Children categories

14. First Aid and Emergency Medical Services (2)

14. First Aid and Emergency Medical Services
Chapter Editor: Antonio J. Dajer
Table of Contents
Tables
First Aid
Antonio J. Dajer
Traumatic Head Injuries
Fengsheng He
Tables
Click a link below to view table in article context.

15. Health Protection and Promotion (25)

15. Health Protection and Promotion
Chapter Editors: Jacqueline Messite and Leon J. Warshaw
Table of Contents
Figures and Tables
Health Protection and Promotion in the Workplace: An Overview
Leon J. Warshaw and Jacqueline Messite
Worksite Health Promotion
Jonathan E. Fielding
Health Promotion in the Workplace: England
Leon Kreitzman
Health Promotion in Small Organizations: The US experience
Sonia Muchnick-Baku and Leon J. Warshaw
Role of the Employee Health Service in Preventive Programmes
John W.F. Cowell
Health Improvement Programmes at Maclaren Industries, Inc.: A Case Study
Ian M.F. Arnold and Louis Damphousse
Role of the Employee Health Service in Prevention Programmes: A Case Study
Wayne N. Burton
Worksite Health Promotion in Japan
Toshiteru Okubo
Health Risk Appraisal
Leon J. Warshaw
Physical Training and Fitness Programmes: An Organizational Asset
James Corry
Worksite Nutrition Programmes
Penny M. Kris-Etherton and John W. Farquhar
Smoking Control in the Workplace
Jon Rudnick
Smoking Control Programmes at Merrill Lynch and Company, Inc.: A Case Study
Kristan D. Goldfein
Cancer Prevention and Control
Peter Greenwald and Leon J. Warshaw
Women’s Health
Patricia A. Last
Mammography Programme at Marks and Spencer: A Case Study
Jillian Haslehurst
Worksite Strategies to Improve Maternal and Infant Health: Experiences of US Employers
Maureen P. Corry and Ellen Cutler
HIV/AIDS Education
B.J. Stiles
Health Protection and Promotion: Infectious Diseases
William J. Schneider
Protecting the Health of the Traveller
Craig Karpilow
Stress Management Programmes
Leon J. Warshaw
Alcohol and Drug Abuse
Sheila B. Blume
Employee Assistance Programmes
Sheila H. Akabas
Health in the Third Age: Pre-retirement Programmes
H. Beric Wright
Outplacement
Saul G. Gruner and Leon J. Warshaw
Tables
Click a link below to view table in the article context.
1. Health-related activities by workforce size
2. Breast & cervical cancer screening rates
3. Themes of “World No-Tobacco Days”
4. Screening for neoplastic diseases
5. Health insurance benefits
6. Services provided by the employer
7. Substances capable of producing dependence
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

16. Occupational Health Services (16)

16. Occupational Health Services
Chapter Editors: Igor A. Fedotov, Marianne Saux and Jorma Rantanen
Table of Contents
Figures and Tables
Standards, Principles and Approaches in Occupational Health Services
Jorma Rantanen and Igor A. Fedotov
Occupational Health Services and Practice
Georges H. Coppée
Medical Inspection of Workplaces and Workers in France
Marianne Saux
Occupational Health Services in Small-Scale Enterprises
Jorma Rantanen and Leon J. Warshaw
Accident Insurance and Occupational Health Services in Germany
Wilfried Coenen and Edith Perlebach
Occupational Health Services in the United States: Introduction
Sharon L. Morris and Peter Orris
Governmental Occupational Health Agencies in the United States
Sharon L. Morris and Linda Rosenstock
Corporate Occupational Health Services in the United States: Services Provided Internally
William B. Bunn and Robert J. McCunney
Contract Occupational Health Services in the United States
Penny Higgins
Labour Union-Based Activities in the United States
Lamont Byrd
Academic-Based Occupational Health Services in the United States
Dean B. Baker
Occupational Health Services in Japan
Ken Takahashi
Labour Protection in the Russian Federation: Law and Practice
Nikolai F. Izmerov and Igor A. Fedotov
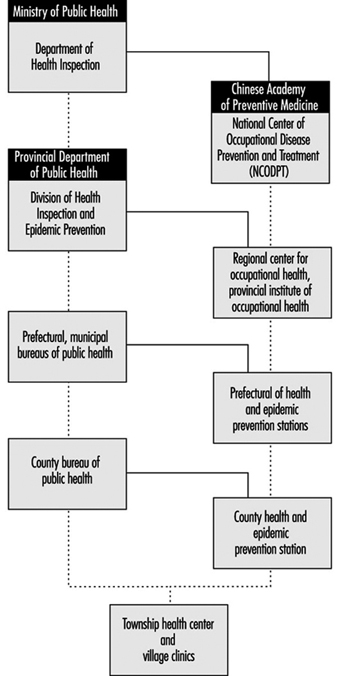
The Practice of Occupational Health Service in the People’s Republic of China
Zhi Su
Occupational Safety and Health in the Czech Republic
Vladimír Bencko and Daniela Pelclová
Practising Occupational Health in India
T. K. Joshi
Tables
Click a link below to view table in article context.
1. Principles for occupational health practice
2. Doctors with specialist knowledge in occ. medicine
3. Care by external occupational medical services
4. US unionized workforce
5. Minimum requirements, in-plant health
6. Periodic examinations of dust exposures
7. Physical examinations of occupational hazards
8. Results of environmental monitoring
9. Silicosis & exposure, Yiao Gang Xian Tungsten Mine
10. Silicosis in Ansham Steel company
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Occupational Health Services and Practice
Infrastructures, Practice and Approaches in Occupational Health
While much progress has been made since the 1980s towards a comprehensive approach in occupational health where the protection and promotion of workers’ health are pursued together with the maintenance and promotion of their working capacity, with a special emphasis on the establishment and maintenance of a safe and healthy working environment for all, there is much room for discussion as to the manner in which occupational health is actually implemented. The expression occupational health practice is currently used to cover the whole spectrum of activities undertaken by employers, workers and their organizations, designers and architects, manufacturers and suppliers, legislators and parliamentarians, labour and health inspectors, work analysts and work organization specialists, standardization organizations, universities and research institutions to protect health and to promote occupational safety and health.
The expression occupational health practice includes the contribution of occupational health professionals, but it is not limited to their practice of occupational health.
Confusion often occurs because the term occupational health services may be used to denote:
- the provision of occupational health services (i.e., the contribution of occupational health professionals to occupational safety and health)
- the institutionalized organizational arrangements to provide such services (i.e., the occupational health services which are part of the infrastructure to protect and promote workers’ health).
In order to overcome this difficulty and several other common causes of misunderstanding, the following wording was used for the second point on the agenda of the Twelfth Session of the Joint ILO/WHO Committee on Occupational Health: “Infrastructures for occupational health practice: options and models for national policies, primary health care approaches, strategies and programmes, and functions of occupational health services” (1995b) with the following understanding of the terms:
- Occupational health practice encompasses the activities of all those who contribute to the protection and promotion of workers’ health and to the improvement of working conditions and environment; these terms should not be understood as merely the practice of occupational health professionals.
- Occupational health approaches embodies a number of principles and approaches to guide action, such as the general principle of primary health care advocated by the WHO and the improvement of the working conditions and environment advocated by the ILO.
- Infrastructures for occupational health practice means the organizational arrangements to implement a national policy and to conduct action at the enterprise level; infrastructures may take the form of “institutionalized” occupational health services and include many other bodies such as national institutes for occupational safety and health.
The use of the key words infrastructures, practice and approaches permits the various actors and partners in prevention to play their individual roles in their respective fields of competence and to act jointly, as well.
Occupational health services contribute to the occupational health practice, which is intrinsically multidisciplinary and intersectoral and involves other specialists both in the enterprise and outside in addition to occupational health and safety professionals, as well as the appropriate governmental authorities, employers, workers and their representatives. Functionally, occupational health services must be considered both a part of country-level health infrastructures as well as of the infrastructures that exist for the implementation of relevant legislation on occupational safety and health. It is a national decision to determine whether such services should be under the supervision of the ministry of labour, the ministry of health, the social security institutions, a tripartite national committee or other bodies.
There are a large number of models for occupational health services. One of them enjoys the support of a large consensus at the international level: the model proposed by the ILO Occupational Health Services Convention (No. 161) and Recommendation (No. 171) adopted by the International Labour Conference in 1985. Countries should consider this model as an objective towards which progress should be made, taking into account, of course, local differences and the availability of specialized personnel and financial resources. A national policy should be adopted to develop progressively occupational health services for all workers, taking into account the specific risks of the undertakings. Such policy should be formulated, implemented and periodically reviewed in the light of national conditions and practice in consultation with the most representative organizations of employers and workers. Plans should be established indicating the steps which will be taken when occupational health services cannot be immediately established for all undertakings.
Multidisciplinary Cooperation and Intersectoral Collaboration: An Overall Perspective
The ILO and the WHO have a common definition of occupational health (see box), which was adopted by the Joint ILO/WHO Committee on Occupational Health at its first session (1950) and revised at its twelfth session (1995).
Governments, in collaboration with employers’ and workers’ organizations and professional organizations concerned, should design adequate and appropriate policies, programmes and plans of action for the development of occupational health with multidisciplinary content and comprehensive coverage. In each country, the scope and content of programmes should be adapted to national needs, should take into account local conditions and should be incorporated into national development plans. The Joint ILO/WHO Committee emphasized that the principles embodied in the ILO Conventions No. 155 and No. 161 and their accompanying Recommendations, as well as WHO resolutions, guidelines and approaches related to occupational health, provide a universally accepted guide for design of such policies and programmes (Joint ILO/WHO Committee on Occupational Health 1992).
Definition of occupational health adopted by the Joint
ILO/WHO Committee on Occupational Health (1950)
Occupational health should aim at the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations; the prevention amongst workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological capabilities and; to summarize: the adaptation of work to man and of each man to his job.
The main focus in occupational health is on three different objectives: (i) the maintenance and promotion of workers’ health and working capacity; (ii) the improvement of working environment and work to become conducive to safety and health and (iii) development of work organizations and working cultures in a direction which supports health and safety at work and in doing so also promotes a positive social climate and smooth operation and may enhance productivity of the undertakings. The concept of working culture is intended in this context to mean a reflection of the essential value systems adopted by the undertaking concerned. Such a culture is reflected in practice in the managerial systems, personnel policy, principles for participation, training policies and quality management of the undertaking.
There are similar features between the ILO strategy for the improvement of the working conditions and environment and the WHO general principle of primary health care. Both rest on similar technical, ethical and social considerations and they both:
- aim at all concerned, workers or the public
- define policies, strategies and means of action
- insist on the responsibility of each employer for the health and safety of the workers in his or her employment
- emphasize primary prevention and the control of risk at the source
- give special importance to information, health education and training
- indicate the need to develop an occupational health practice that is easily accessible to all and available at the workplace
- recognize the central place of participation, community participation in health programmes, inter-sectoral participation and workers’ participation in the improvement of the working conditions and the working environment
- highlight the interactions between health, environment and development, as well as between occupational safety and health and productive employment.
The main focus of ILO activity has been on the provision of international guidelines and a legal framework for the development of occupational health policies and infrastructures on a tripartite basis (including governments, employers and workers) and the practical support for improvement actions at the workplace, while the WHO has concentrated on the provision of scientific backgrounds, methodologies, technical support and on the training of health and related manpower for occupational health (Joint ILO/WHO Committee on Occupational Health 1992).
Multidisciplinary cooperation
For the WHO, occupational health includes safety at work. Hygiene is conceptualized as directed towards disease prevention while safety is thought of as the discipline that prevents bodily injuries due to accidents. For the ILO, occupational safety and health is considered as a discipline aiming at the prevention of work injuries (both occupational diseases and accidents) and at the improvement of working conditions and the environment. The terms occupational safety, occupational health, occupational medicine, occupational hygiene and occupational health nursing are used to acknowledge the contribution of different professions (e.g., engineers, physicians, nurses, hygienists) and in recognition of the fact that the organization of occupational safety and health at the enterprise level very often comprises separate occupational safety services and occupational health services, as well as safety and health committees.
To some extent, occupational safety and primary prevention are more directly linked to the technology which is used, to the process of production and to daily management than is occupational health, which focuses more on the relationships between work and health, in particular on the surveillance of the working environment and of workers’ health (secondary prevention), as well as on human factors and ergonomic aspects. Further, at the enterprise level, engineers are a necessary presence and are inte-gral to the management line (production engineers, maintenance, technicians and so on), while occupational health and hygiene requires the intervention of specialists in the health field who need not be present for the enterprise to function, but can be consultants or belong to an external occupational health service.
Whatever organizational arrangements and terminology are used, the most important thing is that occupational safety and health professionals work as a team. They need not necessarily be in the same unit or service, although this may be desirable where appropriate. The emphasis should not be on the structure of services but on the execution of their functions at the enterprise level in a sound manner (from a scientific, technical and ethical point of view). The emphasis should be on cooperation and coordination in the elaboration and implementation of a programme of action, as well as on the development of unifying concepts, such as “working cultures” (safety culture, labour protection culture, corporate culture) that are conducive to safety and health at work and “continuing quality improvement” of the working conditions and environment.
In 1992, the Joint ILO/WHO Committee emphasized that the scope of occupational health is very broad (as shown in table 1), encompassing disciplines such as occupational medicine, occupational nursing, occupational hygiene, occupational safety, ergonomics, engineering, toxicology, environmental hygiene, occupational psychology and personnel management. Collaboration and participation of employers and workers in occupational health programmes is an essential prerequisite for successful occupational health practice.
Table 1. Six principles and three levels for a sound occupational health practice
|
Principles |
|||||
|
Levels |
Prevention |
Protection |
Adaptation |
Promotion |
Mitigation |
|
Individuals (diversity) |
Accident prevention Industrial hygiene 1920s |
Industrial medicine Personal protective equipment 1930s |
Scientific organization of work Job analysis 1950s |
Employee assistance programmes 1950s |
Treatment compensation 1910s |
|
Groups (exposed groups, special needs) |
Safe and healthy working environment Built-in safety 1970s |
Occupational medicine Machine guarding 1940s |
Ergonomics including design 1950s |
Workers’ health promotion programmes 1980s |
Emergency planning and preparedness 1970s |
|
Society and all workers |
Control technologies Environmental health management 1970s |
Environmental health Epidemiology Preventive health care 1960s |
Appropriate technologies Consumers’ protection 1970s |
Health education and promotion programmes 1970s |
Curative health care 1920s |
Note: The times (1910, 1920, etc.) are arbitrary. Dates are merely given to provide an idea of the time scale for the progressive development of a comprehensive approach in occupational health. Dates will vary from country to country and may indicate the beginning or the full development of a discipline or the appearance of new terms or approaches for a practice which has been carried out for many years. This table does not intend to delineate exact disciplines involved in the process but to present in a concise manner their relationships within the framework of a mutlidisciplinary approach and intersectoral cooperation, towards a safe and healthy working environment and health for all, with a participatory approach and the objective of new forms of development which should be equitable if they are to be sustainable.
The definition of a common goal is one of the solutions to avoid the trap of an excessive compartmentalization of disciplines. Such compartmentalization of disciplines may sometimes be an asset since it allows for a specialized in-depth analysis of the problems. It may often be a negative factor, because it prevents the development of a multidisciplinary approach. There is a need to develop unifying concepts which open fields of cooperation. The new definition of occupational health adopted by the Joint Committee in 1995 serves this purpose.
Sometimes there can be heated arguments as to whether occupational health is a discipline in itself, or is part of labour protection, of environmental health or of public health. When the issue is more than academic and involves such decisions as which organization or ministry is competent for specific subject areas, the outcome can have significant consequences with regard to the allocation of funds and distribution of resources available in the form of expertise and equipment.
One of the solutions to such a problem is to advocate convergent approaches based on the same values with a common objective. The WHO approach of primary health care and the ILO approach of improving the working conditions and environment can serve this purpose. With common values of equity, solidarity, health and social justice in mind, these approaches can be translated into strategies (the WHO’s strategy of occupational health for all) and programmes (the ILO International Programme for the Improvement of Working Conditions and Environment) as well as into plans of action and activities implemented or carried out at the enterprise, national and international levels by all partners in prevention, protection and promotion of workers’ health, independently or jointly.
There are other possibilities. The International Social Security Association (ISSA) proposes the “concept of prevention” as a golden path to social security to address “safety worldwide” at work and at home, on the road and during leisure time. The International Commission on Occupational Health (ICOH) is developing an approach of ethics in occupational health and catalyses a rapprochement and cross-fertilization between occupational health and environment health. A similar trend can be seen in many countries where, for example, professional associations now get together occupational health and environmental health specialists.
Intersectoral collaboration
In 1984, the ILO’s annual International Labour Conference adopted a resolution concerning the improvement of working conditions and environment incorporating the concept that the improvement of the working conditions and environment is an element essential to the promotion of social justice. It stressed that improved working conditions and environment are a positive contribution to national development and represent a measure of success of any economic and social policy. It spelled out three fundamental principles:
- Work should take place in a safe and healthy environment.
- Conditions of work should be consistent with workers’ well-being and human dignity.
- Work should offer real possibilities for personal achievement, self-fulfilment and service to society.
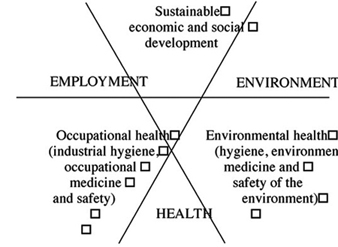
During the 1980s a shift occurred from the concept of development towards the concept of “sustainable development”, which includes “the right to a healthy and productive life in harmony with nature” as indicated in the first principle of the Rio Declaration (United Nations Conference on Environment and Development—UNCED 1992). The objective of a safe and healthy environment has thus become an integral part of the concept of sustainable development, which also implies balancing environment protection with generation of opportunity for employment, improved livelihoods and health for all. Both environmental health and occupational health contribute to make development sustainable, equitable and sound not only from an economic but also from a human, social and ethical point of view. This paradigm shift is illustrated in figure 1.
Figure 1. A multidisciplinary approach towards a sustainable and equitable development
The purpose of this figure is to illustrate the interaction between occupational health and environmental health and their mutually supportive contribution to a sustainable development. It identifies an area which represents the integration of the economic and social objectives which can be met while at the same time taking account of the environment, employment and health.
The WHO Commission on Health and Environment has further recognized that “the kind of development needed to safeguard health and welfare will depend on many conditions, including respect for the environment, while development without regard for the environment would inevitably result in impairment of human health” (WHO 1992). In the same vein, occupational health should be recognized as an “added value”, that is, a positive contribution to national development and a condition of its sustainability.
Of particular significance to the work of the ILO and the WHO are the Declaration and Programme of Action adopted by the World Summit for Social Development held in Copenhagen in 1995. The Declaration commits the nations of the world to pursuing the goal of full, productive and freely chosen employment as a basic priority of their economic and social policies. The Summit clearly indicated that the goal must not be to create just any sort of jobs, but quality jobs that safeguard the basic rights and interests of workers. It made clear that the creation of good quality jobs must include measures to achieve a healthy and safe working environment, to eliminate environmental health hazards and provide for occupational health and safety. This is an indication that the future of occupational health may well be active partnership in reconciling employment, health and environment towards an equitable and sustainable development.
The primary health care approach emphasizes social equity, affordability and accessibility, participation and community involvement, as noted by the Joint ILO/WHO Committee on Occupational Health in 1995. These basic moral and ethical values are common to the ILO and the WHO. The primary health care approach is innovative because it applies social values to preventive and curative health care. This complementarity has not always been clearly understood; sometimes confusion is due to the interpretation of common words, which has led to a degree of misunderstanding in discussing actual roles and activities to be undertaken by the ILO and the WHO, which are complementary and mutually supportive.
Primary health care can be considered to be based on principles of social equity, self-reliance and community development. It may also be considered to be a strategy for reorienting health systems, in order to promote individual and community involvement and collaboration between all sectors concerned with health. A general principle should be that primary health care should incorporate an occupational health component and specialized occupational health services should apply the general principle of primary health care, regardless of the structural model in place.
There are many partners in prevention, sharing the philosophy of both the ILO and the WHO, who should provide the necessary inputs to implement a good occupational practice. The Joint ILO/WHO Committee has indicated that the ILO and the WHO should promote an inclusive approach to occupational health in their member countries. If such an approach is used, occupational health can be seen as a multidisciplinary and integrated subject. Taken in this light, activities of different organizations and ministries will not be competitive or contradictory but will be complementary and mutually supportive, working towards an equitable and sustainable development. The emphasis should be on common goals, unified concepts and basic values.
As pointed out by the Joint ILO/WHO Committee in 1995, there is a need to develop occupational health indicators for the promotion and monitoring of the progression towards health and sustainable development. Forms of development which jeopardize health cannot claim the quality of being equitable or sustainable. Indicators towards “sustainability” necessarily include health indicators, since UNCED emphasized that the commitment of “protecting and promoting human health” is a fundamental principle for sustainable development (Agenda 21, Chapter 6). The WHO has taken a leading role in developing both the concept and use of environmental health indicators, some of which concern health and the working environment.
The WHO and the ILO are expected to develop occupational health indicators which could help countries in the evaluation, both retrospective and prospective, of their occupational health practice, and assist them in monitoring the progress made towards the objectives set by national policies on occupational safety, occupational health and the working environment. The development of such indicators focusing on the interactions between work and health could also assist occupational health services in evaluating and guiding their programmes and their activities to improve the working conditions and environment (i.e., in monitoring the efficiency and the manner in which they carry out their functions).
Standards and Guidance
The ILO Conventions and Recommendations on occupational safety and health define the rights of the workers and allocate duties and responsibilities to appropriate authorities, to the employers, and to the workers in the field of occupational safety and health. The ILO Conventions and Recommendations adopted by the International Labour Conference, taken as a whole, constitute the International Labour Code which defines minimum standards in the labour field.
The ILO policy on occupational health and safety is essentially contained in two international Conventions and their accompanying Recommendations. The ILO Occupational Safety and Health Convention (No. 155) and its Recommendation (No. 164), 1981, provide for the adoption of a national occupational safety and health policy at the national level and describe the actions needed at the national and at the enterprise levels to promote occupational safety and health and to improve the working environment. The ILO Occupational Health Services Convention (No. 161) and its Recommendation (No. 171), 1985, provide for the establishment of occupational health services which will contribute to the implementation of the occupational safety and health policy and will perform their functions at the enterprise level.
These instruments provide for a comprehensive approach to occupational health that includes primary, secondary and tertiary prevention and is consistent with general principles of primary health care. They indicate the manner in which occupational health care should ideally be delivered to the working populations, and propose a model that channels towards the workplace organized activities which require expert staff in order to catalyse an interaction between various disciplines to promote cooperation between all partners in prevention. These instruments also provide an organizational framework wherein occupational health professionals can deliver efficiently quality services to ensure workers’ health protection and promotion and contribute to the health of enterprises.
Functions
Convention No. 161 defines occupational health services as services dedicated to essentially preventive functions and responsible for advising employers, workers and their representatives at the enterprise on the requirements for establishing and maintaining a safe and healthy working environment that will optimize physical and mental health in relation to work and on the adaptation of work to the capabilities of workers, taking into consideration their state of physical and mental health.
The Convention specifies that occupational health services should include those of the following functions that are adequate and appropriate to the occupational risks at the worksite:
- identification and assessment of the risks from health hazards in the workplace
- surveillance of the factors in the working environment and working practices which may affect workers’ health, including sanitary installations, canteens and housing where these facilities are provided by the employer
- advice on planning and organization of work, including the design of workplaces, on the choice, maintenance and condition of machinery and other equipment and on substances used in work
- participation in the development of programmes for the improvement of working practices, as well as testing and evaluation of health aspects of new equipment
- advice on occupational health, safety and hygiene and on ergonomics and individual and collective protective equipment
- surveillance of workers’ health in relation to work
- promoting the adaptation of work to the worker
- contributing to measures of vocational rehabilitation
- collaborating in providing information, training and education in the fields of occupational health and hygiene and ergonomics
- organizing first aid and emergency treatment
- participating in analysis of occupational accidents and occupational diseases.
The ILO Convention and Recommendation are very flexible with regard to the forms of organization of occupational health services. The establishment of occupational health services may be done by laws or regulations, by collective agreements, or in any other manner approved by the appropriate authority, after consultation with the representative organizations of concerned employers and workers. Occupational health services may be organized as a service for a single enterprise or as a service common to a number of enterprises. As far as possible, the occupational health services should be located near the place of employment or should be organized to ensure their proper functioning at the place of employment. They may be organized by the concerned enterprises, by the public authorities or official services, by social security institutions, by any other bodies authorized by the authorities or, indeed, by combination of any of these. This offers a large degree of flexibility and, even in the same country, several or all of these methods may be used, according to local conditions and practice.
The flexibility of the Convention demonstrates that the spirit of the ILO instruments on occupational health services is to place more emphasis on its objectives rather than on the administrative rules for achieving them. It is important to ensure occupational health to all workers, or at least to make progress towards this objective. Such progress is usually achievable by degrees but it is necessary to make some progress towards achieving these aims and to mobilize resources in the most efficient manner for this purpose.
Various methods of financing occupational health exist. In many countries the obligation of establishing and maintaining occupational health services rests with employers. In other countries they are part of national health schemes or public health services. Staffing, financing and training of personnel are not detailed in the Convention but are individual national approaches.
Many examples exist of occupational health services set up by social security institutions or financed by special workers’ insurance schemes. Sometimes their financing is governed by an arrangement agreed upon by the ministry of labour and the ministry of health or by the social security institutions. In some countries trade unions run occupational health services. There are also special arrangements wherein funds are collected from employers by a central institution or tripartite body and then disbursed to provide occupational health care or distributed to finance the functioning of occupational health services.
The sources of financing occupational health services may also vary according to their activities. For example, when they have curative activities, social security may contribute to their financing. If occupational health services take part in public health programmes and in health promotion or in research activities, other funding sources may be found or become available. Financing will depend not only on the structural model chosen to organize the occupational health services, but also on the value that society concedes to health protection and promotion and its willingness to invest in occupational health and in the prevention of occupational hazards.
Conditions of Operation
A special emphasis is placed on the conditions of operation of occupational health services. It is not only necessary for the occupational health services to execute a number of tasks but it is equally important that these tasks should be performed in an appropriate manner, taking into consideration technical and ethical aspects.
There are some basic requirements as regards the operation of occupational health services which are spelled out in the ILO Convention, and especially in the Recommendation on Occupational Health Services. These may be summarized as follows:
- The personnel in occupational health services should be qualified and benefit from a full professional independence.
- Confidentiality should be ensured.
- Workers should be informed of the activities of the services and of the results of their health assessments.
- Employers, workers and their representatives should participate in the operation of the services and in the design of their programmes.
Ethical dimensions of occupational health are increasingly taken into account, and emphasis is placed on the need for both quality and on-going evaluation of occupational health services. It is not only necessary to determine what should be done but also for which purpose and under which conditions. The ILO Recommendation on Occupational Health Services (No. 171) introduced a first set of principles in this respect. Further guidance is given by the International Code of Ethics for Occupational Health Professionals adopted by the International Commission on Occupational Health (ICOH 1992).
In 1995, the Joint ILO/WHO Committee on Occupational Health emphasized that “quality assurance of services must be an integral part of the occupational health services development. It is unethical to give poor quality of service”. The ICOH Code of Ethics prescribes that “occupational health professionals should institute a programme of professional audit of their own activities in order to ensure that appropriate standards have been set, that they are being met and that deficiencies, if any, are detected and corrected”.
Common Goals and Values
The role of institutionalized occupational health services should be seen within the broader framework of health and social policies and infrastructures. The functions of occupational health services contribute to the implementation of the national policies on occupational safety, occupational health and the working environment advocated by the ILO Occupational Safety and Health Convention (No. 155) and Recommendation (No. 164), 1981. Occupational health services contribute also to the attainment of the objectives embodied in the “Health For All” strategy advocated by the WHO as a policy for equity, solidarity and health.
There are signs of an increasing trend to mobilize expertise and resources within the framework of networking arrangements and joint ventures. At the international level, such is already the case for chemical safety, where there is an interorganization me-chanism for chemical safety: the Inter-Organization Programme for the Sound Management of Chemicals (IOMC). There are many other fields where new flexible forms of international cooperation among countries and international organizations are emerging or could be developed, such as radiation protection and biological safety.
Networking arrangements open new fields of cooperation which may be adapted in a flexible manner to the theme which is to be addressed, such as occupational stress, coordinating research or updating this Encyclopaedia. The emphasis is placed on interactions and not any more on vertical compartmentalization of disciplines. The concept of leadership gives way to active partnership. International networking for occupational safety and health is developing rapidly and could be further developed on the basis of existing structures which could be interconnected. The roles of the ILO and the WHO may well be to initiate international networks designed to fulfil the needs and demands of their constituents and to meet the common goal of protecting the people at work.
The social and ethical values agreed upon by the international community are incorporated into the ILO Conventions and Recommendations, as well as in the WHO policy on “Health For All”. Since the 1980s the concept of sustainable development has progressively emerged and, after the Rio Conference and the Social Summit in Copenhagen, now takes into account the interrelationships between employment, health and the environment. The common goal of a safe and healthy working environment for all will reinforce the determination of all those involved in occupational safety and health to better serve the health of workers and to contribute to a sustainable and equitable development for all. One of the main challenges in occupational health may well be to resolve the conflict between values such as the right to health and the right to work at the level both of the individual and all workers, with the aim of protecting health and allowing employment.
Medical Inspection of Workplaces and Workers in France
History
In the 1930s, the application in France of certain clauses of the labour code concerning occupational hygiene demonstrated the value of providing workplace inspectors with access to consulting physicians.
The laws of 17 July 1937 and 10 May 1946 (articles L 611-7 and R 611-4) empowered the Department of Workplace Inspection to order temporary medical interventions. Over time, these interventions, originally conceived of as intermittent, evolved into ongoing activities complementary to and conducted simultaneously with workplace inspection.
The promulgation of the law of 11 October 1946 concerning occupational medicine was soon followed by the establishment of a permanent technical framework for the medical inspection of workplaces and workers. The decree of 16 January 1947 established the context, pay scales, status and functions of medical inspectors of workplaces and workers.
Since 1947, however, technical development in this area has been irregular and sporadic, and the number of medical inspectors has sometimes failed to keep pace with the number of inspection tasks; the latter has also been true of workplace inspections. Thus, while medical departments created in accordance with the law of 11 October 1946 increased in prevalence and importance, the number of medical inspectors was gradually reduced from 44, the number originally called for in 1947, to 21. These contradictory trends partially explain some of the criticism the occupational medicine system has had to face.
However, since 1970, and particularly since 1975, there has been a significant effort to create a Department of Workplace Medical Inspection capable of responding to the needs of the approximately 6,000 physicians responsible for over 12 million workers. In 1980, inspection services were allocated 39 paid positions, of which 36 were actually filled. In 1995, 43 positions were available. Priority Action Plan Number 12 of the VIIth Plan provides for 45 medical inspectors; this will bring staffing levels up to the levels originally envisaged in 1947.
At the same time that French officials were recognizing the necessity of establishing a specialized inspection department responsible for the application of legislative and regulatory directives concerning occupational hygiene and medicine, identical conclusions were being drawn in other countries. In response to this growing consensus, the ILO, in collaboration with the WHO, convened an international colloquium on the medical inspection of workplaces, in Geneva in 1963. Among the noteworthy outcomes of the colloquium were the definition of the responsibilities, duties, and knowledge and training requirements of medical inspectors, and the techniques and methods of medical inspection.
General Organization
The central office of the Department of Workplace and Worker Medical Inspection is part of the Industrial Relations Department and reports directly to the Regional Director of Industrial Relations and Medical Inspection. The Regional Director, in turn, is part of the Regional Labour and Employment Board and reports directly to the Regional Director of Labour and Employment. The number of professionals and workers in France in 1995 were:
- 12.5 million workers benefiting from general coverage
- 6,337 physicians, of which 2,500 are full-time
- 4,000 nurses
- 1,500 medical departments
- 90% of workers are followed up by sectoral medical departments.
The number of medical inspectors in each region depends on the number of salaried occupational medicine positions in that region. In general, each regional medical inspector should be responsible for approximately 300,000 workers. This general rule is, however, subject to modification in either direction, depending on the size and geography of each region.
Mission
Although many of its clauses are no longer relevant or have lapsed, it is nevertheless useful to review the responsibilities of medical inspectors prescribed by the aforementioned decree of 16 January 1947.
The physician in charge of the department is responsible, among other things, for the coordination of all medical problems in the various departments of the Ministry of Labour and Social Security. His or her functions can be extended by decree.
The Medical Inspector of Workplaces and Workers will:
- maintain, with the Technical Committees of the Social Security Credit Unions, direct and permanent contact with the Workplace Inspection Department, and ensure the application of legislation concerning occupational hygiene and the protection of worker health
- carry out, on an ongoing basis, activities designed to protect worker health in the workplace; these activities will include, among other things, the supervision of the Occupational Medical Departments established by virtue of the law of 11 October 1946
- supervise, in close collaboration with psychotechnical departments, medical examinations aimed at determining workers’ fitness for work, and reclassifying and referring workers who are temporarily unfit for work or physically handicapped to rehabilitation centres
- supervise, in collaboration with the Technical Committees of the Social Security Credit Unions, the preparation, compilation and use of statistics concerning the physiopathological characteristics of the workforce.
The Medical Inspector of Workplaces will communicate information he or she possesses concerning the risk of occupational disease and accidents in different companies to the Technical Committees of the Social Security Credit Unions. The note of 15 September 1976 concerning the organization of Industrial Relations Departments assigns the following responsibilities to the Department of Workplace and Worker Medical Inspection:
- the investigation of technical aspects of occupational medicine, pathology, work physiology and ergonomics
- the investigation of questions related to the protection of wor-kers’ health and to work conditions
- the investigation of medical aspects of work
- the monitoring of progress in medicine, physiology and erg-onomics
- the coordination of regional information gathering.
Management of medical inspectors involves:
- the coordination of regional medical inspectors
- the development and application of reports, technical studies and research conducted regionally or transregionally, and ulti-mately, of specialized work groups
- the organization of meetings which provide members of the Department of Workplace and Worker Medical Inspection with an opportunity to compare experiences and define consistent approaches to new problems
- the preparation of recruitment and training procedures for medical inspectors of workplaces and workers
- the continuing education of all regional medical inspectors.
In addition to these core activities, the Department of Workplace and Worker Medical Inspection also collaborates with industrial relations and human resources departments in all cases involving medical aspects of work (especially those involving handicapped workers, candidates for continuing education and job applicants) and is responsible for managing, coordinating, recruiting and training regional medical inspectors and ensuring their continuing technical education. Finally, the central office of the Department also engages in consulting activities and is the government’s official representative in matters concerning occupational medicine.
The Department of Labour’s central or regional Departments of Workplace and Worker Medical Inspection may be called upon to intervene when other governmental departments without their own medical inspection services (most notably the Department of Health and Social Security) find themselves faced with problems related to the prevention or correction of occupational health hazards; these departments of the Department of Labour may also assist in the establishment of a department of medical prevention. Except in cases where the requesting party is another governmental work-inspection service, the Department’s role is usually limited to an advisory one.
From 7 to 10 June 1994, almost 1,500 people attended the XIIIth Journées nationales de médecine du travail (the 23rd National Occupational Medicine Conference) organized by the Société et l’Institut de médecine du travail et d’ergonomie de Franche-Comté (the Society and Institute of Occupational Medicine and Ergonomics of Franche-Comté). The following subjects were discussed:
- neurotoxicity of low-level solvent exposure
- health and the precariousness of health and work
- stress and strain of contemporary work—the role of the occup-ational physician.
The Department is the government’s representative in medicosocial, scientific and professional agencies or institutions in the field of occupational medicine. These include the Conseil National de l’Ordre des Médecins (the National Council of the Order of Physicians), le Haut Comité d’Études et d’Information contre l’alcoolisme (the High Commission for Alcoholism Research and Information) and various university and scientific institutions. In addition, the central Department of Workplace and Worker Medical Inspection is frequently called upon to present the French government’s position on medical questions to the European Economic Community, the WHO and the ILO. Regional departments have similar responsibilities, in accordance with Circular DRT No. 18-79, of 6 July 1979, on the role of cooperation between workplace inspectors and medical inspectors of workplaces in the prevention of occupational hazards. The circular identifies orientation, informational, supervisory, management and intervention activities to be carried out, as needed, in collaboration with the regional, departmental or local workplace inspection departments.
Although both workplace inspectors and medical inspectors share common goals—the prevention of occupational health ha-zards—their specific interventions may differ, depending on the technical expertise required. Other circumstances may, on the other hand, require their collaboration.
Proposed New Circular
A circular in preparation reiterates and updates the clauses of the circular of 6 July 1979. It should be noted that on 1 January 1995, the Departments of Occupational Training assumed the responsibilities of the regional Departments of Labour and Employment. The function, role and mission of medical inspectors of workplaces must therefore be reviewed.
In summary, we can say that by 1980, medical inspection departments had, for all intents and purposes, regained the role and functions originally foreseen for them in the period 1946-47. The most likely next step in medical inspection is towards increasing emphasis on promotion, management and research in workplaces. This evolution, it should be noted, parallels that of occupational medicine itself. Following a long period of development and implementation that may now be considered practically completed, occupational medicine must now embark upon a new era of qualitative improvement and scientific advance.
Occupational Health Services in Small-Scale Enterprises
The coverage of workers in small-scale enterprises (SSEs) is perhaps the most daunting challenge to systems for delivering occupational health services. In most countries, SSEs comprise the vast majority of the business and industrial undertakings—reaching as high as 90% in some of the developing and newly industrialized countries—and they are found in every sector of the economy. They employ on average nearly 40% of the workforce in the industrialized countries belonging to the Organization for Economic Cooperation and Development and up to 60% of the workforce in developing and newly industrialized countries. Although their workers are exposed to perhaps an even greater range of hazards than their counterparts in large enterprises (Reverente 1992; Hasle et al. 1986), they usually have little if any access to modern occupational health and safety services.
Defining Small-Scale Enterprises
Enterprises are categorized as small-scale on the basis of such characteristics as the size of their capital investment, the amount of their annual revenues or the number of their employees. Depending on the context, the number for the last category has ranged from one to 500 employees. In this article, the term SSE will be applied to enterprises having 50 or fewer employees, the most widely accepted definition (ILO 1986).
SSEs are gaining importance in national economies. They are employment-intensive, flexible in adapting to rapidly changing market situations, and provide job opportunities for many who would otherwise be unemployed. Their capital requirements are often low and they can produce goods and services near the consumer or client.
They also present disadvantages. Their lifetime is often brief, making their activities difficult to monitor and, frequently, their small margins of profits are achieved only at the expense of their workers (who are often also their owners) in terms of hours and intensity of workloads and exposure to occupational health risks.
The Workforce of SSEs
The workforce of SSEs is characterized by its diversity. In many instances, it comprises the manager as well as members of his or her family. SSEs provide entry to the world of work for young people and meaningful activities to elderly and redundant workers who have been separated from larger enterprises. As a result, they often expose such vulnerable groups as children, pregnant women and the elderly to occupational health risks. Further, since many SSEs are carried out in or near the home, they often expose family members and neighbours to the physical and chemical hazards of their workplaces and present public health problems through contamination of air or water or of food grown near the premises.
The educational level and socio-economic status of SSE workers vary widely but are often lower than the averages for the entire workforce. Of particular relevance is the fact that their owners/managers may have had little training in operation and management and even less in the recognition, prevention and control of occupational health risks. Even where appropriate educational resources are made available, they often lack the time, energy and financial resources to make use of them.
Occupational Hazards in SSEs and the Health Statusof their Workers
Like all other aspects of SSEs, their working conditions vary widely depending on the general nature of the enterprise, the type of production, the ownership and location. In general, the occupational health and safety hazards are much the same as those encountered in larger enterprises, but as noted above, the exposures to them are often substantially higher than in large enterprises. Occasionally, however, the working conditions in SSEs may be much better than those in larger enterprises with a similar type of production (Paoli 1992).
Although very few studies have been reported, it is not surprising that surveys of the health of workers in SSEs in such industrialized countries as Finland (Huuskonen and Rantala 1985) and Germany (Hauss 1992) have disclosed a relatively high incidence of health problems, many of which were associated with lowered capacity for work and/or were work-related in origin. In SSEs in developing countries an even higher prevalence of occupational diseases and work-related health problems has been reported (Reverente 1992).
Barriers to Occupational Health Services for SSEs
There are formidable structural, economic and psychological barriers to the provision of occupational health services to SSEs. They include the following:
- Traditionally, occupational safety and health legislation in most countries has exempted SSEs and is generally applicable only to manufacturing industries. The “informal sector” (this would include, say, the self-employed) and agriculture were not covered. Even where the legislation had wider coverage, it was not applicable to enterprises with small numbers of employees—500 employees was the usual lower limit. Re-cently, some countries (e.g., France, Belgium and the Nordic countries) have enacted legislation requiring the provision of occupational health service for all enterprises regardless of size or sector of the economy (Rantanen 1990).
- SSEs, as defined for this article, are too small to justify an in-plant occupational health service. Their wide diversity with respect to type of industry and methods of production as well as style of organization and operation, along with the fact that they are spread over wide geographic areas, makes it difficult to organize occupational health services that will meet all their needs.
- Economic barriers are substantial. Many SSEs hover on the edge of survival and just cannot afford any additions to their operating costs even though they may promise significant savings in the future. Further, they may not be able to afford education and training in hazard recognition, prevention and control for their owners/managers, much less their employees. Some countries have addressed the economic problem by providing subsidies either from governmental agencies or social security institutions (Rantanen 1994), or have included occupational health services in programmes promoting the general economic and social development of SSEs (Kogi, Phoon and Thurman 1988).
- Even when financial constraints are not inhibiting, there is often a disinclination among the owners/managers of SSEs to devote the time and energy needed to acquire the necessary basic understanding of the relationships between work and health. Once acquired, however, SSEs may be very successful in applying the information and abilities in their workplaces (Niemi and Notkola 1991; Niemi et al. 1991).
- Enterprises in the informal sector and small farming are seldom registered, and their formal links with official agencies may be weak or non-existent. Activities carried out as a business may be difficult to distinguish from those involving the private household and family. As a result, there may be concerns about privacy and resistance to interventions by “outsiders”. SSEs often resist becoming involved in trade associations and community organizations, and in perhaps the majority of instances their employees are not members of unions. To overcome such barriers, some countries have used extension organizations for the distribution of information, the creation of special training opportunities for the SSEs by official occupational safety and health agencies, and the adoption of the primary care model for the provision of occupational health services (Jeyaratnam 1992).
- Many SSEs are located in communities providing ready access to emergency and primary care services. However, the physicians’ and nurses’ lack of knowledge and experience with respect to occupational hazards and their effects often results in failure to recognize occupational diseases and, probably more important, loss of opportunities to install the necessary prevention and control measures.
International Instruments Covering OccupationalSafety and Health Services
In some countries, occupational safety and health activities are in the jurisdiction of labour ministries and are regulated by a special occupational safety and health authority; in others, this responsibility is shared by their ministries of labour, health and/or social affairs. In some countries, such as Italy, regulations covering occupational health services are embodied in health legislation or, as in Finland, in a special act. In the United States and in England, provision of occupational health services rests on a voluntary basis, while in Sweden, among others, it was once regulated by collective agreement.
The ILO Occupational Safety and Health Convention (No. 155) (ILO 1981a) requires governments to organize a policy for occupational safety and health to be applicable to all enterprises in all sectors of the economy that is to be implemented by a competent authority. This Convention stipulates the responsibilities of the authorities, employers and workers and, supplemented by the concomitant Recommendation No. 164, defines the key occupational safety and health activities of all relevant actors at both national and local levels.
The ILO supplemented these in 1985 by the International Convention No. 161 and Recommendation No. 171 on Occupational Health Services. These contain provisions on policy design, administration, inspection and collaboration of occupational health services, activities by occupational safety and health teams, conditions of operation, and responsibilities of employers and workers, and they furthermore offer guidelines for organizing occupational health services at the level of the enterprise. While they do not specify SSEs, they were developed with these in mind since no size limits were set for occupational health services and the necessary flexibility in their organization was emphasized.
Unfortunately, ratification of these ILO instruments has been limited, particularly in developing countries. On the basis of experience from the industrialized countries, it is likely that without special actions and support by government authorities, the implementation of the ILO principles will not take place in SSEs.
The WHO has been active in promoting the development of occupational health services. Examination of the legal requirements was carried out in a consultation in 1989 (WHO 1989a), and a series of about 20 technical documents on various aspects of occupational health services has been published by WHO headquarters. In 1985 and again in 1992, the WHO Regional Office in Europe carried out and reported surveys of occupational health services in Europe, while the Pan American Health Organization designated 1992 as a special year for occupational health by promoting occupational health activities in general and conducting a special programme in Central and South America.
The European Union has issued 16 directives concerning occupational safety and health, the most important of which is Directive 391/1989, which has been called the “Framework Directive” (CEC 1989). These contain provisions for specific measures such as requiring employers to organize health risk assessments of different technical facilities or to provide health examinations of workers exposed to special hazards. They also cover the protection of workers against physical, chemical and biological hazards including the handling of heavy loads and working at video display units.
While all of these international instruments and efforts were developed with SSEs in mind, the fact is that most of their provisions are practical only for larger enterprises. Effective models for organizing a similar level of occupational health services for SSEs remain to be developed.
Organizing Occupational Health Services for SSEs
As noted above, their small size, geographic dispersion and wide variation in types and conditions of work, coupled with great limitations in economic and human resources, make it difficult to efficiently organize occupational health services for SSEs. Only a few of the various models for delivering occupational health services described in detail in this chapter are adaptable to SSEs.
Perhaps the only exceptions are SSEs that are dispersed operating units of large enterprises. These usually are governed by policies established for the entire organization, participate in company-wide educational and training activities, and have access to a multidisciplinary team of specialists in occupational health located in a central occupational health service that is usually based at the headquarters of the enterprise. A major factor in the success of this model is having all of the costs of occupational safety and health activities covered by the central occupational health unit or the general corporate budget. When, as is increasingly common, the costs are allocated to the operating budget of the SSE, there may be difficulty in enlisting the full cooperation of its local manager, whose performance may be judged on the basis of the profitability of that particular enterprise.
Group services organized jointly by several small or medium-sized enterprises have been successfully implemented in several European countries—Finland, Sweden, Norway, Denmark, the Netherlands and France. In some other countries they have been experimented with, with the help of government subsidies or private foundations, but they have not survived after termination of subsidies.
An interesting modification of the group service model is the branch-oriented service, which provides services for a high number of enterprises operating all in the same type of industry, such as construction, forestry, agriculture, food industry and so on. The model enables the service units to specialize in the problems typical for the branch and thus accumulate high competence in the sector that they serve. A famous example of such a model is the Swedish Bygghälsan, which provides services for construction industries.
A notable exception is the arrangement organized by a trade union whose members are employed in widely scattered SSEs in a single industry (e.g., health care workers, meat cutters, office workers and garment workers). Usually organized under a collective agreement, they are financed by employers’ contributions but are usually governed by a board comprising representatives of both employers and workers. Some operate local health centres providing a broad range of primary and specialist clinical services not only for workers but often for their dependants as well.
In some instances, occupational health services are being provided by hospital outpatient clinics, private health centres and community primary care centres. They tend to focus on the treatment of acute work-related injuries and illnesses and, except perhaps for routine medical examinations, provide little in the way of preventive services. Their staffs often have a low level of sophistication in occupational safety and health, and the fact that they are usually paid on a fee-for-service basis provides no great incentive for their involvement in the surveillance, prevention and control of workplace hazards.
A particular disadvantage of these “external services” arrangements is that the customer or client relationship with those using them generally precludes the participation and collaboration of employers and workers in the planning and monitoring of these services that are stipulated in the ILO Conventions and the other international instruments created to guide occupational safety and health services.
Another variant is the “social security model”, in which occupational health services are provided by the same organization that is responsible for the cost of compensation for occupational diseases and injuries. This facilitates the availability of resources to finance the services in which, although curative and rehabilitative services are featured, preventive services are often prioritized.
An extensive study carried out in Finland (Kalimo et al. 1989), one of the very few attempts to evaluate occupational health services, showed that municipal health centres and private health centres were the dominant providers of occupational health services to SSEs, followed by the group or shared centres. The smaller the enterprise, the more likely it was to use the municipal health centre; up to 70% of SSEs with one to five workers were served by municipal health centres. Significant findings of the study included verification of the value of workplace visits by the personnel of the centres serving the SSEs to gain knowledge (1) of the working conditions and the particular occupational health problems of the client enterprises, and (2) of the need to provide them with special training in occupational safety and health before they undertake the provision of the services.
Types of Activities for Occupational Health Services for SSEs
The occupational health services designed for SSEs vary widely according to national laws and practices, the types of work and work environments involved, the characteristics and health status of the workers and the availability of resources (both in terms of the ability of the SSEs to afford the occupational health services and the availability of health care facilities and personnel in the locality). Based on the international instruments cited above and regional seminars and consultations, a list of activities for comprehensive occupational health services has been developed (Rantanen 1989; WHO 1989a, 1989b). A number of key activities that should always be found in an occupational health services programme, and that are relevant for SSEs, can be picked up from those reports. They include for example:
Assessment of occupational health needs of the enterprise
- preliminary analysis of the activities of the enterprise and identification of the health and safety hazards common to such workplaces
- inspection and surveillance of the workplace to identify and quantify the hazards actually present in the particular enterprise
- assessment of the extent of the risks they present and ranking them in order of their urgency and priority
- repeating the hazard assessment whenever there are changes in production methods, equipment and materials.
Prevention and control activities in the workplace
- communication of the results of the assessment to the owners/managers and the workers’ representatives
- identification of the prevention and control measures that are needed and available, assigning relative priority to them in terms of urgency and feasibility
- overseeing their installation and implementation
- monitoring their continuing effectiveness.
Preventive activities oriented to workers
- assessment and surveillance of workers’ health status by pre-placement, screening and periodic examinations which may be general as well as focused on the biological effects of particular hazards to which the workers may have been exposed
- adaptation of the job, the work station and the workplace environment to promote workers’ ongoing health and safety with special attention to such vulnerable groups as the very young, the elderly and those with acquired diseases and disabilities
- providing workers with health education and training in proper work practices
- providing education and training for owners/managers and supervisors that will inculcate awareness of the health needs of workers and motivation to initiate appropriate prevention and control measures.
Curative activities
- provide or arrange the delivery of the appropriate diagnostic, therapeutic and rehabilitative services for occupational injuries and diseases
- provide or arrange for early rehabilitation to obviate avoidable disability and encourage and oversee adjustments in the job that will permit early return to work
- provide education and training (and periodic retraining) in first aid and emergency procedures
- establish procedures and conduct training drills for coping with major emergencies such as spills, fires, explosions and so on
- provide or arrange for workers’ involvement in programmes that promote general health and well-being.
Record keeping and evaluation
- make and retain appropriate records on occupational accidents, injuries and diseases and if possible on exposure; evaluate the overall health and safety status of the enterprise on the basis of such data
- monitor the effectiveness of hazard prevention and control measures.
Implicit in the above list of core activities is the appropriate availability of advice and consultations in such occupational safety and health specialities as occupational hygiene, ergonomics, work physiology, safety engineering, occupational psychiatry and psychology and so on. Such specialists are not likely to be represented in the personnel of the facilities providing occupational health services to SSEs but, when needed, they can usually be provided by governmental agencies, universities and private consulting resources.
Because of their lack of sophistication and time, owners/managers of SSEs are forced to rely more heavily on the purveyors of safety equipment for the effectiveness and reliability of their products, and on the suppliers of chemicals and other production materials for complete and clear information (e.g., data sheets) about the hazards they may present and how these may be prevented or controlled. It is important, therefore, that there be national laws and regulations covering proper labelling, product quality and reliability, and the provision of easily understood information (in the local language) about equipment use and maintenance as well as product use and storage. As a backup, the trade and community organizations of which SSEs are often members should feature information about the prevention and control of potentially hazardous exposures in their newsletters and other communications.
Conclusions
In spite of their importance for the national economy and their role as employer of a majority of the nation’s workforce, SSEs, the self-employed and agriculture are sectors that are typically underserved by occupational health services. ILO Convention No. 161 and Recommendation No. 171 provide relevant guidelines for the development of such services for SSEs and should be ratified and implemented by all countries. National governments should develop the requisite legal, administrative and financial mechanisms to provide all workplaces with occupational safety and health services that will effectively identify, prevent and control exposures to potential hazards and promote the enhancement and maintenance of optimal levels of health status, well-being and productive capacity of all workers. Collaboration at international, regional and subregional levels, such as that provided by the ILO and the WHO, should be encouraged to foster the exchange of information and experience, the development of appropriate standards and guidelines and the undertaking of relevant training and research programmes.
SSEs may in many instances be reluctant to seek actively the services of occupational health units even though they might be the best beneficiaries of such services. Considering this, some governments and institutions, particularly in Nordic countries, have adopted a new strategy by starting wide-scale interventions for establishment or development of services. For instance the Finnish Institute of Occupational Health currently implements an Action Programme, for 600 SSEs employing 16,000 workers, aimed at the development of occupational health services, maintenance of work ability, prevention of environmental hazards in the neighbourhood and improving the competence of SSEs in occupational health and safety.
Accident Insurance and Occupational Health Services in Germany
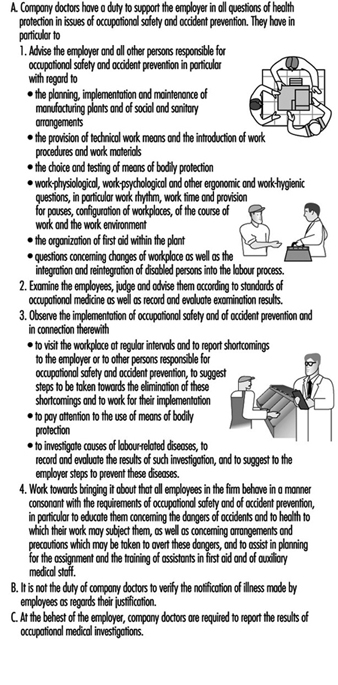
Every employer is contractually obligated to take precautions to guarantee the safety of his employees. The labour-related rules and regulations to which attention must be paid are of necessity just as various as the dangers present in the workplace. For this reason, the Occupational Safety Act (ASiG) of the Federal Republic of Germany includes among the duties of employers a legal obligation to consult specialist professionals on matters of occupational safety. This means that the employer is required to appoint not only specialist staff (particularly for technical solutions) but also company doctors for medical aspects of occupational safety.
The Occupational Safety Act has been in effect since December 1973. There were in the FRG at that time only about 500 doctors trained in what was called occupational medicine. The system of statutory accident insurance has played a decisive role in the development and construction of the present system, by means of which occupational medicine has established itself in companies in the persons of company doctors.
Dual Occupational Health and Safety System in the Federal Republic of Germany
As one of five branches of social insurance, the statutory accident insurance system makes a priority the task of taking all appropriate measures to ensure prevention of work accidents and occupational diseases through detection and elimination of work-related health hazards. In order to fulfil this legal mandate, legislators have granted extensive authority to a self-governing accident insurance system to enact its own rules and regulations concretizing and shaping the requisite preventive precautions. For this reason, the statutory accident insurance system has—within the bounds of existing public law—taken over the role of determining when an employer is required to take on a company doctor, what expert qualifications in occupational medicine the employer may demand of the company doctor and how much time the employer may estimate that the doctor will have to spend on the care of his employees.
The first draft of this accident prevention regulation dates from 1978. At that time, the number of available doctors with expertise in occupational medicine did not appear sufficient to provide all businesses with the care of company doctors. Thus the decision was made at first to establish concrete conditions for the larger businesses. At that time, to be sure, the businesses belonging to large-scale industry had often already made their own arrangements for company doctors, arrangements which already met or even exceeded the requirements stated in the accident prevention regulations.
Employment of a Company Doctor
The hours allocated in firms for the care of employees—called assignment times—are established by the statutory accident insurance system. Knowledge available to insurers concerning the existing risks to health in the various branches formed the basis for the calculation of the assignment times. The classification of firms with regard to particular insurers and the evaluation of possible health risks undertaken by them were thus the basis for the assignment of a company doctor.
Since the care rendered by company doctors is an occupational safety measure, the employer must cover the costs of assignment for such doctors. The number of employees within each of the several areas of hazard multiplied by the time allocated for care determine the sum of financial expenses. The result is a range of different forms of care, since it can pay—depending on the size of a firm—either to employ a doctor or doctors full-time, that is as the company’s own, or part-time, with services rendered on an hourly basis. This variety of requirements has led to a variety of organizational forms in which occupational medical services are offered.
The Duties of a Company Doctor
In principle, a distinction should be made, for legal reasons, between the provisions made by companies to provide care for employees and the work done by the doctors in the public health system responsible for the general medical care of the population.
In order to differentiate clearly which services of occupational medicine employers are responsible for, which are given in figure 1, the Occupational Safety Act has already anchored in law a catalogue of duties for company doctors. The company doctor is not subject to the orders of the employer in the fulfilment of these tasks; still, company doctors have had to fight the image of an employer-appointed doctor up to the present day.
Figure 1. The duties of occupational physicians employed by companies in Germany
One of the essential duties of the company doctor is the occupational medical examination of employees. This examination can become necessary according to the specific features of a given concern, if particular working conditions exist which lead the company doctor to offer, of his own accord, an examination to the employees involved. He cannot, however, force an employee to allow himself to be examined by him, but must rather convince him through trust.
Special Preventive Checkups in Occupational Medicine
There exists, in addition to this kind of examination, the special preventive check-up, participation in which by the employee is expected by the employer on legal grounds. These special preventive checkups end in the issuance of a doctor’s certificate, in which the examining doctor certifies that, based on the examination conducted, he has no objection to the employee’s engaging in work at the workplace in question. The employer may assign the employee only once for each certificate issued.
Special preventive checkups in occupational medicine are legally prescribed if exposure to particular hazardous materials occurs in the workplace or if particular hazardous activities belong to job practice and such health risks cannot be excluded through appropriate occupational safety precautions. Only in exceptional circumstances—as is the case, for example, with radiation protection checkups—is the legal requirement that an examination be performed supplemented by legal regulations concerning what the doctor carrying out the examination must pay attention to, which methods he must apply, which criteria he must use to interpret the outcome of the examination and which criteria he must apply in judging health status with regard to work assignments.
This is why in 1972 the Berufsgenossenschaften, made up of commercial trade associations which provide the accident insurance for trade and industry, authorized a committee of experts to work out commensurate recommendations to doctors working in occupational medicine. Such recommendations have existed for more than 20 years. The Berufsgenossenschaften Guidelines for Special Preventive Checkups, listed in figure 2, now show a total of 43 examination procedures for the various health hazards which can be countered, on the grounds of present knowledge, with appropriate medical precautionary measures so as to prevent diseases from developing.
Figure 2. A summary information on external services of the Berufgenossenschaften in the German building industry
The Berufsgenossenschaften deduce the mandate to make available such recommendations from their duty to take all appropriate measures to prevent occupational diseases from arising. These Guidelines for Special Preventive Checkups are a standard work in the field of occupational medicine. They find application in all spheres of activity, not only in enterprises in the sphere of trade and industry.
In connection with the provision of such occupational medical recommendations, the Berufsgenossenschaften also took steps early on to ensure that in businesses lacking their own company doctor the employer would be required to arrange for these preventive checkups. Subject to certain basic requirements having to do primarily with the specialized knowledge of the doctor, but also with the facilities available in his or her practice, even doctors without expertise in occupational medicine can acquire the authority to offer companies their services in performing preventive checkups, contingent on a policy administered by the Berufsgenossenschaften. This was the precondition for the current availability of the total of 13,000 authorized doctors in Germany who perform the 3.8 million preventive checkups performed annually.
It was the supply of a sufficient number of doctors that also made it possible legally to require that employers initiate these special preventive checkups in complete independence of the question of whether or not the company employs a doctor prepared to do such checkups. In this way, it became possible to use the statutory accident insurance system to ensure enforcement of certain measures of health protection at work, even at the level of small businesses. The relevant legal regulations may be found in the Ordinance on Hazardous Substances and, comprehensively, in the accident prevention regulation, which regulates the rights and duties of the employer and the examined employee and the function of the licensed doctor.
Care Provided by Company Doctors
The statistics released annually by the Federal Board of Doctors (Bundesärztekammer) show that for the year 1994 more than 11,500 doctors fulfil the prerequisites, in the form of specialist knowledge in industrial medicine, to be company doctors (see table 1). In the Federal Republic of Germany, the organization Standesvertretung representing the medical profession regulates autonomously which qualifications must be met by doctors as regards study and subsequent professional development before they may become active as doctors in a given field of medicine.
Table 1. Doctors with specialist knowledge in occupational medicine
|
Number* |
Percentage* |
|
|
Field designation “occupational medicine” |
3,776 |
31.4 |
|
Additional designation “corporate medicine” |
5,732 |
47.6 |
|
Specialist knowledge in occupational medicine |
2,526 |
21.0 |
|
Total |
12,034 |
100 |
* As of 31 December 1995.
The satisfaction of these prerequisites for the activity of a company doctor represents either the attainment of the field designation “occupational medicine” or of the additional designation “corporate medicine”—that is, either four years’ further study after the licence to practice in order to be active exclusively as a work physician, or three years’ further study, after which activity as a company doctor is allowed only in so far as it is connected with medical activity in another field (e.g., as an internist). Doctors tend to prefer the second variant. This means, however, that they themselves see the chief emphasis of their professional work as physicians in a classical field of medical activity, not in occupational medical practice.
For these doctors, occupational medicine has the significance of an auxiliary source of income. This explains at the same time why the medical element of the examination by doctors continues to dominate the practical exercise of the profession of company doctor, although the legislature and the statutory accident insurance system themselves emphasize inspection of companies and medical advice given to employers and employees.
In addition, there still exists a group of doctors who, having acquired specialist knowledge in occupational medicine in earlier years, met different requirements at that time. Of particular significance in this regard are the standards which doctors in the former German Democratic Republic were required to meet in order to be allowed to practice as company doctors.
Organization of Care Provided by Company Doctors
In principle, it is left up to the employer to choose freely a company doctor for the firm from among those offering occupational medical services. Since this supply was not yet available subsequent to the establishment, in the early 1970s, of the relevant legal preconditions, the statutory accident insurance system took the initiative in regulating the market economy of supply and demand.
The Berufsgenossenschaften of the building industry instituted their own occupational medical services by engaging doctors with specialist knowledge in occupational medicine in contracts to provide care, as company doctors, to the firms affiliated with them. Via their statutes, the Berufsgenossenschaften arranged for each of their firms to be cared for by its own occupational medical service. The costs incurred were distributed among all the firms through appropriate forms of financing. A summary of information concerning external occupational medical services of the Berufsgenossenschaften of the building industry is given in table 2.
Table 2. Company medical care provided by external occupational medical services,1994
|
Doctors providing care as primary occupation |
Doctors providing care as secondary occupation |
Centres |
Employees cared for |
|
|
ARGE Bau1 |
221 |
83 mobile: 46 |
||
|
BAD2 |
485 |
72 |
175 mobile: 7 |
1.64 million |
|
IAS3 |
183 |
58 |
500,000 |
|
|
TÜV4 |
72 |
|||
|
AMD Würzburg5 |
60–70 |
30–35 |
1 ARGE Bau = Workers’ Community of the Berufgenossenschaften of Building Industry Trade Associations.
2 BAD = Occupational Medical Service of the Berufgenossenschaften.
3 IAS = Institute for Occupational and Social Medicine.
4 TÜV = Technical Control Association.
5 AMD Würzburg = Occupational Medical Service of the Berufgenossenschaften.
The Berufsgenossenschaften for the maritime industry and that for domestic shipping also founded their own occupational medical services for their businesses. It is a characteristic of all of them that the idiosyncrasies of the businesses in their trade—non-stationary enterprises with special vocational requirements—were a decisive factor in their taking the initiative to make clear to their companies the necessity for company doctors.
Similar considerations occasioned the remaining Berufsgenossenschaften to unite themselves in a confederation in order to found the Occupational Medical Service of the Berufsgenossenschaften (BAD). This service organization, which offers its services to every enterprise in the market, was enabled at an early stage by the financial collateral provided by the Berufsgenossenschaften to be present over the entire area of the Federal Republic of Germany. Its broad coverage, as far as representation goes, was meant to ensure that even those businesses located in the Federal states, or states of relatively poor economic activity, of the Federal Republic would have access to a company doctor in their area. This principle has been maintained up to the present time. The BAD is considered, meanwhile, the largest provider of occupational medical services. Nonetheless, it is forced by the market economy to assert itself against competition from other providers, particularly within urban agglomerations, by maintaining a high level of quality in what it provides.
The occupational medical services of the Technical Control Association (TÜV) and of the Institute for Occupational and Social Medicine (IAS) are the second- and third-largest transregional providers. There are in addition numerous smaller, regionally active enterprises in all of the Federated States of Germany.
Cooperation with Other Providers of Services in Occupational Health and Safety
The Occupational Safety Act, as a legal foundation for care provided to companies by company doctors, provides also for professional supervision of occupational safety, particularly in order to ensure that aspects of occupational safety be handled by personnel schooled in technical precautions. The requirements of industrial practice have changed meanwhile to such an extent that technical knowledge regarding questions of occupational safety must now be supplemented more and more by familiarity with questions of the toxicology of materials used. In addition, questions of ergonomic organization of work conditions and of the physiological effects of biological agents play an increasing role in evaluations of stresses in a place of work.
The requisite knowledge may be mustered only through interdisciplinary cooperation of experts in the field of health and safety at work. Therefore, the statutory accident insurance system supports particularly the development of forms of organization which take such interdisciplinary cooperation into account at the organizational stage, and creates within its own structure the preconditions for this cooperation by redesigning its administrative departments in a suitable fashion. What was once called the Technical Inspection Service of the statutory accident insurance system turns into a field of prevention, within which not only technical engineers but also chemists, biologists and, increasingly, physicians are active together in designing solutions for problems of labour safety.
This is one of the indispensable prerequisites for creating a basis for the type of organization of interdisciplinary cooperation—within businesses and between safety technology service organizations and company doctors—required for efficient solution of the immediate problems of occupational health and safety.
In addition, supervision in respect of safety technology should be advanced, in all companies, just as much as supervision by company doctors. Safety specialists are to be employed by businesses on the same legal basis—the Occupational Safety Act—or appropriately trained personnel affiliated with the industry are to be supplied by the businesses themselves. Just as in the case of the supervision provided by company doctors, the accident prevention regulation, Specialists for Occupational Safety (VBG 122), has formulated the requirements according to which businesses must employ safety specialists. In the case of safety-technical supervision of businesses as well, these requirements take all necessary precautions to incorporate each of the 2.6 million firms currently comprising the commercial economy as well as those in the public sector.
Around two million of these firms have fewer than 20 employees and are classed as small industry. With the full supervision of all enterprises, that is, including the smaller and smallest of businesses, the statutory accident insurance system creates for itself a platform for the establishment of occupational health and safety in all areas.
Occupational Health Services in the United States: Introduction
History
Occupational health services in the United States have always been divided in function and control. The extent to which government at any level should make rules affecting working conditions has been a matter of continuing controversy. Furthermore, there has been an uneasy tension between the state and federal governments about which should take primary responsibility for preventive services based primarily upon laws governing workplace safety and health. Monetary compensation for workplace injury and illness has primarily been the responsibility of private insurance companies, and safety and health education, with only recent changes, has been left largely to unions and corporations.
It was at the state level that the first governmental effort to regulate working conditions took place. Occupational safety and health laws began to be enacted by states in the 1800s when increasing levels of industrial production began to be accompanied by high accident rates. Pennsylvania enacted the first coal mine inspection act in 1869, and Massachusetts was the first state to pass a factory inspection law in 1877.
By 1900 the more industrialized states had some laws in place regulating some workplace hazards. Early in the twentieth century, New York and Wisconsin led the nation in developing more comprehensive occupational safety and health programmes.
Most states adopted worker’s compensation laws mandating private no-fault insurance between 1910 and 1920. A few states, such as Washington, provide a state-run system allowing the collection of data and the targeting of research goals. The compensation laws varied widely from state to state, were generally not well enforced, and omitted many workers, such as agricultural workers, from coverage. Only railway, longshore and harbour workers, and federal employees have national worker’s compensation systems.
In the first decades of the twentieth century, the federal role in occupational safety and health was largely restricted to research and consultation. In 1910 the Federal Bureau of Mines was established in the Department of the Interior to investigate accidents; consult with industry; conduct safety and production research; and provide training in accident prevention, first aid and mine rescue. The Office of Industrial Hygiene and Sanitation was created in the Public Health Service in 1914 to conduct research and assist states in solving occupational safety and health problems. It was located in Pittsburgh because of its close association with the Bureau of Mines and its focus on injuries and illnesses in the mining and steel industries.
In 1913 a separate Department of Labor was established; the Bureau of Labor Standards and the Interdepartmental Safety Council were organized in 1934. In 1936, the Department of Labor began to assume a regulatory role under the Walsh-Healey Public Contracts Act, which required certain federal contractors to meet minimum safety and health standards. Enforcement of these standards was often carried out by the states with varying degrees of effectiveness, under cooperative agreements with the Department of Labor. There were many who felt that this patchwork of state and federal laws was not effective in preventing workplace injuries and illnesses.
The Modern Era
The first comprehensive federal occupational safety and health laws were passed in 1969 and 1970. In November 1968, an explosion in Farmington, West Virginia, killed 78 coalminers, providing impetus to the demands of the miners for tougher federal legislation. In 1969, the Federal Coal Mine Health and Safety Act was passed, which set mandatory health and safety standards for underground coal mines. The Federal Mine Safety and Health Act of 1977 combined and expanded the 1969 Coal Mine Act with other earlier mining laws and created the Mine Safety and Health Administration (MSHA) to establish and enforce safety and health standards for all mines in the United States.
It was not a single disaster, but a steady rise in injury rates during the 1960s that helped spur passage of the Occupational Safety and Health Act of 1970. An emerging environmental consciousness and a decade of progressive legislation secured the new omnibus act. The law covers the majority of workplaces in the United States. It established the Occupational Safety and Health Administration (OSHA) in the Department of Labor to set and enforce federal workplace safety and health standards. The law was not a complete break from the past in that it contained a mechanism by which states could administer their own OSHA programmes. The Act also established the National Institute for Occupational Safety and Health (NIOSH), in what is now the Department of Health and Human Services, to conduct research, train safety and health professionals and develop recommended safety and health standards.
In the United States today, occupational safety and health services are the divided responsibility of a number of different sectors. In large companies, services for treatment, prevention and education are primarily provided by corporate medical departments. In smaller companies, these services are usually provided by hospitals, clinics or physicians’ offices.
Toxicological and independent medical evaluations are provided by individual practitioners as well as academic and public sector clinics. Finally, governmental entities provide for the enforcement, research funding, education and standard setting mandated by occupational safety and health laws.
This complex system is described in the following articles. Drs. Bunn and McCunney from the Mobil Oil Corporation and the Massachusetts Institute of Technology, respectively, report on corporate services. Penny Higgins, RN, BS, of Northwest Community Healthcare in Arlington Heights, Illinois, delineates the hospital-based programmes. The academic clinic activities are reviewed by Dean Baker, MD, MPH, the Director of the University of California, Irvine’s Centre for Occupational and Environmental Health. Dr. Linda Rosenstock, Director of the National Institute for Occupational Safety and Health, and Sharon L. Morris, Assistant Chair for Community Outreach of the University of Washington’s Department of Environmental Health, summarize government activities at the federal, state and local levels. LaMont Byrd, the Director of Health and Safety for the International Brotherhood of Teamsters, AFL-CIO, describes the various activities provided to the membership of this international union by his office.
This division of responsibilities in occupational health often leads to overlapping, and in the case of workers’ compensation, inconsistent requirements and services. This pluralistic approach is both the strength and weakness of the system in the United States. It promotes multiple approaches to problems, but it can confuse all but the most sophisticated user. It is a system that often is in flux, with the balance of power shifting back and forth among the key players—private industry, labour unions, and state or federal governments.
Governmental Occupational Health Agencies in the United States
The Occupational Safety and Health Administration(OSHA)
Purpose and organization
OSHA was created to encourage employers and workers to reduce workplace hazards and to implement effective safety and health programmes. This is accomplished by setting and enforcing standards, monitoring the performance of state OSHA programmes, requiring employers to maintain records of work-related injuries and illnesses, providing safety and health training for employers and employees and investigating complaints of workers who claim they have been discriminated against for reporting safety or health hazards.
OSHA is directed by an Assistant Secretary of Labor for Occupational Safety and Health, who reports to the Secretary of Labor. The OSHA headquarters is in Washington, DC, with ten regional offices and about 85 area offices. About half of the states administer their own state safety and health programmes, with federal OSHA responsible for enforcement in states without approved state programmes. The Occupational Safety and Health Act also requires that each federal government agency maintain a safety and health programme consistent with OSHA standards.
Programme and services
Standards form the basis of OSHA’s enforcement programme, setting out the requirements employers must meet to be in compliance. Proposed standards are published in the Federal Register with opportunities for public comment and hearings. Final standards are also published in the Federal Register and may be challenged in a US Court of Appeals.
In areas where OSHA has not established a standard, employers are required to follow the Occupational Safety and Health Act’s general duty clause, which states that each employer shall furnish “a place of employment which is free from recognized hazards that are causing or are likely to cause death or serious physical harm to his employees”.
OSHA has the right to enter the workplace to determine whether an employer is in compliance with requirements of the Act. OSHA places highest priority on investigating imminent danger situations, catastrophes and fatal accidents, employee complaints and scheduled inspections in highly hazardous industries.
If the employer refuses entry, the inspector can be required to obtain a search warrant from a US district judge or US magistrate. Both worker and employer representatives have a right to accompany OSHA inspectors on their plant visits. The inspector issues citations and proposed penalties for any violations found during the inspection and sets a deadline for correcting them.
The employer may contest the citation to the Occupational Safety and Health Review Commission, an independent body established to hear challenges to OSHA citations and proposed fines. The employer may also appeal an unfavourable Review Commission decision to a federal court.
Consultation assistance is available at no cost to employers who agree to correct any serious hazards identified by the consultant. Assistance can be given in developing safety and health programmes and training workers. This service, which is targeted toward smaller employers, is largely funded by OSHA and provided by state government agencies or universities.
OSHA has a voluntary protection programme (VPP), which exempts workplaces from scheduled inspections if they meet certain criteria and agree to develop their own comprehensive safety and health programmes. Such workplaces must have lower than average accident rates and written safety programmes, make injury and exposure records available to OSHA and notify workers about their rights.
Resources
In 1995, the OSHA budget was $312 million, with about 2,300 employees. These resources are intended to provide coverage for more than 90 million workers throughout the United States.
State OSHA Programmes
Purpose and organization
The Occupational Safety and Health Act of 1970 gave state governments the option of regulating workplace safety and health.
States conduct their own programmes for setting and enforcing safety and health standards by submitting a state plan to OSHA for approval. The state plan details how the state proposes to set and enforce standards that are “at least as effective” as OSHA’s and to assume jurisdiction over state, city and other (non-federal) public employees whom OSHA itself does not otherwise cover. In these states, the federal government gives up direct regulatory responsibilities, and instead provides partial funding to the state programmes, and monitors the state activities for conformance with the national standards.
Programme and services
Approximately half of the states have chosen to administer their own programmes. Two other states, New York and Connecticut, have elected to keep the federal jurisdiction in their states, but to add a state workplace safety and health system that provides protection for public employees.
State-run OSHA programmes allow states to tailor resources and target regulatory efforts to match special needs in their states. For example, logging is done differently in the eastern and western United States. North Carolina, which runs its own OSHA programme, was able to target its logging regulations, outreach, training and enforcement programmes to address the safety and health needs of loggers in that state.
Washington State, which has a large agricultural economic base, developed agriculture safety requirements that exceed the mandated national minimums and translated safety information into Spanish to meet the needs of Spanish-speaking farm workers.
In addition to developing programmes that meet their special needs, states are able to develop programmes and enact regulations for which there might not be sufficient support at the federal level. California, Utah, Vermont and Washington have restrictions on workplace exposure to environmental tobacco smoke; Washington State and Oregon require that each employer develop worksite-specific injury and illness prevention plans; Utah’s standard for oil and gas drilling and the manufacture of explosives exceeds federal OSHA standards.
State programmes are permitted to conduct consultation programmes that provide free assistance to employers in identifying and correcting workplace hazards. These consultations, which are made only at the request of the employer, are kept separate from enforcement programmes.
Resources
In 1993, state-administered programmes had a total of about 1,170 enforcement personnel, according to the Occupational Safety and Health State Plan Association. In addition, they had about 300 safety and health consultants and nearly 60 training and education coordinators. The majority of these programmes are in state labour departments.
Mine Safety and Health Administration (MSHA)
Purpose and organization
The Mine Safety and Health Administration (MSHA) sets and enforces standards to reduce injuries, illnesses and deaths in mines and mineral processing operations regardless of size, number of employees or method of extraction. MSHA is required to inspect every underground mine at least four times a year and every surface mine at least twice a year.
In addition to enforcement programmes, the Mine Safety and Health Act requires that the agency establish regulations on safety and health training for miners, upgrade and strengthen mine safety and health laws and encourage the participation of miners and their representatives in safety activities. MSHA also works with the mine operators to solve safety and health problems through education and training programmes and the development of engineering controls to reduce injuries.
Like OSHA, MSHA is directed by an Assistant Secretary of Labor. The coal mine safety and health activities are administered through ten district offices in the coal mining regions. The metal and non-metal mine safety and health activities are administered through six district offices in the mining areas of the country.
A number of staff offices that assist in administering the agency’s responsibilities are located at the headquarters in Arlington, Virginia. These include the Office of Standards, Regulations and Variances; the Office of Assessments; the Technical Support directorate; and the Office of Program Policy. In addition, the Educational Policy and Development Office oversees the agency’s training programme at the National Mine Health and Safety Academy in Beckley, West Virginia, which is the world’s largest institution devoted entirely to mine safety and health training.
Programme and services
Mining deaths and injuries have declined significantly during the last hundred years. From 1880 to 1910, thousands of coal miners were killed, with 3,242 dying in 1907 alone. Large numbers of miners were also killed in other sorts of mines. The average number of mining deaths has declined over the years to less than 100 per year today.
MSHA enforces the mine act provisions requiring mine operators to have an approved safety and health training plan which provides for 40 hours of basic training for new underground miners, 24 hours of training for new surface miners, 8 hours of annual refresher training for all miners and safety-related task training for miners assigned to new jobs. The National Mine Health and Safety Academy offers a wide variety of safety and health courses. MSHA provides special training programmes for managers and workers at small mining operations. MSHA training materials, including videotapes, films, publications and technical materials are available at the Academy and at district offices.
Resources
In 1995, MSHA had a budget of about $200 million and about 2,500 employees. These resources were responsible for ensuring the health and safety of about 113,000 coal miners and 197,000 miners in metal and non-metal mines.
The National Institute for Occupational Safety and Health (NIOSH)
Purpose and organization
The National Institute for Occupational Safety and Health (NIOSH) is the federal agency responsible for conducting research on occupational injuries and illnesses and transmitting recommended standards to OSHA. NIOSH funds education programmes for occupational safety and health professionals through Educational Resource Centres (ERCs) and training projects at universities throughout the United States. Under the Federal Mine Safety and Health Act of 1977, NIOSH also conducts research and health hazard evaluations, and recommends mine health standards to the Mine Safety and Health Administration.
The Director of NIOSH reports to the Director of the Centers for Disease Control and Prevention within the Department of Health and Human Services. The NIOSH headquarters is in Washington, DC, with administrative offices in Atlanta, Georgia, and laboratories in Cincinnati, Ohio, and Morgantown, West Virginia.
Programme and services
NIOSH research is conducted both in the field and in the laboratory. Surveillance programmes identify the occurrence of work-related injury and disease. These include targeted data collection directed toward specific conditions, such as high blood lead levels in adults or injuries among adolescent workers. NIOSH also links data collected by states and other federal agencies to make it increasingly practicable to obtain a national picture of the effects of occupational hazards.
Field research is conducted at workplaces throughout the United States. These studies make it possible to identify hazards, evaluate the extent of exposures and determine the effectiveness of preventive measures. The right of entry into the workplace is essential to the ability of the Institute to conduct this research. This field research results in articles in the scientific literature as well as recommendations for preventing hazards at specific worksites.
Working with state health departments, NIOSH investigates on-the-job fatalities from specific causes, including electrocutions, falls, machine-related incidents and confined space entry accidents. NIOSH has a special programme to assist small businesses by developing inexpensive and effective technologies to control hazardous exposures at the source.
NIOSH conducts laboratory research to study workplace hazards under controlled conditions. This research assists NIOSH in determining the causes and mechanisms of workplace illnesses and injuries, developing tools for measuring and monitoring exposures, and developing and evaluating control technology and personal protective equipment.
About 17% of the NIOSH budget is devoted to funding service activities. Many of these service activities are also research-based, such as the health hazard evaluation programme. NIOSH conducts hundreds of health hazard evaluations each year when requested by employers, workers or federal and state agencies. After evaluating the worksite, NIOSH provides workers and employers with recommendations to reduce exposures.
NIOSH also responds to requests for information through a toll-free telephone number. Through this number, callers can obtain occupational safety and health information, request a health hazard evaluation or obtain a NIOSH publication. The NIOSH Home Page on the World Wide Web is also a good source of information about NIOSH.
NIOSH maintains a number of databases, including NIOSHTIC, a bibliographic database of occupational safety and health literature, and the Registry of Toxic Effects of Chemical Substances (RTECS), which is a compendium of toxicological data extracted from the scientific literature which fulfils the NIOSH mandate to “list all known toxic substances and concentrations at which toxicity is known to occur”.
NIOSH also tests respirators and certifies that they meet established national standards. This assists employers and workers in choosing the most appropriate respirator for specific hazardous environments.
NIOSH funds programmes at universities throughout the United States to train occupational medicine physicians, occupational health nurses, industrial hygienists and safety professionals. NIOSH also funds programmes to introduce safety and health into business, engineering and vocational schools. These programmes, which are either multidisciplinary ERCs or single-discipline project training grants, have made a significant contribution to the development of occupational health as a discipline and to meeting the need for qualified safety and health professionals.
Resources
NIOSH had about 900 employees and a budget of $133 million in 1995. NIOSH is the only federal agency with statutory responsibility to conduct occupational safety and health research and professional training.
The Future of Occupational Safetyand Health Programmes
The future of these federal occupational safety and health programmes in the United States is very much in doubt in the anti-regulatory climate of the 1990s. There continue to be serious proposals from Congress that would drastically change how these programmes operate.
One proposal would require the regulatory agencies to focus more on education and consultation and less on standards setting and enforcement. Another would set up requirements for complex cost benefit analyses that must be conducted before standards could be established. NIOSH has been threatened with abolition or merger with OSHA. And all these agencies have been targeted for budget reductions.
If enacted, these proposals would greatly decrease the federal role in conducting research and in setting and enforcing uniform occupational safety and health standards throughout the United States.
Corporate Occupational Health Services in the United States: Services Provided Internally
Industrial medical programmes vary in both content and structure. It is a common conception that industrial medical programmes are supported only by large corporations and are comprehensive enough to evaluate all workers for all possible adverse effects. However, the programmes implemented by industries vary considerably in their scope. Some programmes offer only pre-placement screening, while others offer total medical surveillance, health promotion and other special services. In addition, the structures of programmes differ from one another, as do the members of the safety and health teams. Some programmes contract with an off-site physician to perform medical services, while others have a health unit at the site staffed by physicians and nursing personnel and backed by a staff of industrial hygienists, engineers, toxicologists and epidemiologists. The duties and responsibility of these members of the safety and health team will vary according to the industry and the risk involved.
Motivation for Industrial Medical Programmes
The medical monitoring of workers is motivated by multiple factors. First, there is the concern for the general safety and health of the employee. Second, a monetary benefit results from a surveillance effort through increased productivity of the employee and reduced medical care costs. Third, compliance with the Occupational Safety and Health Act (OSHA), with equal employment opportunity requirements (EEO), the Americans with Disabilities Act (ADA) and other statutory guidelines is mandatory. Finally, there is the spectre of civil and criminal litigation if adequate programmes are not established or are found to be inadequate (McCunney 1995; Bunn 1985).
Types of Occupational Health Servicesand Programmes
Occupational health services are determined through a needs assessment. Factors that affect which type of occupational health service is to be utilized include the potential risks of normal operations, the demographics of the workforce and management’s interest in occupational health. Health services are dependent on the type of industry, the physical, chemical or biological hazards present, and the methods used to prevent exposure, as well as government and industry standards, regulations and rulings.
Important general health services tasks include the following:
- evaluation of employees’ ability to perform their assigned duties in a safe manner (via pre-placement evaluations)
- recognition of early symptoms and signs of work-related health effects and appropriate intervention (medical surveillance examinations can reveal these)
- provision of treatment and rehabilitation for occupational injuries and illnesses and non-occupational disorders that affect work performance (work-related injuries)
- promotion and maintenance of employees’ health (wellness)
- evaluation of a person’s ability to work in light of a chronic medical disorder (an independent medical examination is required in such a case)
- supervision of policies and programmes related to worksite health and safety.
Location of Health Services Facilities
Onsite facilities
Delivery of occupational health services today is increasingly provided through contractors and local medical facilities. However, onsite services formed by employers were the traditional approach taken by industry. In settings with a substantial number of employees or certain health risks, onsite services are cost-effective and provide high-quality services. The extent of these programmes varies considerably, ranging from part-time nursing support to a fully-staffed medical facility with full-time physicians.
The need for onsite medical service is usually determined by the nature of the company’s business and the potential health hazards present in the workplace. For example, a company that uses benzene as a raw material or ingredient in its manufacturing process will probably need a medical surveillance programme. In addition, many other chemicals handled or produced by the same plant may be toxic. In these circumstances, it may be economically feasible as well as medically advisable to provide onsite medical services. Some onsite services provide occupa-tional nursing support during daytime working hours and may also cover second and third shifts or weekends.
Onsite services should be performed in plant areas compatible with the practice of medicine. The medical facility should be centrally located to be accessible to all employees. Heating and cooling needs should be considered to permit the most economical use of the facility. A rule of thumb that has been used in allocating floor space to an in-house medical unit is one square foot per employee for units servicing up to 1,000 employees; this figure should probably include a minimum of 300 square feet. The cost of space and several relevant design considerations have been described by specialists (McCunney 1995; Felton 1976).
For some manufacturing facilities located in rural or otherwise remote areas, services may usefully be provided in a mobile van. If such an installation is made available, the following recommendations may be made:
- Assistance should be furnished to companies whose in-house medical services are not fully equipped to cope with medical surveillance programmes that require the use of special equipment, such as audiometers, spirometers or x-ray machines.
- Medical surveillance programmes should be made available in remote geographical areas, especially to ensure uniformity in data collected for epidemiology studies. For example, to enhance the scientific accuracy of a study of occupational lung disorders, a similar spirometer should be used and the preparation of chest films should be performed according to appropriate international standards, such as those of the International Labour Organization (ILO).
- Data from different sites should be coordinated for entry into a computer software programme.
A company that relies on a mobile van service, however, will still require a physician to conduct pre-placement examinations and to assure the quality of the services provided by the mobile van company.
Services Most Commonly Performedin the In-house Facility
An onsite assessment is essential to determine the type of health services appropriate for a facility. The most common services provided in the occupational health setting are pre-placement evaluations, assessment of work-related injury or illness and medical surveillance examinations.
Pre-placement evaluations
The pre-placement examination is performed after a person has been given a conditional offer of a job. The ADA uses pre-employment to mean that the person is to be hired if he or she passes the physical examination.
The pre-placement examination should be performed with attention to the job duties, including physical and cognitive requirements (for safety sensitivity) and potential exposure to hazardous materials. The content of the examination depends on the job and the worksite assessment. For example, jobs that require use of personal protective equipment, such as a respirator, often include a pulmonary function study (breathing test) as part of the pre-placement examination. Those involved in the US Department of Transportation (DOT) activities usually require urinary drug testing. To avoid errors in either the content or the context of the examination, it is advisable to develop standard protocols to which the company and the examining physician agree.
After the examination, the physician provides a written opinion about the person’s suitability for performing the job without health or safety risk to self or others. Under usual circumstances, medical information is not to be divulged on this form, merely fitness for duty. This form of communication can be a standard form that should then be placed in the employee’s file. Specific medical records, however, remain at the health facility and are maintained only by a physician or nurse.
Work-related injuries and illnesses
Prompt, quality medical care is essential for the employee sustaining a work-related injury or occupational illness. The medical unit or contract physician should treat employees who are injured at work or who experience work-related symptoms. The company’s medical service has an important role to play in the management of workers’ compensation costs, especially in performing return-to-work assessments following absence due to an illness or injury. A major function of the medical professional is the coordination of rehabilitation services of such absentees to insure a smooth return to work. The most effective rehabilitation programmes make use of modified-duty or alternative assignments.
An important task of the company’s medical adviser is to determine the relationship between exposure to hazardous agents and illness, injury or impairment. In some states, the employee may choose his or her attending physician, whereas in other states the employer may direct or at least suggest evaluation by a specific physician or health care facility. The employer usually has the right to specify a physician to conduct a “second opinion” examination, especially in the context of a protracted recovery or serious medical disorder.
The nurse or physician advises management on the recordability of occupational injuries and illnesses in accordance with OSHA record-keeping requirements, and needs to be familiar with both OSHA and Bureau of Labor Statistics (BLS) guidelines. Management must assure that the health care provider is thoroughly familiar with these guidelines.
Medical surveillance examinations
Medical surveillance examinations are required by some OSHA standards for exposure to some substances (asbestos, lead and so on) and are recommended as being in accordance with good medical practice for exposure to others, such as solvents, metals and dusts such as silica. Employers must make these examinations, when required by OSHA standards, available at no cost to employees. Although the employee may decline to participate in an examination, the employer may specify that the examination is a condition of employment.
The purpose of medical surveillance is to prevent work-related illnesses through early recognition of problems, such as abnormal laboratory results that may be associated with the early stages of a disease. The employee is then re-evaluated at subsequent intervals. Consistency in the medical follow-up of abnormalities uncovered during medical surveillance examinations is essential. Although management should be apprised of any medical disorders related to work, medical conditions not arising from the workplace should remain confidential and be treated by the family physician. In all cases, employees should be informed of their results (McCunney 1995; Bunn 1985, 1995; Felton 1976).
Management Consultation
Although the occupational health physician and nurse are most readily recognized through their hands-on medical skills, they can also offer significant medical advice to any business. The health professional can develop procedures and practices for medical programmes including health promotion, substance abuse detection and training, and medical record-keeping.
For facilities with an in-house medical programme, a policy for the management of medical waste handling and related activities is necessary in accordance with the OSHA blood-borne pathogen standard. Training with respect to certain OSHA standards, such as the Hazard Communication Standard, the OSHA Standard on Access to Exposure and Medical Records, and OSHA record-keeping requirements, is an essential ingredient to a well-managed programme.
Emergency response procedures should be developed for any facility that is at increased risk of natural disaster or that handles, uses or manufactures potentially hazardous materials, in accordance with the Superfund Act Reauthorization Amendment (SARA). Principles of medical emergency response and disaster management should, with the assistance of the company’s physician, be incorporated in any site emergency response plan. Since the emergency procedures will differ depending on the hazard, the physician and nurse should be prepared to handle both physical hazards, such as those that occur in a radiation accident, and chemical hazards.
Health Promotion
Health promotion and wellness programmes to educate people on the adverse health effects of certain lifestyles (such as cigarette smoking, poor diet and lack of exercise) are becoming more common in industry. Although not essential to an occupational health programme, these services can be valuable to employees.
The incorporation of wellness and health promotion plans in the medical programme is recommended whenever feasible. The objectives of such a programme are a health-conscious, productive workforce. Health care costs can be reduced as a result of health promotion initiatives.
Substance Abuse Detection Programmes
Within the past few years, especially since the US Department of Transportation (DOT) Ruling on Drug Testing (1988), many organizations have developed drug testing programmes. In the chemical and other manufacturing industries, the most common type of urinary drug test is performed at the pre-placement evaluation. The DOT rulings on drug testing for interstate trucking, gas transmission operations (pipelines), and the railroad, coast guard and aviation industries are considerably broader and include periodic testing “for cause,” that is, for reasons of suspected substance abuse. Physicians are involved in drug screening programmes by reviewing results to assure that reasons other than illicit drug use are eliminated for individuals with positive tests. They must ensure the integrity of the testing process and confirm any positive test with the employee before releasing the results to management. An employee assistance programme and uniform company policy are essential.
Medical Records
Medical records are confidential documents which should be maintained by an occupational physician or nurse and stored in such a manner so as to protect their confidentiality. Some records, such as a letter indicating a person’s fitness for respirator use, should be kept onsite in the event of a regulatory audit. Specific medical test results, however, should be excluded from such files. Access to such records should be limited to the health professional, the employee and other persons designated by the employee. In some instances, such as the filing of a workers’ compensation claim, confidentiality is waived. The OSHA Access to Employee Exposure and Medical Records standard (29 CFR 1910.120) requires that employees be informed annually of their right of access to their medical records and of the location of such records.
Confidentiality of medical records must be preserved in accordance with legal, ethical and regulatory guidelines. Employees should be informed when medical information will be released to management. Ideally, an employee will be asked to sign a medical form that authorizes release of certain medical information, including laboratory tests or diagnostic material.
The first item in the American College of Occupational and Environmental Medicine Code of Ethics requires that “Physicians should accord the highest priority to the health and safety of individuals in both the workplace and the environment.” In the practice of occupational medicine, both employer and employee benefit if physicians are impartial and objective and apply sound medical, scientific and humanitarian principles.
International Programmes
In international occupational and environmental medicine, physicians working for US industries will have not only the traditional responsibilities of occupational and environmental physicians but will also have significant clinical management responsibilities. The responsibility of the medical department will include the clinical care of the employees and commonly the spouses and children of the employees. Servants, extended family and the community are often included in the clinical responsibilities. In addition, the occupational physician will also have responsibilities for occupational programmes related to workplace exposures and risks. Medical surveillance programmes, as well as pre-employment and periodic examinations are critical programme components.
Designing appropriate health promotion and prevention programmes is also a major responsibility. In the international arena, these prevention programmes will include issues in addition to those lifestyle issues commonly considered in the United States or Western Europe. Infectious diseases require a systematic approach to needed vaccination and chemoprophylaxis. Educational programmes for prevention must include attention to food-, water- and blood-borne pathogens and to general sanitation. Accident prevention program-mes must be considered in view of the high risk for traffic-related deaths in many developing countries. Special issues such as evacuation and emergency care must be given detailed scrutiny and appropriate programmes implemented. Environmental exposure to chemical, biological and physical hazards is often increased in developing countries. Environmental prevention programmes are based on multi-staged education plans with indicated biological testing. The clinical programmes to be developed internationally may include inpatient, outpatient, emergency and intensive care management of expatriates and national employees.
An ancillary programme for international occupational physicians is travel medicine. The safety of short-term rotational travellers or foreign residents requires special knowledge of the indicated vaccinations and other preventive measures on a global basis. In addition to recommended vaccinations, a knowledge of medical requirements for visas is imperative. Many countries require serologic testing or chest x rays, and some countries may take into account any significant medical condition in the decision to issue a visa for employment or as a residency requirement.
Employee assistance and marine and aviation programmes are also commonly included within the international occupational physician’s responsibilities. Emergency planning and the provision of appropriate medications and training in their use are challenging issues for sea and air vessels. Psychological support both of expatriate and national employees is often desirable and/or necessary. Employee assistance programmes may be extended to expatriates and special support given to family members. Drug and alcohol programmes should be considered within the social context of the given country (Bunn 1995).
Conclusion
In conclusion, the scope and organization of corporate occupational health programmes may vary widely. However, if appropriately discussed and implemented, these programmes are cost-effective, protect the company from legal liabilities and promote the occupational and general health of the workforce.
Contract Occupational Health Services in the United States
Setting
Employers in the United States have long provided medical care for injured workers through the use of private physicians, clinics, immediate-care facilities and hospital emergency departments. This care for the most part has been episodic and rarely coordinated, as only the largest corporations could provide in-house occupational health services.
A recent survey of 22,457 companies of fewer than 5,000 employees in a suburban area of Chicago found that 93% had less than 50 employees and only 1% employed more than 250 employees. Of this group, 52% utilized a specific provider for their work injuries, 24% did not utilize a specific provider and another 24% allowed the employee to seek his or her own provider. Only 1% of the companies utilized a medical director to provide care. These companies make up 99% of all employers in the surveyed area, representing over 524,000 employees (National Health Systems 1992).
Since the passage of the act which created the Occupational Safety and Health Administration in 1970, and with the accompanying changes in health care financing that have taken place since that time, the focus and priorities of care have changed. Insurance costs for workers’ compensation and group health care have risen from 14 to 26% annually from 1988 to 1991 (BNA 1991). In 1990, health care costs accounted for the single largest portion of the $53 billion spent in the United States for workers’ compensation benefits, and in 1995, medical benefits are expected to reach 50% of a total $100 billion price tag for workers’ compensation costs (Resnick 1992).
Premium costs vary by state because of differing workers’ compensation regulations. The Kiplinger Washington Letter of 9 September 1994 states, “In Montana, contractors pay an average of $35.29 in compensation insurance for every $100 of payroll. In Florida, it’s $21.99. Illinois, $19.48. Same coverage costs $5.55 in Indiana or $9.55 in South Carolina.” As the need for economical workers’ compensation care has evolved, employers are demanding more assistance from their health care providers.
The bulk of this medical care is rendered by independently owned medical facilities. Employers may contract for this care, develop a relationship with a provider or secure it on an as-needed basis. Most care is rendered on a fee-for-service basis, with the beginnings of capitation and direct contracting emerging during the later half of the 1990s.
Types of Services
Employers universally require that occupational health services include acute treatment of injuries and illnesses such as sprains, strains, back and eye injuries and lacerations. These make up the majority of acute cases seen in an occupational health programme.
Often, examinations are requested that are given pre-placement or after a job offer, to determine prospective employees’ ability to safely perform the work required without injury to themselves or others. These examinations must be evaluated consistently with US law as embodied in the Americans with Disabilities Act. This law forbids discrimination in hiring based on a disability that does not prevent an individual from performing the essential functions of the prospective job. The employer is further expected to make a “reasonable accommodation” to a disabled employee (EEOC and Department of Justice 1991).
Though required by law only for certain job categories, substance abuse testing for drugs and/or alcohol is now performed by 98% of the Fortune 200 companies in the United States. These tests may include measurements of urine, blood and breath for levels of illicit drugs or alcohol (BNA 1994).
In addition, an employer may require specialized services such as OSHA-mandated medical surveillance tests—for instance, respirator fitness examinations, based on a worker’s physical capacity and pulmonary function, assessing the worker’s ability to wear a respirator with safety; asbestos examinations and other chemical exposure tests, tailored to assess an individual’s health status with respect to possible exposure and long-term effects of a given agent on the person’s overall health.
In order to assess the health status of key employees, some companies contract for physical examinations for their executives. These examinations are generally preventive in nature and offer extensive health assessment, including laboratory testing, x rays, cardiac stress testing, cancer screening and lifestyle counselling. The frequency of these examinations is often based on age rather than type of work.
Periodic fitness examinations are often contracted for by municipalities to assess the health status of fire and police officers, who are generally tested to measure their physical ability to handle physically stressful situations and to determine whether exposures have occurred in the workplace.
An employer may also contract for rehabilitative services, including physical therapy, work hardening, workplace ergonomic assessments as well as vocational and occupational therapies.
More recently, as a benefit to employees and in an effort to decrease health care costs, employers are contracting for wellness programmes. These prevention-oriented screenings and educational programmes seek to assess health so that appropriate interventions might be offered to alter lifestyles that contribute to disease. Programmes include cholesterol screening, health risk appraisals, smoking cessation, stress management and nutrition education.
Programmes are being developed in all areas of health care to meet the needs of employees. The employee assistance program (EAP) is another recent programme developed to provide counselling and referral services to employees with substance abuse, emotional, family and/or financial problems which employers have determined have an effect on the employee’s ability to be productive.
A service that is relatively new to occupational health is case management. This service, usually provided by nurses or clerical personnel supervised by nurses, has effectively reduced costs while ensuring appropriate quality care for the injured worker. Insurance companies have long provided management of claims costs (the dollars spent on workers’ compensation cases) at a point when the injured worker has been off work for a specified length of time or when a certain dollar amount has been reached. Case management is a more proactive and concurrent process which may be applied from the first day of the injury. Case managers direct the patient to the appropriate level of care, interact with the treating physician to determine what types of modified work the patient is medically capable of performing, and work with the employer to ensure that the patient is performing work which will not worsen the injury. The case manager’s focus is to return the employee to a minimum of modified duty as quickly as possible as well as to identify good quality physicians whose results will best benefit the patient.
The Providers
Services are available through a variety of providers with varying degrees of expertise. The private physician’s office may offer pre-placement examinations and substance abuse testing as well as follow-up of acute injuries. The physician’s office generally requires appointments and has limited hours of service. If the capabilities exist, the private physician may also offer executive examinations or may refer the patient to a nearby hospital for extensive laboratory, x-ray and stress testing.
The industrial clinic generally offers acute care of injuries (including follow-up care), pre-placement examinations and substance abuse testing. They often have x-ray and laboratory capabilities and may have physicians who have experience in assessing the workplace. Again, their hours are generally limited to business hours so that employers with second- and third-shift operations may need to utilize an emergency department during evenings and weekends. The industrial clinic rarely treats the private patient, and it is generally perceived as the “company doctor”, since arrangements are usually made to bill the employer or the company’s insurance carrier directly.
Immediate care facilities are another alternative delivery site. These facilities are walk-in providers of general medical care and require no appointments. These facilities generally are equipped with x-ray and laboratory capabilities and physicians experienced in emergency medicine, internal medicine or family practice. The type of client ranges from the paediatrics patient to the adult with a sore throat. In addition to acute injury care and minor follow-up of injured employees, these facilities may perform pre-placement physicals and substance abuse testing. Those facilities which have developed an occupational health component often provide periodic exams and OSHA-mandated screenings, and may have contractual relationships with additional providers for services that they do not themselves offer.
The hospital emergency room is often the site of choice for treatment of acute injuries and has generally been capable of little else in terms of occupational health services. This has been the case although the hospital has had the resources to provide most of the required services with the exception of those offered by physicians with expertise in occupational medicine. Yet an emergency department alone lacks the managed care and return-to-work expertise now being demanded by industry.
Hospital-Based Programmes
Hospital administrations have become cognizant that they not only have the resources and technology available but that workers’ compensation was one of the last “insurance” programmes which would pay fees for service, thereby boosting revenues hurt by discounting arrangements that were made with managed care insurance companies such as HMOs and PPOs. These managed care companies, as well as the federally and state funded Medicare and Medicaid programmes for general health care, have demanded shorter lengths of stay and have imposed a payment system based on “diagnosis-related grouping” (DRG). These schemes have forced hospitals to lower costs by seeking improved coordination of care and new revenue-producing products. Fears arose that costs would be shifted from group health managed care to workers’ compensation; in many cases these fears were well-founded, with costs for treating an injured back under workers’ compensation two to three times the cost under group health plans. A 1990 Minnesota Department of Labour and Industry study reported that costs of treatment for sprains and strains were 1.95 times greater, and those for back injuries 2.3 times greater, under workers’ compensation than under group health insurance plans (Zaldman 1990).
Several different hospital delivery models have evolved. These include the hospital-owned clinic (either on campus or off), the emergency department, the “fast-track” (non-acute emergency department), and administratively managed occupational health services. The American Hospital Association reported that Ryan Associates and Occupational Health Research had studied 119 occupational health programmes in the United States (Newkirk 1993). They found that:
- 25.2% were hospital emergency department based
- 24.4% were hospital non-emergency department based
- 28.6% were hospital free-standing clinics
- 10.9% were independently owned free-standing clinics
- 10.9% were other types of programmes.
All of these programmes assessed costs on a fee-for-service basis and offered a variety of services which, in addition to treatment of acutely injured workers, included pre-placement examinations, drug and alcohol testing, rehabilitation, workplace consulting, OSHA-mandated medical surveillance, executive physicals and wellness programmes. In addition, some offered employee assistance programmes, onsite nursing, CPR, first aid and case management.
More often today hospital occupational health programmes are adding a nursing model of case management. Within such a model incorporating integrated medical management, total workers’ compensation costs can be lowered 50%, which is a significant incentive for the employer to utilize providers that afford this service (Tweed 1994). These cost reductions are generated by a strong focus on the need for early return to work and for consultation on modified work programmes. The nurses work with the specialists to help define medically acceptable work that an injured employee can perform safely and with restrictions.
In most states, US workers receive two-thirds of their salary while receiving temporary workers’ compensation for total disability. When they return to modified work, they continue to provide a service for their employers and maintain their self-esteem through work. Workers who have been off work six or more weeks frequently never return to their full employment and are often forced to perform lower-paying and less skilled jobs.
The ultimate goal of a hospital-based occupational health programme is to allow patients access to the hospital for work injury treatment and to continue with the hospital as their primary provider of all health care services. As the United States moves to a capitated health care system, the number of covered lives a hospital serves becomes the prime indicator of success.
Under this capitated form of health care financing, employers pay a per capita rate to providers for all health care services that their employees and their dependants may need. If the individuals covered under such a plan stay healthy, then the provider is able to profit. If the covered lives are high utilizers of services, the provider may not earn enough revenue from premiums to cover the costs of care and may therefore lose money. Several states in the United States are moving toward capitation for group health insurance and a few are piloting 24-hour coverage for all health care, including workers’ compensation medical benefits. Hospitals will no longer judge success on patient census but on a ratio of covered lives to costs.
Comprehensive hospital-based occupational health programmes are designed to fill a need for a high-quality comprehensive occupational medicine programme for the industrial and corporate community. The design is based on the premise that injury care and pre-placement physicals are important but alone do not constitute an occupational medicine programme. A hospital serving many companies can afford an occupational medicine physician to oversee medical services, and therefore, a broader occupational focus can be gained, allowing for toxicology consultations, worksite evaluations and OSHA-mandated examin-ations for such contaminants as asbestos or lead and for equipment such as respirators, in addition to the usual services of work injury treatment, physical examinations and drug screening. Hospitals also have the resources necessary to provide a compute-rized database and case management system.
By providing employers with a single full service centre for their employees’ health care needs, the occupational health programme can better ensure that the employee receives quality, compassionate health care in the most appropriate setting, at the same time reducing costs to the employer. Occupational health providers can monitor trends within a company or an industry and make recommendations to reduce workplace accidents and improve safety.
A comprehensive hospital-based occupational health programme allows the small employer to share the services of a corporate medical department. Such a programme provides prevention and wellness as well as acute care service and permits a sharper focus on promotion of health for US workers and their families.
Labour Union-Based Activities in the United States
In 1995, the US Department of Labor, Bureau of Labor Statistics, published a report indicating that 18.8 million workers, or approximately 16% of the United States workforce, are either union members or workers who report no union affiliation but are covered by a union contract (US Department of Labor 1995). Table 1 draws upon this report to characterize the unionized workforce by industry. Most of these workers are represented by labour unions affiliated with the American Federation of Labour and Congress of Industrial Organizations (AFL-CIO), which comprises 86 national and international unions (Statistical Abstract of the United States 1994). Labour unions are typically organized into international or national headquarters, regional and district offices and local unions.
Table 1. 1994 distribution of the US unionized workforce according to industry
|
Occupation |
Total employed |
Members of unions* |
Represented by unions** |
||
|
Employed |
Total (%) |
Employed |
Total (%) |
||
|
Agricultural wage |
1,487 |
34 |
2.3 |
42 |
2.8 |
|
Private nonagricultural wage and salary workers |
88,163 |
9,620 |
10.9 |
10,612 |
12 |
|
Mining |
652 |
102 |
15.7 |
111 |
17.1 |
|
Construction |
4,866 |
916 |
18.8 |
966 |
19.9 |
|
Manufacturing |
19,267 |
3,514 |
18.2 |
3,787 |
19.7 |
|
Durable goods |
11,285 |
2,153 |
19.1 |
2,327 |
20.6 |
|
Nondurable goods |
7,983 |
1,361 |
17 |
1,460 |
18.3 |
|
Transportation and public utilities |
6,512 |
1,848 |
28.4 |
1,997 |
30.7 |
|
Transportation |
3,925 |
1,090 |
27.8 |
1,152 |
29.3 |
|
Communications and public utilities |
2,587 |
758 |
29.3 |
846 |
32.7 |
|
Wholesale and retail trade |
22,319 |
1,379 |
6.2 |
1,524 |
6.8 |
|
Wholesale trade |
3,991 |
260 |
6.5 |
289 |
7.2 |
|
Retail trade |
18,328 |
1,120 |
6.1 |
1,236 |
6.7 |
|
Finance, insurance and real estate |
6,897 |
156 |
2.3 |
215 |
3.1 |
|
Services |
27,649 |
1,704 |
6.2 |
2,012 |
7.3 |
|
Government workers |
18,339 |
7,094 |
38.7 |
8,195 |
44.7 |
* Data refer to members of a labour union or an employee association similar to a union.
** Data refer to members of a labour union or an employee association similar to a union, as well as to workers who report no union affiliation but whose jobs are covered by a union or an employee association contract.
Note: Data refer to the sole or principal job of full- or part-time workers. Excluded are self-employed workers whose businesses are incorporated although they technically qualify as wage and salary workers. Data for 1994 are not directly comparable with data for 1993 and earlier years. For additional information, see “Revisions in the current population survey effective January 1994”, in the February 1994 issue of Employment and Earnings.
Labour unions provide comprehensive safety and health services to workers who are members of unions. Through the development of collective bargaining agreements and by providing technical and related services, unions address the needs and concerns of their members.
On the national and international levels, union officers and staff members (safety and health professionals, attorneys, lobbyists and others) work to influence elected officials to pass safety and health laws and rules which protect workers. Union representatives also develop and negotiate collective bargaining agreements with employers containing legally binding safety and health contract language.
Labour unions ensure that workers have safe, healthful work environments through collective bargaining agreements. Ideally these agreements also provide workers with a means of addressing safety and health issues or of resolving safety and health disputes that may arise at the workplace.
Technical Assistance
At the central office, labour unions often employ or contract professional industrial hygienists, ergonomists, occupational physicians, engineers and other safety and health professionals to furnish technical assistance to workers. These professionals provide such services as conducting complaint investigations; carrying out job-site safety and health evaluations; and interpreting and translating environmental monitoring data, medical results and other technical information into language understandable by the average worker.
Safety and health complaint investigations are routinely conducted by labour union professional staff or consultants. Working in conjunction with designated employee representatives from the affected local union, these professionals address issues such as workers’ exposure to chemical or physical hazards, musculoskeletal illnesses and injuries, and non-compliance with applicable safety and health regulations.
In addition, unions may become involved in accident investigations in situations where the employer’s investigation results are disputed by the affected employees.
Labour union representatives may use the information obtained during such investigations to resolve safety and health complaints by working with the employer through the collective bargaining process. Unions may utilize the grievance procedure or specific safety and health contract language to protect workers. However, the union may elect to contact a federal or state regulatory agency if the employer is not in compliance with established laws, rules or regulations.
Union-based safety and health professionals and/or trained designated union workplace representatives—for example, local union safety and health committee members or shop stewards —conduct job-site surveys to evaluate the work environment for hazards.
During the surveys, the manufacturing processes or other operations within the job-site are evaluated. Safety and health records (for instance, OSHA 200 Logs, Department of Transportation (DOT) Accident Reports, environmental monitoring results and written programmes) are reviewed to determine compliance with collective bargaining agreements and governmental standards and regulations. The results of the surveys are documented and any problems are resolved through collective bargaining or by contacting a governmental regulatory agency.
Workers themselves often request technical or regulatory information and reports—for example, chemical fact sheets, environmental monitoring results, biological monitoring results, or federal or state safety and health regulations. Because of the technical nature of this information, the worker may require assistance in understanding the subject matter and how it applies to his or her workplace. Union-based safety and health staff can provide the workers with assistance in understanding technical information. The manner in which the assistance is provided is dependent upon the needs of the worker.
Labour unions also serve as a clearinghouse for specialized medical care or assistance for use in workers’ compensation hearings. Unions typically maintain lists of the names and addresses of reputable independent physicians to whom the worker may be referred, if necessary.
Legislative and Rulemaking Activities
Active involvement in safety and health governmental rulemaking is a very important concern of labour unions; they encourage their members to become involved in legislative and safety and health rulemaking activities on varying levels.
Unions seek to influence politicians to propose legislation to establish adequate workplace safety and health standards; to respond to proposed safety and health rulemaking submitted by governmental regulatory agencies; to influence the manner in which governmental regulatory agencies enforce workplace safety and health regulations; or to organize support for governmental regulatory agencies subject to budgetary reductions or operational changes by the US Congress.
Union lobbyists, technical professionals, research workers and legal staff members are the primary personnel involved in these activities. These staff members are responsible for collecting, analysing and organizing the data necessary to develop a union position on legislative or rulemaking activities. They also make the necessary contacts with agencies or individuals to ensure that the union’s position is presented to elected officials.
Union safety and health staff members may encounter a safety and health issue that affects workers but is not regulated by a governmental agency. In this instance, the union may develop written comments and/or oral testimony to be presented during public hearings. The intent of the comments or testimony is to educate the relevant officials and encourage them to draft legislation to resolve the issue.
Agencies that enforce safety and health regulations are, on occasion, targeted for budget reductions. Often these budget cuts are seen as being adverse to the protection of the safety and health of workers on the job. Labour unions develop and implement strategies to prevent such reductions. This may be done by working with union lobbyists to educate legislative and other officials on the adverse effects that the reductions will have on workers. In addition, there are “grassroots efforts” that include organizing and mobilizing workers to write letters to their elected officials highlighting their opposition to the proposed cuts.
In addition, unions are very involved in preparing and delivering written comments and oral testimony in response to proposed safety and health rulemaking promulgated by federal and state regulatory agencies. It is vitally important that workers have opportunities for meaningful participation in the rulemaking process. Labour unions are the means workers can use to participate fully in the rulemaking process.
Collective Bargaining Agreements
The collective bargaining agreement is the primary tool used by labour unions to implement services to the members. Labour unions use the technical expertise of industrial hygienists, ergonomists, engineers, occupational physicians and other safety and health professionals to collect and analyse safety and health information in order to prepare the union representatives who are responsible for negotiating collective bargaining agreements.
Labour unions utilize collective bargaining agreements as legal, binding documents to provide occupational safety and health protection to workers. The primary goals of the agreements are to provide protection to workers who are either not covered by federal or state workplace safety and health standards and regulations, or to provide protection to workers beyond the minimum state and federal standards.
To prepare for bargaining, unions collect information to document the safety and health issues affecting the membership. This may be accomplished by conducting membership surveys, working with technical staff and/or consultants to identify workplace hazards, reviewing information pertaining to safety and health complaints or investigations that may have been conducted, and by reviewing and evaluating workers’ compensation data, environmental monitoring surveys, or injury and illness logs.
In the final stages of preparation for bargaining, the negotiation committee prioritizes the safety and health issues and considers feasible solutions to the issues.
Worker Education and Training
Labour unions have a very important role in providing safety and health training and education to their members.
The type of training provided ranges from basic workplace safety rights (e.g., hazard communication) to extensive industry-specific training such as that provided to workers who are involved in hazardous waste remediation projects. This training is vitally important for workers who work in rapidly changing work environments.
Worker training provided by unions is usually funded through members’ dues, federal and state grants, and training funds established by employers as negotiated in collective bargaining agreements. Worker training and education courses are developed by professional staff and consultants along with extensive worker input. Often, train-the-trainer courses are provided to allow for peer training.
Research Efforts
Labour unions work with institutions such as universities and governmental agencies to conduct specific occupational safety and health research. The research efforts are typically funded by the union or the employers or through state or federal grants.
The unions use the results of the studies in the safety and health rulemaking process to negotiate contract language in order to eliminate or significantly reduce hazards in the workplace or, alternatively, to develop interventions to eliminate or significantly reduce excessive risk to the union members—for instance, to provide smoking cessation courses among asbestos-exposed workers. In addition, research results may be used to develop or modify various types of equipment used on the job.
The occupational safety and health services provided by labour unions are primarily preventive in nature and require the combined efforts of technical professionals, occupational physicians, lawyers, lobbyists and union members. By providing these services, labour unions are able effectively to ensure the safety and health of their members and of other workers in the workplace.
Academic-Based Occupational Health Services in the United States
During the 1980s and 1990s, academic occupational and environmental medicine clinics have emerged as a small, yet important source of occupational health services in the United States. These clinics are affiliated with academic medical centres, schools of medicine or schools of public health. The physician staff is composed primarily of faculty members of the academic programmes with principal teaching and research interests in occupational medicine. The main activity of these clinics is to provide diagnostic medical evaluations of potential occupational and environmental diseases, although many clinics also provide routine occupational health services. These clinics play an important role in occupational health in the United States by serving as an independent source of medical expertise on occupational diseases. The clinics are also major training sites for specialists in occupational medicine and recently for primary care physicians.
The Setting
Independent sources of medical expertise on occupational diseases are needed in the United States because employers are legally responsible for providing medical care and lost wages only if it can be demonstrated that an injury or illness is related to work. As noted in previous articles of this chapter, the vast majority of medical care for injured workers is provided by employers either directly by the employer or indirectly through contracts with private physicians, clinics, immediate care facilities and hospital-based programmes. This system of care is quite adequate for workers with acute injuries or diseases because the role of work in causing these conditions is clear. Therefore, it is in the employer’s interest to provide timely and effective medical treatment so that the employee returns to work as quickly as possible. However, the workers’ compensation systems in the United States do not function well for workers with chronic injuries and occupational diseases because employers are not required to pay for medical care unless it can be proved that the worker’s job was responsible for the condition. If an employer contests a compensation claim, the employee or workers’ compensation officials must seek an independent evaluation to determine whether the condition is work-related. Academic medical clinics have served as regional consultation programmes to provide this independent source of medical expertise.
Academic occupational medicine clinics have been able to maintain an independent perspective because few of them depend on employer contracts or similar financial incentives which could represent a conflict of interest in evaluating workers’ illnesses. These clinics typically operate as non-profit-making programmes that absorb some of the cost of medical evaluations as part of their teaching and service mission, since complex diagnostic evaluations are rarely cost-effective to undertake without employer support.
The growth of academic-based occupational and environmental medicine clinics has also come about as a consequence of the growth of academic occupational and environmental medicine programmes in schools of medicine and academic medical centres. Until recently, there was a small number of occupational health programmes in the United States, and virtually all of these were based in schools of public health, emphasizing disciplines such as industrial hygiene, toxicology and epidemiology. The number of academic occupational and environmental medicine programmes in schools of medicine increased substantially during the 1980s and 1990s.
This growth occurred for several reasons. The Occupational Safety and Health Act passed in 1970 created the National Institute for Occupational Safety and Health (NIOSH), which implemented a grant programme to support occupational medicine residency training. Many programmes were developed in schools of medicine and were able to provide residency training with the aid of NIOSH grant support. Another reason for the growth of residency programmes is that the professional accreditation organization for occupational medicine in the United States aimed to increase the field’s stature by making completion of a formal training programme (rather than only experience working in the field), a requirement for certification as an occupational medicine specialist. Residency programmes were also established in response to reports by prestigious professional organizations, such as the Institute of Medicine (IOM), documenting the severe shortage of qualified medical practitioners in the field of occupational and environmental medicine (IOM 1993). Many of the new residency programmes established clinics as training sites for the residency programmes. A large proportion of future specialists in the United States will receive their clinical training in the academic-based occupational and environmental medicine clinics.
Organizational Support for the Clinics
The academic-based clinics typically do not provide profitable, routine employee health services like those of the contract providers, so that institutional support has been essential in sustaining these programmes. Several governmental agencies have played an important role in supporting the clinics. As mentioned above, NIOSH has provided support for occupational medicine residency programmes; this support was supplied through the interdisciplinary Educational Resource Centre training consortiums and later through occupational medicine residency training grants. The National Institute for Environmental Health Sciences (NIEHS) has provided research and training support for academic occupational medicine programmes. Many of the most well-established clinics are affiliated with environmental health research centres supported by NIEHS. The clinics support the mission of the centres by identifying populations for clinical and epidemiological research. NIEHS also established the Environmental and Occupational Medicine Academic Award grant programme in the late 1980s to provide support to medical schools for faculty development in the field. This grant programme has now provided support to faculty in a substantial proportion of medical schools with academic-based clinics. The Agency for Toxic Substances and Disease Registry (ATSDR) which was established by the Comprehensive Environmental Response, Compensation, and Liability Act (Superfund) in 1980 to perform environmental health assessments and enhance professional training for evaluating hazardous substances has given essential support for programme development and related professional educational activities as many of the clinics have begun to address environmental as well as occupational health issues.
Several states have programmes to support occupational health services. The largest programme is the University of California Centres for Occupational and Environmental Health. These centres were established in five University campuses and include multidisciplinary research, training and clinical service programmes. Several other states (e.g., New Jersey, Oregon, Michigan and Washington) also support programmes through state schools of medicine or schools of public health. New York State created a statewide network of occupational and environmental health clinics, most of which are affiliated with academic medical centres. This network of clinics is able to evaluate persons with potential environmental or occupational medical problems even if they are not able to pay for these services. The clinics developed a common database system so that the network can serve as an occupational disease surveillance system for the state.
Professional associations have also provided critical support for the growth of academic clinics. Members of the American Public Health Association (APHA) provided an early focus for communication among the emerging clinics. The support of the APHA served to strengthen the public health and prevention orientation of the clinics. In 1987, members of the APHA occupational medicine clinic committee formed a new organization, the Association of Occupational and Environmental Clinics (AOEC), as a “network of clinical facilities dedicated to research and education, as well as the prevention and treatment of occupational and environmental diseases” (AOEC 1995). The AOEC has developed into a national network of more than 50 clinics, most of which are academic-based clinics. Most of the well-established academic-based clinics are members of the AOEC. The Association enhances communication among the clinics, establishes guidelines for quality of care and patient’s rights, seeks funding support for professional and educational activities and is developing a database system so that information from clinics can be systematically collected and analysed.
Programme Characteristics
As mentioned above, the clinics’ principal activity is to identify work-related and environmental diseases, rather than to provide routine employee health services. Because of this focus, the clinics are different from clinical programmes which provide employer-contracted services (Rosenstock 1982). Professionals in the academic clinics relate to potentially affected workers and community members as their primary clients, rather than the employers. The physicians participate in the medical, social, economic and legal aspects of patient problems. The patient-to-provider ratio is low: the clinics, focusing on relatively low-volume but complex medical cases call for longer and more thorough visits that engage the efforts of physician and patient beyond normal clinic hours.
Because of research and teaching responsibilities, the academic clinics usually are part-time, offering up to several sessions per week. A directory of 41 academic clinic members of the AOEC reported a range of one to 13 physicians per clinic, with 85% of the clinics having two to six physicians (AOEC 1995). Another characteristic is that the clinics use multidisciplinary teams of professionals to improve exposure and toxicity evaluation and to provide prevention and education services. For example, of 41 academic clinics in an AOEC directory, most had industrial hygienists (32), while approximately one-half had toxicologists (22), social workers (19) health educators (19) and epidemiologists (24) on the professional staff (AOEC 1995).
The clinics emphasize a community-oriented service perspective. Most clinics establish professional and community outreach programmes, both to establish a referral network for identifying patients and to provide education to health professionals, workers and community residents. Many clinics establish a worker and community advisory committee in order to provide oversight of clinic activities.
Many clinics maintain computer databases so that the experiences of the clinics can be retrieved and analysed. The databases include patient referral source, occupation and industry code of all jobs (or at least current and/or most important jobs), employer name, exposures, work-related diagnoses, assessment of link between exposures and diagnoses, and demographics (Rosenstock, Daniell and Barnhart 1992). So far data collected by the clinics has not been well coordinated, but the AOEC has developed a common database system so this information should be collected more systematically in the future.
Services
The mix of patients seen in academic clinics varies depending on types of employers and community hazards in the region, even more so than among the contract occupational services, which tend to develop in response to employer needs. The clinics may offer specialized diagnostic services depending on the expertise and research interests of the faculty. Patients may go to the clinics based on the expertise and reputation of the academic programme. A patient will usually present with either an actual disease, wanting to know if his or her job or an environmental exposure was responsible, or with a history of a potentially toxic exposure, wanting to know if adverse consequences will result from the exposure.
The most common occupational diagnoses seen in the clinics, as reported in a recent AOEC directory, were as follows (AOEC 1995): asthma, asbestos-related pulmonary diseases and other pulmonary conditions; carpal tunnel syndrome, repetitive strain, musculoskeletal conditions; and dermatological conditions. Few clinics reported neurological problems as a common diagnosis, and very few saw patients with acute injuries. The most common occupational exposure problems reported involved asbestos, lead or other heavy metals, chemicals and solvents.
The distribution of common environmental diagnoses was different from that typifying occupational problems. The most commonly reported diagnoses were determinations of multiple chemical sensitivity syndrome and “sick building syndrome”, or symptoms due to indoor air quality problems. The most common environmental exposure problems reported involved pesticides, lead, chemicals and hazardous waste in communities.
Patients are referred from a variety of sources—they may be self-referred or have been sent by employers, unions, public health agencies, physicians, lawyers and the workers’ compensation systems. Some referrals are made to the programmes because patients want an independent, high-quality medical assessment. Other referrals concern specific practitioners—often faculty members—who have recognized expertise. Choices leading to these latter referrals may be the outcome of a search that is national or even international in scope.
Academic clinics offer services in addition to evaluation of occupational and environmental diseases. Many clinics perform medical screenings for workers at the request of employers, unions or groups of workers who are concerned about a certain exposure, such as lead or asbestos. The clinics also provide medical surveillance examinations mandated by OSHA or state laws. Most clinics serve as regional resources by providing clinical consultations to workers, community residents and physicians, typically via telephone.
In addition to clinical services, the multidisciplinary staff of the academic clinics provide workplace and community hazard evaluations, sometimes including exposure monitoring. Virtually all of the clinics offer health education and prevention training for individuals, communities and health professionals.
The Future
The future of academic clinics in the United States may be affected by overall changes in the workers’ compensation and medical care systems. The need for independent medical evaluations of occupational and environmental problems will continue, but many states have implemented or are considering changes in workers’ compensation laws to restrict the freedom of workers independently to make their own choices regarding a medical evaluation. There is also a trend to integrate medical care for occupational and non-occupational conditions by a single managed care provider. The clinics will need to respond to the growth of managed care in the occupational health field because the independent approach used by these clinics may be largely excluded from a more managed workers’ compensation system.
To respond to these changes in the medical care system, some academic clinics are establishing affiliations with employer contracted programmes so that the clinics function as a speciality referral programme while the other programmes handle routine cases and medical treatment. Academic clinics may also need to establish affiliations with medical centres supplying primary care, urgent care, rehabilitation services and other specialities in order to lend greater comprehensiveness to the services that will be integrally provided by occupational health care and other medical care. This approach will be taken to increase financial stability through the use of contracts in addition to charging fees for service, and to provide training experiences for physicians, many of whom will practise in those settings.
The challenge for academic clinics will be to maintain their independent perspective while functioning in an integrated, managed care system largely financed by employers. The option of independent consultations will be maintained to some degree because of the regional and national referral patterns based on a clinic’s reputation. Clinical practitioners will also continue to provide expert consultations to individuals and lawyers under the tort system, which is also evolving in the United States, albeit more slowly than is the medical care system. However, even with these sources of support, academic clinics in the United States will continue to need support from governmental agencies and professional organizations to continue their role as independent sources of medical consultation, research and training. The future of many of the academic clinics will depend on whether the federal and state governments continue to support these programmes.
More...
Occupational Health Services in Japan
Policy and Legislation
In Japan, the sole administrative body of occupational health is the Ministry of Labour, and the core law is the Industrial Safety and Health Law enacted in 1972 (this law will be termed “the Health Law” for the purposes of this article). The Health Law and its enforcement orders specify the employer’s responsibility to provide occupational safety and health services, including the appointment of an occupational health physician (OP), according to the size of the workplace. It is a requirement that all workplaces employing 50 or more workers appoint an OP (a full-time OP for workplaces that employ 1,000 or more workers). In addition, all workplaces, regardless of employee number, are mandated to provide health examinations for their workers. The mandatory health examinations include pre-employment and periodic general health examinations for full-time workers and specific health examinations for full-time workers engaged in activity described as “harmful work”. Compliance with the above legal requirements is generally good, although a gradient in compliance rate exists according to workplace size.
Organization and Service Provision Models
Organization and service provision models vary considerably according to the size of the workplace. Large-scale workplaces often embody full-size occupational health units, such as a health administration department, a department of health promotion or a clinic/hospital on the premises. These functional units may take the form of independent institutions, especially if they emphasize curative activities, but many are units subordinate to departments such as the labour department or the general affairs department. In some cases, the occupational health unit is run by a corporate health insurance union. The full-time OP is very often appointed to a directorial position of the unit, sometimes nominally matching a managerial post within the corporate hierarchy. The co-medical staff may consist of a variable combination of general nurses, occupational health nurses and x-ray and/or medical technologists.
In contrast, many small-scale workplaces lack the human and facility resources to carry out occupational health functions. In this sector, part-time OPs are recruited from among private general practitioners, hospital- or university-affiliated physicians and independent or non-independent occupational health practitioners. The part-time OPs engage in a variable range of occupational health activities depending on the needs of the workplace and the physician’s expertise. An occupational health organization (OHO), which is defined as an organization delivering occupational health services on a profit-earning basis, have played an essential role in the provision of occupational health services to small-scale workplaces. Services purchasable from OHOs cover provision and follow-up of various health examinations, implementation of environmental measurements and even the dispatch of OPs and nurses. Many small-scale workplaces appoint a part-time OP and contract with an OHO to meet specific legal requirements imposed on the workplace.
Activities and Content
Nationwide questionnaire surveys focusing on the activities of full-time and part-time OPs have been conducted periodically by the Occupational Health Promotion Foundation, an auxiliary non-profit-making organization of the Ministry of Labour. According to the 1991 survey, to which 620 full-time OPs responded, average time allocation was longest for curative activities (495 hours/year) followed by periodic health examinations (136) and health consultations (107). Time allocation to workplace patrols averaged 26.5 hours/year. In the survey, 340 part-time OPs also responded; the average time allocated by part-time OPs was proportionately less than that of full-time OPs. However, a detailed observation reveals that the activities of part-time OPs vary widely in quantity and quality, depending on several inter-related factors:
- size and characteristics of the workplace
- main job and other appointments of the physician
- work commitment.
Personnel Resources
There are no legal provisions on the qualifications of the OP: simply stated, the OP (whether full-time or part-time) can be appointed “from among physicians” (the Health Law). As of 1995, the total number of physicians is estimated to be 225,000, with an annual increase of about 5,000 (i.e., an increase of 7,000 qualifying from graduates of 80 medical schools in Japan and a decrease of 2,000 due to death). The estimated number of OPs as of 1991 was about 34,000 (2,000 full-time and 32,000 part-time), which was equivalent to 16.6% of the total number of physicians (205,000). In addition, an estimated several thousand nurses across the nation play an active part in the field of occupational health, although there is no legal definition of an occupational health nurse. A health supervisor, which is defined by the Health Law as a person who takes charge of technical matters related to health, is recruited from among the workers. The OP interacts closely with the health supervisor, to whom the OP may “give guidance or advice” under the Health Law.
Administration
Within the Ministry of Labour, occupational health is administered directly by the Industrial Safety and Health Department, which is subordinate to the Labour Standards Bureau. The Bureau’s functional units at the local level include the Prefectural Labour Standards Offices (of which there are 47) and the Labour Standards Inspection Offices (there are 347 of these) distributed nationwide and staffed by a total of about 3,200 “Labour Standards Inspectors”, 390 “Industrial Safety Expert Officers” and 300 “Industrial Health Expert Officers”.
The Ministry of Labour has been implementing consecutive five-year plans for the prevention of industrial accidents; the most recent of these (the eighth) was associated with the slogan “realizing a healthier and safer working life on both mental and physical aspects”. Accordingly, the Ministry is pursuing a Total Health Promotion (THP) plan. Under the THP plan, the OP prescribes an exercise menu for each worker based on health measurement data. Training programmes accommodating company representatives are organized by the government to develop necessary skills. The government also gives recognition to OHOs that are capable of providing services related to THP implementation.
Financing Systems
When occupational health services are provided on the premises, as is the case in large-scale workplaces, they will often take the form of an intracorporate department and will thus be placed under the financial constraints of the employer. Another variation involves the presence of an affiliated but self-supporting unit (clinic, hospital or OHO) which employs an occupational health staff. In some cases, the unit is run by a corporate health insurance union. Many small-scale workplaces, lacking the human, facility and financial resources, but under the requirement to appoint a part-time OP, will often do so by contracting with general practitioners, hospital- or university-affiliated physicians and others. As stated previously, the part-time OP will engage in a variable range of occupational health activities depending on the needs of the workplace and the physician’s expertise. The requirements imposed on the workplace, such as provision of periodic health examinations to all employees, often exceed the time capacity and/or the willingness of the contracted physician. This creates a demand-supply gap which is often filled by OHOs.
Research
The Japan Society for Occupational Health (JSOH) is an academic society comprising OPs, occupational health nurses and researchers. Its present membership exceeds 6,000 and is increasing at a rapid rate. The JSOH holds annual scientific meetings at national and regional levels and recently started publishing an English scientific periodical entitled Journal of Occupational Health. Some core research institutes are the National Institute of Industrial Health (periodical: Industrial Health, biannual, English), the Institute for Science of Labour (periodical: Journal of Science of Labour, monthly, Japanese and English), the Japan Industrial Safety and Health Association (publications: Industrial Safety Yearbook and so on) and the Institute of the Industrial Ecological Sciences of the University of Occupational and Environmental Health, Japan (periodical: Journal of UOEH, bimonthly, Japanese and English).
Future Developments
The Ministry of Labour recently launched a comprehensive plan aimed at disease prevention and health promotion for the nation’s workers. It plans to establish government-subsidized occupational health centres (OHCs) at prefectural and regional levels throughout the country within an eight-year plan. Prefectural OHCs are planned to be established for each of the 47 prefectures, and each will be staffed by about 15 personnel, including one administrative full-time physician and three or four part-time physicians. Their primary function will be the provision of training and dissemination of information to OPs working within the vicinity. Regional OHCs are planned for 347 sites nationwide in affiliation with the local divisions of the Japan Medical Association (JMA). They will focus on providing occupational health services to the under-served sector, that is, workers in small-scale industries. The initial budget for the fiscal year 1993 was 2.3 billion yen ($US20 million) for the establishment of six prefectural and 50 regional OHCs. The prefectural and regional OHCs will function interactively as well as with the administration, the JMA, the workers’ hospitals and so on. Collaboration between these various institutions will be the key to the success of this plan.
Labour Protection in the Russian Federation: Law and Practice
The organization of labour protection that was inherited by the Russian Federation from previous times represented a hierarchical structure that had been built up under the former society and functioned under rigorous administrative control accompanied by planning and allocation of resources. Recent changes in the country’s economic and social systems caused by the transition to a market economy have necessitated both the revision of the existing labour legislation and the reorganization of the whole system of labour protection and particularly the provision of occupational health services to the working population.
Labour Legislation
Labour protection in Russia is recognized as a complex system for ensuring safe and healthy working conditions, which includes legal, socio-economic, organizational, preventive, safety, hygienic, technical and other measures.
Labour legislation in the Russian Federation comprises certain provisions of the Russian Constitution, the Labour Code, the Basic Law on Labour Protection, and enabling legislation, which consists of the relevant legal acts, regulations and directives, as well as guidelines, instructions, state standards and various standards approved by the appropriate authorities of the Russian Federation and those of the republics in the territory of Russia.
Article 37 of the Constitution of the Russian Federation stipulates that each citizen has the right to work in an environment that meets occupational safety and health requirements, to remuneration for work that is paid without any discrimination at a rate that is not less than the minimum established by the federal government, and to be protected from unemployment.
The Basic Law on Labour Protection, adopted in August 1993, contains provisions ensuring workers’ rights to protection of their health. It also regulates labour relations between employers and workers in all branches of the economy regardless of the forms of property. According to Article 4 of this Law, workers have the right to:
- safe and healthy working conditions
- workplaces that are protected against occupational hazards that may cause occupational accidents or diseases or decrease working capacity
- compensation for occupational injuries and occupational diseases
- information on existing occupational hazards and health risks and the measures undertaken by the employer to control them
- provision of personal protective equipment at the expense of the employer.
Article 9 of the Basic Law on Labour Protection makes management responsible for ensuring safe and healthy working conditions, while Article 16 specifies economic penalties for allowing unsafe and unhealthy working conditions, as well as for the impairment of workers’ health resulting from occupational exposures, injuries or diseases.
Chapter 10 of the Labour Code of the Russian Federation concerns occupational safety and health in industry. Article 139 stipulates the responsibility of management for the provision of safe and healthy working conditions through the introduction of up-to-date safety procedures and accident prevention measures that will ensure appropriate hazard control and the prevention of occupational accidents and diseases.
Article 143 of the Labour Code requires management to equip worksites with safe machinery and equipment and create safe working conditions in conformity with technical and hygienic standards as well as inter-industry and sectoral regulations on occupational safety and health that have been developed and adopted in accordance with the existing labour legislation.
The inter-industry occupational safety and health regulations cover all branches of industry. They consist of legal requirements applicable to all enterprises regardless of the types of their economic activity (e.g., hygienic norms SN 245-71 for the design of industrial enterprises). The inter-industry regulations are adopted by the Council of Ministries of the Russian Federation, or by other appropriate authorities if requested by the Council of Ministers.
The sectoral occupational safety and health regulations define requirements for diverse industrial processes, types of works and equipment specific for particular branches of industry (e.g., regulations on safety rules for welding operations in construction, or for the operation of loading cranes in dockworks). They take into account specific characteristics of particular branches of the economy and are adopted by respective ministries, state committees, state supervision bodies and other appropriate authorities.
Ministries also issue safety and health guidelines, instructions and technical standards for their respective fields of economic activities. Other instructions such as those that oblige employers to organize in-plant safety and health training for workers or those that oblige workers to comply with safety requirements are subject to consultations with employers’ and workers’ organizations.
Employers have the obligation to provide workers with proper clothing or uniforms and personal and collective protective equipment as specified by the regulations. They are also responsible for the organization of periodic health examinations for certain specific categories of workers, such as those doing heavy work or in hazardous occupations, transport workers and some others.
Along with the duties and responsibilities of the employers (when the state owns the property, the management of the enterprise represents the employer), labour legislation makes workers responsible for complying with the occupational safety and health requirements specified by relevant regulations and instructions. For example, they are required to participate in occupational safety and health training, properly maintain and use personal protective equipment, be trained in fire prevention, maintain the machinery and equipment they use and keep their workplaces clean.
At the enterprise level, everyday supervision of occupational safety and health standards and requirements is the responsibility of the occupational safety and health bureau, which is an integral unit of the enterprise, and enjoys an independent status. Its main functions include evaluation of occupational hazards, risk assessment, recommendation of safety and control measures, prevention of industrial accidents, analysis of the causes of occupational accidents, cooperation with other units of the enterprise in preventing work accidents and injuries, control of machinery and equipment and the implementation of safety programmes. The bureau has the authority to halt the operation of certain machinery or processes or the performance of jobs that may endanger workers’ life and health.
Small-scale enterprises are usually not in a position to organize an occupational safety and health bureau (see “Occupational health services in small-scale enterprises”). Article 8 of the Basic Law on Labour Protection gives them the right to consult external occupational safety and health specialists and to employ them on a contract basis.
In order to make the regulations covering the protection of workers in the Russian Federation more effective, there exists a system for establishing state standards on occupational safety and health (GOST). The state standards have the force of law and appropriate state authorities enforce their implementation.
In all, there are now more than 2,000 regulations, directives, instructions, hygienic norms and state standards on occupational safety and health, most of which had been developed by the various ministries, state committees and other authorities of the former USSR. These rules and regulations are still in effect, even though 700 had been established before 1981 and were intended to be applicable for a period of only five years. Most of them need reconsideration and modification in the light of the new economic situation.
As part of the reorganization of the system of labour protection in Russia, the Presidential Decree of 4 May 1994 created the Federal Labour Inspectorate (Rostrudinspekcija) under the Ministry of Labour and made it responsible for enforcing labour legislation in all territories of the Russian Federation. This established the system of state control and supervision in the field of labour protection. (Before this, the enforcement of labour legislation was the responsibility of trade union inspectors.) Regional Inspectorates with a networking structure are to be set up in all constituent regions of the Russian Federation to complete the organizational structure of the Federal Labour Inspectorate.
Health Legislation
Health legislation of the Russian Federation represents an instrument for the realization of the state policy on public health and epidemiological welfare. The Federal Hygienic and Epidemiological Service of the Russian Federation performs its activities in accordance with health legislation and plays an important role in activities aimed at the promotion of safety and health at work and public health in general.
Health legislation consists of the Hygienic and Epidemiological Welfare of the Population Act, adopted on 13 April 1992 by the Supreme Council of the Russian Federation, and of relevant directives and regulations adopted by respective competent authorities by virtue of this Act.
Article 1 of the Act defines the term hygienic and epidemiological welfare as “such a state of public health and the environment under which there is no hazardous influence of environmental factors on the health of the populations and there exist favourable conditions for creative activities.”
Health legislation establishes hygienic standards for enterprises, new types of machinery and equipment, and new technological processes and materials. It also stipulates the enforcement of existing norms and standards.
State hygienic supervision has two forms:
- Preventive hygienic supervision includes the enforcement of hygienic standards in the design, construction and reconstruction of enterprises, introduction of new technologies, manufacturing of machinery and equipment, and monitoring the environment.
- Routine hygienic supervision involves regular surveillance of the working environment of the enterprises using hygienic methods of exposure monitoring, sampling and analysis. It also includes control of the application of hygienic standards in the operation of machinery and equipment and the maintenance of the enterprise in general.
Article 9 of the Act requires enterprises to comply with health legislation by complying with established hygienic standards and by exercising control over their industrial environment. They are required to prevent environmental pollution and to develop and implement safety and health programmes that are aimed at the improvement of the working environment and the prevention of work accidents and injuries.
Chapter 4 of the Act determines the various degrees of liability for infringement of the Russian health legislation. Persons responsible for breaking the law may be prosecuted either under civil or criminal law (Article 27) of the Russian Federation.
Chapter 5 of the Act stipulates functions of the state hygienic and epidemiological supervision. It includes:
- assessment and prognosis of environmental health for the public
- identification of occurrences of communicable diseases, wide-spread non-communicable diseases and poisonings, and their causes
- development of mandatory measures to ensure hygienic and epidemiological welfare of the population
- supervision of the compliance of enterprises with health legislation and hygienic standards
- prosecution of organizations and persons for non-compliance with health legislation and hygienic standards
- compiling statistics on communicable diseases, occupational diseases, widespread non-communicable diseases and poisonings resulting from adverse environmental factors.
As a result of the structural changes taking place in employment patterns, the Act, for the first time, places obligation for the observance of health legislation, hygienic standards, hygienic quality of products and the prevention of environmental pollution not only on management and workers but also on self-employed persons who are involved in full-time employment (Article 34).
According to Article 32 of the Act, the Federal Hygienic and Epidemiological Service of the Russian Federation is assigned responsibility for enforcement of the health legislation. In addition, the Council of Ministers of the Russian Federation approved Directive No. 375, which reorganized the former hygienic and epidemiological stations into Centres for State Hygienic and Epidemiological Supervision (CSHES), operating in all territories of the Russian Federation.
The new health legislation is a crucial development in the legal regulation of the hygienic and epidemiological welfare of the population, as is the radical restructuring of the Federal Hygienic and Epidemiological Service of the Russian Federation to implement it. The Service has recently received the status of a Federal Service and is now included in the federal bodies of state control. As a result, the Federal Committee of the Russian Federation for Hygienic and Epidemiological Supervision has been established to provide overall supervision of this Service.
The Federal Hygienic and Epidemiological Service of the Russian Federation is made up of the following bodies:
- The Federal Committee of the Russian Federation for Hygienic and Epidemiological Supervision
- Centres for State Hygienic and Epidemiological Supervision (CSHES) at the republic, regional, municipal, district and local levels
- linear CSHES in water and air transport
- Information and Analytical Centre of the Russian Federation
- medical institutes and specialized training centres for the education and training of specialists to staff the CSHES
- research institutes specializing in occupational hygiene and epidemiology
- specialized medical establishments producing vaccines
- disinfection centres.
As defined in Directive No. 375, the main functions of the Federal Hygienic and Epidemiological Service include:
- enforcement of health legislation
- development of hygienic norms and standards
- elaboration of federal, republic, regional and local programmes for health protection and health promotion
- provision of technical information to appropriate authorities, enterprises, employers’ and workers’ organizations and other institutions involved in occupational safety and health activities, including information about hygienic and epidemiological conditions in the country, statistics on population morbidity and interpretation of legal documents relating to health legislation
- coordination of the activities of enterprises, employers’ and workers’ organizations, scientific associations and other institutions and organizations with respect to both the development and implementation of hygienic standards.
CSHES specialists have the right to visit and inspect enterprises in order to enforce health legislation. They investigate causes of occupational diseases and identify potential environmental and occupational hazards that may give rise to work-related diseases, injuries and poisonings. Ideally, where necessary, they cooperate with the occupational physicians and nurses staffing the occupational health services.
CSHES funds are provided directly from the federal budget of the Russian Federation. In addition, the CSHES may provide specialized services and advice under contract to enterprises and any others who may need their expertise. The list of specialized services provided by CSHES is approved by the Federal Committee for Hygienic and Epidemiological Supervision.
Health legislation is enforced through the application of relevant directives, regulations, instructions, norms and standards and legal requirements. These include:
- hygienic regulations, hygienic standards and requirements intended to create safe and healthy working conditions, protect the environment and promote public health in general
- hygienic standards establishing occupational exposure limits and maximum permissible levels for potential hazards encountered in workplaces and the environment
- hygienic norms establishing criteria for specific factors that may affect the health of future generations
- uniform hygienic regulations that combine different norms and standards.
Protection of workers’ health
Article 41 of the Constitution of the Russian Federation states that each citizen has the right to health protection and medical care. New legal acts provide for the development of municipal and private health care systems to supplement the state health care system. Health care in the state and municipal medical settings is provided without charge to patients, the costs being met by federal and local budgetary funds, health insurance funds and other sources.
The Hygienic and Epidemiological Welfare of the Population Act includes the following provisions aimed at the protection of workers’ health:
- Workers at enterprises shall undergo pre-placement and periodic health examinations.
- Pre-placement and periodic health examinations shall be required for all workers exposed to specific occupational hazards and hazardous types of work included in a list approved by the Federal Committee for Hygienic and Epidemiological Supervision and the Ministry of Health of the Russian Federation in consultation with representative organizations of employers and workers.
- Enterprises shall undertake all necessary measures to provide health examinations for workers.
A feature of the country’s health care system is the introduction, in 1991, of compulsory health insurance, which was amended in 1993. The Health Insurance of the Citizens of the Russian Federation Law encompasses a new insurance model under which employers contribute premiums amounting to 3.6% of their total payrolls to local administrations to meet health insurance needs. In 1996, about 40 million workers were covered by the Federal Compulsory Health Insurance Fund of the Russian Federation.
The main aim of the introduction of the compulsory health insurance was to ensure the financing of health care in the post-Soviet economic system based on insurance principles, using funds contributed through compulsory and voluntary dues. Compulsory health insurance introduced two types of public relationships into the health care system of the Russian Federation that had not existed before: the involvement of insurers, represented by local authorities that are responsible for the health insurance covering public employees and the unemployed; and the involvement of industrial insurers represented by the employers and enterprises that are responsible for the coverage of workers. According to Article 23, Health and Epidemiological Welfare of the Population Act health examinations of workers are included in the list of services covered by the compulsory health insurance.
In accordance with the Basic Law on the Health Protection of the Citizens of the Russian Federation, adopted by the Supreme Council of the Russian Federation on 22 July 1993, the basic principles of health protection are:
- observance of human rights in the field of health protection that are guaranteed by the government
- priority of prevention in health protection
- universal access to social and medical care
- social protection of workers in case of disability
- responsibility of the state, appropriate authorities, enterprises regardless of their forms of property, and the management of institutions and organizations for the protection and promotion of workers’ health.
The Basic Law specifies the relationships with respect to health protection and health promotion between the working population and the appropriate authorities, state enterprises, private sector establishments, and the state, municipal and private medical settings providing health care services.
In practice, occupational health services are provided to workers by public health care settings (hospitals and polyclinics) that are located near their residences, and by the specialized occupational health services located for the most part in large enterprises. The objective of this arrangement is to bring qualified health care services as close as possible to the workers and their workplaces.
Occupational health services are normally organized at large enterprises employing over 4,000 workers and in chemical, petrochemical, mining and quarrying industries with over 2,000 employees. An in-plant unit staffed by an occupational physician and an occupational nurse is required for all enterprises with more than 800 workers; those with 300 to 800 workers are required to have only an occupational nurse; the minimal number for enterprises with chemical, petrochemical, mining and quarrying operations is 200 employees. These in-plant units are part of the public health care system.
Small-scale enterprises rely for occupational health services on the hospitals and polyclinics of the public health care system, which are expected to provide an occupational physician to perform the health examinations of workers.
The occupational health service at very large enterprises usually includes a hospital providing inpatient services, a polyclinic providing outpatient services, occupational nursing services and a dispensary. Its services may be “closed” (i.e., limited to individuals working in the enterprise), or “open” (i.e., also providing services to workers’ families and, sometimes, to individuals living in the neighbourhood of the plant).
Conclusions
Significant transformations in Russia’s economic and social systems reflect the transition to a market economy, the appearance of various forms of property, the granting of economic independence to enterprises and the abolition of state administrative control, all of which have resulted in a great many changes in the society.
The system of labour protection in the Russian Federation described above, while preserving its general features, is still undergoing major reorganization to conform with changing realities and to be able to respond effectively to emerging issues. Although well under way, this process is also just beginning.
The provision of occupational health services to the working populations needs special attention because of the partial disintegration of the old network of occupational health services resulting from well-known economic problems, and also because of such innovations as the appearance of a private sector, the introduction of compulsory health insurance, and the integration of private medical settings into the country’s health care system.
Although some progress has been made in reducing the numbers of work accidents and the incidence of occupational injuries and diseases, the rates remain unacceptably high, which may have serious consequences in terms of the deterioration of workers’ health and its resultant impact on the economy. The improvement of working conditions and the working environment and the protection and promotion of workers’ health consequently command a high priority in revising the social policy of the state. Active participation of knowledgeable occupational safety and health professionals in this process is critical.
Some prerequisites for the improvement of the system of labour protection in Russia include:
- creation of economic stimuli for the improvement of working conditions and the working environment
- formulation of a coherent national policy on occupational health, occupational safety and the working environment
- revision of existing labour legislation and the establishment of a solid legislative basis for occupational safety and health practice
- effective enforcement of labour legislation
- wider cooperation of employers and workers on matters related to occupational safety and health
- authorizing state control bodies to close down enterprises with unsafe and unhealthy working conditions, as well as those polluting the environment
- emphasizing the improvement of working environment together with the protection of the general environment
- detailed analysis and prognosis of possible effects of the design and construction of new enterprises on workers’ health and the environment
- providing more options for workers in the procurement of occupational health services and increasing professional independence of occupational health professionals
- providing access to a “standard” package of health care services for all workers
- establishing comprehensive, multidisciplinary occupational health services at large-scale enterprises that are capable of providing a full range of services, including treatment and rehabilitation, to workers and their families
- upgrading the technical facilities of occupational health services and CSHES and enhancing the levels of the expertise of their staff
- organizing and deploying health centres to provide occupational health services for small-scale enterprises
- providing recommended types of health examinations to all workers, including workers in agriculture and the informal sector, through the most efficient use of various medical settings
- upgrading the education and training of occupational health professionals
- emphasizing workers’ education and training in occupational safety and health.
The Practice of Occupational Health Service in the People's Republic of China
China, the world’s largest developing country, is striving to accomplish unprecedented modernization. The “opening-up” policy to outside interests and the economic reform in effect since 1979 have brought profound changes to China’s economy and to every aspect of its society. The GNP increased from 358.8 billion yuan RMB in 1978 to 2,403.6 billion in 1992, an increase of more than three times in terms of constant money value. The average annual growth rate of GNP was 9.0%. The gross industrial output value was 3,706.6 billion in 1992, an average annual growth of 13.2% from 1979 to 1992 (National Statistics Bureau 1993). China is being increasingly regarded as a “potential centre of economic activity” and has attracted 40% of all of the direct foreign investment in the developing world. By the end of 1993, 174,000 foreign-funded projects had been approved, bringing US$63.9 billion into the country, and the total cumulatively pledged foreign input was $224 billion (China Daily 1994a, 1994b).
In order to advance current reforms in a comprehensive manner ensuring harmonious progress in all economic sectors, an in-depth reform decision has been made. The objective of this reform of the economic structure is to establish a socialist market economy that will further liberate and expand China’s productive forces. The centrally planned economy which has been favoured for 40 years is being transformed into a market system. Whatever the market can manage itself should be left to be controlled by the market. The government should guide the growth of the market by economic policies, regulations, planning and necessary administrative means.
During the period of rapid social change and industrialization, especially the transition from a centrally planned economic system to a market-oriented economy, great challenges had to be faced by China’s traditional occupational health service. At the same time, many new occupational health problems are continually emerging while older ones have not yet been solved.
Reviewing the history of over 40 years of development of occupational health in China, one can observe that great achievements have been made and many efforts have proved to be successful. However, there is still a big gap between the growing need for occupational health capabilities and the currently limited service capacity. Like many other aspects of Chinese life, occupational health service is undergoing a tremendous reform.
Historical Review
Occupational health service, as a subsystem of China’s public health services, was established in the early 1950s. In 1949, when the People’s Republic of China was founded, the health status of the Chinese people was poor. Life expectancy at birth was 35 years. The occupational safety and health status of workers presented an even worse picture. The prevalence of occupational diseases, communicable diseases and injuries among workers was high. Workers were generally prematurely withdrawn from their jobs. To counter the hazardous working conditions and poor sanitation left over in the factories of the “old China”, the new government took three measures (Zhu 1990): (1) the establishment of health service institutions in large-scale industrial enterprises; (2) an extensive investigation of sanitation and safety in the factories; and (3) the improvement of sanitary conditions at the workplace and of worker’s living facilities.
The statistical data relating to China’s oldest industrial bases showed that, by 1952, 28 factory hospitals, 795 clinics and 30 sanatoria had been established in eastern China; in the northeastern region, the level of medical and health services in industrial enterprises had increased 27.6%, the number of health workers increased 53.2% and the number of hospital beds increased 12%—all these improvements took place in the three-year period from 1950 through 1952. Most of the seriously unsafe working conditions found in state-run enterprises by governmental checkups were improved through the joint endeavours of government and workers’ participation. The government also gave financial support to the construction of housing and sanitary facilities. By 1952, workers’ housing had increased ten times compared to 1950, the number of bathroom facilities increased 216%, restrooms increased 844% and workers’ clubs increased 207% (from the northeastern region statistics). Nutrition subsidies have been given to workers exposed to occupational hazards since 1950. These developments greatly promoted the resumption of industrial production at the time.
Since 1954, following Chairman Mao Ze-dong’s call for “approaching a socialist industrialized nation step by step”, China speeded up its industrial development. The government’s priorities for workers’ health started to be transferred from sanitation to occupational and environmental health and concentrated on the prevention and control of serious occupational diseases and injuries. The first Constitution of the People’s Republic of China stipulated that labourers should enjoy the right of protection by government and that the health and welfare of all labourers must be improved.
The central government—State Council—has paid great attention to the serious situation of occupational health problems. The First National Conference on Silica Dust Control in Working Environments was jointly convened by the Ministries of Public Health (MOPH) and Labour (MOL), and the All-China Federation of Trade Unions (ACFTU) in Beijing in 1954, just four years after the founding of the People’s Republic of China. The Second Conference on Silica Dust Control was convened five years later by the above-mentioned three agencies in conjunction with such industrial administration sectors as the Ministry of the Coal Industry and the Ministry of Constructive Material Manufacture, among others.
At the same time, heat stress, occupational poisoning, industrial noise injuries and other illnesses induced by physical factors as well as pesticide poisoning in agriculture were put on the agenda of occupational health. Through the active recommendations to the State Council expressed through the joint efforts of MOPH, MOL, ACFTU and the Ministry of Industrial Administration (MOIA), a series of decisions, policies and strategies to strengthen the occupational health programme have been made by the State Council, including those relating to labour insurance, health and safety requirements for working environments, medical care for occupational illnesses, health examinations for workers engaged in hazardous work, establishing “health inspection” systems, and also the large amount of financial support needed to improve working conditions.
Organizational Structure of Occupational Health Delivery
The occupational health service network in China was initially established in the 1950s and has gradually taken shape over forty years. It can be seen at different levels:
In-plant service
As early as 1957, MOPH (1957) published a Recommendation on Establishing and Staffing Medical and Health Institutions in Industrial Enterprises. The principles of the document were adopted as national standards in the Hygienic Standards for Design of Industrial Premises (MOPH 1979) (see table 1). There should be a health department or a health and safety department at the management level of the enterprise, which should also be under the supervision of the local public health authority of the government. A workers’ hospital affiliated with the department functions as a medical/health centre, which provides preventive and curative services, including health surveillance of workers for occupational safety and health purposes, evaluation of working capacity from the medical point of view and approval of sick leaves of workers. There are health care stations near the workshops, which, under the management of and with the technical support of the workers’ hospital, play an important role in first aid, occupational health education for workers, collection of health information of workers at the workplaces and supervision of occupational safety and health jointly with trade unions and safety engineering departments.
Table 1. Minimum requirements of an in-plant health facility
|
Size of enterprise (employees) |
In-plant health facility |
Floor space ( m2 ) |
Minimum requirement |
|
>5,000 |
Hospital* |
To meet the construction standard for Comprehensive Hospitals |
|
|
3,501–5,000 |
Clinic |
140–190 |
Waiting room, consulting room, therapy room, clinic and IH laboratory x-ray room and pharmacy |
|
2,001–3,500 |
Clinic |
110–150 |
(same as above) |
|
1,001–2,000 |
Clinic |
70–110 |
X-ray is not required |
|
300–1,000 |
Clinic |
30–0 |
X-ray and laboratory are not required |
* Industrial enterprises with more than 3,000 employees can establish an in-plant hospital if they have high-risk productive processes, are located at far distances from a city or are situated in mountain areas with poor transportation.
Administrative division-based occupational health delivery
Providing health service is one of the responsibilities of governments. In the early 1950s, to prevent and control serious communicable diseases and to improve environment health, Health and Epidemic Prevention Stations (HEPSs) were established in every administrative division from provinces down to counties. The functions of the HEPSs were expanded with the growing needs of society and economic development to include preventive medical services, which covered occupational health, environmental health, food hygiene, school health, radiation protection as well as control of communicable and some non-communicable diseases. With health legislation being emphasized, the HEPSs are authorized to enforce the public health regulations and standards promulgated by the state or local governments and to implement inspection. The HEPSs, especially those at the provincial level, also provide public health technical assistance and services to the community and are involved in in-service training and scientific research.
The industrialization drive in China in the 1950s and early 1960s greatly accelerated the development of the occupational health service programme, which became one of the biggest departments in the HEPS system. Most medium and small industrial enterprises which were not able to maintain in-plant occupational health and industrial hygiene services could be covered by the HEPSs occupational health services, most of which were free of charge.
During the “Cultural Revolution” from 1966 to 1976, the occupational health service network and its activities were seriously damaged. This is one of the important reasons why some occupational diseases are still seriously prevalent in China. The reconstruction of the occupational health programme started in the late 1970s, when China began to realize once again the importance of economic development. Since the beginning of the 1980s, hospitals for occupational disease prevention and treatment and institutes of occupational health, called occupational health institutions (OHIs) have rapidly been established in most provinces and some industrial administrative sectors under the favourable policy of the government. OHIs were formed mainly on the basis of utilizing occupational health personnel in HEPS integrated with occupational physicians from hospitals. During the period 1983 to 1991, the central and local governments invested 33.8 million yuan RMB in total to support building OHIs. At provincial and prefecture levels, 138 OHIs were set up, with appropriate laboratory or clinical equipment. At present, the number of OHIs has reached 204, of which there are 60 established by the industrial sector. Another 110 million yuan RMB have been invested to equip 1,789 health and epidemic prevention stations at the county level (He 1993). The occupational health programmes in county HEPSs were one of the important parts of the project to be first equipped. To strengthen the national capacity of research, training and coordination of occupational health service, a National Centre for Occupational Disease Prevention and Treatment (NCODPT) was set up in the Institute of Occupational Medicine, Chinese Academy of Preventive Medicine (IOM/CAPM), and seven regional centres of occupational health, located in Beijing, Shanghai, Shenyang, Lanzhou, Chengdu, Changsa and Guangzhou, were also established. The current national network of occupational health services is illustrated in figure 1.
Figure 1. National network of occupational health services
So far, 34 schools or departments of public health have been established in the medical colleges or medical universities. These are the main resources of occupational health personnel. Six national occupational health in-service training centres were established in 1983. The total professional occupational health personnel, including physicians, industrial hygienists, technicians in laboratories and other health workers involved in occupational health programmes, reached about 30,000 in 1992.
Occupational Health Standards and Legislation.
To encourage research in hygienic standards and in their establishment, a National Technical Committee of Hygienic Standards (NTCHS) was set up in 1981 as a consultative and technical reviewing agency of MOPH in hygienic standard setting. At present, NTCHS has eight subcommittees, which are responsible for occupational health, environmental health, school hygiene, food hygiene, radiation protection, occupational disease diagnosis, communicable disease and endemic disease prevention (figure 2). The members of NTCHS are experts from universities, research institutes, governmental agencies and the trade unions. The Hygienic Standards for Design of Industrial Premises (HSDIP) was first formulated in the 1950s and revised and promulgated again in 1979, so that it now contains a list of occupational exposure limits in terms of maximum allowable concentrations (MACs) for 120 toxic agents and dusts, and other requirements for hazards control measures in workplaces, sanitary and health facilities in plants and so forth. Also, there were 50 occupational hygienic standards for hazardous chemical and physical agents in the workplace promulgated by the Ministry of Public Health. Another 127 occupational hygienic standards are being reviewed. Diagnostic criteria for 50 compensable occupational diseases were issued by the Ministry of Public Health.
Figure 2. The management of health standard setting
As is known to all, China has had a centrally planned economic system and has been a country controlled by a unified central government for more than 40 years. So, most regulatory requirements in occupational safety and health at the national level were stipulated in the form of “Red Title” documents of the central government. These documents had, indeed, the highest legal effect and have constituted the basic regulatory framework of China’s occupational health. There are more than 20 documents of this kind promulgated by the State Council or its ministries. The major differences between these documents and legislation are that there are no stipulations for penalties in the documents, the compulsory effect is not as high as it is with laws and enforcement is weak.
Since economic reform has favoured the market-oriented system following the opening-up policy, national legislation has been greatly emphasized. Occupational health management is also being transformed from traditional administration to regulation-based approaches. One of the most important legal documents is the Regulation on Pneumoconioses Prevention and Control, issued by the State Council in 1987. Another milestone in protecting workers’ rights is the promulgation of the Labour Law by the National People’s Congress, with an anticipated effect date of 1 January 1995. The occupational safety and health of workers, as one of the major aims of this measure, is stipulated in the Law. To implement the Labour Law for occupational disease control, a draft law for occupational disease prevention and control was submitted to the Bureau of Legislation of the State Council by the Ministry of Public Health, in which most of the successful occupational health policies basic to occupational institutions, and experiences both in China and abroad. The draft must undergo further review and be submitted to the Standing Committee of the National People’s Congress.
Health Inspection System
“Putting prevention first” has been emphasized by the government and has become an important national basic public health principle. As early as 1954, when industrialization had just begun, the central government made the decision to establish a health inspection system to enforce the national health regulations and policies of industrial hygiene. HEPSs were authorized to implement health inspection on behalf of the public health authorities of the government. The main tasks of health inspection of enterprises include the following:
- to inspect the enterprise for hazard control in workplaces so that the concentrations/intensities of occupational hazards meet national industrial hygienic standards
- to check whether or not the pre-placement and periodic health examinations of exposed workers have been conducted in compliance with related national regulations or local governmental requirements
- to ensure that workers who are suffering from occupational diseases be properly treated, allowed to recuperate, transferred to other jobs or offered some other suitable option in line with related regulations
- to conduct hygienic evaluation and to supervise hazard control measures in workplaces
- to supervise occupational health record keeping, occupational disease reporting and working environmental monitoring in enterprises.
- The above activities are part of “regular health inspection” and are considered routine inspecting tasks that should be carried out periodically. To continue, the remaining chief tasks of health inspection are:
- preventive health inspection on industrial construction projects (prior to a new industrial construction or reconstruc-ting/expanding of old industrial enterprises, all engineering designs, hazard control facilities, medical/health and workers’ living facilities must pass an initial inspection for occupational health purposes)
- toxicological assessment of new industrial chemical substances.
Health inspection, especially preventive health inspection as a fundamental principle of public health intervention measures, has been stipulated in a number of laws and public health regulations. Since the 1970s, as great attention has been paid to the control of environmental pollution, preventive occupational health inspection has further been expanded to whole process inspection. The principle that “hazard control installations must be simultaneously designed, constructed and put into use/operation with the principal part of the project” was one of the important requirements in the Regulation on Pneumoconiosis Prevention and Control and the Environmental Protection Law.
Comprehensive Prevention Strategy for Occupational Diseases
Along the way to controlling pneumoconioses and serious dust contamination in the working environment, comprehensive prevention was emphasized, which was summed up in eight Chinese characters, and so called the “Eight Characters” strategy. The meanings are translated in English as follows:
- innovation: technological improvement, such as using safe or low-risk materials and more productive processes, and replacing outmoded productive methods by appropriate advanced techniques
- keep it wet: keeping a dusty worksite wet to decrease the concentration of dust, especially for drilling and grinding in mining industries
- enclosure: segregating workers, equipment and environmental areas to prevent the escape of dust and operators’ subsequent contamination
- ventilation: improving natural and mechanical ventilation
- protection: providing personal protection for exposed workers
- supervision: setting up regulations and safe operating rules, and supervising workers to ensure that they follow them strictly
- education: implementing health and safety education programmes to promote workers’ participation and enhance their awareness and skills with regard to personal protection
- checking up: inspecting the working environments to meet national standards and regularly examining the workers’ health in line with national requirements.
It has been proved by the practices of many enterprises that the “Eight Characters” strategy is important and effective in improving working conditions.
Environmental Monitoring in Workplaces
Enterprises with hazardous working environments should periodically monitor the concentrations or intensities of the hazards at worksites and take measures to control risks to meet national industrial hygienic standards (for example, with reference to values of MACs). If the enterprises are not able to conduct environmental monitoring by themselves, local OHIs or HEPSs can provide services.
To control the quality of workplace monitoring conducted by enterprises, OHIs or HEPSs must conduct inspection regularly or whenever necessary. NCODPT is responsible for the nationwide quality control of workplace hazard monitoring. A number of technical regulations for air monitoring in the workplace have been promulgated by MOPH or been published as national recommendations by NCODPT—for example, Methods for Airborne Dust Measurement in the Workplace (GB 5748–85) (MOPH 1985) and Methods for Monitoring and Analysis of Chemical Hazards in Air of Workplace (Institute of Occupational Medicine 1987).
To control further the quality of environmental monitoring in workplaces a set of quality assurance norms for measurement of hazardous substances in the working environment has been submitted to MOPH for further review and approval. The qualifications of institutions which undertake workplace monitoring would be reviewed and licensed, requiring:
- professional ability on the part of the person who takes the samples or engages in analytical work
- necessary equipment for sampling and analysis and their proper calibration
- reagents and standard solutions
- quality assurances for air and biological material sampling
- inter-laboratory quality assurances and similar checks.
At present, a pilot study on assessment of the laboratories is being conducting in 200 laboratories or institutions. This is the first step to implement the Quality Assurance Norm.
Health Examinations of Workers
Workers exposed to occupational hazards in workplaces should have occupational health examinations. This was first required for workers exposed to dust in the 1950s. It quickly expanded to cover workers exposed to toxic chemicals and physical hazards.
The health examinations include a pre-employment or fitness-to-work examination and periodic examinations. These medical examinations must be carried out by OHIs or competent medical/health institutions licensed by government public health administrations.
Pre-employment examination
A pre-employment examination is required for new workers or workers newly transferred to hazardous workplaces. The medical examinations focus on assessment of the health of workers in relation to the workplace conditions to ensure that the specific job they intend to hold will be of no damage to their health, and those who are not fit for a given job are excluded. Health criteria to determine job contraindications for different hazardous work conditions have been stipulated in detail in the National Diagnostic Criteria and Principles of Management of Occupational Diseases (Health Standards Office 1993) and Guideline of Occupational Health Service and Inspection promulgated by MOPH (1991b).
Periodic examination
Workers exposed to different hazards have different intervals of medical examinations. The period of examination for workers exposed to dust, for example, is illustrated in table 2. Workers suffering from pneumoconioses should have annual physical examinations.
Table 2. Periodic examination requirement for workers exposed to dust
|
Nature of dust |
Examination intervals (years) |
|
|
Workers in service |
Workers withdrawn |
|
|
Free silica content (%) |
||
|
80 |
0.5–1 |
1 |
|
40 |
1–2 |
2 |
|
10 |
2–3 |
3 |
|
10 |
3–5 |
5 |
|
Asbestos |
0.5–1 |
1 |
|
Other dust |
3–5 |
5 |
All medical records should be well secured both in enterprises and in local OHIs, and should be reported annually to the local government public health authority, and then to the NCODPT and the MOPH.
When anyone transfers to an enterprise from a plant involving risks of hazardous exposure, a health examination must be given by a local OHI to clarify whether his or her health has been damaged by exposure, and the health records must be sent to the new enterprise with the worker (MOPH 1987).
Table 3 shows the statistics of workers’ health examinations in the period 1988-1993. A total of 64 million workers were covered by the network of the occupational health service, which included state-owned and city collective-owned enterprises, and a part of rural industries at the township level. The workers exposed to occupational hazards account for 30% of the total workers. Nearly 4 million exposed workers, about 20% of the total, had medical examinations every year. In 1993, for example, the total number of the industrial population was 64,345,193, according to the report from the National Centre of Occupational Health Reporting (NCOHR 1994) (there was, however, a lack of data from Neimeng, Tibet and Taiwan). The proportion of workers exposed to occupational hazards accounted for 31.28% (20,126,929), of which 3,982,940 were examined, accounting for 19.79%. The total rate of detected compensable occupational diseases was 0.46% in 1993 (MOPH 1994).
Table 3. Physical examinations for workers exposed to occupational hazards
|
Year |
Number of |
Proportion of |
Examination rate |
Detected rate of |
|
1988 |
62,680 |
29.36 |
18.60 |
0.90 |
|
1989 |
62,791 |
29.92 |
20.67 |
0.57 |
|
1990 |
65,414 |
29.55 |
20.47 |
0.50 |
|
1991 |
66,039 |
30.30 |
21.03 |
0.57 |
|
1992 |
64,222 |
30.63 |
20.96 |
0.40 |
|
1993 |
64,345 |
31.28 |
17.97 |
0.46 |
The Management of Occupational Diseases
Compensable occupational diseases
Generally speaking, any illnesses caused by exposure to hazardous factors present in the workplace or resulting from processes of production is considered an occupational disease. However, for compensation purposes, a list of occupational diseases has been issued by the MOPH, the MOL, the Ministry of Finance and the ACFTU (MOPH 1987). The list covers nine categories, including pneumoconioses; acute and chronic occupational poisonings; diseases induced by physical factors; occupational communicable diseases; occupational dermatoses; occupational eye impairments; occupational ear, nose and throat diseases; and occupational tumours. The total is 99 diseases. If any other disease is proposed by local governments or governmental sectors to supplement the list, it should be submitted to the MOPH for approval.
Diagnosis of compensable occupational diseases
According to stipulations of the Administrative Rule of Occupational Disease Diagnosis issued by the MOPH, at the provincial and prefecture levels, compensable occupational diseases must be diagnosed by OHIs or by medical/health institutions licensed by the public health departments of local governments. In order to control the quality of diagnosis and to provide technical assistance for confirmation of complicated cases and adjudications of diagnostic disputes, expert committees on occupational disease diagnosis have been established at the national, provincial and prefecture/municipal levels (figure 3) (MOPH 1984).
Figure 3. The management of occupational disease diagnosis in China
The National Committee on Occupational Disease Diagnosis (NCODD) consists of five subcommittees concerned with occupational poisoning, pneumoconiosis, physical factor-induced occupational disease, radiation sickness and pneumoconiosis pathology, respectively. The headquarters of the Committee is in the Department of Inspection of the MOPH. The executive office of the NCODD is in the IOM/CAPM. All members of the Committee were appointed by the MOPH.
Diagnostic Criteria of occupational illnesses are promulgated by the MOPH. There are such criteria for 66 occupational diseases in effect right now. For other compensable occupational diseases without national diagnostic criteria, the provincial public health departments could formulate temporary diagnostic criteria to be put into effect in their own provinces after being submitted to the MOPH for the records.
According to the Diagnostic Criteria, the diagnosis of occupational disease must be based on the following sorts of evidence: a history of exposure, clinical symptoms and signs, laboratory findings and results of working environmental monitoring, and reasonable exclusion of other diseases. Once the diagnosis is made, an Occupational Disease Certification (ODC) must be issued by the OHI. Three copies of the ODC should be sent: one to the worker, one to the enterprise for proper compensation arrangements and one should be kept in the OHI for further medical treatment and working capacity evaluation.
Management of occupational disease patients
Compensation and other welfare for patients suffering from occupational diseases must be provided by the enterprises according to the Labour Insurance Regulations (LIR). The management, labour union and committee of working capacity evaluation in the enterprise must jointly take part in the discussion and decision on proper treatment and compensation for the patients based on the ODC and the degree of working capacity loss. For those who are proved to be not suitable for doing their original jobs after the completion of proper medical treatment, the enterprise should transfer them to other worksites or make proper employment arrangements according to their health conditions within two months, and for special cases, at the latest in six months. When a worker suffering from occupational disease moves to another enterprise, his or her occupational disease benefits should be borne by the original enterprise where the occupational disease was caused, or shared by both enterprises after they have come to an agreement. All the health records, the ODC and other information relating to the health care of the worker must be transferred to the new enterprise from the original one, and the transfer should be reported by both enterprises to their local OHIs for record-keeping and further follow-up purposes.
If the diagnosis of an occupational disease is made after the worker has moved to a new enterprise, all the compensation or benefits should be paid by the new enterprise where the worker is currently working, regardless of whether or not the affliction is connected with the present working conditions. For a contracted worker or temporarily employed worker, if the occupational disease is diagnosed during unemployed periods and there is evidence proving exposure to related hazardous working environments when he or she was hired by any enterprise, the compensation and medical care should be paid by the enterprise (MOPH 1987).
Achievements in Occupational Disease Prevention and Control
Improvement of working environments
The concentration or intensity of occupational hazards in the workplace has declined significantly. The statistics of working environmental monitoring as supplied from the NCOHR showed that the proportion of worksites in compliance with national standards has increased 15% from 1986 to 1993 (NCOHR 1994). This is particularly true for state-owned and urban collective-owned industrial enterprises, of whose working environments nearly 70% had met the national standards. The situation in rural industrial enterprises is also improving. The compliance rate for occupational hazards increased from 42.5% in 1986 to 54.8% in 1993 (table 4). It is important to note that the estimation of the compliance rates of township industries might be higher than the actual situation, because this routine report can cover only about 15% of the rural industries every year, and most of them are located near cities which have well-developed health service facilities.
Table 4. Results of environmental monitoring for hazards in the workplace
|
Year* |
State-owned industry |
Rural industry |
||
|
No. of environmental locales monitored |
Proportion of locales up to standards (%) |
No. of environmental locales monitored |
Proportion of locales up to standards (%) |
|
|
1986 |
417,395 |
51.40 |
53,798 |
42.50 |
|
1987 |
458,898 |
57.20 |
50,348 |
42.60 |
|
1988 |
566,465 |
55.40 |
68,739 |
38.50 |
|
1989 |
614,428 |
63.10 |
74,989 |
53.50 |
|
1990 |
606,519 |
66.40 |
75,398 |
50.30 |
|
1991 |
668,373 |
68.45 |
68,344 |
54.00 |
|
1992 |
646,452 |
69.50 |
89,462 |
54.90 |
|
1993 |
611,049 |
67.50 |
104,035 |
54.80 |
* Exclusive of data from 1988: Yunnan, Xinjiang; 1989: Tibet, Taiwan; 1990: Tibet, Taiwan; 1991: Tibet, Taiwan; 1992: Tibet, Taiwan; 1993: Neimeng, Tibet, Taiwan.
The prevalence of some serious occupational diseases andthe implementation of comprehensive preventive measures
The national occupational health report data indicated that the prevalence of compensable occupational diseases maintained itself at a rate of 0.4 to 0.6%, although industries developed very quickly in recent years. Silicosis, for example, has been controlled for years in some large state-owned industrial or mining enterprises. Tables 5 and 6illustrate the success of Yiao Gang Xian Tungsten Mine and Anshan Steel Company in controlling silicosis (Zhu 1990).
Table 5. Dust exposure and prevalences of silicosis in Yiao Gang Xian Tungsten Mine
|
Year |
Dust concentrations ( mg/m3 ) |
Detected rates of silicosis (%) |
|
1956 |
66 |
25.8 |
|
1960 |
3.5 |
18.6 |
|
1965 |
2.7 |
2.6 |
|
1970 |
5.1 |
0.3 |
|
1975 |
1.6 |
1.2 |
|
1980 |
0.7 |
2.1 |
|
1983 |
1.1 |
1.6 |
Table 6. Detection rate of silicosis in Anshan Steel Company
|
Year |
No. of examinations |
Cases |
Rate (%) |
Compliance rate of dust (%) |
|
1950s |
6,980 |
1,269 |
18.21 |
23.60 |
|
1960s |
48,929 |
1,454 |
2.97 |
29.70 |
|
1970s |
79,422 |
863 |
1.08 |
28.70 |
|
1980s |
33,786 |
420 |
1.24 |
64.10 |
The nationwide epidemiological survey of pneumoconiosis in 1987-90 has also shown that the average working time of patients from their first exposure to silica dust to the appearance of signs of pneumoconiosis had been significantly prolonged, from 9.54 years in the 1950s to 26.25 years in the 1980s for those with silicosis, and 16.24 years to 24.72 years for those with coal worker’s pneumoconiosis in the same period of time. The average age of patients suffering from silicosis at death had also been increased from 36.64 years to 60.64, and for patients with coal pneumoconiosis from 44.80 years to 61.43 years (MOPH 1992). These improvements could be partly attributed to the successful occupational health policies and interventions of governmental policies as well as to the great efforts of occupational health professionals.
Promoting occupational health programmes in small-scale industries
Facing the continuing rapid development of small-scale industries, especially of township industries, and the growing gap between occupational health services and practical needs, the Ministry of Public Health decided to conduct a further comprehensive intervention field study. This study is important not only for helping to solve occupational health problems in rural industries, but also for exploring approaches to reform the occupational health service system in state-owned enterprises in order to match the changing requirements of the market economic system that is being established. Therefore, in December 1992, the Expert Group for the Field Study of Occupational Health Service Policies for Small-scale Industries was set up in the Department of Health Inspection, Ministry of Public Health. The Group was formed to support provinces in developing occupational health service programmes and approaches to effective intervention in hazardous situations. As the first step, the Group has drafted a “Recommended National Field Study Program” for provincial governments, which was approved and issued by the MOPH in 1992. The primary strategy of the programme is described as follows:
The enterprise, the provider of occupational health and the local government are the three key parts of the programme. The programme focuses on readjusting the relationship among the three parts to establish a new model of development. The basic objectives of the programme are to strengthen the regulatory control of government, to change the attitudes to health and the behaviours of the productive and operation functions of enterprises and to enlarge the coverage of minimum occupational health service while improving working conditions with appropriate technological measures (figure 4). Four counties (or districts) have been selected by the MOPH as national trial areas prior to the nationwide implementation of the programme, which include the Zhangdian district in Zibo municipality, Shandong province; the Baoshan District in Shanghai municipality; Jinhua County in Zhejiang province; and the Yuhong District in Shenyang municipality, Liaoning province.
Figure 4. The strategy of the pilot study on OHS in township enterprises
Seven spheres of policy interventions have been emphasized in the programme:
- strengthening the supervision and inspection provided by local governments of the occupational health of small-scale industries
- exploring how to integrate occupational health services for rural industries, with the goal “Health for All by the Year 2000” in China
- improving grass roots health organization networks to deliver occupational health services, management and supervision to the enterprises
- exploring practical approaches to enforce and implement occupational health inspection and service for township enterprises
- searching for and recommending appropriate technology for hazard control and personal protection for township enterprises
- implementing occupational health education programmes in township industries
- developing occupational health manpower and improving occupational health service working conditions to strengthen the occupational health service network, especially at the township and county levels.
Some preliminary results have been obtained in these four trial areas, and the basic ideas of the programme are being introduced to other areas in China and was scheduled for final evaluation in 1996.
The author thanks Prof. F. S. He for her assistance in reviewing this article.
Occupational Safety and Health in the Czech Republic
Geopolitical Background
The predominant development of heavy industry (the iron and steel industry, smelting and refinery plants), metalworking and machinery industries, and the emphasis on the production of energy in Central and Eastern Europe, have significantly predetermined the structure of the economies in the region for the last four decades. This state of affairs has resulted in the relatively high exposures to certain types of occupational hazards in the workplace. Current efforts to transform the existing economies along the lines of the market economy model and to improve occupational safety and health have been considerably successful so far, given the short period of time for such an endeavour.
Until recently, ensuring the prevention of adverse health effects of chemicals present in occupational settings and in the environment, the drinking water and the food basket of the population was provided for by the compulsory observance of hygienic and sanitary standards and occupational exposure limits such as Maximum Allowable Concentrations (MACs), Threshold Limit Values (TLVs) and Acceptable Daily Intake (ADI). The principles of toxicity testing and exposure evaluation recommended by various international organizations, including standards applied in the countries of the European Union, will become more and more compatible with those used in the Central and Eastern European countries as the latter gradually integrate with other European economies.
During the 1980s the need was increasingly recognized to harmonize the methodologies and scientific approaches in the field of toxicology and hygienic standardization applied in the OECD countries with those used in the member countries of the Council of Mutual Economic Assistance (CMEA). This was mainly due to growing levels of production and trade, including industrial and agricultural chemicals. A contributing factor favouring the urgency with which these considerations were viewed was a growing problem of air and river pollution across national boundaries in Europe (Bencko and Ungváry 1994).
The Eastern and Central European economic model was based on a centrally planned economic policy oriented to the development of basic metal industries and the energy sector. As of 1994, except for minor changes, the economies of the Russian Federation, Ukraine, Belarus, Poland, and the Czech and the Slovak Republics had preserved their old structures (Pokrovsky 1993).
Coal mining is a widely developed industry in the Czech Republic. At the same time, black coal mining (e.g., in the northern Moravian region of the Czech Republic) is a cause of 67% of all new cases of pneumoconioses in the country. Brown coal is extracted in opencast mines in northern Bohemia, southern Silesia and neighbouring parts of Germany. Thermal power stations, chemical plants and brown coal mining heavily contributed to the environmental pollution of this region, forming the so-called “black” or “dirty triangle” of Europe. Uncontrolled use of pesticides and fertilizers in agriculture was not exceptional (Czech and Slovak Federal Republic 1991b).
The labour force of the Czech Republic numbers some 5 million employees. About 405,500 workers (that is, 8.1% of the working population) are involved in hazardous operations (Ministry of Health of the Czech Republic 1992). Figure 1 presents data on the number of workers exposed to different occupational hazards and the proportion of women among them.
Figure 1. Number of workers in the Czech Republic exposed to the most serious occupational risks
Changing Needs
The occupational health system of the Czech Republic underwent three consecutive stages in its development and was influenced by the political and economic changes in the country (Pelclová, Weinstein and Vejlupková 1994).
Stage 1: 1932-48. This period was marked by the foundation of the first Department of Occupational Medicine by Professor J. Teisinger at the oldest university in Central Europe—Charles University (founded in 1348). Later, in 1953, this department became the Clinic of Occupational Medicine, with 27 beds. Professor Teisinger also founded the Research Institute of Occupational Health and in 1962 the Poison Information Centre at the Clinic. He was granted several international awards, including an award from the American Association of Industrial Hygienists in 1972 for his personal contribution to occupational health development.
Stage 2: 1949-88. This period exhibited numerous inconsistencies, in some respects being marked by notable deficiencies and in others showing distinct advantages. It was recognized that the existing system of occupational health, in many ways reliable and well developed, nevertheless had to be reorganized. Health care was considered as a basic civil right guaranteed by the Constitution. The six basic principles of the health system (Czech and Slovak Federal Republic 1991a) were:
- planned integration of health care into the society
- promotion of a healthy lifestyle
- scientific and technical development
- prevention of physical and mental illnesses
- free and universal access to health care services
- concern on the part of the state for a healthy environment.
Despite certain progress none of these goals had been fully achieved. Life expectancy (67 years for men and 76 years for women) is the shortest among the industrialized countries. There is a high mortality rate from cardiovascular diseases and cancer. About 26% of adult Czechs are obese and 44% of them have cholesterol levels above 250 mg/dl. The diet contains much animal fat and is low in fresh vegetables and fruits. Alcohol consumption is relatively high, and around 45% of adults smoke; smoking kills about 23,000 persons a year.
Medical care, dental care and medicines were provided free of charge. The numbers of physicians (36.6 per 10,000 inhabitants) and nurses (68.2 per 10,000) were among the highest in the world. But in the course of time the government became unable to cover the continually increasing and abundant expenses needed for public health. There had been temporary shortages of some drugs and equipment as well as difficulties in providing health care services and rehabilitation. The existing structure, which did not allow a patient to choose his primary health care physician, created many problems. Medical staff working in the state-run hospitals received low fixed salaries and had no incentives to provide more health care services. A private health care system did not exist. In hospitals, the main criterion of acceptable functioning was the “percentage of occupied beds” and not the quality of the health care provided.
However, there were positive features of the state-run centralized system of occupational health. One of them was an almost complete registration of hazardous workplaces and a well-organized system of hygienic control provided by the Hygienic Service. In-plant occupational health services established in large industrial enterprises facilitated the provision of comprehensive health care services, including periodic medical examinations and treatment of workers. Small private enterprises, which usually pose many problems to occupational health programmes, did not exist.
The situation was similar in agriculture, where there were no small private farms, but large-scale cooperative ones: an occupational physician working in a health centre of a factory or a cooperative farm provided occupational health services for the workers.
Enforcement of occupational safety and health legislation was sometimes contradictory. After an inspection of a hazardous workplace was carried out by an industrial hygienist or factory inspector, who had required the reduction of the level of occupational exposure and the enforcement of prescribed health and safety standards, rather than correct the hazards the workers would receive monetary compensation instead. Besides the fact that enterprises often took no action at all to improve working conditions, the workers themselves were not interested in improving their working conditions but opted to continue receiving bonuses in lieu of changes in the working environment. Furthermore, a worker who contracted an occupational disease received a substantial monetary recompense according to the severity of the disease and to the level of his or her previous salary. Such a situation produced conflicts of interests among industrial hygienists, occupational physicians, trade unions and enterprises. As many of the benefits were paid by the state and not by the enterprise, the latter often found it cheaper not to improve safety and health in the workplace.
Strange as it may seem, some hygienic standards, including permissible levels and occupational exposure limits, were more rigorous than those in the United States and in the western European countries. Thus, it was sometimes impossible not to exceed them with outdated machinery and equipment. Workplaces exceeding the limits were classified under “category 4”, or most hazardous, but for economic reasons manufacturing was not stopped and workers were offered compensatory benefits instead.
Stage 3: 1989–the present. The “velvet revolution” of 1989 enabled an inevitable change of the public health care system. The reorganization has been rather complex and sometimes difficult to accomplish: consider, for example, that the health care system has more beds in hospitals and doctors per 10,000 inhabitants than any industrialized country while it uses disproportionately less financial resources.
The Current Status of Occupational Safety and Health
The most frequent occupational hazard at the workplace in the Czech Republic is noise—about 65.8% of all workers at risk are exposed to this occupational hazard (Figure 8). The second major work-related hazard is fibrogenic dust, which represents an occupational hazard to about 21.3% of all workers at risk. Approximately 14.3% of workers are exposed to toxic chemicals. More than one thousand of these are exposed to toluene, carbon monoxide, lead, gasoline, benzene, xylene, organophosphorus compounds, cadmium, mercury, manganese, trichlorethylene, styrene, tetrachloroethylene, aniline and nitrobenzene. Another physical hazard—local hand-arm vibration—is a danger for 10.5% of all workers at risk. Other workers are exposed to chemical carcinogens, ionizing radiation and dangerous substances causing skin lesions.
The number of acknowledged cases of occupational disease in the Czech Republic in 1981-92 is presented in figure 2.
Figure 2. Occupational diseases in the Czech Republic in the period 1981-1992
The increase of morbidity from occupational diseases in 1990–91 had been due to the process of reclassification of occupational illnesses requested by miners and workers in other occupations and by their trade unions. They asked to change the status of “being endangered with an occupational disease”, used for less obvious forms of occupational impairment with low compensation, to fully compensated disease. The status of “endangerment” was reconsidered by the Ministry of Health in 1990 for the following kinds of occupational pathology:
- mild forms of pneumoconioses
- mild forms of chronic musculoskeletal disorders due to overload and vibration
- mild forms of occupational hearing loss.
Reclassification was done for all cases before 1990 and concerned 6,272 cases in 1990 and 3,222 cases in 1991 (figure 2). After that the status of “endangerment” was abolished. Figure 3 presents data on 3,406 new cases of occupational diseases by category diagnosed in the Czech Republic in 1992; 1,022 cases of these occupational diseases were diagnosed in women (Urban, Hamsova and Neecek 1993).
Figure 3. Occupational diseases in the Czech Republic in 1992
Some shortages in the supply of measuring equipment for sampling and analysis of toxic substances make it difficult to conduct occupational hygiene evaluations in the workplace. On the other hand, the use of biomarkers in exposure tests for the monitoring of workers in hazardous occupations is practised for a variety of dangerous substances according to the regulations of the Czech Republic. Similar tests have already been legally codified in Hungary, Slovakia, Slovenia, Croatia, Poland, and in some other countries of Central and Eastern Europe. The use of exposure tests for periodic medical examinations has proved to be a very efficient tool for personnel exposure monitoring. This practice has enabled early detection of some occupational diseases and permitted their prevention, thus decreasing compensation costs.
The transition to the market economy and the rising costs of health care services in the Czech Republic have had their influence on occupational health services. In the past, the in-plant based occupational health service or centre provided both health surveillance and treatment for workers. Nowadays, these activities are subjected to some restrictions. This has resulted in reduced activities in health surveillance and hazard control and in an increased number of occupational accidents and diseases. Workers in rapidly emerging small-scale enterprises, which often operate with unreliable machinery and equipment, are practically out of the reach of occupational health professionals.
Projects for the Future
A new system of public health in the Czech Republic is expected to incorporate the following principles:
- prevention and health promotion
- overall access to “standard” health care
- decentralized policy determining delivery of services
- integration of health services in a territorial network
- increased autonomy of health care professionals
- emphasis on outpatient care
- compulsory health insurance
- community participation
- more options for patients
- new public/private sector partnership to provide an “above standard” health care no longer offered by the public sector.
The introduction of the compulsory health insurance system and the creation of the General Health Insurance Office, which began operating in January 1993, as well as minor health insurance companies in the Czech Republic have marked the beginning of reform in the public health sector. These changes have brought some problems to the occupational health services, given their preventive character and the high cost of treatment in hospitals. Thus, the role of outpatient medical settings in treating patients with conventional as well as work-related diseases is steadily increasing.
The Potential Impact of Continuing Changes on Occupational Safety and Health
The growth of reform in the public health sector has created a need for change for occupational physicians, industrial hygienists and in-patient medical settings, and has also led to a focus on prevention. The ability to focus on prevention and milder forms of disease is partly explained by earlier positive results and by the relatively good functioning of the previous occupational health system, which had worked effectively towards eliminating major serious occupational diseases. The changes have involved a shift of attention from severe forms of occupational pathology that needed urgent treatment (such as industrial poisoning and pneumoconioses with respiratory and right-heart failure) to mild forms of disease. The change in the activities of the occupational health services from a curative orientation to early diagnosis now concerns such conditions as mild forms of pneumoconioses, farmer’s lung, chronic liver illnesses and chronic musculoskeletal disorders due to overload or vibration. Preventive measures at the earlier stages of occupational diseases also should be undertaken.
Industrial hygiene activities are not covered by the health insurance system, and the industrial hygienists in the hygienic stations are still paid by the government. Lowering their number and the reorganization of hygienic stations are also expected.
Another change in the health care system is the privatization of some health services. The privatization of small out-patient medical centres has already started. Hospitals—including university hospitals—are not involved in this process at present and details of their privatization still need to be clarified. New legislation concerning the duties of the enterprises, workers and occupational health services is being gradually created.
Occupational Health at the Crossroads
Thanks to the advanced system of occupational health founded by Professor Teisinger in 1932, the Czech Republic does not face a serious problem of education in occupational health for university students, even though in some countries of Central and Eastern Europe the rate of recognized occupational diseases is about five times less than that of the Czech Republic. The Czech List of Occupational Diseases does not differ notably from that appended to the ILO Employment Injury Benefits Convention, (No. 121), (ILO 1964). The proportion of unrecognized principal occupational diseases is low.
The occupational health system in the Czech Republic is now at the crossroads and there is an obvious need for its reorganization. But it is necessary at the same time to preserve whatever positive features have been acquired from experience with the previous occupational health system, namely:
- registration of working conditions at the workplaces
- maintaining in operation a broad system of periodic medical examinations of employees
- provision of curative health care services at large-scale enterprises
- offering a system of vaccination and communicable disease control
- preserving the system whereby occupational health services admit patients with various occupational illnesses, a system that would involve the university hospitals in providing treatment to patients as well as education and training to medical students and graduates.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."