Children categories

27. Biological Monitoring (6)

27. Biological Monitoring
Chapter Editor: Robert Lauwerys
Table of Contents
Tables and Figures
General Principles
Vito Foà and Lorenzo Alessio
Quality Assurance
D. Gompertz
Metals and Organometallic Compounds
P. Hoet and Robert Lauwerys
Organic Solvents
Masayuki Ikeda
Genotoxic Chemicals
Marja Sorsa
Pesticides
Marco Maroni and Adalberto Ferioli
Tables
Click a link below to view table in article context.
1. ACGIH, DFG & other limit values for metals
2. Examples of chemicals & biological monitoring
3. Biological monitoring for organic solvents
4. Genotoxicity of chemicals evaluated by IARC
5. Biomarkers & some cell/tissue samples & genotoxicity
6. Human carcinogens, occupational exposure & cytogenetic end points
8. Exposure from production & use of pesticides
9. Acute OP toxicity at different levels of ACHE inhibition
10. Variations of ACHE & PCHE & selected health conditions
11. Cholinesterase activities of unexposed healthy people
12. Urinary alkyl phosphates & OP pesticides
13. Urinary alkyl phosphates measurements & OP
14. Urinary carbamate metabolites
15. Urinary dithiocarbamate metabolites
16. Proposed indices for biological monitoring of pesticides
17. Recommended biological limit values (as of 1996)
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

28. Epidemiology and Statistics (12)

28. Epidemiology and Statistics
Chapter Editors: Franco Merletti, Colin L. Soskolne and Paolo Vineis
Table of Contents
Tables and Figures
Epidemiological Method Applied to Occupational Health and Safety
Franco Merletti, Colin L. Soskolne and Paolo Vineis
Exposure Assessment
M. Gerald Ott
Summary Worklife Exposure Measures
Colin L. Soskolne
Measuring Effects of Exposures
Shelia Hoar Zahm
Case Study: Measures
Franco Merletti, Colin L. Soskolne and Paola Vineis
Options in Study Design
Sven Hernberg
Validity Issues in Study Design
Annie J. Sasco
Impact of Random Measurement Error
Paolo Vineis and Colin L. Soskolne
Statistical Methods
Annibale Biggeri and Mario Braga
Causality Assessment and Ethics in Epidemiological Research
Paolo Vineis
Case Studies Illustrating Methodological Issues in the Surveillance of Occupational Diseases
Jung-Der Wang
Questionnaires in Epidemiological Research
Steven D. Stellman and Colin L. Soskolne
Asbestos Historical Perspective
Lawrence Garfinkel
Tables
Click a link below to view table in article context.
1. Five selected summary measures of worklife exposure
2. Measures of disease occurrence
3. Measures of association for a cohort study
4. Measures of association for case-control studies
5. General frequency table layout for cohort data
6. Sample layout of case-control data
7. Layout case-control data - one control per case
8. Hypothetical cohort of 1950 individuals to T2
9. Indices of central tendency & dispersion
10. A binomial experiment & probabilities
11. Possible outcomes of a binomial experiment
12. Binomial distribution, 15 successes/30 trials
13. Binomial distribution, p = 0.25; 30 trials
14. Type II error & power; x = 12, n = 30, a = 0.05
15. Type II error & power; x = 12, n = 40, a = 0.05
16. 632 workers exposed to asbestos 20 years or longer
17. O/E number of deaths among 632 asbestos workers
Figures
Point to a thumbnail to see figure caption, click to see the figure in article context.

29. Ergonomics (27)

29. Ergonomics
Chapter Editors: Wolfgang Laurig and Joachim Vedder
Table of Contents
Tables and Figures
Overview
Wolfgang Laurig and Joachim Vedder
Goals, Principles and Methods
The Nature and Aims of Ergonomics
William T. Singleton
Analysis of Activities, Tasks and Work Systems
Véronique De Keyser
Ergonomics and Standardization
Friedhelm Nachreiner
Checklists
Pranab Kumar Nag
Physical and Physiological Aspects
Anthropometry
Melchiorre Masali
Muscular Work
Juhani Smolander and Veikko Louhevaara
Postures at Work
Ilkka Kuorinka
Biomechanics
Frank Darby
General Fatigue
Étienne Grandjean
Fatigue and Recovery
Rolf Helbig and Walter Rohmert
Psychological Aspects
Mental Workload
Winfried Hacker
Vigilance
Herbert Heuer
Mental Fatigue
Peter Richter
Organizational Aspects of Work
Work Organization
Eberhard Ulich and Gudela Grote
Sleep Deprivation
Kazutaka Kogi
Work Systems Design
Workstations
Roland Kadefors
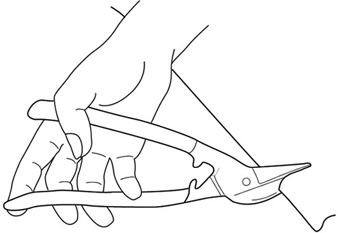
Tools
T.M. Fraser
Controls, Indicators and Panels
Karl H. E. Kroemer
Information Processing and Design
Andries F. Sanders
Designing for Everyone
Designing for Specific Groups
Joke H. Grady-van den Nieuwboer
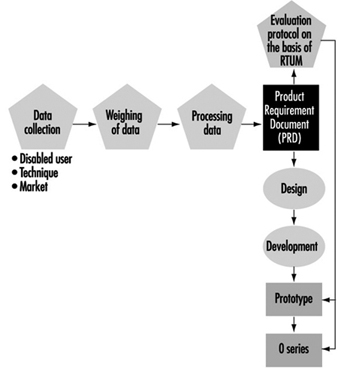
Case Study: The International Classification of Functional Limitation in People
Cultural Differences
Houshang Shahnavaz
Elderly Workers
Antoine Laville and Serge Volkoff
Workers with Special Needs
Joke H. Grady-van den Nieuwboer
Diversity and Importance of Ergonomics--Two Examples
System Design in Diamond Manufacturing
Issachar Gilad
Disregarding Ergonomic Design Principles: Chernobyl
Vladimir M. Munipov
Tables
Click a link below to view table in article context.
1. Basic anthropometric core list
2. Fatigue & recovery dependent on activity levels
3. Rules of combination effects of two stress factors on strain
4. Differenting among several negative consequences of mental strain
5. Work-oriented principles for production structuring
6. Participation in organizational context
7. User participation in the technology process
8. Irregular working hours & sleep deprivation
9. Aspects of advance, anchor & retard sleeps
10. Control movements & expected effects
11. Control-effect relations of common hand controls
12. Rules for arrangement of controls
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

30. Occupational Hygiene (6)

30. Occupational Hygiene
Chapter Editor: Robert F. Herrick
Table of Contents
Tables and Figures
Goals, Definitions and General Information
Berenice I. Ferrari Goelzer
Recognition of Hazards
Linnéa Lillienberg
Evaluation of the Work Environment
Lori A. Todd
Occupational Hygiene: Control of Exposures Through Intervention
James Stewart
The Biological Basis for Exposure Assessment
Dick Heederik
Occupational Exposure Limits
Dennis J. Paustenbach
Tables
1. Hazards of chemical; biological & physical agents
2. Occupational exposure limits (OELs) - various countries
Figures

31. Personal Protection (7)

31. Personal Protection
Chapter Editor: Robert F. Herrick
Table of Contents
Tables and Figures
Overview and Philosophy of Personal Protection
Robert F. Herrick
Eye and Face Protectors
Kikuzi Kimura
Foot and Leg Protection
Toyohiko Miura
Head Protection
Isabelle Balty and Alain Mayer
Hearing Protection
John R. Franks and Elliott H. Berger
Protective Clothing
S. Zack Mansdorf
Respiratory Protection
Thomas J. Nelson
Tables
Click a link below to view table in article context.
1. Transmittance requirements (ISO 4850-1979)
2. Scales of protection - gas-welding & braze-welding
3. Scales of protection - oxygen cutting
4. Scales of protection - plasma arc cutting
5. Scales of protection - electric arc welding or gouging
6. Scales of protection - plasma direct arc welding
7. Safety helmet: ISO Standard 3873-1977
8. Noise Reduction Rating of a hearing protector
9. Computing the A-weighted noise reduction
10. Examples of dermal hazard categories
11. Physical, chemical & biological performance requirements
12. Material hazards associated with particular activities
13. Assigned protection factors from ANSI Z88 2 (1992)
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

32. Record Systems and Surveillance (9)

32. Record Systems and Surveillance
Chapter Editor: Steven D. Stellman
Table of Contents
Tables and Figures
Occupational Disease Surveillance and Reporting Systems
Steven B. Markowitz
Occupational Hazard Surveillance
David H. Wegman and Steven D. Stellman
Surveillance in Developing Countries
David Koh and Kee-Seng Chia
Development and Application of an Occupational Injury and Illness Classification System
Elyce Biddle
Risk Analysis of Nonfatal Workplace Injuries and Illnesses
John W. Ruser
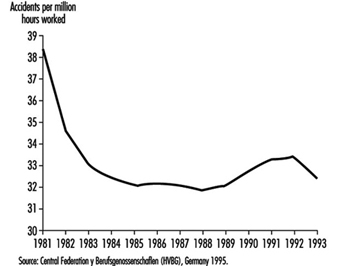
Case Study: Worker Protection and Statistics on Accidents and Occupational Diseases - HVBG, Germany
Martin Butz and Burkhard Hoffmann
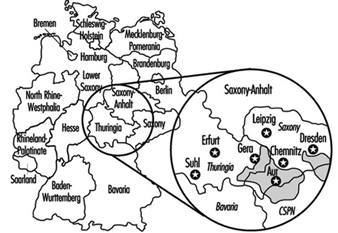
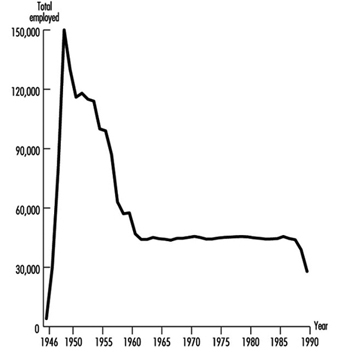
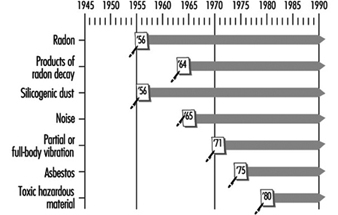
Case Study: Wismut - A Uranium Exposure Revisited
Heinz Otten and Horst Schulz
Measurement Strategies and Techniques for Occupational Exposure Assessment in Epidemiology
Frank Bochmann and Helmut Blome
Case Study: Occupational Health Surveys in China
Tables
Click a link below to view the table in article context.
1. Angiosarcoma of the liver - world register
2. Occupational illness, US, 1986 versus 1992
3. US Deaths from pneumoconiosis & pleural mesothelioma
4. Sample list of notifiable occupational diseases
5. Illness & injury reporting code structure, US
6. Nonfatal occupational injuries & illnesses, US 1993
7. Risk of occupational injuries & illnesses
8. Relative risk for repetitive motion conditions
9. Workplace accidents, Germany, 1981-93
10. Grinders in metalworking accidents, Germany, 1984-93
11. Occupational disease, Germany, 1980-93
12. Infectious diseases, Germany, 1980-93
13. Radiation exposure in the Wismut mines
14. Occupational diseases in Wismut uranium mines 1952-90
Figures
Point to a thumbnail to see figure caption, click to see the figure in article context.

33. Toxicology (21)

33. Toxicology
Chapter Editor: Ellen K. Silbergeld
Table of Contents
Tables and Figures
Introduction
Ellen K. Silbergeld, Chapter Editor
General Principles of Toxicology
Definitions and Concepts
Bo Holmberg, Johan Hogberg and Gunnar Johanson
Toxicokinetics
Dušan Djuríc
Target Organ And Critical Effects
Marek Jakubowski
Effects Of Age, Sex And Other Factors
Spomenka Telišman
Genetic Determinants Of Toxic Response
Daniel W. Nebert and Ross A. McKinnon
Mechanisms of Toxicity
Introduction And Concepts
Philip G. Watanabe
Cellular Injury And Cellular Death
Benjamin F. Trump and Irene K. Berezesky
Genetic Toxicology
R. Rita Misra and Michael P. Waalkes
Immunotoxicology
Joseph G. Vos and Henk van Loveren
Target Organ Toxicology
Ellen K. Silbergeld
Toxicology Test Methods
Biomarkers
Philippe Grandjean
Genetic Toxicity Assessment
David M. DeMarini and James Huff
In Vitro Toxicity Testing
Joanne Zurlo
Structure Activity Relationships
Ellen K. Silbergeld
Regulatory Toxicology
Toxicology In Health And Safety Regulation
Ellen K. Silbergeld
Principles Of Hazard Identification - The Japanese Approach
Masayuki Ikeda
The United States Approach to Risk Assessment Of Reproductive Toxicants and Neurotoxic Agents
Ellen K. Silbergeld
Approaches To Hazard Identification - IARC
Harri Vainio and Julian Wilbourn
Appendix - Overall Evaluations of Carcinogenicity to Humans: IARC Monographs Volumes 1-69 (836)
Carcinogen Risk Assessment: Other Approaches
Cees A. van der Heijden
Tables
Click a link below to view table in article context.
- Examples of critical organs & critical effects
- Basic effects of possible multiple interactions of metals
- Haemoglobin adducts in workers exposed to aniline & acetanilide
- Hereditary, cancer-prone disorders & defects in DNA repair
- Examples of chemicals that exhibit genotoxicity in human cells
- Classification of tests for immune markers
- Examples of biomarkers of exposure
- Pros & cons of methods for identifying human cancer risks
- Comparison of in vitro systems for hepatotoxicity studies
- Comparison of SAR & test data: OECD/NTP analyses
- Regulation of chemical substances by laws, Japan
- Test items under the Chemical Substance Control Law, Japan
- Chemical substances & the Chemical Substances Control Law
- Selected major neurotoxicity incidents
- Examples of specialized tests to measure neurotoxicity
- Endpoints in reproductive toxicology
- Comparison of low-dose extrapolations procedures
- Frequently cited models in carcinogen risk characterization
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Protective Clothing
Hazards
There are several general categories of bodily hazards for which specialized clothing can provide protection. These general categories include chemical, physical and biological hazards. Table 1 summarizes these.
Table 1. Examples of dermal hazard categories
|
Hazard |
Examples |
|
Chemical |
Dermal toxins |
|
Physical |
Thermal hazards (hot/cold) |
|
Biological |
Human pathogens |
Chemical hazards
Protective clothing is a commonly used control to reduce worker exposures to potentially toxic or hazardous chemicals when other controls are not feasible. Many chemicals pose more than one hazard (for example, a substance such as benzene is both toxic and flammable). For chemical hazards, there are at least three key considerations that need attention. These are (1) the potential toxic effects of exposure, (2) likely routes of entry, and (3) the exposure potentials associated with the work assignment. Of the three aspects, toxicity of the material is the most important. Some substances simply present a cleanliness problem (e.g., oil and grease) while other chemicals (e.g., contact with liquid hydrogen cyanide) could present a situation which is immediately dangerous to life and health (IDLH). Specifically, the toxicity or hazardousness of the substance by the dermal route of entry is the critical factor. Other adverse effects of skin contact, besides toxicity, include corrosion, promotion of cancer of the skin and physical trauma such as burns and cuts.
An example of a chemical whose toxicity is greatest by the dermal route is nicotine, which has excellent skin permeability but is not generally an inhalation hazard (except when self-administered). This is only one of many instances where the dermal route offers a much more significant hazard than the other routes of entry. As suggested above, there are many substances that are not generally toxic but are hazardous to the skin because of their corrosive nature or other properties. In fact, some chemicals and materials can offer an even greater acute risk through skin absorption than the most dreaded systemic carcinogens. For example, a single unprotected skin exposure to hydrofluoric acid (above 70% concentration) can be fatal. In this case, as little as a 5% surface burn typically results in death from the effects of the fluoride ion. Another example of a dermal hazard—though not an acute one—is the promotion of skin cancer by substances such as coal tars. An example of a material which has high human toxicity but little skin toxicity is inorganic lead. In this case the concern is contamination of the body or clothing, which could later lead to ingestion or inhalation, since the solid will not permeate intact skin.
Once an evaluation of the routes of entry and toxicity of the materials has been completed, an assessment of the likelihood of exposure needs to be carried out. For example, do workers have enough contact with a given chemical to become visibly wet or is exposure unlikely and protective clothing intended to act simply as a redundant control measure? For situations where the material is deadly although the likelihood of contact is remote, the worker must obviously be provided with the highest level of protection available. For situations where the exposure itself represents a very minimal risk (e.g., a nurse handling 20% isopropyl alcohol in water), the level of protection does not need to be fail-safe. This selection logic is essentially based on an estimate of the adverse effects of the material combined with an estimate of the likelihood of exposure.
The chemical resistance properties of barriers
Research showing the diffusion of solvents and other chemicals through “liquid-proof” protective clothing barriers has been published from the 1980s to the 1990s. For example, in a standard research test, acetone is applied to neoprene rubber (of typical glove thickness). After direct acetone contact on the normal outside surface, the solvent can normally be detected on the inside surface (the skin side) within 30 minutes, although in small quantities. This movement of a chemical through a protective clothing barrier is called permeation. The permeation process consists of the diffusion of chemicals on a molecular level through the protective clothing. Permeation occurs in three steps: absorption of the chemical at the barrier surface, diffusion through the barrier, and desorption of the chemical on the normal inside surface of the barrier. The time elapsed from the initial contact of the chemical on the outside surface until detection on the inside surface is called the breakthrough time. The permeation rate is the steady-state rate of movement of the chemical through the barrier after equilibrium is reached.
Most current testing of permeation resistance extends over periods of up to eight hours, reflecting normal work shifts. However, these tests are conducted under conditions of direct liquid or gaseous contact that typically do not exist in the work environment. Some would therefore argue that there is a significant “safety factor” built into the test. Countering this assumption are the facts that the permeation test is static while the work environment is dynamic (involving flexing of materials or pressures generated from gripping or other movement) and that there may exist prior physical damage to the glove or garment. Given the lack of published skin permeability and dermal toxicity data, the approach taken by most safety and health professionals is to select the barrier with no breakthrough for the duration of the job or task (usually eight hours), which is essentially a no-dose concept. This is an appropriately conservative approach; however, it is important to note that there is no protective barrier currently available which provides permeation resistance to all chemicals. For situations where the breakthrough times are short, the safety and health professional should select the barriers with the best performance (i.e., with the lowest permeation rate) while considering other control and maintenance measures as well (such as the need for regular clothing changes).
Aside from the permeation process just described, there are two other chemical resistance properties of concern to the safety and health professional. These are degradation and penetration. Degradation is a deleterious change in one or more of the physical properties of a protective material caused by contact with a chemical. For example, the polymer polyvinyl alcohol (PVA) is a very good barrier to most organic solvents, but is degraded by water. Latex rubber, which is widely used for medical gloves, is of course water resistant, but is readily soluble in such solvents as toluene and hexane: it would be plainly ineffective for protection against these chemicals. Secondly, latex allergies can cause severe reactions in some people.
Penetration is the flow of a chemical through pinholes, cuts or other imperfections in protective clothing on a nonmolecular level. Even the best protective barriers will be rendered ineffective if punctured or torn. Penetration protection is important when the exposure is unlikely or infrequent and the toxicity or hazard is minimal. Penetration is usually a concern for garments used in splash protection.
Several guides have been published listing chemical resistance data (many are also available in an electronic format). In addition to these guides, most manufacturers in the industrially developed countries also publish current chemical and physical resistance data for their products.
Physical hazards
As noted in table 1, physical hazards include thermal conditions, vibration, radiation and trauma as all having the potential to affect the skin adversely. Thermal hazards include the adverse effects of extreme cold and heat on the skin. The protective attributes of clothing with respect to these hazards is related to its degree of insulation, whereas protective clothing for flash fire and electric flashover requires flame resistance properties.
Specialized clothing can provide limited protection from some forms of both ionizing and non-ionizing radiation. In general, the effectiveness of clothing that protects against ionizing radiation is based on the principle of shielding (as with lead-lined aprons and gloves), whereas clothing employed against non-ionizing radiation, such as microwave, is based on grounding or isolation. Excessive vibration can have several adverse effects on body parts, primarily the hands. Mining (involving hand-held drills) and road repair (for which pneumatic hammers or chisels are used), for example, are occupations where excessive hand vibration can lead to bone degeneration and loss of circulation in the hands. Trauma to the skin from physical hazards (cuts, abrasions, etc.) is common to many occupations, with construction and meat cutting as two examples. Specialized clothing (including gloves) are now available which are cut-resistant and are used in applications such as meat cutting and forestry (using chain saws). These are based either on inherent cut-resistance or the presence of enough fibre mass to clog moving parts (e.g., chain saws).
Biological hazards
Biological hazards include infection due to agents and disease common to humans and animals, and the work environment. Biological hazards common to humans have received great attention with the increasing spread of blood-borne AIDS and hepatitis. Hence, occupations which might involve exposure to blood or body fluids usually require some type of liquid-resistant garment and gloves. Diseases transmitted from animals through handling (e.g., anthrax) have a long history of recognition and require protective measures similar to those used for handling the kind of blood-borne pathogens that affect humans. Work environments that can present a hazard due to biological agents include clinical and microbiological laboratories as well as other special work environments.
Types of Protection
Protective clothing in a generic sense includes all elements of a protective ensemble (e.g., garments, gloves and boots). Thus, protective clothing can include everything from a finger cot providing protection against paper cuts to a fully encapsulating suit with a self-contained breathing apparatus used for an emergency response to a hazardous chemical spill.
Protective clothing can be made of natural materials (e.g., cotton, wool and leather), man-made fibres (e.g., nylon) or various polymers (e.g., plastics and rubbers such as butyl rubber, polyvinyl chloride, and chlorinated polyethylene). Materials which are woven, stitched or are otherwise porous (not resistant to liquid penetration or permeation) should not be used in situations where protection against a liquid or gas is required. Specially treated or inherently non-flammable porous fabrics and materials are commonly used for flash fire and electric arc (flashover) protection (e.g., in the petrochemical industry) but usually do not provide protection from any regular heat exposure. It should be noted here that fire-fighting requires specialized clothing that provides flame (burning) resistance, a water barrier and thermal insulation (protection from high temperatures). Some special applications also require infrared (IR) protection by use of aluminized overcovers (e.g., fighting petroleum fuel fires). Table 2 summarizes typical physical, chemical, and biological performance requirements and common protective materials used for hazard protection.
Table 2. Common physical, chemical and biological performance requirements
|
Hazard |
Performance characteristic required |
Common protective clothing materials |
|
Thermal |
Insulation value |
Heavy cotton or other natural fabrics |
|
Fire |
Insulation and flame resistance |
Aluminized gloves; flame resistent treated gloves; aramid fibre and other special fabrics |
|
Mechanical abrasion |
Abrasion resistence; tensile strength |
Heavy fabrics; leather |
|
Cuts and punctures |
Cut resistance |
Metal mesh; aromatic polyamide fiber and other special fabrics |
|
Chemical/toxicological |
Permeation resistance |
Polymeric and elastomeric materials; (including latex) |
|
Biological |
“Fluid-proof”; (puncture resistant) |
|
|
Radiological |
Usually water resistance or particle resistance (for radionuclides) |
Protective clothing configurations vary greatly depending on the intended use. However, normal components are analogous to personal clothing (i.e., trousers, jacket, hood, boots and gloves) for most physical hazards. Special-use items for applications such as flame resistance in those industries involving the processing of molten metals can include chaps, armlets, and aprons constructed of both treated and untreated natural and synthetic fibres and materials (one historical example would be woven asbestos). Chemical protective clothing can be more specialized in terms of construction, as shown in figure 1 and figure 2.
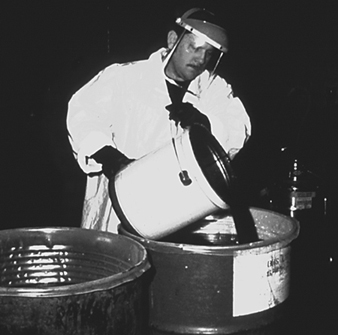
Figure 1. A worker wearing gloves and a chemically protective garment pouring chemical
Figure 2. Two workers in differing configurations of chemical protective clothing
Chemically protective gloves are usually available in a wide variety of polymers and combinations; some cotton gloves, for example, are coated by the polymer of interest (by means of a dipping process). (See figure 3). Some of the new foil and multilaminate “gloves” are only two-dimensional (flat)—and hence have some ergonomic constraints, but are highly chemical resistant. These gloves typically work best when a form-fitting outer polymer glove is worn over the top of the inner flat glove (this technique is called double gloving) to conform the inner glove to the shape of the hands. Polymer gloves are available in a wide variety of thicknesses ranging from very light weight (<2 mm) to heavy weight (>5 mm) with and without inner liners or substrates (called scrims). Gloves are also commonly available in a variety of lengths ranging from approximately 30 centimetres for hand protection to gauntlets of approximately 80 centimetres, extending from the worker’s shoulder to the tip of the hand. The correct choice of length depends on the extent of protection required; however, the length should normally be sufficient to extend at least to the worker’s wrists so as to prevent drainage into the glove. (See figure 4).
Figure 3. Various types of chemically resistant gloves
MISSING
Figure 4. Natural-fibre gloves; also illustrates sufficient length for wrist protection
Boots are available in a wide variety of lengths ranging from hip length to those that cover only the bottom of the foot. Chemical protective boots are available in only a limited number of polymers since they require a high degree of abrasion resistance. Common polymers and rubbers used in chemically resistant boot construction include PVC, butyl rubber and neoprene rubber. Specially constructed laminated boots using other polymers can also be obtained but are quite expensive and in limited supply internationally at the present time.
Chemical protective garments can be obtained as a one-piece fully encapsulating (gas-tight) garment with attached gloves and boots or as multiple components (e.g., trousers, jacket, hoods, etc.). Some protective materials used for construction of ensembles will have multiple layers or laminas. Layered materials are generally required for polymers that do not have good enough inherent physical integrity and abrasion resistance properties to permit manufacture and use as a garment or glove (e.g., butyl rubber versus Teflon®). Common support fabrics are nylon, polyester, aramides and fibreglass. These substrates are coated or laminated by polymers such as polyvinyl chloride (PVC), Teflon®, polyurethane and polyethylene.
Over the last decade there has been an enormous growth in the use of nonwoven polyethene and microporous materials for disposable suit construction. These spun-bonded suits, sometimes incorrectly called “paper suits,” are made using a special process whereby the fibres are bonded together rather than woven. These protective garments are low in cost and very light in weight. Uncoated microporous materials (called “breathable” because they allow some water vapour transmission and hence are less heat stressful) and spun-bonded garments have good applications as protection against particulates but are not normally chemical-or liquid-resistant. Spun-bonded garments are also available with various coatings such as polyethylene and Saranex®. Depending on the coating characteristics, these garments can offer good chemical resistance to most common substances.
Approval, Certification and Standards
The availability, construction, and design of protective clothing varies greatly throughout the world. As might be expected, approval schemes, standards and certifications also vary. Nevertheless, there are similar voluntary standards for performance throughout the United States (e.g., American Society for Testing and Materials—ASTM—standards), Europe (European Committee for Standardization—CEN—standards), and for some parts of Asia (local standards such as in Japan). The development of worldwide performance standards has begun through the International Organization for Standardization Technical Committee 94 for Personal Safety-Protective Clothing and Equipment. Many of the standards and test methods to measure performance developed by this group were based on either CEN standards or those from other countries such as the United States through the ASTM.
In the United States, Mexico, and most of Canada, no certification or approvals are required for most protective clothing. Exceptions exist for special applications such as pesticide applicators clothing (governed by pesticide labelling requirements). Nevertheless, there are many organizations that issue voluntary standards, such as the previously mentioned ASTM, the National Fire Protection Association (NFPA) in the United States and the Canadian Standards Organization (CSO) in Canada. These voluntary standards do significantly affect the marketing and sale of protective clothing and hence act much like mandated standards.
In Europe, the manufacturing of personal protective equipment is regulated under the European Community Directive 89/686/EEC. This directive both defines which products fall within the scope of the directive and classifies them into different categories. For categories of protective equipment where the risk is not minimal and where the user cannot readily identify the hazard easily, the protective equipment must meet standards of quality and manufacture detailed in the directive.
No protective equipment products may be sold within the European Community unless they have the CE (European Community) mark. Testing and quality assurance requirements must be followed to receive the CE mark.
Individual Capabilities and Needs
In all but a few cases, the addition of protective clothing and equipment will decrease productivity and increase worker discomfort. It may also lead to decreased quality, since error rates increase with the use of protective clothing. For chemical protective and some fire-resistant clothing there are some general guidelines that need to be considered concerning the inherent conflicts between worker comfort, efficiency and protection. First, the thicker the barrier the better (increases the time to breakthrough or provides greater thermal insulation); however, the thicker the barrier the more it will decrease ease of movement and user comfort. Thicker barriers also increase the potential for heat stress. Second, barriers which have excellent chemical resistance tend to increase the level of worker discomfort and heat stress because the barrier normally will also act as a barrier to water vapour transmission (i.e., perspiration). Third, the higher the overall protection of the clothing, the more time a given task will take to accomplish and the greater the chance of errors. There are also a few tasks where the use of protective clothing could increase certain classes of risk (e.g., around moving machinery, where the risk of heat stress is greater than the chemical hazard). While this situation is rare, it must be considered.
Other issues relate to the physical limitations imposed by using protective clothing. For example, a worker issued a thick pair of gloves will not be able to perform tasks easily that require a high degree of dexterity and repetitive motions. As another example, a spray painter in a totally encapsulating suit will usually not be able to look to the side, up or down, since typically the respirator and suit visor restrict the field of vision in these suit configurations. These are only some examples of the ergonomic restrictions associated with wearing protective clothing and equipment.
The work situation must always be considered in the selection of the protective clothing for the job. The optimum solution is to select the minimum level of protective clothing and equipment that is necessary to do the job safely.
Education and Training
Adequate education and training for users of protective clothing is essential. Training and education should include:
- the nature and extent of the hazards
- the conditions under which protective clothing should be worn
- what protective clothing is necessary
- the use and limitations of the protective clothing to be assigned
- how to inspect, don, doff, adjust and wear the protective clothing properly
- decontamination procedures, if necessary
- signs and symptoms of overexposure or clothing failure
- first aid and emergency procedures
- the proper storage, useful life, care and disposal of protective clothing.
This training should incorporate at least all of the elements listed above and any other pertinent information that has not already been provided to the worker through other programmes. For those topical areas already provided to the worker, a refresher summary should still be provided for the clothing user. For example, if the signs and symptoms of overexposure have already been indicated to the workers as part of their training for working with chemicals, symptoms that are a result of significant dermal exposures versus inhalation should be reemphasized. Finally, the workers should have an opportunity to try out the protective clothing for a particular job before a final selection is made.
Knowledge of the hazard and of the limitations of the protective clothing not only reduces the risk to the worker but also provides the health and safety professional with a worker capable of providing feedback on the effectiveness of the protective equipment.
Maintenance
The proper storage, inspection, cleaning and repair of protective clothing is important to the overall protection provided by the products to the wearer.
Some protective clothing will have storage limitations such as a prescribed shelf life or required protection from UV radiation (e.g., sunlight, welding flash, etc.), ozone, moisture, temperature extremes or prevention of product folding. For example, natural rubber products usually call for all of the precautionary measures just listed. As another example, many of the encapsulating polymer suits can be damaged if folded rather than allowed to hang upright. The manufacturer or distributor should be consulted for any storage limitations their products may have.
Inspection of protective clothing should be performed by the user on a frequent basis (e.g., with each use). Inspection by co-workers is another technique which may be used to involve wearers in ensuring the integrity of the protective clothing they have to use. As a management policy, it is also advisable to require supervisors to inspect protective clothing (at appropriate intervals) that is used on a routine basis. Inspection criteria will depend on the intended use of the protective item; however, it would normally include examination for tears, holes, imperfections and degradation. As one example of an inspection technique, polymer gloves used for protection against liquids should be blown up with air to check for integrity against leaks.
Cleaning of protective clothing for reuse must be performed with care. Natural fabrics can be cleaned by normal washing methods if they are not contaminated with toxic materials. Cleaning procedures suitable for synthetic fibres and materials are commonly limited. For example, some products treated for flame resistance will lose their effectiveness if not properly cleaned. Clothing used for protection against chemicals which are not water-soluble often cannot be decontaminated by washing with simple soap or detergent and water. Tests performed on pesticide applicators’ clothing indicate that normal washing procedures are not effective for many pesticides. Dry cleaning is not recommended at all since it is often ineffective and can degrade or contaminate the product. It is important to consult the manufacturer or distributor of the clothing before attempting cleaning procedures that are not specifically known to be safe and workable.
Most protective clothing is not repairable. Repairs can be made on some few items such as fully encapsulating polymer suits. However, the manufacturer should be consulted for the proper repair procedures.
Use and Misuse
Use. First and foremost, the selection and proper use of protective clothing should be based on an assessment of the hazards involved in the task for which the protection is required. In light of the assessment, an accurate definition of the performance requirements and the ergonomic constraints of the job can be determined. Finally, a selection that balances worker protection, ease of use and cost can be made.
A more formal approach would be to develop a written model programme, a method that would reduce the chance of error, increase worker protection and establish a consistent approach to the selection and use of protective clothing. A model programme could contain the following elements:
- an organization scheme and administrative plan
- a risk assessment methodology
- an evaluation of other control options to protect the worker
- performance criteria for the protective clothing
- selection criteria and procedures to determine the optimum choice
- purchasing specifications for the protective clothing
- a validation plan for the selection made
- decontamination and reuse criteria, as applicable
- a user training programme
- 10.an auditing plan to assure that procedures are consistently followed.
Misuse. There are several examples of misuse of protective clothing that can commonly be seen in industry. Misuse is usually the result of a lack of understanding of the limitations of protective clothing on the part of management, of the workers, or of both. A clear example of bad practice is the use of nonflame-resistant protective clothing for workers who handle flammable solvents or who work in situations where open flames, burning coals or molten metals are present. Protective clothing made of polymeric materials such as polyethylene may support combustion and can actually melt into the skin, causing an even more severe burn.
A second common example is the reuse of protective clothing (including gloves) where the chemical has contaminated the inside of the protective clothing so that the worker increases his or her exposure on each subsequent use. One frequently sees another variation of this problem when workers use natural-fibre gloves (e.g., leather or cotton) or their own personal shoes to work with liquid chemicals. If chemicals are spilled on the natural fibres, they will be retained for long periods of time and migrate to the skin itself. Yet another variation of this problem is taking contaminated work clothing home for cleaning. This can result in the exposure of an entire family to harmful chemicals, a common problem because the work clothing is usually cleaned with the other articles of clothing of the family. Since many chemicals are not water-soluble, they can be spread to other articles of clothing simply by mechanical action. Several cases of this spread of contaminants have been noted, especially in industries which manufacture pesticides or process heavy metals (e.g., poisoning families of workers handling mercury and lead). These are only a few of the more prominent examples of the misuse of protective clothing. These problems can be overcome by simply understanding the proper use and limitations of the protective clothing. This information should be readily available from the manufacturer and health and safety experts.
Respiratory Protection
In some industries, air contaminated with potentially harmful dusts, fumes, mists, vapours or gases may cause harm to the workers. The control of exposure to these materials is important to decrease the risk of occupational diseases caused by breathing the contaminated air. The best method to control exposure is to minimize workplace contamination. This can be accomplished by using engineering control measures (e.g., by enclosure or confinement of the operation, by general and local ventilation and substitution of less toxic materials). When effective engineering controls are not feasible, or while they are being implemented or evaluated, respirators can be used to protect the health of the worker. For respirators to work as anticipated, an appropriate and well-planned respirator programme is necessary.
Respiratory Hazards
Hazards to the respiratory system can be in the form of air contaminants or due to a lack of sufficient oxygen. The particulates, gases or vapours that constitute air contaminants may be associated with different activities (see table 1).
Table 1. Material hazards associated with particular activities
|
Type of hazard |
Typical sources or activities |
Examples |
|
Dusts |
Sewing, grinding, sanding, chipping, sand blasting |
Wood dust, coal, silica dust |
|
Fumes |
Welding, brazing, smelting |
Lead, zinc, iron oxide fumes |
|
Mists |
Spray painting, metal plating, machining |
Paint mists, oil mists |
|
Fibers |
Insulation, friction products |
Asbestos, fiber glass |
|
Gases |
Welding, combustion engines, water treatment |
Ozone, carbon dioxide, carbon monoxide, chlorine |
|
Vapours |
Degreasing, painting, cleaning products |
Methylene chloride, toluene, mineral spirits |
Oxygen is a normal component of the environment that is necessary to sustain life. Physiologically speaking, oxygen deficiency is a reduction in the availability of oxygen to the body’s tissues. It may be caused by the reduction in the percentage of oxygen in the air or by the reduction in the partial pressure of oxygen. (The partial pressure of a gas equals the fractional concentration of the gas in question times the total atmospheric pressure.) The most common form of oxygen deficiency in working environments occurs when the percentage of oxygen is reduced because it is displaced by another gas in a confined space.
Types of Respirators
Respirators are categorized by the type of cover offered for the respiratory system (inlet covering) and by the mechanism used to protect the wearer from the contaminant or from oxygen deficiency. The mechanism is either air purification or supplied air.
Inlet coverings
The “inlets” to the respiratory system are the nose and the mouth. For a respirator to work, these must be sealed by a cover that will in some way isolate the person’s respiratory system from hazards in the respirable environment while simultaneously permitting the intake of sufficient oxygen. The types of coverings that are used may be either tight or loose.
Tight-fitting coverings may take the form of a quarter mask, a half mask, a full facepiece, or a mouth bit. A quarter mask covers both the nose and the mouth. The sealing surface extends from the bridge of the nose to below the lips (a quarter of the face). A half facepiece forms a seal from the bridge of the nose to underneath the chin (half the face). The seal of a full facepiece extends from above the eyes (but below the hair line) to underneath the chin (covering the full face).
With a respirator employing a mouth bit, the mechanism for covering the respiratory system inlets is slightly different. The person bites onto a rubber bit that is attached to the respirator and uses a nose clip to seal the nose. Thus both of the respiratory system inlets are sealed. Mouth bit type respirators are a special type that are used only in situations that call for escape from a hazardous atmosphere. They will not be discussed further in this chapter, since their use is so specialized.
The quarter, half or full-face types of coverings can be used with either an air-purifying or supplied-air type of respirator. The mouth bit type exists only as an air-purifying type.
Loose-fitting inlet coverings, as suggested by their name, do not rely on a sealing surface to protect the worker’s respiratory system. Rather they cover the face, head, or head and shoulders, providing a safe environment. Also included in this group are suits that cover the entire body. (Suits do not include garments that are worn solely to protect the skin, such as splash suits.) Since they do not seal to the face, loose-fitting inlet coverings operate only in systems that provide a flow of air. The flow of air must be greater than the air required for breathing to prevent the contaminant outside the respirator from leaking to the inside.
Air-purifying respirators
An air-purifying respirator causes ambient air to be passed through an air-purifying element that removes the contaminants. Air is passed through the air-purifying element by means of the breathing action (negative pressure respirators) or by a blower (powered air-purifying respirators, or PAPRs).
The type of air-purifying element will determine which contaminants are removed. Filters of varying efficiencies are used to remove aerosols. The choice of filter will depend on the properties of the aerosol; normally, particle size is the most important characteristic. Chemical cartridges are filled with a material that is specifically chosen to absorb or react with the vapour or gaseous contaminant.
Supplied-air respirators
Atmosphere-supplying respirators are a class of respirators that supply a respirable atmosphere independent of the workplace atmosphere. One type is commonly called an air-line respirator and operates in one of three modes: demand, continuous flow or pressure demand. Respirators operating in demand and pressure-demand modes can be equipped with either a half-face or a full facepiece inlet covering. The continuous-flow type can also be equipped with a helmet/hood or a loose-fitting facepiece.
A second type of atmosphere-supplying respirator, called a self-contained breathing apparatus (SCBA), is equipped with a self-contained air supply. It may be used for escape only or for entry into and escape from a hazardous atmosphere. The air is supplied from a compressed-air cylinder or by a chemical reaction.
Some supplied-air respirators are equipped with a small supplemental air bottle. The air bottle provides the person using the respirator with the ability to escape if the main air supply fails.
Combination units
Some specialized respirators may be made to operate both in a supplied-air mode and in an air-purifying mode. They are called combination units.
Respiratory Protection Programmes
For a respirator to function as intended, a minimal respirator programme needs to be developed. Regardless of the type of respirator used, the number of people involved and the complexity of the respirator use, there are basic considerations that need to be included in every programme. For simple programmes, adequate requirements may be minimal. For larger programmes, one may have to prepare for a complex undertaking.
By way of illustration, consider the need of keeping records of fit testing of equipment. For a one- or two-person programme, the date of last fit test, the respirator fit tested and the procedure could be kept on a simple card, while for a large programme with hundreds of users, a computerized database with a system to track those persons who are due for fit testing may be required.
The requirements for a successful programme are described in the following six sections.
1. Programme administration
The responsibility for the respirator programme should be assigned to a single person, called the programme administrator. A single person is assigned this task so that management clearly understands who is responsible. Just as important, this person is given the status necessary to make decisions and run the programme.
The programme administrator should have sufficient knowledge of respiratory protection to supervise the respirator programme in a safe and effective manner. The programme administrator’s responsibilities include the monitoring of respiratory hazards, maintaining records and conducting programme evaluations.
2. Written operating procedures
Written procedures are used to document the programme so that each participant knows what needs to be done, who is responsible for the activity and how it is to be carried out. The procedure document should include a statement of the goals of the programme. This statement would make it clear that the management of the company is responsible for the health of the workers and the implementation of the respirator programme. A written document setting forth the essential procedures of a respirator programme should cover the following functions:
- respirator selection
- maintenance, inspection and repair
- training of employees, supervisors and the person issuing the respirators
- fit testing
- administrative activities including purchasing, inventory control and record keeping
- monitoring of hazards
- monitoring of respirator use
- medical evaluation
- the provision of emergency-use respirators
- programme evaluation.
3. Training
Training is an important part of a respirator programme. The supervisor of the people using respirators, the users themselves and the people who issue respirators to the users all need to be trained. The supervisor needs to know enough about the respirator being used and why it is being used so that he or she will be able to monitor for proper usage: in effect, the person issuing the respirator to the user needs enough training to be sure that the correct respirator is handed out.
The workers who use respirators need to be given training and periodic retraining. The training should include explanations and discussions of the following:
- the nature of the respiratory hazard and possible health effects if the respirator is not used properly
- the reason a particular type of respirator was selected
- how the respirator works and its limitations
- how to put the respirator on and check that it is working and adjusted properly
- how to maintain, inspect and store the respirator
- a respirator fit test for negative pressure respirators.
4. Respirator maintenance
Respirator maintenance includes regular cleaning, inspection for damage, and replacement of worn parts. The manufacturer of the respirator is the best source of information on how to perform cleaning, inspection, repair and maintenance.
Respirators need to be cleaned and sanitized periodically. If a respirator is to be used by more than a single person, it should be cleaned and sanitized before being worn by others. Respirators intended for emergency use should be cleaned and sanitized after each use. This procedure should not be neglected, since there may be special needs to keep the respirator functioning properly. This may include controlled temperatures for cleaning solutions to prevent damage to the device’s elastomers. Furthermore, some parts may need to be cleaned carefully or in a special manner to avoid damage. The manufacturer of the respirator will provide a suggested procedure.
After cleaning and sanitizing, each respirator needs to be inspected to determine if it is in proper working condition, if it needs replacement of parts or repairs, or if it should be discarded. The user should be sufficiently trained and familiar with the respirator in order to be able to inspect the respirator immediately prior to each use in order to ensure that it is in proper working condition.
Respirators that are stored for emergency use need to be periodically inspected. A frequency of once each month is suggested. Once an emergency use respirator is used, it needs to be cleaned and inspected prior to re-use or storage.
In general, inspection will include a check for tightness of connections; for the condition of the respiratory inlet covering, head harness, valves, connecting tubes, harness assemblies, hoses, filters, cartridges, canisters, end of service life indicator, electrical components and shelf life date; and for the proper function of regulators, alarms and other warning systems.
Particular care needs to be given in the inspection of the elastomers and plastic parts commonly found on this equipment. Rubber or other elastomeric parts can be inspected for pliability and signs of deterioration by stretching and bending the material, looking for signs of cracking or wear. Inhalation and exhalation valves are generally thin and easily damaged. One should also look for the build-up of soaps or other cleaning materials on the sealing surfaces of valve seats. Damage or build-up can cause undue leakage through the valve. Plastic parts need to be inspected for damage, such as having stripped or broken threads on a cartridge, for example.
Air and oxygen cylinders should be inspected to determine that they are fully charged according to the manufacturer’s instructions. Some cylinders require periodic inspection to make sure the metal itself is not damaged or rusting. This might include periodic hydrostatic testing of the integrity of the cylinder.
Parts that are found to be defective need to be replaced by stock supplied by the manufacturer itself. Some parts may look very similar to another manufacturer’s, but may perform differently in the respirator itself. Anyone making repairs should to be trained in proper respirator maintenance and assembly.
For supplied-air and self-contained equipment, a higher level of training is required. Reducing or admission valves, regulators and alarms should be adjusted or repaired only by the respirator manufacturer or by a technician trained by the manufacturer.
Respirators that do not meet applicable inspection criteria should be immediately removed from service and repaired or replaced.
Respirators need to be properly stored. Damage can occur if they are not protected from physical and chemical agents such as vibration, sunlight, heat, extreme cold, excessive moisture or damaging chemicals. The elastomers used in the facepiece can be easily damaged if not protected. Respirators should not be stored in such places as lockers and tool boxes unless they are protected from contamination and damage.
5. Medical evaluations
Respirators may affect the health of the person using the equipment because of added stress on the pulmonary system. It is recommended that a physician evaluate each respirator user to determine that he or she can wear a respirator without difficulty. It is up to the physician to determine what will constitute a medical evaluation. A physician may or may not require a physical examination as part of the health assessment.
To perform this task the physician must be given information on the type of respirator being used and the type and length of work the worker will be performing while using the respirator. For most respirators, a normal healthy individual will not be affected by respirator wear, especially in the case of the lightweight air-purifying types.
Someone expected to use an SCBA under emergency conditions will need a more careful evaluation. The weight of the SCBA by itself adds considerably to the amount of work that must be performed.
6. Approved respirators
Many governments have systems to test and approve the performance of respirators for use in their jurisdictions. In such cases, an approved respirator should be used since the fact of its approval indicates that the respirator has met some minimum requirement for performance. If no formal approval is required by the government, any validly approved respirator is likely to provide better assurance that it will perform as intended when compared to a respirator that has gone through no special approval testing whatsoever.
Problems Affecting Respirator Programmes
There are several areas of respirator use that may lead to difficulties in managing a respirator programme. These are the wearing of facial hair and the compatibility of glasses and other protective equipment with the respirator being worn.
Facial hair
Facial hair can present a problem in managing a respirator programme. Some workers like to wear beards for cosmetic reasons. Others experience difficulty shaving, suffering from a medical condition where the facial hairs curl and grow into the skin after shaving. When a person inhales, negative pressure is built up inside the respirator, and if the seal to the face is not tight, contaminants can leak inside. This applies to both air-purifying and supplied-air respirators. The issue is how to be fair, to allow people to wear facial hair, yet to be protective of their health.
There are several research studies that demonstrate that facial hair in the sealing surface of a tight-fitting respirator leads to excessive leakage. Studies have also shown that in connection with facial hair the amount of leakage varies so widely that it is not possible to test whether workers may receive adequate protection even if their respirators were measured for fit. This means that a worker with facial hair wearing a tight-fitting respirator may not be sufficiently protected.
The first step in the solution of this problem is to determine if a loose-fitting respirator can be used. For each type of tight-fitting respirator—except for self contained breathing apparatus and combination escape/air-line respirators—a loose-fitting device is available that will provide comparable protection.
Another alternative is to find another job for the worker which does not require the use of a respirator. The final action that can be taken is to require the worker to shave. For most people who have difficulty shaving, a medical solution can be found that would allow them to shave and wear a respirator.
Eyeglasses and other protective equipment
Some workers need to wear eyeglasses in order to see adequately and in some industrial environments, safety glasses or goggles have to be worn to protect the eyes from flying objects. With a half-mask respirator, eyeglasses or goggles can interfere with the fit of the respirator at the point where it is seated on the bridge of the nose. With a full facepiece, the temple bars of a pair of eyeglasses would create an opening in the sealing surface of the respirator, causing leakage.
Solutions to these difficulties run as follows. For half-mask respirators, a fit test is first carried out, during which the worker should wear any glasses, goggles or other protective equipment that may interfere the respirator’s function. The fit test is used to demonstrate that eyeglasses or other equipment will not interfere with the function of the respirator.
For full-facepiece respirators, the options are to use contact lenses or special eyeglasses that mount inside the facepiece—most manufacturers supply a special spectacles kit for this purpose. At times, it has been thought that contact lenses should not be used with respirators, but research has shown that workers can use contact lenses with respirators without any difficulty.
Suggested Procedure for Respirator Selection
Selecting a respirator involves analysing how the respirator will be used and understanding the limitations of each specific type. General considerations include what the worker will be doing, how the respirator will be used, where the work is located and any limitations a respirator may have on work, as shown schematically in figure 1.
Figure 1. Guide to Respirator Selection
Worker activity and worker location in a hazardous area need to be considered in selecting the proper respirator (for example, whether the worker is in the hazardous area continuously or intermittently during the work shift and whether the work rate is light, medium or heavy). For continuous use and heavy work a lightweight respirator would be preferred.
Environmental conditions and level of effort required of the respirator wearer may affect respirator service life. For example, extreme physical exertion can cause the user to deplete the air supply in a SCBA such that its service life is reduced by half or more.
The period of time that a respirator must be worn is an important factor that has to be taken into account in selecting a respirator. Consideration should be given to the type of task—routine, nonroutine, emergency, or rescue work—that the respirator will be called upon to perform.
The location of the hazardous area with respect to a safe area having respirable air must be considered in selecting a respirator. Such knowledge will permit planning for the escape of workers if an emergency occurs, for the entry of workers to perform maintenance duties and for rescue operations. If there is a long distance to breathable air or if the worker needs to be able to walk around obstacles or climb steps or ladders, then a supplied-air respirator would not be a good choice.
If the potential for an oxygen-deficient environment exists, measure the oxygen content of the relevant work space. The class of respirator, air-purifying or supplied-air, that can be used will depend on the partial pressure of oxygen. Because air-purifying respirators only purify the air, sufficient oxygen must be present in the surrounding atmosphere to support life in the first place.
Respirator selection involves reviewing each operation to ascertain what dangers may be present (hazard determination) and to select the type or class of respirators that can offer adequate protection.
Hazard Determination Steps
In order to determine the properties of the contaminants that may be present in the workplace, one should consult the key source for this information, namely, the supplier of the material. Many suppliers provide their customers with a material safety data sheet (MSDS) which reports the identity of the materials in a product and supplies information on exposure limits and toxicity as well.
One should determine whether there is a published exposure limit such as a threshold limit value (TLV), permissible exposure limit (PEL), maximum acceptable concentration, (MAK), or any other available exposure limit or estimate of toxicity for the contaminants. It ought to be ascertained whether a value for the immediately dangerous to life or health (IDLH) concentration for the contaminant is available. Each respirator has some use limitation based on the level of exposure. A limit of some sort is needed to determine whether the respirator will provide sufficient protection.
Steps should be taken to discover if there is a legally mandated health standard for the given contaminant (as there is for lead or asbestos). If so, there may be specific respirators required that will help narrow the selection process.
The physical state of the contaminant is an important characteristic. If an aerosol, its particle size should be determined or estimated. The vapour pressure of an aerosol is also significant at the maximum expected temperature of the work environment.
One should determine whether the contaminant present can be absorbed through the skin, produce skin sensitization or be irritating or corrosive to the eyes or skin. It should also be found for a gaseous or vapour contaminant if a known odour, taste or irritation concentration exists.
Once the identity of the contaminant is known, its concentration needs to be determined. This is normally done by collecting the material on a sample medium with subsequent analysis by a laboratory. Sometimes the assessment can be accomplished by estimating exposures, as described below.
Estimating Exposure
Sampling is not always required in hazard determination. Exposures can be estimated by examining data relating to similar tasks or by calculation by means of a model. Models or judgment can be used to estimate the likely maximum exposure and this estimate can be used to select a respirator. (The most basic models suitable to such a purpose is the evaporation model, a given amount of material is either assumed or allowed to evaporate into an air space, its vapour concentration found, and an exposure estimated. Adjustments can be made for dilution effects or ventilation.)
Other possible sources of exposure information are articles in journals or trade publications which present exposure data for various industries. Trade associations and data collected in hygiene programmes for similar processes are also useful for this purpose.
Taking protective action based on estimated exposure involves making a judgement based on experience vis-à-vis the type of exposure. For example, air monitoring data of previous tasks will not be useful in the event of the first occurrence of a sudden break in a delivery line. The possibility of such accidental releases must be anticipated in the first place before the need of a respirator can be decided, and the specific type of respirator chosen can then be made on the basis of the estimated likely concentration and nature of the contaminant. For example, for a process involving toluene at room temperatures, a safety device that offers no more protection than a continuous-flow air line need be chosen, since the concentration of toluene would not be expected to exceed its IDLH level of 2,000 ppm. However, in the case of a break in a sulphur dioxide line, a more effective device—say, an air-supplied respirator with an escape bottle—would be called for, since a leak of this sort could quite readily result in an ambient concentration of contaminant above the IDLH level of 20 ppm. In the next section, respirator selection will be examined in further detail.
Specific Respirator Selection Steps
If one is unable to determine what potentially hazardous contaminant may be present, the atmosphere is considered immediately dangerous to life or health. An SCBA or air line with an escape bottle is then required. Similarly, if no exposure limit or guideline is available and estimates of the toxicity cannot be made, the atmosphere is considered IDLH and an SCBA is required. (See the discussion below on the subject of IDLH atmospheres.)
Some countries have very specific standards governing respirators that can be used in given situations for specific chemicals. If a specific standard exists for a contaminant, the legal requirements must be followed.
For an oxygen-deficient atmosphere, the type of respirator selected depends on the partial pressure and concentration of oxygen and the concentration of the other contaminants that may be present.
Hazard ratio and assigned protection factor
The measured or estimated concentration of a contaminant is divided by its exposure limit or guideline to obtain its hazard ratio. With respect to this contaminant, a respirator is selected that has an assigned protection factor (APF) greater than the value of the hazard ratio (the assigned protection factor is the estimated performance level of a respirator). In many countries, a half mask is assigned an APF of ten. It is assumed that the concentration inside the respirator will be reduced by a factor of ten, that is, the APF of the respirator.
The assigned protection factor can be found in any existent regulations on respirator use or in the American National Standard for Respiratory Protection (ANSI Z88.2 1992). ANSI APFs are listed in table 2.
Table 2. Assigned protection factors from ANSI Z88 2 (1992)
|
Type of respirator |
Respiratory inlet covering |
|||
|
Half mask1 |
Full facepiece |
Helmet/hood |
Loose-fitting facepiece |
|
|
Air-Purifying |
10 |
100 |
||
|
Atmosphere-supplying |
||||
|
SCBA (demand-type)2 |
10 |
100 |
||
|
Airline(demand-type) |
10 |
100 |
||
|
Powered air-purifying |
50 |
10003 |
10003 |
25 |
|
Atmosphere-supplying air-line type |
||||
|
Pressure-fed demand type |
50 |
1000 |
— |
— |
|
Continuous Flow |
50 |
1000 |
1000 |
25 |
|
Self-contained breathing apparatus |
||||
|
Positive pressure (demand open/closed circuit) |
— |
4 |
— |
— |
1 Includes one-quarter mask, disposable half masks and half masks with elastomeric facepieces.
2 Demand SCBA shall not be used for emergency situations such as fire fighting.
3 Protection factors listed are for high efficiency filters and sorbents (cartridges and canisters). With dust filters an assigned protection factor of 100 is to be used due to the limitations of the filter.
4 Although positive pressure respirators are currently regarded as providing the highest level of respiratory protection, a limited number of recent simulated workplace studies concluded that all users may not achieve protection factors of 10,000. Based on this limited data, a definitive assigned protection factor could not be listed for positive pressure SCBAs. For emergency planning purposes where hazardous concentrations can be estimated, an assigned protection factor of no higher than 10,000 should be used.
Note: Assigned protection factors are not applicable for escape respirators. For combination respirators, e.g., air-line respirators equipped with an air-purifying filter, the mode of operation in use will dictate the assigned protection factor to be applied.
Source: ANSI Z88.2 1992.
For example, for a styrene exposure (exposure limit of 50 ppm) with all of the measured data at the worksite less than 150 ppm, the hazard ratio is 3 (that is, 150 ¸ 50 = 3). Selection of a half-mask respirator with an assigned protection factor of 10 will assure that most unmeasured data will be well below the assigned limit.
In some cases where “worst-case” sampling is done or only a few data are collected, judgement must be used to decide if enough data have been collected for an acceptably reliable assessment of exposure levels. For example, if two samples were collected for a short-term task that represents the “worst-case” for that task and both samples were less than two times the exposure limit (a hazard ratio of 2), a half-mask respirator (with an APF of 10) would likely be an appropriate choice and certainly a continuous-flow full facepiece respirator (with an APF of 1,000) would be sufficiently protective. The contaminant’s concentration must also be less than the maximum-use concentration of the cartridge/canister: this latter information is available from the manufacturer of the respirator.
Aerosols, gases and vapours
If the contaminant is an aerosol, a filter will have to be used; the choice of filter will depend on the efficiency of the filter for the particle. The literature provided by the manufacturer will provide guidance on the appropriate filter to use. For example, if the contaminant is a paint, lacquer or enamel, a filter designed specifically for paint mists may be used. Other special filters are designed for fumes or dust particles that are larger than usual.
For gases and vapours, adequate notice of cartridge failure is necessary. Odour, taste or irritation are used as indicators that the contaminant has “broken through” the cartridge. Therefore, the concentration at which the odour, taste or irritation is noted must be less than the exposure limit. If the contaminant is a gas or vapour that has poor warning properties, the use of an atmosphere-supplying respirator is generally recommended.
However, atmosphere-supplying respirators sometimes cannot be used because of the lack of an air supply or because of the need for worker mobility. In this case, air-purifying devices may be used, but it is necessary that it be equipped with an indicator signalling the end of the device’s service life so that the user will be given adequate warning prior to contaminant breakthrough. Another alternative is to use a cartridge change schedule. The change schedule is based on cartridge service data, expected concentration, pattern of use and duration of exposure.
Respirator selection for emergency or IDLH conditions
As noted above, IDLH conditions are presumed to exist when the concentration of a contaminant is not known. Furthermore, it is prudent to consider any confined space containing less than 20.9% oxygen as an immediate danger to life or health. Confined spaces present unique hazards. Lack of oxygen in confined spaces is the cause of numerous deaths and serious injuries. Any reduction in the percentage of oxygen present is proof, at a minimum, that the confined space is not adequately ventilated.
Respirators for use under IDLH conditions at normal atmospheric pressure include either a positive-pressure SCBA alone or a combination of a supplied-air respirator with an escape bottle. When respirators are worn under IDLH conditions, at least one standby person must be present in a safe area. The standby person needs to have the proper equipment available to assist the wearer of the respirator in case of difficulty. Communications have to be maintained between the standby person and the wearer. While working in the IDLH atmosphere, the wearer needs to be equipped with a safety harness and safety lines to permit his or her removal to a safe area, if necessary.
Oxygen-deficient atmospheres
Strictly speaking, oxygen deficiency is a matter only of its partial pressure in a given atmosphere. Oxygen deficiency can be caused by a reduction in the percentage of oxygen in the atmosphere or by reduced pressure, or both reduced concentration and pressure. At high altitudes, reduced total atmospheric pressure can lead to very low oxygen pressure.
Humans need a partial oxygen pressure of approximately 95 mm Hg (torr) to survive. The exact pressure will vary among people depending on their health and acclimatization to reduced oxygen pressure. This pressure, 95 mm Hg, is equivalent to 12.5% oxygen at sea level or 21% oxygen at an altitude of 4,270 meters. Such an atmosphere may adversely affect either the person with reduced tolerance to reduced oxygen levels or the unacclimatized person performing work requiring a high degree of mental acuity or heavy stress.
To prevent adverse effects, supplied-air respirators should be provided at higher oxygen partial pressures, for example, about 120 mm Hg or 16% oxygen content at sea level. A physician should be involved in any decisions where people will be required to work in reduced-oxygen atmospheres. There may be legally mandated levels of oxygen percent or partial pressure that require supplied-air respirators at different levels than these broadly general guidelines suggest.
Suggested Procedures for Fit Testing
Each person assigned a tight-fitting negative-pressure respirator needs to be fit tested periodically. Each face is different, and a specific respirator may not fit a given person’s face. Poor fit would allow contaminated air to leak into the respirator, lowering the amount of protection the respirator provides. A fit test needs to be repeated periodically and must be carried out whenever a person has a condition that may interfere with facepiece sealing, e.g., significant scarring in the area of the face seal, dental changes, or reconstructive or cosmetic surgery. Fit testing has to be done while the subject is wearing protective equipment such as spectacles, goggles, a face shield or a welding helmet that will be worn during work activities and could interfere with respirator fit. The respirator should be configured as it will be used, that is, with a chin canister or cartridge.
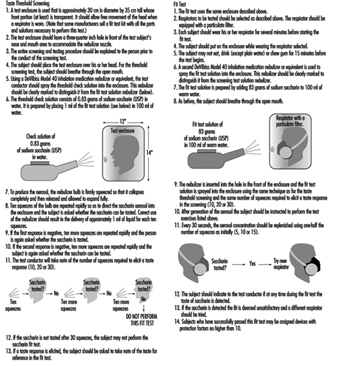
Fit test procedures
Respirator fit testing is conducted to determine if a particular model and size of mask fits an individual’s face. Before the test is made, the subject should be oriented on the respirator’s proper use and donning, and the test’s purpose and procedures should be explained. The person being tested should understand that the he or she is being asked to select the respirator that provides the most comfortable fit. Each respirator represents a different size and shape and, if fit properly and used properly, will provide adequate protection.
No one size or model of respirator will fit all types of faces. Different sizes and models will accommodate a broader range of facial types. Therefore, an appropriate number of sizes and models should be available from which a satisfactory respirator can be selected.
The person being tested should be instructed to hold each facepiece up to the face and eliminate those which obviously do not give a comfortable fit. Normally, selection will begin with a half mask, and if a good fit cannot be found, the person will need to test a full facepiece respirator. (A small percentage of users will not be able to wear any half mask.)
The subject should conduct a negative- or positive-pressure fit check according to the instructions provided by the manufacturer before the test is begun. The subject is now ready for fit testing by one of the methods listed below. Other fit test methods are available, including quantitative fit test methods which use instruments to measure leakage into the respirator. The fit test methods, which are outlined in the boxes here, are qualitative and do not require expensive test equipment. These are (1) the isoamyl acetate (IAA) protocol and (2) the saccharin solution aerosol protocol.
Test exercises. During the fit test, the wearer should carry out a number of exercises in order to verify that the respirator will allow him or her to perform a set of basic and necessary actions. The following six exercises are recommended: standing still, breathing normally, breathing deeply, moving the head from side to side, moving the head up and down, and speaking. (See figure 2 and figure 3).
Figure 2. Isoamly acetate quantitive fit-test method
Figure 3. Sacharin aerosol quantitive fit-test method
Designing for Specific Groups
In designing a product or an industrial process, one focuses on the “average” and “healthy” worker. Information regarding human abilities in terms of muscular strength, bodily flexibility, length of reach, and many other characteristics is for the most part derived from empirical studies carried out by military recruitment agencies, and reflects measured values valid for the typical young male in his twenties. But working populations, to be sure, consist of people of both sexes and a broad range of ages, to say nothing of a variety of physical types and abilities, levels of fitness and health, and functional capacities. A classification of the varieties of functional limitation among people as outlined by the World Health Organization is given in the accompanying article "Case Study: The International Classifcation of Functional Limitation in People." At present, industrial design for the most part takes insufficient account of the general abilities (or inabilities, for that matter) of workers at large, and should take as its point of departure a broader human average as a basis for design. Clearly, a suitable physical load for a 20-year-old may exceed the capacity to manage of a 15-year-old or a 60-year-old. It is the business of the designer to consider such differences not only from the point of view of efficiency, but with a eye to the prevention of job-related injury and illness.
The progress of technology has brought about the state of affairs that, of all the workplaces in Europe and North America, 60% involve the seated position. The physical load in work situations is now on average far less than before, but many worksites, nonetheless, call for physical loads that cannot be sufficiently reduced to fit human physical capabilities; in some developing countries, the resources of current technology are simply not available to relieve the human physical burden to any appreciable extent. And in technologically advanced countries, it is still a common problem that a designer will adapt his or her approach to constraints imposed by product specifications or production processes, either slighting or leaving out human factors related to disability and the prevention of harm due to the workload. With respect to these aims, designers have to be educated to devote attention to all such human factors, expressing the results of their study in a product requirements document (PRD). The PRD contains the system of demands which the designer has to meet in order to achieve both the expected product quality level and the satisfaction of human capability needs in the production process. While it is unrealistic to demand a product that matches a PRD in every respect, given the need of unavoidable compromises, the design method suited to the closest approach to this goal is the system ergonomic design (SED) method, to be discussed following a consideration of two alternative design approaches.
Creative Design
This design approach is characteristic of artists and others involved in the production of work of a high order of originality. The essence of this design process is that a concept is worked out intuitively and through “inspiration”, allowing problems to be dealt with as they arise, without conscious deliberation beforehand. Sometimes, the outcome will not resemble the initial concept, but nonetheless represents what the creator regards as his or her authentic product. Not seldom, too, the design is a failure. Figure 1 illustrates the route of creative design.
System design arose from the need to predetermine the steps in design in a logical order. As design becomes complex, it has to be subdivided into subtasks. Designers or subtask teams thus become interdependent, and design becomes the job of a design team rather than an individual designer. Complementary expertise is distributed through the team, and design assumes an interdisciplinary character.
System design is oriented to the optimal realization of complex and well-defined product functions through the selection of the most appropriate technology; it is costly, but the risks of failure are considerably reduced as compared with less organized approaches. The efficacy of the design is measured against the goals formulated in the PRD.
The way in which the specifications formulated in the PRD are of the first importance. Figure 2 illustrates the relationship between the PRD and other parts of the system design process.
As this scheme shows, the input of the user is neglected. Only at the end of the design process can the user criticize the design. This is unhelpful to both producer and user, since one has to wait for the next design cycle (if there is one) before errors can be corrected and modifications made. Furthermore, user feedback is seldom systematized and imported into a new PRD as a design influence.
System ergonomic design (SED)
SED is a version of system design adapted to ensure that the human factor is accounted for in the design process. Figure 3 illustrates the flow of user input into the PRD.
Figure 3. System ergonomic design
 In system ergonomic design, the human being is considered part of the system: design specification changes are, in fact, made in consideration of the worker’s abilities with respect to cognitive, physical and mental aspects, and the method lends itself as an efficient design approach for any technical system where human operators are employed.
In system ergonomic design, the human being is considered part of the system: design specification changes are, in fact, made in consideration of the worker’s abilities with respect to cognitive, physical and mental aspects, and the method lends itself as an efficient design approach for any technical system where human operators are employed.
For example, to examine the implications of the worker’s physical abilities, task-allocation in the design of the process will call for a careful selection of tasks to be performed by the human operator or by the machine, each task being studied for its aptness to machine or human treatment. Clearly, the human worker will be more effective at interpreting incomplete information; machines however calculate much more rapidly with prepared data; a machine is the choice for lifting heavy loads; and so forth. Furthermore, since the user-machine interface can be tested at the prototype phase, one can eliminate design errors that would otherwise untimely manifest themselves at the phase of technical functioning.
Methods in User Research
No “best” method exists, nor any source of formulae and sure and certain guidelines, according to which design for disabled workers ought to be undertaken. It is a rather a common-sense business of making as exhaustive search of all obtainable knowledge relevant to the problem and of implementing it to its most evident best effect.
Information can be assembled from sources such as the following:
- The literature of research results.
- Direct observation of the disabled person at work and description of his or her particular work difficulties. Such observation should be made at a point in the worker’s schedule when he or she can be expected to be subject to fatigue—the end of a work shift, perhaps. The point is that any design solutions should be adapted to the most arduous phase of the work process, or else such phases may fail to be performed adequately (or at all) owing to the worker’s capacity having been physically exceeded.
- The interview. One has to be aware of the possibly subjective responses which the interview per se may have the effect of eliciting. It is a far better approach that the interview technique be combined with observation. Disabled persons sometimes hesitate to discuss their difficulties, but when workers are aware that the investigator is willing to exert special thoroughness on their behalf, their reticence will diminish. This technique is time-consuming, but quite worthwhile.
- Questionnaires. An advantage of the questionnaire is that it can be distributed to large groups of respondents and at the same time gather data of as specific a sort as one wishes to provide for. The questionnaire must, however, be constructed upon the basis of representative information pertaining to the group to which it will be administered. This means that the type of information to be sought must be obtained on the basis of interviews and observations carried out among a sample of workers and specialists that ought to be reasonably restricted as to size. In the case of disabled persons, it is sensible to include among such a sample the physicians and therapists who are involved with prescribing special aids for disabled persons and have examined them regarding their physical capabilities.
- Physical measurements. Measurements obtained from instruments in the field of bio-instrumentation (e.g., the activity level of muscles, or the amount of oxygen consumed in a given task) and by anthropometrical methods (e.g., the linear dimensions of body elements, the range of motion of limbs, muscular strength) are of indispensable value in human-oriented work designs.
The methods described above are some of the various ways of gathering data about people. Methods exist, too, to evaluate user-machine systems. One of these—simulation—is to construct a realistic physical copy. The development of a more or less abstract symbolic representation of a system is an example of modelling. Such expedients, of course, are both useful and necessary when the actual system or product is not in existence or not accessible to experimental manipulation. Simulation is more often used for training purposes and modelling for research. A mock-up is a full-size, three-dimensional copy of the designed workplace composed, where necessary, of improvised materials, and is of great use in testing design possibilities with the proposed disabled worker: in fact, the majority of design problems can be identified with the aid of such a device. Another advantage to this approach is that the motivation of the worker grows as he or she participates in the design of his or her own future workstation.
Analysis of Tasks
In the analysis of tasks, different aspects of a defined job are subject to analytical observation. These manifold aspects include posture, routing of work manipulations, interactions with other workers, handling tools and operating machines, the logical order of subtasks, the efficiency of operations, static conditions (a worker may have to perform tasks in the same posture over a long time or with high frequency), dynamic conditions (calling for numerous varying physical conditions), material environmental conditions (as in a cold slaughterhouse) or non-material conditions (as with stressful work surroundings or the organization of the work itself).
Work design for the disabled person has, then, to be founded on a thorough task analysis as well as a full examination of the functional abilities of the disabled person. The basic design approach is a crucial issue: it is more efficient to elaborate all possible solutions for the problem in hand without prejudice than to produce a single design concept or a limited number of concepts. In design terminology, this approach is called making a morphological overview. Given the multiplicity of original design concepts, one can proceed to an analysis of the pro and con features of each possibility with respect to material use, construction method, technical production features, ease of manipulation, and so on. It is not unprecedented that more than one solution reaches the prototype stage and that a final decision is made at a relatively late phase in the design process.
Although this may seem a time-consuming way to realize design projects, in fact the extra work it entails is compensated for in terms of fewer problems encountered in the developmental stage, to say nothing that the result—a new workstation or product—will have embodied a better balance between the needs of the disabled worker and the exigencies of the working environment. Unfortunately, the latter benefit rarely if ever reaches the designer in terms of feedback.
Product Requirements Document (PRD) and Disability
After all information relating to a product has been assembled, it should be transformed into a description not only of the product but of all those demands which may be made of it, regardless of source or nature. These demands may of course be divided along various lines. The PRD should include demands relating to user-operator data (physical measurements, range of motion, range of muscular strength, etc.), technical data (materials, construction, production technique, safety standards, etc.), and even conclusions arising out of market feasibility studies.
The PRD forms the designer’s framework, and some designers regard it as an unwelcome restriction of their creativity rather than as a salutary challenge. In view of the difficulties at times accompanying the execution of a PRD, it should always be borne steadily in mind that a design failure causes distress for the disabled person, who may relinquish his or her efforts to succeed in the employment arena (or else fall helpless victim to the progress of the disabling condition), and additional costs for redesign as well. To this end, technical designers should not operate alone in their design work for the disabled, but should cooperate with whatever disciplines are needed for securing the medical and functional information to set up an integrated PRD as a framework for the design.
Prototype Testing
When a prototype is built, it should be tested for errors. Error testing should be carried out not only from the point of view of the technical system and subsystems, but also with a view to its usability in combination with the user. When the user is a disabled person, extra precautions have to be taken. An error to which an unimpaired worker may successfully respond in safety may not afford the disabled worker the opportunity of avoiding harm.
Prototype testing should be carried out on a small number of disabled workers (except in the case of a unique design) according to a protocol matched to the PRD. Only by such empirical testing can the degree to which the design meets the demands of the PRD be adequately judged. Although results on small numbers of subjects may not be generalizable to all cases, they do supply valuable information for the designer’s use in either the final design or in future designs.
Evaluation
The evaluation of a technical system (a work situation, machine or tool) should be judged on its PRD, not by questioning the user or even by attempting comparisons of alternative designs with respect to physical performance. For instance, the designer of a specific knee brace, basing his or her design on research results that show unstable knee joints to exhibit a delayed hamstring reaction, will create a product that compensates for this delay. But another brace may have different design aims. Yet present evaluation methods show no insight as to when to prescribe what kind of knee brace to which patients under what conditions—precisely the sort of insight a health professional needs when prescribing technical aids in the treatment of disabilities.
Current research aims at making this sort of insight possible. A model used to obtain insight into those factors which actually determine whether or not a technical aid ought to be used, or whether or not a worksite is well designed and equipped for the disabled worker is the Rehabilitation Technology Useability Model (RTUM). The RTUM model offers a framework to use in evaluations of existing products, tools or machines, but can also be used in combination with the design process as shown in figure 4.
Figure 4. Rehabilitation Technology Useability Model (RTUM) in combination with the system ergonomic design approach
Evaluations of existing products reveal that as regards technical aids and worksites, the quality of PRDs is very poor. At some times, the product requirements are not recorded properly; at others they are not developed to a useful extent. Designers simply must learn to start documenting their product requirements, including those relevant to disabled users. Note that, as figure 4 shows, RTUM, in conjunction with SED, offers a framework that includes the requirements of disabled users. Agencies responsible for prescribing products for their users must request industry to evaluate those products before marketing them, a task in essence impossible in the absence of product requirement specifications; figure 4 also shows how provision can be made to ensure that the end result can be evaluated as it should (on a PRD) with the help of the disabled person or group for whom the product is intended. It is up to national health organizations to stimulate designers to abide by such design standards and to formulate appropriate regulations.
Occupational Disease Surveillance and Reporting Systems
Occupational disease and injury surveillance entails the systematic monitoring of health events in working populations in order to prevent and control occupational hazards and their associated diseases and injuries. Occupational disease and injury surveillance has four essential components (Baker, Melius and Millar 1988; Baker 1986).
- Gather information on cases of occupational diseases and injuries.
- Distil and analyse the data.
- Disseminate organized data to necessary parties, including workers, unions, employers, governmental agencies and the public.
- Intervene on the basis of data to alter the factors that produced these health events.
Surveillance in occupational health has been more concisely described as counting, evaluating and acting (Landrigan 1989).
Surveillance commonly refers to two broad sets of activities in occupational health. Public health surveillance refers to activities undertaken by federal, state or local governments within their respective jurisdictions to monitor and to follow up on occupational diseases and injuries. This type of surveillance is based on a population, that is, the working public. The recorded events are suspected or established diagnoses of occupational illness and injury. This article will examine these activities.
Medical surveillance refers to the application of medical tests and procedures to individual workers who may be at risk for occupational morbidity, to determine whether an occupational disorder may be present. Medical surveillance is generally broad in scope and represents the first step in ascertaining the presence of a work-related problem. If an individual or a population is exposed to a toxin with known effects, and if the tests and procedures are highly targeted to detect the likely presence of one or more effects in these persons, then this surveillance activity is more aptly described as medical screening (Halperin and Frazier 1985). A medical surveillance programme applies tests and procedures on a group of workers with common exposures for the purpose of identifying individuals who may have occupational illnesses and for the purpose of detecting patterns of illness which may be produced by occupational exposures among the programme participants. Such a programme is usually undertaken under the auspices of the individual’s employer or union.
Functions of Occupational Health Surveillance
Foremost among the purposes of occupational health surveillance is to identify the incidence and prevalence of known occupational diseases and injuries. Gathering descriptive epidemiological data on the incidence and prevalence of these diseases on an accurate and comprehensive basis is an essential prerequisite for establishing a rational approach to the control of occupational disease and injury. Assessment of the nature, magnitude and distribution of occupational disease and injury in any geographic area requires a sound epidemiological database. It is only through an epidemiological assessment of the dimensions of occupational disease that its importance relative to other public health problems, its claim for resources and the urgency of legal standard setting can be reasonably evaluated. Second, the collection of incidence and prevalence data allows analysis of trends of occupational disease and injury among different groups, at different places and during different time periods. Detecting such trends is useful for determining control and research priorities and strategies, and for evaluating the effectiveness of any interventions undertaken (Baker, Melius and Millar 1988).
A second broad function of occupational health surveillance is to identify individual cases of occupational disease and injury in order to find and evaluate other individuals from the same workplaces who may be at risk for similar disease and injury. Also, this process permits the initiation of control activities to ameliorate the hazardous conditions associated with causation of the index case (Baker, Melius and Millar 1988; Baker, Honchar and Fine 1989).An index case of occupational disease or injury is defined as the first ill or injured individual from a given workplace to receive medical care and thereby to draw attention to the existence of a workplace hazard and an additional workplace population at risk. A further purpose of case identification may be to assure that the affected individual receives appropriate clinical follow-up, an important consideration in view of the scarcity of clinical occupational medicine specialists (Markowitz et al. 1989; Castorino and Rosenstock 1992).
Finally, occupational health surveillance is an important means of discovering new associations between occupational agents and accompanying diseases, since the potential toxicity of most chemicals used in the workplace is not known. Discovery of rare diseases, patterns of common diseases or suspicious exposure-disease associations through surveillance activities in the workplace can provide vital leads for a more conclusive scientific evaluation of the problem and possible verification of new occupational diseases.
Obstacles to the Recognition of Occupational Diseases
Several important factors undermine the ability of occupational disease surveillance and reporting systems to fulfil the functions cited above. First, recognition of the underlying cause or causes of any illness is the sine qua non for recording and reporting occupational diseases. However, in a traditional medical model that emphasizes symptomatic and curative care, identifying and eliminating the underlying cause of illness may not be a priority. Furthermore, health care providers are often not adequately trained to suspect work as a cause of disease (Rosenstock 1981) and do not routinely obtain histories of occupational exposure from their patients (Institute of Medicine 1988). This should not be surprising, given that in the United States, the average medical student receives only six hours of training in occupational medicine during the four years of medical school (Burstein and Levy 1994).
Certain features characteristic of occupational disease exacerbate the difficulty of recognizing occupational diseases. With few exceptions—most notably, angiosarcoma of the liver, malignant mesothelioma and the pneumoconioses—most diseases that can be caused by occupational exposures also have non-occupational causes. This non-specificity renders difficult the determination of the occupational contribution to disease occurrence. Indeed, the interaction of occupational exposures with other risk factors may greatly increase the risk of disease, as occurs with asbestos exposure and cigarette smoking. For chronic occupational diseases such as cancer and chronic respiratory disease, there usually exists a long period of latency between onset of occupational exposure and presentation of clinical disease. For example, malignant mesothelioma typically has a latency of 35 years or more. A worker so affected may well have retired, further diminishing a physician’s suspicion of possible occupational aetiologies.
Another cause of the widespread under-recognition of occupational disease is that the majority of chemicals in commerce have never been evaluated with regard to their potential toxicity. A study by the National Research Council in the United States in the 1980s found no information available on the toxicity of approximately 80% of the 60,000 chemical substances in commercial use. Even for those groups of substances that are most closely regulated and about which the most information is available—drugs and food additives—reasonably complete information on possibly untoward effects is available for only a minority of agents (NRC 1984).
Workers may have a limited ability to provide an accurate report of their toxic exposures. Despite some improvement in countries such as the United States in the 1980s, many workers are not informed of the hazardous nature of the materials with which they work. Even when such information is provided, recalling the extent of exposure to multiple agents in a variety of jobs over a working career may be difficult. As a result, even health care providers who are motivated to obtain occupational information from their patients may not be able to do so.
Employers may be an excellent source of information regarding occupational exposures and the occurrence of work-related diseases. However, many employers do not have the expertise to assess the extent of exposure in the workplace or to determine whether an illness is work related. In addition, financial disincentives to finding that a disease is occupational in origin may discourage employers from using such information appropriately. The potential conflict of interest between the financial health of the employer and the physical and mental health of the worker represents a major obstacle to improving surveillance of occupational disease.
Registries and other Data Sources Specific for Occupational Diseases
International registries
International registries for occupational diseases are an exciting development in occupational health. The obvious benefit of these registries is the ability to conduct large studies, which would allow determination of the risk of rare diseases. Two such registries for occupational diseases were initiated during the 1980s.
The International Agency for Research on Cancer (IARC) established the International Register of Persons Exposed to Phenoxy Herbicides and Contaminants in 1984 (IARC 1990). As of 1990, it had enrolled 18,972 workers from 19 cohorts in ten countries. By definition all enrolees worked in industries involving phenoxy herbicides and/or chlorophenols, principally in manufacturing/formulating industries or as applicators. Exposure estimates have been made for participating cohorts (Kauppinen et al. 1993), but analyses of cancer incidence and mortality have not yet been published.
An international registry of cases of angiosarcoma of the liver (ASL) is being coordinated by Bennett of ICI Chemicals and Polymers Limited in England. Occupational exposure to vinyl chloride is the only known cause of angiosarcoma of the liver. Cases are reported by a voluntary group of scientists from companies producing vinyl chloride, governmental agencies and universities. As of 1990, 157 cases of ASL with dates of diagnosis between 1951 and 1990 were reported to the registry from 11 countries or regions. Table 1 also shows that most of the recorded cases were reported from countries where facilities started polyvinyl chloride manufacture before 1950. The registry has recorded six clusters of ten or more cases of ASL at facilities in North America and Europe (Bennett 1990).
Table 1. Number of cases of angiosarcoma of the liver in the world register by country and year of first production of vinyl chloride
|
Country/Region |
Number of PVC |
Year PVC production initiated |
Number of cases |
|
USA |
50 |
(1939?) |
39 |
|
Canada |
5 |
(1943) |
13 |
|
West Germany |
10 |
(1931) |
37 |
|
France |
8 |
(1939) |
28 |
|
United Kingdom |
7 |
(1940) |
16 |
|
Other Western Europe |
28 |
(1938) |
15 |
|
Eastern Europe |
23 |
(pre-1939) |
6 |
|
Japan |
36 |
(1950) |
3 |
|
Central and |
22 |
(1953) |
0 |
|
Australia |
3 |
(1950s) |
0 |
|
Middle East |
1 |
(1987) |
0 |
|
Total |
193 |
157 |
Source: Bennett, B. World Register of Cases of Angiosarcoma of the Liver (ASL)
due to Vinyl Chloride Monomer, January 1, 1990.
Governmental surveys
Employers are sometimes legally required to record occupational injuries and illnesses that occur in their facilities. Like other workplace-based information, such as numbers of employees, wages and overtime, injury and illness data may be systematically collected by governmental agencies for the purpose of surveillance of work-related health outcomes.
In the United States, the Bureau of Labor Statistics (BLS) of the US Department of Labor has conducted the Annual Survey of Occupational Injuries and Illnesses (BLS Annual Survey) since 1972 as required by the Occupational Safety and Health Act (BLS 1993b). The goal of the survey is to obtain the numbers and the rates of illnesses and injuries recorded by private employers as being occupational in origin (BLS 1986). The BLS Annual Survey excludes employees of farms with fewer than 11 employees, the self-employed and employees of the federal, state and local governments. For the most recent year available, 1992, the survey reflects questionnaire data obtained from a stratified random sample of approximately 250,000 establishments in the private sector in the United States (BLS 1994).
The BLS survey questionnaire completed by the employer is derived from a written record of occupational injuries and illnesses which employers are required to maintain by the Occupational Safety and Health Administration (OSHA 200 Log). Although OSHA mandates that the employer keep the 200 Log for examination by an OSHA inspector upon request, it does not require that employers routinely report the log’s contents to OSHA, except for the sample of employers included in the BLS Annual Survey (BLS 1986).
Some well-recognized weaknesses severely limit the ability of the BLS survey to provide a full and accurate count of occupational illnesses in the United States (Pollack and Keimig 1987). Data are employer derived. Any illness that the employee does not report to the employer as being work related will not be reported by the employer on the annual survey. Among active workers, such a failure to report may be due to fear of consequences to the employee. Another major obstacle to reporting is the failure of the employee’s physician to diagnose illness as being work related, especially for chronic diseases. Occupational diseases occurring among retired workers are not subject to the BLS reporting requirement. Indeed, it is unlikely that the employer would be aware of the onset of a work-related illness in a retiree. Since many cases of chronic occupational illnesses with long latency, including cancer and lung disease, are likely to have their onset following retirement, a large proportion of such cases would not be included in the data collected by the BLS. These limitations were recognized by BLS in a recent report on its annual survey (BLS 1993a). In response to recommendations by the National Academy of Sciences, the BLS re-designed and implemented a new annual survey in 1992.
According to the 1992 BLS Annual Survey, there were 457,400 occupational illnesses in private industry in the United States (BLS 1994). This represented a 24% increase, or 89,100 cases, over the 368,300 illnesses recorded in the 1991 BLS Annual Survey. The incidence of new occupational illnesses was 60.0 per 10,000 workers in 1992.
Disorders associated with repeated trauma, such as carpal tunnel syndrome, tendonitis of the wrist and elbow and hearing loss, dominate the occupational illnesses recorded in the BLS Annual survey and have done so since 1987 (table 2). In 1992, they accounted for 62% of all illness cases recorded on the annual survey. Other important categories of disease were skin disorders, pulmonary diseases and disorders associated with physical trauma.
Table 2. Number of new cases of occupational illness by category of illness-US Bureau of Labor Statistics Annual Survey, 1986 versus 1992.
|
Category of Illness |
1986 |
1992 |
% Change 1986–1992 |
|
Skin diseases |
41,900 |
62,900 |
+ 50.1% |
|
Dust diseases of the lungs |
3,200 |
2,800 |
– 12.5% |
|
Respiratory conditions due to toxic agents |
12,300 |
23,500 |
+ 91.1% |
|
Poisonings |
4,300 |
7,000 |
+ 62.8% |
|
Disorders due to physical agents |
9,200 |
22,200 |
+141.3% |
|
Disorders associated with repeated trauma |
45,500 |
281,800 |
+519.3% |
|
All other occupational illnesses |
20,400 |
57,300 |
+180.9% |
|
Total |
136,900 |
457,400 |
+234.4% |
|
Total excluding repeated trauma |
91,300 |
175,600 |
+ 92.3% |
|
Average annual employment in the private sector, United States |
83,291,200 |
90,459,600 |
+ 8.7% |
Sources: Occupational Injuries and Illnesses in the United States by Industry, 1991.
US Department of Labor, Bureau of Labor Statistics, May 1993. Unpublished data,
US Department of Labor, Bureau of Labor Statistics, December, 1994.
Although disorders associated with repeated trauma clearly account for the largest proportion of the increase in cases of occupational illness, there was also a 50% increase in the recorded incidence in occupational illnesses other than those due to repeated trauma in the six years between 1986 and 1992, during which employment in the United States rose by just 8.7%.
These increases in the numbers and rates of occupational diseases recorded by employers and reported to the BLS in recent years in the United States are remarkable. The rapid change in the recording of occupational illnesses in the United States is due to a change in the underlying occurrence of disease and to a change in the recognition and reporting of these conditions. By comparison, during the same time period, 1986 to 1991, the rate of occupational injuries per 100 full-time workers recorded by the BLS went from 7.7 in 1986 to 7.9 in 1991, a mere 2.6% increase. The number of recorded fatalities in the workplace has likewise not increased dramatically in the first half of the 1990s.
Employer-based surveillance
Apart from the BLS survey, many US employers conduct medical surveillance of their workforces and thereby generate a vast amount of medical information that is relevant to the surveillance of occupational diseases. These surveillance programmes are undertaken for numerous purposes: to comply with OSHA regulations; to maintain a healthy workforce through the detection and treatment of non-occupational disorders; to ensure that the employee is fit to perform the tasks of the job, including the need to wear a respirator; and to conduct epidemiological surveillance to uncover patterns of exposure and disease. These activities utilize considerable resources and could potentially make a major contribution to the public health surveillance of occupational diseases. However, since these data are non-uniform, of uncertain quality and largely inaccessible outside the companies in which they are collected, their exploitation in occupational health surveillance has been realized on only a limited basis (Baker, Melius and Millar 1988).
OSHA also requires that employers perform selected medical surveillance tests for workers exposed to a limited number of toxic agents. Additionally, for fourteen well-recognized bladder and lung carcinogens, OSHA requires a physical examination and occupational and medical histories. The data collected under these OSHA provisions are not routinely reported to governmental agencies or other centralized data banks and are not accessible for the purposes of occupational disease reporting systems.
Surveillance of public employees
Occupational disease reporting systems may differ for public versus private employees. For example, in the United States, the annual survey of occupational illnesses and injuries conducted by the federal Department of Labor (BLS Annual Survey) excludes public employees. Such workers are, however, an important part of the workforce, representing approximately 17% (18.4 million workers) of the total workforce in 1991. Over three-fourths of these workers are employed by state and local governments.
In the United States, data on occupational illnesses among federal employees are collected by the Federal Occupational Workers’ Compensation Program. In 1993, there were 15,500 occupational disease awards to federal workers, yielding a rate of 51.7 cases of occupational illnesses per 10,000 full-time workers (Slighter 1994). At the state and local levels, the rates and numbers of illnesses due to occupation are available for selected states. A recent study of state and local employees in New Jersey, a sizeable industrial state, documented 1,700 occupational illnesses among state and local employees in 1990, yielding an incidence of 50 per 10,000 public-sector workers (Roche 1993). Notably, the rates of occupational disease among federal and non-federal public workers are remarkably congruent with the rates of such illness among private sector workers as recorded in the BLS Annual Survey. The distribution of illness by type differs for public versus private workers, a consequence of the different type of work that each sector performs.
Workers’ compensation reports
Workers’ compensation systems provide an intuitively appealing surveillance tool in occupational health, because the determination of work-relatedness of disease in such cases has presumably undergone expert review. Health conditions that are acute and easily recognized in origin are frequently recorded by workers’ compensation systems. Examples include poisonings, acute inhalation of respiratory toxins and dermatitis.
Unfortunately, the use of workers’ compensation records as a credible source for surveillance data is subject to severe limitations, including lack of standardization of eligibility requirements, deficiency of standard case definitions, disincentives to workers and employers to file claims, the lack of physician recognition of chronic occupational diseases with long latent periods and the usual gap of several years between initial filing and resolution of a claim. The net effect of these limitations is that there is significant under-recording of occupational disease by workers’ compensation systems.
Thus, in a study by Selikoff in the early 1980s, less than one-third of US insulators who were disabled by asbestos-related diseases, including asbestosis and cancer, had even filed for workers’ compensation benefits, and many fewer were successful in their claims (Selikoff 1982). Similarly, a US Department of Labor study of workers who reported disability from occupational disease found that less than 5% of these workers received workers’ compensation benefits (USDOL 1980). A more recent study in the state of New York found that the number of people admitted to hospitals for pneumoconioses vastly outnumbered the people who were newly awarded workers’ compensation benefits during a similar time period (Markowitz et al. 1989). Since workers’ compensation systems record simple health events such as dermatitis and musculoskeletal injuries much more readily than complex diseases of long latency, use of such data leads to a skewed picture of the true incidence and distribution of occupational diseases.
Laboratory reports
Clinical laboratories can be an excellent source of information on excessive levels of selected toxins in body fluids. Advantages of this source are timely reporting, quality-control programmes already in place and the leverage for compliance provided by the licensing of such laboratories by governmental agencies. In the United States, numerous states require that clinical laboratories report the results of selected categories of specimens to the state health departments. Occupational agents subject to this reporting requirement are lead, arsenic, cadmium and mercury as well as substances reflecting pesticide exposure (Markowitz 1992).
In the United States, the National Institute for Occupational Safety and Health (NIOSH) began to assemble the results of adult blood lead testing into the Adult Blood Lead Epidemiology and Surveillance programme in 1992 (Chowdhury, Fowler and Mycroft 1994). By the end of 1993, 20 states, representing 60% of the US population, were reporting elevated blood lead levels to NIOSH, and an additional 10 states were developing the capacity to collect and report blood lead data. In 1993, there were 11,240 adults with blood lead levels that equalled or exceeded 25 micrograms per decilitre of blood in the 20 reporting states. The vast majority of these individuals with elevated blood lead levels (over 90%) were exposed to lead at the workplace. Over one-quarter (3,199) of these individuals had blood leads greater than or equal to 40 ug/dl, the threshold at which the US Occupational Safety and Health Administration requires actions to protect workers from occupational lead exposure.
Reporting of elevated levels of toxins to the state health department may be followed by a public health investigation. Confidential follow-up interviews with affected individuals allows timely identification of the workplaces where exposure occurred, categorization of the case by occupation and industry, estimation of the number of other workers at the workplace potentially exposed to lead and assurance of medical follow-up (Baser and Marion 1990). Worksite visits are followed by recommendations for voluntary actions to reduce exposure or may lead to reporting to authorities with legal enforcement powers.
Physicians’ reports
In an attempt to replicate the strategy successfully utilized for the monitoring and control of infectious diseases, an increasing number of states in the United States require physicians to report one or more occupational diseases (Freund, Seligman and Chorba 1989). As of 1988, 32 states required reporting of occupational diseases, though these included ten states where only one occupational disease is reportable, usually lead or pesticide poisoning. In other states, such as Alaska and Maryland, all occupational diseases are reportable. In most states, reported cases are used only to count the number of people in the state affected by the disease. In only one-third of the states with reportable disease requirements does a report of a case of occupational disease lead to follow-up activities, such as workplace inspection (Muldoon, Wintermeyer and Eure 1987).
Despite the evidence of increased recent interest, physician reporting of occupational diseases to appropriate state governmental authorities is widely acknowledged to be inadequate (Pollack and Keimig 1987; Wegman and Froines 1985). Even in California, where a system for physician reporting has been in place for a number of years (Doctor’s First Report of Occupational Illness and Injury) and recorded nearly 50,000 occupational illnesses in 1988, physician compliance with reporting is regarded as incomplete (BLS 1989).
A promising innovation in occupational health surveillance in the United States is the emergence of the concept of the sentinel provider, part of an initiative undertaken by NIOSH called Sentinel Event Notification System for Occupational Risks (SENSOR). A sentinel provider is a physician or other health care provider or facility that is likely to provide care for workers with occupational disorders due to the provider’s specialty or geographic location.
Since sentinel providers represent a small subset of all health care providers, health departments can feasibly organize an active occupational disease reporting system by performing outreach, offering education and providing timely feedback to sentinel providers. In a recent report from three states participating in the SENSOR programme, physician reports of occupational asthma increased sharply after the state health departments developed concerted educational and outreach programmes to identify and recruit sentinel providers (Matte, Hoffman and Rosenman 1990).
Specialized occupational health clinical facilities
A newly emergent resource for occupational health surveillance has been the development of occupational health clinical centres that are independent of the workplace and that specialize in the diagnosis and treatment of occupational disease. Several dozen such facilities currently exist in the United States. These clinical centres can play several roles in enhancing occupational health surveillance (Welch 1989). First, the clinics can play a primary role in case-finding—that is, identifying occupational sentinel health events—since they represent a unique organizational source of expertise in clinical occupational medicine. Second, the occupational health clinical centres can serve as a laboratory for the development and refinement of surveillance case definitions for occupational disease. Third, the occupational health clinics can serve as a primary clinical referral resource for the diagnosis and evaluation of workers who are employed at a worksite where an index case of occupational disease has been identified.
Occupational health clinics have become organized into a national association in the United States (the Association of Occupational and Environmental Clinics) to enhance their visibility and to collaborate on research and clinical investigations (Welch 1989). In some states, such as New York, a statewide network of clinical centres has been organized by the state health department and receives stable funding from a surcharge on workers’ compensation premiums (Markowitz et al. 1989). The clinical centres in New York State have collaborated in the development of information systems, clinical protocols and professional education and are beginning to generate substantial data on the numbers of cases of occupational disease in the state.
Use of Vital Statistics and Other General Health Data
Death certificates
The death certificate is a potentially very useful instrument for occupational disease surveillance in many countries in the world. Most countries have death registries. Uniformity and comparability is promoted by the common use of the International Classification of Diseases to identify cause of death. Furthermore, many jurisdictions include information on death certificates concerning the occupation and industry of the deceased. A major limitation in the use of death certificates for occupational disease surveillance is the lack of unique relationships between occupational exposures and specific causes of death.
The use of mortality data for occupational disease surveillance is most salient for diseases that are uniquely caused by occupational exposures. These include the pneumoconioses and one type of cancer, malignant mesothelioma of the pleura. Table 3 shows the numbers of deaths attributed to these diagnoses as the underlying cause of death and as one of multiple causes of death listed on the death certificate in the United States. The underlying cause of death is considered the principal cause for death, while the listing of multiple causes includes all conditions considered important in contributing to death.
Table 3. Deaths due to pneumoconiosis and malignant mesothelioma of the pleura. Underlying cause and multiple causes, United States, 1990 and 1991
|
ICD-9 Code |
Cause of death |
Numbers of deaths |
|
|
Underlying cause 1991 |
Multiple causes 1990 |
||
|
500 |
Coal workers’ pneumoconiosis |
693 |
1,990 |
|
501 |
Asbestosis |
269 |
948 |
|
502 |
Silicosis |
153 |
308 |
|
503-505 |
Other pneumoconioses |
122 |
450 |
|
Sub-total |
1,237 |
3,696 |
|
|
163.0, 163.1, and 163.9 |
Malignant mesothelioma pleura |
452 |
553 |
|
Total |
1,689 |
4,249 |
|
Source: United States National Center for Health Statistics.
In 1991, there were 1,237 deaths due to the dust diseases of the lung as the underlying cause, including 693 deaths due to coal workers pneumoconioses and 269 deaths due to asbestosis. For malignant mesothelioma, there was a total of 452 deaths due to pleural mesothelioma. It is not possible to identify the number of deaths due to malignant mesothelioma of the peritoneum, also caused by occupational exposure to asbestos, since International Classification of Disease codes are not specific for malignant mesothelioma of this site.
Table 3 also shows the numbers of deaths in the United States in 1990 due to pneumoconioses and malignant mesothelioma of the pleura when they appear as one of multiple causes of death on the death certificate. For the pneumoconioses, the total where they appear as one of multiple causes is important, since the pneumoconioses often co-exist with other chronic lung diseases.
An important issue is the extent to which pneumoconioses may be under-diagnosed and, therefore, missing from death certificates. The most extensive analysis of the under-diagnosis of a pneumoconiosis has been performed among insulators in the United States and Canada by Selikoff and colleagues (Selikoff, Hammond and Seidman 1979; Selikoff and Seidman 1991). Between 1977 and 1986, there were 123 insulator deaths ascribed to asbestosis on the death certificates. When investigators reviewed medical records, chest radiographs and tissue pathology where available, they ascribed 259 of insulator deaths occurring in these years to asbestosis. Over one-half of pneumoconiosis deaths were, thus, missed in this group well-known to have heavy asbestos exposure. Unfortunately, there are not a sufficient number of other studies of the under-diagnosis of pneumoconioses on death certificates to allow a reliable correction of mortality statistics.
Deaths due to causes that are not specific to occupational exposures have also been used as part of occupational disease surveillance when occupation or industry of decedents is recorded on the death certificates. Analysis of these data in a specified geographical area during a selected time period can yield rates and ratios of disease by cause for different occupations and industries. The role of non-occupational factors in the deaths examined cannot be defined by this approach. However, differences in rates of disease in different occupations and industries suggest that occupational factors may be important and provide leads for more detailed studies. Other advantages of this approach include the ability to study occupations that are usually distributed among many workplaces (e.g., cooks or dry cleaner workers), the use of routinely collected data, a large sample size, relatively low expense and an important health outcome (Baker, Melius and Millar 1988; Dubrow, Sestito and Lalich 1987; Melius, Sestito and Seligman 1989).
Such occupational mortality studies have been published over the past several decades in Canada (Gallagher et al. 1989), Great Britain (Registrar General 1986), and the United States (Guralnick 1962, 1963a and 1963b). In recent years, Milham utilized this approach to examine the occupational distribution of all men who died between 1950 and 1979 in the state of Washington in the United States. He compared the proportion of all deaths due to any specific cause for one occupational group with the relevant proportion for all occupations. Proportional mortality ratios are thereby obtained (Milham 1983). As an example of the yield of this approach, Milham noted that 10 of 11 occupations with probable exposure to electrical and magnetic fields showed an elevation in the proportional mortality ratio for leukaemia (Milham 1982). This was one of the first studies of the relationship between occupational exposure to electro-magnetic radiation and cancer and has been followed by numerous studies that have corroborated the original finding (Pearce et al. 1985; McDowell 1983; Linet, Malker and McLaughlin 1988).
As a result of a cooperative effort between NIOSH, the National Cancer Institute, and the National Center for Health Statistics during the 1980s, analyses of the mortality patterns by occupation and industry between 1984 and 1988 in 24 states in the United States have recently been published (Robinson et al. 1995). These studies evaluated 1.7 million deaths. They confirmed several well-known exposure-disease relationships and reported new associations between selected occupations and specific causes of death. The authors emphasize that occupational mortality studies may be useful to develop new leads for further study, to evaluate results of other studies and to identify opportunities for health promotion.
More recently, Figgs and colleagues at the US National Cancer Institute used this 24-state occupational mortality database to examine occupational associations with non-Hodgkin’s lymphoma (NHL) (Figgs, Dosemeci and Blair 1995). A case-control analysis involving approximately 24,000 NHL deaths occurring between 1984 and 1989 confirmed previously demonstrated excess risks of NHL among farmers, mechanics, welders, repairmen, machine operators and a number of white-collar occupations.
Hospital discharge data
Diagnoses of hospitalized patients represent an excellent source of data for the surveillance of occupational diseases. Recent studies in several states in the United States show that hospital discharge data can be more sensitive than workers’ compensation records and vital statistics data in detecting cases of diseases that are specific to occupational settings, such as the pneumoconioses (Markowitz et al. 1989; Rosenman 1988). In New York State, for example, an annual average of 1,049 people were hospitalized for pneumoconioses in the mid-1980s, compared to 193 newly awarded workers’ compensation cases and 95 recorded deaths from these diseases each year during a similar time interval (Markowitz et al. 1989).
In addition to providing a more accurate count of the number of people ill with selected serious occupational diseases, hospital discharge data can be usefully followed up to detect and to alter workplace conditions that caused the disease. Thus, Rosenman evaluated workplaces in New Jersey where individuals who were hospitalized for silicosis had previously worked and found that the majority of these workplaces had never performed air sampling for silica, had never been inspected by the federal regulatory authority (OSHA) and did not perform medical surveillance for the detection of silicosis (Rosenman 1988).
Advantages of using hospital discharge data for the surveillance of occupational disease are their availability, low cost, relative sensitivity to serious illness and reasonable accuracy. Important disadvantages include the lack of information on occupation and industry and uncertain quality control (Melius, Sestito and Seligman 1989; Rosenman 1988). In addition, only individuals with disease sufficiently severe to require hospitalization will be included in the database and, therefore, cannot reflect the full spectrum of morbidity associated with occupational diseases. Nonetheless, it is likely that hospital discharge data will be increasingly used in occupational health surveillance in future years.
National surveys
Special surveillance surveys undertaken on a national or regional basis can be the source of information more detailed than can be obtained through use of routine vital records. In the United States, the National Center for Health Statistics (NCHS) conducts two periodic national health surveys relevant to occupational health surveillance: the National Health Interview Survey (NHIS) and the National Health and Nutrition Examination Survey (NHANES). The National Health Interview Survey is a national household survey designed to obtain estimates of the prevalence of health conditions from a representative sample of households reflecting the civilian non-institutionalized population of the United States (USDHHS 1980). A chief limitation of this survey is its reliance on self-reporting of health conditions. Occupational and industrial data on participating individuals have been used in the past decade for evaluating rates of disability by occupation and industry (USDHHS 1980), assessing the prevalence of cigarette smoking by occupation (Brackbill, Frazier and Shilling 1988) and recording workers’ views about the occupational risks that they face (Shilling and Brackbill 1987).
With the assistance of NIOSH, an Occupational Health Supplement (NHIS-OHS) was included in 1988 in order to obtain population-based estimates of the prevalence of selected conditions that may be associated with work (USDHHS 1993). Approximately 50,000 households were sampled in 1988, and 27,408 currently employed individuals were interviewed. Among the health conditions addressed by the NHIS-OHS are work-related injuries, dermatologic conditions, cumulative trauma disorders, eye, nose and throat irritation, hearing loss and low-back pain.
In the first completed analysis from the NHIS-OHS, Tanaka and colleagues from NIOSH estimated that the national prevalence of work-related carpal tunnel syndrome in 1988 was 356,000 cases (Tanaka et al. 1995). Of the estimated 675,000 people with prolonged hand pain and medically diagnosed carpal tunnel syndrome, over 50% reported that their health care provider had stated that their wrist condition was caused by workplace activities. This estimate does not include workers who had not worked in the 12 months prior to the survey and who may have been disabled due to work-related carpal tunnel syndrome.
In contrast to the NHIS, the NHANES directly assesses the health of a probability sample of 30,000 to 40,000 individuals in the United States by performing physical examinations and laboratory tests in addition to collecting questionnaire information. The NHANES was conducted twice in the 1970s and most recently in 1988. The NHANES II, which was conducted in the late 1970s, collected limited information on indicators of exposure to lead and selected pesticides. Initiated in 1988, the NHANES III collected additional data on occupational exposures and disease, especially concerning respiratory and neurologic disease of occupational origin (USDHHS 1994).
Summary
Occupational disease surveillance and reporting systems have significantly improved since the mid-1980s. Recording of illnesses is best for diseases unique or virtually unique to occupational causes, such as the pneumoconioses and malignant mesothelioma. Identification and reporting of other occupational diseases depends upon the ability to match occupational exposures with health outcomes. Many data sources enable occupational disease surveillance, though all have important shortcomings with regard to quality, comprehensiveness and accuracy. Important obstacles to improving occupational disease reporting include the lack of interest in prevention in health care, the inadequate training of health care practitioners in occupational health and the inherent conflicts between employers and workers in the recognition of work-related disease. Despite these factors, gains in occupational disease reporting and surveillance are likely to continue in the future.
Cultural Differences
Culture and technology are interdependent. While culture is indeed an important aspect in technology design, development and utilization, the relationship between culture and technology is, however, extremely complex. It needs to be analysed from several perspectives in order to be considered in the design and application of technology. Based on his work in Zambia, Kingsley (1983) divides technological adaptation into changes and adjustments at three levels: that of the individual, of the social organization and of the cultural value system of the society. Each level possesses strong cultural dimensions which require special design considerations.
At the same time, technology itself is an inseparable part of culture. It is built, wholly or in part, around the cultural values of a particular society. And as part of culture, technology becomes an expression of that society’s way of life and thinking. Thus, in order for technology to be accepted, utilized and acknowledged by a society as its own, it must be congruent to the overall image of that society’s culture. Technology must complement culture, not antagonize it.
This article will deal with some of the intricacies concerning cultural considerations in technology designs, examining the current issues and problems, as well as the prevailing concepts and principles, and how they can be applied.
Definition of Culture
The definition of the term culture has been debated at length amongst sociologists and anthropologists for many decades. Culture can be defined in many terms. Kroeber and Kluckhohn (1952) reviewed over a hundred definitions of culture. Williams (1976) mentioned culture as one of the most complicated words in the English language. Culture has even been defined as the entire way of life of people. As such, it includes their technology and material artefacts—anything one would need to know to become a functioning member of the society (Geertz 1973). It may even be described as “publicly available symbolic forms through which people experience and express meaning” (Keesing 1974). Summing it up, Elzinga and Jamison (1981) put it aptly when they said that “the word culture has different meanings in different intellectual disciplines and systems of thought”.
Technology: Part and Product of Culture
Technology can be considered both as part of culture and its product. More than 60 years ago the noted sociologist Malinowsky included technology as part of the culture and gave the following definition: “culture comprises inherited artefacts, goods, technical processes, ideas, habits and values.” Later, Leach (1965) considered technology as a cultural product and mentioned “artefacts, goods and technical processes” as “products of culture”.
In the technological realm, “culture” as an important issue in the design, development and utilization of technical products or systems has been largely neglected by many suppliers as well as receivers of technology. One major reason for this neglect is the absence of basic information on cultural differences.
In the past, technological changes have led to significant changes in social life and organization and in people’s value systems. Industrialization has made deep and enduring changes in the traditional lifestyles of many previously agricultural societies since such lifestyles were largely regarded as incompatible with the way industrial work should be organized. In situations of large cultural diversity, this has led to various negative socio-economic outcomes (Shahnavaz 1991). It is now a well-established fact that simply to impose a technology on a society and believe that it will be absorbed and utilized through extensive training is wishful thinking (Martin et al. 1991).
It is the responsibility of the technology designer to consider the direct and indirect effects of the culture and to make the product compatible with the cultural value system of the user and with its intended operating environment.
The impact of technology for many “industrially developing countries” (IDCs) has been much more than improvement in efficiency. Industrialization was not just modernization of the production and service sectors, but to some extent Westernization of the society. Technology transfer is, thus, also cultural transfer.
Culture, in addition to religion, tradition and language, which are important parameters for technology design and utilization, encompasses other aspects, such as specific attitudes towards certain products and tasks, rules of appropriate behaviour, rules of etiquette, taboos, habits and customs. All these must be equally considered for optimum design.
It is said that people are also products of their distinctive cultures. Nevertheless, the fact remains that world cultures are very much interwoven due to human migration throughout history. It is small wonder that there exist more cultural than national variations in the world. Nevertheless, some very broad distinctions can be made regarding societal, organizational and professional culture-based differences that could influence design in general.
Constraining Influences of Culture
There is very little information on both theoretical and empirical analyses of the constraining influences of culture on technology and how this issue should be incorporated in the design of hardware and software technology. Even though the influence of culture on technology has been recognized (Shahnavaz 1991; Abeysekera, Shahnavaz and Chapman 1990; Alvares 1980; Baranson 1969), very little information is available on the theoretical analysis of cultural differences with regard to technology design and utilization. There are even fewer empirical studies that quantify the importance of cultural variations and provide recommendations on how cultural factors should be considered in the design of product or system (Kedia and Bhagat 1988). Nevertheless, culture and technology can still be studied with some degree of clarity when viewed from different sociological viewpoints.
Culture and Technology: Compatibility and Preference
Proper application of a technology depends, to a large extent, on the compatibility of the user’s culture with the design specifications. Compatibility must exist at all levels of culture—at the societal, organizational and professional levels. In turn, cultural compatibility can have strong influence on a people’s preferences and aptness to utilize a technology. This question involves preferences relating to a product or system; to concepts of productivity and relative efficiency; to change, achievement and authority; as well as to the manner of technology utilization. Cultural values can thus affect people’s willingness and ability to select, to use and to control technology. They have to be compatible in order to be preferred.
Societal culture
As all technologies are inevitably associated with sociocultural values, the cultural receptivity of the society is a very important issue for the proper functioning of a given technological design (Hosni 1988). National or societal culture, which contributes to the formation of a collective mental model of people, influences the entire process of technology design and application, which ranges from planning, goal setting and defining design specifications, to production, management and maintenance systems, training and evaluation. Technology design of both hardware and software should, therefore, reflect society-based cultural variations for maximum benefit. However, defining such society-based cultural factors for consideration in the design of technology is a very complicated task. Hofstede (1980) has proposed four dimensional framework variations of national-based culture.
- Weak versus strong uncertainty avoidance. This concerns a people’s desire to avoid ambiguous situations and to what extent their society has developed formal means (such as rules and regulations) to serve this purpose. Hofstede (1980) gave, for example, high uncertainty avoidance scores to countries like Japan and Greece, and low scores to Hong Kong and Scandinavia.
- Individualism versus collectivism. This pertains to the relationship between individuals and organizations in the society. In individualistic societies, the orientation is such that each person is expected to look after his or her own interests. In contrast, in a collectivist culture, social ties between people are very strong. Some examples of individualistic countries are the United States and Great Britain while Colombia and Venezuela can be considered as having collectivist cultures.
- Small versus large power distance. A large “power distance” characterizes those cultures where the less powerful individuals accept the unequal distribution of power in a culture, as well as the hierarchies in the society and its organizations. Examples of large power distance countries are India and the Philippines. Small power distances are typical of countries like Sweden and Austria.
- Masculinity versus femininity. Cultures that put more emphasis on material achievements are regarded as belonging to the former category. Those giving more value to quality of life and other less tangible outcomes belong to the latter.
Glenn and Glenn (1981) have also distinguished between “abstractive” and “associative” tendencies in a given national culture. It is argued that when people of an associative culture (like those from Asia) approach a cognitive problem, they put more emphasis on context, adapt a global thinking approach and try to utilize association among various events. Whereas in the Western societies, a more abstractive culture of rational thinking predominates. Based on these cultural dimensions, Kedia and Bhagat (1988) have developed a conceptual model for understanding cultural constraints on technology transfer. They have developed various descriptive “propositions” which provide information on different countries’ cultural variations and their receptivity with regard to technology. Certainly many cultures are moderately inclined to one or the other of these categories and contain some mixed features.
Consumers’ as well as producers’ perspectives upon technological design and utilization are directly influenced by the societal culture. Product safety standards for safeguarding consumers as well as work-environment regulations, inspection and enforcement systems for protecting the producers are to a large extent the reflection of the societal culture and value system.
Organizational culture
A company’s organization, its structure, value system, function, behaviour, and so on, are largely cultural products of the society in which it operates. This means that what happens within an organization is mostly a direct reflection of what is happening in the outside society (Hofstede 1983). The prevailing organizations of many companies operating in the IDCs are influenced both by the characteristics of the technology producer country as well as those of the technology recipient environment. However, the reflection of the societal culture in a given organization can vary. Organizations interpret the society in terms of their own culture, and their degree of control depends, among other factors, on the modes of technology transfer.
Given the changing nature of organization today, plus a multicultural, diverse workforce, adapting a proper organizational programme is more important than ever before to a successful operation (an example of a workforce diversity management programme is described in Solomon (1989)).
Professional culture
People belonging to a certain professional category may use a piece of technology in a specific fashion. Wikström et al. (1991), in a project aimed to develop hand tools, have noted that despite the designers’ assumption of how plate shares are to be held and used (i.e., with a forward holding grip and the tool moving away from one’s own body), the professional tinsmiths were holding and using the plate share in a reversed manner, as shown in figure 1. They concluded that tools should be studied in the actual field conditions of the user population itself in order to acquire relevant information on the tools characteristics.
Figure 1. The use of plate share tools by professional tinsmiths in practice (the reversed grip)
Using Cultural Features for Optimum Design
As implied by the foregoing considerations, culture provides identity and confidence. It forms opinions about the objectives and characteristics of a “human-technology system” and how it should operate in a given environment. And in any culture, there are always some features that are valuable with regard to technological progress. If these features are considered in the design of software and hardware technology, they can act as the driving force for technology absorption in the society. One good example is the culture of some southeast Asian countries largely influenced by Confucianism and Buddhism. The former emphasizes, among other things, learning and loyalty, and considers it a virtue to be able to absorb new concepts. The latter teaches the importance of harmony and respect for fellow human beings. It is said that these unique cultural features have contributed to the provision of the right environment for the absorption and implementation of advanced hardware and organizational technology furnished by the Japanese (Matthews 1982).
A clever strategy would thus make the best use of the positive features of a society’s culture in promoting ergonomic ideas and principles. According to McWhinney (1990) “the events, to be understood and thus used effectively in projection, must be embedded in stories. One must go to varying depths to unleash founding energy, to free society or organization from inhibiting traits, to find the paths along which it might naturally flow. . . . Neither planning nor change can be effective without embedding it consciously in a narrative.”
A good example of cultural appreciation in designing management strategy is the implementation of the “seven tools” technique for quality assurance in Japan. The “seven tools” are the minimum weapons a samurai warrior had to carry with him whenever he went out to fight. The pioneers of “quality control circles”, adapting their nine recommendations to a Japanese setting, reduced this number in order to take advantage of a familiar term—“the seven tools”—so as to encourage the involvement of all employees in their quality work strategy (Lillrank and Kano 1989).
However, other cultural features may not be beneficial to technological development. Discrimination against women, the strict observation of a caste system, racial or other prejudice, or considering some tasks as degrading, are a few examples that can have a negative influence on technology development. In some traditional cultures, men are expected to be the primary wage-earners. They become accustomed to regarding the role of women as equal employees, not to mention as supervisors, with insensitivity or even hostility. Withholding equal employment opportunity from women and questioning the legitimacy of women’s authority is not appropriate to the current needs of organizations, which require optimum utilization of human resources.
With regard to task design and job content, some cultures consider tasks like manual labour and service as degrading. This may be attributed to past experiences linked to colonial times regarding “master-slave relationships”. In some other cultures, strong biases exist against tasks or occupations associated with “dirty hands”. These attitudes are also reflected in lower-than-average pay scales for these occupations. In turn, these have contributed to shortages of technicians or inadequate maintenance resources (Sinaiko 1975).
Since it usually takes many generations to change cultural values with respect to a new technology, it would be more cost-effective to fit the technology to the technology recipient’s culture, taking cultural differences into consideration in the design of hardware and software.
Cultural Considerations in Product and System Designing
By now it is obvious that technology consists both of hardware and software. Hardware components include capital and intermediary goods, such as industrial products, machinery, equipment, buildings, workplaces and physical layouts, most of which chiefly concern the micro-ergonomics domain. Software pertains to programming and planning, management and organizational techniques, administration, maintenance, training and education, documentation and services. All these concerns fall under the heading of macro-ergonomics.
A few examples of cultural influences that require special design consideration from the micro- and macro-ergonomic point of view are given below.
Micro-ergonomic issues
Micro-ergonomics is concerned with the design of a product or system with the objective of creating a “usable” user-machine-environment interface. The major concept of product design is usability. This concept involves not only the functionality and reliability of the product, but issues of safety, comfort and enjoyment as well.
The user’s internal model (i.e., his or her cognitive or mental model) plays an important role in usability design. To operate or control a system efficiently and safely, the user must have an accurate representative cognitive model of the system in use. Wisner (1983) has stated that “industrialization would thus more or less require a new kind of mental model.” In this view, formal education and technical training, experience as well as culture are important factors in determining the formation of an adequate cognitive model.
Meshkati (1989), in studying the micro- and macro-ergonomic factors of the 1984 Union Carbide Bhopal accident, highlighted the importance of culture on the Indian operators’ inadequate mental model of the plant operation. He stated that part of the problem may have been due to “the performance of poorly trained Third World operators using advanced technological systems designed by other humans with much different educational backgrounds, as well as cultural and psychosocial attributes.” Indeed, many design usability aspects at the micro-interface level are influenced by the user’s culture. Careful analyses of the user’s perception, behaviour and preferences would lead to a better understanding of the user’s needs and requirements for designing a product or system that is both effective and acceptable.
Some of these culture-related micro-ergonomic aspects are the following:
- Interface design. Human emotion is an essential element of product design. It is concerned in such factors as colour and shape (Kwon, Lee and Ahn 1993; Nagamachi 1992). Colour is regarded as the most important factor to do with human emotions with regard to product design. The product’s colour treatment reflects the psychological and sentimental dispositions of the users, which differ from country to country. The symbolism of colour may also differ. For example, the colour red, which indicates danger in Western countries, is an auspicious token in India (Sen 1984) and symbolizes joy or happiness in China.
- Pictorial signs and symbols that are used in many different applications for public accommodations are strongly culture related. Western pictorial information, for example, is difficult to interpret by non-Western people (Daftuar 1975; Fuglesang 1982).
- Control/display compatibility. Compatibility is a measure of how well spatial movements of control, display behaviour or conceptual relationships meet human expectations (Staramler 1993). It refers to the user’s expectation of the stimulus-response relationship, which is a fundamental ergonomic issue for safe and efficient operation of a product or system. A compatible system is one which considers people’s common perceptual-motor behaviour (i.e., their population-stereotype). However, like other human behaviour, perceptual-motor behaviour may also be influenced by culture. Hsu and Peng (1993) compared American and Chinese subjects regarding control/burner relationships in a four-burner stove. Different population-stereotype patterns were observed. They conclude that population stereotypes regarding control/burner linkages were culturally different, probably as a result of differences in reading or scanning habits.
- Workplace design. An industrial workstation design aims to eliminate harmful postures and improve user performance in relation to the user’s biological needs, preferences and task requirements. People from different cultures may prefer different types of sitting posture and work heights. In Western countries, work heights are set near the seated elbow height for maximum comfort and efficiency. However, in many parts of the world people sit on the floor. Indian workers, for example, prefer squatting or sitting cross-legged to standing or to sitting on a chair. In fact it has been observed that even when chairs are provided, the operators still prefer to squat or sit cross-legged on the seats. Daftuar (1975) and Sen (1984) have studied the merits and implications of the Indian sitting posture. After describing the various advantages of sitting on the floor, Sen stated that “as a large population of the world market covers societies where squatting or sitting on the ground predominate, it is unfortunate that up to now no modern machines have been designed to be used in this way.” Thus, variations in preferred posture should be considered in machine and workplace design in order to improve the operator’s efficiency and comfort.
- Design of protective equipment. There exist both psychological and physical constraints with regard to wearing protective clothing. In some cultures, for example, jobs requiring the use of protective wear may be regarded as common labour, suitable only for unskilled workers. Consequently, protective equipment is usually not worn by engineers at workplaces in such settings. Regarding physical constraints, some religious groups, obliged by their religion to wear a head covering (like the turbans of Indian Sikhs or the head covers of Muslim women) find it difficult to wear, for example, protective helmets. Therefore, special designs of protective wear are needed to cope with such cultural variations in protecting people against work-environmental hazards.
Macro-ergonomic issues
The term macro-ergonomics refers to the design of software technology. It concerns the proper design of organizations and management systems. Evidence exists showing that because of differences in culture, sociopolitical conditions and educational levels, many successful managerial and organizational methods developed in industrialized countries cannot be successfully applied to developing countries (Negandhi 1975). In most IDCs, an organizational hierarchy characterized by a down-flow of authority structure within the organization is a common practice. It has little concern for Western values such as democracy or power sharing in decision-making, which are regarded as key issues in modern management, being essential for proper utilization of human resources as regards intelligence, creativity, problem solving potential and ingenuity.
The feudal system of social hierarchy and its value system are also widely practised in most industrial workplaces in the developing countries. These make a participatory management approach (which is essential for the new production mode of flexible specialization and the motivation of the workforce) a difficult endeavour. However, there are reports confirming the desirability of introducing autonomous work systems even in these cultures Ketchum 1984).
- Participatory ergonomics. Participatory ergonomics is a useful macro-ergonomics approach for solving various work-related problems (Shahnavaz, Abeysekera and Johansson 1993; Noro and Imada 1991; Wilson 1991). This approach, mostly used in industrialized countries, has been applied in different forms depending on the organizational culture in which it has been implemented. In a study, Liker, Nagamachi and Lifshitz (1988) compared participatory ergonomics programmes in two US and two Japanese manufacturing plants which were aiming to reduce physical stress on workers. They concluded that an “effective participatory ergonomics programme can take many forms. The best programme for any plant in any culture may depend on its own unique history, structure and culture.”
- Software systems. Societal and organizational culture-based differences should be considered in designing a new software system or introducing a change in the organization. With respect to information technology, De Lisi (1990) indicates that networking capabilities will not be realized unless the networks fit the existing organizational culture.
- Work organization and management. In some cultures, the family is so important an institution that it plays a prominent role in work organization. For example, among some communities in India, a job is generally regarded as a family responsibility and is collectively performed by all family members (Chapanis 1975).
- Maintenance system. Design of maintenance programmes (both preventive and regular) as well as housekeeping are other examples of areas in which work organization should be adapted to cultural constraints. The traditional culture among the sort of agricultural societies predominant in many IDCs is generally not compatible with the requirements of industrial work and how activities are organized. Traditional agricultural activity does not require, for example, formal maintenance programming and precision work. It is for the most part not carried out under time pressure. In the field, it is usually left to the recycling process of nature to take care of maintenance and housekeeping work. The design of maintenance programmes and housekeeping manuals for industrial activities should thus take these cultural constraints into account and provide for adequate training and supervision.
Zhang and Tyler (1990), in a case study related to the successful establishment of a modern telephone cable production facility in China supplied by a US firm (the Essex Company) stated that “both parties realize, however, that the direct application of American or Essex management practices was not always practical nor desirable due to cultural, philosophical, and political differences. Thus the information and instructions provided by Essex was often modified by the Chinese partner to be compatible with the conditions existing in China.” They also argued that the key to their success, despite cultural, economic and political differences, was both parties’ dedication and commitment to a common goal as well as the mutual respect, trust, and friendship which transcended any differences between them.
Design of shift and work schedules are other examples of work organization. In most IDCs there are certain sociocultural problems associated with shift work. These include poor general living and housing conditions, lack of support services, a noisy home environment and other factors, which require the design of special shift programmes. Furthermore, for female workers, a working day is usually much longer than eight hours; it consists of not only the actual time spent working, but also the time spent on travelling, working at home and taking care of children and elderly relatives. In view of the prevailing culture, shift and other work design requires special work-rest schedules for effective operation.
Flexibility in work schedules to allow cultural variances such as an after-lunch nap for Chinese workers and religious activities for Muslims are further cultural aspects of work organization. In the Islamic culture, people are required to break from work a few times a day to pray, and to fast for one month each year from sunrise to sunset. All these cultural constraints require special work organizational considerations.
Thus, many macro-ergonomic design features are closely influenced by culture. These features should be considered in the design of software systems for effective operation.
Conclusion: Cultural Differences in Design
Designing a usable product or system is not an easy task. There exists no absolute quality of suitability. It is the designer’s task to create an optimum and harmonic interaction between the four basic components of the human-technology system: the user, the task, the technological system and the operating environment. A system may be fully usable for one combination of user, task and environmental conditions but totally unsuitable for another. One design aspect which can greatly contribute to the design’s usability, whether it is a case of a single product or a complex system, is the consideration of cultural aspects which have a profound influence on both the user and the operating environment.
Even if a conscientious engineer designs a proper human-machine interface for use in a given environment, the designer is often unable to foresee the effects of a different culture on the product’s usability. It is difficult to prevent possible negative cultural effects when a product is used in an environment different from that for which it was designed. And since there exist almost no quantitative data regarding cultural constraints, the only way the engineer can make the design compatible with regard to cultural factors is to actively integrate the user population in the design process.
The best way to consider cultural aspects in design is for the designer to adapt a user-centred design approach. True enough, the design approach adapted by the designer is the essential factor that will instantly influence the usability of the designed system. The importance of this basic concept must be recognized and implemented by the product or system designer at the very beginning of the design life cycle. The basic principles of user-centred design can thus be summarized as follows (Gould and Lewis 1985; Shackel 1986; Gould et al. 1987; Gould 1988; Wang 1992):
- Early and continual focus on user. The user should be an active member of the design team throughout the whole product development life cycle (i.e., predesign, detail design, production, verification and product improvement phase).
- Integrated design. The system should be considered as a whole, ensuring a holistic design approach. This means that all aspects of the system’s usability should be evolved in parallel by the design team.
- Early and continuous user testing. User reaction should be tested using prototypes or simulations while carrying out real work in the real environment from early development stage to the final product.
- Iterative design. Designing, testing and redesigning are repeated in regular cycles until satisfactory usability results are achieved.
In the case of designing a product on a global scale, the designer has to consider the needs of consumers around the world. In such a case, access to all actual users and operating environments may not be possible for the purpose of adopting a user-centred design approach. The designer has to use a broad range of information, both formal and informal, such as literature reference material, standards, guidelines, and practical principles and experience in making an analytical evaluation of the design and has to provide sufficient adjustability and flexibility in the product in order to satisfy the needs of a wider user population.
Another point to consider is the fact that designers can never be all-knowing. They need input from not only the users but also other parties involved in the project, including managers, technicians, and repair and maintenance workers. In a participatory process, people involved should share their knowledge and experiences in developing a usable product or system and accept collective responsibility for its functionality and safety. After all, everyone involved has something at stake.
Occupational Hazard Surveillance
Hazard surveillance is the process of assessing the distribution of, and the secular trends in, use and exposure levels of hazards responsible for disease and injury (Wegman 1992). In a public health context, hazard surveillance identifies work processes or individual workers exposed to high levels of specific hazards in particular industries and job categories. Since hazard surveillance is not directed at disease events, its use in guiding public health intervention generally requires that a clear exposure-outcome relationship has previously been established. Surveillance can then be justified on the assumption that reduction in the exposure will result in reduced disease. Proper use of hazard surveillance data enables timely intervention, permitting the prevention of occupational illness. Its most significant benefit is therefore the elimination of the need to wait for obvious illness or even death to occur before taking measures to protect workers.
There are at least five other advantages of hazard surveillance which complement those provided by disease surveillance. First, identifying hazard events is usually much easier than identifying occupational disease events, particularly for diseases such as cancer that have long latency periods. Second, a focus on hazards (rather than illnesses) has the advantage of directing attention to the exposures which ultimately are to be controlled. For example, surveillance of lung cancer might focus on rates in asbestos workers. However, a sizeable proportion of lung cancer in this population could be due to cigarette smoking, either independently of or interacting with the asbestos exposure, so that large numbers of workers might need to be studied to detect a small number of asbestos-related cancers. On the other hand, surveillance of asbestos exposure could provide information on the levels and patterns of exposure (jobs, processes or industries) where the poorest exposure control exists. Then, even without an actual count of lung cancer cases, efforts to reduce or eliminate exposure would be appropriately implemented.
Third, since not every exposure results in disease, hazard events occur with much higher frequency than disease events, resulting in the opportunity to observe an emerging pattern or change over time more easily than with disease surveillance. Related to this advantage is the opportunity to make greater use of sentinel events. A sentinel hazard can be simply the presence of an exposure (e.g., beryllium), as indicated via direct measurement in the workplace; the presence of an excessive exposure, as indicated via biomarker monitoring (e.g., elevated blood lead levels); or a report of an accident (e.g., a chemical spill).
A fourth advantage of the surveillance of hazards is that data collected for this purpose do not infringe on an individual’s privacy. Confidentiality of medical records is not at risk and the possibility of stigmatizing an individual with a disease label is avoided. This is particularly important in industrial settings where a person’s job may be in jeopardy or a potential compensation claim may affect a physician’s choice of diagnostic options.
Finally, hazard surveillance can take advantage of systems designed for other purposes. Examples of ongoing collection of hazard information which already exists include registries of toxic substance use or hazardous material discharges, registries for specific hazardous substances and information collected by regulatory agencies for use in compliance. In many respects, the practising industrial hygienist is already quite familiar with the surveillance uses of exposure data.
Hazard surveillance data can complement disease surveillance both for research to establish or confirm a hazard-disease association, as well as for public health applications, and the data collected in either instance can be used to determine the need for remediation. Different functions are served by national surveillance data (as might be developed using the US OSHA Integrated Management Information System data on industrial hygiene compliance sample results—see below) in contrast to those served by hazard surveillance data at a plant level, where much more detailed focus and analysis are possible.
National data may be extremely important in targeting inspections for compliance activity or for determining what is the probable distribution of risks that will result in specific demands on medical services for a region. Plant-level hazard surveillance, however, provides the necessary detail for close examination of trends over time. Sometimes a trend occurs independently of changes in controls but rather in response to product changes which would not be evident in regionally grouped data. Both national and plant-level approaches can be useful in determining whether there is a need for planned scientific studies or for worker and management educational programmes.
By combining hazard surveillance data from routine inspections in a wide range of seemingly unrelated industries, it is sometimes possible to identify groups of workers for whom heavy exposure might otherwise be overlooked. For example, analysis of airborne lead concentrations as determined in OSHA compliance inspections for 1979 to 1985 identified 52 industries in which the permissible exposure limit (PEL) was exceeded in more than one-third of inspections (Froines et al. 1990). These industries included primary and secondary smelting, battery manufacture, pigment manufacture and brass/bronze foundries. As these are all industries with historically high lead exposure, excessive exposures indicated poor control of known hazards. However some of these workplaces are quite small, such as secondary lead smelter operations, and individual plant managers or operators may be unlikely to undertake systematic exposure sampling and could thus be unaware of serious lead exposure problems in their own workplaces. In contrast to high levels of ambient lead exposures that might have been expected in these basic lead industries, it was also noted that over one-third of the plants in the survey in which the PELs were exceeded resulted from painting operations in a wide variety of general industry settings. Structural steel painters are known to be at risk for lead exposure, but little attention has been directed to industries that employ painters in small operations painting machinery or machinery parts. These workers are at risk of hazardous exposures, yet they often are not considered to be lead workers because they are in an industry which is not a lead-based industry. In a sense, this survey revealed evidence of a risk that was known but had been forgotten until it was identified by analysis of these surveillance data.
Objectives of Hazard Surveillance
Programmes of hazard surveillance can have a variety of objectives and structures. First, they permit focus on intervention actions and help to evaluate existing programmes and to plan new ones. Careful use of hazard surveillance information can lead to early detection of system failure and call attention to the need for improved controls or repairs before excess exposures or diseases are actually experienced. Data from such efforts can also provide evidence of need for new or revised regulation for a specific hazard. Second, surveillance data can be incorporated into projections of future disease to permit planning of both compliance and medical resource use. Third, using standardized exposure methodologies, workers at various organizational and governmental levels can produce data which permit focus on a nation, a city, an industry, a plant or even a job. With this flexibility, surveillance can be targeted, adjusted as needed, and refined as new information becomes available or as old problems are solved or new ones appear. Finally, hazard surveillance data should prove valuable in planning epidemiological studies by identifying areas where such studies would be most fruitful.
Examples of Hazard Surveillance
Carcinogen Registry—Finland. In 1979 Finland began to require national reporting of the use of 50 different carcinogens in industry. The trends over the first seven years of surveillance were reported in 1988 (Alho, Kauppinen and Sundquist 1988). Over two-thirds of workers exposed to carcinogens were working with only three types of carcinogens: chromates, nickel and inorganic compounds, or asbestos. Hazard surveillance revealed that a surprisingly small number of compounds accounted for most carcinogen exposures, thus greatly improving the focus for efforts at toxic use reduction as well as efforts at exposure controls.
Another important use of the registry was the evaluation of reasons that listings “exited” the system—that is, why use of a carcinogen was reported once but not on subsequent surveys. Twenty per cent of exits were due to continuing but unreported exposure. This led to education for, as well as feedback to, the reporting industries about the value of accurate reporting. Thirty-eight per cent exited because exposure had stopped, and among these over half exited due to substitution by a non-carcinogen. It is possible that the results of the surveillance system reports stimulated the substitution. Most of the remainder of the exits resulted from elimination of exposures by engineering controls, process changes or considerable decrease in use or exposure time. Only 5% of exits resulted from use of personal protective equipment. This example shows how an exposure registry can provide a rich resource for understanding the use of carcinogens and for tracking the change in use over time.
National Occupational Exposure Survey (NOES). The US NIOSH carried out two National Occupational Exposure Surveys (NOES) ten years apart to estimate the number of workers and workplaces potentially exposed to each of a wide variety of hazards. National and state maps were prepared that show the items surveyed, such as the pattern of workplace and worker exposures to formaldehyde (Frazier, Lalich and Pedersen 1983). Superimposing these maps on maps of mortality for specific causes (e.g., nasal sinus cancer) provides the opportunity for simple ecological examinations designed to generate hypotheses which can then be investigated by appropriate epidemiological study.
Changes between the two surveys have also been examined—for example, the proportions of facilities in which there were potential exposures to continuous noise without functioning controls (Seta and Sundin 1984). When examined by industry, little change was seen for general building contractors (92.5% to 88.4%), whereas a striking decrease was seen for chemicals and allied products (88.8% to 38.0%) and for miscellaneous repair services (81.1% to 21.2%). Possible explanations included passage of the Occupational Safety and Health Act, collective bargaining agreements, concerns with legal liability and increased employee awareness.
Inspection (Exposure) Measures (OSHA). The US OSHA has been inspecting workplaces to evaluate the adequacy of exposure controls for over twenty years. For most of that time, the data have been placed in a database, the Integrated Management Information System (OSHA/IMIS). Overall secular trends in selected cases have been examined for 1979 to 1987. For asbestos, there is good evidence for largely successful controls. In contrast, while the number of samples collected for exposures to silica and lead declined over those years, both substances continued to show a substantial number of overexposures. The data also showed that despite reduced numbers of inspections, the proportion of inspections in which exposure limits were exceeded remained essentially constant. Such data could be highly instructive to OSHA when planning compliance strategies for silica and lead.
Another use of the workplace inspection database has been a quantitative examination of silica exposure levels for nine industries and jobs within those industries (Froines, Wegman and Dellenbaugh 1986). Exposure limits were exceeded to various degrees, from 14% (aluminium foundries) to 73% (potteries). Within the potteries, specific jobs were examined and the proportion where exposure limits were exceeded ranged from 0% (labourers) to 69% (sliphouse workers). The degree to which samples exceeded the exposure limit varied by job. For sliphouse workers excess exposures were, on average, twice the exposure limit, while slip/glaze sprayers had average excess exposures of over eight times the limit. This level of detail should prove valuable to management and workers employed in potteries as well as to government agencies responsible for regulating occupational exposures.
Summary
This article has identified the purpose of hazard surveillance, described its benefits and some of its limitations and offered several examples in which it has provided useful public health information. However, hazard surveillance should not replace disease surveillance for noninfectious diseases. In 1977 a NIOSH task force emphasized the relative interdependence of the two major types of surveillance, stating:
The surveillance of hazards and diseases cannot proceed in isolation from each other. The successful characterization of the hazards associated with different industries or occupations, in conjunction with toxicological and medical information relating to the hazards, can suggest industries or occupational groups appropriate for epidemiological surveillance (Craft et al. 1977).
Elderly Workers
The status of ageing workers varies according to their functional condition, which itself is influenced by their past working history. Their status also depends on the work post that they occupy, and the social, cultural and economic situation of the country in which they live.
Thus, workers who have to perform much physical labour are also, most often, those who have had the least schooling and the least occupational training. They are subject to exhausting work conditions, which can cause disease, and they are exposed to the risk of accidents. In this context, their physical capacity is very likely to decline towards the end of their active life, a fact that makes them more vulnerable at work.
Conversely, workers who have had the advantage of lengthy schooling, followed by occupational training that equips them for their work, in general practise trades where they can put to use the knowledge thus acquired and progressively widen their experience. Often they do not work in the most harmful occupational environments and their skills are recognized and valued as they grow older.
During a period of economic expansion and shortage of labour, ageing workers are recognized as having the qualities of “occupational conscientiousness”, being regular in their work, and being able to keep up their know-how. In a period of recession and unemployment, there will be greater emphasis on the fact that their work performance falls short of that of younger people and on their lower capacity to adapt to changes in work techniques and organization.
Depending on the countries concerned, their cultural traditions and their mode and level of economic development, consideration for ageing workers and solidarity with them will be more or less evident, and their protection will be more or less assured.
The time dimensions of the age/work relationship
The relationship between ageing and work covers a great diversity of situations, which can be considered from two points of view: on the one hand, work appears to be a transformation factor for the worker throughout his or her active life, the transformations being either negative (e.g., wear and tear, decline in skills, illnesses and accidents) or positive (e.g., acquisition of knowledge and experience); on the other hand, work reveals the changes connected with age, and this results in marginalization and even exclusion from the production system for older workers exposed to demands at work that are too great for their declining capacity, or on the contrary allows for progress in their working career if the content of the work is such that a high value is placed on experience.
Advancing age therefore plays the role of a “vector” on which events in life are registered chronologically, both at and outside work. Around this axis are hinged processes of decline and building, which are very variable from one worker to another. In order to take into account the problems of ageing workers in the design of work situations, it is necessary to take into account both the dynamic characteristics of changes connected with age and the variability of these changes among individuals.
The age/work relationship can be considered in the light of a threefold evolution:
- Work evolves. Techniques change; mechanization, automation, computerization and methods of information transfer, among other factors, tend or will tend to become more generalized. New products make their appearance, others disappear. New risks are revealed or extended (e.g., radiation and chemical products), others become less prominent. Work organization, labour management, the distribution of tasks and the work schedules are transformed. Some production sectors develop, while others decline. From one generation to another, the work situations encountered during the active life of the worker, the demands that they make and the skills that they require are not the same.
- Working populations change. Age structures are modified in accordance with demographic changes, the means of entering or retiring from work and attitudes towards employment. Women’s share in the working population continues to evolve. Genuine upheavals are occurring in the field of education, occupational training and access to the health system. All these transformations are at the same time producing generation-related and period-related effects which obviously influence the age/work relationship and which can to a certain extent be anticipated.
- Finally—a point that deserves emphasis—individual changes are in progress throughout one’s working life, and the adjustment between the characteristics of particular work and those of the people who carry it out is therefore frequently called into question.
Some processes of organic ageing and their relationship to work
The main organic functions involved in work decline in an observable way from the ages of 40 or 50, after some of them have undergone development up to the ages of 20 or 25.
In particular, a decline with age is observed in maximum muscular strength and range of joint movement. The reduction in strength is in the order of 15 to 20% between the ages of 20 and 60. But this is only an overall trend, and the variability among individuals is considerable. Moreover, these are maximum capacities; the decline is much less for more moderate physical demands.
One function that is very sensitive to age is regulation of posture. This difficulty is not very apparent for common and stable working positions (standing or sitting) but it becomes obvious in situations of disequilibrium that require precise adjustments, strong muscular contraction or joint movements at extreme angles. These problems become more severe when the work has to be carried out on unstable or slippery supports, or when the worker suffers a shock or unexpected jolt. The result is that accidents due to loss of balance become more frequent with age.
Sleep regulation becomes less reliable from the ages of 40 to 45 onwards. It is more sensitive to changes in working schedules (such as night work or shift work) and to disturbing environments (e.g., noise or lighting). Changes in the length and quality of sleep follow.
Thermoregulation also becomes more difficult with age, and this causes older workers to have specific problems with regard to work in heat, particularly when physically intense work has to be carried out.
Sensory functions begin to be affected very early, but the resulting deficiencies are rarely marked before the ages of 40 to 45. Visual function as a whole is affected: there is a reduction in the amplitude of accommodation (which can be corrected with appropriate lenses), and also in the peripheral visual field, perception of depth, resistance to glare and light transmission through the crystalline lens. The resulting inconvenience is noticeable only in particular conditions: in poor lighting, near sources of glare, with objects or texts of very small size or badly presented, and so on.
The decline in auditory function affects the hearing threshold for high frequencies (high-pitched sounds), but it reveals itself particularly as difficulty in discriminating sound signals in a noisy environment. Thus, the intelligibility of the spoken word becomes more difficult in the presence of ambient noise or strong reverberation.
The other sensory functions are, in general, little affected at this time of life.
It can be seen that, in a general way, organic decline with age is noticeable particularly in extreme situations, which should in any case be modified to avoid difficulties even for young workers. Moreover, ageing workers can compensate for their deficiencies by means of particular strategies, often acquired with experience, when the work conditions and organization permit: the use of additional supports for unbalanced postures, lifting and carrying loads in such a way as to reduce extreme effort, organizing visual scanning so as to pinpoint useful information, among other means.
Cognitive ageing: slowing down and learning
As regards cognitive functions, the first thing to note is that work activity brings into play basic mechanisms for receiving and processing information on the one hand, and on the other, knowledge acquired throughout life. This knowledge concerns mainly the meaning of objects, signals, words and situations (“declarative” knowledge), and ways of doing things (“procedural” knowledge).
Short-term memory allows us to retain, for some dozens of seconds or for some minutes, useful information that has been detected. Processing of this information is carried out by comparing it with knowledge that has been memorized on a permanent basis. Ageing acts on these mechanisms in various ways: (1) by virtue of experience, it enriches knowledge, the capacity to select in the best way both useful knowledge and the method of processing it, especially in tasks that are carried out fairly frequently, but (2) the time taken to process this information is lengthened owing both to ageing of the central nervous system, and to more fragile short-term memory.
These cognitive functions depend very much on the environment in which the workers have lived, and therefore on their past history, their training, and the work situations which they have had to face. The changes that occur with age are therefore manifested in extremely varied combinations of phenomena of decline and reconstruction, in which each of these two factors may be more or less accentuated.
If in the course of their working lives workers have received only brief training, and if they have had to carry out relatively simple and repetitive tasks, their knowledge will be limited and they have difficulties when confronted with new or relatively unfamiliar tasks. If, moreover, they have to perform work under marked time constraints, the changes that have occurred in their sensory functions and the slowing down of their information processing will handicap them. If, on the other hand, they have had lengthy schooling and training, and if they have had to carry out a variety of tasks, they will thereby have been able to enhance their skills so that the sensory or cognitive deficiencies associated with age will be largely compensated for.
It is therefore easy to understand the role played by continued training in the work situation of ageing workers. Changes in work make it necessary more and more often to have recourse to periodic training, but older workers rarely receive it. Firms frequently do not consider it worthwhile to give training to a worker nearing the end of his or her active life, particularly as learning difficulties are thought to increase with age. And the workers themselves hesitate to undergo training, fearing that they will not succeed, and not always seeing very clearly the benefits that they could derive from training.
In fact, with age, the manner of learning is modified. Whereas a young person records the knowledge transmitted to him, an older person needs to understand how this knowledge is organized in relation to what he or she already knows, what is its logic, and what is its justification for work. He or she also needs time to learn. Therefore one response to the problem of training older workers is, in the first place, to use different teaching methods, according to each person’s age, knowledge and experience, with, in particular, a longer training period for older people.
Ageing of men and women at work
Age differences between men and women are found at two different levels. At the organic level, life expectancy is generally greater for women than for men, but what is called life expectancy without disability is very close for the two sexes—up to 65 to 70 years. Beyond that age, women are generally at a disadvantage. Moreover, women’s maximum physical capacity is on average 30% less than men’s, and this difference tends to persist with advancing age, but the variability in the two groups is wide, with some overlap between the two distributions.
At the level of the working career there are great differences. On average, women have received less training for work than men when they start their working life, they most often occupy posts for which fewer qualifications are needed, and their working careers are less rewarding. With age they, therefore, occupy posts with considerable constraints, such as time constraints and repetitiveness of the work. No sexual difference in the development of cognitive capacity with age can be established without reference to this social context of work.
If the design of work situations is to take account of these gender differences, action must be taken especially in favour of the initial and continuing vocational training of women and constructing work careers that increase women’s experiences and enhance their value. This action must, therefore, be taken well before the end of their active lives.
Ageing of working populations: the usefulness of collective data
There are at least two reasons for adopting collective and quantitative approaches with respect to the ageing of the working population. The first reason is that such data will be necessary in order to evaluate and foresee the effects of ageing in a workshop, a service, a firm, a sector or a country. The second reason is that the main components of ageing are themselves phenomena subject to probability: all workers do not age in the same way or at the same rate. It is therefore by means of statistical tools that various aspects of ageing will sometimes be revealed, confirmed or assessed.
The simplest instrument in this field is the description of age structures and of their evolution, expressed in ways relevant to work: economic sector, trade, group of jobs, and so on.
For example, when we observe that the age structure of a population in a workplace remains stable and young, we may ask which characteristics of the work could play a selective role in terms of age. If, on the contrary, this structure is stable and older, the workplace has the function of receiving people from other sectors of the firm; the reasons for these movements are worth studying, and we should equally verify whether the work in this workplace is suited to the characteristics of an ageing workforce. If, finally, the age structure shifts regularly, simply reflecting recruitment levels from one year to another, we probably have a situation where people “grow old on site”; this sometimes requires special study, particularly if the annual number of recruitments is tending to decline, which will shift the overall structure towards higher age groups.
Our understanding of these phenomena can be enhanced if we have quantitative data on working conditions, on the posts currently occupied by the workers and (if possible) on the posts that they no longer occupy. The work schedules, the repetitiveness of work, the nature of the physical demands, the work environment, and even certain cognitive components, can be the subject of queries (to be asked of the workers) or of evaluations (by experts). It is then possible to establish a connection between the characteristics of the present work and of past work, and the age of the workers concerned, and so to elucidate the selection mechanisms to which the work conditions can give rise at certain ages.
These investigations can be further improved by also obtaining information on the health status of the workers. This information can be derived from objective indicators such as the work accident rate or sickness absence rate. But these indicators often require considerable care as regards methodology, because although they do indeed reflect health conditions that may be work-related, they also reflect the strategy of all those concerned with occupational accidents and absence due to illness: the workers themselves, the management and the physicians can have various strategies in this regard, and there is no guarantee that these strategies are independent of the worker’s age. Comparisons of these indicators between ages are therefore often complex.
Recourse will therefore be had, when possible, to data arising from self-evaluation of health by the workers, or obtained during medical examinations. These data may relate to diseases whose variable prevalence with age needs to be better known for purposes of anticipation and prevention. But the study of ageing will rely above all on the appreciation of conditions that have not reached the disease stage, such as certain types of functional deterioration: (e. g., of the joints—pain and limitation of sight and hearing, of the respiratory system) or else certain kinds of difficulty or even incapacity (e. g. in mounting a high step, making a precise movement, maintaining equilibrium in an awkward position).
Relating data concerning age, work and health is therefore at the same time a useful and complex matter. Their use permits various types of connections to be revealed (or their existence to be presumed). It may be a case of simple causal relationships, with some requirement of the work accelerating a type of decline in the functional state as age advances. But this is not the most frequent case. Very often, we shall be led to appreciate simultaneously the effect of an accumulation of constraints on the a set of health characteristics, and at the same time the effect of selection mechanisms in accordance with which workers whose health has declined may find that they are excluded from certain kinds of work (what the epidemiologists call the “healthy worker effect”).
In this way we can evaluate the soundness of this collection of relationships, confirm certain fundamental knowledge in the sphere of psychophysiology, and above all obtain information that is useful for devising preventive strategies as regards ageing at work.
Some types of action
Action to be undertaken to maintain ageing workers in employment, without negative consequences for them, must follow several general lines:
- One must not consider this age group as a category apart, but must instead consider age as one factor of diversity among others in the active population; protective measures that are too targeted or too accentuated tend to marginalize and weaken the position of the populations concerned.
- One should anticipate individual and collective changes related to age, as well as changes in work techniques and organization. The management of human resources can be effectively carried out only over time, so as to prepare appropriate adjustments in work careers and training. The design of work situations can then take account at the same time of the available technical and organizational solutions and the characteristics of the (future) population concerned.
- The diversity of individual development throughout working life should be taken into consideration, so as to create conditions of equivalent diversity in work careers and situations.
- Attention should be devoted to favouring the process of building up skills and attenuating the process of decline.
On the basis of these few principles, several types of immediate action can first be defined. The highest priority of action will concern working conditions that are capable of posing particularly acute problems for older workers. As mentioned earlier, postural stresses, extreme exertion, strict time constraints (e.g., as with assembly-line work or the imposition of higher output goals), harmful environments (temperature, noise) or unsuitable environments (lighting conditions), night work and shift work are examples.
Systematic pinpointing of these constraints in posts that are (or may be) occupied by older workers allows an inventory to be drawn up and priorities to be established for action. This pinpointing can be carried out by means of empirical inspection checklists. Of equal use will be analysis of worker activity, which will permit observation of their behaviour to be linked with the explanations that they give of their difficulties. In these two cases, measures of effort or of environmental parameters may complete the observations.
Beyond this pinpointing, the action to be taken cannot be described here, since it will obviously be specific to each work situation. The use of standards may sometimes be useful, but few standards take account of specific aspects of ageing, and each one is concerned with a particular domain, which tends to give rise to thinking in an isolated fashion about each component of the activity under study.
Apart from the immediate measures, taking ageing into account implies longer-range thinking directed towards working out the widest possible flexibility in the design of work situations.
Such flexibility must first be sought in the design of work situations and equipment. Restricted space, nonadjustable tools, rigid software, in short, all the characteristics of the situation that limit the expression of human diversity in the carrying out of the task are very likely to penalize a considerable proportion of older workers. The same is true of the more constraining types of organization: a completely predetermined distribution of tasks, frequent and urgent deadlines, or too numerous or too strict orders (these, of course, must be tolerated when there are essential requirements relating to the quality of production or the safety of an installation). The search for such flexibility is, therefore, the search for varied individual and collective adjustments that can facilitate the successful integration of ageing workers into the production system. One of the conditions for the success of these adjustments is obviously the establishment of work training programmes, provided for workers of all ages and geared to their specific needs.
Taking ageing into account in the design of work situations thus entails a series of coordinated actions (overall reduction in extreme stresses, using all possible strategies for work organization, and continuous efforts to increase skills), which are all the more efficient and all the less expensive when they are taken over the long term and are carefully thought out in advance. The ageing of the population is a sufficiently slow and foreseeable phenomenon for appropriate preventive action to be perfectly feasible.
Surveillance in Developing Countries
It is estimated that more than 80% of the world’s population live in the developing countries in Africa, the Middle East, Asia and South and Central America. The developing countries are often financially disadvantaged, and many have largely rural and agricultural economies. However, they are widely different in many ways, with diverse aspirations, political systems and varying stages of industrial growth. The status of health among people in the developing countries is generally lower than in the developed countries, as reflected by higher infant mortality rates and lower life expectancies.
Several factors contribute to the need for occupational safety and health surveillance in developing countries. First, many of these countries are rapidly industrializing. In terms of the size of industrial establishments, many of the new industries are small-scale industries. In such situations, safety and health facilities are often very limited or non-existent. In addition, developing countries are often the recipients of technology transfer from developed countries. Some of the more hazardous industries, which have difficulty in operating in countries with more stringent and better enforced occupational health legislation, may be “exported” to developing countries.
Second, with regard to the workforce, the education level of the workers in developing countries is often lower, and workers may be untrained in safe work practices. Child labour is often more prevalent in developing countries. These groups are relatively more vulnerable to health hazards at work. In addition to these considerations, there is generally a lower pre-existing level of health among workers in developing countries.
These factors would ensure that throughout the world, workers in developing countries are among those who are most vulnerable to and who face the greatest risk from occupational health hazards.
Occupational Health Effects are Different from Those Seen in Developed Countries
It is important to obtain data on health effects for prevention and for prioritization of approaches to solve occupational health problems. However, most of the available morbidity data may not be applicable for developing countries, as they originate from the developed countries.
In developing countries, the nature of the occupational health effects from workplace hazards may be different from those in the developed countries. Overt occupational diseases such as chemical poisonings and the pneumoconioses, which are caused by exposures to high levels of workplace toxins, are still encountered in significant numbers in developing countries, while these problems may have been substantially reduced in the developed countries.
For example, in the case of pesticide poisoning, acute health effects and even deaths from high exposures are a greater immediate concern in developing agricultural countries, as compared to the long-term health effects from low dose exposure to pesticides, which might be a more important issue in the developed countries. In fact, the morbidity burden from acute pesticide poisoning in some developing countries, such as Sri Lanka, may even surpass that of traditional public health problems such as diphtheria, whooping cough and tetanus.
Thus, some surveillance of occupational health morbidity is required from the developing countries. The information would be useful for the assessment of the magnitude of the problem, prioritization of plans to cope with the problems, allocation of resources and for subsequent evaluation of the impact of interventions.
Unfortunately, such surveillance information is often lacking in the developing countries. It should be recognized that surveillance programmes in developed countries may be inappropriate for developing countries, and such systems probably cannot be adopted in their entirety for developing countries because of the various problems which may impede surveillance activities.
Problems of Surveillance in Developing Countries
While the need for surveillance of occupational safety and health problems exists in developing countries, the actual implementation of surveillance is often fraught with difficulties.
The difficulties may arise because of poor control of industrial development, the absence of, or an inadequately developed infrastructure for, occupational health legislation and services, insufficiently trained occupational health professionals, limited health services and poor health reporting systems. Very often the information on the workforce and general population may be lacking or inadequate.
Another major problem is that in many developing countries, occupational health is not accorded a high priority in national development programmes.
Activities in Occupational Health and Safety Surveillance
Surveillance of occupational safety and health may involve activities such as the monitoring of dangerous occurrences at work, work injury and work fatalities. It also includes surveillance of occupational illness and surveillance of the work environment. It is probably easier to collect information on work injury and accidental death at work, since such events are fairly easily defined and recognized. In contrast, surveillance of the health status of the working population, including occupational diseases and the state of the work environment, is more difficult.
The rest of this article will therefore deal mainly with the issue of surveillance of occupational illness. The principles and approaches which are discussed can be applied to the surveillance of work injuries and fatalities, which are also very important causes of morbidity and mortality among workers in developing countries.
Surveillance of workers’ health in developing countries should not be limited only to occupational diseases, but should also be for general diseases of the working population. This is because the main health problems among workers in some developing countries in Africa and Asia may not be occupational, but may include other general diseases such as infectious diseases—for example, tuberculosis or sexually transmitted diseases. The information collected would then be useful for planning and allocation of health care resources for the promotion of health of the working population.
Some Approaches to Overcome the Problems of Surveillance
Which types of occupational health surveillance are appropriate in developing countries? In general, a system with simple mechanisms, employing available and appropriate technology, would be best suited for developing countries. Such a system should also take into account the types of industries and work hazards which are important in the country.
Utilization of existing resources
Such a system may utilize the existing resources such as the primary health care and environmental health services. For example, occupational health surveillance activities can be integrated into the current duties of primary health care personnel, public health inspectors and environmental engineers.
For this to happen, primary health care and public health personnel have first to be trained to recognize illness which may be related to the work, and even to perform simple assessments of unsatisfactory workplaces in terms of occupational safety and health. Such personnel should, of course, receive adequate and appropriate training in order to perform these tasks.
The data on conditions of work and illness arising from work activities can be collated while such persons conduct their routine work in the community. The information collected can be channelled to regional centres, and ultimately to a central agency responsible for the monitoring of conditions of work and occupational health morbidity that is also responsible for acting on these problems.
Registry of factories and work processes
A registry of factories and work processes, as opposed to a disease registry, could be initiated. This registry would obtain information from the registration stage of all factories, including work processes and materials used. The information should be updated periodically when new work processes or materials are introduced. Where, in fact, such registration is required by national legislation, it needs to be enforced in a comprehensive manner.
However, for small-scale industries, such registration is often bypassed. Simple field surveys and assessments of the types of industry and the state of working conditions could provide basic information. The persons who could perform such simple assessments could again be the primary health care and public health personnel.
Where such a registry is in effective operation, there is also a need for periodic update of the data. This could be made compulsory for all registered factories. Alternatively, it may be desirable to request an update from factories in various high-risk industries.
Notification of occupational diseases
Legislation for notification of selected occupational health disorders could be introduced. It would be important to publicize and educate people on this matter before implementation of the law. Questions such as what diseases should be reported, and who should be the persons responsible for notification, should first be resolved. For example, in a developing country like Singapore, physicians who suspect the occupational diseases listed in table 1 have to notify the Ministry of Labour. Such a list has to be tailored to the types of industry in a country, and be revised and updated periodically. Furthermore, the persons responsible for notification should be trained to recognize, or at least to suspect, the occurrence of the diseases.
Table 1. Sample list of notifiable occupational diseases
|
Aniline poisoning |
Industrial dermatitis |
|
Anthrax |
Lead poisoning |
|
Arsenical poisoning |
Liver angiosarcoma |
|
Asbestosis |
Manganese poisoning |
|
Barotrauma |
Mercurial poisoning |
|
Beryllium poisoning |
Mesothelioma |
|
Byssinosis |
Noise-induced deafness |
|
Cadmium poisoning |
Occupational asthma |
|
Carbon disulphide poisoning |
Phosphorous poisoning |
|
Chrome ulceration |
Silicosis |
|
Chronic benzene poisoning |
Toxic anaemia |
|
Compressed air illness |
Toxic hepatitis |
Continuous follow-up and enforcement action is needed to ensure the success of such notification systems. Otherwise, gross underreporting would limit their usefulness. For example, occupational asthma was first made notifiable and compensable in Singapore in 1985. An occupational lung disease clinic was also set up. Despite these efforts, a total of only 17 cases of occupational asthma were confirmed. This can be contrasted with the data from Finland, where there were 179 reported cases of occupational asthma in 1984 alone. Finland’s population of 5 million is only about twice that of Singapore. This gross under-reporting of occupational asthma is probably due to the difficulty in diagnosing the condition. Many doctors are unfamiliar with the causes and features of occupational asthma. Hence, even with the implementation of compulsory notification, it is important to continue to educate the health professionals, employers and employees.
When the notification system is initially implemented, a more accurate assessment of the prevalence of the occupational disease can be made. For example, the number of notifications of noise-induced hearing loss in Singapore increased six-fold after statutory medical examinations were introduced for all noise-exposed workers. Subsequently, if the notification is fairly complete and accurate, and if a satisfactory denominator population could be obtained, it may even be possible to estimate the incidence of the condition and its relative risk.
As in many notification and surveillance systems, the important role of notification is to alert the authorities to index cases at the workplace. Further investigations and workplace interventions, if necessary, are required follow-up activities. Otherwise, the efforts of notification would be wasted.
Other sources of information
Hospital and outpatient health information is often underutilized in the surveillance of occupational health problems in a developing country. Hospitals and outpatient clinics can and should be incorporated into the notification system for specific diseases, such as acute work-related poisonings and injuries. The data from these sources would also provide an idea of the common health problems among workers, and can be used for the planning of workplace health promotion activities.
All this information is usually routinely collected, and few extra resources are required to direct the data to the occupational health and safety authorities in a developing country.
Another possible source of information would be the compensation clinics or tribunals. Finally, if the resources are available, some regional occupational medicine referral clinics might also be initiated. These clinics could be staffed by more qualified occupational health professionals, and would investigate any suspected work-related illness.
Information from existing disease registries should also be utilized. In many larger cities of developing countries, cancer registries are in place. Though the occupational history obtained from these registries may not be complete and accurate, it is useful for preliminary monitoring of broad occupational groups. Data from such registries will be even more valuable if registers of workers exposed to specific hazards are available for cross-matching.
The role of data linkage
While this may sound attractive, and has been employed with some success in some developed countries, this approach may not be appropriate or even possible in developing countries at present. This is because the infrastructure required for such a system is often not available in developing countries. For example, disease registries and workplace registers may not be available or, if they exist, may not be computerized and easily linked.
Help from international agencies
International agencies such as the International Labour Organization, the World Health Organization and bodies such as the International Commission on Occupational Health can contribute their experience and expertise in overcoming common problems of occupational health and safety surveillance in a country. In addition, training courses as well as training opportunities for primary care persons may be developed or offered.
Sharing of information from regional countries with similar industries and occupational health problems is also often useful.
Summary
Occupational safety and health services are important in developing countries. This is especially so in view of the rapid industrialization of the economy, the vulnerable work population and the poorly controlled health hazards faced at work.
In the development and delivery of occupational health services in these countries, it is important to have some type of surveillance of occupational ill health. This is necessary for the justification, planning and prioritization of occupational health legislation and services, and the evaluation of the outcome of these measures.
While surveillance systems are in place in the developed countries, such systems may not always be appropriate for developing countries. Surveillance systems in developing countries should take into account the type of industry and hazards which are important in the country. Simple surveillance mechanisms, employing available and appropriate technology, are often the best options for developing countries.
Workers with Special Needs
Designing for Disabled Persons is Designing for Everyone
There are so many products on the market that readily reveal their unfitness for the general population of users. What evaluation should one make of a doorway too narrow to comfortably accommodate a stout person or pregnant woman? Shall its physical design be faulted if it satisfies all relevant tests of mechanical function? Certainly such users cannot be regarded as disabled in any physical sense, since they may be in a state of perfect health. Some products need considerable handling before one can force them to perform as desired—certain inexpensive can openers come, not altogether trivially, to mind. Yet a healthy person who may experience difficulty operating such devices need not be considered disabled. A designer who successfully incorporates considerations of human interaction with the product enhances the functional utility of his or her design. In the absence of good functional design, people with a minor disability may find themselves in the position of being severely hampered. It is thus the user-machine interface that determines the value of design for all users.
It is a truism to remind oneself that technology exists to serve human beings; its use is to enlarge their own capabilities. For disabled persons, this enlargement has to be taken some steps further. For instance in the 1980s, a good deal of attention was paid to the design of kitchens for disabled people. The experience gained in this work penetrated design features for “normal” kitchens; the disabled person in this sense may be considered a pioneer. Occupationally-induced impairments and disabilities—one has but to consider the musculoskeletal and other complaints suffered by those confined to sedentary tasks so common in the new workplace—similarly call for design efforts aimed not only also preventing the recurrence of such conditions, but at the development of user-compatible technology adapted to the needs of workers already affected by work-related disorders.
The Broader Average Person
The designer should not focus on a small, unrepresentative population. Among certain groups it is most unwise to entertain assumptions concerning similarities among them. For example, a worker injured in a certain way as an adult may not necessarily be anthropometrically quite so different from an otherwise comparable, healthy person, and may be considered as part of the broad average. A young child so injured will display a considerably different anthropometry as an adult since his muscular and mechanical development will be steadily and sequentially influenced by preceding growth stages. (No conclusions as to comparability as adults ought to be ventured as regards the two cases. They must be regarded as two distinct, specific groups, only the one being included among the broad average.) But as one strives for a design suitable for, say, 90% of the population, one should exert fractionally greater pains to increase this margin to, say, 95%, the point being that in this way the need for design for specific groups can be reduced.
Another way to approach design for the broader average population is to produce two products, each one designed roughly to fit the two percentile extremes of human differences. Two sizes of chair, for instance, might be built, the one with brackets allowing it to be adjusted in height from 38 to 46 cm, and the other one from 46 to 54 cm; two sizes of pliers already exist, one fitting larger and average sizes of men’s hands and the other fitting average women’s hands and hands of smaller men.
It would be a well-advised company policy to reserve annually a modest amount of money to have worksites analysed and made more suitable for workers, a move that would prevent illness and disability due to excessive physical load. It also increases the motivation of workers when they understand that management is actively trying to improve their work environment, and more impressively so when elaborate measures sometimes have to be undertaken: thorough work analysis, the construction of mock-ups, anthropometrical measurements, and even the specific design of units for the workers. In a certain company, in fact, the conclusion was that the units should be redesigned at every worksite because they caused physical overload in the form of too much standing, there were unsuitable dimensions associated with the seated positions, and there were other deficiencies as well.
Costs, Benefits and Usability of Design
Cost/benefit analyses are developed by ergonomists in order to gain insight into the results of ergonomic policies other than those that are economic. In the present day, evaluation in the industrial and commercial realms includes the negative or positive impact of a policy on the worker.
Methods of evaluating quality and usability are currently the subject of active research. The Rehabilitation Technology Useability Model (RTUM), as shown in figure 1, can be utilized as a model for evaluating the usability of a product within rehabilitation technology and to illuminate the various aspects of the product which determine its usability.
Figure 1. The Rehabilitation Technology Useability Model (RTUM)
From the strictly economic point of view, the costs of creating a system in which a given task can be performed or in which a certain product can be made can be specified; it scarcely needs mentioning that in these terms each company is interested in a maximum return on its investment. But how can the real costs of task performance and product manufacturing in relation to financial investment be determined when one takes into account the varying exertions of workers’ physical, cognitive and mental systems? In fact, the judging of human performance itself is, among other factors, based on the workers’ perception of what has to be done, their view of their own value in doing it, and their opinion of the company. It is actually the intrinsic satisfaction with work that is the norm of value in this context, and this satisfaction, together with the aims of the company, constitute one’s reason for performing. Worker well-being and performance are thus based on a wide spectrum of experiences, associations and perceptions that determine attitudes towards work and the ultimate quality of performance—an understanding upon which the RTUM model is predicated.
If one does not accept this view, it becomes necessary to regard investment only in relation to doubtful and unspecified results. If ergonomists and physicians wish to improve the work environment of disabled people—to produce more from machine operations and enhance the usability of the tools used—they will encounter difficulties in finding ways to justify the financial investment. Typically, such justification has been sought in savings realized by prevention of injury and illness due to work. But if the costs of illness have been borne not by the company but by the state, they become financially invisible, so to speak, and are not seen as work-related.
Nevertheless, the awareness that investment in a healthy working environment is money well spent has been growing with the recognition that the “social” costs of incapacities are translatable in terms of ultimate costs to a country’s economy, and that value is lost when a potential worker is sitting about at home making no contribution to society. Investing in a workplace (in terms of adapting a work station or providing special tools or perhaps even help in personal hygiene) can not only reward a person with job satisfaction but can help make him or her self-sufficient and independent of social assistance.
Cost/benefit analyses can be carried out in order to determine whether special intervention in the workplace is justified for disabled persons. The following factors represent sources of data that would form the object of such analyses:
1. Personnel
- Absence. Will the disabled worker have a satisfactory attendance record?
- Is it likely that extra costs may be incurred for special task instruction?
- Are personnel changes called for? Their costs must be considered also.
- Can accident compensation rates be expected to increase?
2. Safety
- Will the job being considered for the disabled worker involve safety regulations?
- Will special safety regulations be involved?
- Is the work characterized by a considerable frequency of accidents or near accidents?
3. Medical
- As regards the worker whose disability is being examined with a view to his or her re-entry into the workplace, the nature and seriousness of the incapacity must be assessed.
- The extent of the disabled worker’s absence must also be taken into account.
- What is the character and frequency of the worker’s “minor” symptoms, and how are they to be dealt with? Can the future development of related “minor” illnesses capable of hampering the worker’s efficiency be foreseen?
As concerns time lost from work, these calculations can be made in terms of wages, overhead, compensation and lost production. The sort of analyses just described represents a rational approach by which an organization can arrive at an informed decision as to whether a disabled worker is better off back on the job and whether the organization itself will gain by his or her return to work.
In the preceding discussion, designing for the broader population has received a focus of attention heightened by emphasis on specific design in relation to usability and the costs and benefits of such design. It is still a difficult task to make the needed calculations, including all relevant factors, but at present, research efforts are continuing that incorporate modelling methods in their techniques. In some countries, for example the Netherlands and Germany, government policy is making companies more responsible for job-related personal harm; fundamental changes in regulatory policies and insurance structures are, clearly, to be expected to result from trends of this sort. It has already become a more or less settled policy in these countries that a worker who suffers a disabling accident at work should be provided with an adapted work station or be able to perform other work within the company, a policy that has made the treatment of the disabled a genuine achievement in the humane treatment of the worker.
Workers with Limited Functional Capacity
Whether design is aimed at the disabled or at the broader average, it is hindered by a scarcity of research data. Handicapped people have been the subjects of virtually no research efforts. Therefore, in order to set up a product requirements document, or PRD, a specific empirical research study will have to be undertaken in order to gather that data by observation and measurement.
In gathering the information needed about the disabled worker or user it is necessary to consider not only the current functional status of the disabled person, but to make the attempt to foresee whatever changes might be the result of the progression of a chronic condition. This kind of information can, in fact, be elicited from the worker directly, or a medical specialist can supply it.
In designing, for instance, a work action to which data about the worker’s physical strength is relevant, the designer will not choose as a specification the maximum strength which the disabled person can exert, but will take into account any possible diminution in strength that a progression in the worker’s condition might bring about. Thus the worker will be enabled to continue to use the machines and tools adapted or designed for him or at the work station.
Furthermore, designers should avoid designs that involve manipulations of the human body at the far extremes of, say, the range of motion of a body part, but should accommodate their designs to the middle ranges. A simple but very common illustration of this principle follows. A very common part of the drawers of kitchen and office cabinets and desks is a handle that has the form of a little shelf under which one places the fingers, exerting upward and forward force to open the drawer. This manoeuvre requires 180 degrees of supination (with the palm of the hand up) in the wrist—the maximum point for the range of this sort of motion of the wrist. This state of affairs may present no difficulty for a healthy person, provided that the drawer can be opened with a light force and is not awkwardly situated, but makes for strain when the action of the drawer is tight or when the full 180-degree supination is not possible, and is a needless burden on a disabled person. A simple solution—a vertically placed handle—would be mechanically far more efficient and more easily manipulated by a larger portion of the population.
Physical Functioning Ability
In what follows, the three chief areas of limitation in physical functional ability, as defined by the locomotion system, the neurological system and the energy system, will be discussed. Designers will gain some insight into the nature of user/worker constraints in considering the following basic principles of bodily functions.
The locomotion system. This consists of the bones, joints, connective tissues and muscles. The nature of the joint structure determines the range of motion possible. A knee joint, for example, shows a different degree of movement and stability than the joint of the hip or the shoulder. These varying joint characteristics determine the actions possible to the arms, hands, feet, and so on. There are also different types of muscle; it is the type of muscle, whether the muscle passes over one or two joints, and the location of the muscle that determines, for a given body part, the direction of its movement, its speed, and the strength which it is capable of exerting.
The fact that this direction, speed and strength can be characterized and calculated is of great importance in design. For disabled people, one has to take it into account that the “normal” locations of muscles have been disturbed and that the range of motion in joints has been changed. In an amputation, for instance, a muscle may function only partly, or its location may have changed, so that one has to examine the physical ability of the patient carefully to establish what functions remain and how reliable they may be. A case history follows.
A 40-year-old carpenter lost his thumb and the third finger of his right hand in an accident. In an effort to restore the carpenter’s capacity for work, a surgeon removed one of the patient’s great toes and he replaced the missing thumb with it. After a period of rehabilitation, the carpenter returned to work but found it impossible to do sustained work for more than three to four hours. His tools were studied and found to be unfitted to the “abnormal” structure of his hand. The rehabilitation specialist, examining the “redesigned” hand from the point of view of its new functional ability and form was able to have new tools designed that were more appropriate and usable with respect to the altered hand. The load on the worker’s hand, previously too heavy, was now within a usable range, and he regained his ability to continue work for a longer time.
The neurological system. The neurological system can be compared to a very sophisticated control room, complete with data collectors, whose purpose it is to initiate and govern one’s movements and actions by interpreting information relating to those aspects of the body’s components relating to position and mechanical, chemical and other states. This system incorporates not only a feedback system (e.g., pain) that provides for corrective measures, but a “feed-forward” capability which expresses itself anticipatorily so as to maintain a state of equilibrium. Consider the case of a worker who reflexively acts so as to restore a posture in order to protect himself from a fall or from contact with dangerous machine parts.
In disabled persons, the physiological processing of information can be impaired. Both the feedback and the feed-forward mechanisms of visually impaired people are weakened or absent, and the same is true, on an acoustic level, among the hearing-impaired. Furthermore the important governing circuits are interactive. Sound signals have an effect on the equilibrium of a person in conjunction with proprioceptive circuits that situate our bodies in space, so to speak, via data gathered from muscles and joints, with the further help of visual signals. The brain can function to overcome quite drastic deficiencies in these systems, correcting for errors in the coding of information and “filling in” missing information. Beyond certain limits, to be sure, incapacity supervenes. Two case histories follow.
Case 1. A 36-year-old woman suffered a lesion of the spinal cord due to an automobile accident. She is able to sit up without assistance and can move a wheelchair manually. Her trunk is stable. The feeling in her legs is gone, however; this defect includes an inability to sense temperature changes.
She has a sitting workplace at home (the kitchen is designed to allow her to work in a seated position). The safety measure has been taken of installing a sink in a position sufficiently isolated that the risk of burning her legs with hot water is minimized, since her inability to process temperature information in the legs leaves her vulnerable to being unaware of being burned.
Case 2. A five-year-old boy whose left side was paralysed was being bathed by his mother. The doorbell rang, the mother left the boy alone to go to the front door, and the boy, turning on the hot-water tap, suffered burns. For safety reasons, the bath should have been equipped with a thermostat (preferably one that the boy could not have overridden).
The energy system. When the human body has to perform physical labour, physiological changes, notably in the form of interactions in the muscle cells, take place, albeit relatively inefficiently. The human “motor” converts only about 25% of its energy supply to mechanical activity, the remainder of the energy representing thermal losses. The human body is therefore not especially suited to heavy physical labour. Exhaustion sets in after a certain time, and if heavy labour has to be performed, reserve energy sources are drawn upon. These sources of reserve energy are always used whenever work is carried out very rapidly, is started suddenly (without a warm-up period) or involves heavy exertion.
The human organism obtains energy aerobically (via oxygen in the bloodstream) and anaerobically (after depleting aerobic oxygen, it calls upon small, but important reserve units of energy stored in muscle tissue). The need for fresh air supplies in the workplace naturally draws the focus of discussion of oxygen usage toward the aerobic side, working conditions that are strenuous enough to call forth anaerobic processes on a regular basis being extraordinarily uncommon in most workplaces, at least in the developed countries. The availability of atmospheric oxygen, which relates so directly to human aerobic functioning, is a function of several conditions:
- Ambient air pressure (approximately 760 torr, or 21.33 kPa at sea level). High-altitude task performance can be profoundly affected by oxygen deficiency and is a prime consideration for workers in such conditions.
- For workers doing heavy labour, ventilation is necessary to ensure refreshment of the air supply, allowing the volume of air respired per minute to be increased.
- Ambient oxygen makes its way into the bloodstream via the alveoli by diffusion. At higher blood pressures, the diffusion surface is enlarged and thereby the oxygen capacity of the blood.
- An increase in oxygen diffusion to the tissues causes an increase of the diffusion surface and consequently of the oxygen level.
- People with certain heart problems suffer when, with increased cardiac output (together with the oxygen level), the blood circulation changes in favour of the muscles.
- By contrast with oxygen, because of the large reserves of glucose, and especially fat, the energy source (“fuel”) need not be continuously delivered from the outside. In heavy labour, it is merely glucose, with its high energy value, that is used. With lighter work, fat is called upon, at a rate varying with the individual. A brief, general case history follows.
A person suffering from asthma or bronchitis, both of which are diseases affecting the lungs, causes the worker severe limitation in his or her work. The work assignment of this worker should be analysed with respect to factors such as physical load. The environment should be analysed as well: clean ambient air will contribute substantially to workers’ well-being. Furthermore, the workload should be balanced through the day, avoiding peak loads.
Specific Design
In some cases, however, there is still a need for specific design, or design for very small groups. Such a need arises when the tasks to be performed and the difficulties a disabled person is experiencing are excessively large. If the needed specific requirements cannot be made with the available products on the market (even with adaptations), specific design is the answer. Whether this sort of solution may be costly or cheap (and aside from humanitarian issues) it must be nonetheless regarded in the light of workability and support to the firm’s viability. A specially designed worksite is worthwhile economically only when the disabled worker can look forward to working there for years and when the work he or she does is, in production terms, an asset to the company. When this is not the case, although the worker may indeed insist upon his or her right to the job, a sense of realism should prevail. Such touchy problems should be approached in a spirit of seeking a solution by cooperative endeavours at communication.
The advantages of specific design are as follows:
- The design is custom made: it fits the problems to be solved to perfection.
- The worker so served can return to work and a life of social participation.
- The worker can be self-sufficient, independent of welfare.
- The costs of any personnel changes that the alternative might involve are avoided.
The disadvantages of specific design are:
- The design is unlikely to be used for even one other person, let alone a larger group.
- Specific design is often costly.
- Specifically designed products must often be handmade; savings owing to mass methods are most often not realizable.
Case 1. For example, there is the case of a receptionist in a wheelchair who had a speech problem. Her speech difficulty made for rather slow conversations. While the firm remained small, no problems arose and she continued to work there for years. But when the firm enlarged, her disabilities began to make themselves problematic. She had to speak more rapidly and to move about considerably faster; she could not cope with the new demands. However, solutions to her troubles were sought and reduced themselves to two alternatives: special technical equipment might be installed so that the deficiencies that degraded the quality of some of her tasks could be compensated for, or she could simply choose a set of tasks involving a more desk-bound workload. She chose the latter course and still works for the same company.
Case 2. A young man, whose profession was the production of technical drawings, suffered a high level spinal cord lesion due to diving in shallow waters. His injury is severe enough for him to require help with all his daily activities. Nevertheless, with the help of a computer-aided design (CAD) software, he continues to be able make his living at technical drawing and lives, financially independent, with his partner. His work space is a study adapted for his needs and he works for a firm with which he communicates by computer, phone and fax. To operate his personal computer, he had to have certain adaptations made to the keyboard. But with these technical assets he can earn a living and provide for himself.
The approach for specific design is not different from other design as described above. The only insurmountable problem that may arise during a design project is that the design objective cannot be achieved on purely technical grounds—in other words, it can’t be done. For example, a person suffering from Parkinson’s disease is prone, at a certain stage in the progression of his or her condition, to fall over backwards. An aid which would prevent such an eventuality would of course represent the desired solution, but the state of the art is not such that such a device can yet be built.
System Ergonomic Design and Workers with Special Physical Needs
One can treat bodily impairment by medically intervening to restore the damaged function, but the treatment of a disability, or deficiency in the ability to perform tasks, can involve measures far less developed in comparison with medical expertise. As far as the necessity of treating a disability is concerned, the severity of the handicap strongly influences such a decision. But given that treatment is called for, however, the following means, taken singly or in combination, form the choices available to the designer or manager:
- leaving out a task
- compensating for a worker’s deficiency in performing a task element by using a machine or another person’s help
- differentiation of the task order, that is, dividing the task into more manageable subtasks
- modification of the tools used in the task
- special design of tools and machines.
From the specific ergonomic point of view, treatment of a disability includes the following:
- modification of the task
- modification of a tool
- design of new tools or new machines.
The issue of efficacy is always the point of departure in the modification of tools or machines, and is often related to the costs devoted to the modification in question, the technical features to be addressed, and the functional changes to be embodied in the new design. Comfort and attractiveness are qualities that by no means deserve to be neglected among these other characteristics.
The next consideration relating to design changes to be made to a tool or machine is whether the device is one already designed for general use (in which case, modifications will be made to a pre-existing product) or is to be designed with an individual type of disability in mind. In the latter case, specific ergonomic considerations must be devoted to each aspect of the worker’s disability. For example, given a worker suffering from limitations in brain function after a stroke, impairments such as aphasia (difficulty in communication), a paralysed right arm, and a spastic paresis of the leg preventing its being moved upwards might require the following adjustments:
- a personal computer or other device enabling the worker to communicate
- tools that can be operated with the remaining useful arm
- a prosthetic system that would serve to restore the function of the impaired foot as well as to compensate for the patient’s loss of ability to walk.
Is there any general answer to the question of how to design for the disabled worker? The system ergonomic design (SED) approach is an eminently suitable one for this task. Research related to the work situation or to the kind of product at issue requires a design team for the purpose of gathering special information relating either to a special group of disabled workers or to the unique case of an individual user disabled in a particular way. The design team will, by virtue of including a diversity of qualified people, be in possession of expertise beyond the technical sort expected of a designer alone; the medical and ergonomic knowledge shared among them will be as fully applicable as the strictly technical.
Design constraints determined by assembling data related to disabled users are treated with the same objectivity and in the same analytical spirit as are counterpart data relating to healthy users. Just as for the latter, one has to determine for disabled persons their personal patterns of behavioural response, their anthropometrical profiles, biomechanical data (as to reach, strength, range of motion, handling space used, physical load and so forth), ergonomic standards and safety regulations. But one is most regretfully obliged to concede that very little research indeed is done on behalf of disabled workers. There exist a few studies on anthropometry, somewhat more on biomechanics in the field of prostheses and orthoses, but hardly any studies have been carried on physical load capabilities. (The reader will find references to such material in the “Other relevant reading” list at the end of this chapter.) And while it is sometimes easy to gather and apply such data, frequently enough the task is difficult, and in fact, impossible. To be sure, one must obtain objective data, however strenuous the effort and unlikely the chances of doing so, given that the numbers of disabled persons available for research is small. But they are quite often more than willing to participate in whatever research they are offered the opportunity of sharing in, since there is great consciousness of the importance of such a contribution towards design and research in this field. It thus represents an investment not only for themselves but for the larger community of disabled people.
Development and Application of an Occupational Injury and Illness Classification System
Systems of workplace injury and illness surveillance constitute a critical resource for management and reduction of occupational injuries and illnesses. They provide essential data which can be used to identify workplace problems, develop corrective strategies and thus prevent future injuries and illnesses. To accomplish these goals effectively, surveillance systems must be constructed which capture the characteristics of workplace injuries in considerable detail. To be of maximum value, such a system should be able to provide answers to such questions as which workplaces are the most hazardous, which injuries produce the most time lost from work and even what part of the body is injured most frequently.
This article describes the development of an exhaustive classification system by the Bureau of Labor Statistics of the United States Department of Labor (BLS). The system was developed to meet the needs of a variety of constituencies: state and federal policy analysts, safety and health researchers, employers, employee organizations, safety professionals, the insurance industry and others involved in promoting safety and health in the workplace.
Background
For a number of years, the BLS has collected three basic types of information concerning an occupational injury or illness:
- industry, geographic location of the incident and any associated lost workdays
- characteristics of the affected employee, such as age, gender and occupation
- how the incident or exposure occurred, the objects or substances involved, the nature of the injury or illness and part of the body affected.
The previous classification system, though useful, was somewhat limited and did not fully meet the needs described above. In 1989 it was decided that a revision of the existing system was in order that would best suit the needs of the varied users.
The Classification System
A BLS task force was organized in September 1989 to establish requirements for a system that would “accurately describe the nature of the occupational safety and health problem” (OSHA 1970). This team worked in consultation with safety and health specialists from the public and private sectors, with the goal of developing a revamped and expanded classification system.
Several criteria were established governing the individual code structures. The system must have a hierarchical arrangement to allow maximum flexibility for varied users of occupational injury and illness data. The system should be, to the extent possible, compatible with the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) of the WHO (1977). The system should meet the needs of other government agencies involved in the safety and health arena. Finally, the system must be responsive to the differing traits of nonfatal and fatal cases.
Drafts of the case characteristic classification structures were produced and released for comment in 1989 and again in 1990. The system included nature of injury or illness, part of body affected, source of injury or illness, event or exposure structures and secondary source. Comments were received and incorporated from bureau staff, state agencies, Occupational Safety and Health Administration, Employment Standards Administration and NIOSH, after which the system was ready for an onsite test.
Pilot testing of the structures for compiling data for nonfatal injuries and illnesses, as well as the operational application in the Census of Fatal Occupational Injuries, was conducted in four states. Test results were analysed and revisions completed by the fall of 1991.
The final 1992 version of the classification system consists of five case characteristic code structures, an occupational code structure and an industry code structure. The Standard Industrial Classification Manual is used to classify industry (OMB 1987), and the Bureau of the Census Alphabetical Index of Occupations for coding occupation (Bureau of the Census 1992). The BLS Occupational Injury and Illness Classification System (1992) is used to code the following five characteristics:
- nature of injury or illness
- part of body affected
- event or exposure
- source of injury or illness
- secondary source of injury or illness.
Besides numerical codes that represent specific conditions or circumstances, each code structure includes aids to assist in identification and selection of the proper code. These aids include: definitions, rules of selection, descriptive paragraphs, alphabetical listings and edit criteria for each of the structures. The rules of selection offer guidance to choose the appropriate code uniformly when two or more code selections are possible. The descriptive paragraphs provide additional information about the codes such as what is included or excluded in a particular code. For instance, the code for eye includes the eyeball, the lens, the retina and the eyelashes. The alphabetical listings can be used to quickly find the numerical code for a specific characteristic, such as medical terminology or specialized machinery. Finally, edit criteria are quality-assurance tools that can be used to determine which code combinations are incorrect prior to final selection.
Nature of injury or illness codes
The nature of injury or illness code structure describes the principal physical characteristic of the worker’s injury or illness. This code serves as the basis for all other case classifications. Once the nature of injury or illness has been identified, the remaining four classifications represent the circumstances associated with that particular outcome. The classification structure for nature of injury of illness contains seven divisions:
- traumatic injuries and disorders
- systemic diseases or disorders
- infectious and parasitic diseases
- neoplasms, tumours and cancer
- symptoms, signs and ill-defined conditions
- other conditions or disorders
- multiple diseases, conditions or disorders.
Before finalizing this structure, two similar classifications systems were evaluated for possible adoption or emulation. Because the American National Standards Institute (ANSI) Z16.2 standard (ANSI 1963) was developed for use in accident prevention, it does not contain a sufficient number of illness categories for many agencies to accomplish their missions.
The ICD-9-CM, designed for classifying morbidity and mortality information and used by a large portion of the medical community, provides the required detailed codes for illnesses. However, technical knowledge and training requirements for users and compilers of these statistics made this system prohibitive.
The final structure arrived at is a hybrid which combines the application method and rules of selection from the ANSI Z16.2 with the basic divisional organization from the ICD-9-CM. With few exceptions, divisions in the BLS structure can be directly mapped to the ICD-9-CM. For example, the BLS division identifying infectious and parasitic diseases maps directly to Chapter 1, Infectious and Parasitic Diseases, of the ICD-9-CM.
The first division in the BLS nature of injury or illness structure classifies traumatic injuries and disorders, effects of external agents and poisoning, and corresponds to Chapter 17 of the ICD-9-CM. Outcomes in this division are generally the result of a single incident, event or exposure, and include conditions such as fractures, bruises, cuts and burns. In the occupational environment, this division accounts for the great majority of reported cases.
Several situations required careful consideration when establishing rules to select codes in this division. Review of fatality cases revealed difficulties in coding certain types of fatal injuries. For example, fatal fractures usually involve direct or indirect mortal damage to a vital organ, such as the brain or spinal column. Specific coding categories and instructions were required to note the mortal damage associated with these types of injuries.
Gunshot wounds constitute a separate category with special instructions for those instances in which such wounds also resulted in amputations or paralysis. In keeping with an overall philosophy of coding the most serious injury, paralysis and amputations take precedence over less serious damage from a gunshot wound.
Responses to questions on employer reporting forms concerning what happened to the injured or ill worker do not always adequately describe the injury or illness. If the source document indicates only that the employee “hurt his back”, it is not appropriate to assume this is a sprain, strain, dorsopathy or any other specific condition. To solve the problem, individual codes were established for non-specific descriptions of injury or illness like “sore,” “hurt” and “pain”.
Finally, this division has a section of codes to classify the most frequently occurring combinations of conditions that result from the same incident. For example, a worker may suffer both scratches and bruises from a single incident.
Five of the remaining divisions of this classification structure were devoted to identification of occupational diseases and disorders. These sections present codes for specific conditions that are of paramount interest to the safety and health community. In recent years, a growing number of diseases and disorders have been linked to the work environment but were seldom represented in the existing classification structures. The structure has a vastly expanded list of specific diseases and disorders such as carpal tunnel syndrome, Legionnaire’s disease, tendonitis and tuberculosis.
Part of body affected
The part of body affected classification structure specifies the part of the body which was directly affected by the injury or illness. When linked with the nature of injury or illness code, it provides a more complete picture of the damage incurred: amputated finger, lung cancer, fractured jaw. This structure consists of eight divisions:
- head
- neck, including throat
- trunk
- upper extremities
- lower extremities
- body systems
- multiple body parts
- other body parts.
Three issues surfaced during evaluation of redesign options for this theoretically simple and straightforward piece of the classification system. The first was the merit of coding external location (arm, trunk, leg) of the injury or illness versus the affected internal site (heart, lungs, brain).
Test results indicated that coding the internal part of body affected was appropriate for diseases and disorders, but extremely confusing when applied to many traumatic injuries such as cuts or bruises. The BLS developed a policy of coding the external location for most traumatic injuries and coding internal locations, where appropriate, for diseases.
The second issue was how to handle diseases that affect more than one body system simultaneously. For instance, hypothermia, a condition of low body temperature due to exposure to the cold, can affect the nervous and endocrine systems. Because it is difficult for nonmedical personnel to determine which is the appropriate choice, this could lead to a tremendous amount of research time with no clear resolution. Therefore, the BLS system was designed with a single entry, body systems, that categorizes one or more body systems.
Adding detail to identify typical combinations of parts in the upper extremities and the lower extremities was the third major enhancement to this code structure. These combinations, such as hand and wrist, proved to be supportable by the source documents.
Event or exposure
The event or exposure code structure describes the manner in which the injury or illness was inflicted or produced. The following eight divisions were created to identify the primary method of injury or exposure to a harmful substance or situation:
- contact with objects and equipment
- falls
- bodily reaction and exertion
- exposure to harmful substances or environments
- transportation accidents
- fires and explosions
- assaults and violent acts
- other events or exposures.
Injury-producing incidents are frequently composed of a series of events. To illustrate, consider what occurs in a traffic accident: A car hits a guard-rail, crosses the median strip and collides with a truck. The driver has several injuries from striking parts of the car and being struck by broken glass. If the micro-events—such as hitting the windshield or being struck by flying glass—were coded, the overall fact that the person was in a traffic accident could be missed.
In these multiple event instances, the BLS designated several occurrences to be considered primary events and to take precedence over other micro-events associated with them. These primary events included:
- assaults and violent acts
- transportation accidents
- fires
- explosions.
An order of precedence was established within these groups as well because they frequently overlap—for example, a highway accident can involve a fire. This order of precedence is the order which they appear in the above list. Assaults and violent acts were assigned first precedence. Codes within this division generally describe the type of violence, while the weapon is addressed in the source code. Transportation accidents are next in precedence, followed by fires and explosions.
These last two events, fires and explosions, are combined in a single division. Because the two often occur simultaneously, an order of precedence between the two had to be established. In accordance with the ICD-9 Supplementary Classification of External Causes, fires were given precedence over explosions (USPHS 1989).
Selection of codes for inclusion in this structure was influenced by the emergence of non-contact disorders that are associated with the activities and ergonomics of the job. These cases typically involve nerve, muscle or ligament damage brought about by exertion, repetitive motion and even simple body motions such as when the worker’s back “goes out” when reaching over to pick up an item. Carpal tunnel syndrome is now widely recognized to be tied to repetitive actions such as key entry, typing, cutting actions and even operating a cash register. The division bodily reaction and exertion identifies these non-contact, or non-impact, incidents.
The event division “exposure to harmful substances or environments” distinguishes the specific method of exposure to toxic or harmful substances: inhalation, skin contact, ingestion or injection. A separate category to identify the transmission of an infectious agent through a needle stick was developed. Also included in this division are other non-impact incidents in which the worker was harmed by electric power or by environmental conditions, such as extreme cold.
Contact with objects and equipment and falls are the divisions that will capture most impact events that injure workers.
Source of injury or illness
The source of injury or illness classification code identifies the object, substance, bodily motion or exposure which directly produced or inflicted the injury or illness. If a worker is cut on the head by a falling brick, the brick is the source of injury. There is a direct relationship between the source and the nature of the injury or illness. If a worker slips on oil and falls to the floor, breaking an elbow, the fracture is produced by hitting the floor, so the floor is source of injury. This code system contains ten divisions:
- chemicals and chemical products
- containers
- furniture and fixtures
- machinery
- parts and materials
- persons, plants, animals and minerals
- structures and surfaces
- tools, instruments and equipment
- vehicles
- other sources.
The general definitions and coding concepts for the new BLS Source Classification Structure were carried over from the ANSI Z16.2 classification system. However, the task of developing a more complete and hierarchical code listing was initially daunting, since virtually any item or substance in the world can qualify as a source of injury or illness. Not only can everything in the world qualify as source, so can pieces or parts of everything in the world. To add to the difficulty, all candidates for inclusion in the source codes had to be grouped into only ten divisional categories.
Examination of historical data on work injuries and illness identified areas where the previous code structure was inadequate or out of date. The machinery and tools sections needed expansion and updating. There was no code for computers. Newer technology had made the list of power tools obsolete, and many items listed as nonpowered tools were now almost always powered: screwdrivers, hammers and so on. There was a demand from users to expand and update the list of chemicals in the new structure. The US Occupational Safety and Health Administration requested expanded detail for a variety of items, including several types of scaffolds, forklifts and construction and logging machines.
The most difficult aspect of developing the source structure was organizing the items required for inclusion into distinct divisions and groups within the division. To add to the difficulty, the source code categories had to be mutually exclusive. But no matter what categories were developed, there were many items that logically fit in two or more divisions. For example, there was general agreement that there should be separate categories for vehicles and for machines. However, reviewers disagreed about whether certain equipment such as road pavers or forklifts, belonged with machines or vehicles.
Another area of debate developed on how to group the machines within the machinery division. The options included associating machines with a process or an industry (for example, agricultural or garden machines), grouping them by function (printing machines, heating and cooling machinery) or by type of object processed (metal working, woodworking machines). Unable to find a single solution which was workable for all types of machines, the BLS compromised with a listing that uses an industry function for some groups (agricultural machines, construction and logging machines), general function for other groups (material handling machines, office machines), and some material-specific functional groupings (metalworking, woodworking). Where the possibility of overlap occurred, such as a woodworking machine used for construction work, the structure defined the category to which it belonged, to keep the codes mutually exclusive.
Special codes were added to capture information on injuries and illnesses occurring in the health care industry, which has emerged as one of the largest employment sectors in the United States, and one with serious safety and health problems. As an example, many of the participating state agencies recommended inclusion of a code for patients and residents of health care facilities, since nurses and health aides can be hurt while trying to lift, move or otherwise care for their patients.
Secondary source of injury or illness
The BLS and other data users recognized that the occupational injury and illness source classification structure captures the object that produced the injury or illness but sometimes fails to identify other important contributors to the event. In the previous system, for example, if a worker was struck by a piece of wood that flew off a jammed saw, the wood was the source of injury; the fact that a power saw was involved was lost. If a worker was burned by fire, the flame was selected as the source of injury; one could not also identify the source of the fire.
To make up for this potential loss of information, the BLS developed a secondary source of injury or illness which “identifies the object, substance, or person that generated the source or injury or illness or that contributed to the event or exposure”. Within the specific rules of selection for this code, the emphasis is on identifying the machines, tools, equipment or other energy-generating substances (such as flammable liquids) that are not identified through source classification. In the first example noted above, the power saw would be the secondary source, since it threw out the piece of wood. In the latter example, the substance that ignited (grease, gasoline and so on) would be named as the secondary source.
Implementation Requirements: Review, Verification and Validation
Establishing a comprehensive classification system is only one step in assuring that accurate information concerning workplace injuries and illnesses is captured and available for use. It is important that workers in the field understand how to apply the coding system accurately, uniformly and according to the system design.
The first step in quality assurance was to thoroughly train those who will be assigning the classification system codes. Beginning, intermediate and advanced courses were developed to assist in uniform coding techniques. A small group of trainers was charged with delivering these courses to concerned personnel throughout the United States.
Electronic edit checks were devised to assist in the review, verification and validation process for the case characteristic and demographic estimates. Criteria of what can and cannot be combined were identified and an automated system to identify those combinations as errors was put into place. This system has over 550 groups of cross check which verify that the incoming data meet quality checks. For example, a case that identified carpal tunnel syndrome as affecting the knee would be deemed an error. This automated system also identifies invalid codes, that is, codes that do not exist in the classification structure.
Clearly, these edit checks cannot be sufficiently stringent to capture all suspect data. The data should be examined for overall reasonableness. For example, over the years of collecting similar data for the part of body, nearly 25% of the cases named the back as the affected area. This gave review staff a benchmark for validating data. A review of cross tabulations for overall sensibility also gives insight into how well the classification system was applied. Finally, special rare events, such as work-related tuberculosis, should be validated. One important element of a comprehensive validation system could involve recontacting the employer to insure the accuracy of the source document, although this requires additional resources.
Examples
Selected examples from each of the four illness and injury classification coding systems are shown in table 1 in order to illustrate the level of detail and the resulting richness of the final system. The power of the system as a whole is demonstrated in table 2, which shows a variety of characteristics that were tabulated for one set of related injury types—falls. In addition to total falls, the data are further subdivided into falls on the same level, falls to a lower level and jumping to a lower level. It can be seen, for instance, that falls were most likely to occur to workers age 25 to 34 years old, to operators, fabricators and labourers, to workers in the manufacturing industries and to workers with less than five years of service to their current employer (data not shown). The accident was most often associated with work on a floor or ground surface, and the subsequent injury was most likely to be a sprain or strain affecting the back, resulting in the worker spending more than one month away from work.
Table 1. Nature of injury or illness code—Examples
Nature of injury or illness code-Examples
0* Traumatic Injuries and Disorders
08* Multiple traumatic injuries and disorders
080 Multiple traumatic injuries and disorders, unspecified
081 Cuts, abrasions, bruises
082 Sprains and bruises
083 Fractures and burns
084 Fractures and other injuries
085 Burns and other injuries
086 Intracranial injuries and injuries to internal organs
089 Other combinations of traumatic injuries and disorders, n.e.c.
Event or exposure code-Examples
1* Falls
11* Fall to lower level
113 Fall from ladder
114 Fall from piled or stacked material
115* Fall from roof
1150 Fall from roof, unspecified
1151 Fall through existing roof opening
1152 Fall through roof surface
1153 Fall through skylight
1154 Fall from roof edge
1159 Fall from roof, n.e.c.
116 Fall from scaffold, staging
117 Fall from building girders or other structural steel
118 Fall from nonmoving vehicle
119 Fall to lower level, n.e.c.
Source of injury or illness code-Examples
7*Tools, instruments and equipment
72* Handtools-powered
722* Cutting handtools, powered
7220 Cutting handtools, powered, unspecified
7221 Chainsaws, powered
7222 Chisels, powered
7223 Knives, powered
7224 Saws, powered, except chainsaws
7229 Cutting handtools, powered, n.e.c.
723* Striking and nailing handtools, powered
7230 Striking handtools, powered, unspecified
7231 Hammers, powered
7232 Jackhammers, powered
7233 Punches, powered
Part of body affected code-Examples
2* Trunk
23* Back, including spine, spinal cord
230 Back, including spine, spinal cord, unspecified
231 Lumbar region
232 Thoracic region
233 Sacral region
234 Coccygeal region
238 Multiple back regions
239 Back, including spine, spinal cord, n.e.c.
* = division, major group, or group titles; n.e.c. = not elsewhere classified.
Table 2. Number and percentage of nonfatal occupational injuries and illnesses with days away from work involving falls, by selected worker and case characteristics, US 19931
|
Characteristic |
All events |
All falls |
Fall to lower level |
Jump to lower level |
Fall on same level |
|||||
|
Number |
% |
Number |
% |
Number |
% |
Number |
% |
Number |
% |
|
|
Total |
2,252,591 |
100.0 |
370,112 |
100.0 |
111,266 |
100.0 |
9,433 |
100.0 |
244,115 |
100.0 |
|
Sex: |
||||||||||
|
Men |
1,490,418 |
66.2 |
219,199 |
59.2 |
84,868 |
76.3 |
8,697 |
92.2 |
121,903 |
49.9 |
|
Women |
735,570 |
32.7 |
148,041 |
40.0 |
25,700 |
23.1 |
645 |
6.8 |
120,156 |
49.2 |
|
Age: |
||||||||||
|
14 to 15 years |
889 |
0.0 |
246 |
0.1 |
118 |
0.1 |
— |
— |
84 |
0.0 |
|
16 to 19 years |
95,791 |
4.3 |
15,908 |
4.3 |
3,170 |
2.8 |
260 |
2.8 |
12,253 |
5.0 |
|
20 to 24 years |
319,708 |
14.2 |
43,543 |
11.8 |
12,840 |
11.5 |
1,380 |
14.6 |
28,763 |
11.8 |
|
25 to 34 years |
724,355 |
32.2 |
104,244 |
28.2 |
34,191 |
30.7 |
3,641 |
38.6 |
64,374 |
26.4 |
|
35 to 44 years |
566,429 |
25.1 |
87,516 |
23.6 |
27,880 |
25.1 |
2,361 |
25.0 |
56,042 |
23.0 |
|
45 to 54 years |
323,503 |
14.4 |
64,214 |
17.3 |
18,665 |
16.8 |
1,191 |
12.6 |
43,729 |
17.9 |
|
55 to 64 years |
148,249 |
6.6 |
37,792 |
10.2 |
9,886 |
8.9 |
470 |
5.0 |
27,034 |
11.1 |
|
65 years and over |
21,604 |
1.0 |
8,062 |
2.2 |
1,511 |
1.4 |
24 |
0.3 |
6,457 |
2.6 |
|
Occupation: |
||||||||||
|
Managerial and professional |
123,596 |
5.5 |
26,391 |
7.1 |
6,364 |
5.7 |
269 |
2.9 |
19,338 |
7.9 |
|
Technical, sales and administrative support |
344,402 |
15.3 |
67,253 |
18.2 |
16,485 |
14.8 |
853 |
9.0 |
49,227 |
20.2 |
|
Service |
414,135 |
18.4 |
85,004 |
23.0 |
13,512 |
12.1 |
574 |
6.1 |
70,121 |
28.7 |
|
Farming, forestry and fishing |
59,050 |
2.6 |
9,979 |
2.7 |
4,197 |
3.8 |
356 |
3.8 |
5,245 |
2.1 |
|
Precision production, craft and repair |
366,112 |
16.3 |
57,254 |
15.5 |
27,805 |
25.0 |
1,887 |
20.0 |
26,577 |
10.9 |
|
Operators, fabricators and labourers |
925,515 |
41.1 |
122,005 |
33.0 |
42,074 |
37.8 |
5,431 |
57.6 |
72,286 |
29.6 |
|
Nature of injuries, illness: |
||||||||||
|
Sprains, strains |
959,163 |
42.6 |
133,538 |
36.1 |
38,636 |
34.7 |
5,558 |
58.9 |
87,152 |
35.7 |
|
Fractures |
136,478 |
6.1 |
55,335 |
15.0 |
21,052 |
18.9 |
1,247 |
13.2 |
32,425 |
13.3 |
|
Cuts, lacerations punctures |
202,464 |
9.0 |
10,431 |
2.8 |
2,350 |
2.1 |
111 |
1.2 |
7,774 |
3.2 |
|
Bruises, contusions |
211,179 |
9.4 |
66,627 |
18.0 |
17,173 |
15.4 |
705 |
7.5 |
48,062 |
19.7 |
|
Multiple injuries |
73,181 |
3.2 |
32,281 |
8.7 |
11,313 |
10.2 |
372 |
3.9 |
20,295 |
8.3 |
|
With fractures |
13,379 |
0.6 |
4,893 |
1.3 |
2,554 |
2.3 |
26 |
0.3 |
2,250 |
0.9 |
|
With sprains |
26,969 |
1.2 |
15,991 |
4.3 |
4,463 |
4.0 |
116 |
1.2 |
11,309 |
4.6 |
|
Soreness, Pain |
127,555 |
5.7 |
20,855 |
5.6 |
5,614 |
5.0 |
529 |
5.6 |
14,442 |
5.9 |
|
Back pain |
58,385 |
2.6 |
8,421 |
2.3 |
2,587 |
2.3 |
214 |
2.3 |
5,520 |
2.3 |
|
All other |
411,799 |
18.3 |
50,604 |
13.7 |
15,012 |
13.5 |
897 |
9.5 |
33,655 |
13.8 |
|
Part of body affected: |
||||||||||
|
Head |
155,504 |
6.9 |
13,880 |
3.8 |
2,994 |
2.7 |
61 |
0.6 |
10,705 |
4.4 |
|
Eye |
88,329 |
3.9 |
314 |
0.1 |
50 |
0.0 |
11 |
0.1 |
237 |
0.1 |
|
Neck |
40,704 |
1.8 |
3,205 |
0.9 |
1,097 |
1.0 |
81 |
0.9 |
1,996 |
0.8 |
|
Trunk |
869,447 |
38.6 |
118,369 |
32.0 |
33,984 |
30.5 |
1,921 |
20.4 |
80,796 |
33.1 |
|
Back |
615,010 |
27.3 |
72,290 |
19.5 |
20,325 |
18.3 |
1,523 |
16.1 |
49,461 |
20.3 |
|
Shoulder |
105,881 |
4.7 |
16,186 |
4.4 |
4,700 |
4.2 |
89 |
0.9 |
11,154 |
4.6 |
|
Source of injury illness: |
||||||||||
|
Chemicals, chemical products |
43,411 |
1.9 |
22 |
0.0 |
— |
— |
— |
— |
16 |
0.0 |
|
Containers |
330,285 |
14.7 |
7,133 |
1.9 |
994 |
0.9 |
224 |
2.4 |
5,763 |
2.4 |
|
Furniture, fixtures |
88,813 |
3.9 |
7,338 |
2.0 |
881 |
0.8 |
104 |
1.1 |
6,229 |
2.6 |
|
Machinery |
154,083 |
6.8 |
4,981 |
1.3 |
729 |
0.7 |
128 |
14 |
4,035 |
1.7 |
|
Parts and materials |
249,077 |
11.1 |
6,185 |
1.7 |
1,016 |
0.9 |
255 |
2.7 |
4,793 |
2.0 |
|
Worker motion or position |
331,994 |
14.7 |
— |
— |
— |
— |
— |
— |
— |
— |
|
Floor, ground surfaces |
340,159 |
15.1 |
318,176 |
86.0 |
98,207 |
88.3 |
7,705 |
81.7 |
208,765 |
85.5 |
|
Handtools |
105,478 |
4.7 |
727 |
0.2 |
77 |
0.1 |
41 |
0.4 |
600 |
0.2 |
|
Vehicles |
157,360 |
7.0 |
9,789 |
2.6 |
3,049 |
2.7 |
553 |
5.9 |
6,084 |
2.5 |
|
Health care patient |
99,390 |
4.4 |
177 |
0.0 |
43 |
0.0 |
8 |
0.1 |
90 |
0.0 |
|
All other |
83,813 |
3.7 |
15,584 |
4.2 |
6,263 |
5.6 |
414 |
4.4 |
7,741 |
3.2 |
|
Industry division: |
||||||||||
|
Agriculture, forestry and fishing2 |
44,826 |
2.0 |
8,096 |
2.2 |
3,636 |
3.3 |
301 |
3.2 |
3,985 |
1.6 |
|
Mining3 |
21,090 |
0.9 |
3,763 |
1.0 |
1,757 |
1.6 |
102 |
1.1 |
1,874 |
0.8 |
|
Construction |
204,769 |
9.1 |
41,787 |
11.3 |
23,748 |
21.3 |
1,821 |
19.3 |
15,464 |
6.3 |
|
Manufacturing |
583,841 |
25.9 |
63,566 |
17.2 |
17,693 |
15.9 |
2,161 |
22.9 |
42,790 |
17.5 |
|
Transportation and public utilities3 |
232,999 |
10.3 |
38,452 |
10.4 |
14,095 |
12.7 |
1,797 |
19.0 |
21,757 |
8.9 |
|
Wholesale trade |
160,934 |
7.1 |
22,677 |
6.1 |
8,119 |
7.3 |
1,180 |
12.5 |
12,859 |
5.3 |
|
Retail trade |
408,590 |
18.1 |
78,800 |
21.3 |
15,945 |
14.3 |
1,052 |
11.1 |
60,906 |
24.9 |
|
Finance, insurance and real estate |
60,159 |
2.7 |
14,769 |
4.0 |
5,353 |
4.8 |
112 |
1.2 |
9,167 |
3.8 |
|
Services |
535,386 |
23.8 |
98,201 |
26.5 |
20,920 |
18.8 |
907 |
9.6 |
75,313 |
30.9 |
|
Number of days away from work: |
||||||||||
|
Cases involving 1 day |
366,054 |
16.3 |
48,550 |
13.1 |
12,450 |
11.2 |
1,136 |
12.0 |
34,319 |
14.1 |
|
Cases involving 2 days |
291,760 |
13.0 |
42,912 |
11.6 |
11,934 |
10.7 |
1,153 |
12.2 |
29,197 |
12.0 |
|
Cases involving 3-5 days |
467,001 |
20.7 |
72,156 |
19.5 |
20,167 |
18.1 |
1,770 |
18.8 |
49,329 |
20.2 |
|
Cases involving 6-10 days |
301,941 |
13.4 |
45,375 |
12.3 |
13,240 |
11.9 |
1,267 |
13.4 |
30,171 |
12.4 |
|
Cases involving 11-20 days |
256,319 |
11.4 |
44,228 |
11.9 |
13,182 |
11.8 |
1,072 |
11.4 |
29,411 |
12.0 |
|
Cases involving 21-30 days |
142,301 |
6.3 |
25,884 |
7.0 |
8,557 |
7.7 |
654 |
6.9 |
16,359 |
6.7 |
|
Cases involving 31 or more days |
427,215 |
19.0 |
91,008 |
24.6 |
31,737 |
28.5 |
2,381 |
25.2 |
55,329 |
22.7 |
|
Median days away from work |
6 days |
7 days |
10 days |
8 days |
7 days |
|||||
1 Days away from work cases include those which result in days away from work with or without restricted work activity.
2 Excludes farms with fewer than 11 employees.
3 Data conforming to OSHA definitions for mining operators in coal, metal, and nonmetal mining and for employers in railroad transportation are provided to BLS by the Mine Safety and Health Administration, U.S. Department of Labor; the Federal Railroad Administration and U.S. Department of Transportation. Independent mining contractors are excluded from the coal, metal, and nonmetal mining industries.
NOTE: Because of rounding and data exclusion of nonclassifiable responses, data may not sum to the totals. Dashes indicate data that do not meet publication guidelines. The survey estimates of occupational injuries and illnesses are based on a scientifically selected sample of employers. The sample used was one of many possible samples, each of which could have produced different estimates. The relative standard error is a measure of the variation in the sample estimates across all possible samples that could have been selected. The percent relative standard errors for the estimates included here range from less than 1 per cent to 58 per cent.
Survey of Occupational Injuries and Illnesses, Bureau of Labor Statistics, US Department of Labor, April 1995.
It is clear that data such as these can have an important impact upon development of programmes for work-related accident and disease prevention. Even so, they do not indicate which occupations or industries are the most hazardous, since some very dangerous occupations may have small numbers of workers. Determination of levels of risk associated with particular occupations and industries is explained in the accompanying article “Risk analysis of nonfatal workplace injuries and illnesses”.
More...
Risk Analysis of Nonfatal Workplace Injuries and Illnesses
The United States Bureau of Labor Statistics routinely classifies nonfatal workplace injuries and illnesses by worker and case characteristics, using data from the US Survey of Occupational Injuries and Illnesses. While these counts identify groups of workers who experience large numbers of workplace injuries, they do not measure risk. Thus a particular group may sustain many workplace injuries simply because of the large number of workers in that group, and not because the jobs performed are especially hazardous.
In order to quantify actual risk, data on workplace injuries must be related to a measure of exposure to risk, such as number of hours worked, a labour supply measure which may be available from other surveys. The rate of nonfatal workplace injuries for a group of workers may be calculated by dividing the number of injuries recorded for that group by the number of hours worked during the same time period. The rate obtained this way represents the risk of injury per hour of work:
![]()
A convenient way of comparing the risk of injury among various groups of workers is to compute the relative risk:
![]()
The reference group may be a special group of workers, such as all managerial and professional specialty workers. Alternatively, it might consist of all workers. In any case, the relative risk (RR) corresponds to the rate ratio commonly used in epidemiological studies (Rothman 1986). It is algebraically equivalent to the percentage of all injuries which occur to the special group divided by the percentage of hours accounted for by the special group. When the RR is greater than 1.0, it indicates that members of the selected group are more likely to sustain injuries than members of the reference group; when the RR is less than 1.0, it indicates that, on the average, members of this group experience fewer injuries per hour.
The following tables show how indexes of relative risk for different groups of workers can identify those at greatest risk of workplace injury. The injury data are from the 1993 Survey of Occupational Injuries and Illnesses (BLS 1993b) and measure the number of injuries and illnesses with days away from work. The calculation relies upon estimates of annual hours worked taken from the microdata files of the US Bureau of the Census Current Population Surveys for 1993, which is obtained from household surveys (Bureau of the Census 1993).
Table 1 presents data by occupation on the share of workplace injuries, the share of hours worked and their ratio, which is the RR for injuries and illnesses with days away from work. The reference group is taken to be “All nonfarm private industry occupations” with workers of age 15 and older, which comprises 100%. As an example, the group “Operators, fabricators and labourers” experienced 41.64% of all injuries and illnesses, but contributed only 18.37% of the total hours worked by the reference population. Therefore, the RR for “Operators, fabricators and labourers” is 41.64/18.37 = 2.3. In other words, workers in this group of occupations have on average 2.3 times the injury/illness rate of all nonfarm private industry workers combined. Furthermore, they are about 11 times as likely to sustain a serious injury as employees in a managerial or professional specialty.
Table 1. Risk of occupational injuries and illnesses
|
Occupation |
Percentage1 |
Index |
|
|
Injury and illness cases |
Hours worked |
||
|
All nonfarm private industry occupations |
100.00 |
100.00 |
1.0 |
|
Managerial and professional specialty |
5.59 |
24.27 |
0.2 |
|
Executive, administrative and managerial |
2.48 |
13.64 |
0.2 |
|
Professional specialty |
3.12 |
10.62 |
0.3 |
|
Technical, sales and administrative support |
15.58 |
32.19 |
0.5 |
|
Technicians and related support |
2.72 |
3.84 |
0.7 |
|
Sales occupations |
5.98 |
13.10 |
0.5 |
|
Administrative support, including clerical |
6.87 |
15.24 |
0.5 |
|
Service occupations2 |
18.73 |
11.22 |
1.7 |
|
Protective service3 |
0.76 |
0.76 |
1.0 |
|
Service occupations, except protective service |
17.97 |
10.46 |
1.7 |
|
Farming, forestry and fishing occupations4 |
1.90 |
0.92 |
2.1 |
|
Precision production, craft and repair |
16.55 |
13.03 |
1.3 |
|
Mechanics and repairers |
6.30 |
4.54 |
1.4 |
|
Construction trades |
6.00 |
4.05 |
1.5 |
|
Extractive occupations |
0.32 |
0.20 |
1.6 |
|
Precision production occupations |
3.93 |
4.24 |
0.9 |
|
Operators, fabricators and labourers |
41.64 |
18.37 |
2.3 |
|
Machine operators, assemblers and inspectors |
15.32 |
8.62 |
1.8 |
|
Transportation and material moving occupations |
9.90 |
5.16 |
1.9 |
|
Handlers, equipment cleaners, helpers and laborers |
16.42 |
4.59 |
3.6 |
1 Percentage of injuries and illnesses, hours worked and index of relative risk for occupational injuries and illnesses with days away from work, by occupation, US nonfarm private industry employees 15 years and over, 1993.
2 Excludes private household workers and protective service workers in the public sector
3 Excludes protective service workers in the public sector
4 Excludes workers in agricultural production industries
Sources: BLS Survey of Occupational Injuries and Illnesses, 1993; Current Population Survey, 1993.
The various occupational groups may be ranked according to degree of risk simply by comparing their RR indices. The highest RR in the table (3.6) is associated with “handlers, equipment cleaners, helpers and labourers”, while the group at lowest risk is managerial and professional specialty workers (RR = 0.2). More refined interpretations may be made. While the table suggests that workers with lower levels of skills are in jobs with higher risks of injury and illness, even among blue-collar occupations the injury and illness rate is higher for less-skilled operators, fabricators and labourers compared to precision production, craft and repair workers.
In the above discussion, the RRs have been based upon all injuries and illnesses with days away from work, since these data have long been readily available and understood. Using the extensive and newly developed coding structure of the Survey of Occupational Injuries and Illnesses, researchers may now examine specific injuries and illnesses in detail.
As an example, table 2 shows the RR for the same set of occupation groupings, but restricted to the single outcome “Repetitive Motion Conditions” (event code 23) with days away from work, by occupation and gender. Repetitive motion conditions include carpal tunnel syndrome, tendonitis and certain strains and sprains. The group most severely affected by this type of injury is quite clearly female machine operators, assemblers and inspectors (RR = 7.3), followed by female handlers, equipment cleaners, helpers and labourers (RR = 7.1).
Table 2. Index of relative risk for repetitive motion conditions with days away from work, by occupation and gender, US nonfarm private industry employees 15 years and over, 1993
|
Occupation |
All |
Men |
Women |
|
All nonfarm private industry occupations |
1.0 |
0.6 |
1.5 |
|
Managerial and professional specialty |
0.2 |
0.1 |
0.3 |
|
Executive, administrative and managerial |
0.2 |
0.0 |
0.3 |
|
Professional specialty |
0.2 |
0.1 |
0.3 |
|
Technical, sales and administrative support |
0.8 |
0.3 |
1.1 |
|
Technicians and related support |
0.6 |
0.3 |
0.8 |
|
Sales occupations |
0.3 |
0.1 |
0.6 |
|
Administrative support, including clerical |
1.2 |
0.7 |
1.4 |
|
Service occupations1 |
0.7 |
0.3 |
0.9 |
|
Protective service2 |
0.1 |
0.1 |
0.4 |
|
Service occupations, except protective service |
0.7 |
0.4 |
0.9 |
|
Farming, forestry and fishing occupations3 |
0.8 |
0.6 |
1.8 |
|
Precision production, craft and repair |
1.0 |
0.7 |
4.2 |
|
Mechanics and repairers |
0.7 |
0.6 |
2.4 |
|
Construction trades |
0.6 |
0.6 |
— |
|
Extractive occupations |
0.1 |
0.1 |
— |
|
Precision production occupations |
1.8 |
1.0 |
4.6 |
|
Operators, fabricators and laborers |
2.7 |
1.4 |
6.9 |
|
Machine operators, assemblers and inspectors |
4.1 |
2.3 |
7.3 |
|
Transportation and material moving occupations |
0.5 |
0.5 |
1.6 |
|
Handlers, equipment cleaners, helpers and laborers |
2.4 |
1.4 |
7.1 |
1 Excludes private household workers and protective service workers in the public sector
2 Excludes protective service workers in the public sector
3 Excludes workers in agricultural production industries
Note: Long dashes — indicate that data do not meet publication guidelines.
Source: Calculated from the BLS Survey of Occupational Injuries and Illnesses, 1993, and Current Population Survey, 1993.
The table shows striking differences in the risk of repetitive motion conditions that depend on the gender of the worker. Overall, a woman is 2.5 times as likely as a man to lose work due to repetitive motion illness (2.5 = 1.5/0.6). However, this difference does not simply reflect a difference in the occupations of men and women. Women are at higher risk in all of the major occupational groups, as well as the less aggregated occupational groupings reported in the table. Their risk relative to men is especially high in sales and blue-collar occupations. Women are six times as likely as men to lose work time from repetitive motion injuries in sales and in precision production, craft and repair occupations.
Case Study: Worker Protection and Statistics on Accidents and Occupational Diseases - HVBG, Germany
The German Berufsgenossenschaften (BG)
Under the social insurance system in Germany, statutory accident insurance covers the results of accidents at work and accidents on the way to and from work, as well as occupational diseases. This statutory accident insurance is organized into three areas:
- industrial accident insurance (represented by the BGs)
- agricultural accident insurance
- public sector’s own accident insurance scheme.
The 35 Berufsgenossenschaften (BG) cover the various branches of the industrial economy in Germany. They are responsible for 39 million employees insured in 2.6 million enterprises. Every person in a work, service or training position is insured, regardless of age, sex or income level. Their umbrella organization is the Central Federation of the Berufsgenossenschaften (HVBG).
By law, the BG is responsible for using all appropriate means to prevent workplace accidents and occupational diseases, to provide effective first aid and optimal medical, occupational and social rehabilitation, and to pay benefits to the injured and sick, and to survivors. Thus prevention, rehabilitation and compensation are all under one roof.
The premiums to finance these benefits are paid exclusively by the employers. In 1993 all industrial employers paid on average DM 1.44 to the BG for every DM 100 wages, or 1.44%. In all, the premiums came to DM 16 billion (US billion used—one thousand million), of which about 80% was spent for rehabilitation and pensions. The remainder was used primarily for prevention programmes.
Occupational Safety and Health Protection
The employer is responsible for the health and safety of the employee at work. The legal scope of this responsibility is set by government in laws and ordinances, and in the protective labour regulations of the industrial BGs, which complete and concretize governmental protective labour law for each branch of industry. The system of prevention of the BGs is notable for its orientation to actual practice, its constant adaptation to the needs of the industry and to the state of technology, as well as for its effective support of the employer and the employee.
The BGs’ tasks of prevention, which are primarily carried out by the Technical Inspection Service (TAD) of the BG and the Occupational Medical Service (AMD), include:
- advising and motivating the employer
- supervising industrial occupational protective measures
- occupational medical care
- informing and training company staff
- safety checking on appliances and equipment
- initiating, carrying out and financing research.
Responsibility for implementing industrial occupational protection lies with the employer, who is legally obliged to hire appropriately qualified personnel to assist in occupational protection. These are specialists in work safety (safety officers, safety technicians and safety engineers) and company doctors. In companies with more than 20 employees, one or more safety representatives must be hired. The scope of the responsibility of the company for occupational safety specialists and company doctors is set by trade association regulations that are specific to the branch of industry and degree of hazard. In companies where an occupational safety specialist or a company doctor is employed, the employer must organize an occupational safety committee, made up of one company representative, two workers’ representatives, the company doctor, and occupational safety specialists and safety representatives. First-aid personnel, whose training is directed by the BG, also belong to the company occupational safety organization.
Occupational medical care has a special significance. Every employee who is at risk for a specific type of health threat at the workplace is examined in a uniform manner, and the results of the examination are assessed according to stated guidelines. In 1993 approximately four million occupational preventive medical examinations were carried out by specially authorized doctors. Lasting health concerns were ascertained in less than 1% of the examinations.
Employees who work with hazardous/carcinogenic materials also have a right to be medically examined even after the hazardous activity has been completed. The BGs have established services to be able to examine these employees. There are now three such services:
- Organizational Service for On-going Examinations (ODIN)
- Central Registration Service for Asbestos Dust-Endangered Employees (ZAs)
- Wismut Central Care Office (ZeBWis).
The three services cared for approximately 600,000 people in 1993. Collecting examination data assists in individual care and also helps improve scientific research for early detection of cancer cases.
Statistics on Workplace Accidents
Goal. The primary goal of collecting statistics on workplace accidents is to improve workplace safety by assessing and interpreting data on accident occurrences. These data are compiled from reports on workplace accidents; 5% to 10% of the accidents (approximately 100,000 accidents) are investigated each year by the Technical Inspection Services of the BGs.
Employers’ reporting responsibility. Every employer is obliged to report a workplace accident to his responsible BG within three days if the accident results in an incapacity to work for three calendar days or causes the death of the insured (“legally reportable workplace accident”). This includes accidents going to or from work. Accidents that cause only property damage or prevent the injured person from working for less than three days do not have to be reported. For reportable workplace accidents, a form “Accident Notification” (figure 1) is submitted by the employer. The time away from work is the significant factor for reporting purposes, regardless of the seriousness of the injury. Accidents that appear harmless must be reported if the injured person cannot work for longer than three days. This three-day requirement facilitates pursuing later claims. Failure to file an accident report, or filing one late, constitutes a violation of regulations that can be punished by the BG with a monetary fine of up to DM 5,000.
Figure 1. An example of an accident notification form
Notification by the attending physician. To optimize medical rehabilitation and to determine how long the employee is unable to work, the injured person receives treatment from a medical specialist selected for this work. The doctor is paid by the responsible industrial BG. Thus, the BG also receives notification of reportable workplace injuries from the doctor if the employer has failed to (promptly) file an accident report. The BG can then request the employer to file a workplace accident notification. This dual reporting system (employer and doctor) assures the BG of receiving knowledge of practically all reportable workplace accidents.
Using the information on the accident notification report and the medical report, the BG checks whether the accident is, in the legal sense, a workplace accident within its jurisdictional competence. On the basis of the medical diagnosis, the BG can, if needed, proceed immediately to ensuring optimal treatment.
A correct and complete description of the circumstances of the accident is especially important for prevention. This enables the BG’s Technical Inspection Service to draw conclusions about defective machinery and equipment that require immediate action to avoid further similar accidents. In the case of serious or fatal workplace accidents, regulations require the employer to immediately notify the BG. These occurrences are immediately investigated by the BG’s occupational safety experts.
In calculating a company’s premium, the BG takes into account the number and cost of workplace accidents that have taken place at this company. A bonus/malus procedure set by law is used in the calculation, and a portion of the company’s premium is determined by the company’s accident trend. This can lead to a higher or lower premium, thus creating financial incentives for employers to maintain safe workplaces.
Collaboration of the employees’ representatives and the safety representatives. Any accident report must also be signed by the workers’ council (Betriebsrat) and by the safety representatives (if these exist). The purpose of this rule is to inform the workers’ council and the safety representatives of the company’s overall accident situation, so that they can effectively exercise their collaborative rights in questions of workplace safety.
Compiling workplace accident statistics. On the basis of the information that the BG receives on a workplace accident from the accident report and the doctor’s report, the accounts are translated into statistical code numbers. The coding covers three areas, among others:
- description of the injured (age, sex, job)
- description of the injury (location of injury, type of injury)
- description of the accident (location, object causing the accident and circumstances of the accident).
Coding is performed by highly trained data specialists who are familiar with the organization of BG industries, utilizing a list of accident and injury codes which contains over 10,000 entries. In order to achieve the highest quality statistics, the classifications are regularly reworked, in order, for example, to adapt them to new technological developments. Furthermore, coding personnel are periodically retrained, and the data are subject to formal-logical and content-sensitive tests.
Uses of workplace accident statistics
An important task of these statistics is to describe the circumstances of the accident at the workplace. Table 1 portrays trends in reportable workplace accidents, new accident pension cases and fatal workplace accidents between 1981 and 1993. Column 3 (“New pension cases”) shows cases for which, because of the seriousness of the accident, a pension payment was first made by the industrial BGs in the given year.
Table 1. Occurrences of workplace accidents, Germany, 1981-93
|
Year |
Workplace accidents |
||
|
Reportable accidents |
New pension cases |
Deaths |
|
|
1981 |
1,397,976 |
40,056 |
1,689 |
|
1982 |
1,228,317 |
39,478 |
1,492 |
|
1983 |
1,144,814 |
35,119 |
1,406 |
|
1984 |
1,153,321 |
34,749 |
1,319 |
|
1985 |
1,166,468 |
34,431 |
1,204 |
|
1986 |
1,212,064 |
33,737 |
1,069 |
|
1987 |
1,211,517 |
32,537 |
1,057 |
|
1988 |
1,234,634 |
32,256 |
1,130 |
|
1989 |
1,262,374 |
30,840 |
1,098 |
|
1990 |
1,331,395 |
30,142 |
1,086 |
|
1991 |
1,587,177 |
30,612 |
1,062 |
|
1992 |
1,622,732 |
32,932 |
1,310 |
|
1993 |
1,510,745 |
35,553 |
1,414 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
To judge the average accident risk of an insured, the number of workplace accidents is divided by the actual time worked, to produce an accident rate. The rate per one million hours worked is used for comparison internationally and across years. Figure 2 shows how this rate varied between 1981 and 1993.
Figure 2. Frequency of workplace accidents
Industry-specific accident statistics. In addition to describing general trends, workplace statistics can be broken down by industry. For example, one might ask, “How many workplace accidents with portable grinders in the metalworking trade were there in the last few years; how and where did they take place; and what injuries resulted?” Such analyses may be useful to many people and institutions, such as government ministries, supervisory officials, research institutes, universities, businesses and workplace safety experts (table 2).
Table 2. Workplace accidents with portable grinders in metalworking, Germany, 1984-93
|
Year |
Reportable accidents |
New accident pensions |
|
1984 |
9,709 |
79 |
|
1985 |
10,560 |
62 |
|
1986 |
11,505 |
76 |
|
1987 |
11,852 |
75 |
|
1988 |
12,436 |
79 |
|
1989 |
12,895 |
76 |
|
1990 |
12,971 |
78 |
|
1991 |
19,511 |
70 |
|
1992 |
17,180 |
54 |
|
1993 |
17,890 |
70 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
For example, table 2 shows that reportable workplace accidents with portable grinders in metalworking rose continuously from the middle of the 1980s to 1990. From 1990 to 1991 a considerable increase in the accident figures is to be noted. This is an artefact resulting from the inclusion, beginning in 1991, of figures encompassing the new borders of reunited Germany. (The earlier figures cover only the Federal Republic of Germany.)
Other data compiled from accident reports reveal that not all accidents with metalworking portable grinders take place primarily in companies in the metalworking industry. Portable grinders, which of course are often used as angle grinders to cut pipes, iron bars and other objects, are frequently employed on construction sites. Accordingly, nearly one-third of the accidents are concentrated in companies in the construction industry. Working with portable grinders in metalworking results mainly in head and hand injuries. The most common head injuries affect the eyes and the area surrounding the eyes, which are injured by broken pieces, splinters and flying sparks. The tool has a fast-spinning grinding wheel, and hand injuries result when the person using the portable machine loses control of it. The high number of eye injuries proves that the importance and obligation of wearing safety glasses while grinding metal with this portable machine must be emphasized within companies.
Comparison of accident rates within and between industries. Although in 1993 there were nearly 18,000 workplace accidents with portable grinders in metalworking, compared to only 2,800 workplace accidents with hand-held power saws in woodworking, one cannot automatically conclude that this machinery poses a greater risk to metalworkers. To assess accident risk for specific industries, the number of accidents must first be related to a measure of exposure to danger, such as hours worked (see “Risk analysis of nonfatal workplace injuries and illnesses” [REC05AE]). However, this information is not always available. Therefore, a surrogate rate is derived as the proportion which serious accidents make of all reportable accidents. Comparing the serious-injury proportions for portable grinders in metalworking and portable circular saws in woodworking demonstrates that portable circular saws have an accident seriousness rate ten times higher than portable grinders. For prioritizing workplace safety measures, this is an important finding. This type of comparative risk analysis is an important component of an overall industrial accident prevention strategy.
Occupational Disease Statistics
Definition and reporting
In Germany an occupational disease is legally defined as a disease whose cause can be traced to the occupational activity of the affected person. An official list of occupational diseases exists. Therefore, assessing whether a sickness constitutes an occupational disease is both a medical and legal question and is referred by public law to the BG. If an occupational disease is suspected, it is not sufficient to prove that the employee suffers from, for example, an eczema. Additional knowledge is required about substances used at work and their potential for harming the skin.
Compiling occupational disease statistics. Because the BGs are responsible for compensating workers with occupational diseases as well as for providing rehabilitation and prevention, they have a considerable interest in application of statistics derived from occupational disease reports. These applications include targeting preventive measures on the basis of identified high-risk industries and occupations, and also providing their findings to the public, the scientific community and political authorities.
To support these activities, the BGs introduced in 1975 a set of occupational disease statistics, which contain data on every occupational disease report and its final determination—whether recognized or denied—including the reasons for the decision at the level of the individual case. This data base contains anonymous data on:
- the person, such as sex, year of birth, nationality
- diagnosis
- hazardous exposures
- the legal decision, including outcome of claim, determination of disability and any further actions taken by the BGs.
Results of the occupational disease statistics. An important function of the occupational disease statistics is to track the occurrence of occupational diseases over time. Table 3 charts the notifications of suspected occupational disease, the number of recognized occupational disease cases overall and the payment of pensions, as well as the number of fatal cases between 1980 and 1993. It should be cautioned that these data are not easy to interpret, since definitions and criteria differ widely. Furthermore, during this time period the number of officially designated occupational diseases rose from 55 to 64. Also, the figures from 1991 encompass the new borders of reunited Germany, whereas the earlier ones cover the Federal Republic of Germany alone.
Table 3. Occurrences of occupational disease, Germany, 1980-93
|
Year |
Notifications |
Recognized occupational disease cases |
Of those with |
Occupational disease fatalities |
|
1980 |
40,866 |
12,046 |
5,613 |
1,932 |
|
1981 |
38,303 |
12,187 |
5,460 |
1,788 |
|
1982 |
33,137 |
11,522 |
4,951 |
1,783 |
|
1983 |
30,716 |
9,934 |
4,229 |
1,557 |
|
1984 |
31,235 |
8,195 |
3,805 |
1,558 |
|
1985 |
32,844 |
6,869 |
3,439 |
1,299 |
|
1986 |
39,706 |
7,317 |
3,317 |
1,548 |
|
1987 |
42,625 |
7,275 |
3,321 |
1,455 |
|
1988 |
46,280 |
7,367 |
3,660 |
1,363 |
|
1989 |
48,975 |
9,051 |
3,941 |
1,281 |
|
1990 |
51,105 |
9,363 |
4,008 |
1,391 |
|
1991 |
61,156 |
10,479 |
4,570 |
1,317 |
|
1992 |
73,568 |
12,227 |
5,201 |
1,570 |
|
1993 |
92,058 |
17,833 |
5,668 |
2,040 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
Example: infectious diseases. Table 4 shows the decline in the number of recognized cases of infectious diseases during the period 1980 to 1993. It specifically singles out viral hepatitis, for which one can clearly see that a strongly declining trend developed from approximately the mid-1980s in Germany, when employees at risk in the health service were given preventive inoculations. Thus occupational disease statistics can serve not only to find high rates of illnesses, but can also document the successes of protective measures. Declines in disease rates may of course have other explanations. In Germany, for example, the reduction in the number of cases of silicosis during the past two decades is chiefly a result of the decline in the number of jobs in mining.
Table 4. Infectious diseases recognized as occupational diseases, Germany, 1980-93
|
Year |
Total recognized cases |
Of those: hepatitis viral |
|
1980 |
1173 |
857 |
|
1981 |
883 |
736 |
|
1982 |
786 |
663 |
|
1983 |
891 |
717 |
|
1984 |
678 |
519 |
|
1985 |
417 |
320 |
|
1986 |
376 |
281 |
|
1987 |
224 |
152 |
|
1988 |
319 |
173 |
|
1989 |
303 |
185 |
|
1990 |
269 |
126 |
|
1991 |
224 |
121 |
|
1992 |
282 |
128 |
|
1993 |
319 |
149 |
Source: Central Federation of Berufsgenossenschaften (HVBG), Germany.
Sources of Information
The HVBG, as umbrella organization for the BGs, centralizes the common statistics and produces analyses and brochures. Furthermore, the HVBG sees statistical information as an aspect of the overall information that must be available to carry out the broad range of mandated responsibilities of the accident insurance system. For this reason, the Central Information System of the BGs (ZIGUV) was formed in 1978. It prepares relevant literature and makes it available to the BGs.
Workplace safety as an interdisciplinary, comprehensive approach requires optimum access to information. The BGs in Germany have resolutely taken this path and thereby made a considerable contribution to the efficient workplace safety system in Germany.
Case study: Wismut - A Uranium Exposure Revisited
Historical Development
The Erz mountains have been mined since the twelfth century, and beginning in 1470 silver mining brought the area to prominence. Around the year 1500 the first reports of a specific disease among miners appeared in Agricola’s writings. In 1879 this disease was recognized by Haerting and Hesse as lung cancer, but at that time what caused it was not clear. In 1925 “Schneeberg lung cancer” was added to the list of occupational diseases.
The material from which Marie Curie isolated the elements radium and polonium came from the slag heap of the Joachimstal (Jachymov) in Bohemia. In 1936 Rajewsky’s radon measurements near Schneeberg confirmed the already assumed connection between radon in the mining shafts and lung cancer.
In 1945 the Soviet Union intensified its atomic weapons research programme. The search for uranium was extended to the Erz Mountains, as the conditions for mining were better there than in the Soviet deposits. After initial inquiries, the whole area was placed under Soviet military administration and declared a restricted zone.
From 1946 to 1990 the Soviet Wismut Company (SAG), later the Soviet-German Wismut Company (SDAG), carried out uranium mining in Thuringia and Saxony (figure 1). At the time the Soviet Union was under pressure to obtain sufficient quantities of uranium to construct the first Soviet atomic bomb. Appropriate equipment was not available, so achieving the necessary level of uranium production was possible only by disregarding safety measures. Working conditions were especially bad in the years 1946 to 1954. According to an SAG Wismut health report, 1,281 miners had fatal accidents and 20,000 suffered injuries or other detrimental effects to their health just in the second half of 1949.
Figure 1. Mining areas of SDAG Wismut in East Germany
In post-war Germany, the Soviet Union considered uranium mining a form of reparations. Prisoners, conscripts and “volunteers” were mobilized, but at first there were hardly any skilled personnel. In all, Wismut employed between 400,000 and 500,000 people (figure 2).
Figure 2. Wismut employees 1946-90
Bad working conditions, the lack of suitable technology and intense work pressure led to extremely high numbers of accidents and illnesses. The working conditions gradually improved beginning in 1953, when German participation in the Soviet company began.
Dry-drilling, which produced high levels of dust, was employed from 1946 to 1955. No artificial ventilation was available, resulting in high radon concentrations. In addition, the workers’ health was adversely affected by the extremely heavy labour due to the lack of equipment, the lack of safety gear and long work shifts (200 hours per month).
Figure 3. Exposure records of former SDAG Wismut
The exposure level varied over time and from shaft to shaft. The systematic measurement of the exposure also ensued in different phases, as is shown in figure 3. The exposures to ionizing radiation (shown in Working Level Months (WLM)) can be given only very roughly (table 1). Today, comparisons with radiation-exposure situations in other countries, measurements made under experimental conditions and assessments of written records permit a more precise statement of the exposure level.
Table 1. Estimates of radiation exposure (Working Level Months/Year) in the Wismut mines
|
Year |
WLM/Year |
|
1946–1955 |
30–300 |
|
1956–1960 |
10–100 |
|
1961–1965 |
5–50 |
|
1966–1970 |
3–25 |
|
1971–1975 |
2–10 |
|
1976–1989 |
1–4 |
In addition to intensive exposure to rock dust, other factors relevant to illnesses were present, such as uranium dust, arsenic, asbestos and emissions from explosives. There were physical effects from noise, hand-arm vibrations and whole-body vibrations. Under these conditions, silicoses and radiation-related bronchial carcinomas dominate the record of occupational diseases from 1952 to 1990 (table 2).
Table 2. Comprehensive overview of known occupational diseases in Wismut uranium mines 1952-90
|
List No. BKVO 1 |
Absolute number |
% |
|
|
Diseases due to quartz |
40 |
14,733 |
47.8 |
|
Malignant tumours or pretumours from ionizing radiation |
92 |
5,276 |
17.1 |
|
Diseases due to partial body vibration |
54 |
— |
— |
|
Diseases of tendons and extremity joints |
71–72 |
4,950 |
16.0 |
|
Impaired hearing due to noise |
50 |
4,664 |
15.1 |
|
Skin diseases |
80 |
601 |
1.9 |
|
Other |
— |
628 |
2.1 |
|
Total |
30,852 |
100 |
1 Occupational disease classification of the former GDR.
Source: Wismut Health System Annual Reports.
Although over time the health services of SAG/SDAG Wismut provided increasing levels of comprehensive care for the miners, including annual medical examinations, the effects on health of extracting the ore were not systematically analysed. Production and working conditions were kept strictly secret; the Wismut companies were autonomous and organizationally were a “state within a state”.
The full magnitude of the events became known only in 1989-90 with the end of the German Democratic Republic (GDR). In December 1990 uranium mining was discontinued in Germany. Since 1991 the Berufsgenossenschaften (preventing, recording and compensating industrial and trade associations), as the statutory accident insurance carrier have been responsible for recording and compensating all accidents and occupational diseases related to the former Wismut operation. This means that the associations are responsible for providing affected individuals with the best possible medical care and for collecting all relevant occupational health and safety information.
In 1990, approximately 600 claims for bronchial carcinoma were still pending with the Wismut social insurance system; some 1,700 cases of lung cancer had been turned down in earlier years. Since 1991 these claims have been pursued or reopened by the responsible Berufsgenossenschaften. On the basis of scientific projections (Jacobi, Henrichs and Barclay 1992; Wichmann, Brüske-Hohlfeld and Mohner 1995), it is estimated that in the next ten years between 200 and 300 cases of bronchial carcinomas per year will be recognized as resulting from working at Wismut.
The Present: After the Change
The production and working conditions at SDAG Wismut left their mark on both the employees and the environment in Thuringia and Saxony. In accordance with the law of the Federal Republic of Germany, the federal government took over responsibility for cleaning up the environment in the affected region. The costs of these activities for the period 1991-2005 have been estimated at DM 13 billion.
After the GDR joined the Federal Republic of Germany in 1990, the Berufsgenossenschaften, as statutory accident insurance carriers, became responsible for managing occupational diseases in the former GDR. In light of the particular conditions at Wismut, the Berufsgenossenschaften decided to form a special unit to handle occupational safety and health for the Wismut complex. To the extent possible, while respecting legal regulations protecting the privacy of personal data, the Berufsgenossenschaften secured records on former working conditions. Thus when the company was dissolved for economic reasons all evidence that could possibly serve to substantiate the claims of employees in case of illness would not be lost. The “Wismut Central Care Office” (ZeBWis) was established by the Federation on 1 January 1992 and bears responsibility for occupational medical treatment, early detection and rehabilitation.
From ZeBWis’s goal of providing appropriate occupational medical care to former uranium mining employees, four essential health surveillance tasks emerged:
- organizing mass screening examinations for early diagnosis and treatment of diseases
- documenting the screening findings and linking them with data from the occupational disease detection procedures
- scientifically analysing the data
- support of research on early detection and treatment of disease.
Screening is provided to the exposed workers in order to assure early diagnosis whenever possible. Ethical, scientific and economic aspects of such screening procedures require a thorough discussion which is beyond the scope of this article.
A programme of occupational medicine was developed, based on the well-founded trade association principles for special occupational medical examinations. Integrated into this were examination methods known from mining and radiation protection. The component parts of the programme follow from the main agents of exposure: dust, radiation and other hazardous materials.
The ongoing medical surveillance of former Wismut employees is aimed primarily at early detection and treatment of bronchial carcinomas resulting from exposure to radiation or other carcinogenic materials. Whereas the connections between ionizing radiation and lung cancers are proven with adequate certainty, the effects on health of long-term, low-dosage radiation exposure have been less researched. Current knowledge is based on extrapolations of data from survivors of the atomic bombings of Hiroshima and Nagasaki, as well as data obtained from other international studies of uranium miners.
The situation in Thuringia and Saxony is exceptional in that significantly more people underwent a much broader range of exposures. Therefore, a wealth of scientific knowledge can be gained from this experience. To what degree radiation works synergistically with exposure to carcinogens like arsenic, asbestos or diesel motor emissions in causing lung cancer should be scientifically examined using newly obtained data. The early detection of bronchial carcinomas through the introduction of state-of-the-art examination techniques should be an important part of the prospective scientific research.
Available Data from the Wismut Health System
In response to the extreme accident and health problems it faced, Wismut established its own health service, which provided, among other things, annual medical screening examinations, including chest x rays. In later years additional occupational disease examination units were set up. Since the Wismut health service took over not only occupational medicine, but also full medical care for employees and their dependents, by 1990 SDAG Wismut had collected comprehensive health information on many former and current Wismut employees. In addition to complete information on the occupational medical examinations, and a complete archive of occupational diseases, a comprehensive x-ray archive exists with over 792,000 x rays.
In Stollberg the Wismut health system had a central pathology department in which comprehensive histological and pathological material was collected from the miners, as well as from the inhabitants of the area. In 1994 this material was given to the German Cancer Research Center (DKFZ) in Heidelberg for safekeeping and research purposes. A portion of the records of the former health system was first taken over by the statutory accident insurance system. For this purpose, ZeBWis established a temporary archive at Shaft 371 in Hartenstein (Saxony).
These records are used for processing insurance claims, for preparing and administering occupational medical care and for scientific study. In addition to being used by the Berufsgenossenschaften, the records are available to experts and to authorized physicians in the context of their clinical work with and management of each former employee.
The core of these archives consists of the complete files of occupational diseases (45,000) which were taken over, together with the corresponding occupational disease tracing files (28,000), the tracing files for monitoring dust-endangered persons (200,000), as well as targeted documentary records with the results of the occupational medical fitness and monitoring examinations. In addition, the autopsy records of Stollberg Pathology are kept in this ZeBWis archive.
These last-mentioned records, as well as the occupational disease tracing files, have in the meantime been prepared for data processing. Both these forms of documentation will be used for extracting data for a 60,000-person comprehensive epidemiological study by the federal ministry for the environment.
In addition to the data on exposure to radon and radon by-products, the records on the exposure of former employees to other agents are of special interest to the Berufsgenossenschaften. Thus the present-day Wismut GmbH has measurement results available for viewing, in list form, from the early 1970s to the present for silicogenic dusts, asbestos dusts, heavy metal dusts, wood dusts, explosives dusts, toxic vapours, welding fumes, diesel motor emissions, noise, partial- and whole-body vibrations and heavy physical labour. For the years 1987 to 1990 the individual measurements are archived in electronic media.
This is important information for retrospective analysis of the exposures in Wismut’s uranium mining operations. It also constitutes the basis for constructing a job-exposure matrix which assigns exposures to tasks for research purposes.
To round out the picture, further records are stored in the department that safeguards health data at Wismut GmbH, including: patient files of former out-patients, accident reports by the former company and by occupational safety inspections, clinical occupational medical records, biological exposure tests, occupational medical rehabilitation and neoplastic disease reports.
However, not all Wismut archives—primarily paper files—were designed for centralized evaluation. Thus, with the dissolution of SDAG Wismut on 31 December 1990, and the dissolution of the Wismut company health system, the question was posed of what to do with these unique records.
Digression: Incorporating the Holdings
The first task for ZeBWis was to define the people who worked underground or in the preparation plants and to determine their current location. The holdings comprise some 300,000 people. Few of the company’s records were in a form that could be used in data processing. Thus it was necessary to tread the wearisome path of viewing one card at a time. The card files from nearly 20 locations had to be collected.
The next step was to collect the vital statistics and addresses of these people. Information from old personnel and wage records was not useful for this. Old addresses were often no longer valid, in part because a blanket renaming of streets, squares and roads took place after the unification treaty was signed. The Central Inhabitant Registry of the former GDR was also not useful, as by this time the information was no longer complete.
Finding these people was eventually made possible with the assistance of the Association of German Pension Insurance Carriers, through which addresses for nearly 150,000 people were collected to communicate the offer of free occupational medical care.
To give the examining doctor an impression of the hazards and exposure that the patient was subject to from the so-called occupational or work case history a job-exposure matrix was constructed.
Occupational Medical Care
Approximately 125 specially trained occupational physicians with experience in diagnosing dust- and radiation-caused diseases were recruited for the examinations. They work under the direction of ZeBWis and are spread throughout the Federal Republic to ensure that the affected individuals can obtain the indicated examination near their current place of residence. Due to intensive training of the participating physicians, standard high-quality examinations are performed at all examination locations. By distributing uniform documentation forms ahead of time, it is ensured that all relevant information is collected according to set standards and is entered into ZeBWis’s data centres. By optimizing the number of files, every examining doctor carries out an adequate number of exams every year and thereby remains practised and experienced in the examination programme. Through regular exchange of information and continuing education, the physicians always have access to current information. All examining physicians are experienced in assessing chest x rays in accordance with the 1980 ILO guidelines (International Labour Organization 1980).
The data pool, which is growing as a result of the ongoing examinations, is geared to acquaint physicians and risk assessment experts in the occupational disease detection programme with relevant preliminary findings. It furthermore provides a basis for addressing specific symptoms or diseases that appear under defined risk situations.
The Future
Comparing the number of people who worked for Wismut underground and/or in preparation plants with the number who were employed in uranium mining in the Western world, it is evident that, even with big gaps, the data on hand present an extraordinary basis for gaining new scientific understanding. Whereas the 1994 overview by Lubin et al. (1994) on the risk of lung cancer covered approximately 60,000 affected individuals and about 2,700 cases of lung cancer in 11 studies, the data from some 300,000 former Wismut employees are now available. At least 6,500 have died to date from radiation-caused lung cancer. Furthermore, Wismut never collected the exposure information on a great number of persons exposed either to ionizing radiation or other agents.
As precise information as possible on exposure is necessary for optimal occupational disease diagnosis as well as for scientific research. This is taken into account in two research projects that are being sponsored or carried out by the Berufsgenossenschaften. A job-exposure matrix was prepared by consolidating available site measurements, analysing geological data, using information on production figures and, in some cases, reconstructing working conditions in the early years of Wismut. Data of this type are a prerequisite for developing a better understanding, through cohort studies or case-control studies, of the nature and extent of illnesses that result from uranium mining. Understanding the effect of long-term, low-level radiation doses and the cumulative effects of radiation, dust and other carcinogenic materials might also be improved in this manner. Studies of this are now beginning or are being planned. With the help of biological specimens that were collected in Wismut’s former pathology laboratories, scientific knowledge can also be obtained about the type of lung cancer and also about the interactive effects between silicogenic dusts and radiation, as well as other carcinogenic hazardous materials that are inhaled or ingested. Such plans are being pursued at this time by the DKFZ. Collaboration on this issue is now underway between the German research facilities and other research groups such as the US NIOSH and the National Cancer Institute (NCI). Corresponding work groups in countries like the Czech Republic, France and Canada are also cooperating in studying the exposure data.
To what extent malignancies other than lung cancer may develop from radiation exposure during uranium ore mining is poorly understood. At the request of the trade associations, a model of this was developed (Jacobi and Roth 1995) to establish under what conditions cancers of the mouth and throat, liver, kidneys, skin or bones can be caused by working conditions such as those at Wismut.
Measurement Strategies and Techniques for Occupational Exposure Assessment in Epidemiology
Other articles in this chapter present general principles of medical surveillance of occupational illnesses and exposure surveillance. This article outlines some principles of epidemiological methods that may be used to fulfil surveillance needs. Application of these methods must take into account basic principles of physical measurement as well as standard epidemiological data-gathering practice.
Epidemiology can quantify the association between occupational and non-occupational exposure to chemico-physical stressors or behaviour and disease outcomes, and can thus provide information to develop interventions and prevention programmes (Coenen 1981; Coenen and Engels 1993). Availability of data and access to workplace and personnel records usually dictate the design of such studies. Under the most favourable circumstances, exposures can be determined through industrial hygiene measurements that are carried out in an operating shop or factory, and direct medical examinations of workers are used to ascertain possible health effects. Such evaluations can be done prospectively for a period of months or years to estimate risks of diseases such as cancer. However, it is more often the case that past exposures must be reconstructed historically, projecting backwards from current levels or using measurements recorded in the past, which may not completely meet informational needs. This article presents some guidelines and limitations for measurement strategies and documentation that affect epidemiological assessment of workplace health hazards.
Measurements
Measurements should be quantitative wherever possible, rather than qualitative, because quantitative data are subject to more powerful statistical techniques. Observable data are commonly classified as nominal, ordinal, interval and ratio. Nominal level data are qualitative descriptors which differentiate only types, such as different departments within a factory or different industries. Ordinal variables may be arranged from “low” to “high” without conveying further quantitative relationships. An example is “exposed” vs. “unexposed”, or classifying smoking history as non-smoker (= 0), light smoker (= 1), medium smoker (= 2) and heavy smoker (= 3). The higher the numerical value, the stronger the smoking intensity. Most measurement values are expressed as ratio or interval scales, in which a concentration of 30 mg/m3 is double the concentration of 15 mg/m3. Ratio variables possess an absolute zero (like age) while interval variables (like IQ) do not.
Measurement strategy
Measurement strategy takes into account information about the measurement site, the surrounding conditions (e.g., humidity, air pressure) during the measurement, the duration of the measurement and the measurement technique (Hansen and Whitehead 1988; Ott 1993).
Legal requirements often dictate measurement of eight-hour time-weighted averages (TWAs) of levels of hazardous substances. However, not all individuals work eight-hour shifts all the time, and levels of exposures may fluctuate during the shift. A value measured for one person’s job might be considered representative of an eight-hour shift value if the exposure duration is longer than six hours during the shift. As a practical criterion, a sampling duration of at least two hours should be sought. With time intervals that are too short, the sampling in one time period can show higher or lower concentrations, thereby over- or underestimating the concentration during the shift (Rappaport 1991). Therefore, it can be useful to combine several measurements or measurements over several shifts into a single time-weighted average, or to use repeated measurements with shorter sampling durations.
Measurement validity
Surveillance data must satisfy well-established criteria. The measurement technique should not influence the results during the measurement process (reactivity). Furthermore, the measurement should be objective, reliable and valid. The results should not be influenced either by the measurement technique used (execution objectivity) or by the reading or documentation by the measurement technician (assessment objectivity). The same measurement values should be obtained under the same conditions (reliability); the intended thing should be measured (validity) and interactions with other substances or exposures should not unduly influence the results.
Quality of Exposure Data
Data sources. A basic principle of epidemiology is that measurements made at the individual level are preferable to those made at the group level. Thus, the quality of epidemiolological surveillance data decreases in the following order:
- direct measurements taken of persons; information on exposure levels and time progression
- direct measurements taken of groups; information on current exposure levels for specific groups of workers (sometimes expressed as job-exposure matrices) and their variation over time
- measurements abstracted or reconstructed for individuals; estimation of exposure from company records, purchasing lists, descriptions of product lines, interviews with employees
- measurements abstracted or reconstructed for groups; historical estimation of group-based exposure indexes.
In principle, the most precise determination of the exposure, using documented measurement values over time, should always be sought. Unfortunately, indirectly measured or historically reconstructed exposures are often the only data available for estimating exposure-outcome relationships, even though considerable deviations exist between measured exposures and exposure values reconstructed from company records and interviews (Ahrens et al. 1994; Burdorf 1995). The quality of the data declines in the order exposure measurement, activity-related exposure index, company information, employee interviews.
Exposure scales. The need for quantitative monitoring data in surveillance and epidemiology goes considerably beyond the narrow legal requirements of threshold values. The goal of an epidemiological investigation is to ascertain dose-effect relation-ships, taking into account potentially confounding variables. The most precise information possible, which in general can be expressed only with a high scale level (e.g., ratio scale level), should be used. Separation into larger or smaller threshold values, or coding in fractions of threshold values (e.g., 1/10, 1/4, 1/2 threshold value) as is sometimes done, essentially relies on data measured on a statistically weaker ordinal scale.
Documentation requirements. In addition to information on the concentrations and the material and time of measurement, external measurement conditions should be documented. This should include a description of the equipment used, measurement technique, reason for the measurement and other relevant technical details. The purpose of such documentation is to ensure uniformity of measurements over time and from one study to another, and to permit comparisons between studies.
Exposure and health outcome data gathered for individuals are usually subject to privacy laws that vary from one country to another. Documentation of exposure and health conditions must adhere to such laws.
Epidemiological Requirements
Epidemiological studies strive to establish a causal link between exposure and disease. Some aspects of surveillance measurements that affect this epidemiological assessment of risk are considered in this section.
Type of disease. A common starting point for epidemiological studies is the clinical observation of a surge in a particular disease in a company or area of activity. Hypotheses on potential biological, chemical or physical causal factors ensue. Depending on the availability of data, these factors (exposures) are studied using a retrospective or prospective design. The time between the beginning of the exposure and the onset of the disease (latency) also affects study design. The range of latency can be considerable. Infections from certain enteroviruses have latency/incubation times of 2 to 3 hours, whereas for cancers latencies of 20 to 30 years are typical. Therefore, exposure data for a cancer study must cover a considerably longer period of time than for an infectious disease outbreak. Exposures which began in the distant past can continue up to the onset of disease. Other diseases associated with age, such as cardiovascular disease and stroke, can appear in the exposed group after the study begins and must be treated as competing causes. It is also possible that people classified as “not sick” are merely people who have not yet manifested clinical illness. Thus, continued medical surveillance of exposed populations must be maintained.
Statistical power. As previously stated, measurements should be expressed on as high a data level (ratio scale level) as possible in order to optimize the statistical power to produce statistically significant results. Power in turn is affected by the size of the total study population, the prevalence of exposure in that population, the background rate of illness and the magnitude of risk of the disease that is caused by the exposure under study.
Mandated disease classification. Several systems are available for codifying medical diagnoses. The most common are ICD-9 (International Classification of Diseases) and SNOMED (Systematic Nomenclature of Medicine). ICD-O (oncology) is a particularization of the ICD for codifying cancers. ICD coding documentation is legally mandated in many health systems throughout the world, especially in Western countries. However, SNOMED codification can also codify possible causal factors and external conditions. Many countries have developed specialized coding systems to classify injuries and illnesses that also include the circumstances of the accident or exposure. (See the articles “Case study: Worker protection and statistics on accidents and occupational diseases—HVBG, Germany” and “Development and application of an occupational injury and illness classification system”, elsewhere in this chapter.)
Measurements that are made for scientific purposes are not bound by the legal requirements that apply to mandated surveillance activities, such as determination of whether threshold limits have been exceeded in a given workplace. It is useful to examine exposure measurements and records in such a way as to check for possible excursions. (See, for example, the article “Occupational hazard surveillance” in this chapter.)
Treatment of mixed exposures. Diseases often have several causes. Therefore it is necessary to record as completely as possible the suspected causal factors (exposures/confounding factors) in order to be able to distinguish the effects of suspected hazardous agents from one another and from the effects of other contributory or confounding factors, such as cigarette smoking. Occupational exposures are often mixed (e.g., solvent mixtures; welding fumes such as nickel and cadmium; and in mining, fine dust, quartz and radon). Additional risk factors for cancers include smoking, excess alcohol consumption, poor nutrition and age. Besides chemical exposures, exposures to physical stressors (vibration, noise, electromagnetic fields) are possible triggers for diseases and must be considered as potential causal factors in epidemiological studies.
Exposures to multiple agents or stressors may produce interaction effects, in which the effect of one exposure is magnified or reduced by another that occurs contemporaneously. A typical example is the link between asbestos and lung cancer, which is many times more pronounced among smokers. An example of the mixture of chemical and physical exposures is progressive systemic scleroderma (PSS), which is probably caused by a combined exposure to vibration, solvent mixtures and quartz dust.
Consideration of bias. Bias is a systematic error in classifying persons in the “exposed/not exposed” or “diseased/not diseased” groups. Two types of bias should be distinguished: observation (information) bias and selection bias. With observation (information) bias, different criteria may be used to classify subjects into the diseased/not diseased groups. It is sometimes created when the target of a study includes persons employed in occupations known to be hazardous, and who may already be under increased medical surveillance relative to a comparison population.
In selection bias two possibilities should be distinguished. Case-control studies begin by separating persons with the disease of interest from those without that disease, then examine differences in exposure between these two groups; cohort studies determine disease rates in groups with different exposures. In either type of study, selection bias exists when information on the exposure affects classification of subjects as sick or not sick, or when information on disease status affects classification of subjects as exposed or not exposed. A common example of selection bias in cohort studies is the “healthy worker effect”, which is encountered when disease rates in exposed workers are compared with those in the general population. This can result in underestimation of disease risk because working populations are often selected from the general population on the basis of continued good health, frequently based upon medical examination, whereas the general population contains the ill and infirm.
Confounders. Confounding is the phenomenon whereby a third variable (the confounder) alters the estimate of an association between a presumed antecedent factor and a disease. It can occur when the selection of subjects (cases and controls in a case-control study or exposed and unexposed in a cohort study) depends in some way upon the third variable, possibly in a manner unknown to the investigator. Variables associated only with exposure or disease are not confounders. To be a confounder a variable must meet three conditions:
- It must be a risk factor for the disease.
- It must be associated with the exposure in the study population.
- It must not be in the causal pathway from exposure to disease.
Before any data are collected for a study it is sometimes impossible to predict whether or not a variable is a likely confounder. A variable which has been treated as a confounder in a previous study might not be associated with exposure in a new study within a different population, and would therefore not be a confounder in the new study. For instance, if all subjects are alike with respect to a variable (e.g., sex), then that variable cannot be a confounder in that particular study. Confounding by a particular variable can be accounted for (“controlled”) only if the variable is measured along with exposure and illness outcomes. Statistical control of confounding may be done crudely using stratification by the con-founding variable, or more precisely using regression or other multivariate techniques.
Summary
The requirements of measuring strategy, measuring technology and documentation for industrial workplaces are sometimes statutorily defined in terms of threshold limit value surveillance. Data protection regulations also apply to the protection of company secrets and person-related data. These requirements call for the comparable measuring results and measurement conditions and for an objective, valid and reliable measuring technology. Additional requirements put forward by epidemiology refer to the representativeness of measurements and to the possibility of establishing links between exposures for individuals and subsequent health outcomes. Measurements may be representative for certain tasks, i.e. they may reflect typical exposure during certain activities or in specific branches or typical exposure of defined groups of persons. It would be desirable to have measurement data directly attributed to the study subjects. This would make it necessary to include with measurement documentation information about persons working at the concerned workplace during the measurement or to set up a registry allowing such direct attribution. Epidemiological data collected at the individual level are usually preferable to those obtained at the group level.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."