the world. The need for effective occupational health services is growing rather than decreasing. The ILO instruments on occupational health services and the parallel WHO strategies provide a valid basis for the significant development of occupational health services, and should be used by each country as it sets policy objectives to ensure the health and safety of workers in the country.
The developing and newly industrialized countries contain approximately 8 out of 10 of the world’s workers, and no more than 5 to 10% of this working population has access to adequate occupational health services. In many industrialized countries this proportion rises to no higher than 20 to 50%. If such services could be organized and provided for all workers it would not only favourably influence workers’ health, but also have a positive influence on the well-being and economic status of the countries, their communities and their whole populations. This would also help to control the costs of avoidable sickness absenteeism and disability and restrain the escalation of health care and social security costs.
International guidelines for effective occupational health policies and programmes are available but insufficiently applied on national and local levels. Collaboration between countries and the international organizations and among the countries themselves should be fostered to provide the necessary financial, technical and professional support needed to increase access to occupational health services.
The range and quantity of occupational health services required by an enterprise vary widely depending on conditions in the country and the community, the nature of the industry and the processes and materials used, as well as on the characteristics of the workforce. Preventive services should be given highest priority and an acceptable level of quality should be ensured.
A variety of models are available for organizing occupational health services and creating the associated infrastructures. The choice should be determined by the characteristics of the enterprise, the available resources in terms of finances, facilities, qualified personnel, the kinds of problems anticipated, and what is available in the community. Further research on the suitability of various models in different situations is needed.
Providing high-quality occupational health services often requires the involvement of a broad range of occupational health and safety, general health and psychosocial disciplines. The ideal service is staffed by a multidisciplinary team in which a number of these specialities are represented. However, even such services must turn to external sources when infrequently used specialists are required. To meet the growing need for such specialists, adequate numbers must be recruited, trained and provided with the specialization in occupational health needed for optimal effectiveness in the world of work. International collaboration should be encouraged in the collection of available information and design of its application under varied circumstances, and its dissemination through already established networks widely promoted.
Research activities in occupational health have traditionally been focused on such areas as toxicology, epidemiology and the diagnosis and treatment of health problems. More research is needed on the effectiveness of various models and mechanisms for delivering occupational health services, on their cost-effectiveness and their adaptability to different circumstances.
There are a number of goals and objectives of occupational health services, some of which may need to be reconsidered because of the constantly changing world of work. These should be reviewed and revised by the most authoritative international bodies in the light of new and emerging problems of occupational health and safety and the new modes of promoting and protecting the health of workers.
The ILO Occupational Health and Safety Conventions and Recommendations, approaches and standards embodied in them, the WHO strategies and resolutions, as well as international programmes of both organizations constitute a solid basis for national work and wide international cooperation in the further development and improvement of occupational health services and practice. Such instruments and their due implementation are particularly needed throughout the world in times of rapidly changing working life; in implementation of new technologies; and under the growing risk of setting the short-term economic and material objectives ahead of the health and safety values.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."