Children categories

1. Blood (3)

1. Blood
Chapter Editor: Bernard D. Goldstein
Table of Contents
Tables
Haematopoietic and Lymphatic System
Bernard D. Goldstein
Leukaemia, Malignant Lymphomas and Multiple Myeloma
Timo Partanen, Paolo Boffetta, Elisabete Weiderpass
Agents or Work Conditions Affecting the Blood
Bernard D. Goldstein
Tables
Click a link below to view the table in the article context.

2. Cancer (4)

2. Cancer
Chapter Editor: Paolo Boffetta
Table of Contents
Tables
Introduction
Neil Pearce, Paolo Boffetta and Manolis Kogevinas
Occupational Carcinogens
Paolo Boffetta, Rodolfo Saracci, Manolis Kogevinas, Julian Wilbourn and Harri Vainio
Environmental Cancer
Bruce K. Armstrong and Paolo Boffetta
Prevention
Per Gustavsson
Tables
Click a link below to view table in article context.
- Occupational cancer: Key facts
- Estimated proportions of cancer (PAR) attributable to occupations
- Evaluation of evidence of carcinogenicity in the IARC Monographs
- IARC Monograph programme classification groups
- Group 1-Chemicals carcinogenic to humans
- Group 2A—Chemicals probably carcinogenic to humans
- Group 2B—Chemicals possibly carcinogenic to humans
- Pesticides evaluated in IARC Monographs, Volumes 1-63 (1972-1995)
- Drugs evaluated in IARC Monographs, Volumes 1-63 (1972-1995)
- Environmental agents/exposures known or suspected of human cancer
- Industries, occupations, exposures presenting a carcinogenic risk
- Industries, occs., exps. with cancer excess not definitive carcinogens
- Registered population variations of incidence of some common cancers

3. Cardiovascular System (7)

3. Cardiovascular System
Chapter Editors: Lothar Heinemann and Gerd Heuchert
Table of Contents
Tables and Figures
Introduction
Lothar Heinemann and Gerd Heuchert
Cardiovascular Morbidity and Mortality in the Workforce
Gottfried Enderlein and Lothar Heinemann
The Risk Factor Concept in Cardiovascular Disease
Lothar Heinemann, Gottfried Enderlein and Heide Stark
Rehabilitation and Prevention Programmes
Lothar Heinemann and Gottfried Enderlein
Physical, Chemical and Biological Hazards
Physical Factors
Heide Stark and Gerd Heuchert
Chemical Hazardous Materials
Ulrike Tittelbach and Wolfram Dietmar Schneider
Biological Hazards
Regina Jäckel, Ulrike Tittelbach and Wolfram Dietmar Schneider
Tables
Click a link below to view table in article context
- Mortality from cardiovascular diseases
- Mortality rates, special cardiovascular diagnosis groups
- Rate of disease and reduced work ability
- Work associated with cardiovascular hazards
- Occupation-related infection and disease
Figures
Point to a thumbnail to see figure caption, click to see the figure in the article context.

4. Digestive System (6)

4. Digestive System
Chapter Editor: Heikki Savolainen
Table of Contents
Figures
Digestive system
G. Frada
Mouth and teeth
F. Gobbato
Liver
George Kazantzis
Peptic ulcer
K. S. Cho
Liver cancer
Timo Partanen, Timo Kauppinen, Paolo Boffetta and Elisabete Weiderpass
Pancreatic cancer
Timo Partanen, Timo Kauppinen, Paolo Boffetta and Elisabete Weiderpass
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

5. Mental Health (8)

5. Mental Health
Chapter Editors: Joseph J. Hurrell, Lawrence R. Murphy, Steven L. Sauter and Lennart Levi
Table of Contents
Tables and Figures
Work and Mental Health
Irene L.D. Houtman and Michiel A.J. Kompier
Work-related Psychosis
Craig Stenberg, Judith Holder and Krishna Tallur
Mood and Affect
Depression
Jay Lasser and Jeffrey P. Kahn
Work-related Anxiety
Randal D. Beaton
Post-traumatic Stress Disorder and its Relationship to Occupational Health and Injury Prevention
Mark Braverman
Stress and Burnout and their Implication in the Work Environment
Herbert J. Freudenberger
Cognitive Disorders
Catherine A. Heaney
Karoshi: Death from Overwork
Takashi Haratani
Tables
Click a link below to view table in article context.
1. Schematic overview of management strategies & examples
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

6. Musculoskeletal System (14)

6. Musculoskeletal System
Chapter Editors: Hilkka Riihimäki and Eira Viikari-Juntura
Table of Contents
Tables and Figures
Overview
Hilkka Riihimäki
Muscles
Gisela Sjøgaard
Tendons
Thomas J. Armstrong
Bones and Joints
David Hamerman
Intervertebral Discs
Sally Roberts and Jill P.G. Urban
Low-back Region
Hilkka Riihimäki
Thoracic Spine Region
Jarl-Erik Michelsson
Neck
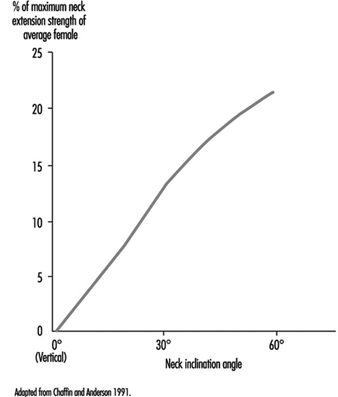
Åsa Kilbom
Shoulder
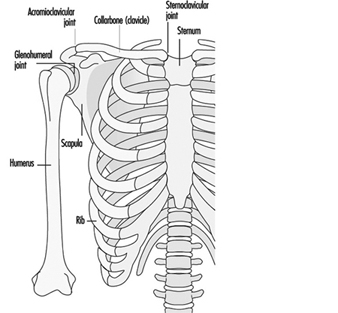
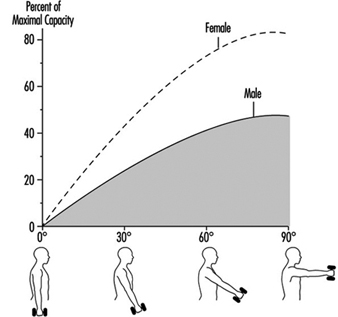
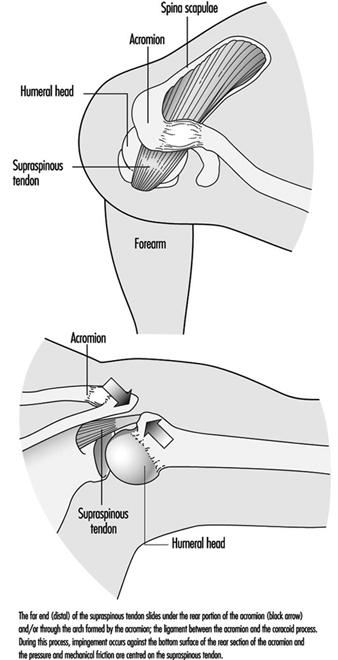
Mats Hagberg
Elbow
Eira Viikari-Juntura
Forearm, Wrist and Hand
Eira Viikari-Juntura
Hip and Knee
Eva Vingård
Leg, Ankle and Foot
Jarl-Erik Michelsson
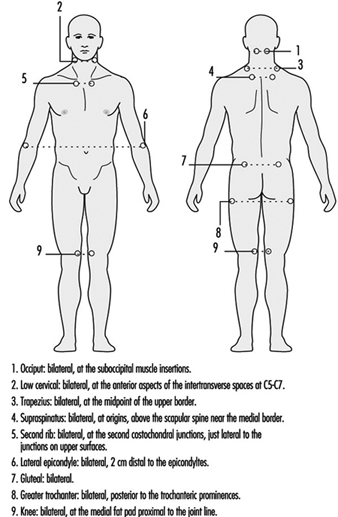
Other Diseases
Marjatta Leirisalo-Repo
Tables
Click a link below to view table in article context.
- Structure-function of joint components
- Prevalence of back disorders, in Finns over 30 years
- Reducing the risks for low-back pain at work
- Classification-low-back disorders (Quebec Task Force)
- Permissible motions for head in prolonged driving
- Incidence of epicondylitis in various populations
- Incidence of tenosynovitis/peritendinitis
- Primary osteoarthrosis of the hip in Malmö, Sweden
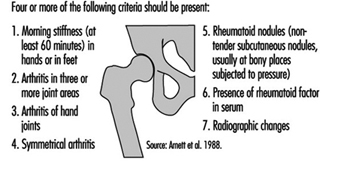
- Guidelines for the treatment of rheumatoid arthritis
- Infections known to trigger reactive arthritis
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

7. Nervous System (9)

7. Nervous System
Chapter Editor: Donna Mergler
Table of Contents
Tables and Figures
Nervous System: Overview
Donna Mergler and José A. Valciukas
Anatomy and Physiology
José A. Valciukas
Chemical Neurotoxic Agents
Peter Arlien-Søborg and Leif Simonsen
Manifestations of Acute and Early Chronic Poisoning
Donna Mergler
Preventing Neurotoxicity at Work
Barry Johnson
Clinical Syndromes Associated with Neurotoxicity
Robert G. Feldman
Measuring Neurotoxic Deficits
Donna Mergler
Diagnosis
Anna Maria Seppäläinen
Occupational Neuroepidemiology
Olav Axelson
Tables
Click a link below to view table in article context.
- Names & main functions of each pair of cranial nerves
- Grouping neurotoxic effects as to neurotoxicity
- Gases associated with neurotoxic effects
- Neurotoxic metals & their inorganic compounds
- Neurotoxic monomers
- Organic solvents associated with neurotoxicity
- Classes of common neurotoxic pesticides
- Other chemicals associated with neurotoxicity
- Chronic symptoms checklist
- Neuro-functional effects of exposures to some neurotoxins
- Chemical exposures & associated neurotoxic syndromes
- Some “core” batteries for assessing early neurotoxic effects
- Decision tree for neurotoxic disease
- Consistent neuro-functional effects of worksite exposures to some leading neurotoxic substances
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

8. Renal-Urinary System (2)

8. Renal-Urinary System
Chapter Editor: George P. Hemstreet
Table of Contents
Tables and Figures
Renal-Urinary Systems
George P. Hemstreet
Renal-Urinary Cancers
Timo Partanen, Harri Vainio, Paolo Boffetta and Elisabete Weiderpass
Tables
Click a link below to view table in article context.
- Drug-metabolism enzymes in kidney
- The most common causes of haematuria, by age & sex
- Criteria for biomarker selection
- Potential biomarkers linked to cell injury
- Acute renal insufficiency & occupation
- Segments of the nephron affected by selected toxicants
- Applications of urinary cytology
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

9. Reproductive System (9)

9. Reproductive System
Chapter Editor: Grace Kawas Lemasters
Table of Contents
Tables and Figures
Reproductive System: Introduction
Lowell E. Sever
Introduction to Male and Female Reproductive Function
Donald R. Mattison
Male Reproductive System and Toxicology
Steven Schrader and Grace Kawas Lemasters
Structure of the Female Reproductive System and Target Organ Vulnerability
Donald R. Mattison
Maternal Occupational Exposures and Adverse Pregnancy Outcomes
Grace Kawas Lemasters
Preterm Delivery and Work
Nicole Mamelle
Occupational and Environmental Exposures to the Newborn
Mary S. Wolff and Patrisha M. Woolard
Maternity Protection in Legislation
Marie-Claire Séguret
Pregnancy and US Work Recommendations
Leon J. Warshaw
Tables
Click a link below to view table in article context.
1. Exposures with multiple adverse endpoints
2. Epidemiological studies of paternal effects on pregnancy outcome
3. Potential female reproductive toxicants
4. Definition of foetal loss & infant death
5. Factors for small for gestational age and foetal loss
6. Identified sources of occupational fatigue
7. Relative risks & fatigue indices for preterm delivery
8. Prematurity risk by number of occupational fatigue indices
9. Relative risks and changes in working conditions
10. Newborn exposure sources and levels
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

10. Respiratory System (18)

10. Respiratory System
Chapters Editors: Alois David and Gregory R. Wagner
Table of Contents
Tables and Figures
Structure and Function
Morton Lippmann
Lung Function Examination
Ulf Ulfvarson and Monica Dahlqvist
Diseases Caused by Respiratory Irritants and Toxic Chemicals
David L.S. Ryon and William N. Rom
Occupational Asthma
George Friedman-Jimenez and Edward L. Petsonk
Diseases Caused by Organic Dusts
Ragnar Rylander and Richard S. F. Schilling
Beryllium Disease
Homayoun Kazemi
Pneumoconioses: Definition
Alois David
ILO International Classification of Radiographs of Pneumoconioses
Michel Lesage
Aetiopathogenesis of Pneumoconioses
Patrick Sébastien and Raymond Bégin
Silicosis
John E. Parker and Gregory R. Wagner
Coal Workers’ Lung Diseases
Michael D. Attfield, Edward L. Petsonk and Gregory R. Wagner
Asbestos-Related Diseases
Margaret R. Becklake
Hard Metal Disease
Gerolamo Chiappino
Respiratory System: The Variety of Pneumoconioses
Steven R. Short and Edward L. Petsonk
Chronic Obstructive Pulmonary Disease
Kazimierz Marek and Jan E. Zejda
Health Effects of Man-Made Fibres
James E. Lockey and Clara S. Ross
Respiratory Cancer
Paolo Boffetta and Elisabete Weiderpass
Occupationally Acquired Infections of the Lung
Anthony A. Marfin, Ann F. Hubbs, Karl J. Musgrave, and John E. Parker
Tables
Click a link below to view table in article context.
1. Respiratory tract regions & particle deposition models
2. Inhalable, thoracic & respirable dust criteria
3. Summary of respiratory irritants
4. Mechanisms of lung injury by inhaled substances
5. Compounds capable of lung toxicity
6. Medical case definition of occupational asthma
7. Steps in diagnostic evaluation of asthma in the workplace
8. Sensitizing agents that can cause occupational asthma
9. Examples of sources of hazards of exposure to organic dust
10. Agents in organic dusts with potential biological activity
11. Diseases induced by organic dusts & their ICD codes
12. Diagnostic criteria for byssinosis
13. Properties of beryllium & its compounds
14. Description of standard radiographs
15. ILO 1980 Classification: Radiographs of Pneumoconioses
16. Asbestos-related diseases & conditions
17. Main commercial sources, products & uses of asbestos
18. Prevalence of COPD
19. Risk factors implicated in COPD
20. Loss of ventilatory function
21. Diagnostic classification, chronic bronchitis & emphysema
22. Lung function testing in COPD
23. Synthetic fibres
24. Established human respiratory carcinogens (IARC)
25. Probable human respiratory carcinogens (IARC)
26. Occupationally acquired respiratory infectious diseases
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

11. Sensory Systems (8)

11. Sensory Systems
Chapter Editor: Heikki Savolainen
Table of Contents
Tables and Figures
The Ear
Marcel-André Boillat
Chemically-Induced Hearing Disorders
Peter Jacobsen
Physically-Induced Hearing Disorders
Peter L. Pelmear
Equilibrium
Lucy Yardley
Vision and Work
Paule Rey and Jean-Jacques Meyer
Taste
April E. Mott and Norman Mann
Smell
April E. Mott
Cutaneous Receptors
Robert Dykes and Daniel McBain
Tables
Click a link below to view table in article context.
1. Typical calculation of functional loss from an audiogram
2. Visual requirements for different activities
3. Recommended illuminance values for the lighting design
4. Visual requirements for a driving licence in France
5. Agents/processes reported to alter the taste system
6. Agents/processes associated with olfactory abnormalities
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

12. Skin Diseases (7)

12. Skin Diseases
Chapter Editor: Louis-Philippe Durocher
Table of Contents
Tables and Figures
Overview: Occupational Skin Diseases
Donald J. Birmingham
Non-Melanocytic Skin Cancer
Elisabete Weiderpass, Timo Partanen, Paolo Boffetta
Malignant Melanoma
Timo Partanen, Paolo Boffetta, Elisabete Weiderpass
Occupational Contact Dermatitis
Denis Sasseville
Prevention of Occupational Dermatoses
Louis-Phillipe Durocher
Occupational Nail Dystrophy
C.D. Calnan
Stigmata
H. Mierzecki
Tables
Click a link below to view table in article context.
1. Occupations at risk
2. Types of contact dermatitis
3. Common irritants
4. Common skin allergens
5. Predisposing factors for occupational dermatitis
6. Examples of skin irritants & sensitizers with occupations
7. Occupational dermatoses in Quebec in 1989
8. Risk factors & their effects on the skin
9. Collective measures (group approach) to prevention
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.

13. Systemic Conditions (3)

13. Systemic Conditions
Chapter Editor: Howard M. Kipen
Table of Contents
Figures
Systemic Conditions: An Introduction
Howard M. Kipen
Sick Building Syndrome
Michael J. Hodgson
Multiple Chemical Sensitivities
Mark R. Cullen
Figures
Point to a thumbnail to see figure caption, click to see figure in article context.
Overview
Musculoskeletal disorders are among the most important occupational health problems in both developed and developing countries. These disorders affect the quality of life of most people during their lifetime. The annual cost of musculoskeletal disorders is great. In the Nordic countries, for example, it is estimated to vary from 2.7 to 5.2 % of the gross national product (Hansen 1993; Hansen and Jensen 1993). The proportion of all musculo-skeletal diseases that are attributable to work is thought to be approximately 30%. Thus, much is to be gained by prevention of work-related musculoskeletal disorders. To accomplish this goal, a good understanding is needed of the healthy musculoskeletal system, musculoskeletal diseases and the risk factors for musculo-skeletal disorders.
Most musculoskeletal diseases cause local ache or pain and restriction of motion that may hinder normal performance at work or in other everyday tasks. Nearly all musculoskeletal diseases are work-related in the sense that physical activity can aggravate or provoke symptoms even if the diseases were not directly caused by work. In most cases, it is not possible to point to one causal factor for musculoskeletal diseases. Conditions caused solely by accidental injuries are an exception; in most cases several factors play a role. For many of the musculoskeletal diseases, mechanical load at work and leisure is an important causal factor. Sudden overload, or repetitive or sustained loading can injure various tissues of the musculoskeletal system. On the other hand, too low a level of activity can lead to deterioration of the condition of muscles, tendons, ligaments, cartilage and even bones. Keeping these tissues in good condition requires appropriate use of the musculoskeletal system.
The musculoskeletal system essentially consists of similar tissues in different parts of the body, which provide a panorama of diseases. The muscles are the most common site of pain. In the lower back the intervertebral discs are common problem tissues. In the neck and the upper limbs, tendon and nerve disorders are common, while in the lower limbs, osteoarthritis is the most important pathological condition.
In order to understand these bodily differences, it is necessary to comprehend basic anatomical and physiological features of the musculoskeletal system and to learn the molecular biology of various tissues, the source of nutrition and the factors affecting normal function. The biomechanical properties of various tissues are also fundamental. It is necessary to understand both the physiology of normal function of the tissues, and pathophysi- ology—that is, what goes wrong. These aspects are described in the first articles for intervertebral discs, bones and joints, tendons, muscles and nerves. In the articles which follow, musculoskeletal disorders are described for the different anatomical regions. Symptoms and signs of the most important diseases are outlined and the occurrence of the disorders in populations is described. Current understanding, based on epidemiological research, of both work-and person- related risk factors is presented. For many disorders there are quite convincing data on work-related risk factors, but, for the time being, only limited data are available on exposure effect relationships between the risk factors and the disorders. Such data are needed in order to set guidelines to design safer work.
Despite the lack of quantitative knowledge, directions for prevention can be proposed. The primary approach to prevention of work-related musculoskeletal disorders is redesign of work in order to optimize the workload and make it compatible with the physical and mental performance capacity of the workers. It is also important to encourage workers to keep fit through regular physical exercise.
Not all musculoskeletal diseases described in this chapter have a causal relationship to work. It is, however, important for occupational health and safety personnel to be aware of such diseases and consider workload also in relation to them. Fitting the work to the performance capacity of the worker will help him or her to work successfully and healthfully.
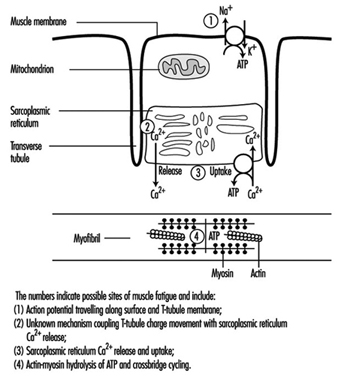
Muscles
Physical activity may increase muscle strength and working capa-city through changes such as growth in muscle volume and increased metabolic capacity. Different activity patterns cause a variety of biochemical and morphological adaptations in the muscles. In general, a tissue must be active to remain capable of living. Inactivity causes atrophy, especially in muscle tissue. Sports medicine and scientific investigations have shown that various training regimes can produce very specific muscular changes. Strength training, which places strong forces on the muscles, increases the number of contractile filaments (myofibrils) and the volume of the sarcoplasmic reticulum (see figure 1). High-intensity exercise increases muscular enzyme activity. The fractions of glycolytic and oxidative enzymes are closely related to the work intensity. In addition, prolonged intense exercise increases the capillary density.
Figure 1. A diagrammatic representation of the major components of a muscle cell involved in excitation-contraction coupling as well as the site for ATP production, the mitochondrion.
Sometimes, too much exercise can induce muscle soreness, a phenomenon well known to everyone who has demanded muscular performance beyond his or her capacity. When a muscle is overused, first deteriorating processes set in, which are followed by reparative processes. If sufficient time for repair is allowed, the muscle tissue may end up with increased capacities. Prolonged overuse with insufficient time for repair, on the other hand, causes fatigue and impairs muscle performance. Such prolonged overuse may induce chronic degenerative changes in the muscles.
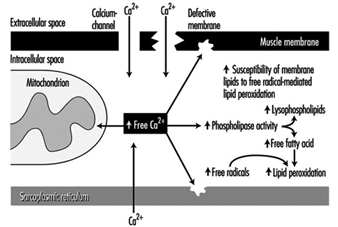
Other aspects of muscle use and misuse include the motor control patterns for various work tasks, which depend on force level, rate of force development, type of contraction, duration and the precision of the muscle task (Sjøgaard et al. 1995). Individual muscle fibres are “recruited” for these tasks, and some recruitment patterns may induce a high load on individual motor units even when the load on the muscle as a whole is small. Extensive recruitment of a particular motor unit will inevitably induce fatigue; and occupational muscle pain and injury may follow and could easily be related to the fatigue caused by insufficient muscle blood flow and intramuscular biochemical changes due to this high demand (Edwards 1988). High muscle tissue pressures may also impede muscle blood flow, which can reduce the ability of essential chemicals to reach the muscles, as well as the ability of the blood to remove waste products; this can cause energy crises in the muscles. Exercise can induce calcium to accumulate, and free radical formation may also promote degenerative processes such as the breakdown of muscle membrane and the impairment of normal metabolism (mitochondrial energy turnover) (figure 2). These processes may ultimately lead to degenerative changes in the muscle tissue itself. Fibres with marked degenerative characteristics have been found more frequently in muscle biopsies from patients with work-related chronic muscle pain (myalgia) than in normal subjects. Interestingly, the degenerated muscle fibres thus identified are “slow twitch fibres”, which connect with low-threshold motor nerves. These are the nerves normally recruited at low sustained forces, not high force related tasks. The perception of fatigue and pain may play an important role in preventing muscle injury. Protective mechanisms induce the muscles to relax and recover in order to regain strength (Sjøgaard 1990). If such biofeedback from the peripheral tissues is ignored, the fatigue and pain may eventually result in chronic pain.
Figure 2. A blow-up of the muscle membrane and structures inside the muscle in figure 2. The chain of events in the pathogenesis of calcium () induced damage in muscle cells is illustrated
Sometimes, after frequent overuse, various normal cellular chemical substances may not only cause pain themselves but may increase the response of muscular receptors to other stimuli, thereby lowering the threshold of activation (Mense 1993). The nerves which carry the signals from the muscles to the brain (sensory afferents) may thus be sensitized over time, which means that a given dose of substances which cause pain elicit a stronger excitation response. That is, the threshold of activation is reduced and smaller exposures may cause larger responses. Interestingly, the cells which normally serve as pain receptors (nociceptors) in uninjured tissue are silent, but these nerves may also develop ongoing pain activity which can persist even after the cause of the pain has terminated. This effect may explain chronic states of pain which are present after the initial injury has healed. When pain persists after healing, the original morphological changes in the soft tissues may be difficult to identify, even if the primary or initial cause of the pain is located in these peripheral tissues. Thus, the real “cause” of the pain may be impossible to trace.
Risk Factors and Preventive Strategies
Work-related risk factors of muscle disorders include repetition, force, static load, posture, precision, visual demand and vibration. Inappropriate work/rest cycles may be a potential risk factor for musculoskeletal disorders if sufficient recovery periods are not allowed before the next working period, thus never affording enough time for physiological rest. Environmental, sociocultural or personal factors may also play a role. Musculoskeletal disorders are multifactorial, and, in general, simple cause-effect relationships are difficult to detect. It is, however, important to document the extent to which occupational factors can be causally related to the disorders, since, only in the case of causality, the elimination or minimization of the exposure will help prevent the disorders. Of course, different preventive strategies must be implemented depending on the type of work task. In the case of high-intensity work the aim is to reduce force and work intensity, while for monotonous repetitive work it is more important to induce variation in the work. In short, the aim is optimization of the exposure.
Occupational Diseases
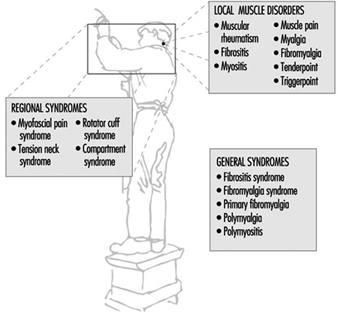
Work-related muscle pain is reported most frequently in the neck and shoulder area, the forearm and the low back. Although it is a major cause of sick-leave there is much confusion with regard to classifying the pain and specifying diagnostic criteria. Common terms which are used are given in three categories (see figure 3).
Figure 3. Classification of muscle diseases.
When muscular pain is assumed to be work-related, it can be classified into one of the following disorders:
- Occupational cervicobrachial disorders (OCD)
- Repetition strain injury (RSI)
- Cumulative trauma disorders (CTD)
- Overuse (injury) syndrome
- Work-related neck and upper-limb disorders.
The taxonomy of the work-related neck and upper-limb disorders clearly demonstrates that the aetiology includes external mechanical loads, which may well occur in the work place. Besides disorders in the muscle tissue itself, this category includes also disorders in other soft tissues of the musculoskeletal system. Of note is, that the diagnostic criteria may not allow to identify the location of the disorder specifically to one of these soft tissues. In fact it is likely that morphological changes at the musculo-tendinous junctions are related to the perception of muscle pain. This advocates the term fibromyalgia to be used among local muscle disorders. (See figure 3)
Unfortunately, different terms are used for essentially the same medical condition. In recent years, the international scientific community has focused increasingly on classification and diagnostic criteria for musculoskeletal disorders. A distinction is made between generalized and local or regional pain (Yunus 1993). Fibromyalgia syndrome is a generalized pain condition but is not considered to be work related. On the other hand, localized pain disorders are likely to be associated with specific work tasks. Myofascial pain syndrome, tension neck and rotator cuff syndrome are localized pain disorders that can be considered as work-related diseases.
Tendons
The deformation that occurs as force is applied and removed is called “elastic” deformation. The deformation that occurs after force application or removal is called “viscous” deformation. Because tissues of the body exhibit both elastic and viscous properties, they are called “viscoelastic”. If the recovery time between successive exertions is not long enough for a given force and duration, the recovery will not be complete and the tendon will be stretched further with each successive exertion. Goldstein et al. (1987) found that when finger flexor tendons were subjected to 8 seconds (s) physiological loads and 2 s rest, the accumulated viscous strain after 500 cycles was equal to the elastic strain. When the tendons were subjected to 2 s work and 8 s rest, the accumulated viscous strain after 500 cycles was negligible. Critical recovery times for given work-rest profiles have not yet been determined.
Tendons can be characterized as composite structures with parallel bundles of collagen fibres arranged in a gelatinous matrix of mucopolysaccharide. Tensile forces on the ends of the tendon cause unfolding of corrugations and straightening of the collagen strands. Additional loads cause stretching of the straightened strands. Consequently, the tendon gets stiffer as it gets longer. Compressive forces perpendicular to the long axis of the tendon cause the collagen strands to be forced closer together, and result in a flattening of the tendon. Shear forces on the side of the tendon cause displacement of the collagen strands closest to the surface with respect to those farthest away, and gives the side view of the tendon a skewed look.
Tendons as Structures
Forces are transmitted through tendons to maintain static and dynamic balance for specified work requirements. Contracting muscles tend to rotate the joints in one direction while the weight of the body and of work objects tends to rotate them in the other. Exact determination of these tendon forces is not possible because there are multiple muscles and tendons acting about each joint structure; however, it can be shown that the muscle forces acting on the tendons are much greater than the weight or reaction forces of work objects.
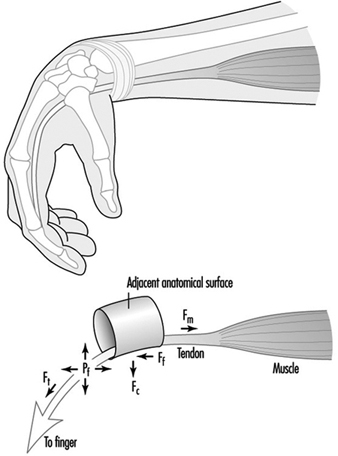
The forces exerted by contracting muscles are called tensile forces because they stretch the tendon. Tensile forces can be demonstrated by pulling on the ends of a rubber band. Tendons also are subjected to compressive and shear forces and to fluid pressures, which are illustrated in Figure 4 for the finger flexor tendons in the wrist.
Figure 1. Schematic diagram of tendon stretched around an anatomical surface or pulley and the corresponding tensile forces (Ft), compressive forces (Fc), friction forces (Ff) and hydrostatic or fluid pressure (Pf).
Exertion of the fingers to grasp or manipulate work objects requires the contraction of muscles in the forearm and hand. As the muscles contract, they pull on the ends of their respective tendons, which pass through the centre and circumference of the wrist. If the wrist is not held in a position so that the tendons are perfectly straight, they will press against adjacent structures. The finger flexor tendons press against the bones and ligaments inside the carpal tunnel. These tendons can be seen to protrude under the skin toward the palm during forceful pinching with a flexed wrist. Similarly, the extensor and abductor tendons can be seen to protrude on the back and side of the wrist when it is extended with outstretched fingers.
Friction or shear forces are caused by dynamic exertions in which the tendons rub against adjacent anatomical surfaces. These forces act on and parallel to the surface of the tendon. Friction forces can be felt by simultaneously pressing and sliding the hand against a flat surface. The sliding of tendons over an adjacent anatomical surface is analogous to a belt sliding around a pulley.
Fluid pressure is caused by exertions or postures that displace fluid out of the spaces around the tendons. Studies of carpal canal pressure show that wrist contact with external surfaces and certain postures produce pressures high enough to impair circulation and threaten tissue viability (Lundborg 1988).
Contraction of a muscle produces an immediate stretching of its tendon. Tendons join muscles together. If the exertion is sustained, the tendon will continue to stretch. Relaxation of the muscle will result in a rapid recovery of the tendon followed by a slowed recovery. If the initial stretching was within certain limits, the tendon will recover to its initial unloaded length (Fung 1972).
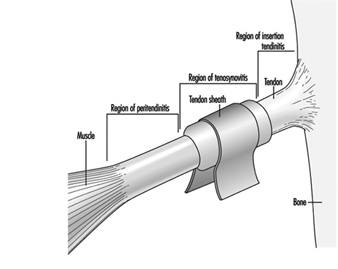
Tendons as Living Tissues
The strength of tendons belies the delicacy of the underlying physiological mechanisms by which they are nourished and heal. Interspersed within the tendon matrix are living cells, nerve endings and blood vessels. Nerve endings provide information to the central nervous system for motor control and warning of acute overload. Blood vessels play an important role in the nourishment of some areas of the tendon. Some areas of tendons are avascular and rely on diffusion from fluid secreted by synovial linings of outer tendon sheaths (Gelberman et al. 1987). Synovial fluid also lubricates movements of the tendons. Synovial sheaths are found at locations where tendons come into contact with adjacent anatomical surfaces.
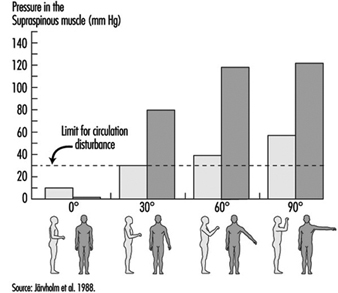
Excessive elastic or viscous deformation of the tendon can damage these tissues and impair their ability to heal. It is hypothesized that deformation may impede or arrest circulation and nourishment of tendons (Hagberg 1982; Viikari-Juntura 1984; Armstrong et al. 1993). Without adequate circulation, cell viability will be impaired and the tendon’s capacity to heal will be reduced. Tendon deformation can lead to small tears that further contribute to cell damage and inflammation. If circulation is restored and the tendon is given adequate recovery time, the damaged tissues will heal (Gelberman et al. 1987; Daniel and Breidenbach 1982; Leadbetter 1989).
Tendon Disorders
It has been shown that tendon disorders occur in predictable patterns (Armstrong et al. 1993). Their locations occur in those parts of the body associated with high stress concentrations (e.g., in the tendons of the supraspinatus, the biceps, the extrinsic finger flexor and extensor muscles). Also, there is an association between the intensity of work and the prevalence of tendon disorders. This pattern also has been shown for amateur and professional athletes (Leadbetter 1989). The common factors in both workers and athletes are repetitive exertions and overloading of the muscle-tendon units.
Within certain limits, the injuries produced by mechanical loading will heal. The healing process is divided into three stages: inflammatory, proliferatory and remodelling (Gelberman et al. 1987; Daniel and Breidenbach 1982). The inflammatory stage is characterized by the presence of polymorphonuclear cell infilt- ration, capillary budding and exudation, and lasts for several days. The proliferatory stage is characterized by the proliferation of fibroblasts and randomly oriented collagen fibres between areas of the wound and adjacent tissues, and lasts for several weeks. The remodelling phase is characterized by the alignment of the collagen fibres along the direction of loading, and lasts for several months. If the tissues are re-injured before healing is complete, recovery may be delayed and the condition may worsen (Leadbetter 1989). Normally healing leads to a strengthening or adaptation of the tissue to mechanical stress.
The effects of repetitive loading are apparent in the forearm finger flexor tendons where they contact the inside walls of the carpal tunnel (Louis 1992; Armstrong et al. 1984). It has been shown that there is progressive thickening of the synovial tissue between the edges of the carpal tunnel and the centre where the contact stresses on the tendons are the greatest. Thickening of the tendons is accompanied by synovial hyperplasia and proliferation of connective tissue. Thickening of the tendon sheaths is a widely cited factor in compression of the median nerve inside the carpal tunnel. It can be argued that thickening of the synovial tissues is an adaptation of the tendons to mechanical trauma. Were it not for the secondary effect on the median nerve compression resulting in carpal tunnel syndrome, it might be considered a desirable outcome.
Until optimal tendon loading regimes are determined, employers should monitor workers for signs or symptoms of tendon disorders so that they can intervene with work modifications to prevent further injuries. Jobs should be inspected for conspicuous risk factors any time an upper limb problem is identified or suspected. Jobs also should be inspected any time there is a change in the work standard, procedure or tooling, to insure that risk factors are minimized.
Bones and Joints
Bone and cartilage are part of the specialized connective tissues that make up the skeletal system. Bone is a living tissue that replaces itself continuously. The hardness of bone is well suited to the task of providing mechanical support function, and the elasticity of cartilage, to the ability of joints to move. Both cartilage and bone consist of specialized cells that produce and regulate a matrix of material outside the cells. The matrix is abundant in collagens, proteoglycans and non-collagenous proteins. Minerals are present in bone matrix as well.
The external part of bone is called the cortex and is compact bone. The more spongy inner part (trabecular bone) is filled with blood-forming (haematopoietic) bone marrow. The inner and outer parts of the bone have different metabolic turnover rates, with important consequences for late life osteoporosis. Trabecular bone regenerates itself at a greater rate than compact bone, which is why osteoporosis is first seen in the vertebral bodies of the spine, which have large trabecular parts.
Bone in the skull and other selected sites forms directly by bone formation (intramembranous ossification) without passing through a cartilage intermediate phase. The long bones of the limbs develop from cartilage through a process known as endochondral ossification. This process is what leads to the normal growth of long bones, to the repair of fractures and, in late adult life, to the unique formation of new bone in a joint which has become osteoarthritic.
The osteoblast is a type of bone cell that is responsible for synthesis of the matrix components in bone: the distinct collagen (type I) and proteoglycans. Osteoblasts also synthesize other non-collagenous proteins of bone. Some of these proteins can be measured in serum to determine the rate of bone turnover.
The other distinct bone cell is called the osteoclast. The osteoclast is responsible for resorption of bone. Under normal circumstances, old bone tissue is resorbed while new bone tissue is generated. Bone is resorbed by production of enzymes that dissolve proteins. Bone turnover is called remodelling and is normally a balanced and coordinated process of resorption and formation. Remodelling is influenced by body hormones and by local growth factors.
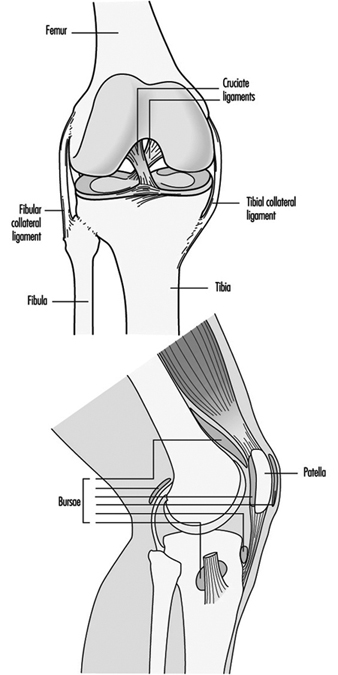
Movable (diarthrodial) joints are formed where two bones fit together. Joint surfaces are designed for weight bearing, and to accommodate a range of motion. The joint is enclosed by a fibrous capsule, whose inner surface is a synovial membrane, which secretes synovial fluid. The joint surface is made of hyaline cartilage, beneath which is a backing of hard (subchondral) bone. Within the joint, ligaments, tendons and fibrocartilaginous structures (menisci in certain joints, such as the knee), provide stability and a close fit between joint surfaces. The specialized cells of these joint components synthesize and maintain the matrix macromolecules whose interactions are responsible for maintaining the tensile strength of ligaments and tendons, the loose connective tissue that supports the blood vessels and cellular elements of the synovial membrane, the viscous synovial fluid, the elasticity of hyaline cartilage, and the rigid strength of subchondral bone. These joint components are interdependent, and their relationships are shown in table 1.
Table 1. Structure-function relationships and inter-dependence of joint components.
|
Components |
Structure |
Functions |
|
Ligaments and tendons |
Dense, fibrous, connective tissue |
Prevents over-extension of joints, provides stability and strength |
|
Synovial membrane |
Areolar, vascular and cellular |
Secretes synovial fluid, dissolves (phagocytoses) particulate material in synovial fluid |
|
Synovial fluid |
Viscous fluid |
Provides nutrients for cartilage injoints, lubricates cartilage during joint motion |
|
Cartilage |
Firm hyaline cartilage |
Constitutes the joint surface, bears weight, responds elastically to compression |
|
Tidemark |
Calcified cartilage |
Separates joint cartilage from underlying bone |
|
Subchondral bone |
Hard bone with marrow spaces |
Provides backing for joint surface; marrow cavity provides nutrients to base of cartilage and is thesource of cells with potential fornew bone formation |
Source: Hamerman and Taylor 1993.
Selected Diseases of Bones and Joints
Osteopenia is the general term used to describe reduced bone substance detected on x rays. Often asymptomatic in early stages, it may eventually manifest itself as weakening of bones. Most of the conditions listed below induce osteopenia, although the mechanisms by which this occurs differ. For example, excessive parathyroid hormone enhances bone resorption, while calcium and phosphate deficiency, which can arise from multiple causes and is often due to inadequate vitamin D, results in deficient mineralization. As people age, there is an imbalance between formation and resorption of bone. In women around the age of menopause, resorption often predominates, a condition called type I osteoporosis. In advanced age, resorption can again dominate and lead to type II osteoporosis. Type I osteoporosis usually affects vertebral bone loss and collapse, while hip fracture predominates in type II.
Osteoarthritis (OA) is the principal chronic disorder of certain movable joints, and its incidence increases with age. By age 80, almost all people have enlarged joints on the fingers (Heberden’s nodes). This is usually of very limited clinical significance. The principal weight-bearing joints which are subject to osteoarthritis are the hip, knee, feet and facets of the spine. The shoulder, while it is not weight bearing, may also suffer from a variety of arthritic changes, including rotator cuff tear, subluxation of the humeral head and an effusion high in proteolytic enzymes—a clinical picture often called “Milwaukee Shoulder” and associated with substantial pain and limitation of motion. The main change in OA is primarily one of degradation of cartilage, but new bone formation called osteophytes is usually seen on x rays.
Intervertebral Discs
The intervertebral discs occupy about one-third of the spine. Since they not only provide the spinal column with flexibility but also transmit load, their mechanical behaviour has a great influence on the mechanics of the whole spine. A high proportion of cases of low-back pain are associated with the disc, either directly through disc herniation, or indirectly, because degenerated discs place other spinal structures under abnormal stress. In this article, we review the structure and composition of the disc in relation to its mechanical function and discuss changes to the disc in disease.
Anatomy
There are 24 intervertebral discs in the human spine, interspersed between the vertebral bodies. Together these make up the anterior (front) component of the spinal column, with the articulating facet joints and the transverse and spinous processes making up the posterior (rear) elements. The discs increase in size down the spine, to approximately 45 mm antero-posteriorly, 64 mm laterally and 11 mm height in the lower back region.
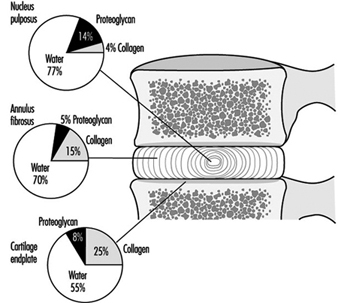
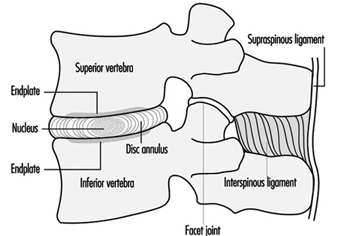
The disc is made of cartilage-like tissue and consists of three distinct regions, (see figure 1). The inner region (nucleus pulposus) is a gelatinous mass, particularly in the young person. The outer region of the disc (annulus fibrosus) is firm and banded. The fibres of the annulus are criss-crossed in an arrangement which allows it to withstand high bending and twisting loads. With increasing age the nucleus loses water, becomes firmer and the distinction between the two regions is less clear than early in life. The disc is separated from the bone by a thin layer of hyaline cartilage, the third region. In adulthood the cartilage endplate and the disc itself normally have no blood vessels of their own but rely on the blood supply of adjacent tissues, such as ligaments and vertebral body, to transport nutrients and remove waste products. Only the outer portion of the disc is innervated.
Figure 1. The relative proportions of the three main components of the normal adult human intervertebral disc and cartilage endplate.
Composition
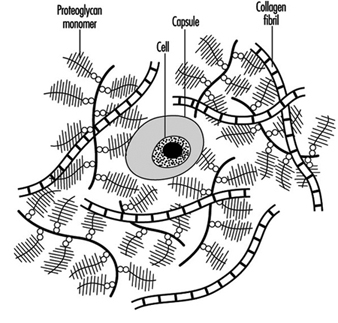
The disc, like other cartilage, consists mainly of a matrix of collagen fibres (which are embedded in a gel of proteoglycan) and of water. These together make up 90 to 95% of the total tissue mass, although the proportions vary with location within the disc and with age and degeneration. There are cells interspersed throughout the matrix that are responsible for synthesizing and maintaining the different components within it (figure 2). A review of the biochemistry of the disc can be found in Urban and Roberts 1994.
Figure 2. Schematic representation of disc structure, showing banded collagen fibres interspersed with numerous bottle-brush-like proteoglycan molecules and few cells.
Proteoglycans: The major proteoglycan of the disc, aggrecan, is a large molecule consisting of a central protein core to which many glycosaminoglycans (repeating chains of disaccharides) are attached (see figure 3). These side chains have a high density of negative charges associated with them, thus making them attractive to water molecules (hydrophilic), a property described as swelling pressure. It is very important to the functioning of the disc.
Figure 3. Diagram of part of a disc proteoglycan aggregate. G1, G2 and G3 are globular, folded regions of the central core protein.
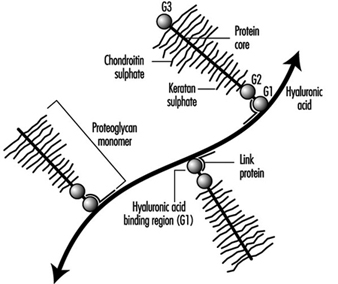 Huge aggregates of proteoglycans can form when individual molecules link onto a chain of another chemical, hyaluronic acid. The size of aggrecans varies (ranging in molecular weight from 300,000 to 7 million dalton) depending on how many molecules make up the aggregate. Other smaller types of proteoglycans have recently also been found in the disc and cartilage endplate—for example, decorin, biglycan, fibromodulin and lumican. Their function is generally unknown but fibromodulin and decorin may be involved in regulating collagen network formation.
Huge aggregates of proteoglycans can form when individual molecules link onto a chain of another chemical, hyaluronic acid. The size of aggrecans varies (ranging in molecular weight from 300,000 to 7 million dalton) depending on how many molecules make up the aggregate. Other smaller types of proteoglycans have recently also been found in the disc and cartilage endplate—for example, decorin, biglycan, fibromodulin and lumican. Their function is generally unknown but fibromodulin and decorin may be involved in regulating collagen network formation.
Water: Water is the main constituent in the disc, making up 65 to 90% of the tissue volume, depending on age and region of the disc. There is a correlation between the quantity of proteoglycan and the water content of the matrix. The amount of water also varies depending on the load applied to the disc, hence water content differs night and day since load will be very different when sleeping. Water is important both to the mechanical functioning of the disc and for providing the medium for transport of dissolved substances within the matrix.
Collagen: Collagen is the main structural protein in the body, and consists of a family of at least 17 distinct proteins. All collagens have helical regions and are stabilized by a series of intra- and inter- molecular crosslinks, which make the molecules very strong in resisting mechanical stresses and enzymatic degradation. The length and shape of different types of collagen molecules and the proportion which is helical, vary. The disc is composed of several types of collagens, with the outer annulus being predominantly type I collagen, and the nucleus and cartilage endplate predominantly type II. Both types form fibrils which provide the structural framework of the disc. The fibrils of the nucleus are much finer (>> mm in diameter) than those of the annulus (0.1 to 0.2 mm in diameter). The disc cells are often surrounded by a capsule of some of the other types of collagen, such as type VI.
Cells: The intervertebral disc has a very low density of cells in comparison to other tissues. Although the density of cells is low, their continuing activity is vital for the health of the disc, as the cells produce macromolecules throughout life, to replace those which break down and are lost with the passage of time.
Function
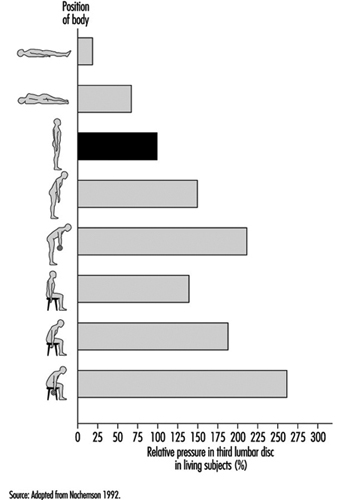
The main function of the disc is mechanical. The disc transmits load along the spinal column and also allows the spine to bend and twist. The loads on the disc arise from body weight and muscular activity, and change with posture (see figure 4). During daily activities the disc is subject to complex loads. Extending or flexing the spine produces mainly tensile and compressive stresses on the disc, which increase in magnitude going down the spine, due to differences in body weight and geometry. Rotating the spine produces crosswise (shear) stresses.
Figure 4. Relative intradiscal pressures in different postures compared to the pressure in upright standing (100%).
Discs are under pressure, which varies with posture from around 0.1 to 0.2 MPa at rest, to around 1.5 to 2.5 MPa while bending and lifting. The pressure is mainly due to water pressure across the nucleus and inner annulus in a normal disc. When load on the disc is increased, pressure is distributed evenly across the endplate and throughout the disc.
During loading the disc deforms and loses height. The endplate and annulus bulge, increasing the tension on these structures, and the pressure of the nucleus consequently rises. The degree of deformation of the disc depends on the rate at which it is loaded. The disc can deform considerably, compressing or extending by 30 to 60% during flexion and extension. Distances between adjacent spinal processes can increase by over 300%. If a load is re- moved within a few seconds, the disc quickly returns to its former state, but if the load is maintained, the disc continues to lose height. This “creep” results from the continuing deformation of the disc structures and also from fluid loss, because discs lose fluid as a result of the increased pressure. Between 10 and 25% of the disc’s fluid is slowly lost during daily activities, when the disc is under much greater pressures, and regained when lying down at rest. This loss of water can lead to a decrease in an individual’s height of 1 to 2 cm from morning to evening among dayworkers.
As the disc changes its composition because of ageing or degeneration, the response of the disc to mechanical loads also changes. With a loss of proteoglycan and thus water content, the nucleus can no longer respond as efficiently. This change results in uneven stresses across the endplate and the annulus fibres, and, in severe cases of degeneration, the inner fibres may bulge inward when the disc is loaded, which, in turn, may lead to abnormal stresses on other disc structures, eventually causing their failure. The rate of creep is also increased in degenerated discs, which thus lose height faster than normal discs under the same load. Narrowing of the disc space affects other spinal structures, such as muscles and ligaments, and, in particular, leads to an increase in pressure on the facet joints, which may be the cause of the degenerative changes seen in the facet joints of spines with abnormal discs.
Contribution of Major Components to Function
Proteoglycans
Disc function depends on maintaining equilibrium in which the water pressure of the disc is balanced by the disc swelling pressure. The swelling pressure depends on the concentration of ions attracted into the disc by the negatively charged proteoglycans, and thus depends directly on the concentration of proteoglycans. If the load on the disc is increased, water pressure rises and disturbs the equilibrium. To compensate, fluid seeps out of the disc, increasing proteoglycan concentration and disc osmotic pressure. Such fluid expression continues either until the balance is restored or the load on the disc is removed.
Proteoglycans affect fluid movement in other ways, as well. Because of their high concentration in the tissue, the spaces between chains are very small (0.003 to 0.004 mm). Fluid flow through such small pores is very slow, and thus even though there is a large pressure differential, the rate at which fluid is lost, and hence the rate of disc creep, is slow. However, since discs which have degenerated have lower proteoglycan concentrations, fluid can flow through the matrix faster. This may be why degenerated discs lose height more quickly than normal discs. The charge and high concentration of proteoglycans control the entry and movement of other dissolved substances into the disc. Small molecules (nutrients like glucose, oxygen) can easily enter the disc and move through the matrix. Electropositive chemicals and ions, such as Na+or Ca2+, have higher concentrations in the negatively charged disc than in the surrounding interstitial fluid. Large molecules, such as serum albumin or immunoglobulins, are too bulky to enter the disc, and are present only in very low concentrations. Proteoglycans may also affect cellular activity and metabolism. Small proteoglycans, such as biglycan, may bind growth factors and other mediators of cellular activity, releasing them when the matrix is degraded.
Water
Water is the major component of the disc and rigidity of the tissue is maintained by the hydrophilic properties of the proteoglycans. With initial loss of water, the disc becomes more flaccid and deformable as the collagen network relaxes. However, once the disc has lost a significant fraction of water, its mechanical properties change drastically; the tissue behaves more like a solid than a composite under load. Water also provides the medium through which nutrients and wastes are exchanged between the disc and the surrounding blood supply.
Collagen
The collagen network, which can support high tensile loads, provides a framework for the disc, and anchors it to the neighbouring vertebral bodies. The network is inflated by the water taken in by the proteoglycans; in turn the network restrains the proteoglycans and prevents them from escaping from the tissue. These three components together thus form a structure which is able to support high compressive loads.
The organization of the collagen fibrils provides the disc with its flexibility. The fibrils are arranged in layers, with the angle at which the fibrils of each layer run between the neighbouring vertebral bodies, alternating in direction. This highly specialized weave allows the disc to wedge extensively, thus allowing bending of the spine, even though collagen fibrils themselves can extend by only about 3%.
Metabolism
The cells of the disc produce both large molecules and enzymes which can break down matrix components. In a healthy disc, the rates of matrix production and breakdown are balanced. If the balance is upset, the composition of the disc must ultimately change. In growth, synthesis rates for new and replacement mol-ecules are higher than degradation rates, and matrix materials accumulate around the cells. With ageing and degeneration, the reverse occurs. Proteoglycans normally last for about two years. Collagen lasts for many more years. If the balance is disturbed, or if cellular activity falls, the proteoglycan content of the matrix eventually decreases, which affects the mechanical properties of the disc.
Disc cells also respond to changes in mechanical stress. Loading affects disc metabolism, although the mechanisms are not clear. At present it is impossible to predict which mechanical demands encourage a stable balance, and which may favour degradation over synthesis of matrix.
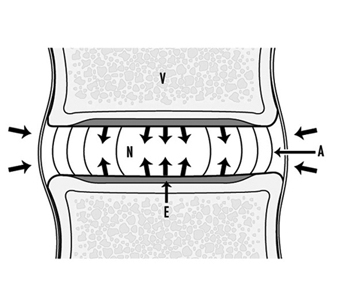
Supply of nutrients
Because the disc receives nutrients from the blood supply of the adjacent tissues, the nutrients such as oxygen and glucose must diffuse through the matrix to the cells in the centre of the disc. Cells may be as much as 7 to 8 mm from the nearest blood supply. Steep gradients develop. At the interface between the disc and the vertebral body, the concentration of oxygen is around 50%, while at the centre of the disc it is below 1%. Disc metabolism is mainly anaerobic. When oxygen falls below 5%, the disc increases production of lactate, a metabolic waste product. The lactate concentration in the centre of the nucleus may be six to eight times higher than that in the blood or interstitium (see figure 5).
Figure 5. The main nutritional pathways to the inter- vertebral disc are by diffusion from the vasculature within the vertebral body (V), through the endplate (E) to the nucleus (N) or from the blood supply outside the annulus (A).
A fall in the supply of nutrients is often suggested to be a major cause of disc degeneration. Endplate permeability of the disc decreases with age, which may impede nutrient transport into the disc and could lead to accumulation of wastes, such as lactate. In discs where nutrient transport has been reduced, oxygen concentrations in the disc centre can fall to very low levels. Here anaerobic metabolism, and consequently lactate production, increases, and the acidity in the disc centre may fall to as low as pH 6.4. Such low values of pH, as well as low oxygen tensions, reduce the rate of matrix synthesis, resulting in a fall in proteoglycan content. In addition, the cells themselves may not survive prolonged exposure to acid pH. A high percentage of dead cells have been found in human discs.
Degeneration of the disc leads to a loss of proteoglycan and a shift in its structure, disorganization of the collagen network and an ingrowth of blood vessels. There is the possibility that some of these changes could be reversed. The disc has been shown to have some capability of repair.
Diseases
Scoliosis: Scoliosis is a sideways bend of the spine, where both the intervertebral disc and vertebral bodies are wedged. It is usually associated with a twisting or rotation of the spine. Because of the manner in which the ribs are attached to the vertebrae this gives rise to a “rib hump”, visible when the affected individual bends forward. Scoliosis may be due to a congenital defect in the spine, such as a wedge-shaped hemi-vertebra, or it may arise secondary to a disorder such as neuromuscular dystrophy. However, in the majority of cases the cause is unknown and it is hence termed idiopathic scoliosis. Pain is rarely a problem in scoliosis and treatment is carried out, mainly to halt further development of the lateral curvature of the spine. (For details on clinical treatment of this and other spinal pathologies see Tidswell 1992.)
Spondylolisthesis: Spondylolisthesis is a forward, horizontal slip of one vertebra in relation to another. It may result from a fracture in the bridge of bone connecting the front to the posterior of the vertebra. Obviously the intervertebral disc between two such vertebrae is stretched and subjected to abnormal loads. The matrix of this disc, and to a lesser extent, adjacent discs, shows changes in composition typical of degeneration—loss of water and proteoglycan. This condition can be diagnosed by x ray.
Ruptured or prolapsed disc: Rupture of the posterior annulus is quite common in physically active young or middle-aged adults. It cannot be diagnosed by x ray unless a discogram is carried out, whereby radio-opaque material is injected into the centre of the disc. A tear can then be demonstrated by the tracking of the discogram fluid. Sometimes isolated and sequestered pieces of disc material can pass through this tear into the spinal canal. Irritation or pressure on the sciatic nerve causes intense pain and paraesthesia (sciatica) in the lower limb.
Degenerative disc disease: This is a term applied to an ill-defined group of patients who present with low-back pain. They may show changes in the x ray appearance, such as a decrease in disc height and possibly osteophyte formation at the rim of the vertebral bodies. This group of patients could represent the endstage of several pathological pathways. For example, untreated annular tears may eventually take on this form.
Spinal stenosis: The narrowing of the spinal canal that occurs in spinal stenosis causes mechanical compression of spinal nerve roots and its blood supply. As such it can lead to symptoms such as weakness, altered reflexes, pain or loss of feeling (paraesthesia), or sometimes have no symptoms. The narrowing of the canal can, in turn, be caused by various factors including protrusion of the intervertebral disc into the canal space, new bone formation in the facet joints (facet hypertrophy) and arthritis with inflammation of other soft connective tissues.
Interpretation of more recent imaging techniques in relation to disc pathology has not been completely established. For example, degenerated discs on magnetic resonance imaging (MRI) give an altered signal from that seen for “normal” discs. However, the correlation between a disc of “degenerate” appearance on MRI and clinical symptoms is poor, with 45% of MRI-degenerate discs being asymptomatic and 37% of patients with low-back pain having normal MRI of the spine.
Risk Factors
Loading
Load on the discs depends on posture. Intradiscal measurements show that the sitting position leads to pressures five times greater than those within the resting spine (see Figure 8). If external weights are lifted this can greatly increase the intradiscal pressure, especially if the weight is held away from the body. Obviously an increased load can lead to a rupture in discs that otherwise might remain intact.
Epidemiological investigations reviewed by Brinckmann and Pope (1990) agree in one respect: repetitive lifting or carrying of heavy objects or performing work in flexed or hyperextended posture represent risk factors for low-back problems. Similarly, certain sports, such as weight lifting, may be associated with a higher incidence of back pain than, for example, swimming. The mechanism is not clear, although the different loading patterns could be relevant.
Smoking
The nutrition of the disc is very precarious, requiring only a small reduction in the flow of nutrients to render it insufficient for the normal metabolism of the disc cells. Cigarette smoking can cause such a reduction because of its effect on the circulatory system outside the intervertebral disc. The transport of nutrients, such as oxygen, glucose or sulphate, into the disc is significantly reduced after only 20 to 30 minutes of smoking, which may explain the higher incidence of low-back pain in individuals who smoke compared to those who do not (Rydevik and Holm 1992).
Vibration
Epidemiological studies have shown that there is an increased incidence of low-back pain in individuals exposed to high levels of vibration. The spine is susceptible to damage at its natural frequencies, particularly from 5 to 10 Hz. Many vehicles excite vibrations at these frequencies. Studies reported by Brinckmann and Pope (1990) have shown a relationship between such vibrations and the incidence of low-back pain. Since vibration has been shown to affect the small blood vessels in other tissues, this may also be the mechanism for its effect on the spine.
Low-Back Region
Low-back pain is a common ailment in populations of working age. About 80% of people experience low-back pain during their lifetime, and it is one of the most important causes for short- and long-term disability in all occupational groups. Based on the aetiology, low-back pain can be classified into six groups: mechanical, infectious (e.g., tuberculosis), inflammatory (e.g., ankylosing spondylitis), metabolic (e.g., osteoporosis), neoplastic (e.g., cancer) and visceral (pain caused by diseases of the inner organs).
The low-back pain in most people has mechanical causes, which include lumbosacral sprain/strain, degenerative disc disease, spondylolisthesis, spinal stenosis and fracture. Here only mechanical low-back pain is considered. Mechanical low-back pain is also called regional low-back pain, which may be local pain or pain radiating to one or both legs (sciatica). It is characteristic for mechanical low-back pain to occur episodically, and in most cases the natural course is favourable. In about half of acute cases low-back pain subsides in two weeks, and in about 90% within two months. About every tenth case is estimated to become chronic, and it is this group of low-back pain patients that accounts for the major proportion of the costs due to low-back disorders.
Structure and Function
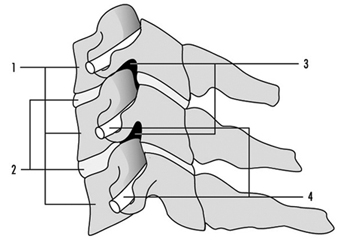
Due to upright posture the structure of the lower part of the human spine (lumbosacral spine) differs anatomically from that of most vertebrate animals. The upright posture also increases mechanical forces on the structures in the lumbosacral spine. Normally the lumbar spine has five vertebrae. The sacrum is rigid and the tail (coccyx) has no function in human beings as shown in figure 1.
Figure 1. The spine, its vertebrae and curvature.
The vertebrae are bound together by intervertebral discs between the vertebral bodies, and by ligaments and muscles. These soft-tissue bindings make the spine flexible. Two adjacent vertebrae form a functional unit, as shown in figure 2. The vertebral bodies and the discs are the weight-bearing elements of the spine. The posterior parts of the vertebrae form the neural arch that protects the nerves in the spinal canal. The vertebral arches are attached to each other via facet joints (zygapophyseal joints) that determine the direction of motion. The vertebral arches are also bound together by numerous ligaments that determine the range of motion in the spine. The muscles that extend the trunk backward (extensors) are attached to the vertebral arches. Important attachment sites are three bony projections (two lateral and the spinal process) of the vertebral arches.
Figure 2. The basic functional unit of the spine.
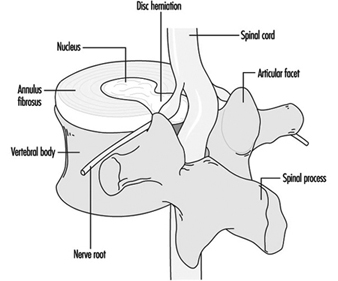
The spinal cord terminates at the level of the highest lumbar vertebrae (L1-L2). The lumbar spinal canal is filled by the extension of the spinal cord, cauda equina, which is composed of the spinal nerve roots. The nerve roots exit the spinal canal pairwise through intervertebral openings (foramina). A branch innervating the tissues in the back departs from each of the spinal nerve roots. There are nerve endings transmitting pain sensations (nociceptive endings) in muscles, ligaments and joints. In a healthy intervertebral disc there are no such nerve endings except for the outermost parts of the annulus. Yet, the disc is considered the most important source of low-back pain. Annular ruptures are known to be painful. As a sequel of disc degeneration a herniation of the semigelatinous inner part of the intervertebral disc, the nucleus, can occur into the spinal canal and lead to compression and/or inflammation of a spinal nerve along with symptoms and signs of sciatica, as shown in figure 3.
Figure 3. Herniation of the intervertebrai disc.
Muscles are responsible for the stability and motion of the back. Back muscles bend the trunk backward (extension), and abdominal muscles bend it forward (flexion). Fatigue due to sustained or repetitive loading or sudden overexertion of muscles or ligaments can cause low-back pain, albeit the exact origin of such pain is difficult to localize. There is controversy about the role of soft tissue injuries in low-back disorders.
Low-Back Pain
Occurrence
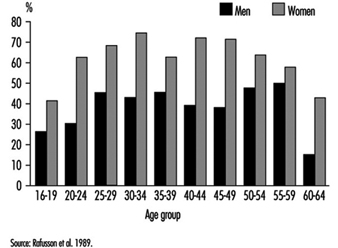
The prevalence estimates of low-back pain vary depending on the definitions used in different surveys. The prevalence rates of low-back pain syndromes in the Finnish general population over 30 years of age are given in table 1. Three in four people have experienced low-back pain (and one in three, sciatic pain) during their lifetime. Every month one in five people suffers from low-back or sciatic pain, and at any point in time, one in six people has a clinically verifiable low-back pain syndrome. Sciatica or herniated intervertebral disc is less prevalent and afflicts 4% of the population. About half of those with a low-back pain syndrome have functional impairment, and the impairment is severe in 5%. Sciatica is more common among men than among women, but other low-back disorders are equally common. Low-back pain is relatively uncommon before the age of 20, but then there is a steady increase in the prevalence until the age of 65, after which there is a decline.
Table 1. Prevalence of back disorders in the Finnish population over 30 years of age, percentages.
|
Men+ |
Women+ |
|
|
Lifetime prevalence of back pain |
76.3 |
73.3 |
|
Lifetime prevalence of sciatic pain |
34.6 |
38.8 |
|
Five-year prevalence of sciatic pain having caused bedrest for at least two weeks |
17.3 |
19.4 |
|
One-month prevalence of low-back or sciatic pain |
19.4 |
23.3 |
|
Point prevalence of clinically verified: |
||
|
Low-back pain syndrome |
17.5 |
16.3 |
|
Sciatica or prolapsed disc* |
5.1 |
3.7 |
+ age-adjusted
* p 0.005
Source: Adapted from Heliövaara et al. 1993.
The prevalence of degenerative changes in the lumbar spine increases with increasing age. About half of 35- to 44-year-old men and nine out of ten men 65 years or older have radiographic signs of disc degeneration of the lumbar spine. Signs of severe disc degeneration are noted in 5 and 38%, respectively. Degener-ative changes are slightly more common in men than in women. People who have degenerative changes in the lumbar spine have low-back pain more frequently than those without, but degener-ative changes are also common among asymptomatic people. In magnetic resonance imaging (MRI), disc degeneration has been found in 6% of asymptomatic women 20 years or younger and in 79% of those 60 years or older.
In general, low-back pain is more common in blue-collar occupations than in white-collar occupations. In the United States, materials handlers, nurses’ aides and truck drivers have the highest rates of compensated back injuries.
Risk factors at work
Epidemiological studies have quite consistently found that low-back pain, sciatica or herniated intervertebral disc and degener-ative changes of the lumbar spine are associated with heavy physical work. Little is known, however, of the acceptable limits of physical load on the back.
Low-back pain is related to frequent or heavy lifting, carrying, pulling and pushing. High tensile forces are directed to the muscles and ligaments, and high compression to the bones and joint surfaces. These forces can cause mechanical injuries to the vertebral bodies, intervertebral discs, ligaments and the posterior parts of the vertebrae. The injuries may be caused by sudden overloads or fatigue due to repetitive loading. Repeated microtrauma, which may even occur without being noticed, have been proposed as a cause for degeneration of the lumbar spine.
Low-back pain is also associated with frequent or prolonged twisting, bending or other non-neutral trunk postures. Motion is necessary for the nutrition of the intervertebral disc and static postures may impair the nutrition. In other soft tissues, fatigue can develop. Also prolonged sitting in one position (for instance, machine seamstresses or motor vehicle drivers) increases the risk of low-back pain.
Prolonged driving of motor vehicles has been found to increase the risk of low-back pain and sciatica or herniated disc. Drivers are exposed to whole-body vibration that has an adverse effect on disc nutrition. Also sudden impulses from rough roads, postural stress and materials handling by professional drivers may contribute to the risk.
An obvious cause for back injuries is direct trauma caused by an accident such as falling or slipping. In addition to the acute injuries, there is evidence that traumatic back injuries contribute substantially to the development of chronic low-back syndromes.
Low-back pain is associated with various psychosocial factors at work, such as monotonous work and working under time pressure, and poor social support from co-workers and superiors. The psychosocial factors affect reporting and recovery from low-back pain, but there is controversy about their aetiological role.
Individual risk factors
Height and overweight: Evidence for a relationship of low-back pain with body stature and overweight is contradictory. Evidence is, however, quite convincing for a relationship between sciatica or herniated disc and tallness. Tall people may have a nutritional disadvantage due to a greater disc volume, and they may also have ergonomic problems at the worksite.
Physical fitness: Study results on an association between physical fitness and low-back pain are inconsistent. Low-back pain is more common in people who have less strength than their job requires. In some studies poor aerobic capacity has not been found to predict future low-back pain or injury claims. The least fit people may have an increased overall risk for back injuries, but the most fit people may have the most expensive injuries. In one study, good back muscle endurance prevented first-time occurrence of low-back pain.
There is considerable variation in the mobility of the lumbar spine among people. People with acute and chronic low-back pain have reduced mobility, but in prospective studies mobility has not predicted the incidence of low-back pain.
Smoking: Several studies have shown that smoking is associated with an increase in the risk of low-back pain and herniated disc. Smoking also seems to enhance disc degeneration. In experimental studies, smoking has been found to impair the nutrition of the disc.
Structural factors: Congenital defects of the vertebrae as well as unequal leg length can cause abnormal loading in the spine. Such factors are, however, not considered very important in the caus-ation of low-back pain. Narrow spinal canal predisposes to nerve root compression and sciatica.
Psychological factors: Chronic low-back pain is associated with psychological factors (e.g., depression), but not all people who suffer from chronic low-back pain have psychological problems. A variety of methods have been used to differentiate low-back pain caused by psychological factors from low-back pain caused by physical factors, but the results have been contradictory. Mental stress symptoms are more common among people with low-back pain than among symptomless people, and mental stress even seems to predict the incidence of low-back pain in the future.
Prevention
The accumulated knowledge based on epidemiological studies on the risk factors is largely qualitative and thus can give only broad guidelines for the planning of preventive programmes. There are three principal approaches in prevention of work-related low-back disorders: ergonomic job design, education and training, and worker selection.
Job design
It is widely believed that the most effective means to prevent work-related low-back disorders is job design. An ergonomic intervention should address the following parameters (shown in table 2).
Table 2. Parameters which should be addressed in order to reduce the risks for low-back pain at work.
|
Parameter |
Example |
|
1. Load |
The weight of the object handled, the size of the object handled |
|
2. Object design |
The shape, location and size of handles |
|
3. Lifting technique |
The distance from the centre of gravity of the object and the worker, twisting motions |
|
4. Workplace layout |
The spatial features of the task, such as carrying distance, range of motion, obstacles such as stairs |
|
5. Task design |
Frequency and duration of the tasks |
|
6. Psychology |
Job satisfaction, autonomy and control, expectations |
|
7. Environment |
Temperature, humidity, noise, foot traction, whole-body vibration |
|
8. Work organization |
Team work, incentives, shifts, job rotation, machine pacing, job security. |
Source: Adapted from Halpern 1992.
Most ergonomic interventions modify the loads, the design of objects handled, lifting techniques, workplace layout and task design. The effectiveness of these measures in controlling the occurrence of low-back pain or medical costs has not been clearly demonstrated. It may be most efficient to reduce the peak loads. One suggested approach is to design a job so that it is within the physical capacity of a large percentage of the working population (Waters et al. 1993). In static jobs restoration of motion can be achieved by restructuring the job, by job rotation or job enrichment.
Education and training
Workers should be trained to perform their work appropriately and safely. Education and training of workers in safe lifting have been widely implemented, but the results have not been convincing. There is general agreement that it is beneficial to keep the load close to the body and to avoid jerking and twisting, but as to the advantages of leg lift and back lift, the opinions of the experts are conflicting.
If mismatch between job demands and the strength of workers is detected and job redesign is not possible, a fitness training programme should be provided for the workers.
In prevention of disability due to low-back pain or chronicity, back school has proven effective in subacute cases, and general fitness training in subchronic cases.
Training needs to be extended also to management. Aspects of management training include early intervention, initial conservative treatment, patient follow-up, job placement and enforcement of safety rules. Active management programmes can significantly reduce long-term disability claims and accident rates.
Medical personnel should be trained in the benefits of early intervention, conservative treatment, patient follow-up and job placement techniques. The Quebec Task Force report on the management of activity-related spinal disorders and other clinical practice guidelines gives sound guidance for proper treatment. (Spitzer et al. 1987; AHCPR 1994.)
Worker selection
In general, pre-employment selection of workers is not considered an appropriate measure for prevention of work-related low-back pain. History of previous back trouble, radiographs of the lumbar spine, general strength and fitness testing—none of these has shown good enough sensitivity and specificity in identifying persons with an increased risk for future low-back trouble. The use of these measures in pre-employment screening can lead to undue discrimination against certain groups of workers. There are, however, some special occupational groups (e.g., fire-fighters and police officers) in which pre-employment screening can be considered appropriate.
Clinical characteristics
The exact origin of low-back pain often cannot be determined, which is reflected as difficulties in the classification of low-back disorders. To a great extent the classification relies on symptom characteristics supported by clinical examination or by imaging results. Basically, in clinical physical examination patients with sciatica caused by compression and/or inflammation of a spinal nerve root can be diagnosed. As to many other clinical entities, such as facet syndrome, fibrositis, muscular spasms, lumbar compartment syndrome or sacro-iliac syndrome, clinical verification has proven unreliable.
As an attempt to resolve the confusion the Quebec Task Force on Spinal Disorders carried out a comprehensive and critical literature review and ended up recommending the use of the classification for low-back pain patients shown in table 3.
Table 3. Classification of low-back disorders according to the Quebec Task Force on Spinal Disorders
1. Pain
2. Pain with radiation to lower limb proximally
3. Pain with radiation to lower limb distally
4. Pain with radiation to lower limb and neurological signs
5. Presumptive compression of a spinal nerve root on a simple radiogram (i.e., spinal instability or fracture)
6. Compression of a spinal nerve root confirmed by: Specific imaging techniques (computerized tomography,
myelography, or magnetic resonance imaging), Other diagnostic techniques (e.g., electromyography,
venography)
7. Spinal stenosis
8. Postsurgical status, 1-6 weeks after intervention
9. Postsurgical status, >6 weeks after intervention
9.1. Asymptomatic
9.2. Symptomatic
10. Chronic pain syndrome
11. Other diagnoses
For categories 1-4, additional classification is based on
(a) Duration of symptoms (7 weeks),
(b) Working status (working; idle, i.e., absent from work, unemployed or inactive).
Source: Spitzer et al. 1987.
For each category, appropriate treatment measures are given in the report, based on critical review of the literature.
Spondylolysis and spondylolisthesis
Spondylolysis means a defect in the vertebral arch (pars inter- articularis or isthmus), and spondylolisthesis denotes forward displacement of a vertebral body relative to the vertebra below. The derangement occurs most frequently at the fifth lumbar vertebra.
Spondylolisthesis can be caused by congenital abnormalities, by a fatigue fracture or an acute fracture, instability between two adjacent vertebrae due to degeneration, and by infectious or neo- plastic diseases.
The prevalence of spondylolysis and spondylolisthesis ranges from 3 to 7%, but in certain ethnic groups the prevalence is considerably higher (Lapps, 13%; Eskimos in Alaska, 25 to 45%; Ainus in Japan, 41%), which indicates a genetic predisposition. Spondylolysis is equally common in people with and without low-back pain, but people with spondylolisthesis are susceptible to recurrent low-back pain.
An acute traumatic spondylolisthesis can develop due to an accident at work. The prevalence is increased among athletes in certain athletic activities, such as American football, gymnastics, javelin throwing, judo and weight lifting, but there is no evidence that physical exertion at work would cause spondylolysis or spondylolisthesis.
Piriformis syndrome
Piriformis syndrome is an uncommon and controversial cause for sciatica characterized by symptoms and signs of sciatic nerve compression at the region of the piriformis muscle where it passes through the greater sciatic notch. No epidemiological data on the prevalence of this syndrome are available. The present knowledge is based on case reports and case series. Symptoms are aggravated by prolonged hip flexion, adduction and internal rotation. Recently piriformis muscle enlargement has been verified in some cases of piriformis syndrome by computed tomography and magnetic resonance imaging. The syndrome can result from an injury to the piriformis muscle.
Thoracic Spine Region
The most common symptoms and signs that occur in the upper region of the back and spine are pain, tenderness, weakness, stiffness and/or deformity in the back. Pain is much more frequent in the lower (lumbar) back and in the neck than in the upper trunk (thoracic back). Besides local symptoms, the thoracic disorders may cause pain that radiates to the lumbar region and the lower limbs, to the neck and shoulders, to the rib cage and to the abdomen.
Painful Soft-Tissue Disorders
The causes of thoracic back pain are multifactorial and often obscure. The symptoms in many cases arise from an overuse, an overstretching and/or usually mild ruptures of the soft tissues. There are, however, also many specific disorders that can lead to back pain, such as severe scoliosis (hunchback) or kyphosis of different aetiology, Morbus Sheuermann (osteochondritis of the thoracic spine, sometimes painful in adolescents but seldom in adults), and other deformities which may follow trauma or some neurologic and muscular diseases. Infection in the spine (spondylitis) is often localized to the thoracic region. Many kinds of microbes may cause spondylitis, such as tuberculosis. Thoracic back pain may occur in rheumatic diseases, especially in ankylosing spondylitis and in severe osteoporosis. Many other intraspinal, intrathoracal and intra-abdominal diseases, such as tumours, may also result in back symptoms. Generally, it is common that the pain may be felt in the thoracic spine (referred pain). Skeletal metastases of cancer from other sites are frequently localized to the thoracic spine; this is especially true of metastatic breast, kidney, lung and thyroid cancers. It is extremely rare for a thoracic disc to rupture, the incidence being 0.25 to 0.5% of all intervertebral disc ruptures.
Examination: At examination many intra- and extraspinal disorders causing symptoms in the thoracic back should always be kept in mind. The older the patient, the more frequent the back symptoms arising from primary tumours or metastases. A comprehensive interview and a careful examination are therefore very important. The purpose of the examination is to clarify the aetio-logy of the disease. The clinical examination should include ordinary procedures, such as inspection, palpation, testing of the muscle strength, the joint mobility, the neurological state and so on. In cases with prolonged and severe symptoms and signs, and when a specific disease is suspected by plain x ray, other radiography tests, such as MRI, CT, isotope imaging and ENMG can contribute to clarifying the aetiological diagnosis and to localizing the disorder process. Nowadays, MRI is usually the radiological method of choice in thoracic back pain.
Degenerative Thoracic Spine Disorders
All adults suffer spinal degenerative changes which progress with age. Most people do not have any symptoms from these changes, which are often found while investigating other diseases, and are usually without any clinical importance. Infrequently, the degenerative changes in the thoracic region lead to local and radiating symptoms—pain, tenderness, stiffness and neurological signs.
Narrowing of the spinal canal, spinal stenosis, may lead to compression of vascular and neurologic tissues resulting in local and/or radiating pain and neurologic deficiency. A thoracic disc prolapse seldom provokes symptoms. In many cases a radiologically detected disc prolapse is a side finding and does not provoke any symptoms.
The main signs of degenerative disorders of the thoracic spine are local tenderness, muscle spasm or weakness and locally decreased mobility of the spine. In some cases there may be neurological disturbances—muscle paresis, reflex and sensation deficiencies locally and/or distally of the affected tissues.
The prognosis in thoracic disc prolapse is usually good. The symptoms subside as in the lumbar and neck region within a few weeks.
Examination. A proper examination is essential especially in old persons in prolonged and severe pain and in paresis. Besides a detailed interview, there should be an adequate clinical examination, including inspection, palpation, testing of mobility, muscle strength and neurological state. Of the radiological examinations, plain radiography, CT and especially MRI are advantageous in evaluating the aetiological diagnosis and the localization of the pathological changes in the spine. ENMG and isotope imaging may contribute to the diagnosis. In the differential diagnosis laboratory tests may be valuable. In pure spinal disc prolapse and degenerative changes there are no specific abnormalities in the laboratory tests.
Neck
Pain and discomfort in the neck are some of the most common symptoms associated with work. They occur in heavy, manual work as well as in seated, sedentary work, and the symptoms often last for prolonged periods of time—in fact, in some cases, over the whole lifetime. It follows that disorders of the neck are difficult to cure once they have arisen, and therefore much emphasis should be put into primary prevention. There are three main reasons why neck disorders are common in working life:
- The load on the neck structures is maintained for prolonged periods of time, due to high visual demands of the job and to the need of stabilization of the neck-shoulder region in working with the arms.
- Psychologically demanding jobs with high demands on concentration and on quality and quantity of work output are common, and induce an increased activity in neck muscles. This tension increases further if the job in general is psychologically stressful, due to, for example, poor industrial relations, little influence on the organization of work and so on.
- The discs and joints of the neck are frequently the site of degenerative changes, which increase in prevalence with age. This reduces the capacity to withstand occupational workloads. It is also likely that the rate of degeneration increases as the result of physical demands of the job.
Anatomy and Biomechanics of the Neck
The musculoskeletal part of the neck consists of seven vertebral bodies, six intervertabral discs (consisting of cartilage), ligaments to hold these together and linking them to the skull and to the thoracic spine, and muscles surrounding the spine. Although each joint of the cervical spine has a very limited range of motion, the neck can be bent, extended, twisted and tilted with a relatively large range of motion (see table 1). In a normal upright posture and looking straight forward, the centre of gravity of the head and neck is actually situated in front of the centre of support, and therefore needs to be balanced by the dorsal muscles, that is, those situated behind the vertebral bodies. When the head is tilted forward more muscle force is needed to balance the head, and when forward tilt of the head is maintained for prolonged periods of time a substantial muscle fatigue can develop. In addition to muscle fatigue, tilting and bending the head leads to increased compression of the inter-vertebral discs, which may accelerate degenerative processes.
Table 1. Normal and permissible for prolonged driving range of motion (ROM) in degrees, for head.
|
Normal1 |
Permissible2 for prolonged driving |
|
|
Lateral bend |
45 |
– |
|
Twist |
60 |
0 – 15 |
|
Flexion |
45 |
0 – 25 |
|
Extension |
–45 |
0 – –5 |
1 American Academy of Orthopedic Surgeons 1988.
2 Hansson 1987
The muscles surrounding the neck are also active in arm work, in order to stabilize the shoulder/arm complex. The trapezius and several other muscles originate on the cervical spine and extend downwards/outwards to insert on the shoulder. These muscles are commonly the site of dysfunction and disorders, especially in static or repetitive work tasks where the arms are elevated and the vision is fixed.
The structures stabilizing the neck are very robust, which serves to protect the nervous tissue inside the spinal canal and the nerves emerging from the intervertebral openings and supplying the neck, upper extremity and upper part of the thorax. The intervertebral discs, the adjoining parts of the vertebral bodies and the facet joints of the intervertebral foramina are often the site of degenerative changes, which can exert pressure on the nerves and narrow their space. (See figure 1).
Figure 1. Schematic drawing of a cross-section of three of the lower cervical vertebral bodies (1) with intervertebral discs; (2) intervertebral foramina; (3) and nerve roots; (4) seen from the side.
As mentioned in the introduction, symptoms like pain, ache and discomfort in the neck are very common. Depending on the criteria used and the method of investigation, the prevalence rates for neck disorders vary. If a postal enquiry or an interview focusing on musculoskeletal disorders is used, the prevalence of disorders is usually higher than in a thorough investigation also including a physical examination. Thus comparisons between groups should be made only when the same investigation technique has been employed. Figure 2 gives one-year prevalence figures for a representative sample of the Icelandic population who answered a postal enquiry, the so-called “Nordic” questionnaire on musculo- skeletal disorders (Kuorinka et al. 1987). Neck trouble (pain, ache or discomfort) was the third most common (38% average for the whole sample), after shoulder (43%), and low-back (56%) problems. Neck trouble among women was more common than among men, and there was an increase in prevalence up to age 25 to 30, when the rates stabilized; they again went down somewhat at age 50 to 55. In a representative sample of 200 men and women from Stockholm, aged 16 to 65 years, the 12-month prevalence was about 30% among the men and 60% among women. The experience of recent pain in the neck with a duration of at least one month, was found among 22% of a population sample in Gothenburg, Sweden—again rated third most common after shoulder and low-back pain.
Figure 2. Twelve-month prevalence of symptoms of neck trouble of a random sample of the Icelandic population (n=1000)
Risk Factors at Work
Neck disorders are considerably more prevalent in certain occupational groups. Using the Nordic questionnaire (Kuorinka et al. 1987), Swedish occupational health services have compiled data from several occupations. The results indicate that the risk of neck trouble (pain, ache or discomfort) is very high among visual display unit (VDU) operators, sewing machine operators, seamstresses and electronic assembly workers, with a 12-month period prevalence greater than 60%. In addition, up to one-third of those who report disorders also state that the problems have an impact on their working lives, either causing them to take sick-leave, or necessitating a change of job or work tasks.
Epidemiological studies of neck and shoulder disorders have been reviewed, and the different studies have been pooled by type of exposure (repetitive work and work above shoulder level, respectively). Soft-tissue disorders of the neck, such as tension neck and other myalgias, were considerably increased in a number of occupational tasks like data entry, typing, scissors manufacturing, lamp assembly and film rolling.
Degenerative disorders of the intervertebral discs of the neck are more common among coal-miners, dentists and meat industry workers (Hagberg and Wegman 1987).
Posture
Prolonged flexion, extension, lateral bending and twisting of the neck induce muscle fatigue, and may lead to chronic muscle injuries and degenerative changes of the cervical spine. The muscle activity needed to counteract the weight of the head in forward flexion of the neck increases with the flexion angle, as shown in figure 3. Fatigue and pain are common in neck flexion if prolonged work is performed. When the head is tilted forward to the extreme of its range of motion, the main load is transferred from muscles to ligaments and joint capsules surrounding the cervical spine. It has been calculated that if the entire cervical spine is flexed maximally, the torque exerted by the head and neck on the disc between the seventh cervical and the first thoracic vertebral body is increased by a factor of 3.6. Such postures lead to pain within only about 15 minutes, and usually the posture has to be normalized within 15 to 60 minutes because of intense pain. Postures where the neck is bent forward for prolonged periods of time—several hours—are common in assembly work in industry, in VDT work and in packaging and inspection tasks where the work stations are poorly designed. Such postures are frequently caused by a compromise between the need to perform work with the hands, without elevating the arms, and the simultaneous need for visual control. For a review of the mechanisms leading from muscle fatigue to injury, see the accompanying article “Muscles”.
Figure 3. Percentage of maximal neck extension strength required at increasing neck inclination (flexion).
Extension of the neck for prolonged periods, as in overhead work in the building industry, can be very tiring for the muscles in front of the cervical spine. Especially when carrying heavy protective equipment like safety helmets, the torque tilting the head backwards can be high.
Repetitive movements
Repetitive movements performed by the hands increase the demands on stabilization of the neck and shoulder region, and thereby increase the risk of neck complaints. Factors like high demands on speed and precision of movements, as well as high demands on force exerted by the hands, imply even larger demands on stabilization of the proximal body regions. Repetitive movements of the head are less common. Rapid and repeated changes between visual targets are usually accomplished through eye movements, unless the distance between the objects observed is fairly large. This may occur for example at large computerized work stations.
Vibration
Local vibration of the hands, such as working with drills and other vibrating hand-held machines, is transferred along the arm but the fraction transferred up to the shoulder-neck region is negligible. However, the holding of a vibrating tool may induce muscle contractions in the proximal shoulder-neck muscles in order to stabilize the hand and the tool, and may thereby exert a tiring effect on the neck. The mechanisms and the prevalence of such vibration-induced complaints are not well known.
Work organization
Work organization in this context is defined as the distribution of work tasks over time and between workers, the duration of work tasks, and the duration and distribution of rest periods and breaks. The duration of work and rest periods has a profound effect on tissue fatigue and recovery. Few specific studies on the effect of work organization on neck disorders have been performed. In a large epidemiological study in Sweden, it was found that VDU work exceeding four hours per day was associated with elevated rates of neck symptoms (Aronsson, Bergkvist and Almers 1992). These findings have subsequently been confirmed in other studies.
Psychological and social factors
Associations between psychological and social factors at work and disorders of the neck region have been demonstrated in several studies. Especially factors such as perceived psychological stress, poor control of work organization, poor relations with management and work mates and high demands on accuracy and speed of work have been highlighted. These factors have been associated with an increased risk (up to twofold) of disorders in cross-sectional studies. The mechanism is likely to be an increase of tension in the trapezius and other muscles surrounding the neck, as part of a general “stress” reaction. Since well-controlled longitudinal studies are scarce, it is still uncertain whether these factors are causal or aggravating. Moreover, poor psychological and social conditions often occur in jobs also characterized by prolonged awkward postures.
Individual factors
Individual characteristics like age, sex, muscle strength and endurance, physical fitness, body size, personality, intelligence, leisure time habits (physical activity, smoking, alcohol, diet) and previous musculoskeletal disorders have been discussed as factors which might modify the response to physical and psychosocial exposures. Age as a risk factor is discussed above and is illustrated in figure 2.
Females usually report a higher prevalence of neck symptoms than males. The most likely explanation is that exposure to both physical and psychosocial risk factors is higher in women than among men, such as in work with VDUs, assembly of small components and machine sewing.
Studies of muscle groups other than those of the neck do not consistently indicate that a low static strength implies an elevated risk of development of disorders. No data are available concerning neck muscles. In a recent study of a random population of Stockholm, low endurance at neck extension was weakly associated with later development of neck disorders (Schüldt et al. 1993). Similar results have been reported for low-back disorders.
In a longitudinal study in Sweden, personality type was a risk factor for development of shoulder-neck disorders (Hägg, Suurküla and Kilbom 1990). Those employees who had a type A personality (e.g., were ambitious and impatient) developed more serious problems than others, and these associations were not related to individual productivity.
Little is known of the association between other individual characteristics and neck disorders.
Prevention
Work station design
The work station should be organized so that the head is not statically bent, extended or twisted beyond the limits given for the permissible range of motion given for prolonged driving in table 1. Now and then, movements that are within the limits for normal range of motion are acceptable, as well as the occasional movement to the individual extremes. Experimental studies have shown that the load of the neck muscles is lower with a slightly backward tilted trunk than with a straight upright posture, which in turn is better than a forward tilted trunk (Schüldt 1988).
The set-up of the workstation and the positioning of the work object requires a careful consideration and a trade-off between the demands for optimal head and shoulder-arm posture. Usually the work object is positioned somewhat below elbow height, which may however induce a high strain on the neck muscles (e.g., in assembly work). This requires individually adjustable work stations.
Visual strain will increase the tension of the neck muscles, and therefore attention should be given to the lighting and contrasts of the work station and to readability of information given on VDUs and on printed material. For VDU work the viewing distance should be optimized to about 45 to 50 cm and the viewing angle to 10 to 20 degrees. The vision of the worker should be optimized with the aid of glasses.
Work organization
In work with static loads on the neck, such as in assembly and data entry VDU work, frequent breaks should be introduced to provide recovery from fatigue. Recommendations to introduce one break of about 10 minutes per hour and to limit VDU work to a maximum of four hours per day have been issued in some localities. As pointed out above, the scientific basis for these recommendations with regard to the neck is relatively weak.
Clinical Characteristics and Treatmentof Neck Disorders
Painful soft-tissue disorders
Tension neck and other myalgias
The most common localization for neck tension and other myalgias is in the upper part of the trapezius muscle, but other muscles originating in the neck are often affected simultaneously. Symptoms are stiffness of the neck and ache at work and at rest. Frequently, excessive muscle fatigue is perceived, even during short-lasting and low-level periods of work. The muscles are tender, and often “tender points” can be found on palpation. Tension neck is common in jobs with prolonged static loads on neck and shoulders. Microscopic examination of the tissue has shown changes in the muscle morphology, but the mechanisms are incompletely understood and are likely to involve both the blood circulation and the nervous regulation.
Acute torticollis
This state of acute pain and stiffness of the neck can be provoked by sudden twisting of the head and extension of the opposite arm. Sometimes no provoking event can be identified. Acute torticollis is believed to be caused by strain and partial ruptures of the ligaments of the neck. Usually the pain and stiffness subsides within a week following rest, external support of the neck (collar) and muscle-relaxing medication.
Degenerative disorders
Acute disorder (disc herniation)
Degeneration of the cervical spine involves the discs, which lose some of their resistance to even mild stresses. Herniation of the disc with extrusion of its contents, or bulging of it, can compromise nervous tissue and blood vessels laterally and posteriorly to the disc. One acute degenerative disorder of the disc is compression of the nerve roots extending from the spinal cord and supplying the neck, arms and upper thorax. Depending on the level of compression (disc between second and third cervical vertebrae, third and fourth, and so on), acute sensory and motor symptoms arise from the regions supplied by the nerves. The investigation of acute symptoms of the neck and arms includes a thorough neurological examination in order to identify the level of a possible disc prolapse and plain x-ray examination, usually supplemented with CT scanning and MRI.
Chronic disorders (Cervical spondylosisand cervical syndrome)
Degeneration of the cervical spine involves narrowing of the disc, formation of new bone (so-called osteophytes) extending from the edges of the cervical vertebra, and thickening of the ligaments as in acute disorder. When osteophytes extend into the foramina, they may compress the nerve roots. Spondylosis is the term used for the radiological changes in the neck. Sometimes these changes are associated with chronic local symptoms. Radiological changes may be advanced without serious symptoms and vice versa. Symptoms are usually ache and pain in the neck, sometimes extending to the head and the shoulder region, and reduced mobility. Whenever nerve roots are compressed, the diagnosis cervical syndrome is used. Symptoms of cervical syndrome are ache and pain in the neck, reduced mobility of the neck, and sensory and motor symptoms from the side of the compressed nerve root. Symptoms like reduced sensitivity to touch, numbness, tingling and reduced strength are common in the hand and arm. Thus symptoms are similar to those arising from acute disc prolapse, but usually the onset is more gradual and the severity may fluctuate depending on the external workload. Both cervical spondylosis and cervical syndrome are common in the general population, particularly among aged persons. The risk of cervical spondylosis is elevated in occupational groups with a sustained, high biomechanical load on the neck structures, like coal-miners, dentists and meat industry workers.
Traumatic disorders (whiplash injuries)
In rear-end car accidents, the head (if not restricted by support from behind) is tilted backward at high speed and with great force. In less severe accidents only partial muscle ruptures may occur, whereas severe accidents may seriously damage the muscles and ligaments in front of the cervical spine and also damage nerve roots. The most serious cases occur when the cervical vertebrae are dislocated. Whiplash injuries need careful examination and treatment, as long-lasting symptoms such as headaches may persist if the injury is not cared for properly.
Shoulder
Disorders of the shoulder region are common problems in both the general and working population. As many as one-third of all women and one-quarter of all men report feeling pain in the neck and shoulder every day or every other day. It is estimated that the prevalence of shoulder tendinitis in the general population is about 2%. Among male and female workers in the United States, the prevalence of shoulder tendinitis has been estimated to be as high as 8% among those exposed to highly repetitive or high-force hand motions, compared to about 1% for those without this type of musculoskeletal stress.
Anatomy
The bones in the shoulder include the collarbone (clavicle), the shoulder blade (scapula) and the (shoulder) glenohumeral joint, as shown in figure 1. The collarbone is connected to the body by the sternoclavicular joint, and to the shoulder-blades by the acromioclavicular joint. The sternoclavicular joint is the sole connection between the upper extremity and the rest of the body. The shoulder blade has no direct connection of its own and thus the shoulder is dependent on muscles for being fixed to the trunk. The upper arm is connected to the shoulder blade by the glenohumeral joint.
Figure 1. Schematic view of the skeletal parts of the shoulder-girdle.
The function of the shoulder is to provide a platform for the upper extremity, and for some of its muscles. Although the glenohumeral joint has a greater range of movement than, for example, the lower extremity in the hip, this flexibility has developed at the price of stability. While the hip joint has very strong ligaments, the ligaments in the glenohumeral joint are few and weak. In order to compensate for this comparative weakness, the glenohumeral joint is surrounded by shoulder muscles in the form of a cuff and is called the rotator cuff.
Biomechanics
The arm represents about 5% of the total body weight, and its centre of gravity is about midway down between the glenohumeral joint and the wrist. When the arm is raised and bent either away from or towards the body (abduction or flexion), a lever is created in which the distance from the centre of gravity increases, and hence the twisting force, and the loading torque, on the glenohumeral joint increases. The rate at which the torque increases, however, is not simply directly proportional to the angle at which the arm is bent, because the mathematical function which describes the biomechanical forces is not linear but is rather a sine function of the abduction angle. The torque will decrease only by about 10% if the flexion or abduction angle is decreased from 90 to 60 degrees. However, if the angle is decreased from 60 to 30 degrees, torque is reduced by as much as 50%.
The flexion strength in the glenohumeral joint is about 40 to 50 Nm for women and about 80 to 100 Nm for men. When the arm is held straight out (90-degree forward flexion) and no external load is placed on the arm—that is, the person is not holding anything or using the arm to exert a force—the static load is still about 15 to 20% of the maximal voluntary capacity (MVC) for women and about 10 to 15% MVC for men. If a tool weighing 1 kg is held in the hand with an arm extended, the corresponding load in the shoulder would be about 80% of the MVC for women, as illustrated in figure 2.
Figure 2. Female and male strength showing the results of holding a 1 kilogramme tool in the hand with the arm held straight at different angles of shoulder flexion.
The most important muscles for abduction—or raising the arm away from the body to the side—are the deltoid muscle, the rotator cuff muscles and the long head of the biceps. The most important muscles for forward flexion—raising the arm away from the body to the front—are the anterior part of the deltoid muscle, the rotator cuff muscles, the coracobrachialis muscle and the short head of the biceps brachii muscle. Inward rotation is performed by the pectoralis major muscle, the subscapularis muscle, the anterior part of the deltoid muscle and by the latissimus dorsi muscle. Outward rotation is performed by the posterior part of the deltoid muscle, the infraspinatus muscle and the minor and major teres muscles.
Rotator cuff muscles are engaged in any movement of the glenohumeral joint, which is to say any movement of the arm. The rotator cuff muscles originate from the shoulder blade, and their tendons are arranged around the humerus in the form of a cuff, from which their name is derived. The four rotator cuff muscles are the supraspinate, the infraspinate, the teres minor and the subscapularis muscle. These muscles function as ligaments in the glenohumeral joint and also keep the humeral head against the shoulder-blade. A rupture of the rotator cuff (e.g., of the supraspinous tendon) will cause a reduction in abduction strength, particularly involving those positions where the arm is bent away from the body. When the function of the deltoid muscles is lost, the abduction strength can be reduced by as much as 50%, regardless of the angle at which the arm is being bent.
Any time there is forward flexion or abduction of the arm, a load will be placed on the system. Many motions will cause a twisting force, or torque, as well. Since the arm is connected to the shoulder blade by the glenohumeral joint, any load that is placed on this joint will be transferred to the shoulder-blade. The load in the glenohumeral joint, measured in % MVC, is almost directly proportional to the load placed on the muscle which fixes the shoulder blade into place, the upper trapezius.
Major Specific Work-Related Diseases
Rotator cuff disorders and biceps tendinitis
Tendinitis and tenosynovitis are inflammations of a tendon and the synovial membrane of a tendon sheath. The tendons to the rotator cuff muscles (supraspinatus, infraspinatus, subscapularis, and teres minor muscles) and the long head of the biceps brachii are common sites for inflammation in the shoulder. Large movements of the tendons are involved at these locations. During elevation, as the tendons pass to the shoulder joint and under the bony structure there (the coraco-acromial arch), they may be impinged upon, and inflammation may result. These disorders are sometimes termed impingement syndromes. Inflammation of a tendon may be part of a general inflammatory disease, such as in rheumatoid arthritis, but also may be caused by local inflammation which results from mechanical irritation and friction.
Shoulder joint and acromioclavicular joint osteoarthritis
Shoulder joint and acromioclavicular joint osteoarthritis, OA, are degenerative changes of cartilage and bone in the joints and intervertebral discs.
Epidemiology
There is a high prevalence of shoulder tendinitis among welders and steel-platers, with rates of 18% and 16%, respectively. In one study which compared welders and steel-platers to male office workers, the welders and steel-platers were 11 to 13 times more likely to suffer from the disorder, as measured by the odds ratio. A similar odds ratio of 11 was found in a case-control study of male industrial workers who worked with their hands held at or about shoulder level. Automobile assemblers who suffered from acute shoulder pain and tendinitis were required to elevate their arms more frequently and for longer durations than were workers who did not have such job requirements.
Studies of industrial workers in the United States have shown there to be a prevalence of 7.8% of shoulder tendinitis and degenerative joint disease (shoulder) of cumulative trauma disorders (CTDs) among workers whose tasks involved exerting force or repetitive motions, or both, on the wrist and hands. In one study, female students performing repetitive shoulder flexion developed reversible shoulder tendinitis. They developed the condition when the flexion rate, over the course of one hour, was 15 forward flexions per minute and the angle of flexion was between 0 and 90 degrees. Boarding, folding and sewing workers suffered about twice as much shoulder tendinitis as did knitting workers. Among professional baseball pitchers, approximately 10% have experienced shoulder tendinitis. A survey of swimmers in Canadian swimming clubs found that 15% of the swimmers reported having significant shoulder disability, primarily due to impingement. The problem was particularly related to the butterfly and freestyle strokes. Tendinitis of the biceps brachii was found in 11% of the 84 best tennis players in the world.
Another study showed that shoulder joint osteoarthritis was more common in dentists than among farmers, but the ergonomic exposure related to shoulder joint OA has not been identified. An increased risk for acromioclavicular OA has been reported among construction workers. Heavy lifting and handling of heavy tools with hand-arm vibration have been suggested as the exposure related to acromioclavicular joint OA.
Mechanisms and Risk Factors of Disease
Pathophysiology of shoulder tendinitis
Tendon degeneration is often the predisposing factor for development of shoulder tendinitis. Such degeneration of the tendon can be caused by impairment of circulation to the tendon so that metabolism is disrupted. Mechanical stress may also be a cause. Cell death within the tendon, which forms debris and in which calcium may deposit, may be the initial form of degeneration. The tendons to the supraspinatus, the biceps brachii (long head) and the upper parts of the infraspinatus muscles have a zone in which there are no blood vessels (avascularity), and it is in this area that signs of degeneration, including cell death, calcium deposits and microscopic ruptures, are predominantly located. When blood circulation is impaired, such as through compression and static load on the shoulder tendons, then degeneration can be accelerated because normal body maintenance will not be functioning optimally.
Compression of the tendons occurs when the arm is elevated. A process that is often referred to as impingement involves forcing the tendons through the bony passageways of the shoulder, as illustrated in figure 3. Compression of the rotator cuff tendons (especially the supraspinatus tendon) results because the space between the humeral head and the tight coracoacromial arch is narrow. People who are suffering with long-term disability due to chronic bursitis or complete or partial tears of the rotator cuff tendons or biceps brachii usually also have impingement syndrome.
Figure 3. Impingement
The circulation of blood to the tendon also depends on muscle tension. In the tendon, circulation will be inversely proportional to the tension. At very high tension levels, circulation may cease completely. Recent studies have shown that the intramuscular pressure in the supraspinous muscle can exceed 30 mm Hg at 30 degrees of forward flexion or abduction in the shoulder joint, as shown in figure 4. Impairment of blood circulation occurs at this pressure level. Since the major blood vessel supplying the supraspinous tendon runs through the supraspinous muscle, it is likely that the circulation of the tendon may even be disturbed at 30 degrees of forward flexion or abduction in the shoulder joint.
Figure 4. Raising the arm to different elevations and at different angles exerts different intramuscular pressures on the supraspinous muscle.
Because of these biomechanical effects, it is not surprising to find a high risk of shoulder tendon injuries among those who are involved in activities that require static contractions of the supraspinatus muscle or repetitive shoulder forward flexions or abductions. Welders, steel-platers and sewers are among the occupational groups whose work involves static tension of these muscles. Assembly line workers in the automotive industry, painters, carpenters and athletes such as swimmers are other occupational groups in which repetitive shoulder joint movements are performed.
In the degenerated tendon, exertion may trigger an inflammatory response to the debris of dead cells, resulting in an active tendinitis. Also, infection (e.g., viral, urogenital) or systemic inflammation may predispose an individual to reactive tendinitis in the shoulder. One hypothesis is that an infection, which makes the immune system active, increases the possibility of a foreign body response to the degenerative structures in the tendon.
Pathogenesis of osteoarthrosis
The pathogenesis of osteoarthrosis, OA, is not known. Primary (idiopathic) OA is the most common diagnosis in absence of predisposing factors such as previous fractures. If predisposing factors exist, the OA is termed secondary. There are disputes between those who claim (primary) OA to be a metabolic or genetic disorder and those who claim that cumulative mechanical trauma also may play a part in the pathogenesis of primary OA. Microfractures due to sudden impact or repetitive impact loading may be one pathogenic mechanism for load-related OA.
Management and Prevention
In this section, non-medical management of shoulder disorders is considered. A change of workplace design or change of work task is necessary if the tendinitis is considered to be due to high local shoulder load. A history of shoulder tendinitis makes a worker doing repetitive or overhead work susceptible to a relapse of tendinitis. Loading of the osteoarthritic joint should be minimized by ergonomic optimization of work.
Primary prevention
Prevention of work-related musculoskeletal disorders in the shoulder can be achieved by improving work postures, motions, material handling and work organization, and eliminating external hazardous factors such as hand-arm vibration or whole body vibration. A methodology that may be advantageous in improving ergonomic working conditions is participatory ergonomics, taking a macro-ergonomic approach.
- Work postures: Since compression of the shoulder tendons occurs at 30 degrees of arm elevation (abduction), work should be designed that allows the upper arm to be kept close to the trunk.
- Motions: Repetitive arm elevations may trigger shoulder tendinitis, and work should be designed to avoid highly repetitive arm motions.
- Material handling: Handling of tools or objects may cause severe loading on shoulder tendons and muscles. Hand-held tools and objects should be kept at the lowest weight feasible and should be used with supports to assist in lifting.
- Work organization: Work organization should be designed to allow pauses and rests. Vacations, rotations and job enlargement are all techniques which may avoid repetitive loading of single muscles or structures.
- External factors: Impact vibration and other impacts from power tools may cause strain on both tendons and joint structures, increasing risk of osteoarthrosis. Vibration levels of power tools should be minimized and impact vibration and other types of impact exposure avoided by using different types of support or levers. Whole-body vibrations may cause reflectory contractions of shoulder muscles and increase the load on the shoulder.
- Participatory ergonomics: This method involves workers themselves in defining the problems, and solutions, and in the evaluation of the solutions. Participatory ergonomics starts from a macro-ergonomic view, involving analysis of the whole production system. Results of this analysis might lead to large-scale changes in production methods that could increase health and safety as well as profit and productivity. The analysis could lead to smaller-scale changes as well, such as in workstation design.
- Preplacement examinations: Current available information does not support the idea that preplacement screening is effective in reducing the occurrence of work-related shoulder disorders.
- Medical control and surveillance: Surveillance of shoulder symptoms is readily carried out using standardized questionnaires and inspection walk-throughs of workplaces.
Elbow
Epicondylitis
Epicondylitis is a painful condition which occurs at the elbow, where muscles which permit the wrist and fingers to move, meet the bone. When this painful condition occurs on the outside it is called tennis elbow (lateral epicondylitis). When it occurs on the inside of the elbow bend, it is called golfer’s elbow (medial epicondylitis). Tennis elbow is a fairly common disease in the general population, and in some studies high occurrence has been observed in some occupational groups with hand-intensive tasks (table 1); it is more common than medial epicondylitis.
Table 1. Incidence of epicondylitis in various populations.
|
Study population |
Rate per 100 person-years |
Reference |
|
5,000 workers of diverse trades |
1.5 |
Manz and Rausch 1965 |
|
15,000 subjects of a normal population |
<1.0 |
Allander 1974 |
|
7,600 workers of diverse trades |
0.6 |
Kivi 1982 |
|
102 male meatcutters |
6.4 |
Kurppa et al. 1991 |
|
107 female sausage makers |
11.3 |
Kurppa et al. 1991 |
|
118 female packers |
7.0 |
Kurppa et al. 1991 |
|
141 men in non-strenuous jobs |
0.9 |
Kurppa et al. 1991 |
|
197 women in non-strenuous jobs |
1.1 |
Kurppa et al. 1991 |
Epicondylitis is thought to be caused by repetitive and forceful exertions of the wrist and fingers; controlled studies have, however, given contradictory results concerning the role of hand- intensive tasks in the development of the disease. Trauma can also play a role, and the proportion of cases occurring after trauma has ranged from 0 to 26% in different studies. Epicondylitis usually occurs in people aged 40 years and older. The disease is rare under the age of 30. Little is known of other individual risk factors. A common view about the pathology is that there is a tear at the insertion of the muscles. Symptoms of epicondylitis include pain, especially during exertion of the hand and wrist, and gripping with the elbow extended may be extremely painful.
There are various concepts of the pathogenesis of epicondylitis. The duration of epicondylitis is usually from some weeks to some months, after which there is usually complete recovery. Among workers with hand-intensive tasks the length of sick-leave due to epicondylitis has usually been about or slightly over two weeks.
Olecranon Bursitis
Olecranon bursitis is an inflammation of a liquid-filled sac on the dorsal side of the elbow (olecranon bursa). It may be caused by repeated mechanical trauma (traumatic or “student’s” bursitis). It may also be due to infection or associated with gout. There is local swelling and wavelike motion on palpation due to accumulation of fluid in the bursa. When there is raised skin temperature, an infectious process (septic bursitis) is suggested.
Osteoarthrosis
Osteoarthrosis or degenerative disease that results from a breakdown of cartilage in the elbow is rarely observed in people under the age of 60. However, an excess prevalence of osteoarthrosis has been found among some occupational groups whose work includes intensive use of hand tools or other heavy manual work, such as coal miners and road construction workers. Valid studies with no excessive risk in such occupations have also been reported, however. Elbow arthrosis has also been associated with vibration, but it is believed that osteoarthrosis of the elbow is not specific to vibration.
The symptoms include local pain, first during movement and later also during rest, and limitation of the range of motion. In the presence of loose bodies in the joint, locking of the joint may occur. Loss of the ability to extend the joint completely is especially disabling. Abnormalities seen on x rays include the growth of new bone tissue at the sites where ligaments and tendons meet the bone. Sometimes loose pieces of cartilage or bone can be seen. Damage to the joint cartilage may result in destruction of the underlying bone tissue and deformation of joint surfaces.
The prevention and treatment of elbow osteoarthrosis emphasize optimizing work load by improving tools and work methods to decrease the mechanical loads imposed on the upper limb, and minimizing exposure to vibration. Active and passive movement therapy may be used in order to minimize restrictions in the range of motion.
More...
Forearm, Wrist and Hand
Tenosynovitis and Peritendinitis
Wrist and finger extensors and flexors
In the wrist and hand the tendons are surrounded by tendon sheaths, which are tubular structures containing fluid to provide lubrication and protection for the tendon. An inflammation of the tendon sheath is called tenosynovitis. Inflammation of the site where the muscle meets the tendon is called peritendinitis The location of wrist tenosynovitis is at the tendon sheath area in the wrist, and the location of peritendinitis is above the tendon sheath area in the forearm. Insertion tendinitis denotes an inflammation of the tendon at the site where it meets the bone (figure 1).
Figure 1. The muscle-tendon unit.
The terminology for the diseases of the tendon and its adjacent structures is often used loosely, and sometimes “tendinitis” has been used for all painful conditions in the forearm-wrist-hand region, regardless of the type of clinical appearance. In North America an umbrella diagnosis “cumulative trauma disorder” (CTD) has been used for all upper extremity soft tissue disorders believed to be caused, precipitated or aggravated by repetitive exertions of the hand. In Australia and some other countries, the diagnosis of “repetitive strain injury” (RSI) or “overuse injury” has been used, while in Japan the concept of “occupational cervicobrachial disorder” (OCD) has covered soft-tissue disorders of the upper limb. The two latter diagnoses include also shoulder and neck disorders.
The occurrence of tenosynovitis or peritendinitis varies widely according to the type of work. High incidences have been reported typically among manufacturing workers, such as food-processing workers, butchers, packers and assemblers. Some recent studies show that high incidence rates exist even in modern industries, as shown in table 1. Tendon disorders are more common on the back side than on the flexor side of the wrist. Upper extremity pain and other symptoms are prevalent also in other types of tasks, such as modern keyboard work. The clinical signs that keyboard workers present are, however, rarely compatible with tenosynovitis or peritendinitis.
Table 1. Incidence of tenosynovitis/peritendinitis in various populations.
|
Study population |
Rate per 100 person-years |
Reference |
|
700 Muscovite tea packers |
40.5 |
Obolenskaja and Goljanitzki 1927 |
|
12,000 car factory workers |
0.3 |
Thompson et al. 1951 |
|
7,600 workers of diverse trades |
0.4 |
Kivi 1982 |
|
102 male meatcutters |
12.5 |
Kurppa et al. 1991 |
|
107 female sausage makers |
16.8 |
Kurppa et al. 1991 |
|
118 female packers |
25.3 |
Kurppa et al. 1991 |
|
141 men in non-strenuous jobs |
0.9 |
Kurppa et al. 1991 |
|
197 women in non-strenuous jobs |
0.7 |
Kurppa et al. 1991 |
Frequent repetition of work movements and high force demands on the hand are powerful risk factors, especially when they occur together (Silverstein, Fine and Armstrong 1986). Generally accepted values for acceptable repetitiveness and use of force do not, however, yet exist (Hagberg et al. 1995). Being unaccustomed to hand-intensive work, either as a new worker or after an absence from work, increases the risk. Deviated or bent postures of the wrist at work and low environmental temperature have also been considered as risk factors, although the epidemiological evidence to support this is weak. Tenosynovitis and peritendinitis occur at all ages. Some evidence exists that women might be more susceptible than men (Silverstein, Fine and Armstrong 1986). This has, however, been difficult to investigate, because in many industries the tasks differ so widely between women and men. Tenosynovitis may be due to bacterial infection, and some systemic diseases such as rheumatoid arthritis and gout are often associated with tenosynovitis. Little is known about other individual risk factors.
In tenosynovitis the tendon sheath area is painful, especially at the ends of the tendon sheath. The movements of the tendon are restricted or locked, and there is weakness in gripping. The symptoms are often worst in the morning, and functional ability improves after some activity. The tendon sheath area is tender on palpation, and tender nodes may be found. Bending of the wrist increases pain. The tendon sheath area may also be swollen, and bending the wrist back and forth may produce crepitation or crackling. In peritendinitis, a typical fusiform swelling is often visible on the backside of the forearm.
Tenosynovitis of the flexor tendons at the palmar aspect of the wrist may cause entrapment of the median nerve as it runs through the wrist, resulting in carpal tunnel syndrome.
The pathology at an acute stage of the disease is characterized by the accumulation of fluid and a substance called fibrin in the tendon sheath in tenosynovitis, and in the paratenon and between the muscle cells in peritendinitis. Later, cell growth is noticed (Moore 1992).
It should be emphasized that tenosynovitis or peritendinitis that is clinically identifiable as occupational is found in only a minor proportion of cases of wrist and forearm pain among working populations. The majority of workers first seek medical attention with the symptom of tenderness to palpation as the sole clinical finding. It is not fully known whether the pathology in such conditions is similar to that in tenosynovitis or peritendinitis.
In the prevention of tenosynovitis and peritendinitis, highly repetitive and forceful work movements should be avoided. In addition to attention to work methods, work organizational factors (the quantity and pace of work, pauses and work rotation) also determine the local load imposed on the upper limb, and the possibility of introducing variability to work by affecting these factors should be considered as well. New workers and workers returning from a leave or changing tasks should be gradually accustomed to repetitive work.
For industrial workers with hand-intensive tasks, the typical length of sick leave due to tenosynovitis or peritendinitis has been about ten days. The prognosis of tenosynovitis and peritendinitis is usually good, and most workers are able to resume their previous work tasks.
De Quervain’s tenosynovitis
De Quervain’s tenosynovitis is a stenosing (or constricting) tenosynovitis of the tendon sheaths of the muscles that extend and abduct the thumb at the outer aspect of the wrist. The condition occurs in early childhood and at any age later. It may be more common among women than among men. Prolonged repetitive movements of the wrist and blunt trauma have been suggested as causative factors, but this has not been epidemiologically investigated.
The symptoms include local pain at the wrist and weakness of grip. The pain may sometimes extend into the thumb or up into the forearm. There is tenderness and eventual thickening on palpation at the constriction site. Sometimes nodular thickening may be visible. Bending the wrist towards the little finger with the thumb flexed in the palm (Finkelstein’s test) typically exacerbates the symptoms. Some cases show triggering or snapping upon moving the thumb.
The pathological changes include thickened outer layers of the tendon sheaths. The tendon may be constricted and show enlargement beyond the site of constriction.
Stenosing tenosynovitis of the fingers
The tendon sheaths of the flexor tendons of the fingers are held close to the joint axes by tight bands, called pulleys . The pulleys may thicken and the tendon may show nodular swelling beyond the pulley, resulting in stenosing tenosynovitis often accompanied by painful locking or triggering of the finger. Trigger finger or trigger thumb have been used to denote such conditions.
The causes of trigger finger are largely unknown. Some cases that occur in early childhood are likely to be congenital, and some seem to appear after trauma. Trigger finger has been postulated to be caused by repetitive movements, but no epidemiological studies to test this have been carried out.
The diagnosis is based on local swelling, eventual nodular thickening, and snapping or locking. The condition is often encountered in the palm at the level of the metacarpal heads (the knuckles), but may occur also elsewhere and in multiple sites.
Osteoarthrosis
The prevalence of radiographically detectable osteoarthrosis in the wrist and hand is rare in the normal population under the age of 40, and is more common among men than women (Kärkkäinen 1985). After the age of 50, hand arthrosis is more prevalent among women than among men. Heavy manual labour with and without exposure to low-frequency (below 40 Hz) vibration have been associated, although not consistently, with excess prevalence of osteoarthrosis in the wrist and hand. For higher frequencies of vibration, no excess joint pathology has been reported (Gemne and Saraste 1987).
Osteoarthrosis of the first joint between the base of the thumb and the wrist (carpometacarpal joint) occurs fairly commonly among the general population and is more common among women than men. Osteoarthrosis is less common in the knuckles (metacarpo-phalangeal joints), with the exception of the meta- carpophalangeal joint of the thumb. Aetiology of these disorders is not well known.
Osteoarthrotic changes are common in the joints closest to the fingertip (distal interphalangeal joints of fingers), in which the age-adjusted prevalence of radiographically detectable changes (mild to severe) in different fingers varies between 9 and 16% among the men and 13 and 22% among the women of a normal population. Distal interphalangeal osteoarthrosis can be detected by clinical examination as nodular outgrowths on the joints, called Heberden’s nodes. In a Swedish population study among 55-year-old women and men, Heberden’s nodes were detected in 5% of men and 28% of women. Most subjects showed changes in both hands. The presence of Heberden’s nodes showed a correlation with heavy manual labour (Bergenudd, Lindgärde and Nilsson 1989).
Joint load associated with the manipulation of tools, repetitive movements of the hand and arm possibly together with minor traumatization, loading of the joint surfaces in extreme postures, and static work have been considered as possible causative factors for wrist and hand osteoarthrosis. Although osteoarthrosis has not been considered specific to low-frequency vibration, the following factors might play a role as well: damage of the joint cartilage from shocks from the tool, additional joint load associated with a vibration- induced increase in the need for joint stabilization, the tonic vibration reflex and a stronger grip on the tool handle induced when sensitivity to touch is diminished by vibration (Gemne and Saraste 1987).
The symptoms of osteoarthrosis include pain during movement in the initial stages, later also during rest. Limitation of motion in the wrist does not markedly interfere with work activities or other activities of daily living, whereas osteoarthrosis of the finger joints may interfere with gripping.
To avoid osteoarthrosis, tools should be developed that help to minimize heavy manual labour. Vibration from tools should be minimized as well.
Compartment Syndrome
The muscles, nerves and blood vessels in the forearm and hand are located in specific compartments limited by bones, membranes and other connective tissues. Compartment syndrome denotes a condition in which the intracompartmental pressure is constantly or repeatedly increased to a level at which the compartmental structures may be injured (Mubarak 1981). This may occur after trauma, such as fracture or crush injury to the arm. Compartment syndrome after strenuous exertion of the muscles is a well-known disease in the lower extremity. Some cases of exertional compartment syndrome in the forearm and hand have also been described, although the cause of these conditions is not known. Neither have generally accepted diagnostic criteria nor indications for treatment been defined. The afflicted workers have usually had hand-intensive work, although no epidemiological studies on the association between work and these diseases have been published.
The symptoms of compartment syndrome include tenseness of the fascial boundaries of the compartment, pain during muscle contraction and later also during rest, and muscle weakness. In clinical examination, the compartment area is tender, painful on passive stretching, and there may be diminished sensitivity in the distribution of the nerves running through the compartment. Intracompartmental pressure measurements during rest and activity, and after activity, have been used to confirm the diagnosis, but full agreement on normal values does not exist.
Intracompartmental pressure increases when the volume of the contents increases in the rigid compartment. This is followed by an increase in venous blood pressure, a decrease in the arterial and venous blood pressure difference which in turn affects blood supply of the muscle. This is followed by anaerobic energy production and muscle injury.
The prevention of exertional compartment syndrome includes avoiding or restricting the activity causing the symptoms to a level that can be tolerated.
Ulnar Artery Thrombosis(Hypothenar Hammer Syndrome)
The ulnar artery may undergo damage and subsequent thrombosis and occlusion of the vessel in the Guyon’s canal on the inner (ulnar) aspect of the palm. A history of repeated trauma to the ulnar side of the palm (hypothenar eminence), such as intensive hammering or using the hypothenar eminence as a hammer, has often preceded the disease (Jupiter and Kleinert 1988).
The symptoms include pain and cramping and cold intolerance of the fourth and fifth fingers. Neurological complaints may also be present, such as aching, numbness and tingling, but the performance of the muscles is usually normal. On clinical examination, coolness and blanching of the fourth and fifth fingers may be observed, as well as nutritional changes of the skin. The Allen’s test is usually positive, indicating that after compressing the radial artery, no blood flows to the palm via the ulnar artery. A palpable tender mass may be found in the hypothenar region.
Dupuytren’s Contracture
Dupuytren’s contracture is a progressive shortening (fibrosis) of the palmar fascia (connective tissue joining the flexor tendons of the fingers) of the hand, leading to permanent contracture of the fingers in a flexion posture. It is a common condition in people of North-European origin, affecting about 3% of the general population. The prevalence of the disease among the men is twice that among the women, and may be as high as 20% among males aged over 60. Dupuytren’s contracture is associated with epilepsy, type 1 diabetes, alcohol consumption and smoking. There is evidence for an association between vibration exposure from hand-held tools and Dupuytren’s contracture. The presence of the disease has been associated also with single injury and heavy manual labour. Some evidence exists to support an association between heavy manual work and Dupuytren’s contracture, whereas the role of single injury has not been adequately addressed (Liss and Stock 1996).
The fibrotic change appears first as a node. Later the fascia thickens and shortens, forming a chordlike attachment to the digit. As the process progresses, the fingers turn to permanent flexion. The fifth and fourth fingers are usually affected first, but other fingers also may be involved. Knuckle pads may be seen on the back side of the digits.
Wrist and Hand Ganglia
A ganglion is a soft, liquid-filled small sac; ganglia represent the majority of all soft tissue tumours of the hand. Ganglia are common, although the prevalence in populations is not known. In clinical populations, women have shown a higher prevalence than men, and both children and adults have been represented. Controversy exists on the causes of ganglia. Some consider them inborn while others believe that acute or repeated trauma play a role in their development. Different opinions exist also on the development process (Angelides 1982).
The most typical location of the ganglion is at the outer aspect of the back of the wrist (dorsoradial ganglion), where it can present as a soft, clearly visible formation. A smaller dorsal ganglion may not be noticeable without flexing the wrist markedly. The volar wrist ganglion (at the palmar aspect of the wrist) is typically located on the outer side of the tendon of the radial flexor of the wrist. The third commonly occurring ganglion is located at the pulley of the finger flexor tendon sheath at the level of the knuckles. A volar wrist ganglion may cause entrapment of the median nerve in the wrist, resulting in carpal tunnel syndrome. In rare cases a ganglion may be located in the ulnar canal (Guyon’s canal) in the inner palm and cause entrapment of the ulnar nerve.
The symptoms of wrist ganglia include local pain typically during exertion and deviated postures of the wrist. The ganglia in the palm and fingers are usually painful during gripping.
Disorders of Motor Control of the Hand(Writer’s Cramp)
Tremor and other uncontrolled movements may disturb hand functions which demand high precision and control, such as writing, assembly of small parts and playing musical instruments. The classical form of the disorder is writer’s cramp . The occurrence rate of writer’s cramp is not known. It affects both sexes and seems to be common in the third, fourth and fifth decades.
The causes of writer’s cramp and the related disorders are not fully understood. A hereditary predisposition has been suggested. The conditions are nowadays considered as a form of task-specific dystonia. (Dystonias are a group of disorders characterized by involuntary sustained muscle contractions, causing twisting and repetitive movements, or abnormal postures.) Pathological evidence of brain disease has not been reported for patients with writer’s cramp. Electrophysiological investigations have revealed abnormally prolonged activation of muscles involved in writing, and excess activation of those muscles that are not directly involved with the task (Marsden and Sheehy 1990).
In writer’s cramp, usually painless muscle spasm appears immediately or shortly after starting to write. The fingers, wrist and hand may assume abnormal postures, and the pen is often gripped with excessive force. The neurological status may be normal. In some cases an increased tension or tremor of the affected arm is observed.
Some of the subjects with writer’s cramp learn to write with the non-dominant hand, and a small proportion of these do develop cramp in the non-dominant hand as well. Spontaneous healing of writer’s cramp is rare.
Hip and Knee
The hip joint is a ball-and-socket joint surrounded by ligaments, strong muscles and bursae. The joint is weight bearing and has both high intrinsic stability and a wide range of motion. In young people pain in the hip region usually originates in the muscles, tendon insertions or bursae, while in older people, osteoarthrosis is the predominant disorder causing hip pain.
The knee is a weight-bearing joint that is important for walking, standing, bending, stooping and squatting. The knee is rather unstable and depends for support on ligaments and strong muscles as shown in figure 1. There are two joints in the knee, the femorotibial and the femoropatellar. On both inner and outer side of the joint there are strong ligaments, and in the centre of the femorotibial joint are the cruciate ligaments, which give stability and assist in the normal mechanical function of the knee. The menisci are curved, fibrocartilaginous structures that lie between the femoral (femoral condyles) and the tibial bones (tibial plateau). The knee joint is both stabilized and empowered by muscles that originate above the hip joint and at the shaft of the femur and are inserted upon bony structures below the knee joint. Around the knee joint there is a synovial capsule, and the joint is protected by several bursae.
Figure 1. The knee.
All these structures are easily hurt by trauma and overuse, and medical treatment for knee pain is rather common. Osteoarthrosis of the knee is a common disorder among the elderly, leading to pain and disability. In younger people, patellar bursitis and patellofemoral pain syndromes like a painful pes anserinus are rather common.
Osteoarthrosis
Osteoarthrosis (OA) is a common degenerative joint disorder in which the cartilage is more or less destroyed and the structure of the underlying bone is affected. Sometimes it is accompanied by few symptoms, but usually OA causes suffering, changes in ability to work and a decreased quality of life. Changes in the joint can be seen on x ray, and an OA sufferer usually seeks medical care because of pain, which is present even at rest, and a diminished range of motion. In severe cases, the joint may become totally stiff, and even destroyed. Surgery to replace a destroyed joint and replace it with a prosthesis is well developed today.
Studying the causes of osteoarthrosis of the hip is difficult. The onset of the disorder is usually hard to pinpoint; the development is usually slow and insidious (that is, one doesn’t necessarily know it is happening). The end point, for research purposes, can be different things, varying from slight changes in x rays to symptomatic disorders that require surgery. Indeed the end points used to identify the condition may differ because of different traditions in different countries, and even between different clinics in the same town. These factors cause problems in the interpretation of research studies.
Epidemiological research tries to identify associations between exposures such as physical load, and outcomes, such as osteo-arthrosis. When combined with other knowledge, it is possible to find associations that could be considered causal, but the cause-effect chain is complicated. Osteoarthrosis is common in every population, and one must remember that the disorder exists among persons with no known hazardous exposure, while there are healthy subjects in the group with high and well-known harmful exposure. Unknown paths between exposure and disorder, unknown health factors, genetics and selection forces may be a few of the contributors to that.
Individual risk factors
Age: The occurrence of arthrosis increases with age. X-ray investigations of osteoarthrosis of different joints, mainly the hip and the knee, have been made in different populations and the prevalences found to vary. The explanation might be ethnic differences or variations in investigation techniques and diagnostic criteria.
Congenital and developmental diseases and changes: Early changes in the joint, such as congenital malformations, those caused by infections and so on, lead to an earlier and faster progression of osteoarthrosis of the hip. Knock-knees (varus) and bandy-legs (valgus) put an uneven distribution of forces on the knee joint, for example, which can have some importance for arthrosis development.
Heredity: Hereditary factors are present for osteoarthrosis. For example, osteoarthrosis of the hip is a rare disease among people of Asian origin but more common among Caucasians, which suggests a hereditary factor. Osteoarthrosis in three or more joints is called generalized osteoarthrosis and has a hereditary pattern. The hereditary pathway for osteoarthrosis of the knee is not very well known.
Overweight: Overweight can probably cause osteoarthrosis of the knee and hip. The relationship between overweight and knee osteoarthrosis has been shown in large epidemiological studies of the general population, such as the National Health and Nutrition Examination Survey (NHANES) and Framingham study in the United States. The association was strongest for women but existed even for men (Anderson and Felson 1988; Felson et al. 1988).
Trauma: Accidents or causes of trauma or injury, especially those that interfere with the mechanics and circulation of the joint and ligament, can give rise to an early osteoarthrosis.
Sex and oestrogen use: Osteoarthrosis of the hip and knee seems to be equally distributed among men and women. From a study on female participants in the Framingham study, it was concluded that oestrogen use in women is associated with a modest but insignificant protective effect against osteoarthrosis of the knee (Hannan et al. 1990).
Mechanical load
Experimental studies in monkeys, rabbits, dogs and sheep have shown that compression forces on a joint, especially when it is held in an extreme position, with or without simultaneous shifting loads, can lead to changes in the cartilage and bone similar to those of osteoarthrosis in human beings.
Sports activities: Participation in sports can increase the load on different joints. The risk of trauma is also increased. On the other hand, however, good muscle function and coordination are developed at the same time. Few data are available as to whether participating in sports prevents trauma or is harmful to the joints. Data drawn from good scientific studies are very limited, and some are described here. Several studies of soccer players have shown that both professionals and amateurs have more osteoarthrosis of the hip and knee than the general male population. For example, one Swedish study of 50- to 70-year-old men with a severe osteoarthrosis who were compared with healthy men in the same age group, showed that the men with osteoarthrosis had been more heavily involved in sports activities in their youth. Track and field, racket sports, and soccer seemed to be most harmful (Vingård et al. 1993). In the scientific literature there are other studies that have not shown any differences between athletes and those who do not participate in sports. However most of them are performed on still active athletes and are thus not conclusive.
Workload factors
The aetiology of osteoarthrosis of the knee and hip is, as for all diseases, complex and multifactorial. Recent well-performed studies have shown that physical load on the joint from occupational exposures will play a role as a contributing cause for the development of premature osteoarthrosis.
Most epidemiological studies concerning physical workload are cross-sectional and carried out on occupational groups without making individual exposure assessments. These serious methodological problems make generalizing the results of such studies extremely difficult. Farmers have been found to have more osteoarthrosis of the hip than other occupational groups in several studies. In a Swedish study of 15,000 farmers, farmers’ wives and other farm workers were asked about past x-ray examinations in which the hip joint could be seen. Among the 565 men and 151 women who had been examined, hip joints were studied using the same criteria and the same investigator as in a population study from Sweden 1984. The distribution of osteoarthrosis of the hip among male farmers and the male population of Malmö is shown in table 1 (Axmacher and Lindberg 1993).
Table 1. Prevalence of primary osteoarthrosis of the hip among male farmers and population of different age groups in the city of Malmö.
|
Male farmers |
Male Malmö population |
|||||
|
Age group |
N |
Cases |
Prevalence |
N |
Cases |
Prevalence |
|
40–44 |
96 |
1 |
1.0% |
250 |
0 |
0.0% |
|
45–49 |
127 |
5 |
3.9% |
250 |
1 |
0.4% |
|
50–54 |
156 |
12 |
6.4% |
250 |
2 |
0.8% |
|
55–59 |
127 |
17 |
13.4% |
250 |
3 |
1.2% |
|
60–64 |
59 |
10 |
16.9% |
250 |
4 |
1.6% |
N = Number of men studied; cases = men with osteoarthrosis of the hip.
Source: Axmacher and Lindberg 1993.
In addition to farmers, construction workers, food-processing workers (grain-mill workers, butchers and meat preparers), firefighters, mail carriers, shipyard workers and professional ballet dancers have all been found to be at an increased risk of hip osteoarthrosis. It is important to realize that an occupational title alone does not adequately describe the stress on a joint—the same job type can mean different loads for different workers. Further, the load of interest in a study is the exact pressure placed on a joint. In a study from Sweden, physical workload has been quantified retrospectively through individual interviews (Vingård et al. 1991). Men with high physical load exposures due to their occupations up to the age of 49 had more than double the risk for developing osteoarthrosis of the hip compared to those with low exposure. Both dynamic exposures, such as heavy lifting, and static exposure, such as prolonged sitting in a twisted position, seemed to be equally harmful to the joint.
The risk of knee osteoarthrosis has been found to be increased in coal miners, dockers, shipyard workers, carpet and floor layers and other construction workers, firefighters, farmers and cleaners. Moderate to heavy physical demands at work, knee bending and traumatic injury increase the risk.
In another English study from 1968, dockers were found to have more osteoarthrosis of the knee than civil servants in sedentary occupations (Partridge and Duthie 1968).
In Sweden, Lindberg and Montgomery investigated workers in a shipyard and compared them to office workers and teachers (Lindberg and Montgomery 1987). Among shipyard workers 3.9% had gonarthrosis, compared to 1.5% among office workers and teachers.
In Finland, Wickström compared concrete reinforcement workers with painters, but no differences in disability from the knees were found (Wickström et al. 1983). In a later Finnish study, knee disorders in carpet and floor layers and painters were compared (Kivimäki, Riihimäki and Hänninen 1992). Knee pain, knee accidents, and treatment regimes for the knees, as well as osteophytes around the patella, were more common among carpet and floor layers than among the painters. The authors suggest that kneeling work increases the risk of knee disorders and that the changes observed in x rays might be an initial sign of knee degeneration.
In the United States, factors associated with osteoarthrosis of the knee in the first National Health and Nutrition Examination Survey (NHANES 1) were examined for a total of 5,193 men and women aged 35 to 74 years, 315 of whom had x-ray-diagnosed osteoarthrosis of the knee (Anderson 1988). In investigating occupational load the authors characterized the physical demands and knee-bending stress from occupational titles in US Department of Labor Dictionary of Occupational Titles. For both men and women, for those whose jobs were described as involving a lot of knee-bending, the risk for developing an osteoarthrosis of the knee was more than double that for those without such jobs. When controlling for age and weight in the statistical analysis, they found that 32% of the osteoarthrosis of the knee occurring in these workers was attributable to occupation.
In the Framingham study in the United States, subjects from Framingham, a town outside Boston, have been followed in an epidemiological study for more than 40 years (Felson 1990). Occupational status was reported for the years 1948–51 and 1958–61 and the results of x rays looking for radiographic osteo- arthrosis of the knee during the years 1983–85. Each subject’s job was characterized by its level of physical demand and whether the job was associated with knee-bending. This study also found that the risk for developing osteoarthrosis of the knee was doubled for those with a lot of knee bending and at least medium physical demands in their occupation.
In a study from California the roles of physical activity, obesity and knee injury on the development of severe osteoarthrosis of the knee was evaluated (Kohatsu and Schurman 1990). Forty-six people with gonarthrosis and 46 healthy people from the same community were studied. The persons with osteoarthrosis were two to three times more likely than the controls to have performed moderate to heavy work earlier in life and 3.5 times more likely to have been obese at the age of 20. They were almost five times more likely to have had a knee injury. There was no difference in the leisure time activities reported in the two groups.
In a register-based cohort study from Sweden (Vingärd et al. 1991) subjects born between 1905 and 1945, living in 13 of the 24 counties in Sweden in 1980 and reporting that they held the same blue-collar occupation in the censuses of 1960 and of 1970, were studied. The blue-collar occupations reported were then classified as to whether they were associated with high (more than average) or low (less than average) load on the lower extremity. During 1981, 1982 and 1983 it was determined whether the study population sought hospital care for osteoarthrosis of the knee. Firefighters, farmers and construction workers had an elevated relative risk among men to develop osteoarthrosis of the knee. Among women, cleaners were found to be at greater risk.
Chondromalacia patellae
A special case of osteoarthrosis is chondromalacia patellae, which often starts in the young. It is a degenerative change in the cartilage on the back of the patella bone. The symptom is pain in the knee, especially while bending it. Among sufferers, the patella is very tender when tapped, and especially if pressure is put on it. The treatment is quadriceps muscle training and, in severe cases, surgery. The connection to occupational activity is unclear.
Patellar bursitis
In the knee, there is a bursa between the skin and the patella. The bursa, which is a sac containing fluid, can be subject to mechanical pressure during kneeling and thus become inflamed. Symptoms are pain and swelling. A substantial amount of serous fluid can be aspirated from the bursa. This disorder is rather common among occupational groups that do a lot of kneeling. Kivimäki (1992) has investigated soft-tissue changes in the front of the knee using ultrasonography in two occupational groups. Among carpet and floor layers 49% had thickening of the prepatellar or superficial infrapatellar bursa, compared to 7% among painters.
Pes anserinus bursitis
The pes anserinus consists of the tendons of the sartorius, semimembranous and gracilis muscles at the inner aspect of the knee joint. Under the insertion point of these tendons, there is a bursa that can be inflamed. Pain is increased by forceful extension of the knee.
Trochanter bursitis
The hip has many bursae that surround it. The trochanteric bursa lies between the tendon of the gluteus maximus muscle and the posterolateral prominence of the greater trochanter (the other side of the hip). Pain in this area is usually called trochanter bursitis. Sometimes it is a true bursitis. The pain can radiate down the thigh and may simulate sciatic pain.
Theoretically it is possible that a special occupational posture can cause the disorder, but there are no scientific investigations.
Meralgia paresthetica
Meralgia paresthetica belongs to the entrapment disorders, and the cause is probably an entrapment of the nervus cutaneus femoris lateralis where the nerve comes out between muscles and fasciae above the edge of the pelvis (spina iliaca anterior superior). The sufferer will have pain along the front and lateral side of the thigh. The disorder can be rather tricky to cure. Different remedies, from pain killers to surgery, have been used with varying success. Since there are occupational exposures which cause pressure against the nerve, so this condition may be an occupational disorder. Anecdotal accounts of this exist, but there are no epidemiological investigations available that verify it.
Leg, Ankle and Foot
In general, pain is the main symptom of disorders of the leg, ankle and foot. It often follows exercise and may be aggravated by exercise. Muscle weakness, neurological deficiency, problems with fitting shoes, instability or stiffness of joints, and difficulties in walking and running are common problems in these disorders.
The causes of problems are usually multifactorial, but most often they arise from biomechanical factors, infections and/or systemic diseases. Foot, knee and leg deformities, bone and/or soft-tissue changes that follow an injury, excessive stress such as repetitive use, instability or stiffness and improper shoes are common causes of these symptoms. Infections may occur in the bony or soft tissues. Diabetes, rheumatic diseases, psoriasis, gout and blood circulation disturbances often lead to such symptoms in the lower limb.
Besides the history, a proper clinical examination is always necessary. Deformities, function disturbances, the blood circulation and the neurological state should be carefully examined. Analysis of gait may be indicated. Plain radiographs, CT, MRI, sonography, ENMG, vascular imaging and blood tests may contribute to the pathological and aetiological diagnosis and treatment.
Principles of treatment . The treatment should always be directed towards eliminating the cause. Except in traumas, the main treatment is usually conservative. The deformity will be, if possible, corrected by proper shoes and/or orthosis. Good ergonomic advice, including correction of wrong walking and running behaviour, is often beneficial. Diminishing of excessive loading, physiotherapy, anti-inflammatory drugs and in rare cases a short immobilization may be indicated. Redesign of work may be indicated.
Surgery may also be recommended in some acute traumas, especially for some persistent symptoms which have not benefited from conservative therapy, but specific medical advice is needed for each case.
Achilles Tendinitis
The disorder is usually due to overuse of the Achilles tendon, which is the strongest tendon in the human organism and is found in the lower leg/ankle. The tendon is exposed to excessive loading, especially in sports, resulting in pathological inflammatory and degenerative changes in the tendon and its surrounding tissues, bursae and paratenon. In severe cases a complete rupture may follow. Predisposing factors are improper shoes, malalignment and deformities of the foot, weakness or stiffness of the calf muscles, running on hard and uneven surfaces and intensive training. Achilles tendinitis occasionally occurs in some rheumatic diseases, after fractures of the crus or foot, in some metabolic diseases and following renal transplantation.
Pain and swelling in the region of the calcaneal tendon, the Achilles tendon, are rather common symptoms, especially in sportsmen. The pain is located in the tendon or its attachment to the calcaneum.
More men than women develop Achilles tendinitis. The symptoms are more frequent in recreational sports than in professional athletics. Running and jumping sports may especially lead to Achilles tendinitis.
The tendon is tender, often nodular, with swelling, and the tendon is fibrotic. Microruptures may be present. A clinical examination can be supported mainly by MRI and ultrasonography (US). MRI and US are superior to CT for demonstration of the region and quality of the soft-tissue changes.
Proper shoes in misalignment, orthotics, and advice in correct biomechanical training may prevent the development of Achilles tendinitis. When symptoms are present a conservative treatment is often successful: prevention of excessive training, proper shoes with heal lifts and shock absorption, physiotherapy, anti-inflammatory drugs, stretching and strengthening of the calf muscles.
Calcaneal Bursitis
Pain behind the heel, usually aggravated by walking, is often caused by a calcaneal bursitis, which frequently is associated with Achilles tendinitis. The disorder may be found in both heels and can occur at any age. In children, calcaneal bursitis is often combined with an exostosis or osteochondritis of the calcaneum.
In most cases improper footwear with narrow and hard back of the shoe is the cause of this disorder. In athletics excessive loading of the heel region, as in running, may provoke Achilles tendinitis and retrocalcaneal bursitis. A deformity of the back of the foot is a predisposing factor. There is usually no infection involved.
Upon examination, the tender heel is thickened and the skin may be red. There is often an inward bending of the hind part of the foot. Especially for differential diagnosis, radiographs are important and may reveal changes in the calcaneum (e.g., Sever’s disease, osteochondral fractures, osteophytes, bone tumours and osteitis). In most cases the history and the clinical examination will be supported by MRI or sonography. A retrocalcaneal bursogram can provide further insight into chronic cases.
The symptoms may subside without any treatment. In mild cases conservative treatment is usually successful. The painful heel should be protected with strapping and proper shoes with soft backs. An orthosis correcting the wrong position of the hind part of the foot may be valuable. A correction of the walking and running behaviour is often successful.
Surgical excision of the bursa and the impinging part of the calcaneum is indicated only when conservative treatment has failed.
Morton’s Metatarsalgia
Metatarsalgia is pain in the forefoot. It may be due to a neuroma of the plantar digital nerve, Morton’s neuroma. The typical pain is in the forefoot, usually radiating in the third and fourth toes, rarely in the second and third toes. The pain occurs on standing or walking at any age but is most frequent in middle-aged women. At rest the pain disappears.
The condition is often connected with flat forefoot and callosities. Compression of the metatarsal heads from side to side and of the space between the metatarsal heads may elicit pain. In plain radiographs the neuroma is not seen but other changes (e.g., bony deformities causing metatarsalgia) may be visible. MRI may reveal the neuroma.
Conservative treatment—proper shoes and pads—to support the anterior arch is often successful.
Tarsal Tunnel Syndrome
Burning pain along the sole of the foot and in all toes which may be due to compression of the posterior tibial nerve within the fibro-osseous tunnel under the flexor retinacle of the ankle, are all symptoms of tarsal tunnel syndrome. There are many conditions leading to compression of the nerve. The most common causes are bone irregularities, ankle fractures or dislocations, local ganglia or tumours, or bad footwear.
There may be loss of feeling in the areas where the medial and lateral plantar nerves lie, weakness and paralysis of foot muscles, especially the toe flexors, a positive Tinel’s sign and tenderness in the region of the nerve course.
A proper clinical examination of the function and the neurological and vascular state is essential. The syndrome may also be diagnosed by electrophysiological tests.
Compartment Syndromes of the Lower Limb
A compartmental syndrome is a result of prolonged high pressure of a closed intrafascial muscle space leading to markedly reduced blood circulation in the tissues. The high intracompartmental pressure is usually due to trauma (crush injuries, fractures and dislocations), but it will also result from overuse, from tumours and from infections. A tight cast may lead to a compartmental syndrome, as may diabetes and blood vessel disorders. The first symptoms are tense swelling, pain and curtailment of function which are not relieved when the leg is elevated, immobilized or treated with common drugs. Later on there will be paresthesia, numbness and paresis. In growing persons, a compartment syndrome may result in growth disturbances and deformities in the affected region.
If a compartment syndrome is suspected, a good clinical examination should be performed including that of the vascular, the neurological and the muscular state, the active and passive mobility of the joint and so on. Measurement of the pressure by multi-stick catheterization of the compartments should be performed. MRI, Doppler investigation and sonography may be helpful in the diagnosis.
Foot and Ankle Region Tenosynovitises
Of many symptoms in the foot, pain following tenosynovitis is rather common, especially in the ankle region and the longitudinal arch. The cause of the synovitis may be deformities of the foot, such as planovalgus, excessive stress, improper shoe fit, or sequelae to fractures and other injuries, rheumatological disorders, diabetes, psoriasis and gout. Synovitis may occur in many tendons, but the Achilles tendon is most often affected. Only rarely does tendinitis involve infection. A medical history and clinical examination are essential in the diagnosis of synovitis. Local pain, tenderness and painful movement are the main symptoms. Plain radiographs that show the bone changes and MRI, especially for changes in the soft tissues, are needed.
Ergonomic advice is needed. Proper shoes, correction of the walking and running habits and prevention of excessive stress situations on the job are usually beneficial. A short period of rest, immobilization in a cast and anti-inflammatory drugs are often indicated.
Hallux Valgus
Hallux valgus consists of extreme deviation of the first joint of the great toe towards the midline of the foot. It is often associated with other foot disorders (varus of the first metatarsal; flat foot, pes planotransversus or planovalgus). Hallux valgus may occur at any age, and it is seen more commonly in women than in men. The condition is in most cases familial, and it is often due to the wearing of improperly fitted shoes, such as ones with high heels and narrow pointed toe boxes.
The metatarsal joint is prominent, the first metatarsal head is enlarged, and there may be a (often inflamed) bursa bunion over the medial aspect of the joint in this condition. The great toe frequently overrides the second toe. The soft tissues of the toe are often changed due to the deformity. The range of extension and flexion of the metatarsophalangeal joint is usually normal, but it may be stiff due to osteoarthritis (hallux rigidus). In the vast majority of cases the hallux valgus is painless and requires no treatment. In some cases, however, hallux valgus causes shoe fitting problems and pain.
The treatment should be individualized according to the age of the patient, the degree of the deformity and the symptoms. Especially with adolescents and cases with mild symptoms, conservative treatment is recommended—proper shoes, insoles, pads to protect the bunion and so on.
Surgery is reserved especially for adult patients with severe shoe-fitting problems and pain, whose symptoms are not relieved by conservative treatment. The surgical procedures are not always successful, and therefore mere cosmetic factors should not be a real indication for surgery; but there is a great range of opinions regarding the usefulness of the approximately 150 different surgical procedures for hallux valgus.
Fascitis Plantaris
The sufferer feels pain under the heel, especially on long standing and walking. The pain radiates frequently to the sole of the foot. Plantar fascitis may occur at any age, but it is most frequent in middle-aged persons. The patients are often obese. It is also a rather common disorder in people who engage in sports. Often the foot has a flattened longitudinal arch.
There is local tenderness especially beneath the calcaneum at the attachment of the plantar fascia. All the fascia may be tender. On x ray a bony spur is seen in the calcaneum in about 50% of the patients, but it is also present in 10 to 15% of symptomless feet.
The causes of fascitis plantaris are not always clear. An infection, particularly gonorrhaea, rheumatoid arthritis and gout may cause the symptoms. Most frequently no specific diseases are connected to the condition. Increased pressure and tension of the fascia may be the main cause of the tenderness. The calcaneal spur may be a result of overusing of the fascia plantaris. It is probably not the primary cause of the calcaneal tenderness, because so many patients with those symptoms have no calcaneal spur and many with calcaneal spur are symptomless.
Other Diseases
Primary Fibromyalgia
The cause of fibromyalgia is not known. Some patients associate trauma and infections with the development of symptoms, but there is no hard evidence in favour of such triggering events. However, many factors are known to aggravate the existing symptoms. Cold, damp weather, mental disturbance, physical or mental stress, and also physical inactivity have all been associated with fibromyalgia (Wolfe 1986).
A major feature is patients waking up in the morning feeling tired. Abnormal serotonin metabolism is associated with both the sleep disturbance and decreased pain threshold typical in these patients (Goldberg 1987).
The symptoms of fibromyalgia start insidiously with persisting widespread musculoskeletal pains, multiple general symptoms such as fatigue, stiffness, subjective swelling of the fingers not observed by the examining physician, non-refreshing sleep and muscular pain after exertion. About one-third of the patients have additional symptoms, such as irritable bowel syndrome, tension headaches, premenstrual syndrome, numbness and tingling in the extremities, dryness of mouth and eyes and constriction of the blood vessels in the fingers when exposed to cold (Raynaud’s phenomenon).
Typically, a patient with fibromyalgia has a large variety of symptoms, which, with the exception of tender points, have no objective counterparts. Fibromyalgia runs a chronic course. Most of the patients continue to have symptoms with varying intensity. Complete remission is an exception. In primary fibromyalgia, no laboratory signs referring to inflammatory arthritis are present. Patients with inflammatory arthritis (e.g. rheumatoid arthritis) can also have fibromyalgic symptoms, in which case the term secondary fibromyalgia is applied.
There is no one test for fibromyalgia. The diagnosis of fibro- myalgia is based on the history of the patient and on the clinical observation of tender points (figure 1). The prevalence of fibro-myalgia in the general population is 0.5 to 1%. Most (75 to 90%) of the patients are women, usually between 25 and 45 years of age; children are rarely affected.
Figure 1. Tender point sites in fibromyalgia.
The American College of Rheumatology has set criteria for the classification of fibromyalgia (figure 2).
Figure 2. The American College of Rheumatology 1990 criteria for the diagnosis of fibromyalgia.
Diagnosis
Other ailments with similar symptoms must be excluded. Widespread pain must be present for at least three months. In addition there must be pain in 11 of the 18 tender point sites shown in figure 1 when pressed by an examiner’s finger.
Rheumatoid Arthritis
About 1% of the adult population has rheumatoid arthritis. The onset of the disease is usually at 30 to 50 years of age, with females having a threefold higher risk than males. The prevalence of the disease increases in older populations.
The cause of rheumatoid arthritis is not known. It is not inherited, but genetic factors increase the risk for the development of the disease. In addition to one or multiple genetic factors, some environmental triggering factors are thought to play a role in its pathogenesis, and viral or bacterial infections are heavily suspected.
Rheumatoid arthritis usually starts gradually. Typically, the patient has mild swelling of the small joints of fingers, and tenderness of the feet that manifests in a symmetrical fashion. If joints on one hand, for example, are involved it is likely that the same joints on the other hand will be affected. Stiffness of hands and feet in the morning is a major symptom. The patient often has fatigue and can have mild fever. Laboratory features include evidence of inflammation (elevated erythrocyte sedimentation rate and C-reactive protein level) and often mild anaemia. About 70% of the patients have circulating rheumatoid factor (autoantibody against IgG-class immunoglobulin). In early cases, radiological examination of hands and feet is often normal, but later on, most patients develop radiological evidence of joint destruction (erosions). The diagnosis of rheumatoid arthritis is based on a mixture of clinical, laboratory and radiological findings (see figure 3).
Figure 3. Criteris for the diagnosis of rheumatoid arthritis.
The diseases which most often cause differential diagnostic problems are degenerative joint diseases of the hands, arthritis following infections, spondylarthropathies, and some rare connective tissue diseases (Guidelines 1992).
Patient education to diminish the work-load of the joints, use of ergonomic appliances, good footwear, and proper treatment of infections form the basis of preventive measures. Treatment guidelines are given in table 1.
Table 1. Guidelines for the treatment of rheumatoid arthritis
|
1. |
Treatment of joint pain |
Nonsteroidal anti-inflammatory drugs Acetaminophen (Dextropropoxyphen) |
|
2. |
Treatment of joint inflammation (disease-modifying antirheumatic drugs) |
Intramuscular gold Sulfasalazine Auranofin Antimalarials D-penicillamine Methotrexate Azathioprine Cyclosporine (Cyclophosphamide) Glucocorticosteroid therapy |
|
3. |
Local injections |
Glucocorticosteroid Chemical synovectomy osmium tetroxide Injection of radioactive isotopes |
|
4. |
Surgery |
Early reparative surgery (synovectomy, tenosynovectomy) Reconstructive surgery |
|
5. |
Rehabilitation |
Occupational therapy Physiotherapy Education Evaluation of needs of aids and appliances |
Spondylarthropathies
Epidemiology and aetiology
Spondylarthropathies include typical clinical entities such as ankylosing spondylitis and some forms of arthritides associated with psoriasis, with chronic inflammatory bowel diseases, or with bacterial infections in the urogenital tract or in the gut (so called reactive arthritis). The diseases are common. The prevalence of the most chronic form, ankylosing spondylitis, in Western populations varies between 0.1 and 1.8% (Gran and Husby 1993). Three new cases of transient arthritis such as reactive arthritis compared to one patient with ankylosing spondylitis are estimated to occur annually in a population of 10,000. Most of the patients who develop spondylarthropathy are young adults, between 20 and 40 years of age. There is evidence that the mean onset of symptoms for patients with ankylosing spondylitis is increasing (Calin et al. 1988).
Spondylarthropathies have a strong genetic component since a majority of the patients have an inherited genetic marker, HLA-B27. The frequency of this marker is about 7 to 15% in Western populations; 90 to 100% of patients with ankylosing spondylitis and 70 to 90% of patients with reactive arthritis are HLA-B27 positive. However, at population levels, most of the subjects with this marker are healthy. Therefore, it is thought that exogenous factors, in addition to the genetic susceptibility, are needed for the development of the disease. Such triggering factors include bacterial infections in the urogenital tract or in the gut (table 2) skin lesions, and chronic inflammatory bowel diseases. The evidence in favour of infections is most direct in the case of reactive arthritis. Salmonella infections are widely increasing, as a sequel of which an increase in the cases with joint complications can be expected. Agriculture and poultry can be the sources of these infections. As to yersinia infections, pigs harbour yersinia bacteria in their tonsils. Slaughtering followed by storage of the meat products in the cold has been suggested to contribute to the dispersion of infections in humans. In patients with ankylosing spondylitis, however, usually no preceding infections can be traced as an initiating event. Recent results have, however, focused on the finding that patients with ankylosing spondylitis often have asymptomatic chronic gut inflammation, which could serve as a triggering factor or as a contributing inflammatory focus in the chronicity of the disease.
Table 2. Infections known to trigger reactive arthritis
|
Focus |
Bacteria |
|
Upper respiratory tract |
Chlamydia pneumoniae Beta-haemolytic streptococcus (usually causes rheumatic fever) |
|
Gut |
Salmonella Shigella Yersinia enterocolitica Yersinia pseudotuberculosis Campylobacter jejuni |
|
Urogenital tract |
Chlamydia trachomatis Neisseria gonorrhoeae |
Signs and symptoms
Peripheral arthritis is asymmetric, affects large joints, and has a predilection to low extremities. The patients often also have inflammatory low back pain, worse by night and relieved by movement, not by rest. A typical feature is a tendency to inflammation of the junction between tendons and bones (enthesopathy), which can manifest itself as pain under the heel or in calcaneus at the insertion of Achilles tendon. In addition to inflammation in the joints and at ligamentous insertions, patients also can have inflammatory symptoms in eyes (iritis or conjunctivitis), skin (psoriasis, skin lesions in palms, soles, or leg induration) and sometimes in the heart.
The following are the diagnostic criteria for spondylarthro- pathy (Dougados et al. 1991).
Inflammatory low back pain
or
Joint inflammation (synovitis):
- asymmetric
- predilection to low extremities
and
at least one of the following:
- positive family history for spondylarthropathy
- psoriasis
- inflammatory bowel disease
- buttock pain changing from side to side
- pain at the junction between tendon and bone (enthesopathy).
Patients with ankylosing spondylitis have low-back pain, worse by night, and tenderness between the spine and the pelvis at the sacroiliac joints. They can have limited mobility of the spine with chest tenderness. A third of the patients have peripheral arthritis and enthesopathy. The cornerstone of the diagnosis of ankylosing spondylitis is the presence of radiological changes in the sacroiliac joints; there is a loss of space between the joints, and bony outgrowths. Such changes add to the diagnostic accuracy of patients with spondylarthropathy but are necessary only in the case of ankylosing spondylitis.
Gout
Epidemiology and aetiology
Gout is a metabolic disorder that is the most common cause of inflammatory arthritis in men. Its prevalence among adults varies from 0.2 to 0.3 per 1000, and is 1.5% in adult males. The prevalence of gout increases with age and with increasing serum urate levels.
Hyperuricemia (high level of uric acid in serum) is a risk factor. Contributing factors are chronic kidney diseases which lead to renal insufficiency, hypertension, use of diuretic drugs, high alcohol intake, lead exposure and obesity. Gouty attacks are precipitated by hypersaturation of joint fluid with uric acid; the precipitated crystals irritate the joint, with the development of acute arthritis.
Signs and symptoms
The natural course of gout runs through several stages from a- symptomatic hyperuricemia to acute gouty arthritis, asymptomatic periods, and to chronic tophaceous gout (gout with nodules).
Acute gouty arthritis often manifests itself as an acute inflammation in one joint, usually at the base of the big toe. The joint is very tender, swollen and highly painful; it is often red. The acute attack can subside spontaneously within days. If untreated, repeated attacks can occur, and in some patients these continue (during the subsequent years) so that the patient develops chronic arthritis. In these patients, urate deposits can be observed in the ear helices, at the elbows, or at the Achilles tendons, where they form non-tender subcutaneous palpable masses (tophi).
Infectious Arthritis
Epidemiology and aetiology
In children, infectious arthritis often develops in a previously healthy child, but adults often have some predisposing factor, such as diabetes, chronic arthritis, use of glucocorticosteroid or immunosuppressive therapy, previous injections or trauma in the joint. Patients with endoprosthesis are also susceptible to infections in the operated joint.
Bacteria are most often the cause of infectious arthritis. In immunosuppressed patients, fungi can be found. Although bacterial infection in the joint is rare, it is very important to recognize, because, if untreated, the infection rapidly destroys the joint. The microbes can reach the joint by circulation (septic infection), by direct penetrating wound or during a joint injection, or from an adjacent infectious focus.
Signs and symptoms
In a typical case, a patient has acute joint inflammation, usually in one single joint, which is painful, hot, red and tender to movement. There are general symptoms of infection (fever, chills) and laboratory evidence of acute inflammation. The joint aspiration is turbid, and in microscopic examination a high number of white blood cells are seen, with positive stain and cultures for bacteria. The patient can have signs of a focus of infection elsewhere, such as pneumonia.
Osteoporosis
Epidemiology and aetiology
Bone mass increases from childhood until adolescence. Women gain 15% less bone density than men. It is at its highest between 20 and 40 years, after which there is a constant decrease. Osteoporosis is a condition in which bone mass decreases and bones become susceptible to fracture. Osteoporosis is a major cause of morbidity in the elderly. The most important manifestation is lumbar and hip fractures. About 40% of women who have reached 70 years have suffered from fractures.
Peak bone mass is influenced by genetic factors. In women, bone mass decreases after menopause. The decrease of bone mass in men is less distinct than in women. In addition to lack of oestrogen, other factors influence the rate of bone loss and the development of osteoporosis. These include physical inactivity, low amount of calcium in the diet, smoking, coffee consumption and low body weight. Use of systemic corticosteroid therapy is also associated with enhanced risk for osteoporosis.
Signs and symptoms
Osteoporosis can be asymptomatic. On the other hand, the most distinct manifestation of osteoporosis is bone fracture, typically that of the hip, vertebrae (spine) and wrist. Hip and wrist fractures usually are a result of falling, but vertebral fractures can develop insidiously after a trivial trauma. The patient has back pain, kyphosis and loss of height.
Bone Cancer
Epidemiology and aetiology
Primary malignant bone tumours are uncommon. They occur most often in children and young adults. Osteosarcoma is the most frequent of the malignant bone tumours. It is most frequently observed in the second decade of life, and in older adults it can result secondary to a bone disease (Paget’s disease). Ewing’s sarcoma is also mostly observed in children, who present with destructive changes in the pelvis or in the long bones. Malignant tumours originating from the cartilage (chondrosarcoma) can occur in many cartilage areas. In adults, malignant bone lesions are often metastatic (i.e., the primary malignant disease is somewhere else in the body).
Most malignant primary tumours have no known aetiology. However, Paget’s disease of bone, osteomyelitis, osteonecrosis and radiation injury have been associated with malignant transformation. Bone metastases are frequent in primary cancers of the breast, lung, prostate, kidney or thyroid gland.
Signs and symptoms
Pain, limitation of movement and swelling are present in patients with osteosarcoma. In addition to bone pain, patients with Ewing’s sarcoma often have systemic symptoms such as fever, malaise and chills. Chondrosarcomas can cause varying symptoms depending on the site of the tumour and its histologic details.
Osteomyelitis
Epidemiology and aetiology
Osteomyelitis is a bone infection that is usually bacterial, but can be fungal or viral. In an otherwise healthy person, osteomyelitis is a rare event, but in patients with chronic diseases such as diabetes or rheumatoid arthritis, infection in the body can spread by the bloodstream or by direct invasion to bones. In children, the most favoured site for the spreading is the shaft of long bone, but in adults the infection is often in the spine. A focal point from which an infection can spread by bloodstream or by direct invasion, penetrating or blunt trauma, prior orthopaedic surgery (insertion of prosthesis) can all be complicated by osteomyelitis.
Signs and symptoms
Acute bone infection of the long bones is associated with fever, chills and bone pain. Spinal osteomyelitis can cause more vague symptoms with progressive pain and low-grade fever. Infections around a prosthesis cause pain and tenderness when moving the operated joint.
" DISCLAIMER: The ILO does not take responsibility for content presented on this web portal that is presented in any language other than English, which is the language used for the initial production and peer-review of original content. Certain statistics have not been updated since the production of the 4th edition of the Encyclopaedia (1998)."